Abstract
Background
Obesity threatens to undo the improvements that have been made in life expectancy over the last two centuries. It disproportionately affects lower socioeconomic and ethnic minority groups and has become one of the most important global health challenges of the 21stcentury. Whilst obesity is not confined to city populations, cities are home to more than half of the world's population with concentrated groups at high risk of obesity. Cities have also long been the forefront of social and technological change that has led to our current obesogenic environment. The aim of this study was to systematically identify city-wide interventions to address obesity, from which recommendations for policy makers, health system leaders and political leaders in cities could be made.
Methods
Systematic review, conducted according to PRISMA guidelines, examining Embase, Ovid Medline, Central, Scopus, Campbell Library, CINALH, Health Business Elite; Health Management Information Consortium (HMIC), PyschINFO and Prospero. No restrictions on article type, date range or geographic location were applied. Along with classic academic sources, books and policy white papers were sought and reviewed. Studies that described a city-wide intervention to reduce obesity were included, irrespective of study design or perceived methodological quality. Only studies in English language were included. The primary outcome indicators that were sought and extracted were: reduction in obesity, reduction in weight and/or reduction in BMI. Where a primary outcome indicator was not stated, any other secondary impact measure was identified and recorded. This manuscript represents thematic analysis of a sub-set of data from the Prospero study, registration number: CRD42020166210
Findings
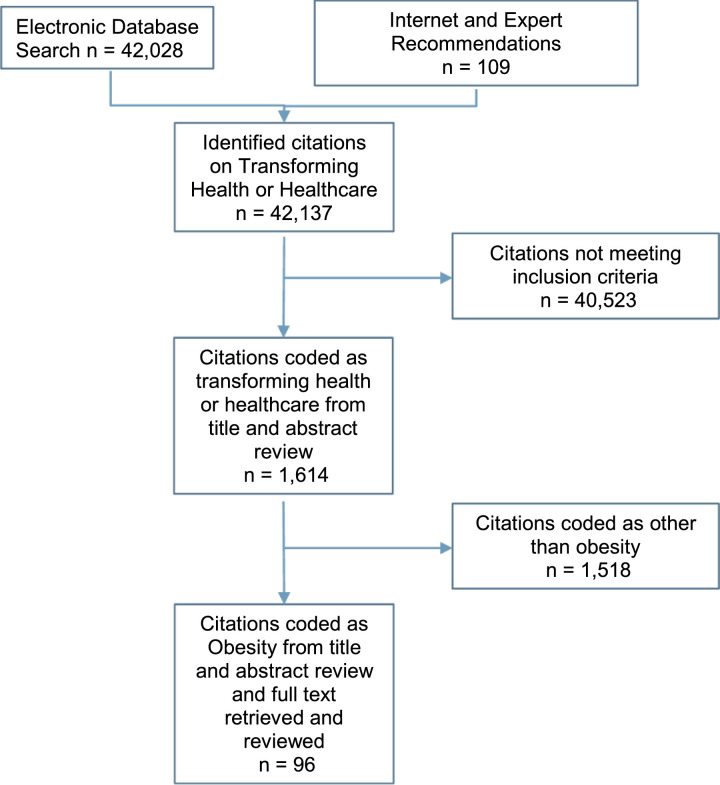
Our search yielded 42,137 original citations of which 1614 met the inclusion criteria and 96 were coded as relating to obesity. The 96 citations, ranging in year of publication 1997 to 2019, were conducted in 36 cities, with 13 citations either not stating a city or covering multiple cities, across 5 continents. The highest proportion of publications were from North America (59 / 96) and in particular the USA (56/96) and New York City (23/96). Primary outcome indicators were only stated in one quarter of the identified studies (24/96). Overall, there was heterogeneity of study design, descriptive methodologies and publication types, with a majority being descriptive texts using qualitative instruments of assessment.
Interpretation
Multi-level and multi-component interventions, at the individual, community and city level, done in concert, are needed to address obesity. A composite of interventions that cities can utilise to address obesity is provided. These interventions will also be beneficial to the environment and make the case that personal health and planetary health are inextricably linked and should be considered as one.
Funding
None
Keywords: City, Cities, Mayor, Obesity, Childhood obesity, Non-communicable disease, Wider determinants health, Improvement, Transformation
Research in Context.
Evidence before the study
The World Health Organization (WHO) estimates that more than 60% of global disease burden is the result of obesity related disorders. In this context, it is unsurprising there continues to be an increasing volume of research studies in the area of obesity. These studies include Cochrane reviews on interventions for preventing and treating obesity in children, adults, specific cohorts of the population and in specific settings. In addition, there are numerous systematic reviews on interventions for preventing obesity. and a significant number of studies covering individual city-wide interventions to address obesity, including the 96 studies found through this systematic review. There is a significant and growing body of evidence in respect of interventions to prevent and treat obesity.
Added value of the study
To our knowledge, this is the first systematic review of city-wide interventions to address obesity. Whilst obesity is not confined to city populations, cities are home to more than half of the world's population with concentrated groups at high risk of obesity. Therefore, a focus on city level interventions has the benefit of impact at scale on a significant number of the population that are disproportionately affected by obesity. This study adds to the literature by integrating identified studies to provide a comprehensive summary of city-wide interventions that cities have taken to address obesity. Using the evidence, the authors have produced a composite model of interventions that any city can consider within their local and national context when wanting to take action to reduce obesity.
Implications of all the evidence
Obesity is a global epidemic. There is emerging academic consensus that obesity is a complex problem that requires a multi-component and multidisciplinary approach. The interventions to address obesity do not provide quick fixes and there is a need for sustained focus and attention. The evidence from this systematic review demonstrates that multi-level, multi-component interventions carried out in concert, with the leadership of the Mayor (or equivalent city political leadership), give cities the best chance of reducing obesity.
Alt-text: Unlabelled box
Introduction
Obesity threatens to undo the gains that we have made in life expectancy over the last two centuries [1,2]. It has rapidly become a global epidemic; more than half the population is now overweight in 34 out of 36 OECD countries with almost one in four people with obesity [3]. The impact of obesity disproportionately affects lower socioeconomic and ethnic minority groups [[4], [5], [6], [7], [8]] and has broader short and long term consequences including; children who are overweight do less well at school, are up to three times more likely to be bullied, are more likely to miss school, and, when they grow up, are less likely to complete higher education [3] and five times more likely to have obesity as an adult and therefore likely to have associated health issues [6]. Obesity has become one of the most important global health challenges of the 21st century and yet is largely preventable [9].
The aim of this review was to systematically identify the interventions being taken by cities to reduce the prevalence of obesity and provide recommendations that will be useful to academics, policy makers, politicians, city health system managers and anyone interested in improving the health of city populations. Whilst obesity is not confined to city populations, cities are home to more than half of the world's population with concentrated groups at high risk of obesity [10]. Cities have long been at the forefront of social and technological change that has led to our current obesogenic environment [11]. Therefore, a focus on city level interventions brings the benefit of offering the ability to impact at scale on a significant number of the population that are disproportionately affected by obesity.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12]. The following databases were searched in March 2019 by one of the authors (SD); Embase and Embase classic; Ovid Medline ® in process and other non-indexed citations and Ovide Medline ® 1946-present; Central (Cochrane Central Register for controlled trials); Scopus; Campbell Library; CINALH; Health Business Elite; Health Management Information .Consortium (HMIC); PyschINFO; Prospero (Centre for Reviews and Dissemination). No date limitations were applied. Specific and pre-determined search terms were developed, tested and finalised for each database. These are available in the supplementary file Appendix A. The inclusion criteria was; city-wide interventions that aimed to transform health or healthcare. The definition of transformation, for the purposes of this research, was purposefully broad and includes any aim to improve health outcomes or healthcare services. The study was registered with PROSPERO (CRD42020166210). The data extracted was then coded to the issue it was seeking to address. The data used in this manuscript was the subset of data coded as relating to addressing obesity.
The inclusion criteria for this obesity subset was; city-wide interventions which had the primary purpose of supporting a reduction in obesity. The key factor was the study needed to state the intention was to address obesity; all interventions were included irrespective of how ambitious there were; all study design were included; the primary outcome indicators that were sought and extracted were: reduction in obesity, reduction in weight and/or reduction in BMI. Where it was uncertain whether the interventions was city-wide they were included. Studies that were an evaluation of how obesity has changed over time, without any description of an intervention, were excluded. Only studies in English language were included.
Predetermined data fields were agreed prior to data extraction. These were; date of publication; type of publication; intervention; how the intervention was implemented; city; city population; country; continent; quantitative outcome; authors qualitative conclusion. We developed a template (excel) for data extraction and analysis. Where any of this data was not presented, it was coded as ‘not stated’. Studies that did not name a specific city were still included as long as they indicated they were from a city. The authors carried out inductive thematic analysis in line with the guidelines of Braun and Clarke, [13] as it offered optimum flexibility and breadth. The source of study heterogeneity and necessary contextual information for interpreting the results have been highlighted through the document. The authors applied a modified thematic approach to this data to arrive at the composite of interventions. The reporting of this study conforms to the STROBE statement [14].
Role of the funding source
The was no funding associated with any element this study. The corresponding author had full access to all the data in the study. All authors had final responsibility for the decision to submit for publication and all authors approved the final version of the manuscript submitted for publication.
Results
The database search yielded 42,028 original citations after duplicates were removed through Endnote standard duplicate check. These electronic searches were augmented with an additional 109 citations found through expert recommendations or internet searches, giving a total of 42,137 original citations. These were assessed independently by SD and HLP1 against the inclusion criteria stated in the methods section. The level of inter-reviewer agreement on the articles was on average 96% (range 91%–98%) and resulted in 1614 citations meeting the inclusion criteria. The title and abstract of these 1614 citations were assessed and coded to the issue the intervention was seeking to address, with 96 papers being coded as seeking to address obesity and therefore included in this manuscript (Fig. 1).
Fig. 1.
PRISMA[12] Study Attrition Flow Chart.
The 96 citations, ranging in year of publication from 1997 to 2019, were conducted in 36 cities, with 13 citations either not stating a city or covering multiple cities, across 5 continents. The majority of the publications were from North America (59/96) with a high incidence from the USA (56/96) and New York City (23/96). Only one quarter of the identified studies (24/96) included one or more of the predefined outcome measures of: reduction in obesity, reduction in weight and/or reduction in BMI. Where the predefined outcome measure wasn't stated a secondary impact measure was sought and, where found, recorded. This secondary impact measure was any measure of impact provided in the article. There was heterogeneity of study design and reporting of impact, with a majority being descriptive texts using qualitative instruments of assessment. The full list of the 96 citations is available in the supplementary file Appendix B
Schools and child care settings
Interventions to address childhood obesity in schools and childcare settings provided the most citations (27 representing 28%). These included programmes of education and support for children, teachers, parents and caregivers on healthy eating and physical activity in a range of cities [[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31]], restricting unhealthy food provision and advertising around schools [24,32,33] and increasing the provision of free healthy school meals [34]. Two cities, New York [[35], [36], [37], [38], [39], [40], [41], [42], [43]] and Singapore [44,45] report a breadth of interventions within schools and child care settings.
Marketing and nutritional information labelling
Two cities, Amsterdam [28] followed by London [46], implemented city-wide unhealthy food advertising bans on public transport. Amsterdam went a step further and also banned unhealthy food and drinks sponsorship of sports events where more than 25% of the audience are children [28]. Two cities, New York City [47] and Philadelphia [48] mandated calorie labelling at fast food restaurants. Stevenson, a very small city (population 1200) in the USA, selected a grocery store as the location for a nutrition and food label education booth on the weekends [49].
Healthy food availability
Baltimore implemented a multi-level, multi component intervention to increase the availability and demand for healthier food, targeting low-income African American youth and their families [[50], [51], [52], [53], [54]]. Similarly, New York City implemented a number of interventions, from 2008 through to 2017, to improve healthy food availability and affordability. These included, mandatory nutritional standards for all food sold by city agencies (hospitals, prisons, aged care and health facilities) [55], providing zoning and financial incentives to heathy grocery stores in underserved communities [56] and launching 1000 mobile ‘Green Cart’ vendors selling only fruits and vegetables in more deprived neighbourhoods [57,58]. Philadelphia also targeted local stores with its ‘Healthy Corner Store Initiative, a public–private initiative, to support corner stores operating in food deserts [59]. Three cities, New York City [24], Charleston [60], and Michigan [59] implemented interventions around farmers markets. Whilst Carson (USA), implemented a healthy vending policy [61].
Restaurants and food outlets
Los Angeles took firm action in 2008 by banning new fast-food establishments for one year [62]. London took a more targeted approach by restricting unhealthy food within 400 m ‘super zones’ around schools [63]. New York City tried – and failed – to limit restaurant portion sizes of most sugar sweetened beverages and restrict consumption of sugar drinks purchased through the federal Supplemental Nutrition Assistance Program (SNAP), with the State court overturning the regulation one day before it was to take effect [64,65]. San Marco took a voluntary partnership approach to change children's menus through removing sugar-sweetened beverages and increasing fruit and vegetable offerings [66]. Baltimore implemented an intervention which promoted heather options with significantly increased healthy food items sales [67,68].
Education and support programmes (including media campaigns)
Education and support programme interventions ranged from very targeted and limited to a proportionately small number of people from the city [[69], [70], [71], [72], [73], [74], [75]] with only Moose Jaw [69,70], Sydney [73], Rockingham and Geraldton [76] and a US city (name not stated) [74] reporting a direct impact on weight of participants. Other interventions were on a much wider scale, aiming to impact the whole population. These included, Singapore's creative campaign to draw parents’ attention to their child's waistline which were placed all across Singapore [77], campaigns in New York City [78] and Philadelphia [79] to reduce sugar sweetened beverages. Liverpool [80] and Omaha [81] ran social marketing campaigns to challenge residents to lose weight and increase cycling, respectively. Fransen et al. [82] examined the Dutch cities of Nijmegen, Wijchen and Maasdriel and found there were numerous, ranging from 13 to 29, predominantly educational interventions in each city. The city of Oulu (Finland) introduced a cognitive behavioural based programme which was evaluated in a randomised clinical trial showing successful weight reduction [83]. The pioneer, in 1992, was the Dutch city of Alkmaar which lead on a community-based 'Fat Watch' campaign, which aimed for a 10% reduction in fat intake amongst the general population [84]. Cities have used their wider assets, such as professional sports teams, to promote and provide education and support programmes targeted at individuals who are overweight or have obesity [[85], [86], [87]].
Physical infrastructure to promote physical activity
Organisations in cities across Douglas County (Nebraska, USA) were supported to implement one or more policies to promote healthy eating or physical activity. In total, 952 individual policy changes, such as installing bike racks, were implemented [88]. Similarly, La Mesa (USA) made changes to the built environment to promote walking [24]. Somerville implemented community based environmental changes [89] with reported decreases in Body Mass Index (BMI) in males that were overweight or had obesity [[89], [90], [91]]. New York City [92] used legislation to change the way new buildings and renovations are designed, making stairways more visible and creating streetscapes. Indianapolis found that building recreation areas reduced the average weight of children from those areas [87]. Oklahoma City used the city's infrastructure development program to improve parks, sidewalks, trails, bike lanes, and sports facilities targeting neighbourhoods with high rates of heart disease [59,93]. In Atlanta Beltline (Georgia) they combined economic development with transportation planning and health to create new small businesses, housing, parks, and transit along 22 miles of repurposed trails [59]. Similarly, in Columbus (Ohio) they established ‘Columbus Healthy Places (CHP)’ to promote active travel through linking public health to urban planning [94]. Others looked to use the existing transport infrastructure. In Mexico City, motion sensors were installed in subway stations throughout the city and if commuters complete 10 squats they gained a free transport ticket [95]. In the Netherlands, a company called 'Wewatt' installs free bike riding stations that generate enough power to charge a phone [96]. These are available at stations and airports across the country and have since been replicated in France and Australia [96]. The Red Dear (Alberta) Primary Care Network invested in improving health not just treating ill health through working with the community and supporting ten outdoor gyms in city parks [97]. Other cities have temporarily changed the physical environment, such as, ‘Play Streets’ which is a popular intervention in many cities. It involves closing streets to traffic temporarily and opens up reclaimed space for children's play and physical activity [59].
Multi-component
Ten cities were identified that had taken a multicomponent approach. Multicomponent is defined as one or more interventions from two or more themes simultaneously. Each is worthy of a short description here. In Alexandria (Virginia (USA), a coordinated effort across school and pre-school facilities to increase active play; SNAP food stamps used at farmers’ markets; starting gardens, gardening and nutrition clubs; and inter-agency agreement on healthy vending machines and breastfeeding promotion [98]. In Geelong (Victoria, Australia), their Healthy Together Geelong programme implemented a number of systemic changes to address determinants of health to improve people's lives where they live, learn, work and play. Healthy Together Geelong is one of 12 prevention areas under the Victorian State Government's Healthy Together Victoria initiative which is a $100 m cluster randomised trial of a novel, 'whole system' intervention [99]. ‘The Healthy Auckland Together Programme’ in Auckland (New Zealand) is a collation of 26 organisations which provides resources to support people living in Auckland to eat well, live physically active lives and maintain a healthy body weight [100]. Nizwa City (Oman) took a community based approach which included; training for teachers in physical activities, building of gymnasiums and pathways for communities and awareness campaigns [101]. These four city case studies did not report an outcome measure.
In Amsterdam, the Healthy Weight Programme took a comprehensive whole systems approach, from which they report to have achieved a reduction in children that are overweight or have obesity from 21% to 18.5% and the number of overweight children fell by 12% between 2012–2015 [28,102,103]. Anchorage (Alaska) achieved similarly impressive results with a 5.4% decline in the overweight and obesity rates amongst children from 2004 to 2014 (2.2% relative decrease) through a range of interventions across the childcare and school settings and community action plans [104]. In Cambridge (USA) a multidisciplinary team developed and implemented Healthy Living Cambridge Kids (HLCK), a comprehensive multicomponent intervention targeting community, school, family, and individuals to mobilize environmental and policy interventions. BMI and obesity reduced modesty [105]. Philadelphia launched ‘Get Healthy Philly’, an initiative to improve the city's nutrition, physical activity, and tobacco environments by making healthy choices easier for all Philadelphians [106]. They achieved a 6.5% reduction in childhood obesity rates for students and achieved a larger reduction amongst children of colour (African Americans and Asians) than whites – the only city in the US to have achieved this [107]. In Seinajoki (Finland) they adopted a health in all policies approach with interventions across various settings (maternity clinics, day care centres, primary schools and after school clubs and community clubs). This resulted in 1 in 10 five year olds being overweight or having obesity in 2015 compared to 1 in 6 in 2009 [108,109]. Finally, after decades of increases in obesity, New York City saw obesity decline 5.5% between 2006 and 07 to 2010–11, through a comprehensive programme of activities [110,111].
Discussion
This systematic review identified 96 original citations across seven themes. Schools and childcare settings had the most studies (27), with the remaining being distributed across; education and support (20); multi-component (17); healthy food availability (11); physical infrastructure (11); restaurants and food outlets (6) and; marketing and nutritional information (4).
Schools and childcare settings are ideal for interventions to address obesity in children. However, individual school-based interventions show mixed results. Only three studies [16,20,22] reported a positive impact on reducing BMI, obesity prevalence or mean weight reduction. All of these four studies had multiple reinforcing interventions within this setting (i.e. they were not a simple single intervention).
Interventions in schools to prevent and treat obesity are important. This is unsurprising given schools represent a contained setting where children spend one third of their day. However, single interventions of a time bound period have less limited impact compared to a coherent suite of interventions that are consistently and relentlessly pursued.
There is mounting evidence of the importance of ‘first 1000 days [[112], [113], [114]] which is defined as conception to age two. Given this and the widely accepted importance this period has on broader child development, there was surprisingly little found in literature. Only Amsterdam, which screened for the risk of obesity in babies and provided intensive counselling for expectant mothers deemed to be at an elevated risk [28] took it to the very earliest opportunity to intervene. Others, such as Leeds (UK), [29] Seinajoki (Finland) [108], Geelong (Australia) [22], had a focus on early childhood.
People living in cities have numerous constraints to the maintenance of a healthy diet, including proximity to food sources and lack of various healthy foods in local food stores [68]. When it comes to food we are anything but fully autonomous; we are heavily influenced in what we eat by our food environment and our context [65,115]; this is particularly true for children [87,116]. It is well established that richer people have healthier diets than poorer people [6]. It is therefore understandable that cities are trying numerous interventions to improve access to healthy food for poorer communities. Whilst the interventions showed some positive results at ameliorating healthy food availability, this alone didn't show an impact on obesity. Indeed, a study found that making the same healthy food available to poorer communities that are available to wealthier communities only addresses 10% of the issue [117]. The real issue – and solution – is that the poor need more money. So, whilst interventions to improve availability of healthy food are admirable, and in part beneficial, we should not lose sight of addressing the real issue – reducing poverty.
Results and impacts from the education and support interventions were variable. Leveraging existing assets [[85], [86], [87]] and developing a support network for the individual [69,70,80] appear to contribute to more positive impacts on reducing obesity. Whilst it is important to educate individuals to eat more healthily and do more exercise, the evidence would suggest solely educating or telling is not enough. What comes through as an important factor for success is involving parents (in relation to children with obesity) and peer groups generally [118] – there must be multiple reinforcing and supportive messages. Healthcare professionals, particularly family doctors, are well placed to deliver effective lifestyle interventions with high-risk patients, discussing weight loss strategies and providing referrals to weight management programmes [119,120].
Physical inactivity is also a key component to increased obesity. Changes in the structure and ability for active travel in cities and our work and home environments have led to declining rates of daily energy expenditure [121]. A report by the Children's Commissioner for England [122] identifies that children today are the least active ever, in part because the area around a home where children can play unsupervised has shrunk by 90% since the 1970s. Busy lives, busy roads, fewer communal spaces — all of these things are making activity something that needs to be ‘planned, scheduled, supervised and often paid for’ [122].
Cities are increasingly using multi-component programmes. Fitzgerald [123] examined residents perspectives using photographs and found participants spontaneously articulated the need for a multi-component and multi-level approach [123]. This approach shows the strongest impact on outcomes. It is however not a quick fix; Amsterdam and Anchorage – both of whom now show impressive results – have had multi-component programmes of work for over 5 years.
A number of multi-component programmes were Mayoral led [10,24,91,92,124]. Two of the most striking were Oklahoma and New York City. In Oklahoma City, Mayor Mick Cornett stood before the elephant cage at the zoo and challenged residents to lose one million pounds – it took them five years but they duly did it – whilst reportedly generating a culture shift towards healthier lifestyles and revitalising the economy [59,93]. Whilst in New York City, the city Health Commissioner credited their achievement to the multi-component approach taken [125,126] and decisive mayoral leadership [127]. The approach of having mutually supporting interventions at numerous levels is supported by other studies [121,128]. A number of authors [28,82,124] reference the EPODE approach. Ensemble Prévenons l'Obésité Des Enfants (EPODE) originated in France but has been implemented in more than 500 communities across different countries, it stress the importance of action at all levels and the prominent role of Mayors [129]. Mayors have a unique position to convene, champion and challenge stakeholders around a shared city-wide vision and action to reduce obesity.
If the ambition is to reduce obesity at a city population level then individual interventions whether it be in schools, an education programme or any other single area are simply not enough. The obesity epidemic is a result of the environment in which we live, which has been created by policies spanning building regulations to food quality standards to transport. The issue of systemic policy factors driving increases in obesity [130] will only be addressed by systemic policy action to reduce obesity. Again, Mayors, with their powers and access to the policy levers spanning areas such as planning and public transport, will be key. Therefore, in addition to their role in providing leadership, they must role model and take direct action on policy interventions to reduce obesity. In addition, the link between the drivers of and actions to address obesity and climate change have been known for a number of years [131] and building on this and more recently, Swinburn et al. [132] describe the interconnected nature of food security (including obesity) and climate change, which they call a ‘Global Syndemic’.
This study has several limitations. Firstly, although it is a comprehensive systematic review it is likely it has only shown a snapshot of what cities are doing to address obesity. This is because of the limited nature of the information available and publication bias towards interventions that have a demonstrable impact. Notwithstanding this, only a quarter (24/96) of the included studies reported an impact on obesity, weight or BMI. Secondly, only publications in English language were included and the process of initial article selection was performed by just one author. This will negatively impact the comprehensiveness of the results but also bring in bias towards missing interventions with poor or negative results that may be published in local language journals. Thirdly, due to the variation in study designs, reporting types, and variation in intervention types and number (single intervention versus multiply interventions at multiple levels), along with the majority of results deriving from simple descriptive texts; we did not carry out any formal quality assessment. This limits the confidence on the relative impact of different interventions and ultimately our recommendations. Finally, almost a quarter of the studies came from New York City which will bring in bias. However, the purpose of this research was to develop a composite model of interventions, based on evidence, that cities could follow and further test. The authors are content it has served this purpose. In respect of the generalisability of the composite model of interventions to address obesity in cities (Fig. 2 below), it needs to acknowledge the important role that context has for the success or failure of a particular intervention. Context can be the prevailing political context, the legal context or precedents, the fiscal or economic context, the social context and vested interests. Entrenched health challenges cannot be addressed through simple, single, generic solutions, they require multiple context relevant interventions [133] This study did not specifically set out to study the impact of leadership of Mayors; this would be an interesting area of future study.
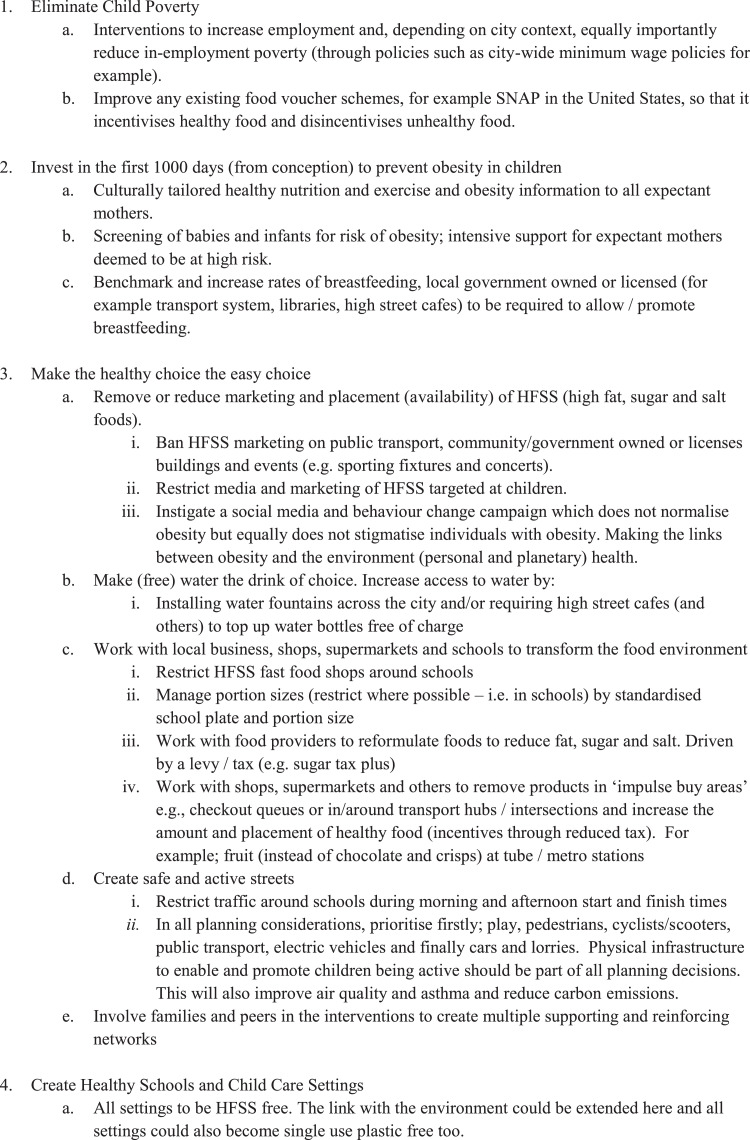
Fig. 2.
Composite Model of Interventions to Address Obesity in Cities.
Obesity is a global epidemic. There is emerging academic consensus that obesity is a complex problem that requires a multi-component and multidisciplinary approach. However, for the most part action in cities has been at best piecemeal. Multi-level, multi-component interventions in concert are needed due to the multi-factorial nature of obesity and its proven links to both the social and built environment. This could be describe this as a composite approach.
The interventions to address obesity do not provide quick fixes and there is a need for sustained and a relentless focus. This is the bad news. However, there is good news. The diagnosis of obesity is not difficult and whilst the issue is complex the solutions are not complicated – they are very simple – and there is evidence from cities across the world that they work. Furthermore, action taken to address obesity will also be good for the environment. For example, active travel increases physical exercise and reduces air pollution from cars. Improved diet reduces processed foods and increases natural plant-based diet. Water availability to fill bottles reduces the use of single use plastic bottles. Personal health and planetary health are intimately and inextricably intertwined.
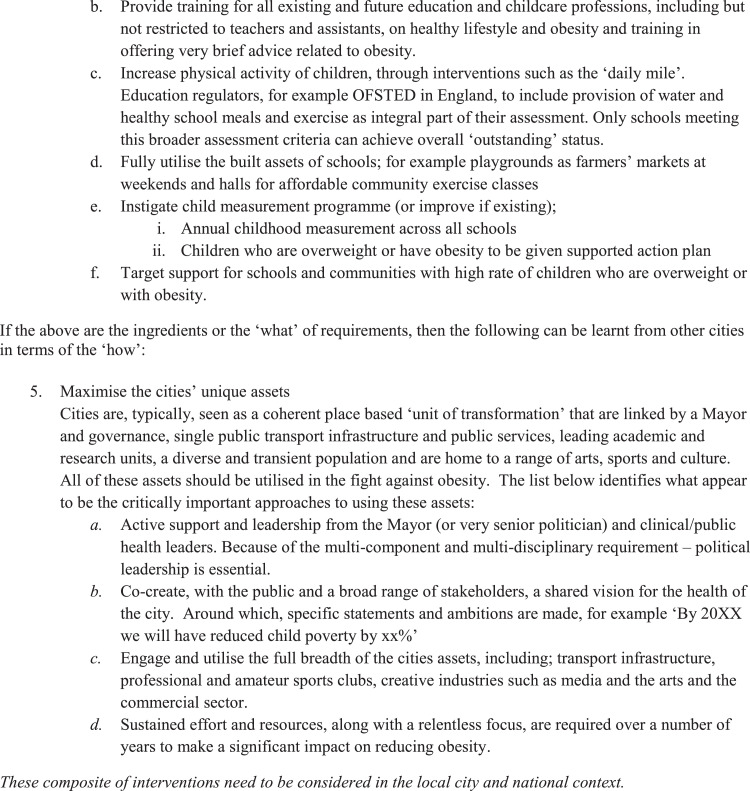
The objective of this research was to connect academic research with policy interventions to aid the real world. Based on this academic review, the authors debated the necessary interventions to reduce obesity and produced the following ‘composite model of interventions to address obesity in cities’. The interventions are a combination of educational, fiscal, regulatory and environmental approaches. They are across a range of settings and are set against five aspirational areas. It is important to acknowledge that it is not the case of simply choosing one or two interventions. The solution to decreasing obesity is multiple reinforcing interventions.
Declaration of Competing Interest
The authors declare there is no conflict of interest.
Acknowledgments
Contributors
SD and HA conceived the idea for the study. SD performed the data extraction and synthesis with input from TC, HA and AD. SD wrote the first draft of the manuscript and all authors made substantial contributions. All authors contributed to the study design, interpretation of findings, and critical revision of the manuscript. All authors approved the final version of the manuscript for submission.
Acknowledgments
We thank the members of the Healthy London Partnership (HLP)* that helped on providing a second review of titles and abstracts. These were: Patrice Donnelly, Pascale Montiel, Emily Treder, Claire Ruiz, Dominic Jones, Suzi Griffiths, Steve Solasta, Raman Patria, David Groom, Emile Radyte, Jess Drummond, Gabriella Baker, Martina Dalton, Lise Hansen and Katie Horrell.
We would also like to thank John Lotherington and Astrid Koblmuller from the Salzburg Global Seminar, Jamie Bussell from Robert Wood Johnson Foundation and all the participants of the Halting the Childhood Obesity Epidemic: Identifying Decisive Interventions in Complex Systems (14th–19th December 2019) for their expert views that fed into this review, both explicitly and implicitly. Infrastructure support for this research was provided by the NIHR Imperial Biomedical Research Centre (BRC).
Data sharing statement
The authors declare that the data collected was gathered from publicly available studies and is available upon reasonable request. Request should be made to the corresponding author.
Funding
The authors received no financial support for the research, authorship or publication of this article.
Footnotes
See Acknowledgements section at the end of this manuscript
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2020.100710.
Appendix. Supplementary materials
References
- 1.Hruby A., Hu F.B. The Epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zylke J.W., Bauchner H. The unrelenting challenge of obesity. JAMA. 2016;315(21):2277–2278. doi: 10.1001/jama.2016.6190. [DOI] [PubMed] [Google Scholar]
- 3.OECD. The Heavy Burden of Obesity; 2019.
- 4.Korkodilos M. Childhood obesity: london's super-sized challenge. In: england PH, editor; 2018.
- 5.Shah R, Hagell A, Cheung R. International comparisons of health and wellbeing in adolescence and early adulthood; 2019.
- 6.Thomas F., Thomas C., Hooper L., Rosenberg G., Vohra J., Bauld L. Area deprivation, screen time and consumption of food and drink high in fat salt and sugar (HFSS) in young people: results from a cross-sectional study in the UK. BMJ Open. 2019;9(6) doi: 10.1136/bmjopen-2018-027333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kauh T.J., Dawkins-Lyn N., Dooyema C. Childhood obesity declines project: an effort of the national collaborative on childhood obesity research to explore progress in four communities. Childh Obes. 2018;14:S1–S4. doi: 10.1089/chi.2018.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iguacel I., Fernández-Alvira J.M., Ahrens W. Prospective associations between social vulnerabilities and children's weight status. Results from the IDEFICS study. Int J Obes. 2018;42(10):1691–1703. doi: 10.1038/s41366-018-0199-6. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Obesity and Overweight Fact Sheet. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed 17 April 2020 2020).
- 10.Freudenberg N., Atkinson S. Getting food policy on the Mayoral table: a comparison of two election cycles in New York and London. Public Health. 2015;129(4):295–302. doi: 10.1016/j.puhe.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 11.McMichael A.J. Will considerations of environmental sustainability revitalise the policy links between the urban environment and health? N S W Public Health Bull. 2007;18(3–4):41–45. doi: 10.1071/nb07023. [DOI] [PubMed] [Google Scholar]
- 12.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 14.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 15.GLA The London Health Inequalities Strategy. London. 2018 [Google Scholar]
- 16.Llargues EF R., Recasens A., Nadal A., Vila M., Perez M.J., Manresa J.M., Recasens I., Salvador G., Serra J., Roure E., Castells C. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. 2011;65(10):896–901. doi: 10.1136/jech.2009.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Safdie ML L., González-Casanova I., Salvo D., Islas A., Hernández-Cordero S., Bonvecchio A., Rivera J.A. Promoting healthful diet and physical activity in the Mexican school system for the prevention of obesity in children. Salud pública de México. 2013 doi: 10.21149/spm.v55s3.5137. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/364/CN-01124364/frame.html http://www.scielosp.org/pdf/spm/v55s3/v55s3a3.pdf (accessed. [DOI] [PubMed] [Google Scholar]
- 18.Kanan M.S. Childhood obesity prevention intervention and policy in the Mexican school system. Dissertation Abstr Int Sect C: Worldwide. 2018;75(1–C) No Pagination Specified. [Google Scholar]
- 19.Vilchis-Gil J., Klünder-Klünder M., Duque X., Flores-Huerta S. Decreased body mass index in schoolchildren after yearlong information sessions with parents reinforced with web and mobile phone resources: community trial. J Med Internet Res. 2016;18(6):e174. doi: 10.2196/jmir.5584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kain JL B., Cerda R., Vio F., Uauy R. Two-year controlled effectiveness trial of a school-based intervention to prevent obesity in Chilean children. Public Health Nutr. 2009 doi: 10.1017/S136898000800428X. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/366/CN-00754366/frame.html http://journals.cambridge.org/download.php?file=%2FPHN%2FPHN12_09%2FS136898000800428Xa.pdf&code=2a761c2290413d204579326df0a7aa58 (accessed. [DOI] [PubMed] [Google Scholar]
- 21.Kain JU R., Leyton B., Cerda R., Olivares S., Vio F. DO NOT USE - NOT IN ENGLISH SEE 16608 [Effectiveness of a dietary and physical activity intervention to prevent obesity in school age children. Revista médica de Chile. 2008 http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/902/CN-00665902/frame.html http://www.scielo.cl/pdf/rmc/v136n1/art03.pdf (accessed. [PubMed] [Google Scholar]
- 22.Desilva-Sanigorski A.M., Colin Bell A., Kremer Peter. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91(4):831–841. doi: 10.3945/ajcn.2009.28826. [DOI] [PubMed] [Google Scholar]
- 23.Thibault HB S., Carriere C., Ruello M., Atchoarena S., Delmas C., Baratchart B.A., Tison S.M. Prevention and treatment of childhood obesity in the Aquitaine region (France) Int J Pediatr Obes. 2010;5:39–40. [Google Scholar]
- 24.National League of Cities. Community wellness: comprehensive city-school strategies to reduce childhood obesity: a report on the city and school leaders collaborating on local wellness policies project. 2010.
- 25.Ravelo JL. Cities and NCDs: the growing threat of childhood obesity in Quito. 2018. https://www.devex.com/news/cities-and-ncds-the-growing-threat-of-childhood-obesity-in-quito-92510 (accessed 24 May 2019.
- 26.Verlyn Williams DW. Get fit kids: a feasibility study of a pedometer-based walking program. Bariatr Nurs Surg Patient Care. 2011;6(3):139–144. [Google Scholar]
- 27.Xu F., Ware R.S., Leslie E. Effectiveness of a randomized controlled lifestyle intervention to prevent obesity among Chinese primary school students: click-obesity study. PLoS ONE. 2015;10(10) doi: 10.1371/journal.pone.0141421. (no pagination // (NIH) *National Institutes of Health*) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hawkes C, Russell S, Isaacs A, Rutter H, Viner R. Obesity Policy Research Unit (OPRU): rapid response briefing paper, 2017.
- 29.T W., B P., C H., M R. Training community practitioners to work more effectively with parents to prevent childhood obesity: the impact of HENRY upon children's centres and their staff. J Hum Nutr Diet. 2012;25(5):460–468. doi: 10.1111/j.1365-277X.2012.01247.x. [DOI] [PubMed] [Google Scholar]
- 30.Fu Y.C.A., To K.C., Tao W.Y. School accreditation scheme reduces childhood obesity in Hong Kong. Glob Health Promot. 2018 doi: 10.1177/1757975918764318. [DOI] [PubMed] [Google Scholar]
- 31.Koch P.A., Contento I.R., Gray H.L. Food, Health, & Choices: curriculum and Wellness Interventions to Decrease Childhood Obesity in Fifth-Graders. J Nutr Educ Behav. 2019 doi: 10.1016/j.jneb.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Mayor of London. Mayor cracks down on opening of new hot-food takeaways around schools. 2017. https://www.london.gov.uk/press-releases/mayoral/mayor-cracks-down-on-new-takeaways-near-schools (accessed 17 May 2019.
- 33.Korea Consumer Agency. Concerns are also raised about 53 food products with increased side effects due to using compound colors 2013. http://english.kca.go.kr/brd/m_11/view.do?seq=232 (accessed 18 June 2019.
- 34.Colquhoun DP J. Childhood obesity prevention: international research, controversies and interventions. Oxford University Press; 2011. Effective school meal interventions: lessons learned from Eat Well Do Well in Hull, England. [Google Scholar]
- 35.Cathy Perlman EN, Lindstrom L., Choe-Castillo Julia, McKie Herman, Alberti M. A Menu for Health: changes to New York City School Food, 2001 to 2011* A Menu for Health: changes to New York City School Food, 2001 to 2011. Journal of School Health. 2012;82(10):484–492. doi: 10.1111/j.1746-1561.2012.00726.x. [DOI] [PubMed] [Google Scholar]
- 36.Sekhobo J., Edmunds L., Dalenius K. Neighborhood Disparities in Prevalence of Childhood Obesity Among Low-Income Children Before and After Implementation of New York City Child Care Regulations. Prev Chronic Dis. 2014;11:E181. doi: 10.5888/pcd11.140152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nonas C.S., D. L., Kettel Khan L., Leviton L. Rationale for New York City's regulations on nutrition, physical activity, and screen time in early child care centers. Prev Chronic Dis. 2014;11:E182. doi: 10.5888/pcd11.130435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sekhobo J.P.E., S. L., Dalenius K., Jernigan J., Davis C.F., Giddings M., Lesesne C., Kettel Khan L. Neighborhood disparities in prevalence of childhood obesity among low-income children before and after implementation of New York City child care regulations. Prev Chronic Dis. 2014;11:E181. doi: 10.5888/pcd11.140152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease CP Effects of switching from whole to low-fat/fat-free milk in public schools - New York city, 2004-2009. MMWR - Morbid Mortal Wkly Rep. 2010;59(3):70–73. [PubMed] [Google Scholar]
- 40.Boss-Bicak S. Schools winning the food fight. Crain's New York Bus. 2004;20(31):18. [Google Scholar]
- 41.Spake A. THE WORLD OF CHEF JORGE. US News World Rep. 2005;138(17):64–67. [PubMed] [Google Scholar]
- 42.Lessard LL C., Kakietek J., Breck A., Jernigan J., Dunn L., Nonas C., O'Dell S.A., Stephens R.L., Xu Y., Khan L.K. Measurement of compliance with New York City's regulations on beverages, physical activity, and screen time in early child care centers. Prev Chronic Dis. 2014;11(10) doi: 10.5888/pcd11.130433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alberti P., Perlman S., Nonas C., Hadler J., Choe J., Bedell J. Effects of switching from whole to low-fat/fat-free milk in public schools - New York city, 2004-2009. Mmwr. 2010;59(3):70–73. Morbidity and mortality weekly report. [PubMed] [Google Scholar]
- 44.Foo L.L., Vijaya K., Sloan R.A., Ling A. Obesity prevention and management: singapore's experience. Obes Rev. 2013;14(S2):106–113. doi: 10.1111/obr.12092. [DOI] [PubMed] [Google Scholar]
- 45.Gupta N, Kai Chin M, Yang J, et al. Obesity prevention in Singapore: collaborative efforts among government, health professionals and the community; 2010.
- 46.News; B. London transport network junk food advert ban starts. 2019. https://www.bbc.co.uk/news/uk-england-london-47318803 (accessed 25 February 2019.
- 47.Elbel B. Consumer estimation of recommended and actual calories at fast food restaurants. Obesity. 2011;19(10):1971–1978. doi: 10.1038/oby.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elbel B., Mijanovich TD L.B., Abrams C., Weitzman B., Kersh R., Auchincloss A.H., Ogedegbe G. Calorie labeling, fast food purchasing and restaurant visits. Obesity (Silver Spring, Md) 2013;21(11):2172–2179. doi: 10.1002/oby.20550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tran A.D. Addressing eating habits through food label education in Stevenson, WA. J Investig Med. 2010;58(1):204. [Google Scholar]
- 50.Gittelsohn JAS E., Mui Y., Kharmats A.Y., Hopkins L.C., Dennis D. B'More Healthy Communities for Kids: design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Truiett-Theodorson RT S., Bowie J.V., Summers A.C., Kelber-Kaye J. Building effective partnerships to improve birth outcomes by reducing obesity: the B'more Fit for healthy babies coalition of Baltimore. Eval Program Plann. 2015;51:53–58. doi: 10.1016/j.evalprogplan.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 52.Trude A., Steeves E.A., Shipley C., Sato P.M., Lachenmayr L., Gittelsohn J. Impact of a multi-level multi-component food environment/behavioral intervention on youth leaders. FASEB J Confer: Exp Biol. 2017;31(1 Supplement 1) [Google Scholar]
- 53.Trude A.C.B., Surkan P.J., Anderson Steeves E., Pollack Porter K., Gittelsohn J. The impact of a multilevel childhood obesity prevention intervention on healthful food acquisition, preparation, and fruit and vegetable consumption on African-American adult caregivers. Public Health Nutr. 2018 doi: 10.1017/S1368980018003038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ruggiero C.F., Poirier L., Trude A.C.B. Implementation of B'More Healthy Communities for Kids: process evaluation of a multi-level, multi-component obesity prevention intervention. Health Educ Res. 2018;33(6):458–472. doi: 10.1093/her/cyy031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.NYC. NYC Food Standards. 2017. https://www1.nyc.gov/site/doh/health/health-topics/nyc-food-standards.page (accessed 24 November 2018.
- 56.NYC FRESH. FRESH Fact Sheet. http://www.nyc.gov/html/misc/pdf/fresh_fact_sheet_eng.pdf (accessed 17 August 2018.
- 57.Pofeldt E. Child obesity epidemic weighs heavily on NYC. Crain's New York Bus. 2008;24(34):18. [Google Scholar]
- 58.Leggat M., Kerker B., Nonas C., Marcus E. Pushing produce: the New York City Green Carts initiative. J Urban Health: Bull New York Acad Med. 2012;89(6):937–938. doi: 10.1007/s11524-012-9688-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reeve BA M., Farias R., Gostin L. State and municipal innovations in obesity policy: why localities remain a necessary laboratory for innovation. Am J Public Health. 2015;105(3):442–450. doi: 10.2105/AJPH.2014.302337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Payne GHW H., Olsho L., Jernigan J., Farris R., Walker D.K. Implementing a farmers' market incentive program: perspectives on the New York City Health Bucks Program. Prev Chronic Dis. 2013;10:E145. doi: 10.5888/pcd10.120285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Narain K., Mata A., Flores J. Nutrition policy decreases sugar-sweetened beverages in municipal parks: lessons learned from Carson, California. Journal of Public Health Management And Practice: JPHMP. 2016;22(4):392–394. doi: 10.1097/PHH.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 62.Sturm RC A. Zoning for health? the year-old ban on new fast-food restaurants in South LA. Health Aff. 2009;28 doi: 10.1377/hlthaff.28.6.w1088. w1088-NaN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Donnelly P. London health and care strategic partnership board focus areas, 2018.
- 64.Berg J. Why New York City's attempt to ban soda fizzled. Obes Res Clin Pract. 2014;8:7. [Google Scholar]
- 65.Diller A. The Illusion of Autonomy in "Food" Litigation. Am J Law Med. 2015;41(2/3):274–284. doi: 10.1177/0098858815591518. [DOI] [PubMed] [Google Scholar]
- 66.Crixell SHF B.J., Fisher D.T., Biediger-Friedman L. Improving children's menus in community restaurants: best food for families, infants, and toddlers (Best food fits) intervention, South Central Texas, 2010-2014. Prev Chronic Dis. 2014;11(12) doi: 10.5888/pcd11.140361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee S.H. Changing the food environment in Baltimore city: impact of an intervention to improve carry-outs in low-income neighborhoods. Dissertation Abstr Int: Section B: Sci Eng. 2014;74(11–B(E)) No Pagination Specified. [Google Scholar]
- 68.Development Song H-J. implementation and evaluation of an urban food store intervention for Korean corner stores in Baltimore city. Dissertation Abstr Int: Sect B: Sci Eng. 2008;69(4–B):2277. [Google Scholar]
- 69.Lemstra M. The healthy weights initiative. Circul Confer: Am Heart Assoc. 2015;132 no pagination. [Google Scholar]
- 70.Lemstra M., Rogers M.R. The importance of community consultation and social support in adhering to an obesity reduction program: results from the Healthy Weights Initiative. Patient Prefer Adherence. 2015;9:1473–1480. doi: 10.2147/PPA.S91912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gottschalk LBS D.L., Jensen A., Beyrouty M., Skursky N., Murphy J., Schwartz M., Sherman S. The fit kid & fit teen coaching program: addressing obesity with the added support of health coaches. J Adolesc Health. 2015;(1):S104–S1S5. [Google Scholar]
- 72.Wang HEL M., Hart A., Summers A.C., Anderson Steeves E., Gittelsohn J. Process evaluation of Healthy Bodies, Healthy Souls: a church-based health intervention program in Baltimore City. Health Educ Res. 2013;28(3):392–404. doi: 10.1093/her/cyt049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Charles Perkin Centre. How mobile phones could save us from obesity. 2015. https://sydney.edu.au/news-opinion/news/2015/08/13/how-mobile-phones-could-save-us-from-obesity.html (accessed 17 February 2019.
- 74.Ahn S.N., Lee J., Bartlett-Prescott J., Carson L., Post L., Ward K.D. Evaluation of a Behavioral Intervention With Multiple Components Among Low-Income and Uninsured Adults With Obesity and Diabetes. Am J Health Promot. 2018;32(2):409–422. doi: 10.1177/0890117117696250. [DOI] [PubMed] [Google Scholar]
- 75.Nair R. Improving physical activity among Hispanic women by identifying barriers. Dissertation Abstr Int: Sect B: Sci Eng. 2019;80 4-B(E)No Pagination Specified. [Google Scholar]
- 76.Rudez ML K. ActiveSmart physical activity behaviour change program. J Sci Med Sport. 2014;18:e66. [Google Scholar]
- 77.Staff M. ‘Which way is your child growing?’ asks Singapore anti-obesity ad. 2017. https://www.mumbrella.asia/2017/08/way-child-growing-asks-singapore-anti-obesity-ad (accessed 29 June 2019.
- 78.Kansagra S.M., Kennelly M.O., Nonas C.A. Reducing sugary drink consumption: new York City's approach. Am J Public Health. 2015;105(4):e61–ee4. doi: 10.2105/AJPH.2014.302497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jordan AP J.T., Bleakley A., Mallya G. Developing media interventions to reduce household sugar-sweetened beverage consumption. Ann Am Acad Political Soc Sci. 2012;640(1):118–135. [Google Scholar]
- 80.Thomas J. Using social marketing to address obesity: the ongoing 'Liverpool's Challenge' social marketing programme. J Commun Healthc. 2009;2(3):216–228. [Google Scholar]
- 81.Huberty JLD T., Peterson K., Balluff M. Activate Omaha: the journey to an active living environment. Am J Prev Med. 2009;37(6 SUPPL. 2):S428–SS35. doi: 10.1016/j.amepre.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 82.Fransen GAJK M., Molleman G.R.M. Towards an integrated community approach of overweight prevention: the experiences of practitioners and policymakers. Fam Pract. 2012;29(SUPPL. 1):i104–i1i9. doi: 10.1093/fampra/cmr123. [DOI] [PubMed] [Google Scholar]
- 83.Teeriniemi A.M., Salonurmi T., Jokelainen T. A randomized clinical trial of the effectiveness of a Web-based health behaviour change support system and group lifestyle counselling on body weight loss in overweight and obese subjects: 2-year outcomes. J. Intern. Med. 2018;284(5):534–545. doi: 10.1111/joim.12802. [DOI] [PubMed] [Google Scholar]
- 84.Van Wechem SNVA P., Brug J., Kistemaker C., Riedstra M., Hardeman W., Löwik M.R.H. Results of a community-based campaign to reduce fat intake. Nutr Health. 1997;11(3):207–218. doi: 10.1177/026010609701100306. [DOI] [PubMed] [Google Scholar]
- 85.Irwin CI R., Richey P., Miller M., Boddie J., Dickerson T. Get fit with the Grizzlies: a community-school-home initiative to fight childhood obesity led by a professional sports organization. Stud Health Technol Inform. 2012;172:163–167. [PubMed] [Google Scholar]
- 86.Irwin C.C., Irwin R.L., Miller M.E., Somes G.W., Richey P.A. Get fit with the grizzlies: a community-school-home initiative to fight childhood obesity. J Sch Health. 2010;80(7):333–339. doi: 10.1111/j.1746-1561.2010.00510.x. [DOI] [PubMed] [Google Scholar]
- 87.The Health Foundation. A recipe for action: using wider evidence for a healhier UK. 2018. https://www.health.org.uk/publications/a-recipe-for-action-using-wider-evidence-for-a-healthier-uk (accessed Accessed: 15 November 2019.
- 88.Feyerherm L., Tibbits M., Wang H., Schram S., Balluff M. Partners for a healthy city: implementing policies and environmental changes within organizations to promote health. Am J Public Health. 2014;104(7):1165–1168. doi: 10.2105/AJPH.2014.301875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Economos CDH R.R., Must A., Goldberg J.P., Kuder J., Naumova E.N., Collins J.J., Nelson M.E. DO NOT USE DUCPLICATE RECORD WITH 16257 Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57(4):322–327. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 90.Economos D. A community intervention reduces BMI z-score in children: shape Up Somerville first year results. Obesity. 2007 doi: 10.1038/oby.2007.155. [DOI] [PubMed] [Google Scholar]
- 91.Economos C.D.C., Joseph A. Shaping up Somerville: a community initiative in Massachusetts. Prevent Med: Int J Devoted Pract Theory. 2010;50(Suppl):S97–SS8. doi: 10.1016/j.ypmed.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 92.Burney D, Farley T, Sadik-Khan J, Burden A. Active Design Guidelines Promoting Physical Activity and Health in Design, 2010.
- 93.McGill N. Weight-loss challenges unifying communities around health. Nation's Health. 2013;43(3):1–3. [Google Scholar]
- 94.Green CGK G. Promoting active transportation as a partnership between urban planning and public health: the Columbus healthy places program. Public Health Rep. 2011;126:41–50. doi: 10.1177/00333549111260S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Carter K. Mexico's latest way to beat the obesity epidemic: make commuters do squats for free subway tickets. 2015. https://www.theguardian.com/society/shortcuts/2015/jan/27/mexico-beat-obesity-make-commuters-do-squats-for-free-subway-tickets (accessed 26 June 2019.
- 96.Wewatt. Bike Powered Furniture. https://wewatt.com/ (accessed Accessed 19th Novemer 2019 2019).
- 97.Bouch P, Milkovich L, Lamy J, Saringo J. Health basics: investing in a three-wave community-based approach to promote health and reduce obesity; 2011.
- 98.A-COAN;. Alexandria Childhood Obesity Action Network (A-COAN). 2006. http://healthieralexandria.org/content.aspx?id=29854 (accessed 23 April 2019.
- 99.Foulkes C. Lessons from healthy together geelong: delivering systems change at scale across two levels of government. Obes Res Clin Pract. 2014;8:33. [Google Scholar]
- 100.Healthier Auckland Together Plan. The Healthier Auckland Together Plan 2015–2020. 2015.
- 101.Alanqoudi Z, Alhinai S. Nizwa healthy lifestyle project evaluation report 2010; 2010.
- 102.AAGG Website. Amsterdam healthy weight programme. 2019. https://www.amsterdam.nl/sociaaldomein/blijven-wij-gezond/amsterdam-healthy/.
- 103.City of Amsterdam. Amsterdam will become the Healthiest City for Children!, 2017.
- 104.Willocks S, Reddy K. Signs of progress in childhood obesity declines site summary report Anchorage, Alaska 2015, 2015.
- 105.Chomitz VRM R.J., Wendel J.M., Williams S.A., Cabral H.J., King S.E., Olcott D.B., Cappello M., Breen S., Hacker K.A. Healthy living cambridge kids: a community-based participatory effort to promote healthy weight and fitness. Obesity. 2010;18(SUPPL. 1):S45–S53. doi: 10.1038/oby.2009.431. [DOI] [PubMed] [Google Scholar]
- 106.ICF Macro. Signs of progress in childhood obesity declines site summary report Philadelphia, PA 2015. 2015.
- 107.Robbins J.M., Mallya G., Wagner A., Buehler J.W. Prevalence, disparities, and trends in obesity and severe obesity among students in the school district of Philadelphia, Pennsylvania, 2006-2013. Prev Chronic Dis. 2015;12:E134. doi: 10.5888/pcd12.150185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.City of Seinäjoki. City of Seinäjoki, Overcoming Obesity Programme 2013–2020. 2012. https://www.seinajoki.fi/material/attachments/seinajokifi/sosiaalijaterveys/terveyspalvelut/asiakas-japotilasasiakirjat/Fnp1Zw3JF/OVERCOMING_OBESITY_PROGRAMME_2013-2020.pdf (accessed 16 May 2019.
- 109.WHO. Finland curbs childhood obesity by integrating health in all policies. 2015. https://www.who.int/features/2015/finland-health-in-all-policies/en/june 2015).
- 110.Kelly P.M., Davies A., Greig A.J.M., Lee K.K. Obesity Prevention in a City State: lessons from New York City during the Bloomberg Administration. Front Public Health. 2016;4 doi: 10.3389/fpubh.2016.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ottley P, Willocks S. Signs of progress in childhood obesity declines: site summary report. New York, NY., 2015.
- 112.Woo Baidal J.A., Locks L.M., Cheng E.R., Blake-Lamb T.L., Perkins M.E., Taveras E.M. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;50(6):761–779. doi: 10.1016/j.amepre.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 113.Mameli C., Mazzantini S., Zuccotti G.V. Nutrition in the First 1000 Days: the Origin of Childhood Obesity. Int J Environ Res Public Health. 2016;13(9):838. doi: 10.3390/ijerph13090838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Black R.E., Victora C.G., Walker S.P. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013;382(9890):427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 115.Public Health England. Using the planning system to promote healthy weight environments Guidance and supplementary planning document template for local authority public health and planning teams, 2020.
- 116.Wang YCV S.M. Caloric effect of a 16-ounce (473-mL) portion-size cap on sugar-sweetened beverages served in restaurants. Am J Clin Nutr. 2013;98(2):430–435. doi: 10.3945/ajcn.112.054833. [DOI] [PubMed] [Google Scholar]
- 117.Allcott H, Diamond R, Dub´e JP, Handbury J, Rahkovsky I, Schnell M. Food Deserts and the Causes of Nutritional Inequality. 2019.
- 118.Kovalskys I., Indart Rougier P., Luciana L., Rauch Herscovici C., De Gregorio M.J. Mini salten: a case study on learnings from Argentina on outcomes and challenges. Ann Nutr Metab. 2017;71(Supplement 2):96–97. [Google Scholar]
- 119.Aveyard P., Lewis A., Tearne S. Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomised trial. The Lancet. 2016;388(10059):2492–2500. doi: 10.1016/S0140-6736(16)31893-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jackson S.E., Wardle J., Johnson F., Finer N., Beeken R.J. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: a cross-sectional analysis. BMJ Open. 2013;3(11) doi: 10.1136/bmjopen-2013-003693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Maddock J. Evaluation of community-based physical activity programs. Eval Program Plann. 2006;29(3):240–241. [Google Scholar]
- 122.Longfield A. Playing Out A Children's Commissioner's report on the importance to children of play and physical activity 2018.
- 123.FitzGerald EAF R., Dean L.T., Johnson T.E., Solomon S., Bugos E., Mallya G., Cannuscio C.C. Community-Generated recommendations regarding the urban nutrition and tobacco environments: a Photo-Elicitation study in Philadelphia. Prev Chronic Dis. 2013;10(6) doi: 10.5888/pcd10.120204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.De Henauw SVA J., Reynaert H. Childhood obesity prevention: in need of urban governance? the case of childhood obesity prevention in two Flemish cities. Obesity Reviews. 2010;11:458. [Google Scholar]
- 125.Farley T., Dowell D. Preventing childhood obesity: what are we doing right? Am J Public Health. 2014;104(9):1579–1583. doi: 10.2105/AJPH.2014.302015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Farley T., Van-Wye G. Reversing the obesity epidemic: the importance of policy and policy research. Am J Prev Med. 2012;43(3, Suppl 2):S93–SS4. doi: 10.1016/j.amepre.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 127.Sisnowski J., Street J.M., Braunack-Mayer A. Targeting population nutrition through municipal health and food policy: implications of New York City's experiences in regulatory obesity prevention. Food Policy. 2016;58:24–34. [Google Scholar]
- 128.Nonas C.S., D. L., Kettel Khan L. Insights and implications for health departments from the evaluation of New York City's regulations on nutrition, physical activity, and screen time in child care centers. Prev Chronic Dis. 2014;11:E178. doi: 10.5888/pcd11.130429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Borys J.M., Le Bodo Y., Jebb S.A. EPODE approach for childhood obesity prevention: methods, progress and international development. Obes Rev. 2012;13(4):299–315. doi: 10.1111/j.1467-789X.2011.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Swinburn B.A., Sacks G., Hall K.D. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 131.Friel S., Marmot M., McMichael A.J., Kjellstrom T., Vågerö D. Global health equity and climate stabilisation: a common agenda. The Lancet. 2008;372(9650):1677–1683. doi: 10.1016/S0140-6736(08)61692-X. [DOI] [PubMed] [Google Scholar]
- 132.Swinburn B.A., Kraak V.I., Allender S. The Global Syndemic of Obesity, Undernutrition, and Climate Change: the Lancet Commission report. Lancet. 2019;393(10173):791–846. doi: 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 133.Breda J., Wickramasinghe K., Peters D.H. One size does not fit all: implementation of interventions for non-communicable diseases. BMJ. 2019;367:l6434. doi: 10.1136/bmj.l6434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.