Abstract
Chiliadenus lopadusanus Brullo is an Asteraceae plant species endemic to Lampedusa island, the largest island of the Pelage archipelago, Italy. The organic extract of its whole aerial parts, showing antibiotic activity against Staphylococcus aureus and Acinetobacter baumannii, wasfractionated employing bioguided purification procedures affording three main farnesane-type sesquiterpenoids. They were identified by spectroscopic methods (NMR and ESIMS data) as the (E)-3,7,11-trimethyldodeca-1,6,10-triene-3,9-diol, (E)-10-hydroxy-2,6,10-trimethyldodeca-2,6,11- trien-4-one and (E)-10-hydroxy-2,6,10-trimethyl-dodeca-6,11-dien-4-one, commonly named 9-hydroxynerolidol, 9-oxonerolidol, and chiliadenol B, respectively. These three sesquiterpenes, isolated for the first time from C. lopadusanus, were tested on methicillin-resistant S. aureus and A. baumannii showing antibacterial and antibiofilm activities. This plant could be used as a source to isolate secondary metabolites as potential new antibiotics.
Keywords: Chiliadenus lopadusanus, sesquiterpenes, antibacterial activity, antibiofilm activity
1. Introduction
Antimicrobial resistance (AMR) is a phenomenon that seriously endangers the control of diseases around the world [1]. Microorganisms resistant to antimicrobials, including multidrug-resistant ones, are often the cause of healthcare-associated infections but also infections of outpatients. In addition, they can be present in the normal bacterial flora of all healthy people, in companion animals and in the environment [2,3,4]. Resistant microorganisms are also present in food-producing animals, and sometimes even in food [5].
Until now, the threat of bacterial resistance to antibiotics has been underestimated. However, antibiotic resistance is now a phenomenon recognized all over the world as a priority in the health sector due to the important implications both from a clinical point of view (longer hospital stays, higher mortality) and from an economic point of view (rising costs) [6,7].
The World Health Organization (WHO) is sounding the alarm on the AMR phenomenon which in recent decades has practically rendered most of the available antibiotics useless, including the most recent carbapenem drugs associated with innovative inhibitors of resistance enzymes. In fact, both Gram-positive and Gram-negative pathogens such as, for example, the ESKAPE group (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacter spp.) are multiresistant. Therefore, the clinical efficacy of many classes of antibiotics is compromised with a consequent increase in mortality associated with infections [8,9]. The WHO has also estimated that about 80% of chronic infections are related to the formation of biofilms. Biofilms are defined as communities of properly organized microorganisms attached to an inert or living substrate and embedded in a self-produced extracellular exopolysaccharidic matrix. Biofilm formation is regarded as the most important virulence factor protecting the sessile bacteria against antibacterial compounds and host immune responses [10]. Biofilm-related infections represent a major global problem in the hospital setting due to their intrinsic recalcitrance toward antibiotics and to difficulties in treatment.
Unfortunately, the development of new antibiotics proceeds very slowly, making it necessary to search for new potential antimicrobial scaffolds from different sources [11,12,13,14,15]. Herbal medicine, according to the WHO classification, belongs to the vast system of traditional medicine. Many populations living in poor countries and especially in rural areas, consider the world of plants as the main pivot for their primary health, relying on the beneficial properties of trees, herbs, and fruits to cure certain diseases and heal wounds [16,17,18].
Plants are a rich reservoir of compounds with several biological activities, including antimicrobial properties [19,20,21,22,23]. Plant extracts can have a good activity on their own or can be sources of antimicrobial compounds effective against pathogens responsible for infections, which are difficult to treat also for their ability to form biofilms [24,25,26].
A screening on endemic plants collected in different regions of the Mediterranean basin was aimed to find new antibiotics. Among the corresponding organic extracts, that of Chiliadenus lopadusanus showed a growth inhibiting activity against some human pathogenic bacteria. C. lopadusanus Brullo (Figure 1) is an Asteraceae endemic species growing spontaneously on Lampedusa island, the largest island of the Pelage archipelago, about 100 km from the North Africa coast and 200 km from the Sicily coast, Italy [27].
Figure 1.
Chiliadenus lopadusanus in Conigli bay, Lampedusa island, Italy.
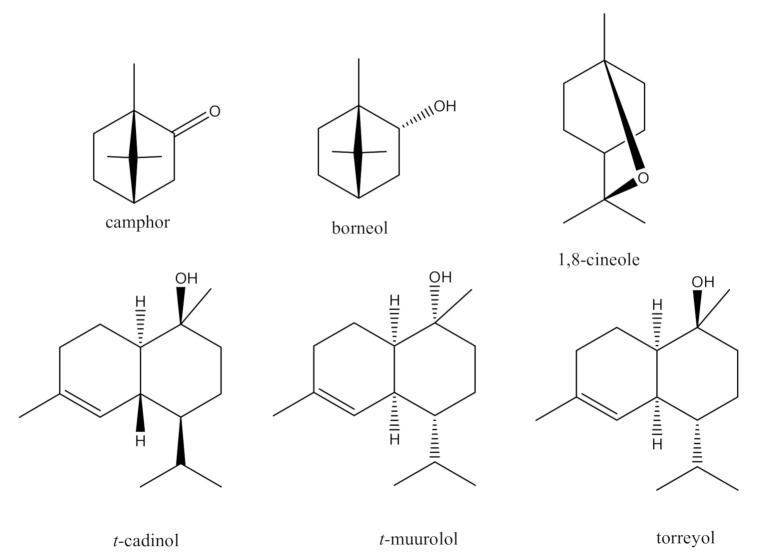
The essential oils produced by the leaves and flowers of C. lopadusanus were first investigated by Sacco and Maffei [28] using GC and GC-MS spectrometry and camphor, borneol, and 1,8-cineole (Figure 2) were identified as the major constituents. More recently, the essential oils of the same plant were extracted by hydrodistillation and analyzed by GC-MS leading to the identification of 98 compounds [27]. Camphor was identified as the main constituent together with the monoterpene 1,8-cineole and the sesquiterpenes t-cadinol, t-muurolol, and torreyol (Figure 2). These terpenes are reported in the literature to play a role in the potential spasmolytic, antibacterial, antifungal, and allelopathic activity [28,29,30]. However, complete chemical studies of all the major metabolites of C. lopadusanus to characterize their biological activity have not been performed.
Figure 2.
The chemical structures of camphor, borneol, 1,8-cineole, t-cadinol, t-muurolol, and torreyol.
In fact, the chemical investigation of the secondary metabolites produced by the plants belonging to the genus Chiliadenus (Asteraceae family) is very limited. The components of the essential oil obtained from leaves extract of Spanish wild growing Chiliadenus glutinosa were analyzed for the first time by GC-MS and GC [31]. Several terpenoid derivatives were identified including camphor and borneol as the main components. Successively, a comparison of the essential oil extracted with direct thermal desorption techniques was reported [32]. The essential oil obtained from Chiliadenus iphionoides, a plant endemic to the eastern Mediterranean area and growing wild in Jordan was analyzed by Avato et al. [33]. Borneol and its acetyl and formyl esters with a potential antispasmodic activity were identified as the major constituents by GC and GC—MS [33]. Eight new compounds and eight previously identified metabolites were instead isolated from Chiliadenus montanus, an hearb endogeneous of the North Sinai region of Egypt. Their antimicrobial activity was evaluated against a panel of bacterial and fungal strains [34].
Therefore, this manuscript reports the extraction, bioguided purification, and the chemical characterization by spectroscopic methods of the main metabolites produced by C. lopadusanus. Antibacterial and antibiofilm activities of the isolated metabolites were assayed against Staphylococcus aureus and Acinetobacter baumannii, nosocomial pathogenic bacteria responsible for severe infections.
2. Results and Discussion
2.1. Isolation and Identification of Bio-Active Metabolites
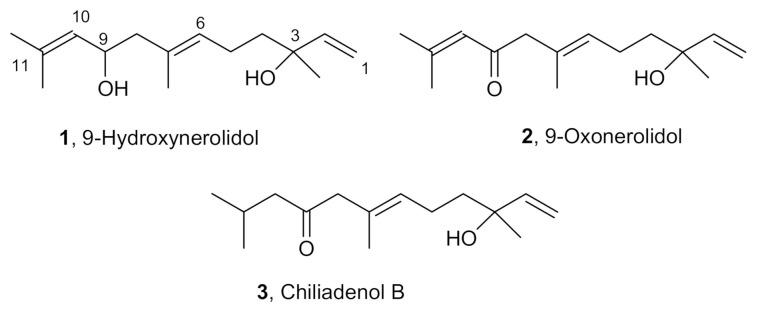
The n-hexane extract of the whole aerial parts of C. lopadusanus was chromatographed, as reported in detail in the Materials and Methods section, to afford (E)-3,7,11-trimethyldodeca-1,6,10-triene-3,9-diol, (E)-10-hydroxy-2,6,10-trimethyldodeca- 2,6,11-trien-4-one, and (E)-10-hydroxy-2,6,10-trimethyl-dodeca-6,11-dien-4-one, commonly named 9-hydroxynerolidol, 9-oxonerolidol, and chiliadenol B (compounds 1–3, Figure 3).
Figure 3.
Structures of 9-hydroxynerolidol, 9-oxonerolidol, and chiliadenol B (1–3).
Compounds 1–3 were identified comparing their physics (specific rotation) spectroscopic (mono and bidimensional NMR spectra and ESIMS) with data partially reported in the literature and in particular, for 9-hydroxynerolidol and 9-oxonerolidol (1 and 2) with data reported by Stoessl et al. [33] and for chiliadenol B (3) with those reported by Hegazy et al. [34]. Therefore, in Tables S1–S3, the chemical shifts of all the protons and carbons of the three sesquiterpenoids (1–3) were unambiguously reported with some updated values with respect to the ones already reported [34,35].
This is the first isolation of farnesane-type sesquiterpenoids 1–3 (Figure 3) from C. lopadusanus. 9-Hydroxynerolidol (1) was first isolated as a stress metabolite from Solanum melongena [35] together with 9-oxonerolidol (2) which was preliminarily isolated also from the leaf oil of the camphor tree by Hiroi and Takaoka [36]. Chiliadenol B (3) was isolated for the first time from the Egyptian herbal medicine Chiliadenus montanus [34].
2.2. Antibacterial and Anti-Biofilm Activities
The organic extract of C. lopadusanus was tested for its antibacterial activity against the methicillin-resistant reference strain Staphylococcus aureus ATCC43300 and reference strain Acinetobacter baumannii ATCC747. At the concentration of 500 μg/mL, the n-hexane extract showed a total inhibition of planktonic growth of both strains (Table 1).
Table 1.
Antibacterial activity of the leaves extract, expressed as a percentage of growth inhibition, and of compounds 1–3, expressed as MIC (μg/mL) ± standard deviation (SD), against test strains.
| Strains | Plant Extract (500 µg/mL) |
Compound 1 MIC | Compound 2 MIC | Compound 3 MIC | CO MIC | TE MIC |
|---|---|---|---|---|---|---|
| S. aureus | 100% inhibition | 75 ± 1.8 | 150 ± 3.8 | nd | - | 1 ± 0.1 |
| A. baumannii | 100% inhibition | 150 ± 4.2 | 150 ± 3.2 | nd | 0.78 ± 0.0 | - |
Colistin (CO) and teicoplanin (TE) were used as positive controls; nd: not detected.
The secondary metabolites 1, 2, 3 obtained from the extract, were tested individually against the reported strains identifying the minimal inhibitory concentration (MIC) and minimal bactericidal concentration (MBC) values. Both compounds 1 and 2 showed antibacterial activity: Compound 1 exhibited MIC values of 150 μg/mL on the A. baumannii strain and 75 μg/mL on the S. aureus strain, while compound 2 showed a MIC value of 150 μg/mL for both test strains (Table 1). The MBC values of compounds 1 and 2 were higher than 300 μg/mL for both tested strains. No antimicrobial activity on the planktonic bacterial growth was detected for substance 3.
These results are in agreement with those of Hegazy et al. [34] who previously tested chiliadenol B on a different panel of bacterial species and did not show any antimicrobial activity. The ability to inhibit the bacterial growth has been documented for several terpenes and terpenoid derivatives [37,38,39]. The antibacterial activity is most frequently explained by their ability to destroy the plasma membrane integrity [40], but it has also been hypothesized that they can inhibit efflux pumps or ATPases on the bacterial membranes [41]. In this large group of phytochemicals, it is known that sesquiterpenoid compounds also have antimicrobial activity. Gomes et al. [42] showed that farnesol was able to inhibit Staphylococcus epidermidis planktonic cells. Structurally diverse halosesquiterpenoids from Laurencia composita Yamada showed an antibacterial effect against S. aureus [43]. However, the antibacterial activity of sesquiterpenoids 1 and 2 from C. lopadosanus has not been previously described. Interestingly, the structural differences between these two compounds and chiliadenol B are related to a clear difference in antimicrobial activity.
In fact, the two compounds 1 and 2 are structurally related and differed only in the presence of the hydroxyl group at C-9 in 1, which is oxidized in 2. In 3, the double bond between C-10 and C-11 was absent. The α,β-unsaturated carbonyl group present in 1 could be responsible for its antibiotic activity as probably it is a site for nucleophile Michael addition, as frequently reported for other natural bio-active metabolites [44,45]. Similarly, the mode of action could be invoked for 2 as the hydroxyl group at C-9 could be easily oxidized within the cells as given by the more stable α,β-unsaturated carbonyl group as in 1. This does not occur in 3 as it lacks the double bond to be conjugated with the carbonyl at C-9.
Noteworthy, Li et al. [46] reported that (3S)-(+)-9-oxonerolidol from Cinnamomum camphora (L.) J. Presl showed an in vitro anti-inflammatory activity by inhibiting the nuclear factor κB (NF-κB). However, its absolute configuration was only assigned by comparison of its specific optical rotation with that previously reported for the same sesquiterpene [35]. This assignment requires confirmation using chiroptical and computational methods. The simultaneous presence of antibacterial and anti-inflammatory activity in the same compound can be very useful as the inflammatory response that represents the early defense against the antibacterial infection can at the same time contribute to tissue damage.
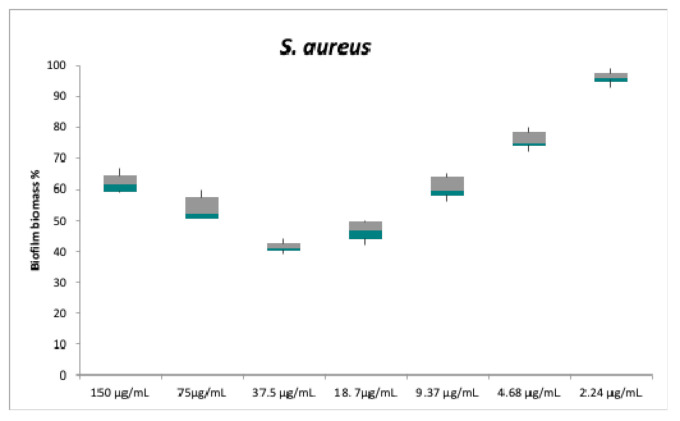
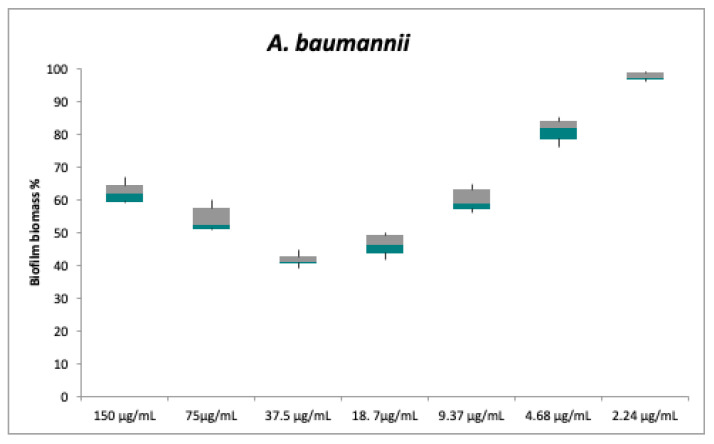
Regarding the anti-biofilm activity, compounds 1 and 2 do not appear to be effective. Despite the lack of antibacterial activity against planktonic cells, compound 3 was instead able to inhibit the biofilm formation of both strains: The test strains were cultured in multiwells in the biofilm growth mode in the presence of different concentrations of compound 3 (between 2.24 to 150 μg/mL). Biofilm formation by S. aureus and A. baumannii was already weakly inhibited at the concentration of 9.37 μg/mL (Figure 4 and Figure 5).
Figure 4.
In vitro biofilm formation of S. aureus following an overnight treatment with serial dilutions of compound 3. Biofilm formation was determined by the cristal violet assay. Biofilm biomass values are presented as the mean percentage ± standard deviation (SD) and S. aureus biofilm biomass without a treatment is assumed to be 100%. Each pair of means was compared using a Tukey’s multiple comparisons test; no significant differences were detected between the following pairs: 150℃9.37 μg/mL; 37.5℃18.7 μg/mL.
Figure 5.
In vitro biofilm formation of A. baumannii following an overnight treatment with serial dilutions of compound 3. Biofilm formation was determined by the cristal violet assay. Biofilm biomass values are presented as the mean percentage ± SD and A. baumannii biofilm biomass without a treatment is assumed to be 100%. Each pair of means was compared using a Tukey’s multiple comparisons test; no significant differences were detected between the following pairs: 150℃9.37 μg/mL; 37.5℃18.7 μg/mL.
The concentration value of 18 μg/mL caused a biofilm inhibition of 53 ± 3.5% for S. aureus and 54 ± 3.3% for A. baumannii. For both bacterial strains, the maximum inhibition was obtained at 37.5 μg/mL, a concentration that caused nearly 60% reduction in the biofilm mass (59 ± 1.7% and 58.5 ± 2% inhibition for S. aureus and A. baumannii, respectively), despite the lack of statistically significant difference compared to the previous dose.
At concentrations greater than 37.5 μg/mL, the biofilm formation gradually resumes increasing for both test strains. High concentrations probably allow the formation of intra- or inter-molecular hydrogen bond between the hydroxyl group at C-3 and the carbonyl at C-9 in 3. However, this hypothesis needs to be confirmed.
Compound 3, as above reported, differed from both 1 and 2, for lack of the double bound between C-10 and C-11. Consequently, a nucleophile Michael addiction to the α, β-unsaturated carbonyl group as in 1 and 2 could be not possible. A different mechanism of action of 3 can be suggested with respect to that of 1 and 2. This structural factor confers to compound 3 a greater conformational freedom than 1 and 2, as also observed by an inspection of a Drieding model.
Biofilm formation is a complex process that takes place through several stages: Adhesion of bacterial cell to a surface, cell multiplication, production of the extracellular matrix, and dispersal. Communication between microbial cells through the quorum sensing system is critical during biofilm formation. Quorum sensing also regulates the expression of virulence genes and the metabolic activity of bacterial cells [47]. Rukayadi et al. [48] showed that xanthorrhizol, a bisabolane-type sesquiterpenoid extracted from Curcuma xanthorrhiza, inhibited biofilm formation by Streptococcus mutans in the adhesion phase. Alves et al. [49] reported that linalool, a monoterpenoid present in the essential oil of Coriandrum sativum, showed anti-biofilm activity against A. baumanni by inhibiting bacterial adhesion and interfering with the quorum-sensing system. T-farnesol, a natural sesquiterpenoid alcohol found in propolis, was able to markedly reduce the bacterial viability and production of extracellular insoluble polysaccharide in the S. mutans biofilm [50]. Farnesol was also effective in reducing the average thickness and substrate coverage of Staphylococcus epidermidis biofilm, even in the case of quorum sensing mutants [51]. Further studies will be useful to understand if compound 3 interferes with the adhesion, growth, cell-to-cell communication, or maturation phase of the biofilm.
The structural differences between the three compounds could determine a different interaction with components of the bacterial surface or the intercellular matrix and explain their different antibiofilm activities. Therefore, structure-function correlation studies may suggest modifications to these skeletons to enhance antibacterial activity.
3. Materials and Methods
3.1. General Experimental Procedures
1H and 13C nuclear magnetic resonance (NMR) spectra were recorded at 400 and 100 MHz, respectively, in CDCl3 by Bruker spectrometers (Karlsruhe, Germany). The same solvent was used as an internal standard. Carbon multiplicities were determined using distortions enhancement by polarization transfer (DEPT) spectra [52]. DEPT, correlation spectroscopy with a 45° mixing pulse (COSY-45), heteronuclear single quantum correlation (HSQC), and heteronuclear multiple bond correlation (HMBC) experiments [52] were performed using Bruker microprograms. Electrospray ionization mass spectra (ESIMS) and liquid chromatography/mass spectrometry (LC/MS) analyses were carried out using the LC/MS TOF system (Agilent 6230B, HPLC 1260 Infinity) (Milan, Italy). The high-performance liquid chromatography (HPLC) separation was performed using a Phenomenex LUNA (C18 (2) 5 u 150 × 4.6 mm) (Torrance, CA, USA). Analytical, preparative, and reverse phase thin-layer chromatography (TLC) were carried out on silica gel (Merck, Kieselgel 60, F254, 0.25, 0.5 mm, and RP-18 F254s, respectively) plates (Merck, Darmstadt, Germany). The spots were visualized by exposure to ultraviolet (UV) radiation, or by spraying first with 10% H2SO4 in MeOH, and then with 5% phosphomolybdic acid in EtOH, followed by heating at 110 °C for 10 min. Column chromatography (CC) was performed using silica gel (Kieselgel 60, 0.063–0.200 mm) (Merck, Darmstadt, Germany). All the solvents were supplied by Sigma-Aldrich (Milan, Italy).
3.2. Plant Material
Whole aerial parts of Chiliadenus lopadusanus plants were collected fresh at a pre-flowering stage in May 2019 in Lampedusa island (Italy) by Mr. Fabio Giovanetti and identified by Prof. G. Surico, University of Florence, Italy. The plant specimen is deposited in the collection of Department of Agriculture, Food, Environment, and Forestry (DAGRI), Section of Agricultural Microbiology, Plant Pathology and Enthomology, University of Florence, Italy, n. DAGRI-56. The air-dried plant material was then grinded to obtain a tiny powder using a laboratory mill and packaged in plastic bags under a vacuum until its use.
3.3. Isolation of Fungal Metabolites
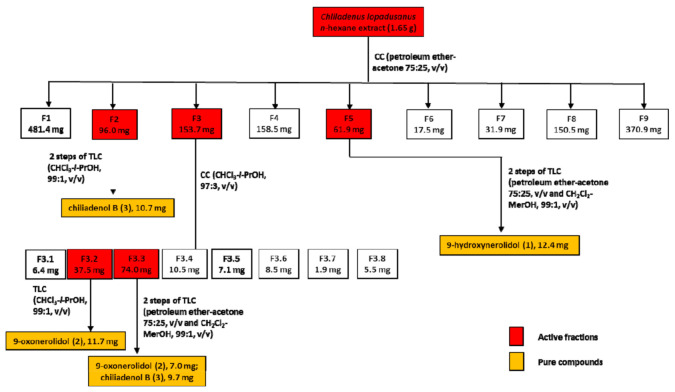
Plant material (450 g) was extracted (1 × 1 L) by H2O/MeOH (1/1, v/v) under stirred conditions at room temperature for 24 h, the suspension centrifuged and the supernatant extracted by n-hexane (3 × 400 mL) and successively with CH2Cl2 (3 × 400 mL). The residue (1.65 g) of n-hexane organic extract, showing interesting antibacterial activity against S. aureus and A. baumannii, was purified by CC eluted with petroleum ether/acetone (75/25, v/v), yielding nine groups of homogeneous fractions. Among them, the residues of fractions F2, F3, and F5 retained an antibiotic activity and were further purified using different steps of CC and TLC, as shown in Figure 6.
Figure 6.
Chromatographic purification diagram of the metabolites extracted from C. lopadusanus.
F2 was further purified by two TLC steps giving a homogeneous compound identified as chiliadenol B (3, Rf 0.65, 10.7 mg). F3 was further purified by CC yielding eight groups of homogeneous fractions. Among them, only fractions F3.2 and F3.3 retain the activity. The purification of F3.2 by TLC gave a homogeneous compound identified as 9-oxonerolidol (2, Rf 0.65, 11.7 mg). F.3.3 was further purified through two TLC steps giving a further amount of chiliadenol B (3, 9.7 mg) and of 9-oxonerolidol (2, 7.0 mg). The residue of F5 of the original column was further purified by two TLC steps giving a pure oil identified as 9-hydroxynerolidol (1, Rf 0.65, 12.4 mg).
3.3.1. 9-Hydroxynerolidol (1)
9-Hydroxynerolidol (1): [α]25D + 5.2 (c 0.04, CHCl3) (lit. [33]: [α]25D + 0 (5 mg/mL, EtOH); 1H NMR (see Table S1), δ (J in Hz): 5.93 (dd, 17.2 and 10.7, H-2), 5.29 (br t, 7.3, H-6), 5.23 (dd, 17.2 and 1.2, H-1A), 5.17 (br dd, 8.5 and 1.3, H-10), 5.08 (dd, 10.7 and 1.2, H-1B), 4.66 (ddd, 11.8, 8.5 and 2.7, H-9), 2.10 (2H, m, H-4), 2.02 (2H, m, H-8), 1.74 (3H, s, Me-12), 1.71 (3H, s, Me-13), 1.68 (3H, s, Me-14), 1.60 (2H, m, H-5), 1.30 (s, Me-15); 13C NMR (see Table S1), δ: 144.9 (d, C-2), 134.6 (s, C-7), 131.8 (s, C-11), 128.4 (d, C-10), 127.5 (d, C-6), 111.7 (t, C-1), 73.4 (s, C-3), 66.0 (d, C-9), 48.1 (t, C-8), 41.8 (t, C-4), 27.9 (q, C-15), 25.7 (q, Me-12), 22.9 (t, C-5), 18.1 (q, Me-13), 16.2 (q, Me-14); ESIMS (+), m/z 221 [M − H2O + H]+, 239 [M + H]+.
3.3.2. 9-Oxoxynerolidol (2)
9-Oxoxynerolidol (2): [α]25D + 14.4 (c 0.04, CHCl3) (lit. [34]: [α]25D + 15.38 (CCl4); (lit. Stoessl et al., 1975) [α]25D + 24 (c 1.0, CCl4); 1H NMR (see Table S2), δ (J in Hz): 6.11 (s, H-10), 5.94 (dd, 17.5 and 10.5, H-2), 5.29 (br t, 7.0, H-6), 5.26 (br d, 17.5, H-1A), 5.09 (br d, 10.5, H-1B), 3.06 (2H, s, H-8), 2.16 (3H, s, Me-13), 2.10 (2H, m, H-5), 1.90 (3H, s, Me-12), 1.63 (3H, s, Me-14), 1.62 (3H, m, H-4), 1.31 (3H, s, Me-15); 13C NMR (see Table S2), δ: 199.2 (s, C-9), 155.7 (s, C-11), 144.5 (d, C-2), 129.9 (s, C-7), 129.1 (d, C-10), 122.4 (d, C-6), 111.5 (t, C-1), 73.0 (s, C-3), 55.3 (t, C-8), 41.3 (t, C-4), 27.9 (q, Me-15), 27.5 (q, Me-12), 22.9 (t, C-5), 20.4 (q, Me-13), 16.3 (q, Me-14); ESIMS (+), m/z 219 [M − H2O + H]+, 237 [M + H]+.
3.3.3. Chiliadenol B (3)
Chiliadenol B (3): [α]25D + 4.0 (c 0.04, CHCl3) (lit. [28]: [α]25D + 3.67 (c 0.03, CHCl3); 1H NMR (see Table S3), δ (J in Hz): 5.94 (dd, 17.3 and 10.7, H-2), 5.28 (t, 7.3, H-6), 5.26 (br d, 17.3, H-1A), 5.10 (br d, 10.7, H-1B), 3.04 (2H, s, H-8), 2.30 (2H, d, 6.7, H-10), 2.14 (m, H-11), 2.10 (2H, m, H-5), 1.67 (2H, m, H-4), 1.62 (3H, s, Me-14), 1.31 (3H, s, Me-15), 0.93 (3H, br s, Me-12), 0.91 (3H, br s, Me-13); 13C NMR (see Table S3), δ: 209.4 (s, C-9), 144.8 (d, C-2), 129.4 (d, C-6), 128.9 (s, C-7), 73.0 (s, C-3), 54.0 (t, C-8), 50.4 (t, C-10), 41.4 (t, C-4), 27.9 (q, Me-15), 24.2 (t, C-11), 22.7 (t, C-5), 22.6 (q, overlapped signals of Me-12 and Me-13), 16.3 (q, Me-14); ESIMS (+), m/z 221 [M − H2O + H]+, 239 [M + H]+.
3.4. Test Bacterial Strains and Culture Conditions
Bacterial strains used in this study were methicillin-resistant Staphylococcus aureus ATCC 43,300, and Acinetobacter baumannii ATCC 747. All strains were stored as 15% (v/v) glycerol stocks at −80 °C. Before each experiment, cells were sub-cultured from the stocks onto tryptic soy agar (TSA; Becton Dickinson, Franklin Lakes, NJ, USA) plates at 37 °C for 24 h. The identification and antibiotic susceptibility profile of the reference bacteria were performed using the Vitek II (bioMérieux, Marcy-l’Étoile, France) and Phoenix (Becton Dickinson) systems.
3.5. Antimicrobial Assays
The antibacterial activity of plant extract and secondary metabolites was assayed on test strains by a standard broth micro-dilution method in 96-well polystyrene plates using Mueller-Hinton Broth 2 (MHB2). For each strain, starting from bacterial suspensions with a turbidity of 0.5 McFarland (corresponding to 1–5 × 108 cells/mL) and subsequently adjusted to approximately 5 × 106 CFU/mL, 100 μL aliquots of these bacterial suspensions were dispensed in all the wells. Then, the activity of the extract was tested by adding 100 µL of a 500 µg/mL solution to the wells, while to test the three metabolites the wells were added with 100 μL of two-fold dilutions starting from 300 µg/mL. The wells without substances were used as a positive growth control. Conventional antibiotics, selected depending on antibiotic-susceptibility profiles of the test strains, were included as the control: Colistin (ranged from 0.2 to 12.5 µg/mL) was used for A. baumannii and teicoplanin (ranged from 0.5 to 4 µg/mL) for S. aureus. Plates were incubated at 37 °C for 19 h under shaking (300 rpm). Then, the medium turbidity was measured by a spectrophotometer at 595 nm (Bio-Rad Laboratories Srl, Hercules, CA, USA). The antimicrobial activity was expressed as a percentage of microbial growth inhibition.
The minimal inhibitory concentration (MIC) and minimal bactericidal concentration (MBC) of secondary metabolites were determined: The MIC was defined as the lowest concentration of metabolite that caused no visible bacterial growth in the wells. The MBC was defined as the lowest compound concentration that yields no microbial growth on the agar plates of each sample, previously treated with compound concentrations equal to or higher than the MIC. The extract and each metabolite were tested in triplicate and each experiment was performed twice. To be sure that the 2% of dimethyl sulfoxide (DMSO; Sigma-Aldrich, St. Louis, MO, USA) present in the 2× stock solutions of the metabolites did not act on the bacterial growth, the effect of serial dilutions of DMSO starting from 1% on the growth of the test strains was separately tested.
3.6. Biofilm Formation Inhibition Assay
The total biomass of the biofilm formed in vitro in the presence of the test compounds was analyzed using the crystal violet (CV) staining method in flat-bottomed 96-well microplates, as described by Stepanović et al. [53]. For each strain, a cell suspension in MHB2 supplemented with 10% (w/v) glucose was prepared and diluted to obtain a suspension of 1 × 106 CFU/mL. One hundred microliters of this suspension were incubated with 100 µL of serial dilutions of sub-MIC concentrations in MHB2 of the compounds test. The negative control was represented by the microbial suspension inactivated by boiling. The positive controls were compound-free wells. The microtiter was incubated at 37 °C for 19 h. The non-adherent cells were then removed with gentle aspiration and gentle washings with a phosphate-buffered saline (PBS; Sigma-Aldrich) and the biofilm was dried at 60 °C for 1 h and subsequently stained with a 0.1% (w/v) crystal violet solution for 30 min.
After washing with PBS and solubilization with absolute ethanol to release the dye from the biofilm, the spectrophotometric reading is performed at 570 nm. The absorbance recorded was correlated to the amount of biofilm produced. The percentage of biofilm mass reduction was calculated using the formula: [(Ac − At)/Ac] × 100, where Ac is the OD570 for control wells and At is the OD570 in the presence of the tested compound.
3.7. Statistical Analysis
Statistical analyses of biofilm inhibition data were carried out using the ordinary one-way analysis of variance (ANOVA) and Tukey’s multiple comparisons test. The box plots shown in this study were built by the QI Macros software and the results were presented as the mean ± standard deviation. Differences with a p < 0.005 were considered statistically significant.
4. Conclusions
Antibiotic resistance poses a major threat to human health. In medicine, plants have been used for millennia as a treatment for human diseases and can represent a source of many antibacterial compounds. For the first time, our study reports the isolation of the three sesquiterpenes, namely 9-hydroxynerolidol, 9-oxonerolidol, and chiliadenol B, from the plant C. lopadusanus Brullo. The antimicrobial activity of compounds 9-hydroxynerolidol and 9-oxonerolidol, as well as the anti-biofilm activity of chiliadenol B were also reported. Therefore, it would be of considerable interest to evaluate the possible use of a combination of the three compounds for the prevention of biofilm-related infections.
Acknowledgments
We thank Fabio Giovanetti who collected the plant in Lampedusa island, Italy. A. Evidente is associated with the Istituto di Chimica Biomolecolare, CNR, Pozzuoli, Italy.
Supplementary Materials
The following are available online at https://www.mdpi.com/2079-6382/10/2/148/s1. Figure S1. 1H NMR spectrum of 9-hydroxynerolidol, 1 (CDCl3, 400 MHz); Figure S2. 13C NMR spectrum of 9-hydroxynerolidol, 1 (CDCl3, 100 MHz). Figure S3. COSY spectrum of 9-hydroxynerolidol, 1 (CDCl3, 400 MHz); Figure S4. HSQC spectrum of 9-hydroxynerolidol, 1 (CHCl3, 400/100 MHz); Figure S5. HMBC spectrum of 9-hydroxynerolidol, 1 (CHCl3, 400/100 MHz); Figure S6. NOESY spectrum of 9-hydroxynerolidol, 1 (CDCl3, 400 MHz). Figure S7. ESIMS spectrum of 9-hydroxynerolidol, 1, recorded in positive modality; Figure S8. 1H NMR spectrum of 9-oxonerolidol, 2 (CDCl3, 400 MHz); Figure S9. 13C NMR spectrum of 9-oxonerolidol, 2 (CDCl3, 100 MHz). Figure S10. COSY spectrum of 9-oxonerolidol, 2 (CDCl3, 400 MHz); Figure S11. HSQC spectrum of 9-oxonerolidol, 2 (CDCl3, 400/100 MHz); Figure S12. HMBC spectrum of 9-oxonerolidol, 2 (CDCl3, 400/100 MHz). Figure S13. NOESY spectrum of 9-oxonerolidol, 2 (CDCl3, 400 MHz); Figure S14. ESIMS spectrum of 9-oxonerolidol, 2, recorded in positive modality; Figure S15. 1H NMR spectrum of chiliadenol B, 3 (CDCl3, 400 MHz); Figure S16. 13C NMR spectrum of chiliadenol B, 3 (CDCl3, 100 MHz); Figure S17. COSY spectrum of chiliadenol B, 3 (CDCl3, 400 MHz); Figure S18. HSQC spectrum of chiliadenol B, 3 (CDCl3, 400/100 MHz); Figure S19. HMBC spectrum of chiliadenol B, 3 (CDCl3, 400/100 MHz); Figure S20. NOESY spectrum of chiliadenol B, 3 (CDCl3, 400 MHz); Figure S21. ESIMS spectrum of chiliadenol B, 3 recorded in positive modality. Table S1. 1H and 13C NMR data of 9-hydroxynerolidol (1); Table S2. 1H and 13C NMR data of 9-oxonerolidol (2); Table S3. 1H and 13C NMR data of chiliadenol B (3).
Author Contributions
Conceptualization, E.R., M.M., A.C., M.R.C., G.S. and A.E.; methodology, E.R., M.M., and A.C.; investigation, E.R., M.M. and A.C.; data curation, E.R., M.R.C., M.M., A.C. and A.E.; writing—original draft preparation, E.R., M.R.C., M.M., A.C. and A.E.; writing—review and editing, M.R.C., A.C., G.S. and A.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the text.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) Antimicrobial Resistance No Time to Wait: Securing the Future from Drug-Resistant Infections. Report to the Secretary-General of the United Nations. [(accessed on 8 April 2020)]; Available online: https://www.who.int/antimicrobial-resistance/interagency-coordination-group/IACG_final_report_EN.pdf?ua=1.
- 2.Da Costa P.M., Loureiro L., Matos A.J. Transfer of multidrug-resistant bacteria between intermingled ecological niches: The interface between humans, animals and the environment. Int. J. Environ. Res. Public Health. 2013;1:278–294. doi: 10.3390/ijerph10010278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Argudín M.A., Deplano A., Meghraoui A., Dodémont M., Heinrichs A., Denis O., Nonhoff C., Roisin S. Bacteria from animals as a pool of antimicrobial resistance genes. Antibiotics. 2017;6:12. doi: 10.3390/antibiotics6020012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Food Safety Authority, European Centre for Disease Prevention and Control The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2017. EFSA J. 2019;17:5598. doi: 10.2903/j.efsa.2019.5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoelzer K., Wong N., Thomas J., Talkington K., Jungman E., Coukell A. Antimicrobial drug use in food-producing animals and associated human health risks: What, and how strong, is the evidence? BMC Vet. Res. 2017;13:211. doi: 10.1186/s12917-017-1131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marturano J.E., Lowery T.J. ESKAPE pathogens in bloodstream infections are associated with higher cost and mortality but can be predicted using diagnoses upon admission. Open Forum Infect. Dis. 2019;6:ofz503. doi: 10.1093/ofid/ofz503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giraldi G., Montesano M., Napoli C., Frati P., La Russa R., Santurro A., Scopetti M., Orsi G.B. Healthcare-associated infections due to multidrug-resistant organisms: A surveillance study on extra hospital stay and direct costs. Curr. Pharm. Biotechnol. 2019;20:643–652. doi: 10.2174/1389201020666190408095811. [DOI] [PubMed] [Google Scholar]
- 8.Yelin I., Kishony R. Antibiotic resistance. Cell. 2018;172:1136. doi: 10.1016/j.cell.2018.02.018. [DOI] [PubMed] [Google Scholar]
- 9.Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D.L., Pulcini C., Kahlmeter G., Kluytmans J., Carmeli Y., et al. Discovery, research, and development of new antibiotics: The Who Priority List of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018;18:318–327. doi: 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 10.Hall C.W., Mah T.F. Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol. Rev. 2017;41:276–301. doi: 10.1093/femsre/fux010. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen T.B., Brass E.P., Gilbert D.N., Bartlett J.G., Spellberg B. Sustainable discovery and development of antibiotics—is a nonprofit approach the future? N. Engl. J. Med. 2019;381:503–505. doi: 10.1056/NEJMp1905589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ventola C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015;40:277–283. [PMC free article] [PubMed] [Google Scholar]
- 13.Dg B., Lister T., May-Dracka T.L. New natural products as new leads for antibacterial drug discovery. Bioorganic Med. Chem. Lett. 2014;24:413–418. doi: 10.1016/j.bmcl.2013.12.059. [DOI] [PubMed] [Google Scholar]
- 14.Betts J.W., Hornsey M., La Ragione R.M. Novel antibacterials: Alternatives to traditional antibiotics. Adv. Microb. Physiol. 2018;73:123–169. doi: 10.1016/bs.ampbs.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Roscetto E., Masi M., Esposito M., Di Lecce R., Delicato A., Maddau L., Calabrò V., Evidente A., Catania M.R. Anti-Biofilm activity of the fungal phytotoxin sphaeropsidin A against clinical isolates of antibiotic-resistant bacteria. Toxins. 2020;12:444. doi: 10.3390/toxins12070444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dewick P.M. Medicinal Natural Products. 3rd ed. John Wiley and Sons Ltd.; Chicester, UK: 2009. [Google Scholar]
- 17.Osbourn A.E., Lanzotti V. Plant-Derived Natural Products. Springer; Dordrecht, The Netherlands: 2009. [Google Scholar]
- 18.Newman D.J., Cragg G.M. Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J. Nat. Prod. 2020;83:770–803. doi: 10.1021/acs.jnatprod.9b01285. [DOI] [PubMed] [Google Scholar]
- 19.Ferrazzano G.F., Roberto L., Catania M.R., Chiaviello A., De Natale A., Roscetto E., Pinto G., Pollio A., Ingenito A., Palumbo G. Screening and scoring of antimicrobial and biological activities of italian vulnerary plants against major oral pathogenic bacteria. Evid. Based Complement. Alternat. Med. 2013:316280. doi: 10.1155/2013/316280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollio A., Zarrelli A., Romanucci V., Di Mauro A., Barra F., Pinto G., Crescenzi E., Roscetto M., Palumbo G. Polyphenolic profile and targeted bioactivity of methanolic extracts from Mediterranean ethnomedicinal plants on human cancer cell lines. Molecules. 2016;21:395. doi: 10.3390/molecules21040395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romulo A., Ea Z., Rondevaldova J., Kokoska L. Screening of in vitro antimicrobial activity of plants used in traditional Indonesian medicine. Pharm. Biol. 2018;56:287–293. doi: 10.1080/13880209.2018.1462834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ribeiro I.C.D.O., Mariano E.G.A., Careli R.T., Morais-Costa F., De Sant’Anna F.M., Pinto M.S., De Souza M.R., Duarte E.R. Plants of the Cerrado with antimicrobial effects against Staphylococcus spp. and Escherichia coli from cattle. BMC Vet. Res. 2018;14:32. doi: 10.1186/s12917-018-1351-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oo O., Pa S., Ps F. Antimicrobial and antiprotozoal activities of twenty-four Nigerian medicinal plant extracts. S. Afr. J. Bot. 2018;117:240–246. [Google Scholar]
- 24.Ferrazzano G.F., Cantile T., Roberto L., Ingenito A., Catania M.R., Roscetto E., Palumbo G., Zarrelli A., Pollio A. Determination of the in vitro and in vivo antimicrobial activity on salivary Streptococci and Lactobacilli and chemical characterisation of the phenolic content of a Plantago lanceolata infusion. BioMed Res. Int. 2015;2015:286817. doi: 10.1155/2015/286817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bocquet L., Sahpaz S., Bonneau N., Beaufay C., Mahieux S., Samaillie J., Roumy V., Jacquin J., Bordage S., Hennebelle T., et al. Phenolic compounds from Humulus lupulus as natural antimicrobial products: New weapons in the fight against methicillin resistant Staphylococcus aureus, Leishmania mexicana and Trypanosoma brucei strains. Molecules. 2019;24:1024. doi: 10.3390/molecules24061024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naz R., Roberts T.H., Bano A., Nosheen A., Yasmin H., Hassan M.N., Keyani R., Ullah S., Khan W., Anwar Z. GC-MS analysis, antimicrobial, antioxidant, antilipoxygenase and cytotoxic activities of Jacaranda mimosifolia methanol leaf extracts and fractions. PLoS ONE. 2020;15:e0236319. doi: 10.1371/journal.pone.0236319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zito P., Sajeva M., Scirica E., Bruno M., Maggio A., Senatore F. Essential oils of Chiliadenus lopadusanus (Asteraceae) Nat. Prod. Commun. 2013;8:1159–1162. doi: 10.1177/1934578X1300800833. [DOI] [PubMed] [Google Scholar]
- 28.Sacco T., Maffei M. Essential oil of Chiliadenus lopadusanus growing spontaneously in Lampedusa Island (Italy) Planta Med. 1987;53:582. doi: 10.1055/s-2007-969050. [DOI] [PubMed] [Google Scholar]
- 29.Hammerschmidt F.J., Clark A.M., Soliman F.M., El-Kashoury E.S.A., El-Kawy M.M.A., El-Fishawy A.M. Chemical composition and antimicrobial activity of essential oils of Jasonia candicans and Jasonia montana. Planta Med. 1993;59:68–70. doi: 10.1055/s-2006-959607. [DOI] [PubMed] [Google Scholar]
- 30.Satyal P., Paudel P., Kafle A., Pokharel S.K., Lamichhane B., Dosoky N.S., Moriarity D.M., Setzer W.N. Bioactivities of volatile components from Nepalese Artemisia species. Nat. Prod. Commun. 2012;7:1651–1658. doi: 10.1177/1934578X1200701228. [DOI] [PubMed] [Google Scholar]
- 31.Guillén M.D., Ibargoitia M.L. Volatile components obtained from the leaves of Jasonia glutinosa. Food Chem. 1996;56:155–158. doi: 10.1016/0308-8146(95)00156-5. [DOI] [Google Scholar]
- 32.Romero V., Costas-Mora I., Lavilla I., Bendicho C. Cold vapor-solid phase microextraction using amalgamation in different Pd-based substrates combined with direct thermal desorption in a modified absorption cell for the determination of Hg by atomic absorption spectrometry. Spectrochim. Acta Part B At. Spectrosc. 2011;66:156–162. doi: 10.1016/j.sab.2011.01.005. [DOI] [Google Scholar]
- 33.Avato P., Raffo F., Aldouri N.A., Vartanian S.T. Essential oils of Varthemia iphionoides from Jordan. Flavour Fragr. J. 2004;19:559–561. doi: 10.1002/ffj.1351. [DOI] [Google Scholar]
- 34.Hegazy M.E.F., Matsusa H., Nakamura S., Hussein T.A., Yoshikawa M., Parè P.W. Chemical constituents and their antibacterial and antifungal activity from the Egyptian herbal medicine Chiliadenus montanus. Phytochemistry. 2014;103:154–161. doi: 10.1016/j.phytochem.2014.03.027. [DOI] [PubMed] [Google Scholar]
- 35.Stoessl A., Stothers J.B., Ward E.W.B. The structures of some stress metabolites from Solanum melongena. Can. J. Chem. 1975;53:3351–3358. doi: 10.1139/v75-478. [DOI] [Google Scholar]
- 36.Hiroi M., Takaoka D. 9-oxonerolidol from camphor leaf oil. Chem. Lett. 1972;1:1213–1214. doi: 10.1246/cl.1972.1213. [DOI] [Google Scholar]
- 37.Zengin H., Baysal A.H. Antibacterial and antioxidant activity of essential oil terpenes against pathogenic and spoilage-forming bacteria and cell structure-activity relationships evaluated by SEM microscopy. Molecules. 2014;19:17773–17798. doi: 10.3390/molecules191117773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guimarães A.C., Meireles L.M., Lemos M.F., Guimarães M.C.C., Endringer D.C., Fronza M., Scherer R. Antibacterial activity of terpenes and terpenoids present in essential oils. Molecules. 2019;24:2471. doi: 10.3390/molecules24132471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aleksic Sabo V., Nikolic I., Mimica-Dukic N., Knezevic P. Anti-Acinetobacter baumannii activity of selected phytochemicals alone, in binary combinations and in combinations with conventional antibiotics. Nat. Prod. Res. 2020:1–4. doi: 10.1080/14786419.2020.1808635. [DOI] [PubMed] [Google Scholar]
- 40.Xu J., Zhou F., Ji B.P., Pei R.S., Xu N. The antibacterial mechanism of carvacrol and thymol against Escherichia coli. Lett. Appl. Microbiol. 2008;47:174–179. doi: 10.1111/j.1472-765X.2008.02407.x. [DOI] [PubMed] [Google Scholar]
- 41.Kachur K., Suntres Z. The antibacterial properties of phenolic isomers, carvacrol and thymol. Crit. Rev. Food Sci. Nutr. 2020;60:3042–3053. doi: 10.1080/10408398.2019.1675585. [DOI] [PubMed] [Google Scholar]
- 42.Gomes F.I.A., Teixeira P., Azeredo J., Oliveira R. Effect of farnesol on planktonic and biofilm cells of Staphylococcus epidermidis. Curr. Microbiol. 2009;59:118–122. doi: 10.1007/s00284-009-9408-9. [DOI] [PubMed] [Google Scholar]
- 43.Hu Z.B., Yu X.Q., Wang B., Liu A.H., Zhao T.S., Guo Y.W., Huang H.L., Mao S.C. Structurally diverse halosesquiterpenoids from the red alga Laurencia composita Yamada. Fitoterapia. 2020;146:104716. doi: 10.1016/j.fitote.2020.104716. [DOI] [PubMed] [Google Scholar]
- 44.Evidente A., Kornienko A., Cimmino A., Andolfi A., Lefranc F., Mathieu V., Kiss R. Fungal metabolites with anticancer activity. Nat. Prod. Rep. 2014;31:617–627. doi: 10.1039/C3NP70078J. [DOI] [PubMed] [Google Scholar]
- 45.Masi M., Nocera P., Reveglia P., Cimmino A., Evidente A. Fungal metabolites antagonists towards plant pests and human pathogens: Structure-activity relationship studies. Molecules. 2018;23:834. doi: 10.3390/molecules23040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li Y.R., Fu C.S., Yang W.J., Wang X.L., Feng D., Wang X.N., Ren D.-M., Lou H.-X., Shen T. Investigation of constituents from Cinnamomum camphora (L.) J. Presl and evaluation of their anti-inflammatory properties in lipopolysaccharide-stimulated RAW 264.7 macrophages. J. Ethnopharmacol. 2018;221:37–47. doi: 10.1016/j.jep.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 47.Li Y.H., Tian X. Quorum sensing and bacterial social interactions in biofilms. Sensors. 2012;12:2519–2538. doi: 10.3390/s120302519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rukayadi Y., Hwang J.K. In vitro activity of xanthorrhizol against Streptococcus mutans biofilms. Lett. Appl. Microbiol. 2006;42:400–404. doi: 10.1111/j.1472-765X.2006.01876.x. [DOI] [PubMed] [Google Scholar]
- 49.Alves S., Duarte A., Sousa S., Domingues F.C. Study of the major essential oil compounds of Coriandrum sativum against Acinetobacter baumannii and the effect of linalool on adhesion, biofilms and quorum sensing. Biofouling. 2016;32:155–165. doi: 10.1080/08927014.2015.1133810. [DOI] [PubMed] [Google Scholar]
- 50.Leyva Del Rio D., Sartori N., Tomblin N.B., Phark J.H., Pardi V., Murata R.M., Duarte S., Jr. Bioactive dental adhesive system with tt-farnesol: Effects on dental biofilm and bonding properties. Front. Bioeng. Biotechnol. 2020;8:865. doi: 10.3389/fbioe.2020.00865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pammi M., Liang R., Hicks J.M., Barrish J., Versalovic J. Farnesol decreases biofilms of Staphylococcus epidermidis and exhibits synergy with nafcillin and vancomycin. Pediatr. Res. 2011;70:578–583. doi: 10.1203/PDR.0b013e318232a984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berger S., Braun S. 200 and More Basic NMR Experiments—A Practical Course. 1st ed. Wiley-VCH; Weinheim, Germany: 2004. [Google Scholar]
- 53.Stepanović S., Vuković D., Hola V., Di Bonaventura G., Djukić S., Cirković I., Ruzicka F. Quantification of biofilm in microtiter plates: Overview of testing conditions and practical recommendations for assessment of biofilm production by Staphylococci. APMIS. 2007;115:891–899. doi: 10.1111/j.1600-0463.2007.apm_630.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are contained within the text.