Abstract
The Community Health Club (CHC) model is a community-based health promotion program that utilizes water, sanitation, and hygiene (WASH) education as the first stage of a longitudinal development process. Although the CHC model has been implemented in fourteen countries over 20 years, this is the first review of the literature describing the model’s outcomes and impact. We conducted a review of the literature that provided quantitative or qualitative evidence of CHC interventions focused on WASH in low- and middle-income countries. We identified 25 articles that met our inclusion criteria. We found six major outcomes: WASH behaviors and knowledge, social capital, collective action, health, and cost or cost-effectiveness. The most consistent evidence was associated with WASH behaviors and knowledge, with significant effects on defecation practices, hand washing behaviors, and WASH knowledge. We also found qualitative evidence of impact on social capital and collective action. CHCs catalyze favorable changes in WASH behaviors and knowledge, yielding outcomes commensurate with other WASH promotion strategies. This review provides insights into the model’s theory of change, helping identify areas for further investigation. The CHC model’s holistic focus and emphasis on individual and collective change offer promising potential to address multiple health and development determinants.
Keywords: water, sanitation and hygiene, community health clubs, health promotion, behavior change, community-based
1. Introduction
The impact of inadequate water, sanitation, and hygiene (WASH) is significant. Approximately 4.2% of global morbidity is attributable to inadequate WASH, the majority of which is associated with infectious diarrhea, which kills more children under the age of five each year than HIV/AIDS, tuberculosis, and malaria combined [1,2,3]. Although global access to clean water and safe sanitation has improved since 1990, 785 million people remain without access to basic drinking water sources, 2 billion people remain without access to basic sanitation services, and 3 billion people still lack basic hand washing facilities at home [4]. Furthermore, progress has been uneven, with least developed countries lagging and a growing disparity between urban and rural communities [4]. One approach to improve WASH, the Community Health Club (CHC) model, is a participatory, community-based program that holds promise because of its wide implementation and evaluation indicating positive outcomes.
Community health clubs (CHCs) are voluntary, community-based organizations that provide a forum for the dissemination of preventive health information and opportunities for consensus building, behavior change, and collective action [5]. The CHC model utilizes WASH education as the first of a four-stage integrated development process. Subsequent stages of the model vary by program, but may include nutrition, reproductive and sexual health, women’s empowerment, and income-generating activities. Under the first stage, the CHC model is designed to alter WASH practices and create demand for water and sanitation infrastructure by leveraging the power of the peer group and promoting community cohesion [6]. CHCs provide a forum for experiential learning, discussion, and problem solving that draws upon multiple behavioral theories, including the health belief model, the theory of reasoned action and planned behavior, and social learning theory, and is set within the conceptual frameworks of participatory development and social capital [6,7].
CHC theory and practice have been described in more detail elsewhere [5,6,7,8,9]. In brief, the CHC model aims to bridge the gap in WASH knowledge and behaviors by creating a peer group dedicated to learning and taking collective action to improve the health of their community [5,6]. CHCs aim to facilitate changes in communal norms and values by promoting community cohesion, creating collective knowledge, and building group consensus. The model recognizes that knowledge is necessary for WASH behavior change but is insufficient without a critical mass providing individuals an incentive to change based upon the need for group conformity. To normalize new behaviors and achieve shared values, CHCs meet weekly at a regular venue where people explore their individual and collective knowledge using participatory health education techniques. These techniques encourage people to engage with new ideas and compare traditional knowledge and beliefs with current scientific knowledge and safe practices. This process of self-discovery, facilitated by a trained community health worker, rather than top-down transfer of knowledge through expert advice, is essential to the creation of new knowledge and achievement of sustainable behavioral changes and collective action.
Although several WASH education and behavior change interventions have been implemented and researched over the past 25 years (e.g., participatory hygiene and sanitation transformation, community-led total sanitation, sanitation marketing, total sanitation), the CHC model merits special attention due to its holistic WASH focus (e.g., not just hand washing or latrine construction) and relatively widespread dissemination [10]. Since 1994, over 3000 CHCs have been formed in low- and middle-income countries, benefiting over two million people across Africa, Asia, and the Caribbean. To date, CHC programs focused primarily on WASH have been implemented in both rural and urban communities in Zimbabwe, Uganda, South Africa, Rwanda, Sierra Leone, Tanzania, Kenya, Burkina Faso, the Democratic Republic of Congo, Namibia, Haiti, Dominican Republic, Vietnam, and Papua New Guinea [11].
Despite widespread use of the CHC model across different contexts over the past 20 years, gaps remain to strengthen and improve its implementation and evaluation. Apart from Zimbabwe, where CHCs originated, the model has only been implemented and evaluated at scale in Rwanda [12]. To our knowledge, the peer-reviewed literature has never been systematically reviewed in order to synthesize and describe the impact of the model. Therefore, we conducted a comprehensive literature review of CHC programs, focused specifically on the first stage of WASH promotion. Our specific aims were to: (1) identify the commonly reported outcomes of CHC WASH programs and (2) synthesize the impact of CHC programs by each outcome. This review expands our understanding of the outcomes of a commonly used WASH promotion intervention, thereby allowing practitioners and researchers alike to more effectively compare outcomes across WASH promotion interventions. This manuscript also synthesizes the WASH outcomes most commonly associated with the CHC model, informing our understanding of this model’s theory of change and enhancing future evaluations of this intervention.
2. Materials and Methods
We conducted a review of the CHC literature using the PubMed, Global Health, Scopus, and Google Scholar electronic databases. We identified additional studies and manuscripts through expert recommendations and by mining the citations of relevant articles discovered through the database search. The search terms for our database search strategy are provided in Table 1. The final search was completed on 28 April 2020.
Table 1.
Community health club (CHC) literature review search terms.
| Concept | Key Words/Search Terms |
|---|---|
| Community Health Club | “Community Health Club” OR “Health Club” |
| AND | |
| Water, Sanitation, and Hygiene (WASH) | “water” OR “sanitation” OR “hygiene” OR “WASH” OR “WaSH” OR “WatSan” OR “WATSAN” OR “water and sanitation” |
To be included in this review, studies and papers had to: (1) describe and evaluate CHC interventions focused only on WASH in low- and middle-income countries; (2) provide empirical and/or qualitative evidence of the impact of a CHC intervention; and (3) be published in English. Due to limited peer-reviewed evidence describing the impact of CHC WASH interventions, this review included published papers, program reports, conference proceedings, and working papers. Studies and papers were excluded if: (1) the focus of the CHC intervention was not WASH; (2) the intervention was implemented in a high-income country; and (3) a study referenced or utilized previously reported monitoring or evaluation data. For studies that referenced previously reported data, we retained the document that reported the data first and excluded all subsequent citations.
We first screened articles by title, abstract, and keywords to remove clearly irrelevant articles. We then reviewed the full text of the remaining articles for adherence to our inclusion and exclusion criteria. The following information was then abstracted from each of the included articles: type of article (e.g., peer-reviewed journal article, doctoral dissertation, master’s thesis, conference paper, working paper, and programmatic report), study design or methods, reported outcomes, and country. Data were extracted into Microsoft OneNote for Windows 10 (Version 16001.13328.20478.0) and Microsoft Excel for Microsoft 365 (Version 13127.21064), Redmond, WA, USA.
3. Results
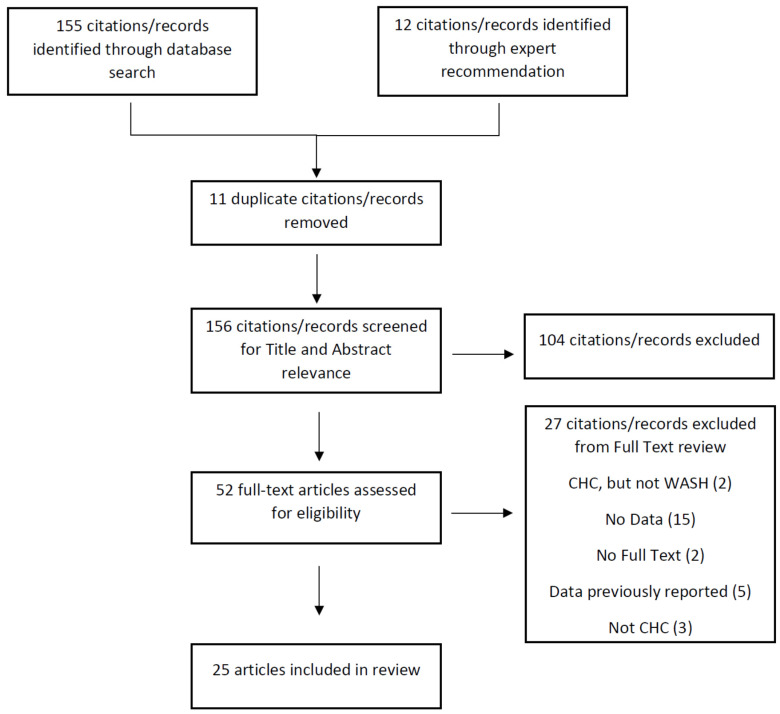
Twenty-five citations were included in this review. Figure 1 shows the PRISMA diagram of the study selection process. The characteristics of the articles, including the main outcomes measured, are presented in Table 2, while Table 3 presents the article’s study samples, measures, and results. Our review included five peer-reviewed research articles [6,7,8,12,13], seven conference papers [14,15,16,17,18,19,20], six master’s theses [21,22,23,24,25,26], four program reports [27,28,29,30], two doctoral dissertations [5,9], and one working paper [31]. Of the 25 articles reviewed, eleven used a cross-sectional study design [5,6,7,14,16,17,22,23,24,25,27], five utilized a quasi-experimental design [9,18,19,20,31], three utilized a case study design [8,13,21], three reported qualitative data abstracted from field reports and site visits [28,29,30], two utilized a time series design [15,26], and one used a cluster randomized controlled study design [12]. Of the 24 non-randomized designs, 14 included a comparison group [5,6,7,8,9,12,13,19,20,21,22,24,27,31] and 14 utilized mixed methods [5,6,7,8,9,13,19,20,21,22,23,25,27,31]. A majority of articles (n = 21) described CHC interventions in Africa, 11 of which were from Zimbabwe [5,6,7,13,15,17,18,21,22,23,25], followed by four from Rwanda [12,20,24,26], three from South Africa [16,18,19], three from the Democratic Republic of Congo [28,29,30], two from Uganda [14,17], and one from Sierra Leone [27]. The remaining described programs from the Caribbean island of Hispaniola in Haiti [8,9] and the Dominican Republic [31]. Finally, the articles in this review reported outcomes of CHC interventions in six categories: most (n = 23) reported WASH behavioral outcomes [5,6,7,8,9,12,13,14,16,17,18,19,20,21,22,23,24,25,26,27,28,29,31], about half (n = 13) reported changes in WASH knowledge [5,7,8,9,21,22,23,25,27,28,29,30,31], and ten reported outcomes associated with both social capital [5,6,7,8,9,13,21,22,27,29] and collective action [8,9,16,19,20,21,22,23,27,28], while six reported health outcomes [12,15,27,28,29,30] and four reported cost and cost-effectiveness outcomes [5,17,18,24].
Figure 1.
PRISMA Diagram. Note: WASH refers to Water, Sanitation and Hygiene and CHC refers to Community Health Clubs.
Table 2.
Characteristics of reviewed articles.
| Author(s) | Type of Article | Study Design | Data Source(s) | Outcome(s) | Countries |
|---|---|---|---|---|---|
| Waterkeyn, Okot, and Kwame (2005) | Conference Paper |
|
|
WASH Behaviors | Uganda |
| Waterkeyn and Cairncross (2005) | Peer-Reviewed Manuscript |
|
|
WASH Behaviors Social |
Zimbabwe |
| Waterkeyn (2005) | Conference Paper |
|
|
Health | Zimbabwe |
| Waterkeyn (2006) | Doctoral Dissertation |
|
|
WASH Behaviors WASH Knowledge Social Cost |
Zimbabwe |
| Azurduy, Stakem, and Wright (2007) | Program Report |
|
|
WASH Behaviors WASH Knowledge Social Collective Action Health |
Sierra Leone |
| Rosenfeld (2008) | Conference Paper |
|
|
WASH Behaviors Collective Action |
South Africa |
| Waterkeyn, Matimati, and Muringaniza (2009) | Conference Paper |
|
|
WASH Behaviors Cost |
Uganda and Zimbabwe |
| Waterkeyn and Rosenfeld (2009) | Conference Paper |
|
|
WASH Behaviors Cost |
South Africa and Zimbabwe |
| Maksimoski and Waterkeyn (2010) | Conference Paper |
|
|
WASH Behaviors Collective Action |
South Africa |
| Whaley and Webster (2011) | Peer-Reviewed Manuscript |
|
|
WASH Behaviors Social |
Zimbabwe |
| Ncube (2013) | Master’s Thesis |
|
|
WASH Behaviors WASH Knowledge Social Collective Action |
Zimbabwe |
| Waterkeyn and Waterkeyn (2013) | Peer-Reviewed Manuscript |
|
|
WASH Behaviors WASH Knowledge Social |
Zimbabwe |
| Chingono (2013) | Master’s Thesis |
|
|
WASH Behaviors WASH Knowledge Social Collective Action |
Zimbabwe |
| Brooks et al. (2015) | Peer-Reviewed Manuscript |
|
|
WASH Behaviors WASH Knowledge Social Collective Action |
Haiti |
| Rosenfeld and Taylor (2015) | Working Paper |
|
|
WASH Behaviors WASH Knowledge |
Dominican Republic |
| Beesley and Feeny (2016a) | Program Report |
|
|
WASH Behaviors WASH Knowledge Collective Action Health |
Democratic Republic of Congo |
| Beesley and Feeny (2016b) | Program Report |
|
|
WASH Behaviors WASH Knowledge Social Health |
Democratic Republic of Congo |
| Beesley et al. (2016) | Program Report |
|
|
WASH Knowledge Health |
Democratic Republic of Congo |
| Ndayambaje (2016) | Master’s Thesis |
|
|
WASH Behaviors Cost |
Rwanda |
| Munyoro (2016) | Master’s Thesis |
|
|
WASH Behavior WASH Knowledge Collective Action |
Zimbabwe |
| Sinharoy et al. (2017) | Peer-Reviewed Manuscript |
|
|
WASH Behaviors Health |
Rwanda |
| Ntakarutimana and Ekane (2017) | Conference Paper |
|
|
WASH Behaviors Collective Action |
Rwanda |
| Matimati (2017) | Master’s Thesis |
|
|
WASH Behaviors WASH Knowledge |
Zimbabwe |
| Pantoglou (2018) | Master’s Thesis |
|
|
WASH Behaviors | Rwanda |
| Rosenfeld (2019) | Doctoral Dissertation |
|
|
WASH Behaviors WASH Knowledge Social Collective Action |
Haiti |
Table 3.
Samples, measures, and results of reviewed articles.
| Author(s) | Sample | Reported Measures | Results |
|---|---|---|---|
| WASH Behaviors | |||
| Waterkeyn, Okot, and Kwame (2005) |
|
|
|
| Waterkeyn and Cairncross (2005) |
|
|
|
| Waterkeyn (2006) |
|
|
|
| Azurduy, Stakem, and Wright (2007) |
|
|
|
| Rosenfeld (2008) |
|
|
|
| Waterkeyn, Matimati, and Muringaniza (2009) |
|
|
|
| Waterkeyn and Rosenfeld (2009) |
|
|
|
| Maksimoski and Waterkeyn (2010) |
|
|
|
| Whaley and Webster (2011) |
|
|
|
| Ncube (2013) |
|
|
|
| Waterkeyn and Waterkeyn (2013) |
|
|
|
| Chingono (2013) |
|
|
|
| Brooks et al. (2015) |
|
|
|
| Rosenfeld and Taylor (2015) |
|
|
|
| Beesley and Feeny (2016a) |
|
|
|
| Beesley and Feeny (2016b) |
|
|
|
| Ndayambaje (2016) |
|
|
|
| Munyoro (2016) |
|
|
|
| Sinharoy et al. (2017) |
|
|
|
| Ntakarutimana and Ekane (2017) |
|
|
|
| Matimati (2017) |
|
|
|
| Pantoglou (2018) |
|
|
|
| Rosenfeld (2019) |
|
|
|
| WASH Knowledge | |||
| Waterkeyn (2006) |
|
|
|
| Azurduy, Stakem, and Wright (2007) |
|
|
|
| Ncube (2013) |
|
|
|
| Waterkeyn and Waterkeyn (2013) |
|
|
|
| Chingono (2013) |
|
|
|
| Brooks et al. (2015) |
|
|
|
| Rosenfeld and Taylor (2015) |
|
|
|
| Beesley and Feeny (2016a) |
|
|
|
| Beesley and Feeny (2016b) |
|
|
|
| Beesley et al. (2016) |
|
|
|
| Munyoro (2016) |
|
|
|
| Matimati (2017) |
|
|
|
| Rosenfeld (2019) |
|
|
|
| Social Capital | |||
| Waterkeyn and Cairncross (2005) |
|
|
|
| Waterkeyn (2006) |
|
|
|
| Azurduy, Stakem, and Wright (2007) |
|
|
|
| Whaley and Webster (2011) |
|
|
|
| Ncube (2013) |
|
|
|
| Waterkeyn and Waterkeyn (2013) |
|
|
|
| Chingono (2013) |
|
|
|
| Brooks et al. (2015) |
|
|
|
| Beesley and Feeny (2016b) |
|
|
|
| Rosenfeld (2019) |
|
|
|
| Collective Action | |||
| Azurduy, Stakem, and Wright (2007) |
|
|
|
| Rosenfeld (2008) |
|
|
|
| Maksimoski and Waterkeyn (2010) |
|
|
|
| Ncube (2013) |
|
|
|
| Chingono (2013) |
|
|
|
| Brooks et al. (2015) |
|
|
|
| Beesley and Feeny (2016a) |
|
|
|
| Munyoro (2016) |
|
|
|
| Ntakarutimana and Ekane (2017) |
|
|
|
| Rosenfeld (2019) |
|
|
|
| Health | |||
| Waterkeyn (2005) |
|
|
|
| Azurduy, Stakem, and Wright (2007) |
|
|
|
| Beesley and Feeny (2016a) |
|
|
|
| Beesley and Feeny (2016b) |
|
|
|
| Beesley et al. (2016) |
|
|
|
| Sinharoy et al. (2017) |
|
|
|
| Cost | |||
| Waterkeyn (2006) |
|
|
|
| Waterkeyn, Matimati, and Muringaniza (2009) |
|
|
|
| Waterkeyn and Rosenfeld (2009) |
|
|
|
| Ndayambaje (2016) |
|
|
|
3.1. Behavior
All but two studies included in this review reported WASH behavioral outcomes. Nineteen studies reported quantitative results [5,6,7,8,9,12,13,14,16,17,18,19,20,21,22,24,25,26,31], while four provided qualitative or observational data [23,27,28,29] related to WASH behavioral changes. We categorized behavioral outcomes into the following dimensions: sanitation, hand washing, composite WASH behavioral scores, drinking water, and other WASH practices (including environmental management, kitchen hygiene, and personal hygiene).
3.1.1. Sanitation
The majority of studies (n = 15) reported sanitation outcomes, which we further categorized into latrine construction and ownership [7,12,13,14,17,20,21,28,29], reduction in open defecation [7,8,9,13,19], and improved latrine hygiene [8,20,22,24,25] practices. Of these, 10 included a comparison group [7,8,9,12,13,19,20,21,22,24], six (40%) of which reported significant differences between samples in latrine construction and ownership [7,12,13,20], open defecation practices [7,8,13], and latrine hygiene [8,20]. One study reported a significant improvement in latrine hygiene behaviors from pre- to post-intervention within a sample of CHC participants [25]. Two studies from Rwanda, one randomized controlled trial (RCT) and one case–control study, reported that households who completed the full six-month WASH curriculum were significantly more likely to have a latrine post-intervention as compared to controls (RCT: 0.085, CI: 0.015–0.16, p = 0.017; CC: peri-urban: 89.4% vs. 74.2%, p = 0.0001; rural: 95.2% vs. 14.2%, p = 0.0001) [12,20]. In Zimbabwe, CHC participants were significantly more likely to practice safe sanitation (own a hygienic latrine and not practice open defecation) at final than comparison respondents (93.4% vs. 43.2%, p < 0.001) [7]. Finally, CHC participants in urban Haitian communities were significantly more likely than a comparison sample to report sharing a latrine with others rather than openly defecate (84.6% vs. 43.8%, p < 0.02) and have an observably clean latrine (74.4% vs. 38.9%, p < 0.001) [8].
3.1.2. Hand Washing
Hand washing behaviors were the second most commonly reported outcome (n = 12), which we further categorized into observations of hand washing facilities [13,17,20,21,24,28,29] and hand washing practices [8,9,22,23,25]. Of these, seven included a comparison group [8,9,13,20,21,22,24] and two (17%) reported significant results [20,25]. A retrospective case–control study of the CHC program in Rwanda reported that participants who completed the full six-month WASH curriculum were significantly more likely than controls to have an observably functional hand washing facility (peri-urban: 74.2% vs. 13.7%, p = 0.0001; rural: 91.4% vs. 43.3%, p = 0.0001) and soap (peri-urban: 38.4% vs. 7.7%, p = 0.0001; rural: 92.4% vs. 4.2%, p = 0.0001) [20]. A study comparing a CHC and Community Led Total Sanitation (CLTS) program in Zimbabwe found that households in CHC communities were significantly more likely to own a hand washing facility (64% vs. 10%, p < 0.0001) six months after the intervention and were more likely to sustain use of that facility two years later (37% vs. 2%, p < 0.0001) [13]. Finally, one study from Zimbabwe explored a dose response of CHC participation and found a significant association between the number of CHC sessions attended and the use of soap during hand washing (χ2 = 30, df = 1, p < 0.0001) [25].
3.1.3. Composite WASH Behavioral Scores
Eight of the studies reported grouped WASH behaviors [5,6,7,18,26] or composite scores of WASH behaviors [9,19,31]. These studies measured a range of 10–29 behaviors across five WASH dimensions: sanitation and defecation, drinking water, hand washing, kitchen hygiene, and environmental management. Six included a comparison group [5,6,7,9,19,31] and four (50%) reported significant results for grouped WASH behaviors [5,6,7,26]. None of the studies using composite scores reported significant results. In two studies of CHCs in Zimbabwe, the authors measured 20 observable indicators of good hygiene and reported that CHC households were significantly more likely than a comparison sample to practice 16 recommended WASH behaviors (p < 0.001) in one district, 9 recommended WASH behaviors (p < 0.01) in a second district, and 10 recommended WASH behaviors in a third district [6,7]. A retrospective analysis of program monitoring data from households in 50 communities that completed the full six-month WASH curriculum in Rwanda reported statistically significant increases in average hygiene scores (29 observable indicators) from baseline to six months (p = 0.01), after one year (p < 0.05), after two years (p < 0.05), and after three years (p < 0.05) and that 100% of hygiene indicators were observed in sample households three years after the intervention ended [26].
3.1.4. Drinking Water
Seven studies reported changes in drinking water practices [8,12,16,21,23,24,25], specifically water treatment practices [8,12,16,24,25], use of safe or improved drinking water sources [16,21], and safe drinking water storage [8,23]. Four studies included a comparison group [8,12,21,24] and two (29%) reported significant results associated with drinking water treatment behaviors [12,25]. In the Rwandan RCT, the authors reported households that completed the full six-month WASH curriculum were significantly more likely than the control group to treat their drinking water (0.086, CI: 0.029–0.14; p = 0.003) [12]. In Zimbabwe, one study found a significant association between the number of CHC sessions attended and self-reported drinking water treatment behaviors (χ2 = 22.53, df = 1, p < 0.0001) [25].
3.1.5. Other WASH Behaviors
Finally, nine studies reported WASH behaviors associated with environmental management [8,22,23,27,28,29], kitchen hygiene [14,17,21,27,29], and personal hygiene [14,17,21,23,27]. Of these studies, four included a comparison group [8,21,22,27] and none reported significant results. For environmental management, all studies reported observational data about the visible presence of garbage or of household garbage pits to manage solid waste. Two studies reported quantitative changes in environmental cleanliness, with one study from Zimbabwe reporting a 30–40% increase in observably clean yards in CHC households [22]. For kitchen hygiene, the studies reported observational data about the presence of pot racks for dish drying. In a study from Uganda, 58% of CHC participants were observed to have constructed a pot rack by project conclusion [17]. Finally, the studies reporting personal hygiene behaviors described quantitative and qualitative observations of bathing shelters and clotheslines or self-reported personal hygiene practices (e.g., teeth brushing, combing hair, bathing, cutting nails). In two studies from Uganda, the authors reported CHC participants constructed 6062 bathing shelters after four months, and after six months, 43% of CHC participants were observed to have constructed a bathing shelter [14,17].
3.2. Knowledge
The second most common outcome reported in the literature was WASH knowledge. Of the 13 studies that reported changes in WASH knowledge, six measured WASH knowledge quantitatively [5,7,8,9,22,31], while seven reported qualitative evidence about participants’ WASH knowledge [21,23,25,27,28,29,30]. All of the studies reporting quantitative results included a comparison sample, and five of the six reported significant increases in knowledge among CHC participants [5,7,8,9,31]. The studies that reported quantitative results measured respondents’ knowledge about the transmission or prevention of common WASH diseases (e.g., diarrhea, skin diseases, intestinal parasites, and malaria) and recommended WASH behaviors (e.g., hand washing, drinking water storage, composition of a homemade oral rehydration solution). Respondents were asked a series of four to nine questions and the number of correct responses was recorded. The total number of correct responses was then reported as a continuous variable [9,31], where higher scores equated to greater knowledge, or categorized as low, medium, or high knowledge [5,7,8,22]. Two studies analyzed the relationship between categorical WASH knowledge scores and WASH behaviors [5,7].
In the first Zimbabwe program, the author reported that CHC participants from two districts were significantly more likely to have “good” health knowledge (e.g., could describe the symptoms, transmission, and prevention of a disease) about nine questions about oral rehydration, diarrhea, malaria, bilharzia, worms, skin diseases, HIV/AIDS, TB, and child care than comparison respondents (p < 0.0001) [5]. A follow-up study describing the results from a third district found that 68.3% of CHC participants demonstrated “full knowledge” on the average of 10 topics compared to 38.2% of comparison respondents (p < 0.001) [7]. Similar results were reported in studies from Haiti. Urban CHC participants were significantly more likely to have “high” preventive WASH knowledge scores compared to a comparison sample from the same communities (71.2% vs. 4.1%, χ2 = 107.4, df = 3, p < 0.0001) [8]. In rural Haiti, the author analyzed the impact of the CHC intervention on composite WASH knowledge scores and found the intervention contributed to a 1.78-point increase in WASH knowledge scores from baseline to final in the CHC sample (CI (0.94, 2.62), p < 0.0001) [9]. The remainder of the studies reported qualitative changes in CHC participant WASH knowledge, one of which attributed CHC participants’ knowledge about the fecal oral route of diarrheal transmission to increases in latrine ownership and presence of hand washing facilities at the end of the program [21].
This relationship between WASH knowledge and behaviors was explored further by two studies from Zimbabwe. In two districts, 79% of CHC participants had “good” health knowledge and were significantly more likely to cover their drinking water container (p = 0.006), use a hand washing facility (p < 0.0001), have soap for hand washing (p < 0.0001), use the pour to waste method of hand washing (p < 0.0001), have a garbage pit (p = 0.01), and have no observable child feces in the yard (p = 0.03) than those with “partial” or “poor” knowledge [5]. In the third district, 80% of CHC members had “full” knowledge of diarrhea prevention and transmission and were significantly more likely to practice 10 WASH behaviors (e.g., covered drinking water, pour to waste for hand washing, use hand washing facility, soap for hand washing, pot rack, garbage pit, use of garbage pit, clean yard, no open defecation, and have a home nutrition garden) than 50% of the comparison sample with “full” knowledge of diarrhea (p < 0.0001) [7].
3.3. Social Capital
Ten papers described social capital outcomes, a multi-dimensional concept that scholars broadly agree is a by-product of social relationships that can generate positive externalities, including cooperation [32,33,34]. There are two main dimensions of social capital, structural (e.g., social networks and group participation) and cognitive (e.g., trust, reciprocity, cohesion, support). The articles in this review described outcomes from both dimensions. One paper reported these dimensions using both quantitative and qualitative data [9], while the remaining nine described qualitative outcomes [5,6,7,8,13,21,22,27,29]. The majority of the ten studies (n = 9) reported themes associated with social bonding or bonding relationships [5,6,7,8,9,13,21,27,29]. Many (n = 7) reported changes in social support [5,7,9,13,21,22,29], social cohesion, and/or social solidarity [5,6,7,8,9,22,27]. Thereafter, three papers described the role of peer pressure [9,21,29], two described bridging and linking relationships [9,21], and one study described themes associated with interpersonal trust [9]. Finally, six of the studies reported social capital as an outcome [5,6,7,8,13,22], while four reported social capital as both an outcome and a mediator of change in WASH knowledge [9], WASH behaviors [9,29], and collective action [9,21,27,29].
The one study that quantitatively explored the relationship between a CHC intervention and social capital assessed whether the intervention influenced levels of social capital and whether pre-intervention levels of social capital influenced knowledge and behavioral outcomes within the CHC sample. The author did not find a significant treatment effect of the intervention on CHC member household respondents’ self-reported trust, social support, group participation, or social solidarity factor scores. However, within a sub-sample of CHC member respondents, there was a marginally significant decrease in trust (−0.26, CI (−0.53, 0.02), p = 0.07) and social solidarity (−0.27, CI (−0.56, 0.02), p = 0.07) factor scores from baseline to final. Further, baseline social solidarity factor scores were found to be associated with a significant increase in average WASH behavioral scores in both the CHC member household respondent (0.23, CI (0.05, 0.41), p = 0.01) and the CHC member respondent (0.25, CI (0.03, 0.46), p = 0.03) samples. In the same study, program participants qualitatively reported that the CHC intervention increased trust, social bonding, and social solidarity amongst the participants. In turn, members used their social capital to apply social pressure and leverage new relationships with other leaders and communities to facilitate WASH behavioral changes and collective action within their community [9].
The remainder of the studies reported qualitative changes in social capital. For example, a study comparing CHCs to a CLTS intervention in Zimbabwe noted how the CHCs created a dynamic in which social bonds were formed and strengthened, which resulted in increased likelihood that CHC members would work together and provide social support [13]. In Sierra Leone, authors reported that a CHC program helped create communal unity and a collective spirit, which resulted in social healing in post-conflict communities, an increase in decision making by women and the formation of new income generation and social support groups [27]. In Zimbabwe, Haiti, and the Dominican Republic, CHC participants described how they used social pressure to encourage maintenance of newly agreed upon behaviors such as hand washing, environmental management, and latrine use and hygiene [9,21,29]. Finally, two papers described how bridging and linking relationships with other communities and governmental/non-governmental stakeholders provided external support and reinforcement, which facilitated participation in and sustainability of the CHCs and engagement in collective action [9,21].
3.4. Collective Action
Ten papers reported outcomes associated with collective action. Two papers provided quantitative evidence [19,22], neither of which reported significant findings. The remaining eight papers provided qualitative data [8,9,16,20,21,23,27,28]. Of these ten papers, eight reported collective action around WASH-specific issues, five on environmental management [8,9,19,22,23], and three on drinking water management [9,16,28], while four reported collective action in other areas [9,20,21,27].
A study of a program in a high-density informal settlement in South Africa reported a 50% reduction in informal dumping sites (from four to two), which were converted into community gardens, after three months of implementation [19]. Similarly, a study in three peri-urban communities in Zimbabwe reported that participants organized 17 clean-up campaigns over one year [22]. Qualitative evidence of CHC participants working together to protect, repair, or improve communal drinking water points was reported by two programs in Haiti [8,9] and one in the Democratic Republic of Congo [28]. Finally, CHC participants were also reported to be more likely to participate in village savings and loans programs in Sierra Leone [27] and Rwanda [20] and to work together to repair roads and street lights in Rwanda [20] and Haiti [9].
3.5. Health
Six papers reported health outcomes associated with a CHC program. Four studies reported qualitative evidence [27,28,29,30]. The remaining two studies provided quantitative evidence [12,15], one of which included a comparison sample [12]. In Zimbabwe, a retrospective analysis of data from one clinic that served a district where 80% of households participated in four years of CHC program activities found a 10-fold decrease in all WASH-related communicable diseases (e.g., diarrhea, schistosomiasis, acute respiratory illnesses, and skin diseases) from one year prior to the start of the intervention to four years after the intervention concluded [15]. Conversely, a RCT conducted in Rwanda reported no difference between the three study arms (classic CHC, lite CHC, controls) in health (diarrhea) and anthropomorphic outcomes (height for age, length for age, and weight for height) in children under one, two, and five years of age after a two-year intervention [12].
3.6. Cost
Four papers described the cost or cost-effectiveness of CHC interventions, with three studies reporting cost per beneficiary [5,17,18] and one study reporting subjective assessments of program cost-effectiveness [24]. The study with the most robust cost per beneficiary analyses was the original CHC program implemented in Zimbabwe. In this paper, the author reported a cost of USD 0.66 per beneficiary for two years of WASH promotion programming that reached 11,450 participants or 68,700 beneficiaries (11,450 × 6 people per household) in three districts and resulted in the formation of 265 CHCs [5]. One author explored the cost-effectiveness of a CHC program using the full six-month WASH curriculum compared to a CHC program with reduced sessions in one district of Rwanda. This study first compiled cost data and then asked program staff to rate the cost-effectiveness of each arm. The author reported that the program using the full curriculum cost a total of USD 191,017 or USD 3820 per household (50 households), while the reduced session program cost a total of USD 59,815 or USD 1196 per household (50 households). In addition, respondents rated the program using the full curriculum as more cost-effective than the reduced session program (p < 0.0001) [24].
4. Discussion
In this review, we documented and described the major outcomes of CHC programs focused on WASH promotion. The programs were implemented across various social, cultural, and geographical contexts, primarily in African and Caribbean settings. We found six major outcomes reported in the literature, which align in many ways with the outcomes of other WASH promotion programs and provide insights into the CHC model’s theory of change.
4.1. WASH Behaviors
The CHC model has demonstrated consistent impact, sometimes significant, on WASH behaviors. The most consistent behavioral outcome reported in the CHC literature is related to defecation practices (n = 15). However, significant results were reported for grouped WASH behaviors (multiple behaviors across five dimensions—sanitation/defecation, hand washing, drinking water, kitchen hygiene, and environmental management), defecation practices (latrine construction, latrine hygiene, and stopping open defecation), drinking water treatment practices, and hand washing behaviors (construction of hand washing facilities and use of soap). Two papers reported a dose response effect, where completion of the full six-month WASH curriculum was associated with increased likelihood of adopting WASH behaviors. Another study found a temporal association where adoption of WASH behaviors consistently increased over time, eventually reaching 100% adoption three years after the intervention ended.
These WASH behavioral outcomes are similar to those of other WASH promotion programs where defecation, hand washing, and water treatment behaviors are the most commonly reported outcomes. Although the results were mixed for all intervention types, a review of WASH promotion models found that community-based interventions achieved the most consistent increases in hand washing and defecation behaviors, while directive hygiene messaging and interventions derived from formal psychosocial theory had mixed, limited, or no evidence of impact on both behaviors [35]. The impact of social marketing on hand washing and defecation practices has been mixed, although these approaches have demonstrated consistent increases in purchase of oral rehydration therapies and point-of-use water treatment technologies [35,36]. Sanitation-specific campaigns have achieved increases in latrine construction and use, with India’s Total Sanitation Campaign, infrastructure interventions, and sanitation education interventions such as CLTS and CHCs achieving the most consistent increases [37]. For CLTS specifically, one review reported a dearth of rigorous quantitative evaluations of behavioral impact but reported significant increases in latrine construction and reductions in open defecation in the available quantitative evaluations [38]. Measurement of kitchen hygiene, environmental management, and grouped WASH behaviors appears unique to evaluations of CHC programs and to our knowledge, no other WASH promotion programs have reported any form of a dose response between participation and WASH behaviors.
4.2. WASH Knowledge
Half (n = 13) of the studies in this review described increases in WASH knowledge amongst CHC participants, with five reporting significant differences in categorical WASH knowledge scores between CHC participants and comparison samples. Of the papers that provided quantitative results, measures included knowledge of the transmission and prevention of WASH-related diseases (including diarrhea, skin diseases, intestinal worms, and malaria) as well as when to wash hands to prevent diarrhea and how to make a homemade oral rehydration solution. Further, two papers described associations between WASH knowledge and behaviors; CHC participants with higher knowledge scores were more likely to practice preventive WASH behaviors, while a comparison sample with high knowledge scores were less likely to practice WASH behaviors than a CHC sample with high knowledge scores [5,7].
Two prior reviews of WASH promotion programs (including community-based, directive hygiene messaging and psychosocial theory, and social marketing interventions) described the impact of interventions on WASH knowledge. Aligned with our results, one prior review of hand washing and sanitation interventions found that community-based interventions consistently and significantly improved knowledge about key times to wash hands; however, this prior review indicated the impact on knowledge of diarrhea was mixed [35]. This prior review also found no consistent or demonstrable effect of directive hygiene messaging and psychosocial interventions on diarrhea or hand washing knowledge. The impact of social marketing interventions is mixed, with one review reporting no demonstrable effect on diarrhea knowledge and mixed results on hand washing knowledge, while another reported consistent increases in awareness about WASH products, such as oral rehydration solutions and point-of-use water treatment, and hand washing behaviors [35,36].
4.3. Social Capital and Collective Action
This review highlighted a potential relationship between social capital and collective action, where CHCs appear to increase social cohesion and social support, which contributes to increased collective action. The type of collective action was mostly associated with communal clean-up campaigns and participation in other community development projects. Qualitative evidence indicates that the CHC model contributes to increased bonding, social support, social solidarity, and women’s empowerment. CLTS programs have reported similar qualitative evidence of increased community mobilization beyond WASH and impacts on women and girls [38]. However, it must be noted that the current evidence regarding social capital and collective action in CHC programs is weak. Of the ten papers that described a relationship with social capital in this review, only one measured social capital quantitatively and the results were inconclusive.
4.4. Health
The evidence of health impacts associated with the CHC model is limited. One study using clinical data reported a substantial decrease in WASH-related diseases over a four-year period, while the only RCT in this review found no impact on childhood diarrhea or anthropometrics after two years. This is not surprising as most WASH promotion programs have struggled to demonstrate consistent and significant impacts on health outcomes, especially diarrhea due to limitations of self-report data and temporality. For example, a prior review found that community-based WASH interventions had some, but no consistent, impact on diarrhea, while directive hygiene education and psychosocial interventions had no impact on diarrhea [35]. Social marketing interventions were found to have limited impact on health [35,36]. Finally, CLTS programs reported a similar, inconsistent impact of reductions in open defecation on diarrhea [38].
4.5. Program Theory
The evidence we gathered from this review sheds light on the CHC model’s theory of change. The model aims to increase adoption of recommended WASH practices and thus improve health. CHCs achieve this goal by increasing participants’ knowledge and encouraging praxis, or the application of knowledge in daily life [39]. The model theorizes that the gap between WASH knowledge and behavior change is addressed through increased social capital, which facilitates consensus building and changes in communal norms around WASH behaviors and collective action.
This review found both quantitative and qualitative evidence of increased WASH knowledge amongst CHC participants. This is an expected outcome since the WASH curriculum takes six months to complete and all studies measured knowledge immediately after the intervention concluded. Although the evidence is limited, this review also documented significant associations between high WASH knowledge and increased adoption of recommended WASH behaviors amongst CHC participants. Comparison samples with equally high knowledge were less likely to adopt recommended WASH behaviors. This supports the theory that knowledge is a necessary pre-requisite for behavior change but is insufficient by itself.
There is also evidence that CHC programs achieve the goal of increasing adoption of recommended WASH behaviors amongst program participants. The studies in this review reported changes in observable WASH behaviors across five dimensions (e.g., defecation practices, personal hygiene and hand washing, drinking water, environmental management, and kitchen hygiene), which align with the content of the six-month WASH curriculum. Most studies provided quantitative evidence, but significant results were reported in only a handful of studies, most consistently around defecation practices and composite WASH behavior scores. Although determining the factors that led to greater adoption of WASH behaviors was outside the scope of this review, we did find studies that reported evidence of potential dose response and temporal effects of the CHC intervention. These findings lend support to the theory that social processes facilitate behavior change.
Further, the social capital evidence provides some insight into this possible dose response. All of the studies describing social capital provided qualitative evidence that the CHC model increases social bonding, social support, and social cohesion. It is logical that longer engagement with a CHC might lead to greater bonding and cohesion, which should increase trust. Increased trust and cohesion would allow participants to leverage social support and apply social pressure to facilitate behavioral changes. Interestingly, there is evidence that higher levels of pre-intervention social capital are a determinant of greater WASH behavior change, which supports findings from the broader social capital and WASH literature [9,40]. Further, the evidence about collective action might also help explain the observed temporal associations. If CHC participants continue their engagement beyond the six-month WASH curriculum, participants would continue to strengthen their social relationships, thereby facilitating continued and sustained behavioral changes. Much of this is conjecture and the impact of the model on social capital and collective action outcomes and the role of social capital as a moderator of knowledge and behavioral outcomes remains an area for further investigation.
4.6. Limitations
This review was limited in that we did not formally rate the quality of the study designs, nor did we consider variation in outcomes based upon country or setting (urban vs. rural). Although desirable, we found such assessments challenging due to the high degree of variability in the study designs and the inconsistent outcome measures reported in the literature. Further, there have been limited peer-reviewed publications describing the impact of CHC programs on WASH outcomes. Much of the evidence is found in the gray literature and in programmatic reports, which are challenging to identify and access. It is possible that we missed some documents in our review.
5. Conclusions
This is the first review of the literature describing outcomes associated with global CHC programs focused on WASH promotion. Although there is evidence of an association between CHCs and changes in WASH knowledge and behavior, there is considerable room to strengthen the quality of the research and evaluation of the CHC model globally. Most of the evidence around CHC programs globally is derived from program monitoring data and field reports. There is an urgent need for more rigorous, experimental study designs that can empirically describe the impact of the intervention on both intermediate outcomes (knowledge, behavior) and more distal outcomes (social capital and health). Furthermore, these studies should also include process evaluations in order to capture key factors of implementation that may influence outcomes such as fidelity to the six-month curricula, the amount of resources provided for implementation, methods used to recruit participants, and socio-political contextual factors. Due to the difficulties and costs associated with conducting experimental study designs, we recommend rigorously designed, quasi-experiments using mixed methods research. In addition, we note a need to standardize outcome measures across countries and contexts, especially those related to WASH behaviors and social capital. Such standardization would improve our understanding of program theory and the true impact of the intervention and allow for cross-program assessments.
We also recommend studies that compare the CHC model to other WASH promotion and behavior change interventions. Only one study compared CHCs to CLTS in Zimbabwe. Although the results for the CHC program were encouraging, particularly as they relate to short-term outcomes, this was an isolated study in a country where CHCs have been implemented by the same organization for two decades. Additional side-by-side assessments would help determine the relative strengths and weaknesses of each intervention in achieving knowledge, behavioral, social, and health outcomes. Finally, there is a need for longitudinal studies that measure the sustainability of knowledge and behavioral changes beyond one-year post-implementation and that explore the relationship between sustained behavioral changes and long-term health and social outcomes.
The CHC model is one intervention model in our international toolkit for WASH promotion and behavior change that has demonstrated the potential to achieve community-wide impact. However, despite the relatively widespread adoption of CHC models, ours is the first review to synthesize its potential impact. While the evidence is promising, our understanding of the true impact of the CHC model remains limited by a lack of rigorous research of both processes and outcomes. It is our hope that this review will stimulate interest amongst both WASH practitioners and researchers to further evaluate the potential of this intervention. Furthermore, WASH promotion is only the first step in a multi-stage community development process where the CHC serves as the vehicle for the achievement of wider community development. As we are now in the era of the Sustainable Development Goals, which, in part, challenge the historical focus on vertical (single outcomes) interventions, this model offers the opportunity for practitioners to address multiple health and development determinants.
Acknowledgments
We would like to thank the WellMed Charitable Trust and the Christ is Our Salvation Foundation for supporting Rosenfeld’s salary these past four years, without which this review would not have been possible. We would also like to thank Juliet and Anthony Waterkeyn, founders of the Zimbabwe AHEAD organization and originators of the Community Health Club model, for their support in identifying some of the non-peer-reviewed articles included in this review.
Author Contributions
Conceptualization, J.R. and L.F.; methodology, J.R.; validation, J.R.; formal analysis, J.R.; writing—original draft preparation, J.R.; writing—review and editing, J.R., L.F., and R.B.; funding acquisition, J.R. and R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prüss-Üstün A., Bos R., Gore F., Bartram J. Safer Water, Better Health: Costs, Benefits and Sustainability of Interventions to Protect and Promote Health. World Health Organization; Geneva, Switzerland: 2008. p. 53. [Google Scholar]
- 2.Boschi-Pinto C., Velebit L., Shibuya K. Estimating child mortality due to diarrhoea in developing countries. Bull. World Health Organ. 2008;86:710–717. doi: 10.2471/BLT.07.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prüss-Ustün A., Bartram J., Clasen T., Colford J.M., Jr., Cumming O., Curtis V., Bonjour S., Dangour A.D., de France J.D., Fewtrell L., et al. Burden of disease from inadequate water, sanitation and hygiene in low- and middle-income settings: A retrospective analysis of data from 145 countries. Trop. Med. Int. Health. 2014;19:894–905. doi: 10.1111/tmi.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNICEF. WHO . Progress on Household Drinking Water, Sanitation and Hygiene: 2000-2017-Special Focus on Inequalities. United Nations Children’s Fund (UNICEF); World Health Organization (WHO); New York, NY, USA: 2019. [(accessed on 30 November 2020)]. Available online: https://www.who.int/water_sanitation_health/publications/jmp-report-2019/en/ [Google Scholar]
- 5.Waterkeyn J.A. Cost Effective Health Promotion and Hygiene Behaviour Change through Community Health Clubs. London School of Tropical Medicine & Hygiene; London, UK: 2006. [Google Scholar]
- 6.Waterkeyn J., Cairncross S. Creating demand for sanitation and hygiene through Community Health Clubs: A cost-effective intervention in two districts in Zimbabwe. Soc. Sci. Med. 2005;61:1958–1970. doi: 10.1016/j.socscimed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Waterkeyn J.A., Waterkeyn A.J. Creating a culture of health: Hygiene behaviour change in community health clubs through knowledge and positive peer pressure. J. Water Sanit. Hyg. Dev. 2013;3:144–155. doi: 10.2166/washdev.2013.109. [DOI] [Google Scholar]
- 8.Brooks J., Adams A., Bendjemil S., Rosenfeld J. Putting heads and hands together to change knowledge and behaviours: Community Health Clubs in Port-au-Prince, Haiti. Waterlines. 2015;34:379–396. doi: 10.3362/1756-3488.2015.033. [DOI] [Google Scholar]
- 9.Rosenfeld J.A. Social Capital and Community Health Clubs in Haiti. University of North Carolina; Chapel Hill, NC, USA: 2019. [Google Scholar]
- 10.Peal A., Evans B., van der Voorden C. Hygiene and Sanitation Software: An Overview of Approaches. Water Supply and Sanitation Collaborative Council; Geneva, Switzerland: 2010. [Google Scholar]
- 11.Africa AHEAD Countries of Operation. [(accessed on 17 March 2020)];2020 Available online: https://www.africaahead.org/countries/
- 12.Sinharoy S.S., Schmidt W.P., Wendt R., Mfura L., Crossett E., Grépin K.A., Jack W., Rwabufigiri B.N., Habyarimana J., Clasen T. Effect of community health clubs on child diarrhoea in western Rwanda: Cluster-randomised controlled trial. Lancet Glob. Health. 2017;5:e699–e709. doi: 10.1016/S2214-109X(17)30217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whaley L., Webster J. The effectiveness and sustainability of two demand-driven sanitation and hygiene approaches in Zimbabwe. J. Water, Sanit. Hyg. Dev. 2011;1:20–36. doi: 10.2166/washdev.2011.015. [DOI] [Google Scholar]
- 14.Waterkeyn J., Okot P., Kwame V. Maximizing the Benefits from Water and Environmental Sanitation, Proceedings of the 31st WEDC Conference, Kampala, Uganda, 31 October–4 November 2005. Loughborough University; Loughborough, UK: 2005. Rapid sanitation uptake in the internally displaced people camps of Northern Uganda through community health clubs; p. 4. [Google Scholar]
- 15.Waterkeyn J. Decreasing communicable diseases through improved hygiene in community health clubs, In Maximizing the Benefits from Water and Environmental Sanitation, Proceedings of the 31st WEDC Conference, Kampala, Uganda, 31 October–4 November 2005. Loughborough University; Loughborough, UK: 2005. pp. 138–145. [Google Scholar]
- 16.Rosenfeld J.A. Incremental Improvements to Community Water Supply Systems through Community Health Clubs in the Umzimkhulu Local Municipality. Water Institute of South Africa; Durban, South Africa: 2008. [(accessed on 30 November 2020)]. Available online: https://africaahead.org/wp-content/uploads/2015/08/2010_WISA_-Rosenfeld.pdf. [Google Scholar]
- 17.Waterkeyn J., Matimati R., Muringaniza A. International Water Association Conference. Mexico City, Mexico: 2009. [(accessed on 30 November 2020)]. ZOD for all–Scaling up the community Health Club Model to meet the MDGs for Sanitation in rural and urban areas: Case Studies from Zimbabwe and Uganda; pp. 1–5. Available online: https://africaahead.org/wp-content/uploads/2011/01/2009.IWA_ZimUganda.pdf. [Google Scholar]
- 18.Waterkeyn J., Rosenfeld J. International Water Association Conference. Mexico City, Mexico: 2009. [(accessed on 30 November 2020)]. Monitoring Hygiene Behaviour Change through Community Health Clubs; pp. 1–12. Available online: https://www.africaahead.org/wp-content/uploads/2011/01/2009_IWA.monitor.pdf.pdf. [Google Scholar]
- 19.Maksimoski N., Waterkeyn A. The Community Health Club Approach in Informal Settlements: Case Study from Ethekwini Municipality, Kzn, South Africa. Water Institute of South Africa; Durban, South Africa: 2010. [Google Scholar]
- 20.Ntakarutimana A., Ekane N. Performance of community health clubs in transforming sanitation and hygiene conditions; Proceedings of the Local Action with International Cooperation to Improve and Sustain Water, Sanitation and Hygiene services: 40th WEDC International Conference; Loughborough, UK. 24–28 July 2017; pp. 1–6. [Google Scholar]
- 21.Chingono A.M. An Investigation on the Impact of Community Health Clubs Approach on Community Health–Case of Ward 19 in Mberengwa District, Project Submitted in Partial Fulfillment of the Post Graduate Diploma in Water. Institute of Water and Sanitation Development; Harare, Zimbabwe: 2013. [Google Scholar]
- 22.Ncube K. An Assessment of the Effectiveness of Community Health Clubs as Drivers of Health and Hygiene in Mzilikazi District, Bulawayo. Department of Development Studies, Midlands State University; Gweru, Zimbabwe: 2013. [Google Scholar]
- 23.Munyoro M. Effectiveness of Podcasting in Water, Sanitation and Hygiene (WASH) Education: A Case of Bindura Town. Department of Development Studies, Midlands State University; Gweru, Zimbabwe: 2016. [Google Scholar]
- 24.Berthe N.R. Cost Effectiveness Analysis of Community Health Programs in Rwanda: A Case Study of Rusizi District. University of Rwanda; Kigali, Rwanda: 2016. [Google Scholar]
- 25.Matimati R. Perceptions towards Water, Sanitation and Hygiene among Communities in Chipinge District. University of Roehampton; London, UK: 2017. [(accessed on 30 November 2020)]. Available online: https://www.africaahead.org/wp-content/uploads/2018/12/Regis-Matimati-Masters-Thesis.pdf. [Google Scholar]
- 26.Pantoglou J. Evaluating Hygiene Behaviour Change within Community Health Clubs in the Rusizi District of Rwanda. Charité–Universitätsmedizin Berlin; Berlin, Germany: 2018. [Google Scholar]
- 27.Azurduy L., Stakem M., Wright L. Assessment of the Community Health Club Approach: Koinadugu District, Sierra Leone. CARE International; Atlanta, GA, USA: 2007. [Google Scholar]
- 28.Beesley J., Feeny E. ‘This Club Is Now the Light of Our Village’: A Community Health Club Set Up by SWIFT Promotes Health and Well-Being in Katchungwe. SWIFT Consortium; London, UK: 2016. [Google Scholar]
- 29.Beesley J., Feeny E. ‘When Others See What We Are Achieving, They Want to Join’: A Community Health Club Set Up by SWIFT Inspires Improvements in Hygiene and Sanitation in Mwandiga I. SWIFT Consortium; London, UK: 2016. [Google Scholar]
- 30.Beesley J., Feeny E., Thomas M.A., Mathiabu K. ‘I’ve Learned a Lot of Things’: A Community Health Club Set Up by SWIFT Changes Sanitation and Hygiene Habits in Matongo. SWIFT Consortium; London, UK: 2016. [Google Scholar]
- 31.Rosenfeld J., Taylor B. Global Health in the Dominican Republic: Progress and Obstacles to Scale Up and Implementation of Successful Programs. Northwestern University; Chicago, IL, USA: 2015. Equality Development and Globalization Studies (EDGS) Working Paper, Number 35. [Google Scholar]
- 32.Eriksson M. Social capital and health-implications for health promotion. Glob. Health Action. 2011;4:5611. doi: 10.3402/gha.v4i0.5611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. Am. J. Public Health. 1997;87:1491–1498. doi: 10.2105/AJPH.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schuller T., Baron S., Field J. Social capital: A review and critique. In: Baron S., Field J., Schuller T., editors. Social Capital: Critical Perspectives. Oxford University Press; Oxford, UK: 2000. pp. 1–39. [Google Scholar]
- 35.De Buck E., Van Remoortel H., Hannes K., Govender T., Naidoo S., Avau B., Vande Veegaete A., Musekiwa A., Lutje V., Cargo M., et al. Approaches to promote handwashing and sanitation behaviour change in low- and middle-income countries: A mixed method systematic review. Campbell Syst. Rev. 2017;7 doi: 10.4073/csr.2017.7. [DOI] [Google Scholar]
- 36.Evans W.D., Pattanayak S.K., Young S., Buszin J., Rai S., Bihm J.W. Social marketing of water and sanitation products: A systematic review of peer-reviewed literature. Soc. Sci. Med. 2014;110:18–25. doi: 10.1016/j.socscimed.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 37.Garn J.V., Sclar G.D., Freeman M.C., Penakalapati G., Alexander K.T., Brooks P., Rehfuess E.A., Boisson S., Medlicott K.O., Clasen T.F. The impact of sanitation interventions on latrine coverage and latrine use: A systematic review and meta-analysis. Int. J. Hyg. Environ. Health. 2017;220:329–340. doi: 10.1016/j.ijheh.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venkataramanan V., Crocker J., Karon A., Bartram J. Community-led total sanitation: A mixed-methods systematic review of evidence and its quality. Environ. Health Perspect. 2018;126 doi: 10.1289/EHP1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freire P. Pedagogy of the Oppressed. Herder & Herder; New York, NY, USA: 1970. [Google Scholar]
- 40.Cameron L.A., Olivia S., Shah M. Initial Conditions Matter: Social Capital and Participatory Development. [(accessed on 30 November 2020)];SSRN Electron. J. 2015 doi: 10.2139/ssrn.2704614. Available online: https://ssrn.com/abstract=2704614 or http://dx.doi.org/10.2139/ssrn.2704614. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.