Abstract
The purpose of this study is to measure posttraumatic stress, grief, burnout, and secondary trauma experienced by employed social workers in the United States and to describe organizational support provided to social workers during the novel coronavirus disease 2019 (COVID-19) pandemic. This study used data from the first wave of the COVID-19 Pandemic and Emotional Well-Being Study, a prospective panel study examining the psychological impact of the COVID-19 pandemic, and includes a sample of 181 social workers. We conducted univariate analyses. Over a quarter (26.21%) of social workers met the diagnostic criteria for PTSD and 16.22% reported severe grief symptoms. While 99.19% of the sample reported average to high compassion satisfaction, 63.71% reported average burnout and 49.59% reported average secondary trauma. Findings indicate that social workers are reporting higher than national estimates of PTSD, indicating a greater need for more emotional support during the COVID-19 pandemic. Given the significance and severity of the pandemic, it is essential that organizations provide resources for both immediate and ongoing support for the emotional well-being of their employees.
Keywords: COVID-19 pandemic, Posttraumatic stress, Compassion fatigue, Burnout, Secondary trauma, Social work
Introduction
There is rising concern that the novel coronavirus disease 2019 (COVID-19) pandemic could inflict long-lasting mental health problems on an unprecedented global scale. This collective emotional trauma has combined stressors that have been studied before in other disasters and disease outbreaks (Adams et al. 2005; Mak et al. 2009; Person et al. 2004; Shultz et al. 2016; Silver et al. 2002), but have never been consolidated in one global crisis. Not even the 9/11 terrorist attacks or the 2003 SARS and the 2014 Ebola virus diseases are adequate comparisons to this pandemic. The emotional stress caused by those events was limited by geography, did not involve mandatory quarantines or isolation, and did not pose the ongoing risk of life-threatening illness, all of which independently have been documented by research to increase emotions of anxiety, depression, and post-traumatic stress symptoms (Adams et al. 2005; Brooks et al. 2020; Mak et al. 2009; Person et al. 2004; Shultz et al. 2016; Silver et al. 2002).
At the time of this writing, the United States has the largest COVID-19 outbreak and has experienced the most casualties in the world, yet the extent to which the pandemic is affecting the mental health of American social workers is unknown. Social workers are in a unique position in that they are experiencing the stress of COVID-19 pandemic in their professional lives by providing services to clients who are often in states of crisis or adversity, while simultaneously experiencing the same trauma in their personal lives. This dual exposure may increase their risk of burnout and secondary trauma, particularly if organizational leadership is also struggling to provide support to their employees during the pandemic. The purpose of this study is to measure the extent of posttraumatic stress, grief, burnout, and secondary trauma experienced by employed social workers in the United States and to describe organizational support provided to social workers during the COVID-19 pandemic.
COVID-19 Compared with Other Disasters and Disease Outbreaks
The COVID-19 pandemic is unprecedented in scale, affecting communities, health systems, and economies throughout the world and imposing the ongoing risk of life-threatening illness. Based on research conducted on the two closest disease outbreaks––the 2003 SARS and the 2014 Ebola virus diseases––it is likely that many people are struggling emotionally during the COVID-19 pandemic. Research on both disease outbreaks demonstrate that generalized fear, depression, anxiety, and posttraumatic stress symptoms were prevalent among high-risk individuals (Person et al. 2004; Shultz et al. 2016), and especially among frontline healthcare workers (Mak et al. 2009).
Additionally, research on the 9/11 terrorist attacks indicate that an individual does not have to directly experience the event to develop mental health symptoms. For example, the psychological effects of 9/11 spread across the United States with nearly half of Americans reporting posttraumatic stress symptoms (Schuster et al. 2001) and many of those symptoms persisted for weeks and months (Silver et al. 2002). Emerging research on the psychological effect of COVID-19 on China’s frontline medical staff working with COVID-19 patients also shows elevated levels of fear, anxiety, and depression (Lu et al. 2020; Cao et al. 2020). There is emerging, yet limited, evidence that COVID has led to significant distress among American workers and families (Kirzinger et al. 2020), but that research on frontline social service workers is limited. Currently it is unknown how COVID-19 is affecting the mental health of Americans who work in the field of social work.
COVID-19 as Collective Trauma
Collective trauma occurs when an entire society feels this intense threat or overwhelming amount of stress that exceeds one’s ability to cope (Hirschberger 2018). The COVID-19 pandemic is considered collective trauma due to the intense threat experienced by many that we or our loved ones will become seriously ill and die, and are experiencing related concerns about our ability to access resources, maintain employment, care for others, and manage ongoing physical isolation. Likewise, trauma tends to be inextricably intertwined with loss and grief. Individuals across the world are facing losses during the COVID-19 pandemic––loss of people, loss of resources, loss of opportunities, and loss of control, among many others. Social workers and other mental health professions are experiencing loss and trauma through providing client services to people who are in emotional distress because of COVID-19, while also experiencing the same trauma in their own personal lives.
The term shared trauma emerged after the 9/11 terrorist attacks as a way to more precisely describe these experiences of trauma in both personal and professional life (Altman and Davies 2002; Tosone et al. 2016). Previously used terms, such as compassion fatigue, secondary trauma (Figley 1995), or vicarious trauma (McCann and Pearlmann 1990) did not adequately describe this dual exposure of 9/11. Specifically, vicarious trauma is experienced through the accumulation of stress due to continuous empathic engagement that exposes the individual to another’s trauma, leading to an adverse shift in one’s cognitive schema and belief system (Pearlman and Saakvitne 1995). Secondary trauma is nearly identical to posttraumatic stress disorder (PTSD), involving the symptom clusters of re-experiencing, avoidance, and hyperarousal in reaction to someone else’s traumatic event (Stamm 1995). Compassion fatigue is the cumulative effects of being exposed to the impact of trauma on others, though it specifically involves the reduced capacity to empathize with others, and is a result of feeling overwhelmed and preoccupied by another’s traumatic or stressful experiences (Figley 1995). Compassion fatigue, secondary trauma, and vicarious trauma share the element of the professional practitioner’s adverse response out of exposure to another’s trauma, and do not require the practitioner to have experienced or to be currently experiencing the same trauma as the client.
Social workers as Wounded Healers
Wounded healers, first conceptualized by Carl Jung (1966), Referred to physicians as helping professionals who experienced their own trauma and adversity and were therefore better able to understand the patient’s trauma. Zerubavel and Wright (2012) furthered this concept for psychologists by suggesting they could more effectively empathize with their clients if their prior traumatic experiences had been therapeutically addressed. More recently, Straussner, Senreich, and Steen (2018) applied the wounded healer concept to social workers, reporting that half of social workers in their study indicated that they experienced mental health problems prior to or during their career. Of particular importance is the conclusion drawn by Straussner et al. (2018) that additional supports and wellness programs offered through their organization of employment need to be developed and implemented for wounded healers.
Research has shown that social workers often experience high workplace stress (Bride 2007; Harris et al. 2006; Johnson et al. 2005), secondary traumatic stress (Bride 2007; Caringi et al. 2017; Pelon 2017), and burnout, which is when they feel exhausted emotionally and physically as a result of their work experience (Stalker et al. 2007; Stevens and Higgins 2002). Interestingly, despite high levels of secondary traumatic stress and burnout, many social workers simultaneously report high levels of compassion satisfaction, which is the harboring of positive feelings about the work they are doing to help others (Pelon 2017; Stalker et al. 2007). Recent research in this area demonstrates that social workers who have organizational support such as good supervision and feeling safe from harm predict lower levels of workplace stress (Senreich et al. 2020). Such organizational support may reduce workplace stress that leads to burnout.
The gaps in our knowledge of the current collective trauma of COVID-19 combined with the framework of wounded healers guides our study research aims. The purpose of this study is to better understand the extent of posttraumatic stress, grief, burnout, and secondary trauma experienced by employed social workers in the United States, and to describe organizational support provided to social workers during the COVID-19 pandemic.
Method
Participants and Procedures
The COVID-19 Pandemic and Emotional Well-Being Study is a prospective panel study examining the psychological effect of the COVID-19 pandemic on first responders, essential classified workers, and the general public. This study received Institutional Review Board approval from Case Western Reserve University. Participants were recruited via online advertisements posted to social media and sent to email listservs, and asked to answer questions about how the COVID-19 pandemic may be affecting their emotional well-being and the type of coping strategies used to minimize emotional distress. After informed consent, participants completed questions capturing demographics, the extent to which they were concerned with COVID-19 issues, level of contact with confirmed cases, coping strategies used to reduce stress, and their mental health and relational health. The current study used baseline data collected between April 12, 2020, and May 22, 2020. A total of 808 participants consented to participate, of which 181 reported they were employed in the social work field and had either a bachelor’s of social work (BSW) or a master’s of social work (MSW) degree. Social work participants were surveyed from 27 states with 65% of the sample from the states of Missouri, Ohio, Pennsylvania, and Virginia.
Measures
Demographic Questions
Demographic questions included gender, age, race, ethnicity, level of education, employment status, industry they work in, and if they consider their current work to be that of a “helper,” meaning someone working alongside other people or networks in many different kinds of supportive capacities, such as providing assistance, communication, resources, or care to other people, organizations, or environments. Additional questions were asked about average hours per week worked prior to COVID-19; average hours per week worked during COVID-19; being unemployed as a result of COVID-19; if their job was considered essential, meaning they were required to report to work while others were able to work from home or not required or able to work at all; if they had tested positive or suspected they or loved ones had COVID-19; and if friends or family members had died from COVID-19.
Posttraumatic Stress
PTSD Checklist for DSM-5 (PCL-5) is a 20-item self-report measure that assesses the 20 DSM-5 symptoms of PTSD (Weathers et al. 2013). The PCL-5 was scored as a total symptom score (range 0–20) by summing the number of symptoms rated as "Moderately" or higher as a symptom endorsed. Total symptom score was identified for each DSM-5 cluster (i.e., intrusive symptoms, avoidance of stimuli, negative alterations in cognitions and mood, marked alterations in arousal and reactivity). PTSD diagnosis was determined if the participant met the criteria following the DSM-5 diagnostic rule. α = .96.
Grief
The Adult Attitude to Grief Scale is a 9-item measure that assess grief and loss symptoms with three subscales: overwhelmed, control, and resilience (Sim et al. 2014). Overwhelmed reactions are feelings of grief and loss experienced as intrusive thoughts, painful emotions, or life losing meaning. Controlled reactions focus on avoiding or denying feelings of grief and loss through a belief of stoicism, avoiding expressions of distress, or diverting attention away from the loss. Resilient coping is a balanced capacity to deal with feelings and manage the consequences of grief through facing feelings, a sense of personal resourcefulness, and hopefulness and positivity. Total severity was calculated by summing responses reported on a 5-point Likert scale where greater than 20 was determined to have high/severe vulnerability. α = .68–.73.
Compassion Satisfaction and Fatigue
The Professional Quality of Life Measure (ProQOL) is a 30-item scale that measures compassion satisfaction (the pleasure derived from being able to do your work well) and compassion fatigue, which is measured by two subscales: burnout (feelings of hopelessness and difficulties in dealing with work or in doing your job effectively) and secondary trauma (work‐related, secondary exposure to people who have experienced extremely or traumatically stressful events; Stamm 2010). Each item contains a 5-point Likert scale with potential total scores for each scale ranging from 10 to 50. Scores of 22 or less are considered “low” compassion satisfaction, the range of 23 to 41 is considered “average,” and scores 42 and higher are considered “high” compassion satisfaction. This scale is used only with those who identified themselves as a helper (defined in demographics). α = .71–.89.
Indirect Trauma Organizational Capacity
The Indirect Trauma Organizational Capacity Index was developed for the COVID-19 Pandemic and Emotional Well-Being Study, and is based on evidence showing specific areas of organizational support that build resilience to indirect trauma among staff (Cocker and Joss 2016; Cohen and Collens 2013; Figley Institute 2013; Kim and Stoner 2008; Office for Victims of Crime 2016; van Mol et al. 2015). It is a 10-item index that measures the extent to which the participant’s organization of employment addresses indirect trauma prior to and since the COVID-19 pandemic. Participants responded using a 5-point Likert scale (never to always) to five areas in which their organization provided wellness activities (e.g., fitness programs, mindful/meditation, yoga); sponsored debriefing and or support sessions after major stressful or traumatic events; provided opportunities for co-workers to support one another; provided opportunities to discuss or manage exposure to trauma or stressful events; and promoted a sense of safety. α = .91.
Analyses
The purpose of this article is to provide an initial glimpse into how the COVID-19 pandemic may be affecting social workers in the United States. Therefore, univariate analyses were conducted to describe the distribution and characteristics of the variables in the study. Paired t test was used to test if the means of the indirect trauma organizational capacity prior to COVID-19 significantly differed to the means reported during COVID-19.
Results
Table 1 presents the sample demographics. The study sample (n = 181) had a mean age of 39.76 years (SD: 12.71, range 22–83) and was primarily female (91.71%) and White non-Hispanic (82.87%). Over half of the sample had an MSW (n = 117, 64.64%) and was considered an essential worker during the COVID-19 pandemic (n = 118, 65.19%). On average, social workers reported working 11.66 (SD = 10.59, range 0–60) years, 43.51 (SD = 14.86, range 0–90) hours per week prior to COVID-19, and 41.89 (SD = 17.16, range 5–110) hours during COVID-19. At the time of surveying, no participants had tested positive for COVID-19 but 16.86% (n = 29) suspected they had COVID-19 but did not get tested. Nearly half of the participants (n = 72, 42.35%) had one or more friends or loved ones tested positive or suspected they had COVID-19, and 4.76% (n = 8) reported having one or more friends or loved ones died from COVID-19.
Table 1.
Sample demographics (N = 181)
| n | % | M (SD) | |
|---|---|---|---|
| Age, years | 177 | 39.76 (12.71) | |
| Gender | |||
| Male | 14 | 7.73 | |
| Female | 166 | 91.71 | |
| Nonbinary | 1 | 0.55 | |
| Race/ethnicity | |||
| White non-Hispanic | 150 | 82.87 | |
| Black/African American | 9 | 4.97 | |
| Other/mixed | 7 | 3.87 | |
| Hispanic/Latinx | 15 | 8.29 | |
| Education | |||
| BSW | 64 | 35.36 | |
| MSW | 117 | 64.64 | |
| Number of years employed as a social worker | 181 | 11.66 (10.59) | |
| Average hours worked per week prior to COVID-19 | 180 | 43.51 (14.86) | |
| Average hours worked per week during COVID-19 | 181 | 41.89 (17.16) | |
| Essential Worker during COVID-19 | |||
| Yes | 118 | 65.19 | |
| No | 63 | 34.81 | |
| Positive COVID-19 test | |||
| Tested positive to COVID-19 | 0 | 0 | |
| Suspected had COVID-19 but did not get tested? | 29 | 16.86 | |
| Family or Friends COVID-19 | |||
| One or more friends or loved ones tested positive or suspected they had COVID-19 | 72 | 42.35 | |
| One or more friends or loved ones died from COVID-19 | 8 | 4.76 | |
Table 2 presents descriptives of study variables. Participants endorsed a median of 6.66 posttraumatic stress symptoms (SD: 5.68, range 0–20). Over a quarter (26.21%) of the study sample met the diagnostic criteria for PTSD. The most common criteria endorsed were intrusion symptoms (54.30%), negative alterations in cognitions and mood (54.00%), and marked alterations in arousal and reactivity (53.95%). Severe grief symptoms were reported by 16.22% of social workers with controlled reactions most often endorsed (72.00%), followed by overwhelmed reactions reported by 27.33% of the sample. Under 10% of social workers reported high to severe vulnerability to coping with loss.
Table 2.
Descriptives of PTSD, grief, compassion satisfaction and fatigue among social workers during COVID-19 pandemic
| n | % | M (SD) | |
|---|---|---|---|
| Posttraumatic stress | |||
| Number of symptoms endorsed | 145 | 6.66 (5.68) | |
| PTSD diagnosis | 38 | 26.21 | |
| Criterion B: intrusion symptoms | 82 | 54.30 | |
| Criterion C: avoidance of stimuli | 63 | 40.91 | |
| Criterion D: negative alterations in cognitions and mood | 81 | 54.00 | |
| Criterion E: marked alterations in arousal and reactivity | 82 | 53.95 | |
| Grief (high/severe symptoms) | 24 | 16.22 | |
| Overwhelmed (high/severe symptoms) | 41 | 27.33 | |
| Control (high/severe symptoms) | 108 | 72.00 | |
| Vulnerability to coping (high/severe symptoms) | 14 | 9.21 | |
| Compassion satisfactiona | 124 | 38.29 (6.36) | |
| Low | 1 | .81 | |
| Average | 84 | 67.74 | |
| High | 39 | 31.45 | |
| Compassion fatiguea | |||
| Burnout | 124 | 25.14 (6.29) | |
| Low | 45 | 36.29 | |
| Average | 79 | 63.71 | |
| High | 0 | 0 | |
| Secondary trauma | 124 | 22.57 (6.39) | |
| Low | 62 | 50.41 | |
| Average | 61 | 49.59 | |
| High | 0 | 0 | |
aSample for Compassion satisfaction and Compassion fatigue is 124 and includes only those who self-identified as a “helper,” someone who works alongside other people in a supportive capacity, and completed the measure for burnout and secondary trauma
Although 99.19% of the sample reported average to high compassion satisfaction with a mean score of 38.29 (SD = 6.36, range 19–50), 63.71% reported average burnout (M = 25.629, SD = 6.29, range 11–40) and 49.59% reported average secondary trauma (M = 22.57, SD = 6.39, range 10–40). No participants fell into the range of high scores for burnout or secondary trauma.
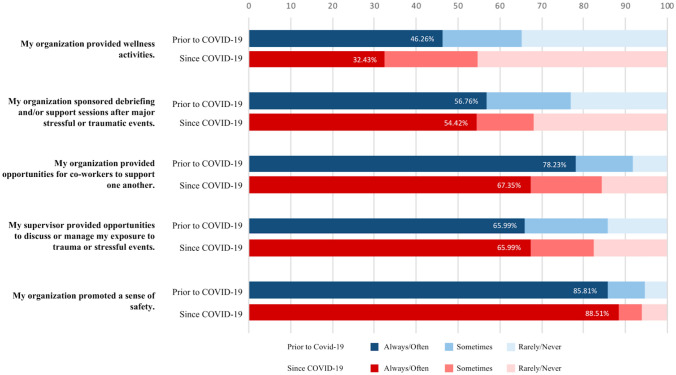
Figure 1 shows the reported organizational support prior to COVID-19 compared with since COVID-19. There was a significant difference in the scores for organizational wellness activities prior to COVID-19 M = 2.47, SD = .137) and since COVID-19 (M = 2.13, SD = 1.30), t(146) = 3.67, p < .001, and for opportunities for co-workers to support one another prior to COVID-19 (M = 3.44, SD = 1.19) and since COVID-19 (M = 3.12, SD = 1.29), t(145) = 4.42, p < .001). All other areas of organizational support remained nearly the same prior to COVID-19 compared with since COVID-19.
Fig. 1.
Organizational support prior to and since COVID-19. Note There was a significant difference in the scores for organization provided wellness activities prior to COVID-19: M = 2.47, SD = .137) and since COVID-19 (M = 2.13, SD = 1.30), t(146) = 3.67, p < .001, and for opportunities for co-workers to support one another prior to COVID-19 (M = 3.44, SD = 1.19) and since COVID-19 (M = 3.12, SD = 1.29), t(145) = 4.42, p < .001)
Discussion
Using preliminary data from Wave 1 of the COVID-19 Pandemic and Emotional Well-Being Study, we have a better sense of the extent of posttraumatic stress, grief, burnout, and secondary trauma experienced by employed social workers in the United States and the organizational supports provided to social workers during the COVID-19 pandemic. The past-12-month PTSD prevalence of 26.21% reported by the social worker study sample is five times higher than the current national estimates of 5.3% (Kilpatrick et al. 2013), seven times higher than the 3.7% of licensed social workers who self-reported experience of PTSD in 2015 (Senreich et al. 2020), and over three times higher than the 7.6% reported PTSD rates of active duty and Reserve/National Guard personnel deployed to Afghanistan and Iraq with combat exposure (Smith et al. 2008). However, the proportion of social workers who met the diagnostic criteria for PTSD is comparable with the whole sample of participants from the COVID-19 Pandemic and Emotional Well-Being Study where 28.27% met the diagnostic criteria for PTSD, indicating that this is truly a collective trauma experienced and felt by entire populations. These elevated rates of PTSD show that our society is experiencing COVID-19 as an intense threat and/or is reporting an overwhelming amount of stress that exceeds one’s ability to cope.
Though not measured in the current study, the concept of shared trauma is relevant here and may hold both positive and negative implications for social workers. For example, in line with the wounded healer framework, because social workers have experienced trauma and adversity, they may be more suited to understand and empathize with their clients. Furthermore, research on mental health workers’ shared trauma with clients during the aftermath of Hurricane Katrina demonstrated that social workers reported greater empathy with their clients who had similar experiences of the natural disaster (Tosone et al. 2016). Likewise, research following the 9/11 terrorist attacks found that social workers reported increased compassion, enhanced clinical skills, and higher levels of self-care (Bauwens and Tosone 2010). On the other hand, the nature of shared trauma means that many social workers will be navigating their own experiences of trauma related to the COVID-19 pandemic while also being exposed to their client’s trauma through the therapeutic relationship. Participants reported they had COVID-19, knew friends or family who had COVID-19, or had a friend or loved one die from COVID-19. In other research on man-made and natural disasters, a personal history of potentially traumatic events, insecure attachment, and enduring distress were significantly associated with shared traumatic stress (Tosone et al. 2011, 2015). Because of this shared traumatic reality, social workers may experience an increased sense of vulnerability with a higher potential of self-disclosure because of the blurring of professional and personal boundaries (Tosone et al. 2012; Baum 2010). It is imperative that social workers not only attend to self-care but also that organizational leaders and supervisors minimize risks of shared trauma of their staff by carefully planning caseload assignments and building capacity to promote an organizational culture of staff support and resilience.
The current study found that both burnout and secondary trauma are at an average level. At the time this data were collected, most parts of the United States had been under “shelter in place” orders for approximately 6 to 8 weeks. Although none of the social workers met the threshold for high levels of compassion fatigue, it will be important to continue to monitor workplace stress and compassion fatigue as time goes on. Compassion fatigue coupled with the high rate of social workers reporting grief and loss symptoms, posttraumatic symptoms, subthreshold PTSD, or meeting the diagnostic criteria for PTSD highlights the need for organizational support of employees to navigate these emotional difficulties. In the aftermath of Hurricane Katrina, social workers reported seeking additional information, changing practice orientation, making their practice more manageable, and developing a greater appreciation for strengths and limitations of the mental health profession (Tosone et al. 2016).
The current study examined organizational capacity to address secondary trauma prior to the COVID-19 pandemic compared with during the COVID-19 pandemic. Although organizational wellness offerings (e.g., yoga, meditation) and opportunities for co-workers to provide support for each other significantly decreased during the COVID-19 pandemic, the other areas assessed remained the same from prior to the pandemic to during the pandemic. Those areas included organization-sponsored debriefings or support sessions after major or stressful events, supervisors providing opportunities to discuss or manage exposure to trauma, and organizations promoting a sense of safety. Because the way individuals are delivering services has changed from mostly in person to mostly telehealth, further examination into how organizations may have been able to maintain a supportive environment for staff is needed.
This study showed less than 1% of social workers scoring in the low compassion satisfaction area, whereas other research has reported 20% of hospice social workers scored in the low range of compassion satisfaction (Pelon 2017). However, the percentage of scores falling in the average (67.74%) and high (31.45%) range for compassion satisfaction were more comparable with other studies. For example, 46% of social workers and psychologists working in the trauma field scored in the high range of compassion satisfaction (Craig and Sprang 2010), and another study found that nearly 60% of social workers scored in the high range of compassion satisfaction (Senreich et al. 2020). More research examining the concept of compassion satisfaction during COVID-19 and how these levels of satisfaction may change over time is needed. Particularly interesting may be mapping trends of compassion satisfaction to societal views of the heroic nature of frontline workers during the COVID-19 pandemic. It may be that because society is currently viewing the work of social workers, nurses, doctors, and other frontline or essential workers in a positive light, those working to help others may internalize those positive and heroic messages into higher levels of compassion satisfaction.
Future research will also need to examine posttraumatic growth, which is a transformative process that leads to recovery and positive changes in perception and relationships as a person creates new meaning out of a traumatic experience (Tedeschi and Calhoun 1996). Past research has examined posttraumatic growth from working as a mental health professional (Arnold et al. 2005; Linley and Joseph 2007; Linley et al. 2005; Putterman 2005; Tehrani 2007) as well as growth fostered following collective traumas of the 9/11 terrorist attacks (Bauwens and Tosone 2010; Eidelson et al. 2003) and Hurricane Katrina (Bauwens 2012). It will also be important to examine the influence of relational health on posttraumatic growth. The COVID-19 pandemic “shelter in place” and “social distancing” practices, which reduce or eliminate social contact, challenge the most reliable methods of mitigating the effects of trauma––relational connectedness to consistent, predictable, trustworthy people. The importance of relational health and connectedness in mitigating the effects of trauma has been well documented (Dobson and Perry 2010). Given the quarantine circumstances, individuals have been forced to adapt their coping strategies to manage the stress of COVID-19. Coping is defined as an individual's use of behavioral and cognitive strategies to modify adverse aspects of their environment, as well as minimize or escape internal threats induced by stress or trauma (Gil 2005; Weinberg et al. 2014). Future research should examine what coping strategies were being used during the COVID-19 pandemic and whether these strategies led to positive change and growth from the experiences of collective trauma.
Strengths and Limitations
As with all studies, some limitations should be noted. Given that we used preliminary data from Wave 1 of the COVID-19 Pandemic and Emotional Well-Being Study, which was still in the data collection phase at the time of this writing, these descriptive data need to be viewed as preliminary. More collected data may change the distribution of reported variables. However, there is merit in reporting these data as they provide a snapshot into the effect of the pandemic on social workers during the early stages of COVID-19, which has the potential to be an ongoing threat as geographic regions begin to see a rise in cases at the time of this writing. This is important because it may provide organizational leaders a better understanding of how COVID-19 may be affecting their employees and therefore provide rationale for building a higher capacity to support the emotional distress experienced by their employees. Similarly, these descriptive data may also provide information to social work educators on how they can prepare our future workforce with tools to monitor posttraumatic stress and compassion fatigue as well as ways to cope and strategize self-care.
The sample used in this study is mostly White and female, which is a significant limitation given that racial and gender minority populations are disproportionately represented among those who test positive for COVID-19 and face worse outcomes, with evidence reinforcing the fact that social risk factors arising from systemic inequalities negatively impact physical health of racial and ethnic minorities (Tai et al. 2020). Minority populations face additional stressors to manage during this pandemic and may report differences in coping, resilience, organizational support, grief, and trauma indicators. Despite this limitation, our sample is similar to Straussner, Senreich, and Steen’s (2018) and to Whitaker, Weismiller, and Clark’s (2006) samples of licensed social workers, and provides a glimpse of the traumatic stressors faced by helpers during a global pandemic. Future iterations of this study with more diverse representation among helpers will need to examine PTSD and indirect trauma while also identifying the unique elements of pandemic-related stress, coping, and factors of resilience experienced by minorities. Additionally, respondents to this study largely reside in the midwestern region of the United States––areas impacted by stay-at-home public health mandates yet not considered epicenters of COVID-19 mortality and morbidity at the time of data collection. In states with the highest rates of COVID-19, social workers in overcrowded, under-resourced hospital settings may experience different rates of indirect trauma and PTSD. Our research team is actively networking to reach a more inclusive and geographically comprehensive sample population.
Gathering information regarding the length of time respondents have been employed in the social work profession would provide additional information in the consideration of compassion satisfaction and fatigue scores. Lack of historical information should also be considered in the interpretation of grief and loss symptom scores. We also did not ask questions about prior mental health symptoms, diagnosis of PTSD or other behavioral health disorders, or history of mental health treatment services; each of which will be important to include in future data collection. Future research will also need to examine how or whether PTSD and grief were enhancing or interfering with their work as a clinician, or whether the social workers felt they were better able to understand their client's COVID-related trauma and experiences because of their own COVID-19 experiences. Finally, as stay-at-home mandates require schools to close and children to engage in remote learning, it is possible that social workers who are also parents or caregivers experience stress related to work-life balance that impacts their functioning and their reported symptoms; an area to be considered in future study.
Conclusion
This study is a preliminary snapshot into the effect of the COVID-19 pandemic on U.S. social workers’ mental health, compassion fatigue, and organizational support. Findings indicate that social workers are reporting higher than national estimates of PTSD, and given previous estimates of PTSD among social workers, this indicates there is a greater need for more emotional support for these social workers during the COVID-19 pandemic. Given the significance and severity of the COVID-19 pandemic, it is essential that organizations provide resources for both immediate and ongoing support for the emotional well-being of their employees.
Biographies
Megan R. Holmes
PhD, MSW, LISW-S is an Associate Professor and Founding Director of the Center on Trauma and Adversity in the Jack, Joseph and Morton Mandel School of Applied Social Sciences at Case Western Reserve University
C. Robin Rentrope
MSSA, MPH, is research assistant in the Webel Research Lab, in the Frederick Payne Bolton School of Nursing at Case Western Reserve University. Her current research aims to improve the quality of life and overall health for vulnerable populations
Amy Korsch-Williams
MSSA, CNM, LISW-S is a Senior Instructor at the Jack, Joseph and Morton Mandel School of Applied Social Sciences at Case Western Reserve University and a faculty affiliate of the Center on Trauma and Adversity
Jennifer A. King
DSW, MSW, LISW is an is an Assistant Professor and the Assistant Director of the Center on Trauma and Adversity in the Jack, Joseph and Morton Mandel School of Applied Social Sciences at Case Western Reserve University
Author Contributions
(Optional: please review the submission guidelines from the journal whether statements are mandatory).
Funding
(Information that explains whether and by whom the research was supported) Not Applicable.
Data Availability
(Data transparency).
Code Availability
(Software application or custom code).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adams RE, Boscarino JA, Galea S. Social and psychological resources and health outcomes after the World Trade Center disaster. Social Science & Medicine. 2005;62(1):176–188. doi: 10.1016/j.socscimed.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman N, Davies JM. Out of the blue: Reflections on a shared trauma. Psychoanalytic Dialogues. 2002;12:359–360. doi: 10.1080/10481881209348672. [DOI] [Google Scholar]
- Arnold D, Calhoun LG, Tedeschi RG, Cann A. Vicarious posttraumatic growth in psychotherapy. Journal of Humanistic Psychology. 2005;45:239–263. doi: 10.1177/0022167805274729. [DOI] [Google Scholar]
- Baum N. Shared traumatic reality in communal disasters: Toward a conceptualization Psychotherapy Theory. Research, Practice. 2010;47(2):249–259. doi: 10.1037/a0019784. [DOI] [PubMed] [Google Scholar]
- Bauwens, J. (2012). Clinicians’ posttraumatic growth following Hurricane Katrina: The influence of life events, professional quality of life, and primary and secondary traumatic stress. (Order No. 3488432, New York University). ProQuestDissertations and Theses, 193.
- Bauwens J, Tosone C. Professional posttraumatic growth after a shared traumatic experience: Manhattan clinicians’ perspectives on post 9/11 practice. Journal of Loss and Trauma. 2010;15:498–517. doi: 10.1080/15325024.2010.519267. [DOI] [Google Scholar]
- Bride BE. Prevalence of secondary traumatic stress among social workers. Social Work. 2007;52(1):63–70. doi: 10.1093/sw/52.1.63. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, J., Wei, J., Zhu, H., Duan, Y., Geng, W., Hong, X., ... Zhu, B. (2020). A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychotherapy and Psychosomatics, 1. doi: 1159/000507453 [DOI] [PMC free article] [PubMed]
- Caringi JC, Hardiman ER, Weldon P, Fletcher S, Devlin M, Stanick C. Secondary traumatic stress and licensed clinical social workers. Traumatology. 2017;23(2):186–195. doi: 10.1037/trm0000061. [DOI] [Google Scholar]
- Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: A systematic review. International Journal of Environmental Research and Public Health. 2016;13(6):618. doi: 10.3390/ijerph13060618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen K, Collens P. The Impact of trauma work on trauma workers: A metasynthesis on vicarious trauma and vicarious posttraumatic growth. Psychological Trauma. 2013;5(6):570–580. doi: 10.1037/a0030388. [DOI] [Google Scholar]
- Craig CD, Sprang G. Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress, & Coping. 2010;23(3):319–339. doi: 10.1080/10615800903085818. [DOI] [PubMed] [Google Scholar]
- Dobson C, Perry B. The role of healthy relational interactions in buffering the impact of childhood trauma. In: Gil E, editor. Working with children to heal interpersonal trauma: The power of play. New York, NY: Guilford Press; 2010. pp. 26–43. [Google Scholar]
- Eidelson RJ, D’Alessio GR, Eidelson JI. The impact of September 11 on psychologists. Professional Psychology. 2003;34:144–150. doi: 10.1037/0735-7028.34.2.144. [DOI] [Google Scholar]
- Figley C. Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York, NY: Brunner-Routledge; 1995. [Google Scholar]
- Gil S. Coping style in predicting posttraumatic stress disorder among Israeli students. Anxiety, Stress, and Coping. 2005;18(4):351–359. doi: 10.1080/10615800500392732. [DOI] [Google Scholar]
- Harris LM, Cumming SR, Campbell AJ. Stress and psychological well-being among allied health professionals. Journal of Allied Health. 2006;35(4):198–207. [PubMed] [Google Scholar]
- Hirschberger G. collective trauma and the social construction of meaning. Frontiers in Psychology. 2018;9:1441. doi: 10.3389/fpsyg.2018.01441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figley Institute. (2013). Basics of Compassion Fatigue. Retrieved from http://www.figleyinstitute.com/documents/Workbook_AMEDD_SanAntonio_2012July20_RevAugust2013.pdf.
- Johnson S, Cooper C, Cartwright S, Donald I, Taylor P, Millet C. The experience of work-related stress across occupations. Journal of Managerial Psychology. 2005;20(2):178–187. doi: 10.1108/02683940510579803. [DOI] [Google Scholar]
- Jung CG. The practice of psychotherapy. 2. New York, NY: Bollingen Foundation; 1966. [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress. 2013;26(5):537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Stoner M. Burnout and turnover intention among social workers: Effects of role stress, job autonomy and social support. Administration in Social Work. 2008;32(3):5–25. doi: 10.1080/03643100801922357. [DOI] [Google Scholar]
- Kirzinger, A., Hamel, L., Muñana, C., Kearney, A. & Brodie, M. (2020). KFF Health Tracking Poll-late April 2020: Coronavirus, social distancing, and contact tracing. Retrieved from: https://www.kff.org/report-section/kff-health-tracking-poll-late-april-2020-economic-and-mental-health-impacts-of-coronavirus/.
- Linley PA, Joseph S. Therapy work and therapists’ positive and negative well-being. Journal of Social and Clinical Psychology. 2007;26:385–403. doi: 10.1521/jscp.2007.26.3.385. [DOI] [Google Scholar]
- Linley PA, Joseph S, Loumidis K. Trauma work, sense of coherence, and positive and negative changes in therapists. Psychotherapy & Psychosomatics. 2005;74:185–188. doi: 10.1159/000084004. [DOI] [PubMed] [Google Scholar]
- Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 112936. [DOI] [PMC free article] [PubMed]
- Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann L, Pearlman LA. Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress. 1990;3:131–147. doi: 10.1007/BF00975140. [DOI] [Google Scholar]
- Office for Victims of Crime. (2016). Guidelines for a Vicarious Trauma-Informed Organization: Human Resources. Retrieved from https://ovc.ojp.gov/sites/g/files/xyckuh226/files/media/document/os_hr_guidelines-508.pdf.
- Pearlman L, Saakvitne K. Trauma and the therapist: Countertransference and vicarious traumatization in psychotherapy with incest survivors. New York, NY: Norton; 1995. [Google Scholar]
- Pelon SB. Compassion fatigue and compassion satisfaction in hospice social work. Journal of Social Work in End-of-Life and Palliative Care. 2017;13(2/3):134–150. doi: 10.1080/15524256.2017.1314232. [DOI] [PubMed] [Google Scholar]
- Person B, Sy F, Holton K, Govert B, Liang A, Garza B. National Center for Infectious Diseases/SARS Community Outreach Team. Fear and stigma: The epidemic within the SARS outbreak. Emerging Infectious Diseases. 2004;10:358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putterman, I. (2005). The relationship between posttraumatic growth and professional quality of life (Compassion fatigue/secondary trauma, compassion satisfaction, and burnout) among social workers in Texas. (Doctoral dissertation, University of Houston). Dissertation Abstracts International, 66, 11.
- Schuster MA, Stein BD, Jaycox LH, Collins RL, Marshall GN, Elliott MN. A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine. 2001;45:1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- Senreich E, Straussner SLA, Steen J. The work experiences of social workers: Factors impacting compassion satisfaction and workplace stress. Journal of Social Service Research. 2020;46(1):93–109. doi: 10.1080/01488376.2018.1528491. [DOI] [Google Scholar]
- Shultz, J. M., Cooper, J. L, Baingana, F., Oquendo, M. A, Espinel, Z., & Althouse, B. M. ... Rechkemmer, A. (2016). The role of fear-related behaviors in the 2013–2016 West Africa Ebola virus disease outbreak. Current Psychiatry Reports, 18, 104 [DOI] [PMC free article] [PubMed]
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. Journal of the American Medical Association. 2002;288:1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- Sim J, Machin L, Bartlam B. Identifying vulnerability in grief: Psychometric properties of the Adult Attitude to Grief Scale. Quality of Life Research. 2014;23(4):1211–1220. doi: 10.1007/s11136-013-0551-1. [DOI] [PubMed] [Google Scholar]
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Stalker CA, Mandell D, Frensch KM, Harvey C, Wright M. Child welfare workers who are exhausted yet satisfied with their jobs: How do that do it? Child and Family Social Work. 2007;12(2):182–191. doi: 10.1111/j.1365-2206.2006.00472.x. [DOI] [Google Scholar]
- Stamm BH. The professional quality of life scale: Compassion satisfaction, burnout, & compassion fatigue/secondary trauma scales. Pocatello, ID: Sidran Press; 1995. [Google Scholar]
- Stamm BH. The concise ProQOL manual. 2. Pocatello, ID: ProQOL.org; 2010. [Google Scholar]
- Stevens M, Higgins DJ. The influence of risk and protective factors on burnout experienced by those who work with maltreated children. Child Abuse Review. 2002;11(5):313–331. doi: 10.1002/car.754. [DOI] [Google Scholar]
- Straussner SLA, Senreich E, Steen JT. Wounded healers: A multistate study of licensed social workers’ behavioral health problems. Social Work. 2018;63(2):125–133. doi: 10.1093/sw/swy012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai, D.B., Shah, A., Doubeni, C.A., Sia, I.G., & Wieland, M.L. (2020). The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States, Clinical Infectious Diseases, ciaa815, doi:10.1093/cid/ciaa815 [DOI] [PMC free article] [PubMed]
- Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9:451–471. doi: 10.1002/jts.2490090305. [DOI] [PubMed] [Google Scholar]
- Tehrani N. The cost of caring—the impact of secondary trauma on assumptions, values and beliefs. Counseling Psychology Quarterly. 2007;20:325–339. doi: 10.1080/09515070701690069. [DOI] [Google Scholar]
- Tosone C, Bauwens J, Glassman M. The shared traumatic and professional posttraumatic growth inventory. Research on Social Work Practice. 2016;26(3):286–294. doi: 10.1177/1049731514549814. [DOI] [Google Scholar]
- Tosone C, McTighe JP, Bauwens J. Shared traumatic stress among social workers in the aftermath of Hurricane Katrina. British Journal of Social Work. 2015;45(4):1313–1329. doi: 10.1093/bjsw/bct194. [DOI] [Google Scholar]
- Tosone C, McTighe J, Bauwens J, Naturale A. Shared traumatic stress and the long-term impact of September 11th on Manhattan clinicians. Journal of Traumatic Stress. 2011;24(5):546–552. doi: 10.1002/jts.20686. [DOI] [PubMed] [Google Scholar]
- Tosone C, Nuttman-Shwartz O, Stephens T. Shared trauma: When the professional is personal. Clinical Social Work Journal. 2012;40(2):231–239. doi: 10.1007/s10615-012-0395-0. [DOI] [Google Scholar]
- van Mol M, Kompanje E, Benoit D, Bakker J, Nijkamp M. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. PLoS ONE. 2015;10(8):e0136955. doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5)–standard. (Measurement instrument). Available from www.ptsd.va.gov.
- Weinberg M, Gil S, Gilbar O. Forgiveness, coping, and terrorism: Do tendency to forgive and coping strategies associate with the level of posttraumatic symptoms of injured victims of terror attacks? Journal of Clinical Psychology. 2014;70(7):693–703. doi: 10.1002/jclp.22056. [DOI] [PubMed] [Google Scholar]
- Whitaker T, Weismiller T, Clark E. Assuring the sufficiency of a frontline workforce: A national study of licensed social workers. Executive summary. Washington, DC: National Association of Social Workers; 2006. [Google Scholar]
- Zerubavel N, Wright MO. The dilemma of the wounded healer. Psychotherapy. 2012;49(4):482–491. doi: 10.1037/a0027824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
(Data transparency).
(Software application or custom code).