Abstract
Bats act as a natural reservoir for many viruses, including coronaviruses, and have played a crucial epidemiological role in the emergence of many viral diseases. Coronaviruses have been known for 60 years. They are usually responsible for the induction of mild respiratory signs in humans. However, since 2002, the bat-borne virus started to induce fatal epidemics according to WHO reports. In this year, the first serious human coronavirus epidemic (severe acute respiratory syndrome; SARS) occurred (China, 8098 cases, 774 deaths [9.5% of the cases] in 17 countries). The case fatality was higher in elderly patients above 60 years and reached 50% of the cases. SARS epidemic was followed 10 years later by the emergence of the middle east respiratory syndrome (MERS) in Saudi Arabia (in 2012, 2260 cases, 803 deaths [35.5% of the cases] in 27 countries). Finally, in December 2019, a new epidemic in Wuhan, China, (corona virus disease 2019, COVID-19) emerged and could spread to 217 countries infecting more than 86,255,226 cases and killing 1,863,973 people by the end of 2020. There are many reasons why bats are ideal reservoir hosts for viral diseases such as the tolerance of their immune system to the invading viruses for several months. They can actively shed the viruses, although they develop no clinical signs (will be discussed in details later in the review). Bats were directly or indirectly involved in the three previous coronavirus epidemics. The indirect transmission takes place via intermediate hosts including civet cats for SARS and dromedary camels in the case of MERS. Although bats are believed to be the source of COVID-19 pandemic, direct pieces of evidence are still lacking. Therefore, coronaviruses’ role in epidemics induction and the epidemiological role of bats are discussed. The current work also presents different evidence (phylogenetic data, animal experiments, bats artificial infection studies, and computerized models of SARS-CoV2 evolution) that underline the involvement of bats in the epidemiology of the pandemic.
Keywords: MERS, SARS, Coronaviruses, Bats, Wuhan, COVID-19
Introduction
About 75% of the human emerging infectious diseases are zoonotic in origin and are mainly associated with wild animals (Markotter et al. 2020). The last few days of the year 2019 showed the emergence of a new epidemic of coronavirus (severe acute respiratory syndrome -2; SARS-CoV2). The pandemic, which was first reported in the Wuhan market in China, could spread to infect more than 86 million and to kill more than 1.8 million in 217 countries by the end of the year 2020. The pandemic not only has a huge impact on public health and world economy, but it also lead to radical changes in social habits and lifestyles (Decaro and Lorusso 2020). However, this virus was not the first coronavirus (CoVs) to emerge in the last decades. Bats, snakes, and pangolins meat are considered a delicacy in China (Cyranoski 2020) where large markets for wild animals exist. Wild animals are usually slaughtered for meat consumption or traditional medicine. The newly emerged coronavirus is believed to be evolved in wild animals such as snake (Bungarus multicinctus and Naja atra), Malayan pangolin (Manis javanica), Himalayan palm civets (Paguma larvata), Asian palm civet (Paradoxurus hermaphroditus), or bats like Aselliscus stoliczkanus, Rhinolophus affinis, and Rhinolophus sinicus (Li et al. 2020). The genomes of coronaviruses are characterized by their exceptional genetic plasticity and their ability to evolve rapidly. Therefore, it is possible to be evolved through the recombination of two unknown coronaviruses inside a bat. This flexibility enables them also to change their host range, tissue tropism, and their antigenic profile (Ji et al. 2020; Insights 2020; Decaro and Lorusso 2020; Guo et al. 2020).
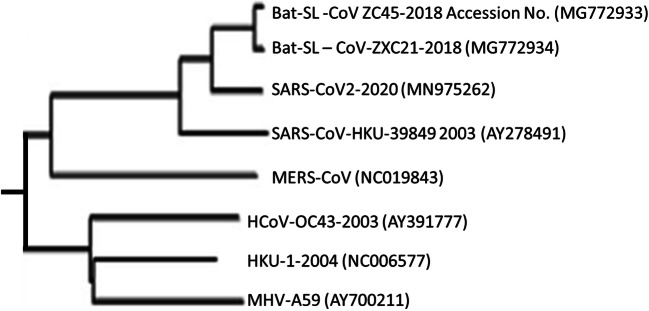
However, the primary SARS-CoV2 isolates in Wuhan were almost genomically identical and had genomic sequences homology of 99.9%. However, as a consequence of viral circulation in the human population, the virus started to adapt to the human environment by mutations, mostly in S, N, ORF8, ORF3a, and ORF1ab genes (Giandhari et al. 2020; Li et al. 2020; Awadasseid et al. 2021). Few days ago, new mutations were reported in the UK and South Africa. The new mutations are characterized by the high contagiousness and their rapid spread rate (Conti et al. 2021; Rahman et al. 2021). Genome analysis of the virus revealed a high sequence relationship with the two coronaviruses of Chinese’s bats (highest homology with the bat coronavirus RaTG13). Phylogenetic tree of betacoronaviruses showing that the SARS-CoV2 is related to the bat coronaviruses ZC45 and ZXC21 (Fig. 1). SARS-CoV2 showed, in addition, 99% sequence homology with CoV of pangolins according to the findings of a research team from South China Agricultural University. International panic and alarm signals have been released worldwide. This international panic is related to the high contagiousness of the virus (Cyranoski 2020). The ongoing coronavirus disease 2019 (COVID-19) is not the first serious coronavirus epidemic. In the last few years, many lethal variants of coronaviruses emerged, such as the SARS-CoV (severe acute respiratory syndrome) virus (origin China, in 2002, with 774 deaths) and MERS-CoV (Middle East respiratory syndrome) virus (origin Saudi Arabia, in 2012, with 803 deaths). While SARS originated from civet cats, MERS evolved in dromedary camels. However, both SARS and MERS viruses are believed to be of bat origin and have been adapted later to civets and camels (Zaki et al. 2012; Fehr and Perlman 2015; Lacroix et al. 2020).
Fig. 1.
Phylogenetic tree of betacoronaviruses showing that the SARS-CoV-2 is related to the bat coronaviruses ZC45 and ZXC21
Some researchers believe that even MERS could also be originated from China as all three types of bat MERS-cluster of coronavirus could be detected in China (van Boheemen et al. 2012; Fan et al. 2019). A third severe outbreak of coronaviruses occurred in pigs in 2017, where swine acute diarrhoea syndrome (SADS) induced significant economic losses to the swine industry worldwide (Fan et al. 2019; Zhou et al. 2018).
Coronaviruses
The first characterized member of the coronavirus was the avian infectious bronchitis virus which was isolated in the year 1937 from chicken eggs. Later on, in the 1940s, another two members have been identified: the porcine transmissible gastroenteritis virus (in swine) and mouse hepatitis virus (from mice). Then, the human coronaviruses and porcine hemagglutinating encephalomyelitis virus were identified in the 1960s and, subsequently, the feline coronavirus, canine coronavirus, bovine coronavirus, turkey coronavirus, and the porcine epidemic diarrhoea virus (in the 1970s). Finally, the porcine respiratory coronavirus was the last discovered member of the corona family in the twentieth century (1984). The continuous evolution of coronaviruses due to their ability to recombine and jump among different host species makes them a serious public health threat (Wang 2016). For example, laboratory investigations have shown that although the bat coronavirus HKU4 is closely related to MERS-CoV, the S protein of HKU4 is not able to support viral entry to human cells unless two required mutations are introduced to the viral spike (S) protein-encoding gene. The field isolates of MERS-CoV were found to harbour these two mutations, which are necessary to mediate bat-human infection either directly or via an intermediate host as dromedaries (Yang et al. 2015).
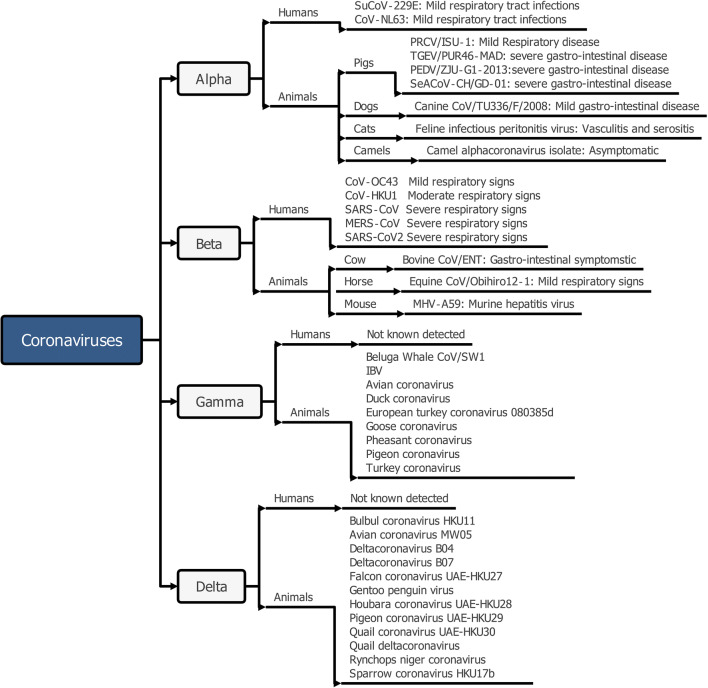
The name “coronavirus” is derived from the word corona (a Latin word meaning “crown”) because of the characteristic appearance of the viral particles under the electron microscope. Coronaviruses (CoVs) are enveloped positive-sense single-strand RNA viruses. They are characterized by their large RNA genome (27–32 kb in size) and their club-like spikes (S) that project from their outer surface to facilitate adhesion to host receptors. They own unusually large RNA genomes. Coronaviruses cause various diseases in mammals and birds, ranging from enteritis in cows and pigs and upper respiratory disease chickens to potentially lethal human respiratory infections. Coronaviruses (CoVs) are members of the subfamily Coronavirinae, family Coronaviridae. CoVs are subdivided into genera, Alpha-, Beta-, Gamma-, and Deltacoronavirus (Fig. 2) (Fehr and Perlman 2015). Alpha and Beta CoV have a limited host scope and can only infect mammals. Meanwhile, gamma and delta CoV infect mainly birds with some exceptional members that can infect birds and mammals (Woo et al. 2012).
Fig. 2.
Coronaviruses affecting humans and animals
In turn, Betacoronavirus can be divided into five subgenera (Embecovirus, Sarbecovirus, Merbecovirus, Nobecovirus, and Hibecovirus) (ICTV 2019). The three CoV responsible for the COVID-19, MERS, and SARS outbreaks belong to the subgenus Betacoronavirus. The zoonotic potential of both Merbecovirus and Sarbecovirus has been previously documented. They primarily infected camels and civets as intermediate hosts before they initiated MERS and SARS pan-epidemics, respectively. Later on, the human-to-human nosocomial transmission of the virus was possible (Wong et al. 2019; Dong et al. 2020; Cui et al. 2019).
CoVs are also characterized by their highly conserved genomic structure and their unique replication mechanisms which, in addition to other factors, are responsible for their continuous recombination and evolution (Wong et al. 2019). Coronaviruses vary in their degree of genetic flexibility. While some of them are highly conserved (e.g., HCoV-229E) which kept its genetic code conserved even among isolates from different countries with minimal sequence changes, others (e.g., HCoV-OC43) showed clear genetic variations even among field isolates revealed from the same locality over the years. Viruses with structural flexibility can usually adapt to new hosts (Chibo and Birch 2006; Vijgen et al. 2005).
Bats antiviral innate immunity and coronaviruses
Bats are unique mammals belonging to the order Chiroptera. They are the only mammals capable of sustained flight. They are the second-largest group of mammals after rodents and represent about 20% of mammalian diversity with more than 1400 species. Most of them are nocturnal (night-active). The order Chiroptera is divided into two suborders: megabats and microbats. However, this classification was changed based on transcriptome/genetic relationships into the suborder Yinpterochiroptera, or Pteropodiformes (including the megabats in addition to five microbat families, namely, Rhinopomatidae, Megadermatidae, Hipposideridae, Rhinolophidae, and Craseonycteridae) and the suborder Yangochiroptera or Vespertilioniformes (involving the remaining microbat families, namely, the families Emballonuridae, Furipteridae, Miniopteridae, Molossidae, Mormoopidae, Mystacinidae, Myzopodidae, Natalidae, Noctilionidae, Nycteridae, Phyllostomidae, Thyropteridae, Cistugidae, and Vespertilionidae). The megabats are large and mainly frugivores (fruit-eating) bats, while the rest of the species are either frugivores or insectivores. Few species were fed on animal blood (vampire bats). Microbats are additionally characterized by their echo-locating properties (Hutcheon and Kirsch 2006; Tsagkogeorga et al. 2013; Teeling et al. 2005). Bats are gregarious mammals. They usually live in large dense populations of millions of individuals in dense aggregations up to 3000 bats/m2. The high density and the extreme closeness of bats supports the transmission of viruses among the roosts and the spillover of the viruses to other animal species (Roes 2020). Therefore, they represent a potential threat to public health due to their role as a natural reservoir for many serious zoonotic viruses. The epidemiological role of bats in disease emerge was first recognized in the 1920s in connection with their role in spreading rabies and rabies-related lyssaviruses to humans and livestock. This epidemiological role was again confirmed in 1994 via their role in the spread of Hendra virus among horses and Nipah, SARS, and filoviruses (Marburg, Ebola, and Mengla virus) among humans (Peiris et al. 2004; Johnson et al. 2010; Li et al. 2005). Bat examination revealed the presence of viruses from most of the known viral families, including Rhabdoviruses, paramyxoviruses, filoviruses, and coronaviruses without showing any clinical signs (Wang and Cowled 2015; Markotter et al. 2020). The simultaneous presence of various viral genomes in bats enables the permanent evolution of new unknown viruses in bats (Woo et al. 2012). Their epidemiological role is supported by and attributed to many factors, including (1) their long-life span and lifestyle. Bats can live relatively long and fly to cover large geographical areas, which allow horizontal and vertical viral spread among bats themselves or bats and humans/animals (Olival et al. 2017); (2) their roosting behaviour in huge numbers even millions of bats in caves, trees, and also in human-made buildings increases the bat-bat and bat-human viral transmission (Chege et al. 2015) (3) being the only flying mammals modified their metabolic activities. The increase in their body temperature during flying resembles the febrile response by other mammals and activates the immune system. The modification of their metabolic activity leads to the tolerance of a greater diversity of co-existing viruses in their environment (O’Shea et al. 2014; Canale and Henry 2010); and finally, (4) bat/viruses co-evolutionary relationship and interaction allowed their parallel existence in an equilibrium pattern. This enabled their immune system to tolerate invading viruses without expressing any clinical signs (remain asymptomatic) (Banerjee et al. 2018). The adaptation of their immune system to control viral replication depends on a mixture of factors including their multiple immunoglobulins, different antibody responses, produced interferons, interleukins and cytokines, receptor recognition, and even modified cell-mediated T-cell responses (Baker et al. 2013; Skirmuntt et al. 2020). All these factors make them ideal viral host reservoirs for humans and other mammalian species. In parallel, the coexistence of different coronaviruses at the same time in one bat was reported. The tolerance of the viruses in the bats and the coexistence of many CoV enable their recombination, mutations, and persistence and as well as enhance the emergence and evolution of new CoV diseases (Wang et al. 2011; Calisher et al. 2006; Fan et al. 2019).
As a reservoir host of many viruses, the immune system of bats was evolved to counteract the protein-mediated modulation of antiviral responses. Basically, the immune system of bats differs from other mammals and has bat-specific transcripts. The tolerance of the bats’ innate immune system to viruses could only be explained following the sequencing of their whole genome. Genome comparison identified clear differences between human and bat genome structure. While the immune genes in the human genome represent 7% of the whole genome, they represent only 2.75 to 3.5% in bat genomes according to species. Bats evolved unique mechanisms to limit virus-induced pro-inflammatory responses meanwhile keeping type I IFN responses in order to limit the propagation of invading viruses (Banerjee et al. 2020). Bat genome contains only 3 IFN type 1 alpha genes that are important for antiviral pathways and innate immunity in contrast to the human genome (13 genes) and cattle genome (24 genes) (Baker et al. 2013). The unstimulated bat cells usually contain high interferon levels that provide bats with high and permanent protection niveau, contrary to other mammalian tissues that contain low levels of interferon. The interferon level increases only upon stimulation through viral invasion. The on-demand increase in interferon level is important due to the toxic effect of high interferon levels on mammalian cells except for bats (Samuel 2001; Smith and Wang 2013). Moreover, although bats produce considerable levels of antibodies in response to viral infection, the produced antibodies have less neutralizing power. It is suggested that produced antibodies in bats control viral invasion in a different pattern independent of viral neutralization (Banerjee et al. 2020).
Bats and SARS-CoV2
Bats are the natural reservoir host for potentially zoonotic viruses. Till date, researchers could isolate over 200 viruses from almost all viral families from bats (Misra 2020). Despite decades of intensive research concerning bat-borne zoonotic viruses, the epidemiology and mechanisms of viral evolution in bats, the patterns of viral co-infection, and competition dynamics are still nascent. Many questions remain open and largely unexplored, limiting our ability to prepare for the next coronavirus outbreak (Letko et al. 2020).
Bats can normally harbour various members of coronaviruses over several months without showing any clinical symptoms. Moreover, infected bats with CoV produce lower levels of IL-1β secretion and ASC (apoptosis-associated speck-like protein containing a CARD) than other mammals without affecting the viral propagation capacity which makes them ideal reservoir hosts for viruses (Ahn et al. 2019; Hall et al. 2020). Therefore, bats are considered to be exceptional mammals that provide a large genomic pool for the emerge of novel human coronavirus (Zhu et al. 2020). This may be attributed to the extreme genomic flexibility of coronaviruses which makes it difficult to pinpoint the exact reservoir (Bonilla-Aldana et al. 2020). Although almost all literature consider bats as the source of SARS-CoV2, direct pieces of evidence are still lacking (Lacroix et al. 2020). However, enough arguments for bat accusation are available which are based mainly on four argumentative approaches: (1) experience gathered from previous Betacoronavirus (Beta-CoV) epidemics where all known human coronavirus pandemics originated from bats (as discussed above) (Zhu et al. 2020); (2) phylogenic relationship of SARS-CoV2 and related clades; (3) data obtained through artificial infection of bats with SARS-CoV2; and (4) computerized models of SARS-CoV2 evolution.
Phylogenic relationship of SARS-CoV2 clades
Recently, it has been shown that bat isolates of coronaviruses are the major parent contributor for fractions of coronavirus sequences (Zhu et al. 2020). Full-genome sequencing and phylogenetic analysis of various SARS-CoV2 clusters revealed a variable degree of relationship to other bats coronaviruses (Zhou et al. 2020; Boni et al. 2020; Yan et al. 2020). Coronaviruses of bat origin could closely align with isolates of 32 other host species and possess the highest number of coronaviruses subclades (Zhu et al. 2020).
A recent study showed that the bat coronavirus 3CLpro shares 99.02% of sequence identity with SARS-CoV2. Sequencing of both 3CLpro and SARS-CoV2 viruses revealed key genomic differences between them and the remaining clades of betacoronaviruses (Sofi et al. 2020). Similarly, closely related SARS-CoV-2 isolates could also be detected in R. cornutus bats in Japan (Murakami et al. 2020).
In addition to bats, whole-genome blasting studies detected further SARS-CoV2 closely related to coronavirus that originates from pangolin (pangolin-MP789 strain). Both viruses share 99% sequence homology (Alexandrova et al. 2020). Notably, the evolution of SARS-CoV2 through the recombination between the genome of the horseshoe bats isolate and the receptor-binding domain of pangolin-CoV was suggested by many researchers (Bonilla-Aldana et al. 2020).
In summary, the phylogenetic investigation indicated that SARS and SARS-related viruses have likely diverged from a common ancestral bat-derived coronavirus. Meanwhile, the bat CoV and SARS-CoV-2 may be diverged from their common ancestor 40–70 years ago. From the epidemiological viewpoint, it is almost evident that SARS-CoV2 spilled from a bat reservoir host to humans, either directly or indirectly through an intermediate animal species (Fenton et al. 2020; Boni et al. 2020; Yan et al. 2020) .
However, contrary to the findings of the phylogenetic studies based on virus genome, phylogenetic classification based on spike glycoprotein (S protein) amino acid sequences refers to significant differences in the structure of the key receptor binding and O-linked glycan residues. Only one isolate (PRJNA573298 / Malayan pangolin isolate) showed 100% identity with SARS-CoV2 (Malaiyan et al. 2020).
Artificial infection of bats with SARS-CoV2
Only one publication could be found in the data bank describing artificial infection of bats with SARS-CoV2. The work reported intranasal infection of fruit bats (Rousettus aegyptiacus) with the virus. The obtained data from bat inoculation revealed the characteristics signs of a reservoir host and differed from that obtained by artificial infection of other mammals such as ferrets. The inoculated bats showed neither clinical signs nor fever, no bodyweight loss or mortalities could also be reported in all inoculated bats. However, low levels of neutralizing antibodies could be measured in some bats. Besides, oral, and faecal shedding of the virus have been also observed. Inoculated bats could infect other bats in contact. The viral RNA could be detected in the respiratory and digestive tract epithelium and the associated lymph nodes by RT-qPCR assay. Notably, autopsy and histopathology studies carried on infected bats did not reveal any gross pathological lesions except minimal epithelial necrosis, oedema, and WBCs infiltrating in the nasal mucosa (Schlottau et al. 2020).
In another study, using stem cell technology, human enteroids and enteroids prepared from horseshoe bats (Rhinolophus sinicus) were inoculated with the SARS-CoV2 virus. Both tissues developed progressive cytopathic effect (CPE) associated with the substantial increase in the viral load in the culture media. The robust replication of SARS-CoV-2 replication in bat enteroids suggests a possible role of the intestinal mucosa of horseshoe bats in the maintenance of the virus in nature (Zhou et al. 2020).
Computational analysis of SARS-CoV-2 and related clades
Analysis of different origins was also used to determine the source of SARS-CoV-2 pandemic using a large collection of contemporary methodologies. Such computational studies compared the sequences of the six open reading frames (ORFs) of the isolates, in addition to the sequence of the 16 non-structural proteins and the four structural proteins (M, N, E, and S). Moreover, the studies compared their codon usage, missense mutations, and variant levels. Furthermore, the studies compared the CpG dinucleotide contents and mutation patterns of SARS-CoV-2 clades and their related viruses (Dimonaco et al. 2020; Matyášek and Kovařík 2020). The performed computational analysis supported other reports considering RaTG13 coronavirus isolated from Rhinolophus affinis (horseshoe bat) as the ancestor of SARS-CoV-2 virus. Uniquely, both RaTG13 and SARS-CoV-2 clades exhibited CpG depletion in their genomes in contrast to other known coronaviruses (Matyášek and Kovařík 2020). Behind RaTG13 isolate, the pangolin-MP789 isolate ranked in the second position as closest relative to SARS-Co2 virus (Dimonaco et al. 2020; Alexandrova et al. 2020). Finally, members of order Chiroptera consist of more than 1400 different species of bats, not all of them can support SARS-CoV-2 replication (Boni et al. 2020). The obtained data through the four previously discussed approaches provide strong pieces of evidence that consider certain species of bats as the natural reservoir host and source of SARS-CoV-2.
Animal and human diseases caused by CoVs
CoVs are mainly animal pathogens responsible for significant economic losses in livestock, pets, and birds. The virus induces gastroenteritis in calves and piglets and for renal and upper respiratory diseases in poultry. Four coronaviruses (two α-CoVs: HCoV-NL63, HCoV-229E) and two β-CoVs (HCoV-OC43 and HKU1 CoV) are known to cause mild respiratory signs in humans, which may result in pneumonia and bronchiolitis in children, elderly, or immunocompromised individuals. However, they came into focus only after the emergence of the pandemic SARS in 2002, characterized by severe respiratory signs that may lead to life-threatening respiratory failure. In addition to SARS, other emerging coronaviruses lead to human pandemics (MERS and COVID-19) or severe animal outbreaks (e.g., porcine delta coronaviruses) (Su et al. 2016; Forni et al. 2017; van der Hoek 2007; van der Hoek et al. 2005). Bats were found to be the reservoir host for most coronaviruses, namely, 10 out of 17 α-CoV and 7 out of 12 β-CoV from viruses that may have the zoonotic potential(Leopardi et al. 2018).
Animal pathogenic members of the CoV are listed in Table 1 while the human-specific coronaviruses are listed in Table 2.
Table 1.
Some of the most commonly known animal pathogenic coronaviruses are listed in relation to their host species
| Coronavirus | Host | Reference |
|---|---|---|
| Transmissible gastroenteritis virus (TGEV) | Swine | (Banerjee et al. 2019) |
| Porcine epidemic diarrhoea virus (PEDV) and swine acute diarrhoea syndrome coronavirus (SADS-CoV) | Swine | (Schulz and Tyler 2006) |
| Porcine hemagglutinating encephalomyelitis virus (PHEV) | Swine | (Mora-Díaz et al. 2019) |
| Feline enteric coronavirus (FCoV) | Feline | (Harun et al. 2013) |
| Feline infectious peritonitis virus (FIPV) | Feline | (Harun et al. 2013) |
|
Co. bronchitis virus. Bovine CoV: infectious bronchitis co. Virus (IBV) |
Bovine, Camels, Deer | (Perlman and Netland 2009, Colvero et al. 2015) |
|
Rat CoV: infectious bronchitis virus (IBV) in rats and chickens Poultry CoV: respiratory and urogenital disease |
Rats, Poultry | |
| Whale CoV: CoV. respiratory disease | Whales | (Mihindukulasuriya et al. 2008) |
| Murine hepatitis virus (MHV) | Mice | (Kuo and Masters 2013) |
Table 2.
Seven known human-specific CoV in relation to the severity of their infection in humans
| CoV | Severity of the disease | Reference |
|---|---|---|
| HCoV-229E and HCoV-OC43 (known for decades) | Mild resp. signs | (McIntosh et al. 1967) |
| HCoV-NL63 and HCoV-HKU1 (recently discovered) | Mild resp. signs | (Woo et al. 2005) |
| SARS | Serious respiratory signs with low mortality rate | (Lim et al. 2016, Lau et al. 2005, Peiris et al. 2004) |
| MERS | Serious respiratory signs with high mortality rate | (Yang et al. 2015) |
| SARS-CoV2 | Serious respiratory signs with high contagiousness and low mortality rate | (CDC 2020) |
Pathogenesis of coronavirus in humans
In the past, prior to SARS, coronavirus infections were only responsible for mild and self-limiting clinical signs, so there was no need for hospitalization or the development of special treatment (Hamre and Procknow 1966; van der Hoek et al. 2005).
Following exposure to CoV, it adheres to the cell receptors by their surface spike (S) protein.
The spike (S) protein of SARS can be cleaved by human proteases into two subunits (S1 and S2). The receptor-binding domain (RBD) present in S1 is responsible for binding to ACE2 host receptors. A small fraction of the RBD, known as the receptor-binding motif (RBM), is very important as it determines the viral tissue tropism and host range (Xu et al. 2004b; Xu et al. 2004a; Hofmann et al. 2004). Successful adhesion of S1 to the host receptors stimulates the S2 subunit to start fusion between the viral envelope and cell membrane (Sainz et al. 2005).
However, the three newly emerged serious human CoV used different human cell receptors. The availability of specific receptors determines the viral tropism and host range. CoV uses four types of receptors: (1) angiotensin-converting enzyme 2 (ACE2) by SARS-CoV, SARS-CoV2, and HCoV-NL63; (2) dipeptidyl peptidase 4 (DPP4) by MERS-CoV; (3) aminopeptidase N by HCoV-229E; and (4) 9-O-acetylated sialic acid by HCoV-OC43 and HKU1 viruses. Some viruses can adhere to many receptors (e.g., SARS uses mainly ACE2, while CD209L can be used as an alternative one). The type of receptors used indicates the target cells of the pathogen (tissue tropism). While viruses using ACE2 receptors mainly infect ciliated bronchial epithelial cells and type II pneumocytes, viruses that use DPP4 receptors mainly infect unciliated bronchial epithelial cells and type II pneumocytes (Cui et al. 2019; Li et al. 2003; Yeager et al. 1992; Li et al. 2007; Wu et al. 2009; van Doremalen et al. 2014; Jeffers et al. 2004).
Most CoVs can enter the cells via the conventional endosomal route, while some of them enter the cells through a non-endosomal pathway or a combination of both routes (Bosch et al. 2008; Qian et al. 2013). Besides, host proteases are also required for viral entrance as cathepsin L for both SARS- and MERS-CoV, transmembrane protease serine 2 (TMPRSS2), and airway trypsin-like protease TMPRSS11D for SARS and furin for MERS (Bertram et al. 2013; Bertram et al. 2011; Millet and Whittaker 2014).
Human coronaviruses spread directly among humans via aerosol droplets (person-to-person contact) and possibly from infected mothers to their unborn babies (WOMB infection) according to some reports (Jeffers et al. 2004). Following infection, the virus binds to cell receptors which are found on the endothelial cell lining of mucous membranes, and this step is followed by the viral spread to various organs of the body. At this stage, different body secretions (such as sweat, urine, faeces, sputum, and respiratory discharges) become loaded with the viral particles (Ding et al. 2004).
The severe elevation of proinflammatory chemokines and cytokine levels in SARS patients can lead to an atypical type of pneumonia accompanied by respiratory failure (Ding et al. 2004). On the other hand, the receptors of MERS-CoV in the human body are mainly DPP4/CD26 which are present on the mucosal surface of the respiratory system, liver, kidney, and even the prostate gland. Therefore, the tissue tropism of MERS is broader than that of SARS, which explains the severity of MERS and its higher fatality rate in comparison with SARS (Widagdo et al. 2016; Stewart et al. 2005; Chu et al. 2014). Besides, in contrast to SARS, MERS was found to dysregulate the immune system and cause apoptosis of renal tissues (Yeung et al. 2016; Liu et al. 2017; Chan et al. 2013).
Diagnosis and control of CoV diseases in both animals and humans
Before 2002, the known CoV infections were mild. Therefore, accurate diagnosis and development of specific treatments/vaccines did not have high priority. However, after the emergence of fatal epidemics like SARS, MERS, and COVID-19 in humans and SADS-CoV in swine, diagnostic RT-PCR and multiplex RT-PCR assays were developed for the diagnosis of CoVs (Emery et al. 2004; Gaunt et al. 2010; El-Sayed and Kamel 2021). Similarly, for the diagnosis of the COVID-19, the WHO recommended the use of RT-PCR assays (WHO 2020). These systems were developed early following the successful isolation and cultivation of the virus at the Peter Doherty Institute for Infection and Immunity, Melbourne, Australia, January 29, 2020, available at https://www.doherty.edu.au/news-events/news/coronavirus and its whole genome sequencing (Wuhan Seafood market pneumonia virus GenBank: MN908947.3). In addition to RT-PCR, various serological assays were also approved to be used for the diagnosis and differential diagnosis of the disease (Fehr and Perlman 2015).
At the time, no specific treatment is available against CoVs. Virus-specific neutralizing antibodies are available for use in critical cases. Meanwhile, commercial CoV vaccines are available only for veterinary use against IBV, PEDV, TGEV, and canine CoV. Other vaccines developed for human use are under trial and have not yet been approved (Stockman et al. 2006; Fehr and Perlman 2015). Both S1 and S2 proteins are good candidates for vaccine development. Antibodies targeting one of both subunits protect against virus infection of target cells (Keng et al. 2005; Zhou et al. 2004). However, the use of S proteins in vaccine preparation was not promising and promoted infection (Vennema et al. 1990). On the other hand, the use of a naturally attenuated living viral vaccine showed promising results in the control of TGEV outbreaks in Europe and the USA using an attenuated strain (PRCV) or the use of artificially mutated/manipulated variants of the virus. However, possible viral recombination of the vaccinal strain and other viruses represents an additional public health concern (Laude et al. 1993; Graham et al. 2012).
Several trials were carried out to construct attenuated live vaccines, subunit, recombinant vector, or DNA vaccines targeting one or both subunits to protect against SARS or MERS. However, many of these vaccines have achieved various degrees of success in laboratory animals. They are not used for human protection against SARS or MERS due to their lack of efficiency or public health risk (Tai et al. 2017; Wang et al. 2015; Gilbert and Warimwe 2017; Kim et al. 2014; Modjarrad 2016; Vickers 2017).
To minimize the possible viral recombination, deletion of the large fragment from the viral nsp1 gene (encoding nonstructural RNA-binding protein responsible for viral replication) or envelope (E) encoding gene (encodes a membrane protein involved in budding, envelope formation, and virus pathogenesis). Deletion of one or both of these genes could be the best available concept for this purpose or via the modification of the TRS sequence (Züst et al. 2007; Netland et al. 2010; Yount et al. 2006).
As mentioned above, the absence of both effective therapeutics and protective vaccines against corona outbreaks makes the performance of adequate control measures strongly recommended (Fehr and Perlman 2015).
In conclusion
The current work summarizes different emerging human and animal diseases caused by coronaviruses. The review discusses briefly, besides, possible sources of the SARS-CoV-2 virus and the epidemiological role of bats as a natural reservoir host of coronaviruses. Understanding the immunological and physiological factors that enable bats from playing this epidemiological public health threatening role will help in the early prediction, prevention, management, and control of future coronavirus epidemics. Understanding the mechanisms by which they can inhibit virus protein-mediated modulation following viral invasion will enable the development of novel therapeutic approaches. It is certainly the right time to strictly regulate wildlife markets due to the well-documented role of wild animals in the emerge of serious human pathogens in the last decades.
Author contribution
AE and MK wrote the initial draft of the manuscript. All authors (AE and MK) have read, edited, and finally approved the final manuscript.
Data Availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Highlights
• Coronaviruses and their emergence
• Epidemiological role of bats in coronaviruses emergence
• Bats antiviral innate immunity
• Role of coronaviruses in disease induction
• SARS, MERS, and SARS-CoV2 outbreaks
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Amr El-Sayed and Mohamed Kamel contributed equally to this works.
References
- Ahn M, Anderson DE, Zhang Q, Tan CW, Lim BL, Luko K, Wen M, Chia WN, Mani S, Wang LC, Ng JHJ, Sobota RM, Dutertre C-A, Ginhoux F, Shi Z-L, Irving AT, Wang L-F (2019) Dampened NLRP3-mediated inflammation in bats and implications for a special viral reservoir host. Nature microbiology:789–799. 10.1038/s41564-019-0371-3 [DOI] [PMC free article] [PubMed]
- Alexandrova R, Beykov P, Vassilev D, Jukić M, Podlipnik Č. The virus that shook the world: questions and answers about SARS-CoV-2 and COVID-19. Biotechnol Biotechnol Equip. 2020;35(1):74–102. doi: 10.1080/13102818.2020.1847683. [DOI] [Google Scholar]
- Awadasseid A, Wu Y, Tanaka Y, Zhang W. SARS-CoV-2 variants evolved during the early stage of the pandemic and effects of mutations on adaptation in Wuhan populations. Int J Biol Sci. 2021;17(1):97–106. doi: 10.7150/ijbs.47827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker ML, Schountz T, Wang L-F. Antiviral immune responses of bats: a review. Zoonoses Public Health. 2013;60(1):104–116. doi: 10.1111/j.1863-2378.2012.01528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A, Misra V, Schountz T, Baker ML. Tools to study pathogen-host interactions in bats. Virus Res. 2018;248:5–12. doi: 10.1016/j.virusres.2018.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A, Kulcsar K, Misra V, Frieman M, Mossman K. Bats and coronaviruses. Viruses. 2019;11(1):41. doi: 10.3390/v11010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A, Baker ML, Kulcsar K, Misra V, Plowright R, Mossman K (2020) Novel insights into immune systems of bats. Front Immunol 11. 10.3389/fimmu.2020.00026 [DOI] [PMC free article] [PubMed]
- Bertram S, Glowacka I, Müller MA, Lavender H, Gnirss K, Nehlmeier I, Niemeyer D, He Y, Simmons G, Drosten C. Cleavage and activation of the severe acute respiratory syndrome coronavirus spike protein by human airway trypsin-like protease. J Virol. 2011;85(24):13363–13372. doi: 10.1128/JVI.05300-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram S, Dijkman R, Habjan M, Heurich A, Gierer S, Glowacka I, Welsch K, Winkler M, Schneider H, Hofmann-Winkler H. TMPRSS2 activates the human coronavirus 229E for cathepsin-independent host cell entry and is expressed in viral target cells in the respiratory epithelium. J Virol. 2013;87(11):6150–6160. doi: 10.1128/JVI.03372-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boni MF, Lemey P, Jiang X, Lam TT-Y, Perry BW, Castoe TA, Rambaut A, Robertson DL. Evolutionary origins of the SARS-CoV-2 sarbecovirus lineage responsible for the COVID-19 pandemic. Nat Microbiol. 2020;5(11):1408–1417. doi: 10.1038/s41564-020-0771-4. [DOI] [PubMed] [Google Scholar]
- Bonilla-Aldana DK, Jimenez-Diaz SD, Arango-Duque JS, Aguirre-Florez M, Balbin-Ramon GJ, Paniz-Mondolfi A, Suárez JA, Pachar MR, Perez-Garcia LA, Delgado-Noguera LA, Sierra MA, Muñoz-Lara F, Zambrano LI, Rodriguez-Morales AJ. Bats in ecosystems and their Wide spectrum of viral infectious potential threats: SARS-CoV-2 and other emerging viruses. Int J Infect Dis. 2020;102:87–96. doi: 10.1016/j.ijid.2020.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch BJ, Bartelink W, Rottier PJ. Cathepsin L functionally cleaves the severe acute respiratory syndrome coronavirus class I fusion protein upstream of rather than adjacent to the fusion peptide. J Virol. 2008;82(17):8887–8890. doi: 10.1128/jvi.00415-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calisher CH, Childs JE, Field HE, Holmes KV, Schountz T. Bats: important reservoir hosts of emerging viruses. Clin Microbiol Rev. 2006;19(3):531–545. doi: 10.1128/CMR.00017-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canale CI, Henry P-Y. Energetic costs of the immune response and torpor use in a primate. Funct Ecol. 2010;25(3):557–565. doi: 10.1111/j.1365-2435.2010.01815.x. [DOI] [Google Scholar]
- CDC (2020) Novel Coronavirus (2019-nCoV) Situation Summary
- Chan RWY, Chan MCW, Agnihothram S, Chan LLY, Kuok DIT, Fong JHM, Guan Y, Poon LLM, Baric RS, Nicholls JM. Tropism of and innate immune responses to the novel human betacoronavirus lineage C virus in human ex vivo respiratory organ cultures. J Virol. 2013;87(12):6604–6614. doi: 10.1128/JVI.00009-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chege HN, Schepers C, Wolfaardt GJJ. Documenting the bat species assemblages of the Meletse Bat Research and Conservation Training Centre in Limpopo Province, Thabazimbi. South Africa. Afr Bat Conserv News. 2015;38:5–8. [Google Scholar]
- Chibo D, Birch C. Analysis of human coronavirus 229E spike and nucleoprotein genes demonstrates genetic drift between chronologically distinct strains. J Gen Virol. 2006;87(5):1203–1208. doi: 10.1099/vir.0.81662-0. [DOI] [PubMed] [Google Scholar]
- Chu H, Zhou J, Wong BH-Y, Li C, Cheng Z-S, Lin X, Poon VK-M, Sun T, Lau CC-Y, Chan JF-W. Productive replication of Middle East respiratory syndrome coronavirus in monocyte-derived dendritic cells modulates innate immune response. Virology. 2014;454:197–205. doi: 10.1016/j.virol.2014.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colvero LP, Villarreal LYB, Torres CA, Brañdo PE. Assessing the economic burden of avian infectious bronchitis on poultry farms in Brazil. Rev Sci Tech. 2015;34(3):993–999. doi: 10.20506/rst.34.3.2411. [DOI] [PubMed] [Google Scholar]
- Conti P, Caraffa A, Gallenga CE, Kritas SK, Frydas I, Younes A, Di Emidio P, Tetè G, Pregliasco F, Ronconi G (2021) The British variant of the new coronavirus-19 (Sars-Cov-2) should not create a vaccine problem. J Biol Regul Homeost Agents [PubMed]
- Cui J, Li F, Shi Z-L. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranoski D (2020) Did pangolins spread the China coronavirus to people? https://www.nature.com/articles/d41586-020-00364-2 [DOI] [PubMed]
- Decaro N, Lorusso A. Novel human coronavirus (SARS-CoV-2): a lesson from animal coronaviruses. Vet Microbiol. 2020;244:108693. doi: 10.1016/j.vetmic.2020.108693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimonaco NJ, Salavati M, Shih BB. Computational analysis of SARS-CoV-2 and SARS-like coronavirus diversity in human, bat and pangolin populations. Viruses. 2020;13(1):49. doi: 10.3390/v13010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y, He L, Zhang Q, Huang Z, Che X, Hou J, Wang H, Shen H, Qiu L, Li Z. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol. 2004;203(2):622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong N, Yang X, Ye L, Chen K, Chan EW-C, Yang M, Chen S (2020) Genomic and protein structure modelling analysis depicts the origin and infectivity of 2019-nCoV, a new coronavirus which caused a pneumonia outbreak in Wuhan, China. bioRxiv
- El-Sayed A, Kamel M. Future threat from the past. Environ Sci Pollut Res. 2021;28(2):1287–1291. doi: 10.1007/s11356-020-11234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery SL, Erdman DD, Bowen MD, Newton BR, Winchell JM, Meyer RF, Tong S, Cook BT, Holloway BP, McCaustland KA. Real-time reverse transcription–polymerase chain reaction assay for SARS-associated coronavirus. Emerg Infect Dis. 2004;10(2):311–316. doi: 10.3201/eid1002.030759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Y, Zhao K, Shi ZL, Zhou P (2019) Bat coronaviruses in China. Viruses 11(3). 10.3390/v11030210 [DOI] [PMC free article] [PubMed]
- Fehr AR, Perlman S (2015) Coronaviruses: an overview of their replication and pathogenesis. In: Coronaviruses. Springer, pp 1–23 [DOI] [PMC free article] [PubMed]
- Fenton MB, Mubareka S, Tsang SM, Simmons NB, Becker DJ. COVID-19 and threats to bats. FACETS. 2020;5(1):349–352. doi: 10.1139/facets-2020-0028. [DOI] [Google Scholar]
- Forni D, Cagliani R, Clerici M, Sironi M. Molecular evolution of human coronavirus genomes. Trends Microbiol. 2017;25(1):35–48. doi: 10.1016/j.tim.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaunt ER, Hardie A, Claas ECJ, Simmonds P, Templeton KE. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48(8):2940–2947. doi: 10.1128/JCM.00636-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giandhari J, Pillay S, Wilkinson E, Tegally H, Sinayskiy I, Schuld M, Lourenco J, Chimukangara B, Lessells R, Moosa Y, Gazy I, Fish M, Singh L, Khanyile KS, Fonseca V, Giovanetti M, Alcantara LC, Petruccione F, de Oliveira T (2020) Early transmission of SARS-CoV-2 in South Africa: an epidemiological and phylogenetic report. medRxiv. 10.1101/2020.05.29.20116376 [DOI] [PMC free article] [PubMed]
- Gilbert SC, Warimwe GM. Rapid development of vaccines against emerging pathogens: the replication-deficient simian adenovirus platform technology. Vaccine. 2017;35(35):4461–4464. doi: 10.1016/j.vaccine.2017.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham RL, Becker MM, Eckerle LD, Bolles M, Denison MR, Baric RS. A live, impaired-fidelity coronavirus vaccine protects in an aged, immunocompromised mouse model of lethal disease. Nat Med. 2012;18(12):1820–1826. doi: 10.1038/nm.2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Hu B-J, Yang X-L, Zeng L-P, Li B, Ouyang S, Shi Z-L (2020) Evolutionary arms race between virus and host drives genetic diversity in bat severe acute respiratory syndrome-related coronavirus spike genes. J Virol 94. 10.1128/JVI.00902-20 [DOI] [PMC free article] [PubMed]
- Hall JS, Knowles S, Nashold SW, Ip HS, Leon AE, Rocke T, Keller S, Carossino M, Balasuriya U, Hofmeister E (2020) Experimental challenge of a North American bat species, big brown bat (Eptesicus fuscus), with SARS-CoV-2. Transbound Emerg Dis. 10.1111/tbed.13949 [DOI] [PubMed]
- Hamre D, Procknow JJ. A new virus isolated from the human respiratory tract. Proc Soc Exp Biol Med. 1966;121(1):190–193. doi: 10.3181/00379727-121-30734. [DOI] [PubMed] [Google Scholar]
- Harun MSR, Kuan CO, Selvarajah GT, Wei TS, Arshad SS, Bejo MH, Omar AR. Transcriptional profiling of feline infectious peritonitis virus infection in CRFK cells and in PBMCs from FIP diagnosed cats. Virol J. 2013;10(1):329. doi: 10.1186/1743-422X-10-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann H, Hattermann K, Marzi A, Gramberg T, Geier M, Krumbiegel M, Kuate S, Überla K, Niedrig M, Pöhlmann S. S protein of severe acute respiratory syndrome-associated coronavirus mediates entry into hepatoma cell lines and is targeted by neutralizing antibodies in infected patients. J Virol. 2004;78(12):6134–6142. doi: 10.1128/JVI.78.12.6134-6142.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheon JM, Kirsch JAW. A moveable face: deconstructing the Microchiroptera and a new classification of extant bats. Acta Chiropterol. 2006;8(1):1–10. doi: 10.3161/1733-5329(2006)8[1:AMFDTM]2.0.CO;2. [DOI] [Google Scholar]
- ICTV (2019) Taxonomy history: Cornidovirineae. https://talk.ictvonline.org/taxonomy/p/taxonomy-history?taxnode_id=20186105.
- Insights N (2020) Novel coronavirus complete genome from the Wuhan outbreak now available in GenBank
- Jeffers SA, Tusell SM, Gillim-Ross L, Hemmila EM, Achenbach JE, Babcock GJ, Thomas WD, Thackray LB, Young MD, Mason RJ. CD209L (L-SIGN) is a receptor for severe acute respiratory syndrome coronavirus. Proc Natl Acad Sci. 2004;101(44):15748–15753. doi: 10.1073/pnas.0403812101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji W, Wang W, Zhao X, Zai J, Li X (2020) Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol [DOI] [PMC free article] [PubMed]
- Johnson N, Vos A, Freuling C, Tordo N, Fooks AR, Müller T. Human rabies due to lyssavirus infection of bat origin. Vet Microbiol. 2010;142(3-4):151–159. doi: 10.1016/j.vetmic.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Keng C-T, Zhang A, Shen S, Lip K-M, Fielding BC, Tan THP, Chou C-F, Loh CB, Wang S, Fu J. Amino acids 1055 to 1192 in the S2 region of severe acute respiratory syndrome coronavirus S protein induce neutralizing antibodies: implications for the development of vaccines and antiviral agents. J Virol. 2005;79(6):3289–3296. doi: 10.1128/JVI.79.6.3289-3296.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E, Okada K, Kenniston T, Raj VS, AlHajri MM, Farag EA, AlHajri F, Osterhaus AD, Haagmans BL, Gambotto A. Immunogenicity of an adenoviral-based Middle East Respiratory Syndrome coronavirus vaccine in BALB/c mice. Vaccine. 2014;32(45):5975–5982. doi: 10.1016/j.vaccine.2014.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo L, Masters PS. Functional analysis of the murine coronavirus genomic RNA packaging signal. J Virol. 2013;87(9):5182–5192. doi: 10.1128/JVI.00100-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacroix A, Vidal N, Keita AK, Thaurignac G, Esteban A, de Nys H, Diallo R, Toure A, Goumou S, Soumah AK, Povogui M, Koivogui J, Monemou J-L, Raulino R, Nkuba A, Foulongne V, Delaporte E, Ayouba A, Peeters M (2020) Wide diversity of coronaviruses in frugivorous and insectivorous bat species: a pilot study in Guinea, West Africa. Viruses 12(8). 10.3390/v12080855 [DOI] [PMC free article] [PubMed]
- Lau SKP, Woo PCY, Li KSM, Huang Y, Tsoi H-W, Wong BHL, Wong SSY, Leung S-Y, Chan K-H, Yuen K-Y. Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proc Natl Acad Sci. 2005;102(39):14040–14045. doi: 10.1073/pnas.0506735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laude H, van Reeth K, Pensaert M (1993) Porcine respiratory coronavirus: molecular features and virus-host interactions [PubMed]
- Leopardi S, Holmes EC, Gastaldelli M, Tassoni L, Priori P, Scaravelli D, Zamperin G, de Benedictis P. Interplay between co-divergence and cross-species transmission in the evolutionary history of bat coronaviruses. Infect Genet Evol. 2018;58:279–289. doi: 10.1016/j.meegid.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letko M, Seifert SN, Olival KJ, Plowright RK, Munster VJ. Bat-borne virus diversity, spillover and emergence. Nat Rev Microbiol. 2020;18:461–471. doi: 10.1038/s41579-020-0394-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426(6965):450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, Wang H, Crameri G, Hu Z, Zhang H. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310(5748):676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- Li W, Sui J, Huang I-C, Kuhn JH, Radoshitzky SR, Marasco WA, Choe H, Farzan M. The S proteins of human coronavirus NL63 and severe acute respiratory syndrome coronavirus bind overlapping regions of ACE2. Virology. 2007;367(2):367–374. doi: 10.1016/j.virol.2007.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Yang Y, Ren L (2020) Genetic evolution analysis of 2019 novel coronavirus and coronavirus from other species. Infect Genet Evol:104285. 10.1016/j.meegid.2020.104285 [DOI] [PMC free article] [PubMed]
- Lim YX, Ng YL, Tam JP, Liu DX. Human coronaviruses: a review of virus–host interactions. Diseases. 2016;4(3):26. doi: 10.3390/diseases4030026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu WJ, Lan J, Liu K, Deng Y, Yao Y, Wu S, Chen H, Bao L, Zhang H, Zhao M. Protective T cell responses featured by concordant recognition of Middle East respiratory syndrome coronavirus–derived CD8+ T cell epitopes and host MHC. J Immunol. 2017;198(2):873–882. doi: 10.4049/jimmunol.1601542. [DOI] [PubMed] [Google Scholar]
- Malaiyan J, Arumugam S, Mohan K, Gomathi Radhakrishnan G (2020) An update on the origin of SARS-CoV-2: despite closest identity, bat (RaTG13) and pangolin derived coronaviruses varied in the critical binding site and O-linked glycan residues. J Med Virol. 10.1002/jmv.26261 [DOI] [PMC free article] [PubMed]
- Markotter W, Coertse J, de Vries L, Geldenhuys M, Mortlock M (2020) Bat-borne viruses in Africa: a critical review. J Zool (1987). 10.1111/jzo.12769 [DOI] [PMC free article] [PubMed]
- Matyášek R, Kovařík A. Mutation patterns of human SARS-CoV-2 and bat RaTG13 coronavirus genomes are strongly biased towards C>U transitions, indicating rapid evolution in their hosts. Genes (Basel) 2020;11(7):761. doi: 10.3390/genes11070761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh K, Becker WB, Chanock RM. Growth in suckling-mouse brain of “IBV-like” viruses from patients with upper respiratory tract disease. Proc Natl Acad Sci U S A. 1967;58(6):2268–2273. doi: 10.1073/pnas.58.6.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihindukulasuriya KA, Wu G, Leger JS, Nordhausen RW, Wang D. Identification of a novel coronavirus from a beluga whale by using a panviral microarray. J Virol. 2008;82(10):5084–5088. doi: 10.1128/JVI.02722-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millet JK, Whittaker GR. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc Natl Acad Sci. 2014;111(42):15214–15219. doi: 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra V. Bats and viruses. Lancet Infect Dis. 2020;20(12):1380. doi: 10.1016/S1473-3099(20)30743-X. [DOI] [Google Scholar]
- Modjarrad K. MERS-CoV vaccine candidates in development: the current landscape. Vaccine. 2016;34(26):2982–2987. doi: 10.1016/j.vaccine.2016.03.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora-Díaz JC, Piñeyro PE, Houston E, Zimmerman J, Giménez-Lirola LG (2019) Porcine Hemagglutinating encephalomyelitis virus: a review. Front Vet Sci 6 [DOI] [PMC free article] [PubMed]
- Murakami S, Kitamura T, Suzuki J, Sato R, Aoi T, Fujii M, Matsugo H, Kamiki H, Ishida H, Takenaka-Uema A, Shimojima M, Horimoto T. Detection and characterization of bat sarbecovirus phylogenetically related to SARS-CoV-2, Japan. Emerg Infect Dis. 2020;26(12):3025–3029. doi: 10.3201/eid2612.203386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netland J, DeDiego ML, Zhao J, Fett C, Álvarez E, Nieto-Torres JL, Enjuanes L, Perlman S. Immunization with an attenuated severe acute respiratory syndrome coronavirus deleted in E protein protects against lethal respiratory disease. Virology. 2010;399(1):120–128. doi: 10.1016/j.virol.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea TJ, Cryan PM, Cunningham AA, Fooks AR, Hayman DTS, Luis AD, Peel AJ, Plowright RK, Wood JLN. Bat flight and zoonotic viruses. Emerg Infect Dis. 2014;20(5):741–745. doi: 10.3201/eid2005.130539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olival KJ, Hosseini PR, Zambrana-Torrelio C, Ross N, Bogich TL, Daszak P. Host and viral traits predict zoonotic spillover from mammals. Nature. 2017;546(7660):646–650. doi: 10.1038/nature22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris JSM, Guan Y, Yuen KY. Severe acute respiratory syndrome. Nat Med. 2004;10(12):S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. 2009;7(6):439–450. doi: 10.1038/nrmicro2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Z, Dominguez SR, Holmes KV. Role of the spike glycoprotein of human Middle East respiratory syndrome coronavirus (MERS-CoV) in virus entry and syncytia formation. PLoS One. 2013;8(10):e76469. doi: 10.1371/journal.pone.0076469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman MS, Hoque MN, Islam MR, Islam I, Mishu ID, Rahaman MM, Sultana M, Hossain MA (2021) Mutational insights into the envelope protein of SARS-CoV-2. Gene Rep:100997. 10.1016/j.genrep.2020.100997 [DOI] [PMC free article] [PubMed]
- Roes FL. On the evolution of virulent zoonotic viruses in bats. Biol Theory. 2020;15(4):223–225. doi: 10.1007/s13752-020-00363-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sainz B, Rausch JM, Gallaher WR, Garry RF, Wimley WC. Identification and characterization of the putative fusion peptide of the severe acute respiratory syndrome-associated coronavirus spike protein. J Virol. 2005;79(11):7195–7206. doi: 10.1128/JVI.79.11.7195-7206.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel CE. Antiviral actions of interferons. Clin Microbiol Rev. 2001;14(4):778–809. doi: 10.1128/CMR.14.4.778-809.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlottau K, Rissmann M, Graaf A, Schön J, Sehl J, Wylezich C, Höper D, Mettenleiter TC, Balkema-Buschmann A, Harder T, Grund C, Hoffmann D, Breithaupt A, Beer M. SARS-CoV-2 in fruit bats, ferrets, pigs, and chickens: an experimental transmission study. Lancet Microbe. 2020;1(5):e218–e225. doi: 10.1016/S2666-5247(20)30089-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz LL, Tyler JK. The histone chaperone ASF1 localizes to active DNA replication forks to mediate efficient DNA replication. FASEB J. 2006;20(3):488–490. doi: 10.1096/fj.05-5020fje. [DOI] [PubMed] [Google Scholar]
- Skirmuntt EC, Escalera-Zamudio M, Teeling EC, Smith A, Katzourakis A. The potential role of endogenous viral elements in the evolution of bats as reservoirs for zoonotic viruses. Ann Rev Virol. 2020;7:103–119. doi: 10.1146/annurev-virology-092818-015613. [DOI] [PubMed] [Google Scholar]
- Smith I, Wang L-F. Bats and their virome: an important source of emerging viruses capable of infecting humans. Curr Opin Virol. 2013;3(1):84–91. doi: 10.1016/j.coviro.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofi MS, Hamid A, Bhat SU. SARS-CoV-2: a critical review of its history, pathogenesis, transmission, diagnosis and treatment. Biosaf Health. 2020;2(4):217–225. doi: 10.1016/j.bsheal.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart T, Jung FF, Manning J, Vehaskari VM. Kidney immune cell infiltration and oxidative stress contribute to prenatally programmed hypertension. Kidney Int. 2005;68(5):2180–2188. doi: 10.1111/j.1523-1755.2005.00674.x. [DOI] [PubMed] [Google Scholar]
- Stockman LJ, Bellamy R, Garner P. SARS: systematic review of treatment effects. PLoS Med. 2006;3(9):e343. doi: 10.1371/journal.pmed.0030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, Liu W, Bi Y, Gao GF. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24(6):490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai W, Wang Y, Fett CA, Zhao G, Li F, Perlman S, Jiang S, Zhou Y, Du L. Recombinant receptor-binding domains of multiple Middle East respiratory syndrome coronaviruses (MERS-CoVs) induce cross-neutralizing antibodies against divergent human and camel MERS-CoVs and antibody escape mutants. J Virol. 2017;91(1):e01651–e01616. doi: 10.1128/JVI.01651-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeling EC, Springer MS, Madsen O, Bates P, O’brien SJ, Murphy WJ. A molecular phylogeny for bats illuminates biogeography and the fossil record. Science. 2005;307(5709):580–584. doi: 10.1126/science.1105113. [DOI] [PubMed] [Google Scholar]
- Tsagkogeorga G, Parker J, Stupka E, Cotton JA, Rossiter SJ. Phylogenomic analyses elucidate the evolutionary relationships of bats. Curr Biol. 2013;23(22):2262–2267. doi: 10.1016/j.cub.2013.09.014. [DOI] [PubMed] [Google Scholar]
- van Boheemen S, de Graaf M, Lauber C, Bestebroer TM, Raj VS, Zaki AM, Osterhaus AD, Haagmans BL, Gorbalenya AE, Snijder EJ. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. MBio. 2012;3(6):e00473–e00412. doi: 10.1128/mBio.00473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Hoek L. Human coronaviruses: what do they cause? Antivir Ther. 2007;12(4 Pt B):651. doi: 10.1177/135965350701200S01.1. [DOI] [PubMed] [Google Scholar]
- van der Hoek L, Sure K, Ihorst G, Stang A, Pyrc K, Jebbink MF, Petersen G, Forster J, Berkhout B, Überla K (2005) Croup is associated with the novel coronavirus NL63. PLoS Med 2(8) [DOI] [PMC free article] [PubMed]
- van Doremalen N, Miazgowicz KL, Milne-Price S, Bushmaker T, Robertson S, Scott D, Kinne J, McLellan JS, Zhu J, Munster VJ. Host species restriction of Middle East respiratory syndrome coronavirus through its receptor, dipeptidyl peptidase 4. J Virol. 2014;88(16):9220–9232. doi: 10.1128/JVI.00676-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vennema H, de Groot RJ, Harbour DA, Dalderup M, Gruffydd-Jones T, Horzinek MC, Spaan WJ. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J Virol. 1990;64(3):1407–1409. doi: 10.1128/jvi.64.3.1407-1409.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers NJ. Animal communication: when I’m calling you, will you answer too? Curr Biol. 2017;27(14):R713–R715. doi: 10.1016/j.cub.2017.05.064. [DOI] [PubMed] [Google Scholar]
- Vijgen L, Keyaerts E, Lemey P, Moës E, Li S, Vandamme A-M, van Ranst M. Circulation of genetically distinct contemporary human coronavirus OC43 strains. Virology. 2005;337(1):85–92. doi: 10.1016/j.virol.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L. Animal coronaviruses. 1. NY: Springer Protocolas; 2016. [Google Scholar]
- Wang L-F, Cowled C (2015) Bats and viruses: a new frontier of emerging infectious diseases. Wiley
- Wang L-F, Walker PJ, Poon LLM. Mass extinctions, biodiversity and mitochondrial function: are bats ‘special’as reservoirs for emerging viruses? Curr Opin Virol. 2011;1(6):649–657. doi: 10.1016/j.coviro.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Shi W, Joyce MG, Modjarrad K, Zhang Y, Leung K, Lees CR, Zhou T, Yassine HM, Kanekiyo M. Evaluation of candidate vaccine approaches for MERS-CoV. Nat Commun. 2015;6(1):1–11. doi: 10.1038/ncomms8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2020) Diagnostic detection of Wuhan coronavirus 2019 by real-time RTPCR
- Widagdo W, Raj VS, Schipper D, Kolijn K, van Leenders GJ, Bosch BJ, Bensaid A, Segalés J, Baumgärtner W, Osterhaus AD. Differential expression of the Middle East respiratory syndrome coronavirus receptor in the upper respiratory tracts of humans and dromedary camels. J Virol. 2016;90(9):4838–4842. doi: 10.1128/JVI.02994-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong ACP, Li X, Lau SKP, Woo PCY. Global epidemiology of bat coronaviruses. Viruses. 2019;11(2):174. doi: 10.3390/v11020174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo PCY, Lau SKP, C-m C, Chan K-H, Tsoi H-W, Huang Y, Wong BHL, Poon RWS, Cai JJ, W-k L. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol. 2005;79(2):884–895. doi: 10.1128/JVI.79.2.884-895.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo PCY, Lau SKP, Lam CSF, Lau CCY, Tsang AKL, Lau JHN, Bai R, Teng JLL, Tsang CCC, Wang M. Discovery of seven novel Mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J Virol. 2012;86(7):3995–4008. doi: 10.1128/JVI.06540-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K, Li W, Peng G, Li F. Crystal structure of NL63 respiratory coronavirus receptor-binding domain complexed with its human receptor. Proc Natl Acad Sci. 2009;106(47):19970–19974. doi: 10.1073/pnas.0908837106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Liu Y, Lou Z, Qin L, Li X, Bai Z, Pang H, Tien P, Gao GF, Rao Z. Structural basis for coronavirus-mediated membrane fusion crystal structure of mouse hepatitis virus spike protein fusion core. J Biol Chem. 2004;279(29):30514–30522. doi: 10.1074/jbc.M403760200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Lou Z, Liu Y, Pang H, Tien P, Gao GF, Rao Z. Crystal structure of severe acute respiratory syndrome coronavirus spike protein fusion core. J Biol Chem. 2004;279(47):49414–49419. doi: 10.1074/jbc.M408782200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H, Jiao H, Liu Q, Zhang Z, Wang X, Guo M, Wang B-J, Lan K, Chen Y, Zhao H (2020) Many bat species are not potential hosts of SARS-CoV and SARS-CoV-2: evidence from ACE2 receptor usage. 10.1101/2020.09.08.284737
- Yang Y, Liu C, Du L, Jiang S, Shi Z, Baric RS, Li F. Two mutations were critical for bat-to-human transmission of Middle East respiratory syndrome coronavirus. J Virol. 2015;89(17):9119–9123. doi: 10.1128/JVI.01279-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager CL, Ashmun RA, Williams RK, Cardellichio CB, Shapiro LH, Look AT, Holmes KV. Human aminopeptidase N is a receptor for human coronavirus 229E. Nature. 1992;357(6377):420–422. doi: 10.1038/357420a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung M-L, Yao Y, Jia L, Chan JFW, Chan K-H, Cheung K-F, Chen H, Poon VKM, Tsang AKL, To KKW. MERS coronavirus induces apoptosis in kidney and lung by upregulating Smad7 and FGF2. Nat Microbiol. 2016;1(3):1–8. doi: 10.1038/nmicrobiol.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B, Roberts RS, Lindesmith L, Baric RS. Rewiring the severe acute respiratory syndrome coronavirus (SARS-CoV) transcription circuit: engineering a recombination-resistant genome. Proc Natl Acad Sci. 2006;103(33):12546–12551. doi: 10.1073/pnas.0605438103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Am Fouchier R. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- Zhou T, Wang H, Luo D, Rowe T, Wang Z, Hogan RJ, Qiu S, Bunzel RJ, Huang G, Mishra V. An exposed domain in the severe acute respiratory syndrome coronavirus spike protein induces neutralizing antibodies. J Virol. 2004;78(13):7217–7226. doi: 10.1128/JVI.78.13.7217-7226.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P, Fan H, Lan T, Yang X-L, Shi W-F, Zhang W, Zhu Y, Zhang Y-W, Xie Q-M, Mani S. Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin. Nature. 2018;556(7700):255–258. doi: 10.1038/s41586-018-0010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Li C, Liu X, Chiu MC, Zhao X, Wang D, Wei Y, Lee A, Zhang AJ, Chu H, Cai J-P, Yip CC-Y, Chan IH-Y, Wong KK-Y, Tsang OT-Y, Chan K-H, Chan JF-W, To KK-W, Chen H, Yuen KY. Infection of bat and human intestinal organoids by SARS-CoV-2. Nat Med. 2020;26(7):1077–1083. doi: 10.1038/s41591-020-0912-6. [DOI] [PubMed] [Google Scholar]
- Zhu Z, Meng K, Meng G. Genomic recombination events may reveal the evolution of coronavirus and the origin of SARS-CoV-2. Sci Rep. 2020;10(1):1–10. doi: 10.1038/s41598-020-78703-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Züst R, Cervantes-Barragán L, Kuri T, Blakqori G, Weber F, Ludewig B, Thiel V. Coronavirus non-structural protein 1 is a major pathogenicity factor: implications for the rational design of coronavirus vaccines. PLoS Pathog. 2007;3(8):e109. doi: 10.1371/journal.ppat.0030109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.