Summary
Several pathological conditions, other than gastro-esophageal reflux disease and its complications, can affect the esophagus. While some of these can present with unspecific lesions (i.e. ulcers and epithelial damage) and require clinico-pathological correlation for diagnosis (i.e. drug-induced esophagitis and corrosive esophagitis) other conditions show distinctive histological lesions which enable the pathologist to reach the diagnosis (i.e. some specific infectious esophagites and Crohn’s disease). In this context eosinophilic esophagitis is the condition which has been increasingly studied in the last two decades, while lymphocytic esophagitis, a relatively new entity, still represents an enigma. This overview will focus on and describe histologic lesions which allow pathologists to differentiate between these conditions.
Key words: drug-induced esophagitis, esophagitis dissecans superficialis, esophageal Crohn’s disease, lymphocytic esophagitis, eosinophilic esophagitis
Introduction
Gastro-esophageal reflux disease (GERD) and its complications, such as Barrett’s esophagus (BE), are a major concern when facing esophageal biopsies. However, other than GERD and BE, many other pathological conditions can affect the esophagus, either as the unique and typical localization of an illness or as an expression of diseases which can affect any part of the gastro-intestinal tract (i.e. Crohn disease) or also as complications in patients with immunodeficiency (i.e. infectious esophagitis). Some of these conditions, such as eosinophilic esophagitis (EE), have received much attention in the last decades in order to better define both clinico-pathological aspects and possible therapeutic approaches. Other conditions have been only recently described (ie lymphocytic esophagitis) and still represent an enigma or, as stated by Ronkainen “a condition in search for a disease”. Finally, there are numerous drugs and exogenous substances which can affect the esophagus: in this setting the importance of a close relationship with the gastroenterologist in order to obtain relevant clinical information and the knowledge of rare entities which can enter in the differential diagnosis are fundamental.
This overview on non-neoplastic esophageal disease has the main aim of furnishing a practical diagnostic approach to biopsy samples in the principal illnesses affecting the esophagus tract, referring to the most recent published recommendations, guidelines and expert opinions.
Infectious esophagitis
DEFINITION
Infectious esophagites are a group of diseases in which inflammation and damage of the esophagus is attributable to various infectious agents.
CLINICAL PICTURE
The clinical presentation is extremely variable ranging from no symptoms to severe dysphagia, retrosternal chest pain and fever.
Infectious esophagites occur more often in immunocompromised patients, and in particular in Human Immunodeficiency Virus (HIV) infection, in post-transplant immunosuppression and in long-term oral corticosteroid use. In immunocompetent subjects, infectious esophagites are rare and favored by conditions that cause a relative weakening of the immune system (i.e. diabetes mellitus, cirrhosis, etc.) or functional (dysmotility) and structural (strictures) disorders 1.
ENDOSCOPY PICTURE
The endoscopic appearances vary depending on the infectious agent. In Candida esophagitis, which more often affects HIV patients, white mucosal plaque-like lesions and exudates tenaciously adherent to the mucosa and not removable with water from irrigation, are observed along the esophageal surface 2; subsequent disease manifestations may include friability and ulceration. Diversely, Herpes Simplex Virus (HSV) and Cytomegalovirus (CMV) infections are more frequent in post-transplant patients; endoscopic manifestations vary from vesicles to unspecific erosions to large, well circumscribed, volcano-like ulcerations with exudates 3,4 for HSV while CMV presents with erosions and ulcers in the middle and distal portion of the esophagus.
Mycobacterium tuberculosis rarely affects the esophagus, even in endemic areas. Human Papillomavirus has been occasionally documented as cause of acute esophagitis, while it can play a role in esophageal squamous papilloma and esophageal squamous carcinoma.
BIOPSY SITE
Histology is considered the gold standard for identifying specific infectious agents. Biopsies must be taken on the more pronounced lesions. For HSV infections, biopsies obtained at the ulcer edges are more informative as they permit the recognition of pathologic lesions seen in epithelial cells, while in CMV infection, biopsies from the ulcer center, where endothelial and stromal cells are easily identified, are more reliable.
HISTOLOGIC ELEMENTARY LESIONS
The inflammatory background is non-specific and composed of a mixed inflammatory infiltrate with erosion, ulcer and necrotic debris. Typical lesions include recognition of hyphae and spores for Candida, multinucleated giant cells and glassy eosinophilic intranuclear inclusions for HSV 5 and nucleomegaly with ‘owl’s eye’ intranuclear inclusions for CMV (Fig. 1). Histochemical stains for hyphae/spores (PAS, Grocott), mycobacteria (Ziehl Neelsen) and immunohistochemistry (CMV or HSV) help in confirming diagnosis.
Figure 1.
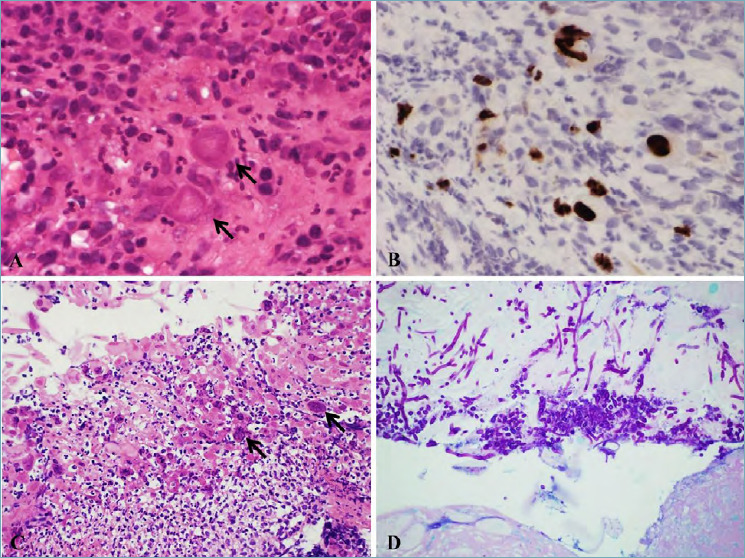
(A) Cytomegalovirus esophagitis (magnification 40x). Nucleomegaly with intranuclear inclusions (black arrow). (B) Cytomegalovirus esophagitis (magnification 40x). Immunohistochemistry with anti-CMV antibody, showing sparse positive nuclei. (C) Herpes Simplex Virus esophagitis (magnification 10x). Multinucleated giant cells and ground glass intranuclear inclusions (black arrow) with necrotic debris and inflammation. (D) Candida Albicans esophagitis (magnification 20x). Alcian Blu PAS staining showing hyphae and spores on the surface of squamous epithelium.
DIAGNOSIS
When typical lesions are histologically recognized, and eventually confirmed by histochemistry and/or immunohistochemistry, a diagnosis of specific infectious esophagitis can be made. In other cases, a clinical integration with microbiologic/sierologic studies is recommended.
Drug-induced esophagitis
DEFINITION
Drug-induced esophagitis can present either as pill-induced esophagitis or radiation and chemotherapy esophagitis.
The term pill-induced esophagitis refers to esophageal injury caused by almost 100 different types of substances ingested in form of pills. Antibiotics are one of the major contributors, especially tetracycline and doxycycline; other major contributors are biphosphonates, non-steroidal anti-inflammatory drugs and iron pills 6. Injuries occur when caustic medicinal pills dissolve in the esophagus rather than passing rapidly into the stomach 7; usually this occurs for larger pills and/or in correspondence of lumen reduction or strictures which make swallowing more difficult 8.
Radiation esophagitis affects less than 1% of patients receiving radiation treatment for advanced stages of common cancers such as lung, breast and esophageal carcinomas 9.
Several chemotherapeutic agents (bleomycin, 5-fluorouracil, methotrexate, vincristine) may cause esophageal and oropharyngeal mucositis 10.
CLINICAL PICTURE
Common symptoms for pill-induced esophagitis are odynophagia, chest pain, vomiting, dysphagia and, less frequently, hematemesis 11. Perforation and fatal injuries have also been reported.
Radiation esophagitis generally presents with nonspecific symptoms, such as dysphagia and odynophagia, occurring within the first 2 months of treatment.
Chemotherapy can directly damage the esophageal mucosa and manifests with unspecific symptoms, or incrementing radio-sensitizing action (as in the case of doxorubicin and bleomicin) 10.
The referral information concerning pill ingestion and type of treatment is fundamental for a correct diagnosis of drug induced esophagitis.
ENDOSCOPY PICTURE
The endoscopic description of pill-induced esophagitis can vary from erythema, which is the most frequent endoscopic alteration, to erosions and ulcers which are present, on the whole, in about 50-60% of patients.
Radiation and chemotherapy esophagitis show nonspecific and non-diagnostic endoscopic changes such as erythema and ulceration.
BIOPSY SITE
Biopsies are taken in the endoscopically affected areas.
HISTOLOGIC ELEMENTARY LESIONS
Biopsies show variable inflammatory changes with erosion, ulcer, acute inflammation and granulation tissue. In radiation esophagitis, early damage is represented by ballooning degeneration and edema with inflammation and vessels hyalinization (Fig. 2A). Radiation-related atypia of endothelial and stromal cells can guide diagnosis. This aspect can mimic cytomegalovirus cytopathic changes which need to be ruled out through negative CMV specific immunostaining.
Figure 2.
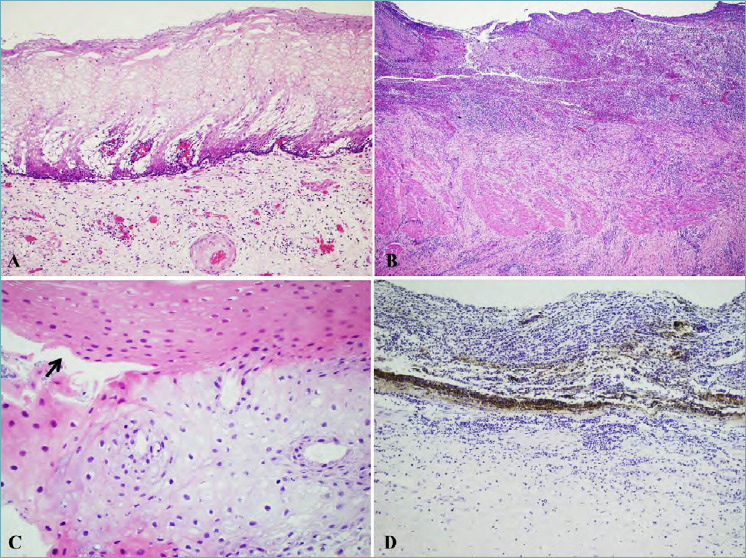
(A) Radiation esophagitis (magnification 10x). Ballooning degeneration of squamous epithelium with edema; a vessel with hyalinized wall is present in the submucosal layer. (B) Corrosive esophagitis (magnification 10x) in a patient with accidental ingestion of sodium hydroxide (lye or caustic soda) showing necrosis and inflammation with diffuse ulceration of the mucosa and submucosa. (C) Esophagitis dissecans superficialis (magnification 40x). An intraepithelial cleft (black arrow) is visible with two strips of squamous epithelium showing a different color tone. (D) Black esophagus (magnification 10x). Autopsy finding, revealing necrosis of the esophagus with abundant neutrophils and abundant brown pigmented granules.
DIAGNOSIS
When a certain correlation with pill ingestion or chemo-radiation treatment is clinically referred, the diagnosis of drug-induced esophagitis can be suggested even though histological lesions are unspecific.
Corrosive esophagitis
DEFINITION
Corrosive esophagitis is the consequence of voluntary (suicide, attempted suicide or parasuicide) or accidental ingestion of strong alkaline or, less frequently, acidic substances (liquid or solid mainly in form of crystals). Daily consumption of vinegar drinks with pH value lower than 5.5 has also been reported to cause corrosive damage in the esophagus 12.
CLINICAL PICTURE
Clinical presentation depends on type of substance, its amount and physical form. Liquid substances affect the esophagus and stomach more easily, while crystals (more difficult to swallow) provoke greater damage in the oral cavity, oropharynx and upper airways. Patients with esophageal damage complain of stridor, drooling, dysphagia and odynophagia. In about 70% of patients there is contemporary gastric involvement manifesting with epigastric pain and bleeding. Perforation can occur within 2 weeks from ingestion 13.
ENDOSCOPY PICTURE
Endoscopy can be safely performed up to the 4th day after corrosive liquid ingestion with minimal air insufflation; risk of perforation after this time set, significantly increases. Severity of mucosal lesions on endoscopy can be graded from 1 to 4 14,15 varying from mucosal edema and erythema (grade 1) to superficial (2A) or deep (2B) mucosal and submucosal ulcerations, transmural ulcerations with focal (3A) or extensive (3B) necrosis and perforation (4). High grade (2B-4) damage may lead to the development of chronic complications, such as esophageal strictures and extensive fibrosis, more frequently than low grade injuries (1-2A) 16.
BIOPSY SITE
Biopsies are not indicated in the acute setting. Pathologists can face acute damage in surgical specimens (Fig. 2B) or autopsy. In chronic complications biopsies are performed in the affected area without a specific protocol.
HISTOLOGIC ELEMENTARY LESIONS
Acute damage
Acidic liquids cause acute coagulative necrosis, while alkaline substances provoke liquefactive necrosis. Other than necrosis, in the acute phase, small vessel thrombosis, mucosal sloughing and bacterial overgrowth are present.
Chronic damage
Esophageal mucosa repair starts after 10 days with subsequent re-epithelialization of ulcers. Esophageal biopsies show variable degree of esophagitis with basal cell hyperplasia, papillae elongation, dilatation of intercellular space and intraepithelial inflammatory infiltrates with erosion/ulcers; hyper-parakeratosis are frequent. Repair of lesions include scar tissue formation with marked fibrosis and consequent strictures; in the lower esophagus this leads to sphincter impairment with gastro-esophageal reflux worsening histologic damage 13.
DIAGNOSIS
Clinical correlation with type of ingested substances and timing is necessary to express diagnosis with certainty.
Esophagitis dissecans superficialis (sloughing esophagitis)
DEFINITION
Esophagitis dissecans superficialis (EDS) is a benign, self-limited, desquamative disorder of the esophagus, characterized by sloughing of the superficial mucosa.
CLINICAL PICTURE
EDS affects older women more frequently, often with chronic illness and in poly-medication therapy, including benzodiazepines, selective serotonin re-uptake inhibitors, opiates and antiepiletics 17.
More than half of patients are asymptomatic and EDS is discovered during upper GI endoscopy for other reasons. When symptomatic, dysphagia, abdominal pain or heartburn can be part of the symptomatic spectrum 18.
ENDOSCOPY PICTURE
Endoscopically, esophageal mucosa appears sloughed in streaks and patches. These features are more pronounced in the distal two thirds of the esophagus 19.
BIOPSY SITE
Biopsies are taken in the endoscopically affected areas.
HISTOLOGIC ELEMENTARY LESIONS
The main histologic feature is the presence of an intraepithelial cleft which separate the squamous epithelium in two strips with a different color tone: the superficial sloughed layers are intensely eosinophilic, while the layers under the cleft are almost normal (Fig. 2C). Inflammation can be present, with neutrophilic and eosinophilic infiltrates, but is not a constant feature; necrotic debris mixed with bacteria and fungi can be seen within the superficial sloughed epithelium 20.
DIAGNOSIS
EDS histologic diagnosis can be suggested when there is a clear color-tone change between layers over and under the cleft; epithelium detachments, as a consequence of withdrawal traumatism during biopsy procedures, have to be excluded.
Black esophagus (acute esophageal necrosis or Gurvits syndrome)
DEFINITION
Black esophagus is an uncommon entity characterized by a diffuse, circumferential black color of the esophageal mucosa.
CLINICAL PICTURE
Typical patients are older men with multiple comorbidities (including vascular disease, diabetes mellitus, hypertension, chronic liver, kidney and pulmonary diseases, malnutrition, malignancy, or alcohol abuse) presenting with hematemesis or melena. A combination of esophageal ischemia, corrosive damage caused by gastro-esophageal reflux of acid and pepsin and impaired mucosal reparative mechanisms contribute to the mucosal damage 21,22. Recurrence or death are frequent and affect over a quarter of cases 23.
ENDOSCOPY PICTURE
On endoscopy, esophageal mucosa appears diffusely black colored, sometimes with small whitish areas, and circumferential extension involving the lower third of the esophagus with an abrupt transition at the gastroesophageal junction and variable proximal extension 22,24.
BIOPSY SITE
The endoscopic picture is diagnostic and biopsies are usually not required to confirm the diagnosis 22. Pathologists more often make the diagnosis of black esophagus on autopsy cases or on surgical specimens when no response to medical treatment is seen.
HISTOLOGICAL ELEMENTARY LESIONS
Histology reveals complete mucosal necrosis with abundant neutrophils above the muscularis mucosae which remains viable. Vessels with intravascular thrombi and golden brown pigmented granules (Fig. 2D) negative for Prussian blue and referable to lipofuscin complete the picture 25.
DIAGNOSIS
The endoscopic aspect drives the diagnosis which is eventually confirmed by the presence of the histologic mucosal damage.
Esophageal Crohn’s disease
DEFINITION
Crohn’s disease (CD) can localize in the entire gastro-intestinal tract; in the vast majority of patients with esophageal involvement, CD is already diagnosed in its more common ileal and colonic localizations with only exceptional cases being diagnosed in the esophagus as the unique primary involved site 26.
CLINICAL PICTURE
The incidence of esophageal CD is less than 2% in adults, while it can reach up to 25-40% in children. Esophageal symptoms are often mild, non-specific and generally overcome by typical intestinal symptoms. Moreover, in just under 50% of patients, gastro-esophageal CD can be completely asymptomatic 27. Upper gastrointestinal CD involvement plays an important role because it predicts a more severe disease with a greater frequency of complications such as obstruction and perforation 28.
ENDOSCOPY PICTURE
Esophageal CD most commonly involves the mid and distal portions of the esophagus while the proximal esophagus is rarely affected. Endoscopic alterations range from erythema and erosions to superficial and deep ulcers in the majority of cases. Pseudopolyps, fistulas and strictures may be rarely associated 26.
BIOPSY SITE
Upper gastro-esophageal endoscopy is not routinely performed in patients with CD and a biopsy protocol is not suggested; biopsies are, as a rule, taken in affected areas.
HISTOLOGIC ELEMENTARY LESIONS
Histologic lesions are more commonly unspecific with chronic inflammation, erosions, ulcers and necrotic debris. Non-caseating granulomas, epithelioid and/or giant cells, in lamina propria are identified only in a minority of patients (Fig. 3A), making this diagnosis challenging in the absence of intestinal manifestations of CD.
Figure 3.
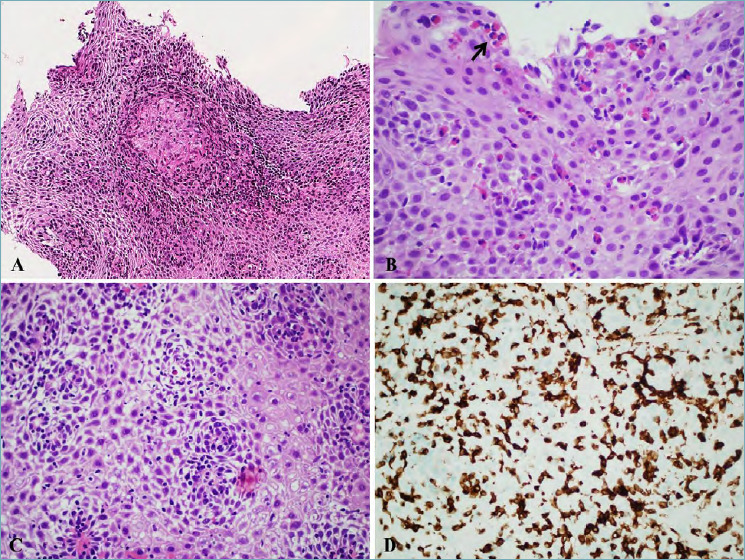
(A) Esophageal Crohn’s disease (magnification 20x). Presence of an epithelioid granuloma within squamous epithelium, diagnostic for esophageal localization of Crohn’s disease in a patient with previous diagnosis in the distal ileum; (B) Eosinophilic esophagitis (magnification 40x). A high number of intraepithelial eosinophils is present, also forming microabscesses (black arrow) in the superficial layer. (C) Lymphocytic esophagitis (magnification 40x). Marked spongiosis is present with an increase in intraepithelial lymphocytes in the peri-papillary areas. (D) Lymphocytic esophagitis (magnification 40x). Immunostains for CD3 showing a marked increase in intraepithelial T lymphocytes.
Lymphocytic esophagitis (LE; see later) has been associated in a quarter of cases with CD in pediatric patients 29. This association was not confirmed with the same incidence by other authors nor in adulthood, however, even though it may be rarer, there are enough reports to confirm that an association between CD and LE does exist.
DIAGNOSIS
In patients with previously diagnosed CD, unspecific inflammatory changes and ulcers can suggest esophageal involvement, while non-caseating granulomas are diagnostic.
For first suspicions of diagnosis of CD, it is essential to exclude infectious etiology.
Lymphocytic esophagitis
DEFINITION
Lymphocytic esophagitis (LE) was initially described by Rubio as a novel histologic phenotype of chronic esophagitis characterized by a high number of intraepithelial lymphocytes surrounding papillae, associated with marked spongiosis 30; the same pattern was also described in other primates 31,32.
CLINICAL PICTURE
LE seems to be a rare condition, diagnosed in about 1 every 1000 esophageal endoscopies. Different studies have reported a different age and sex related prevalence, varying from younger male to older female patients.
It is emerging that LE is a histologic pattern common to different clinical diseases: 1) in children and younger patients, LE is frequently associated with CD 33; 2) in older women, presenting with dysphagia, LE can be an expression of motility disorders 34 - adult patients with LE, stratified immunophenotypically, showed a high prevalence of non-achalasia primary esophageal motility disorders with a predominant CD4+ T cell infiltrate 35; 3) some reports finally suggest that in adults, LE with a predominant CD8+ T cell infiltrate, can be expression of gastroesophageal reflux disease in absence of motility disorders 36.
Patients can be completely asymptomatic or present with unspecific upper gastro-intestinal symptoms, ranging from dysphagia to reflux/heartburn, abdominal and chest pain, or nausea and vomiting 37.
ENDOSCOPIC PICTURE
Endoscopy is negative in about a third of patients; in about another third of patients, LE can endoscopically resemble eosinophilic esophagitis with multiple concentric rings giving an aspect of ‘feline esophagus’. Other possible observations are strictures, erythema, furrows and webs 38.
BIOPSY SITE
The mid esophagus is involved more frequently and with more pronounced endoscopic lesions than the proximal or distal part; if LE is clinically or endoscopically suspected, biopsies from all the esophagus segments are suggested.
HISTOLOGIC ELEMENTARY LESIONS
The main histologic feature is the notable increase in intraepithelial lymphocytes in the peri-papillary areas, associated with marked spongiosis (Fig. 3 C-D). Different studies have tried to better define this lymphocytic increase using cut-off values ranging from 10 to 50 per HPF with 20 lymphocytes/HPF being the commonly used cut off. This results in a marked increase of LE diagnoses and therefore, the use of a cut off value (in particular, with a such a low count as 20/HPF, which is present in some healthy volunteers and in reflux disease) is not recommended. The main criteria continues to be of a high number of peri-papillary lymphocytes with marked spongiosis in the absence of both neutrophils and eosinophils 39. Candida Albicans can superimpose on LE, so attention must be paid to lymphocytes even in other conditions.
DIAGNOSIS
Given the variability of clinical conditions associated with this histological aspect 40, a diagnosis of compatibility with LE is suggested in the presence of histologic hallmarks: clinicians should investigate which conditions (among CD, motility disorders, GERD and maybe others) are responsible for the histologic lesions.
Eosinophilic esophagitis
DEFINITION
Eosinophilic esophagitis (EoE) is a chronic allergen driven immune mediated clinico-pathological disorder diagnosed by clinicians taking into consideration both clinical and pathologic information. EoE is defined by the following criteria: symptoms related to esophageal dysfunction; ≥ 15 eosinophils per HPF; eosinophilia limited to the esophagus excluding other causes of esophageal eosinophilia 41.
CLINICAL PICTURE
EoE shows a white male predominance (both in children and adults) with a 6.5% prevalence in all patients undergoing upper endoscopy 42.
In pediatric patients, symptoms are heterogeneous and include abdominal pain, nausea, reflux-like symptoms and feeding difficulties with consequent growth failure.
In adults, EoE predominately presents with dysphagia for solid food associated with food impaction.
Currently, two different forms of EoE are recognized on the basis of response to treatment: proton pump inhibitor (PPI)-responsive EoE and steroid-responsive EoE. PPI-responsive EoE substantially differs from GERD as it shows mast cell signature genes and the expression of genes involved in type 2 (Th2)-associated allergic inflammation, and is similar to steroid-responsive EoE. The introduction of PPI-responsive EoE in the spectrum of EoE has changed the diagnostic algorithm of this condition 43,44.
ENDOSCOPY PICTURE
The clinical diagnosis of EoE does not require the presence of endoscopic features; however, prospective studies have identified endoscopic lesions in as much as 93% of patients 45. Endoscopically detectable features vary from multiple concentric rings with ‘feline esophagus’ which is the most evocative lesion, to strictures and narrowing of lumen. Longitudinal furrows and white exudates complete the spectrum of possible lesions that affect both the distal and proximal esophagus. Rings and strictures are the outcome of multiple inflammatory insults with esophageal remodeling, thus they can be completely absent in children 43.
BIOPSY SITE
The recommended biopsy protocol includes at least six biopsies taken from the distal, middle and proximal esophagus, focusing on areas with endoscopic mucosal abnormalities 46.
HISTOLOGIC ELEMENTARY LESIONS
The main histological feature is the presence of a high number of intraepithelial eosinophils, characteristically forming microabscesses in the superficial layer (Fig. 3B). At a formal count, a number of ≥ 15 eosinophils per HPF (standard size of 0.3 mm2) in hot spots is required 46.
In addition to eosinophils, basal cell hyperplasia, papillae elongation and dilatation of intercellular spaces complete the histologic picture.
DIAGNOSIS
The diagnosis, as already mentioned, is performed by clinicians taking into account clinical and pathological information. For this reason, finding ≥ 15 eosinophils per HPF should lead to a report of ‘compatible with EoE’ rather than ‘diagnostic for EoE’.
Conclusions
In conclusion, as seen in this brief overview, many non-neoplastic diseases can affect the esophagus. Endoscopic biopsies of the esophagus are often required to establish the correct diagnosis within an appropriate clinical context. Indeed, information on endoscopic and clinical findings are a fundamental basis for the interpretation of histology, which may be similar in diverse settings, thus leading to a correct histopathologic diagnosis.
Figures and tables
References
- 1.Ahuja NK, Clarke JO. Evaluation and management of infectious esophagitis in immunocompromised and immunocompetent individuals. Curr Treat Options Gastro 2016;14:28-38. https://doi.org/10.1007/s11938-016-0082-2 10.1007/s11938-016-0082-2 [DOI] [PubMed] [Google Scholar]
- 2.Mohamed AA, Lu XL, Mounmin FA. Diagnosis and treatment of esophageal candidiasis: current updates. Can J Gastroenterol Hepatol. 2019:3585136. https://doi.org/10.1155/2019/3585136 10.1155/2019/3585136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Itoh T, Takahashi T, Kusaka K, et al. Herpes simplex esophagitis from 1307 autopsy cases. J Gastroenterol Hepatol. 2003;18:1407-1411. https://doi.org/10.1046/j.1440-1746.2003.03166.x 10.1046/j.1440-1746.2003.03166.x [DOI] [PubMed] [Google Scholar]
- 4.Wang HW, Kuo CJ, Lin WR, et al. The clinical characteristics and manifestations of cytomegalovirus esophagitis. Dis Esophagus 2016;29:392-399. https://doi.org/10.1111/dote.12340 10.1111/dote.12340 [DOI] [PubMed] [Google Scholar]
- 5.Maguire A, Sheahan K. Pathology of oesophagitis. Histopathology. 2012;60:864-879. https://doi.org/10.1111/j.1365-2559.2011.03855.x 10.1111/j.1365-2559.2011.03855.x [DOI] [PubMed] [Google Scholar]
- 6.Bestari MB, Agustanti N, Abdurachman SA. Clindamycin-Induced Esophageal Injury: Is It an Underdiagnosed entity? Clin Med Insights Case Rep. 2019;12:1179547619884055. https://doi.org/10.1177/1179547619884055 10.1177/1179547619884055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kikendall JW. Pill esophagitis. J Clin Gastroenterol 1999;28:298-305. https://doi.org/10.1097/00004836-199906000-00004 10.1097/00004836-199906000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Panarelli NC. Other forms of esophagitis: it is not gastroesophageal reflux disease, so now what do I do? Surg Pathol Clin 2017;10:765-779. https://doi.org/10.1016/j.path.2017.07.001 10.1016/j.path.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 9.Murro D, Jakate S. Radiation esophagitis. Arch Pathol Lab Med 2015;139:827-830. https://doi.org/10.5858/arpa.2014-0111-RS 10.5858/arpa.2014-0111-RS [DOI] [PubMed] [Google Scholar]
- 10.Grossi L, Ciccaglione AF, Marzio L. Esophagitis and its causes: Who is “guilty” when acid is found “not guilty”?. World J Gastroenterol 2017;23:3011-3016. https://doi.org/10.3748/wjg.v23.i17.3011 10.3748/wjg.v23.i17.3011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abid S, Mumtaz K, Jafri W, et al. Pill-induced esophageal injury: endoscopic features and clinical outcomes. Endoscopy. 2005;37:740-744. https://doi.org/10.1055/s-2005-870129 10.1055/s-2005-870129 [DOI] [PubMed] [Google Scholar]
- 12.Chang J, Han SE, Paik SS, et al. Corrosive esophageal injury due to a commercial vinegar beverage in an adolescent. Clin Endosc 2019. https://doi.org/10.5946/ce.2019.066. 10.5946/ce.2019.066 Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918-3930. https://doi.org/10.3748/wjg.v19.i25.3918 10.3748/wjg.v19.i25.3918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zargar SA, Kochhar R, Nagi B, et al. Ingestion of corrosive acids. Spectrum of injury to upper gastrointestinal tract and natural history. Gastroenterology 1989;97:702-7. [PubMed] [Google Scholar]
- 15.Zargar SA, Kochhar R, Nagi B, et al. Ingestion of strong corrosive alkalis: spectrum of injury to upper gastrointestinal tract and natural history. Am J Gastroenterol 1992;87:337-41. [PubMed] [Google Scholar]
- 16.Kamat R, Gupta P, Reddy YR, et al. Corrosive injuries of the upper gastrointestinal tract: a pictorial review of the imaging features. Indian J Radiol Imaging 2019;29:6-13. https://doi.org/10.4103/ijri.IJRI_349_18 10.4103/ijri.IJRI_349_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Purdy JK, Appelman HD, McKenna BJ. Sloughing esophagitis is associated with chronic debilitation and medications that injure the esophageal mucosa. Mod Pathol 2012;25:767-775. https://doi.org/10.1038/modpathol.2011.204 10.1038/modpathol.2011.204 [DOI] [PubMed] [Google Scholar]
- 18.Hart PA, Romano RC, Moreira RK, et al. Esophagitis dissecans superficialis: clinical, endoscopic, and histologic features. Dig Dis Sci 2015;60:2049-2057. https://doi.org/10.1007/s10620-015-3590-3 10.1007/s10620-015-3590-3 [DOI] [PubMed] [Google Scholar]
- 19.Longman RS, Remotti H, Green PH. Esophagitis dissecans superficialis. Gastrointest Endosc 2011;74:403-404. https://doi.org/10.1016/j.gie.2011.03.1117 10.1016/j.gie.2011.03.1117 [DOI] [PubMed] [Google Scholar]
- 20.Moawad FJ, Appleman HD. Sloughing esophagitis: a spectacular histologic and endoscopic disease without a uniform clinical correlation. Ann N Y Acad Sci 2016;1380:178-182. https://doi.org/10.1111/nyas.13112 10.1111/nyas.13112 [DOI] [PubMed] [Google Scholar]
- 21.Khan H, Ahmed M, Daoud M, et al. Acute Esophageal Necrosis: a view in the dark. Case Rep Gastroenterol 2019;13:25-31. https://doi.org/10.1159/000496385 10.1159/000496385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dias E, Santos-Antunes J, Macedo G. Diagnosis and management of acute esophageal necrosis. Ann Gastroenterol 2019;32:529-540. https://doi.org/10.20524/aog.2019.0418 10.20524/aog.2019.0418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim SM, Song KH, Kang SH, et al. Evaluation of prognostic factor and nature of acute esophageal necrosis: restropective multicenter study. Medicine (Baltimore) 2019;98:e17511. https://doi.org/10.1097/MD.0000000000017511 10.1097/MD.0000000000017511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah J, Savlania A, Bush N, et al. Three cases of an unusual cause of haematemesis: black oesophagus. Trop Doct 2020;14:49475519900756. https://doi.org/10.1177/0049475519900756 10.1177/0049475519900756 [DOI] [PubMed] [Google Scholar]
- 25.Jessurun J, Cui I, Aristi-Urista G. Acute (gangrenous) esophageal necrosis (black esophagus). A rare form of injury with specific histologic features and diverse clinical associations with a common pathogenesis. Hum Pathol. 2019;87:44-50. https://doi.org/10.1016/j.humpath.2019.02.003 10.1016/j.humpath.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 26.De Felice KM, Katzka DA, Raffals LE. Crohn’s Disease of the esophagus: clinical features and treatment outcomes in the biologic era. Inflamm Bowel Dis 2015;21:2106-2113. https://doi.org/10.1097/MIB.0000000000000469 10.1097/MIB.0000000000000469 [DOI] [PubMed] [Google Scholar]
- 27.Saadah OI, Fallatah KB, Baumann C, et al. Histologically confirmed upper gastrointestinal Crohn’s disease: is it rare or are we just not searching hard enough? Intest Res 2020. https://doi.org/10.5217/ir.2019.00091 10.5217/ir.2019.00091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laube R, Liu K, Schifter M, et al. Oral and upper gastrointestinal Crohn’s disease. J Gastroenterol Hepatol 2018;33:355-364. https://doi.org/10.1111/jgh.13866 10.1111/jgh.13866 [DOI] [PubMed] [Google Scholar]
- 29.Ebach DR, Vanderheyden AD, Ellison JM, et al. Lymphocytic esophagitis. A possible manifestation of pediatric upper gastrointestinal Crohn’s disease. Inflamm Bowel Dis 2011;17:4549. https://doi.org/10.1002/ibd.21347 10.1002/ibd.21347 [DOI] [PubMed] [Google Scholar]
- 30.Rubio CA, Sjödahl K, Lagergren J. Lymphocytic esophagitis. A histologic subset of chronic esophagitis. Am J Clin Pathol 2006;125:432-437. [PubMed] [Google Scholar]
- 31.Rubio CA, Dick EJ, Jr, Orrego A, et al. Incidence of lymphocytic esophagitis in baboons. In vivo 2008;22:613-616. [PubMed] [Google Scholar]
- 32.Rubio CA, Dick EJ, Orrego A, et al. The frequency of lymphocytic and reflux esophagitis in non-human primates. Int J Clin Exp Pathol 2008;1:531-535. [PMC free article] [PubMed] [Google Scholar]
- 33.Sutton LM, Heintz DD, Patel AS, et al. Lymphocytic esophagitis in children Inflamm Bowel Dis 2014;20:1324-1328. https://doi.org/10.1097/MIB.0000000000000100 10.1097/MIB.0000000000000100 [DOI] [PubMed] [Google Scholar]
- 34.Haque S, Genta RM. Lymphocytic oesophagitis: clinicopathological aspects of an emerging condition. Gut 2012;61:1108-1114. https://doi.org/10.1136/gutjnl-2011-301014 10.1136/gutjnl-2011-301014 [DOI] [PubMed] [Google Scholar]
- 35.Xue Y, Suriawinata A, Liu X, et al. Lymphocytic Esophagitis With CD4 T-cell-predominant intraepithelial lymphocytes and primary esophageal motility abnormalities: a potential novel clinicopathologic entity. Am J Surg Pathol 2015;39:1558-67. https://doi.org/10.1097/PAS.0000000000000493 10.1097/PAS.0000000000000493 [DOI] [PubMed] [Google Scholar]
- 36.Lisovsky M, Westerhoff M, Zhang X. Lymphocytic esophagitis: a histologic pattern with emerging clinical ramifications. Ann N Y Acad Sci 2016;1381:133-138. https://doi.org/10.1111/nyas.13260 10.1111/nyas.13260 [DOI] [PubMed] [Google Scholar]
- 37.Cohen S, Saxena A, Waljee AK, et al. Lymphocytic esophagitis: a diagnosis of increasing frequency. J Clin Gastroenterol 2012;46:828-832. https://doi.org/10.1097/MCG.0b013e3182500de8 10.1097/MCG.0b013e3182500de8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rouphael C, Gordon IO, Thota PN. Lymphocytic esophagitis: still an enigma a decade later. World J Gastroenterol 2017:23:949-956. https://doi.org/10.3748/wjg.v23.i6.949 10.3748/wjg.v23.i6.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Genta RM. Lymphocytic Esophagitis. Gastroenterol Hepatol 2015;11:559-561. [PMC free article] [PubMed] [Google Scholar]
- 40.Ronkainen J, Walker MM, Aro P, et al. Lymphocytic oesophagitis, a condition in search of a disease? Gut 2012;61:1776. https://doi.org/10.1136/gutjnl-2012-302329 10.1136/gutjnl-2012-302329 [DOI] [PubMed] [Google Scholar]
- 41.Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol 2013;108:679-692. https://doi.org/10.1038/ajg.2013.71 10.1038/ajg.2013.71 [DOI] [PubMed] [Google Scholar]
- 42.Veerappan GR, Perry JL, Duncan TJ. Prevalence of eosinophilic esophagitis in an adult population undergoing upper endoscopy: a prospective study. Clin Gastroenterol Hepatol. 2009;7:420-426. https://doi.org/10.1016/j.cgh.2008.10.009 10.1016/j.cgh.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 43.Molina-Infante J, Bredenoord AJ, Cheng E, et al. Proton pump inhibitor-responsive oesophageal eosinophilia: an entity challenging current diagnostic criteria for eosinophilic oesophagitis. Gut 2016;65:524-31. https://doi.org/10.1136/gutjnl-2015-310991 10.1136/gutjnl-2015-310991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Molina-Infante J, Hirano I, Spechler SJ, et al. Clarifying misunderstandings and misinterpretations about oesophageal eosinophilia. Gut. 2017;66:1173-1174. https://doi.org/10.1136/gutjnl-2016-312851 10.1136/gutjnl-2016-312851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim HP, Vance RB, Shaheen NJ, et al. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis:a meta-analysis. Clin Gastroenterol Hepatol 2012;10:988-996. https://doi.org/10.1016/j.cgh.2012.04.019 10.1016/j.cgh.2012.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lucendo AJ, Molina-Infante J, Arias Á, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J 2017;5:335-358. https://doi.org/10.1177/2050640616689525 10.1177/2050640616689525 [DOI] [PMC free article] [PubMed] [Google Scholar]


