Abstract
The COVID-19 pandemic has and will continue to result in negative mental health outcomes such as depression, anxiety and traumatic stress in people and populations throughout the world. A population mental health perspective informed by clinical psychology, psychiatry and dissemination and implementation science is ideally suited to address the broad, multi-faceted and long-lasting mental health impact of the pandemic. Informed by a systematic review of the burgeoning empirical research on the COVID-19 pandemic and research on prior coronavirus pandemics, we link pandemic risk factors, negative mental health outcomes and appropriate intervention strategies. We describe how social risk factors and pandemic stressors will contribute to negative mental health outcomes, especially among vulnerable populations. We evaluate the scalability of primary, secondary and tertiary interventions according to mental health target, population, modality, intensity and provider type to provide a unified strategy for meeting population mental health needs. Traditional models, in which evidence-based therapies delivered are delivered in-person, by a trained expert, at a specialty care location have proved difficult to scale. The use of non-traditional models, tailoring preventive interventions to populations based on their needs, and ongoing coordinated evaluation of intervention implementation and effectiveness will be critical to refining our efforts to increase reach.
Keywords: COVID-19, Mental health, Risk factor, Intervention, Evidence-based psychotherapy, Population mental health
The COVID-19 pandemic will result in a colossal negative mental health impact due to the many people affected by the pandemic, its disruption of most, if not all, aspects of everyday life, and its multiple waves and protracted nature. Indeed, the COVID-19 pandemic has already been linked to negative mental health outcomes such as depression, anxiety, and traumatic stress in populations across the world (Alzueta et al., 2020; de Pablo et al., 2020; Salari et al., 2020; Taquet, Luciano, Geddes, & Harrison, 2020; Xiong et al., 2020). More people will experience these outcomes as the pandemic and its negative consequences, such as economic hardship, continue. These outcomes will be long-lasting and quite substantial among some people and populations, as evidenced by research on the severe acute respiratory syndrome (SARS) and middle east respiratory syndrome (MERS) coronavirus pandemics (Lam et al., 2009; Mak, Chu, Pan, Yiu, & Chan, 2009). A population mental health perspective informed by clinical psychology, psychiatry and dissemination and implementation science is ideally suited to address the negative mental health impact of the COVID-19 pandemic (United Nations, 2020).
Population mental health considers how multiple determinants of health contribute to dissimilar outcomes across populations of people (Kindig & Stoddardt, 2003). Included among these determinants are factors that increase risk of negative mental health outcomes that should be proactively identified and targeted for intervention. Within this framework, appropriate intervention is defined by the scale of population needs. Primary prevention addresses ‘universal’ determinants of mental health across populations, ‘selective’ populations with elevated pandemic-related risk (e.g., healthcare workers), and ‘indicated’ populations with early signs of pandemic-related distress. Secondary prevention includes screening, early identification and brief interventions that prevent the progression of distress and slow the incidence of disorder among populations. Tertiary prevention includes relatively intensive evidence-based interventions shown to improve functioning and reduce the consequences of mental disorders on quality of life.
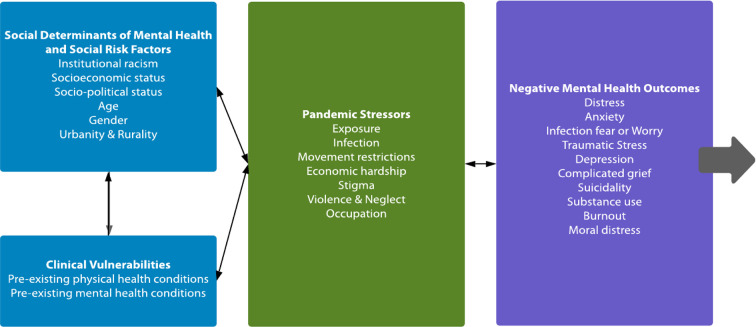
We use a population mental health framework to link risks, outcomes and interventions to population needs (see Fig. 1 ). We outline targets of prevention efforts – social determinants of health and social risk factors and pandemic-related stressors (hereafter labeled ‘risks’) and negative mental health outcomes (hereafter labeled ‘outcomes’) – identified via a systematic review of the burgeoning empirical research on the mental health impact of the COVID-19 pandemic. To provide comprehensive coverage of the topic, including evidence of links between coronavirus pandemics and long-term negative mental health outcomes, we also review empirical research on SARS and MERS coronavirus pandemics (see Boden, 2020 for details). We then describe a framework that matches prevention targets to appropriate primary, secondary and tertiary interventions based on their evidence of effectiveness and the feasibility of implementation at the scale of population needs.
Fig. 1.
Targets of population health interventions: social determinants of health and social risk factors as they interact with pandemic stressors to increase risk of negative mental health outcomes.
Social determinants of mental health and social risk factors (socio-demographic characteristics & clinical vulnerabilities) and pandemic stressors may increase risk of adverse mental health outcomes in isolation or together in synergistic ways. Pandemic stressors directly increase risk of mental health outcomes. Social determinants of mental health and social risk factors increase risk by increasing the likelihood or impact of pandemic stressors. As represented by grey the arrow, mental health outcomes may persist indefinitely.
1. Prevention targets
A growing literature on social determinants of health identifies the complex systems that powerfully shape prevalence patterns for various outcomes and drive avoidable differences in health across populations (Braveman & Gottlieb, 2014). The COVID-19, SARS and MERS, and social determinants of health scientific literatures together provide evidence that multiple social risk factors are likely to heighten the impact of pandemic stressors among people and populations with selective and indicated primary prevention risks, thus increasing risk of a variety of negative mental health outcomes (see Fig. 1). Included among these social risk factors are (a) institutional racism and discrimination that targets Black, Indigenous People of Color (BIPOC; Novacek, Hampton-Anderson, Ebor, Loeb, & Wyatt, 2020; Raifman & Raifman, 2020; van Dorn, Cooney, & Sabin, 2020; Yancy, 2020), (b) socioeconomic systems that lead to poverty (Bu, Steptoe, & Fancourt, 2020; Hawkins, Charles, & Mehaffey, 2020), (c) socio-political policies that target undocumented immigrants (van Dorn et al., 2020), (d) developmental factors that impact old and young persons (Cheung, Chau, & Yip, 2008; Xie et al., 2020), (e) sexism and misogyny that targets women (Wenham, Smith, & Morgan, 2020) and heteronormative ideology that targets LGTBQ identities (Salerno, Williams, & Gattamorta, 2020), (f) characteristics of urban and rural living areas that disproportionately impact BIPOC and people with limited economic means (Omary, 2020; Stack et al., 2020), and (g) physical and mental health vulnerabilities that disproportionately impact BIPOC, people with limited economic means, and older adults (Hao et al., 2020; Taquet et al., 2020).
Empirical research on COVID-19, SARS and MERS has identified key pandemic stressors that will increase risk of a negative mental health outcome broadly, and especially among targeted communities exposed to the social risk factors we discuss. Key pandemic stressors include: (a) exposure (to the virus, media exposure, exposure to death; Garfin, Silver, & Holman, 2020; Taylor et al., 2020), (b) viral infection (Rogers et al., 2020), (c) movement restriction (Brooks et al., 2020), (d) economic hardship (Witteveen & Velthorst, 2020), (e) stigma, prejudice and discrimination (Bagcchi, 2020; Misra, Le, Goldmann, & Yang, 2020), (f) intimate partner violence (Boserup, McKenney, & Elkbuli, 2020; Gosangi et al., 2020) and child abuse and neglect (Bryant, Oo, & Damian, 2020), and (g) occupations that increase risk of exposure/infection, stress and other challenges to health and well-being (Baker, 2020; de Pablo et al., 2020).
We posit that social determinants and risk factors combine with pandemic stressors in additive and interactive ways to contribute to negative mental health outcomes, including (a) distress (Twenge & Joiner, 2020), (b) anxiety (Alzueta et al., 2021; Fitzpatrick, Harris, & Drawve, 2020), (c) infection fear/worry (Lee, Jobe, Mathis, & Gibbons, 2020; Taylor et al., 2020), (d) traumatic stress (Cooke, Eirich, Racine, & Madigan, 2020), (e) depression (Alzueta et al., 2021; Bueno-Notivol et al., 2020), (f) complicated grief (Wallace, Wladkowski, Gibson, & White, 2020), (g) suicidality (Petterson, Westfall, & Miller, 2020), (h) substance use (Czeisler et al., 2020), (i) burnout (Kannampallil et al., 2020; Matsuo et al., 2020), and (j) moral distress (Dunham, Rieder, & Humbyrd, 2020). Negative mental health outcomes resulting from the pandemic may be immediate or have a delayed onset and may be of relatively shorter or longer duration. Some outcomes may be adaptive in circumscribed contexts and for limited durations. For example, infection-related fear may facilitate self-protective behaviors (Rosen & Schulkin, 1998). Other outcomes may be functionally impairing and a sign/symptom of a diagnosable mental disorder (American Psychiatric Association, 2013).
We distill from multiple broad scientific literatures a simplified framework to inform data collection and research (see Fig. 1). Such work is needed to transition our simplified framework into a detailed model through investigation of the multiple pathways through which risks independently and interactively contribute to a diversity of outcomes (see Zvolensky et al., 2020 for a related discussion). Our framework is also intended to provide a basis for the intervention strategy we discuss in the second half of the paper. There, we discuss how social risk factors and pandemic stressors will be most frequently targeted through primary and secondary intervention efforts. Secondary prevention will be targeted to preventing distress and the development of mental disorders, and tertiary prevention will be targeted to reducing the impact of mental disorders once they have occurred.
1.1. Social determinants of mental health and social risk factors
Institutional racism and discrimination and low socioeconomic status will increase risk of distress, anxiety, depression and traumatic stress in populations through varying degrees of structural inequity, exploitation, and oppression. BIPOC and people with limited economic means will be systematically exposed to more pandemic-related stressors (e.g., Bu et al., 2020; Hawkins et al., 2020; Mackey et al., 2020; Novacek et al., 2020; Raifman & Raifman, 2020). These populations are overrepresented in ‘essential’ jobs that increase risk of exposure, don't provide telework or paid sick leave, and are being furloughed and laid-off (Czeisler et al., 2020). Reduced access to healthcare, including testing for infection, heightens risk of an outcome. Language, educational and technological barriers (e.g., lack of high-speed internet) will limit learning of and engaging in preventive measures and access to therapeutic resources. Pre-existing conditions (hypertension, diabetes) that increase COVID-19 severity are highly prevalent among BIPOC and people with limited economic means (Yancy, 2020). Pre-existing mental health conditions may be exacerbated by racial/ethnic and economic disparities. The loss of social capital and relationship, community networks and factors that ease the burdens of pandemic-related economic hardship (d'Hombres, Rocco, Suhrcke, & McKee, 2010) may also increase risk. Indigenous populations such as Native Americans and Canadian First Nations will be structurally vulnerable due to a combination of severe shortages in and chronic underfunding of healthcare, severe lack of resources (e.g., in-home water, electricity), and pre-existing health conditions (Raifman & Raifman, 2020; van Dorn et al., 2020).
Socio-political status will systematically burden undocumented persons residing in the United States, and asylum-seekers (Page, Venkataramani, Beyrer, & Polk, 2020). Undocumented persons and their families are made exceptionally vulnerable to mental health outcomes through the synergistic intersection of multiple inequities: social-political status, high-risk occupations (e.g., essential work of migrant farm labor, meat processing, restaurant cooking, domestic care, and hotel services), low-income, low levels of English literacy, lack of sick leave and health insurance coverage, and crowded living conditions (Mucci et al., 2019). Unaccompanied minors at the US-Mexico border will be at additional risk of an outcome due to high exposure/infection rates while detained in group settings.
Due to the increased risks of both severe infection and death, old age will increase the risk of distress and anxiety. Additionally, older adults limited in functioning, movement, social support, etc. are likely to be at disproportionate risk of outcomes such as distress and depression from deprivation and loss of social support resulting from movement restrictions (Cheung et al., 2008; D'cruz & Banerjee, 2020; cf. de Bruin, 2021). Children will also be at heightened risk due to movement restrictions and disruptions in routine (Xie et al., 2020), infection of caregivers (e.g., parents), and efforts to limit infection through quarantine and isolation. Risk will be amplified among children whose caregivers are severely infected and who die. A subset of children will be at lasting risk of a mental health outcome due to increased exposure to child abuse (see Pandemic Stressors section).
The pandemic is likely to heighten existing gender inequalities that favor men over women, placing women at greater risk of distress, anxiety, depression and traumatic stress. Approximately 70% of healthcare workers are women (Boniol et al., 2019), putting them at increased risk of an outcome related to exposure, infection, job type, and stigma (Wenham et al., 2020). While recessions are thought to more adversely impact employment of men versus women, movement restrictions disproportionately affect sectors with high female employment (Alon, Doepke, Olmstead-Rumsey, & Tertilt, 2020) and disruption in childcare needs particularly impact working mothers. Furthermore, woman who are denied access to contraception, safe abortions, and treatments of sexually transmitted infections (United Nations, 2020) may be at heightened risk of distress and anxiety. Women and girls are at higher risk (than men and boys) of intimate partner violence, and thus, resulting anxiety, depression and traumatic stress. Members of the lesbian, gay, bisexual, transgender, and queer or questioning (LGBTQ) community will face additional risk for an outcome as existing social inequities (e.g., less access to healthcare, higher poverty) and mental health disparities (i.e., higher rates of mood disorders) are exacerbated by the pandemic (Salerno et al., 2020). For example, LGBTQ youth subject to school closures may be cut-off from school-based mental health services while residing in unwelcoming or abusive environments (Witteveen & Velthorst, 2020). Though we posit that females and members of the LGBTQ community are at higher risk of an outcome than are males, male gender has the potential to increase risk of an outcome via increased risk of severe infection and mortality (Jin et al., 2020).
Urbanity and Rurality will also influence risk of an outcome. Persons living in densely populated areas, such as urban neighborhoods relegated to people of color and people with low income, will be at greater risk for COVID-19 exposure, infection and associated mental health outcomes. Among persons living in rural areas who are infected or exposed to other pandemic stressors, limited access to preventative information, healthcare services, and other resources will be especially acute and heighten risk for a negative mental health outcome (Omary, 2020; Stack et al., 2020).
1.2. Clinical vulnerabilities
Clinical vulnerabilities including pre-existing physical/mental health conditions that are variable, disruptive, contribute to poor physical/mental health, limit functioning, or require ongoing or costly treatment - will increase risk of an outcome, and especially, distress and anxiety at times during the pandemic that are characterized by stress and uncertainty. Physical conditions (e.g., diabetes, COPD) and treatments (e.g., immunosuppressants) that specifically increase risk of (severe) infection are likely to increase risk of a mental health outcome (see Pandemic Stressors section). Mental disorders such as generalized anxiety disorder and obsessive-compulsive disorder may be exacerbated by threat of infection (Neelam, Duddu, Anyim, Neelam, & Lewis, 2020; Taquet et al., 2020). Restrictions in movement will potentially exacerbate depression and anxiety (Hao et al., 2020). Further heightening these risks are limitations to treatment access (e.g., regular psychotherapy), resources (e.g., health foods, supplements), social support, and disruptions in medication supply (e.g., chloroquine for Lupus patients) and economic hardship (McAlpine & Alang, 2020). Pre-existing conditions that increase COVID-19 severity are highly prevalent among BIPOC and people with limited economic means (Yancy, 2020).
1.3. Pandemic stressors
Key pandemic stressors include exposure to the virus, media exposure and exposure to death. Physical exposure to infected people when one's infection status is unknown that results in threat (of being infected) and uncertainty (about one's infection status; Taha, Matheson, Cronin, & Anisman, 2014), will thus increase risk of distress and anxiety (Lai et al., 2020; Liu et al., 2012; Taylor et al., 2020). By increasing perceptions of threat, loss and deprivation, media exposure will also increase risk (Garfin et al., 2020). Exposure to death (of family, friends, colleagues, patients) will increase risk of depression, traumatic stress and complicated grief due to (a) the suddenness and unexpectedness of the death, (b) difficulties communicating prior to death, (c) limitations to social support and mourning rituals (Wallace et al., 2020). Continual exposure to reminders of the loss via media exposure will also exacerbate risk (Kristensen, Dyregrov, Dyregrov, & Heir, 2016).
Asymptomatic and minor infection will increase risk of distress and anxiety about one's health and exposure of other people to infection (Alzueta et al., 2021; Taylor et al., 2020). Severe infections, and especially those requiring hospitalization, intensive care, and mechanical ventilation, will exacerbate risk due to greater disruption to routines (e.g., missing work), threat to health and mortality, and trauma related to the illness and treatment (Bienvenu et al., 2018; Rogers et al., 2020; Wu, Chan, & Ma, 2005). Risk may be long-lasting even among recovered persons and could contribute to persistent negative outcomes, including depressive, anxiety, and traumatic stress disorders (Lam et al., 2009; Mak et al., 2009). Persons who know or presume they have infected others will be at increased risk of guilt and anxiety, amplified, for example, by the psychological/emotional closeness of infected persons.
Movement restrictions ranging from relatively unenforced stay-at-home/shelter-in-place orders to restrictive lockdowns and quarantine/isolation will increase risk of loneliness, distress, anxiety, depression, and substance use/abuse, especially among structurally vulnerable populations (e.g., elderly adults) and those subjected to longer and more substantial restrictions (Brooks et al., 2020; Kim & Laurence, 2020). These outcomes may result from limited (a) physical and social contact with loved ones, (b) access to jobs and material resources needed to fulfill basic needs (e.g., food), and (c) engagement in routines and activities that provide purpose and meaning, and improve health and mood. Movement restrictions may also necessitate sustained contact with abusive and violent people, increasing exposure to intimate partner violence and child abuse that result in negative mental health outcomes (Bryant et al., 2020; Gosangi et al., 2021).
Pandemic-related economic hardship includes related loss of jobs, wages, benefits and health insurance, each occurring on a massive scale since the start of pandemic-related movement restrictions. Economic hardship is likely to persist for years, and to disproportionality impact people with limited economic means. Preliminary evidence has demonstrated linked increased reports of depression and health anxiety to COVID-19-related economic hardship (Witteveen & Velthorst, 2020), with specific groups such as Black people, young people and adults with children living at home expressing increased anxiety (Mann, Krueger, & Vohs, 2020). Furthermore, COVID-19-related job loss has been found to be associated with maltreatment of children (Lawson, Piel, & Simon, 2020). Ongoing economic hardship will increase risk of immediate and long-term distress and anxiety regarding survival and well-being, depression (e.g., due to the loss of meaning/purpose provided by sustained employment), substance use to cope, and violence (Elbogen et al., 2020; Schneider, Harknett, & McLanahan, 2016; Schneider, Waldfogel, & Brooks-Gunn, 2017).
Stigma, prejudice, and discrimination directed towards SARS-CoV-2 infected and exposed people, people of Asian descent (in Western countries) and healthcare workers has been reported (Bagcchi, 2020; Misra et al., 2020). Those who have lost their job and/or receiving government assistance as a result of the pandemic will also potentially face an increased risk of stigma, prejudice and discrimination (Karren, Karren, & Sherman, 2012). Among the pernicious effects of coronavirus-related stigma, prejudice and discrimination are heightened risks for distress, anxiety and depression (Park, Lee, Park, & Choi, 2018), especially among already stigmatized people (e.g., those with mental disorders and low socioeconomic status).
Pandemic stressors and outcomes (e.g., substance use) will increase the risk of intimate partner violence (Gosangi et al., 2021) and child abuse/neglect (Bryant et al., 2020; Schneider et al., 2016; Schneider et al., 2017) occurring among vulnerable couples and families. Couples sheltering together due to movement restrictions will potentially experience increased tension, especially if one or both partners are unemployed and/or infected. Increases in intimate partner violence have been documented in multiple countries (Boserup et al., 2020) and is predicted to worsen as economic hardship becomes more acute. Risk of substance use, anxiety, depression and traumatic stress resulting from intimate partner violence may be exacerbated due to limitations to access to resources, advocates and a court system that could mitigate the harm.
Prolonged school closures will increase financial burden and other (e.g., teaching) responsibilities for many parents, some of whom will not have the resources or capability to provide for their children. Children who utilized school lunches, medical care, and mental health treatment resources provided by school prior to the pandemic may not have access to them. Many children are currently disconnected from peers, social support, and a safe environment, which will adversely impact children's future mental health for years to come. Some children will experience abuse and neglect, which can result in outcomes ranging from low self-esteem to post-traumatic stress disorder (PTSD) (Campbell, 2002; Leeb, Lewis, & Zolotor, 2011). Preliminary evidence also suggests that school closures and isolation have exacerbated mental health concerns reported by children and adolescents (Xie et al., 2020).
Particular occupations will increase risk of distress, anxiety, burnout, and traumatic stress during the pandemic. At risk are people with service industry jobs that increase contact with potentially or known infected people (e.g., janitorial and food service employees in hospital settings, delivery persons, food service employees, waste collectors, meat processing workers), those whose jobs are negatively impacted by the economic downturn (e.g., hospitality service) and first responders (e.g., emergency medical technicians, law enforcement; Baker, 2020). Front-line healthcare providers, in particular, may be exposed to numerous stressors, including sustained and repeated exposure to severely infected and dying people, intense and stressful work environments, long working hours, and morally ambiguous decisions regarding who receives treatment (Lai et al., 2020; Liu et al., 2012). These risks will increase risk of numerous negative outcomes, including depression, anxiety, traumatic stress and related disorders (de Pablo et al., 2020). Caregiving in a professional (e.g., to people with mental disabilities) or personal capacity (e.g., to children or elderly parents) will increase risk of distress, burnout, anxiety, depression, and, in the event of loss, complicated grief (Adelman, Tmanova, Delgado, Dion, & Lachs, 2014). Providing care to a person known or presumed to be infected, and at greater risk of (severe) infection (e.g., due to pre-existing physical illness) may increase uncertainty and threat (to oneself and the recipient of care), and thus, anxiety (Czeisler et al., 2020). The burden of providing care is likely to increase due to economic hardship and movement restrictions, impacting not only professional caregivers but people who care for their children and parents (Griffith, 2020).
1.4. Negative mental health outcomes
Distress is likely to be a common psychological/emotional response to the pandemic (Qiu et al., 2020; Twenge & Joiner, 2020), and the first and most easily identified outcome in most people (Kessler et al., 2002). Non-specific distress may dissipate as the pandemic subsides (Daly & Robinson, 2020), or be long-lasting and further evolve into a specific symptom or symptoms, and a diagnosable mental disorder.
Anxiety will be quite common (Alzueta et al., 2021; Fitzpatrick et al., 2020) as any given person will face numerous threats, including exposure, infection, severe infection, mortality, infection of others, economic deprivation, and isolation, in addition to uncertainty. Intolerance of uncertainty and efforts to avoid feared stimuli (e.g., the virus) will reinforce and exacerbate anxiety in some people (Newman & Llera, 2011; Rettie & Daniels, 2020). Anxiety may be more generalized or focus on individual threats. An example of the latter, infection-related fear/worry will be a common mental health outcome among people exposed to and infected by the virus, those whose loved ones are exposed or infected, and those without resources to cope should they become infected (Lee et al., 2020; Taylor et al., 2020; Wu et al., 2005). Among anxiety disorders resulting from the pandemic, we expect that illness anxiety, somatic symptoms, and generalized anxiety disorder will be most common (Lam et al., 2009; Mak et al., 2009). People exposed to potentially traumatic events resulting from infection (e.g., invasive treatments, witnessing death) and other pandemic stressors (e.g., violence at home) will be at risk of experiencing acute stress, and potentially post-traumatic stress symptoms and disorders (e.g., PTSD) over time (Jones, Hughes, & Unterstaller, 2001; Lai et al., 2020; Mak et al., 2009).
Stressful events associated with depression (e.g., severe illness, interpersonal loss, unemployment and economic hardship; Dooley, Catalano, & Wilson, 1994; Hammen, 2005), will be common experiences during the pandemic (Alzueta et al., 2021; Bueno-Notivol et al., 2020; Lai et al., 2020; Liu et al., 2012; Mak et al., 2009). Among vulnerable populations (e.g., elderly; Cheung et al., 2008), suicidality (i.e., suicidal ideation and behavior) and completed suicide are likely to increase (Elbogen et al., 2020; Petterson et al., 2020). As more people fall-ill and die of COVID-19, the prevalence of complicated grief will likely increase among their friends, families, caregivers and healthcare providers (Wallace et al., 2020).
Health services and addictions researchers have raised concerns that as the pandemic continues, we will see an increase in substance use and related disorders (Rehm et al., 2020; Stack et al., 2020) and more severe health consequences from these conditions (Marsden et al., 2020; also see Mak et al., 2009). These outcomes may be attributable to the use of alcohol and other substances to cope with pandemic stressors (e.g., economic hardship) and outcomes (e.g., stress, anxiety, depression) or for recreation or pleasure that is otherwise unavailable (Cooper, Frone, Russell, & Mudar, 1995; Spagnolo, Montemitro, & Leggio, 2020). During the pandemic, barriers to receiving detox and other treatments (e.g., opiate agonist treatment; mutual self-help groups) may increase or perpetuate substance use, in addition to heightening medical risk and the more severe symptoms of a use disorder (Narasimha et al., 2020).
Occupational burnout is heightened among people working under new, potentially burdensome and/or stressful circumstances (Van Mol, Kompanje, Benoit, Bakker, & Nijkamp, 2015). Thus, workers of the occupation types we mention above, such as healthcare providers (Kannampallil et al., 2020; Matsuo et al., 2020) and caregivers (Adelman et al., 2014), may experience higher rates of burnout due to the pandemic. Even parents may experience pandemic-related occupational burnout (Griffith, 2020). Healthcare workers are also at risk of moral distress when they engage in actions and make choices are inconsistent with their morals, ethics, or values (e.g., how to allocate limited life-saving resources; Dunham et al., 2020; Lamiani, Borghi, & Argentero, 2017).
2. Prevention interventions
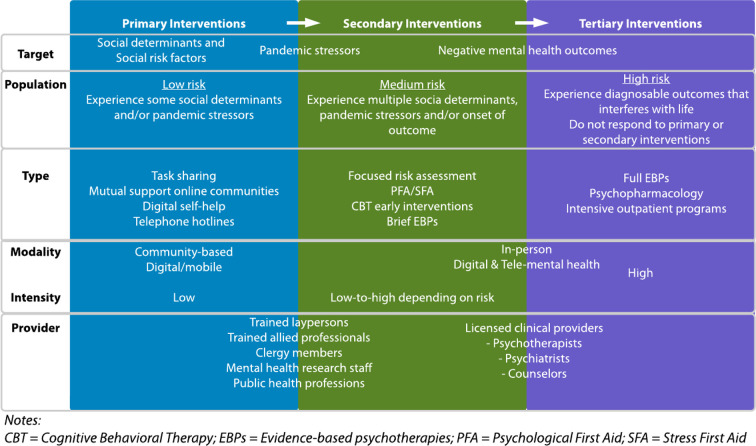
We describe appropriate primary, secondary, and tertiary preventive interventions based on population size and anticipated need, with a focus on how intervention target, population, modality, intensity and provider type can be leveraged to scale intervention implementation (see Fig. 2 ) within specified services systems. Evidence for the efficacy of mental health interventions to address the impact of pandemics, including COVID-19, is accumulating (see Yue et al., 2020 for a review). Central to pandemic-related prevention efforts is the scalability of mental health intervention to retain effectiveness when expanded to increase reach (Milat, King, Bauman, & Redman, 2013). The scalability of effective interventions is affected by the costs, workforce, and technical resources required, and acceptable delivery modes in social and organizational contexts. These factors are likely to present tradeoffs. An effective intervention for the large population of people with limited risk exposure and outcomes may not be adequate for fewer people with greater needs. A highly effective intervention for a mental disorder (e.g., prolonged exposure for PTSD; Foa et al., 2018) will be more difficult to apply to large segments of the population (see Moring et al., 2020; Wells et al., 2020). As a result, population mental health focuses primary preventive interventions on the largest populations, saving the more intensive secondary and tertiary interventions for populations with greater needs.
Fig. 2.
Characteristics of primary, secondary and tertiary prevention interventions suitable for addressing the mental health impact of COVID-19.
Notes: CBT = Cognitive Behavioral Therapy; EBPs = Evidence-based psychotherapies; PFA = Psychological First Aid; SFA = Stress First Aid.
2.1. Primary prevention
Primary prevention addresses ‘universal’ determinants of mental health across populations (e.g., people with limited economic means), ‘selective’ populations with elevated pandemic-related risk (e.g., healthcare workers), and ‘indicated’ populations with early signs of pandemic-related distress (e.g., cashier who must continue to risk exposure to support her family). Initial primary intervention phase efforts occurring while the pandemic continues should focus on implementing community-wide interventions and digital self-management tools to populations with known universal risk factors. These interventions allow broad reach at low cost, and may mitigate the development of later or persistent outcomes. Yet, as discussed below, there is a dearth of research on larger scale community interventions and digital mental health tools that might be leveraged to support mental health in the context of COVID-19. Additionally, primary intervention efforts would ideally focus on addressing universal social determinants of health and selective populations with social risk factors through existing interventions that pre-date the pandemic or through new interventions designed for this purpose.
Intervening to address universal social determinants of health will require coordination among multiple levels of care and agency over long periods of time. Braveman, Egerter, and Williams (2011) state: “Recognizing the expense and methodologic challenges, we need multifaceted approaches that operate simultaneously across domains to interrupt damaging (and activate favorable) pathways at multiple points at which the underlying differences in social advantage and the consequent health inequalities are produced, exacerbated, and perpetuated” (pg. 391). Theorists have clarified the need to address upstream social determinants of health, such as socioeconomic status, that impact proximal behavioral determinants of health (Braveman et al., 2011; Braveman & Gottlieb, 2014). Yet, few interventions have been developed to address upstream social determinants of mental health and social risk factors we describe above, or have been adapted for selective and indicated populations at risk. Thus, we are limited to interventions that target downstream factors (e.g., access to mental healthcare), while positing that addressing upstream factors will improve our odds of successfully addressing future pandemics (e.g., by reducing virus transmission in vulnerable groups with high likelihood of infection).
With respect to these challenging circumstances, ideally, existing policies and guidelines (e.g., CDC, 2021; Nelson, 2002; World Health Organization, 2020), and interventions (see Williams & Purdie-Vaughns, 2015) will be leveraged to address health disparities that are exacerbated by the pandemic. New policies and interventions can also be harnessed to address pandemic-related health disparities. For example, United States government stimulus checks (Long & Stein, 2021) might provide exceptional benefits to people with limited socioeconomic means who are at higher risk of infection (Arno, House, Viola, & Schechter, 2011). Yet, the impact of these relatively limited supplements on downstream health outcomes are unclear. Evidence-based psychotherapies, which play a large role in our suggested intervention strategy will likely require swift adaptation to address vulnerable populations that do not as readily seek or receive such treatments due to cultural factors, social risk factors and unmet social needs (Miranda et al., 2005; Primm et al., 2010; Snowden & Yamada, 2005). Without directly targeting these social determinants of health and related risk factors, it will be challenging to implement the recommended primary, secondary and tertiary interventions we discuss below.
Community-based interventions include a range of approaches from mutual support online communities to outreach to elderly adults in affected neighborhoods and regions. Collective trauma can be managed regionally by developing partnerships that leverage local resources and nationwide programs. For example, after the Northern California fires, the VA's National Center for PTSD worked with locals to develop Sonoma Rises, a free mental health app, locals developed free trauma informed yoga classes, and community members articulated needs in town halls. Interventions might best be offered by local public health departments, community organizations and non-profits. Because of limited evidence regarding larger scale community interventions for mental health in the context of COVID-19, we must rely on theory and anecdotal reports when developing, implementing and disseminating community-based interventions, and collect data o evaluate effectiveness as we go (Naslund, Aschbrenner, Marsch, & Bartels, 2016). Furthermore, we might try to build upon social settings and cultural practices that likely support mental wellbeing, generally and in response to adversity and traumatic experiences.
The risk of infection and nationwide implementation of social distancing measures has interfered with access to a wide range of social settings and cultural practices that likely support positive mental health. Social settings that support such activities as religious practices, workplace socialization, sports activities, participation in hobbies and recreational activities, and performance of social roles of many kinds likely strengthen mental health by increasing positive mood, access to social support, perceptions of self-efficacy, aerobic exercise, physical relaxation, and stress reduction via multiple mechanisms of action. The disruption in access to such social settings, activities, and roles probably also increases loneliness, worry about the future, and various negative appraisals. Ordinary cultural and community practices related to loss and grief, spiritual practice and belief, medical care, elder support, family relationships, developmental milestones, and mutual aid have been interrupted by the limitation in face-to-face contact and communication that is the bedrock for many of these practices.
The impact of the pandemic serves to draw attention to the role of such institutions and practices in helping individuals and groups tolerate distress and adapt to adversity, and underlines the need for more research into these processes, as well as their increased incorporation into larger scale mental health interventions. In the face of such disruption of the natural social ecology of coping, wellbeing, and resilience, there has been widespread use of social media and videoconferencing technologies to facilitate social contact at a distance and enable continued participation in social activities and cultural rituals. However, little is known about the protective and supportive impact of this use, or the effects of deliberate therapeutic efforts to increase access using remote technologies. While encouragement of participation in a wide range of social settings and activities in creative ways that are consistent with public health safety recommendations is certainly to be recommended in the face of the COVID-19 pandemic, this approach to intervention requires significant research and evaluation efforts.
As technology is increasingly utilized to provide clinical care while maintaining public health, ideal primary interventions will include Internet-based treatment and mobile mental health apps that reach broad segments of the population at relatively low cost along with traditionally underserved populations who are disproportionately affected by the pandemic (e.g., migrant workers). These tools add to established (e.g., e.g., National Domestic Violence Hotline, Veterans Crisis Hotline) and newly developed telephone hotlines that are now being widely used for pandemic-related stressors and outcomes in select populations (e.g., healthcare workers: Geoffroy et al., 2020) and nation-wide (e.g., Hermida, Santolaya, & García-Vera, 2020). Goals of digital self-management tools can include psychoeducation, assessment and monitoring of mental health symptoms (including provision of tailored feedback and recommendations for when to seek a higher level of care), skills training (e.g., mindfulness, problem solving, cognitive restructuring), and support (e.g., via peers, artificial intelligence). While the effectiveness of most mental health apps is unknown, some organizations have developed rating and evaluation systems that can be helpful for directing consumers, clinicians, and organizations to tools with demonstrated effectiveness (www.psyberguide.org). Dissemination via academic partnerships would be ideal, though, non-profit organizations, healthcare systems, and government public health departments could all disseminate with low effort. Subscription based mental health apps with high credibility ratings from experts (e.g., Headspace, Calm, MoodMission) might help some people manage COVID-19-related stress and anxiety. Some apps have partnered with public libraries to offer library patrons free access to these phone-based mental health apps. Adequate engagement with Internet-based treatment and mobile mental health apps presents a challenge, with potential for high dropout, especially in the absence of social support for use.
Existing mobile and Internet-based health programs that target specific outcomes might be implemented as-is, or adapted to address pandemic-related outcomes in the context of ongoing risk. A new mobile app developed by the VA National Center for PTSD, COVID Coach, provides psychoeducation, self-care tools, emotional well-being tools, mental health monitoring, and goal setting tools. Community-wide and digital interventions ideally should be tailored to the pandemic and culturally, developed and modified with input and participation from the intended populations, and made easily accessible. Given the many challenges associated with developing, evaluating, and implementing mobile and Internet-based interventions, an ‘open source’ infrastructure for technology interventions could enable greater scale if housed in a reputable academic, government, or non-profit institution. Interventions could be easily and inexpensively developed, modified, shared and tested, with findings replicated by independent teams of researchers in different settings (Mohr, Riper, & Schueller, 2018).
Intervention intensity can be matched to hypothesized risk level for efficient use of scarce mental health resources, although for some, the intensity of needed treatment may vary over time. Low-intensity primary interventions may provide enough support for people experiencing mild and transient outcomes who can benefit from self-guided or minimally assisted psychoeducation and coping skills training. For example, public health initiatives focused on virus containment could be augmented by mental health assessment and resource provision (e.g., integrated into contact tracing initiatives). With additional training, public health professionals might also be able to provide basic psychological first aid (see below) and/or other brief psychoeducation or other interventions. For selective or indicated groups, risk and outcomes should be assessed regularly to determine when more intense secondary interventions are needed. For example, interventions delivered by employee wellness programs and focused on intensive and active communication within hospitals may substantially reduce burnout and depression among healthcare workers on an intensive care unit (Quenot et al., 2012).
2.2. Secondary prevention
Secondary prevention includes screening, early identification and brief interventions that prevent the progression of distress and slow the incidence of disorder among populations. Assessment of risks and outcomes will be essential in the post-pandemic phase for identifying treatment need, which is expected to exceed the capacity of available mental health resources. Risk identification provides a clear and potentially early signal of treatment need, and can be used to tailor interventions to populations, for example, through application of risk indices that can be developed from systematic data collection (e.g., via research, healthcare, contact-tracing) throughout and after the pandemic.
Virus exposure and movement restrictions are likely to increase risk among most people, and economic hardship will impact many people in countries with prolonged periods of infection and resulting movement restrictions. Factors such as severe infection that require mechanical ventilation, intimate partner violence and child abuse are especially potent stressors. Also potent are particular combinations of factors that increase risk exponentially. For example, a front-line healthcare worker who is continually exposed to death resulting from difficult triage decisions is likely to be at especially high risk of a negative outcome (de Pablo et al., 2020; Lai et al., 2020). Rapid and repeated occurrence of a risk factor (e.g., infection resulting from exposure following a lift of shelter-in-place mandate) may impart a sense of powerlessness and loss of control that is likely to amplify risk of an outcome (Lamiani et al., 2017). Some factors will confer risk to more outcomes, and increase risk of a severe and functionally impairing outcome.
Co-occurring factors may accumulate risks of poor mental health, perhaps in a dose-response manner with a threshold at which a diagnosable disorder occurs. Most people will experience combinations of precipitating, potentiating and perpetuating risk factors over time. A risk factor may precipitate the occurrence of a second, more proximal risk factor. For example, substance use may increase for the unemployed and those working in occupations that place them at risk of exposure and infection. Risk factors may also potentiate other risks. For example, known exposure to the virus will be a potent risk factor for infection-related worry among those with pre-existing COPD. Risk factors may perpetuate each other over time. For example, low socioeconomic status and pandemic-related economic hardship may perpetuate each other and result in increased likelihood of a negative mental health outcome. More generally, social determinants of health and social risk factors increase the likelihood of occurrence, potency and impact of pandemic stressors (see Fig. 1). Thus, it will be useful to proactively identify risk in structurally vulnerable populations as part of primary and secondary prevention. This can be done at initial points of care- emergency rooms, primary care, employee health and school clinic settings. as well as social welfare agencies. Ideally, this processes and results would be coordinated by an oversight body, such as a local public health department.
We hypothesize that low-risk groups include people with minimal exposure to infection, who continued to work in low-risk occupations during the pandemic, and/or who were able to manage movement restrictions with minimal disruptions. People at low risk may experience none, or acute and minor negative outcomes (e.g., increases in distress) that, for most, will subside as the pandemic wanes, but may still benefit from primary preventive measures (e.g., mobile health apps). Moderate-risk groups include people who contended with COVID-19 more directly (e.g., became ill, had an acquaintance who died), experienced significant isolation, faced major economic hardship, and/or whose pre-existing living and health conditions significantly increased stress. People at moderate risk who develop negative outcomes that persist after the acute phase of the pandemic may benefit from secondary interventions matched to their needs and designed to reduce progression of outcomes (e.g., brief evidence-based psychotherapies [EBPs]). Tertiary interventions (e.g., evidence-based psychotherapy) may be indicated those whose outcomes have progressed to a diagnosable disorder. High-risk groups include people who were hospitalized with COVID-19, had a loved one die, worked in high-risk occupations (e.g., healthcare workers), and experienced multiple risk factors. People at high risk may develop outcomes that are severe, lasting, and require established, evidence-based tertiary interventions.
Mapping common trajectories of risk and outcomes over time will facilitate identification and prediction of people at-risk of immediate vs. longer term outcomes, mild vs. severe outcomes, and outcomes that increase risk for more severe outcomes (e.g., burnout leading to a major depressive episode). This will require extensive data, and collaboration between clinicians, researchers, and organizations (e.g., healthcare systems) that come into contact with at-risk people. This knowledge can be used to maximize the timeliness and effectiveness of interventions and guide resource allocation at the population-level. It will be useful to understand why some at-risk people do not develop negative outcomes (Chen & Bonanno, 2020) and the protective factors that lessen the likelihood of such outcomes. Given that mental and physical health are closely linked, research examining risks and outcomes would benefit from assessing physical health, along with overall functioning and well-being.
We hypothesize that some risk factors (e.g., severe infection, death of a spouse) will independently or together be related to outcomes strongly enough to serve as a screening tool for negative outcomes and treatment need (Wald, Hackshaw, & Frost, 1999). A broadly applied risk factor checklist may prove useful in this regard (McLean & Cloitre, 2020; Taylor et al., 2020). Risk factors (and outcomes) might also be targeted by mental health surveillance systems based on electronic medical records (Oliva et al., 2017), and included in predictive models that can be leveraged for use in forecasting outcomes and allocating resources. Such systems address many limitations of existing population-based surveys while providing a basis for proactive identification and treatment of at-risk people, especially those already engaged in public and private health care systems. Though, additional efforts will be needed to collect data from people not actively receiving healthcare, and surveys will still be useful in this regard (e.g., administered at food-banks and other agencies providing resources to people impacted by the pandemic).
Systematic and empirically grounded assessments of risk and outcome facilitate early interventions to mitigate risk before more substantial and costly treatment becomes necessary. For example, Psychological First Aid (PFA) (Brymer et al., 2006) is recommended by experts in the immediate aftermath of a disaster (Hobfoll et al., 2007), and for particular populations (e.g., medically frail people; Vernberg et al., 2008). PFA has been adapted for use with Ebola virus disease outbreaks (World Health Organization et al., 2014) and more recently, COVID-19 (International Federation of Red Cross and Red Crescent Societies, 2020) and is similar to Stress First Aid (SFA), which was developed for those in high-risk occupations and has been applied in occupational settings to help staff manage ongoing stress related to the pandemic. If also adapted for delivery from a distance, PFA or SFA might be applied at relatively low-cost to treat pandemic-related mental health impact, while collecting effectiveness data. PFA and SFA can be delivered in multiple settings, thru health insurance programs, in school and workplace settings, in the field during disasters, and congregate settings where unhoused people reside.
Populations experiencing elevated distress may benefit from brief interventions that can be delivered online. There are now numerous services (e.g., Talkspace, 7 cups, WeChat) that connect individuals with trained counselors online. Several research groups have developed and are currently evaluating the effects of brief (1–4 session) online mindfulness and cognitive behavioral therapy (CBT) interventions to target stress and anxiety related to COVID-19 (e.g., Bäuerle et al., 2020; Mullarkey et al., 2020; Pizzoli, Marzorati, Mazzoni, & Pravettoni, 2020). Online interventions that are self-administered can more easily be scaled up to meet the mental health needs of large numbers of people than those requiring human facilitation.
Selected populations who have or are at risk for a mental disorder may benefit from brief EBPs that can be delivered by trained allied or paraprofessionals in settings where vulnerable patients/clients are more likely to access care, such as non-profit organizations and in faith community settings. Brief EBPs have lower drop out than standard EBPs, making them more acceptable and scalable. For example, delivering brief treatment in primary care or emergency rooms can greatly increase access to effective treatment and serve as a bridge to specialty care for those with greater needs (Cigrang et al., 2011).
CBT early interventions are a type of EBP for treating mental health symptoms, for example, reducing PTSD symptoms shortly after traumatic events (Giummarra, Lennox, Dali, Costa, & Gabbe, 2018; International Society for Traumatic Stress Studies, 2019). Early interventions can be utilized as both secondary and tertiary interventions, though they are likely to require adaptations to address issues associated with COVID-19, and relatively few practitioners implement these interventions. Thus, large-scale training and consultation for practitioners will be needed to increase access to and scalability of these services.
PFA and SFA and early, brief, and full EBPs can be administered via digital or tele-mental health (TMH) programs, which have the benefit of addressing limitations of in-person mental health care, such as limited availability of providers who deliver evidence-informed interventions which is a particular problem in rural and low- and middle-income areas (Ebert, Cuijpers, Muñoz, & Baumeister, 2017; Ruzek & Yeager, 2019). Internet-based interventions for secondary (and tertiary prevention) may be self-directed or human-supported by clinicians or paraprofessional “coaches.” Internet-delivered CBT has a growing evidence base (e.g., for PTSD: Kuester, Niemeyer, & Knaevelsrud, 2016), with effect sizes comparable to face-to-face CBT, though evidence of better quality is needed (Andrews et al., 2018). Providing needed technological support to people unfamiliar with this technology (e.g., elderly adults) may reduce costs in the long-term. A lack of broadband internet and personal computers that will limit access for segments of the population including those with limited economic means can be addressed by increasing privacy and security in public spaces with these resources (e.g., libraries). Nevertheless, adaptations to these treatments could result in delivery in community settings by trained allied professionals, substantially increasing reach. Strategic partnerships between academic institutions and the non-profit sector could also increase reach by disseminating trainees to more diverse settings.
2.3. Tertiary prevention
Tertiary prevention includes relatively intensive evidence-based interventions shown to improve functioning and reduce the consequences of mental disorders on quality of life. High intensity treatments will be needed for people with persistent and/or severe outcomes, who develop and maintain mental disorders, and who do not respond to lower-level interventions. High intensity treatments include full EBPs, psychopharmacology, and in the most severe cases intensive outpatient programs and in-patient residential treatment programs. The frequent contact and physical proximity of participants and providers in these programs may put them at increased risk for infection, necessitating significant adaptation to program procedures to maintain patient safety. Those identified as needing high intensity care should be connected to traditional mental health services (i.e., individual psychotherapy) as early as possible. Tertiary interventions could be made available thru employee, veteran, public, and tribal health care plans. Since US based insurance often caps the number of visits, public policy changes are needed to allow for extended mental health coverage.
Full EBPs, most of which are CBTs, have extensive evidence supporting their use for most disorders expected to occur as result of the pandemic (Butler, Chapman, Forman, & Beck, 2006), including EBPs for depression (Beck & Beck, 1995), PTSD (Foa et al., 2018), generalized anxiety disorder (e.g., (Robichaud, Koerner, & Dugas, 2019), illness anxiety disorder (Salkovskis, Warwick, & Deale, 2003), insomnia disorder (Edinger & Carney, 2014), complicated grief (Wittouck, Van Autreve, De Jaegere, Portzky, & van Heeringen, 2011), suicidality (Zalsman et al., 2016), and moral injury (Litz et al., 2009). Condensing treatment to daily sessions has recently been found effective (Foa et al., 2018).
Most evidence-based mental health interventions and especially EBPs, which are well integrated into mental health systems and have demonstrated efficacy for specific disorders, are designed for in-person delivery to individuals. Yet, existing challenges to recruiting people into treatment, high dropout rates and cost and limited scalability, and pandemic-related movement restriction make in-person treatment contraindicated. Fortuitously, EBPs have increasingly been tested and delivered in new ways (e.g., TMH and Internet treatments). Randomized clinical trials demonstrate that EBPs delivered using TMH are as effective as traditional in-person services (e.g., PTSD: Morland et al., 2014) in terms of outcomes and therapeutic alliance (Gros, Lancaster, López, & Acierno, 2018). TMH interventions have been found effective when delivered in real-world settings at large scale (Gilbody et al., 2017; Ruzek, Kuhn, Jaworski, Owen, & Ramsey, 2016), and were rapidly adopted for use in response to the COVID-19 pandemic (Ferguson et al., 2020; Pierce, Perrin, Tyler, McKee, & Watson, 2021). TMH includes video-teleconferencing, telephone support, and adjunctive tools such as text messaging. TMH can be delivered directly in clients' homes though any Internet-connected device. Promoting health equity in TMH dissemination and identifying and implementing means by which to increase access are pivotal to these efforts. For example, digital apothecaries - online repositories of evidence-based digital interventions (i.e., Massive Open Online Interventions) - hosted in multiple languages provide evidence-based care targeted to vulnerable populations including non-English speaking and indigenous peoples (Muñoz, Pineda, & Llamas, 2019).
Many barriers to provider uptake including logistical barriers (e.g., access to equipment, HIPAA-compliant platforms), privacy and safety concerns, and worries about impact on the client-therapist relationship (Gershkovich et al., 2016) have been overcome by necessity due to restrictions on movement and contact. Early adopters of telehealth, such as the VA, relatively swiftly transitioned to facilitate continuity of care (Rosen et al., 2020). A critical barrier to access was lifted when, at the outset of the pandemic, insurance companies agreed to reimburse telehealth at the same rate as in-person services. We suspect that high rates of TMH use will persist after the pandemic has subsided, and benefit many at-risk groups (e.g., those with limited mobility or residing in rural communities; Nagata, 2021). To the extent they have the ability to provide in-person contact, clinicians may choose to do so with people at-risk of and suffering from outcomes due to movement restrictions and its consequences (e.g., intimate partner violence). Where TMH is utilized, providers and systems should prioritize EBP protocols in order to achieve tertiary intervention goals such as improving functioning and reducing the impact of mental illness on quality of life. Further, providers may prioritize brief or condensed EBPs (i.e., daily sessions) to accelerate recovery and free up capacity to initiate care with new patients. Providers may also consider using transdiagnostic EBPs that can efficiently address multiple related outcomes concurrently. Clinicians, organizations, and governments should systematically assess outcomes in their treated clients/patients using validated measures (e.g., SAMHSA, 2020; also see Scott & Lewis, 2015) to ensure their beneficial impact for patients.
We must keep in mind that the availability of evidence-based treatments such as EBPs is currently so limited that they are unlikely to make a significant impact at the population level without substantial scaling. Thus, we will need to increase reach while maintaining (or increasing) the effectiveness of interventions for particular populations. We will need to substantially enlarge our population of providers to scale interventions to effectively target the large population with primary prevention needs and the smaller populations with secondary and tertiary needs who require more intensive treatments. In the United States, multiple provider types/professions engage in activities designed to support mental health and alleviate mental disorders and symptoms. Licensed clinical providers (e.g., psychotherapists, psychiatrists, licensed counselors) are likely needed only for tertiary preventive interventions and a limited set of secondary prevention interventions (e.g., brief EBPs). To meet the mental health needs of the population following the pandemic, it will be critical to scale-up the workforce and deploy professionals with various levels of training in mental health. For primary and secondary interventions, trained allied professionals, clergy members, mental health research staff, and public health professionals could provide supportive services, which will be the extent of need for many at-risk people. For example, peer-support specialists and health and wellness coaches can mitigate negative mental and physical health outcomes through psycho-social support and by facilitating self-care behaviors designed to reduce stress (Azevedo et al., 2020; Long, Howells, Peters, & Blakemore, 2019; Lungu, Boone, Chen, Chen, & Walser, 2020). Many of these professionals have the clinical acumen, workplace experience, and local connections necessary for deployment as supportive providers in their respective organizations. Even trained laypersons might act as service providers, for example, through “task sharing” (Patel et al., 2007; Rahman et al., 2016) focused on enabling people to better manage COVID-19 adversity. Needed, though, are training initiatives for paraprofessionals to deliver pandemic-related supportive services (e.g., PFA, suicide prevention, motivational interviewing) and to facilitate integration of internet-based treatments and mobile mental health apps into care and manage security and privacy concerns (Schueller, Washburn, & Price, 2016).
Even institutions that promote extensive EBP use, such as the Veterans Health Administration (VHA), recognize the profound importance of religious and spiritual communities in health and wellbeing. Most VHA medical centers, as well as many US medical centers, have a chapel and chaplains representing multiple faith communities which are trained to provide emotional and social support in times of crisis, especially in dealing with grief and loss. Collaborative public mental health efforts that provide education and support to chaplains and members of faith communities is key to not only adapting religious rituals so people can safely memorialize those who have passed but it also lays the groundwork for cooperation between public health departments and religious institutions which have for centuries cared for its members in hard times thru culturally syntonic rituals.
As we apply interventions in standard ways to new populations, and in non-standard ways to meet the needs of populations as they change over time it will be essential to systematically collect data on intervention effectiveness and implementation and dissemination (see Curran, Bauer, Mittman, Pyne, & Stetler, 2012). Frameworks and tools that guide effective implementation and scaling efforts are available (e.g., www.re-aim.org).
3. Conclusions
Countless people will suffer a negative mental health outcome due to COVID-19, with already vulnerable and underserved populations at disproportionate risk. Data and research are needed to identify the multiple pathways through which risks contribute to a diversity of outcomes among various populations. Tailoring preventive interventions to populations based on their needs will allow us to most effectively allocate limited resources to alleviate the substantial mental health impact of COVID-19. This will require strong interdisciplinary partnerships among policy makers, administrators, researchers and practitioners in the fields of health services, public health and epidemiology, and mental health (clinical psychology, psychiatry, social work, and allied professions) to implement interventions at the scale of the global need. The pandemic presents unprecedented opportunities to implement stepped-care models of intervention that step patients up to higher levels of care, and lower levels of care, based on their needs. Though non-traditional models of care delivery are often utilized for clinicians working with vulnerable populations, not much supporting evidence has been gained. Traditional models, where EBTs are delivered in-person, by a trained expert, at a specialty care location have proved difficult to scale (Kazdin, 2017). As such, ongoing evaluation of intervention implementation (e.g., pragmatic program evaluation) and effectiveness (e.g., measurement-based care) will be critical to refining our efforts to increase the reach of intervention resources and to improve our understanding of how best to respond to future pandemics. Now is the time to mobilize communities and populations to mitigate a forthcoming pandemic of negative mental health.
Declaration of competing interest
Dr. Boden consulted for Beneath the Surface Foundation. Dr. Zimmerman received funding as principal investigator from the National Institute on Drug Abuse (R21DA04219801; R01DA046651) and VA Health Services Research and Development (I0X002521). Dr. McLean received funding from the Department of Defense (W81XWH-17-C-0236).
Acknowledgements
We thank Susanna Martins, Suzanne Tamang and Clara Dismuke-Greer for providing guidance and feedback. The views expressed here do not necessarily represent those of the Department of Veterans Affairs or any other U.S. government agency or entity.
References
- Adelman R.D., Tmanova L.L., Delgado D., Dion S., Lachs M.S. Caregiver burden: A clinical review. Jama. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- Alon T.M., Doepke M., Olmstead-Rumsey J., Tertilt M. The impact of COVID-19 on gender equality (No. w26947) National Bureau of Economic Research. 2020 [Google Scholar]
- Alzueta E., Perrin P., Baker F.C., Caffarra S., Ramos-Usuga D., Yuksel D., Arango-Lasprilla J.C. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. Journal of Clinical Psychology. 2021;77:556–570. doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M., McEvoy P., English C., Newby J. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: An updated meta-analysis. Journal of Anxiety Disorders. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Arno P.S., House J.S., Viola D., Schechter C. Social security and mortality: The role of income support policies and population health in the United States. Journal of Public Health Policy. 2011;32(2):234–250. doi: 10.1057/jphp.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azevedo K.J., Ramirez J.C., Kumar A., LeFevre A., Factor A., Hailu E.…Jain S. Rethinking violence prevention in rural and underserved communities: How veteran peer support groups help participants deal with sequelae from violent traumatic experiences. The Journal of Rural Health. 2020;36(2):266–273. doi: 10.1111/jrh.12362. [DOI] [PubMed] [Google Scholar]
- Bagcchi S. Stigma during the COVID-19 pandemic. The Lancet Infectious Diseases. 2020;20(7):782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker M.G. Nonrelocatable occupations at increased risk during pandemics: United States, 2018. American Journal of Public Health. 2020;110(8):1126–1132. doi: 10.2105/AJPH.2020.305738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bäuerle A., Graf J., Jansen C., Musche V., Schweda A., Hetkamp M.…Skoda E.M. E-mental health mindfulness-based and skills-based “CoPE it” intervention to reduce psychological distress in times of COVID-19: Study protocol for a bicentre longitudinal study. BMJ Open. 2020;10(8) doi: 10.1136/bmjopen-2020-039646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck J.S., Beck A.T. Guilford Press New York; 1995. Cognitive therapy: Basics and beyond. [Google Scholar]
- Bienvenu O.J., Friedman L.A., Colantuoni E., Dinglas V.D., Sepulveda K.A., Mendez-Tellez P.…Needham D.M. Psychiatric symptoms after acute respiratory distress syndrome: A 5-year longitudinal study. Intensive Care Medicine. 2018;44(1):38–47. doi: 10.1007/s00134-017-5009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden M. 2020. Estimating the mental health impact of COVID19 on United States Populations. [cited 2020 Sep 19]; Available from: https://osf.io/ytd92. [Google Scholar]
- Boniol M., McIsaac M., Xu L., Wuliji T., Diallo K., Campbell J. World Health Organization; Geneva: 2019. Gender equity in the health workforce: Analysis of 104 countries. Working paper 1. (WHO/HIS/HWF/Gender/WP1/2019.1). License: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. American Journal of Emergency Medicine. 2020;38:2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Egerter S., Williams D.R. The social determinants of health: Coming of age. Annual Review of Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Braveman P., Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Reports. 2014;129(supplement 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin W. Age differences in COVID-19 risk perceptions and mental health: Evidence from a national US survey conducted in March 2020. The Journals of Gerontology: Series B. 2021;76(2):e24–e29. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant D.J., Oo M., Damian A.J. The rise of adverse childhood experiences during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S193–S194. doi: 10.1037/tra0000711. [DOI] [PubMed] [Google Scholar]
- Brymer M., Layne C., Jacobs A., Pynoos R., Ruzek J., Steinberg A.…Watson P. 2006. Psychological first aid field operations guide. (National Child Traumatic Stress Network) [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. International Journal of Clinical and Health Psychology. 2020;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler A.C., Chapman J.E., Forman E.M., Beck A.T. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Campbell J.C. Health consequences of intimate partner violence. The Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- CDC Policy resources to support SDOH. 2021, February 11. https://www.cdc.gov/socialdeterminants/policy/index.htm
- Chen S., Bonanno G.A. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychological Trauma Theory Research Practice and Policy. 2020;12(S1):S51. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- Cheung Y., Chau P.H., Yip P.S. A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. International Journal of Geriatric Psychiatry: A Journal of the Psychiatry of Late Life and Allied Sciences. 2008;23(12):1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Cigrang J.A., Rauch S.A., Avila L.L., Bryan C.J., Goodie J.L., Hryshko-Mullen A., Peterson A.L. Treatment of active-duty military with PTSD in primary care: Early findings. Psychological Services. 2011;8(2):104–113. [Google Scholar]
- Cooke J.E., Eirich R., Racine N., Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Research. 2020;292:113347. doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper M.L., Frone M.R., Russell M., Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69(5):990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Curran G.M., Bauer M., Mittman B., Pyne J.M., Stetler C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care. 2012;50(3):217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R.…Czeisler C.A. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research. 2020 doi: 10.1016/j.jpsychires.2020.10.035. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’cruz M., Banerjee D. “An invisible human rights crisis”: The marginalization of older adults during the COVID-19 pandemic–an advocacy review. Psychiatry Research. 2020;292 doi: 10.1016/j.psychres.2020.113369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Hombres B., Rocco L., Suhrcke M., McKee M. Does social capital determine health? Evidence from eight transition countries. Health Economics. 2010;19(1):56–74. doi: 10.1002/hec.1445. [DOI] [PubMed] [Google Scholar]
- van Dorn A., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. The Lancet. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley D., Catalano R., Wilson G. Depression and unemployment: Panel findings from the Epidemiologic Catchment Area study. American Journal of Community Psychology. 1994;22(6):745–765. doi: 10.1007/BF02521557. [DOI] [PubMed] [Google Scholar]
- Dunham A.M., Rieder T.N., Humbyrd C.J. A bioethical perspective for navigating moral dilemmas amidst the COVID-19 pandemic. The Journal of the American Academy of Orthopaedic Surgeons. 2020;28:471–476. doi: 10.5435/JAAOS-D-20-00371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert D.D., Cuijpers P., Muñoz R.F., Baumeister H. Prevention of mental health disorders using internet-and mobile-based interventions: A narrative review and recommendations for future research. Frontiers in Psychiatry. 2017;8:1–16. doi: 10.3389/fpsyt.2017.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger J.D., Carney C.E. Oxford University Press; 2014. Overcoming insomnia: A cognitive-behavioral therapy approach, therapist guide. [Google Scholar]
- Elbogen E.B., Lanier M., Montgomery A.E., Strickland S., Wagner H.R., Tsai J. Financial strain and suicide attempts in a nationally representative sample of US adults. American Journal of Epidemiology. 2020;189(11):1266–1274. doi: 10.1093/aje/kwaa146. [DOI] [PubMed] [Google Scholar]
- Ferguson J., Jacobs J., Yefimova M., Greene L., Heyworth L., Zulman D. Virtual care expansion in the veterans health administration during the COVID-19 pandemic: Clinical services and patient characteristics associated with utilization. Journal of the American Medical Informatics Association. 2020;28(3):453–462. doi: 10.1093/jamia/ocaa284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Foa E.B., McLean C.P., Zang Y., Rosenfield D., Yadin E., Yarvis J.S.…Dondanville K.A. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. Jama. 2018;319(4):354–364. doi: 10.1001/jama.2017.21242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffroy P.A., Le Goanvic V., Sabbagh O., Richoux C., Weinstein A., Dufayet G., Lejoyeux M. Psychological support system for hospital workers during the Covid-19 outbreak: Rapid design and implementation of the Covid-Psy hotline. Frontiers in Psychiatry. 2020;11(511):1–8. doi: 10.3389/fpsyt.2020.00511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershkovich M., Herbert J.D., Glassman L.H., Ibrahim A., Forman E.M., Kaye J.L. Clinicians’ attitudes and experiences regarding telemental health services. The Behavior Therapist. 2016;39(1):14–20. [Google Scholar]
- Gilbody S., Brabyn S., Lovell K., Kessler D., Devlin T., Smith L.…Cooper C. Telephone-supported computerised cognitive–behavioural therapy: REEACT-2 large-scale pragmatic randomised controlled trial. The British Journal of Psychiatry. 2017;210(5):362–367. doi: 10.1192/bjp.bp.116.192435. [DOI] [PubMed] [Google Scholar]
- Giummarra M.J., Lennox A., Dali G., Costa B., Gabbe B.J. Early psychological interventions for posttraumatic stress, depression and anxiety after traumatic injury: A systematic review and meta-analysis. Clinical Psychology Review. 2018;62:11–36. doi: 10.1016/j.cpr.2018.05.001. [DOI] [PubMed] [Google Scholar]
- Gosangi B., Park H., Thomas R., Gujrathi R., Bay C.P., Raja A.S.…Harris M.B. Exacerbation of physical intimate partner violence during COVID-19 lockdown. Radiology. 2021;298:E38–E45. doi: 10.1148/radiol.2020202866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith A.K. Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. 2020:1–7. doi: 10.1007/s10896-020-00172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros D.F., Lancaster C.L., López C.M., Acierno R. Treatment satisfaction of home-based telehealth versus in-person delivery of prolonged exposure for combat-related PTSD in veterans. Journal of Telemedicine and Telecare. 2018;24(1):51–55. doi: 10.1177/1357633X16671096. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y.…Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R.B., Charles E.J., Mehaffey J.H. Socioeconomic status and coronavirus disease 2019 (COVID-19) related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermida J.R.F., Santolaya F., García-Vera M.P. The COVID-19 psychological helpline of the Spanish Ministry of Health and Spanish psychological association: Characteristics and demand. Revista Española de Salud Pública. 2020;94 [PMC free article] [PubMed] [Google Scholar]
- Hobfoll S.E., Watson P., Bell C.C., Bryant R.A., Brymer M.J., Friedman M.J.…Layne C.M. Five essential elements of immediate and mid–term mass trauma intervention: Empirical evidence. Psychiatry: Interpersonal and Biological Processes. 2007;70(4):283–315. doi: 10.1521/psyc.2007.70.4.283. [DOI] [PubMed] [Google Scholar]
- International Federation of Red Cross and Red Crescent Societies Remote Psychological First Aid during the COVID-19 outbreak. Interim guidance-March 2020. 2020. redcross.org.rs
- International Society for Traumatic Stress Studies . Chicago International Society for Traumatic Stress Studies; USA: 2019. Posttraumatic stress disorder prevention and treatment guidelines: Methodology and recommendations; p. 2019.https://istss.org/clinical-resources/treating-trauma/new-istss-prevention-and-treatment-guidelines Retrieved August 1, 2020, from. [DOI] [PubMed] [Google Scholar]
- Jin J.M., Bai P., He W., Wu F., Liu X.F., Han D.M.…Yang J.K. Gender differences in patients with COVID-19: Focus on severity and mortality. Frontiers in Public Health. 2020;8(152):1–6. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L., Hughes M., Unterstaller U. Post-traumatic stress disorder (PTSD) in victims of domestic violence: A review of the research. Trauma, Violence & Abuse. 2001;2(2):99–119. [Google Scholar]
- Kannampallil T.G., Goss C.W., Evanoff B.A., Strickland J.R., McAlister R.P., Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One. 2020;15(8) doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karren R., Karren R., Sherman K. Layoffs and unemployment discrimination: A new stigma. Journal of Managerial Psychology. 2012;27(8):848–863. [Google Scholar]
- Kazdin A.E. Addressing the treatment gap: A key challenge for extending evidence-based psychosocial interventions. Behaviour Research and Therapy. 2017;88:7–18. doi: 10.1016/j.brat.2016.06.004. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L.…Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kim H.H., Laurence J. COVID-19 restrictions and mental distress among American adults: Evidence from Corona impact survey (W1 and W2) Journal of Public Health. 2020;42(4):704–711. doi: 10.1093/pubmed/fdaa148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D., Stoddardt G. What is population health? American Journal of Public Health. 2003;93(3):380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen P., Dyregrov K., Dyregrov A., Heir T. Media exposure and prolonged grief: A study of bereaved parents and siblings after the 2011 Utøya Island terror attack. Psychological Trauma Theory Research Practice and Policy. 2016;8(6):661–668. doi: 10.1037/tra0000131. [DOI] [PubMed] [Google Scholar]
- Kuester A., Niemeyer H., Knaevelsrud C. Internet-based interventions for posttraumatic stress: A meta-analysis of randomized controlled trials. Clinical Psychology Review. 2016;43:1–16. doi: 10.1016/j.cpr.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N.…Li R. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam M.H.-B., Wing Y.-K., Yu M.W.-M., Leung C.-M., Ma R.C., Kong A.P.…Lam S.-P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Archives of Internal Medicine. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Lamiani G., Borghi L., Argentero P. When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. Journal of Health Psychology. 2017;22(1):51–67. doi: 10.1177/1359105315595120. [DOI] [PubMed] [Google Scholar]
- Lawson M., Piel M.H., Simon M. Child maltreatment during the covid-19 pandemic: Consequences of parental job loss on psychological and physical abuse towards children. Child Abuse & Neglect. 2020;110 doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Jobe M., Mathis A., Gibbons J. Incremental validity of Coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. Journal of Anxiety Disorders. 2020;74:102268. doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeb R.T., Lewis T., Zolotor A.J. A review of physical and mental health consequences of child abuse and neglect and implications for practice. American Journal of Lifestyle Medicine. 2011;5(5):454–468. [Google Scholar]
- Litz B.T., Stein N., Delaney E., Lebowitz L., Nash W.P., Silva C., Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review. 2009;29(8):695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J.…Wu P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long H., Howells K., Peters S., Blakemore A. Does health coaching improve health-related quality of life and reduce hospital admissions in people with chronic obstructive pulmonary disease? A systematic review and meta-analysis. British Journal of Health Psychology. 2019;24(3):515–546. doi: 10.1111/bjhp.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long H., Stein J. Washington Post; 2021, February 9. Here’s the new democratic plan for $1,400 stimulus payments.https://www.washingtonpost.com/business/2021/02/03/biden-stimulus-checks-what-you-need-to-know/ Retrieved February 1, 2020, from. [Google Scholar]
- Lungu A., Boone M.S., Chen S.Y., Chen C.E., Walser R.D. Effectiveness of a cognitive behavioral coaching program delivered via video in real world settings. Telemedicine and E-Health. 2020;27 doi: 10.1089/tmj.2019.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S.…Smith M. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review. Annals of Internal Medicine. 2020 doi: 10.7326/M20-6306. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann F., Krueger R., Vohs K. Personal economic anxiety in response to COVID-19. Personality and Individual Differences. 2020;167:110233. doi: 10.1016/j.paid.2020.110233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsden J., Darke S., Hall W., Hickman M., Holmes J., Humphreys K.…West R. Mitigating and learning from the impact of COVID-19 infection on addictive disorders. Addiction. 2020;115(6):1007–1010. doi: 10.1111/add.15080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo T., Kobayashi D., Taki F., Sakamoto F., Uehara Y., Mori N., Fukui T. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Network Open. 2020;3(8):e2017271. doi: 10.1001/jamanetworkopen.2020.17271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlpine D., Alang S. Employment and economic outcomes of persons with mental illness and disability: The impact of the great recession in the United States. Psychiatric Rehabilitation Journal. 2020 doi: 10.1037/prj0000458. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- McLean C.P., Cloitre M. Unpublished Scale; 2020. Coronavirus stressor survey. [Google Scholar]
- Milat A.J., King L., Bauman A.E., Redman S. The concept of scalability: Increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promotion International. 2013;28(3):285–298. doi: 10.1093/heapro/dar097. [DOI] [PubMed] [Google Scholar]
- Miranda J., Bernal G., Lau A., Kohn L., Hwang W.C., LaFromboise T. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 2005;1:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra S., Le P.D., Goldmann E., Yang L.H. Psychological impact of anti-Asian stigma due to the COVID-19 pandemic: A call for research, practice, and policy responses. Psychological Trauma Theory Research Practice and Policy. 2020;12(5):461–464. doi: 10.1037/tra0000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., Riper H., Schueller S.M. A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry. 2018;75:113–114. doi: 10.1001/jamapsychiatry.2017.3838. [DOI] [PubMed] [Google Scholar]
- Moring J., Dondanville K., Fina B., Hassija C., Chard K., Monson C.…Resick P. Cognitive processing therapy for posttraumatic stress disorder via telehealth: Practical considerations during the COVID-19 pandemic. Journal of Traumatic Stress. 2020;33:371–379. doi: 10.1002/jts.22544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland L.A., Mackintosh M.A., Greene C.J., Rosen C.S., Chard K.M., Resick P., Frueh B.C. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: A randomized noninferiority clinical trial. The Journal of Clinical Psychiatry. 2014;75(5):470–476. doi: 10.4088/JCP.13m08842. [DOI] [PubMed] [Google Scholar]
- Mucci N., Traversini V., Giorgi G., Tommasi E., De Sio S., Arcangeli G. Migrant workers and psychological health: A systematic review. Sustainability. 2019;12(1):1–28. [Google Scholar]
- Mullarkey M.C., Dobias M., Sung J., Shumake J., Beevers C.G., Schleider J.L. Unpublished manuscript; 2020. A scalable, single session intervention for perceived control over anxiety during COVID-19.https://psyarxiv.com/qp7c2 Retrieved December 3, 2020, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz R.F., Pineda B.S., Llamas J.A. Indigeneity, diversity, and equity in internet interventions: Could ISRII contribute to making health care a universal human right? Internet Interventions. 2019;18(100269):1–9. doi: 10.1016/j.invent.2019.100269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata J. Rapid scale-up of telehealth during the COVID-19 pandemic and implications for subspecialty care in rural areas. The Journal of Rural Health. 2021;37(1):145. doi: 10.1111/jrh.12433. [DOI] [PubMed] [Google Scholar]
- Narasimha V.L., Shukla L., Mukherjee D., Menon J., Huddar S., Panda U.K.…Murthy P. Complicated alcohol withdrawal—An unintended consequence of COVID-19 lockdown. Alcohol and Alcoholism. 2020;55(4):350–353. doi: 10.1093/alcalc/agaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund J.A., Aschbrenner K.A., Marsch L.A., Bartels S.J. The future of mental health care: Peer-to-peer support and social media. Epidemiology and Psychiatric Sciences. 2016;25(2):113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neelam K., Duddu V., Anyim N., Neelam J., Lewis S. Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, Behavior, & Immunity - Health. 2020;100177 doi: 10.1016/j.bbih.2020.100177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson A. Unequal treatment: Confronting racial and ethnic disparities in health care. Journal of the National Medical Association. 2002;94(8):666–668. [PMC free article] [PubMed] [Google Scholar]
- Newman M.G., Llera S.J. A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry. Clinical Psychology Review. 2011;31(3):371–382. doi: 10.1016/j.cpr.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novacek D., Hampton-Anderson J., Ebor M., Loeb T., Wyatt G. Mental health ramifications of the COVID-19 pandemic for black Americans: Clinical and research ramifications. Psychological Trauma Theory Research Practice and Policy. 2020;12(5):449–451. doi: 10.1037/tra0000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva E.M., Bowe T., Tavakoli S., Martins S., Lewis E.T., Paik M.…Avoundjian T. Development and applications of the veterans health Administration’s stratification tool for opioid risk mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychological Services. 2017;14(1):34–49. doi: 10.1037/ser0000099. [DOI] [PubMed] [Google Scholar]
- Omary L. The COVID-19 pandemic mental health crisis ahead. Journal of Rural Mental Health. 2020;44(4):274–275. [Google Scholar]
- de Pablo G.S., Serrano J.V., Catalan A., Arango C., Moreno C., Ferre F.…Fusar-Poli P. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. Journal of Affective Disorders. 2020;275:48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page K.R., Venkataramani M., Beyrer C., Polk S. Undocumented US immigrants and Covid-19. New England Journal of Medicine. 2020;382(21) doi: 10.1056/NEJMp2005953. [DOI] [PubMed] [Google Scholar]
- Park J.-S., Lee E.-H., Park N.-R., Choi Y.H. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Archives of Psychiatric Nursing. 2018;32(1):2–6. doi: 10.1016/j.apnu.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Araya R., Chatterjee S., Chisholm D., Cohen A., Silva M.…van Ommeren M. Treatment and prevention of mental disorders in low-income and middle-income countries. The Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- Petterson S., Westfall J.M., Miller B.F. Well Being Trust; 2020. Projected deaths of despair from COVID-19.https://wellbeingtrust.org/wp-content/uploads/2020/05/WBT_Deaths-of-Despair_COVID-19-FINAL-FINAL.pdf Retrieved October 29, 2020, from. [Google Scholar]
- Pierce B., Perrin P., Tyler C., McKee G., Watson J. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. American Psychologist. 2021;76(1):14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- Pizzoli S.M.F., Marzorati C., Mazzoni D., Pravettoni G. An internet-based intervention to alleviate stress during social isolation with guided relaxation and meditation: Protocol for a randomized controlled trial. JMIR Research Protocols. 2020;9(6) doi: 10.2196/19236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primm A.B., Vasquez M.J., Mays R.A., Sammons-Posey D., McKnight-Eily L.R., Presley-Cantrell L.R.…Perry G.S. The role of public health in addressing racial and ethnic disparities in mental health and mental illness. Preventing Chronic Disease: Public Health Research, Practice, and Policy. 2010;7(1):A20. [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33(2):1–3. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quenot J.-P., Rigaud J.-P., Prin S., Barbar S., Pavon A., Hamet M.…Charles P.E. Suffering among carers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Medicine. 2012;38(1):55–61. doi: 10.1007/s00134-011-2413-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Hamdani S.U., Awan N.R., Bryant R.A., Dawson K.S., Khan M.F.…Chiumento A. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: A randomized clinical trial. Jama. 2016;316(24):2609–2617. doi: 10.1001/jama.2016.17165. [DOI] [PubMed] [Google Scholar]
- Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from covid-19 by race/ethnicity and income. American Journal of Preventive Medicine. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.…Manthey J. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug and Alcohol Review. 2020;39(4):301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rettie H., Daniels J. Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. American Psychologist. 2020 doi: 10.1037/amp0000710. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Robichaud M., Koerner N., Dugas M.J. Routledge; 2019. Cognitive behavioral treatment for generalized anxiety disorder: From science to practice. [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P.…David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen C.S., Morland L.A., Glassman L.H., Marx B.P., Weaver K., Smith C.A.…Schnurr P.P. Virtual mental health care in the veterans health Administration’s immediate response to coronavirus disease-19. The American Psychologist. 2020;76:26–38. doi: 10.1037/amp0000751. [DOI] [PubMed] [Google Scholar]
- Rosen J.B., Schulkin J. From normal fear to pathological anxiety. Psychological Review. 1998;105(2):325–350. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- Ruzek J.I., Kuhn E., Jaworski B.K., Owen J.E., Ramsey K.M. Mobile mental health interventions following war and disaster. Mhealth. 2016;2(37):1–11. doi: 10.21037/mhealth.2016.08.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruzek J.I., Yeager C.M. Mobile mental health interventions for trauma survivors. MHealth. 2019;5(9):1–5. doi: 10.21037/mhealth.2019.02.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M.…Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno J.P., Williams N.D., Gattamorta K.A. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychological Trauma Theory Research Practice and Policy. 2020;12(S1):S239–S242. doi: 10.1037/tra0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M., Warwick H.M., Deale A.C. Cognitive-behavioral treatment for severe and persistent health anxiety (hypochondriasis) Brief Treatment and Crisis Intervention. 2003;3(3):353–367. [Google Scholar]
- SAMHSA . SAMHSA-HRSA Center for Integrated Health Solutions; 2020. Screening tools.https://www.integration.samhsa.gov/clinical-practice/screening-tools Retrieved May 4, 2020, from. [Google Scholar]
- Schneider D., Harknett K., McLanahan S. Intimate partner violence in the great recession. Demography. 2016;53(2):471–505. doi: 10.1007/s13524-016-0462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider W., Waldfogel J., Brooks-Gunn J. The great recession and risk for child abuse and neglect. Children and Youth Services Review. 2017;72:71–81. doi: 10.1016/j.childyouth.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schueller S.M., Washburn J.J., Price M. Exploring mental health providers’ interest in using web and mobile-based tools in their practices. Internet Interventions. 2016;4:145–151. doi: 10.1016/j.invent.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K., Lewis C.C. Using measurement-based care to enhance any treatment. Cognitive and Behavioral Practice. 2015;22(1):49–59. doi: 10.1016/j.cbpra.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden L.R., Yamada A.M. Cultural differences in access to care. Annual Review of Clinical Psychology. 2005;1:143–166. doi: 10.1146/annurev.clinpsy.1.102803.143846. [DOI] [PubMed] [Google Scholar]
- Spagnolo P.A., Montemitro C., Leggio L. New challenges in addiction medicine: COVID-19 infection in patients with alcohol and substance use disorders—The perfect storm. American Journal of Psychiatry. 2020;177(9):805–807. doi: 10.1176/appi.ajp.2020.20040417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack, E., Leichtling, G., Larsen, J. E., Gray, M., Pope, J., Leahy, J. M., … Korthuis, P. T. (2020). The impacts of COVID-19 on mental health, substance use, and overdose concerns of people who use drugs in rural communities. Journal of Addiction Medicine. Advanced online publication. [DOI] [PMC free article] [PubMed]
- Taha S., Matheson K., Cronin T., Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. British Journal of Health Psychology. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30462-4. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37(8):706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. Mental distress among U.S. adults during the COVID-19 pandemic. Journal of Clinical Psychology. 2020;76(12):2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations COVID-19 and the need for action on mental health. 2020, May 13. https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf Retrieved November 16, 2020, from.
- Van Mol M.M., Kompanje E.J., Benoit D.D., Bakker J., Nijkamp M.D. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernberg E.M., Steinberg A.M., Jacobs A.K., Brymer M.J., Watson P.J., Osofsky J.D.…Ruzek J.I. Innovations in disaster mental health: Psychological first aid. Professional Psychology: Research and Practice. 2008;39(4):381–388. [Google Scholar]
- Wald N., Hackshaw A., Frost C. When can a risk factor be used as a worthwhile screening test? Bmj. 1999;319(7224):1562–1565. doi: 10.1136/bmj.319.7224.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace C.L., Wladkowski S.P., Gibson A., White P. Grief during the COVID-19 pandemic: Considerations for palliative care providers. Journal of Pain and Symptom Management. 2020;60(1):e70–e76. doi: 10.1016/j.jpainsymman.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells S.Y., Morland L.A., Wilhite E.R., Grubbs K.M., Rauch S.A., Acierno R., McLean C.P. Delivering prolonged exposure therapy via videoconferencing during the COVID-19 pandemic: An overview of the research and special considerations for providers. Journal of Traumatic Stress. 2020;33(4):380–390. doi: 10.1002/jts.22573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. COVID-19: The gendered impacts of the outbreak. The Lancet. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Purdie-Vaughns V. In: Population health: Behavioral and social science insights. Kaplan R.M., Spittel M.L., David D.H., editors. Agency for Healthcare Research and Quality, National Institutes of Health; Rockville, MD: 2015. Social and behavioral interventions to improve health and reduce disparities in health; pp. 51–66. [Google Scholar]
- Witteveen D., Velthorst E. Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences. 2020;117(44):27277–27284. doi: 10.1073/pnas.2009609117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittouck C., Van Autreve S., De Jaegere E., Portzky G., van Heeringen K. The prevention and treatment of complicated grief: A meta-analysis. Clinical Psychology Review. 2011;31(1):69–78. doi: 10.1016/j.cpr.2010.09.005. [DOI] [PubMed] [Google Scholar]
- World Health Organization Policy brief: COVID-19 and the need for action on mental health. 2020. https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf Retrieved February 11, 2021, from.
- World Health Organization, CBM, World Vision International, UNICEF . WHO; Geneva: 2014. Psychological first aid during Ebola virus disease outbreaks (provisional version)https://apps.who.int/iris/bitstream/handle/10665/144725/9789241548977_eng.pdf?sequence=1 September 2014. Retrieved July 16, 2020, from. [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) Journal of Traumatic Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L.…McIntyre R. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorder. 2020;277(1):55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- Yue J.L., Yan W., Sun Y.K., Yuan K., Su S.Z., Han Y.…Bullmore E. Mental health services for infectious disease outbreaks including COVID-19: A rapid systematic review. Psychological Medicine. 2020;50:2498–2513. doi: 10.1017/S0033291720003888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalsman G., Hawton K., Wasserman D., van Heeringen K., Arensman E., Sarchiapone M.…Balazs J. Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry. 2016;3(7):646–659. doi: 10.1016/S2215-0366(16)30030-X. [DOI] [PubMed] [Google Scholar]
- Zvolensky M.J., Garey L., Rogers A.H., Schmidt N.B., Vujanovic A.A., Storch E.A.…O’Cleirigh C. Psychological, addictive, and health behavior implications of the COVID-19 pandemic. Behaviour Research and Therapy. 2020;134:103715. doi: 10.1016/j.brat.2020.103715. [DOI] [PMC free article] [PubMed] [Google Scholar]