Highlights
-
•
Immediate surgical decompression and stabilization for spinal cord injury give significant improvement in motoric and sensory function.
-
•
Spinal cord injury usually not standing alone. It might be together with associated injuries, the most common is sacral fracture.
-
•
In managing a Covid-19 patient who needs immediate surgical treatment, we have to do the surgery effectively as possible to minimize the risk of viral exposure.
Keywords: Spinal cord injury, Sacral fracture, Covid-19
Abstract
Introduction and importance
Spinal cord injury is mostly caused by traumatic accident and usually associated with several injuries. The ideal treatment of orthopaedic injury is to perform surgical decompression and stabilization early.
Case presentation
A 24-year-old-male patient came in emergency department with history of severe pain in his thoracic vertebrae after fell from 10 m height. His buttock was hit the ground first and patient was alert. He felt hypoesthesia below the injured level and dysfunctional motor and sensory of both lower extremities. We put pedicle screw at the C7, Th1, Th2 and Th 3. Then we put rods and nuts. After that, we did decompression by laminectomy of the C7 and Th1 and we put vacuumed drain for the wound.
Clinical discussion
This patient was diagnosed with traumatic spinal cord injury of 1st thoracic vertebra ASIA Impairment Scale (AIS) C and sacral fracture Denis classification zone II of right side with confirmed Covid-19 case. First patient treated with 1000 mg methyl prednisolone. An early surgical treatment was open reduction and internal fixation (ORIF) sacral fracture. We put a two-hole 4.5 narrow dynamic compression plate (DCP) at the lateral side of posterior ridge of iliac bone, between posterior superior iliac spine (PSIS) and posterior inferior iliac spine (PIIS).
Conclusion
Immediate surgical decompression and stabilization for spinal cord injury give significant improvement in motor and sensory function. Appropriate management for Covid-19 patient with Favipiravir and some supplements, had been proved control the virus and give patient good quality of life.
1. Introduction
More than 90% of spinal cord injuries are caused by traumatic incident. Male patients are more common than female. Clinical outcome and prognosis are depend on the severity, location and early management [1].
Spinal cord injury usually not standing alone. It might be associated with other injuries. One of the associated injury was sacral fracture. In the management of the sacral fracture, we have to decide whether the pelvic ring was stable or not. In the future, we also have to decide whether the patient could be managed by non-operative treatment or must undergo surgery [2]. Appropriate management could save lives and had better outcome.
Nowadays, in the pandemic situation, surgeons are facing difficulties to manage multiple injuries patient with confirmed case of Covid-19. In an emergency case, surgeon needs to do immediate surgery without also being infected with SARS-CoV-2 [3]. We have to do surgery effectively as possible to minimize the risk of viral exposure.
2. Case presentation
A 24-years-old male was brought to emergency ward with chief complaint of severe pain on his thoracic vertebrae, pelvic and weakness of both lower extremities. Patient had history of fell down from 10 m height while he was going down from helicopter using a rappelling rope and harness 30 min before hospital admission. His buttock was hit the ground first. Patient was alert and has no lacerated wound. There was no drug history, family history including any relevant genetic information and psychosocial history.
His blood pressure was 102/62 mmHg, heart rate was 68 rpm, respiratory rate was 22 rpm. From physical examination we found that he felt hypoesthesia below the injured level, dysfunctional motoric and sensory of both lower extremities. His muscle strength for hip flexion, knee extension, great toe extension, dorsal flexion and plantar flexion were grade two on the right side and grade three for the left side. When the patient came to emergency ward, we put pelvic binder immediately.
We also did MRI examination and pelvic CT Scan (Fig. 1). We found a compression fracture of 1st thoracic vertebra with compression at the spinal canal. From pelvic CT Scan we found a vertical fracture line through the right side of the sacrum. We also found pubic diastasis 1 cm width (Fig. 2).
Fig. 1.
Radiologic examination.
Fig. 2.
Pelvic CT scan examination.
Laboratory examination was shown normal level of hemoglobin (11.8 g/dL), hematocrit, leucocyte, thrombocyte, prothrombin time and activated partial thromboplastin time. Patient had elevated serum level of D-Dimer (15,100).
In our center, all emergency ward patients must undergo PCR swab test for Covid-19. This patient result was confirmed positive. However, he did not show any sign and symptoms of respiratory tract infection nor other viral infection. His body temperature was 36.5 °C.
The patient diagnosed with traumatic spinal cord injury of 1st thoracic vertebra ASIA Impairment Scale (AIS) C and sacral fracture Denis classification zone II of right side with confirmed Covid-19 case. We immediately gave the patient intravenous bolus of 1000 mg methylprednisolone (MP) within 3 h after the incident. Patient’s body weight was 60 kg.
We had done immediate surgery in negative pressure operating theatre with full covered personal protective device. We did emergency surgical decompression and sacroiliac fixation to achieve golden period of the neuronal recovery and intrapelvic bleeding control.
The patient underwent surgery by orthopaedic surgeons in spine consultant, hip and knee consultant and orthopaedic resident in Jakarta, Indonesia. We did posterior decompression and stabilization of the thoracic vertebra within 9 h after the incident. We put pedicle screw at the C7, Th1, Th2 and Th3. Then we put rods and nuts. After that, we did decompression by laminectomy of the C7 and Th1 and we also put vacuumed drain for the wound.
Simultaneously we did open reduction and internal fixation (ORIF) on the sacral fracture. When the patient in prone position, we identify the landmark before we did the incision. We palpate the posterior superior iliac spine (PSIS) of the right side and then about 1 fingerbreadth laterally we made a longitudinal incision. We did the opening layer-by-layer until we found the PSIS, then we clean the surrounding soft tissue using elevator. Next, using the Weber clamp we reduced the fracture fragment. We put one edge at the spinous process and the other lateral to ilium. Make sure the fragment was reduced. Then we put a two-hole 4.5 narrow dynamic compression plate (DCP) at the lateral side of posterior ridge of iliac bone, between posterior superior iliac spine (PSIS) and posterior inferior iliac spine (PIIS). The fixation of the plate to the bone using 2 partial threaded cancellous screws. We did fixation under image intensifier guided. Intraoperative bleeding was 1200 cc. We gave 750 cc of packed red cells intraoperatively. Post operatively, the patient’s condition was stable and no need for ventilator.
After the surgery, the patient was sent to Covid-19 intensive care unit (ICU) for hemodynamic evaluation. After 24 h monitoring, the vital sign and hemodynamic were stable and transferred to negative pressure ordinary ward. At the 1st to 3rd day after the incident, we administered MP 250 mg per 6 h intravenously. Next, we tapering off the MP by 125 mg per 6 h for the next 3 days. Then, we gave 125 mg per 12 h for 3 days. Finally, we administered MP 125 mg per day for the last 3 days. So, the MP was given for 12 days to this patient.
At 48 h after surgery, patient shown significant improvement. His bilateral muscle strength for inferior extremities was grade three. At 120 h after surgery, the patient’s muscle grade was four and the ability to sense was gradually improve. The patient also felt great improvement after the surgery, based on his ability to move the extremities better.
Post-discharged, for the Covid-19 management the patient was given 1600 mg Favipiravir as a single dose for 2 days, begun from the first day the patient was diagnosed. At the 3rd day after being confirmed positive Covid-19, we gave the patient with 600 mg per 12 h for 14 days. Followed up on the 7th day, the patient did the 2nd PCR swab test and the result was still positive. But at the 14th day, the 3rd PCR swab result was negative [4]. One week after surgery, the patient had been followed up at the clinic with great improvement of the ability to move better than before the surgery.
3. Discussion
Spinal cord injury commonly caused by traumatic incident. The condition could lead to loss of sensory and motor function [5]. The spinal cord consists of gray matter and white matter that connecting brain to the distal organ. When a traumatic event disrupts the spinal cord, it called primary injury. Then it leads to a cascade of biological event and make a secondary injury. This caused a neurological damage.
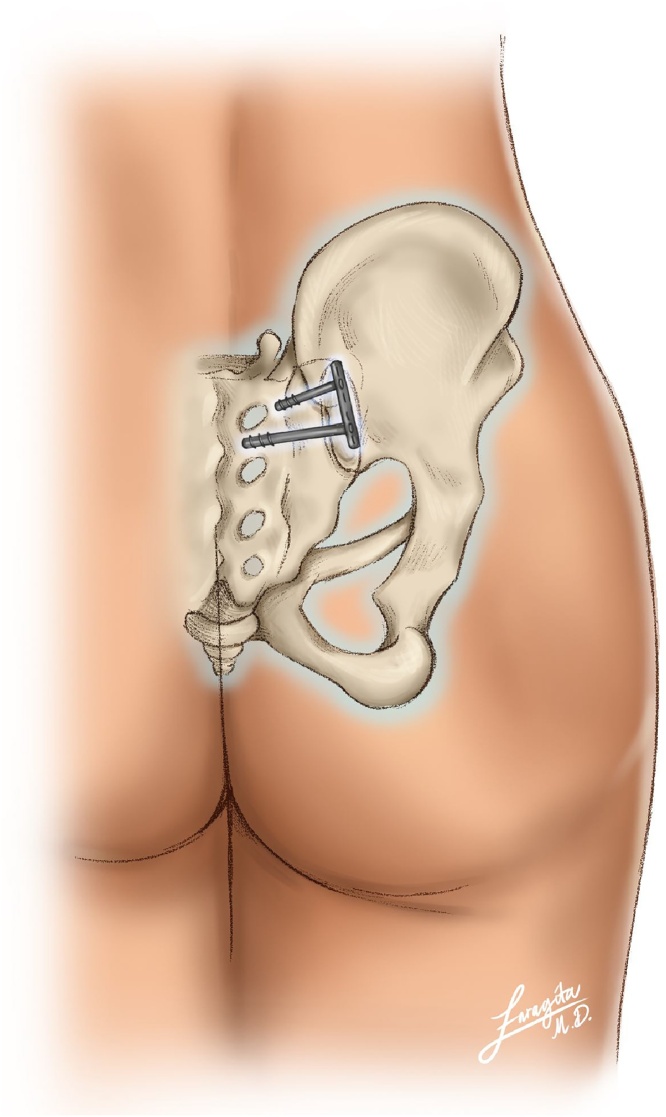
When primary injury happened, immediate decompression has a neuroprotective effect. Decompression prior to 24 h after spinal cord injury could improve 2 grade AIS within 6 months [6]. Other study shown decompression within 8 h has significant effect to motor and sensory function after 1 year [7]. On this patient, within 48 h after surgery, the motoric strength of lower extremity had increased from grade 2–3. After 120 h, the muscle strength had increased to grade 4 and the sensory function also gradually showed improvement.There were varies method for sacral fracture fixation (Fig. 3) [8]. The principle was to compress the fragment fracture as possible. To gaining more compressive area, we used a 2-hole 4.5 narrow DCP plate. First screw was inserted perpendicular to the plate until reach outer border of posterior sacral foramen. The second screw was inserted just below to the foramen and make sure that we did not hit the nerve, confirmed by using image intensifier. Before fixation, there was massive bleeding came out from the fragment fracture and the bleeding was reduced after fixation. For the pubic diastasis, we did not put any fixation since the diastasis was 1 cm (Fig. 4) [9]. In our center, the management for Covid-19 patient without sign and symptoms was Favipiravir with some supplement and vitamin (include: cholecalciferol 1000 IU once per day, vitamin C twice per day, zinc 20 mg twice per day, combination of probiotic and prebiotic twice per day, D-Alpha tocopherol 400 IU once per day). We also give curcuma tablet as hepatoprotective agent twice per day [4].
Fig. 3.
Sacral fracture fixation method.
Fig. 4.
Post-surgery radiographic examination.
4. Conclusion
Immediate surgical decompression and stabilization for spinal cord injury give significant improvement in motoric and sensory function. Adequate compression of sacral fracture gives a significant reduction in intrapelvic bleeding. Pubic diastasis which less than 2.5 cm could be managed conservatively [9].
An appropriate management for Covid-19 patient with Favipiravir and some supplements, had been proved could control the virus and give the patient good quality of life [4].
In managing a Covid-19 patient who needs immediate surgical treatment, we have to do the surgery effectively as possible to minimize the risk of viral exposure. There is no need to be afraid of doing surgery in the pandemic situation since the facility was appropriate and supported. The work has been reported in line with SCARE 2018 criteria [10].
Declaration of competing interest
The authors report no declarations of interest.
Source of funding
The authors report no external source of funding during the writing of this article.
Ethical approval
Ethical approval was not required in the treatment of the patient in this report.
Disclaimer
No patient or author details are included in the figures.
Consent
Written consent has been received from the subject.
Author contribution
A. J. Didy contributes in the study concept or design, data collection, analysis and interpretation, oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Yanuarso contributes in the study concept or design, data collection, analysis and interpretation, oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Danar Lukman Akbar contributes to the study concept or design, data collection and writing the paper.
Registration of research studies
Not applicable.
Guarantor
A. J. Didy is the sole guarantor of this submitted article.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Alizadeh A., Dyck S.M., Karimi-abdolrezaee S. Traumatic spinal cord injury: an overview of patophysiology, models and acute injury mechanisms. Front. Neurol. 2019;10(282) doi: 10.3389/fneur.2019.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodrigues-pinto R., Kurd M.F., Schroeder G.D., Kepler C.K., Krieg J.C., Holstein H. Sacral fractures and associated injuries. Glob Spine J. 2017;XX:1–8. doi: 10.1177/2192568217701097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alyami A.H., Alyami A.H., Almaeen B.N. Impact of COVID-19 on orthopedic surgery: experience from Saudi Arabia. Ann. Med. Surg. 2020;56(May):61–63. doi: 10.1016/j.amsu.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burhan E., Susanto A.D., Nasution S.A., Ginanjar E., Pitoyo W., Susilo A. 2020. Pedoman Tatalaksana COVID-19. 1–138 p. [Google Scholar]
- 5.Silva N.A., Sousa N., Reis R.L., Algado S.A.J. Progress in neurobiology from basics to clinical: a comprehensive review on spinal cord injury. Prog. Neurobiol. 2013:1–34. doi: 10.1016/j.pneurobio.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Fehlings M.G., Vaccaro A., Wilson J.R., Singh A., Cadotte D.W., Harrop J.S. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS) PLoS One. 2012;7(2):1–8. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grassner L., Wutte C., Klein B., Mach O., Riesner S., Panzer S. Early decompression (<8h) after traumatic cervical spinal cord injury improves functional outcome as assessed by Spinal Cord Independence Measure (SCIM) after 1 year. J. Neurotrauma. 2015;1(5):1–47. doi: 10.1089/neu.2015.4325. [DOI] [PubMed] [Google Scholar]
- 8.Simonian P.T., Routt M.L.C., Jr, Harrington R.M., Tencer Allan F. Internal fixation for the transforaminal sacral fracture. Clin. Orthop. Relat. Res. 1996;(323):202–209. doi: 10.1097/00003086-199602000-00028. [DOI] [PubMed] [Google Scholar]
- 9.Aggarwal S., Bali K., Krishnan V., Kumar V., Meena D., Sen R.K. Management outcomes in pubic diastasis : our experience with 19 patients. J. Orthop. Surg. Res. 2011;6(21):1–9. doi: 10.1186/1749-799X-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]