Abstract
Background
Interfacility transfers between emergency department (EDs) are common and at times unnecessary. We sought to examine the role of health insurance status with potentially avoidable transfers.
Methods
We conducted a retrospective observational analysis using hospital electronic administrative data of all interfacility ED‐to‐ED transfers to a single, quaternary care adult ED in 2018. We defined a potentially avoidable transfer as an ED‐to‐ED transfer in which the patient did not receive a procedure from a specialist at the receiving hospital and was discharged from the ED or the receiving hospital within 24 hours of arrival. We constructed a multivariable logistic regression model to examine whether insurance status was associated with potentially avoidable transfers among all ED‐to‐ED transfers adjusting for patient demographics, severity, mode of arrival, clinical condition, and rurality.
Results
Among 7508 transfers, 1862 (25%) were potentially avoidable and were more likely to be uninsured (20% vs 9%). In the multivariable analysis, among ED‐to‐ED transfers for adults aged 18–64 years old who were uninsured (vs any insurance) were significantly more likely to be potentially avoidable (adjusted odds ratio [aOR] 2.1 [1.7, 2.4]) and there is a significant interaction with age. Potentially avoidable transfers increased with younger age, male sex, black (vs white), small rural classification (vs urban), and arrival by ground ambulance (vs flight).
Conclusions
Potentially avoidable transfers comprised 1 in 4 transfers. Patients who lack insurance were more than twice as likely to be classified as potentially avoidable even after evaluating for confounders and interactions. This effect was most pronounced among younger patients. Further research is needed to explore why uninsured patients are disproportionately more likely to experience potentially avoidable transfers.
Keywords: appropriateness of care, care transitions, decision‐making, emergency care, emergency medicine, inter‐facility transfer, quality of care, regionalization
1. INTRODUCTION
1.1. Background
According to the Agency for Healthcare Research and Quality's (AHRQ) HCUPNet, there were 2.3 million US emergency department patients transferred to another acute care hospital in 2016, and these have nearly doubled over the preceding 10 years. 1 Interfacility transfer of patients may be necessary when patients initially present to an ED without the required services to care for that patient (eg, specialists). As interfacility transfers rates have increased, a substantial proportion of interfacility transfers may not be necessary 2 , 3 , 4 , 5 , 6 and may occur for reasons other than clinical necessity. 5 , 6 , 7 , 8 , 9 , 10
In a 2006 case‐control study of 97,393 patients pulled from the National Trauma Data Bank, the rate of interfacility transfer was statistically higher for male versus female, pediatric versus adult, black versus white, and Medicaid‐insured versus otherwise‐insured patients. 8 These patterns were largely consistent in similar studies in 2010 and 2014, although uninsured status rather than Medicare was also found to be associated with higher odds of interfacility transfer. 7 , 10 Among patients with ST‐elevation myocardial infarction (STEMI), a time‐sensitive emergency, patients who were uninsured were 60% more likely to experience interfacility transfer. 11
1.2. Importance
Determining the appropriateness of interfacility transfer can be challenging to retrospectively identify. Retrospective chart review is time consuming and identifying the appropriateness of decisionmaking can be subjective. Alternatively, some investigators have used final patient ED and hospital disposition, including length of stay and the receipt of specialty procedures following transfer, to classify transfers as "potentially avoidable." 5 , 6 , 10 , 12 Although the appropriateness of transfers meeting these criteria remains a challenge, the likelihood increases in this population and such transfers could potentially be handled through alternative means (eg, telehealth) or are entirely avoidable. Although the most commonly cited reason for such transfers is need for higher level of care, a study of interfacility transfer between EDs in 6 states for trauma patients in 2011 found that 36% were discharged from the receiving ED without receiving any procedure. 13 , 14 , 15 In a similar study examining transferred trauma patients who were ultimately admitted by the receiving ED between 2000 and 2004, nearly 7% of patients were discharged alive within 1 day and did not receive a surgical procedure, suggesting that some patients who are admitted may not require a higher level of care. 10
1.3. Goals of this investigation
Several important gaps in research on the appropriateness of emergent interfacility transfers remain. The factors influencing adult interfacility transfers, particularly across a broad array of clinical conditions, remain poorly understood. Further, how non‐clinical factors are associated with these transfers, specifically the role of insurance status, remains an important source of investigation. Understanding how lack of insurance influences interfacility transfer remains an important step toward the development of interventions to deliver care through alternative means rather than requiring interfacility transfers.
2. METHODS
2.1. Study design and setting
We conducted a retrospective observational analysis of all adult patients who experienced interfacility transfer to Vanderbilt University Medical Center (VUMC) ED, a single quaternary care academic ED, in Nashville, TN, that occurred between January 1, 2018 and December 31, 2018. VUMC is a major referral center as the region's only Level 1 Trauma Center and a major referral center for cardiovascular and neurovascular services. VUMC receives interfacility transfer patients from a catchment area of ≈ 65,000 square miles. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational studies. 16
2.2. Selection of participants
Cases were retrospectively identified as an interfacility transfer to the VUMC ED using VUMC's Transfer Center interfacility transfer logs. Transfer center logs included all potential and completed interfacility transfers. These records were used to identify transferring hospital and mode of arrival. Transfers were linked through a unique visit number created in the electronic health record and updated in the transfer logs. Visit numbers were used to link patients transferred with their demographic (eg, age, sex, race, and insurance status) and clinical (eg, durations, triage acuity, diagnostic and procedure codes, and disposition status) data in the electronic health record. All adult (18 years of age or older) patients who experienced interfacility transfer from another ED to the ED at VUMC within the study time frame were included. We excluded transfers who left before completion of treatment (ie, against medical advice), direct admission to the hospital bypassing the VUMC ED, transfer by personal vehicle, and incomplete data necessary to link across data sources (eg, visit identification number). We did not include language spoken nor ethnicity as these were not reliably available in the electronic record. This study was approved by the VUMC institutional review board under waiver of informed consent.
2.3. Outcomes
The primary outcome was the classification of an interfacility transfer as a potentially avoidable transfer. We have adapted the definition of a potentially avoidable transfer for the adult population as an interfacility transfer to the VUMC ED that (1) did not receive a specialty procedure at the receiving hospital, and either (2) was discharged directly from the ED or was admitted (including observation status) in any capacity and discharged within 24 hours of admission. 6 Similar to prior definitions of potentially avoidable transfer, 12 specialty procedures were defined as any procedure classified by a current procedural terminology (CPT) code. Although transfers meeting this definition may be appropriate and still require the transfer, the purpose of this definition is to identify factors associated with interfacility transfers that may be suitable to alternative forms of care (eg, telehealth).
2.4. Measurements
We collected patient demographic data including age, sex, race (white, black), and insurance status (Medicare, Medicaid, commercial, other, and uninsured), with insurance status defined as the primary payor listed for the ED encounter at VUMC. In addition, we also collected characteristics of the transferring ED as well as the patient encounter itself, including transfer distance, rurality, mode of transportation (ground vs flight), time of presentation to the referring hospital (business hours [Monday‐Friday between 8:00 am and 5:00 pm CST] vs non), clinical classification software (CCS) category of the diagnostic code, and ED disposition at the receiving hospital.
Rurality was defined using Rural‐Urban Commuting Area (RUCA) Codes and grouped according to the 4‐classification system (urban, large rural, small rural, isolated). 17 Transfer distance was defined as the distance (in miles) between the transferring and receiving EDs and was measured using Google Maps (maps.google.com). Clinical category was defined using the primary International Classification of Diseases, 10th Revision, Clinical Modification (ICD‐10‐CM) code using AHRQ's CCS classification software. 18
The Bottom Line
Interfacility transfers between emergency departments (EDs) are common and potentially disruptive. In this study of 7508 transfers to a quaternary care ED, 1862 (25%) were potentially avoidable. Younger patients lacking medical insurance were more than twice as likely to be associated with an avoidable transfer. Future work may help elucidate strategies to streamline safe and effective interfacility transfers.
2.5. Analysis
We performed descriptive statistics on the study population and conducted a multivariable logistic regression with the primary outcome being a potentially avoidable transfer. Insurance status was the primary exposure with planned interactions by insurance type (Medicare, Medicaid, commercial, other, and uninsured) with age groups (18–34 years, 35–49 years, 50–64 years vs reference 65+years). We planned this interaction because insurance status is age dependent with most patients aged 65 years and older already having Medicare. We adjusted for the following covariates: sex, race, encounter details including transfer distance (in miles), time of day (reference = business hours), mode of transportation (reference = flight), and rurality (reference = urban). We further planned an a priori subgroup analysis of the trauma population (injury CCS category) to examine whether factors associated with potentially avoidable transfers were distinct from the broader population.
To preserve all observations identified, single‐value imputation was applied on missing values. For the 54 (0.7%) observations with missing values on travel distance, their values were imputed by the median (64 miles). For the 35 (0.5%) observations with unknown value on acuity, their values were best‐guessed by the mode (3‐Urgent).
To show the interaction between age and insurance type, the age and insurance variables were coded into a variable with 14 categories, aged 65+ years as 1 group, other insurance as another group, insurance type of Medicare, Medicaid, commercial were each categorized by 3 age groups, 18–34 years, 35–49 years, and 50–64 years.
AUC (area under the receiver operating characteristic curve) was reported, and its 95% confidence interval was computed with Delong's method. Relative variable importance was calculated as the percentage of overall deviance for each variable. Statistical analysis was conducted using R (version 3.6.2) with rROC and car packages. 19 , 20 , 21
3. RESULTS
3.1. Characteristics of study subjects
Between January 1, 2018, and December 31, 2018, we identified 11,058 interfacility transfers in which the transfer process to VUMC was initiated from 263 unique facilities. Nearly 2,900 of these were excluded because the transfer either originated outside of the ED (eg, hospitalized patient) or were transferred by personal vehicle. Another 208 had missing or incomplete data, 207 of which were for a missing visit number to connect the transfer logs with patient demographic and visit data. Lack of a visit number represents an incomplete transfer; whereas, 1 record had an invalid visit number. An additional 445 transfers were excluded for not meeting the receiving ED disposition criteria of either being discharged or admitted to the hospital. Among these, 358 (80%) were missing and 47 (11%) were against medical advice. Finally, 24 transfers were under the age of 18 years old. Thus, we identified a subset of 7508 patients who experienced interfacility transfer from 1 ED to the VUMC ED (Figure 1) meeting our study criteria. As seen in Table 1, the median age was 56 years (interquartile range [IQR] 39, 69) , of which 33% were 65 years or older. Among all transfers, 4298 (57%) were male patients and 6253 (83%) were white. Nearly 80% of transfers had insurance and ≈ 25% (N = 1873) of all transfers met the criteria to be defined as a potentially avoidable transfer.
FIGURE 1.
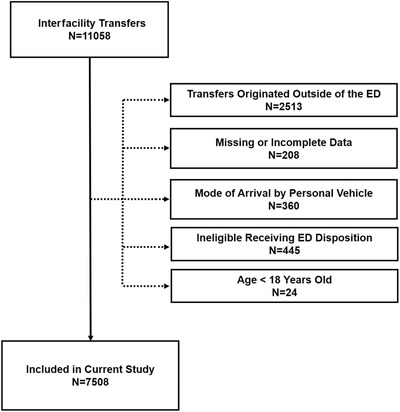
CONSORT diagram of the included patient population. ED, emergency department
TABLE 1.
Patient demographics by potentially avoidable transfer classification
| Overall | Not avoidable | Potentially avoidable | |||
|---|---|---|---|---|---|
| Characteristic | N = 7508 | N = 5646 | N = 1862 | P | |
| Age, years (median [IQR]) | 55.8 [38.7, 69.1] | 58.4 [43.0, 70.7] | 44.4 [30.6, 61.3] | <0.001 | |
| Sex (%) | Male | 4281 (57.0) | 3117 (55.2) | 1164 (62.5) | <0.001 |
| Female | 3227 (43.0) | 2529 (44.8) | 698 (37.5) | ||
| Race (%) | White | 6235 (83.0) | 4765 (84.4) | 1470 (78.9) | <0.001 |
| Black | 966 (12.9) | 666 (11.8) | 300 (16.1) | ||
| Other | 307 (4.1) | 215 (3.8) | 92 (4.9) | ||
| Insurance Type (%) | Uninsured | 880 (11.7) | 503 (8.9) | 377 (20.2) | <0.001 |
| Medicare | 3171 (42.2) | 2681 (47.5) | 490 (26.3) | ||
| Medicaid | 1177 (15.7) | 878 (15.6) | 299 (16.1) | ||
| Commercial | 1632 (21.7) | 1157 (20.5) | 475 (25.5) | ||
| Other | 648 (8.6) | 427 (7.6) | 221 (11.9) | ||
| Mode of transport (%) | Ambulance | 6314 (84.1) | 4632 (82.0) | 1682 (90.3) | <0.001 |
| Medical flight | 931 (12.4) | 799 (14.2) | 132 (7.1) | ||
| Other | 263 (3.5) | 215 (3.8) | 48 (2.6) | ||
| Transferring hospital type (%) | Urban | 3704 (49.3) | 2700 (47.8) | 1004 (53.9) | <0.001 |
| Large rural | 2589 (34.5) | 2061 (36.5) | 528 (28.4) | ||
| Small rural | 933 (12.4) | 671 (11.9) | 262 (14.1) | ||
| Isolated | 282 (3.8) | 214 (3.8) | 68 (3.7) | ||
| Travel distance (median [IQR]) | 64.0 [32.0, 95.0] | 69.0 [34.8, 101.0] | 47.0 [32.0, 83.0] | <0.001 | |
| Business hour (%) | Business hours | 2096 (27.9) | 1623 (28.7) | 473 (25.4) | 0.006 |
| Non‐business hours | 5412 (72.1) | 4023 (71.3) | 1389 (74.6) | ||
| Timing of presentation (%) | Weekday | 4242 (56.5) | 3212 (56.9) | 1030 (55.3) | <0.001 |
| Weekend | 3266 (43.5) | 2434 (43.1) | 832 (44.7) | ||
| Triage acuity (%) | 1‐Immediate | 229 (3.1) | 203 (3.6) | 26 (1.4) | <0.001 |
| 2‐Emergent | 3109 (41.4) | 2590 (45.9) | 519 (27.9) | ||
| 3‐Urgent | 4092 (54.5) | 2809 (49.8) | 1283 (68.9) | ||
| 4‐Less Urgent | 42 (0.6) | 11 (0.2) | 31 (1.7) | ||
| 5‐Non‐Urgent | 1 (0.0) | 1 (0.0) | 0 (0.0) | ||
| Unknown | 35 (0.5) | 32 (0.6) | 3 (0.2) | ||
| Clinical characteristic software group (%) | Injury | 2750 (36.6) | 1833 (32.5) | 917 (49.2) | <0.001 |
| Digestive system | 965 (12.9) | 861 (15.2) | 104 (5.6) | ||
| Circulatory system | 761 (10.1) | 687 (12.2) | 74 (4.0) | ||
| Undifferentiated symptoms | 542 (7.2) | 354 (6.3) | 188 (10.1) | ||
| Nervous system | 412 (5.5) | 264 (4.7) | 148 (7.9) | ||
| Infectious diseases | 364 (4.8) | 347 (6.1) | 17 (0.9) | ||
| Remaining groups | 1714 (22.8) | 1300 (23.0) | 414 (22.2) | ||
| ED disposition status (%) | Discharge | 1425 (19.0) | 3 (0.1) | 1422 (76.4) | |
| Admit | 5981 (79.7) | 5541 (98.1) | 440 (23.6) | ||
| Other | 102 (1.4) | 102 (1.8) | 0 (0.0) | ||
| Hours from arrival to discharge (median [IQR]) | 67.3 [22.7, 141.9] | 96.3 [55.3, 179.1] | 8.3 [5.0, 15.0] | <0.001 | |
| Total length of stay < = 24 hours (%) | 1940 (25.8) | 96 (1.7) | 1844 (99.0) | <0.001 | |
| Specialty procedure performed (%) | 2046 (27.3) | 2046 (36.2) | 0 (0.0) | <0.001 |
ED, emergency department; IQR, interquartile range.
More than one‐third of transfers received an injury diagnostic code, and 72% of transfers occurred outside of business hours. The most frequent primary ICD‐10 diagnostic codes assigned at the receiving ED for potentially avoidable transfers were for headache (ICD‐10 R51) with 46 transfers among which 85% met the potentially avoidable definition. However, these represented only 2.1% of all 1862 potentially avoidable transfers. The remainder of the top 3 primary diagnostic codes included periapical abscess (ICD‐10 K04.7) with 45 transfers among which 64% were potentially avoidable, multiple rib fractures of both left and right side (ICD‐10 S22.41XA and S22.42XA; N = 96, 29% potentially avoidable).
Among 263 unique transferring facilities, the top 10 facilities accounted for 40% of both overall transfers and potentially avoidable transfers. Potentially avoidable transfer rates from these facilities ranged from 15% to 34%, The majority of transfers were transferred by ground ambulances (84%). Among transfers, 19% were discharged directly from the receiving VUMC hospital ED without admission.
3.2. Main results
In multivariable analyses, non‐medical factors had the strongest association with potentially avoidable transfers (Table 2). Here, we present the results of the logistic model with interaction. The model yields a moderate AUC (area under the curve) ROC (receiver operating characteristics) curve of 75.9% (95% confidence interval [CI], 74.6%, 77.1%). The factors with the strongest association of an ED‐to‐ED transfer being potentially avoidable were CCS category, age‐insurance interaction group, triage acuity, mode of transportation, and transfer distance, with relative variable importance of 38.1%, 34.9%, 15.8%, 3.3%, and 2.6%, respectively.
TABLE 2.
Multivariable logistic regression model results of being classified a potentially avoidable transfer by factor
| Variable | Level | Estimate (95% CI) |
|---|---|---|
| Sex | Male | Ref |
| Female | 0.8 (0.7, 0.9) | |
| Race group | White | Ref |
| Black | 1.2 (1.1, 1.5) | |
| Other | 1.0 (0.8, 1.4) | |
| Patient stability | Systolic BP > = 90 mmHg | Ref |
| Systolic BP < 90 mmHg | 0.5 (0.3, 1.0) | |
| Unknown | 1.5 (1.2, 1.8) | |
| Age (years) and insurance | Age 65 + | Ref |
| Medicare 50–64 | 1.1 (0.8, 1.4) | |
| Medicare 35–49 | 1.3 (0.9, 1.8) | |
| Medicare 18–34 | 1.7 (1.0, 2.9) | |
| Medicaid 50–64 | 1.1 (0.8, 1.5) | |
| Medicaid 35–49 | 1.9 (1.5, 2.5) | |
| Medicaid 18–34 | 2.6 (2.1, 3.3) | |
| Commercial 50–64 | 1.5 (1.2, 1.9) | |
| Commercial 35–49 | 2.6 (2.1, 3.4) | |
| Commercial 18–34 | 3.1 (2.4, 3.9) | |
| Uninsured 50–64 | 1.9 (1.4, 2.7) | |
| Uninsured 35–49 | 2.9 (2.2, 3.9) | |
| Uninsured 18–34 | 6.6 (5.1, 8.6) | |
| Other insurance | 2.9 (2.4, 3.7) | |
| Mode of transport | Ambulance | ref |
| Medical flight | 0.6 (0.5, 0.7) | |
| Other | 0.7 (0.5, 0.9) | |
| Travel distance (10 miles) | Per unit | 1.0 (1.0, 1.0) |
| Transferring hospital type | Urban | ref |
| Large rural | 1.0 (0.8, 1.1) | |
| Small rural | 1.4 (1.2, 1.7) | |
| Isolated | 1.2 (0.9, 1.7) | |
| Business hour | Business hours | ref |
| Non‐business hours | 1.1 (1.0, 1.3) | |
| Timing of presentation | Weekday | ref |
| Weekend | 1.0 (0.9, 1.2) | |
| Triage acuity | 1‐Immediate | ref |
| 2‐Emergent | 1.7 (1.1, 2.6) | |
| 3‐Urgent | 3.2 (2.0, 5.0) | |
| 4/5‐less/non‐urgent | 17.8 (7.7, 41.3) | |
| Clinical characteristic software group | Injury | ref |
| Digestive system | 0.2 (0.2, 0.3) | |
| Circulatory system | 0.4 (0.3, 0.5) | |
| Undifferentiated symptoms | 1.2 (1.0, 1.5) | |
| Nervous system | 1.4 (1.07, 1.7) | |
| Infectious diseases | 0.1 (0.1, 0.2) | |
| Remaining groups | 0.7 (0.6, 0.8) |
BP, blood pressure; CI, confidence interval.
Compared with patients aged 65 years and older (Table 2), uninsured transferred patients were more likely to be classified as a potentially avoidable transfer. Within age groups, ED‐to‐ED transfers involving uninsured 18–34 year‐olds (adjusted odds ratio [aOR], 6.6; 95% CI, 5.1, 8.6), 35–49 year‐olds (aOR, 2.9; 95% CI, 2.2, 3.9) and 50–64 year‐olds (aOR, 1.94; 95% CI, 1.4, 2.7) groups were most likely to be classified as potentially avoidable. Other factors associated with lower odds of an ED‐to‐ED transfer being a potentially avoidable transfer included female sex, transfer by medical flight, increased travel distance, and when compared with transfers with an injury diagnostic code, gastrointestinal, circulatory, and infectious diagnostic codes. Alternatively, ED‐to‐ED transfers for patients who are black, from small rural sites, with a lower severity triage acuity, and transfers with a nervous system diagnostic code were associated with higher odds of an ED‐to‐ED transfer being a potentially avoidable transfer.
Further examining the age and insurance status interaction, the overall 18–64 year‐old groups comparing uninsured transfers relative to transfers with any form of insurance were more likely to be classified as a potentially avoidable transfer (aOR, 2.1; 95% CI, 1.7, 2.4). There is evidence of an interaction of insurance status with age when examining the contrasts (Figure 2). For example, when comparing younger patients aged 18–34 years old with 50–64 years old, the aOR for commercial insurance is 2.0 (95% CI, 1.5, 2.7), Medicare is 1.6 (95% CI, 0.9, 2.7); whereas, within the uninsured group the aOR is 3.4 (95% CI, 2.3, 5.0). Thus, there is a significant interaction between insurance status and age. In other words, the age effect when comparing younger with older groups, the younger group is more likely to be a potentially avoidable transfer in the uninsured group compared with other forms of insurance. However, this effect was most pronounced among the uninsured group suggesting that an interaction between age (<65 years old) and insurance status exists.
FIGURE 2.
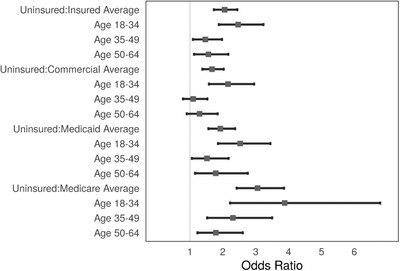
Adjusted odds ratio of the interactions between insurance and age group. The filled rectangle represents the adjusted odds ratio and the whiskers represent the 95% confidence interval
Subgroup analyses of the ED‐to‐ED transfers with an injury diagnostic code were unchanged from the overall transfer population. However, such ED‐to‐ED interfacility transfers during non‐business hours were more likely to be classified as a potentially avoidable transfer (aOR, 1.3; 95% CI, 1.0, 1.5).
3.3. Limitations
The results of this study should be considered in the context of potential limitations. First, we used administrative data with the known limitation of such data. For example, the validity of language spoken and ethnicity in the electronic health record limited our ability to include this as a potential factor influencing potentially avoidable transfers. Another limitation of administrative data in this context is the complete identification of potential transfers through the transfer logs. However, transfers that bypass the transfer center are exceedingly rare (estimated by clinical leadership at < 10 per year) and all transfers were required to have records created in the transfer logs. Although there were 208 exclusions for missing or incomplete data, 207 represented transfers that were not completed (eg, patient died before transfer). Combined with regular monthly review of the transfer logs by operational staff, the quality and completeness of the transfer records were very high.
Second, although we used a single quaternary care center that encompasses a large catchment area in middle Tennessee, the transfer protocols and patterns that govern these interfacility transfers may not be generalizable to other hospitals and geographic regions. Finally, making a retrospective determination of the appropriateness of the interfacility transfer is severely limited by the availability of the transferring facility's resources at the time of transfer and the transferring clinician's decisionmaking process. Thus, our use of the term “potentially avoidable” was used to describe interfacility transfers that may not require actual transfer to another ED. Instead, if specialty consultation is needed, this population may be amenable to remote consultation through telehealth or a subset of interfacility transfers.
4. DISCUSSION
We conducted a retrospective observational analysis of all adult ED‐to‐ED interfacility transfers in 2018 to a single quaternary care ED to examine the association of potentially avoidable transfers with insurance status. Our research revealed the following 3 key findings: (1) nearly 1 in 4 transfers met our definition of a potentially avoidable transfer; (2) lack of insurance and lower age were significantly associated with increased odds of being a potentially avoidable transfer; and (3) patient demographic factors for ED‐to‐ED‐transfers including patient sex and race were significantly associated with classification of a transfer as potentially avoidable.
In retrospective analyses of interfacility transfers, the need for specialist care is one of the most commonly cited reasons for interfacility transfer. 6 With access to on‐call specialists diminishing, particularly in rural EDs, rates of interfacility transfers have risen. 1 , 15 , 22 Our findings further support the broad impact of such transfers with nearly one‐quarter of the > 7000 interfacility transfers to our quaternary care center ED meeting the potentially avoidable transfer definition.
Our work is consistent with the frequency of trauma patients transferred for care that may be unnecessary. Previous studies of trauma patients transferred from another ED found that between 24% and 36% met study definitions of unnecessary transfer. 13 , 23 However, non‐trauma patients were excluded in these studies and they primarily focused on injury types rather than patient and visit‐level factors. Notably, potentially avoidable transfers were not different from the broader population.
The transfer process may be necessary for accessing specialist care and improving clinical outcomes, but it is not without medical and financial cost to both patients, their families, hospital systems, and the broader society. Compared with patients admitted directly from the ED, patients experiencing interfacility transfer from another hospital have a longer length of stay, higher costs, fewer discharges to home, and higher inpatient mortality even after adjusting for patient characteristics and mortality risks. 24 Although rapid transfer of patients may improve mortality and clinical outcomes for select acute conditions, such as stroke or acute myocardial infarction, interfacility transfer of patients is highly disruptive to patients and their families and can disproportionately burden transferring and receiving EDs by delaying care for other patients seeking care. 12 , 25
In multivariable analysis of patient‐ and facility‐level factors, we found that ED‐to‐ED transfers involving patients who lack insurance, were black, younger, and male were associated with higher odds of experiencing a potentially avoidable transfer. Lack of insurance was previously identified as a risk factor for transfer in a 2016 study evaluating adult ED visits for STEMI. 11 Among the current population, there are 2 potential explanations for these findings. First, non‐medical factors may be influencing the appropriateness of transfers and the likelihood for intervention. Alternatively, these patient populations may be specifically targeted for transfer, whether implicitly or explicitly.
Racial disparities are known to exist in acute care. Among hospitalized patients with acute myocardial infarction, prior work found that black patients were less likely to be transferred for percutaneous coronary intervention. 26 , 27 Lack of insurance may contribute to this disparity. 28 Further, the receiving EDs must absorb patients in already crowded settings and the system must bear the additional costs of these transfers that the patient may be fiscally responsible for.
Another consideration is the use of the term “potentially avoidable transfer.” Although we used an accepted definition of a potentially avoidable transfer, such transfers may have been necessary given the context surrounding each transfer. For example, the transferring clinician may have required specialty consultation to determine whether a patient requires intervention, even if they did not ultimately require a procedure. Alternatively, the patient may have requested the transfer despite having the capabilities to treat the patient locally. Understanding the appropriateness of such transfers is an important step and may require a qualitative approach to examine why these transfers occurred.
Another important step is to understand and the role that potential sources of unconscious bias may play in transfer decisionmaking. Prior work in acute surgical emergencies identified that physician decisionmaking at the referral and receiving centers, particularly around end‐of‐life care, may affect potentially avoidable transfers. 29 Potential interventions to reduce unnecessary transfers may include the development of interfacility transfer protocols 30 and telehealth. 31 , 32 Other potential policy interventions such as expanded Medicaid access (ie, the Affordable Care Act) may address potential racial inequities in the transfer of for patients with acute myocardial infarction for percutaneous coronary intervention in California 33 but remain to be explored in other acute care settings and conditions. Finally, reducing potentially avoidable transfers must be balanced with the unintended consequences of compromising necessary transfers.
In summary, we identified that interfacility transfers meeting the potentially avoidable transfer definition to our quaternary care ED were common. Lack of insurance was independently associated with higher odds of being a potentially avoidable transfer. Other non‐medical factors associated with transfers, such as black race, male sex, younger age, after‐hours presentation, and more rural locations, were independently‐associated with higher rates of potentially avoidable transfers. Future research should examine reasons for such transfers, the appropriateness of such transfers, and the efficacy of interventions to deliver care through alternative means.
FINANCIAL DISCLOSURES
None.
FUNDING INFORMATION
Dr. Ward is supported by K23 HL127130 and VA ORH‐10808. REDCap was funded by UL1TR000445 from NCATS/NIH. Dr. Gong and Ms. Hart were also supported by the Vanderbilt Trans‐Institutional Programs and a VICTR grant from CTSA (NCATS UL1 TR002243). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health nor the U.S. Department of Veteran Affairs.
AUTHOR CONTRIBUTIONS
Conceptualization: MJW, MKW, WHS, KH. Data curation: WG, KH. Formal analysis: WG, KH, MJW. Funding acquisition: MJW, MKW. Methodology: All authors; Roles/Writing: original draft MJW, MKW. Writing‐review and editing: All authors. Final responsibility of the article is taken by: MJW.
Biography
Michael J. Ward, MD, PhD is Assistant Professor in the Department of Emergency Medicine at Vanderbilt University Medical Center.

Wright MK, Gong W, Hart K, Self WH, Ward MJ. Association of insurance status with potentially avoidable transfers to an academic emergency department: A retrospective observational study. JACEP Open. 2021;2:e12385. 10.1002/emp2.12385
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Bernard P. Chang, MD, PhD.
REFERENCES
- 1. Agency for Healthcare Research and Quality. HCUPnet: Healthcare Cost and Utilization Project (HCUP). 2019. https://hcupnet.ahrq.gov/#setup. Accessed January 26, 2021. [PubMed] [Google Scholar]
- 2. Franca UL, McManus ML. Outcomes of hospital transfers for pediatric abdominal pain and appendicitis. JAMA Netw Open. 2018;1(6):e183249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Safaee MM, Morshed RA, Spatz J, Sankaran S, Berger MS, Aghi MK. Interfacility neurosurgical transfers: an analysis of nontraumatic inpatient and emergency department transfers with implications for improvements in care. J Neurosurg. 2018;131(1):281‐289. [DOI] [PubMed] [Google Scholar]
- 4. Bible JE, Kadakia RJ, Kay HF, Zhang CE, Casimir GE, Devin CJ. How often are interfacility transfers of spine injury patients truly necessary? Spine J. 2014;14(12):2877‐2884. [DOI] [PubMed] [Google Scholar]
- 5. Snyder CW, Kauffman JD, Pracht EE, Danielson PD, Ciesla DJ, Chandler NM. Risk factors for avoidable transfer to a pediatric trauma center among patients 2 years and older. J Trauma Acute Care Surg. 2019;86(1):92‐96. [DOI] [PubMed] [Google Scholar]
- 6. Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially avoidable pediatric interfacility transfer is a costly burden for rural families: a cohort study. Acad Emerg Med. 2016;23(8):885‐894. [DOI] [PubMed] [Google Scholar]
- 7. Delgado MK, Yokell MA, Staudenmayer KL, Spain DA, Hernandez‐Boussard T, Wang NE. Factors associated with the disposition of severely injured patients initially seen at non‐trauma center emergency departments: disparities by insurance status. JAMA Surg. 2014;149(5):422‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koval KJ, Tingey CW, Spratt KF. Are patients being transferred to level‐I trauma centers for reasons other than medical necessity? J Bone Joint Surg Am. 2006;88(10):2124‐2132. [DOI] [PubMed] [Google Scholar]
- 9. Mueller SK, Zheng J, Orav EJ, Schnipper JL. Rates, predictors and variability of interhospital transfers: a National evaluation. J Hosp Med. 2017;12(6):435‐442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Osen HB, Bass RR, Abdullah F, Chang DC. Rapid discharge after transfer: risk factors, incidence, and implications for trauma systems. J Trauma. 2010;69(3):602‐606. [DOI] [PubMed] [Google Scholar]
- 11. Ward MJ, Kripalani S, Zhu Y, et al. Role of health insurance status in interfacility transfers of patients with ST‐elevation myocardial infarction. Am J Cardiol. 2016;118(3):332‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mohr NM, Wu C, Ward MJ, McNaughton CD, Richardson K, Kaboli PJ. Potentially avoidable inter‐facility transfer from veterans health administration emergency departments: a cohort study. BMC Health Serv Res. 2020;20(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Medford‐Davis LN, Holena DN, Karp D, Kallan MJ, Delgado MK. Which transfers can we avoid: multi‐state analysis of factors associated with discharge home without procedure after ED to ED transfer for traumatic injury. Am J Emerg Med. 2018;36(5):797‐803. [DOI] [PubMed] [Google Scholar]
- 14. Nacht J, Macht M, Ginde AA. Interhospital transfers from U.S. emergency departments: implications for resource utilization, patient safety, and regionalization. Acad Emerg Med. 2013;20(9):888‐893. [DOI] [PubMed] [Google Scholar]
- 15. Li J, Pryor S, Choi B, et al. Profile of interfacility emergency department transfers: transferring medical providers and reasons for transfer. Pediatr Emerg Care. 2019;35(1):38‐44. [DOI] [PubMed] [Google Scholar]
- 16. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (Strobe) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495‐1499. [DOI] [PubMed] [Google Scholar]
- 17. Center RHR. WWAMI Rural Health Research Center. Rural‐Urban Commuting Area Codes (RUCAs). http://depts.washington.edu/uwruca/index.php. Accessed August 5, 2019.
- 18. Agency for Healthcare Research and Quality . Clinical Classifications Software (CCS) for ICD‐10‐PCS (beta version). Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed September 19, 2019.
- 19. Fox J, Weisberg S. An R Companion to Applied Regression. Sage publications; 2018. [Google Scholar]
- 20. Robin X, Turck N, Hainard A, et al. pROC: an open‐source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 22. Menchine MD, Baraff LJ. On‐call specialists and higher level of care transfers in California emergency departments. Acad Emerg Med. 2008;15(4):329‐336. [DOI] [PubMed] [Google Scholar]
- 23. Sorensen MJ, von Recklinghausen FM, Fulton G, Burchard KW. Secondary overtriage: the burden of unnecessary interfacility transfers in a rural trauma system. JAMA Surg. 2013;148(8):763‐768. [DOI] [PubMed] [Google Scholar]
- 24. Sokol‐Hessner L, White AA, Davis KF, Herzig SJ, Hohmann SF. Interhospital transfer patients discharged by academic hospitalists and general internists: characteristics and outcomes. J Hosp Med. 2016;11(4):245‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McNaughton C, Bonnet K, Schlundt D, et al. Rural interfacility emergency department transfers: framework and qualitative analysis. West J Emerg Med. 2020;21(4):858‐865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cooke CR, Nallamothu B, Kahn JM, Birkmeyer JD, Iwashyna TJ. Race and timeliness of transfer for revascularization in patients with acute myocardial infarction. Med Care. 2011;49(7):662‐667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Popescu I, Vaughan‐Sarrazin MS, Rosenthal GE. Differences in mortality and use of revascularization in black and white patients with acute MI admitted to hospitals with and without revascularization services. JAMA. 2007;297(22):2489‐2495. [DOI] [PubMed] [Google Scholar]
- 28. Graham GN, Jones PG, Chan PS, Arnold SV, Krumholz HM, Spertus JA. Racial disparities in patient characteristics and survival after acute myocardial infarction. JAMA Netw Open. 2018;1(7):e184240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kummerow Broman K, Ward MJ, Poulose BK, Schwarze ML. Surgical transfer decision making: how regional resources are allocated in a regional transfer network. Jt Comm J Qual Patient Saf. 2018;44(1):33‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pontell ME, Colazo JM, Drolet BC. Unnecessary interfacility transfers for craniomaxillofacial trauma. Plast Reconstr Surg. 2020;145(5):975e‐983e. [DOI] [PubMed] [Google Scholar]
- 31. Paik AM, Granick MS, Scott S. Plastic surgery telehealth consultation expedites emergency department treatment. J Telemed Telecare. 2017;23(2):321‐327. [DOI] [PubMed] [Google Scholar]
- 32. du Toit M, Malau‐Aduli B, Vangaveti V, Sabesan S, Ray RA. Use of telehealth in the management of non‐critical emergencies in rural or remote emergency departments: a systematic review. J Telemed Telecare. 2019;25(1):3‐16. [DOI] [PubMed] [Google Scholar]
- 33. Valdovinos EM, Niedzwiecki MJ, Guo J, Hsia RY. The association of medicaid expansion and racial/ethnic inequities in access, treatment, and outcomes for patients with acute myocardial infarction. PLoS One. 2020;15(11):e0241785. [DOI] [PMC free article] [PubMed] [Google Scholar]


