Abstract
From 1985 to 2016, the prevalence of underweight decreased, and that of obesity and severe obesity increased, in most regions, with significant variation in the magnitude of these changes across regions. We investigated how much change in mean body mass index (BMI) explains changes in the prevalence of underweight, obesity, and severe obesity in different regions using data from 2896 population-based studies with 187 million participants. Changes in the prevalence of underweight and total obesity, and to a lesser extent severe obesity, are largely driven by shifts in the distribution of BMI, with smaller contributions from changes in the shape of the distribution. In East and Southeast Asia and sub-Saharan Africa, the underweight tail of the BMI distribution was left behind as the distribution shifted. There is a need for policies that address all forms of malnutrition by making healthy foods accessible and affordable, while restricting unhealthy foods through fiscal and regulatory restrictions.
Research organism: None
Introduction
Underweight as well as obesity can lead to adverse health outcomes (Prospective Studies Collaboration et al., 2009; Global BMI Mortality Collaboration, 2016; Emerging Risk Factors Collaboration et al., 2011). For at least four decades, the prevalence of underweight has decreased, and that of obesity has increased, in most countries with significant variation in the magnitude of these changes across regions of the world (NCD Risk Factor Collaboration (NCD-RisC), 2017a; NCD Risk Factor Collaboration (NCD-RisC), 2019).
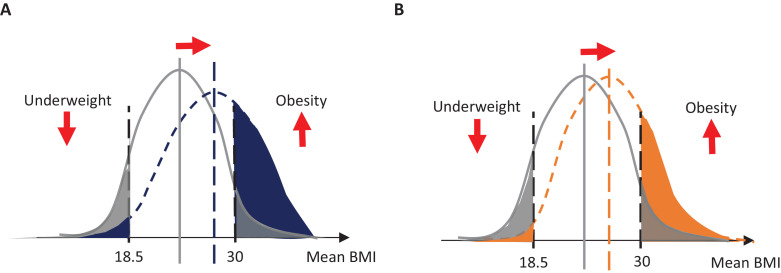
A shift in the whole distribution of body mass index (BMI) would simultaneously affect mean BMI as well as the prevalence of underweight and obesity (Razak et al., 2018; Rose and Day, 1990). In contrast, changes in the shape of BMI distribution – for example, widening or narrowing of the BMI distribution, becoming more or less skewed, or having a thinner or thicker tail – would affect the prevalence of underweight and obesity with only small impacts on the population mean, as shown schematically in Figure 1. Understanding these two mechanisms is essential as they may require different public health and clinical responses (Penman and Johnson, 2006). But it is unclear how much the two mechanisms have contributed to the observed decline in underweight and rise in obesity in different world regions.
Figure 1. Schematic diagram of contribution of change in mean body mass index (BMI) to change in total prevalence of underweight or obesity.
(A) Change in the prevalence of underweight and obesity if the distribution shifts, represented by a change in its mean and its shape. In this example, the change (shown as the difference between blue and gray) results in a small decrease of underweight and a large increase in obesity. (B) Change in the prevalence of underweight and obesity when only mean BMI changes (shown as the difference between orange and gray), without a change in the shape of the distribution.
Some studies have investigated whether the rise in obesity or the decrease of underweight over time, or differences across countries, were due to a shift in BMI distribution versus changes in the low- or high-BMI tails of the distribution (Razak et al., 2018; Wang et al., 2007; Wagner et al., 2019; Vaezghasemi et al., 2016; Razak et al., 2013; Popkin and Slining, 2013; Popkin, 2010; Peeters et al., 2015; Ouyang et al., 2015; Monteiro et al., 2002; Midthjell et al., 2013; Lebel et al., 2018; Khang and Yun, 2010; Helmchen and Henderson, 2004; Hayes et al., 2015; Green et al., 2016; Flegal and Troiano, 2000; Stenholm et al., 2015; Hayes et al., 2017; Flegal et al., 2012; Bovet et al., 2008). Most of these studies focused on a single or small number of countries over relatively short durations or covered only one sex, a narrow age group, or specific social groups. To understand whether weight gain occurs across all BMI levels or disproportionately affects the underweight or obese segments of the distribution, and how this phenomenon varies geographically, there is a need for a population-based study that simultaneously investigates both underweight and obesity in relation to mean BMI in different regions of the world. We used a comprehensive global database to investigate how much change in mean BMI can explain the corresponding changes in prevalence of adults with underweight (defined as BMI <18.5 kg/m2), total obesity (BMI ≥30 kg/m2), and severe obesity (BMI ≥35 kg/m2) over three decades from 1985 to 2016 in different regions of the world.
Results
Data sources
The Non-Communicable Disease Risk Factor Collaboration (NCD-RisC) database contains 2896 population-based studies conducted from 1985 to 2019 with height and weight measurements of 187 million participants. Of these, 2033 studies had measurements of height and weight on 132.6 million participants aged 20–79 years. The number of studies with participants aged 20–79 years in different regions ranged from 53 in Oceania to 637 in the high-income western region. The number of data sources by country is shown in Figure 2. The list of data sources and their characteristics is provided in Supplementary file 4.
Figure 2. Number of data sources with participants aged 20-79 years.
Change in mean BMI and prevalence of underweight, obesity, and severe obesity by region
In 2016, the age-standardised prevalence of underweight was highest (>16% in different sex-age groups) in South Asia; it was <2.5% in Central and Eastern Europe; the high-income western region; Latin America and the Caribbean; Oceania; and Central Asia, the Middle East, and North Africa for most age and sex groups. The age-standardised prevalence of obesity was highest (>24%) in these same regions for most age and sex groups. It was lowest (<7%) in men and women from South Asia; the high-income Asia Pacific region; and men from sub-Saharan Africa. The age-standardised prevalence of severe obesity was highest (12–18%) in women aged 50–79 years from Central Asia, the Middle East, and North Africa; the high-income western region; Central and Eastern Europe; and Latin America and the Caribbean. It was lowest (<2%) in South Asia; East and Southeast Asia; the high-income Asia Pacific region; and men in sub-Saharan Africa.
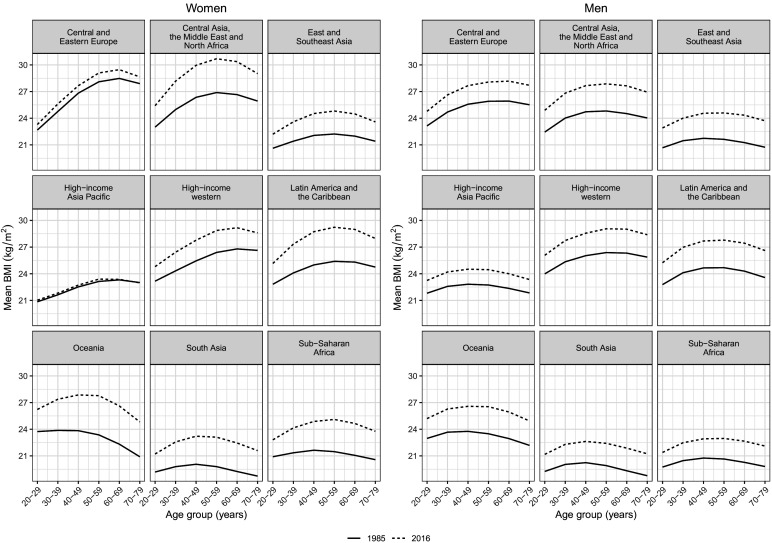
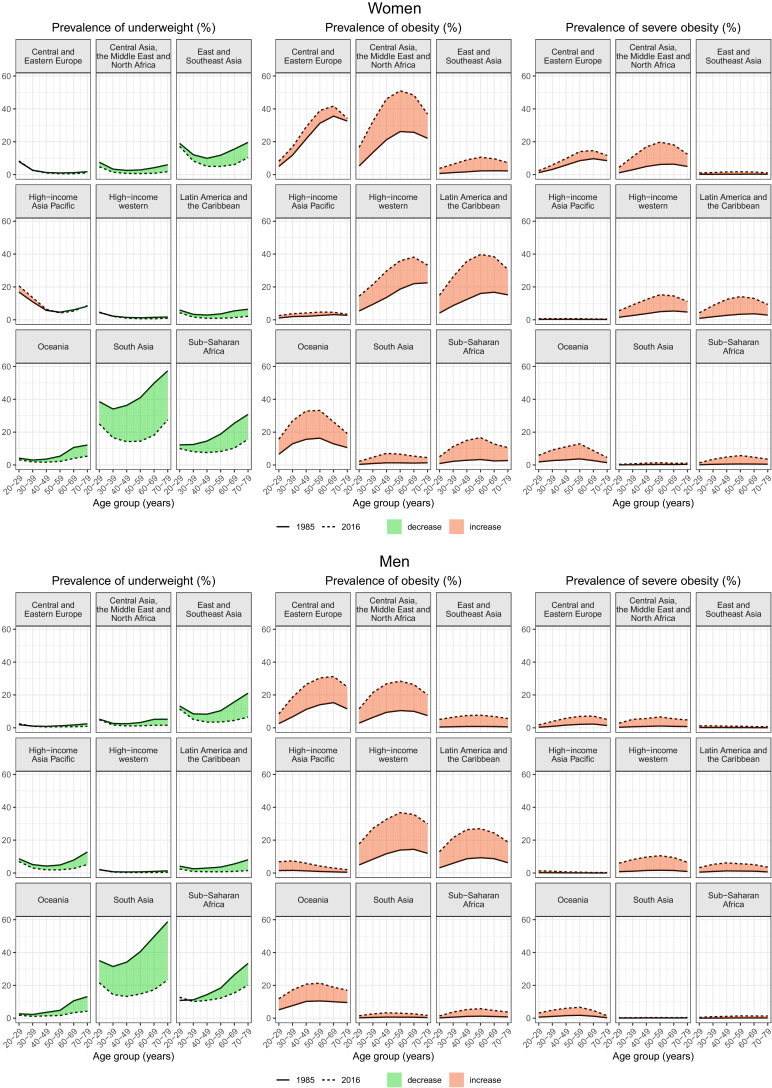
From 1985 to 2016, age-standardised mean BMI increased by 1–4 kg/m2 in all regions, with the exception of women in the high-income Asia Pacific region and Central and Eastern Europe whose mean BMI changed by less than 1 kg/m2 (Figure 3). The prevalence of underweight decreased or stayed unchanged and that of obesity and severe obesity increased from 1985 to 2016 in all regions, with the exception of an increase in the prevalence of underweight in younger women in the high-income Asia Pacific region. The largest absolute decrease in underweight prevalence from 1985 to 2016 was seen in South Asia; East and Southeast Asia; and sub-Saharan Africa, where it declined by 14–35 percentage points in different age–sex groups (Figure 4). Nonetheless, underweight prevalence remained higher in these three regions than elsewhere in 2016. Prevalence of underweight changed only marginally in regions such as Central and Eastern Europe and the high-income western region, where prevalence was already low in 1985.
Figure 3. Change in mean body mass index (BMI) from 1985 to 2016 by region, sex, and age group.
Figure 4. Change in prevalence of underweight, obesity, and severe obesity from 1985 to 2016 by region, sex, and age group.
The largest absolute increase in obesity prevalence from 1985 to 2016 occurred in Central Asia, the Middle East, and North Africa; the high-income western region; Latin America and the Caribbean; Oceania (women); and Central and Eastern Europe (men) (Figure 4). Women in these regions also experienced the largest increase in severe obesity prevalence, along with men in the high-income western region. In these regions and sexes, obesity prevalence increased by 16–24 percentage points in different age groups, and severe obesity increased by 5–13 percentage points. The increase in obesity was less than five percentage points in the high-income Asia Pacific region; South Asia; and in men in sub-Saharan Africa; in the same regions, along with East and Southeast Asia, the increase in severe obesity was less than two percentage points.
Associations of underweight, obesity, and severe obesity prevalence with mean BMI
There was a strong association between the prevalence of underweight, obesity, and severe obesity with mean BMI as measured by R-squared of the regressions of prevalence on mean (Supplementary files 1 and 2). These indicate that 93% (men) and 96% (women) of variation in obesity, and between 83% and 92% of variation in underweight and severe obesity, were explained by mean BMI and other variables (year, region, and age group) in the regression models. The coefficients of the mean BMI terms represent the changes in (probit-transformed) prevalence associated with a unit change in mean BMI, and their interactions with region represent variations in this association across regions. For all three outcomes, the association of prevalence with mean BMI varied across regions.
The inter-regional variation in the prevalence–mean association was stronger for obesity and severe obesity than underweight, as seen in larger inter-regional range of the interaction terms. The extent to which prevalence changes with any variation in mean BMI in each region is an outcome of the main BMI term and its interaction with region; to be epidemiologically interpretable, this will have to be converted from probit-transformed to original prevalence scale. For example, in the year 2016, for women aged 50–59 years, at a mean BMI of 25 kg/m2 (which was approximately the global age-standardised mean level of BMI) (NCD Risk Factor Collaboration (NCD-RisC), 2017a), prevalence of underweight would have varied by seven percentage points across regions, being lowest in Central and Eastern Europe and highest in sub-Saharan Africa; a unit increase in mean BMI would have been associated with a relative change in prevalence ranging from −49% in the high-income Asia Pacific region to −14% in Oceania. Also for women aged 50–59 years and a mean BMI of 25 kg/m2, the prevalence of obesity and severe obesity would both have been the highest in Oceania and the lowest in the high-income Asia Pacific region, with a difference of 12 and 6 percentage points, respectively, for the two outcomes; a unit increase in mean BMI would have been associated with a relative change ranging from 21% to 46% for obesity and from 30% to 59% for severe obesity, the smallest change for both being in Oceania and the largest in East and Southeast Asia. There was similar inter-regional variation in the other year–age–sex strata.
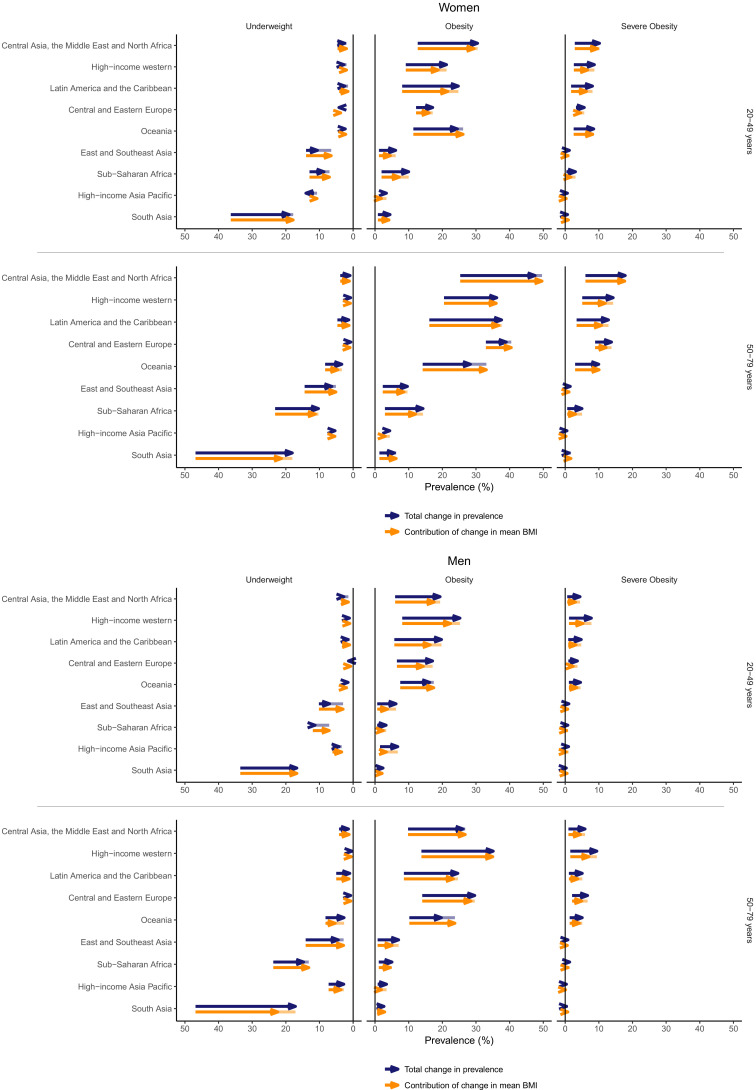
Contribution of mean BMI to changes in underweight and obesity prevalence
The rise in mean BMI accounted for >82% of the decline in underweight in different age–sex groups in South Asia, where underweight prevalence declined by over 16 percentage points for all age–sex groups (Figure 5). The remainder of the decline was due to change in the shape of the BMI distribution which reduced underweight prevalence beyond the effects of the population mean. In contrast, in sub-Saharan Africa and East and Southeast Asia, the total change in prevalence of underweight (3–12 percentage points) was 20–80% less than what was expected based on the increase in mean BMI (Figure 5). In other words, in these regions the underweight tail of the BMI distribution was left behind as the distribution shifted.
Figure 5. Contribution of change in mean body mass index (BMI) to total change from 1985 to 2016 in prevalence of underweight, obesity, or severe obesity by region, sex, and age group.
Blue arrows show the total change in prevalence of underweight, obesity, or severe obesity. Orange arrows show the contribution of change in mean BMI to the change in prevalence. The difference between these two arrows is shown with a line, whose colour follows the shorter arrow.
Where obesity increased the most – Central Asia, the Middle East, and North Africa; Latin America and the Caribbean; and the high-income western region – the rise in mean BMI accounted for over three quarters of the increase in different age–sex groups (Figure 5). In Oceania, the actual rise in prevalence of obesity (8–14 percentage points for all age–sex groups) was about two-thirds to one-half of what would have been expected by the observed increase in mean BMI in men and women (Figure 5). Change in mean BMI consistently accounted for a smaller share of the change in severe obesity than it did for change in total obesity. Specifically, in regions where prevalence of severe obesity changed by more than one percentage point, the contribution of change in mean BMI to change in severe obesity in different regions was 53–90% of the corresponding contribution for total obesity (Figure 5).
In other regions, the change in the prevalence of underweight, obesity, or severe obesity was too small for the contribution of change in mean BMI to be epidemiologically relevant (Figure 5).
Discussion
We found that the trends in the prevalence of underweight, total obesity, and, to a lesser extent, severe obesity are largely driven by shifts in the distribution of BMI, with smaller contributions from changes in the shape of the distribution. The notable exceptions to this pattern were the decline in the prevalence of underweight in East and Southeast Asia and sub-Saharan Africa and the rise of obesity in Oceania, which were both smaller than expected based on change in mean BMI.
Our results are consistent with a recent cross-sectional study (Razak et al., 2018) using data from women in low- and middle-income countries that found a strong association between mean BMI and prevalence of obesity, and a moderate association between mean BMI and prevalence of underweight. Being cross-sectional, this study did not consider changes over time, as we have. Our results are also consistent with another study which found that changes in median BMI contributed more than 75% to the increase in obesity in the USA from 1980 to 2000 (Helmchen and Henderson, 2004).
Previous studies used one or more approaches to investigate changes in population BMI distribution: some analysed percentiles of the BMI distribution (Wagner et al., 2019; Vaezghasemi et al., 2016; Razak et al., 2013; Popkin and Slining, 2013; Popkin, 2010; Peeters et al., 2015; Ouyang et al., 2015; Lebel et al., 2018; Hayes et al., 2015), others focused on the change in prevalence above or below pre-specified BMI thresholds (Wang et al., 2007; Razak et al., 2013; Popkin, 2010; Peeters et al., 2015; Ouyang et al., 2015; Khang and Yun, 2010; Flegal and Troiano, 2000), or evaluated how the shape of the BMI distribution has changed via examining metrics such as standard deviation and skewness (Peeters et al., 2015; Ouyang et al., 2015; Lebel et al., 2018; Khang and Yun, 2010; Hayes et al., 2015; Flegal and Troiano, 2000). Most of these studies reached the same conclusion as our study that, as the BMI distribution shifts upwards, the prevalence of underweight declines somewhat more slowly than the prevalence of obesity rises.
Our study has strengths in scope, data, and methods: the strengths of our study include presenting the first global analysis of how much the rise in mean BMI versus changes in the shape of its distribution influenced changes in both underweight and obesity prevalence. We used an unprecedented amount of data from different regions covering three decades and used only measured data on height and weight to avoid biases in self-reported data.
As with all global analyses, our study has some limitations. Despite using the most comprehensive global collection of population-based studies to date, some regions, especially Oceania and sub-Saharan Africa, had less data, especially early in our analysis period. Further, given the large number of age, sex, and region subgroups of population in our analysis, and its long duration, it was not possible to visually explore how the shape of BMI distribution has changed in the underweight and obesity ranges where changes in the mean did not fully explain change in prevalence. Finally, there are variations in characteristics such as response rate and measurement protocol across studies. Some of these, such as exclusion of studies with self-reported height and weight, were a part of our inclusion and exclusion criteria. Others may affect population mean or prevalence.
The finding that the majority of the rise in the prevalence of obesity from 1985 to 2016 is mostly the result of a distributional shift points towards an important role for societal drivers, including lower availability and higher price of healthy and fresh foods compared to caloric-dense and nutrient-deficient foods (Swinburn et al., 2011), and mechanisation of work and motorisation of transport throughout the world that have reduced energy expenditure in populations around the world (NCD Risk Factor Collaboration (NCD-RisC), 2019; Ng and Popkin, 2012). First, although there is a genetic component to BMI at the individual level (Silventoinen et al., 2017; Silventoinen et al., 2016; Locke et al., 2015; Brandkvist et al., 2019), genetics explain only a small part of changes over time, especially when people have access to healthy food and living environment. When the environment becomes more obesogenic, some people or population subgroups may gain more weight than others, implying that the environment remains the main contributor (Brandkvist et al., 2019). This interplay of genetic predisposition and changes in the environment might account for some of the excess rise in obesity and severe obesity beyond the effect of distributional shift alone (Brandkvist et al., 2019). The exception observed in Oceania is possibly because in 1985 obesity prevalence in this region was already so high (NCD Risk Factor Collaboration (NCD-RisC), 2017a) that the rise in BMI did not change overall obesity status (but there was a substantial increase in those with severe obesity, mostly accounted for by the change in mean BMI). The smaller decline in underweight than expected in sub-Saharan Africa and East and Southeast Asia may be because underweight is associated with lower socioeconomic status, food insecurity, and for sub-Saharan Africa widening difference between rural and urban BMI levels which is different from other regions (NCD Risk Factor Collaboration (NCD-RisC), 2019; Brandkvist et al., 2019; Di Cesare et al., 2015; Subramanian and Smith, 2006; Di Cesare et al., 2013). If the benefits of economic development do not sufficiently reach the poor, they remain nutritionally vulnerable, as has been seen for height and weight during childhood and adolescence (NCD Risk Factor Collaboration (NCD-RisC), 2020; Subramanyam et al., 2011; Sanchez and Swaminathan, 2005; Pongou et al., 2006; Haddad, 2003; Stevens et al., 2012). Together with the rise in mean BMI and obesity (and short stature which is not a topic of this paper but addressed in other studies) (NCD Risk Factor Collaboration (NCD-RisC), 2020; Stevens et al., 2012; NCD Risk Factor Collaboration (NCD-RisC), 2016a), this creates a double burden of malnutrition (Popkin et al., 2020).
In summary, we found that the worldwide rise in obesity and the decline in underweight are primarily driven by the shift in the population distribution of BMI. At the same time, there is an evidence of both excess obesity, and especially severe obesity, and persistent underweight beyond the distributional shift in some regions, which may be related to growing social inequalities that restrict access to healthy foods in those at highest risk of undernutrition (Popkin et al., 2020; Wells et al., 2020; Darmon and Drewnowski, 2015). The response to these trends must motivate ‘double-duty actions’ that prevent and tackle all forms of malnutrition through both fiscal and regulatory restrictions on unhealthy foods, and making healthy foods available, accessible, and affordable especially to those at high risks of underweight and obesity (Powell et al., 2013; Hawkes et al., 2020; Bleich et al., 2017).
Materials and methods
Study design
Our aim was to quantify, for all regions of the world, how much of the change in prevalence of underweight (defined as BMI <18.5 kg/m2), (total) obesity (BMI ≥30 kg/m2), and severe obesity (BMI ≥35 kg/m2) among men and women aged 20–79 years from 1985 to 2016 could be accounted for by change in mean BMI. In the first step, we used data from a global database of human anthropometry to estimate the associations of the prevalence of underweight, prevalence of obesity, or prevalence of severe obesity with population mean BMI, including how the association varies in relation to age group and region. We then used the fitted association to estimate the contribution of change in the population mean BMI to change in the prevalence of underweight, obesity, or severe obesity in different regions.
Data sources
In the first step of the analysis, we estimated the prevalence-mean associations, using data from a comprehensive database on cardiometabolic risk factors collated by NCD-RisC as described below. In the second step, we needed consistent estimates of mean BMI for all regions. For this purpose, we used data from a recent comprehensive analysis of worldwide trends in mean BMI from 1985 to 2016 (NCD Risk Factor Collaboration (NCD-RisC), 2017a) which had fitted a Bayesian hierarchical model to the NCD-RisC data.
Data in the NCD-RisC database were obtained from publicly available multi-country and national measurement surveys (e.g., Demographic and Health Surveys, WHO-STEPwise approach to Surveillance [STEPS] surveys, and those identified via the Inter-University Consortium for Political and Social Research and European Health Interview and Health Examination Surveys Database). With the help of the World Health Organization (WHO) and its regional and country offices as well as the World Heart Federation, we identified and accessed population-based survey data from national health and statistical agencies. We searched and reviewed published studies as detailed previously (NCD Risk Factor Collaboration (NCD-RisC), 2017a) and invited eligible studies to join NCD-RisC, as we did with data holders from earlier pooled analysis of cardiometabolic risk factors (Finucane et al., 2011; Farzadfar et al., 2011; Danaei et al., 2011a; Danaei et al., 2011b).
Data inclusion and exclusion
We carefully checked that each data source met our inclusion criteria as listed below:
measurement data on height and weight were available;
study participants were 5 years of age and older (as described earlier data used here were for those 20–79 years);
data were collected using a probabilistic sampling method with a defined sampling frame;
data were from population samples at the national, sub-national (i.e., covering one or more sub-national regions, with more than three urban or five rural communities), or community level; and
data were from the countries and territories listed in Supplementary file 3.
We excluded all data sources that only used self-reported weight and height without a measurement component because these data are subject to biases that vary with geography, time, age, sex, and socioeconomic characteristics (Tolonen et al., 2014; Hayes et al., 2011; Ezzati et al., 2006). We also excluded data on population subgroups whose anthropometric status may differ systematically from the general population, including
studies that had included or excluded people based on their health status or cardiovascular risk;
studies whose participants were only ethnic minorities;
specific educational, occupational, or socioeconomic subgroups, with the exception noted below; and
those recruited through health facilities, with the exception noted below.
We included school-based data in countries and age–sex groups with enrolment of 70% or higher. We also included data whose sampling frame was health insurance schemes in countries where at least 80% of the population were insured. Finally, we included data collected through general practice and primary care systems in high-income and Central European countries with universal insurance because contact with the primary care systems tends to be as good as or better than the response rates for population-based surveys. The list of data sources with participants aged 20–79 years and their characteristics is provided in Supplementary file 4, with additional information in Source data 1.
Duplicate data were identified by comparing studies from the same country and year, and then discarded. All NCD-RisC members are also periodically asked to review the list of sources from their country, to verify that the included data meet the inclusion criteria and are not duplicates, and to suggest additional sources. The NCD-RisC database is continuously updated through all the above routes. For each data source, we recorded the study population, sampling approach, years of measurement, and measurement methods. Only population-representative data were included, and these were assessed in terms of whether they covered the whole country, multiple sub-national regions, or one or a small number of communities, and whether rural, urban, or both participants were included. All submitted data were checked independently by at least two persons. Questions and clarifications were discussed with NCD-RisC members and resolved before data were incorporated in the database.
We calculated mean BMI and the associated standard errors by sex and age. All analyses incorporated sample weights and complex survey design, when applicable, in calculating summary statistics, with computer code provided to NCD-RisC members who requested assistance.
Additionally, summary statistics for nationally representative data from sources that were identified but not accessed via the above routes were extracted from published reports. Data were also extracted for nine STEPS surveys that were not publicly available, one Countrywide Integrated Non-communicable Diseases Intervention survey, and five sites of the WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) project that were not deposited in the MONICA Data Centre. We also included data from a previous global data pooling study (Finucane et al., 2011) when they had not been accessed as described above.
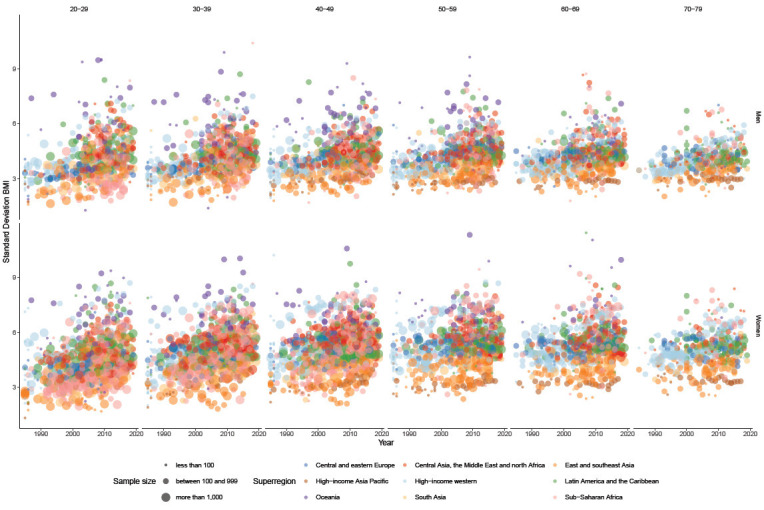
Here, to estimate the association of underweight, obesity, and severe obesity prevalence with mean BMI as described below, we used data collected from 1985 to 2019 with measured height and weight among men and women aged 20–79 years, in 10-year age groups. Data that did not cover the complete 10-year age groups, for example, 25–29 or 60–64 years, were excluded. We included data from study–age–sex strata with a prevalence between 0 and 1 to allow probit transformation and with at least 25 participants in each stratum. These data were summarised into 11,652 study–age–sex-specific pairs of mean and prevalence of adults with underweight, obesity, or severe obesity.
Statistical methods
Anonymised data from studies in the NCD-RisC database were reanalysed according to a common protocol. We calculated mean BMI and prevalence of underweight, obesity, and severe obesity by sex and age group in each study in the NCD-RisC database from 1985 to 2019. We used data through 2019 so that the prevalence–mean association is informed by as much data as possible. All calculations took into account complex survey design where relevant. We excluded study–age–sex groups with less than 25 participants because their means and prevalence have larger uncertainty.
We then estimated the relationship between probit-transformed prevalence of underweight, obesity, and severe obesity and mean BMI in a regression model, separately for each of these prevalences. The correlation coefficient between mean BMI and median BMI was ≥0.98 in different age–sex groups, indicating a strong correlation between the two. In our statistical model, described below, the prevalence of underweight, obesity, or severe obesity depends on population mean BMI as well as on age group, region, and year.
All analyses were done separately for men and women. We chose a probit-transformed prevalence because it changes in an approximately linear manner as the mean changes, thus providing a better fit to the data. The regressions also included age group in 10-year bands, region and the year when the data were collected. The regions, used in previous analyses of cardiometabolic risk factors (NCD Risk Factor Collaboration (NCD-RisC), 2017a; NCD Risk Factor Collaboration (NCD-RisC), 2019; NCD Risk Factor Collaboration (NCD-RisC), 2020; NCD Risk Factor Collaboration (NCD-RisC), 2016a; NCD Risk Factor Collaboration (NCD-RisC), 2018; NCD Risk Factor Collaboration (NCD-RisC), 2017b; NCD Risk Factor Collaboration (NCD-RisC), 2016b; NCD Risk Factor Collaboration (NCD-RisC), 2016c), were Central and Eastern Europe; Central Asia, the Middle East, and North Africa; East and Southeast Asia; high-income Asia Pacific region; high-income western region; Latin America and the Caribbean; Oceania; South Asia; and sub-Saharan Africa. Countries in each region are listed in Supplementary file 3. The model also included interactions between mean BMI and age group, mean BMI and region, age group and region, age group and year, and year and region. These terms allowed the prevalence–mean association to vary by age group, region, and over time. The models were fitted in statistical software R (version 4.0.2) (Source code 1). The coefficients of the regression models are presented in Supplementary files 1 and 2.
We used the fitted regressions to quantify how much of the change over time in the prevalence of underweight, obesity, or severe obesity in each region and age group can be explained by the corresponding change in mean BMI. To do so, we first used the region- and age–sex-specific mean BMI in 1985 and 2016 in the fitted association and then estimated the total change in prevalence of underweight, obesity, or severe obesity by region. The mean BMI values were from a recent comprehensive analysis of worldwide trends in mean BMI (NCD Risk Factor Collaboration (NCD-RisC), 2017a) and are listed in Supplementary file 5. We then calculated the contribution of change in mean BMI to the change in prevalence of underweight or obesity by allowing mean BMI for each age group and region to change over time, while keeping year fixed at 1985. Results were calculated by 10-year age group and then aggregated into two age bands, 20–49 and 50–79 years, by taking weighted average of age-specific results using weights from the WHO standard population (Ahmad et al., 2001).
Acknowledgements
We thank WHO country and regional offices and World Heart Federation for support in data identification and access. The NCD-RisC database was funded by the Wellcome Trust. Maria LC Iurilli was supported by a Medical Research Council studentship. Sylvain Sebert received funding by the European Commission with grant agreements 633595 and 874739, respectively, for the DynaHEALTH and LongITools projects. The following contributors have deceased: Konrad Jamrozik, Altan Onat, Robespierre Ribeiro, Michael Sjöström, Agustinus Soemantri, Jutta Stieber, and Dimitrios Trichopoulos. The list of authors shows their last affiliation.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
NCD Risk Factor Collaboration (NCD-RisC), Email: majid.ezzati@imperial.ac.uk, s.filippi@imperial.ac.uk.
Christine M Friedenreich, University of Calgary, Canada.
Eduardo Franco, McGill University, Canada.
NCD Risk Factor Collaboration (NCD-RisC):
Maria LC Iurilli, Bin Zhou, James E Bennett, Rodrigo M Carrillo-Larco, Marisa K Sophiea, Andrea Rodriguez-Martinez, Honor Bixby, Bethlehem D Solomon, Cristina Taddei, Goodarz Danaei, Mariachiara Di Cesare, Gretchen A Stevens, Leanne M Riley, Stefan Savin, Melanie J Cowan, Pascal Bovet, Albertino Damasceno, Adela Chirita-Emandi, Alison J Hayes, Nayu Ikeda, Rod T Jackson, Young-Ho Khang, Avula Laxmaiah, Jing Liu, J Jaime Miranda, Olfa Saidi, Sylvain Sebert, Maroje Sorić, Gregor Starc, Edward W Gregg, Leandra Abarca-Gómez, Ziad A Abdeen, Shynar Abdrakhmanova, Suhaila Abdul Ghaffar, Hanan F Abdul Rahim, Niveen M Abu-Rmeileh, Jamila Abubakar Garba, Benjamin Acosta-Cazares, Robert J Adams, Wichai Aekplakorn, Kaosar Afsana, Shoaib Afzal, Imelda A Agdeppa, Javad Aghazadeh-Attari, Carlos A Aguilar-Salinas, Charles Agyemang, Mohamad Hasnan Ahmad, Noor Ani Ahmad, Ali Ahmadi, Naser Ahmadi, Soheir H Ahmed, Wolfgang Ahrens, Gulmira Aitmurzaeva, Kamel Ajlouni, Hazzaa M Al-Hazzaa, Badreya Al-Lahou, Rajaa Al-Raddadi, Monira Alarouj, Fadia AlBuhairan, Shahla AlDhukair, Mohamed M Ali, Abdullah Alkandari, Ala'a Alkerwi, Kristine Allin, Mar Alvarez-Pedrerol, Eman Aly, Deepak N Amarapurkar, Parisa Amiri, Norbert Amougou, Philippe Amouyel, Lars Bo Andersen, Sigmund A Anderssen, Lars Ängquist, Ranjit Mohan Anjana, Alireza Ansari-Moghaddam, Hajer Aounallah-Skhiri, Joana Araújo, Inger Ariansen, Tahir Aris, Raphael E Arku, Nimmathota Arlappa, Krishna K Aryal, Thor Aspelund, Felix K Assah, Maria Cecília F Assunção, May Soe Aung, Juha Auvinen, Mária Avdicová, Shina Avi, Ana Azevedo, Mohsen Azimi-Nezhad, Fereidoun Azizi, Mehrdad Azmin, Bontha V Babu, Maja Bæksgaard Jørgensen, Azli Baharudin, Suhad Bahijri, Jennifer L Baker, Nagalla Balakrishna, Mohamed Bamoshmoosh, Maciej Banach, Piotr Bandosz, José R Banegas, Joanna Baran, Carlo M Barbagallo, Alberto Barceló, Amina Barkat, Aluisio JD Barros, Mauro Virgílio Gomes Barros, Abdul Basit, Joao Luiz D Bastos, Iqbal Bata, Anwar M Batieha, Rosangela L Batista, Zhamilya Battakova, Assembekov Batyrbek, Louise A Baur, Robert Beaglehole, Silvia Bel-Serrat, Antonisamy Belavendra, Habiba Ben Romdhane, Judith Benedics, Mikhail Benet, Ingunn Holden Bergh, Salim Berkinbayev, Antonio Bernabe-Ortiz, Gailute Bernotiene, Heloísa Bettiol, Jorge Bezerra, Aroor Bhagyalaxmi, Sumit Bharadwaj, Santosh K Bhargava, Zulfiqar A Bhutta, Hongsheng Bi, Yufang Bi, Daniel Bia, Elysée Claude Bika Lele, Mukharram M Bikbov, Bihungum Bista, Dusko J Bjelica, Peter Bjerregaard, Espen Bjertness, Marius B Bjertness, Cecilia Björkelund, Katia V Bloch, Anneke Blokstra, Simona Bo, Martin Bobak, Lynne M Boddy, Bernhard O Boehm, Heiner Boeing, Jose G Boggia, Elena Bogova, Carlos P Boissonnet, Stig E Bojesen, Marialaura Bonaccio, Vanina Bongard, Alice Bonilla-Vargas, Matthias Bopp, Herman Borghs, Lien Braeckevelt, Lutgart Braeckman, Marjolijn CE Bragt, Imperia Brajkovich, Francesco Branca, Juergen Breckenkamp, João Breda, Hermann Brenner, Lizzy M Brewster, Garry R Brian, Lacramioara Brinduse, Sinead Brophy, Graziella Bruno, H Bas Bueno-de-Mesquita, Anna Bugge, Marta Buoncristiano, Genc Burazeri, Con Burns, Antonio Cabrera de León, Joseph Cacciottolo, Hui Cai, Tilema Cama, Christine Cameron, José Camolas, Günay Can, Ana Paula C Cândido, Felicia Cañete, Mario V Capanzana, Nadežda Capková, Eduardo Capuano, Vincenzo Capuano, Marloes Cardol, Viviane C Cardoso, Axel C Carlsson, Esteban Carmuega, Joana Carvalho, José A Casajús, Felipe F Casanueva, Ertugrul Celikcan, Laura Censi, Marvin Cervantes-Loaiza, Juraci A Cesar, Snehalatha Chamukuttan, Angelique W Chan, Queenie Chan, Himanshu K Chaturvedi, Nish Chaturvedi, Norsyamlina Che Abdul Rahim, Miao Li Chee, Chien-Jen Chen, Fangfang Chen, Huashuai Chen, Shuohua Chen, Zhengming Chen, Ching-Yu Cheng, Bahman Cheraghian, Angela Chetrit, Ekaterina Chikova-Iscener, Arnaud Chiolero, Shu-Ti Chiou, María-Dolores Chirlaque, Belong Cho, Kaare Christensen, Diego G Christofaro, Jerzy Chudek, Renata Cifkova, Michelle Cilia, Eliza Cinteza, Frank Claessens, Janine Clarke, Els Clays, Emmanuel Cohen, Hans Concin, Susana C Confortin, Cyrus Cooper, Tara C Coppinger, Eva Corpeleijn, Simona Costanzo, Dominique Cottel, Chris Cowell, Cora L Craig, Amelia C Crampin, Ana B Crujeiras, Semánová Csilla, Alexandra M Cucu, Liufu Cui, Felipe V Cureau, Ewelina Czenczek-Lewandowska, Graziella D'Arrigo, Eleonora d'Orsi, Liliana Dacica, María Ángeles Dal Re Saavedra, Jean Dallongeville, Camilla T Damsgaard, Rachel Dankner, Thomas M Dantoft, Parasmani Dasgupta, Saeed Dastgiri, Luc Dauchet, Kairat Davletov, Guy De Backer, Dirk De Bacquer, Giovanni de Gaetano, Stefaan De Henauw, Paula Duarte de Oliveira, David De Ridder, Karin De Ridder, Susanne R de Rooij, Delphine De Smedt, Mohan Deepa, Alexander D Deev, Vincent Jr DeGennaro, Abbas Dehghan, Hélène Delisle, Francis Delpeuch, Stefaan Demarest, Elaine Dennison, Katarzyna Dereń, Valérie Deschamps, Meghnath Dhimal, Augusto F Di Castelnuovo, Juvenal Soares Dias-da-Costa, María Elena Díaz-Sánchez, Alejandro Diaz, Zivka Dika, Shirin Djalalinia, Visnja Djordjic, Ha TP Do, Annette J Dobson, Maria Benedetta Donati, Chiara Donfrancesco, Silvana P Donoso, Angela Döring, Maria Dorobantu, Ahmad Reza Dorosty, Kouamelan Doua, Nico Dragano, Wojciech Drygas, Jia Li Duan, Charmaine A Duante, Priscilla Duboz, Rosemary B Duda, Vesselka Duleva, Virginija Dulskiene, Samuel C Dumith, Anar Dushpanova, Vilnis Dzerve, Elzbieta Dziankowska-Zaborszczyk, Ricky Eddie, Ebrahim Eftekhar, Eruke E Egbagbe, Robert Eggertsen, Sareh Eghtesad, Gabriele Eiben, Ulf Ekelund, Mohammad El-Khateeb, Jalila El Ati, Denise Eldemire-Shearer, Marie Eliasen, Paul Elliott, Reina Engle-Stone, Macia Enguerran, Rajiv T Erasmus, Raimund Erbel, Cihangir Erem, Louise Eriksen, Johan G Eriksson, Jorge Escobedo-de la Peña, Saeid Eslami, Ali Esmaeili, Alun Evans, David Faeh, Albina A Fakhretdinova, Caroline H Fall, Elnaz Faramarzi, Mojtaba Farjam, Victoria Farrugia Sant'Angelo, Farshad Farzadfar, Mohammad Reza Fattahi, Asher Fawwad, Francisco J Felix-Redondo, Trevor S Ferguson, Romulo A Fernandes, Daniel Fernández-Bergés, Daniel Ferrante, Thomas Ferrao, Marika Ferrari, Marco M Ferrario, Catterina Ferreccio, Eldridge Ferrer, Jean Ferrieres, Thamara Hubler Figueiró, Anna Fijalkowska, Günther Fink, Krista Fischer, Leng Huat Foo, Maria Forsner, Heba M Fouad, Damian K Francis, Maria do Carmo Franco, Ruth Frikke-Schmidt, Guillermo Frontera, Flavio D Fuchs, Sandra C Fuchs, Isti I Fujiati, Yuki Fujita, Matsuda Fumihiko, Takuro Furusawa, Zbigniew Gaciong, Mihai Gafencu, Andrzej Galbarczyk, Henrike Galenkamp, Daniela Galeone, Myriam Galfo, Fabio Galvano, Jingli Gao, Manoli Garcia-de-la-Hera, Marta García-Solano, Dickman Gareta, Sarah P Garnett, Jean-Michel Gaspoz, Magda Gasull, Adroaldo Cesar Araujo Gaya, Anelise Reis Gaya, Andrea Gazzinelli, Ulrike Gehring, Harald Geiger, Johanna M Geleijnse, Ali Ghanbari, Erfan Ghasemi, Oana-Florentina Gheorghe-Fronea, Simona Giampaoli, Francesco Gianfagna, Tiffany K Gill, Jonathan Giovannelli, Glen Gironella, Aleksander Giwercman, Konstantinos Gkiouras, Justyna Godos, Sibel Gogen, Marcel Goldberg, Rebecca A Goldsmith, David Goltzman, Santiago F Gómez, Aleksandra Gomula, Bruna Goncalves Cordeiro da Silva, Helen Gonçalves, David A Gonzalez-Chica, Marcela Gonzalez-Gross, Margot González-Leon, Juan P González-Rivas, Clicerio González-Villalpando, María-Elena González-Villalpando, Angel R Gonzalez, Frederic Gottrand, Antonio Pedro Graça, Sidsel Graff-Iversen, Dušan Grafnetter, Aneta Grajda, Maria G Grammatikopoulou, Ronald D Gregor, Tomasz Grodzicki, Else Karin Grøholt, Anders Grøntved, Giuseppe Grosso, Gabriella Gruden, Dongfeng Gu, Emanuela Gualdi-Russo, Pilar Guallar-Castillón, Andrea Gualtieri, Elias F Gudmundsson, Vilmundur Gudnason, Ramiro Guerrero, Idris Guessous, Andre L Guimaraes, Martin C Gulliford, Johanna Gunnlaugsdottir, Marc J Gunter, Xiu-Hua Guo, Yin Guo, Prakash C Gupta, Rajeev Gupta, Oye Gureje, Beata Gurzkowska, Enrique Gutiérrez-González, Laura Gutierrez, Felix Gutzwiller, Seongjun Ha, Farzad Hadaegh, Charalambos A Hadjigeorgiou, Rosa Haghshenas, Hamid Hakimi, Jytte Halkjær, Ian R Hambleton, Behrooz Hamzeh, Dominique Hange, Abu AM Hanif, Sari Hantunen, Jie Hao, Rachakulla Hari Kumar, Seyed Mohammad Hashemi-Shahri, Maria Hassapidou, Jun Hata, Teresa Haugsgjerd, Jiang He, Yuan He, Yuna He, Regina Heidinger-Felso, Mirjam Heinen, Tatjana Hejgaard, Marleen Elisabeth Hendriks, Rafael dos Santos Henrique, Ana Henriques, Leticia Hernandez Cadena, Sauli Herrala, Victor M Herrera, Isabelle Herter-Aeberli, Ramin Heshmat, Allan G Hill, Sai Yin Ho, Suzanne C Ho, Michael Hobbs, Michelle Holdsworth, Reza Homayounfar, Clara Homs, Wilma M Hopman, Andrea RVR Horimoto, Claudia M Hormiga, Bernardo L Horta, Leila Houti, Christina Howitt, Thein Thein Htay, Aung Soe Htet, Maung Maung Than Htike, Yonghua Hu, José María Huerta, Ilpo Tapani Huhtaniemi, Laetitia Huiart, Constanta Huidumac Petrescu, Martijn Huisman, Abdullatif Husseini, Chinh Nguyen Huu, Inge Huybrechts, Nahla Hwalla, Jolanda Hyska, Licia Iacoviello, Jesús M Ibarluzea, Mohsen M Ibrahim, Norazizah Ibrahim Wong, M Arfan Ikram, Violeta Iotova, Vilma E Irazola, Takafumi Ishida, Muhammad Islam, Sheikh Mohammed Shariful Islam, Masanori Iwasaki, Jeremy M Jacobs, Hashem Y Jaddou, Tazeen Jafar, Kenneth James, Kazi M Jamil, Konrad Jamrozik, Imre Janszky, Edward Janus, Juel Jarani, Marjo-Riitta Jarvelin, Grazyna Jasienska, Ana Jelakovic, Bojan Jelakovic, Garry Jennings, Anjani Kumar Jha, Chao Qiang Jiang, Ramon O Jimenez, Karl-Heinz Jöckel, Michel Joffres, Mattias Johansson, Jari J Jokelainen, Jost B Jonas, Jitendra Jonnagaddala, Torben Jørgensen, Pradeep Joshi, Farahnaz Joukar, Dragana P Jovic, Jacek J Jóźwiak, Anne Juolevi, Gregor Jurak, Iulia Jurca Simina, Vesna Juresa, Rudolf Kaaks, Felix O Kaducu, Anthony Kafatos, Eero O Kajantie, Zhanna Kalmatayeva, Ofra Kalter-Leibovici, Yves Kameli, Freja B Kampmann, Kodanda R Kanala, Srinivasan Kannan, Efthymios Kapantais, Argyro Karakosta, Line L Kårhus, Khem B Karki, Marzieh Katibeh, Joanne Katz, Peter T Katzmarzyk, Jussi Kauhanen, Prabhdeep Kaur, Maryam Kavousi, Gyulli M Kazakbaeva, Ulrich Keil, Lital Keinan Boker, Sirkka Keinänen-Kiukaanniemi, Roya Kelishadi, Cecily Kelleher, Han CG Kemper, Andre P Kengne, Maryam Keramati, Alina Kerimkulova, Mathilde Kersting, Timothy Key, Yousef Saleh Khader, Davood Khalili, Kay-Tee Khaw, Bahareh Kheiri, Motahareh Kheradmand, Alireza Khosravi, Ilse MSL Khouw, Ursula Kiechl-Kohlendorfer, Stefan Kiechl, Japhet Killewo, Dong Wook Kim, Hyeon Chang Kim, Jeongseon Kim, Jenny M Kindblom, Heidi Klakk, Magdalena Klimek, Jeannette Klimont, Jurate Klumbiene, Michael Knoflach, Bhawesh Koirala, Elin Kolle, Patrick Kolsteren, Jürgen König, Raija Korpelainen, Paul Korrovits, Magdalena Korzycka, Jelena Kos, Seppo Koskinen, Katsuyasu Kouda, Viktoria A Kovacs, Sudhir Kowlessur, Slawomir Koziel, Jana Kratenova, Wolfgang Kratzer, Susi Kriemler, Peter Lund Kristensen, Steinar Krokstad, Daan Kromhout, Herculina S Kruger, Ruzena Kubinova, Renata Kuciene, Urho M Kujala, Enisa Kujundzic, Zbigniew Kulaga, R Krishna Kumar, Marie Kunešová, Pawel Kurjata, Yadlapalli S Kusuma, Kari Kuulasmaa, Catherine Kyobutungi, Quang Ngoc La, Fatima Zahra Laamiri, Tiina Laatikainen, Carl Lachat, Youcef Laid, Tai Hing Lam, Christina-Paulina Lambrinou, Edwige Landais, Vera Lanska, Georg Lappas, Bagher Larijani, Tint Swe Latt, Laura Lauria, Maria Lazo-Porras, Gwenaëlle Le Coroller, Khanh Le Nguyen Bao, Agnès Le Port, Tuyen D Le, Jeannette Lee, Jeonghee Lee, Paul H Lee, Nils Lehmann, Terho Lehtimäki, Daniel Lemogoum, Naomi S Levitt, Yanping Li, Merike Liivak, Christa L Lilly, Wei-Yen Lim, M Fernanda Lima-Costa, Hsien-Ho Lin, Xu Lin, Yi-Ting Lin, Lars Lind, Allan Linneberg, Lauren Lissner, Mieczyslaw Litwin, Lijuan Liu, Wei-Cheng Lo, Helle-Mai Loit, Khuong Quynh Long, Luis Lopes, Oscar Lopes, Esther Lopez-Garcia, Tania Lopez, Paulo A Lotufo, José Eugenio Lozano, Janice L Lukrafka, Dalia Luksiene, Annamari Lundqvist, Robert Lundqvist, Nuno Lunet, Charles Lunogelo, Michala Lustigová, Edyta Łuszczki, Guansheng Ma, Jun Ma, Xu Ma, George LL Machado-Coelho, Aristides M Machado-Rodrigues, Luisa M Macieira, Ahmed A Madar, Stefania Maggi, Dianna J Magliano, Sara Magnacca, Emmanuella Magriplis, Gowri Mahasampath, Bernard Maire, Marjeta Majer, Marcia Makdisse, Päivi Mäki, Fatemeh Malekzadeh, Reza Malekzadeh, Rahul Malhotra, Kodavanti Mallikharjuna Rao, Sofia K Malyutina, Lynell V Maniego, Yannis Manios, Jim I Mann, Fariborz Mansour-Ghanaei, Enzo Manzato, Paula Margozzini, Anastasia Markaki, Oonagh Markey, Eliza Markidou Ioannidou, Pedro Marques-Vidal, Larissa Pruner Marques, Jaume Marrugat, Yves Martin-Prevel, Rosemarie Martin, Reynaldo Martorell, Eva Martos, Katharina Maruszczak, Stefano Marventano, Luis P Mascarenhas, Shariq R Masoodi, Ellisiv B Mathiesen, Prashant Mathur, Alicia Matijasevich, Tandi E Matsha, Christina Mavrogianni, Artur Mazur, Jean Claude N Mbanya, Shelly R McFarlane, Stephen T McGarvey, Martin McKee, Stela McLachlan, Rachael M McLean, Scott B McLean, Breige A McNulty, Sounnia Mediene Benchekor, Jurate Medzioniene, Parinaz Mehdipour, Kirsten Mehlig, Amir Houshang Mehrparvar, Aline Meirhaeghe, Jørgen Meisfjord, Christa Meisinger, Ana Maria B Menezes, Geetha R Menon, Gert BM Mensink, Maria Teresa Menzano, Alibek Mereke, Indrapal I Meshram, Andres Metspalu, Haakon E Meyer, Jie Mi, Kim F Michaelsen, Nathalie Michels, Kairit Mikkel, Karolina Milkowska, Jody C Miller, Cláudia S Minderico, GK Mini, Juan Francisco Miquel, Mohammad Reza Mirjalili, Daphne Mirkopoulou, Erkin Mirrakhimov, Marjeta Mišigoj-Durakovic, Antonio Mistretta, Veronica Mocanu, Pietro A Modesti, Sahar Saeedi Moghaddam, Bahram Mohajer, Mostafa K Mohamed, Shukri F Mohamed, Kazem Mohammad, Zahra Mohammadi, Noushin Mohammadifard, Reza Mohammadpourhodki, Viswanathan Mohan, Salim Mohanna, Muhammad Fadhli Mohd Yusoff, Iraj Mohebbi, Farnam Mohebi, Marie Moitry, Drude Molbo, Line T Møllehave, Niels C Møller, Dénes Molnár, Amirabbas Momenan, Charles K Mondo, Michele Monroy-Valle, Eric Monterrubio-Flores, Kotsedi Daniel K Monyeki, Jin Soo Moon, Mahmood Moosazadeh, Leila B Moreira, Alain Morejon, Luis A Moreno, Karen Morgan, Suzanne N Morin, Erik Lykke Mortensen, George Moschonis, Malgorzata Mossakowska, Aya Mostafa, Anabela Mota-Pinto, Jorge Mota, Mohammad Esmaeel Motlagh, Jorge Motta, Marcos André Moura-dos-Santos, Malay K Mridha, Kelias P Msyamboza, Thet Thet Mu, Magdalena Muc, Boban Mugoša, Maria L Muiesan, Parvina Mukhtorova, Martina Müller-Nurasyid, Neil Murphy, Jaakko Mursu, Elaine M Murtagh, Kamarul Imran Musa, Sanja Music Milanovic, Vera Musil, Norlaila Mustafa, Iraj Nabipour, Shohreh Naderimagham, Gabriele Nagel, Balkish M Naidu, Farid Najafi, Harunobu Nakamura, Jana Námešná, Ei Ei K Nang, Vinay B Nangia, Martin Nankap, Sameer Narake, Paola Nardone, Matthias Nauck, William A Neal, Azim Nejatizadeh, Chandini Nekkantti, Keiu Nelis, Liis Nelis, Ilona Nenko, Martin Neovius, Flavio Nervi, Chung T Nguyen, Nguyen D Nguyen, Quang Ngoc Nguyen, Ramfis E Nieto-Martínez, Yury P Nikitin, Guang Ning, Toshiharu Ninomiya, Sania Nishtar, Marianna Noale, Oscar A Noboa, Helena Nogueira, Teresa Norat, Maria Nordendahl, Børge G Nordestgaard, Davide Noto, Natalia Nowak-Szczepanska, Mohannad Al Nsour, Irfan Nuhoglu, Eha Nurk, Terence W O'Neill, Dermot O'Reilly, Galina Obreja, Caleb Ochimana, Angélica M Ochoa-Avilés, Eiji Oda, Kyungwon Oh, Kumiko Ohara, Claes Ohlsson, Ryutaro Ohtsuka, Örn Olafsson, Maria Teresa A Olinto, Isabel O Oliveira, Mohd Azahadi Omar, Altan Onat, Sok King Ong, Lariane M Ono, Pedro Ordunez, Rui Ornelas, Ana P Ortiz, Pedro J Ortiz, Merete Osler, Clive Osmond, Sergej M Ostojic, Afshin Ostovar, Johanna A Otero, Kim Overvad, Ellis Owusu-Dabo, Fred Michel Paccaud, Cristina Padez, Ioannis Pagkalos, Elena Pahomova, Karina Mary de Paiva, Andrzej Pajak, Domenico Palli, Alberto Palloni, Luigi Palmieri, Wen-Harn Pan, Songhomitra Panda-Jonas, Arvind Pandey, Francesco Panza, Dimitrios Papandreou, Soon-Woo Park, Suyeon Park, Winsome R Parnell, Mahboubeh Parsaeian, Ionela M Pascanu, Patrick Pasquet, Nikhil D Patel, Ivan Pecin, Mangesh S Pednekar, Nasheeta Peer, Gao Pei, Sergio Viana Peixoto, Markku Peltonen, Alexandre C Pereira, Marco A Peres, Napoleón Pérez-Farinós, Cynthia M Pérez, Valentina Peterkova, Annette Peters, Astrid Petersmann, Janina Petkeviciene, Ausra Petrauskiene, Emanuela Pettenuzzo, Niloofar Peykari, Son Thai Pham, Rafael N Pichardo, Daniela Pierannunzio, Iris Pigeot, Hynek Pikhart, Aida Pilav, Lorenza Pilotto, Francesco Pistelli, Freda Pitakaka, Aleksandra Piwonska, Andreia N Pizarro, Pedro Plans-Rubió, Bee Koon Poh, Hermann Pohlabeln, Raluca M Pop, Stevo R Popovic, Miquel Porta, Georg Posch, Anil Poudyal, Dimitrios Poulimeneas, Hamed Pouraram, Farhad Pourfarzi, Akram Pourshams, Hossein Poustchi, Rajendra Pradeepa, Alison J Price, Jacqueline F Price, Rui Providencia, Jardena J Puder, Iveta Pudule, Soile E Puhakka, Maria Puiu, Margus Punab, Radwan F Qasrawi, Mostafa Qorbani, Tran Quoc Bao, Ivana Radic, Ricardas Radisauskas, Salar Rahimikazerooni, Mahfuzar Rahman, Mahmudur Rahman, Olli Raitakari, Manu Raj, Ellina Rakhimova, Sherali Rakhmatulloev, Ivo Rakovac, Sudha Ramachandra Rao, Ambady Ramachandran, Jacqueline Ramke, Elisabete Ramos, Rafel Ramos, Lekhraj Rampal, Sanjay Rampal, Vayia Rarra, Ramon A Rascon-Pacheco, Mette Rasmussen, Cassiano Ricardo Rech, Josep Redon, Paul Ferdinand M Reganit, Valéria Regecová, Luis Revilla, Abbas Rezaianzadeh, Lourdes Ribas-Barba, Robespierre Ribeiro, Elio Riboli, Adrian Richter, Fernando Rigo, Natascia Rinaldo, Tobias F Rinke de Wit, Ana Rito, Raphael M Ritti-Dias, Juan A Rivera, Cynthia Robitaille, Romana Roccaldo, Daniela Rodrigues, Fernando Rodríguez-Artalejo, María del Cristo Rodriguez-Perez, Laura A Rodríguez-Villamizar, Ulla Roggenbuck, Rosalba Rojas-Martinez, Nipa Rojroongwasinkul, Dora Romaguera, Elisabetta L Romeo, Rafaela V Rosario, Annika Rosengren, Ian Rouse, Joel GR Roy, Adolfo Rubinstein, Frank J Rühli, Jean-Bernard Ruidavets, Blanca Sandra Ruiz-Betancourt, Maria Ruiz-Castell, Emma Ruiz Moreno, Iuliia A Rusakova, Kenisha Russell Jonsson, Paola Russo, Petra Rust, Marcin Rutkowski, Charumathi Sabanayagam, Elena Sacchini, Harshpal S Sachdev, Alireza Sadjadi, Ali Reza Safarpour, Saeid Safiri, Nader Saki, Benoit Salanave, Eduardo Salazar Martinez, Diego Salmerón, Veikko Salomaa, Jukka T Salonen, Massimo Salvetti, Margarita Samoutian, Jose Sánchez-Abanto, Sandjaja, Susana Sans, Loreto Santa Marina, Diana A Santos, Ina S Santos, Lèlita C Santos, Maria Paula Santos, Osvaldo Santos, Rute Santos, Sara Santos Sanz, Jouko L Saramies, Luis B Sardinha, Nizal Sarrafzadegan, Thirunavukkarasu Sathish, Kai-Uwe Saum, Savvas Savva, Mathilde Savy, Norie Sawada, Mariana Sbaraini, Marcia Scazufca, Beatriz D Schaan, Angelika Schaffrath Rosario, Herman Schargrodsky, Anja Schienkiewitz, Sabine Schipf, Carsten O Schmidt, Ida Maria Schmidt, Peter Schnohr, Ben Schöttker, Sara Schramm, Stine Schramm, Helmut Schröder, Constance Schultsz, Aletta E Schutte, Aye Aye Sein, Rusidah Selamat, Vedrana Sember, Abhijit Sen, Idowu O Senbanjo, Sadaf G Sepanlou, Victor Sequera, Luis Serra-Majem, Jennifer Servais, Ludmila Ševcíková, Svetlana A Shalnova, Teresa Shamah-Levy, Morteza Shamshirgaran, Coimbatore Subramaniam Shanthirani, Maryam Sharafkhah, Sanjib K Sharma, Jonathan E Shaw, Amaneh Shayanrad, Ali Akbar Shayesteh, Lela Shengelia, Zumin Shi, Kenji Shibuya, Hana Shimizu-Furusawa, Dong Wook Shin, Majid Shirani, Rahman Shiri, Namuna Shrestha, Khairil Si-Ramlee, Alfonso Siani, Rosalynn Siantar, Abla M Sibai, Antonio M Silva, Diego Augusto Santos Silva, Mary Simon, Judith Simons, Leon A Simons, Agneta Sjöberg, Michael Sjöström, Gry Skodje, Jolanta Slowikowska-Hilczer, Przemyslaw Slusarczyk, Liam Smeeth, Hung-Kwan So, Fernanda Cunha Soares, Grzegorz Sobek, Eugène Sobngwi, Morten Sodemann, Stefan Söderberg, Moesijanti YE Soekatri, Agustinus Soemantri, Reecha Sofat, Vincenzo Solfrizzi, Mohammad Hossein Somi, Emily Sonestedt, Yi Song, Thorkild IA Sørensen, Elin P Sørgjerd, Charles Sossa Jérome, Victoria E Soto-Rojas, Aïcha Soumaré, Slavica Sovic, Bente Sparboe-Nilsen, Karen Sparrenberger, Angela Spinelli, Igor Spiroski, Jan A Staessen, Hanspeter Stamm, Maria G Stathopoulou, Kaspar Staub, Bill Stavreski, Jostein Steene-Johannessen, Peter Stehle, Aryeh D Stein, George S Stergiou, Jochanan Stessman, Ranko Stevanovic, Jutta Stieber, Doris Stöckl, Tanja Stocks, Jakub Stokwiszewski, Ekaterina Stoyanova, Gareth Stratton, Karien Stronks, Maria Wany Strufaldi, Lela Sturua, Ramón Suárez-Medina, Machi Suka, Chien-An Sun, Johan Sundström, Yn-Tz Sung, Jordi Sunyer, Paibul Suriyawongpaisal, Boyd A Swinburn, Rody G Sy, Holly E Syddall, René Charles Sylva, Moyses Szklo, Lucjan Szponar, E Shyong Tai, Mari-Liis Tammesoo, Abdonas Tamosiunas, Eng Joo Tan, Xun Tang, Maya Tanrygulyyeva, Frank Tanser, Yong Tao, Mohammed Rasoul Tarawneh, Jakob Tarp, Carolina B Tarqui-Mamani, Radka Taxová Braunerová, Anne Taylor, Julie Taylor, Félicité Tchibindat, William R Tebar, Grethe S Tell, Tania Tello, Yih Chung Tham, KR Thankappan, Holger Theobald, Xenophon Theodoridis, Lutgarde Thijs, Nihal Thomas, Betina H Thuesen, Lubica Tichá, Erik J Timmermans, Anne Tjonneland, Hanna K Tolonen, Janne S Tolstrup, Murat Topbas, Roman Topór-Madry, Liv Elin Torheim, María José Tormo, Michael J Tornaritis, Maties Torrent, Laura Torres-Collado, Stefania Toselli, Giota Touloumi, Pierre Traissac, Thi Tuyet-Hanh Tran, Dimitrios Trichopoulos, Antonia Trichopoulou, Oanh TH Trinh, Atul Trivedi, Lechaba Tshepo, Maria Tsigga, Shoichiro Tsugane, Azaliia M Tuliakova, Marshall K Tulloch-Reid, Fikru Tullu, Tomi-Pekka Tuomainen, Jaakko Tuomilehto, Maria L Turley, Gilad Twig, Per Tynelius, Themistoklis Tzotzas, Christophe Tzourio, Peter Ueda, Eunice Ugel, Flora AM Ukoli, Hanno Ulmer, Belgin Unal, Zhamyila Usupova, Hannu MT Uusitalo, Nalan Uysal, Justina Vaitkeviciute, Gonzalo Valdivia, Susana Vale, Damaskini Valvi, Rob M van Dam, Johan Van der Heyden, Yvonne T van der Schouw, Koen Van Herck, Hoang Van Minh, Natasja M Van Schoor, Irene GM van Valkengoed, Dirk Vanderschueren, Diego Vanuzzo, Anette Varbo, Gregorio Varela-Moreiras, Patricia Varona-Pérez, Senthil K Vasan, Tomas Vega, Toomas Veidebaum, Gustavo Velasquez-Melendez, Biruta Velika, Giovanni Veronesi, WM Monique Verschuren, Cesar G Victora, Giovanni Viegi, Lucie Viet, Salvador Villalpando, Paolo Vineis, Jesus Vioque, Jyrki K Virtanen, Marjolein Visser, Sophie Visvikis-Siest, Bharathi Viswanathan, Mihaela Vladulescu, Tiina Vlasoff, Dorja Vocanec, Peter Vollenweider, Henry Völzke, Ari Voutilainen, Sari Voutilainen, Martine Vrijheid, Tanja GM Vrijkotte, Alisha N Wade, Aline Wagner, Thomas Waldhör, Janette Walton, Elvis OA Wambiya, Wan Mohamad Wan Bebakar, Wan Nazaimoon Wan Mohamud, Rildo de Souza Wanderley Júnior, Ming-Dong Wang, Ningli Wang, Qian Wang, Xiangjun Wang, Ya Xing Wang, Ying-Wei Wang, S Goya Wannamethee, Nicholas Wareham, Adelheid Weber, Niels Wedderkopp, Deepa Weerasekera, Daniel Weghuber, Wenbin Wei, Aneta Weres, Bo Werner, Peter H Whincup, Kurt Widhalm, Indah S Widyahening, Andrzej Wiecek, Rainford J Wilks, Johann Willeit, Peter Willeit, Julianne Williams, Tom Wilsgaard, Bogdan Wojtyniak, Roy A Wong-McClure, Andrew Wong, Jyh Eiin Wong, Tien Yin Wong, Jean Woo, Mark Woodward, Frederick C Wu, Jianfeng Wu, Li Juan Wu, Shouling Wu, Haiquan Xu, Liang Xu, Nor Azwany Yaacob, Uruwan Yamborisut, Weili Yan, Ling Yang, Xiaoguang Yang, Yang Yang, Nazan Yardim, Mehdi Yaseri, Tabara Yasuharu, Xingwang Ye, Panayiotis K Yiallouros, Moein Yoosefi, Akihiro Yoshihara, Qi Sheng You, San-Lin You, Novie O Younger-Coleman, Safiah Md Yusof, Ahmad Faudzi Yusoff, Luciana Zaccagni, Vassilis Zafiropulos, Ahmad A Zainuddin, Seyed Rasoul Zakavi, Farhad Zamani, Sabina Zambon, Antonis Zampelas, Hana Zamrazilová, Maria Elisa Zapata, Abdul Hamid Zargar, Ko Ko Zaw, Tomasz Zdrojewski, Kristyna Zejglicova, Tajana Zeljkovic Vrkic, Yi Zeng, Luxia Zhang, Zhen-Yu Zhang, Dong Zhao, Ming-Hui Zhao, Wenhua Zhao, Shiqi Zhen, Wei Zheng, Yingfeng Zheng, Bekbolat Zholdin, Maigeng Zhou, Dan Zhu, Marie Zins, Emanuel Zitt, Yanina Zocalo, Julio Zuñiga Cisneros, Monika Zuziak, Majid Ezzati, and Sarah Filippi
Funding Information
This paper was supported by the following grants:
Wellcome Trust to Majid Ezzati.
Medical Research Council to Maria LC Iurilli.
Additional information
Competing interests
No competing interests declared.
Author contributions
Conceptualization, Resources, Data curation, Software, Formal analysis, Supervision, Funding acquisition, Validation, Investigation, Visualization, Methodology, Writing - original draft, Writing - review and editing, Project administration.
Additional files
Data availability
Names and characteristics of data sources included in this pooling analysis are listed in Supplementary file 4. Of these data, some are from public sources, for which we have provided the data in Source data 1. Others are from individual researchers and/or from government and international agencies; these should be requested from the data holders on a study to study basis using the information in Source data 1.
References
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. Geneva: World Health Organization; 2001. https://www.who.int/healthinfo/paper31.pdf [Google Scholar]
- Bleich SN, Rimm EB, Brownell KD. U.S. nutrition assistance, 2018 - Modifying SNAP to promote population health. New England Journal of Medicine. 2017;376:1205–1207. doi: 10.1056/NEJMp1613222. [DOI] [PubMed] [Google Scholar]
- Bovet P, Chiolero A, Shamlaye C, Paccaud F. Prevalence of overweight in the Seychelles: 15 year trends and association with socio-economic status. Obesity Reviews. 2008;9:511–517. doi: 10.1111/j.1467-789X.2008.00513.x. [DOI] [PubMed] [Google Scholar]
- Brandkvist M, Bjørngaard JH, Ødegård RA, Åsvold BO, Sund ER, Vie GÅ. Quantifying the impact of genes on body mass index during the obesity epidemic: longitudinal findings from the HUNT study. BMJ. 2019;366:l4067. doi: 10.1136/bmj.l4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. The Lancet. 2011a;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure) National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. The Lancet. 2011b;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutrition Reviews. 2015;73:643–660. doi: 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, Guerrero R, Ikeda N, Kyobutungi C, Msyamboza KP, Oum S, Lynch JW, Marmot MG, Ezzati M, Lancet NCD Action Group Inequalities in non-communicable diseases and effective responses. The Lancet. 2013;381:585–597. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- Di Cesare M, Bhatti Z, Soofi SB, Fortunato L, Ezzati M, Bhutta ZA. Geographical and socioeconomic inequalities in women and children's nutritional status in Pakistan in 2011: an analysis of data from a nationally representative survey. The Lancet Global Health. 2015;3:e229–e239. doi: 10.1016/S2214-109X(15)70001-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, Ridker P, Salomaa V, Stevens J, Woodward M, Sattar N, Collins R, Thompson SG, Whitlock G, Danesh J. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. The Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report Bias: analysis of health surveys. Journal of the Royal Society of Medicine. 2006;99:250–257. doi: 10.1177/014107680609900517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, Singh GM, Lin JK, Stevens GA, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Cholesterol) National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. The Lancet. 2011;377:578–586. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. The Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. Jama. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. International Journal of Obesity. 2000;24:807–818. doi: 10.1038/sj.ijo.0801232. [DOI] [PubMed] [Google Scholar]
- Global BMI Mortality Collaboration Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet. 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MA, Subramanian SV, Razak F. Population-level trends in the distribution of body mass index in England, 1992-2013. Journal of Epidemiology and Community Health. 2016;70:832–835. doi: 10.1136/jech-2015-206468. [DOI] [PubMed] [Google Scholar]
- Haddad L. Reducing child malnutrition: how far does income growth take Us? The World Bank Economic Review. 2003;17:107–131. doi: 10.1093/wber/lhg012. [DOI] [Google Scholar]
- Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. The Lancet. 2020;395:142–155. doi: 10.1016/S0140-6736(19)32506-1. [DOI] [PubMed] [Google Scholar]
- Hayes AJ, Clarke PM, Lung TW. Change in Bias in self-reported body mass index in Australia between 1995 and 2008 and the evaluation of correction equations. Population Health Metrics. 2011;9:53. doi: 10.1186/1478-7954-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A, Gearon E, Backholer K, Bauman A, Peeters A. Age-specific changes in BMI and BMI distribution among Australian adults using cross-sectional surveys from 1980 to 2008. International Journal of Obesity. 2015;39:1209–1216. doi: 10.1038/ijo.2015.50. [DOI] [PubMed] [Google Scholar]
- Hayes AJ, Lung TW, Bauman A, Howard K. Modelling obesity trends in Australia: unravelling the past and predicting the future. International Journal of Obesity. 2017;41:178–185. doi: 10.1038/ijo.2016.165. [DOI] [PubMed] [Google Scholar]
- Helmchen LA, Henderson RM. Changes in the distribution of body mass index of white US men, 1890-2000. Annals of Human Biology. 2004;31:174–181. doi: 10.1080/03014460410001663434. [DOI] [PubMed] [Google Scholar]
- Khang YH, Yun SC. Trends in general and abdominal obesity among Korean adults: findings from 1998, 2001, 2005, and 2007 Korea national health and nutrition examination surveys. Journal of Korean Medical Science. 2010;25:1582–1588. doi: 10.3346/jkms.2010.25.11.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel A, Subramanian SV, Hamel D, Gagnon P, Razak F. Population-level trends in the distribution of body mass index in Canada, 2000-2014. Canadian Journal of Public Health. 2018;109:539–548. doi: 10.17269/s41997-018-0060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, Powell C, Vedantam S, Buchkovich ML, Yang J, Croteau-Chonka DC, Esko T, Fall T, Ferreira T, Gustafsson S, Kutalik Z, Luan J, Mägi R, Randall JC, Winkler TW, Wood AR, Workalemahu T, Faul JD, Smith JA, Zhao JH, Zhao W, Chen J, Fehrmann R, Hedman ÅK, Karjalainen J, Schmidt EM, Absher D, Amin N, Anderson D, Beekman M, Bolton JL, Bragg-Gresham JL, Buyske S, Demirkan A, Deng G, Ehret GB, Feenstra B, Feitosa MF, Fischer K, Goel A, Gong J, Jackson AU, Kanoni S, Kleber ME, Kristiansson K, Lim U, Lotay V, Mangino M, Leach IM, Medina-Gomez C, Medland SE, Nalls MA, Palmer CD, Pasko D, Pechlivanis S, Peters MJ, Prokopenko I, Shungin D, Stančáková A, Strawbridge RJ, Sung YJ, Tanaka T, Teumer A, Trompet S, van der Laan SW, van Setten J, Van Vliet-Ostaptchouk JV, Wang Z, Yengo L, Zhang W, Isaacs A, Albrecht E, Ärnlöv J, Arscott GM, Attwood AP, Bandinelli S, Barrett A, Bas IN, Bellis C, Bennett AJ, Berne C, Blagieva R, Blüher M, Böhringer S, Bonnycastle LL, Böttcher Y, Boyd HA, Bruinenberg M, Caspersen IH, Chen YI, Clarke R, Daw EW, de Craen AJM, Delgado G, Dimitriou M, Doney ASF, Eklund N, Estrada K, Eury E, Folkersen L, Fraser RM, Garcia ME, Geller F, Giedraitis V, Gigante B, Go AS, Golay A, Goodall AH, Gordon SD, Gorski M, Grabe HJ, Grallert H, Grammer TB, Gräßler J, Grönberg H, Groves CJ, Gusto G, Haessler J, Hall P, Haller T, Hallmans G, Hartman CA, Hassinen M, Hayward C, Heard-Costa NL, Helmer Q, Hengstenberg C, Holmen O, Hottenga JJ, James AL, Jeff JM, Johansson Å, Jolley J, Juliusdottir T, Kinnunen L, Koenig W, Koskenvuo M, Kratzer W, Laitinen J, Lamina C, Leander K, Lee NR, Lichtner P, Lind L, Lindström J, Lo KS, Lobbens S, Lorbeer R, Lu Y, Mach F, Magnusson PKE, Mahajan A, McArdle WL, McLachlan S, Menni C, Merger S, Mihailov E, Milani L, Moayyeri A, Monda KL, Morken MA, Mulas A, Müller G, Müller-Nurasyid M, Musk AW, Nagaraja R, Nöthen MM, Nolte IM, Pilz S, Rayner NW, Renstrom F, Rettig R, Ried JS, Ripke S, Robertson NR, Rose LM, Sanna S, Scharnagl H, Scholtens S, Schumacher FR, Scott WR, Seufferlein T, Shi J, Smith AV, Smolonska J, Stanton AV, Steinthorsdottir V, Stirrups K, Stringham HM, Sundström J, Swertz MA, Swift AJ, Syvänen AC, Tan ST, Tayo BO, Thorand B, Thorleifsson G, Tyrer JP, Uh HW, Vandenput L, Verhulst FC, Vermeulen SH, Verweij N, Vonk JM, Waite LL, Warren HR, Waterworth D, Weedon MN, Wilkens LR, Willenborg C, Wilsgaard T, Wojczynski MK, Wong A, Wright AF, Zhang Q, Brennan EP, Choi M, Dastani Z, Drong AW, Eriksson P, Franco-Cereceda A, Gådin JR, Gharavi AG, Goddard ME, Handsaker RE, Huang J, Karpe F, Kathiresan S, Keildson S, Kiryluk K, Kubo M, Lee JY, Liang L, Lifton RP, Ma B, McCarroll SA, McKnight AJ, Min JL, Moffatt MF, Montgomery GW, Murabito JM, Nicholson G, Nyholt DR, Okada Y, Perry JRB, Dorajoo R, Reinmaa E, Salem RM, Sandholm N, Scott RA, Stolk L, Takahashi A, Tanaka T, van 't Hooft FM, Vinkhuyzen AAE, Westra HJ, Zheng W, Zondervan KT, Heath AC, Arveiler D, Bakker SJL, Beilby J, Bergman RN, Blangero J, Bovet P, Campbell H, Caulfield MJ, Cesana G, Chakravarti A, Chasman DI, Chines PS, Collins FS, Crawford DC, Cupples LA, Cusi D, Danesh J, de Faire U, den Ruijter HM, Dominiczak AF, Erbel R, Erdmann J, Eriksson JG, Farrall M, Felix SB, Ferrannini E, Ferrières J, Ford I, Forouhi NG, Forrester T, Franco OH, Gansevoort RT, Gejman PV, Gieger C, Gottesman O, Gudnason V, Gyllensten U, Hall AS, Harris TB, Hattersley AT, Hicks AA, Hindorff LA, Hingorani AD, Hofman A, Homuth G, Hovingh GK, Humphries SE, Hunt SC, Hyppönen E, Illig T, Jacobs KB, Jarvelin MR, Jöckel KH, Johansen B, Jousilahti P, Jukema JW, Jula AM, Kaprio J, Kastelein JJP, Keinanen-Kiukaanniemi SM, Kiemeney LA, Knekt P, Kooner JS, Kooperberg C, Kovacs P, Kraja AT, Kumari M, Kuusisto J, Lakka TA, Langenberg C, Marchand LL, Lehtimäki T, Lyssenko V, Männistö S, Marette A, Matise TC, McKenzie CA, McKnight B, Moll FL, Morris AD, Morris AP, Murray JC, Nelis M, Ohlsson C, Oldehinkel AJ, Ong KK, Madden PAF, Pasterkamp G, Peden JF, Peters A, Postma DS, Pramstaller PP, Price JF, Qi L, Raitakari OT, Rankinen T, Rao DC, Rice TK, Ridker PM, Rioux JD, Ritchie MD, Rudan I, Salomaa V, Samani NJ, Saramies J, Sarzynski MA, Schunkert H, Schwarz PEH, Sever P, Shuldiner AR, Sinisalo J, Stolk RP, Strauch K, Tönjes A, Trégouët DA, Tremblay A, Tremoli E, Virtamo J, Vohl MC, Völker U, Waeber G, Willemsen G, Witteman JC, Zillikens MC, Adair LS, Amouyel P, Asselbergs FW, Assimes TL, Bochud M, Boehm BO, Boerwinkle E, Bornstein SR, Bottinger EP, Bouchard C, Cauchi S, Chambers JC, Chanock SJ, Cooper RS, de Bakker PIW, Dedoussis G, Ferrucci L, Franks PW, Froguel P, Groop LC, Haiman CA, Hamsten A, Hui J, Hunter DJ, Hveem K, Kaplan RC, Kivimaki M, Kuh D, Laakso M, Liu Y, Martin NG, März W, Melbye M, Metspalu A, Moebus S, Munroe PB, Njølstad I, Oostra BA, Palmer CNA, Pedersen NL, Perola M, Pérusse L, Peters U, Power C, Quertermous T, Rauramaa R, Rivadeneira F, Saaristo TE, Saleheen D, Sattar N, Schadt EE, Schlessinger D, Slagboom PE, Snieder H, Spector TD, Thorsteinsdottir U, Stumvoll M, Tuomilehto J, Uitterlinden AG, Uusitupa M, van der Harst P, Walker M, Wallaschofski H, Wareham NJ, Watkins H, Weir DR, Wichmann HE, Wilson JF, Zanen P, Borecki IB, Deloukas P, Fox CS, Heid IM, O'Connell JR, Strachan DP, Stefansson K, van Duijn CM, Abecasis GR, Franke L, Frayling TM, McCarthy MI, Visscher PM, Scherag A, Willer CJ, Boehnke M, Mohlke KL, Lindgren CM, Beckmann JS, Barroso I, North KE, Ingelsson E, Hirschhorn JN, Loos RJF, Speliotes EK, LifeLines Cohort Study. ADIPOGen Consortium. AGEN-BMI Working Group. CARDIOGRAMplusC4D Consortium. CKDGen Consortium. GLGC. ICBP. MAGIC Investigators. MuTHER Consortium. MIGen Consortium. PAGE Consortium. ReproGen Consortium. GENIE Consortium. International Endogene Consortium Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midthjell K, Lee CM, Langhammer A, Krokstad S, Holmen TL, Hveem K, Colagiuri S, Holmen J. Trends in overweight and obesity over 22 years in a large adult population: the HUNTstudy, Norway. Clinical Obesity. 2013;3:12–20. doi: 10.1111/cob.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro CA, Conde WL, Popkin BM. Is obesity replacing or adding to undernutrition? Evidence from different social classes in Brazil. Public Health Nutrition. 2002;5:105–112. doi: 10.1079/PHN2001281. [DOI] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) A century of trends in adult human height. eLife. 2016a;5:e13410. doi: 10.7554/eLife.13410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. The Lancet. 2016b;387:1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet. 2016c;387:1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet. 2017a;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. The Lancet. 2017b;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Contributions of mean and shape of blood pressure distribution to worldwide trends and variations in raised blood pressure: a pooled analysis of 1018 population-based measurement studies with 88.6 million participants. International Journal of Epidemiology. 2018;47:872–883. doi: 10.1093/ije/dyy016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569:260–264. doi: 10.1038/s41586-019-1171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants. The Lancet. 2020;396:1511–1524. doi: 10.1016/S0140-6736(20)31859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity Reviews. 2012;13:659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang Y, Wang H, Su C, Wang Z, Song Y, Xiao Y, Du W, Zhang B. Use of quantile regression to investigate changes in the body mass index distribution of Chinese adults aged 18-60 years: a longitudinal study. BMC Public Health. 2015;15:278. doi: 10.1186/s12889-015-1606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters A, Gearon E, Backholer K, Carstensen B. Trends in the skewness of the body mass index distribution among urban Australian adults, 1980 to 2007. Annals of Epidemiology. 2015;25:26–33. doi: 10.1016/j.annepidem.2014.10.008. [DOI] [PubMed] [Google Scholar]
- Penman AD, Johnson WD. The changing shape of the body mass index distribution curve in the population: implications for public health policy to reduce the prevalence of adult obesity. Preventing Chronic Disease. 2006;3:A74. [PMC free article] [PubMed] [Google Scholar]
- Pongou R, Salomon JA, Ezzati M. Health impacts of macroeconomic crises and policies: determinants of variation in childhood malnutrition trends in Cameroon. International Journal of Epidemiology. 2006;35:648–656. doi: 10.1093/ije/dyl016. [DOI] [PubMed] [Google Scholar]
- Popkin BM. Recent dynamics suggest selected countries catching up to US obesity. The American Journal of Clinical Nutrition. 2010;91:284S–288. doi: 10.3945/ajcn.2009.28473C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. The Lancet. 2020;395:65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM, Slining MM. New dynamics in global obesity facing low- and middle-income countries. Obesity Reviews. 2013;14 Suppl 2:11–20. doi: 10.1111/obr.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obesity Reviews. 2013;14:110–128. doi: 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prospective Studies Collaboration. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. The Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razak F, Corsi DJ, Subramanian SV. Change in the body mass index distribution for women: analysis of surveys from 37 low- and middle-income countries. PLOS Medicine. 2013;10:e1001367. doi: 10.1371/journal.pmed.1001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razak F, Subramanian SV, Sarma S, Kawachi I, Berkman L, Davey Smith G, Corsi DJ. Association between population mean and distribution of deviance in demographic surveys from 65 countries: cross sectional study. BMJ. 2018;362:k3147. doi: 10.1136/bmj.k3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G, Day S. The population mean predicts the number of deviant individuals. BMJ. 1990;301:1031–1034. doi: 10.1136/bmj.301.6759.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez PA, Swaminathan MS. Hunger in Africa: the link between unhealthy people and unhealthy soils. The Lancet. 2005;365:442–444. doi: 10.1016/S0140-6736(05)17834-9. [DOI] [PubMed] [Google Scholar]
- Silventoinen K, Jelenkovic A, Sund R, Hur YM, Yokoyama Y, Honda C, Hjelmborg J, Möller S, Ooki S, Aaltonen S, Ji F, Ning F, Pang Z, Rebato E, Busjahn A, Kandler C, Saudino KJ, Jang KL, Cozen W, Hwang AE, Mack TM, Gao W, Yu C, Li L, Corley RP, Huibregtse BM, Christensen K, Skytthe A, Kyvik KO, Derom CA, Vlietinck RF, Loos RJ, Heikkilä K, Wardle J, Llewellyn CH, Fisher A, McAdams TA, Eley TC, Gregory AM, He M, Ding X, Bjerregaard-Andersen M, Beck-Nielsen H, Sodemann M, Tarnoki AD, Tarnoki DL, Stazi MA, Fagnani C, D'Ippolito C, Knafo-Noam A, Mankuta D, Abramson L, Burt SA, Klump KL, Silberg JL, Eaves LJ, Maes HH, Krueger RF, McGue M, Pahlen S, Gatz M, Butler DA, Bartels M, van Beijsterveldt TC, Craig JM, Saffery R, Freitas DL, Maia JA, Dubois L, Boivin M, Brendgen M, Dionne G, Vitaro F, Martin NG, Medland SE, Montgomery GW, Chong Y, Swan GE, Krasnow R, Magnusson PK, Pedersen NL, Tynelius P, Lichtenstein P, Haworth CM, Plomin R, Bayasgalan G, Narandalai D, Harden KP, Tucker-Drob EM, Öncel SY, Aliev F, Spector T, Mangino M, Lachance G, Baker LA, Tuvblad C, Duncan GE, Buchwald D, Willemsen G, Rasmussen F, Goldberg JH, Sørensen TIa, Boomsma DI, Kaprio J. Genetic and environmental effects on body mass index from infancy to the onset of adulthood: an individual-based pooled analysis of 45 twin cohorts participating in the COllaborative project of development of anthropometrical measures in twins (CODATwins) study. The American Journal of Clinical Nutrition. 2016;104:371–379. doi: 10.3945/ajcn.116.130252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silventoinen K, Jelenkovic A, Sund R, Yokoyama Y, Hur YM, Cozen W, Hwang AE, Mack TM, Honda C, Inui F, Iwatani Y, Watanabe M, Tomizawa R, Pietiläinen KH, Rissanen A, Siribaddana SH, Hotopf M, Sumathipala A, Rijsdijk F, Tan Q, Zhang D, Pang Z, Piirtola M, Aaltonen S, Öncel SY, Aliev F, Rebato E, Hjelmborg JB, Christensen K, Skytthe A, Kyvik KO, Silberg JL, Eaves LJ, Cutler TL, Ordoñana JR, Sánchez-Romera JF, Colodro-Conde L, Song YM, Yang S, Lee K, Franz CE, Kremen WS, Lyons MJ, Busjahn A, Nelson TL, Whitfield KE, Kandler C, Jang KL, Gatz M, Butler DA, Stazi MA, Fagnani C, D'Ippolito C, Duncan GE, Buchwald D, Martin NG, Medland SE, Montgomery GW, Jeong HU, Swan GE, Krasnow R, Magnusson PK, Pedersen NL, Dahl Aslan AK, McAdams TA, Eley TC, Gregory AM, Tynelius P, Baker LA, Tuvblad C, Bayasgalan G, Narandalai D, Spector TD, Mangino M, Lachance G, Burt SA, Klump KL, Harris JR, Brandt I, Nilsen TS, Krueger RF, McGue M, Pahlen S, Corley RP, Huibregtse BM, Bartels M, van Beijsterveldt CE, Willemsen G, Goldberg JH, Rasmussen F, Tarnoki AD, Tarnoki DL, Derom CA, Vlietinck RF, Loos RJ, Hopper JL, Sung J, Maes HH, Turkheimer E, Boomsma DI, Sørensen TI, Kaprio J. Differences in genetic and environmental variation in adult BMI by sex, age, time period, and region: an individual-based pooled analysis of 40 twin cohorts. The American Journal of Clinical Nutrition. 2017;106:457–466. doi: 10.3945/ajcn.117.153643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenholm S, Vahtera J, Kawachi I, Pentti J, Halonen JI, Westerlund H, Razak F, Subramanian SV, Kivimäki M. Patterns of weight gain in middle-aged and older US adults, 1992-2010. Epidemiology. 2015;26:165–168. doi: 10.1097/EDE.0000000000000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens GA, Finucane MM, Paciorek CJ, Flaxman SR, White RA, Donner AJ, Ezzati M, Nutrition Impact Model Study Group (Child Growth) Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: a systematic analysis of population representative data. The Lancet. 2012;380:824–834. doi: 10.1016/S0140-6736(12)60647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Smith GD. Patterns, distribution, and determinants of under- and overnutrition: a population-based study of women in India. The American Journal of Clinical Nutrition. 2006;84:633–640. doi: 10.1093/ajcn/84.3.633. [DOI] [PubMed] [Google Scholar]
- Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Is economic growth associated with reduction in child undernutrition in India? PLOS Medicine. 2011;8:e1000424. doi: 10.1371/journal.pmed.1000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. The Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- Tolonen H, Koponen P, Mindell JS, Männistö S, Giampaoli S, Dias CM, Tuovinen T, Göβwald A, Kuulasmaa K, European Health Examination Survey Pilot Project Under-estimation of obesity, hypertension and high cholesterol by self-reported data: comparison of self-reported information and objective measures from health examination surveys. The European Journal of Public Health. 2014;24:941–948. doi: 10.1093/eurpub/cku074. [DOI] [PubMed] [Google Scholar]
- Vaezghasemi M, Razak F, Ng N, Subramanian SV. Inter-individual inequality in BMI: an analysis of Indonesian family life surveys (1993-2007) SSM - Population Health. 2016;2:876–888. doi: 10.1016/j.ssmph.2016.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner KJP, Boing AF, Cembranel F, Boing A, Subramanian SV. Change in the distribution of body mass index in Brazil: analysing the interindividual inequality between 1974 and 2013. Journal of Epidemiology and Community Health. 2019;73:544–548. doi: 10.1136/jech-2018-211664. [DOI] [PubMed] [Google Scholar]
- Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20-45 years (1989-2000) International Journal of Obesity. 2007;31:272–278. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A. The double burden of malnutrition: aetiological pathways and consequences for health. The Lancet. 2020;395:75–88. doi: 10.1016/S0140-6736(19)32472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]