Abstract
Physician burnout and other forms of occupational distress are a significant problem in modern medicine, especially during the COVID19 pandemic, yet few doctors are familiar with the neurobiology that contributes to these problems. Burnout has been linked to changes that reduce a physician’s sense of control over their own practice, undermine connections with patients and colleagues, interfere with work–life integration, and result in uncontrolled stress. Brain research has demonstrated that uncontrollable stress, but not controllable stress, impairs the functioning of the prefrontal cortex, a recently evolved brain region that provides top-down regulation over thought, action and emotion. The prefrontal cortex governs many cognitive operations essential to physicians, including abstract reasoning, higher order decision-making, insight, and the ability to persevere through challenges. However, the prefrontal cortex is remarkably reliant on arousal state, and is impaired under conditions of fatigue and/or uncontrollable stress when there are inadequate or excessive levels of the arousal modulators (e.g. norepinephrine, dopamine, acetylcholine). With chronic stress exposure, prefrontal gray matter connections are lost, but can be restored by stress relief. Reduced PFC self-regulation may explain several challenges associated with burnout in physicians including reduced motivation, unprofessional behavior, and suboptimal communication with patients. Understanding this neurobiology may help physicians have a more informed perspective to help relieve or prevent symptoms of burnout, and may help administrative leaders to optimize the work environment to create more effective organizations. Efforts to restore a sense of control to physicians may be particularly helpful.
Occupational distress, including professional burnout and moral distress, are widespread problems in modern medicine 1. These challenges existed before the COVID19 pandemic, and are likely being amplified by the continuing challenges posed by this event. Burnout refers to an occupational syndrome associated with affective and cognitive changes, including emotional exhaustion, depersonalization or cynicism, and diminished feelings of personal efficacy resulting from chronic occupational stress. Burnout is formally recognized by the World Health Organization as an occupational syndrome and increases the risk of hypertension, atrial flutter, cardiovascular disease, depression and suicide 2, 3. By definition, occupational burnout is primarily precipitated by characteristics of the work environment rather than by individual problems with resilience or coping, and thus changes in the work environment are key to reducing risk.
Large scale studies suggest that occupational stress and symptoms of professional burnout are more prevalent among physicians than among workers in other fields, even after adjustment for work hours and level of education 4, 5 Burnout can have many professional and personal consequences, including increased physician turnover, reduced quality of care for patients, broken personal relationships, and problematic alcohol use 5.
The high prevalence of physician burnout has been longstanding, linked to changes in the practice environment that reduce physicians’ control over their work, undermine connections with patients and colleagues, interfere with work–life integration, and thus result in uncontrolled stress 5. In situations like the current COVID19 pandemic, perceived loss of control and overwhelming workloads can further exacerbate this process. In more typical times, financial pressures and administrative requirements from payers and regulators have resulted in greater productivity demands, increased workload, and reduced independence for physicians in many practice settings. Physicians must also keep up with the rapid expansion of medical knowledge and deal with increased administrative burdens related to electronic health records and regulatory requirements. They also face unprecedented levels of scrutiny from administrators on sub-optimal metrics that often fail to recognize the nature of their work (e.g. RVUs, patient satisfaction scores, percent of charts closed in 24 hours).
Although it is triggered by characteristics of the work environment, chronic occupational stress ultimately affects biologic function. The lack of control over many stressors in modern medicine can have toxic effects on brain circuitry 6–8. An appreciation for the ways in which the brain changes in response to uncontrollable stress can help physicians recognize symptoms and lead to constructive personal and organizational interventions. Neuroscientists have discovered that exposure to uncontrollable stress -but not to controllable stress- has marked deleterious effects on the prefrontal cortex (PFC), the brain region that governs higher cognition and provides top-down control of thought, action, and emotion 6–8. Here we provide a brief review of PFC functions, the susceptibility of PFC to uncontrollable stress, and how understanding this neurobiology can help physicians and medical organizations develop rational and informed strategies to reduce the risk of burnout.
The higher functions of the prefrontal cortex
The PFC resides in the frontal lobe, anterior to the motor cortices (Fig. 1A). Many of the cognitive operations performed by the PFC 9 are an essential part of a physician’s mental toolbox: the PFC governs high-order reasoning, social cognition, and complex decision-making, including the integration, conceptualization, and critical evaluation of information (Fig. 1A). It is essential for executive functions such as attentional regulation, planning and organization, and guiding appropriate social behaviors including placing patients’ interest above one’s own, and maintaining integrity despite challenges. The most anterior aspects of PFC govern metacognitive abilities (thinking about thinking) that permit such capacities as insight about oneself and others, moral conscience, emotional intelligence and empathy — all of which are critical for optimal physician performance. The right PFC is specialized for inhibitory control, and dysfunction can lead to inappropriate behaviors or lapses in professionalism, while the left PFC is specialized for language production in most right-handed individuals. The PFC can also act as a “mental cheerleader,” motivating higher goals, and regulating emotional circuits, including those that mediate mood and anxiety.
Figure 1-. The higher cognitive functions of the prefrontal cortex are impaired by fatigue or uncontrollable stress: Potential ramifications to clinical practice –
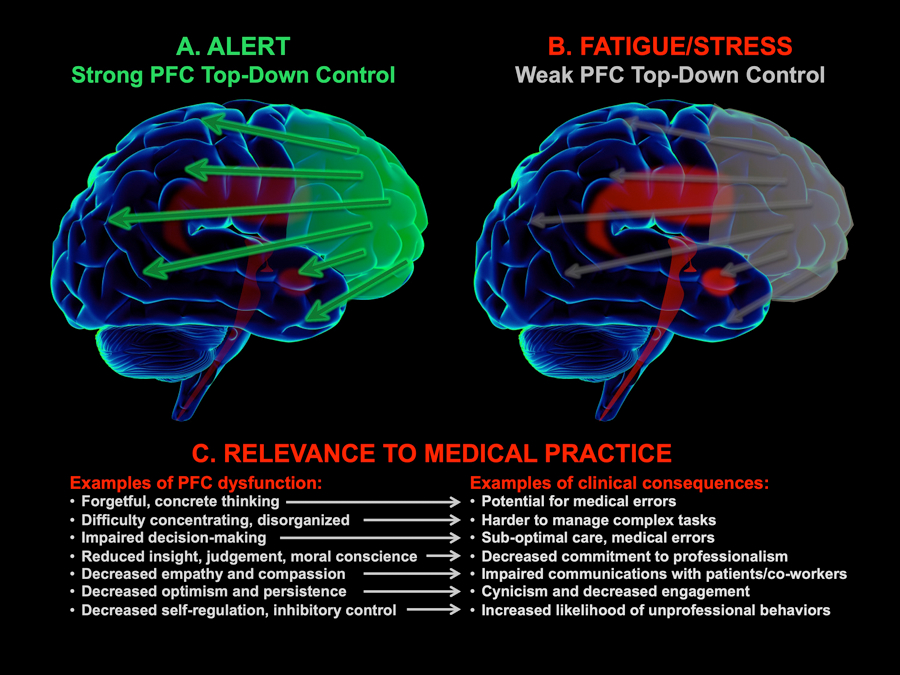
A. The prefrontal cortex (PFC, highlit in green) resides in the brain’s frontal lobe, anterior to the motor cortices. The PFC has extensive connections with cortical and subcortical brain areas that provide top-down control over thought, attention, action, and emotion when we feel rested, interested and in control. B. Under conditions of uncontrollable stress or fatigue, PFC connections are weakened (gray) and there is a loss of top-down control and impaired PFC cognitive functions. Stress also activates more primitive brain circuits (highlit in red) that mediate unconscious responses and habits. Chronic stress exposure causes atrophy of PFC connections, weakening the thoughtful, evaluative responding needed for professional and personal fulfillment. C. Examples of some of the cognitive changes that occur with PFC dysfunction and their potential consequences to physician performance. For a brief summary of these neurobiological mechanisms at the Yale Medical School Youtube Channel, see: www.youtube.com/watch?v=vdDvChLuQsA .
Stress impairs prefrontal cortex functioning: The importance of control
Although the PFC is capable of remarkable cognitive functions, these cortical operations are very energy-intensive and highly sensitive to arousal state. As summarized in Figure 2, arousal has an “inverted-U” dose-response on PFC function, where PFC higher order abilities are weakened both by fatigue and by uncontrollable stress, either of which can take the PFC “off-line” 10. Sleep deprivation particularly impacts PFC functioning, with impairments in PFC metabolic and physiologic activity correlating with cognitive deficits 11. PFC functioning is also impaired by uncontrollable stress exposure, including an acute stressor if the subject feels threatened by the situation. This evokes a series of chemical events in the brain that rapidly disconnect PFC circuits. For example, during incontrollable stress, high levels of norepinephrine and dopamine are released in brain, which weaken PFC function. These catecholamines initiate intracellular signaling cascades that rapidly open potassium channels near PFC synapses to weaken circuit connections 10. This impairs PFC cognitive functions, which can result in diminished working memory and attention regulation, poor decision-making and other cognitive deficits that can be measured in both animals10, 12, 13 and humans14–16 (Fig. 1B). High levels of norepinephrine and dopamine are also released in more primitive brain circuits such as the amygdala, striatum and brainstem, where they have the opposite effect and strengthen the unconscious habits and emotional responses that are the purview of these more ancient brain structures17–19. These changes can occur very rapidly, for example when one is cut-off while driving on the highway, or in response to unexpected, bad news. These alterations in brain physiology may be helpful in the former situation, allowing one to rapidly step on the brakes, but may be detrimental when a complicated challenge requires thoughtful evaluation and guidance by the PFC. In contrast to uncontrollable stress, controllable stressors do not elicit these detrimental chemical actions5. Thus, if one feels confident that one can handle a challenging situation, or that there are sufficient supports to maintain one’s safety, the PFC can inhibit the stress response and maintain a more optimal neurochemical environment.
Figure 2-. The effects of arousal on prefrontal cortical function.
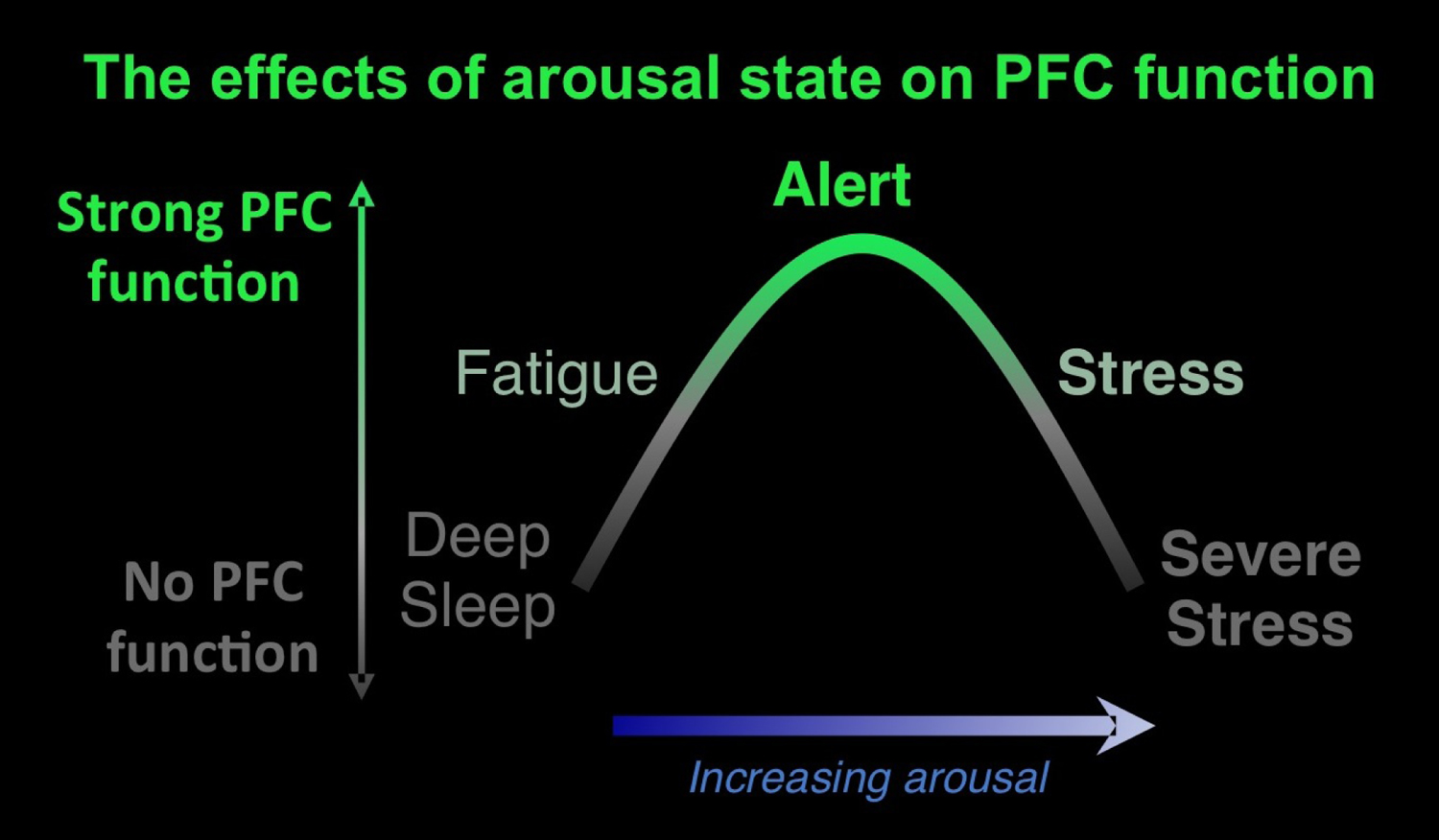
Arousal state has an “inverted-U” dose response effect on PFC functioning. PFC synapses require stimulation from the arousal systems (acetylcholine, norepinephrine, dopamine, serotonin) in order to function properly, and inadequate levels e.g. during fatigue, weaken PFC function. Conversely, excessive norepinephrine and dopamine release during uncontrollable stress also weakens PFC function, by rapidly weakening PFC synaptic connections. It is noteworthy that caffeine increases the release of acetylcholine in the PFC, which may explain why it can be helpful to cognitive function in rested individuals.
With sustained uncontrollable stressors there are additional, more substantial changes in brain circuits. Chronic uncontrollable stress causes PFC synaptic connections to atrophy, while those in more primitive brain circuits expand, a phenomenon documented in both animal and human brains 12, 13, 20–22. This work is directly relevant to the syndrome of burnout, as human subjects with occupational exhaustion have thinner PFC gray matter 8, and have to recruit larger volumes of PFC to maintain the same levels of cognitive performance 23. Although these physiologic studies were not performed in physicians, they represent fundamental human biology and are thus applicable to burnout in doctors as well. Fortunately, animal and human studies show that PFC connections can regrow during sustained periods of nonstress, allowing the return of top–down control 8, 10, 12, 24.
The relevance of impaired prefrontal cortical function to occupational burnout
Just as it is useful to understand the mechanisms by which the immune system, which is typically our ally, can inappropriately attack the body in an autoimmune disorder, it is helpful to know the molecular mechanisms that actively weaken higher brain circuits during uncontrollable stress. This neurobiological perspective provides a rational understanding of symptoms and can inform strategies for prevention and treatment. Impaired PFC self-regulation may explain a number of the challenges associated with occupational burnout, such as reduced motivation, unprofessional behavior, decreased compassion, and suboptimal communication with patients (Fig. 1C). During a time of intense workload, such as a global health emergency, physicians and other healthcare professionals may be under extraordinary stress. Evidence indicates that having a sense of control can protect against cognitive deficits during stress exposure 14. Thus, understanding that changes in mental state are part of the natural neurobiological response may provide perspective and a sense of control, especially with the knowledge that PFC connections and function can be restored when the stressor abates.
Building emotional intelligence skills can also increase control by enhancing self-awareness as a means to enhance self-regulation and social management 25,26. Recognizing when work demands have become depleting or triggering frustration, allows individuals to be aware of their needs and make choices over the dimensions they do control such as naming emotions (i.e. frustration, exhaustion, anger, moral distress, grief), taking a break to attend to physical needs (hunger), and increasing prioritization of sleep or other needs. Strengthening social awareness as a means to attending social management can also help physicians more effectively support colleagues dealing with uncontrolled stress.
Awareness of the neurobiology and focus on short-term responses can set the stage for rational longer-term actions. Specifically, opportunities for clinicians to regain control (e.g., creating organization and structure in a time of chaos, advocating for change, the ability to identify inefficient processes and lead efforts to improve work flows, working part-time as a means to enhance control) may help relieve burnout symptoms 5. A sense of control can also be enhanced by gaining perspective, perhaps by engaging in activities that are meaningful and refreshing (e.g., recognizing meaning and purpose in serving patients and society, mindfulness-based stress reduction, recreational exercise) and by learning about the underlying neurobiology of the stress response, which can help reduce self-blame and promote a more compassionate view of oneself and others 27. Deliberate decisions to foster work-life integration can also increase perceived control. Professional coaching is a proven strategy for physicians to advance such efforts. 28
Additional behaviors that respect the physiological needs of the PFC may also have an impact. Exercise and healthy diet and snacks can support the high energy demands of the PFC. Maintaining these activities, despite intensive work-loads, should be a priority to facilitate efficacy over an extended interval. In contrast, alcohol consumption, while offering temporary relief from stress, can worsen PFC physiology in the long run 29. It is also important to recognize when occupational stress has become more global distress (such as depression 30), since proper treatment (e.g. selective serotonin reuptake inhibitors or psychotherapy) has been shown to restore balance in PFC circuits and function.
Understanding the neurobiology can guide system-based strategies to reduce burnout
A better understanding of the neurobiology of uncontrolled stress also has implications for organization and system efforts to reduce burnout by improving medical practice environments. Efforts to restore control to physicians may be particularly helpful, even under conditions when an overwhelming work load taxes the entire system 31. Such efforts may involve changes in the behavior of organizational leaders, regularly asking physicians for input, providing them greater voice in decision making, developing and providing clear structure to rapidly expanded care teams, and providing authentic opportunities to organize and shape their working conditions 5. These opportunities could include incorporation of stress-reducing periods such as breaks which can be facilitated by means of scheduling and creation of physician breakrooms or respite spaces. In more typical times, such opportunities also include choice and flexibility of work schedules, the ability to lead work-flow redesign, and compensation systems that incentivize, rather than discourage, taking vacations. 5, 31 Supporting activities that provide and enhance social supports (fostering collegiality, for example, or developing peer-support programs) and that provide meaning in work (e.g. professional development, mentorship, adequate time to develop connections with patients) provide perspective and purpose that also enhance the perception of control 32.
The physician and healthcare workforce was plagued with a high prevalence of burnout and occupational distress even prior to the COVID19 pandemic 33. A lack of control precipitated by the abrupt and dramatic increase in professional workload, unpredictability of the surge in patients with infection, deployment of physicians to areas outside their expertise, exposure to suffering, and inability to reverse the disease process for many patients, can all contribute to an acute exacerbation of this chronic problem that will likely persist after the pandemic. An understanding of the neurobiology of burnout and the importance of control may allow administrative leaders to identify the characteristics of the work environment that contribute to occupational stress and identify opportunities to increase physicians sense of control to create more effective organizations.
Learning Objectives.
On completion of this article, you should be able to:
1 Differentiate the neurobiology of how uncontrolled stress, but not controlled stress, contributes to burnout
2 Recognize how the impact of chronic stress on prefrontal cortex regulation may explain several challenges associated with burnout in physicians including reduced motivation, unprofessional behavior, and suboptimal communication with patients.
3 Describe how organizational efforts to restore control to physicians maybe particularly helpful for reducing burnout
Funding/Support:
Dr. Arnsten is funded by NIH grants R01 AG061190–01, MH093354–05 and MH108643–01, and by an endowed chair honoring Albert E. Kent to Yale University. Dr. Shanafelt’s research is funded by an endowed chair honoring Jeanie and Stewart Ritchie to Stanford University.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures:
Dr. Arnsten and Yale University receive royalties from the USA sales of Intuniv from Shire/Takeda Pharmaceuticals. They do not receive royalties for nonUSA or generic sales. Dr. Arnsten often lectures on the neurobiology of prefrontal cortex and the stress response, and receives honoraria for some of these activities. She also consults with Lundbeck Pharmaceuticals in the development of potential cognitive protecting agents. Dr. Shanafelt is co-inventor of the Physician Well-being Index, Medical Student Well-being Index, Nurse Well-being Index, the Well-being Index and Participatory Management Leadership Index. Mayo Clinic holds the copyright to these instruments and has licensed them for use outside Mayo Clinic. Mayo Clinic pays Dr. Shanafelt a portion of royalties they receive. As an expert on the topic of health care professional well-being, Dr. Shanafelt often presents grand rounds/keynote lecture presentation as well as advises healthcare organizations. He receives honoraria for some of these activities.
Contributor Information
Amy F.T. Arnsten, Department of Neuroscience, Yale University School of Medicine, New Haven, CT
Tait Shanafelt., Department of Medicine, Stanford University School of Medicine, Stanford, CA
References
- 1.National Academies of Sciences E, and Medicine; National Academy of Medicine; , Well-Being. CoSAtIPCbSC. Taking Action Against Burnout: A Systems Approach to Professional Well-Being Washington, D.C.2019. [PubMed] [Google Scholar]
- 2.Appels A, Schouten E. Burnout as a risk factor for coronary heart disease. Behav Med 1991;17:53–59. [DOI] [PubMed] [Google Scholar]
- 3.Kakiashvili T, Leszek J, Rutkowski K. The medical perspective on burnout. Int J Occup Med Environ Health 2013;26:401–412. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt TD, Noseworthy JH. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clin Proc. 2017;92:129–146. [DOI] [PubMed] [Google Scholar]
- 6.Maier SF, Amat J, Baratta MV, Paul E, Watkins LR. Behavioral control, the medial prefrontal cortex, and resilience. Dialogues Clin Neurosci 2006;8:397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnsten AFT. Stress signaling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience 2009;10:410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Savic I, Perski A, Osika W. MRI Shows that Exhaustion Syndrome Due to Chronic Occupational Stress is Associated with Partially Reversible Cerebral Changes. Cereb Cortex 2018;28:894–906. [DOI] [PubMed] [Google Scholar]
- 9.Szczepanski SM, Knight RT. Insights into human behavior from lesions to the prefrontal cortex. Neuron 2014;83:1002–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnsten AF. Stress weakens prefrontal networks: molecular insults to higher cognition. Nat Neurosci 2015;18:1376–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muzur A, Pace-Schott EF, Hobson JA. The prefrontal cortex in sleep. Trends Cogn Sci 2002;6:475–481. [DOI] [PubMed] [Google Scholar]
- 12.Liston C, McEwen BS, Casey BJ. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proc Nat Acad Sci USA 2009;106:912–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hains AB, Vu MA, Maciejewski PK, van Dyck CH, Gottron M, Arnsten AF. Inhibition of protein kinase C signaling protects prefrontal cortex dendritic spines and cognition from the effects of chronic stress. Proc Natl Acad Sci U S A 2009;106:17957–17962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glass DC, Reim B, Singer JE. Behavioral consequences of adaptation to controllable and uncontrollable noise. J. Exp. Social Psychol 1971;7:244–257. [Google Scholar]
- 15.Qin S, Hermans EJ, van Marle HJF, Lou J, Fernandez G. Acute psychological stress reduces working memory-related activity in the dorsolateral prefrontal cortex. Biological Psychiatry 2009;66:25–32. [DOI] [PubMed] [Google Scholar]
- 16.Porcelli AJ, Delgado MR. Stress and Decision Making: Effects on Valuation, Learning, and Risk-taking. Curr Opin Behav Sci. 2017;14:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Packard MG, Teather LA. Amygdala modulation of multiple memory systems: hippocampus and caudate-putamen. Neurobiol. Learning Mem 1998;69:163–203. [DOI] [PubMed] [Google Scholar]
- 18.Ferry B, Roozendaal B, McGaugh JL. Basolateral amygdala noradrenergic influences on memory storage are mediated by an interaction between beta- and alpha-1-adrenoceptors. J. Neurosci 1999;19:5119–5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodrigues SM, LeDoux JE, Sapolsky RM. The influence of stress hormones on fear circuitry. Annu Rev Neurosci 2009;32:289–313. [DOI] [PubMed] [Google Scholar]
- 20.Vyas A, Mitra R, Shankaranarayana Rao BS, Chattarji S. Chronic stress induces contrasting patterns of dendritic remodeling in hippocampal and amygdaloid neurons. J Neurosci. 2002;22:6810–6818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radley JJ, Rocher AB, Miller M, et al. Repeated stress induces dendritic spine loss in the rat medial prefrontal cortex. Cereb Cortex 2006;16:313–320. [DOI] [PubMed] [Google Scholar]
- 22.Ansell EB, Rando K, Tuit K, Guarnaccia J, Sinha R. Cumulative adversity and smaller gray matter volume in medial prefrontal, anterior cingulate, and insula regions. Biol Psychiatry 2012;72:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gavelin HM, Neely AS, Andersson M, Eskilsson T, Järvholm LS, Boraxbekk CJ. Neural activation in stress-related exhaustion: Cross-sectional observations and interventional effects. Psychiatry Res Neuroimaging 2017;269:17–25. [DOI] [PubMed] [Google Scholar]
- 24.Bloss EB, Janssen WG, Ohm DT, et al. Evidence for reduced experience-dependent dendritic spine plasticity in the aging prefrontal cortex. J Neurosci. 2011;31:7831–7839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weng HC, Hung CM, Liu YT, et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ 2011;45:835–842. [DOI] [PubMed] [Google Scholar]
- 26.Fessell DP, Goleman D. EMOTIONAL INTELLIGENCE: How Health Care Workers Can Take Care of Themselves: Harvard Business Review; 2020. [Google Scholar]
- 27.Trockel MT, Hamidi MS, Menon NK, et al. Self-valuation: Attending to the Most Important Instrument in the Practice of Medicine. Mayo Clin Proc. 2019;94:2022–2031. [DOI] [PubMed] [Google Scholar]
- 28.Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a Professional Coaching Intervention on the Well-being and Distress of Physicians: A Pilot Randomized Clinical Trial. JAMA Intern Med 2019;179:1406–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zou X, Durazzo TC, Meyerhoff DJ. Regional Brain Volume Changes in Alcohol-Dependent Individuals During Short-Term and Long-Term Abstinence. Alcohol Clin Exp Res 2018;42:1062–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koutsimani P, Montgomery A, Georganta K. The relationship between burnout, depression, and anxiety: A systematic review and meta-analysis. Front Psychol. 2019;10:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swensen S, Shanafelt TD. Mayo Clinic Strategies to Reduce Burnout: 12 Actions to Create the Ideal Workplace New York, NY: Oxford University Press; 2020. [Google Scholar]
- 32.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. . JAMA Intern Med 2014;174:527–533. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt TD, West CP, Sinsky C, et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc 2019;94:1681–1694. [DOI] [PubMed] [Google Scholar]


