Abstract
Objective:
To estimate the prevalence of psychiatric disorders and their continuity since childhood among young adults from the same ethnic group living in two low-income contexts.
Method:
Young adults (N=2,004; ages 15–29) were followed (82.8% retention) as part of the Boricua Youth Study, a study of Puerto Rican youth recruited at ages 5–13 in the South Bronx (SBx), NY, and Puerto Rico (PR). We estimated prevalence (lifetime; past year) of major depressive (MDD), mania, hypomania, generalized anxiety (GAD), tobacco dependence, and any other substance use disorders (SUD).
Results:
The prevalence of every disorder was higher among young women from the SBx compared with those from PR (eg, 9.2% versus 4.1% past-year SUD; 14% versus 6.8% for MDD/GAD). Among SBx young men, tobacco dependence and illicit SUD were elevated. Across both contexts, men had higher adjusted odds of illicit SUD than women, while women had higher GAD than men. MDD did not differ by gender. Young adulthood disorders (except for AUD, GAD) followed childhood disorders. For example, childhood externalizing disorders preceded both MDD (young men and women) and illicit SUD (young women only).
Conclusion:
Young women raised in a context where adversities like ethnic discrimination concentrate are at high risk for psychiatric disorders. In certain high-poverty contexts, young men may present with MDD as often as women. Interventions to prevent psychiatric disorders may need to address gender-specific processes and childhood disorders. However, SUD prevention among young men may need to address other factors.
Keywords: young adult, depression, substance abuse, ethnicity, development
Introduction
Young adulthood,1 when most psychiatric disorders - both mental and substance use disorders (SUD) - peak or emerge,2,3 is a period of critical developmental challenges for youth from vulnerable populations.4 This may be true particularly for ethnic minority youth who experience high levels of poverty and stress and are exposed to discrimination as well as other cultural stressors.5–7 During this period of challenges and increased risk, a better understanding of psychiatric disorders among youth living in disadvantaged contexts due to poverty and stress provides an opportunity to promote healthy development in circumstances of risk and to identify points of intervention to alter negative trajectories that can persist into adulthood.
The prevalence of lifetime and past-year psychiatric disorders in young adults,8,9 and how psychiatric disorders in childhood influence psychiatric disorders in young adulthood are yet to be described specifically among young adults of a homogeneous diverse ethnic group raised in low-income contexts.8 In addition, youth of diverse ethnic background raised in a context where they are part of a disadvantaged minority population, such as Latino youth living in the United States, are likely to experience specific stressors.10 For example, acculturation, or the process of adaptation to a different culture, has been linked to psychiatric disorders and substance use in children and adults of certain Latino subgroups in the United States.7,11–18 Among Latino subgroups in the US, Puerto Rican adults report the highest rates of substance use and abuse disorder, suicidal behavior, depressive disorders, and anxiety disorders.11,19,20 This may be due to the high level of acculturation, migration patterns, and specific contextual factors.
There is also variation in psychiatric disorders within the same group living in different contexts. A recent cross-sectional study compared past year psychiatric disorders among island Puerto Rican adults (ages 18–64) and Puerto Rican adults in the mainland, and showed higher rates of most psychiatric disorders among the mainland compared to the island population.21 As Latino youth living in a context where they are part of a minority group become more independent, they may experience new hardships or forms of discrimination and social disadvantage related to education, employment, housing, and others that place them at increased risk of mental health problems. A better understanding of the influence of context on an earlier developmental period (young adulthood), and its relationship to incidence of psychopathology later on, is now warranted.
Our formulations about the origins of mental disorders in young adulthood among Puerto Rican children is based on a developmental psychopathology framework,22 that originally aimed to integrate developmental psychology, clinical psychiatry and clinical psychology, but has since evolved to include cultural influences.23 Within this expanded framework, culture is conceptualized at the social and individual levels, and development of psychopathology is not independent of cultural risks and protective factors such as discrimination, acculturation and familism.24,25
Previous examinations of externalizing disorders during early childhood in the present cohort (Boricua Youth Study; see Bird at al.26 and Duarte et al.27 for study methodology) indicate that there initially were no differences in antisocial behaviors between Puerto Ricans living in the South Bronx, New York (SBx) and those living in San Juan, Puerto Rico (PR).28 However, as the cohort aged, elevated levels of antisocial behaviors were observed in youth in the SBx during late childhood/early adolescence.29 A recent analysis examined a subsample of participants in young adulthood and found elevated rates of generalized anxiety disorder and MDD (marginal) among those living in the SBx when compared to those living in PR.30 However, this analysis aimed to identify specific socio-cultural mechanisms related to increased risk, and did not generate estimates of psychiatric disorders for the full sample. Also, it did not focus specifically on gender differences or on the developmental course of psychiatric disorders.
In the case of children growing up as an ethnic minority in a disadvantaged urban area, such as the SBx, where adversities cluster, increased risk of poor mental health may be closely related to challenges associated with the experience of discrimination and the integration of Spanish-based values and practices with American ones. Context may also shape gender-specific expression of psychiatric disorders because of its influence on role expectations and values, particularly during the transition from adolescence to adulthood. Generally, the prevalence of SUD is higher among men than women,31 while the prevalence of depression and anxiety is higher among women.32,33 Among Latino young adults, these differences could be accentuated by traditional gender norms and child-rearing practices that establish specific gender expectations for behaviors. For example, values such as machismo (male dominant gender roles) have been related to SUD while simpatia (kindness) and marianismo (purity in women) have been linked to internalizing disorders.34,35
While the onset of some psychiatric disorders may occur in young adulthood, the overwhelming majority of disorders present in young adulthood have been preceded by disorders in childhood and early adolescence; these earlier disorders can either be the same36–38 or a different disorder.38–40 However, it remains to be seen whether the same patterns appear in non-White racial/ethnic groups. As the levels and types of stressors that youth of certain ethnic backgrounds may face can differ, it is possible that the patterns of continuity of psychiatric disorders are different.
The current study examines selected psychiatric disorders including MDD, GAD, mania, hypomania, tobacco dependence, alcohol use disorder, and illicit SUD (club drugs, cocaine, hallucinogens, inhalants, marijuana, opioids, painkillers, sedatives, stimulants, and other drugs) in a general population sample of Puerto Rican young adults growing up in two distinct contexts that are of high risk for the development of psychopathology due to growing up in contexts of poverty and other stressors. One group lives in a context where the young adults are part of an ethnic minority group (the South Bronx, NYC) living in an urban context where poverty is compounded by other risks such as neighborhood violence or high substance abuse. The other group also lives in a low-income context, however, in which they are the ethnic majority (San Juan, Puerto Rico). We examine differences in the prevalence of psychiatric disorders in young adulthood by recruitment site (or context), gender, and continuity of psychopathology from childhood/early adolescence.
Method
Sample Description
The Boricua Youth Study is a longitudinal study of two sub-samples of Puerto Rican youth: one from the SBx, New York (N=1,138), and another from the Standard Metropolitan Area of San Juan and Caguas, Puerto Rico (PR) (N=1,353). Each sub-sample is a multistage probability sample of Puerto Rican households in the target areas. To be eligible for participation, there had to be at least one child between the ages of 5 and 13 present in the household, and the child and at least one caregiver had to identify as being of Puerto Rican background. Up to three randomly selected children were enrolled per household. Information about the sampling design and study procedures have been presented elsewhere in greater detail.26
Briefly, participants were initially assessed in year 2000 at Wave 1 (W1) and were interviewed yearly for a total of three waves over three years, in Waves 2 and 3 (W2, W3), through 2004. A fourth wave (W4) of data collection (2013–2017) was more recently carried out when participants were between 15 and 29 years of age (Mage=22.88, SD=2.85). As fewer than 5% of those who participated in Wave 4 were ages 15–17 and only 0.2% were 29 years old, for simplicity we refer to BYS participants at Wave 4 as young adults.27 The present analysis focuses primarily on the Wave 4 assessment (N=2,004; retention rate = 83.1% in the SBx; 82.5% in PR, calculated based on eligible participants) but also includes data from the prior assessments. The Institutional Review Boards at the New York State Psychiatric Institute and the University of Puerto Rico Medical School approved study procedures.
Measures
Psychiatric disorders and substance abuse in young adulthood.
Psychiatric disorders in young adulthood were assessed at Wave 4 through youth self-report, using the World Mental Health Organization Composite International Diagnostic Interview (WMH-CIDI).41,42 The WMH-CIDI is a standardized diagnostic interview to ascertain past year and lifetime psychiatric disorders per the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) criteria.43 A Spanish translation of the WMH-CIDI is available.41 The instrument has demonstrated adequate concordance with the Structured Clinical Interview for Axis 1 Disorders (SCID) in both languages, and for most DSM-IV diagnoses.44–46 Importantly, study retention rates were satisfactory for those who had internalizing (80.5%) and externalizing (80.2%) disorders as children. For W4, we assessed tobacco dependence, alcohol abuse/dependence (AUD), illicit substance abuse/dependence (illicit SUD), major depressive disorder (MDD), mania, hypomania, and generalized anxiety disorder (GAD). To facilitate understanding of processes that may be shared across similar types of disorders, we created composite variables to represent classes of disorders: any substance abuse/dependence (or “any SUD”, which includes illicit SUD and/or AUD but excludes tobacco dependence), either major depressive disorder or generalized anxiety disorder (“MDD/GAD”), and either any substance abuse/dependence (excluding tobacco), major depressive disorder or generalized anxiety disorder (“any SUD or MDD/GAD”).
Psychiatric disorders in childhood.
We use parental reports of any lifetime internalizing diagnosis which included depressive disorder (MDD or dysthymia) and anxiety disorder (generalized anxiety disorder, social phobia, specific phobia, panic disorder, and post-traumatic stress disorder); and of any externalizing disorder, including disruptive behavior disorder (conduct disorder or oppositional defiant disorder), and attention deficit hyperactivity disorder, reported at Waves 1, 2, or 3 according to the Diagnostic Interview Schedule for Children-IV (DISC-IV).47 A positive diagnosis was one in which the child met full symptom criteria, according to parental report. Previous reports have documented the psychometrics of the DISC-IV in English and Spanish.47,48 Figure S1, available online, summarizes the different psychiatric disorders assessed in each developmental stage.
Poverty and maternal education:
Young adulthood poverty status was based on the young adult’s report of household income and number of people in household at time of interview. Mother’s level of education was assessed through youth report (W4). Education level was dichotomized to indicate whether or not the mother had completed High School.
Data Analysis
Descriptive demographic information and the prevalence of psychiatric disorders in childhood in the entire sample and by site of initial recruitment in childhood (or recruitment site) were summarized. Lifetime and past-year prevalence of specific psychiatric disorders in young adulthood by site and by gender within each site were also calculated. Disorder prevalence by site (PR vs. SBx), by site stratified by gender (e.g., young man vs. women in PR), and by gender stratified by site (e.g., PR vs. SBx in young women) were compared, and differences were assessed using chi-square tests.
Next, we fitted a series of logistic regression models to estimate the odds ratios (OR) and 95% confidence intervals (CI) for each past-year psychiatric disorder in young adulthood, including the effects of gender (young woman/man), recruitment site (PR/SBx), age group (15–20, 21–24, 25+), and presence of psychiatric disorders in childhood (any childhood internalizing disorder and any childhood externalizing disorder). To examine whether young adult psychopathology differed by gender and site or presence of childhood psychiatric disorders, three 2-way interactions between gender and site, gender and any childhood externalizing psychiatric disorder, plus gender and any childhood internalizing psychiatric disorder were included in the model.
All analyses were performed using SAS 9.4 and weighted using non-response weights combined with the original sampling weights to reflect the BYS reference population in each site (or BYS site-specific weights).27
Results
Descriptive Results
Table 1 shows descriptive statistics by recruitment site. There were no significant site differences by age group (p=0.986) or gender (p=0.987) as reported in young adulthood. Poverty status in young adulthood differed across sites (p=0.0001) with a higher proportion meeting the federal poverty threshold in PR (65.0%) compared to the SBx (56.7%). In addition, the majority of mothers of young adults from PR had obtained a high school diploma or GED (80.8%) compared to mothers of young adults initially recruited in the SBx (59.3%), p <0.0001). The prevalence of externalizing disorders in childhood was similar in the SBx and PR (18.5% versus 15.6%, p=0.112). The prevalence of childhood internalizing disorders was also not significantly different by site (12.2% versus 13.3%, p=0.509).
Table 1.
Descriptive Statistics of Boricua Youth Study Participants at Young Adulthood Assessment
| Total | SBx (N=921) | PR (N=1083) | pa | |
|---|---|---|---|---|
| n (Weighted %) | n (Weighted %) | |||
| Age at young adulthood assessment | ||||
| 15–17 | 88 | 39 (4.9) | 49 (4.7) | 0.9857 |
| 18–20 | 475 | 219 (26.1) | 256 (25.4) | |
| 21–24 | 917 | 415 (44.1) | 502 (44.8) | |
| 25+ | 524 | 248 (24.9) | 276 (25.0) | |
| Gender | ||||
| Young men | 981 | 459 (50.9) | 522 (50.9) | 0.9868 |
| Young women | 1023 | 462 (49.1) | 561 (49.1) | |
| In young adulthood | ||||
| Poverty | 1014 | 473 (56.7) | 541 (65.0) | 0.0001 |
| Mother obtained high school diploma/GED | 1274 | 499 (59.3) | 775 (80.8) | <.0001 |
| Young adulthood place of residency | ||||
| SBx | 484 | 483 (52.5) | 1 (0.1) | <.0001 |
| PR | 992 | 7 (0.8) | 985 (90.1) | |
| Other | 528 | 431 (46.7) | 97 (9.8) | |
| In childhood | ||||
| Externalizing disorder | 316 | 158 (18.5) | 158 (15.6) | 0.1116 |
| Internalizing disorder | 239 | 103 (12.2) | 136 (13.3) | 0.5092 |
Note: Percentages are weighted. Due to missing data, the total sample size for poverty, mother’s education, childhood externalizing and childhood internalizing disorder is: SBx (N=852, 833, 873, 872), PR: (847, 937, 1045, 1050) respectively. PR = Puerto Rico; SBx = South Bronx.
p value is calculated using sample weights.
Prevalence of psychiatric disorders in young adulthood
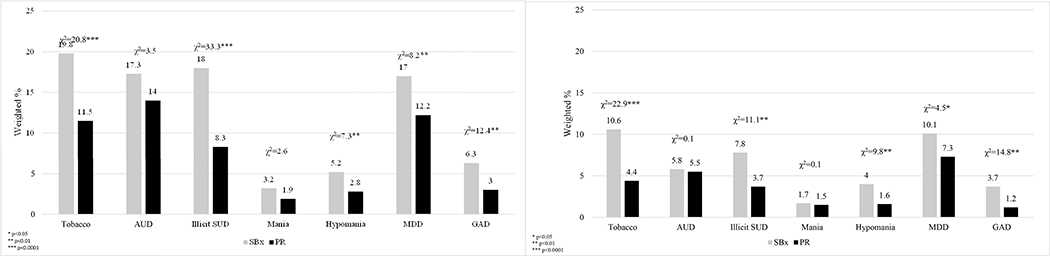
Figures 1a and 1b show the lifetime and past-year prevalence of psychiatric disorders in young adulthood by site. Lifetime prevalence (Table 2) for the disorders examined ranged from 3.2% for mania to 19.8% for tobacco dependence in participants from the SBx, and from 1.9% for mania to 14.0% for alcohol abuse or dependence in participants from PR. Past-year prevalence among participants ranged from 1.7% for mania to 10.6% for tobacco dependence in the SBx, and from 1.2% for GAD to 7.3% for MDD in PR. For most disorders, lifetime and past-year prevalence results were significantly higher in the SBx than in PR. Exceptions were AUD and mania for which no statistically significant differences were observed between sites.
Figure 1.
Prevalence of Psychiatric Disorders by Site
Note: Figure 1A presents lifetime prevalence of psychiatric disorders by site. Figure 1B presents past year prevalence of psychiatric disorders by site. Illicit SUD includes drug abuse and dependence. GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico. SBx = South Bronx; SUD = substance use disorder
Table 2.
Lifetime Prevalence of Mental and Substance Abuse Disorders in Young Adulthood
| Lifetime, n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|
| SBx |
PR |
Between Site |
||||||
| Young Men (n=459) | Young Women (n=462) | Within Site Gender p-value | Young Men (n=522) | Young Women (n=561) | Within Site Gender p-value | Young Men p-value | Young Women p-value | |
| Tobacco Dependence | 104 (22.6) | 80 (16.8) | 0.0312* | 86 (16.5) | 31 (6.3) | <.0001* | 0.0275* | <.0001* |
| Alcohol Abuse/Dependence | 93 (20.2) | 70 (14.2) | 0.0168* | 103 (19.7) | 43 (8.1) | <.0001* | 0.8322 | 0.0039* |
| Illicit SUD (Drug Abuse/Dependence) | 103 (22.6) | 62 (13.3) | 0.0004* | 59 (11.6) | 28 (4.9) | 0.0004* | <.0001* | <.0001* |
| Mania | 14 (3.2) | 14 (3.1) | 0.9772 | 15 (3.1) | 3 (0.6) | 0.0072* | 0.9799 | 0.0076* |
| Hypomania | 20 (4.2) | 29 (6.2) | 0.1642 | 22 (3.3) | 15 (2.2) | 0.2546 | 0.5104 | 0.0013* |
| MDD | 68 (15.0) | 90 (19.1) | 0.1054 | 71 (13.3) | 70 (11.1) | 0.3154 | 0.4761 | 0.0005* |
| GAD | 14 (3.5) | 44 (9.2) | 0.0011* | 16 (2.9) | 22 (3.0) | 0.9296 | 0.6329 | <.0001* |
| MDD/GAD | 72 (16.0) | 110 (23.2) | 0.0074* | 78 (14.8) | 80 (12.6) | 0.3474 | 0.6140 | <.0001* |
| Any SUDa | 151 (32.9) | 97 (20.5) | <.0001* | 135 (26.3) | 60 (10.9) | <.0001* | 0.0419* | <.0001* |
| Any SUDa or MDD/GAD | 192 (42.0) | 163 (34.5) | 0.0227* | 182 _(35.1) | 129 (21.7) | <.0001* | 0.0418* | <.0001* |
Note: GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
excluding tobacco dependence
p < .05.
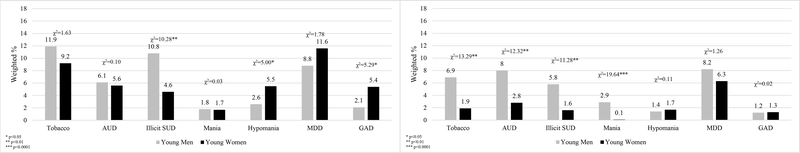
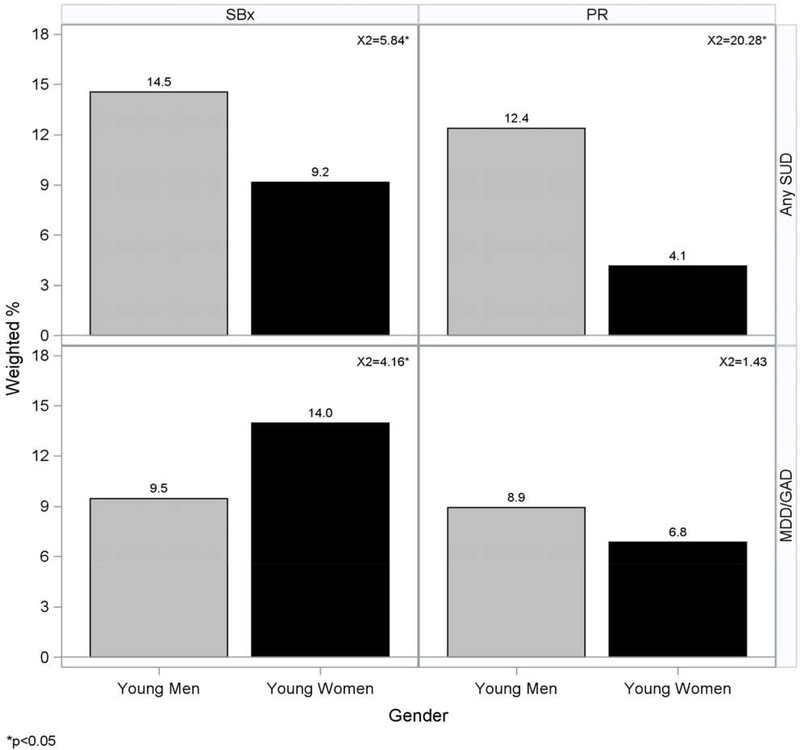
Within site, significant gender differences were found for past-year prevalence of psychiatric disorders (Figures 2a and 2b, Table 3). In the SBx, past-year prevalence of illicit SUD was higher among young men (10.8%) than young women (4.6%), while hypomania was higher among young women (5.5%) than young men (2.6%), as was GAD (5.4% in women, 2.1% in men) (Figure 2a). In PR, men had higher past year prevalence of Tobacco Dependence (6.9% vs. 1.9%), AUD (8.0% vs. 2.8%), illicit SUD (5.8% vs. 1.6%), and mania (2.9% vs. 0.1%) compared to women (Figure 2b). Figure 3 further summarizes the data by focusing on mental (MDD or GAD) and substance (SUD excluding tobacco dependence) composites by site. For these composites, significant gender differences were detected for a composite measure of any SUD (excluding tobacco dependence) and of MDD/GAD, indicating a higher past year prevalence of any SUD among men in both sites compared to women (SBx: 14.5% vs. 9.2%; PR: 12.4% vs. 4.1%), and a higher prevalence of MDD/GAD among women in the SBx compared with men (14.0% vs. 9.5%).
Figure 2.
Past Year Prevalence of Psychiatric Disorders by Site and Gender
Note: Figure 2A presents past year prevalence of psychiatric disorders in the South Bronx, by gender. Figure 2B presents past year prevalence of psychiatric disorders in Puerto rico, by gender. GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder. Illicit SUD includes drug abuse and dependence.
TABLE 3.
Past Year Prevalence of Mental and Substance Abuse Disorders in Young Adulthood
| Past Year, n (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SBx |
PR |
Between Site |
||||||||||
| Young Men | (n = 459) | Young Women | (n = 462) | Within Site Gender p | Young Men | (n = 522) | Young Women | (n = 561) | Within Site Gender p | Young Men p | Young Women p | |
| Tobacco dependence | 53 | (11.9) | 43 | (9.2) | .2023 | 35 | (6.9) | 10 | (1.9) | .0003* | .0127* | < .0001* |
| Alcohol abuse/dependence | 28 | (6.1) | 27 | (5.6) | .7503 | 43 | (8.0) | 15 | (2.8) | .0004* | .2670 | .0326* |
| Illicit SUD (drug abuse/dependence) | 49 | (10.8) | 19 | (4.6) | .0013* | 27 | (5.8) | 9 | (1.6) | .0008* | .0145* | .0077* |
| Mania | 7 | (1.8) | 8 | (1.7) | .8625 | 13 | (2.9) | 1 | (0.1) | < .0001* | .3510 | .0013* |
| Hypomania | 12 | (2.6) | 25 | (5.5) | .0254* | 7 | (1.4) | 12 | (1.7) | .7456 | .2674 | .0007* |
| MDD | 39 | (8.8) | 53 | (11.6) | .1819 | 42 | (8.2) | 42 | (6.3) | .2614 | .7811 | .0043* |
| GAD | 8 | (2.1) | 25 | (5.4) | .0214* | 7 | (1.2) | 11 | (1.3) | .8795 | .2518 | < .0001* |
| MDD/GAD | 42 | (9.5) | 64 | (14.0) | .0415* | 46 | (8.9) | 45 | (6.8) | .2325 | .7874 | .0002* |
| Any SUDa | 66 | (14.5) | 41 | (9.2) | .0157* | 62 | (12.4) | 22 | (4.1) | < .0001* | .3749 | .0022* |
| Any SUDa or MDD/GAD | 97 | (21.5) | 92 | (19.9) | .5762 | 94 | (18.6) | 63 | (10.3) | .0003* | .3065 | < .0001* |
Note: GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
Excluding tobacco dependence
p < .05.
Figure 3.
Past Year Prevalence of Psychiatric Disorders by Site and Gender
Note: Illicit SUD includes drug abuse and dependence. GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
Main effect of sociodemographic characteristics and childhood psychiatric disorders
Table 4, Table 5 and Table 6 shows the results of the logistic regression models. The adjusted models without interactions revealed that on average, women have a lower risk for Tobacco Dependence, AUD, illicit SUD, any SUD and any SUD or MDD/GAD; but increased risk for GAD. No gender differences were observed for MDD or MDD/GAD combined. Young adults from the SBx were at higher risk than those from PR for all disorders examined except AUD. Age was not related to any of the psychiatric disorders examined, except for tobacco dependence. Externalizing and internalizing disorders during childhood/early adolescence were associated with increased odds of young adult MDD/GAD, and any SUD or MDD/GAD.
TABLE 4.
Adjusted Logistic Regression Models Predicting Past-Year Psychiatric Disorders in Young Adulthood
| Tobacco Dependence |
Alcohol Abuse/Dependence |
Illicit SUDa |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| AOR | (95% CI) | p | AOR | (95% CI) | P | AOR | (95% CI) | p | |
| Adjusted models without interaction | |||||||||
| Young women (reference young men) | 0.57* | (0.41, 0.79) | .0007 | 0.56* | (0.39, 0.81) | .0021 | 0.35* | (0.24, 0.52) | < .0001 |
| SBx site in childhood (reference PR) | 2.51* | (1.81, 3.48) | < .0001 | 1.11 | (0.77, 1.58) | .5817 | 2.30* | (1.59, 3.31) | < .0001 |
| Age group | .1279 | .2713 | .4313 | ||||||
| 21–24 (reference 15–20) | 0.85 | (0.58, 1.24) | .3918 | 1.41 | (0.91, 2.17) | .1237 | 0.77 | (0.51, 1.15) | .1962 |
| ≥ 25 (reference 15–20) | 1.25 | (0.83, 1.86) | .2825 | 1.29 | (0.79, 2.12) | .3112 | 0.77 | (0.48, 1.23) | .2755 |
| 21–24 (reference ≥ 25) | 0.68* | (0.46, 1.00) | .0491 | 1.09 | (0.70, 1.68) | .7064 | 1.00 | (0.63, 1.58) | .9845 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 2.22* | (1.56, 3.16) | < .0001 | 1.39 | (0.90, 2.14) | .1399 | 1.23 | (0.78, 1.92) | .3725 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.31 | (0.84, 2.03) | .2278 | 1.43 | (0.89, 2.32) | .1422 | 1.04 | (0.62, 1.77) | .8705 |
| Adjusted models with interactions | |||||||||
| Young women (reference young men) | 0.42* | (0.28, 0.63) | < .0001 | 0.51* | (0.35, 0.76) | .0009 | 0.30* | (0.19, 0.48) | < .0001 |
| SBx site in childhood (reference PR) | 2.98* | (2.06, 4.31) | < .0001 | 1.28 | (0.87, 1.87) | .2100 | 2.61* | (1.70, 4.00) | < .0001 |
| Age group | |||||||||
| 21–24 (reference 15–20) | 0.84 | (0.57, 1.22) | .3583 | 1.40 | (0.90, 2.15) | .1315 | 0.75 | (0.50, 1.13) | .1725 |
| ≥ 25 (reference 15–20) | 1.21 | (0.81, 1.81) | .3588 | 1.27 | (0.77, 2.10) | .3394 | 0.75 | (0.47, 1.20) | .2311 |
| 21–24 (reference ≥ 25) | 0.69 | (0.47, 1.02) | .0624 | 1.10 | (0.71, 1.69) | .6818 | 1.01 | (0.64, 1.60) | .9770 |
| Site × gender | .0033* | .0031* | .2307 | ||||||
| Comparing young women with young men | |||||||||
| In SBx | 0.75 | (0.50, 1.11) | .1517 | 0.96 | (0.57, 1.61) | .8812 | 0.41* | (0.25, 0.66) | .0003 |
| In PR | 0.26* | (0.14, 0.50) | < .0001 | 0.31* | (0.17,0.54) | < .0001 | 0.24* | (0.11, 0.49) | .0001 |
| Comparing SBx with PR | |||||||||
| Among young women | 5.08* | (2.71, 9.54) | < .0001 | 2.30* | (1.24, 4.26) | .0084 | 3.45* | (1.62, 7.36) | .0013 |
| Among young men | 1.80* | (1.21, 2.68) | .0038 | 0.73 | (0.46, 1.16) | .1814 | 2.01* | (1.32, 3.07) | .0012 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 2.39* | (1.67, 3.42) | < .0001 | 1.45 | (0.93, 2.25) | .1006 | 1.45 | (0.91, 2.30) | .1175 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.33 | (0.85, 2.08) | .2054 | 1.45 | (0.89, 2.38) | .1375 | 1.09 | (0.62, 1.92) | .7585 |
| Any externalizing childhood psychiatric diagnosis × gender | .3001 | .5175 | .0482* | ||||||
| Comparing any externalizing childhood diagnosis with none | |||||||||
| Among young women | 2.87* | (1.56, 5.26) | .0007 | 1.71 | (0.80, 3.65) | .1627 | 2.27* | (1.02, 5.09) | .0455 |
| Among young men | 1.76* | (1.14, 2.71) | .0110 | 1.11 | (0.65, 1.90) | .6904 | 0.82 | (0.48, 1.40) | .4679 |
| Any internalizing childhood psychiatric diagnosis × gender | .6244 | .8726 | .9749 | ||||||
| Comparing any internalizing childhood diagnosis to none | |||||||||
| Among young women | 1.68 | (0.86, 3.27) | .1305 | 1.60 | (0.75, 3.43) | .2227 | 1.34 | (0.54, 3.32) | .5276 |
| Among young men | 1.11 | (0.61, 2.00) | .7321 | 1.37 | (0.73, 2.55) | .3298 | 0.95 | (0.49, 1.82) | .8724 |
Note: AOR = adjusted odds ratio; GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
Illicit SUD includes drug abuse and dependence.
p < .05.
TABLE 5.
Adjusted Logistic Regression Models Predicting Past-Year Psychiatric Disorders in Young Adulthood
| MDD |
GAD |
MDD/GAD |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| AOR | (95% CI) | p | AOR | (95% CI) | p | AOR | (95% CI) | p | |
| Adjusted models without interaction | |||||||||
| Young women (reference young men) | 1.11 | (0.83, 1.48) | .4849 | 1.97* | (1.14, 3.40) | .0152 | 1.19 | (0.91, 1.57) | .2086 |
| SBx site in childhood (reference PR) | 1.42* | (1.06, 1.89) | .0174 | 3.15* | (1.77, 5.60) | < .0001 | 1.54* | (1.17, 2.02) | .0021 |
| Age group | .4569 | .9427 | .6557 | ||||||
| 21–24 (reference 15–20) | 0.88 | (0.63, 1.24) | .4798 | 0.88 | (0.48, 1.62) | .6842 | 1.00 | (0.72, 1.38) | .9797 |
| ≥ 25 (reference 15–20) | 1.12 | (0.77, 1.63) | .5554 | 0.97 | (0.49, 1.94) | .9403 | 1.16 | (0.81, 1.67) | .4206 |
| 21–24 (reference ≥ 25) | 0.79 | (0.55, 1.13) | .1942 | 0.90 | (0.47, 1.75) | .7653 | 0.86 | (0.61, 1.20) | .3733 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.62* | (1.15, 2.28) | .0060 | 1.23 | (0.64, 2.39) | .5342 | 1.47* | (1.06, 2.06) | .0229 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.37 | (0.92, 2.04) | .1174 | 1.58 | (0.80, 3.12) | .1920 | 1.50* | (1.04, 2.18) | .0305 |
| Adjusted models with interactions | |||||||||
| Young women (reference young men) | 1.04 | (0.77, 1.40) | .7906 | 1.61 | (0.86, 3.00) | .1361 | 1.10 | (0.83, 1.47) | .4958 |
| SBx site in childhood (reference PR) | 1.41* | (1.05, 1.88) | .0212 | 2.85* | (1.57, 5.17) | .0005 | 1.51* | (1.14, 1.99) | .0037 |
| Age group | |||||||||
| 21–24 (reference 15–20) | 0.88 | (0.63, 1.24) | .4675 | 0.88 | (0.48, 1.63) | .6874 | 0.99 | (0.72, 1.37) | .9638 |
| ≥ 25 (reference 15–20) | 1.11 | (0.77, 1.62) | .5724 | 0.96 | (0.48, 1.93) | .9127 | 1.15 | (0.80, 1.66) | .4438 |
| 21–24 (reference ≥ 25) | 0.79 | (0.55, 1.13) | .1969 | 0.92 | (0.47, 1.78) | .7970 | 0.86 | (0.61, 1.21) | .3860 |
| Site × gender | .0557 | .1809 | .0126* | ||||||
| Comparing young women with young men | |||||||||
| In SBx | 1.41 | (0.94, 2.12) | .0945 | 2.54* | (1.28, 5.02) | .0076 | 1.62* | (1.11, 2.37) | .0129 |
| In PR | 0.81 | (0.53, 1.23) | .3228 | 1.10 | (0.41, 2.92) | .8556 | 0.80 | (0.53, 1.20) | .2853 |
| Comparing SBx with PR | |||||||||
| Among young women | 1.87* | (1.24, 2.83) | .0028 | 4.38* | (2.01, 9.52) | .0002 | 2.17* | (1.47, 3.20) | .0001 |
| Among young men | 1.07 | (0.71, 1.62) | .7409 | 1.89 | (0.77, 4.62) | .1625 | 1.07 | (0.72, 1.59) | .7392 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.58* | (1.12, 2.25) | .0099 | 1.07 | (0.50, 2.30) | .8546 | 1.43* | (1.02, 2.02) | .0392 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.36 | (0.91, 2.03) | .1327 | 1.59 | (0.78, 3.24) | .2061 | 1.50* | (1.03, 2.17) | .0335 |
| Any externalizing childhood psychiatric diagnosis × gender | .1125 | .2518 | .1007 | ||||||
| Comparing any externalizing childhood diagnosis with none | |||||||||
| Among young women | 2.18* | (1.32, 3.60) | .0024 | 1.86 | (0.82, 4.23) | .1396 | 2.07* | (1.28, 3.36) | .0030 |
| Among young men | 1.32 | (0.82, 2.12) | .2537 | 0.85 | (0.28, 2.63) | .7798 | 1.17 | (0.73, 1.87) | .5127 |
| Any internalizing childhood psychiatric diagnosis × gender | .2494 | .6687 | .4789 | ||||||
| Comparing any internalizing childhood diagnosis with none | |||||||||
| Among young women | 1.17 | (0.66, 2.08) | .5857 | 1.53 | (0.65, 3.59) | .3248 | 1.43 | (0.85, 2.39) | .1767 |
| Among young men | 1.58 | (0.91, 2.75) | .1065 | 1.60 | (0.50, 5.07) | .4279 | 1.57 | (0.91, 2.68) | .1020 |
Note: AOR = adjusted odds ratio; GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
p < .05.
TABLE 6.
Adjusted Logistic Regression Models Predicting Past-Year Psychiatric Disorders in Young Adulthood
| Any SUDa |
Any SUDa or MDD/GAD |
|||||
|---|---|---|---|---|---|---|
| AOR | (95% CI) | p | AOR | (95% CI) | p | |
| Adjusted models without interaction | ||||||
| Young women (reference young men) | 0.44* | (0.33, 0.59) | < .0001 | 0.71* | (0.57, 0.89) | .0022 |
| SBx site in childhood (reference PR) | 1.57* | (1.20, 2.07) | .0012 | 1.56* | (1.26, 1.93) | < .0001 |
| Age group | .6337 | .4507 | ||||
| 21–24 (reference 15–20) | 1.15 | (0.84, 1.59) | .3833 | 1.14 | (0.89, 1.47) | .3081 |
| ≥ 25 (reference 15–20) | 1.04 | (0.71, 1.51) | .8451 | 1.15 | (0.86, 1.54) | .3390 |
| 21–24 (reference ≥ 25) | 1.11 | (0.79, 1.56) | .5464 | 0.99 | (0.76, 1.29) | .9441 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.31 | (0.93, 1.85) | .1193 | 1.39* | (1.06, 1.81) | .0172 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.17 | (0.79, 1.74) | .4259 | 1.36* | (1.00, 1.84) | .0474 |
| Adjusted models with interactions | ||||||
| Young women (reference young men) | 0.39* | (0.29, 0.54) | < .0001 | 0.67* | (0.53, 0.83) | .0004 |
| SBx site in childhood (reference PR) | 1.80* | (1.33, 2.42) | .0001 | 1.62* | (1.30, 2.02) | < .0001 |
| Age group | ||||||
| 21–24 (reference 15–20) | 1.14 | (0.83, 1.57) | .4175 | 1.14 | (0.88, 1.46) | .3271 |
| ≥ 25 (reference 15–20) | 1.02 | (0.70, 1.48) | .9252 | 1.14 | (0.85, 1.53) | .3729 |
| 21–24 (reference ≥ 25) | 1.12 | (0.80, 1.58) | .5119 | 0.99 | (0.76,1.30) | .9700 |
| Site × gender | .0112* | .0041* | ||||
| Comparing young women with young men | ||||||
| In SBx | 0.60* | (0.41, 0.88) | .0088 | 0.95 | (0.71, 1.28) | .7269 |
| In PR | 0.27* | (0.17, 0.44) | < .0001 | 0.50* | (0.36, 0.69) | < .0001 |
| Comparing SBx with PR | ||||||
| Among young women | 2.69* | (1.63, 4.46) | .0001 | 2.26* | (1.62, 3.17) | < .0001 |
| Among young men | 1.23 | (0.88, 1.71) | .2237 | 1.18 | (0.89, 1.57) | .2449 |
| Any externalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.44* | (1.02, 2.04) | .0386 | 1.42* | (1.08, 1.86) | .0114 |
| Any internalizing childhood psychiatric diagnosis (reference no diagnoses) | 1.22 | (0.81, 1.83) | .3390 | 1.35 | (0.99, 1.84) | .0542 |
| Any externalizing childhood psychiatric diagnosis × gender | .0636 | .0281* | ||||
| Comparing any externalizing childhood diagnosis with none | ||||||
| Among young women | 2.04* | (1.13, 3.69) | .0180 | 1.99* | (1.30, 3.05) | .0017 |
| Among young men | 0.93 | (0.61, 1.41) | .7237 | 1.04 | (0.74, 1.47) | .8126 |
| Any internalizing childhood psychiatric diagnosis × gender | .7308 | .6207 | ||||
| Comparing any internalizing childhood diagnosis with none | ||||||
| Among young women | 1.51 | (0.80, 2.82) | .1999 | 1.40 | (0.89, 2.19) | .1479 |
| Among young men | 1.03 | (0.62, 1.72) | .9002 | 1.34 | (0.89, 2.02) | .1660 |
Note: AOR = adjusted odds ratio; GAD = generalized anxiety disorder; MDD = major depressive disorder; PR = Puerto Rico; SBx = South Bronx; SUD = substance use disorder.
Excluding tobacco dependence.
p < .05.
Interactions between gender and site
Multiplicative effect modification between gender and site were significant for Tobacco Dependence (p=0.003), AUD (p=0.003), MDD/GAD (p=0.013), any SUD (p=0.011) and any SUD or MDD/GAD (p=0.004). For these outcomes, the interaction indicated that (a) gender differences were stronger in PR than in the SBx, except for MDD/GAD, for which the gender effect was only significant in the SBx and (b) that site differences were more prominent among young women, rather than young men. Specifically, gender differences in tobacco dependence, AUD, and any SUD or MDD/GAD were observed in PR but not in the SBx. For example, PR, women had lower odds of AUD (OR=0.31; 95%CI=0.17–0.54) than men; whereas no significant differences between men and women were found in the SBx (OR=0.96; 95%CI=0.57–1.61). Also, among women, compared to those in PR, those from the SBx had elevated odds of Tobacco Dependence (OR=5.08; 95%CI=2.71–9.54), AUD (OR=2.30; 95%CI=1.24–4.26), MDD/GAD (OR=2.17; 95%CI=1.47–3.20), any SUD (OR=2.69; 95%CI=1.63–4.46) and any SUD or MDD/GAD (OR=2.26; 95%CI=1.62–3.17), while among men, elevated risk was only identified for Tobacco Dependence (OR=1.80; 95%CI=1.21–2.68) and illicit SUD (OR=2.01; 95%CI=1.32–3.07).
Interactions between gender and childhood disorders
Externalizing disorders during childhood/early adolescence by gender interactions were significant for illicit SUD (p=0.048) and any SUD or MDD/GAD (p=0.028). Specifically, the odds of past year illicit SUD (OR=2.27, 95%CI=1.02–5.09) and any SUD or MDD/GAD (OR=1.99, 95%CI = 1.30–3.05) were higher among young women with any externalizing childhood disorder compared to young women without any externalizing childhood disorders. There were no significant interactions between internalizing childhood disorders and gender.
Discussion
In the first population-based study of Puerto Rican young adults from the SBx and PR, we identified approximately one in three young men and one in five young women from the South Bronx, and about one in four young men and one in ten young women in Puerto Rico presented with a lifetime SUD (alcohol or drug). Lifetime prevalence of MDD was 15% among young men and 19% among young women in the SBx; in PR, it was 13% and 11%, respectively. While direct comparisons to national estimates are not possible because of differences in the diagnostic criteria, or because of a lack of gender-specific prevalence of disorders for this ethnic group as young adults, our findings suggest a risk for psychiatric disorders comparable to the general population for the SBx sample and mostly lower for the PR sample.9,49
We observed three significant variations in the prevalence of mental disorders and SUD by gender and by context. First, young women of Puerto Rican background originally from the SBx had elevated risk of all measured past year disorders compared to young women originally from PR; among men, differences by context were not as pronounced with only prevalence of tobacco dependence and illicit SUD being higher among men in the SBx. Second, for all psychiatric disorders studied, patterns of gender differences were consistent with prior studies31,33 except for MDD in both sites, for which young women and men did not differ. Third, young adulthood disorders (with the exception of AUD and GAD) were preceded by childhood psychiatric disorders. For example, young adulthood MDD was related to childhood externalizing disorders, as was young adulthood illicit SUD but only among young women.
Our first finding was that the prevalence of several disorders was higher among youth from the SBx than those from PR. Detailed analysis revealed that the elevated prevalence among the SBx young adults compared to those in PR was mostly due to young women in the SBx having higher prevalence than those in PR. This was true for any psychiatric disorder (any SUD or MDD/GAD) and even more so for tobacco dependence. Puerto Rican youth living in the South Bronx are an ethnic minority group living in a context where they will likely experience poverty coupled with different types of adversities. As Puerto Rican youth assimilate to such context, they may experience their (and their parents’) hopes of integration into mainstream America failing to happen as expected. Demoralization and frustration often accompany such experiences and may underlie the development of psychiatric disorders.50
According to the second finding, gender differences were as expected for all disorders examined, except for MDD.2 In the present study, young women and men presented a similar prevalence of MDD, rather than women having higher prevalence. This agrees with findings from the World Mental Health survey in China,51 but differs from results of a review and meta-analysis of studies of gender differences in MDD, which showed that the overall OR was 1.95 for women’s risk compared to men’s with consistency in women’s higher levels of MDD and its symptoms.52 The authors found that overall, gender differences peak in adolescence, decline through the 20s, then stabilize. In that meta-analysis, few studies included substantial numbers of U.S. Hispanic participants and no moderating effect of ethnicity on the association between gender and depression was detected.52
Studies about Puerto Rican young adults also indicate that women are at higher risk for depression than men.53 A study of adolescents ages 11 to 17 conducted 20 years ago in Puerto Rico found that the prevalence of past-year MDD was significantly higher among girls (7.23%) than boys (1.73%).35 However, there were no gender differences in prevalence or odds of major depressive disorder. In this younger sample, the prevalence for girls was similar to what we found among BYS young women from PR (6.3%). However, the prevalence among BYS young men from PR (8.2%) was almost five times higher.30 Among adults, two studies conducted in the 1990s53,54 agreed with the National Latino and Asian American Study, conducted 17 years ago, which also showed women having a higher prevalence of lifetime (19.8%) and past-year (10.8%) MDD than men (10.9% and 6.4%, respectively).55 In the BYS, prevalence of lifetime MDD was 15.0% for men from the SBx and 13.3% for men from PR. Thus, the lack of gender differences in MDD found in the present study seems to be due to the unusually high prevalence of depression among men from both contexts.
Lack of opportunities as evidenced in low social mobility and high rates of poverty might explain these elevated rates of MDD among men. In both the SBx and PR, men may feel responsible for providing for their families financially and therefore may be especially susceptible to consequences of “frustrated freedom”,45 as they become young adults growing up in close contact with the financial achievements of certain groups in the American culture and experiencing high unemployment rates, limited opportunities, and inequity and discrimination both at the individual and societal (e.g. the status of PR as a U.S. territory) level.46 In 2014, the unemployment rate for Puerto Ricans in New York (12.2%) and Puerto Ricans on the island (18.9%) were both high, compared to the US national average at the time (6%).56 Studies of Puerto Ricans have reported high prevalence of depression among unemployed participants and elevated risk for depression among underemployed men.20 In both contexts, more than one quarter of those 25 years and older do not have a high school diploma or equivalent. These socioeconomic limitations – both at the individual and the community level – could specifically impact depression levels of BYS young men in both contexts. Future research should examine how the influence of individual and contextual opportunities for social mobility on depression impacts men.
The third study finding was that certain disorders in young adulthood were predicted by psychiatric disorders occurring more than ten years earlier (between the ages of 5 and 15). Externalizing disorders in childhood, but not internalizing as found by others,38,40 predicted MDD in young adulthood. Consistent with a recent meta-analysis of 37 longitudinal studies,57 externalizing disorders in childhood predicted tobacco dependence and illicit SUD, but in our sample the association with illicit SUD was found among young women only. It is unclear why boys with externalizing childhood disorders were also not more likely to present with illicit SUD in young adulthood. It is possible that for illicit SUD in young men, previously mentioned socio-cultural factors that are likely relevant for this specific ethnic group, are more important for understanding later risk than the presence of a childhood disorder itself.
Interestingly, MDD was also predicted by externalizing disorders in childhood, as also reported in prior studies.40 As children with externalizing disorders tend to experience critical deficiencies in academic performance and relationships with their peers and families, the cumulative impact of these “failures” might result in the development of depression over time.58 As presence of externalizing disorders was related to future development of both MDD and SUD in young adulthood, prevention of these conditions early in life may reduce psychiatric disorders in early adulthood, with particular impact for young women.
The fact that AUD or GAD in young adulthood were not related to any type of childhood disorder may indicate that, for these disorders, concurrent socioenvironmental factors could be more important than earlier psychopathology. Findings based on other high-risk samples (e.g.59) also suggest a developmental psychopathology process that may contrast to those from other population-based developmental research that frequently observes that anxiety disorders are likely to follow most disorders earlier in life.38,47,60 Other factors may be at play for youth living in high-risk contexts. For example, a longitudinal study of ethnically diverse students enrolled in schools in high-risk neighborhoods in Seattle found that a strong attachment to school and good parenting (e.g. monitoring, proper rewards) in childhood and adolescence were protective against AUD in young adulthood (age 21).61 In that study children/adolescents with more problem behaviors and more opportunities to associate with and bond to antisocial peers were at greater risk for AUD in young adulthood. If future research confirms that there may be some variations in the way psychiatric disorders in childhood are related to those in young adulthood based on gender or other socio-cultural factors, interventions need to be tailored to address the needs of specific groups.
This study needs to be considered in light of its limitations. First, the youngest age group (ages 16–17) is quite small and needed to be combined with the next age bracket so that stable models could be examined. Therefore, additional work would be required to better understand if the same patterns occur when late adolescents transition to young adulthood. Second, analyses were restricted to two mental disorders (MDD and GAD) and SUD. It is possible that if a wider range of problems had been examined, the patterns here described would be different. Third, when examining psychiatric disorders in childhood and in young adulthood, there were methodological differences (instrument and informant) between the first three compared to the fourth study wave, which may have influenced study results. These differences were methodologically motivated (e.g., parents were the only possible informant for children who were too young). However, as many of our results are consistent with others in the literature, it is unlikely that this limitation would have biased our results in a systematic way. Finally, due to the multiple hypotheses tested, study findings could be the result of type I error and warrant replication to be confirmed.
Elucidating context- and gender-based patterns of psychopathology, in a non-selected, probability-based sample of young adults belonging to the Latino subgroup (Puerto Ricans) at highest risk for psychopathology and SUD,11 is highly relevant to focus intervention efforts. A recent BYS paper focused on MDD and anxiety disorders in young adulthood points to the relevance of socio-cultural processes for understanding the early development of psychopathology among youth.30 Earlier BYS work focused on childhood and early adolescence, together with existing literature, has identified the importance of socio-cultural risk and protective factors. For example, higher parental acculturation and experiences of discrimination and cultural stress in children have been related to higher symptomatology and poor outcomes.7,15,16,62 On the other hand, the well-established relationship between parenting behaviors and children’s antisocial behaviors was modified by experiences of cultural stress.16 However, traditional cultural values (e.g., familism, maternal warmth) may offer protection and promote positive outcomes.63,64
The longitudinal study design allowed the prospective examination of childhood psychopathology as an early determinant of current problems, with substantial implications for improving knowledge on etiology and prevention among children from an ethnic group living in low-SES contexts. Future research, utilizing this sample and others, should aim to deepen our understanding of the socio-cultural and developmental mechanisms contributing to different manifestation of psychiatric disorders among Puerto Ricans, and possibly other ethnically diverse youth, growing up in disadvantaged contexts.
Supplementary Material
Figure S1. Psychiatric Diagnoses Assessed in the Boricua Youth Study
Acknowledgments
The Boricua Youth Study was supported by the National Institutes of Health [Waves 1–3 by MH56401 (Bird), Wave 4 by DA033172 (Duarte), and MH098374 (Alegria, Canino, Duarte)].
Dr. Wall, Mr. Adams, and Ms. Choi served as the statistical experts for this research.
Footnotes
Disclosure: Drs. Duarte, Canino, Wall, Ramos-Olazagasti, Elkington, Bird, Carliner, Wainberg, and Alegria, Ms. Choi, Mr. Adams, and Ms. Klotz have reported no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Cristiane S. Duarte, Columbia University, New York, NY; New York State Psychiatric Institute, Columbia University Medical Center, New York, New York.
Glorisa J. Canino, Behavioral Sciences Research Institute, University of Puerto Rico School of Medicine, San Juan.
Melanie Wall, Columbia University, New York, NY; New York State Psychiatric Institute, Columbia University Medical Center, New York, New York.
Maria Ramos-Olazagasti, Child Trends, Bethesda, MD.
Katherine S. Elkington, Columbia University, New York, NY; New York State Psychiatric Institute, Columbia University Medical Center, New York, New York.
Hector Bird, Columbia University, New York, NY.
C. Jean Choi, Columbia University, New York, NY.
Christopher Adams, Columbia University, New York, NY.
Jaimie Klotz, Columbia University, New York, NY.
Hannah Carliner, Columbia University, New York, NY; New York State Psychiatric Institute, Columbia University Medical Center, New York, New York.
Milton L. Wainberg, Columbia University, New York, NY; New York State Psychiatric Institute, Columbia University Medical Center, New York, New York.
Margarita Alegria, Massachusetts General Hospital, Harvard Medical School, Boston.
References
- 1.Institute of Medicine and National Research Council. Investing in the health and well-being of young adults. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 2.Merikangas KR, McClair VL. Epidemiology of substance use disorders. Hum Genet. 2012;131(6):779–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maughan B, Collishaw S. Development and psychopathology: a life course perspective. Rutter’s Child and Adolescent Psychiatry. 2015:1–16. [Google Scholar]
- 4.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469. [PubMed] [Google Scholar]
- 5.McLaughlin KA, Breslau J, Green JG, et al. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Soc Sci Med. 2011;73(7):1088–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stuber J, Galea S, Ahern J, Blaney S, Fuller C. The association between multiple domains of discrimination and self-assessed health: a multilevel analysis of Latinos and blacks in four low-income New York City neighborhoods. Health Serv Res. 2003;38(6p2):1735–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duarte CS, Bird HR, Shrout PE, et al. Culture and psychiatric symptoms in Puerto Rican children: longitudinal results from one ethnic group in two contexts. J Child Psychol Psychiatry. 2008;49(5):563–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mennis J, Stahler G, Mason M. Risky substance use environments and addiction: a new frontier for environmental justice research. Int J Environ Res Public Health. 2016;13(6):607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007;97(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canino G, Alegría M. Understanding psychopathology among the adult and child Latino population from the United States and Puerto Rico. Handbook of US Latino psychology: Developmental and Community-based Perspectives. 2009:31. [Google Scholar]
- 13.Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;188(11):728–735. [DOI] [PubMed] [Google Scholar]
- 14.Broudy R, Brondolo E, Coakley V, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. J Behav Med. 2007;30(1):31–43. [DOI] [PubMed] [Google Scholar]
- 15.Ramos-Olazagasti MA, Shrout PE, Yoshikawa H, Canino GJ, Bird HR. Contextual risk and promotive processes in Puerto Rican youths’ internalizing trajectories in Puerto Rico and New York. Dev Psychopathol. 2013;25(3):755–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wei C, Eisenberg RE, Ramos-Olazagasti MA, et al. Developmental psychopathology in a racial/ethnic minority group: are cultural risks relevant? J Am Acad Child Adolesc Psychiatry. 2017;56(12):1081–1088. e1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawton KE, Gerdes AC. Acculturation and Latino adolescent mental health: integration of individual, environmental, and family influences. Clin Child Fam Psychol Rev. 2014;17(4):385–398. [DOI] [PubMed] [Google Scholar]
- 18.Schwartz SJ, Unger JB, Zamboanga BL, et al. Developmental trajectories of acculturation: links with family functioning and mental health in recent-immigrant Hispanic adolescents. Child Dev. 2015;86(3):726–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fortuna LR, Perez DJ, Canino G, Sribney W, Alegria M. Prevalence and correlates of lifetime suicidal ideation and attempts among Latino subgroups in the United States. J Clin Psychiatry. 2007;68(4):572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): the association between birthplace, acculturation and alcohol abuse and dependence across Hispanic national groups. Drug Alcohol Depend. 2009;99(1):215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canino G, Shrout PE, NeMoyer A, et al. A comparison of the prevalence of psychiatric disorders in Puerto Rico with the United States and the Puerto Rican population of the United States. Soc Psychiatry Psychiatr Epidemiol. 2019:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cicchetti D The emergence of developmental psychopathology. Child Dev. 1984;55(1):1–7. [PubMed] [Google Scholar]
- 23.Causadias JM. A roadmap for the integration of culture into developmental psychopathology. Dev Psychopathol. 2013;25(4pt2):1375–1398. [DOI] [PubMed] [Google Scholar]
- 24.García Coll C, Akerman A, Cicchetti D. Cultural influences on developmental processes and outcomes: Implications for the study of development and psychopathology. Dev Psychopathol. 2000;12(3):333–356. [DOI] [PubMed] [Google Scholar]
- 25.García Coll C, Crnic K, Lamberty G, et al. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996;67(5):1891–1914. [PubMed] [Google Scholar]
- 26.Bird HR, Canino GJ, Davies M, et al. A study of disruptive behavior disorders in Puerto Rican youth: I. background, design, and survey methods. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1032–1041. [DOI] [PubMed] [Google Scholar]
- 27.Duarte C, Canino GJ, Alegria M, et al. Developmental psychopathology & ethnicity: I. the young adulthood assessment of the Boricua Youth Study. J Am Acad Child Adolesc Psychiatry. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bird HR, Davies M, Duarte CS, Shen S, Loeber R, Canino GJ. A study of disruptive behavior disorders in Puerto Rican youth: II. baseline prevalence, comorbidity, and correlates in two sites. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1042–1053. [DOI] [PubMed] [Google Scholar]
- 29.Bird HR, Shrout PE, Davies M, et al. Longitudinal development of antisocial behaviors in young and early adolescent Puerto Rican children at two sites. J Am Acad Child Adolesc Psychiatry. 2007;46(1):5–14. [DOI] [PubMed] [Google Scholar]
- 30.Alegria MS, Patrick E, Canino G, et al. The effect of minority status and social context on the development of depression and anxiety: a longitudinal study of Puerto Rican descent youth. World Psychiatry. 2019;18(3):298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry. 2016;73(1):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 33.Vesga-López O, Schneier F, Wang S, et al. Gender differences in generalized anxiety disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. 2008;69(10):1606. [PMC free article] [PubMed] [Google Scholar]
- 34.Stone RAT, Meyler D. Identifying potential risk and protective factors among non-metropolitan Latino youth: cultural implications for substance use research. J Immigr Minor Health. 2007;9(2):95–107. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez-Guarda RM, Ortega J, Vasquez EP, De Santis J. La mancha negra: substance abuse, violence, and sexual risks among Hispanic males. West J Nurs Res. 2010;32(1):128–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sourander A, Multimäki P, Nikolakaros G, et al. Childhood predictors of psychiatric disorders among boys: a prospective community-based follow-up study from age 8 years to early adulthood. J Am Acad Child Adolesc Psychiatry. 2005;44(8):756–767. [DOI] [PubMed] [Google Scholar]
- 37.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66(7):764–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60(7):709–717. [DOI] [PubMed] [Google Scholar]
- 39.Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. J Child Psychol Psychiatry. 2006;47(3–4):276–295. [DOI] [PubMed] [Google Scholar]
- 40.Copeland WE, Adair CE, Smetanin P, et al. Diagnostic transitions from childhood to adolescence to early adulthood. J Child Psychol Psychiatry. 2013;54(7):791–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alegria M, Vila D, Woo M, et al. Cultural relevance and equivalence in the NLAAS instrument: integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. Int J Methods Psychiatr Res. 2004;13(4):270–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: 1994. [Google Scholar]
- 44.Alegria M, Shrout PE, Torres M, et al. Lessons learned from the clinical reappraisal study of the Composite International Diagnostic Interview with Latinos. Int J Methods Psychiatr Res. 2009;18(2):84–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sen A Development as freedom In: Roberts J, Hite AB & Chorev N, ed. The globalization and development reader: perspectives on development and global change. Vol 2: Wiley-Blackwell; 1999:525–547. [Google Scholar]
- 46.Falcón A Colonial reparations for Puerto Rico: a framework for a postcolonial transition. Latino Studies. 2018;16(4):559–562. [Google Scholar]
- 47.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. [DOI] [PubMed] [Google Scholar]
- 48.Bravo M, Ribera J, Rubio-Stipec M, et al. Test-retest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC-IV). J Abnorm Child Psychol. 2001;29(5):433–444. [DOI] [PubMed] [Google Scholar]
- 49.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74(3):223–234. [DOI] [PubMed] [Google Scholar]
- 50.Lewis-Fernández R, Morcillo C, Wang S, et al. Acculturation dimensions and 12-month mood and anxiety disorders across US Latino subgroups in the National Epidemiologic Survey of Alcohol and Related Conditions. Psychol Med. 2016;46(9):1987–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. 2017;143(8):783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Potter L, Rogler L, Mościcki E. Depression among Puerto Ricans in New York City: the Hispanic health and nutrition examination survey. Soc Psychiatry Psychiatr Epidemiol. 1995;30(4):185–193. [DOI] [PubMed] [Google Scholar]
- 54.Vera M, Alegría M, Freeman D, Robles RR, Ríos R, Ríos CF. Depressive symptoms among Puerto Ricans: island poor compared with residents of the New York City area. Am J Epidemiol. 1991;134(5):502–510. [DOI] [PubMed] [Google Scholar]
- 55.Lorenzo-Blanco EI, Cortina LM. Latino/a depression and smoking: an analysis through the lenses of culture, gender, and ethnicity. Am J Community Psychol. 2013;51(3–4):332–346. [DOI] [PubMed] [Google Scholar]
- 56.The Center for Puerto Rican Studies. Puerto Ricans in New York, the United States, and Puerto Rico, 2014. 2016. Accessed June 26, 2019.
- 57.Groenman AP, Janssen TW, Oosterlaan J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(7):556–569. [DOI] [PubMed] [Google Scholar]
- 58.Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. Am Psychol. 1989;44(2):329–335. [DOI] [PubMed] [Google Scholar]
- 59.Abram KM, Zwecker NA, Welty LJ, Hershfield JA, Dulcan MK, Teplin LA. Comorbidity and continuity of psychiatric disorders in youth after detention: a prospective longitudinal study. JAMA Psychiatry. 2015;72(1):84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry. 2011;52(10):1015–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Guo J, Hawkins JD, Hill KG, Abbott RD. Childhood and adolescent predictors of alcohol abuse and dependence in young adulthood. J Stud Alcohol. 2001;62(6):754–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morcillo C, Ramos-Olazagasti MA, Blanco C, et al. Socio-cultural context and bullying others in childhood. J Child Fam Stud. 2015;24(8):2241–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morcillo C, Duarte CS, Shen S, Blanco C, Canino G, Bird HR. Parental familism and antisocial behaviors: development, gender, and potential mechanisms. J Am Acad Child Adolesc Psychiatry. 2011;50(5):471–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Santesteban-Echarri O, Ramos-Olazagasti MA, Eisenberg RE, et al. Parental warmth and psychiatric disorders among Puerto Rican children in two different socio-cultural contexts. J Psychiatr Res. 2017;87:30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Psychiatric Diagnoses Assessed in the Boricua Youth Study