Abstract
Exercise training can improve lower‐limb cutaneous microvascular reactivity in adults with venous leg ulceration; however, there is a lack of research on patients' views about the acceptability and feasibility of exercise interventions. The aim of this study was to explore participants' experiences of the trial “Exploring the Feasibility of Implementing a Supervised Exercise Training and Compression Hosiery Intervention in Patients with Venous Ulceration” (FISCU). Semi‐structured face‐to‐face and telephone interviews were used to investigate participants' experiences (n = 16) of taking part in the FISCU trial. Data were analysed using thematic analysis. Three overarching themes were identified, along with 11 sub‐themes: (a) sedentary cautious living (because of pain and reduced mobility, treatment and perceived control, and advice to rest and be careful), (b) key components of the exercise trial (including motivation, an individualised intervention supervised by a specialist exercise professional, and satisfaction with the intervention), and (c) benefits of exercise (physical benefits and healing, psychological well‐being, positive impact on comorbidities, and an improved self‐management strategy). This study found that an exercise intervention was viewed by participants as positive, acceptable, and feasible while living with a venous leg ulcer. An individualised and supervised exercise programme was key to build confidence to exercise.
Keywords: exercise, feasibility, participant experience, qualitative, venous leg ulcers
1. INTRODUCTION
1.1. Rationale
Exercise training can improve lower‐limb cutaneous microvascular reactivity in adults with venous leg ulceration.1 However, there is a lack of research on participants' views about the acceptability and feasibility of exercise as an adjunct therapy to compression therapy. The most common treatment for venous ulcers is compression therapy, providing graded external compression to the leg, opposing the hydrostatic forces of venous hypertension.2, 3 It is accepted that, in order to break the circle of ulceration and chronic venous insufficiency recurrence (which reaches up to 33% within a year),4 lifestyle factors such as nutrition, exercise, and smoking should also be considered part of a strategy for managing venous leg ulcers (VLUs).5 Published research from our group6 and others7, 8 has explored the feasibility of using such interventions in this clinical group. Such modifiable lifestyle factors are mentioned in clinical guidelines on the management of VLUs9, 10, 11 but have received relatively little emphasis from a patient perspective to date.
Given the infancy of the research in the area, there has been little exploration of patient‐reported experiences of engaging in exercise therapy interventions designed to improve ulcer‐healing outcomes. However, The National Institute for Health and Care Excellence9 and Scottish Intercollegiate Guidelines Network10 guidelines currently advocate that people with VLUs should be given advice about healthy lifestyle choices, and patients are advised to keep physically active by using calf muscle pump exercises. The process of obtaining participant insight data is recommended by the Medical Research Council in the development and evaluation of complex health interventions.12 If people with VLUs are expected to engage in and sustain these behaviours, then we must understand the patient experience of doing so. Much contemporary research on active living behaviour among older adults is guided by Social Cognitive Theory (SCT).13 Physical activity interventions based on SCT have demonstrated success in promoting increased physical activity for people with VLUs14 and have provided a framework for factors influencing adherence, such as focusing on self‐efficacy.15 Identifying the barriers, enablers, and benefits of exercise therapy in this population will help to plan effective interventions and inspire other members of this clinical population to initiate and maintain exercise therapy.
O'Brien and colleagues provided important qualitative insights into the perspectives of adults with VLUs on the topic of exercise.16 Findings demonstrated that adults with VLUs are interested in becoming active or maintaining active lifestyles. A host of noteworthy factors that underpin adults' understanding of the relationship between chronic venous insufficiency and perceived or actual exercise patterns was uncovered through semi‐structured interviews and discussions. These factors included the following: exercise knowledge can act as a motivator for exercise, adults with VLUs can accrue general physiological benefits through exercise, and knowing if one's condition was acute or chronic could influence one's appreciation of the importance of exercise for condition management. Furthermore, this work offers important insights into perceived factors that limit exercising, how structured management facilitates exercise, and how fear of harm critically impacts positive beliefs and attitudes to exercise.16 The current research project will add to existing knowledge by exploring the key components of an exercise intervention for people with VLUs from the patients' perspective.
1.2. Objective
The aim of this study was to explore participants' experiences of taking part in a trial that investigated the feasibility of exercise training alongside compression therapy for the management of VLU healing—“Exploring the Feasibility of Implementing a Supervised Exercise Training and Compression Hosiery Intervention in People with Venous Ulceration” (FISCU), an National Institute for Health Research (NIHR)‐funded study (PB‐PG‐0213‐30029). Given that exercise training for the management of VLU healing is an emerging, new, potential therapy, the research team was keen to understand participants' experiences and perspectives of the acceptability and feasibility of the exercise training programme.
2. METHODS
2.1. Study design
Ethical approval for this study was received from the South Yorkshire Ethics Committee (14/YH/0091). The study used semi‐structured face‐to‐face and telephone interviews to investigate participant's experiences of taking part in the FISCU trial. Face‐to‐face or telephone interviews were selected as they allowed for a more personalised experience to be explored rather than exploring themes in a group session, such as a focus group. To minimise the burden of travel on participants with limited mobility, face‐to‐face interviews were offered alongside their physiological follow‐up health assessment. Prior to commencing the interviews, participants had p 12 weeks of participation in the FISCU trial (post‐baseline). Participants who had been randomised to the exercise arm of the trial followed an exercise training programme while wearing their compression hosiery or bandaging as described in the trial protocol.17 This included three supervised exercise sessions each week comprising of aerobic, resistance, and flexibility exercises.
2.2. Sample
Qualitative sub‐study inclusion criteria required that participants:
were part of the main FISCU trial
had participated for a minimum of 12 weeks of exercise post‐baseline.
2.3. Recruitment
Sixteen participants with VLUs were recruited using purposive sampling that ensured a mixture of genders and younger and older participants. Participants included those treated with a mixture of compression hosiery and bandaging. Participants were approached either in person or by telephone by the main research assistant on the study to take part in the qualitative study as they were about to complete their 12‐week follow‐up assessment. All participants who were invited to take part in the interview agreed to be interviewed.
2.4. Data collection
A semi‐structured interview guide was formulated based on previous literature and the authors' past experience in qualitative research (Table 1). Rapport was established between all participants and the interviewer prior to conducting the interviews by considering their health and fitness assessments. Interviews took place at Sheffield Hallam University (the same location as the exercise sessions and health assessments).
Table 1.
Semi‐structured interview topic guide
Background:
|
The research study:
|
All interviews were audio‐recorded and transcribed verbatim. Interviews lasted between 15 minutes and 60 minutes according to the length of participant responses. All transcripts were checked for accuracy, with a sample being reviewed by coinvestigators. After 16 interviews, there was an agreement between authors that data saturation was reached and that no new information relevant to the research aims was evident.
2.5. Data analysis
The interview data were analysed by a process guided by the principles of thematic analysis,18 particularly framework analysis.19 Framework analysis offers a systematic approach that is somewhat inductive; that is, it is based on the original interview transcripts but framed within an a priori framework, such as a topic guide, whereby questions are known at the outset of the interview. Framework analysis is well‐suited to the needs of health services research and participants with long‐term health conditions.16 The five stages of framework analysis consist of (a) familiarisation, (b) reading and re‐reading the transcripts, (c) identifying a thematic framework, (d) coding or indexing, and (e) charting and mapping.19
An initial thematic framework was produced, drawing on the trial's a priori interviews and reading the transcripts highlighting salient issues. Transcripts were coded to offer insight into the topic areas being investigated, making constant reference to the study aim. Multiple codes were assigned to elements of the data. Any feature of the data that demonstrated insight into the phenomenon being studied was eligible for coding. Coded data extracts (quotes) were charted for each participant case. Comparison of coded quotes was conducted within and between the transcripts. Codes were subsequently collated to illustrate broad themes and define further sub‐themes. Discussions and consensus between lead researchers finalised the mapping and interpretation of key themes and sub‐themes.
Prior to analysis, participants were offered the opportunity to review their transcripts, providing triangulation to the methods and verification of content. H.J.C, who has over a decade of experience in qualitative research methods and has published numerous qualitative research studies on exercise for people with long‐term chronic health conditions, performed the initial coding. S.K. led the interviews and reviewed the codes and also has several years' experience in qualitative research methods in exercise for people with different medical conditions. A third mixed‐methods researcher, E.M., transcribed the interviews verbatim and independently read the transcripts and read the thematic framework and confirmed the validity of the themes and sub‐themes.
3. RESULTS
Sixteen participants took part in this qualitative study (12 face‐to‐face and four telephone interviews) of the 39 participants who took part in the main research trial. All except one participant were White British people (similar ethnicity to participants in the FISCU trial). Of the participants, 56% were male (n = 9). The mean age of participants was 65 ± 11 years; 81% were retired, and the remainder (19%) were employed in a sedentary occupation. The mean time since participants' first VLU diagnosis was 7 ± 11 years. At the time of interview, the mean duration of participants' current VLU was 7 ± 14 months.
Three overarching themes and 11 sub‐themes were identified through thematic data analysis (presented in Figure 1):
Sedentary cautious living can be a result of a fear of movement because of pain and reduced mobility, treatment and perceived control, and advice to rest and be careful.
Key components of the exercise trial included motivation for taking part, an individualised intervention supervised by a specialist exercise professional, and satisfaction with the exercise intervention.
Benefits of exercise included perceived physical benefits and healing, psychological well‐being, positive impact on comorbidities, and an improved self‐management strategy.
Figure 1.
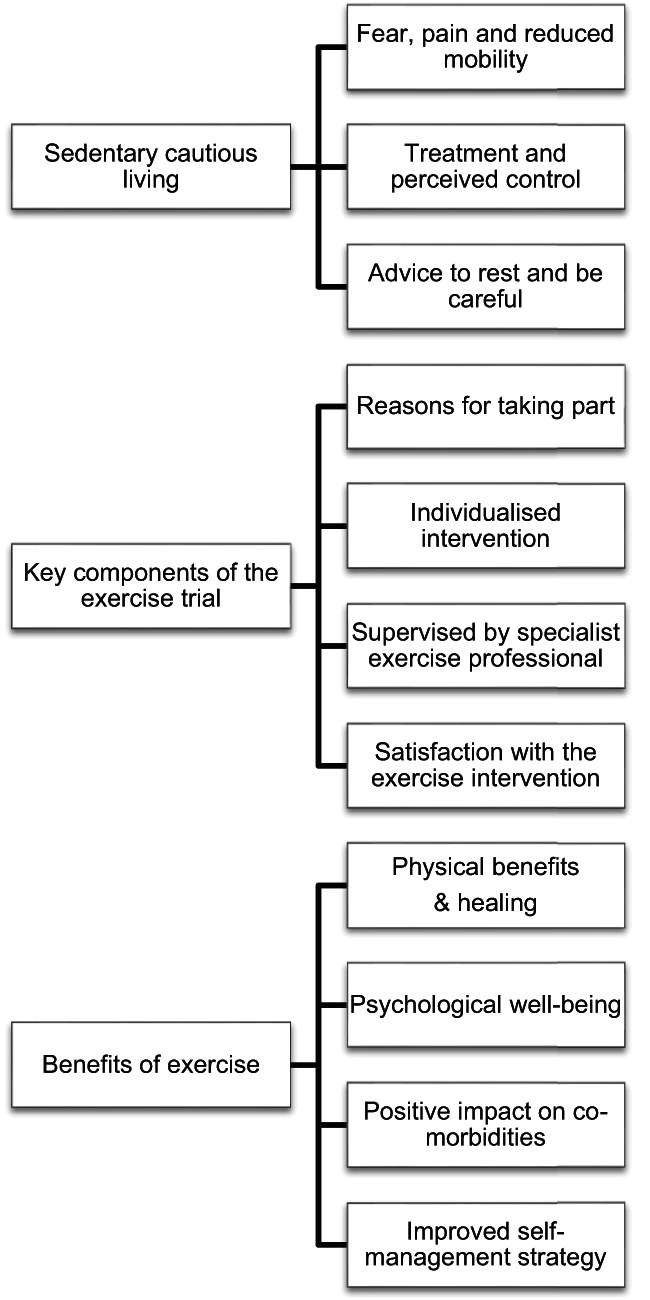
Themes from participant views taking part in an exercise randomised control trial
3.1. Sedentary cautious living
3.1.1. Fear, pain, and reduced mobility
Participants' insights demonstrated a chronic, complex, and unpredictable condition that, at times, could be painful, physically limiting, and emotionally challenging with the potential to negatively impact their well‐being and quality of life and ability to exercise. Therefore, many participants were uncertain and (in some cases) fearful about participating in an exercise programme. Half of the participants had experienced pain that was considered to be a significant debilitating feature of the condition. For example, one participant stated:
There has been times when the pain has controlled me and that can be challenging because I try not let them dominate my life but sometimes you do have to sit back and say well today I'm just going to sit here. (participant 014, exercise group)
3.1.2. Treatment and perceived control
It was not uncommon for participants to be treated in a specialist tissue viability clinic two to three times a week to have their wounds redressed and re‐bandaged. Some participants were concerned about the added commitment of travelling to starting an exercise programme on top of treatment time commitments. A combination of treatment modalities included compression bandaging and compression hosiery, dressings antibiotics, painkiller medication, and skin care regimes with creams. Some of individuals also believed that compression stockings and bandages limited motion and leg muscle activity. Showering and bathing were highlighted as day‐to‐day activities that were negatively impacted by the condition. Some participants needed assistance to put on and take off their compression stockings, which caused a challenge to personal hygiene for exercising, with one participant stating:
It is difficult to wash and I can't get my stockings on and off on my own without help. (participant 015, exercise group)
Most participants had experienced the condition for several months and even years, and several participants disclosed that the near‐constant intrusion into their lives had created behaviour patterns based on settling for doing less, just pottering, talking themselves out of doing physical activity, and becoming more sedentary than they were previously. For example, one participant said:
I tend to settle for stuff … this sitting doing nothing kind of thing you think oh well maybe if I'd been a bit the other way I'd been thinking no you need to get up and do something don't just settle for this. (participant 019, exercise group)
Participants also felt limited as to how much personal influence they had on the ulcer‐healing process:
I seem to win little battles with them, they seem to start to heal and then they deteriorate again it's like two steps backwards one step forwards. I've really struggled for the past on and off for 10 years. (participant 013, Exercise group)
In some participants, it was clear that their ulcer experience had a negative impact on their lives, and they were “fed‐up” with the condition:
The last thing I want to do is going back to sitting doing nothing because it really is soul destroying and it's that makes you feel worthless because you can't do anything. (participant 019, Exercise group)
3.1.3. Advice to rest and be careful
The key messages of advice regarding condition management that participants readily recalled were: to be careful; to protect the leg from knocks and elevate the leg when, for example, playing with grandchildren, dogs jumping up at them, and exposure to insect bites in summer; and to generally be in a state of heightened awareness. This resulted in the majority of the participants living what can be described as anxious and “cautious lives”, including avoidance of physical activity. Participants believed that health professionals' advice to rest, emphasised the importance of being cautious:
I dared not exercise or move in case it made the leg ulcer worse. I was frightened that if I accidentally knocked it I would be back to square one again. So I just started doing less and less activity. (participant 014, Exercise group)
They've (nurses) always told me you know rest keep your leg up that is what I was told before for years. (participant 009, exercise group)
The constant perceived risk of aggravating a current ulcer or somehow triggering a new ulcer created feelings of fear towards activity. Participants were constantly mindful and fearful of the risk of making things worse, possible recurrences, and setbacks. One participant recalled:
I was simply worn out but it was difficult my greatest fear was getting it so badly infected that I would end up with gangrene. (participant 001, exercise group)
Reflections on exercise advice from health care professionals concluded that the majority of participants (n = 12) had not received any specific exercise advice and that the benefits of exercise had never been explicitly linked to their condition:
They didn't suggest exercise they just say elevate your leg keep it elevated you know, go and lay down for an hour every afternoon and do it that way but that's all they could say. (participant 017, exercise group)
The lack of specific advice on exercise goals was perceived to be confusing:
It is contradictory in a way I had this out with the nurse yesterday when she wrapped my legs will break it down a bit more on my right leg with ulcer she says “you are resting aren't you?” and I said yes course I am and I put my legs up while you know while I am sat watching telly and that and “you're exercising them aren't you?” so it's like contradicting itself are you resting a lot or are you exercising it is contradictory to what they want me to do. (participant 008, exercise group)
3.2. Key components of the exercise trial
3.2.1. Reasons for taking part in the project
Participants commented that they chose to take part in the study for the following reasons: to help with research, to learn more about exercise, to meet other people, to have an incentive to leave the house, and having a perception that the study was trustworthy as it was being run by a university and was unlikely to do harm. Participants stated:
It was positive it was a different treatment it wasn't just drugs it wasn't just bandages it was an alternative to try something new because I've had this ulcer for years. (participant 001, exercise group)
The support of family and a health care professional advocating and endorsing study participation helped participants decide to take part in the study:
I actually saw this booklet and I took the trouble to read it because I could see the word exercise and then I saw there was a personal trainer and I thought that sounds interesting. I thought well I will just send an email on for a bit more information and that and I spoke to my family my daughter and my son and that and said what I was thinking of doing and they just said just go for it. So I thought well it can't do any harm. (participant 009, exercise group)
A couple of participants offered the following comments, which demonstrate their partial understanding of the aetiology of the condition and how exercise might be beneficial for their condition:
She (nurse) often mentioned, she would say things like you should you get up and do stuff. But nobody has actually said till I came here, or pointed out the benefits towards healing a leg ulcer, but after it was said to me, well that kind of makes complete sense. It's (exercise has) got to benefit everything you do but I think when you think about exercise, you don't apply the benefits to the healing process. You don't think about that, but once it's mentioned it become obvious and you think we'll of course. (participant 019, exercise group)
3.2.2. Individualised intervention
The supervised exercise intervention was specifically tailored to the condition and also took account of existing comorbidities. It was described as being adaptable to the individual's ability with regard to gradual, paced progression of exercise intensity. For those who took part in the exercise intervention arm of the trial and completed the interview, they described the set routine of exercises as being manageable as they were able to perform the exercises within their own limitations while wearing compression hosiery or bandages:
Well we have been doing the treadmill then various stretching exercises, ankle exercises, standing up & sitting down, going up and down on tip toes. (participant 015, exercise group)
Another participant also stated:
Yes you can do proper exercises that are aimed at that sort of thing rather than just walking; walking is fine but to be able to do exercises that you know are working on the leg area and that problem. (participant 017, exercise group)
3.2.3. Supervised by a specialist exercise professional
The exercise programme offered a further social benefit of engaging in a supportive therapeutic relationship with the exercise instructor. Given that participants were undergoing treatment at the time of the study and had not experienced a similar type of approach, having a supervised intervention was an important consideration for ensuring safety, monitoring intensity, and progression and an opportunity to openly discuss the condition:
Yeah and it gives you a lot of confidence knowing that there is somebody there knowing you don't want to get you heart rate above a certain amount there's someone there to reign you in if you're trying to push too hard or gee you up if you're not going as hard as you should think that's very good thing. (participant 019, exercise group)
Another participant commented:
But here whether or not it's because you got personal training with you and talking to you, you don't really realise actually what you doing when you're on it (the treadmill) but I mean I got up to the 15 which is the highest incline you can get on it and I've never done that before. I've noticed when I'm out walking I'm walking quicker I am walking better people have told me I am walking better. (participant 009, exercise group)
3.2.4. Satisfaction with the exercise intervention
All participants remarked that they had enjoyed the exercise intervention, and they reported that it had been a worthwhile experience:
I am very happy about the research programme, everyone has been really nice and it has benefited me in a big way. (participant 007, exercise group)
Another participant agreed:
the advice has been perfect perfectly pitched for the purpose so no I can't think of anything that could be bettered I just think it's all a benefit. (participant 019, exercise group)
An additional participant commented:
The benefits I got from the course itself I feel a lot better from attending it and the instructor was excellent very, very helpful and I had a good experience. (participant 008, exercise group)
The only features of the study that were not well received related to accessing the venue in the cold weather; for some, it was awkward having to make the journey on buses as this was time consuming. In addition, one participant suggested that it would be good to have additional peers exercising at the same time to foster a social atmosphere (group sessions were available where possible for other participants):
Although I did enjoy it, at that time of year it was very cold and a lot of travelling on buses which is very hard work for me. (participant 001, exercise group)
3.3. Benefits of exercise
3.3.1. Physical benefits and healing
Participants communicated that the exercise training resulted in improvements in their physical health that translated into meaningful, functional improvements in well‐being, such as being able to walk further and quicker, helping with weight loss, reducing fatigue, and feeling stronger in the legs. For example, one participant reported:
I have a vast improvement to the way I'm feeling to the way I'm holding myself the way I move people are saying you look totally different you're walking a lot better I'm walking a lot further and it's not until I felt the benefits from this that I realised fully how bad things had got. (participant 019, exercise)
Another participant mentioned:
Over last few weeks I've noticed a big change in my legs I feel a lot more sturdy on my legs and I don't seem to tire as quick either but that might be due to the weight loss as well but I think it's all combined factors. (participant 014, exercise group)
Performing exercise had, for one participant, prevented the usual pattern of fluid build‐up, which was associated with ulcer onset:
The benefits I've had from this are absolutely amazing I don't feel like the same fella anymore and I'm sure I heal quickly anyway but I'm sure the fact that I'd started exercising also had a lot to do with that and its healed and it's been healed for a few weeks. (participant 019, exercise group)
Another participant said:
I should say from the beginning it just sort of healed so quickly that you know I have never seen my leg heal that quickly before I can honestly say that and I think they were a bit surprised at the clinic. (participant 009, exercise group)
An additional participant talked about his or her improvements:
I can do 30mins now and we started at 10/15 minutes so it's all built up and improved everything and I say the ulcer is almost healed almost, I'm sure the exercise has helped it, definitely. (participant 017, exercise group)
3.3.2. Psychological well‐being
Several participants reported a new confidence in their ability to exercise, which was mediated by progression in fitness and increased exercise competence:
The exercise has been useful in as I say helping your well‐being and I've really enjoyed it and look forward to coming, I look forward to it. (participant 015, exercise group)
3.3.3. Positive impact on comorbidities
Participants explained how they were not only living with venous leg ulceration but also with other conditions. The types of conditions included: type II diabetes, musculoskeletal conditions (back), depression, anxiety, rheumatoid arthritis, chronic obstructive pulmonary disease (COPD), and knee pain. The presence of other long‐term comorbidities was responsible for further limiting daily activities and general health and well‐being. Participants expressed the view that the current FISCU exercise intervention, although designed specifically for adults with leg ulcers, also had transferable benefits that helped them manage the symptoms of their other conditions:
I've got COPD and the programme that I've had has been modified to allow for my breathing, I feel like a different fella from the one that came in here a few weeks ago. (participant 019, exercise group)
The same participant noted:
I'm moving better and faster because of this programme compared to when I first came. For example if I parked in the car park and made my way up here I would have to stop half a dozen times to catch my breath now I'm parking up and coming straight up. If you'd have told me before I started that I would be able to do that I would have laughed at you… the benefits I feel from this programme are just immeasurable. (participant 019, exercise group)
3.3.4. Improved self‐management strategy for a long‐term health condition
A common finding for the majority who engaged in the exercise arm of the study was that they were capable of participating in structured exercise and could obtain meaningful well‐being benefits from that participation. For many, this was counterintuitive as previously held beliefs to rest and “be careful” had led to talking oneself out of activities and adopting a more sedentary lifestyle. The realisation that participants could perform exercise training that might result in improved ulcer healing was a powerful incentive to adhere to the programme and continue exercising beyond the study. For example, one participant thought:
I've always had the opinion that when you've got leg ulcers you don't need to be going to the gym, that's it, you don't do it. Now I'm thinking the total opposite I'm thinking really I do need to get back in that gym and even my nurse said you want to carry on doing this now because she said I've noticed the improvement in your ulcers. (participant 014, exercise group)
Other participants stated:
I'd convinced myself I couldn't do stuff and you and this programme have convinced me that I can and I can do a lot more than I thought I could. (participant 019, exercise group)
Instead of just sat looking at the television I've started to take the dog for a walk or go to the shops to get some fruit… things I'm doing different now and staying more active which I plan to continue. (participant 021, exercise group)
4. DISCUSSION
The purpose of this research was to understand participants' experience of taking part in a trial that investigated the feasibility of supervised aerobic and resistance exercise training alongside compression therapy for the management of VLUs. Interviews indicated that the exercise intervention was viewed as positive, acceptable, and a feasible approach to physical activity while living with a VLU. Themes that emerged included participants adopting sedentary and cautious living prior to the programme because of fear of movement linked to pain, reduced mobility, the time burden of treatment, and advice to rest and be careful. Confidence to take part increased by having exercise sessions supervised by a health professional tailored to meet the individual's needs and medical conditions. Participants reported that the training programme had benefits for both physical and mental well‐being and quality of life and had a positive impact on additional comorbidities. Our findings suggest that participants value support on how to exercise safely to give them the confidence to become more physically active.
Participants expressed fear prior to commencing the exercise intervention over knocking the leg with the ulcer, causing either pain or regression of healing. Fear of injury is related to fear of movement or kinesiophobia,20 which is associated with avoidance of physical activity to minimise the risk of injury or re‐injury. Avoidance of accident or trauma to the leg through safety thinking, precautions, compression treatment, and clothing is an important issue in preventing leg ulcers. However, fear becomes dysfunctional as soon as it goes beyond safety thinking and precautions.21 This was seen in those individuals, who believed that physical activity was a risk‐taking action, described as “fear of injury.” Qualitative research exploring perspectives of adults with VLUs on exercise agree with these findings that a patient's fear of harm can impact their positive beliefs and attitudes to exercise.7, 22 This suggests that experiential learning while participants take part in a supervised exercise training programme can reduce fear of harm, particularly if participants experience benefits of exercise as opposed to adverse effects.
Participants described previously receiving conflicting advice from health professionals on whether they needed to rest and “elevate the leg” or take part in exercise. This is similar to findings of previous research, which found that participants reported contradictory advice given from health professionals in relation to exercise or physical activity.23 Our findings agree with Roaldsen et al, who reported that lifestyle advice such as “live as usual” and contradictory exercise advice is not a useful approach.21 This confusing advice could be because of the lack of current guidelines for participants in relation to what type of exercise or physical activity is recommended for their chronic disease of VLUs. However, research providing the evidence base to underpin guidelines on physical activity for VLUs is growing.1, 8, 24, 25 This suggests that providing specific information, rather than general advice, on exercise is important for people with leg ulcers. This guidance needs to include information on the specific types of activity that are suitable.
Participants believed that supervised exercise sessions tailored to their individual needs increased their confidence to be physically active. According to SCT, the construct of self‐efficacy, or confidence, is a key determinant of self‐management of behaviours.26 Previous research has found that self‐efficacy is significantly related to adherence to an exercise programme for people with leg ulcers.15 The mechanism behind increased self‐confidence in our study is likely to be because of increased participant belief that they were able to achieve their exercise goals.
Our study found that travel to and from the exercise facilities was reported to be a barrier for some participants, particularly those with limited mobility. Travel to and from exercise facilities has previously been reported to be a barrier to exercise and physical activity.27 The concept of lack of time is particularly pertinent for people with leg ulcers who are visiting tissue viability clinics several times a week, perhaps alongside work or other family commitments, over several months or years.16 Other research has looked at the patient experience of both supervised and home‐based exercise for participants with leg ulcers.23, 28 Home‐based exercise programmes with telephone support have been found to increase a patient's self‐efficacy.15 A home‐based exercise, with specialised exercise instruction at the start of the programme to increase patient confidence, would be a useful area for further research, particularly for participants with reduced mobility for travel.
Some patients faced practical barriers, including limitation of movement, and challenges maintaining personal hygiene after exercising because of bandages and dressings or needed assistance to take off or put on their compression hosiery. Previous research also reports participants discussing difficulties getting into the bath or being unable to have their foot or leg washed for a long time.29 Other literature also found that patients feared compressions stockings and bandages limiting motion and leg muscle activity.21 Participants found that timing exercise sessions before an appointment with a specialist tissue nurse or using assisting devices to help get compression hosiery on and off gave them support with personal hygiene. This highlights the importance of education about how to manage the side effects of physical activity, including advice on practical considerations for VLUs.
An important aspect of self‐management of a long term health condition is an understanding of the benefits of physical activity, specifically in relation to that condition.21 However, research suggests that there is a lack of patient knowledge about leg ulcer healing and prevention of reoccurrence.30 Our study supports previous work, suggesting that participants who understand the underlying pathophysiology of chronic venous insufficiency are more likely to be able to relate the benefits of exercise, such as improving blood flow, to improvement in their condition and poor venous return.16, 21 The current therapy for leg ulcer healing is compression bandaging; however, this can affect the range of ankle motion, which can affect walking. Previous researchers have suggested that an opportunity exists for health professionals to teach simple exercises to activate the calf muscle pump31 and maintain or improve their range of ankle motion by demonstrating simple ankle movement and heel‐raising exercises, perhaps while bandaging their ulcers.16
Participants perceived that exercise had improved their physical health, including having a positive impact on other comorbidities and overall well‐being. Research has shown that participants who adhere to the exercise programme as an adjunctive treatment to standard care are more likely to heal and have better functional outcomes than those who do not adhere to the exercises in conjunction with usual care.8 Previous research found that one of the main reasons participants with VLUs did not adhere to leg exercises included health deterioration because of their other chronic conditions.15 Participants appraised their overall well‐being within the context of living with leg ulceration and existing comorbidities; at times, the comorbidities were as debilitating, if not more so, than leg ulceration. The importance of well‐being and proactive preventative approaches (such as exercise) rather than a sole focus on treatment (in a hospital or clinic setting) is emphasised as important for people with VLUs.32
4.1. Strengths and limitations
The research provides in‐depth insight into the specific experiences of participants taking part in a supervised exercise intervention for adults with VLUs. Hence, the aim was achieved, and important influences on participation in exercise were identified. The findings can be used to extrapolate practical implications for promotion of physical activity and exercise for people with leg ulcers. The consistency of themes with previous literature supports the credibility of the findings and methodological rigour. However, the findings should be considered in light of methodological issues. First, the sample was not necessarily representative of the wider VLU population. The majority of patients interviewed where of White British ethnicity (similar to those who took part in the randomised controlled trial); therefore, caution should be applied when generalising these results to patients from other cultural backgrounds. Second, it is worth noting that this study used a mixture of face‐to‐face and telephone interviews. From the researchers' perspective, face‐to‐face interviews provided richer data compared with telephone interviews as the researcher was able to convey more empathy using body language. Telephone interviews were offered to participants who were unable to travel because of their leg ulcers or other commitments (such as multiple visits to the leg ulcer clinic or needing to wait for the day for a nurse to dress their ulcers). Interviews have been used by previous researchers to gather perspectives of adults with VLUs16 and can therefore be considered a valid approach. Third, participants included those with a range of treatments, including both compression hosiery and bandaging; however, different treatments may affect mobility and therefore affect the experience of exercise. Previous research has found that patients report a difference in mobility depending on compression vs bandaging as bandaging can restrict mobility more than compression hosiery.33 Therefore, future studies may wish to focus on larger and more representative samples and participant experiences of exercise, comparing those with compression hosiery with multiple‐layer bandaging.
4.2. Implications for practice
The current advice from many health professionals, to rest and be careful, can lead to participants living more sedentary lifestyles, which in turn can lead to poorer physical and psychological well‐being for participants with VLUs. Participants report that supervised exercise can lead to a perception of increased confidence to be physically active and physical benefits such as accelerated venous ulcer healing and a positive impact on other health conditions. Exercise therapy has the potential to holistically improve the well‐being of participants with VLUs by addressing both their leg ulceration and existing comorbidities.
5. CONCLUSION
The current study found that the opportunity to engage in a supervised, individualised exercise intervention specifically for the purpose of managing leg ulceration was welcomed by people with leg ulcers who had taken part in the exercise intervention. The opportunity to safely exercise and experience tangible benefits in physical and psychological health offered participants a new approach to future self‐management. This was seen as an extension to specialist care, fulfilling a gap in current provision. Overall, an individualised and supervised exercise programme was viewed by participants as an acceptable and feasible approach for people with VLUs as part of a self‐management strategy.
ACKNOWLEDGEMENTS
This study was funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit Programme (Grant Reference no. PB‐PG‐0213‐30029). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Kesterton S, Crank HJ, Tew GA, et al. Participant experiences in a feasibility trial of supervised exercise training in adults with venous leg ulcers: A qualitative study. Int Wound J. 2019;16:1559–1569. 10.1111/iwj.13252
Funding information Research for Patient Benefit Programme, Grant/Award Number: PB‐PG‐0213‐30029
REFERENCES
- 1. Tew GA, Gumber A, McIntosh E, et al. Effects of supervised exercise training on lower‐limb cutaneous microvascular reactivity in adults with venous ulcers. Eur J Appl Physiol. 2018;118(2):321‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2014;130(4):333‐346. [DOI] [PubMed] [Google Scholar]
- 3. O'Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012;11: CD0002651465‐1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kulkarni SR, Gohel MS, Whyman MR, Poskitt KR. Significance of limb trauma as an initiating factor in chronic leg ulceration. Phlebology. 2008;23(3):130‐136. [DOI] [PubMed] [Google Scholar]
- 5.A National Clinical Guideline. In Guideline No. 120. Edinburgh; 2010.
- 6. Klonizakis M, Tew GA, Gumber A, et al. Supervised exercise training as an adjunct therapy for venous leg ulcers: a randomized controlled feasibility trial. Br J Dermatol. 2018;178(5):1072‐1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Brien JA, Finlayson KJ, Kerr G, Edwards HE. Testing the effectiveness of a self‐efficacy based exercise intervention for adults with venous leg ulcers: protocol of a randomised controlled trial. BMC Dermatol. 2014;14(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. O'Brien J, Finlayson K, Kerr G, Edwards H. Evaluating the effectiveness of a self‐management exercise intervention on wound healing, functional ability and health‐related quality of life outcomes in adults with venous leg ulcers: a randomised controlled trial. Int Wound J. 2016;14(1):130‐137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Institute of Health and Care Excellence . Leg Ulcers – Venous; 2016. http://cks.nice.org.uk/leg-ulcer-venous. Accessed September 2019.
- 10. Scottish Intercollegiate Guidelines Network . Management of Chronic Venous Leg Ulcers: A National Clinical Guideline. Edinburgh, Scotland: Healthcare Improvement Scotland; 2010. [Google Scholar]
- 11. Australian Wound Management Association . Australian and New Zealand Clinical Practice Guideline for Prevention and Management of Venous Leg Ulcers; Cambridge, UK: Cambridge Publishing; 2011. [Google Scholar]
- 12. Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Br Med J. 2008;337(1655):979‐983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bandura A. Self‐Efficacy: The Exercise of Control. London, UK: Macmillan; 1997. [Google Scholar]
- 14. Heinen M, Borm G, Van Der Vleuten C, Evers A, Oostendorp R, Van Achterberg T. International Journal of Nursing Studies The Lively Legs self‐management programme increased physical activity and reduced wound days in leg ulcer patients: results from a randomized. Int J Nurs Stud. 2012;49(2):151‐161. 10.1016/j.ijnurstu.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 15. O'Brien J, Finlayson K, Kerr G, Shortridge‐Baggett LEH. Using a theoretical approach to identify factors influencing adherence to an exercise programme for adults with venous leg ulcers. J Health Psychol. 2018;5(23):691‐700. [DOI] [PubMed] [Google Scholar]
- 16. O'Brien J, Finlayson K, Kerr G, Edwards H. The perspectives of adults with venous leg ulcers on exercise: an exploratory study. J Wound Care. 2014;23(10):496‐509. [DOI] [PubMed] [Google Scholar]
- 17. Klonizakis M, Tew G, Michaels J, Saxton J. Exercise training improves cutaneous microvascular endothelial function in post‐surgical varicose vein patients. Microvasc Res. 2009;78(1):67‐70. [DOI] [PubMed] [Google Scholar]
- 18. Braun V, Clarke V. Using thematic analysis in psychology Virginia. Qual Res Psychol. 2006;3(2):77‐101. [Google Scholar]
- 19. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi‐disciplinary health research. BMC Med Res Methodol. 2013;13(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kori SH. Kinisophobia: a new view of chronic pain behavior. Pain Manag. 1990;1(1):35‐43. [Google Scholar]
- 21. Roaldsen KS, Biguet G, Elfving B. Physical activity in patients with venous leg ulcer – between engagement and avoidance. A patient perspective. Clin Rehabil. 2011;25(3):275‐286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roaldsen K, Elfving B, Stanghelle JK, Talme T, Mattsson E. Fear‐avoidance beliefs and pain as predictors for low physical activity in patients with leg ulcer. Physiother Res Int. 2009;14(3):167‐180. [DOI] [PubMed] [Google Scholar]
- 23. O'Brien J, Edwards H, Stewart I, Gibbs H. A home‐based progressive resistance exercise programme for patients with venous leg ulcers: a feasibility study. Int Wound J. 2013;10(4):389‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yim E, Kirsner RS, Gailey RS, Mandel DW, Chen SC, Tomic‐Canic M. Effect of physical therapy on wound healing and quality of life in patients with venous leg ulcers a systematic review. JAMA Dermatol. 2015;151(3):320‐327. [DOI] [PubMed] [Google Scholar]
- 25. Smith D, Lane R, McGinnes R, et al. What is the effect of exercise on wound healing in patients with venous leg ulcers? a systematic review. Int Wound J. 2018;15(3):441‐453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goldberg JF. Albert Bandura and the exercise of self‐efficacy. Int J Cogn Ther. 1999;9(49):601‐602. [Google Scholar]
- 27. Chao D, Foy CG, Farmer D. Exercise adherence among older adults: challenges and strategies. Control Clin Trials. 2000;5(21):S212‐S217. [DOI] [PubMed] [Google Scholar]
- 28. Jull A, Parag V, Walker N, Maddison R, Kerse N, Johns T. The PREPARE pilot RCT of home‐based progressive resistance exercises for venous leg ulcers. J Wound Care. 2009;18(12):497‐503. [DOI] [PubMed] [Google Scholar]
- 29. Walshe C. Living with a venous leg ulcer: a descriptive study of patients' experiences. J Adv Nurs. 1995;22(6):1092‐1100. [DOI] [PubMed] [Google Scholar]
- 30. Finlayson K, Edwards H, Courtney M. Factors associated with recurrence of venous leg ulcers: a survey and retrospective chart review. Int J Nurs Stud. 2009;8(46):1071‐1078. [DOI] [PubMed] [Google Scholar]
- 31. Padberg FT, Johnston MV, Sisto SA, Burnand KG, Wakefield TW, Perkowski P. Structured exercise improves calf muscle pump function in chronic venous insufficiency: a randomized trial. J Vasc Surg. 2004;1(39):79‐87. [DOI] [PubMed] [Google Scholar]
- 32. Upton D, Andrews A, Upton P. Venous leg ulcers: what about well‐being? J Wound Care. 2014;23(1):14‐17. [DOI] [PubMed] [Google Scholar]
- 33. Persoon A, Heinen MM, Van Der Vleuten CJM, De Rooij MJ, Van De Kerkhof PCM, Van Achterberg T. Leg ulcers: a review of their impact on daily life. J Clin Nurs. 2004;13(3):341‐354. [DOI] [PubMed] [Google Scholar]


