Abstract
Study Objectives
To characterize objectively assessed sleep–wake patterns in infants at approximately 1 month and 6 months and examine the differences among infants with different racial/ethnic backgrounds and household socioeconomic status (SES).
Methods
Full-term healthy singletons wore an ankle-placed actigraph at approximately 1 month and 6 months and parents completed sleep diaries. Associations of racial/ethnic and socioeconomic indices with sleep outcomes were examined using multivariable analyses. Covariates included sex, birth weight for gestational age z-score, age at assessment, maternal education, household income, bed-sharing, and breastfeeding.
Results
The sample included 306 infants, of whom 51% were female, 42.5% non-Hispanic white, 32.7% Hispanic, 17.3% Asian, and 7.5% black. Between 1 month and 6 months, night sleep duration increased by 65.7 minutes (95% CI: 55.4, 76.0), night awakenings decreased by 2.2 episodes (2.0, 2.4), and daytime sleep duration decreased by 73.3 minutes (66.4, 80.2). Compared to change in night sleep duration over this development period for white infants (82.3 minutes [66.5, 98.0]), night sleep increased less for Hispanic (48.9 minutes [30.8, 66.9]) and black infants (31.6 minutes [−5.9, 69.1]). Night sleep duration also increased less for infants with lower maternal education and household income. Asian infants had more frequent night awakenings. Adjustment for maternal education and household income attenuated all observed day and night sleep duration differences other than in Asians, where persistently reduced nighttime sleep at 6 months was observed.
Conclusions
Racial/ethnic differences in sleep emerge in early infancy. Night and 24-hour sleep durations increase less in Hispanic and black infants compared to white infants, with differences largely explained by SES.
Keywords: sleep, infant, actigraphy, disparity
Statement of Significance.
Previous evidence, composed mainly of studies with parent-reported sleep, has indicated that children with minority racial/ethnic backgrounds have short sleep duration, but the age at which such differences first emerge remains unknown. Sleep estimates based on objective 24-hour sleep–wake assessments in infants are limited. Using actigraphy, an objective assessment of sleep/wake patterns in the home environment, we found that differences in sleep–wake patterns emerged between 1 month and 6 months across racial/ethnic groups and infants from different socioeconomic status (SES) households. Hispanic/Latino, Asian, and black infants or infants from lower SES families had less consolidated and shorter 24-hour sleep.
Introduction
Rapid development of sleep–wake patterns is one of the major physiological changes over the first months of life. During this period, infants’ sleep problems are a common concern to both parents and pediatric professionals. Parent reports indicate that approximately 20% to 30% of infants experience sleep problems such as difficulties in sleep initiation and excessive nighttime awakenings [1, 2]. Sleep problems often persist into childhood [1, 3, 4], and short or fragmented sleep is associated with long-term medical, psychological, and social consequences, such as obesity [5, 6], elevated blood pressure [7, 8], poor language acquisition [9], anxiety [10], suboptimal cognitive development [11], and poor academic performance [12]. Understanding sleep–wake patterns at early ages may shed light on the origins of chronic health conditions and provide an evidence base for refining pediatric sleep recommendations and for developing early-life sleep interventions. However, few studies have reported longitudinal changes of objectively estimated sleep patterns during early infancy.
Driven by the maturation of the circadian system and sleep–wake homeostasis [13, 14] as well as environmental and parenting factors, such as exposures to light, sound, and timing of feeding, sleep undergoes profound changes during the first six months of life. Previous studies of change in infant sleep mainly using parent-reported questionnaires, reported increased regularity and consolidation (i.e. longer night sleep intervals [15–19], fewer wake bouts during night sleep [15, 16, 18, 20–22], fewer daytime naps [23], and less overall sleep time [15, 24–26]). Prior parent-reported survey data in children and adolescents indicated that Hispanic [27, 28], Asian [18, 28], and black [27–29] children have shorter sleep duration compared to non-Hispanic white children, and that differences may be partially explained by socioeconomic and environmental factors [27, 28]. Cross-country/cultural studies also reported the poor sleep quantity and quality in Hispanic, Asian, and black children [18, 30]. However, the timing of when differences first emerge is unknown [28, 29, 31], and the evidence from objectively assessed sleep–wake patterns is limited.
With the current study, we fill these gaps by characterizing 24-hour sleep–wake patterns in the earliest and fastest sleep development period (i.e. between approximately 1 month and 6 months of age), using actigraphy, an objective sleep assessment tool able to be used at home [32]. We evaluated the associations of race/ethnicity and socioeconomic status (SES) with sleep–wake patterns and quantified the extent to which controlling for SES indicators (maternal education and household income), as well as breastfeeding and co-sleeping attenuates racial/ethnic differences in sleep–wake patterns.
Methods
Subjects
As a part of the ongoing Rise & SHINE (Sleep Health in Infancy & Early Childhood) study, a birth cohort examining associations between sleep–wake patterns and growth in early life, infants were recruited from the newborn unit of Massachusetts General Hospital in Boston, MA. Full-term singletons with no genetic or congenital abnormalities and their biological mothers without diagnosed chronic medical or mental conditions participated in this study. Other eligibility criteria included mother’s fluency in English or Spanish, mother’s age of at least 18 years old, and the family living within 40 miles without plans to move from the area within study period. The study was approved by Partners HealthCare Office of Research. Signed informed consent was obtained from all the participating families during enrollment.
Demographic information
Parents completed questionnaires regarding race/ethnicity, maternal education, household annual income, marital status, exclusive/mixed/none breastfeeding, childcare (hours staying at childcare per week), and parenting practices such as bed-sharing (days per week sharing bed with parent at night). Other demographic and perinatal information, including mother’s age, gestational age, child’s sex, birth weight, was obtained from electronic health record database. Birth weight for gestational age z-score was calculated using the US national reference [33].
Assessment of sleep measures
During home visits, a research coordinator instructed mothers how to use an actigraph and complete a paper-based, 24-hour, 7-day sleep diary. In a sleep diary, parents recorded sleep periods, wake, sleep in motion (e.g. asleep in the stroller), and actigraph “off” periods, providing annotations using a time line shown as 5-minute intervals for the period overlapping the actigraphy monitoring. Parents also completed the Brief Infant Sleep Questionnaire (BISQ) [20, 34].
A Philips Actiwatch 2 (Philips Healthcare, Andover, MD) was placed on infants’ left ankle for 7 continuous days after the home visit. Data were recorded in 30-second epochs at a sampling rate of 32 Hz [35, 36], and analyzed at the low activity threshold settings of 80 counts for wake detection. An earlier model of the Actiwatch AW64 demonstrated an agreement rate of 87%–94% with polysomnography (PSG) and 85%–89% with direct observation using the 80 counts per epoch threshold in infants [37, 38]. In the validation study between actigraphy and PSG in infants younger than 6 months, the data using low threshold yielded better sensitivity (89%–96%) and appreciable specificity (39%–76%) compared to high (20 counts), median (40 counts), and auto threshold (mean activity in full active period × 0.888) [37]. Matched data of AW64 and Actiwatch 2 in healthy adults demonstrated no differences in performance of the two models [39]. A trained research assistant, blinded to other clinical data, annotated the actigraphy data using caregiver-completed sleep diary and processed the records using the commercially available algorithms for Actiwatch 2, Respironics Actiware 6 (Version 6.0.9, Philips/Respironics) scoring algorithm. Sleep onset was denoted as the clock time when activity counts dropped for 5 consecutive minutes in association with bedtime reported by sleep diary. Sleep offset was the clock time when activity counts increased after the main sleep period and coincided with prior reported wake time [40]. Average values were calculated across measurement days. Data lost due to technical failure, parent nonadherence, or artifacts were 11 out of 375 (3%) at 1 month, and 8 out of 323 (2%) at 6 months. Three hundred six infants who completed sleep assessment at both time points, at least 3 nights for each, were finally analyzed. In the analytical sample, the average nights for actigraphy data collection were 7.5 (SD: 1.2) at 1 month, and 7.3 (1.2) at 6 months.
Primary exposures
This study focused on three primary exposures: race/ethnicity of the infant, collected and defined according to Race and Ethnic Standards for Federal Statistics and Administrative Reporting [41]; maternal education, collected as: <Bachelor’s degree, Bachelor’s degree, and graduate degree; and annual household income, collected as: <$80k, $80–199k, and ≥$200k.
Primary outcomes
Sleep intervals were determined by the combination of information from the diary and the activity patterns on the actigraph [42]. The night and day sleep intervals were defined as between 07:00 pm and 07:59 am and 08:00 am and 06:59 pm, respectively, reflecting the cutoffs in the sleep questionnaire we used for nighttime and daytime sleep periods [20]. Based on these, six sleep-related outcomes were considered: (1) night sleep duration (minutes); (2) longest continuous night sleep (minutes), taken to be the sum of sleep epochs within the longest sleep interval between sleep onset and offset; (3) wake after sleep onset (WASO, minutes), taken to be the total amount of minutes of all wake epochs over the night sleep period; (4) night wake bouts, the number of episodes of wakefulness showing a sharp increase of activity for longer than 5 minutes between intervals of nighttime sleep; (5) daytime sleep duration (minutes); and (6) total (24-hour) sleep duration (minutes). Each of these outcomes was assessed at 1 month and 6 months. In addition, for each, we calculated the change between 1 month and 6 months.
Statistical analyses
Infant and maternal demographic information and actigraphy measurements were summarized using means/SDs and counts/percentages (as appropriate), overall and by race/ethnicity. Then, we fit a series of multiple linear models to the six sleep outcomes for each of the three primary exposures. Due to potential differences across groups in sex, birth weight for gestational age z-score, and age at assessment, these variables were included in each model to eliminate any potential confounding influence associated with sex or age. From these, we calculated differences in the predicted marginal means across the levels of each of the three primary exposures.
In addition, multiple linear regression was used to examine the impact of adjusting for socioeconomic and behavioral factors on the association between race/ethnicity and sleep duration (night, daytime, and total). Toward this, three models were fit: Model 1 included race/ethnicity, sex, birth weight for gestational age z-score, and age at assessment; Model 2 additionally adjusted for maternal education and household income (measures of household SES); Model 3 additionally adjusted for bed-sharing and breastfeeding (parental practices).
Following data collection, 127 parents who consented did not provide valid actigraphy data for both time points due to several reasons, such as parenting challenge, travel, frequent drop of the actigraph, and medical conditions. As sensitivity analyses, we performed each analysis using inverse probability weighting (IPW) based on a logistic regression model for whether valid actigraphy data were provided as a function of race and maternal education [43].
All statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC), with the LSMEANS statement used to calculated predicted marginal means. Throughout, we used a p-value of <0.05 together with evidence of consistency of findings across models to identify associations of interest.
Results
Of 1459 eligible mother–infant dyads, 433 consented to participate, and 306 infants completed actigraphy at both 1 month and 6 months, which included at least 3 nights of sleep monitoring at both time points. Among the 306 infants, 42% were non-Hispanic white, 33% were Hispanic, 17% were Asian, and 8% were black. Compared to the 306 participants in the analyses, fewer nonparticipants (N = 1026) had college-educated mothers (56% vs. 85%). The analytic sample included a higher percentage of Hispanic (33% vs. 17%) and Asian infants (17% vs. 12%), and lower percentage of white (42% vs. 55%) and black infants (8% vs. 14%) compared to nonparticipants. Participants who consented but failed to provide valid sleep data for both time points (N = 127) also had higher education level than nonparticipants (68% vs. 56% for college education) and included higher percentage of Hispanic (45% vs. 17%) and lower percentage of white infants (30% vs. 55%). Variation in infant and mother characteristics by race/ethnicity is shown in Table 1. Average gestational age was 39.5 weeks (SD: 1.0) and infant birth weight was 3.4 kg (0.4). Average infant age at the two home exams were 36.2 days (7.6) and 194.6 days (16.8), respectively.
Table 1.
Characteristics of subjects by infant race/ethnicity
| Characteristics | Overall (N = 306) | Non-Hispanic white (N = 130) | Hispanic or Latino (N = 100) | Asian (N = 53) | Black (N = 23) |
|---|---|---|---|---|---|
| Infant characteristics | Mean (SD) | ||||
| Gestational age (weeks) | 39.5 (1.0) | 39.7 (1.0) | 39.5 (1.0) | 39.4 (1.1) | 39.1 (1.0) |
| Birth weight (kg) | 3.4 (0.4) | 3.4 (0.4) | 3.4 (0.4) | 3.2 (0.4) | 3.3 (0.5) |
| Birth weight for gestational age z-score | −0.2 (0.9) | −0.2 (0.9) | −0.1 (0.8) | −0.6 (0.7) | −0.4 (1.1) |
| Age at 1-month visit (days) | 36.2 (7.6) | 36.8 (9.2) | 36.0 (6.9) | 35.5 (4.4) | 34.6 (6.2) |
| Age at 6-month visit (days) | 194.6 (16.8) | 196 (17.5) | 192.2 (16.9) | 192.6 (15.9) | 194.3 (16.5) |
| Bed-sharing at 1 month (days per week) | 1.9 (2.8) | 0.9 (2.1) | 2.9 (3.1) | 2.1 (3.0) | 3.2 (3.2) |
| Bed-sharing at 6 months (days per week) | 2.2 (3.0) | 1.2 (2.4) | 3.2 (3.2) | 2.6 (3.3) | 3.3 (3.1) |
| Childcare (hours per week at 6 months) | 11.1 (17.1) | 15.4 (18.9) | 7.7 (14.4) | 10.0 (17.1) | 4.3 (10.5) |
| n (%) | Percentage | ||||
| Infant sex, female | 156 (51.0) | 46.9 | 59.0 | 52.8 | 34.8 |
| Breast feeding at 1 month | |||||
| Exclusive | 141 (46.1) | 64.6 | 25.0 | 45.3 | 34.8 |
| Mixed | 143 (46.7) | 30.8 | 64.0 | 49.1 | 56.5 |
| None | 22 (7.2) | 4.6 | 11.0 | 5.7 | 8.7 |
| Breast feeding at 6 months | |||||
| Exclusive | 119 (38.9) | 46.2 | 27.0 | 49.1 | 26.1 |
| Mixed | 94 (30.7) | 31.5 | 28.0 | 30.2 | 39.1 |
| None | 93 (30.4) | 22.3 | 45.0 | 20.8 | 34.8 |
| Mother characteristics | Mean (SD) | ||||
| Age | 32.8 (4.9) | 34.0 (3.6) | 30.6 (5.6) | 33.9 (4.2) | 32.7 (5.9) |
| n (%) | Percentage | ||||
| U.S. born | 144 (47.1) | 77.7 | 24.0 | 22.6 | 30.4 |
| Marital status | |||||
| Married | 253 (82.7) | 94.6 | 62.0 | 92.5 | 82.6 |
| Not married, living together | 34 (11.1) | 4.6 | 24.0 | 5.7 | 4.4 |
| Not married, living separate | 18 (5.9) | 0.8 | 14.0 | 1.9 | 8.7 |
| Refused | 1 (0.3) | 0 | 0 | 0 | 4.3 |
| Education | |||||
| < Bachelor’s degree | 80 (26.1) | 7.7 | 60.0 | 0 | 43.5 |
| Bachelor’s degree | 77 (25.2) | 27.7 | 23.0 | 20.8 | 30.4 |
| Graduate degree | 149 (48.7) | 64.6 | 17.0 | 79.2 | 26.1 |
| Annual household income | |||||
| <$80k | 110 (36.0) | 11.5 | 69.0 | 18.9 | 69.6 |
| $80–199k | 104 (34.0) | 42.3 | 22.0 | 43.4 | 17.4 |
| >$200k | 84 (27.5) | 43.9 | 7.0 | 35.8 | 4.3 |
| Refused | 8 (2.6) | 2.3 | 2.0 | 1.9 | 8.7 |
At 1 month, night sleep duration and longest continuous night sleep duration averaged 461.2 (95% CI: 453.0, 469.4) and 282.8 minutes (271.2, 294.4), respectively. Over the follow-up period, average night sleep duration and average longest night sleep duration increased by 65.7 (55.4, 76.0) and 177.6 minutes (162.8, 192.4), respectively (both p < 0.001). Night wake bouts decreased by 2.2 episodes (2.0, 2.4) per night (p < 0.001). Daytime sleep duration decreased by 73.3 minutes (66.4, 80.2) (p < 0.001).
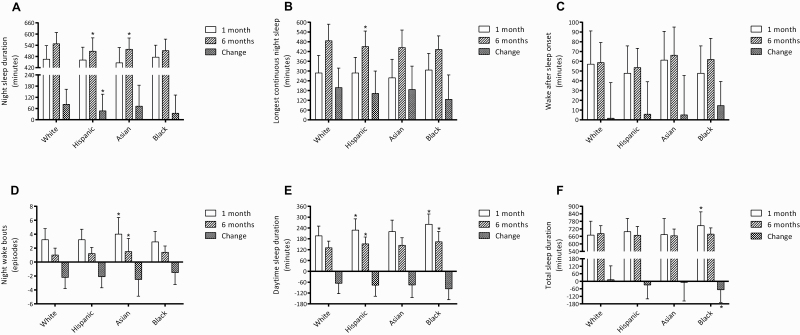
Unadjusted values for sleep indices by race/ethnicity are shown in Figure 1, with Table 2 further showing values adjusted for sex, birth weight for gestational age z-score, and age at assessment. At approximately 1 month, both unadjusted and adjusted analyses showed that night sleep duration and longest continuous night sleep duration did not significantly differ by race/ethnicity. In contrast, Asian infants had more frequent awakenings compared to black and white infants and longer WASO compared to Hispanic/Latino infants. Daytime and 24-hour sleep durations were longer in Hispanic/Latino and black infants compared to white and Asian infants. For example, 24-hour sleep duration was approximately 75.1 minutes more in black than white infants (746.8 [700.5, 793.1] vs. 671.7 [652.3, 691.1]).
Figure 1.
Sleep–wake patterns by race/ethnicity. (A) Night sleep duration. (B) Longest continuous night sleep. (C) Wake after sleep onset. (D) Night wake bouts. (E) Daytime sleep duration. (F) Total sleep duration. *p < 0.05 compared to white infants.
Table 2.
Infant sleep–wake patterns overall and by race/ethnicity, adjusted for sex, birth weight for gestational age, and age at assessment
| Sleep–wake patterns | Overall (N = 306) | White (N = 130) | Hispanic or Latino (N = 100) | Asian (N = 53) | Black (N = 23) | F (df) | P |
|---|---|---|---|---|---|---|---|
| 1 month | |||||||
| Night sleep duration (minutes) | 461.2 (453.0, 469.4) | 465.8 (453.2, 478.4) | 459.0 (444.6, 473.5) | 445.7 (425.8, 465.7) | 478.2 (448.1, 508.3) | 1.38 (3, 299) | 0.25 |
| Longest continuous night sleep (minutes) | 282.8 (271.2, 294.4) | 286.4 (268.7, 304.1) | 283.7 (263.4, 304.0) | 259.7 (231.7, 287.7) | 309.6 (267.4, 351.8) | 1.46 (3, 299) | 0.23 |
| WASO (minutes) | 54.0 (50.5, 57.5) | 56.5 (51.2, 61.7) | 47.5 (41.5, 53.5) | 62.4 (54.1, 70.7) | 48.4 (35.9, 60.9) | 3.38 (3, 299) | 0.02 |
| Night wake bouts (episodes) | 3.3 (3.1, 3.5) | 3.2 (2.9, 3.5) | 3.3 (2.9, 3.6) | 3.9 (3.5, 4.4) | 2.8 (2.1, 3.5) | 3.73 (3, 299) | 0.02 |
| Daytime sleep duration (minutes) | 215.6 (208.7, 222.5) | 197.6 (187.4, 207.7) | 227.7 (216.1, 239.3) | 217.3 (201.3, 233.3) | 259.6 (235.4, 283.7) | 9.81 (3, 299) | <0.001 |
| Total sleep duration (minutes) | 685.2 (672.4, 698.0) | 671.7 (652.3, 691.1) | 695.5 (673.3, 717.8) | 671.0 (640.3, 701.7) | 746.8 (700.5, 793.1) | 3.49 (3, 299) | 0.02 |
| 6 months | |||||||
| Night sleep duration (minutes) | 526.9 (519.4, 534.4) | 547.8 (536.6, 558.9) | 508.0 (495.2, 520.7) | 518.8 (501.2, 536.5) | 510.3 (483.7, 536.8) | 8.15 (3, 299) | <0.001 |
| Longest continuous night sleep (minutes) | 460.4 (449.2, 471.6) | 482.8 (465.6, 499.9) | 446.1 (426.5, 465.7) | 444.2 (417.1, 471.3) | 432.9 (392.1, 473.6) | 3.94 (3, 299) | 0.009 |
| WASO (minutes) | 58.5 (56.0, 61.0) | 58.9 (55.1, 62.7) | 53.5 (49.1, 57.8) | 66.0 (60.0, 72.0) | 61.3 (52.3, 70.4) | 3.81 (3, 299) | 0.01 |
| Night wake bouts (episodes) | 1.1 (1.0, 1.2) | 0.9 (0.7, 1.1) | 1.1 (0.9, 1.4) | 1.5 (1.2, 1.8) | 1.3 (0.8, 1.7) | 3.67 (3, 299) | 0.03 |
| Daytime sleep duration (minutes) | 142.3 (137.7, 146.9) | 130.8 (123.8, 137.7) | 151.2 (143.3, 159.2) | 143.3 (132.3, 154.3) | 165.2 (148.7, 181.8) | 7.72 (3, 299) | <0.001 |
| Total sleep duration (minutes) | 674.4 (667.3, 681.5) | 682.2 (671.2, 693.2) | 667.9 (655.2, 680.5) | 665.1 (647.7, 682.5) | 678.9 (652.7, 705.0) | 1.39 (3, 299) | 0.24 |
| Change between 1 month and 6 months* | |||||||
| Night sleep duration (minutes) | 65.7 (55.4, 76.0) | 82.3 (66.5, 98.0) | 48.9 (30.8, 66.9) | 72.7 (47.8, 97.6) | 31.6 (−5.9, 69.1) | 3.75 (3, 298) | 0.01 |
| Longest continuous night sleep (minutes) | 177.6 (162.8, 192.4) | 196.8 (174.0, 219.6) | 162.3 (136.2, 188.4) | 183.8 (147.8, 219.9) | 122.5 (68.2, 176.8) | 2.75 (3, 298) | 0.04 |
| WASO (minutes) | 4.6 (0.6, 8.6) | 2.3 (−3.9, 8.4) | 6.0 (−1.0, 13.0) | 3.7 (−6.0, 13.3) | 13.3 (−1.3, 27.8) | 0.71 (3, 298) | 0.55 |
| Night wake bouts (episodes) | −2.2 (−2.4, −2.0) | −2.2 (−2.5, −1.9) | −2.1 (−2.5, −1.8) | −2.4 (−2.9, −1.9) | −1.5 (−2.2, −0.7) | 1.48 (3, 298) | 0.19 |
| Daytime sleep duration (minutes) | −73.3 (−80.2, −66.4) | −67.2 (−77.7, −56.6) | −76.3 (−88.4, −64.2) | −73.8 (−90.5, −57.1) | −93.6 (−118.8, −68.4) | 1.36 (3, 298) | 0.26 |
| Total sleep duration (minutes) | −11.0 (−24.4, 2.4) | 10.7 (−9.6, 31.0) | −28.2 (−51.7, −4.8) | −6.4 (−38.5, 25.8) | −67.8 (−116.3, −19.4) | 3.99 (3, 298) | 0.008 |
df = degrees of freedom. Overall sleep–wake patterns are described with raw mean and 95% confidence interval (95% CI); sleep–wake patterns in different race/ethnicity groups are described using mean and 95% CI adjusted for sex, birth weight for gestational age z-score, and age at assessment.
*Positive value means increased sleep duration from 1 month to 6 months; negative means decreased.
At approximately 6 months (Figure 1; Table 2), night sleep duration was shorter by an average of 39.8, 29.0, and 37.5 minutes in Hispanic/Latino, Asian, and black infants compared to white infants, respectively, after adjustment for sex, birth weight for gestational age z-score, and age at assessment. Longest continuous night sleep duration was also shorter in Hispanic/Latino, Asian, and black infants compared to white infants. Conversely, in adjusted analyses, daytime sleep duration was higher by 20.4, 12.5, and 34.4 minutes in Hispanic/Latino, Asian, and black infants, compared to white infants, respectively. Night wake bouts and duration were higher in Asian infants compared to white infants.
Between 1 month and 6 months, night sleep duration increased by 82.3 minutes (66.5, 98.0) in white infants, which was significantly higher than in Hispanic and black infants (48.9 minutes [30.8, 66.9] and 31.6 minutes [−5.9, 69.1], F [df] = 3.75 [3, 298], p = 0.01). Change in daytime sleep duration did not significantly differ across racial/ethnic groups. However, 24-hour sleep duration increased in white infants but decreased in the other groups and was lower in black compared to white infants.
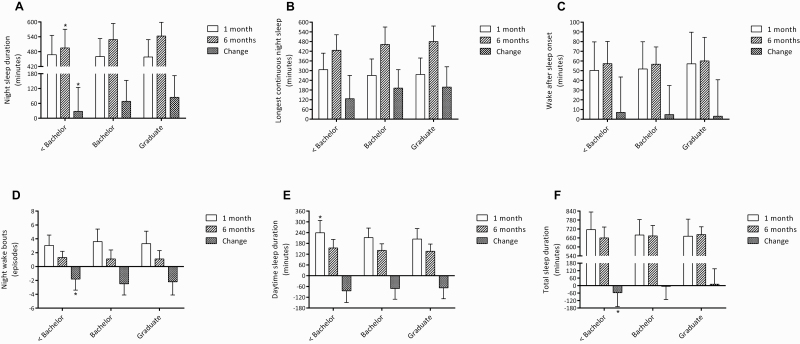
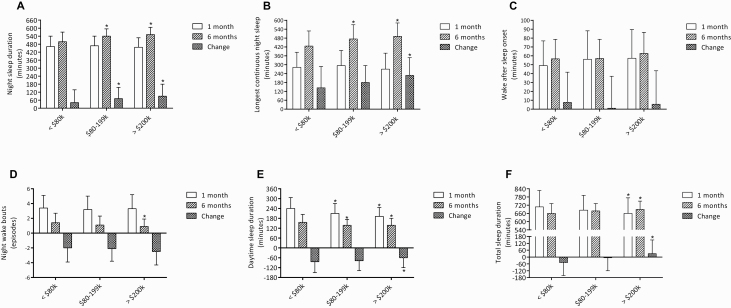
Sleep–wake patterns also varied by SES indicators. Sleep–wake patterns by maternal education are shown in Figure 2 and Table 3, and by annual household income in Figure 3 and Table 4. At approximately 1 month, night sleep duration and longest continuous night sleep duration did not differ among infants with different levels of maternal education or household income. However, daytime sleep duration and 24-hour sleep duration were higher in infants of mothers with lower education or annual household income. WASO and wake bouts did not differ by SES.
Figure 2.
Sleep–wake patterns by maternal education. (A) Night sleep duration. (B) Longest continuous night sleep. (C) Wake after sleep onset. (D) Night wake bouts. (E) Daytime sleep duration. (F) Total sleep duration. *p < 0.05 compared to bachelor’s degree.
Table 3.
Infant sleep–wake patterns by maternal education, adjusted for sex, birth weight for gestational age, and age at assessment
| Sleep–wake patterns | < Bachelor’s degree (N = 80) | Bachelor’s degree (N = 77) | Graduate degree (N = 149) | F (df) | P |
|---|---|---|---|---|---|
| 1 month | |||||
| Night sleep duration (minutes) | 467.7 (451.6, 483.9) | 460.4 (443.9, 476.8) | 457.8 (446.0, 469.7) | 0.48 (2, 300) | 0.62 |
| Longest continuous night sleep (minutes) | 303.4 (280.9, 325.9) | 268.7 (245.8, 291.6) | 278.7 (262.3, 295.2) | 2.47 (2, 300) | 0.09 |
| WASO (minutes) | 49.6 (42.9, 56.4) | 51.9 (45, 58.7) | 57.4 (52.5, 62.3) | 1.93 (2, 300) | 0.15 |
| Night wake bouts (episodes) | 3.0 (2.6, 3.3) | 3.6 (3.2, 4.0) | 3.3 (3.0, 3.5) | 2.53 (2, 300) | 0.08 |
| Daytime sleep duration (minutes) | 240.7 (227.7, 253.8) | 212.8 (199.5, 226.1) | 203.3 (193.7, 212.9) | 10.45 (2, 300) | <0.001 |
| Total sleep duration (minutes) | 717.2 (692.4, 741.9) | 680.5 (655.3, 705.7) | 670.1 (652.0, 688.2) | 4.63 (2, 300) | 0.01 |
| 6 months | |||||
| Night sleep duration (minutes) | 495.1 (481.0, 509.1) | 527.9 (513.6, 542.2) | 543.6 (533.3, 553.9) | 15.07 (2, 300) | <0.001 |
| Longest continuous night sleep (minutes) | 427.6 (406.0, 449.3) | 460.4 (438.3, 482.4) | 477.9 (462.1, 493.8) | 6.80 (2, 300) | 0.001 |
| WASO (minutes) | 57.2 (52.3, 62.1) | 56.3 (51.3, 61.3) | 60.4 (56.8, 64.0) | 1.04 (2, 300) | 0.35 |
| Night wake bouts (episodes) | 1.3 (1.0, 1.5) | 1.1 (0.9, 1.4) | 1.1 (0.9, 1.3) | 0.54 (2, 300) | 0.52 |
| Daytime sleep duration (minutes) | 154.6 (145.6, 163.6) | 141.4 (132.2, 150.5) | 135.9 (129.4, 142.5) | 5.46 (2, 300) | 0.005 |
| Total sleep duration (minutes) | 659.8 (645.8, 673.8) | 673.6 (659.4, 687.7) | 682.4 (672.2, 692.6) | 3.33 (2, 300) | 0.04 |
| Change between 1 month and 6 months* | |||||
| Night sleep duration (minutes) | 26.8 (7.2, 46.5) | 67.3 (47.3, 87.3) | 86.2 (71.8, 100.6) | 11.46 (2, 299) | <0.001 |
| Longest continuous night sleep (minutes) | 123.5 (95.1, 152.0) | 191.3 (162.3, 220.2) | 199.8 (178.9, 220.7) | 9.58 (2, 299) | <0.001 |
| WASO (minutes) | 7.3 (−0.5, 15.1) | 4.6 (−3.4, 12.5) | 3.1 (−2.7, 8.8) | 0.37 (2, 299) | 0.69 |
| Night wake bouts (episodes) | −1.8 (−2.2, −1.4) | −2.4 (−2.8, −2.0) | −2.2 (−2.5, −1.9) | 3.15 (2, 299) | 0.04 |
| Daytime sleep duration (minutes) | −86.4 (−99.8, −73.0) | −71.3 (−84.9, −57.6) | −67.3 (−77.1, −57.4) | 2.62 (2, 299) | 0.07 |
| Total sleep duration (minutes) | −59.5 (−85.2, −33.8) | −7.1 (−33.1, 18.8) | 13.1 (−5.6, 31.8) | 10.09 (2, 299) | <0.001 |
df = degrees of freedom. Sleep patterns in different education groups are described using mean and 95% confidence interval adjusted for sex, birth weight for gestational age z-score, and age at assessment.
*Positive value means increased sleep duration from 1 month to 6 months; negative means decreased.
Figure 3.
Sleep–wake patterns by household income. (A) Night sleep duration. (B) Longest continuous night sleep. (C) Wake after sleep onset. (D) Night wake bouts. (E) Daytime sleep duration. (F) Total sleep duration. *p < 0.05 compared to annual household income <$80k.
Table 4.
Infant sleep–wake patterns by annual household income, adjusted for sex, birth weight for gestational age, and age at assessment
| Sleep–wake patterns | <$80k (N = 110) | $80–199k (N = 104) | >$200k (N = 84) | F (df) | P |
|---|---|---|---|---|---|
| 1 month | |||||
| Night sleep duration (minutes) | 460.0 (446.2, 473.9) | 465.0 (450.8, 479.3) | 457.4 (441.6, 473.2) | 0.26 (2, 300) | 0.77 |
| Longest continuous night sleep (minutes) | 283.4 (264.1, 302.7) | 291.6 (271.7, 311.5) | 267.5 (245.5, 289.5) | 1.30 (2, 300) | 0.27 |
| WASO (minutes) | 48.6 (42.9, 54.4) | 56.4 (50.5, 62.3) | 57.4 (50.9, 64.0) | 2.53 (2, 300) | 0.08 |
| Night wake bouts (episodes) | 3.4 (3.1, 3.7) | 3.2 (2.9, 3.6) | 3.3 (2.9, 3.7) | 0.15 (2, 300) | 0.83 |
| Daytime sleep duration (minutes) | 239.8 (228.8, 250.7) | 209.9 (198.7, 221.2) | 193.0 (180.6, 205.5) | 16.28 (2, 300) | <0.001 |
| Total sleep duration (minutes) | 708.4 (687.2, 729.6) | 684.5 (662.7, 706.3) | 657.5 (633.3, 681.7) | 4.86 (2, 300) | 0.008 |
| 6 months | |||||
| Night sleep duration (minutes) | 499.9 (488.1, 511.7) | 539.4 (527.2, 551.6) | 548.4 (534.8, 561.9) | 17.05 (2, 300) | <0.001 |
| Longest continuous night sleep (minutes) | 424.8 (406.8, 442.8) | 472.2 (453.6, 490.8) | 491.9 (471.3, 512.5) | 12.87 (2, 300) | <0.001 |
| WASO (minutes) | 56.4 (52.2, 60.5) | 57.5 (53.2, 61.8) | 62.5 (57.7, 67.2) | 1.98 (2, 300) | 0.14 |
| Night wake bouts (episodes) | 1.4 (1.2, 1.6) | 1.1 (0.9, 1.4) | 0.9 (0.6, 1.1) | 4.60 (2, 300) | 0.01 |
| Daytime sleep duration (minutes) | 154.4 (146.8, 162.0) | 134.8 (126.9, 142.7) | 135.5 (126.8, 144.3) | 7.79 (2, 300) | <0.001 |
| Total sleep duration (minutes) | 662.3 (650.4, 674.2) | 678.0 (665.8, 690.2) | 687.3 (673.8, 700.8) | 3.94 (2, 300) | 0.02 |
| Change between 1 month and 6 months* | |||||
| Night sleep duration (minutes) | 39.5 (22.8, 56.3) | 74.9 (57.6, 92.1) | 90.8 (71.7, 109.9) | 8.60 (2, 299) | <0.001 |
| Longest continuous night sleep (minutes) | 141.0 (116.8, 165.1) | 181.5 (156.5, 206.4) | 223.9 (196.4, 251.5) | 9.96 (2, 299) | <0.001 |
| WASO (minutes) | 7.7 (1.0, 14.3) | 1.2 (−5.7, 8.1) | 5.1 (−2.5, 12.7) | 0.88 (2, 299) | 0.42 |
| Night wake bouts (episodes) | −2.0 (−2.3, −1.6) | −2.1 (−2.5, −1.8) | −2.5 (−2.8, −2.1) | 1.90 (2, 299) | 0.15 |
| Daytime sleep duration (minutes) | −85.5 (−96.9, −74.1) | −75.1 (−86.9, −63.4) | −57.3 (−70.3, −44.3) | 5.21 (2, 299) | 0.006 |
| Total sleep duration (minutes) | −47.4 (−69.3, −25.6) | −5.6 (−28.0, 16.9) | 29.8 (5.0, 54.6) | 10.74 (2, 299) | <0.001 |
df = degrees of freedom. Sleep patterns in different household income groups are described using mean and 95% confidence interval adjusted for sex, birth weight for gestational age z-score, and age at assessment.
*Positive value means increased sleep duration from 1 month to 6 months; negative means decreased.
At approximately 6 months, night sleep duration, longest continuous night sleep duration, and 24-hour sleep duration were lower but daytime duration was higher in infants of mothers with less education and families with lower household income. WASO did not significantly differ across SES, but wake bouts were higher in infants of families with lower household income.
Over the first 6 months of life, night sleep duration and longest continuous sleep duration increased less in infants from families with less educated mothers and lower household income. Daytime sleep duration decreased more in infants of lower income families. Hence, 24-hour sleep duration decreased in infants with lower SES, whereas it increased in infants with higher SES. Night wake bouts also decreased less in infants with less educated mothers.
Multivariable analyses are shown in Table 5 that considered both race/ethnicity and SES. Across various statistical models, no racial/ethnic differences were observed for 1-month nighttime sleep duration. For 6-month nighttime sleep duration, adjustment for SES (maternal education and annual household income) markedly attenuated the previously observed differences in nighttime sleep duration for Hispanic and black infants as compared to white infants, which were minimal and no longer significant in adjusted analyses. In contrast, Asian infants were estimated to have an approximately 29-minute lower nighttime sleep duration than white infants in models with and without SES adjustment. Racial/ethnic differences in night sleep duration change from 1 month to 6 months for Hispanic and black infants were also markedly attenuated after adjustment for SES. Models that included breastfeeding (exclusive/mixed/none) and bed-sharing (days per week) did not appreciably change estimates from models that only adjusted for SES.
Table 5.
Multivariable associations of race/ethnicity and sleep duration, adjusted for SES or parenting behaviors
| Night sleep duration (minutes) | Daytime sleep duration (minutes) | Total sleep duration (minutes) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| 1 month | p = 0.25* | p = 0.18 | p = 0.13 | p < 0.001 | p = 0.01 | p = 0.03 | p = 0.02 | p = 0.18 | p = 0.20 |
| White | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Hispanic | −6.74 (−25.97, 12.48) | −10.72 (−35.43, 13.99) | −13.31 (−38.85, 12.23) | 30.11 (14.68, 45.53) | 6.53 (−12.83, 25.88) | 3.41 (−16.70, 23.53) | 23.84 (−5.71, 53.38) | −3.73 (−41.55, 34.09) | −9.65 (−48.81, 29.52) |
| Asian | −20.04 (−43.78, 3.70) | −20.02 (−44.33, 4.28) | −23.63 (−48.35, 1.10) | 19.72 (0.68, 38.77) | 20.37 (1.33, 39.42) | 18.01 (−1.46, 37.49) | −0.66 (−37.15, 35.82) | 0.10 (−37.11, 37.30) | −6.09 (−44.01, 31.82) |
| Black | 12.40 (−20.27, 45.06) | 15.54 (−21.44, 52.53) | 11.70 (−25.63, 49.03) | 62.01 (35.80, 88.21) | 40.98 (12.00, 69.96) | 38.13 (8.73, 67.53) | 75.11 (24.91, 125.31) | 55.65 (−0.97, 112.27) | 48.7 (−8.54, 105.95) |
| 6 months | p < 0.001 | p = 0.06 | p = 0.13 | p < 0.001 | p = 0.04 | p = 0.04 | p = 0.25 | p = 0.22 | p = 0.22 |
| White | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Hispanic | −39.83 (−56.80, −22.86) | −9.22 (−30.03, 11.59) | −3.82 (−24.61, 16.97) | 20.48 (9.92, 31.05) | 12.39 (−1.07, 25.85) | 12.26 (−1.40, 25.91) | −14.30 (−31.08, 2.47) | 4.79 (−16.27, 25.85) | 10.11 (−10.92, 31.14) |
| Asian | −28.94 (−49.94, −7.94) | −29.04 (−49.70, −8.39) | −24.47 (−45.16, −3.77) | 12.52 (−0.55, 25.59) | 12.07 (−1.29, 25.43) | 12.71 (−0.88, 26.31) | −17.12 (−37.79, 3.56) | −17.12 (−38.02, 3.77) | −11.18 (−32.11, 9.74) |
| Black | −37.52 (−66.34, −8.70) | −8.48 (−39.75, 22.78) | −0.74 (−31.94, 30.45) | 34.46 (16.51, 52.40) | 25.93 (5.71, 46.16) | 25.87 (5.37, 46.36) | −3.3 (−31.69, 25.09) | 14.89 (−16.73, 46.52) | 22.58 (−8.95, 54.12) |
| Change between 1 month and 6 months | p = 0.01 | p = 0.62 | p = 0.70 | p = 0.26 | p = 0.43 | p = 0.44 | p = 0.008 | p = 0.27 | p = 0.34 |
| White | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Hispanic | −33.41 (−57.36, −9.46) | 2.12 (−27.71, 31.94) | 6.65 (−23.63, 36.92) | −9.17 (−25.26, 6.91) | 7.13 (−13.38, 27.64) | 8.93 (−11.96, 29.81) | −38.94 (−69.98, −7.90) | 9.92 (−28.94, 48.79) | 15.42 (−24.03, 54.88) |
| Asian | −9.55 (−39.17, 20.07) | −9.52 (−38.93, 19.89) | −5.35 (−35.13, 24.43) | −6.65 (−26.54, 13.25) | −7.89 (−28.11, 12.33) | −6.65 (−27.19, 13.90) | −17.08 (−55.33, 21.18) | −17.94 (−56.25, 20.37) | −12.60 (−51.41, 26.21) |
| Black | −50.72 (−91.43, −10.00) | −23.49 (−68.14, 21.17) | −17.69 (−62.81, 27.43) | −26.41 (−53.76, 0.93) | −13.66 (−44.37, 17.04) | −11.38 (−42.51, 19.75) | −78.53 (−131.11, −25.94) | −38.48 (−96.68, 19.71) | −31.43 (−90.25, 27.39) |
β (95% confidence interval); Model 1 adjusts for sex, birth weight for gestational age z-score, and age at assessment; each subsequent model includes the adjustments in the preceding model, with the following further adjustments: Model 2 includes socioeconomic variables (maternal education and household income), and Model 3 includes parenting behavioral factors (exclusive or mixed/none breastfeeding and frequency of bed-sharing).
*P-values for the racial/ethnic effects are shown.
Italic values represent P-value for race/ethnicity joint hypothesis test for linear trend.
After adjustment for SES, 1-month daytime sleep duration remained higher in black and Asian infants compared to white infants. At 6 months, SES-adjusted daytime sleep differences were only significant for black infants. After adjusting for SES, total sleep duration at 1 month and the change between two time points were no longer different across race/ethnic categories.
Models for sensitivity analyses that included childcare did not appreciably change estimates for racial/ethnic differences in sleep durations (Supplementary Table S1). In addition, application of IPW in the regression analyses, as a means to adjust for differential participation in the actigraphy study by race/ethnicity and maternal education, yielded the same range of estimates and significance compared to our primary analyses (Supplementary Table S2).
Discussion
In this prospective birth cohort study, we observed a significant increase in nighttime sleep duration, more consolidated sleep, and less daytime sleep between 1 month and 6 months of age using actigraphy. Additionally, racial/ethnic and SES differences in day and night sleep patterns emerged in early life. While at 1 month there were no differences in night sleep duration across racial/ethnic or SES groups, daytime sleep duration was longer in infants with racial/ethnic minority background and lower SES. More striking differences in sleep across groups were observed at 6 months of age: shorter night sleep, longer daytime sleep, and more awakenings in Hispanic, Asian, and black infants. Differences in sleep duration between white infants and Hispanic or black infants were largely explained by differences in SES. In contrast, SES-adjusted analyses showed that Asian infants had more frequent wake bouts and, at 6 months, shorter nocturnal sleep compared to white infants.
Our findings based on objective sleep measures are consistent with previous studies using parent-reported surveys [28, 44–48] and actigraphy in older children [49]. In these studies, Hispanic [28, 46–48], Asian [28, 46, 47], and black children [28, 44–49] from 6 months to 11 years old had less night sleep duration or were at a higher risk of chronic sleep curtailment. The current study extends the literature by providing objective evidence that the sleep differences emerging in early infancy, are unlikely to be attributable to reporting biases, and are more prominent at 6 months compared to 1 month of age. Moreover, the objective and longitudinal measurements provide the ability to characterize both day and night sleep, showing that infants from minority backgrounds (or lower SES households) have longer daytime sleep but shorter nighttime sleep at 6 months, and over this period, both nocturnal and 24-hour sleep increase more in white (or infants from higher SES households) compared to minority infants.
Differences in SES across racial/ethnic groups accounted for much of the difference in sleep–wake patterns between black and Hispanic as compared to white infants. Other possible reasons for differences in nocturnal sleep of young children include stress [50–52], maternal mental health [53], culture/tradition (i.e. habitual daytime napping [18, 44] and co-sleeping/co-rooming [31, 54, 55]), sleep environment (i.e. TV in room [28]), and behavioral factors (i.e. lack awareness of benefits from bedtime routines [50]). Hispanic and black women may more frequently experience postpartum depression [56], and their families are more likely to co-sleep [54, 55] and have a TV in their infant’s bedroom [57]. Parents with low SES may have less resources to provide an optimal sleep environment, consistent bedtimes, and bedtime routines [50, 51]. In contrast, differences between white and Asian infants were not explained by SES, and Asian infants had the highest frequency of nighttime awakenings and wake duration, perhaps due to different cultural parenting practices [18, 31]. While our objectives in this report were not to identify the specific drivers of race/ethnic differences, we found that adjusting for breastfeeding and co-sleeping did not alter the study results.
There is a paucity of research on 24-hour sleep patterns and sleep regulatory mechanisms in infants [58]. Our study highlights the importance of not only assessing nocturnal but also daytime sleep in young children. In our study, Hispanic/Latino, Asian, and black infants slept less than white infants at night but more during the day. Differences in 24-hour sleep patterns may reflect an interactive relationship between day and night sleep (disturbed nighttime sleep may lead to daytime sleep compensation; or, daytime napping may reduce homeostatic drive, resulting in less nighttime sleep). Differences in the distribution of sleep across the day may also reflect inopportune light exposures or timing of feeding, factors that can vary by cultural practices and SES. In addition, development of consolidated sleep and mature patterns of sleep architecture also reflect the development of the neural circuitry of the developing brain, which reciprocally may be influenced by electrophysiological oscillations generated during sleep. Some data indicate that daytime naps enhance learning and memory consolidation [59] and are protective against injury in children [60]. However, other studies indicate that more napping is associated with poorer nighttime sleep [61–66] and poorer neurocognitive function in preschool children [64]. Hence, 24-hour sleep distribution, circadian misalignment, and the association with physiological stress in infants require further investigation.
We recently described patterns of infant sleep duration ascertained by the caregiver-completed BISQ in this same cohort [48]. Similar to the current actigraphy results, that study also showed a decrease in daytime sleep and increase in nighttime sleep during child’s first 6 months of life. However, compared to actigraphy, caregiver report overestimated sleep (by approximately 1 hour for nighttime sleep at both time points, more than 2 hours for daytime sleep at 1 month, and more than half an hour for daytime sleep at 6 months). Caregiver reported nighttime sleep duration at 6 months was also shorter among racial/ethnic minority infants compared to the white infants. However, the shortest nighttime sleep was reported by caregivers of Hispanic infants; nighttime sleep was significantly shorter among Hispanic infants than white infants at both 1 month and 6 months. Daytime caregiver reported sleep tended to be longer at both time points in Hispanic and black infants, but those estimates were imprecise and not statistically significant. In contrast, with actigraphy we found night sleep duration at 6 months to be similarly curtailed in Hispanic and black infants, and at both 1 month and 6 months we observed significantly longer daytime sleep in Hispanic and black infants. These findings suggest that caregiver report overestimates infant sleep compared to actigraphy, especially for the daytime in early infancy, but provides information on sleep duration changes across the first 6 months of life that generally reflect the patterns observed using actigraphy. The actigraphy findings generally were more precise and yielded somewhat different estimates of relative differences across the race/ethnic groups compared to caregiver report. While the latter suggests that there may be systematic reporting biases across groups, we did not observe systematic differences in actigraphy–BISQ biases (unpublished data). Nonetheless, given differences in reporting biases across race/ethnic groups in adults [67], the differences across these studies suggest caution in interpreting demographic differences in sleep when relying on self-report.
This study had several potential limitations. First, actigraphy did not directly measure sleep and could overestimate wakefulness due to external motion (e.g. rocking) during sleep transitions [68]. To address this challenge, we required parents to record time such as when the infant was in a stroller or car seat (“sleep in motion”) and used this information to annotate the actigraphy records. Second, the overall sample included a relatively small proportion of African Americans, reflecting the local clinic population. Race/ethnicity was also highly correlated with SES, making it difficult to fully separate these influences. Third, of the enrolled sample, 29% did not provide valid actigraphy data for both time points, raising a concern over the generalizability of the findings. However, in sensitivity analyses, we applied IPW [43] to adjust for potential selection biases, and these analyses did not identify substantive differences compared to our primary analyses. Fourth, we conducted multiple statistical tests, including among six sleep variables that are highly interrelated with each other and over time, as well as exposures (race/ethnicity and SES) that are highly correlated. These tests were likely not independent of one another, but because this was the first longitudinal study using actigraphy to assess sleep patterns from 1 month to 6 months in a diverse sample, we did not adjust for multiple comparisons. Instead, we highlighted findings that met the usual nominal level of significance (i.e. p < 0.05) and were internally consistent and biologically plausible. The findings, therefore, should be replicated in other cohorts.
This study had several strengths, including its prospective design with repeated measurements of sleep–wake patterns over 24-hour periods in a diverse sample using objective recordings. While objective assessment of sleep–wake patterns in early infancy is challenging due to fragmented sleep–wake patterns, frequent feedings, and more sleep time in “motion” (during rocking, driving in cars, etc.), actigraphy has been used in prior studies for infants as early as 3 months of age [16, 23, 69, 70] as it has provided estimates of infant sleep that agreed with parent report [34], sleep diary [42], behavioral observation [38], and PSG [37].
Conclusion
Infants sleep more at night but less during the day from approximately 1 month to 6 months of age. Nighttime sleep duration increases less in Hispanic and black infants than white infants, although these differences are largely explained by lower maternal education and household income, suggesting social-environmental factors contribute to sleep health differences across race/ethnicity in early life. Asian infants have more frequent night awakenings and less night sleep duration compared to white infants. Moreover, 24-hour sleep duration increases less or even decreases in infants from low SES households. Differences in both circadian distributions and quantity of sleep emerge in early infancy, underscoring a need to identify modifiable determinants of these differences and better understand their impact on health and development.
Supplementary Material
Supplementary material is available at SLEEP online.
Table S1. Multivariable associations of race/ethnicity and sleep duration, adjusted for socioeconomic status or parenting behaviors including childcare
Table S2. Multivariable associations of race/ethnicity and sleep duration, adjusted for socioeconomic status or parenting behaviors with inverse probability weighting
Funding
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK107972). Dr. Susan Redline is partly supported by National Heart, Lung, and Blood Institute (R35 HL 135818).
Conflict of interest statement. None declared.
References
- 1. Zuckerman B, et al. Sleep problems in early childhood: continuities, predictive factors, and behavioral correlates. Pediatrics. 1987;80(5):664–671. [PubMed] [Google Scholar]
- 2. Armstrong KL, et al. The sleep patterns of normal children. Med J Aust. 1994;161(3):202–206. [DOI] [PubMed] [Google Scholar]
- 3. Lam P, et al. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics. 2003;111(3):e203–e207. [DOI] [PubMed] [Google Scholar]
- 4. Byars KC, et al. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129(2):e276–e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fatima Y, et al. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137–149. [DOI] [PubMed] [Google Scholar]
- 6. Halal CS, et al. Short sleep duration in the first years of life and obesity/overweight at age 4 years: a birth cohort study. J Pediatr. 2016;168:99–103.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sung RY, et al. Oscillometrically measured blood pressure in Hong Kong Chinese children and associations with anthropometric parameters. J Hypertens. 2008;26(4):678–684. [DOI] [PubMed] [Google Scholar]
- 8. Mezick EJ, et al. Sleep duration and ambulatory blood pressure in black and white adolescents. Hypertension. 2012;59(3):747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fallone G, et al. Experimental restriction of sleep opportunity in children: effects on teacher ratings. Sleep. 2005;28(12):1561–1567. [DOI] [PubMed] [Google Scholar]
- 10. Gregory AM, et al. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol. 2005;33(2):157–163. [DOI] [PubMed] [Google Scholar]
- 11. Dewald-Kaufmann JF, et al. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep Med. 2013;14(6):510–517. [DOI] [PubMed] [Google Scholar]
- 12. Gruber R, et al. Short sleep duration is associated with poor performance on IQ measures in healthy school-age children. Sleep Med. 2010;11(3):289–294. [DOI] [PubMed] [Google Scholar]
- 13. Zornoza-Moreno M, et al. Assessment of circadian rhythms of both skin temperature and motor activity in infants during the first 6 months of life. Chronobiol Int. 2011;28(4):330–337. [DOI] [PubMed] [Google Scholar]
- 14. Borbély AA, et al. Sleep homeostasis and models of sleep regulation. J Biol Rhythms. 1999;14(6):557–568. [DOI] [PubMed] [Google Scholar]
- 15. Montgomery-Downs HE, et al. Sleep habits and risk factors for sleep-disordered breathing in infants and young toddlers in Louisville, Kentucky. Sleep Med. 2006;7(3):211–219. [DOI] [PubMed] [Google Scholar]
- 16. Tikotzky L, et al. Maternal sleep-related cognitions and infant sleep: a longitudinal study from pregnancy through the 1st year. Child Dev. 2009;80(3):860–874. [DOI] [PubMed] [Google Scholar]
- 17. Tikotzky L, et al. Sleep and physical growth in infants during the first 6 months. J Sleep Res. 2010; 19(1 Pt 1): 103–110. [DOI] [PubMed] [Google Scholar]
- 18. Mindell JA, et al. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010; 11(3):274–280. [DOI] [PubMed] [Google Scholar]
- 19. Bruni O, et al. Longitudinal study of sleep behavior in normal infants during the first year of life. J Clin Sleep Med. 2014;10(10):1119–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sadeh A, et al. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18(1):60–73. [DOI] [PubMed] [Google Scholar]
- 21. Teng A, et al. Infant and toddler sleep in Australia and New Zealand. J Paediatr Child Health. 2012;48(3):268–273. [DOI] [PubMed] [Google Scholar]
- 22. Burnham MM, et al. Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry. 2002;43(6):713–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tikotzky L, et al. Infant sleep development from 3 to 6 months postpartum: links with maternal sleep and paternal involvement. Monogr Soc Res Child Dev. 2015;80(1):107–124. [DOI] [PubMed] [Google Scholar]
- 24. Iglowstein I, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111(2):302–307. [DOI] [PubMed] [Google Scholar]
- 25. Blair PS, et al. Childhood sleep duration and associated demographic characteristics in an English cohort. Sleep. 2012;35(3):353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Galland BC, et al. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012; 16(3):213–222. [DOI] [PubMed] [Google Scholar]
- 27. Taveras EM, et al. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125(4):686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Peña MM, et al. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carnethon MR, et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med. 2016;18:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Xiao Q, et al. ; ISCOLE Research Group. Sleep characteristics and health-related quality of life in 9- to 11-year-old children from 12 countries. Sleep Health. 2020;6(1):4–14. [DOI] [PubMed] [Google Scholar]
- 31. Mindell JA, et al. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11(4):393–399. [DOI] [PubMed] [Google Scholar]
- 32. So K, et al. The use of actigraphy for assessment of the development of sleep/wake patterns in infants during the first 12 months of life. J Sleep Res. 2007;16(2):181–187. [DOI] [PubMed] [Google Scholar]
- 33. Oken E, et al. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. [DOI] [PubMed] [Google Scholar]
- 35. Barr RG, et al. Parental diary of infant cry and fuss behaviour. Arch Dis Child. 1988;63(4):380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sadeh A. Assessment of intervention for infant night waking: parental reports and activity-based home monitoring. J Consult Clin Psychol. 1994;62(1):63–68. [DOI] [PubMed] [Google Scholar]
- 37. So K, et al. Actigraphy correctly predicts sleep behavior in infants who are younger than six months, when compared with polysomnography. Pediatr Res. 2005;58(4):761–765. [DOI] [PubMed] [Google Scholar]
- 38. Sung M, et al. Validation of actigraphy for determining sleep and wake in preterm infants. Acta Paediatr. 2009;98(1):52–57. [DOI] [PubMed] [Google Scholar]
- 39. Philips Respironics. Equivalence of Activity Recordings and Derived Sleep Statistics. http://www.actigraphy.com/assets/AWDataEquivalenceReport_0309_final-e69f789615144b7e1b8a3b3959e94556fee79f5ec67e2f02edea641c427524c3.pdf. Accessed July 16, 2019.
- 40. Meltzer LJ, et al. Use of actigraphy for assessment in pediatric sleep research. Sleep Med Rev. 2012;16(5):463–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity (1997). https://www.whitehouse.gov/wp-content/uploads/2017/11/Revisions-to-the-Standards-for-the-Classification-of-Federal-Data-on-Race-and-Ethnicity-October30-1997.pdf. Accessed November 5, 2019.
- 42. Schoch SF, et al. Actimetry in infant sleep research: an approach to facilitate comparability. Sleep. 2019;42(7). doi: 10.1093/sleep/zsz083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Seaman SR, et al. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–295. [DOI] [PubMed] [Google Scholar]
- 44. Crosby B, et al. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115(1 Suppl):225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McLaughlin Crabtree V, et al. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–324. [DOI] [PubMed] [Google Scholar]
- 46. Adam EK, et al. Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. J Fam Psychol. 2007;21(1):4–19. [DOI] [PubMed] [Google Scholar]
- 47. Nevarez MD, et al. Associations of early life risk factors with infant sleep duration. Acad Pediatr. 2010;10(3):187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ash T, et al. Emergence of racial/ethnic differences in infant sleep duration in the first 6 months of life. Sleep Med X. 2019;1:100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Vaughn BE, et al. Sleep as a support for social competence, peer relations, and cognitive functioning in preschool children. Behav Sleep Med. 2015;13(2):92–106. [DOI] [PubMed] [Google Scholar]
- 50. Hale L, et al. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr. 2009;30(5):394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Patrick KE, et al. Sleep differences by race in preschool children: the roles of parenting behaviors and socioeconomic status. Behav Sleep Med. 2016;14(5):467–479. [DOI] [PubMed] [Google Scholar]
- 52. Rodriquez EJ, et al. Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults, 2005–2012 NHANES. Prev Med. 2018; 110:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McHale SM, et al. Family Contexts of Sleep and Health Across the Life Course. Cham, Switzerland: Springer International Publishing; 2017. [Google Scholar]
- 54. Lozoff B, et al. Cosleeping in urban families with young children in the United States. Pediatrics. 1984;74(2):171–182. [PubMed] [Google Scholar]
- 55. Schachter FF, et al. Cosleeping and sleep problems in Hispanic-American urban young children. Pediatrics. 1989;84(3):522–530. [PubMed] [Google Scholar]
- 56. Howell EA, et al. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rideout V, et al. Media Use Among White, Black, Hispanic, and Asian American Children. Boston, MA: Northwestern University; 2011. [Google Scholar]
- 58. Jenni OG, et al. Sleep behavior and sleep regulation from infancy through adolescence. Sleep Med Clin. 2012; 7(3): 529–538. [Google Scholar]
- 59. Kurdziel L, et al. Sleep spindles in midday naps enhance learning in preschool children. Proc Natl Acad Sci U S A. 2013;110(43):17267–17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Boto LR, et al. Sleep deprivation and accidental fall risk in children. Sleep Med. 2012;13(1):88–95. [DOI] [PubMed] [Google Scholar]
- 61. Jones CH, et al. Napping in English preschool children and the association with parents’ attitudes. Sleep Med. 2013;14(4):352–358. [DOI] [PubMed] [Google Scholar]
- 62. Ward TM, et al. Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. J Pediatr Psychol. 2008; 33(6):666–672. [DOI] [PubMed] [Google Scholar]
- 63. Yokomaku A, et al. A study of the association between sleep habits and problematic behaviors in preschool children. Chronobiol Int. 2008;25(4):549–564. [DOI] [PubMed] [Google Scholar]
- 64. Lam JC, et al. The effects of napping on cognitive function in preschoolers. J Dev Behav Pediatr. 2011;32(2):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Thorpe K, et al. Napping, development and health from 0 to 5 years: a systematic review. Arch Dis Child. 2015;100(7):615–622. [DOI] [PubMed] [Google Scholar]
- 66. Iwata S, et al. Determinants of sleep patterns in healthy Japanese 5-year-old children. Int J Dev Neurosci. 2011;29(1):57–62. [DOI] [PubMed] [Google Scholar]
- 67. Jackson CL, et al. Concordance between self-reported and actigraphy-assessed sleep duration among African-American adults: findings from the Jackson Heart Sleep Study. Sleep. 2020;43(3). doi: 10.1093/sleep/zsz246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Camerota M, et al. Assessment of infant sleep: how well do multiple methods compare? Sleep. 2018;41(10). doi: 10.1093/sleep/zsy146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Volkovich E, et al. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep Med. 2015;16(11):1305–1312. [DOI] [PubMed] [Google Scholar]
- 70. Volkovich E, et al. Mother-infant sleep patterns and parental functioning of room-sharing and solitary sleeping families: a longitudinal study from 3 to 18 months. Sleep. 2017;41(2). doi: 10.1093/sleep/zsx207 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.