Abstract
Study objectives
The main aim of this study was to estimate the association between sleep deficiency in adolescence and subsequent prescription opioid misuse in adulthood using United States nationally representative longitudinal data.
Methods
Self-reported data captured in the National Longitudinal Study of Adolescent to Adult Health at baseline (Wave 1; mean age = 16 years) and 12 year follow-up (Wave 4; mean age = 29 years). Participants (n = 12,213) reported on four measures of sleep during adolescence (Wave 1) and on lifetime prescription opioid misuse during adulthood (Wave 4). Associations between adolescent sleep and adult opioid misuse were estimated using multivariate logistic regression analysis controlling for sociodemographics, chronic pain, mental health, childhood adverse events, and a history of substance use.
Results
During adolescence, 59.2% of participants reported sleep deficiency. Prospectively, adolescents reporting not getting enough sleep, chronic unrestful sleep, and insomnia were associated with an increased risk for prescription opioid misuse (adjusted odds ratios [OR] = 1.2, p < 0.005 for all three variables). Short sleep duration was not associated with opioid misuse.
Conclusion
This is the first study to longitudinally link sleep deficiency as an independent risk factor for the development of prescription opioid misuse. Sleep deficiency could be a driver of the opioid crisis affecting young people in the United States. Future studies should determine whether early and targeted sleep interventions may decrease risk for opioid misuse in high-risk patients prescribed opioids for pain.
Keywords: adolescent, sleep deficiency, insomnia, opioid misuse
Statement of Significance.
The current opioid epidemic remains a severe public health crisis facing the United States. Sleep deficiency is common among individuals with problematic opioid behaviors. Yet, whether sleep problems precede or are caused by opioid use is not well known. Understanding the temporal relationship between sleep and opioid use is an important first step toward improving sleep for patients at risk for problematic opioid use. Future studies are needed to investigate the mechanisms underlying associations between sleep and opioid misuse.
Introduction
Adolescence is often a “perfect storm” for poor sleep due to interactions between biological, social, and behavioral factors that result in shortened sleep duration and reduced sleep quality [1]. Recent data indicate that sleep deficiency (defined as inadequate sleep duration to meet sleep needs and/or poor sleep quality) is very common among adolescents in the United States [2–4]. Indeed, adolescent sleep deficiency is now recognized as a major public health burden in the United States due to known associations between poor sleep and adverse psychosocial and physical health outcomes including greater depressive symptoms, poor school performance, cardiometabolic health problems, motor vehicle accident risk, and problematic substance use [5, 6].
Prescription opioid misuse refers to the use of prescription opioids in a manner other than directed by a health care provider, such as in greater amounts, more often, longer than prescribed, or using someone else’s prescription [7]. Among adolescents, prescription opioid misuse is associated with several negative outcomes, including driving under the influence [8] and sexual victimization [9]. However, prescription opioid misuse also precedes more severe opioid behaviors, including heroin use and opioid overdose which has contributed to an unprecedented opioid crisis facing adolescents and young adults in the United States [10].
There are compelling data to suggest that sleep deficiency is associated with prescription opioid misuse in adolescents. For example, up to 26.7% of adolescents misuse opioids in order to help with sleep [11]. Furthermore, recent research points to several putative biological mechanisms underlying the sleep and opioid association such as connections between reward-circuitry dopaminergic neurons impacting sleep and wakefulness which, in turn are influenced by opioid receptor activation [12]. However, we do not know whether sleep deficiency in adolescence is longitudinally associated with opioid misuse later in life.
To our knowledge, only one prospective study examined the relationship between sleep in childhood and risk for substance use problems in adulthood [13]. In a sample of 386 youth from the community, Wong et al. found that those who had trouble sleeping in adolescence were 2.4 times more likely to have had a problem with illicit drug use in young adulthood [14]. However, this study has several important limitations. Participants did not report specifically on opioid use, “trouble sleeping” was assessed using a single item, and other potentially important risk factors for drug use in adulthood (e.g. chronic pain, adverse childhood experiences [ACEs]) were not assessed. Determining whether sleep deficiency in adolescence increases risk for later prescription opioid misuse could inform the development of sleep-specific intervention strategies aimed at reducing the impact of the opioid crisis.
Therefore, the primary objective of this study was to prospectively determine the temporal association between sleep deficiency during adolescence and the subsequent risk of prescription opioid misuse in adulthood. We addressed this aim using nationally representative data from a large sample of individuals in the United States participating in the National Longitudinal Survey of Adolescent Health. We hypothesized that a history of sleep deficiency during adolescence (as captured by four sleep measures) would increase risk for prescription opioid misuse in adulthood.
Methods
Participants and procedure
For this analysis, we used data from the National Longitudinal Study of Adolescent Health (Add Health) [15]. Add Health is a nationally representative, stratified, random sample of United States individuals starting in 1995 when participants were 11–21 years of age (Mage = 16 years, SD = 1.7 years). Add Health combines longitudinal survey data on respondents’ sociodemographic factors, physical and mental health, and substance use, providing unique opportunities to identify how risk factors in adolescence may be linked to health outcomes in adulthood.
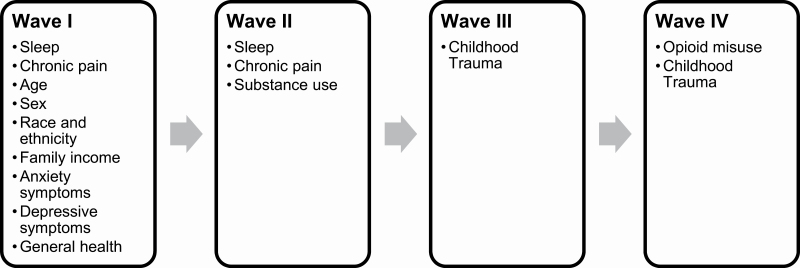
Add Health uses a complex, multistage sample design, and oversamples minorities. By applying survey weights, estimates are representative of the United States population. Thus far, participants have completed four subsequent waves of in-home interviews, the most recent of which was in 2008 when participants were between the ages of 24 and 34 years (Mage = 29 years, SD = 1.7 years). Waves include: Wave 1 (adolescence, 11–21 years of age, assessed in 1995); Wave 2 (adolescence, 12–22 years of age, assessed in 1996); Wave 3 (early adulthood, 18–28 years of age, assessed in 2002); and Wave 4 (adulthood, 24–34 years of age, assessed in 2008). We extracted data from all four Waves. The sample size included participants who completed all of the relevant items and waves (n = 12,213). No participants were excluded from our study. Participant characteristics are presented in Table 1. Additional information on Add Health is available at http://www.cpc.unc.edu/projects/addhealth. Add Health data are publicly available and therefore the Institutional Review Board at Seattle Children’s Hospital deemed this study exempt from review. Figure 1 outlines Add Health waves and measures assessed at each time point for the purposes of our study.
Table 1.
Baseline sample characteristics of participants in the National Longitudinal Study of Adolescent to Adult Health (Add Health) by sleep disturbance present during adolescence
| Total sample | Sleep deficiency present* (95% CI) | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | N = 12,213 | Weighted % | No, N = 4,806 (40.7%) | Yes, N = 7,407 (59.2%) | P | ||
| <0.001 | |||||||
| Age | 12,213 | 100.0 | 15.7 | (15.5–16.0) | 16.1 | (15.8–16.3) | |
| Sex | <0.001 | ||||||
| Male | 5,568 | 49.0 | 52.6 | (50.7–54.5) | 46.6 | (44.9–48.3) | |
| Female | 6,645 | 51.0 | 47.4 | (45.5–49.3) | 53.4 | (51.7–55.1) | |
| Race/ethnicity | 0.01 | ||||||
| White | 6,573 | 66.7 | 69.1 | (63.2–74.4) | 65.1 | (58.9–70.7) | |
| Black | 2,467 | 14.5 | 13 | (9.7–17.2) | 15.6 | (11.9–20.1) | |
| Hispanic | 1,900 | 11.6 | 11.6 | (8.6–15.5) | 11.6 | (8.7–15.4) | |
| Other | 1,273 | 7.2 | 6.4 | (4.6–8.7) | 7.8 | (6.0–9.9) | |
| Health reported as fair-poor | <0.001 | ||||||
| No | 11,320 | 92.8 | 95.3 | (94.2–96.2) | 91.1 | (89.9–92.2) | |
| Yes | 893 | 7.2 | 4.7 | (3.8–5.8) | 8.9 | (7.8–10.1) | |
| Chronic pain | <0.001 | ||||||
| No | 9,538 | 77.6 | 88.4 | (87.1–89.6) | 70.2 | (68.1–72.2) | |
| Yes | 2,675 | 22.4 | 11.6 | (10.4–12.9) | 29.8 | (27.8–31.9) | |
| High depression score | <0.001 | ||||||
| No | 11,216 | 92.4 | 98.1 | (97.5–98.5) | 88.5 | (87.5–89.5) | |
| Yes | 997 | 7.6 | 1.9 | (1.5–2.5) | 11.5 | (10.5–12.5) | |
| Adverse childhood events (ACEs) | <0.001 | ||||||
| No | 8,584 | 70.8 | 75.6 | (73.8–77.3) | 67.6 | (65.8–69.3) | |
| Yes | 3,629 | 29.2 | 24.4 | (22.7–26.2) | 32.4 | (30.7–34.2) | |
| Any substance use at baseline | <0.001 | ||||||
| No | 6,919 | 56.2 | 65.9 | (62.4–69.2) | 49.6 | (46.3–52.9) | |
| Yes | 5,294 | 43.8 | 34.1 | (30.8–37.6) | 50.4 | (47.1–53.7) | |
*Participant reported the presence of at least one of the four sleep measures, including chronic insufficient sleep, chronic unrestful sleep, insomnia, and sleep <8 h.
Figure 1.
National Longitudinal Study of Adolescent to Adult Health (Add Health) waves and measures assessed at each wave for the purposes of our study.
Measures
Sleep deficiency
During Waves I and II, participants were surveyed about four sleep behaviors, including (1) chronic insufficient sleep, (2) chronic unrestful sleep, (3) insomnia symptoms, and (4) short sleep duration.
(1) Chronic insufficient sleep was measured by asking participants whether they “usually get enough sleep.” Those who responded “no” were categorized as having chronic insufficient sleep.
(2) Chronic unrestful sleep was measured by asking participants how often they had “woken up feeling tired?” over the past 12 months and classified as a binary indicator if they reported “almost every day” or “every day.”
(3) Insomnia symptoms were measured by asking adolescents how often they “had trouble falling asleep or staying asleep?” over the past 12 months and classified as a binary indicator if adolescents reported “almost every day” or “every day” [16].
(4) Adolescents who reported sleeping less than 8 h on average in response to the question “How many hours of sleep do you usually get?” were classified as having short sleep duration, consistent with the National Sleep Foundation’s recommendations for adolescent sleep times.
Participants who reported the presence of at least one of the above described sleep measures were defined as having “sleep deficiency.”
Prescription opioid misuse
Prescription opioid misuse at Wave IV was operationalized as lifetime prescription opioid misuse using the following question: “Which of the following prescription drugs have you taken that were not prescribed for you, taken in larger amounts than prescribed, for longer periods than prescribed, or that you only took for the feeling or experience they caused: pain killers or opioids such as Vicodin, OxyContin, Percocet, Demerol, Percodan or Tylenol with codeine not prescribed?” with a binary response option of “yes” or “no.”
Covariates
Numerous cross-sectional studies indicate that adolescents with sleep problems and opioid misuse share several risk factors, including a history of chronic pain [17, 18], depression [19], other substance use [20], and a history of ACEs [21, 22]. Therefore because these factors have previously been shown to be associated with both sleep deficiency and prescription opioid misuse, we included them as a priori covariates.
Chronic pain
Adolescents reported how often they had headache, stomachache, and aches, pain, or soreness in muscles or joints over the past 12 months. Those who reported experiencing pain “almost every day” or “every day” were classified as having chronic pain, consistent with previous publications from Add Health [23, 24].
Depressive symptoms
Adolescents completed the 20-item Center for Epidemiologic Studies-Depression Scale (CES-D) at Wave 1. Items were scored based on the frequency at which depressive symptoms were experienced in the past week using a four-point Likert scale (anchors: “never/rarely” and “most/all of the time”). Total scores were calculated as a sum of the 20 items and could range from 0 (no depressive symptoms) to 60 (frequent/severe depressive symptoms) [11]. For this study, in order to ease presentation, the depression variable was categorized as either high symptoms (>24/60) versus low symptoms (≤23/60) consistent with previous Add Health publications [11].
General health
Adolescents responded to the question “In general, how is your health?” with five response options ranging from “excellent” to “poor” in Wave 1. For analyses, response options were dichotomized as either “good” (responses of “excellent”, “very good”, or “good”) or “fair-poor” (responses of “fair” or “poor”). For analyses, the referent of “fair-poor” was coded as 0 and “good” was coded as 1.
Other substance use in adolescence
At Wave 2, adolescents responded to the following 6 items assessing other substance use behaviors: “Have you” (1) “ever regularly smoked one or more cigarettes per day”, (2) “had 5 or more drinks in a row over the past 12 months”, (3) “ever tried marijuana”, (4) “ever tried cocaine”, (5) “ever tried inhalants, such as glue”, and (6) “ever tried any other illegal drugs such as LSD, PCP, heroin, pills, etc.” Response options for all 6 items were binary (“yes” vs. “no”). For the current analyses, we used a binary variable (“yes” = 1, “no” = 0) to determine whether adolescents used any other substances [25].
Adverse childhood events
Using data from Waves I, III, and IV, adolescents responded to nine items assessing exposure to childhood adverse events. Specifically, adolescents were asked how often the following happened: (1) “being left alone when an adult should have been present >6 times”; (2) “not having adults taking care of their basic needs >6 times”; (3) “being slapped, kicked, or hit by an adult caregiver >6 times”; (4) “being touched in a sexual way or being forced to touch an adult in a sexual way”; (5) “having Social Services investigate or try to take them out of their living situation”; (6) “witnessed or threatened with physical violence,” (7) “someone stabbed you,” (8) “someone shot at you”; or (9) “someone physically assaulted/beaten you up.” Response options for all nine items were binary (“yes” vs. “no”). For the current analyses, we used a binary variable (“yes” = 1, “no” = 0) to determine whether adolescents experienced any adverse childhood events.
Sociodemographics
During Wave 1, adolescents reported their age, sex, race, and ethnicity.
Statistical analysis plan
All analyses were conducted using the survey package contained in Stata version 14.2 (StataCorp College Station, TX); α was set at 0.05, and hypothesis testing was two-tailed. We adjusted for the complex sample design of Add Health by using sampling weights, regional stratification, and primary sampling unit information to provide nationally representative estimates of the USA population.
To address our primary aim, we performed multivariate logistic regression analysis to determine the association between adolescent sleep deficiency and adult prescription opioid misuse. Each sleep variable (chronic insufficient sleep, chronic unrestful sleep, insomnia, and short sleep duration) was entered into a separate model. Multivariate models controlled for age, sex, race, and ethnicity, depressive symptoms, physical health, chronic pain, other adolescent substance use/abuse, and exposure to childhood adverse events.
Results
Sample characteristics
Our analytic sample included 12,213 participants weighted to represent 17.9 million individuals nationally. Of these, 7,407 (weighted percentage: 59.2%) reported having at least 1 of the 4 sleep disturbances surveyed as adolescents during Wave 1 (Mean age = 16 years) (Table 1). Deficient sleep was common among adolescent participants: 52.4% reported sleeping less than 8 h per night, followed by chronic insufficient sleep (37.5%), chronic unrestful sleep (30.4%), and insomnia symptoms (14.0%). In this sample, 15.2% (95% confidence interval [CI]: 13.7%–16.8%) reported prescription opioid misuse by adulthood. Baseline sample characteristics, displayed by whether adolescents reported any sleep deficiency, are presented in Table 1. Adolescents with sleep deficiency systematically differed from those without reported sleep deficiency in all of the measured covariates: females were more likely to report sleep deficiency compared to males; and Black, non-Hispanic adolescents more commonly reported sleep deficiency as compared to White, non-Hispanic adolescents. Sleep deficiency was also more common among adolescents who reported their health as fair-poor, those with chronic pain, those with higher depression scores, those with a history of substance use, and individuals with a history of ACEs.
Associations between adolescent sleep deficiency and prescription opioid misuse in adulthood
Univariate associations between measures of sleep deficiency in adolescence and prevalence of prescription opioid misuse in adulthood are presented in Table 2. Adults with prescription opioid misuse were more likely to have had chronic insufficient sleep during adolescence as compared with adults without prescription opioid misuse (41.9% vs. 36.7%), as well as had higher rates of chronic unrestful sleep and higher rates of insomnia symptoms. However, rates of receiving <8 h of sleep were similar between groups.
Table 2.
Rates of adult prescription opioid misuse by sleep disturbance during adolescence
| Adolescent sleep measure | Total sample (N = 12,213) |
No opioid misuse (N = 10,612; 84.8%) |
Opioid misuse (N = 1,601; 15.2%) |
||||
|---|---|---|---|---|---|---|---|
| Weighted % | 95% CI | Weighted % | 95% CI | Weighted % | 95% CI | P | |
| Chronic insufficient sleep | 37.5 | 35.4–39.6 | 36.7 | 34.5–39.0 | 41.9 | 38.2–45.7 | 0.008 |
| Chronic unrestful sleep | 30.4 | 29.1–31.9 | 28.9 | 27.5–30.3 | 39.2 | 36.0–42.5 | <0.001 |
| Insomnia | 14.0 | 13.2–15.0 | 13.2 | 12.3–14.2 | 19.3 | 16.9–21.9 | <0.001 |
| Sleep <8 h | 52.4 | 49.9–55.0 | 52.3 | 49.6–54.9 | 53.3 | 49.3–57.4 | 0.58 |
Associations between sleep deficiency in adolescence and prescription opioid misuse in adulthood that we found in our univariate analysis, held in multivariate logistic regression analysis (Table 3). After controlling for multiple covariates as specified in our logistic regression models, individuals who reported chronic insufficient sleep (adjusted OR = 1.2; 95% CI: 1.1–1.5; p = 0.033), chronic unrestful sleep (OR = 1.2; 95% CI: 1.1–1.4; p = 0.004), and insomnia symptoms (OR = 1.2; 95% CI: 1.1–1.5; p = 0.032) during adolescence had significantly increased odds of prescription opioid misuse in adulthood. However, similar to univariate findings, short sleep duration was not significantly associated with prescription opioid misuse (OR = 1.1; 95% CI: 0.9–1.3; p = 0.339).
Table 3.
Associations between each individually measured sleep variable (chronic insufficient sleep, chronic unrestful sleep, insomnia, and sleep duration <8 h) during adolescence and the development of prescription opioid misuse in adulthood
| Chronic insufficient sleep | Chronic unrestful sleep | Insomnia | Sleep duration < 8 h | |||||
|---|---|---|---|---|---|---|---|---|
| Variables | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| Presence of sleep deficiency variable | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 1.2 | 1.1–1.5* | 1.2 | 1.1–1.4** | 1.2 | 1.1–1.5* | 1.1 | 0.9–1.3 |
| Model covariates | ||||||||
| Age at Wave 1 | 0.8 | 0.8–0.9*** | 0.8 | 0.8–0.9*** | 0.8 | 0.8–0.9*** | 0.8 | 0.8–0.9*** |
| Sex | ||||||||
| Male | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Female | 0.6 | 0.5–0.7*** | 0.6 | 0.5–0.7*** | 0.6 | 0.5–0.7*** | 0.6 | 0.5–0.7*** |
| Race and ethnicity | ||||||||
| White | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Black | 0.2 | 0.1–0.2*** | 0.2 | 0.1–0.2*** | 0.2 | 0.1–0.2*** | 0.2 | 0.1–0.2*** |
| Hispanic | 0.5 | 0.4–0.6*** | 0.5 | 0.4–0.6*** | 0.5 | 0.4–0.6*** | 0.5 | 0.4–0.6*** |
| Other | 0.7 | 0.5–0.9*** | 0.7 | 0.5–0.9** | 0.7 | 0.5–0.9** | 0.7 | 0.5–0.9*** |
| Health reported as fair-poor | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 1.2 | 0.9–1.6 | 1.2 | 0.9–1.6 | 1.2 | 0.9–1.6 | 1.2 | 0.9–1.6 |
| Chronic pain | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 1.2 | 1.0–1.4 | 1.1 | 0.9–1.4 | 1.2 | 1.0–1.4 | 1.2 | 1.0–1.4 |
| High depressive score | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 1.3 | 1.0–1.7 | 1.3 | 1.0–1.7 | 1.3 | 1.0–1.6 | 1.3 | 1.0–1.7* |
| Adverse childhood events | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 1.4 | 1.2–1.6*** | 1.4 | 1.2–1.7*** | 1.4 | 1.2–1.6*** | 1.4 | 1.2–1.7*** |
| Any substance use at baseline | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Yes | 2.5 | 2.2–2.9*** | 2.5 | 2.2–2.9*** | 2.5 | 2.2–2.9*** | 2.5 | 2.2–2.9*** |
AOR, adjusted odds ratio; CI, confidence interval. Each column presents the results of multivariate model examining association between that single sleep deficiency measure and prescription opioid misuse. Multivariate logistic regression analyses adjusted for age, sex, race & ethnicity, general health, chronic pain, depressive symptoms, adverse childhood events, and any substance use at baseline.
*p < 0.05.
**p < 0.01.
***p < 0.001 in adjusted logistic regression analyses.
We also found that, across all multivariate analyses, younger participants were less likely to report opioid misuse compared to older participants, and that females were less likely to report opioid misuse as compared to males. In addition, Black, non-Hispanic, and Hispanic participants were less likely to report opioid misuse compared to White, non-Hispanic participants. Across all models having a history of substance use and ACEs in adolescence were both associated with increased odds of reported prescription opioid misuse in adulthood. However, chronic pain, self-reported depressive symptoms, and overall physical health reported as fair or poor were not associated with prescription opioid misuse.
Discussion
We examined longitudinal associations between sleep deficiency during adolescence and prescription opioid misuse in adulthood using data from a large, nationally representative sample of individuals in the United States. In our sample, 37.5% of participants self-reported chronic insufficient sleep during adolescence, 30.4% reported chronic unrestful sleep, 14% had chronic insomnia symptoms, and 52.4% reported sleeping less than the recommended 8 h per night. Moreover, 15.2% of participants reported prescription opioid misuse by adulthood. Consistent with our hypothesis, we found that chronic insufficient sleep, unrestful sleep, and insomnia during adolescence was prospectively associated with risk for prescription opioid misuse during adulthood, over and above known risk factors for prescription opioid misuse, including sociodemographics, general health, chronic pain history, depressive symptoms, history of other substance use, and a history of childhood adverse events. We did not find an association between sleep duration and opioid misuse.
Our finding is consistent with extant literature that 60%–70% of adolescents report sleep-related problems, including receiving less than the recommended amount of sleep [26] and having daytime sleep-related impairment [27]. Indeed, chronic sleep deficiency during adolescence is considered a significant public health concern by the Center for Disease Control and is increasingly recognized as a risk factor for physical and mental health problems. However, the association between sleep deficiency and another critical public health crisis, the opioid epidemic, has been poorly defined.
The opioid crisis affects Americans of all ages but is concentrated in older adolescents and young adults. Indeed, among 16–28 year olds in the United States, 7.8% reported prescription opioid misuse in 2016 as compared with 3.6% of older adults [28]. Among young adults, prescription opioid misuse is associated with a host of negative consequences such as driving under the influence and sexual victimization [9] and is a common precursor for more serious opioid-related problems, including opioid use disorder, overdose [29], and heroin use [30]. Driving factors for opioid misuse that are commonly reported by adolescents and adults include self-treatment of physical pain, to “get high,” and to experiment [20]. However, it is becoming increasingly evident that self-treatment of sleep problems is also a major driver for prescription opioid misuse [20]. Using data from the Monitoring The Future (MTF) Study, researchers found that 8% of high school seniors reported past-year opioid misuse, and of these 26.5% reported using opioids “to get to sleep” [13]. In a smaller sample of 640 young adults who misused prescription opioids, McCabe et al. found that 13.7% used opioids to improve sleep [31]. Similarly, in a sample of adolescents who misused prescribed opioids, sleep was the third most commonly cited reason for opioid misuse after pain relief and to get high, with 12.3% using opioids for sleep [32].
It is likely that a bidirectional relationship exists between sleep and opioid use, however, the direction of sleep deficiency on subsequent opioid use remains poorly described. Several studies have found strong cross-sectional associations between chronic opioid use, including methadone [33] and buprenorphine [34] and disrupted sleep. In addition, lab-based experiments by Shaw et al. [35] and Dimsdale et al. [36] showed that opioids significantly disrupted sleep architecture in healthy adults. Furthermore, a longitudinal evaluation from a large, web-based survey of adolescents in the Detroit area revealed that prescription opioid misuse was associated with higher rates of sleep problems the subsequent year [37].
To the best of our knowledge, however, our report is the first longitudinal study to evaluate the strength of association between sleep deficiency preceding subsequent prescription opioid misuse. Pre-clinical evidence supports the plausibility of biological and psychological mechanisms underlying the directional relationship of sleep deficiency leading to future opioid misuse. For example, sleep deficiency changes the neural circuitry of the reward system toward increased sensitivity and impulsivity, resulting in impaired emotional regulation, and increased risk-taking behavior, which may in turn increase susceptibility to opioid misuse [38, 39]. Similarly, sleep deficiency is known to increase depressive symptoms as well as sensitivity to pain, both of which are motivators for opioid misuse [40]. Our study addresses this gap in knowledge, by providing initial evidence to suggest that sleep deficiency in adolescence may increase risk for adult opioid misuse.
Surprisingly, we did not find an association between sleep duration and risk for prescription opioid misuse. This finding is consistent with previous studies by Dimsdale [36] and Shaw [35] that also did not reveal an association between opioid use and sleep duration. The reason for this finding is unclear, however, short sleep duration has been associated with an increased risk of other substance use behaviors, including tobacco, alcohol, and substance use in other large, nationally representative surveys [41], and thus warrants further study. Other methods for evaluating sleep duration (e.g. prospective sleep diaries and actigraphy) may extend future research on the associations between sleep duration and prescription opioid misuse.
Our findings also highlight several sociodemographic risk factors for opioid misuse in adulthood including male sex, White, non-Hispanic ethnicity, a history of adverse childhood events, and a history of other substance use. These findings are consistent with previous research [21, 42]. However, surprisingly, we found that adolescent chronic pain was not associated with prescription opioid misuse in multivariate analysis. This is contrary to a previous study done by our group finding a strong association between chronic pain and opioid misuse using the same dataset [17]. One possible explanation for this difference is that the definition for prescription opioid misuse in the Add Health dataset has changed over time. All of the recent studies examining prescription opioid misuse in Add Health used the Wave 4 outcome (similar to our current report), while previous studies used combined data from both Wave 3 and Wave 4 (as in our own prior study). Regardless, it is important to identify subgroups of adolescents who may be at higher risk for future opioid misuse and how sleep health may play a role. Future studies are needed to understand how these sociodemographic and psychological risk factors influence adolescent and adult sleep deficiency and prescription opioid misuse.
Implications of our findings include that sleep deficiency may serve as a marker for patients at increased risk for prescription opioid misuse. Indeed, Hah et al. found, in a cohort of adults presenting with chronic pain, that in addition to a history of substance use and current opioid use, sleep deficiency in adulthood predicted which adults were at increased risk for having prescription opioid misuse [43]. They suggest that clinicians should screen for sleep deficiency in adults with chronic pain in order to identify those at risk for prescription opioid misuse. Our findings support this recommendation. Researchers should consider sleep deficiency as a novel, yet important potential target to prevent future prescription opioid misuse. For example, clinical trials of interventions for sleep deficiency such as Cognitive Behavioral Therapy for Insomnia could consider including opioid and other substance use as a treatment outcome to determine their effectiveness in preventing or reducing opioid misuse. Indeed, treating sleep in adolescents with existing substance abuse has been shown to reduce both sleep problems and substance use behaviors [44].
This study has several limitations that should be considered. First, while we establish a temporal association between sleep and opioid misuse, the design limits our ability to draw a cause–effect relationship between sleep and opioid misuse. Further, the Add Health study did not include the same adult measures of sleep to identify either how changes in sleep health over time influence future opioid misuse or whether there are concurrent associations between sleep and opioid misuse in adulthood. Second, variables used in this study were all self-report, which are subject to recall bias and social desirability bias. Future studies should include objectively measured sleep variables such as actigraphy. Another limitation is that participants are only asked about lifetime opioid misuse at Wave 4 and no questions were included about frequency or intensity of opioid misuse. Finally, Add Health was not specifically designed to answer research questions about sleep deficiency, thus there were limited measures of sleep available for analysis and several important sleep health domains were not evaluated. Future studies should include comprehensive evaluation of sleep health using standardized measures. Despite these limitations, there are significant strengths of our findings relative to the research in this area, including the use of longitudinal data and the use of more detailed sleep measures as compared to existing epidemiological studies examining associations between sleep and opioid use.
In conclusion, we prospectively link adolescent sleep deficiency to an increased future risk for prescription opioid misuse in a large nationally, representative database designed to track health behaviors and outcomes from adolescence to early adulthood. Both sleep deficiency and prescription opioid misuse are significant public health concerns affecting the health of young people in the United States. It is important that we consider sleep deficiency as an independent risk factor for future problematic opioid misuse in adolescents and young adults.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by Grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due to Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from Grant P01-HD31921 for this analysis. There are no conflicts of interest to report.
Funding
Dr Groenewald was supported by grant K23HL138155 from the National Heart, Lung, and Blood Institute. Dr Law was supported by K23NS089966 from the National Institute of Neurological Disorders and Stroke. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by the NIH.
Disclosure statement
Financial disclosure: None.
Non-financial disclosure: None.
References
- 1. Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin North Am. 2011;58(3):637–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Basch CE, et al. Prevalence of sleep duration on an average school night among 4 nationally representative successive samples of American high school students, 2007–2013. Prev Chronic Dis. 2014;11:E216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keyes KM, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015;135(3):460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maslowsky J, et al. Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. J Adolesc Health. 2014;54(6):691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hale L, et al. Embracing the school start later movement: adolescent sleep deprivation as a public health and social justice problem. Am J Public Health. 2018;108(5):599–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sleep Health. A Federal Government Web site managed by the U.S. Department of Health and Human Services, Washington, DC. https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health. Accessed March 12, 2020.
- 7. Centers for Disease Control and Prevention. Opioid Overdose. Commonly Used Terms. https://www.cdc.gov/drugoverdose/opioids/terms.html. Accessed March 24, 2020.
- 8. Chihuri S, et al. Trends in prescription opioids detected in fatally injured drivers in 6 US States: 1995–2015. Am J Public Health. 2017;107(9):1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jessell L, et al. Sexual violence in the context of drug use among young adult opioid users in New York City. J Interpers Violence. 2017;32(19):2929–2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lankenau SE, et al. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rushton JL, et al. Epidemiology of depressive symptoms in the national longitudinal study of adolescent health. J Am Acad Child Adolesc Psychiatry. 2002;41(2):199–205. [DOI] [PubMed] [Google Scholar]
- 12. Eacret D, et al. Bidirectional relationship between opioids and disrupted sleep: putative mechanisms. Mol Pharmacol. 2020;98(4):445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rabiner DL, et al. Motives and perceived consequences of nonmedical ADHD medication use by college students: are students treating themselves for attention problems? J Atten Disord. 2009;13(3):259–270. [DOI] [PubMed] [Google Scholar]
- 14. Wong MM, et al. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcohol Clin Exp Res. 2015;39(2):355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Von Korff M, et al. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155(5):325–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Roane BM, et al. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351–1356. [PMC free article] [PubMed] [Google Scholar]
- 17. Groenewald CB, et al. Associations between adolescent chronic pain and prescription opioid misuse in adulthood. J Pain. 2019;20(1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Badawy SM, et al. the interrelationship between sleep and chronic pain in adolescents. Curr Opin Physiol. 2019;11:25–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Young A, et al. Nonmedical use of prescription opioids among adolescents: subtypes based on motivation for use. J Addict Dis. 2012;31(4):332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schepis TS, et al. Prescription opioid misuse motive latent classes: outcomes from a nationally representative US sample. Epidemiol Psychiatr Sci. 2020;29:e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Quinn K, et al. The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alcohol Depend. 2016;169:190–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sullivan K, et al. Adverse childhood experiences affect sleep duration for up to 50 years later. Sleep. 2019;42(7). doi: 10.1093/sleep/zsz087 [DOI] [PubMed] [Google Scholar]
- 23. Noel M, et al. Chronic pain in adolescence and internalizing mental health disorders: a nationally representative study. Pain. 2016;157(6):1333–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Tilburg MA, et al. Chronic pain in adolescents is associated with suicidal thoughts and behaviors. J Pain. 2011;12(10):1032–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stewart TD, et al. Lifetime nonmedical use of prescription medications and socioeconomic status among young adults in the United States. Am J Drug Alcohol Abuse. 2015;41(5):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eaton DK, et al. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students—United States, 2007. J Adolesc Health. 2010;46(4):399–401. [DOI] [PubMed] [Google Scholar]
- 27. Strauch I, et al. Sleep need in adolescents: a longitudinal approach. Sleep. 1988;11(4):378–386. [DOI] [PubMed] [Google Scholar]
- 28. National Survey on Drug Use and Health (NSDUH) 2016. Rockville, MD: Administration SAaMHS; 2017. [Google Scholar]
- 29. Scholl L, et al. Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kelley-Quon LI, et al. Association of nonmedical prescription opioid use with subsequent heroin use initiation in adolescents. JAMA Pediatr. 2019;173(9):e191750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCabe SE, et al. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict Behav. 2007;32(3):562–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McCabe SE, et al. Motives for medical misuse of prescription opioids among adolescents. J Pain. 2013;14(10):1208–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bertz JW, et al. Sleep reductions associated with illicit opioid use and clinic-hour changes during opioid agonist treatment for opioid dependence: measurement by electronic diary and actigraphy. J Subst Abuse Treat. 2019;106:43–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hallinan R, et al. Insomnia and excessive daytime sleepiness in women and men receiving methadone and buprenorphine maintenance treatment. Subst Use Misuse. 2019;54(10):1589–1598. [DOI] [PubMed] [Google Scholar]
- 35. Shaw IR, et al. Acute intravenous administration of morphine perturbs sleep architecture in healthy pain-free young adults: a preliminary study. Sleep. 2005;28(6):677–682. [DOI] [PubMed] [Google Scholar]
- 36. Dimsdale JE, et al. The effect of opioids on sleep architecture. J Clin Sleep Med. 2007;3(1):33–36. [PubMed] [Google Scholar]
- 37. McCabe SE, et al. Medical use, medical misuse, and nonmedical use of prescription opioids: results from a longitudinal study. Pain. 2013;154(5):708–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hasler BP, et al. Circadian rhythms, sleep, and substance abuse. Sleep Med Rev. 2012;16(1):67–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Logan RW, et al. Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biol Psychiatry. 2018;83(12):987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Finan PH, et al. The association of sleep and pain: an update and a path forward. J Pain. 2013;14(12):1539–1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kwon M, et al. Association between substance use and insufficient sleep in U.S. high school students. J Sch Nurs. 2020. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 42. Vaughn MG, et al. Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004–2013. J Psychiatr Res. 2016;73:17–24. [DOI] [PubMed] [Google Scholar]
- 43. Hah JM, et al. Factors associated with prescription opioid misuse in a cross-sectional cohort of patients with chronic non-cancer pain. J Pain Res. 2017;10:979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Birnbaum HG, et al. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–667. [DOI] [PubMed] [Google Scholar]