Abstract
Background
Most women occupy multiple social roles during midlife. Perceived stress and rewards from these roles may influence health behaviors and risk factors. This study examined whether social role stress and reward were associated with the American Heart Association Life’s Simple 7 in a cohort of midlife women in the United States.
Methods and Results
Women (n=2764) rated how stressful and rewarding they perceived their social roles during cohort follow‐up (age range, 42–61 years). Body mass index, blood pressure, glucose, cholesterol, physical activity, diet, and smoking were assessed multiple times. All components were collected at the fifth study visit for 1694 women (mean age, 51 years). Adjusted linear and logistic regression models were used in analyses of the number of ideal components and the odds of achieving the ideal level of each component, respectively. Longitudinal analyses using all available data from follow‐up visits were conducted. At the fifth visit, more stressful and less rewarding social roles were associated with fewer ideal cardiovascular factors. Higher average stress was associated with lower odds of any component of a healthy diet and an ideal blood pressure. Higher rewards were associated with greater odds of ideal physical activity and nonsmoking. Longitudinal analyses produced consistent results; moreover, there was a significant relationship between greater stress and lower odds of ideal glucose and body mass index.
Conclusions
Perceived stress and rewards from social roles may influence cardiovascular risk factors in midlife women. Considering social role qualities may be important for improving health behaviors and risk factors in midlife women.
Keywords: midlife, psychosocial stress, risk factors, women’s health
Subject Categories: Cardiovascular Disease, Women, Risk Factors, Exercise, Diet and Nutrition
Nonstandard Abbreviations and Acronyms
- AHA
American Heart Association
- AHAS7
American Heart Association Life’s Simple 7
- MRQ
Multiple Role Questionnaire
- NHS
Nurse’s Health Study
- SWAN
Study of Women’s Health Across the Nation
- WHS
Women’s Health Study
Clinical Perspective
What Is New?
In a multiethnic population‐based cohort study of women in midlife, stress related to social roles, including employment, parenting, caregiving, and marriage, was related to achieving fewer components of ideal cardiovascular health, after adjusting for age, study site, race/ethnicity, education, and menopause status.
In the same group of women, those who rated those social roles as more rewarding achieved more ideal components of a healthy lifestyle, with stress and reward being related to different components of ideal cardiovascular health when examined separately: stress being related to diet, blood pressure, and body size; and rewards being related to physical activity and smoking behaviors.
What Are the Clinical Implications?
Clinicians addressing risk factors for cardiovascular disease in midlife women should consider social role stress and reward as potential influences of adherence to interventions and healthy behaviors.
The American Heart Association (AHA) has identified 7 key health behaviors and risk factors, known as the AHA Life’s Simple 7 (AHAS7), to target for initiatives to improve cardiovascular health. 1 The AHAS7 is a combination of behavioral (smoking, physical activity, and diet) and biologic (body mass index [BMI], glucose, cholesterol, and blood pressure) risk factors. In developing and promoting this index, the AHA emphasized the need for “primordial prevention,” or prevention of the development of any risk, as opposed to preventing events in high‐risk populations, or preventing additional events after a first event. Midlife, defined as the years between the ages of 40 and 65, is a potential time to intervene to prevent cardiovascular disease in later life. This life stage is particularly important for women, because of the additional physical, mental, and social changes associated with the menopause transition.
Psychosocial factors have been hypothesized to influence cardiovascular risk. Moreover, depressive symptoms, 2 indicators of socioeconomic status, 3 financial strain, 4 and social risk (measured by marital status, education, family support, and income) 5 have been associated with the AHAS7, as well as positive psychosocial factors, including optimism and well‐being. 6 , 7 , 8 , 9 , 10 Although stress is an extensively studied risk factor for cardiovascular disease in midlife women, 11 only 2 studies of stress and the AHAS7 in US cohorts have been published, which found that stressful life events and past‐year stress were related to lower odds of achieving ideal cardiovascular health, according to the AHAS7. One study was in an exclusively Black population 12 and found that sex did not significantly modify the association between stress and the AHAS7. The other study used only a single question to assess presence of past‐year stress, 13 and observed in stratified analyses that past‐year stress influenced adherence to the AHAS7 in both women and men.
To better understand the psychosocial determinants of the AHAS7 in women, studies with more detailed assessments of specific stressors are needed. Women in midlife can occupy multiple social roles, including employee, caregiver, parent, and spouse, which they may perceive as stressful, but also rewarding. These social roles, as well as how a woman perceives her roles, may influence her health behaviors and risk factors for cardiovascular disease. There have been few studies of social role–specific (ie, job‐related) stress and the AHAS7 in non‐US settings with mixed findings. 14 , 15 , 16 In addition, no studies of the relationship between rewarding social roles and the AHAS7 have been published.
The objective of this study was to assess the relationship between social role–related stress and reward and the AHAS7 (smoking, BMI, physical activity, diet, cholesterol, blood pressure, and glucose) in a cohort of women transitioning through menopause. We hypothesized that women who rated their social roles as more stressful would achieve fewer ideal AHAS7 components, and that greater ratings of social role reward would be related to more ideal AHAS7 components. A secondary aim was to examine the relationships between average social role stress and reward and the odds of achieving ideal levels of each individual component. Understanding which specific components of the AHAS7 are affected by social role qualities may help guide interventions to improve cardiovascular disease health.
Methods
Transparency and Reproducibility
Data collected during the baseline and first 9 annual study visits of the longitudinal SWAN (Study of Women’s Health Across the Nation) cohort were used in the analyses for this article. Public use SWAN data sets from baseline through the 10th annual follow‐up visit can be accessed by visiting the SWAN web site: http://www.swanstudy.org/swan‐research/data‐access. Some, but not all, of the data used for this analysis are contained in the public use data sets. Members of the scientific community who are interested in working with SWAN data that are not contained in the public use data sets may apply to become a SWAN investigator on the SWAN website.
SWAN is a longitudinal cohort study that was initiated in 1996 to 1997 that recruited women at 7 US sites with the following criteria: those aged 42 to 52 years who had a uterus and experienced a menstrual period in the past 3 months, who had at least one intact ovary, and who were not taking exogenous hormones. Women were recruited through an initial telephone survey to determine eligibility and enrolled at sites in California, Massachusetts, Michigan, Illinois, Pennsylvania, and New Jersey. Each site was required to recruit a prespecified number of women from a specific racial or ethnic minority group. The initial cohort included 3302 women, half of whom self‐reported being a member of a racial or ethnic minority group. Annual in‐person visits included assessments of physical, mental, and social health. Data from the first 9 SWAN follow‐up visits were used in the current analyses. SWAN protocols were approved by institutional review boards at each study site, and all participants provided written informed consent.
Measures of Role Stress and Reward
Role‐related stress and reward were calculated from a self‐administered, adapted version of the Multiple Role Questionnaire (MRQ) by Stephens et al. 17 This version of the scale was modified to accommodate 4 social roles: employee, mother or stepmother, wife or partner, and caregiver to an older or disabled adult relative. For each social role, a woman was asked if she occupied that role, and if she occupied that role, she was then asked to rate how stressful she perceived that role using a Likert scale from 1 to 5, with 1 representing “not at all” and 5 representing “extremely.” Women were also asked to rate how rewarding that role was using an identical Likert scale. Overall levels of role‐related stress and role‐related reward were calculated separately by taking the average stress and reward ratings across all roles that a woman endorsed at a given visit, as done in prior SWAN analyses. 18 The 2 continuous scores were used as the main exposure variables in this study. Women completed the MRQ at visits 1 to 6 and 8. At visit 8, a third of the sample did not complete the questionnaire because of changes to the protocol.
Cardiovascular Risk Component Outcomes
Data on the AHAS7 components were collected at baseline and over the first 9 SWAN follow‐up visits. Three components were measured at all visits (smoking, blood pressure, and BMI), whereas the others were measured intermittently. A summary of the visits with the different AHAS7 components is presented in Table S1. We present the distribution of the AHAS7 levels of each component at visit 5, the only visit where all 7 were collected concurrently, by “poor,” “intermediate,” and “ideal” levels of that component.
Body Mass Index
BMI was calculated from measurements of height and weight taken without shoes and in light indoor clothing at all study visits.
Blood Pressure
Blood pressure was measured with readings taken on the right arm, with the respondent seated and feet flat on the floor for at least 5 minutes before measurement. Respondents had not smoked or consumed any caffeinated beverage within 30 minutes of blood pressure measurement. Appropriate cuff size was determined on the basis of arm circumference. A standard mercury sphygmomanometer was used to record systolic and diastolic pressures at the first and fifth phase Korotkoff sounds. Two sequential blood pressure values were completed, with a minimum 2‐minute rest period between measures, and the average of the 2 values was used. Information about medications was collected during the in‐person interview, when women were asked if they had taken blood pressure pills since their last study visit, and asked to provide the name of the medication and show the container if they brought it. Medication data were coded by trained study personnel.
Cholesterol and Glucose
Achievement of ideal levels of total cholesterol and glucose was determined from fasting blood samples and medication data from questionnaire at baseline and follow‐up visits 1, 3, 4, 5, 6, and 7. Total cholesterol was measured on EDTA‐treated plasma using enzymatic methods on a Hitachi 747 analyzer (Boehringer Mannheim Diagnostics, Indianapolis, IN). Serum glucose was measured using a hexokinase‐coupled reaction on a Hitachi 747‐200 (Boehringer Mannheim Diagnostics). Cholesterol medications were obtained when women were asked if they had taken any medications for cholesterol or “fats in your blood” since their last study visit, and asked to provide the name of the medication and show the container if they brought it. Glucose medications were obtained when women were asked if they had taken any insulin or “pills for sugar in your blood” since their last study visit, and asked to provide the name of the medication and show the container if they brought it.
Physical Activity
Levels of regular physical activity were based on estimates from the Kaiser Physical Activity Survey, which asks about activity habits during the past year and was administered at baseline and visits 3, 5, 6, and 9. Questions about intensity, frequency, and duration of moderate and vigorous planned physical activity were used to determine whether women met “ideal,” “intermediate,” or “poor” levels of physical activity. To qualify for “ideal” physical activity, women had to participate in at least 2 hours of moderate or vigorous physical activity per week for at least 4 months of the past year. Any other amount of moderate or vigorous physical activity for at least 4 months was considered “intermediate,” and a lack of participation in any sports or planned exercise for at least 4 months was considered “poor.”
Smoking
A questionnaire asking about smoking since the last study visit was administered at all follow‐up visits.
Diet
A modified Block Food Frequency questionnaire was administered at baseline, visit 5, and visit 9, asking women how often they ate different food items on average during the past year. 19 , 20 A “healthy diet score” was calculated according to the AHA criteria for 5 components of a healthy diet: fruits and vegetables, fiber from whole grains, sodium, fish, and sugar‐sweetened beverages (Table S1).
Covariates
The following variables were used as covariates in all models: age, study site, race/ethnicity, education, and menopause status. Level of education was determined at the baseline visit using a questionnaire and categorized by high school or less, some college, or college or more. Income data were collected at all follow‐up visits using a questionnaire and categorized by <$35 000, $35 000 to $75 000, and >$75 000. Menopause status was based on self‐reported bleeding patterns over the past 12 months, reported surgery (hysterectomy or bilateral oophorectomy), and/or hormone use.
Exclusion Criteria
For the cross‐sectional analysis, women were excluded if they self‐reported a heart attack or stroke on or before visit 5. For the longitudinal analyses, data were excluded if they were from visits after which women self‐reported a heart attack or stroke. Thus, if a woman had AHAS7 data for all 7 visits, but reported a cardiac event at the third visit, only data from the first 2 visits were used in analyses. Women who were pregnant were excluded from analyses at the visit they reported the pregnancy.
Statistical Analysis
Means, SDs, frequencies, and percentages of key variables were used to describe the study sample. t‐Tests and χ2 tests were used to compare demographic characteristics and the AHAS7 of women who were included in this analysis with women who were excluded.
For the main analysis of role‐related stress and reward and the AHAS7, we first analyzed the total number of ideal AHAS7 components achieved as a continuous outcome variable. Next, achievement of the ideal level of each individual component was examined as separate outcomes (except for diet, for which we examined the presence of any of the 5 components of a healthy diet as the outcome, as no women achieved the AHA‐defined “ideal” diet of 4–5 components).
Two sets of analyses were conducted on the basis of the availability of the data: (1) cross‐sectional analyses using data from SWAN visit 5 (the only visit where all components of the AHAS7 and MRQ were collected concurrently) and (2) longitudinal analyses, using adjacent visit data when a component was missing because of study design (eg, the physical activity questionnaire was not collected at visit 1, and thus baseline data were used for that visit). See Table S1 for a summary of how data were carried forward for longitudinal analyses. Participants who did not have complete AHAS7 data at visit 5 were included in longitudinal analyses if data were available for other visits.
In cross‐sectional analyses, multivariate linear regression was used to model the number of ideal AHAS7 components a woman achieved as the outcome. Average role‐related stress and reward ratings were tested as independent variables in separate models, then were included in the same model to adjust for each other. Interactions were tested one at a time between stress and reward, stress and race/ethnicity, and reward and race/ethnicity by including the product terms of those variables in the models. Logistic regression was used to model the odds ratio (OR) of achieving an “ideal” level of each component associated with role stress and reward. Because no women had an “ideal” diet, the odds of having any component of a healthy diet was the outcome in those models. In addition, because obesity was prevalent in the population, the odds of having a BMI <30 kg/m2 was modeled as an outcome.
In longitudinal analyses using data over time, the concurrent relationship between role‐stress and role‐reward scores was examined using the number of ideal components as the dependent variable in linear mixed effects regression models with a random intercept to account for within‐woman correlation. For individual component analyses over time, the odds of an ideal level of individual components were the dependent variable in generalized linear mixed effects models with a logit link and random intercept.
SAS version 9.4 was used for analyses, and P<0.05 was considered statistically significant in the reporting of findings.
Results
Of the original cohort of SWAN women (n=3302), 2764 had data from at least one visit with the AHAS7 and social role–related stress and reward. Women who were excluded from all analyses because of missing data were more likely to be ethnic minorities, were less likely to have a college degree, were more likely to have a household income <$35 000, and were less likely to be married or in a committed relationship or employed for pay at baseline. Excluded women were also more likely to have poor levels of glucose, blood pressure, BMI, and smoking at baseline (Table 1).
Table 1.
Comparison of Baseline Characteristics of SWAN Women Included in Analysis and Excluded From Any Analyses
| Characteristic | Excluded | Included |
|---|---|---|
| No. | 538 | 2764 |
| Age, mean (SD), y | 46.18 (2.63) | 46.37 (2.7) |
| Race/ethnicity, n (%) | ||
| White | 197 (36.6) | 1354 (49) |
| Black | 193 (35.9) | 741 (26.8) |
| Hispanic | 112 (20.8) | 174 (6.3) |
| Chinese | 12 (2.2) | 238 (8.6) |
| Japanese | 24 (4.5) | 257 (9.3) |
| Education, n (%) | ||
| High school or less | 204 (38.4) | 615 (22.4) |
| Some college | 176 (33.1) | 875 (31.9) |
| College or postgraduate school | 151 (28.4) | 1250(45.6) |
| Income, n (%) | ||
| <$35 000 | 243 (46.6) | 761 (28.3) |
| $35 000–$75 000 | 170 (32.6) | 1138 (42.3) |
| >$75 000 | 108 (20.7) | 792 (29.4) |
| Marital status, n (%) | ||
| Not married or committed relationship | 161 (30) | 595 (21.6) |
| Currently married or living as married | 375 (70) | 2166 (78.4) |
| Menopause status, n (%) | ||
| Early perimenopause | 259 (49.1) | 1234 (45.2) |
| Premenopause | 267 (50.6) | 1494 (54.7) |
| Unknown attributable to hormone use | 2 (0.4) | 4 (0.1) |
| Hormone use, ever, n (%) | 2 (0.4) | 4 (0.1) |
| Employed for pay, n (%) | 392 (73.4) | 2251 (81.6) |
| Cholesterol score, n (%) | ||
| Poor | 63 (11.8) | 280 (10.2) |
| Intermediate | 165 (30.9) | 844 (30.7) |
| Ideal | 306 (57.3) | 1621 (59.1) |
| Glucose score, n (%) | ||
| Poor | 51 (10.4) | 126 (4.8) |
| Intermediate | 91 (18.6) | 480 (18.3) |
| Ideal | 347 (71) | 2024 (77) |
| BP score, n (%) | ||
| Poor | 45 (8.4) | 189 (6.9) |
| Intermediate | 274 (51) | 1143 (41.5) |
| Ideal | 218 (40.6) | 1425 (51.7) |
| BMI score, n (%) | ||
| Poor | 208 (39.7) | 868 (31.7) |
| Intermediate | 153 (29.2) | 723 (26.4) |
| Ideal | 163 (31.1) | 1145 (41.8) |
| Activity score, n (%) | ||
| Poor | 476 (89.8) | 2244 (82) |
| Intermediate | 12 (2.3) | 113 (4.1) |
| Ideal | 42 (7.9) | 381 (13.9) |
| Diet score, n (%) | ||
| Poor | 130 (79.3) | 2342 (84.7) |
| Intermediate | 34 (20.7) | 422 (15.3) |
| Smoking score, n (%) | ||
| Poor | 156 (29.5) | 413 (15.1) |
| Intermediate | 8 (1.5) | 46 (1.7) |
| Ideal | 364 (68.9) | 2283 (83.3) |
BMI indicates body mass index; BP, blood pressure; and SWAN, Study of Women’s Health Across the Nation.
Descriptive Statistics at Visit 5
At visit 5, the included women (n=1694) had an average age of 51 years. Of the 4 social roles, the most common role was mother (83%), followed by job (82%), relationship (76%), and caregiver (13%). Over half of the cohort occupied 3 roles, and 6.7% occupied all 4 roles. The average role stress rating was 2.8 (SD, 0.84), and the average role reward rating was 3.9 (SD, 0.74).
The average AHAS7 score at visit 5 (range, 0–13) was 7.9, with an SD of 2.2. No women had ideal levels of all AHAS7 components, as no women had a healthy diet at visit 5, according to AHA criteria. Of the 1694 women at visit 5 with data on all AHAS7 components, 320 (18%) had 5 to 6 ideal components, 897 (50%) had 3 to 4 components, and 572 (32%) had 0 to 2 components, and the average number of ideal components was 3.2 (SD, 1.9). Over 90% of women had ideal smoking behaviors, and close to 50% of women had ideal levels of cholesterol, BMI, and physical activity and 51% met the criteria for ideal blood pressure (Figure). At this visit, 6.6% of the women included in the analysis were on antilipid medication (6.2% were on a statin), 24% were on an antihypertensive medication, and 4.7% were on an antidiabetic.
Figure 1. Distribution of poor, intermediate, and ideal levels of each American Heart Association Life’s Simple 7 component at SWAN (Study of Women’s Health Across the Nation) visit 5 (definitions of each level in Table S1).
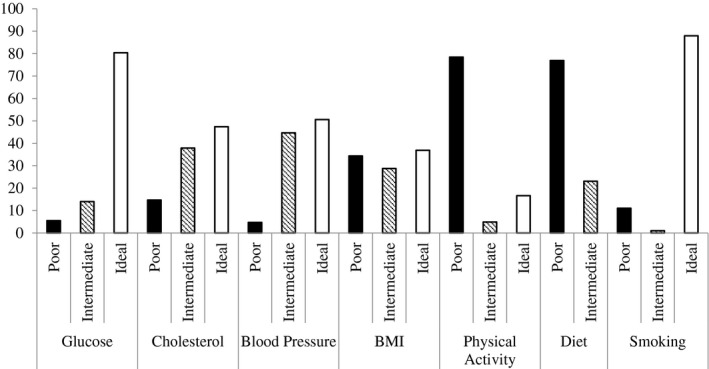
BMI indicates body mass index.
Cross‐Sectional Analyses of Role Stress, Reward, and AHAS7
Number of Ideal Components
Average role‐related stress and reward scores were associated with the number of ideal AHAS7 components at visit 5. A greater overall role‐related stress score was associated with achieving fewer ideal AHAS7 components, and greater role‐related rewards score was associated with achieving more (Table 2). Furthermore, when stress and reward were in the same model, both were independently related to the number of ideal AHAS7 components. No statistically significant interactions between stress and reward, or between stress and race/ethnicity or reward and race/ethnicity, were observed in cross‐sectional analyses.
Table 2.
Relationship Between Role‐Related Stress and Reward and the AHAS7 Components at SWAN Visit 5
| Variable | Stress and Reward in Separate Models | Stress and Reward in the Same Model | ||
|---|---|---|---|---|
| Stress β (95% CI) | Reward β (95% CI) | Stress β (95% CI) | Reward β (95% CI) | |
| No. of AHAS7 ideal components | −0.11 (−0.19 to −0.04) | 0.16 (0.08 to 0.24) | −0.09 (−0.16 to −0.01) | 0.14 (0.06 to 0.22) |
| AHAS7 component* | Stress OR (95% CI) | Reward OR (95% CI) | Stress OR (95% CI) | Reward OR (95% CI) |
| Glucose | 0.89 (0.77 to 1.03) | 1.15 (0.97 to 1.35) | 0.91 (0.78 to 1.06) | 1.12 (0.95 to 1.33) |
| Cholesterol | 0.97 (0.86 to 1.09) | 1.07 (0.93 to 1.22) | 0.98 (0.87 to 1.11) | 1.06 (0.93 to 1.22) |
| Blood pressure | 0.87 (0.76 to 0.98) | 1.08 (0.94 to 1.24) | 0.87 (0.77 to 0.995) | 1.05 (0.91 to 1.21) |
| BMI | 0.89 (0.77 to 1.02) | 1.13 (0.97 to 1.32) | 0.9 (0.78 to 1.04) | 1.10 (0.94 to 1.29) |
| Physical activity | 0.90 (0.76 to 1.06) | 1.59 (1.29 to 1.94) | 0.99 (0.83 to 1.17) | 1.58 (1.28 to 1.95) |
| Any healthy diet | 0.84 (0.73 to 0.95) | 0.96 (0.83 to 1.11) | 0.82 (0.72 to 0.94) | 0.91 (0.78 to 1.06) |
| Smoking | 0.83 (0.69 to 0.99) | 1.34 (1.1 to 1.64) | 0.88 (0.73 to 1.06) | 1.30 (1.06 to 1.59) |
All analyses done for women with nonmissing data for all 7 components. All models are adjusted for age, race, site, education, and menopause status. AHAS7 indicates American Heart Association Life’s Simple 7; BMI, body mass index; OR, odds ratio; and SWAN, Study of Women’s Health Across the Nation.
Represents an ideal level for all components, except for diet, which represents the presence of any healthy diet component.
Individual Components
In models for achieving ideal levels of each component, greater role‐related stress was related to a lower odds of ideal blood pressure and having any component of a healthy diet (Table 2). Although greater role‐related stress was not related to ideal BMI (ie, <25 kg/m2), greater stress was related to lower odds of a BMI <30 kg/m2 in the model with stress only (OR, 0.79; 95% CI, 0.69–0.91) and when role rewards were included (OR, 0.82; 95% CI, 0.71–0.94). A 1‐point greater role stress score was related to 10% reduced odds of achieving ideal physical activity, but this was not observed when role‐related rewards were included in the model.
Role‐related rewards were consistently related to significantly greater odds of physical activity and nonsmoking. At visit 5, for each point increase in average role‐related rewards, women had 58% higher odds of ideal physical activity. At visit 5, women who had more rewarding roles had 30% higher odds of having healthy smoking habits.
Interactions
There were borderline statistically significant interactions between stress and reward in models of the odds of any component of the healthy diet score (P=0.049) and ideal blood pressure (P=0.071). After stratifying on high versus low reward (on the basis of a cut point of a score of ≥4 for average role rewards), the continuous role stress score was significantly or nearly significantly related to lower odds of having any component of the healthy diet score (OR, 0.68; 95% CI, 0.55‐0.85) and ideal blood pressure (OR, 0.82; 95% CI, 0.67–1.01) among women who had low role‐related rewards but was not among women who had high role‐related rewards (diet OR, 0.94 [95% CI, 0.79–1.12]; blood pressure OR, 0.92 [95% CI, 0.78–1.1]).
Longitudinal Analyses of Role Stress, Reward, and AHAS7
Number of Ideal Components
In longitudinal models of the number of ideal AHAS7 components over time, role‐related stress was related to achieving fewer components, and role‐related rewards were related to more ideal components. In models with both role‐related stress and reward included, stress but not reward was statistically significantly related to the AHAS7 (Table 3).
Table 3.
Relationship Between Role‐Related Stress and Reward and the AHAS7 Components at SWAN From Longitudinal SWAN Data
| Variable | Stress and Reward in Separate Models | Stress and Reward in the Same Model | ||
|---|---|---|---|---|
| Stress β (95% CI) | Reward β (95% CI) | Stress β (95% CI) | Reward β (95% CI) | |
| No. of AHAS7 ideal components | −0.05 (−0.08 to −0.02) | 0.04 (0.01 to 0.08) | −0.04 (−0.07 to −0.01) | 0.03 (−0.001 to 0.07) |
| AHAS7 component* | Stress OR (95% CI) | Reward OR (95% CI) | Stress OR (95% CI) | Reward OR (95% CI) |
| Glucose | 0.89 (0.81 to 0.97) | 1.06 (0.96 to 1.18) | 0.89 (0.82 to 0.98) | 1.04 (0.93 to 1.15) |
| Cholesterol | 0.95 (0.88 to 1.03) | 1.00 (0.92 to 1.09) | 0.95 (0.88 to 1.03) | 0.99 (0.91 to 1.08) |
| Blood pressure | 0.94 (0.87 to 1.004) | 0.94 (0.87 to 1.02) | 0.93 (0.86 to 0.99) | 0.93 (0.85 to 1.01) |
| BMI | 0.89 (0.81 to 0.99) | 1.10 (0.98 to 1.23) | 0.90 (0.82 to 0.998) | 1.08 (0.96 to 1.21) |
| Physical activity | 0.83 (0.75 to 0.9) | 1.38 (1.24 to 1.53) | 0.87 (0.8 to 0.96) | 1.33 (1.19 to 1.48) |
| Any healthy diet | 0.92 (0.85 to 0.99) | 1.05 (0.97 to 1.15) | 0.92 (0.86 to 0.996) | 1.03 (0.94 to 1.12) |
| Smoking | 0.90 (0.81 to 0.99) | 1.10 (0.98 to 1.23) | 0.91 (0.82 to 1.002) | 1.08 (0.96 to 1.21) |
All models adjusted for age, race, site, education, and menopause status. Overall AHAS7 model uses data from visits with all 7 factors. Component‐specific models use all available data from all possible visits. See Table S1 for data availability. AHAS7 indicates American Heart Association Life’s Simple 7; BMI, body mass index; OR, odds ratio; and SWAN, Study of Women’s Health Across the Nation.
Represents an ideal level for all components, except for diet, which represents the presence of any healthy diet component.
Individual Components
In component‐specific longitudinal models, results for role stress were consistent with the cross‐sectional findings for BMI <30 kg/m2, diet, and smoking. In addition, an increase in 1 point of the stress score was significantly associated with 11% reduced odds of ideal glucose, 10% reduced odds of ideal BMI, and 33% reduced odds of ideal physical activity (Table 3). There were also 33% increased odds of achieving ideal levels of physical activity for each point increase in the role rewards score.
Interactions
There were no statistically significant interactions between stress and reward in the longitudinal analyses. However, there was a statistically significant interaction between reward and race on the number of ideal components (P=0.032). On stratification by race/ethnicity, role rewards were positively related to number of ideal AHAS7 in White women, and the effect of rewarding roles was negative (but not statistically significant) in Black and Hispanic women (Table 4).
Table 4.
Effect of Role‐Related Rewards on the Number of Ideal AHAS7 Components Over Time, Stratified by Race/Ethnicity
| Race/Ethnicity | No. | Reward, β (95% CI)* |
|---|---|---|
| White | 1347 | 0.08 (0.03 to 0.13) |
| Black | 729 | −0.03 (−0.09 to 0.04) |
| Hispanic | 172 | −0.08 (−0.23 to 0.08) |
| Chinese | 238 | −0.0003 (−0.11 to 0.11) |
| Japanese | 256 | 0.1 (−0.005 to 0.20) |
All models adjusted for age, race, site, education, and menopause status and restricted to women with data for all 7 components. AHAS7 indicates American Heart Association Life’s Simple 7.
β Value corresponds to the effect of a 1‐point difference in role‐related reward.
When race by reward interactions were tested for individual AHAS7 components, there was a statistically significant interaction only in models of ideal blood pressure (P=0.009). On stratification, greater role rewards were significantly related to lower odds of achieving ideal blood pressure in Black women (OR, 0.84; 95% CI, 0.72–0.98) and Hispanic women (OR, 0.73; 95% CI, 0.57–0.94) and were unrelated among White, Chinese, and Japanese women.
Discussion
In this study of midlife women, women who rated their social roles as more stressful and less rewarding on average achieved fewer ideal AHAS7 components, after adjusting for age, race, site, education, and menopause status. When individual components were examined, role stress was associated with decreased odds of achieving ideal levels of blood pressure, smoking, glucose, BMI, and any component of a healthy diet, whereas role rewards were associated with increased odds of achieving ideal physical activity and nonsmoking. Rewarding roles may have “buffered” the effects of stress on diet and blood pressure in cross‐sectional analyses, such that women who rated their roles as less rewarding experienced a negative effect of stress on these outcomes, but not among women who rated their roles as highly rewarding. In analyses incorporating data from multiple study visits, stress and reward did not significantly interact, but role rewards did interact significantly with race/ethnicity. In particular, rewarding social roles appeared to be related to lower odds of achieving ideal blood pressure in Black and Hispanic women.
There were marked differences in the achievement of ideal levels of the 7 individual components in our study, and when compared with other studies in older and middle‐aged women. At the one SWAN visit with data on all 7 components, about half of women achieved ideal levels of blood pressure, glucose, and cholesterol, but only a third had an ideal BMI and none achieved a healthy diet. The estimates of prevalence of AHAS7 components in our cohort are consistent with estimates for the US population based on National Health and Nutrition Examination Survey data, 21 except for physical activity. In National Health and Nutrition Examination Survey, 40% of middle‐aged women reported ideal physical activity, whereas <20% of our cohort achieved those levels. This could be attributable to differences in the questionnaires used to estimate activity in the different studies. Similarly, in the WHS (Women’s Health Study) cohort, the average number of ideal AHAS7 components was between 4.1 and 5.0 when stratified by race, compared with 3.2 in our study. 22 In that study, 73.8% to 88.6% of women were classified as having ideal physical activity levels. This difference could be attributable to differences in the classification. In our study, women were considered as having “regular” physical activity if they reported an activity for >4 months of the year. In addition, in the WHS, psychosocial stress (including measures of work‐family stress, relationship stress, and work stress) had a small but statistically significant correlation with the number of ideal AHA components, and psychosocial stress did not explain racial differences in number of ideal AHAS7.
In this study, stressful roles were related to lower odds of achieving ideal blood pressure, glucose, and BMI. These results are consistent with the hypothesis that chronic stress results in elevated hypothalamic‐pituitary axis activity and cortisol secretion and a dysregulated physiologic response (including increased blood pressure and glucose secretion), resulting in metabolic dysfunction and increased adiposity. 23 , 24 In addition, the fact that stress was associated with diet is consistent with prior research in Hispanic Americans 25 and Australian women in economically deprived areas, 26 and consistent with the hypothesis that stress influences diet quality by increasing appetite for calorie‐dense, high‐fat food. 27 The findings of this study contribute to the substantial existing literature on the health effects of stress, and extend it by using a specific measure of role‐related stress, rather than general life stress or stressors.
A novel finding from this study was a strong and consistent relationship between rewarding social roles and higher odds of achieving ideal levels of physical activity in this cohort of midlife women. The research on social role quality and physical activity in women has mainly focused on demanding roles as a barrier to activity, with limited findings. In 2 studies of Australian women aged <45 years, role overload was weakly related to leisure‐time physical activity, 28 and family barriers were correlated with leisure‐time physical activity in cross‐sectional analyses, but did not predict future activity. 29 These studies did not concurrently examine positive aspects of social roles or family dynamics that might facilitate participation in physical activity, such as social support. Social support for physical activity has been extensively studied as a predictor of physical activity participation and improvement, 30 , 31 with support from certain social relationships (such as family members) appearing to be more important for older adults, 32 but not in middle‐aged women from racial or ethnic minorities, who are more likely to exercise whether they report support from friends or family members, 33 or have a friend who is highly active. 34 Rewarding roles may provide a woman with social support for physical activity or encourage her to maintain her physical health through physical activity to preserve the relationships.
Because the present study was cross‐sectional and observational, it is possible that reverse causation accounts for the observed relationship between rewarding roles and physical activity, such that women who are more physically active are able to engage more in their social roles and in consequence perceive their social roles to be more rewarding. Physical activity may improve life satisfaction in middle‐aged and older adults, 35 , 36 by improving functioning and health. The finding that women who report more rewarding social roles also have higher odds of achieving ideal levels of physical activity is a novel finding that should be explored in future research.
The interaction between race and reward on the AHAS7 in longitudinal analyses was an interesting finding, particularly because it demonstrated a null or negative effect of role‐related rewards on the health of women of racial or ethnic minorities. Women in these groups may have a different perception of rewarding social roles or have additional stressors that outweigh the impact of reward on their health. They also may have additional social roles to the 4 in the MRQ, which may provide more significant stress or reward. Additional research is needed on the quality of social roles in diverse populations and their impact on health and well‐being.
This study had several strengths. First, our sample focused exclusively on women. Few prior studies of social risk or stress on AHAS7 conducted sex‐stratified analyses or tested interactions, even though the prevalence of risk factors differs by sex. 21 Midlife women are a unique population that may be undergoing significant changes to their social roles that can impact behaviors and health. Understanding perception of these social roles and their relationship with AHAS7 can provide insight for intervention design to improve these factors across populations. Next, our cohort had representation from multiple racial and ethnic minority groups, and we were able to test for interaction and conduct stratified analyses for these groups. Finally, the data from this study were collected over time, resulting in repeated measures available for analysis, whereas most prior studies of stress and the AHAS7 have been limited to data collected at a single time point.
There are some methodological limitations to this study. First, physical activity, diet, and smoking were measured with questionnaires, which increases the possibility of measurement error. Second, not all AHAS7 components were collected at every SWAN visit. To use as many visits with social role stress and reward data as possible, we used data from adjacent visits (or, in the case of diet for visit 3, from the baseline visit) when possible, carrying observations for the AHAS7 forward (in the case of visit 7, glucose, cholesterol, and baseline diet and physical activity) or backward (in the case of visit 9, diet and physical activity). Although diet and physical activity behaviors are relatively stable over midlife, this could have reduced our ability to see significant relationships between stress and reward and these behaviors. This could also be the reason why the magnitude of the relationship between social role quality and the AHAS7 was decreased in longitudinal analyses compared with the cross‐sectional analyses.
Next, the SWAN women who were excluded from any analysis were significantly different than included women on sociodemographic characteristics (race/ethnicity, education, marital status, and employment) and AHAS7 components at baseline; thus, our findings are not generalizable to these women, and may have been different had these women been included in the analyses.
Finally, the MRQ, although a better estimate of role‐related stress than single‐role instruments, may not capture all relevant social roles, particularly among racial and ethnic minorities, who are more likely to care for grandchildren, and experience detrimental effects on their health related to this caregiving. 37 Prior research in the NHS (Nurse’s Health Study) found an increased risk of coronary heart disease among women who provided care for nonill grandchildren for ≥9 hours per week. 38 The omission of caregiving for grandchildren from the questionnaire on role‐related stress may underestimate the amount of stress experienced by women, and the impact of role‐related stress on health.
Conclusions
In conclusion, women’s social role quality influences their achievement of the AHA’s recommendations for ideal cardiovascular health in midlife. Social roles in midlife may have consequences for later‐life cardiovascular health, possibly through their effect on midlife levels of risk factors. Stress associated with social roles in midlife was related to fewer ideal components of cardiovascular health, and rewarding social roles were related to achieving more components. Role‐related stress was related to different components of the AHAS7 than role‐related rewards. More research is needed to determine whether having more rewarding social roles increases physical activity, or if women with more physically active social roles perceive them to be more rewarding. Future interventions targeting improvement in women’s health behaviors in midlife, in particular physical activity, may benefit from considering the impact of both positive and negative qualities of social roles. In clinical practice, healthcare practitioners should take into account women’s social role experiences and their potential for increasing motivation for physical activity and other healthy behaviors.
Sources of Funding
The SWAN (Study of Women's Health Across the Nation) has grant support from the National Institutes of Health (NIH), DHHS (US Department of Health and Human Services), through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR), and the NIH Office of Research on Women’s Health (ORWH) (grants U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, and U01AG012495). This work was completed in partial fulfillment of Dr Stewart’s doctoral dissertation research, for which she was supported by the Cardiovascular Epidemiology T32 Training Program (5T32HL083825‐10). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH, or the NIH.
Disclosures
None.
Supporting information
Table S1
Acknowledgments
We thank the study staff at each site and all the women who participated in SWAN (Study of Women’s Health Across the Nation). Clinical Centers: University of Michigan, Ann Arbor, Siobán Harlow, principal investigator (PI), 2011 to present; MaryFran Sowers, PI, 1994 to 2011; Massachusetts General Hospital, Boston, MA, Joel Finkelstein, PI, 1999 to present; Robert Neer, PI, 1994 to 1999; Rush University, Rush University Medical Center, Chicago, IL, Howard Kravitz, PI, 2009 to present; Lynda Powell, PI, 1994 to 2009; University of California, Davis/Kaiser, Ellen Gold, PI; University of California, Los Angeles, Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY, Carol Derby, PI, 2011 to present; Rachel Wildman, PI, 2010 to 2011; Nanette Santoro, PI, 2004 to 2010; University of Medicine and Dentistry–New Jersey Medical School, Newark, NJ, Gerson Weiss, PI, 1994 to 2004; and the University of Pittsburgh, Pittsburgh, PA, Karen Matthews, PI. National Institutes of Health Program Office: National Institute on Aging, Bethesda, MD, Chhanda Dutta, 2016 to present; Winifred Rossi, 2012 to 2016; Sherry Sherman, 1994 to 2012; Marcia Ory, 1994 to 2001; National Institute of Nursing Research, Bethesda, MD, Program Officers. Central Laboratory: University of Michigan, Ann Arbor, Daniel McConnell (Central Ligand Assay Satellite Services). Coordinating Center: University of Pittsburgh, Pittsburgh, PA, Maria Mori Brooks, PI, 2012 to present; Kim Sutton‐Tyrrell, PI, 2001 to 2012; New England Research Institutes, Watertown, MA, Sonja McKinlay, PI, 1995 to 2001. Steering Committee:Susan Johnson, Current Chair; Chris Gallagher, Former Chair.
(J Am Heart Assoc. 2020;9:e017489. DOI: 10.1161/JAHA.120.017489.)
For Sources of Funding and Disclosures, see page 10.
References
- 1. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 2. Kronish IM, Carson AP, Davidson KW, Muntner P, Safford MM. Depressive symptoms and cardiovascular health by the American Heart Association's definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS One. 2012;7:e52771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boylan JM, Robert SA. Neighborhood SES is particularly important to the cardiovascular health of low SES individuals. Soc Sci Med. 2017;188:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cabeza de Baca T, Burroughs Pena MS, Slopen N, Williams D, Buring J, Albert MA. Financial strain and ideal cardiovascular health in middle‐aged and older women: data from the Women's Health Study. Am Heart J. 2019;215:129–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Caleyachetty R, Echouffo‐Tcheugui JB, Muennig P, Zhu W, Muntner P, Shimbo D. Association between cumulative social risk and ideal cardiovascular health in US adults: F 1999–2006. Int J Cardiol. 2015;191:296–300. [DOI] [PubMed] [Google Scholar]
- 6. Boehm JK, Soo J, Chen Y, Zevon ES, Hernandez R, Lloyd‐Jones D, Kubzansky LD. Psychological well‐being's link with cardiovascular health in older adults. Am J Prev Med. 2017;53:791–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hernandez R, Gonzalez HM, Tarraf W, Moskowitz JT, Carnethon MR, Gallo LC, Penedo FJ, Isasi CR, Ruiz JM, Arguelles W, et al. Association of dispositional optimism with Life's Simple 7's Cardiovascular Health Index: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study (SCAS). BMJ Open. 2018;8:e019434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hernandez R, Kershaw KN, Siddique J, Boehm JK, Kubzansky LD, Diez‐Roux A, Ning H, Lloyd‐Jones DM. Optimism and cardiovascular health: Multi‐Ethnic Study of Atherosclerosis (MESA). Health Behav Policy Rev. 2015;2:62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Loucks EB, Britton WB, Howe CJ, Eaton CB, Buka SL. Positive associations of dispositional mindfulness with cardiovascular health: the New England Family Study. Int J Behav Med. 2015;22:540–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Serlachius A, Pulkki‐Raback L, Elovainio M, Hintsanen M, Mikkila V, Laitinen TT, Jokela M, Rosenstrom T, Josefsson K, Juonala M, et al. Is dispositional optimism or dispositional pessimism predictive of ideal cardiovascular health? The Young Finns Study. Psychol Health. 2015;30:1221–1239. [DOI] [PubMed] [Google Scholar]
- 11. Stewart AL, Kathawalla UK, Wolfe AG, Everson‐Rose SA. Women's heart health at mid‐life: what is the role of psychosocial stress? Women's Midlife Health. 2018;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brewer LC, Redmond N, Slusser JP, Scott CG, Chamberlain AM, Djousse L, Patten CA, Roger VL, Sims M. Stress and achievement of cardiovascular health metrics: the American Heart Association Life's Simple 7 in Blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7:e008855. DOI: 10.1161/JAHA.118.008855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mathews L, Ogunmoroti O, Nasir K, Blumenthal RS, Utuama OA, Rouseff M, Das S, Veledar E, Feldman T, Agatston A, et al. Psychological factors and their association with ideal cardiovascular health among women and men. J Women's Health. 2018;27:709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Veromaa V, Kautiainen H, Saxen U, Malmberg‐Ceder K, Bergman E, Korhonen PE. Ideal cardiovascular health and psychosocial risk factors among Finnish female municipal workers. Scand J Public Health. 2017;45:50–56. [DOI] [PubMed] [Google Scholar]
- 15. Chou LP, Tsai CC, Li CY, Hu SC. Prevalence of cardiovascular health and its relationship with job strain: a cross‐sectional study in Taiwanese medical employees. BMJ Open. 2016;6:e010467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rocco PTP, Bensenor IM, Griep RH, Moreno AB, Alencar AP, Lotufo PA, Santos IS. Job strain and cardiovascular health score (from the Brazilian Longitudinal Study of Adult Health [ELSA‐Brasil] Baseline). Am J Cardiol. 2017;120:207–212. [DOI] [PubMed] [Google Scholar]
- 17. Stephens MA, Franks MM, Townsend AL. Stress and rewards in women's multiple roles: the case of women in the middle. Psychol Aging. 1994;9:45–52. [DOI] [PubMed] [Google Scholar]
- 18. Lanza di Scalea T, Matthews KA, Avis NE, Thurston RC, Brown C, Harlow S, Bromberger JT. Role stress, role reward, and mental health in a multiethnic sample of midlife women: results from the Study of Women's Health Across the Nation (SWAN). J Women's Health. 2012;21:481–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data‐based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. [DOI] [PubMed] [Google Scholar]
- 20. Huang MH, Schocken M, Block G, Sowers M, Gold E, Sternfeld B, Seeman T, Greendale GA. Variation in nutrient intakes by ethnicity: results from the Study of Women's Health Across the Nation (SWAN). Menopause (New York, NY). 2002;9:309–319. [DOI] [PubMed] [Google Scholar]
- 21. Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd‐Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Burroughs Peña MS, Mbassa RS, Slopen NB, Williams DR, Buring JE, Albert MA. Cumulative psychosocial stress and ideal cardiovascular health in older women. Circulation. 2019;139:2012–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McEwen BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. [DOI] [PubMed] [Google Scholar]
- 24. Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences: MacArthur studies of successful aging. Arch Intern Med. 1997;157:2259–2268. [PubMed] [Google Scholar]
- 25. Isasi CR, Parrinello CM, Jung MM, Carnethon MR, Birnbaum‐Weitzman O, Espinoza RA, Penedo FJ, Perreira KM, Schneiderman N, Sotres‐Alvarez D, et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol. 2015;25:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mouchacca J, Abbott GR, Ball K. Associations between psychological stress, eating, physical activity, sedentary behaviours and body weight among women: a longitudinal study. BMC Public Health. 2013;13:828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–458. [DOI] [PubMed] [Google Scholar]
- 28. Lovell GP, Butler FR. Physical activity behavior and role overload in mothers. Health Care Women Int. 2015;36:342–355. [DOI] [PubMed] [Google Scholar]
- 29. Santos I, Ball K, Crawford D, Teixeira PJ. Motivation and barriers for leisure‐time physical activity in socioeconomically disadvantaged women. PLoS One. 2016;11:e0147735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Choi J, Lee M, Lee JK, Kang D, Choi JY. Correlates associated with participation in physical activity among adults: a systematic review of reviews and update. BMC Public Health. 2017;17:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kouvonen A, De Vogli R, Stafford M, Shipley MJ, Marmot MG, Cox T, Vahtera J, Vaananen A, Heponiemi T, Singh‐Manoux A, et al. Social support and the likelihood of maintaining and improving levels of physical activity: the Whitehall II Study. Eur J Pub Health. 2012;22:514–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lindsay Smith G, Banting L, Eime R, O'Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle‐ and older‐aged minority women: results from a US survey. Soc Sci Med. 1999;49:781–789. [DOI] [PubMed] [Google Scholar]
- 34. Janssen I, Dugan SA, Karavolos K, Lynch EB, Powell LH. Correlates of 15‐year maintenance of physical activity in middle‐aged women. Int J Behav Med. 2014;21:511–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maher JP, Pincus AL, Ram N, Conroy DE. Daily physical activity and life satisfaction across adulthood. Dev Psychol. 2015;51:1407–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Elavsky S, McAuley E. Physical activity, symptoms, esteem, and life satisfaction during menopause. Maturitas. 2005;52:374–385. [DOI] [PubMed] [Google Scholar]
- 37. Chen F, Mair CA, Bao L, Yang YC. Race/ethnic differentials in the health consequences of caring for grandchildren for grandparents. J Gerontol Ser B, Psychol Sci Soc Sci. 2015;70:793–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lee S, Colditz G, Berkman L, Kawachi I. Caregiving to children and grandchildren and risk of coronary heart disease in women. Am J Public Health. 2003;93:1939–1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


