Abstract
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, clonal, complement-mediated hemolytic anemia with protean manifestations. PNH can present as a hemolytic anemia, a form of bone marrow failure, a thrombophilia, or any combination of the above. Terminal complement inhibition is highly effective for treating intravascular hemolysis from PNH and virtually eliminates the risk of thrombosis, but is not effective for treating bone marrow failure. Here, I present a variety of clinical vignettes that highlight the clinical heterogeneity of PNH and the attributes and limitations of the 2 US Food and Drug Administration–approved C5 inhibitors (eculizumab and ravulizumab) to treat PNH. I review the concept of pharmacokinetic and pharmacodynamic breakthrough hemolysis and briefly discuss new complement inhibitors upstream of C5 that are in clinical development. Last, I discuss the rare indications for bone marrow transplantation in patients with PNH.
Visual Abstract
Introduction
Paroxysmal nocturnal hemoglobinuria (PNH) is a complement-driven hemolytic anemia resulting from the clonal expansion of stem cells harboring a somatic PIGA mutation.1,2 The PIGA gene product is required for the biosynthesis of glycosylphosphatidylinositol (GPI) anchors, a glycolipid moiety that attaches numerous proteins to the cell surface.3 PNH blood cells have a deficiency of all GPI-anchored proteins. The absence of CD55 and CD59, both GPI-anchored complement regulators leads to complement-driven erythrocyte lysis and a marked predisposition for venous and arterial thrombosis.
PIGA mutations alone are not are not sufficient for clonal expansion in PNH.4,5 GPI-anchor protein deficiency on stem cells leads to a conditional survival advantage of PNH stem cells compared with normal stem cells in the setting of autoimmunity. This explains why PNH frequently evolves from acquired aplastic anemia (an autoimmune disease that targets hematopoietic stem/progenitor cells). PNH is not associated with inherited forms of aplastic anemia such as dykeratosis congenita, Fanconi anemia, or Schwachman-Diamond syndrome.6 Thus, immunologic escape, alone or in combination with other somatic mutations, allows for the clonal expansion PNH blood cells.4 Mutations associated with clonal hematopoiesis such as JAK2V617F and CALR have also been found in patients with PNH, which explains how patients without a history of acquired aplastic anemia sometimes develop PNH.7-9
Complement inhibitors that target terminal complement are the treatment of choice for PNH.10-13 The median survival for patients with PNH before 2007 was 15 to 20 years; thrombosis was the leading cause of death.14-16 In 2007, eculizumab, a monoclonal antibody that blocks terminal complement at C5, changed the natural history of PNH.17 There are now several new complement inhibitors that inhibit complement at C5 and upstream of C5, but thus far only eculizumab and ravulizumab are approved by the US Food and Drug Administration (FDA) and the European Medicines Agency for the treatment of PNH. With appropriate treatment, survival of patients with PNH now matches that of aged-matched controls.18,19
Here, I present 4 clinical vignettes that are representative of my clinical practice based on the biology of the disease, clinical experience, and evidence-based medicine.
Patient 1: PNH presenting with thrombosis in a 45-year-old woman
This 45-year-old woman with no medical history presented with 3 weeks of intermittent, crampy, right upper quadrant abdominal pain, fatigue, dyspnea, and pleuritic chest pain. An abdominal ultrasound raised the possibility of acalculous cholecystitis, so the patient was admitted to the hospital where a computed tomography (CT) scan was done, revealing a right-sided pulmonary embolism. Lower extremity dopplers did not reveal any deep venous thrombi, and a Tech–hepatobiliary iminodiacetic acid scan was normal; however, a CT scan of the abdomen revealed hepatic and splenic vein thrombosis with extensive collaterals. She denied gross hemoglobinuria, difficulty swallowing, or headache. Her medical history was unremarkable other than preeclampsia with her second pregnancy. She was on no regular medications and had no family history of thrombosis. Intravenous heparin was administered, and she was transitioned to warfarin with a goal international normalized ratio of 2.0 to 3.0. A complete blood count revealed a leukocyte count of 3.7 × 109/L, a hemoglobin of 7.7 g/dL, and a platelet count of 102 × 109/L. She presented with an absolute reticulocyte count of 181 000 mm3 and a lactate dehydrogenase (LDH) level of 647 IU/L (reference range, 119-226). PNH flow cytometry revealed an absence of GPI-anchored proteins on 60% of her erythrocytes, 88% of her monocytes, and 94% of her granulocytes, establishing the diagnosis of PNH. She was vaccinated against Neisseria meningitides and started on eculizumab. Following the standard eculizumab introduction period (600 mg intravenously, weekly), she was maintained on 900 mg intravenously (biweekly). Her dyspnea and abdominal pain resolved, and her warfarin was discontinued after 3 months of anticoagulation. Repeat blood counts revealed a hemoglobin level of 9.7 g/dL, 7.0% reticulocytes, and an LDH of 271 IU/L.
Comments about patient 1
This patient illustrates the devastating complement-dependent thrombophilia associated with PNH. It also highlights that not all patients with PNH present with hemoglobinuria.20 The diagnosis was established by documenting the presence of a hemolytic anemia in conjunction with severe deficiency of GPI-anchored protein on multiple cell lineages by flow cytometry.21,22 Thrombosis in PNH is more common in patients with large PNH clones (>50% PNH granulocytes) but may occur in patients with smaller clones.15 Before 2007, the year eculizumab was approved, thrombosis was the leading cause of death in patients with PNH.16,23 PNH-associated thrombosis is predominantly venous, but arterial thrombosis is also reported. The abdominal veins (hepatic, portal, splenic, mesenteric) are the most commons sites; other common venous sites include cerebral and dermal vein thrombosis.
The mechanism of thrombosis in PNH is multifactorial.20 Intravascular hemolysis and activation of PNH platelets have been proposed as contributing factors. The involvement of signaling pathways that depend on the activation of complement C5 is suggested by the observation that eculizumab therapy can substantially reduce the number of thrombotic events.19,24 C5 activation promotes coagulation via various mechanisms25; in turn, coagulation factors can also activate the complement cascade.26 However, it is now clear, based on laboratory and clinical evidence, that complement is the major driver of thrombosis in PNH.27,28
Anticoagulation with heparin or low-molecular-weight heparin is still the first action to take in the setting of an acute thrombotic event. Direct oral anticoagulants are likely equivalent but have not been well studied in PNH. Eculizumab or ravulizumab should be started as soon as possible to prevent further thrombosis because anticoagulation alone is insufficient for long-term control.24 I now consider ravulizumab the treatment of choice for PNH. It targets the same C5 epitope as eculizumab and has been shown to be noninferior in head-to-head clinical trials.12,13,29 The major advantage is that ravulizumab’s terminal half-life is 4 times that of eculizumab, and it can be administered intravenously every 8 weeks after the 2-week induction phase. I consider untreated PNH a provoking factor, and do not feel patients with PNH need indefinite anticoagulation; however, some hematologists recommend indefinite anticoagulation. I usually overlap anticoagulation and complement inhibition for 3 to 6 months as long as there are no other provoking factors. I discontinue anticoagulation if thrombotic symptoms are resolved and the patient is well controlled (LDH <1.5× the upper limit of normal) on a complement inhibitor30,31; however, discussion with the patient is advised given the paucity of data concerning the risks vs benefit of this recommendation.
Patient 2: a 44-year-old man with classical PNH
This 44-year-old man presents with a chief complaint of bright red hemoglobinuria, fatigue, chest pain, dyspnea on exertion, and difficulty swallowing liquids and solids after mowing his lawn on a hot summer day. Complete blood count reveals a hemoglobin of 6.7 g/dL, leukocytes of 3.8 × 109/L, platelets of 98 × 109/L, and an absolute reticulocyte count of 287 000 mm3. LDH level is 2800 IU/L. A direct antiglobulin test is negative. He reports reddish-dark urine in the morning most days of the week, a dull backache, and transient impotence. He had required 6 units of packed red cells in the past month to maintain a hemoglobin greater than 7.5 g/dL. PNH flow cytometry reveals 18% PNH erythrocytes, 85% PNH granulocytes, and 87% PNH monocytes. Eculizumab is administered. Following induction, he is maintained on eculizumab 900 mg every 2 weeks but continuing to require 1 to 2 units of packed red cells every 4 to 6 weeks. His LDH decreases to 302 IU/L during his induction phase. He notes that his urine often turns dark and that many of his PNH symptoms (impotence and fatigue) return the day or two before his next infusion. LDH immediately before his most recent infusion was 732 IU/L. He is switched to intravenous ravulizumab and maintained on a dose of 3300 mg (weight, 87 kg) every 8 weeks. His breakthrough PNH flares stop, and he has been transfusion independent for 3 months but still reports mild fatigue and dyspnea on exertion. A complete blood count (CBC) before his infusion last week reveals a hemoglobin of 9.4 g/dL, an absolute reticulocyte count of 265 000 mm3, and a platelet count of 107 × 109/L. His LDH level is 291 IU/L. A direct antiglobulin test is positive for C3d but negative for IgG.
Comments about patient 2
Patient 2 has PNH with relatively well-preserved bone marrow function, a large PNH clone, and signs and symptoms of intravascular hemolysis. Smooth muscle dystonia is common in PNH. Intravascular hemolysis leads to high levels of free hemoglobin in the plasma, often 10 times that seen in hemoglobinopathies.32,33 Free hemoglobin scavenges nitric oxide preventing the normal relaxation of smooth muscle leading to abdominal/back pain, esophageal spasm, difficulty swallowing food and liquids, and erectile dysfunction in males. Some patients even describe transient ischemic attack symptoms during severe hemolytic attacks from vasoconstriction of vessels in the central nervous system. These vascular symptoms often resolve within hours after administration of eculizumab or ravulizumab. It also explains why headache (caused by vasodilation of cerebral blood vessels) is so common after the first dose of these medications but is not prominent with subsequent doses or when complement inhibition is used for non-PNH indications (eg, atypical hemolytic uremic syndrome or myasthenia gravis).
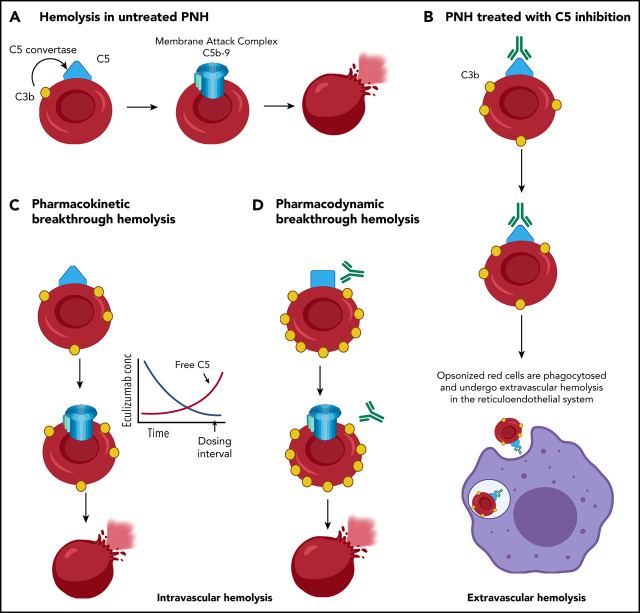
Patient 2 is experiencing breakthrough hemolysis on eculizumab, which is defined as a return of PNH symptoms (hemoglobinuria, abdominal pain, or other classical PNH symptoms) in association with a rise in LDH (defined as LDH ≥2 times the upper limit of normal (ULN) after prior LDH reduction to <1.5× ULN on therapy).29 Ravulizumab is noninferior to eculizumab.12,13 Breakthrough hemolysis from C5 inhibition is either pharmacokinetic or pharmacodynamic (Figure 1).34 Pharmacokinetic breakthrough results from suboptimal C5 inhibition (free C5 ≥0.5 µg/mL) because of inadequate drug levels. Pharmacokinetic breakthrough tends to occur regularly and usually 10 days or more after the last dose of drug, as is happening with patient 3. Pharmacodynamic breakthrough occurs despite adequate drug levels. Under strong complement activation (third trimester pregnancy, infection, major surgery etc) PNH red cells densely coated with C3b can cause C5 to adopt a C5b-like conformation that is not inhibited by eculizumab or ravulizumab.35 In the 2 largest clinical trials of ravulizumab, no breakthrough hemolysis was associated with elevations in free C5 levels (pharmacokinetic breakthrough).29 Pharmacokinetic breakthrough hemolysis was less frequent with ravulizumab compared with eculizumab. There was no difference in pharmacodynamics breakthrough between the 2 drugs. Pharmacokinetic breakthrough responds to increasing the dose of eculizumab or shortening the interval in between doses; switching to ravulizumab is also effective and more convenient for the patient.
Figure 1.

Mechanisms of hemolysis in PNH. (A) Loss of CD55 and CD59 on PNH red cells leaves them vulnerable to complement-mediated intravascular hemolysis. (B) PNH red cells from patients with PNH treated with C5 inhibition (eculizumab or ravulizumab) often become coated with C3 fragments that serve as opsonins and lead to extravascular hemolysis in the spleen and liver. C5 inhibition compensates for the loss of CD59 and prevents intravascular hemolysis; however, CD55, upstream to C5 is important for accelerating decay of the C3 convertase. The lack of CD55 from PNH red cells leads to the accumulation of C3b and its processed forms iC3b and C3dg. (C) Pharmacokinetic intravascular hemolysis caused by insufficient drug dosing allows free C5 levels to rise. (D) Pharmacodynamic intravascular hemolysis. Complement amplifying conditions (pregnancy, infection, major surgery) can result in excess C3b accumulation on PNH red cells that leads to a conformational change in C5 and decrease the binding of eculizumab or ravulizumab to C5, resulting in breakthrough hemolysis even in the absence of a rise in free C5.
Pharmacokinetic breakthrough hemolysis abated after ravulizumab, but patient 2, like virtually all patients treated with eculizumab and ravulizumab, continues to experience extravascular hemolysis and a mild to moderate anemia. PNH red cells are deficient in CD59, which inhibits formation of the membrane attack complex. They are also deficient in CD55, which inhibits the C3 and C5 convertases. Ravulizumab binds to C5 and inhibits the C5 convertase (C3bBbC3b·P) from cleaving C5 into C5a and C5b. It inhibits complement upstream of CD59 and decreases intravascular hemolysis by preventing formation of the membrane attack complex.36 CD55 is upstream of C5. Patients with PNH on ravulizumab accumulate C3 fragments on the PNH erythrocytes, and these patients have varying degrees of extravascular hemolysis (Figure 1).37 This explains why patient 2 has a positive direct antiglobulin test with C3d only. Newer complement inhibitors that work upstream of CD55 are in clinical development.
Patient 3: 25-year-old pregnant woman with PNH
A 25 year-old, gravida 2, para 1, woman presents at 33 weeks of pregnancy with fatigue, a single episode of “cola-colored” hemoglobinuria. Three days before admission, her hemoglobin was 9.9 g/dL, LDH level was 820 IU/L, haptoglobin level was <10 mg/dL, and absolute reticulocyte count was 185 000 mm3. Leukocyte count and differential are normal, and platelets are 112 × 109/L. Peripheral smear reveals a normochromic, normocytic anemia with polychromasia. No schistocytes are present. Direct antiglobulin test is negative. The day of admission, her hemoglobin is now 7.8 g/dL, and LDH level is 1740 IU/L. Total bilirubin is 4.8 mg/dL with a direct bilirubin of 0.8 mg/dL. Renal function and electrolytes are within normal limits, although some of her results are reported as hemolyzed. She has mild dyspnea on exertion and reports difficulty in swallowing her prenatal vitamins. She has no chest pain, cough, or hemoptysis. Pulse is 95 beats per minute, respirations are 16 breaths per minute, blood pressure is 110/68 mm Hg, and her temperature is 36.6°C. She is pale and has scleral icterus. The remainder of her examination is normal other than an appropriate gravid uterus. Peripheral blood flow cytometry reveals 56% PNH granulocytes, 55% PNH monocytes, and 13% PNH red cells. She takes prenatal vitamins but no other regular medications. She has no allergies. The next day, eculizumab 600 mg is administered intravenously. She is also started on enoxaparin 40 mg subcutaneously daily and amoxicillin/clavulanate 500/125 mg by mouth every 12 hours × 14 days, and she is vaccinated against Neisseria A and B. Two days later, her hemoglobinuria and dysphagia resolve, and her fatigue and dyspnea improve. A week later her hemoglobin is 8.9 g/dL, LDH level is 278 IU/L, absolute reticulocyte count is 197 000 mm3, and total bilirubin is 2.6 mg/dL. She is induced at 39 weeks and delivers a healthy boy weighing 7 pounds and 2 ounces. She is planning on switching to ravulizumab once she finishes breast feeding.
Comments about patient 3
Managing PNH and pregnancy is challenging because complement activation increases during pregnancy, especially after 20 weeks.38,39 Close collaboration between hematology and obstetrics is essential. Historically, morbidity and mortality were high for mother and fetus, such that pregnancy for patients with PNH was discouraged.40,41 Maternal mortality approached 20%, mainly because of thromboembolic events, and fetal mortality approached 9%, largely because of premature births. Complement inhibition has made pregnancy less risky for patients with PNH. Eculizumab is currently the drug of choice for pregnant patients with PNH; it does not cross the placenta at doses high enough to affect complement activation and is not excreted into breast milk.42 Thus, any potential risk of eculizumab in pregnant patients with PNH seems far outweighed by the benefits. The International PNH registry reported data from 75 pregnancies in 61 women with PNH on eculizumab. There were no maternal deaths and 3 (4%) fetal deaths. A total of 25 babies were breastfed, and in 10 cases, the breast milk was examined for the presence of eculizumab; none was detected.43 Given the structural similarities, ravulizumab is also likely to be safe in pregnancy, but there is very little clinical experience with this drug in pregnancy. Breakthrough hemolysis, especially beyond the second trimester, is common. The mechanism can be caused by both pharmacokinetic and pharmacodynamic breakthrough. Thus, up to 50% of patients required increased dosing. In the PNH registry study, the dose of eculizumab was increased or the interval between dosing was decreased in 23 of the pregnancies. The patient in the vignette manifested with PNH late in her third trimester of pregnancy, likely related to the increased terminal complement activation typical of the third trimester of pregnancy. Thromboembolic prophylaxis during pregnancy for patients with PNH is not well studied. I administer prophylactic enoxaparin (40 mg daily, subcutaneously) at the start of the second trimester and continue for at least 8 weeks after delivery. When therapy needs to be started urgently (pregnancy, thrombosis, massive hemolysis), I vaccinate the patient against Neisseria and treat with prophylactic antibiotics for 2 weeks.
Patient 4: a symptomatic PNH clone in the setting of acquired severe aplastic anemia
A 27-year-old previously healthy man presents with 3 weeks of increasing fatigue, easy bruising, and dyspnea when climbing stairs. Leukocytes are 1.9 × 109/L, with 8% neutrophils and 92% lymphocytes. Hemoglobin is 7.2 g/dL with an absolute reticulocyte count of 36 500 mm3. Platelet count is 12 × 109/L. The bone marrow is less than 10% cellular with absent megakaryocytes and no increase in blasts. Cytogenetics are normal. An employment physical CBC 3.5 years ago revealed a normal CBC. PNH flow cytometry reveals 12% PNH granulocytes, 11% PNH monocytes, and 1% PNH erythrocytes. Fanconi screen is negative, and flow-fish telomere examination reveals telomere length in the lymphocytes that are in the 25th percentile for age. HLA typing reveals that he shares a haplotype with his healthy ABO-compatible, 23-year-old healthy sister. His parents are both 55 years old and healthy. Two weeks later, he is being evaluated for allogeneic bone marrow transplant (BMT) from his sister and reports multiple bouts of nausea and anorexia with 7/10 left-sided abdominal pain with guarding. A CT scan of the abdomen with contrast reveals a normal appendix, liver, and spleen. There are no masses. Small bowel thickening and a small amount of free fluid posterior to the bladder are noted. His D-dimer is 3.7. His LDH is 340 IU/L, and repeat PNH flow cytometry now reveals 31% PNH granuloctyes and 37% PNH monocytes. He remains deeply pancytopenic and requires twice weekly platelet infusions and weekly red cells. He is started on eculizumab 600 mg weekly with amoxicillin for Neisseria prophylaxis. His abdominal pain resolves several hours after his first eculizumab infusion. One day after his second dose of eculizumab, he starts his BMT conditioning regimen of antithymocyte globulin and cyclophosphamide. Eculizumab is discontinued, and the patient becomes transfusion independent with 100% donor chimerism 30 days after BMT. He is off immunosuppression in complete remission without graft-versus-host disease 1 year after BMT.
Comments about patient 4
Small clinically silent PNH clones are found in up to 70% of adults and 10% of children with acquired aplastic anemia. It is important to screen all aplastic anemia for the presence of PNH cells. First, it helps exclude the inherited forms of bone marrow failure (ie, Fanconi anemia, dyskeratosis congenita) as PNH is almost never associated with inherited forms of bone marrow failure.6 Second, some patients (patient 4) can present with an overlap syndrome of PNH and aplastic anemia. In these cases, definitive therapy is directed at the aplastic anemia, but in rare cases, as above, the PNH clone also needs to be addressed. This patient meets criteria for severe aplastic anemia; thus, allogeneic BMT is indicated and has the potential to eradicate both the aplastic anemia and the PNH clone.44,45 Eculizumab was administered in this case to treat the potentially life-threatening thrombosis. The abdominal pain, elevated D-dimer, and small bowel thickening suggest microvascular thrombosis. Eculizumab is useful as a “bridge” therapy to prevent further pain and thrombosis until transplant.44 Because long-term complement inhibition is not needed after successful transplantation, eculizumab is a reasonable choice. I typically continue the drug until administration of the conditioning regimen. The C5 inhibition does not adversely affect outcomes of BMT. Transplant-related mortality using modern bone marrow transplant regimens is low for severe aplastic anemia; however, registry data from 1978 through 2007 suggest that thromboembolism in aplastic anemia patients with a PNH clone predicts for higher transplant-related mortality.46
Final considerations and future directions
Eculizumab and ravulizumab are presently the only FDA-approved drugs for the treatment of PNH. Thrombosis, severe anemia, or PNH symptoms (chronic fatigue, pain, dyspnea) are strong indications for initiating therapy. Terminal complement inhibition increases the risk for Neisseria infection; thus, all patients should be vaccinated against Neisseria.47 Even with vaccination, the risk of acquiring a Neisseria infection is >1000-fold that of healthy controls, with an absolute risk up to 0.5% per year.48,49 For that reason, I recommend penicillin prophylaxis (500 mg twice a day) in addition to vaccination for all patients less than 45 years old. Ravulizumab is my treatment of choice for patients with PNH requiring indefinite therapy given its more convenient dosing, lower cost, and more reliable C5 blockade.
Next-generation complement inhibitors for PNH
Eculizumab and ravulizumab prevent intravascular hemolysis and prevent thrombosis (the leading cause of death) in the natural history of PNH; however, there is room for improvement. More than 50% of patients with PNH on C5 inhibitors have mild to moderate symptoms from PNH, and up to 20% still need occasional transfusions. The most common reason for continued anemia is extravascular hemolysis (patient 2). New complement inhibitors50 are being developed to treat PNH, and several may become FDA approved in the next year or two. Pegcetacoplan is a C3 inhibitor that is administered subcutaneously, twice weekly, and is capable of blocking both intravascular and extravascular hemolysis. The drug is being compared head-to-head with eculizumab in a phase 3 clinical trial. Danicopan is another promising drug that blocks the alternative pathway of complement by inhibiting complement factor D.51 Danicopan is administered orally, raises hemoglobin levels, and eliminates the need for blood transfusion in transfusion-dependent patients with PNH on eculizumab.
Acknowledgments
This work was supported, in part, by National Institutes of Health, National Heart, Lung, and Blood Institute grant R01HL133113. Figure 1 was made with the assistance of BioRender.
Authorship
Contribution: R.A.B. wrote the paper.
Conflict-of-interest disclosure: R.A.B. reports grants and other from Alexion outside the submitted work.
Correspondence: Robert A. Brodsky, Division of Hematology, Johns Hopkins Medicine, Ross Research Bldg, Rm 1025, 720 Rutland Ave, Baltimore, MD 21205-2196; e-mail: brodsro@jhmi.edu.
REFERENCES
- 1.Hill A, DeZern AE, Kinoshita T, Brodsky RA. Paroxysmal nocturnal haemoglobinuria. Nat Rev Dis Primers. 2017;3(1):17028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luzzatto L. PNH phenotypes and their genesis. Br J Haematol. 2020;189(5):802-805. [DOI] [PubMed] [Google Scholar]
- 3.Kinoshita T, Fujita M. Biosynthesis of GPI-anchored proteins: special emphasis on GPI lipid remodeling. J Lipid Res. 2016;57(1):6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luzzatto L, Bessler M, Rotoli B. Somatic mutations in paroxysmal nocturnal hemoglobinuria: a blessing in disguise? Cell. 1997;88(1):1-4. [DOI] [PubMed] [Google Scholar]
- 5.Yuan X, Braunstein EM, Ye Z, et al. Generation of glycosylphosphatidylinositol anchor protein-deficient blood cells from human induced pluripotent stem cells. Stem Cells Transl Med. 2013;2(11):819-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeZern AE, Symons HJ, Resar LS, Borowitz MJ, Armanios MY, Brodsky RA. Detection of paroxysmal nocturnal hemoglobinuria clones to exclude inherited bone marrow failure syndromes. Eur J Haematol. 2014;92(6):467-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen W, Clemente MJ, Hosono N, et al. Deep sequencing reveals stepwise mutation acquisition in paroxysmal nocturnal hemoglobinuria. J Clin Invest. 2014;124(10):4529-4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fraiman YS, Cuka N, Batista D, Vuica-Ross M, Moliterno AR. Development of paroxysmal nocturnal hemoglobinuria in CALR-positive myeloproliferative neoplasm. J Blood Med. 2016;7:107-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inoue N, Izui-Sarumaru T, Murakami Y, et al. Molecular basis of clonal expansion of hematopoiesis in 2 patients with paroxysmal nocturnal hemoglobinuria (PNH). Blood. 2006;108(13):4232-4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hillmen P, Young NS, Schubert J, et al. The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria. N Engl J Med. 2006;355(12):1233-1243. [DOI] [PubMed] [Google Scholar]
- 11.Brodsky RA, Young NS, Antonioli E, et al. Multicenter phase 3 study of the complement inhibitor eculizumab for the treatment of patients with paroxysmal nocturnal hemoglobinuria. Blood. 2008;111(4):1840-1847. [DOI] [PubMed] [Google Scholar]
- 12.Lee JW, Sicre de Fontbrune F, Wong Lee Lee L, et al. Ravulizumab (ALXN1210) vs eculizumab in adult patients with PNH naive to complement inhibitors: the 301 study. Blood. 2019;133(6):530-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kulasekararaj AG, Hill A, Rottinghaus ST, et al. Ravulizumab (ALXN1210) vs eculizumab in C5-inhibitor-experienced adult patients with PNH: the 302 study. Blood. 2019;133(6):540-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Socié G, Mary JY, de Gramont A, et al. ; French Society of Haematology . Paroxysmal nocturnal haemoglobinuria: long-term follow-up and prognostic factors. Lancet. 1996;348(9027):573-577. [DOI] [PubMed] [Google Scholar]
- 15.Moyo VM, Mukhina GL, Garrett ES, Brodsky RA. Natural history of paroxysmal nocturnal haemoglobinuria using modern diagnostic assays. Br J Haematol. 2004;126(1):133-138. [DOI] [PubMed] [Google Scholar]
- 16.Hillmen P, Lewis SM, Bessler M, Luzzatto L, Dacie JV. Natural history of paroxysmal nocturnal hemoglobinuria. N Engl J Med. 1995;333(19):1253-1258. [DOI] [PubMed] [Google Scholar]
- 17.Rother RP, Rollins SA, Mojcik CF, Brodsky RA, Bell L. Discovery and development of the complement inhibitor eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria [published correction in Nat Biotechnol. 2007;25:1488]. Nat Biotechnol. 2007;25(11):1256-1264. [DOI] [PubMed] [Google Scholar]
- 18.Hillmen P, Muus P, Röth A, et al. Long-term safety and efficacy of sustained eculizumab treatment in patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol. 2013;162(1):62-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelly RJ, Hill A, Arnold LM, et al. Long-term treatment with eculizumab in paroxysmal nocturnal hemoglobinuria: sustained efficacy and improved survival. Blood. 2011;117(25):6786-6792. [DOI] [PubMed] [Google Scholar]
- 20.Hill A, Kelly RJ, Hillmen P. Thrombosis in paroxysmal nocturnal hemoglobinuria. Blood. 2013;121(25):4985-4996, quiz 5105. [DOI] [PubMed] [Google Scholar]
- 21.Brodsky RA, Mukhina GL, Li S, et al. Improved detection and characterization of paroxysmal nocturnal hemoglobinuria using fluorescent aerolysin. Am J Clin Pathol. 2000;114(3):459-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borowitz MJ, Craig FE, Digiuseppe JA, et al. ; Clinical Cytometry Society . Guidelines for the diagnosis and monitoring of paroxysmal nocturnal hemoglobinuria and related disorders by flow cytometry. Cytometry B Clin Cytom. 2010;78(4):211-230. [DOI] [PubMed] [Google Scholar]
- 23.de Latour RP, Mary JY, Salanoubat C, et al. ; French Association of Young Hematologists . Paroxysmal nocturnal hemoglobinuria: natural history of disease subcategories. Blood. 2008;112(8):3099-3106. [DOI] [PubMed] [Google Scholar]
- 24.Hillmen P, Muus P, Dührsen U, et al. Effect of the complement inhibitor eculizumab on thromboembolism in patients with paroxysmal nocturnal hemoglobinuria. Blood. 2007;110(12):4123-4128. [DOI] [PubMed] [Google Scholar]
- 25.Ritis K, Doumas M, Mastellos D, et al. A novel C5a receptor-tissue factor cross-talk in neutrophils links innate immunity to coagulation pathways. J Immunol. 2006;177(7):4794-4802. [DOI] [PubMed] [Google Scholar]
- 26.Gavriilaki E, Brodsky RA. Complementopathies and precision medicine. J Clin Invest. 2020;130(5):2152-2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foley JH, Walton BL, Aleman MM, et al. Complement activation in arterial and venous thrombosis is mediated by plasmin. EBioMedicine. 2016;5:175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Conway EM. Complement-coagulation connections. Blood Coagul Fibrinolysis. 2018;29(3):243-251. [DOI] [PubMed] [Google Scholar]
- 29.Brodsky RA, Peffault de Latour R, Rottinghaus ST, et al. Characterization of breakthrough hemolysis events observed in the phase 3 randomized studies of ravulizumab versus eculizumab in adults with paroxysmal nocturnal hemoglobinuria. Haematologica. 2020;106(1):230-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brodsky RA. How I treat paroxysmal nocturnal hemoglobinuria. Blood. 2009;113(26):6522-6527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emadi A, Brodsky RA. Successful discontinuation of anticoagulation following eculizumab administration in paroxysmal nocturnal hemoglobinuria. Am J Hematol. 2009;84(10):699-701. [DOI] [PubMed] [Google Scholar]
- 32.Bunn HF, Nathan DG, Dover GJ, et al. Pulmonary hypertension and nitric oxide depletion in sickle cell disease. Blood. 2010;116(5):687-692. [DOI] [PubMed] [Google Scholar]
- 33.Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA. 2005;293(13):1653-1662. [DOI] [PubMed] [Google Scholar]
- 34.Peffault de Latour R, Brodsky RA, Ortiz S, et al. Pharmacokinetic and pharmacodynamic effects of ravulizumab and eculizumab on complement component 5 in adults with paroxysmal nocturnal haemoglobinuria: results of two phase 3 randomised, multicentre studies. Br J Haematol. 2020;191(3):476-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harder MJ, Kuhn N, Schrezenmeier H, et al. Incomplete inhibition by eculizumab: mechanistic evidence for residual C5 activity during strong complement activation. Blood. 2017;129(8):970-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rother RP, Rollins SA, Mojcik CF, Brodsky RA, Bell L. Discovery and development of the complement inhibitor eculizumab for the treatment of paroxysmal nocturnal hemoglobinuria [published correction in Nat Biotechnol. 2007;25:1488]. Nat Biotechnol. 2007;25(11):1256-1264. [DOI] [PubMed] [Google Scholar]
- 37.Risitano AM, Notaro R, Marando L, et al. Complement fraction 3 binding on erythrocytes as additional mechanism of disease in paroxysmal nocturnal hemoglobinuria patients treated by eculizumab. Blood. 2009;113(17):4094-4100. [DOI] [PubMed] [Google Scholar]
- 38.Derzsy Z, Prohászka Z, Rigó J Jr., Füst G, Molvarec A. Activation of the complement system in normal pregnancy and preeclampsia. Mol Immunol. 2010;47(7-8):1500-1506. [DOI] [PubMed] [Google Scholar]
- 39.Girardi G. Complement activation, a threat to pregnancy. Semin Immunopathol. 2018;40(1):103-111. [DOI] [PubMed] [Google Scholar]
- 40.Fieni S, Bonfanti L, Gramellini D, Benassi L, Delsignore R. Clinical management of paroxysmal nocturnal hemoglobinuria in pregnancy: a case report and updated review. Obstet Gynecol Surv. 2006;61(9):593-601. [DOI] [PubMed] [Google Scholar]
- 41.Ray JG, Burows RF, Ginsberg JS, Burrows EA. Paroxysmal nocturnal hemoglobinuria and the risk of venous thrombosis: review and recommendations for management of the pregnant and nonpregnant patient. Haemostasis. 2000;30(3):103-117. [DOI] [PubMed] [Google Scholar]
- 42.Kelly RJ, Höchsmann B, Szer J, et al. Eculizumab in pregnant patients with paroxysmal nocturnal hemoglobinuria. N Engl J Med. 2015;373(11):1032-1039. [DOI] [PubMed] [Google Scholar]
- 43.Hill A, Rother RP, Hillmen P. Improvement in the symptoms of smooth muscle dystonia during eculizumab therapy in paroxysmal nocturnal hemoglobinuria. Haematologica. 2005;90(suppl 12):ECR40. [PubMed] [Google Scholar]
- 44.DeZern AE, Jones RJ, Brodsky RA. Eculizumab bridging before bone marrow transplant for marrow failure disorders is safe and does not limit engraftment. Biol Blood Marrow Transplant. 2018;24(12):e26-e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DeZern AE, Zahurak ML, Symons HJ, et al. Haploidentical BMT for severe aplastic anemia with intensive GVHD prophylaxis including posttransplant cyclophosphamide. Blood Adv. 2020;4(8):1770-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peffault de Latour R, Schrezenmeier H, Bacigalupo A, et al. Allogeneic stem cell transplantation in paroxysmal nocturnal hemoglobinuria. Haematologica. 2012;97(11):1666-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Densen P. Complement deficiencies and meningococcal disease. Clin Exp Immunol. 1991;86(suppl 1):57-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Konar M, Granoff DM. Eculizumab treatment and impaired opsonophagocytic killing of meningococci by whole blood from immunized adults. Blood. 2017;130(7):891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Socié G, Caby-Tosi MP, Marantz JL, et al. Eculizumab in paroxysmal nocturnal haemoglobinuria and atypical haemolytic uraemic syndrome: 10-year pharmacovigilance analysis. Br J Haematol. 2019;185(2):297-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Risitano AM, Marotta S, Ricci P, et al. Anti-complement treatment for paroxysmal nocturnal hemoglobinuria: time for proximal complement inhibition? A position paper from the SAAWP of the EBMT. Front Immunol. 2019;10:1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yuan X, Gavriilaki E, Thanassi JA, et al. Small-molecule factor D inhibitors selectively block the alternative pathway of complement in paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome. Haematologica. 2017;102(3):466-475. [DOI] [PMC free article] [PubMed] [Google Scholar]