Abstract
Background
Overdose education and naloxone distribution programmes are known to reduce opioid-related deaths. A state-wide naloxone distribution effort of 8250 rescue kits was undertaken by government, community and university partners in West Virginia in 2016–2017. The purpose of this study was to discern the barriers, facilitators and lesson learnt from implementing this endeavour in a rural state with the highest opioid overdose fatality rate in the US.
Methods
Structured interviews (n=26) were conducted among both internal and external stakeholders. Those who participated were >18 years of age and were the lead representative from agencies that either received naloxone (ie, external stakeholders) or helped implement the distribution (ie, internal stakeholders). The interviews followed standardised scripts and lasted approximately 40 min. Sessions were audio-recorded and transcribed. Qualitative content analysis was performed by two researchers to determine themes surrounding facilitators or barriers to programme implementation.
Results
The primary facilitators reported by stakeholders included collaborative partnerships, ease of participating in the programme, being established in prevention efforts, demand for naloxone and the need for personal protection from overdose. The primary barriers identified by stakeholders included bureaucracy/ policy/procedures of their organisation or agency, stigma, logistical or planning issues, problems with reporting, lack of communication post distribution and sustainability. Numerous lessons were learnt.
Conclusions
Based on the implementation of the programme in 87 organisations, including law enforcement and fire departments, the impact of facilitators outweighed that of barriers. These findings may inform others planning to conduct a similar, large-scale project.
INTRODUCTION
Naloxone (also known as Narcan) is an opioid antagonist which can quickly restore normal respiration to a person whose breathing has slowed or stopped as a result of overdosing on heroin or prescription opioid pain medications.1,2 Overdose education and naloxone distribution (OEND) programmes focus on getting naloxone into the hands of laypersons (eg, non-medical professionals), especially high-risk individuals and/or their acquaintances who use opioids. These programmes initially appeared in the 1990s as ‘take-home naloxone’ efforts, designed to address an increase in heroin overdoses in European and US cities.3 People who were using heroin were recruited, trained and provided with kits that contained naloxone. These programmes effectively reduced overdose deaths and have been widely implemented as an evidence-based public health strategy.4,5 In 2010, only 188 OEND programmes existed in the US.6 By 2014, 644 OEND programmes were recognised, which provided naloxone to >152 000 individuals and resulted in >26 000 overdose reversals.6 However, some states, such as West Virginia, which has the highest opioid overdose fatality rate in the nation, did not have any OEND programmes in effect in 2014.6,7 Thus, there was an impetus to implement OEND programmes in this rural, medically underserved, Appalachian state.
Numerous studies describing the implementation and/or evaluation of OEND programmes are present in the extant literature; most studies focus on the quantitative aspects of implementation/evaluation, such as the demographics of clients served, number of kits dispensed, number of naloxone prescriptions written, number of overdose reversals or deaths, and so on.8–18 Few US (n=4) or international studies (n=3) have focused on qualitative facets such as facilitators and barriers to OEND programme implementation.19–25 Existing US studies have examined the facilitators and barriers to OEND programme implementation mainly in healthcare settings such as pharmacies, in an individual emergency department, in an individual clinic and in addiction treatment programmes located in an urbanised area of one state.19,20,23,24 The facilitators and barriers to implementing a large-scale, state-wide distribution, encompassing different types of organisations, including non-emergency medical service (EMS) first responders (ie, police, fire departments), correction facilities, schools and day report centres, were unknown. In rural states such as West Virginia, non-EMS first responders often encounter overdosed individuals or may arrive on-scene much quicker than EMS personnel and thus can play a critical role in overdose reversals. Among the extant studies, common facilitators of implementing OEND programmes are strong community partnerships, the need for overdose prevention, the need for education (for the public, employees, healthcare providers), support for naloxone and being able to give naloxone directly to individuals at high risk of overdose.19–25 Common barriers are costs associated with purchasing the drug, lack of reimbursement by insurers, existing policy/legal barriers, logistics of dispensing the drug, patient/client/employee concerns, stigma about drug use and/or rescue medications, and complex reporting requirements associated with reversals.19–25
Knowing the facilitators and barriers to OEND implementation in healthcare settings, combined with the need to distribute naloxone to individuals at risk of overdose, a state-wide naloxone distribution effort was undertaken by government, community and university partners in West Virginia in 2016–2017. The goal was to train and distribute naloxone to non-EMS first responders (eg, law enforcement and fire departments) as well as existing and incipient OEND programmes state-wide. Because this large-scale approach had not been attempted previously in US studies, a process evaluation was conducted during implementation to facilitate quality improvement, identify factors that may influence programme impact and enable translation to other states. An analysis of qualitative data generated from stakeholder interviews was conducted to identify facilitators, barriers and lessons learnt during the launch of the state-wide programme, including the ability of internal partners to give naloxone to local OEND programmes and the ability of these programmes to receive the product, which are highlighted within.
Overview of the naloxone distribution effort
An overview of the naloxone distribution effort is described in detail in the online supplementary appendix. Ultimately, 8250 kits were assembled and distributed to 87 different programmes representing 38 of West Virginia’s 55 counties between February and June 2017. Before the kits were distributed to an organisation, it had to provide evidence that their staff were trained and that it had a standing order from a licensed physician because naloxone is considered a prescription drug in West Virginia. Some OEND programmes that were identified did not ultimately receive naloxone kits because they failed to respond to communications (email and/or phone calls) about the project.
METHODS
Study design
To learn about potential facilitators and barriers, structured interviews were conducted either inperson or via telephone using standardised and pilot-tested scripts.
Interview scripts
Two separate interview scripts were created for the evaluation: one for external partners and one for internal partners. External partners consisted of individuals from organisations that received naloxone rescue kits. Internal partners included individuals who had been directly involved in the design, planning, purchasing, training, implementation and evaluation of the project, as well as individuals from organisations that participated in storing the naloxone or assembling/delivering the naloxone kits. The questions for external partners focused on the process of the naloxone programme from the first point of contact to the effects of the programme after it concluded. The questions for the internal stakeholders focused on all aspects of the project and included questions on ordering, planning, creating the needs assessment survey, conducting trainings, kit assembly and kit delivery. The interview scripts contained open-ended questions to allow for probing and follow-up questions. To ensure validity, interviewers asked for clarification during the interview if they felt the interviewees’ responses were vague or unclear (ie, this served as a ‘member check’).26 Both interview scripts were pilot-tested prior to administration.
Participant eligibility and recruitment
The sampling frame consisted of lead representatives, ≥18 years of age, who were considered an external or internal partner. For external partners, the sampling frame was stratified by organisation type. Representatives from each organisation type were randomly selected, then called on the phone and/or emailed. After three attempts and there was no response, another organisation from that type was selected and contacted. This was done to ensure that all organisational types were represented in the analysis. When contact was established, convenient interview date, time and mechanism (ie, inperson or via telephone) were determined. Participation in the interview was voluntary and informed consent and permission were obtained from all participants.
Data collection for structured interviews
Because several individuals conducted the interviews, all interviewers were trained on proper interview techniques by more experienced study personnel. All interviews were audio-recorded, lasted ~40 min in duration, and were conducted in a private area to ensure clear recording and confidentiality. The audio recordings were transcribed verbatim by a professional transcription service. To ensure accurate transcription, the audio recordings were compared with the transcripts by study personnel; if discrepancies were identified, the transcripts were corrected prior to data analysis.
Non-responsive organisations
Not all OEND programmes that were identified and sent a needs assessment survey participated in the programme. A random sample of lead representatives from these non-participating agencies (n=5) were contacted via telephone. This was done to discern if any additional barriers to participation existed and to determine if there were fundamental differences between those who did and did not participate.
Data analysis
The data were analysed using content analysis to identify themes among reported facilitators of and barriers to programme participation and implementation.27 Two researchers partook in the analysis process. The analysis began with both researchers thoroughly reading and rereading the transcripts. Each researcher independently developed code words/phrases to label thoughts or concepts that emerged from the transcripts. The researchers met and compared their initial coding schemes. A consensus was then reached on how thoughts or concepts should be coded.28 These codes were then operationally defined and documented in a data dictionary within the software.28,29 After all transcripts were coded, the researchers sorted and collapsed the operationally defined codes into broader, more encompassing themes or subthemes. A thematic map was constructed to direct this process.30 Inter-rater reliability was evaluated using Cohen’s kappa statistic. It was determined a priori that if a minimum kappa of 0.8 was not met, the coding process would occur iteratively until that value was reached (k=0.92).31 After core themes were determined, the transcripts were reread to ensure that these themes accurately depicted the data. Data management, including searching, coding and categorisation of the text from transcripts, was done with NVivo V.12.
Patient and public involvement
It was not possible to involve the patients or the public in the design, or conduct, or reporting or dissemination plans of our research.
RESULTS
A total of 26 structured interviews were conducted.
Internal partners
Six internal partners were interviewed (response rate=100%).
Facilitators
For internal partners, the primary facilitator was collaborative partnerships (figure 1). Partner organisations included those both internally and those located throughout the state that worked to move the project past the initial stages quickly and efficiently. These partners included individuals from administration, procurement, prevention organisations in the state and supply vendors. Some local organisations volunteered and helped assemble the thousands of naloxone kits.
Figure 1.
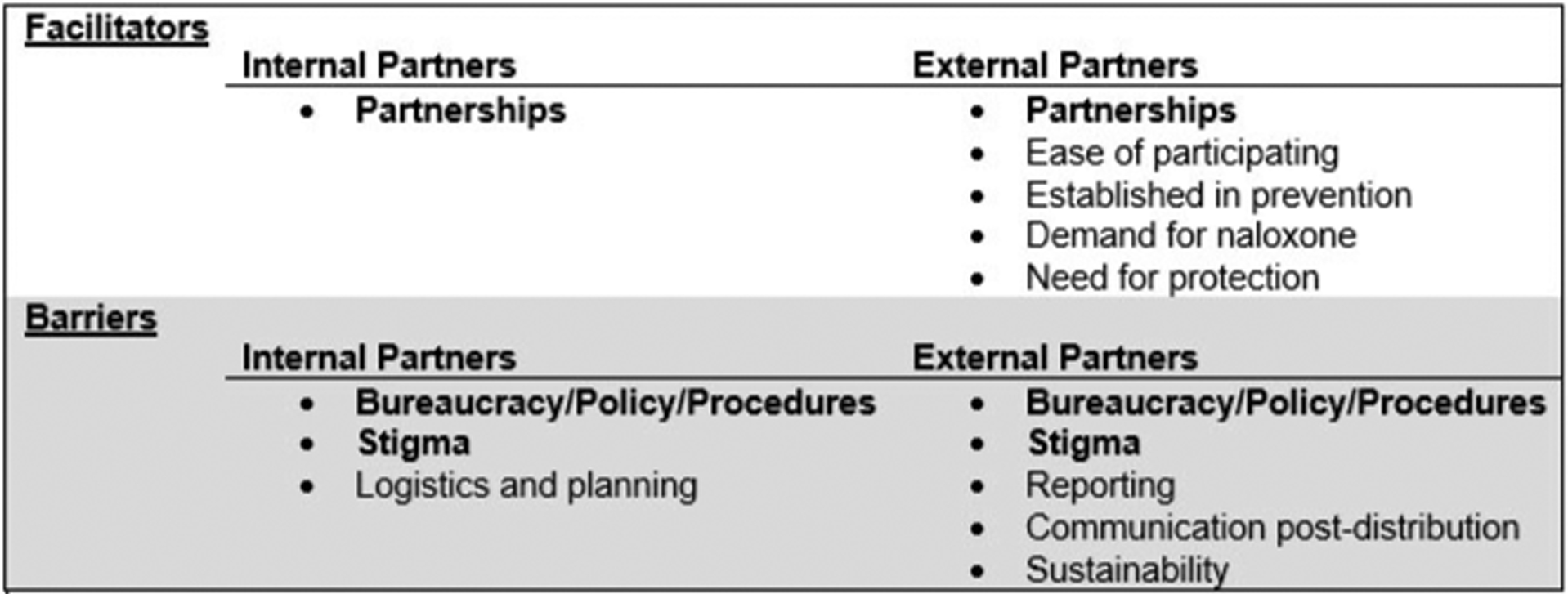
Summary of the facilitators and barriers experienced by individuals involved in the first state-wide naloxone distribution conducted in West Virginia in 2016–2017. Themes in bold font are shared between both internal and external partners.
Barriers
There were three overarching barriers to the distribution effort discussed among internal partners. These included (1) logistics and planning, (2) bureaucracy/policies/procedures, and (3) stigma. These are discussed in detail in the following sections.
Logistics and planning
Logistics and planning were probably the most prevailing barriers to programme implementation. During the interviews five major subthemes emerged, including tight deadlines, storage space requirements, identification and assessment of organisations, training needs, and sustainability of naloxone distribution.
When the funding and approval for the project were received from partnering government agencies, the turnaround time to plan and spend the funding before expiration was a major driving force of the project. All kit materials needed to be ordered, assembled and distributed quickly especially given the naloxone’s shelf-life of 21 months. As one participant explained in detail:
There were about six weeks in which we had to do all the research and specifications. Contact the vendors. Negotiate the best prices we could. Make sure we bought everything we needed. Make sure we could get it all delivered before the deadline. It was really a challenge. It was kind of a cart before the horse too. The best approach would have been to identify all the programs in the state and those organizations that wanted to do naloxone distribution or carry programs and had a better idea of who it could be distributed to before we purchased the naloxone.
In addition to coordinating all the materials, finding a proper location to store the substantial amount of supplies (boxes, paper, tape, labels, plastic cases and so on) was a logistical quandary. Consequently, an off-premises storage unit had to be rented to accommodate these materials. Thus, there were unanticipated costs and logistics to navigate.
Given the short turnaround time to plan the distribution, identifying organisations and assessing how much naloxone each needed became a logistical barrier, since there was no master list of agencies available. Additionally, a needs assessment survey had to be created very quickly in order to assess the population that the organisations served, their current demand and how much naloxone they thought they needed. The needs assessment survey was especially challenging from the design aspect as different types of organisations were involved and it had to be applicable to all organisations involved (eg, law enforcement, fire departments, correction facilities, schools, day report centres, harm reduction programmes and so on).
After organisations were identified and naloxone needs were determined, the research team had to assess if the organisations needed training on naloxone administration. Most organisations needed to receive train-the-trainer sessions for their programme staff, given that most of the organisations identified were take-home naloxone programmes. One partnering agency strived to provide trainings to organisations as needed. This proved to be a barrier due to the geography of the state. Thus, mass trainings were conducted when possible. Coordinating with organisations and other agencies made this difficult to do in such a short amount of time.
Another issue that emerged with the organisations that received kits was that some did not have an actual plan for distributing kits. As a result, some organisations were not sure what to do with the kits, or how to promote in their communities that kits were available. Some organisations ran out of kits quickly. Other organisations had to scramble to dispense kits before the drug expired. Some were not sure what to do with expired kits.
Bureaucracy/policies/procedures
In addition to the compressed timeframe for logistics and planning, bureaucracy/policy/procedures of their organisations were a major barrier to the project. This was mentioned by virtually all internal interviewees. The overall speed at which contracts were signed and funding provided was unanimously viewed as extremely slow.
Stigma
The final perceived barrier was stigma associated with addiction, opioids, and naloxone specifically. One individual explained:
I attribute a lot of the low response in West Virginia to the continuing stigma and bias against folks who, for whatever reason, have become opioid use dependent. That’s one thing that I think is a great challenge to statewide naloxone distribution: in the hills and hollows of West Virginia there’s a resistance in practically every quarter…If we could deal with that and reduce the amount of bias and stigma across West Virginia, future programs would go a lot better.
External partners
Fifteen interviews were conducted with external partners (ie, 17% of organisations that received naloxone). The response rate for external partners was 60%.
Facilitators
During interviews with external partners, several facilitators to participation were mentioned and included: (1) ease of participation, (2) collaborative partnerships, (3) establishment in prevention, (4) demand for naloxone and cost, and (5) need for protection/safety against overdose (figure 1).
Ease of participation
Most participants thought that the state-wide distribution was easy to participate in. Participants generally thought that the needs assessment survey was simple and straightforward and did not take a long time to complete. Coordination of the delivery and shipping of naloxone was straightforward as well. Several organisations picked the kits up directly or had naloxone personally delivered by study staff. Project documentation (ie, signing of forms/receipt) was completed on-site. The ease of the process was a major benefit. As one participant explained:
I really thought it was straight-forward and simple. I’m not a big paper guy myself. It was very simple for me to get it moving forward. I didn’t have to reach out and get anybody to help me, so very user friendly.
Collaborative partnerships
One of the major facilitators for external partners was the amount of collaboration that already existed throughout the state. Many of the organisations had already established working relationships. As one individual explained:
…we are always definitely in contact with other places trying to better every program as much as we can; helping each other out.
Establishment in prevention
In addition to having those relationships with other organisations, many of the recipient organisations were already established in prevention, so it was easy for them to incorporate naloxone distribution as part of a harm reduction programme.
Demand for naloxone
Another helpful factor was the high demand for naloxone, training and education due to the severity of the epidemic in West Virginia. As one participant described:
I think this project has great value because it meets a need and it’s critically important. We’re losing a generation of people to overdose death, and that’s just not acceptable. So this is certainly, it’s not a cure, it is not a cure for the drug abuse problem and the addiction overdose issue. But it certainly is a tool in the toolkit, so it’s valuable.
All external partners acknowledged that receiving naloxone free of charge was paramount. Not only is the medication expensive, it is also hard to find in more rural areas of the state. One participant explained:
Well, probably the biggest hassle part that we have is the actual product, not the devices, but the actual product itself. Getting it to the pharmacy and paying for it and the cost, because the costs have doubled in the last three years.
Need for protection and safety against overdose
An interesting facilitator that was brought up in the interviews many times was that having the naloxone and training fulfilled a need for personal protection and safety among public safety officials such as police officers, healthcare providers and fire personnel. This was considered especially important given the rise of fentanyl and fentanyl derivatives that are often mixed with other opioids. Providers and responders can be exposed to these powerful drugs while trying to save others. One public safety official explained:
I would like to see, on a state and national level, that this process be pushed out to all public safety, because it is so serious and there’s such a high probability of exposure, counter exposure and people running into these overdoses just as the normal course of their duties.
While public safety officials had the highest concern with personal protection, community businesses also saw the value of having naloxone on hand in case an overdose occurred on their property. Many businesses have been contacting prevention agencies and harm reduction programmes in order to receive training and/or naloxone.
Barriers
Numerous barriers were mentioned during the interviews with external partners and included (1) stigma, (2) difficulties with reporting, (3) bureaucracy/policies/procedures of their organisations, (4) communication after distribution, and (5) no sustainability.
Stigma
One of the major barriers brought up by external partners was stigma surrounding naloxone and drug use on all levels in their communities, including the general public, first responders, healthcare providers and local government officials. Despite this, many organisations implied that community members were grateful to have naloxone available for those who needed it and that negative attitudes towards addiction are improving. As one individual stated:
Well, that’s one thing we’ve tried to instruct, we said it’s not our job to judge these people, it’s our job to save them. If they’re making the wrong choices, that’s their…I mean, that’s on them, but…your job’s not to stand there and judge them, your job’s to save them.
Difficulties with reporting
Due to the stigma surrounding addiction, there were difficulties with collection of information about naloxone administration and overdose reversals. Many users and their friends and family wanted to remain anonymous due to fear of repercussions. While it has been difficult to get the naloxone administration cards returned, some organisations found ways to collect this important information. Multiple organisations worked diligently to establish trust between them and individuals who received the naloxone kits. Some agencies fill out the naloxone administration cards with clients not only for support but also to assure anonymity. An individual explained:
And I think you have to, when you’re dealing with injection drug users, you have to have that anonymity piece, or they’re not going to participate.
Bureaucracy/policies/procedures
While several community organisations have been working directly with drug users, there were still some difficulties in getting the proper support needed to distribute naloxone on a larger scale. Several participants spoke about issues with finding physicians to fulfil standing orders, as well as a general sense of confusion on where to start in finding one. Many were unsure about the training and reporting requirements, how to properly interpret state laws relating to naloxone or opioids, or even how to create policies relating to naloxone within their specific organisation. One individual gave an example:
Sometimes you gotta jump through quite a lot to get support, assistance, and financial supplies from state of West Virginia. That is understandable, because there is the restraints, they have on it.
Communication after distribution
There were also some barriers regarding how an agency that received naloxone was to proceed after the delivery of the medication. Many organisations stated that they would have liked follow-up instructions on what to do with expired kits and how to replenish kits when the organisation ran out. Several also said that they would like some way to show that their organisation members were trained in naloxone administration and also that the kits needed more information in them regarding what a layperson should do after naloxone is administered and follow-up information on addiction resources.
Sustainability
Virtually all individuals interviewed discussed sustainability. They were concerned about finding and obtaining naloxone after the distribution.
Non-responsive organisations
There were few barriers discussed during the interviews conducted among non-responsive organisations. The most frequent barrier mentioned was oversight (eg, lost communication).
DISCUSSION
The findings from this analysis showed that numerous facilitators and barriers to implementing a state-wide naloxone distribution in West Virginia existed. Collaborative partnership between organisations was a critical factor in implementing the distribution for both internal and external stakeholders. Many agencies had to work together in order to carry out all aspects of the distribution. The demand for naloxone due to its high cost and often limited availability also helped facilitate the distribution to external partners. These findings were similar to other studies which have qualitatively evaluated naloxone distribution efforts in healthcare settings in other states or countries.19–25 However, one facilitator of this project not previously discussed in the literature was the need for protection and safety against overdose (ie, the need to protect the public and non-EMS first responders in case of exposure). This facilitator was likely driven by the continual rise of fentanyl and fentanyl derivatives that are mixed with other opioids in the state. Also, due to West Virginia’s extreme rurality, many non-EMS first responders may come in contact with overdose victims before EMS arrives. While this was a clear facilitator in West Virginia, worker or personal safety could potentially be a barrier for others implementing a similar effort.
As for barriers, bureaucracy/policies/procedures and stigma were identified as common dilemmas for stakeholders. Both state laws and organisational policies appeared to complicate numerous facets of the distribution; common bureaucratic barriers mentioned were the need for a physician’s standing order and the laws regarding naloxone training and distribution. Moreover, while logistics and planning were problematic for internal partners, reporting requirements and sustainability were additional concerns for external partners. These findings were similar to previous studies conducted in healthcare settings in other states or countries as well.19–25 However, one barrier seen among external partners, which had not been identified previously in the literature, was the need for communication or technical assistance after the agency received naloxone. Many of the organisations that were less experienced in harm reduction were not sure what to do with the naloxone once they received it. Many did not have internal protocols on who to give the naloxone to or what data they needed to collect or maintain. Some took so much time trying to figure out these matters that their naloxone almost expired.
Thus, numerous lessons were learnt from this novel, large-scale project which involved numerous types of organisations. First, it is recommended that programme priorities, strategies and needs be determined first. Time should be taken to identify, prioritise and assess need among organisations, accomplish training objectives, and provide technical assistance to recipients. It is also recommended to consider procuring naloxone formulations that are tailored to the end user (eg, some lay individuals prefer nasal spray). Providing documentation to those who received training to dispense naloxone, such as a certification card, could be useful to clients and employees of agencies who received naloxone. Second, programmes of this magnitude require strong collaborative partnerships. Many organisations, especially newer programmes, need support after the distribution. It may be useful to have a ‘toolkit’ developed to assist them, which includes information such as advice on implementation, training and reporting requirements, naloxone vendor information, legal information, and so on. It may even be useful to connect agencies to one another. For example, some agencies that were not able to distribute their naloxone quickly were able to switch their kits out with other agencies that were distributing quickly to avoid the naloxone expiring. Third, organisations need assistance with data collection and reporting. Forms should be created for agencies to ensure consistent and more complete reporting. Also, it may be beneficial to have multiple modes of reporting available for agencies or clients to use. West Virginia uses mail-in naloxone reversal cards. Additional modes, such as cell phone applications, may encourage reporting. Fourth, many agencies were concerned about the sustainability of their naloxone distribution programmes; educating them on grant writing resources or available grants may be beneficial to sustainability. Lastly, there were numerous bureaucratic barriers encountered by recipients. Finding ways to make naloxone easier to obtain and distribute, such as having a state-wide standing order or making naloxone a non-prescription drug, could improve this.
Limitations
While the findings of this study are important, they are not without limitations. First, all information was self-reported by stakeholders and subject to reporting bias. It is possible that some individuals may or may not have chosen to discuss certain facilitators or barriers. Second, those who volunteered to participate in interviews may have been fundamentally different from those who did not. Third, four individuals performed the interviews. While interviewers were trained, it is possible that interview bias existed. Lastly, because of the geographical area, two modes were used to conduct the interviews (eg, inperson or via telephone), which could have impacted participants’ responses.
CONCLUSION
Through collaboration, 8250 naloxone rescue kits were successfully distributed to 87 organisations located in 38 of West Virginia’s 55 counties in 2016–2017. Numerous facilitators and barriers to the project implementation existed for stakeholders. The primary facilitator was collaborative partnerships, while the primary barriers were bureaucracy/policies/procedures and stigma regarding naloxone and drug use. Numerous lessons were learnt from this project which may inform others looking to replicate a similar large-scale effort.
Supplementary Material
What is already known on the subject.
Overdose education and naloxone distribution programmes reduce opioid overdose deaths.
Overdose education and naloxone distribution programmes have been increasing in the US.
Few studies have highlighted the facilitators and barriers to implementing these types of programmes.
What this study adds.
Numerous facilitators and barriers were experienced by internal and external stakeholders who participated in the first state-wide naloxone distribution programme.
Facilitators and barriers to implementation differed by stakeholder type.
Various lessons were learnt from this endeavour which could inform others planning to conduct a project of this magnitude.
Funding
TMR, AJA, HIL, SS and KKG all received support from the Centers for Disease Control and Prevention (grant R49 CE002109). All authors received support from the Centers for Disease Control and Prevention’s Prevention for States award (CDC-RFA-CE15-1501) and Substance Abuse and Mental Health Services Administration funding (B08T1010058).
Footnotes
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
Ethics approval Institutional review board approval was obtained for this project (protocol #1609265464) from West Virginia University.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available.
► Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/injuryprev-2020-043666).
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Naloxone, 2019. Available: https://www.samhsa.gov/medication-assisted-treatment/treatment/naloxone [Accessed 1 Dec 2019].
- 2.United States food and drug administration. The clinical use of naloxone, 2019. Available: https://www.fda.gov/downloads/Drugs/NewsEvents/UCM454748.Pdf [Accessed 1 Dec 2019].
- 3.McDonald R, Campbell ND, Strang J. Twenty years of take-home naloxone for the prevention of overdose deaths from heroin and other opioids-Conception and maturation. Drug Alcohol Depend 2017;178:176–87. [DOI] [PubMed] [Google Scholar]
- 4.McDonald R, Strang J. Are take-home naloxone programmes effective? systematic review utilizing application of the Bradford Hill criteria. Addiction 2016;111:1177–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Community-based opioid overdose prevention programs providing naloxone - United States, 2010. MMWR Morb Mortal Wkly Rep 2012;61:101–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Wheeler E, Jones TS, Gilbert MK, et al. Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014. MMWR Morb Mortal Wkly Rep 2015;64:631–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Diseas Control and Prevention. Data and statistics (WISQARS): fatal injury data, 2019. Available: https://www.cdc.gov/injury/wisqars/fatal.html [Accessed 1 Dec 2019].
- 8.Haegerich TM, Jones CM, Cote P-O, et al. Evidence for state, community and systems-level prevention strategies to address the opioid crisis. Drug Alcohol Depend 2019;204:107563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haegerich TM, Paulozzi LJ, Manns BJ, et al. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend 2014;145:34–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bennett AS, Bell A, Doe-Simkins M, et al. From Peers to lay Bystanders: findings from a decade of naloxone distribution in Pittsburgh, PA. J Psychoactive Drugs 2018;50:240–6. [DOI] [PubMed] [Google Scholar]
- 11.Bozat-Emre S, Marshall SG, Zhong C, et al. At-a-glance - Lessons learned from launching the Manitoba Take-Home Naloxone Program. Health Promot Chronic Dis Prev Can 2018;38:252–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bounthavong M, Devine EB, Christopher MLD, et al. Implementation evaluation of academic detailing on naloxone prescribing trends at the United States Veterans health administration. Health Serv Res 2019;54:1055–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chronister KJ, Lintzeris N, Jackson A, et al. Findings and lessons learnt from implementing Australia’s first health service based take-home naloxone program. Drug Alcohol Rev 2018;37:464–71. [DOI] [PubMed] [Google Scholar]
- 14.Gunn AH, Smothers ZPW, Schramm-Sapyta N, et al. The emergency department as an opportunity for naloxone distribution. West J Emerg Med 2018;19:1036–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panther SG, Bray BS, White JR. The implementation of a naloxone rescue program in university students. J Am Pharm Assoc 2017;57:S107–12. [DOI] [PubMed] [Google Scholar]
- 16.Pearce LA, Mathany L, Rothon D, et al. An evaluation of take home naloxone program implementation in British Columbian correctional facilities. Int J Prison Health 2019;15:46–57. [DOI] [PubMed] [Google Scholar]
- 17.Lambdin BH, Zibbell J, Wheeler E, et al. Identifying gaps in the implementation of naloxone programs for laypersons in the United States. Int J Drug Policy 2018;52:52–5. [DOI] [PubMed] [Google Scholar]
- 18.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakhireva LN, Bautista A, Cano S, et al. Barriers and facilitators to dispensing of intranasal naloxone by pharmacists. Subst Abus 2018;39:331–41. [DOI] [PubMed] [Google Scholar]
- 20.Drainoni M-L, Koppelman EA, Feldman JA, et al. Why is it so hard to implement change? A qualitative examination of barriers and facilitators to distribution of naloxone for overdose prevention in a safety net environment. BMC Res Notes 2016;9:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dr. Freeman LK, Bourque S, Etches N, et al. Alberta’s provincial take-home naloxone program: A multi-sectoral and multi-jurisdictional response to overdose. Can J Public Health 2017;108:398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leece PN, Hopkins S, Marshall C, et al. Development and implementation of an opioid overdose prevention and response program in Toronto, Ontario. Can J Public Health 2013;104:e200–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winstanley EL, Clark A, Feinberg J, et al. Barriers to implementation of opioid overdose prevention programs in Ohio. Subst Abus 2016;37:42–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilder CM, Brason FW, Clark AK, et al. Development and implementation of an opioid overdose prevention program within a preexisting substance use disorders treatment center. J Addict Med 2014;8:164–9. [DOI] [PubMed] [Google Scholar]
- 25.Matheson C, Pflanz-Sinclair C, Aucott L, et al. Reducing drug related deaths: a pre-implementation assessment of knowledge, barriers and enablers for naloxone distribution through general practice. BMC Fam Pract 2014;15:12–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birt L, Scott S, Cavers D, et al. Member checking. Qual Health Res 2016;26:1802–11. [DOI] [PubMed] [Google Scholar]
- 27.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- 28.Strauss A, Corbin J. Grounded theory methodology. In: Denzin NK, Lincoln YS, eds. Handbook of qualitative research. Thousand Oaks, CA: SAGE, 1994: 273–85. [Google Scholar]
- 29.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007;42:1758–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 31.Cohen J Statistical power analysis for the behavioral sciences. New York, NY: Academic Press, 1988: 1–41. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


