Abstract
Objectives. To estimate total life expectancy (TLE), disability-free life expectancy (DFLE), and disabled life expectancy (DLE) by US state for women and men aged 25 to 89 years and examine the cross-state patterns.
Methods. We used data from the 2013–2017 American Community Survey and the 2017 US Mortality Database to calculate state-specific TLE, DFLE, and DLE by gender for US adults and hypothetical worst- and best-case scenarios.
Results. For men and women, DFLEs and DLEs varied widely by state. Among women, DFLE ranged from 45.8 years in West Virginia to 52.5 years in Hawaii, a 6.7-year gap. Men had a similar range. The gap in DLEs across states was 2.4 years for women and 1.6 years for men. The correlation among DFLE, DLE, and TLE was particularly strong in southern states. The South is doubly disadvantaged: residents have shorter lives and spend a greater proportion of those lives with disability.
Conclusions. The stark variation in DFLE and DLE across states highlights the large health inequalities present today across the United States, which have significant implications for individuals’ well-being and US states’ financial costs and medical care burden.
US state disparities in population health are striking.1–4 For example, people in North Carolina experience disability about 10 years earlier and die 2 years sooner than people in North Dakota.5,6 Such stark and growing2,7,8 disparities have fueled a renewed interest among researchers to investigate the role of US state contexts in shaping population health.2,3,9–11 Much of that research has examined state disparities in 2 health-related indicators: the risk of disability or death. Less attention has been given to the intersection of those indicators—sometimes referred to as disability-free life expectancy (DFLE), and its complement, disabled life expectancy (DLE)—and their relationship with total life expectancy (TLE). This study addresses that gap to provide a clearer understanding of how the lived experiences of people differ across states, as well as the consequent personal, medical, economic, and social costs.
DFLE is the number of years that an individual can expect to live without disability. Relatedly, DLE is the number of expected years lived with disability. Both are a function of 2 processes: disability and mortality. Importantly, these processes do not necessarily operate in tandem: mortality and disability are far from isomorphic concepts.12,13 For example, longer TLE in the United States is accompanied by longer DFLE among some subgroups (e.g., non-Hispanic Whites, college-educated individuals) but shorter DFLE among others, such as Hispanic individuals.12,14,15 That is, non-Hispanic and Hispanic adults live roughly the same number of years, but the latter spend a greater proportion of their lives with disability.
By focusing on DFLE, DLE, and their association with TLE across US states, this study provides a new dimension for understanding contemporary cross-state disparities in population health. Comparisons of DFLE, DLE, and TLE provide insights into the extent to which processes influencing disability and mortality are similar, which might occur when disability is part of a health “trajectory” ending in death.15 If states with higher TLE consistently have higher DFLE and lower DLE, this implies that the processes underlying disability and mortality are similar across states, leading to a compressed period of disability. In contrast, the 2 underlying processes may be disjointed in certain states. Residents of states with a long TLE but short DFLE spend a larger proportion of their long lives with disability. In such states, individuals can face significant caregiving costs associated with living with disability for a protracted period,16 and state budgets can face substantial economic and health care costs.17
AIMS
This study extends recent work documenting disparities in health across states in several ways. It uses the most recent and largest data sets on disability and mortality; examines the associations among TLE, DFLE, and DLE; identifies clusters of states where the associations are strongest and weakest; and simulates how much longer or shorter TLE and DFLE for the United States could become, based on best- and worst-case scenarios for disability and mortality drawn from the 50 states. Specifically, the study addresses 3 main questions:
How large are disparities in TLE, DFLE, and DLE among US states?
To what extent are TLE, DFLE, and DLE associated among states?
How long (or short) could TLE and DFLE for the United States be under “best and worst conditions”?
We examined these questions separately for men and women. This is necessary given large differences between men and women in the risks of disability and death18 and the possibility that state contexts have differential consequences for men and women.19 To glean additional insights, we also highlight the results for the southern region of the United States compared with the rest of the United States, given the well-established and persistent southern disadvantage.2,20
METHODS
The analysis required state-level information on age-specific disability prevalence and mortality rates. We estimated disability prevalence from the 2013–2017 American Community Survey (ACS), which contains representative samples from each state.21 We obtained mortality rates from the 2017 US Mortality Database (USMD). The 2017 information is the most recent data available. We focused on ages 25 to 89 years because we were interested in adult disability and because the ACS top-codes age at 90 years. The 2013–2017 ACS contains 10 937 852 adults aged 25 to 89 years.
Disability and Mortality
Disability is frequently assessed in terms of difficulties with activities of daily living and instrumental activities of daily living.3,22 The ACS includes 1 question for each domain. Respondents are asked whether, because of a physical, mental, or emotional condition, they had difficulty dressing or bathing (activities of daily living) or doing errands alone such as visiting a doctor’s office or shopping (instrumental activities of daily living). We combined these questions into a single binary measure, in which an affirmative response to either question was designated as having a disability. Analyses using the separate measures provided similar results.
We obtained age-specific mortality risks from the 2017 USMD.23 This database contains the only published set of complete, single-year life tables for each US state. The tables were created using data from the US vital statistics system (i.e., death counts, birth counts) and data from the US Census Bureau (i.e., census counts, population estimates).
Analysis
We estimated age-specific disability prevalence based on logistic regression models of the form shown in equation 1:
 |
The model estimates the age-specific log odds of disability for each 5-year age group from 25 to 89 years, with the group aged 85 to 89 years as the omitted reference. Ancillary analyses that used a continuous measure of age provided similar findings. We estimated gender-specific models for each US state and adjusted for the sampling design of the ACS. We performed all analyses with Stata version 15.1 (StataCorp LP, College Station, TX). After estimating each of the 100 state–gender models, we used the Stata margins command to convert the log odds of disability for each age group into the probability of disability for each group.
For all state–gender combinations, we merged the probability of disability for each 5-year age group with mortality data for that group, the latter obtained from the USMD (Appendix Figure A, available as a supplement to the online version of this article at http://www.ajph.org, shows that these 5-year estimates vary markedly across states, especially for disability and younger adults). We then employed the Sullivan-based Life Table Method to estimate DFLE and DLE across ages 25 to 89 years.24 To estimate DFLE, we first multiplied the probability of not having a disability within an age group (from the ACS) by the total number of years lived within the age group (from the USMD) to obtain the total number of years lived without disability within each age group. We then summed these quantities across the age groups to obtain the total number of years lived without disability between ages 25 and 89 years. To obtain DLE, we subtracted DFLE from TLE for ages 25 to 89 years.
We also calculated the standard errors for DFLE and DLE, following standard procedure.24 Because of large sample sizes and relatively low prevalence of disability until later life, the standard errors were close to zero. We therefore did not include them in our tables or figures for parsimony.
To answer the second research question, we calculated correlations between TLE and DFLE, and between TLE and DLE. This step allows us to determine whether and by how much greater life expectancy across states is associated with more years without disability and fewer years lived with disability. For example, a positive association between TLE and DFLE would show that greater life expectancy is associated with more years without disability across states, indicating that the additional years of life are not years lived with disability.
To assess our third research question, we created 2 synthetic populations. We created the population reflecting the “best-case disability scenario” by using the lowest disability prevalence from among the 50 states for each 5-year age group. We created the population reflecting the “worst-case disability scenario” by using the highest disability prevalence for each of the 5-year age groups. In a similar fashion, we created best- and worst-case mortality scenarios. We combined all this information into 1 synthetic population that merged the best-case disability and mortality rates, and another that merged the worst-case rates. Again, we implemented the Sullivan-based Life Table Method to estimate TLE, DFLE, and DLE for these synthetic populations.
RESULTS
First, we sought to evaluate state disparities in TLE, DFLE, and DLE. Estimates of TLE, DFLE, and DLE for each sex–state combination are provided in Table 1; a graphical summary is in Figure 1. The Figure 1a shows TLE and DFLE among women for each state while Figure 1b shows TLE and DLE. The dashed lines in the figure represent US average values. Recall that these measures reflect a 25- to 89-year age range; therefore, the maximum possible value for each measure is 65 years. Across the 50 states, TLE for women ranged from 51.6 years in West Virginia to 57.1 years in Hawaii, a 5.5-year gap. DFLE ranged from 45.8 years in West Virginia to 52.5 years in Hawaii, a 6.7-year gap. DLE ranged from 3.8 years in North Dakota to 6.2 years in Mississippi.
TABLE 1—
Total Life Expectancy (TLE), Disability-Free Life Expectancy (DFLE), and Disabled Life Expectancy (DLE) by State and Gender for Ages 25–89 Years: United States, 2013–2017
| State | Men | Women | South (S)/ Nonsouth (NS) | ||||||
| TLE, Years | DFLE, Years | DLE, Years | % of Life With Disability | TLE, Years | DFLE, Years | DLE, Years | % of Life With Disability | ||
| Alabama | 48.0 | 44.1 | 3.9 | 8.1 | 52.6 | 47.0 | 5.7 | 10.8 | S |
| Alaska | 51.3 | 48.0 | 3.3 | 6.5 | 54.6 | 49.6 | 5.1 | 9.3 | NS |
| Arizona | 51.5 | 48.3 | 3.2 | 6.1 | 55.5 | 51.0 | 4.5 | 8.1 | NS |
| Arkansas | 48.5 | 44.6 | 4.0 | 8.2 | 52.5 | 46.7 | 5.8 | 11.1 | S |
| California | 52.9 | 49.4 | 3.6 | 6.7 | 56.5 | 51.2 | 5.3 | 9.4 | NS |
| Colorado | 52.6 | 49.7 | 3.0 | 5.7 | 55.8 | 51.7 | 4.1 | 7.3 | NS |
| Connecticut | 52.5 | 49.5 | 3.0 | 5.7 | 56.1 | 51.8 | 4.3 | 7.7 | NS |
| Delaware | 50.4 | 47.6 | 2.8 | 5.6 | 54.6 | 50.5 | 4.1 | 7.5 | S |
| Florida | 51.3 | 48.1 | 3.2 | 6.3 | 55.5 | 51.0 | 4.5 | 8.1 | S |
| Georgia | 50.2 | 46.7 | 3.4 | 6.9 | 54.0 | 49.0 | 5.0 | 9.3 | S |
| Hawaii | 52.7 | 49.4 | 3.2 | 6.1 | 57.1 | 52.5 | 4.7 | 8.2 | NS |
| Idaho | 51.9 | 48.5 | 3.4 | 6.5 | 55.0 | 50.5 | 4.5 | 8.2 | NS |
| Illinois | 51.4 | 48.0 | 3.3 | 6.5 | 55.1 | 50.5 | 4.7 | 8.4 | NS |
| Indiana | 49.5 | 46.1 | 3.5 | 7.0 | 53.4 | 48.6 | 4.8 | 9.0 | NS |
| Iowa | 51.6 | 48.8 | 2.8 | 5.5 | 55.1 | 51.2 | 3.9 | 7.1 | NS |
| Kansas | 50.9 | 47.8 | 3.1 | 6.1 | 54.5 | 50.0 | 4.5 | 8.2 | NS |
| Kentucky | 47.9 | 43.7 | 4.3 | 8.9 | 52.2 | 46.3 | 5.9 | 11.3 | S |
| Louisiana | 48.4 | 44.5 | 3.9 | 8.1 | 52.8 | 47.3 | 5.5 | 10.4 | S |
| Maine | 50.7 | 46.9 | 3.8 | 7.5 | 54.7 | 50.1 | 4.6 | 8.4 | NS |
| Maryland | 50.9 | 48.0 | 2.9 | 5.7 | 55.0 | 50.7 | 4.3 | 7.8 | S |
| Massachusetts | 52.0 | 48.8 | 3.2 | 6.2 | 56.0 | 51.2 | 4.8 | 8.5 | NS |
| Michigan | 50.5 | 46.8 | 3.7 | 7.2 | 54.2 | 49.2 | 5.0 | 9.2 | NS |
| Minnesota | 52.9 | 50.0 | 2.9 | 5.6 | 56.2 | 52.1 | 4.1 | 7.3 | NS |
| Mississippi | 47.5 | 43.1 | 4.4 | 9.3 | 52.1 | 46.0 | 6.2 | 11.8 | S |
| Missouri | 49.7 | 46.1 | 3.6 | 7.2 | 53.9 | 48.8 | 5.1 | 9.4 | NS |
| Montana | 51.2 | 48.1 | 3.2 | 6.1 | 54.6 | 50.3 | 4.3 | 7.8 | NS |
| Nebraska | 51.8 | 49.1 | 2.8 | 5.3 | 55.2 | 51.4 | 3.8 | 6.9 | NS |
| Nevada | 50.6 | 47.5 | 3.1 | 6.1 | 54.3 | 49.8 | 4.5 | 8.3 | NS |
| New Hampshire | 51.6 | 48.7 | 2.8 | 5.5 | 55.4 | 51.0 | 4.3 | 7.8 | NS |
| New Jersey | 52.0 | 48.9 | 3.0 | 5.8 | 55.7 | 51.4 | 4.4 | 7.8 | NS |
| New Mexico | 49.8 | 45.6 | 4.2 | 8.5 | 54.4 | 48.9 | 5.5 | 10.1 | NS |
| New York | 52.6 | 49.2 | 3.5 | 6.6 | 56.3 | 51.2 | 5.1 | 9.0 | NS |
| North Carolina | 50.3 | 46.6 | 3.7 | 7.3 | 54.1 | 49.0 | 5.1 | 9.3 | S |
| North Dakota | 52.0 | 49.3 | 2.8 | 5.3 | 55.3 | 51.5 | 3.8 | 6.9 | NS |
| Ohio | 49.2 | 45.8 | 3.4 | 6.8 | 53.4 | 48.5 | 4.9 | 9.1 | NS |
| Oklahoma | 48.8 | 45.1 | 3.7 | 7.5 | 52.4 | 47.2 | 5.2 | 10.0 | S |
| Oregon | 52.0 | 48.5 | 3.5 | 6.7 | 55.3 | 50.5 | 4.8 | 8.7 | NS |
| Pennsylvania | 50.3 | 46.9 | 3.4 | 6.8 | 54.5 | 49.6 | 4.8 | 8.9 | NS |
| Rhode Island | 51.6 | 48.2 | 3.4 | 6.6 | 55.4 | 50.1 | 5.3 | 9.6 | NS |
| South Carolina | 49.2 | 45.5 | 3.7 | 7.5 | 53.7 | 48.5 | 5.2 | 9.6 | S |
| South Dakota | 51.3 | 48.5 | 2.9 | 5.6 | 54.9 | 50.7 | 4.2 | 7.7 | NS |
| Tennessee | 48.5 | 44.7 | 3.9 | 8.0 | 52.7 | 47.1 | 5.6 | 10.6 | S |
| Texas | 51.1 | 47.6 | 3.5 | 6.8 | 54.8 | 49.7 | 5.1 | 9.4 | S |
| Utah | 52.5 | 49.6 | 2.9 | 5.5 | 55.3 | 51.2 | 4.2 | 7.5 | NS |
| Vermont | 52.0 | 48.6 | 3.3 | 6.4 | 55.1 | 50.7 | 4.4 | 8.0 | NS |
| Virginia | 51.6 | 48.4 | 3.1 | 6.1 | 55.0 | 50.6 | 4.5 | 8.1 | S |
| Washington | 52.4 | 49.1 | 3.3 | 6.3 | 55.6 | 50.8 | 4.8 | 8.6 | NS |
| West Virginia | 47.4 | 43.1 | 4.3 | 9.0 | 51.6 | 45.8 | 5.8 | 11.3 | S |
| Wisconsin | 51.7 | 48.8 | 2.9 | 5.7 | 55.4 | 51.2 | 4.1 | 7.5 | NS |
| Wyoming | 51.5 | 48.7 | 2.8 | 5.4 | 54.8 | 50.9 | 3.8 | 7.0 | NS |
| Worst case | 46.7 | 42.1 | 4.6 | 9.9 | 51.4 | 45.0 | 6.4 | 12.5 | Synthetic |
| Best case | 53.5 | 51.2 | 2.3 | 4.3 | 57.5 | 54.0 | 3.6 | 6.2 | Synthetic |
Note. The worst-case synthetic population consists of the highest disability and mortality rates among the 50 states for each 5-year age group; the best-case synthetic population consists of the lowest 5-year rates.
FIGURE 1—
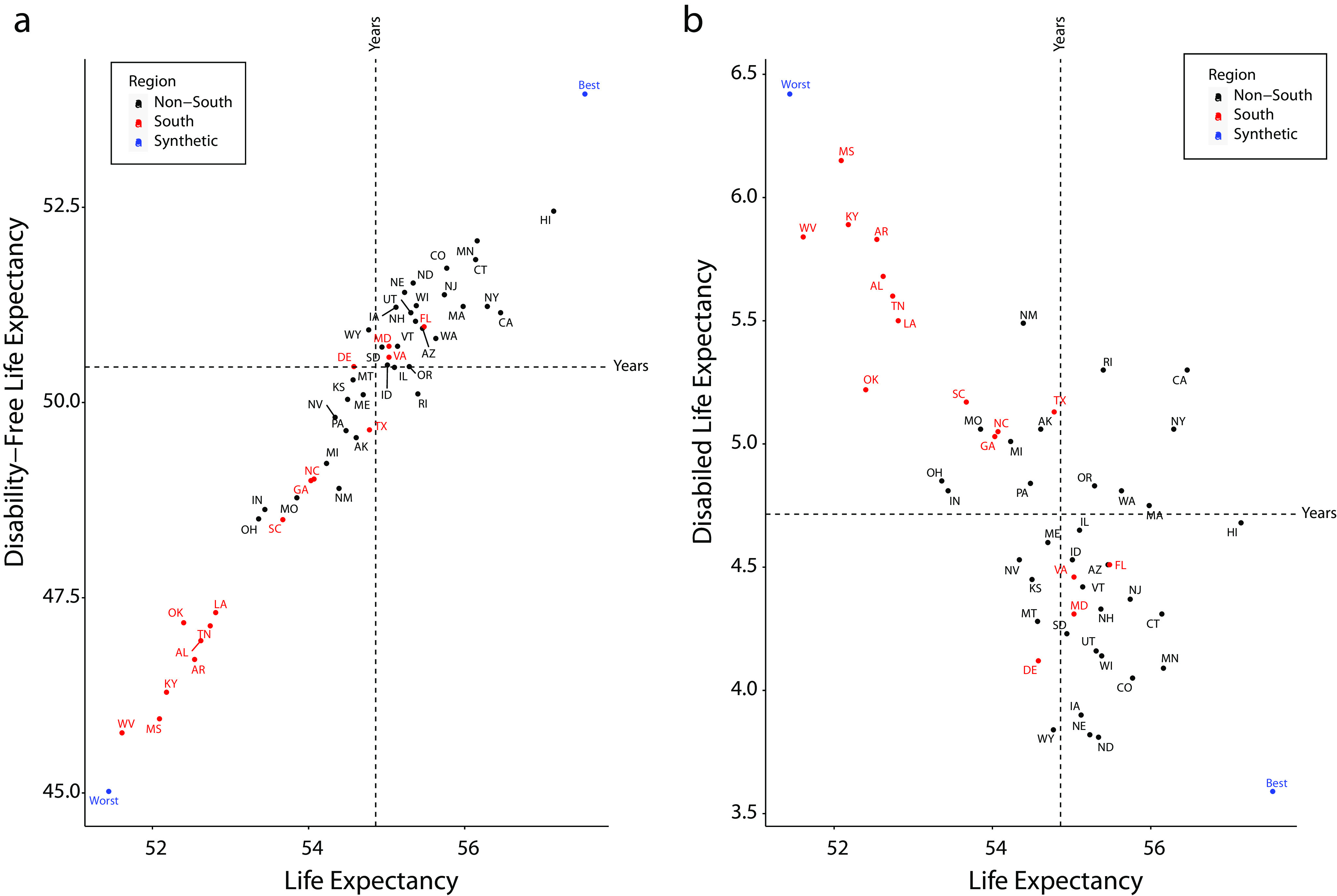
Total Life Expectancy by US State for Women by (a) Disability-Free Life Expectancy and (b) Disabled Life Expectancy: 2013–2017
Note. The 2-letter abbreviations within each figure indicate the US state. The dot indicated by “best” represents a hypothetical state that for each 5-year age band takes on the value of an actual state with the lowest disability (and mortality, respectively). Because no actual US state is “best” at every age band, this hypothetical state has lower disability than any actual state. Following the same technique as best, the dot indicated by “worst” represents the hypothetical worst-case scenario.
The fact that the range of DFLE across states was larger than the range of TLE suggests that cross-state differences in TLE are merely the tip of the population health iceberg. We also report statistical evidence in the Appendix showing greater variation for DLE and DFLE than TLE, which further illustrates the importance of assessing these health markers to understand state disparities. Also important to note, the worst-performing states on both TLE and DFLE tended to be in the South. The 8 worst-performing states on these measures were West Virginia, Mississippi, Kentucky, Alabama, Louisiana, Tennessee, Arkansas, and Oklahoma. Similarly, the South also had some of the greatest DLE for men and women. However, the DLE difference between southern and nonsouthern states was not as stark the difference in DFLE; California and Maine had greater DLEs than some southern states.
Disparities in TLE, DFLE, and DLE across states were similar in magnitude for men as they were for women. These measures for men are shown in Figure 2 and in the right panel of Table 1. For men, TLE ranged from 47.4 years in West Virginia to 52.9 years in Minnesota, a difference of 5.5 years. DFLE ranged from 43.1 years in Mississippi to 50.0 years in Minnesota, a difference of 6.9 years. The figures also show that the states that performed best (or worst) for women also performed best (or worst) for men. More specifically, the correlation of TLEs and DFLEs for men and women were 0.97 and 0.98, respectively.
FIGURE 2—
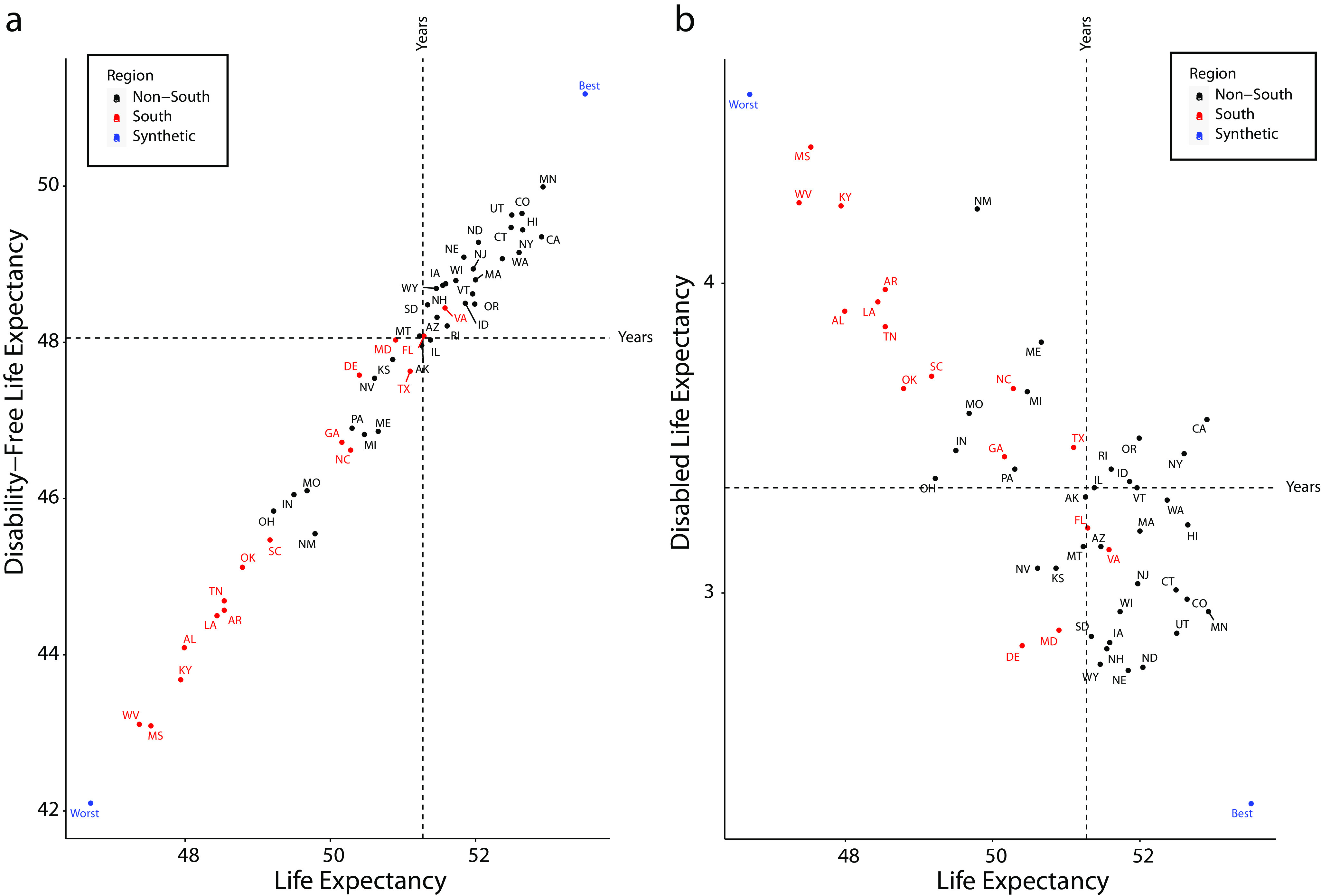
Total Life Expectancy by US State for Men by (a) Disability-Free Life Expectancy and (b) Disabled Life Expectancy: 2013–2017
Note. The 2-letter abbreviations within each figure indicate the US state. The dot indicated by “best” represents a hypothetical state that for each 5-year age band takes on the value of an actual state with the lowest disability (and mortality, respectively). Because no actual US state is “best” at every age band, this hypothetical state has lower disability than any actual state. Following the same technique as best, the dot indicated by “worst” represents the hypothetical worst-case scenario.
Correlations Among States
The association between TLE and DFLE across the 50 states was very strong, with a correlation of r = 0.97 for women and r = 0.99 for men. People residing in states with longer TLEs also tended to spend more of those years without disability. The correlation between TLE and DLE across the 50 states was not as strong, with r = −0.75 for men and r = −0.67 for women. This discrepancy can occur when TLE and DFLE move in tandem, with either a stochastic or fairly consistently sized gap between them. As an example, imagine 2 states, 1 with TLE of 55 years and DFLE of 53 years and another with TLE of 60 years and DFLE of 58 years. The TLE and DFLE are perfectly correlated. However, the DLE is 2 years in both states, so DLE is uncorrelated with TLE and DFLE.
When we examined the patterns for southern and nonsouthern states, we found that the correlation between TLE and DFLE was similarly strong in the South (r = 0.99 for men and women) as it was in the rest of the country (0.97 for men, 0.90 for women). However, the correlation between TLE and DLE was much stronger in the South (–0.89 for men and women) than the rest of the country (–0.45 for men and −0.15 for women). In fact, women’s TLE and DLE were essentially unrelated in the rest of the country; testing the sample correlation against 0 provided a Z statistic of −0.086, with a P value of .38.
We can draw several insights from these patterns. First, for all states, the number of years that one lived with disability was closely tied to the total number lived; DFLE and TLE moved in tandem. Second, the number of years that one lived with disability was smaller and more consistent in size among nonsouthern states than among southern states. As a consequence, the correlation between TLE and DLE was much smaller in nonsouthern states. In fact, the correlation in the nonsouthern states was modest for men and negligible for women. Third, southern states were doubly disadvantaged. They had relatively low TLE combined with relatively high DLE; as a consequence, residents of these states live a higher proportion of their life with disability.
Figures 1 and 2 contain several other interesting patterns. For instance, some contiguous states had notably disparate TLE and DFLE. Take Oklahoma, Kansas, and Texas as an example. Oklahoma is one of the worst-performing states, with a TLE of 52.4 years and DFLE of 47.2 years. It shares its northern border with Kansas, which performs similar to the national average, with a TLE of 54.5 years and DFLE of 50.0 years. Oklahoma shares its southern border with Texas, which also performs better, with a TLE of 54.8 years and DFLE of 49.7 years. Similar discrepancies exist between other contiguous states.
US Life Expectancy Under Current Conditions
For each 5-year age group of women, we identified the state with the lowest disability prevalence and the lowest mortality risk separately (Table 2). We combined these estimates to create a synthetic population who experienced the best-case scenarios. We predicted that this synthetic population would have a TLE of 57.5 years, which is 0.4 years longer than the highest state TLE. This population would also have a DFLE of 54.0 years, which is 1.5 years longer than the actual DFLE, and a DLE of 3.6 years, which is 0.2 years fewer than the lowest state DLE. On the other extreme, if we used the highest age-specific disability and mortality rates among the states, TLE would fall to 51.4 years, DFLE would fall to 45.0 years, and DLE would rise to 6.4 years.
TABLE 2—
Minimum and Maximum Disability Prevalence and Mortality Risk by Age Group: United States, 2013–2017
| Age, Years | Disability Prevalence | Mortality Risk | ||
| Minimum Rate (State) | Maximum Rate (State) | Minimum Rate (State) | Maximum Rate (State) | |
| Women | ||||
| 25–29 | 0.0121 (NE) | 0.0436 (AK) | 0.0020 (CA) | 0.0067 (AK) |
| 30–34 | 0.0135 (WY) | 0.0512 (VT) | 0.0026 (OR) | 0.0114 (WV) |
| 35–39 | 0.0166 (ND) | 0.0519 (AR) | 0.0040 (CA) | 0.0121 (WV) |
| 40–44 | 0.0250 (NJ) | 0.0735 (WV) | 0.0057 (CA) | 0.0156 (WV) |
| 45–49 | 0.0298 (NE) | 0.0800 (MT) | 0.0079 (CT) | 0.0197 (OK) |
| 50–54 | 0.0390 (HI) | 0.1066 (WV) | 0.0122 (MN) | 0.0302 (WV) |
| 55–59 | 0.0449 (ND) | 0.1208 (MS) | 0.0202 (MA) | 0.0427 (MS) |
| 60–64 | 0.0498 (ND) | 0.1215 (KY) | 0.0293 (CT) | 0.0593 (WV) |
| 65–69 | 0.0571 (ND) | 0.1356 (MS) | 0.0418 (HI) | 0.0775 (WV) |
| 70–74 | 0.0644 (MT) | 0.1883 (MS) | 0.0615 (HI) | 0.1203 (MS) |
| 75–79 | 0.1243 (IA) | 0.2643 (MS) | 0.1030 (HI) | 0.1860 (KY) |
| 80–84 | 0.1990 (VT) | 0.3849 (MS) | 0.1539 (HI) | 0.2745 (AL) |
| 85–89 | 0.3374 (AK) | 0.5524 (AR) | 0.2749 (HI) | 0.4202 (WV) |
| Men | ||||
| 25–29 | 0.0140 (ND) | 0.0426 (MS) | 0.0055 (NE) | 0.0131 (WV) |
| 30–34 | 0.0186 (NJ) | 0.0419 (WV) | 0.0063 (CA) | 0.0189 (WV) |
| 35–39 | 0.0156 (NE) | 0.0616 (ME) | 0.0073 (MN) | 0.0231 (WV) |
| 40–44 | 0.0172 (NE) | 0.0722 (WV) | 0.0098 (CA) | 0.0246 (WV) |
| 45–49 | 0.0274 (MN) | 0.0772 (MS) | 0.0143 (MN) | 0.0334 (WV) |
| 50–54 | 0.0216 (WY) | 0.0905 (WV) | 0.0226 (ND) | 0.0442 (MS) |
| 55–59 | 0.0398 (WY) | 0.1040 (WV) | 0.0319 (CT) | 0.0713 (MS) |
| 60–64 | 0.0472 (NH) | 0.1176 (MS) | 0.0487 (MN) | 0.0967 (MS) |
| 65–69 | 0.0423 (SD) | 0.1290 (MS) | 0.0705 (MN) | 0.1219 (MS) |
| 70–74 | 0.0589 (AK) | 0.1378 (MS) | 0.1012 (CO) | 0.1740 (MS) |
| 75–79 | 0.0763 (WY) | 0.1919 (MS) | 0.1637 (CO) | 0.2450 (MS) |
| 80–84 | 0.1631 (WY) | 0.2662 (AK) | 0.2258 (HI) | 0.3560 (MS) |
| 85–89 | 0.2299 (ND) | 0.4911 (MS) | 0.3747 (HI) | 0.4964 (KY) |
Note. Disability estimates are from the 2013–2017 American Community Survey, and the mortality estimates are from the 2017 US Mortality Database. Rates are per 100 adults.
As illustrated previously, the best-case and worst-case scenarios would produce 2 dramatically different population health environments. There is a 6.1-year gap in TLE and an 8.9-year gap in DFLE between the scenarios. Interestingly, as shown in Table 2, many states contributed to the 2 scenarios. Fourteen states contributed to the best-case scenario. Nine states contributed to the worst-case scenario, with West Virginia and Mississippi contributing the most.
For men, the best-case scenario would produce a TLE as high as 53.5 years, which is 0.57 years above the highest TLE; a DFLE of 51.8 years, which is 1.55 years above the highest state DFLE; and, lastly, a DLE of 2.32 years, which is 0.34 years lower than the lowest state DLE. In contrast, the worst-case scenario would result in a TLE of just 46.7 years, a DFLE of 42.1 years, and a DLE of 4.61 years. The states that contributed to the best- and worst-case scenarios were similar for men and women.
DISCUSSION
Recent research on geographic differences in US health has focused on mortality; however, this study makes clear that mortality differences across geographic areas are a tip of the population health iceberg. We found that DFLE differs greatly across US states, more so than TLE. We also noted substantial variation among DLE across states: the worst-performing state has more than 1.5 times more years of DLE as the best-performing state. Our results reinforce the idea that US state of residence significantly affects US individuals’ health destinies—both life span and years of life with and without disability.
The complexity of the relationship among TLE, DFLE, and DLE among states has implications for how state contexts shape disability and mortality. We posed several questions to understand how these associations may be affected by state contexts. In general, the pattern for TLE and DFLE adhered to our expectation: more years of life in US states corresponded with more years without disability.
By contrast, the association between TLE and DLE varied. It was only moderately strong in states with relatively long TLE (mainly nonsouthern states) but strong in states with relatively short TLE (mainly southern states). One possible explanation is that, for states with longer TLE (mainly nonsouthern states), the underlying processes that affect disability and mortality are not as closely tied. It may be that, after a certain threshold of overall population health, state contexts influence disability and mortality through different underlying processes. Another possible explanation is that states with relatively low TLE (mainly southern states) are doubly disadvantaged. Their residents live fewer years and spend a greater proportion of those years with disability.
This latter finding has 2 possible implications: (1) the southern context may be pernicious to the extent that all body systems are independently at risk, leading to simultaneously higher rates for disability and mortality at younger ages, or (2) people with disability are less likely to survive. Because these types of health outcomes are a long time in the making, the observed clustering of southern states likely reflects shared, long-term, and cumulative state policy changes over several decades. The factors that might moderate mortality risk among persons with disability, such as social supports, medical care, and housing accommodations, are relatively weak in the South. Southern states, in particular, have invested less in their populations’ well-being on multiple dimensions such as maintaining low cigarette excise taxes, opting out of Medicaid expansion, providing weak antipoverty programs, and actively implementing state preemption laws, which prohibit local authority from legislating on many domains that could improve population health.10,11
Although we did not assess how specific state policies and contexts are associated with the variation in TLE, DFLE, and DLE among states, our analysis was nonetheless informed by recent studies that have examined how state-level contexts are associated with adult mortality and disability. Montez et al.19 documented, for example, that more than 50% of state variation in women’s mortality during 1980 to 2000 reflected states’ characteristics as compared with women’s characteristics. In addition, Fenelon2 illustrated the importance of smoking for regional differences in adult mortality, a finding consistent with the importance of tobacco control policies (e.g., excise taxes on cigarettes) for state differences in mortality.10,19
State legislatures also make a variety of decisions about key “inputs” to a healthy population and have played an increasingly large role in shaping population health because of structural changes through deregulation (affecting industries and local economies), preemption (state legislatures taking away local control over policies), and devolution (the transfer of responsibility of social insurance programs from the federal government to the states).9,25 State policies also appear to be increasingly clustered in terms of their political nature (e.g., more conservative or more liberal), which may account for the growth in regional clustering of mortality.26 This clustering may have contributed significantly to the growing importance of states as battlegrounds for population health.
Limitations
This study had some limitations that should be noted. First, the ACS data only provide information on people up to the age of 90 years. Nonetheless, it is unlikely that the inclusion of the oldest old would materially alter the patterns documented here given the small number of survivors at the very advanced ages. Second, we did not adjust for individual-level factors because the USMD lacks information on sociodemographic characteristics such as race, education, or income, which are known important correlates of both disability and mortality. The data also do not contain information on interstate migration histories. Although the possibility that interstate migration might contribute to the patterns we reported should not be ignored, previous studies examining its potential contribution concluded that its effect on state variation in health outcomes is modest.3 State differences in sociopolitical contexts that may help account for the disparities in TLE, DFLE, and DLE should be investigated in future. For instance, states’ investments in education systems affect their residents’ education levels, the structure of states’ tax policies affect poverty rates, and states’ civil rights and antidiscrimination protections affect gender, racial, and other disparities in health and mortality.
Public Health Implications
As life expectancy increased gradually, policymakers and researchers faced a critical question: are the added years of life healthy years or disabled years? This is a critical issue because disability is enormously costly to individuals,27 states, and the nation. In 2006, for instance, disability-associated costs for health care expenditures alone reached nearly $400 billion nationwide. The associated costs ranged widely from $600 million in Wyoming to $40 billion in New York.17 The inextricable links between disability and longevity make it imperative that research on the health status of US states provide estimates of healthy life expectancy, in addition to its component measures of disability and mortality. We showed that states with higher life expectancy, such as Hawaii, Minnesota, or Colorado, have not more but fewer disabled years. This suggests that state policy contexts can support longer lives and longer healthy lives. Subsequent research should examine health-related, but also economic, educational, social, and other policies to understand how all US states can achieve comparable results.
ACKNOWLEDGMENTS
This work was supported in part by grants R24AG045061 (PIs: Montez, Ailshire, Burgard, Hummer), T32AG000037 (PI: Crimmins), and R01AG055481 (PI: Montez) from the National Institute on Aging; and infrastructure grants P2CHD042849 and T32HD007081 (Population Research Center, University of Texas at Austin) from National Institutes of Child Health and Human Development.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
Human participant protection was not required for this study because the data are publicly available and de-identified.
Footnotes
REFERENCES
- 1.Chetty R, Stepner M, Abraham S et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fenelon A. Geographic divergence in mortality in the United States. Popul Dev Rev. 2013;39(4):611–634. doi: 10.1111/j.1728-4457.2013.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montez JK, Zajacova A, Hayward MD. Disparities in disability by educational attainment across US states. Am J Public Health. 2017;107(7):1101–1108. doi: 10.2105/AJPH.2017.303768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montez JK, Hayward MD, Wolf DA. Do US states’ socioeconomic and policy contexts shape adult disability? Soc Sci Med. 2017;178:115–126. doi: 10.1016/j.socscimed.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mokdad AH, Ballestros K, Echko M et al. The state of US health. JAMA. 1990–2016;2018;319(14):1444–1472. doi: 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ezzati M, Friedman AB, Kulkarni SC, Murray CJL. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med. 2008;5(4):557–568. doi: 10.1371/journal.pmed.0050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilmoth JR, Boe C, Barbieri M. Geographic differences in life expectancy at age 50 in the United States compared with other high-income countries. In: Crimmins EM, Preston SH, Cohen B, editors. International Differences in Mortality at Older Ages: Dimensions and Sources. Washington, DC: The National Academies Press; 2011. pp. 333–366. [Google Scholar]
- 9.Montez JK. Deregulation, devolution, and state preemption laws’ impact on US mortality trends. Am J Public Health. 2017;107(11):1749–1750. doi: 10.2105/AJPH.2017.304080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karas Montez J, Hayward MD, Zajacova A. Educational disparities in US adult health: US states as institutional actors on the association. Socius. 2019;5 doi: 10.1177/2378023119835345. doi: 10.1177/2378023119835345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Montez JK, Zajacova A, Hayward MD, Woolf S, Chapman D, Beckfield J. Educational disparities in adult mortality across US states: how do they differ and have they changed since the mid-1980s? Demography. 2019;56(2):621–644. doi: 10.1007/s13524-018-0750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayward MD, Heron M. Racial inequality in active life among adult Americans. Demography. 1999;36(1):77–91. doi: 10.2307/2648135. [DOI] [PubMed] [Google Scholar]
- 13.Crimmins EM, Hayward MD, Saito Y. Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography. 1994;31(1):159–175. doi: 10.2307/2061913. [DOI] [PubMed] [Google Scholar]
- 14.Montez JK, Hayward MD. Cumulative childhood adversity, educational attainment, and active life expectancy among US adults. Demography. 2014;51(2):413–435. doi: 10.1007/s13524-013-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayward MD, Hummer RA, Chiu C-T, González-González C, Wong R. Does the Hispanic paradox in US adult mortality extend to disability? Popul Res Policy Rev. 2014;33(1):81–96. doi: 10.1007/s11113-013-9312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freedman V, Spillman B. Disability and Care Needs of Older Americans: An Analysis of the 2011 National Health and Aging Trends Study. Washington, DC: US Department of Health and Human Services, Office of Disability, Aging, and Long-Term Care Policy; 2014. [Google Scholar]
- 17.Anderson WL, Armour BS, Finkelstein EA, Wiener JM. Estimates of state-level health-care expenditures associated with disability. Public Health Rep. 2010;125(1):44–51. doi: 10.1177/003335491012500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crimmins EM, Shim H, Zhang YS, Kim JK. Differences between men and women in mortality and the health dimensions of the morbidity process. Clin Chem. 2019;65(1):135–145. doi: 10.1373/clinchem.2018.288332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montez JK, Zajacova A, Hayward MD. Explaining inequalities in women’s mortality between US states. SSM Popul Health. 2016;2:561–571. doi: 10.1016/j.ssmph.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elo IT, Hendi AS, Ho JY, Vierboom YC, Preston SH. Trends in non-Hispanic White mortality in the United States by metropolitan–nonmetropolitan status and region, 1990–2016. Popul Dev Rev. 2019;45(3):549–583. doi: 10.1111/padr.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Community Survey. Available at: https://www.census.gov/programs-surveys/acs. Accessed December 23, 2019.
- 22.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 23.US Mortality Database. Available at: https://usa.mortality.org. Accessed April 15, 2020.
- 24.Jagger C. Health Expectancy Calculation by the Sullivan Method: A Practical Guide. European Concerted Action on the Harmonization of Health Expectancy Calculations in Europe. 2001. Available at: https://reves.site.ined.fr/fichier/s_rubrique/20184/rp408.fr.pdf. Accessed November 9, 2018.
- 25.Montez JK. Policy polarization and death in the United States. Temple Law Rev. 2020;92(4):889–916. [PMC free article] [PubMed] [Google Scholar]
- 26.Grumbach JM. From backwaters to major policymakers: policy polarization in the states, 1970–2014. Perspect Polit. 2018;16(2):416–435. doi: 10.1017/S153759271700425X. [DOI] [Google Scholar]
- 27.Mitra S, Palmer M, Kim H, Mont D, Groce N. Extra costs of living with a disability: a review and agenda for research. Disabil Health J. 2017;10(4):475–484. doi: 10.1016/j.dhjo.2017.04.007. [DOI] [PubMed] [Google Scholar]


