Abstract
Achalasia is a disease characterized by the inability to relax the esophageal sphincter due to a degeneration of the parasympathetic ganglion cells located in the wall of the thoracic esophagus. Achalasia has been associated with extraesophageal dysmotility, suggesting alterations of the autonomic nervous system (ANS) that extend beyond the esophagus. The purpose of the present contribution is to investigate whether achalasia may be interpreted as the esophageal manifestation of a more generalized disturbance of the ANS which includes alterations of heart rate and/or blood pressure. Therefore simultaneous non-invasive records of the heart inter-beat intervals (IBI) and beat-to-beat systolic blood pressure (SBP) of 14 patients (9 female, 5 male) with achalasia were compared with the records of 34 rigorously screened healthy control subjects (17 female, 17 male) in three different conditions: supine, standing up, and controlled breathing at 0.1 Hz, using a variety of measures in the time and spectral domains. Significant differences in heart rate variability (HRV) and blood pressure variability (BPV) were observed which seem to be due to cardiovagal damage to the heart, i.e., a failure of the ANS, as expected according to our hypothesis. This non-invasive methodology can be employed as an auxiliary clinical protocol to study etiology and evolution of achalasia, and other pathologies that damage ANS.
Introduction
Achalasia, a cause of esophageal motor disorders, is an autoimmune disease with a failure of the lower esophageal sphincter to relax after swallowing [1]. It is characterized by degeneration of parasympathetic ganglion cells in its myenteric plexus [2, 3]. Clinical manifestations include dysphagia, regurgitation, chest pain, cough, aspiration, weight loss and heartburn [4, 5]. It affects both sexes and all ages with an annual incidence of 0.3–1.6/100,000 [6]. The diagnosis is confirmed by high resolution manometric studies (HRM) [7]. In a Mexican population no difference in bio-geographic ancestry between patients and controls occur, however, the frequency of some alleles and extended haplotypes are increased [8].
Achalasia has a widespread effect on the body. Extraesophageal denervation has been found in the stomach [9], the vagal trunk and the dorsal motor nuclei [10–16]. Functional and motor abnormalities have been observed in the stomach [17–22], the gallbladder [19], and the small bowel [23, 24]. It has an important local and systemic inflammatory autoimmune component, associated with the presence of specific anti-myenteric autoantibodies, as Herpes Simplex Virus (HSV-1) infection [2]. Moreover, achalasia may occur in primary autonomic dysfunction diseases, such as orthostatic hypotension [25], acute autonomic neuropathy [26], among others [27–30], and in secondary autonomic disorders, such as diabetes mellitus [31–36]. Autonomic reflex tests (Ewing battery) and statistical measures of heart rate variability (HRV) on achalasia subjects are inconclusive, as half of the studies detected autonomic alterations [37–40], but the other half did not [41–44].
Autonomous nervous system (ANS) regulates blood pressure homeostasis [45] by the cardiac cycle through central (e.g., vasomotor and respiratory centers) and peripheral (e.g., arterial pressure and respiratory movements) oscillators. Parasympathetic modulation decreases the heart rate and cardiac contractility, whereas activity of the sympathetic branch opposes these effects and regulates peripheral vasoconstriction [46–49]. Thus, ANS activity can be evaluated through HRV [47, 48, 50–56], and by the homeostatic regulatory mechanism [45, 57–59]. This strategy allowed us to increase the statistical significance to distinguish between controls, recently diagnosed and long-standing diabetic patients [54, 55]. Short term HRV has a temporal structure with robust long-range correlations, with fractal and non-linear features that break down under pathologic conditions like Diabetes Mellitus (DM), reflecting changes in the neuro-autonomic control mechanisms [54, 55, 60–66]. HRV has been used as an early sign of DM autonomic neuropathy [54, 55], but has not been studied for achalasia.
Systolic blood pressure (SBP) variability in control subjects changes under different maneuvers [49], and during active standing and handgrip reflecting lower parasympathetic cardiac activity at rest [67]. Interestingly, whereas HRV at rest appears to be a protective health factor [45], it has been suggested that SBP variability is a risk factor [67–70]. Therefore, it would be interesting to see how blood pressure changes in patients with achalasia. To our knowledge this type of study has not been previously performed.
The objective of the present contribution is to evaluate extraesophageal autonomic function in achalasia. To do that, we compare blood pressure and heart rate variability between controls and patients with achalasia in 3 selected conditions: clinostatism, orthostatism, and rhythmic breathing at 0.1Hz. As far as we know, this is the first analysis involving simultaneous blood pressure and heart rate variability data using quantitative measures in the time and frequency domains to compare control subjects and patients with achalasia. Our hypothesis is that achalasia may be associated to damage to the parasympathetic fibers to the sinus node and some other areas of the heart innervated by the vagal cardiovascular innervation. If the parasympathetic neurons of the myenteric plexus of the esophagus are damaged there is a strong possibility that the cholinergic neurons that innervate the sinus auricular node are also damaged and therefore this denervation could be demonstrated analyzing the blood pressure and heart rate variability.
Research design and methodology
All subjects provided written informed consent, their medical history was screened and underwent a physical examination. The Ethical Committee of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán approved the protocol for the physiological monitoring of the achalasia patients.
SBP and HR data were recorded simultaneously with a Portapress® device of Finapres Medical Systems, The Netherlands [71]. The Portapress® quantifies the blood pressure waveform at the finger with a precision of 1 mmHg and a time resolution of 1 ms, which allows us to derive other hemodynamic parameters. Here only the IBI and the SBP are analyzed, because the diastolic blood pressure (DBP) has an analogous time series as SBP as seen in S1 Fig. IBI is measured in units of seconds and SBP as mmHg. The detailed methodology for time series analysis is given in the S1 Appendix.
Student’s t test was used to compare the different study groups of control subjects and achalasia patients. A value of p<0.05 was considered statistically significant in the hypothesis test of different means of the moments (standard deviation, skewness and kurtosis), HMP α, LF/HF, frequency radius rf, and resonance parameter β.
Results and discussion
The study population was composed of 48 subjects clinically classified in 2 distinct groups as follows:
34 healthy control subjects, 17 women with a body mass index (BMI = height/weight^2) from 19.1 to 28.5 kg/m2 (with a mean and standard deviation of (24±3) kg/m2), aged from 21 to 50 years old, (35±8) years old, and 17 men with BMI from 19.5 to 28.7 kg/m2, (25±3) kg/m2, aged from 20 to 50 years old, (30±7) yr. Subjects were classified as controls if they did not smoke, had no cardiac diseases, and did not take medication. They were not hypertensive and had blood pressure levels below 120/80 mmHg.
14 patients with achalasia, 9 women with BMI from 19.6 to 35.7 kg/m2, (25±4) kg/m2, aged between 25 and 70 years old, (49±15) yr; and 5 men with BMI from 21.0 to 35.8 kg/m2, (28±5) kg/m2, aged between 30 and 63 years old, (41±13) yr. These patients were diagnosed with achalasia by a team of gastroenterologists.
Achalasia patients were all asymptomatic of cardiovascular disease. They did not have syncope or presyncope. Neither they had palpitations, arrhythmias or symptoms or signs of heart failure. They were not hypertensive. Control subjects and achalasia patients abstained from caffeine, beta-blockers, anticholinergics, antihistamines, opioids and adrenergic medication for the 48 hours before the test. Data consisted of short-term 5 minutes recordings measured non-invasively with the Portapress® equipment. IBI and SBP were registered simultaneously while the subject was in supine position. Then, subjects were made to stand up, relaxed for 1 minute and stayed in this position for another 5 minutes. Finally, a controlled breathing test at 0.1 Hz was realized (subjects were asked to inspire and expire at six breaths per minute, 5 seconds in and 5 seconds out when standing up).
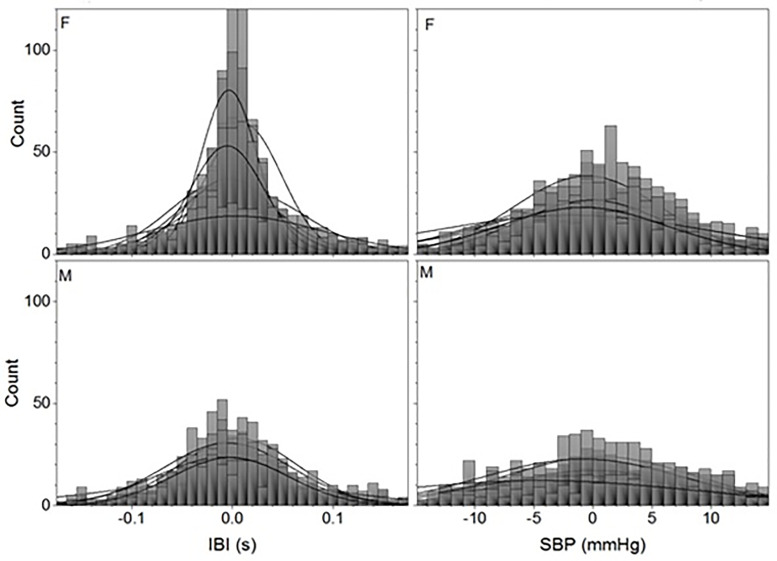
Histograms of the achalasia patients show a clear gender difference. IBI and SBP for all the included autonomic reflex tests have more rigid, symmetric, and mesokurtic histograms for male patients than for female achalasia patients, as seen in Fig 1 which shows the overlapping histograms of all the patients standing up.
Fig 1. Histograms of detrended time series for achalasia patients standing up.
IBI records (left-hand panels) and SBP (right-hand panels) for all 9 female (F) (upper row) and all 5 male (M) (bottom row) patients are shown with the best normal distribution fit (continuous lines).
Even when the histograms for each subject have tails and do not follow Gaussian distributions, the moments for each group of study (30 control subjects, 14 achalasia patients) follow Normal distributions (verified by different normality test: Shapiro-Wilk, Kolmogorov-Smirnov, Anderson-Darling, and Chen-Shapiro).
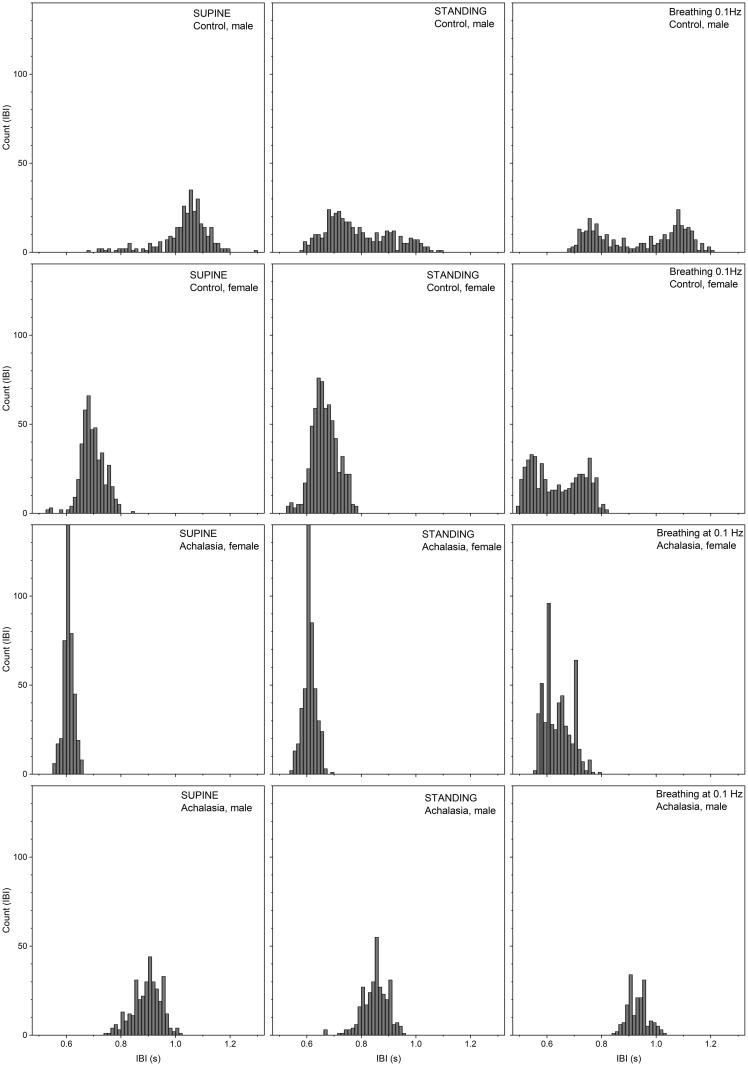
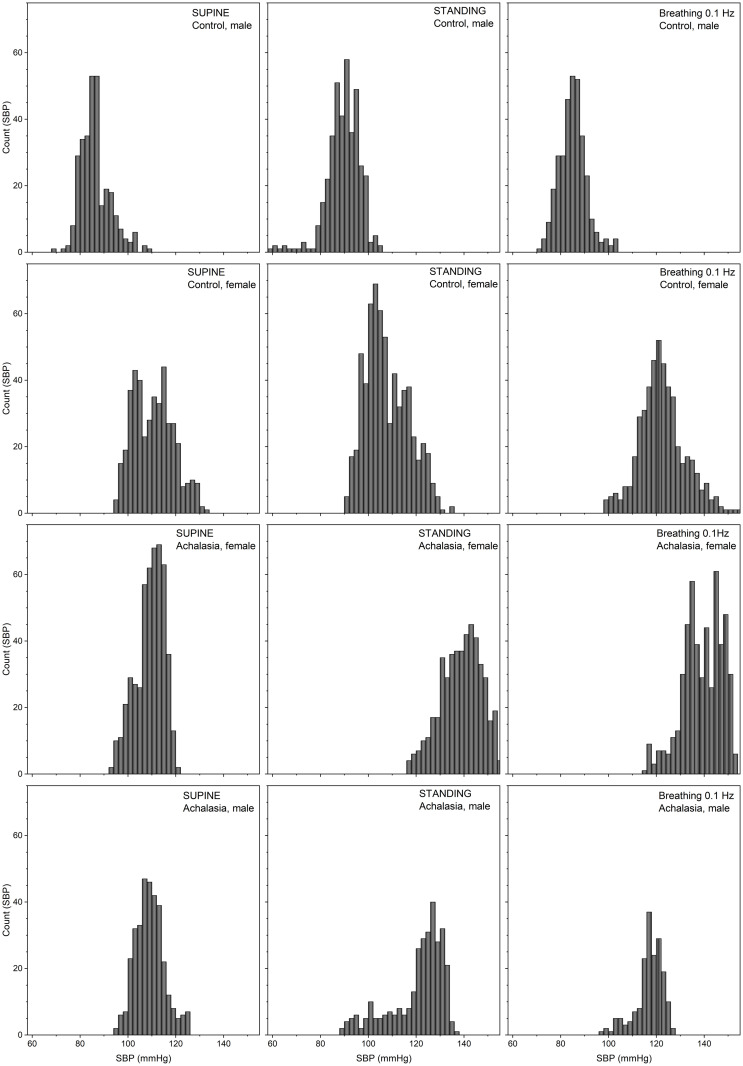
Results for the statistical moments of IBI records are in Table 1, while those of SBP are in Table 2. Results for control subject values in Tables 1 and 2 were calculated as a reference [72]. Average and standard deviations of our controls agree with previous publications [73]. Histograms of the detrended IBI records for a typical female and male control, female (F) and male (M) achalasia patients, all with similar BMI and age, for supine position, standing up position, and under controlled breathing at 0.1 Hz test are plotted in Fig 2, while Fig 3 shows the SBP. Continuous curves correspond to the best normal distribution fit to the histograms. Histograms of IBI and SBP signals during controlled breathing tend to be more platykurtic than the corresponding ones for supine and standing up positions. From these figures, it is evident that blood pressure shows less variability than heart rate. HRV is more altered during the standing position. SBP histograms are more disperse and platykurtic than IBI ones, in fact, standing up, the SBP distribution is flatter over a wider range. Moreover, for male achalasia patients, the IBI record does not show a strong difference under supine, standing up, or controlled breathing (Table 1) indicating a loss of adaptation capacity (less HRV) to different stressors, in contrast to control female subjects that have statistically significant changes under positional changes [49].
Table 1. Heart interbeat interval in the time domain.
| Maneuver | Sex | μ (s) | SD (s) | sk | κ | SD/μ | |
|---|---|---|---|---|---|---|---|
| Controls | Supine | F | 0.9 ± 0.1 | 0.05 ± 0.02 | -0.2 ± 0.5 | 1 ± 1 | 0.05 ± 0.02 |
| M | 1.0 ± 0.1 | 0.06 ± 0.02 | -0.3 ± 0.4 | 0.4 ± 0.8 | 0.06 ± 0.02 | ||
| Standing up | F | 0.8 ± 0.1 | 0.05 ± 0.02 | 0.1 ± 0.4 | 0.03 ± 0.6 | 0.06 ± 0.03 | |
| M | 0.8 ± 0.1 | 0.07 ± 0.04 | 0.3 ± 0.5 | 0.2 ± 1 | 0.09 ± 0.03 | ||
| Breathing at 0.1 Hz | F | 0.8 ± 0.1 | 0.09 ± 0.03 | 0.0 ± 0.4 | -0.8 ± 0.8 | 0.11 ± 0.04 | |
| M | 0.9 ± 0.1 | 0.09 ± 0.04 | 0.1 ± 0.4 | -0.6 ± 0.8 | 0.10 ± 0.04 | ||
| Achalasia | Supine | F | 0.8 ± 0.1 | 0.03 ± 0.01* (p = 0.007) | 0.2 ± 0.6* (p = 0.01) | 0.7 ± 2 | 0.04 ± 0.01 |
| M | 1.0 ± 0.2 | 0.05 ± 0.02 | -0.4 ± 0.1 | 0.4 ± 1 | 0.06 ± 0.03 | ||
| Standing up | F | 0.7 ± 0.1 | 0.05 ± 0.02 | -0.8 ± 1* (p = 0.04) | 5 ± 6* (p = 0.03) | 0.06 ± 0.02 | |
| M | 0.9 ± 0.2 | 0.08 ± 0.02 | -0.4 ± 0.4* (p = 0.04) | 0.7 ± 0.7* (p = 0.04) | 0.08 ± 0.02 | ||
| Breathing at 0.1 Hz | F | 0.8 ± 0.1 | 0.06 ± 0.03* (p = 0.002) | 0.1 ± 0.4 | -0.6 ± 0.8 | 0.08 ± 0.04 | |
| M | 0.9 ± 0.1 | 0.08 ± 0.03 | 0.2 ± 0.1 | -1.0 ± 0.5 | 0.10 ± 0.03 |
* indicates statistically significant difference with respect to control (p value <0.05).
Table 2. Systolic blood pressure in the time domain.
| Maneuver | Sex | μ (mmHg) | SD (mmHg) | sk | κ | SD/μ | |
|---|---|---|---|---|---|---|---|
| Controls | Supine | F | 100 ± 10 | 5 ± 2 | 0.6 ± 0.6 | 0.9 ± 3 | 0.05 ± 0.02 |
| M | 110 ± 10 | 6 ± 3 | 0.3 ± 0.5 | 0.2 ± 1 | 0.05 ± 0.02 | ||
| Standing up | F | 110 ± 10 | 6 ± 3 | -0.02 ± 0.7 | 0.6 ± 2 | 0.06 ± 0.03 | |
| M | 100 ± 10 | 6 ± 2 | -0.03 ± 0.5 | 0.3 ± 0.9 | 0.06 ± 0.02 | ||
| Breathing 0.1 Hz | F | 110 ± 20 | 8 ± 3 | 0.07 ± 0.3 | -0.3 ± 0.4 | 0.07 ± 0.02 | |
| M | 110 ± 20 | 7 ± 2 | -0.04 ± 0.5 | 0.08 ± 1 | 0.06 ± 0.02 | ||
| Achalasia | Supine | F | 100 ± 20 | 5 ± 2 | 0.2 ± 0.4 | -0.1 ± 0.5* (p = 0.03) | 0.05 ± 0.02 |
| M | 100 ± 10 | 6 ± 1 | 0.1 ± 0.5 | -0.4 ± 0.4* (p = 0.04) | 0.06 ± 0.01 | ||
| Standing up | F | 110 ± 20 | 9 ± 2* (p = 0.4) | -1.1 ± 0.8* (p = 0.02) | 4 ± 4* (p = 0.02) | 0.07 ± 0.01 | |
| M | 110 ± 10 | 10 ± 2* (p = 0.3) | -0.5 ± 0.3* (p = 0.04) | 0.4 ± 1 | 0.09 ± 0.02 * (p = 0.04) | ||
| Breathing 0.1 Hz | F | 110 ± 20 | 7 ± 2 | 0.04 ± 0.5 | -0.09 ± 1* (p = 0.03) | 0.07 ± 0.02 | |
| M | 104 ± 9 | 8 ± 2 | -0.3 ± 0.6* (p = 0.01) | 0.1 ± 0.9* (p = 0.04) | 0.08 ± 0.02 * (p = 0.04) |
* indicates statistically significant difference with respect to control (p value <0.05).
Fig 2. Histograms of IBI detrended time series for typical patients (30 years old).
Male M30C01 and female F30C01 control (upper rows), female F30A01 achalasia (middle row), and male M30A01 achalasia patients (lower row) in supine position (left-hand column), standing up position (middle column), and under controlled breathing at 0.1 Hz (right-hand column).
Fig 3. Histograms of SBP detrended time series for typical patients (30 years old).
Male M30C01 and female F30C01 control (upper rows), female F30A01 achalasia patients (middle row) and male M30A01 achalasia patients (lower row) on supine position (left-hand column), standing up (middle column), and under controlled breathing at 0.1 Hz (right-hand column).
The HRV of achalasia patients have in supine position, IBI Gaussian distributions (null sk and κ) with small SD/μ (rigid behavior); while standing up, IBI distributions have tails to the left (negative sk), are leptokurtic (κ positive) with larger SD/μ and range than in supine position (SD is almost the double); while IBI rhythmic breathing distributions are symmetric (null sk), platykurtic (κ negative) with similar values of SD/μ and range than standing up (see Fig 2, Table 1). Comparing with control, there is a statistically significant difference on IBI in supine and standing up positions for female achalasia patients while male only differ standing up (Table 1), reflecting more rigid distributions for achalasia female patients.
With respect to the SBPV of achalasia patients, SBP supine distributions are almost Gaussian (null sk and κ) with small SD/μ (rigid behavior); standing up, SBP distributions have tails to the left (negative sk), are leptokurtic (κ positive) with larger SD/μ and range than in supine position (SD is the double); while SBP rhythmic breathing distributions are almost Gaussian (null sk and κ) with similar values of SD/μ than standing up (see Fig 3, Table 2). Comparing with control, there is a statistically significant difference on SBP symmetry for achalasia patients on all maneuvers, in standing up maneuvers for female achalasia patients while male differ standing up and during rhythmic breathing (Table 2).
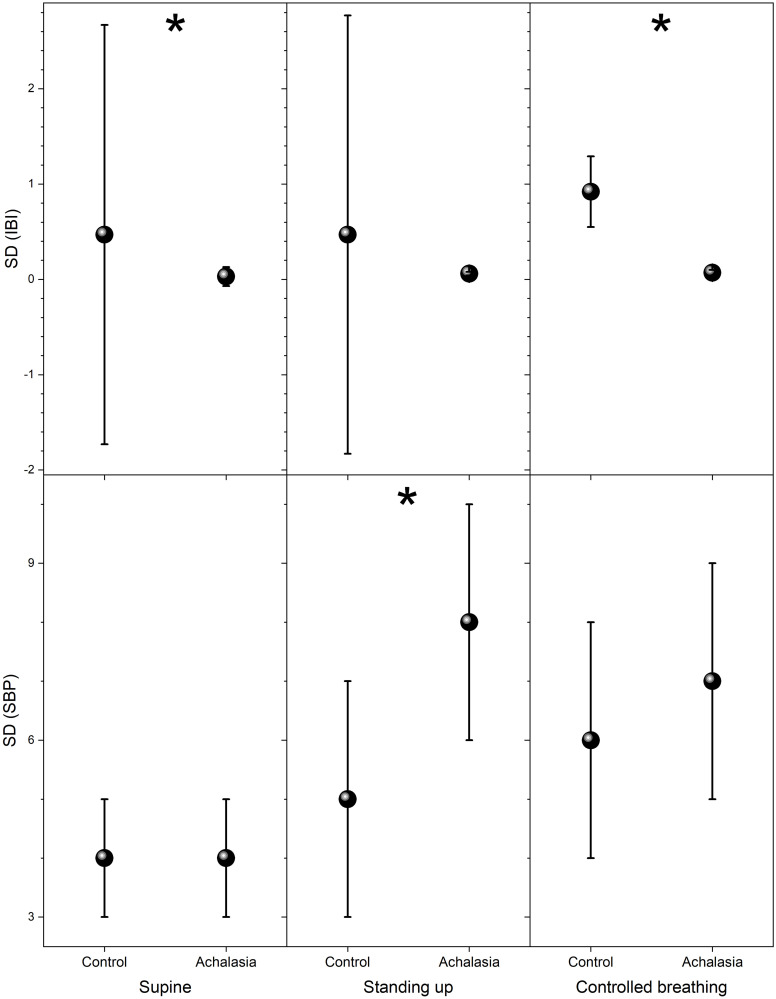
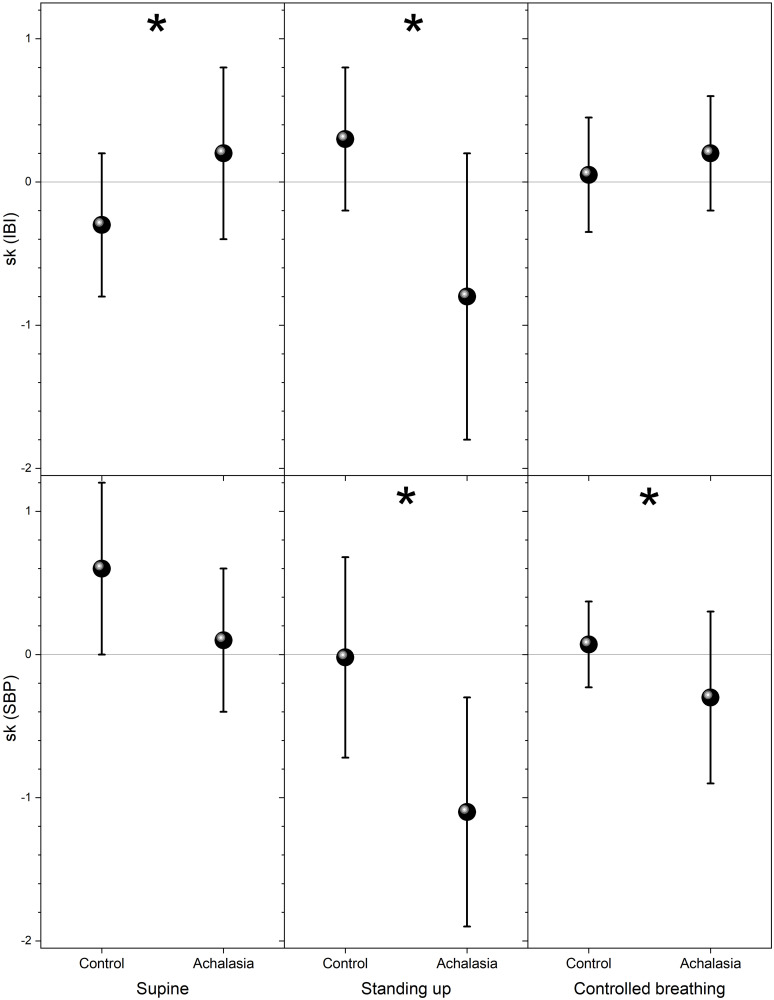
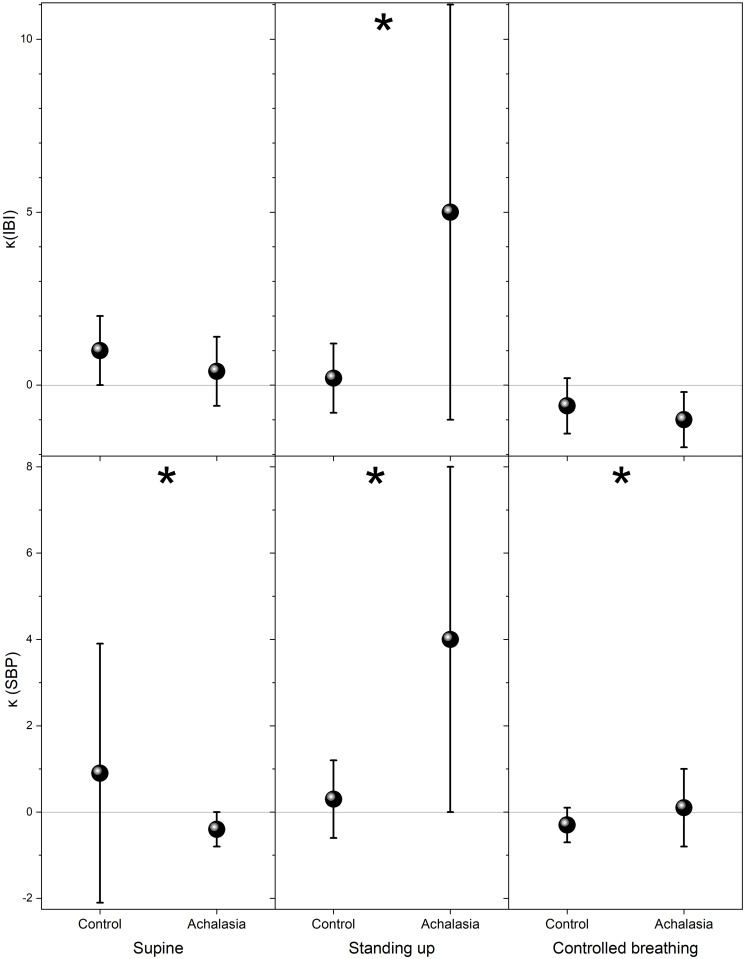
The usual parameter employed in HRV analysis to distinguish health from illness is the standard deviation of the IBI and SBP records, which we plot for comparison in Fig 4. For IBI, statistically significant separation of the groups is on the controlled breathing test, while for SBP is standing up (see Tables 1 and 2). Higher statistical moments of the distribution are shown in Fig 5 (skewness with respect to the median) and in Fig 6 (kurtosis with respect to the median) for control subjects and achalasia patients’ groups during all the autonomic reflex tests. Qualitatively, a negative skewness indicates that the tail on the left side of the probability density function is longer than the right side and the bulk of the values lie to the right of the mean, while a positive skewness indicates that the bulk of the values lie to the left of the mean. In these graphs, it is possible to visually separate the different groups, especially for IBI in supine position and SBP under controlled breathing. In all these tests, control subjects present a larger dispersion of the data in IBI and SBP records than achalasia patients (Tables 1 and 2).
Fig 4. Standard deviation of detrended data for the different groups for IBI (upper panels) and SBP (bottom panels) during supine position (left-hand panels), standing up (middle panels), and controlled breathing (right-hand panels).
The vertical crosshair corresponds to one standard deviation around the population average, while the dot is the median; * indicates statistically significant difference with respect to control (p value < 0.05).
Fig 5. Skewness with respect to the median for control and achalasia groups during supine position (left-hand panels), standing up (middle panels), and controlled breathing (right-hand panels), IBI (top row), and SBP (bottom row).
The vertical crosshair corresponds to one standard deviation around the population average, while the dot is the median; * indicates statistically significant difference with respect to control (p value <0.05).
Fig 6. Kurtosis with respect to the median for control and achalasia groups during supine position (left-hand panels), standing up (middle panels), and controlled breathing (right-hand panels), IBI (top row) and SBP (bottom row).
The vertical crosshair corresponds to one standard deviation around the population average, while the dot is the median; * indicates statistically significant difference with respect to control (p value <0.05).
Table 3 resumes the results for IBI analysis in the frequency domain for control [72] and achalasia patients. For achalasia patients, HF is the same for all the maneuvers, LF and rF standing up or in supine position are similar, while under rhythmic breathing, LF and rF are one order of magnitude larger, LF/HF increases from supine position to standing up and doubles under controlled breathing. Power spectral density (PSD) standing up is almost scale invariant (slope close to -1). For rhythmic breathing at 0.1 Hz, the PSD shows stronger time series correlation, more like Brownian motion than free scale. Under controlled breathing at 0.1 Hz, achalasia patients also show a characteristic resonance peak showing that they do not lose the cardio-respiratory coupling, in contrast with diabetic patients [55]. However, LF, HF and rF are statistically significant different for all maneuvers for achalasia patients (Table 3).
Table 3. Interbeat interval in the frequency domain.
| Maneuver | Sex | LF (s2) (0.04–0.15 Hz) | HF (s2) (0.14–0.4 Hz) | LF/HF | rF (s2) | slope PSD (s2) | β | |
|---|---|---|---|---|---|---|---|---|
| Control | Supine | F | 6 ± 3 | 9 ± 3 | 0.7 ± 0.2 | 11 ± 4 | -0.6 ± 0.5 | |
| M | 7 ± 3 | 10 ± 4 | 0.7 ± 0.3 | 12 ± 4 | -1.0 ± 0.4 | |||
| Standing up | F | 10 ± 3 | 11 ± 4 | 0.9 ± 0.3 | 15 ± 4 | -0.8 ± 0.6 | ||
| M | 12 ± 5 | 11 ± 3 | 1.2 ± 0.3 | 16 ± 6 | -1.1 ± 0.9 | |||
| Breathing at 0.1 Hz | F | 16 ± 7 | 12 ± 6 | 1.5 ± 0.4 | 20 ± 9 | -1.2 ± 0.4 | 0.29 ± 0.07 | |
| M | 15 ± 5 | 10 ± 4 | 1.5 ± 0.4 | 18 ± 6 | -1.2 ± 0.3 | 0.3 ± 0.1 | ||
| Achalasia | Supine | F | 4 ± 2 | 5 ± 3* (p = 0.01) | 0.8 ± 0.2 | 6 ± 4* (p = 0.002) | -0.3 ± 0.9 | |
| M | 5 ± 1* | 7 ± 1* (p = 0.02) | 0.7 ± 0.2 | 9 ± 2* (p = 0.007) | -0.4 ± 0.8 * (p = 0.01) | |||
| Standing up | F | 4 ± 2* | 4 ± 2*(p = 0.0005) | 1.0 ± 0.2 | 6 ± 3* (p = 0.0001) | -0.5 ± 0.7 | ||
| M | 8 ± 3* | 6 ± 1* (p = 0.003) | 1.4 ± 0.4 | 10 ± 3* (p = 0.01) | -0.8 ± 0.6 * (p = 0.02) | |||
| Breathing at 0.1 Hz | F | 14 ± 6 | 6 ± 1* (p = 0.03) | 2.5 ± 0.9* (p = 0.02) | 15 ± 6 | -1.7 ± 0.7 * (p = 0.02) | 0.3 ± 0.1 | |
| M | 18 ± 4 | 6 ± 2* (p = 0.04) | 3.1 ± 0.7* (p = 0.01) | 19 ± 4 | -1.7 ± 0.7 * (p = 0.02) | 0.3 ± 0.2 |
* indicates statistically significant difference with respect to control (p value <0.05).
Results for the homeostatic measure parameter α appear in Table 4. For achalasia patients, HMP α is similar under all maneuvers, reflecting that for the achalasia patients it is more difficult to respond to external changes, they have parameters that are more rigid but during the upright position also the ratio between the frequency radius of IBI and SBP decreases significantly. Controlled breathing allows us to distinguish the populations. During this test, control subjects have higher values of α with large SD reflecting the correlation between IBI and SBP. With achalasia, HMPα diminishes not only in value but also in variability. That is, not only the heart response becomes more rigid, but the variability of the blood pressure also increases, in agreement with HRV being a protective health factor and blood pressure variability a risk factor.
Table 4. Homeostatic measure parameter α.
| Maneuver | Sex | α for control | α for achalasia |
|---|---|---|---|
| Supine | F | 2.1 ± 2 | 1.9 ± 2 |
| M | 2.6 ± 3 | 1.5 ± 1 * (p = 0.03) | |
| Standing up | F | 1.1 ± 0.9 | 2.4 ± 3 * (p = 0.04) |
| M | 1.3 ± 1 | 1.4 ± 1 | |
| Rhythmic breathing (0.1 Hz) | F | 2.2 ± 1 | 2.1 ± 1 |
| M | 1.5 ± 1 | 1.7 ± 1 |
* indicates statistically significant difference with respect to control (p value <0.05).
Conclusions
The analysis of IBI and SBP detrended time series in the time domain shows that all moments of the distribution are relevant parameters that allow significant differentiation between control subjects and achalasia patients, they also indicate harm to the parasympathetic damage to the heart that is concomitant to the vagal damage to the esophagus. The analysis in this study is relatively simple to perform in patients, since it only employs the moments of the distributions and their ratios, so it can be relatively easily adapted to clinical inspection and quantitative evaluation.
Supporting information
(PDF)
(PDF)
Dots are detrended data points and continuous line is interpolation.
(PDF)
Data Availability
All results from the processing and interpretation of the experimental data are included in the manuscript. Due to patient confidentiality issues and legal restrictions of the experimental protocol approved by the Ethical Committee of the "Instituto Nacional de Ciencias Medicas y Nutrición Salvador Zubiran" (INCMN), Mexico, the original de-identified data set is not publicly available on the web, but can be obtained by any interested parties upon request to the coordinator of the research committee of INCMN (carlos.aguilars@incmnsz.mx).
Funding Statement
This work was partially financially supported by CONACyT through grants FORDECYT-PRONACES 610285/2020, 263377/2020, the Universidad Nacional Autónoma de México through grants DGAPA-PAPIIT IA100120 and IN113619.
References
- 1.Furness JB. The enteric nervous system and neurogastroenterology. Nat Rev Gastroenterol Hepatol 2012; 9(5): 286. 10.1038/nrgastro.2012.32 [DOI] [PubMed] [Google Scholar]
- 2.Furuzawa-Carballeda J, Aguilar-León D, Gamboa-Domínguez A, Valdovinos MA, Nuñez-Álvarez C, Martín-del-Campo LA, et al. Achalasia—an autoimmune inflammatory disease: a cross-sectional study. J Immunol Res 2015; 2015: 729217. 10.1155/2015/729217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen RP, Martin AV, Pellegrini CA, and Oelschlager BK. Synopsis of investigations into proposed theories on the etiology of achalasia. Dis Esophagus 2012; 25(4): 305–310. 10.1111/j.1442-2050.2009.01030.x [DOI] [PubMed] [Google Scholar]
- 4.Bruley des Varannes S, Chevalier J, Pimont S, Le Neel JC, Klotz M, Schafer KH, et al. Serum from achalasia patients alters neurochemical coding in the myenteric plexus and nitric oxide mediated motor response in normal human fundus. Gut 2006; 55: 319–326. 10.1136/gut.2005.070011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, et al. Endoscopic and surgical treatments for Achalasia: A systematic review and meta-analysis. Ann Surg 2009; 249(1): 45–57. 10.1097/SLA.0b013e31818e43ab [DOI] [PubMed] [Google Scholar]
- 6.Mayberry JF. Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am 2001; 11(2): 235–247. 10.1016/S1052-5157(18)30068-0 [DOI] [PubMed] [Google Scholar]
- 7.Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, and Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008; 135(5): 1526–1533. 10.1053/j.gastro.2008.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furuzawa-Carballeda J, Zuñiga J, Hernández-Zaragoza DI, et al. An original Eurasian haplotype, HLA-DRB1*14:54-DQB1*05:03, influences the susceptibility to idiopathic achalasia. PLoS One 2018; 13(8): e0201676. 10.1371/journal.pone.0201676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Csendes A, Smok G, Braghetto I, Gonzalez P, Henriques A, Csendes P, et al. Histological studies of Auerbach’s plexuses of the oesophagus, stomach, jejunum, and colon in patients with achalasia of the oesophagus: presence of parietal cells and gastric emptying of solids. Gut 1992; 33: 150–154. 10.1136/gut.33.2.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franzini C, Pellegrino C. Electron Microscopy (5th International Congress of Electron Microscopy, Philadelphia, Pennsylvania). New York: Academic Press, 1962: 55–61. [Google Scholar]
- 11.Cassella RR, Brown AL Jr, Sayre GP, Ellis FH Jr. Achalasia of the esophagus: pathologic and etiologic considerations. Ann Surg 1964; 160474–87. 10.1097/00000658-196409000-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cassella RR, Ellis FH Jr, Brown AL Jr. Fine-structure changes in achalasia of the esophagus. Am I. Pathol 1965; 46: 279–288. [PMC free article] [PubMed] [Google Scholar]
- 13.Smith B. The neurological lesion in achalasia of the cardia. Gut 1970; 11: 388–391. 10.1136/gut.11.5.388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De la Fuente A, Garcia-Calvo M, Ramon Y Cajal S, Paya JM, Cuesta G. Alteraciones ultraestructurales del nervio vago en la acalasia del esofago. Rev ESP Enf Ap Digest 1977; 51: 659–666. [PubMed] [Google Scholar]
- 15.Qualman SJ, Haupt HM, Yang P, Hamilton SR. Esophageal Lewy bodies associated with ganglion cell loss in achalasia. Similarity to Parkinson’s disease. Gastroenterology 1984; 87: 848–856. 10.1016/0016-5085(84)90079-9 [DOI] [PubMed] [Google Scholar]
- 16.Ge F, Li Z, Ke M. Abnormal cardiovascular re exes in patients with achalasia. Chin Med Sci J 1994; 9: 194–196. [PubMed] [Google Scholar]
- 17.Dooley CP, Taylor IL, Valenzuela JE. Impaired acid secretion and pancreatic polypeptide release in some patients with achalasia. Gastroenterology 1983; 84: 809–13. 10.1016/0016-5085(83)90150-6 [DOI] [PubMed] [Google Scholar]
- 18.Eckardt VF, Krause, Bolle D. Gastrointestinal transit and gastric acid secretion in patients with achalasia. Dig Dis Scz 1989; 34: 665–671. 10.1007/BF01540335 [DOI] [PubMed] [Google Scholar]
- 19.Annese V, Caruso N, Accadia L, et al. Gallbladder function and gastric liquid cmptying in achalasia. Dig Dis Sci 1991; 36: 1116–1120. 10.1007/BF01297456 [DOI] [PubMed] [Google Scholar]
- 20.Benini L, Castellani G, Sembenini C, et al. Gastric emptying of solid meals in achalasic patients after successful pneumatic dilatation of the cardia. Dig DIS Sci 1994; 39: 733–737. 10.1007/BF02087415 [DOI] [PubMed] [Google Scholar]
- 21.Bittinger M, Barnet J, Eberl T, Wienbeck M. Postprandial gastric relaxation in achalasia. Eur J Gastroenterol Hepatol 1998; 10: 741–744. 10.1097/00042737-199809000-00003 [DOI] [PubMed] [Google Scholar]
- 22.Mearin F, Papo M, Malagelada JR. Impaired gastric relaxdsation in patients with achalasia. Gut 1995; 36: 363–368. 10.1136/gut.36.3.363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erckenbrecht JF, Berges W, Wienbeck M. Interdigestive Dunndarmmotilitat bei Achalasie. Z Gastroenterologie 1983; 21: 249. [Google Scholar]
- 24.Kellow JE, Gill RC, Wingate DL, Calam IE. Small bowel motor activity and bacterial overgrowth. Gastrointest Mot 1990; 2: 180–183. [Google Scholar]
- 25.Camilleri M, Malagelada JR, Stanghellini V, Fealey RD, Sheps SG. Gastrointestinal motility disturbances in patients with orthostatic hypotension. Gastroenterology 1985; 88: 1852–1859. 10.1016/0016-5085(85)90010-1 [DOI] [PubMed] [Google Scholar]
- 26.Hopkins A., Neville B., & Bannister R. Autonomic neuropathy of acute onset. The Lancet, 1974; 303(7861): 769–771. 10.1016/s0140-6736(74)92840-2 [DOI] [PubMed] [Google Scholar]
- 27.Allgrove J, Clayden GS, Grant DB. Familial glucocorticoid deficiency with achalasia of the cardia and deficient tear production. Lancet 1978; 17: 1284–1286. 10.1016/s0140-6736(78)91268-0 [DOI] [PubMed] [Google Scholar]
- 28.Stuckey BG, Mastaglia FL, Reed D, Pullan PT: Glucocorticoid insufficiency, achalasia, alacrima with autonomic and motor neuropathy. Ann Intern Med 1987; 106(1): 62–64. 10.7326/0003-4819-106-1-62 [DOI] [PubMed] [Google Scholar]
- 29.Maayan C, Oren A, Goldin E, Dinour D, Goldberg M, Molge P: Megaesophagus and recurrent apnea in an adult patient with familial dysautonomia. Am J Gastroenterol 1990; 85(6): 729–732. [PubMed] [Google Scholar]
- 30.Firouzi M, Keshavarzian A. Guillain-Barré syndrome and achalasia: Two manifestations of a viral disease or coincidental association? Am J Gastroenterol 1994; 89(9): 1585–1587. [PubMed] [Google Scholar]
- 31.Stewart IM, Hosking DJ, Preston BJ, Atkinson M: Oesophageal motor changes in diabetes mellitus. Thorax 1976; 31: 278–283. 10.1136/thx.31.3.278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hollis JB, Castell DO, Braddom RL: Esophageal function in diabetes mellitus and its relation to peripheral neuropathy. Gastroenterology 1977; 73: 1098–1102. 10.1016/S0016-5085(19)31865-7 [DOI] [PubMed] [Google Scholar]
- 33.Russell C, Gannan R, Coatsworth J et al. Relationship among esophageal dysfunction diabetic gastroenteropathy and peripherical neuropathy. Dig Dis Sci 1983; 28: 289–293. 10.1007/BF01324943 [DOI] [PubMed] [Google Scholar]
- 34.Espi F, Soria T, Ortiz MA, Benages A, Parrilla P, Carmena R. Neuropatía autonómica y peristaltismo esofágico en la diabetes mellitus: análisis de 30 pacientes. Cir Esp 1987; 41: 237–239. [Google Scholar]
- 35.Lluch I, Ascaso JF, Mora F, et al. Gastroesophagealrefluxin diabetes mellitus. Am J Gastroenterol 1999; 94: 919–924. 10.1111/j.1572-0241.1999.987_j.x [DOI] [PubMed] [Google Scholar]
- 36.Ascaso JF, Herreros B, Sanchiz V et al. Oesophageal motility disorders in type I diabetes mellitus and their relation to cardiovascular autonomic neuropathy. Neurogastroenterol Motil 2006; 18: 813–822. 10.1111/j.1365-2982.2006.00799.x [DOI] [PubMed] [Google Scholar]
- 37.Eckardt VF, Stenner F, Liewen H, Röder R, Koop H, Bernhard G. Autonomic dysfunction in patients with achalasia. Neurogastroenterol Motil 1995; 7(1): 55–61. 10.1111/j.1365-2982.1995.tb00209.x [DOI] [PubMed] [Google Scholar]
- 38.von Herbay A, Heyer T, Olk W, Kiesewalter B, Auer P, Enck P, et al. Autonomic dysfunction in patients with achalasia of the oesophagus. Neurogastroenterol Motil 1998; 10(5): 387–93. 10.1046/j.1365-2982.1998.00120.x [DOI] [PubMed] [Google Scholar]
- 39.Olk W, Kiesewalter B, Auer P, Enck P, Kuhlbusch R, Von Giesen HJ, et al. Extraesophageal autonomic dysfunction in patients with achalasia. Dig Dis Sci 1999; 44(10): 2088–93. 10.1023/a:1026638822259 [DOI] [PubMed] [Google Scholar]
- 40.Ohlsson B, Ekberg O, Sundkvist G. Achalasia: a vagal disease. Scand J Gastroenterol 2004; 39(6):527–30. 10.1080/00365520410004460 [DOI] [PubMed] [Google Scholar]
- 41.Atkinson M, Ogilvie AL, Rovertson CS, Smart HL. Vagal function in achalasia of the cardia. Q J Med 1987; 63(240): 297–303. 10.1080/00365520410004460 [DOI] [PubMed] [Google Scholar]
- 42.Trudgill NJ, Hussain FN, Smith LF, Riley SA. Studies of autonomic function in patients with achalasia and nutcracker oesophagus. Eur J Gastroenterol Hepatol 1999; 11(12): 1349–1354. 10.1097/00042737-199912000-00002 [DOI] [PubMed] [Google Scholar]
- 43.Rinaldi R, Cortelli P, Di Simone MP, Pierangeli G, D’Alessandro R, Mattioli S. Cardiovascular autonomic function in patients with primary achalasia. Dig Dis Sci 2000; 45(4): 825–829. 10.1023/a:1005472400263 [DOI] [PubMed] [Google Scholar]
- 44.Herreros B, Ascaso JF, Mora F, Costa AJ, Sanchiz V, Minguez M, et al. Absence of cardiovascular autonomic dysfunction and vagal pancreatic impairment in idiopathic achalasia of the oesophagus. Neurogastroenterol Motil 2007; 19(8): 646–52. 10.1111/j.1365-2982.2007.00920.x [DOI] [PubMed] [Google Scholar]
- 45.Fossion R, Rivera AL, and Estañol B. A physicist’s view of homeostasis: How time series of continuous monitoring reflect the function of physiological variables in regulatory mechanisms. Physiol Meas. 2018; 39(8): 084007. 10.1088/1361-6579/aad8db [DOI] [PubMed] [Google Scholar]
- 46.Bauer A, Kantelhardt JW, Barthel P, Schneider R, Mäkikallio T, Ulm K, et al. Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: cohort study. Lancet 2006; 367: 1674–1681. 10.1016/S0140-6736(06)68735-7 [DOI] [PubMed] [Google Scholar]
- 47.Levy MN. Sympathetic-parasympathetic interactions in the heart. Circ Res 1971; 29: 437–445. 10.1161/01.res.29.5.437 [DOI] [PubMed] [Google Scholar]
- 48.Robles-Cabrera A, Michel-Chávez A, Callejas-Rojas RC, Malamud-Kessler C, Delgado G, and Estañol-Vidal B. The cardiovagal, cardiosympathetic and vasosympathetic arterial baroreflexes and the control of blood pressure. Rev Neurol 2014; 59(11): 508–516. [PubMed] [Google Scholar]
- 49.Estañol B, Rivera AL, Martínez-Memije R, Fossion R, Gómez F, Bernal K, et al. From supine to standing: in vivo segregation of myogenic and baroreceptor vasoconstriction in humans. Physiol Rep 2016; 4(24): e13053. 10.14814/phy2.13053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, and Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat to beat cardiovascular control. Science 1981; 213(4504): 220–222. 10.1126/science.6166045 [DOI] [PubMed] [Google Scholar]
- 51.Malliani A, Pagani M, Lombardi F, and Cerutti S. Cardiovascular neural regulation explored in the frequency domain. Circulation 1991; 84: 1482–1492. 10.1161/01.cir.84.2.482 [DOI] [PubMed] [Google Scholar]
- 52.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 1996; 17: 354–381. 10.1161/01.CIR.93.5.1043 [DOI] [PubMed] [Google Scholar]
- 53.Berntson GG, Bigger JT, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology 1997; 34: 623–648. 10.1111/j.1469-8986.1997.tb02140.x [DOI] [PubMed] [Google Scholar]
- 54.Rivera AL, Estañol B, Sentíes-Madrid H, Fossion R, Toledo-Roy JC, Mendoza-Temis J, et al. Heart rate and systolic blood pressure variability in the time domain in patients with recent and long-standing Diabetes Mellitus. PLoS One 2016; 11(2): e0148378. 10.1371/journal.pone.0148378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rivera AL, Estañol B, Fossion R, Toledo-Roy JC, Callejas-Rojas RC, Gien-López JA, et al. Loss of breathing modulation of heart rate variability in patients with recent and long standing Diabetes Mellitus type II. PLoS One 2016; 11(11): e0165904. 10.1371/journal.pone.0165904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rivera AL, Estañol B, Toledo-Roy JC, Fossion R, and Frank A. Looking for biomarkers in physiological time series, in Quantitative Models for Microscopic to Macroscopic Biological Macromolecules and Tissues, 2018. ed. Olivares L, Resendis O, Springer, pp. 111–131. 10.1007/978-3-319-73975-5_6 [DOI] [Google Scholar]
- 57.Fossion R, Fossion JPJ, Rivera AL, Lecona OA, Toledo-Roy JC, García-Pelagio KP, et al. Homeostasis from a Time-Series Perspective: An Intuitive Interpretation of the Variability of Physiological Variables, in Quantitative Models for Microscopic to Macroscopic Biological Macromolecules and Tissues, 2018b. ed. Olivares L, Resendis O, Springer, pp. 111–131. 10.1007/978-3-319-73975-5_5 [DOI] [Google Scholar]
- 58.Fossion R, Sáenz–Burrola A, Zapata–Fonseca L. On the stability and adaptability of human physiology: Gaussians meet heavy–tailed distributions. Interdisciplina 2020; 8(20): 55–81. 10.22201/ceiich.24485705e.2020.20.71195 [DOI] [Google Scholar]
- 59.Rivera A. L., Toledo-Roy J. C., Frank A. Symmetry, and signs of self-organized criticality in living organisms. J. Phys.: Conf. Ser. 1612:012024. 10.1088/1742-6596/1612/1/012024 [DOI] [Google Scholar]
- 60.Kitney RI, Byrne S, Edmonds ME, Watkins PJ, and Roberts VC. Heart rate variability in the assessment of autonomic diabetic neuropathy. Automedica 1982; 4: 155–167. [Google Scholar]
- 61.Appel ML, Berger RD, Saul JP, Smith JM, and Cohen RJ. Beat to beat variability in cardiovascular variables: Noise or music? J Am Coll Cardiol 1989; 14: 1139–1148. 10.1016/0735-1097(89)90408-7 [DOI] [PubMed] [Google Scholar]
- 62.Freeman R, Saul JP, Roberts MS, Berger RD, Broadbridge C, and Cohen RJ. Spectral analysis of heart rate in diabetic autonomic neuropathy: a comparison with standard tests of autonomic function. Arch Neurol 1991; 48(2): 185–190. 10.1001/archneur.1991.00530140079020 [DOI] [PubMed] [Google Scholar]
- 63.American Diabetes Association and the American Academy of Neurology. Consensus statement: Standardized measure in diabetes neuropathy. Diabetes Care 1995; 18(Supp 1): 59–82. 10.2337/diacare.18.1.S59 [DOI] [Google Scholar]
- 64.Ziegler D, Zentai CP, Perz S, Rathmann W, Haastert B, Döring A, et al. Prediction of mortality using measures of cardiac autonomic dysfunction in the diabetic and nondiabetic population: the MONICA/KORA Augsburg Cohort Study. Diabetes Care 2008; 31: 556–561. 10.2337/dc07-1615 [DOI] [PubMed] [Google Scholar]
- 65.Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010; 33(10): 2285–2293. 10.2337/dc10-1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Michel-Chávez A, Estañol B, Gien-López JA, Robles-Cabrera A, Huitrado-Duarte ME, Moreno-Morales R, et al. Variabilidade da frequência cardíaca e da pressão arterial sistólica em Diabéticos com diagnóstico recente. Arq Bras Cardiol 2015; 105(3): 276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mancia G, Ferrari A, Gregorini L, Parati G, et al. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ Res 1983; 53: 96–104. 10.1161/01.res.53.1.96 [DOI] [PubMed] [Google Scholar]
- 68.Floras JS. Blood pressure variability: A novel and important risk factor. Canad J Cardiol 2013; 29: 557–563. 10.1016/j.cjca.2013.02.012 [DOI] [PubMed] [Google Scholar]
- 69.Parati G, Ochoa JE, Lombardi C, and Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol 2013; 10: 143–155. 10.1038/nrcardio.2013.1 [DOI] [PubMed] [Google Scholar]
- 70.Parati G, Ochoa JE, Salvi P, Lombardi C, and Bilo G. Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care 2013; 36: S312–S324. 10.2337/dcS13-2043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eckert S, and Horstkotte D. Comparison of Portapres non-invasive blood pressure measurement in the finger with intra-aortic pressure measurement during incremental bicycle exercise. Blood Press Monit 2002; 7(3): 179–183. 10.1097/00126097-200206000-00006 [DOI] [PubMed] [Google Scholar]
- 72.Lavín-Pérez R, Diferencias de género y edad en la variabilidad a corto plazo de la frecuencia cardíaca. Master Degree Thesis. (Universidad Nacional Autónoma de México, México, 2018). http://132.248.9.195/ptd2018/mayo/0774746/Index.html.
- 73.Corrales M, Torres B, Esquivel A, Salazar M, and Naranjo Orellana J. Normal values of heart rate variability at rest in a young, healthy and active Mexican population. Health 2012; 4: 377–385. 10.4236/health.2012.47060 [DOI] [Google Scholar]
- 74.Huang NE, Shen Z, Long SR, Wu MC, Shih HH, Zheng Q, et al. The empirical mode decomposition and the Hilbert spectrum for nonlinear and non-stationary time series analysis. Proc R Soc Lon Ser-A 1998; 454: 903–993. 10.1098/rspa.1998.0193 26953177 [DOI] [Google Scholar]
- 75.Griffin MP, and Moorman JR. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 2001; 107: 97–104. 10.1542/peds.107.1.97 [DOI] [PubMed] [Google Scholar]
- 76.Shaffer F, and Ginsberg JP. An overview of heart rate variability metrics and norms. Frontiers in Public Health 2017; 5: 258. 10.3389/fpubh.2017.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Houle MS, & Billman GE. Low-frequency component of the heart rate variability spectrum: a poor marker of sympathetic activity. American Journal of Physiology-Heart and Circulatory Physiology 1999; 276(1): H215–H223. 10.1152/ajpheart.1999.276.1.H215 [DOI] [PubMed] [Google Scholar]
- 78.Reyes del Paso GA, Langewitz W, Mulder LJ, Van Roon A, & Duschek S. The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: a review with emphasis on a reanalysis of previous studies. Psychophysiology 2013; 50(5): 477–487. 10.1111/psyp.12027 [DOI] [PubMed] [Google Scholar]
- 79.Prokhorov MD, Ponomarenko VI, Gridnev VI, Bodrov MB, and Bespyatov AB. Synchronization between main rhythmic processes in the human cardiovascular system. Phys Rev E 2003; 68(4): 041913. 10.1103/PhysRevE.68.041913 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Dots are detrended data points and continuous line is interpolation.
(PDF)
Data Availability Statement
All results from the processing and interpretation of the experimental data are included in the manuscript. Due to patient confidentiality issues and legal restrictions of the experimental protocol approved by the Ethical Committee of the "Instituto Nacional de Ciencias Medicas y Nutrición Salvador Zubiran" (INCMN), Mexico, the original de-identified data set is not publicly available on the web, but can be obtained by any interested parties upon request to the coordinator of the research committee of INCMN (carlos.aguilars@incmnsz.mx).