Summary
Background
Hearing loss affects access to spoken language, which can affect cognition and development, and can negatively affect social wellbeing. We present updated estimates from the Global Burden of Disease (GBD) study on the prevalence of hearing loss in 2019, as well as the condition's associated disability.
Methods
We did systematic reviews of population-representative surveys on hearing loss prevalence from 1990 to 2019. We fitted nested meta-regression models for severity-specific prevalence, accounting for hearing aid coverage, cause, and the presence of tinnitus. We also forecasted the prevalence of hearing loss until 2050.
Findings
An estimated 1·57 billion (95% uncertainty interval 1·51–1·64) people globally had hearing loss in 2019, accounting for one in five people (20·3% [19·5–21·1]). Of these, 403·3 million (357·3–449·5) people had hearing loss that was moderate or higher in severity after adjusting for hearing aid use, and 430·4 million (381·7–479·6) without adjustment. The largest number of people with moderate-to-complete hearing loss resided in the Western Pacific region (127·1 million people [112·3–142·6]). Of all people with a hearing impairment, 62·1% (60·2–63·9) were older than 50 years. The Healthcare Access and Quality (HAQ) Index explained 65·8% of the variation in national age-standardised rates of years lived with disability, because countries with a low HAQ Index had higher rates of years lived with disability. By 2050, a projected 2·45 billion (2·35–2·56) people will have hearing loss, a 56·1% (47·3–65·2) increase from 2019, despite stable age-standardised prevalence.
Interpretation
As populations age, the number of people with hearing loss will increase. Interventions such as childhood screening, hearing aids, effective management of otitis media and meningitis, and cochlear implants have the potential to ameliorate this burden. Because the burden of moderate-to-complete hearing loss is concentrated in countries with low health-care quality and access, stronger health-care provision mechanisms are needed to reduce the burden of unaddressed hearing loss in these settings.
Funding
Bill & Melinda Gates Foundation and WHO.
Introduction
Hearing loss is common and can negatively affect multiple aspects of an individual's life when unaddressed or when individuals' communication needs are unsupported. Auditory deprivation can detract from quality of life and access to spoken communication, which can impede development of child spoken language1 and contribute to the risk of dementia2 and cognitive decline in older ages.3 Deafness in early life when unaddressed is associated with poor literacy outcomes and reduced employment opportunities in later life. The emotional effects of hearing loss can include loneliness, isolation, depression, and anxiety.4, 5, 6 In many countries, children with hearing loss rarely receive schooling7 and adults have a much higher unemployment rate compared with their hearing peers.8
The effect of hearing loss is broadly recognised by several stakeholders, including researchers, clinicians, policy makers, and people living with the condition.9 Announced during the celebration of World Hearing Day 2019, the Lancet Commission on Global Hearing Loss aims to examine how to reduce the burden of hearing loss, convening expert working groups on prevention, policy, technology, and protection.10 Efforts from The Lancet are complemented by plans from WHO to release the first-ever world report on hearing. The report seeks to utilise best available evidence to present a consistent narrative on hearing loss and hearing health care, call attention to priorities and best practices for hearing health care, and describe trends in the global distribution of hearing loss.11 Initiatives from researchers and other key decision makers underscore the relevance of hearing loss within the global health landscape and the condition's effects.
Researchers have called for urgent multi-disciplinary action on hearing health care, including comprehensive screening programmes, increased access to hearing devices, and noise-reduction strategies.12 Despite the effects of hearing loss on spoken communication and wellbeing, literature on the prevalence of hearing loss is relatively sparse, making the understanding of who is most affected and where resources should be allocated difficult.
Research in context.
Evidence before this study
The prevalence of hearing loss is estimated annually through the Global Burden of Disease (GBD) study, a systematic overview of the prevalence of 369 diseases and injuries. The latest GBD study on hearing loss was based on estimates from 10 years ago. Since then, we have obtained new sources of data through systematic reviews of population-representative studies, collaborator input, and additional targeted searches. Sources up to Dec 31, 2008, were obtained from a previously published systematic review. In GBD 2013, we did a systematic review of sources published 2008–13 onward using the following PubMed search string: “(hearing loss[Title/Abstract] OR deafness[Title/Abstract] OR hearing loss[Title/Abstract]) AND (prevalence[Title/Abstract]) AND (“2008”[PDAT] : “3000”[PDAT]) AND (cross sectional OR survey)”.
In GBD 2016, we did an update systematic review of sources published between Nov 26, 2008, and Nov 30, 2016, using the following PubMed search string: “(hearing loss[Title/Abstract] OR deafness[Title/Abstract] OR hearing loss[Title/Abstract] OR audiometry[Title/Abstract]) AND (prevalence[Title/Abstract]) AND (“2008/11/26”[PDAT]: “3000”[PDAT]) AND (cross sectional OR survey)”, without any language restrictions. Sources that included self-reported data, did not report hearing loss in the less severe ear, were not population representative, or did not report a definitive decibel-level threshold for reported hearing loss were excluded. Sources that reported bilateral hearing loss according to the GBD reference definition were included.
Added value of this study
The GBD hearing loss paper published in 2010 was informed by 42 studies in 29 countries. Our analysis provides an update that is informed by 215 survey sources from 77 countries. Method changes for the GBD 2019 iteration include new methods of adjusting data using non-standard hearing thresholds and splitting data with gender unspecified by sex. These GBD estimates are accompanied by forecasts of hearing loss prevalence until 2050, providing a comprehensive picture of current and future disease trends. We found that 1·57 billion people (95% uncertainty interval 1·51–1·64) had hearing loss in 2019, contributing to 43·45 million (29·68–61·80) years lived with disability as the third largest cause of disability in GBD. The global number of individuals with hearing loss is also projected to increase by 56·1% (47·3–65·2) in the next 30 years despite stable age-standardised prevalence.
Implications of all the available evidence
This study accompanies the 2021 WHO World Hearing Report, which describes the burden of hearing loss using the GBD 2019 results and standards for ear and hearing care, and sets standards for policy and prevention. Our analysis provides evidence that hearing loss is largely caused by ageing, will increase in prevalence in coming years, and is more prevalent in countries with low health-care access. Cost-effective, preventive, and treatment interventions for hearing loss are available, including school-based screening programmes, hearing devices (eg, hearing aids or cochlear implants), and clinical management of ear disease. Health-care services must be prepared for large projected increases in burden, particularly in low-income and middle-income countries where ear specialists and audiologists are scarce.
The Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study is a comprehensive attempt to quantify the contribution of hearing loss relative to other causes of ill health. The study provides annual data on the prevalence and associated levels of disability for 369 diseases and injuries, as well as 87 risk factors. Estimates are updated annually, most recently for GBD 2019—the most recent GBD paper on hearing loss was based on GBD 2010 estimates.13 In this Article, we aimed to estimate the prevalence, severity, and distribution of global hearing loss and added forecasts of future disease prevalence through 2050.
Methods
Overview
The 2019 GBD produced estimates for 369 diseases and injuries; high-level methods have been described in detail elsewhere.14 Data for the prevalence and incidence of non-fatal conditions were pooled in DisMod-MR 2.1, a Bayesian meta-regression tool (described elsewhere).15
In addition to prevalence and incidence, GBD uses the years lived with disability (YLDs) metric to compare the morbidity associated with different non-fatal conditions. YLDs are calculated by multiplying the prevalence of a condition with its associated disability weight, reflecting the severity of that disease relative to all other health states. Disability weights range from 0 (meaning perfect health) to 1, which is equivalent to death.
This study complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations (appendix p 16).16
Definition of hearing loss
GBD defines hearing loss as the quietest sound an individual can hear in their better ear, taken as the pure-tone average of audiometric thresholds of 0·5 kHz, 1 kHz, 2 kHz, and 4 kHz. Hearing loss is reported in the GBD by seven mutually exclusive severity categories (table 1).17 Two health states were assigned to each severity category on the basis of the presence of tinnitus, a ringing or buzzing in the ears that is associated with hearing loss.18 Moderate-to-complete hearing loss consisted of all hearing loss greater than 35 dB and is most often associated with reduced functional outcomes in individuals.11 All hearing loss is defined as any hearing loss above 20 dB, ranging from mild to complete in severity.
Table 1.
Hearing loss health states, lay descriptions, thresholds on pure tone audiometry, and disability weights
| Lay description | Range | Disability weight (95% UI) | |
|---|---|---|---|
| Normal | Normal hearing | 0–19 dB | 0 |
| Mild | Has great difficulty hearing and understanding another person talking in a noisy place (eg, on an urban street) | 20–34 dB | 0·010 (0·004–0·019) |
| Mild with ringing | Has great difficulty hearing and understanding another person talking in a noisy place (eg, on an urban street), and sometimes has annoying ringing in the ears | 20–34 dB | 0·021 (0·012–0·036) |
| Moderate | Is unable to hear and understand another person talking in a noisy place (eg, on an urban street), and has difficulty hearing another person talking even in a quiet place or on the telephone | 35–49 dB | 0·027 (0·015–0·042) |
| Moderate with ringing | Is unable to hear and understand another person talking in a noisy place (eg, on an urban street), and has difficulty hearing another person talking even in a quiet place or on the telephone, and has annoying ringing in the ears for more than 5 min at a time, almost every day | 35–49 dB | 0·074 (0·048–0·107) |
| Moderately severe | No lay description available | 50–64 dB | 0·092 (0·064–0·129) |
| Moderately severe with ringing | No lay description available | 50–64 dB | 0·167 (0·114–0·231) |
| Severe | Is unable to hear and understand another person talking, even in a quiet place, and unable to take part in a telephone conversation; difficulties with communicating and relating to others sometimes cause emotional effects (eg, worry or depression) | 65–79 dB | 0·158 (0·104–0·227) |
| Severe with ringing | Is unable to hear and understand another person talking, even in a quiet place, and unable to take part in a telephone conversation, and has annoying ringing in the ears for more than 5 min at a time, almost every day; difficulties with communicating and relating to others sometimes cause emotional effects (eg, worry or depression) | 65–79 dB | 0·261 (0·174–0·361) |
| Profound | Is unable to hear and understand another person talking, even in a quiet place, is unable to take part in a telephone conversation, and has great difficulty hearing anything in any other situation; difficulties with communicating and relating to others often cause worry, depression, and loneliness | 80–94 dB | 0·204 (0·134–0·288) |
| Profound with ringing | Is unable to hear and understand another person talking, even in a quiet place, is unable to take part in a telephone conversation, has great difficulty hearing anything in any other situation, and has annoying ringing in the ears for more than 5 min at a time, several times a day; difficulties with communicating and relating to others often cause worry, depression, or loneliness | 80–94 dB | 0·277 (0·182–0·388) |
| Complete | Cannot hear at all in any situation, including even the loudest sounds, and cannot communicate verbally or use a telephone; difficulties with communicating and relating to others often cause worry, depression, or loneliness | 95+ dB | 0·215 (0·143–0·307) |
| Complete with ringing | Cannot hear at all in any situation, including even the loudest sounds, and cannot communicate verbally or use a telephone, and has very annoying ringing in the ears for more than half of the day; difficulties with communicating and relating to others often cause worry, depression, or loneliness | 95+ dB | 0·316 (0·211–0·436) |
Lay descriptions as listed were used in GBD disability weight surveys (appendix p 3). GBD=Global Burden of Disease. UI=uncertainty interval.
This manuscript was produced as part of the GBD Collaborator Network and in accordance with the GBD Protocol.
Data processing
We used input data obtained via systematic reviews of epidemiological, population-representative surveys. Sources up to Nov 26, 2008, were obtained via a published systematic review, 19 and two additional systematic reviews done in 2013 and 2016 identified newer sources (appendix p 3). Sources were excluded that recorded self-reported hearing loss, were not population-representative, did not report bilateral (better ear) hearing loss, or did not use pure-tone audiometry to quantify hearing loss.
For data sources that reported prevalence by age and sex separately, we applied the proportion of female and male prevalence to age-specific data. We then ran a meta-regression on the log ratio of female and male prevalence in MR-BRT (meta-regression—Bayesian, regularised, trimmed; methodology has been described elsewhere14) and applied the model results to sex-split data reported for both sexes combined (appendix p 3).
Data sources that reported hearing loss by severity categories that differed from the GBD categories were adjusted using data from US National Health and Nutrition Examination surveys (NHANES).20 NHANES reported individual-level data on the exact decibel at which hearing loss was experienced. Adjustment factors were derived by running a meta-regression on the logit difference between the prevalence of the alternative and reference categories (appendix p 3). Data sources that reported prevalence in age groups larger than 20 years were split into 5-year age groups by applying the global age pattern of the GBD 2017 model.
Modelling strategy
To model hearing loss, we first ran three DisMod-MR 2.1 models to estimate the prevalence of no hearing loss (0–19 dB), mild hearing loss (20–34 dB), and moderate-to-complete hearing loss (≥35 dB). Socio-demographic Index (a summary measure of fertility, education, and gross domestic product)14 was used as a covariate in each model. These models were rescaled so that prevalence rates summed to one for each age, year, sex, and location. Second, we ran five DisMod models for the more severe levels of hearing loss and rescaled these to the prevalence of at least 35 dB hearing loss. Third, we ran one DisMod model for hearing aid coverage (defined as the proportion of individuals who use a hearing aid) and another for the proportion of hearing loss attributable to age-related or other factors. Uncertainty of final estimates was derived from the uncertainty in input data, data manipulations, and predictive covariates. We estimated uncertainty by running each model until convergence, then taking the 975th and 25th ordered draw from 1000 posterior model runs as 95% uncertainty intervals (UIs) for each point estimate.
Fourth, severity-specific prevalence of hearing loss was adjusted to account for hearing aid usage (appendix p 4). We calculated hearing aid coverage rates for each severity, age, sex, and location, using survey data and regression methods (appendix p 4). The identified proportion of individuals at each severity level who used a hearing aid were then shifted to the category directly below. Adjusted hearing loss refers to estimates that were adjusted downwards to account for hearing aid usage. By contrast, unadjusted hearing loss refers to estimates that were not adjusted downwards for hearing aid usage.
Fifth, we estimated the prevalence of hearing loss due to underlying causes—ie, chronic otitis media, congenital birth defects, meningitis, and age-related or other factors (appendix p 4). From birth to age 20 years, we scaled hearing loss prevalence due to congenital birth defects, otitis media, age-related and other factors, and meningitis to the total prevalence of each severity level. Above age 20 years, the difference between total hearing loss prevalence and hearing loss prevalence due to otitis media, meningitis, and congenital birth defects was assigned to age-related and other hearing loss.
Sixth, we estimated the prevalence of hearing loss with and without tinnitus (appendix p 5). We estimated the proportion of individuals with tinnitus using NHANES data, which reported the proportion of respondents with hearing impairment who experienced ringing, roaring, or buzzing. In the absence of cause-specific estimates of tinnitus, we assumed the same distribution across all causes. We applied proportions from NHANES data to our estimates to split hearing loss prevalence into prevalence with and without tinnitus.
Healthcare Access and Quality Indexand WHO regions
Results are presented by Healthcare Access and Quality (HAQ) Index as well as by WHO region. HAQ Index is a summary measure of the quality of national health systems that ranges from 0 to 100 and is based on analysis of avoidable deaths for 32 causes (methods described elsewhere).21
WHO member states are classified into six distinct regions: the Western Pacific region, South-East Asia region, European region, Region of the Americas, African region, and Eastern Mediterranean region (appendix p 6). Regional results in this paper are restricted to WHO member states and were produced in collaboration with WHO for the 2021 World Hearing Report.11
Forecasting global and regional hearing loss prevalence
Forecasts of hearing loss prevalence were generated using age-specific prevalence rates for the years 1990, 1995, 2000, 2005, 2010, 2015, and 2019 as input data into a regression, with year, WHO region, and age as predictors. We included an interaction term between region and year and a cubic spline on age. Sex-specific regression models were run 1000 times, and the resulting coefficients were used to predict rates in the years 2030, 2040, and 2050. Predicted rates were multiplied by forecasted population for each WHO location to obtain case numbers, and then aggregated to obtain global estimates.22
Results
Source counts were calculated by summing all surveys that were considered for incorporation into the model, including those that were eventually excluded from the analysis (because of poor survey methodology, etc). We counted a survey reporting data from multiple countries as multiple data sources. In total, input data consisted of 215 survey sources in 77 countries (surveys were only counted once in the total summation, even if they were used in multiple aspects of hearing loss estimation). Modelling of hearing loss prevalence considered 113 survey sources in 54 countries. Modelling of hearing aid coverage considered 100 survey sources in 44 countries. Other data came from ten data sources in two countries (data coverage and age-standardised coverage rates are shown in the appendix [pp 7, 9]).
An estimated 1·57 billion (95% UI 1·51–1·64) people had hearing loss in 2019, accounting for 20·3% (19·5–21·1) of the global population. Of these, 1·17 billion (1·12–1·22) people (74·3% [71·8–76·8]) had mild hearing loss. 12·65 million (10·34–15·48) individuals had complete hearing loss. Without adjustment for hearing aid use, 430·4 million (381·7–479·6) people globally had moderate-to-complete hearing loss in the better-hearing ear.
Globally, the number of people with moderate-to-complete hearing loss increased from 225·3 million (95% UI 197·6–250·9) in 1990, to 403·3 million (357·3–449·5) in 2019, a 79·1% (73·8–84·1) increase.
Age-standardised prevalence of moderate-to-complete hearing loss remained constant over the same period (age-standardised prevalence for all hearing loss is presented in the appendix [p 9]), ranging from 5·8% (95% UI 5·2–6·5) in the South-East Asia region to 3·5% (3·1–3·9) in the European region. The largest number of people with moderate-to-complete hearing loss resided in the Western Pacific region (127·1 million [112·3–142·6]), the South-East Asia region (103·4 million [90·9–115·4]), and the region of the Americas (58·8 million [51·7–66·2]; table 2).
Table 2.
Global and regional prevalent cases (in millions) and age-standardised prevalence by severity of hearing loss
| Age-standardised rate (95% UI) | Cases in millions (95% UI) | |
|---|---|---|
| Hearing loss, ≥20dB | ||
| Global | 19·3% (18·5–20·0) | 1571·3 (1511·9–1635·5) |
| African region | 18·9% (18·2–19·6) | 136·7 (130·1–143·4) |
| Eastern Mediterranean region | 14·9% (14·3–15·6) | 78·8 (75·3–82·4) |
| European region | 14·3% (13·7–15·0) | 194·5 (185·4–204·0) |
| Region of the Americas | 18·0% (17·3–18·9) | 215·5 (205·9–225·6) |
| South-East Asia region | 21·2% (20·4–22·0) | 400·0 (385·2–415·8) |
| Western Pacific region | 21·5% (20·7–22·3) | 540·2 (519·6–562·0) |
| Moderate-to-complete hearing loss, ≥35 dB | ||
| Global | 5·1% (4·5–5·6) | 403·3 (357·3–449·5) |
| African region | 5·4% (4·8–6·1) | 38·7 (33·1–44·5) |
| Eastern Mediterranean region | 4·7% (4·1–5·2) | 21·3 (18·6–23·9) |
| European region | 3·5% (3·1–3·9) | 52·8 (46·2–59·6) |
| Region of the Americas | 4·7% (4·2–5·3) | 58·8 (51·7–66·2) |
| South-East Asia region | 5·8% (5·2–6·5) | 103·4 (90·9–115·4) |
| Western Pacific region | 5·1% (4·5–5·7) | 127·1 (112·3–142·6) |
| Mild hearing loss, 20–34 dB | ||
| Global | 14·2% (13·6–14·8) | 1167·9 (1116·4–1219·6) |
| African region | 13·4% (12·8–14·0) | 98·0 (93·4–102·5) |
| Eastern Mediterranean region | 10·3% (9·8–10·7) | 57·6 (54·8–60·4) |
| European region | 10·8% (10·3–11·4) | 141·7 (134·8–148·9) |
| Region of the Americas | 13·3% (12·6–14·0) | 156·7 (148·0–165·1) |
| South-East Asia region | 15·3% (14·7–16·0) | 296·6 (284·0–309·3) |
| Western Pacific region | 16·4% (15·7–17·1) | 413·2 (393·3–431·4) |
| Moderate hearing loss, 35–49 dB | ||
| Global | 3·3% (2·9–3·8) | 268·8 (235·5–302·4) |
| African region | 3·2% (2·8–3·6) | 22·5 (19·0–26·3) |
| Eastern Mediterranean region | 3·0% (2·6–3·3) | 13·6 (11·8–15·4) |
| European region | 2·4% (2·1–2·7) | 36·2 (31·4–41·3) |
| Region of the Americas | 3·3% (2·9–3·7) | 41·1 (35·9–46·3) |
| South-East Asia region | 3·8% (3·4–4·3) | 69·1 (60·1–78·0) |
| Western Pacific region | 3·3% (2·9–3·7) | 85·5 (75·0–96·9) |
| Moderately severe hearing loss, 50–64 dB | ||
| Global | 1·1% (0·9–1·3) | 85·0 (71·6–101·3) |
| African region | 1·4% (1·2–1·6) | 8·8 (7·3–10·6) |
| Eastern Mediterranean region | 1·1% (0·9–1·3) | 4·7 (3·9–5·5) |
| European region | 0·7% (0·6–0·9) | 11·8 (9·6–14·3) |
| Region of the Americas | 0·9% (0·8–1·1) | 11·7 (9·7–14·1) |
| South-East Asia region | 1·3% (1·1–1·6) | 21·9 (18·1–26·3) |
| Western Pacific region | 1·0% (0·9–1·2) | 25·8 (21·5–31·2) |
| Severe hearing loss, 65–79 dB | ||
| Global | 0·3% (0·2–0·3) | 19·6 (15·8–24·1) |
| African region | 0·5% (0·4–0·6) | 3·7 (2·9–4·6) |
| Eastern Mediterranean region | 0·3% (0·2–0·3) | 1·2 (1·0–1·5) |
| European region | 0·1% (0·1–0·2) | 1·8 (1·4–2·3) |
| Region of the Americas | 0·2% (0·2–0·2) | 2·3 (1·8–2·9) |
| South-East Asia region | 0·3% (0·2–0·3) | 4·8 (3·8–6·0) |
| Western Pacific region | 0·2% (0·2–0·3) | 5·7 (4·5–7·1) |
| Profound hearing loss, 80–94 dB | ||
| Global | 0·2% (0·2–0·3) | 17·3 (13·7–21·5) |
| African region | 0·2% (0·2–0·3) | 2·0 (1·5–2·7) |
| Eastern Mediterranean region | 0·2% (0·1–0·2) | 1·1 (0·8–1·4) |
| European region | 0·1% (0·1–0·2) | 1·6 (1·3–2·0) |
| Region of the Americas | 0·2% (0·1–0·2) | 2·1 (1·7–2·7) |
| South-East Asia region | 0·2% (0·2–0·3) | 4·8 (3·7–6·1) |
| Western Pacific region | 0·3% (0·2–0·3) | 5·5 (4·4–6·9) |
| Complete hearing loss, ≥95 dB | ||
| Global | 0·2% (0·1–0·2) | 12·6 (10·3–15·5) |
| African region | 0·2% (0·2–0·2) | 1·7 (1·3–2·1) |
| Eastern Mediterranean region | 0·1% (<0·1–0·1) | 0·7 (0·5–0·8) |
| European region | 0·1% (<0·1–0·1) | 1·4 (1·1–1·7) |
| Region of the Americas | 0·1% (0·1–0·2) | 1·6 (1·3–1·9) |
| South-East Asia region | 0·2% (0·1–0·2) | 2·8 (2·2–3·5) |
| Western Pacific region | 0·2% (0·2–0·2) | 4·5 (3·7–5·5) |
UI=uncertainty interval.
Between 1990 and 2019, the global number of YLDs attributable to hearing loss increased by 73·6% (95% UI 67·1–79·2), from 25·02 million (16·96–35·34) to 43·45 million (29·68–61·80). Of the YLDs attributed to hearing loss in 2019, 65·2% (52·5–76·6) were caused by moderate-to-complete cases and 34·8% (23·4–47·5) were caused by mild cases. In 2019, 7·00 million (4·76–10·06) YLDs were attributable to occupational noise exposure (appendix p 5).
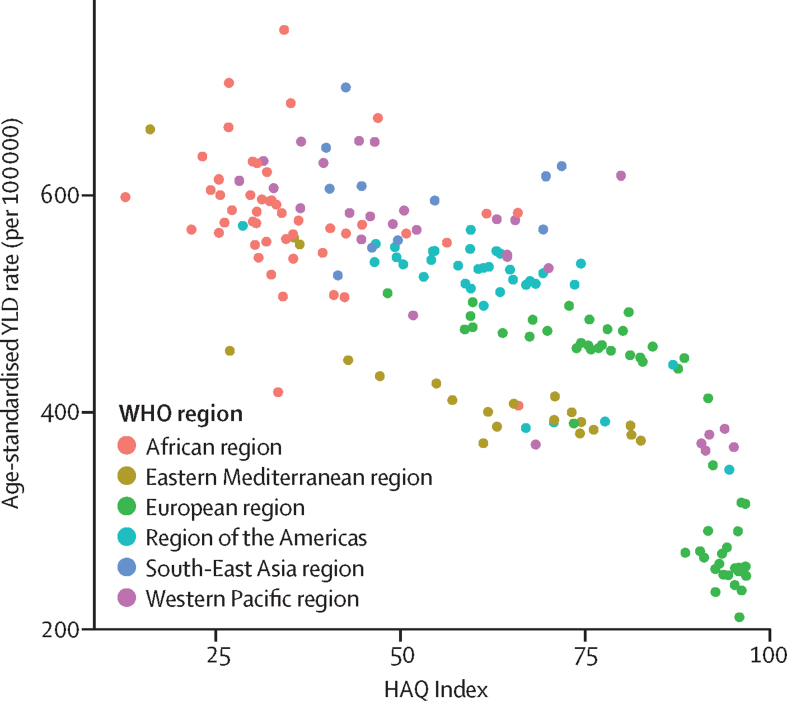
The burden of all hearing loss is greatest at lowest levels of the HAQ Index, with a difference of more than 3 times in YLD rates between countries with the lowest and highest HAQ Index values (figure 1). A linear regression analysis of age-standardised national YLD rates of hearing loss and HAQ Index found that HAQ Index explained 65·8% of the variation in YLD rates (adjusted r2 0·66).
Figure 1.
Age-standardised YLD rates for all hearing loss (per 100 000 population) by HAQ Index
HAQ=Healthcare Access and Quality. YLD=years lived with disability.
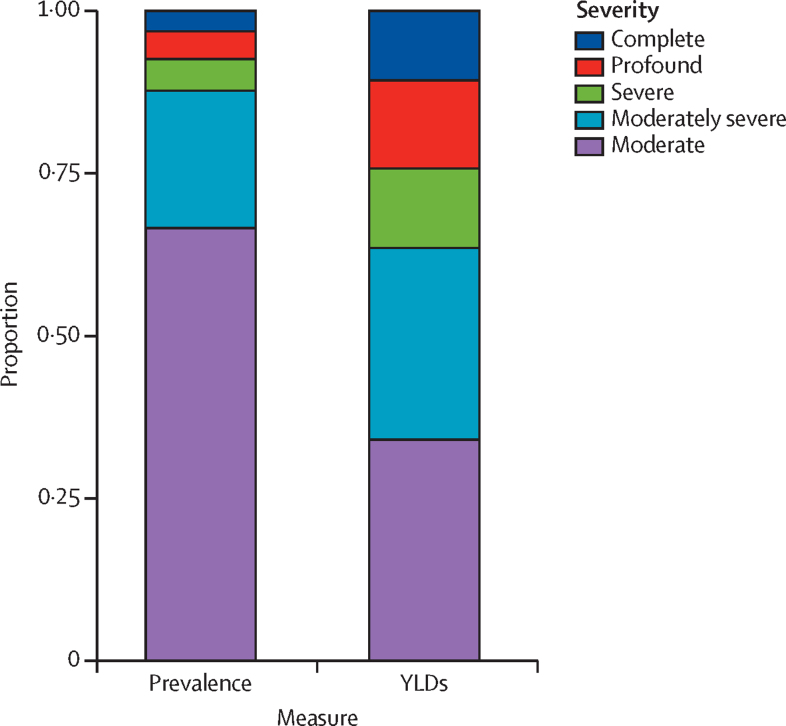
Although 66·6% (95% UI 62·9–69·9) of moderate-to-complete hearing loss cases were moderate in severity (35–49 dB), this severity accounted for 34·0% (26·2–42·6) of disability attributed to moderate-to-complete hearing loss (figure 2). Of all YLDs attributable to moderate-to-complete cases, 34·0% (26·2–42·6) were attributable to moderate cases, followed by moderately severe (29·6% [25·6–33·8]), profound (13·6% [10·5–17·2]), severe (12·1% [9·7–14·8]), and complete cases (10·7% [8·3–13·6]).
Figure 2.
Proportion of individuals with moderate-to-complete hearing loss by measure and severity
YLD=years lived with disability.
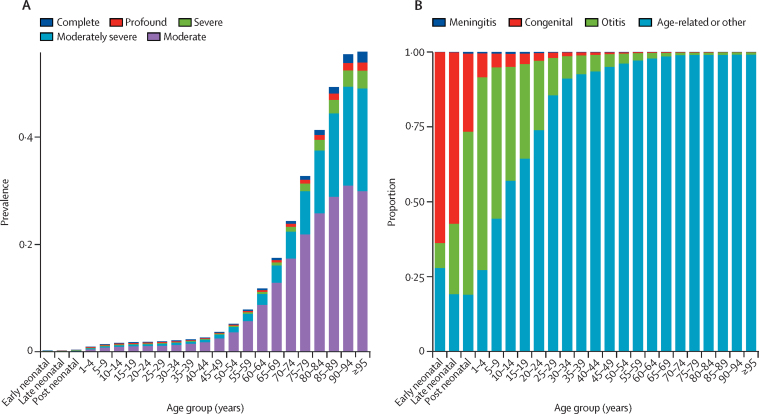
Across the age spectrum, hearing loss was most severe in those approximately younger than 5 years and those older than 70 years, meaning that the proportion of cases that were moderately severe, severe, profound, or complete was much larger in these age groups (appendix p 10). Hearing loss was also more prevalent at older ages, most notably after age 50 years (figure 3). In 2019, 62·1% (95% UI 60·2–63·9) of all people with hearing impairment were older than 50 years, and 4·4% (3·9–5·0) were younger than 15 years (69·7 million individuals [59·9–78·8]). Compared with other disease categories in the GBD, age-related and other hearing loss was the third largest cause of global YLDs in 2019, and the leading cause of global YLDs for individuals older than 70 years. Full rankings are available at GBD Compare.
Figure 3.
Prevalence of hearing loss 35 dB or greater by age, severity, and cause
Prevalence of hearing loss 35 dB or greater by age and severity (A) and proportion of individuals with hearing loss by age and cause for all severities (B).
The cause of hearing loss changed from infections and congenital birth defects to other factors over age (figure 3). Under age 5 years, hearing loss was mostly attributable to otitis media (63·7% [95% UI 56·9–70·2]). By comparison, 96·2% (94·5–97·6) of hearing loss was attributable to age-related and other factors for adults aged 50–54 years.
Between 1990 and 2019, the crude prevalence rate of all hearing loss increased by 27·8% (95% UI 26·6–29·0), from 15·9% (15·3–16·6) in 1990 to 20·3% (19·5–21·1) in 2019. By contrast, the global age-standardised prevalence rate of all hearing loss remained stable, changing from 19·1% (18·4–19·9) in 1990 to 19·3% (18·5–20·0) in 2019. The increase in hearing loss cases while age-standardised reates remained stable indicates that increases in prevalent cases are driven by population growth and ageing.
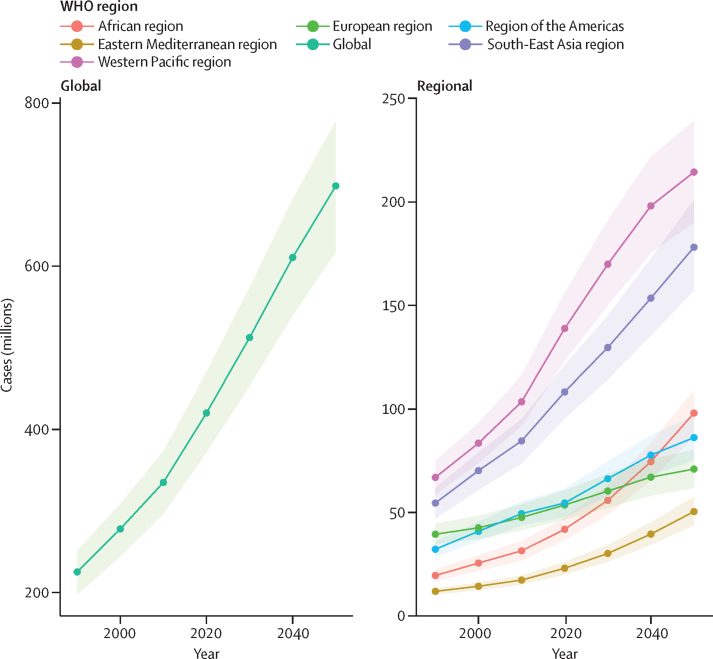
By 2050, a projected 2·45 billion (95% UI 2·35–2·56) people will have hearing loss, a 56·1% (47·3–65·2) increase from 2019, despite stable age-standardised prevalence (appendix p 15). An estimated 698·4 million (617·7–777·8) people will have moderate-to-complete hearing loss in 2050, with most people with moderate-to-complete hearing loss residing in the Western Pacific region (214·5 million [190·1–239·1]; figure 4). The greatest percentage increase is projected in the African region, where the number of those with moderate-to-complete hearing loss is predicted to increase from 38·70 million (33·08–44·47) to 98·08 million (86·94–109·09), an increase of 154·9% (110·5–208·0). This region is followed by the Eastern Mediterranean region, where cases are projected to rise from 21·25 million (18·62–23·88) to 50·45 million (43·84–57·59), a projected increase of 138·4% (96·7–184·8).
Figure 4.
Prevalence of hearing loss 35 dB or greater, 1990–2019, with forecasts to 2050, by WHO region
Shading represents 95% UI. UI=uncertainty interval.
Discussion
Responsible for over 40 million YLDs, hearing loss was ranked as the third most common cause of YLDs in the GBD. Compared with other disease categories in the GBD, age-related and other hearing loss was the third largest cause of global YLDs in 2019 after low back pain and migraine, and was ranked first among sensory disorders. Age-related and other hearing loss was the leading cause of global YLDs compared with all causes that were explicitly modelled in the GBD for individuals older than 70 years.
Over 1·5 billion people live with hearing loss, 403 million (26%) of whom have moderate-to-complete hearing loss in their better ear. All others have mild hearing loss. Although referred to as mild, such hearing loss can cause difficulties depending on its nature and the individual's hearing needs.6, 23 This effect is especially marked in children who are developing language skills and gaining education.23 Among adults, those with moderate-to-severe hearing loss in the better-hearing ear are most likely to benefit from clinical attention and interventions such as hearing aids.24 The burden of such hearing loss is concentrated mostly in low-income and middle-income countries, which exhibit higher age-standardised rates of moderate-to complete-hearing loss compared with those of high-income countries. Moreover, the burden of disability attributable to hearing loss is concentrated in countries with poor health-care access, where hearing aid coverage is low and individuals are least likely to receive the care they need.
The distribution of individuals with moderate-to-complete hearing loss varies across regions. Geographical variation could be attributable to several factors, including the prevalence of occupational noise exposure, preventable infections such as chronic otitis media and meningitis, and health-care access. A clear association exists between ageing and hearing loss, given that most of those with hearing loss are older than 50 years. The progression of hearing loss with age also means that high-income countries have the highest all-age prevalence of hearing loss, driven mainly by their ageing population profile.
Although hearing loss is common in old ages, globally 70 million children aged 0–15 years also live with this condition. Although the prevalence of hearing loss is low in children compared with in adults, hearing loss was most severe in both the youngest and oldest individuals. When unaddressed, childhood hearing loss can affect spoken language development, literacy skills,25 and education, which might affect cognition and social wellbeing.4, 6, 8 These facts underline the importance of this affected population. Two of the causal factors that are responsible for hearing loss in children, otitis media and meningitis, are preventable. Our results align with WHO estimates that 60% of hearing loss in children is due to preventable causes such as ear infections and vaccine-preventable diseases.26
The clear association between hearing loss and age means that nearly everyone, if they live long enough, will have some degree of hearing loss, and at least 50% will have moderate-to-complete hearing loss requiring intervention. As the world population grows and ages over the coming decades,22 the need for hearing care will rise. The results of this study anticipate that by 2050, 698 million people will have moderate-to-complete hearing loss that could benefit from rehabilitation services. Rehabilitation services refer to comprehensive and holistic approaches that can include hearing aids and implants; rehabilitative therapy; sign language learning; other sensory substitutions like speechreading; and use of assistive technologies (eg, personal FM systems) and services (eg captioning). These interventions are detailed in the WHO world report on hearing.11 Although overall numbers are forecasted to be highest in the Western Pacific region in 2050, the greatest percentage increase is projected in the African region and the Eastern Mediterranean region.
Although hearing loss poses a substantial burden that will increase in coming years, methods of addressing this burden are available and cost-effective. Models indicate that passive screening in conjunction with hearing aid provision is an efficient intervention, with a cost of almost US$1000 per disability-adjusted life-year averted.27 GBD estimates suggest that there is an 83% unmet need for hearing aids globally, calculated as the proportion of individuals with moderate-to-severe hearing loss who do not use a hearing aid.28 Other studies show that early rehabilitation along with use of hearing devices such as cochlear implants are also cost-effective, despite large costs associated with initial technology investments and the risks of infectious complications after implantation.29, 30, 31, 33 For children with severe hearing loss, access to sign language and support for speechreading can improve access to education.32 The treatment of infections that can cause hearing loss (such as otitis media or meningitis) is similarly cost-effective, with variation in cost by treatment strategy.27 Although cost-effective interventions for hearing loss exist, they remain prohibitively expensive for health systems in low-income and middle-income countries. These methods of reducing burden should be introduced to meet high need, accompanied by scale-up of health systems and universal health coverage for effective administration of interventions.
Our study was developed in close collaboration with WHO and links closely with its world report on hearing. This report further elaborates on the public health implications of the rising prevalence of hearing loss. With the figures and projections noted in our study as its basis, the world report outlines the framework of a global public health response that is focused on integrated people-centred ear and hearing care. By the use of available technological solutions with evidence-based public health approaches, hearing loss can be prevented, identified, treated, and rehabilitated, to curtail the condition's projected increase in prevalence and overcome the adverse affects on individuals and society. This approach includes cost-effective interventions and strategies such as hearing screening for newborn babies, school-aged children, adults, and older adults as well as the use of hearing technology (eg, hearing aids or cochlear implants) and clinical management of ear diseases.27–31,33 Health-care services need to be prepared for the projected increases in burden, particularly in low-income and middle-income countries where ear specialists and audiologists are scarce.
We acknowledge the limitations of this study, most importantly the sparsity of the data on which these estimates are based. The lack of prevalence data is most marked in low-income countries, which have increased prevalence of severe hearing loss and insufficient access to audiometric technologies required for diagnosis. Data on hearing aid coverage is particularly sparse, with no severity-specific data outside of high-income countries and almost no data sources at all in Asia, north Africa, or Central Africa. This data gap might lead to overestimation of hearing aid coverage (and therefore underestimation of hearing loss prevalence) in low-income or under-represented locations. Moreover, we exclusively relied on NHANES data to calculate severity adjustment factors for hearing loss prevalence and split prevalence by presence of tinnitus, neglecting geographical variation in the prevalence of hearing loss and tinnitus. Additional research is needed to gain a deeper understanding of hearing loss prevalence, concurrence with tinnitus, and hearing aid coverage in areas where data are limited.
Data on the causes of hearing loss are also sparse because few surveys report prevalence of hearing loss by underlying cause. This difficulty presents challenges because the causes of hearing loss differ substantially in children compared with in adults.26, 34 Because more data exist on the cause of hearing loss in children, we scaled cause-specific hearing loss prevalence to total prevalence up to age 20 years. After this age, we treated age-related and other hearing loss as the residual between total prevalence and other causes of hearing loss. This residual approach has the potential to mask the contribution of other non-age factors to hearing loss burden. Moreover, other causes of hearing loss such as labour complications, vaccine-preventable diseases, non-occupational noise exposure, diabetes,35 and ototoxic medications such as aminoglycosides were not accounted for in our estimates because of insufficient data. Strengthened data on the causes of hearing loss in older ages (as opposed to assuming that all hearing loss in old age is age-related) would improve this method.
Although meta-regression tools enable us to leverage information from data-rich locations to estimate prevalence in locations with no data, data sparsity can make distinguishing between true variation in prevalence and measurement error particularly difficult. This issue is compounded by few predictive covariates or risk factors, because the association between hearing loss and other factors (like noise exposure) is not well quantified and likely to be masked by age. Data on self-reported hearing loss or audiometric data recorded with mobile technologies could potentially assess disease burden in locations where audiologists are sparse. However, telehealth methodologies are not yet widely used, and the generalisability of self-reported data is unclear.
GBD estimates of hearing loss are adjusted for hearing aid coverage, shifting the proportion of people with a hearing aid in each severity category to the category directly below. This adjustment might be crude in nature, masking the effect of hearing health care in reducing disability and neglecting variation in treatment effect between individuals. Whereas providers in eye care refer to best-corrected vision loss to mobilise resources towards those who are most amenable to treatment, no complementary best-corrected measure for hearing loss exists. Acquisition of data on best-corrected hearing loss could contribute to an understanding of the proportion of individuals with hearing loss who are amenable to intervention.
A systematic review of hearing loss prevalence will be completed for GBD 2020 to identify new sources of information in data-sparse locations. Additionally, we aim to revise modelling methods in upcoming years, assessing how prevalence is adjusted on the basis of hearing aid coverage, the proportion of individuals with hearing loss concurrent with tinnitus, and the severity distribution of hearing loss due to otitis media. We aim to forecast the avoidable burden of hearing loss with rapid implementation of hearing health-care interventions, provided additional data on intervention coverage is obtained. This forecast could provide policy makers with tools to effectively allocate hearing health-care services and plan for future scenarios.
The results of this study point to a growing public health challenge, which needs global attention and a definitive response. The increasing prevalence of hearing loss, high contribution to global disability, and large unmet need for hearing aids together serve as a call for urgent attention. Cost-effective, preventive, and treatment solutions to mitigate the effects of hearing loss exist, including childhood screening programmes, earplugs and other noise-reduction technologies, hearing devices, and early treatment of otitis media and meningitis. Health system capacity must be scaled up to address growing needs, particularly in low-income settings.
Correspondence to: Prof Theo Vos, Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA 98195, USA tvos@uw.edu
Data sharing
Data presented in this manuscript are made publicly available at https://vizhub.healthdata.org/gbd-compare.
Acknowledgments
Acknowledgments
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of institutions with which they are affiliated. This manuscript was produced as part of the GBD Collaborator Network and in accordance with the GBD protocol. TWB acknowledges support by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor award, funded by the German Federal Ministry of Education and Research. AAB acknowledges funding (FRGS/1/2017/SKK06iUNISZA/02/1) under Kementerian Pendidikan Malaysia and Universiti Sultan Zainal Abidin focusing on Streptococcus pneumoniae as one of the main causes of otitis media globally. IL is member of the Sistema Nacional de Investigación, which is supported by the Secretaría Nacional de Ciencia, Tecnología e Innovación, Panama. JRP acknowledges the support towards research given by Manipal Academy of Higher Education, Manipal, India. AMS acknowledges support from the Egyptian Fulbright Mission Program. MMS-M acknowledges the support of the Ministry of Education, and Science and Technological Development of the Republic of Serbia (Contract 175087). The views expressed herein do not represent those of the NIHR or the UK Department of Health and Social Care.
Contributors
Jaimie Steinmetz, Christopher J L Murray, and Theo Vos contributed to managing the estimation or publications process. Lydia Haile, Kaloyan Kamemov, Jaimie Steinmetz, and Shelly Chadha contributed to writing the first draft of the manuscript. Lydia Haile, Paul Briant, Aislyn Orji, and Jaimie Steinmetz had the primary responsibility of applying analytical methods to produce estimates. Lydia Haile, Aislyn Orji, and Jaimie Steinmetz had the primary responsibility of seeking, cataloguing, extracting, or cleaning data, and designing or coding figures and tables. Lydia Haile, Jaimie Steinmetz, Amir Abdoli, Mohammad Abdollahi, Haroon Ahmed, Tarik Ahmed Rashid, Hanadi Al Hamad, Fares Alahdab, Fahad Alanezi, Turki Alanzi, Liaqat Ali, Hubert Amu, Jalal Arabloo, Morteza Arab-Zozani, Judie Arulappan, Palash Chandra Banik, Till Bärnighausen, Sadia Bibi, Sonali Chaudhary, Dinh Toi Chu, Rosa Couto, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Mandira Lamichhane Dhimal, Meghnath Dhimal, Kerrie Doyle, Michael Ekholuenetale, Irina Filip, Richard Franklin, Shilpa Gaidhane, Syed Amir Gilani, Mahaveer Golechha, Bárbara Goulart, Veer Bala Gupta, Vivek Gupta, Howard J Hoffman, Mehdi Hosseinzadeh, Mowafa Househ, Segun Emmanuel Ibitoye, Sheikh Mohammed Shariful Islam, Sathish Kumar Jayapal, Jost B Jonas, Nawzad Kameran Al-Salihi, Gbenga Kayode, Rovshan Khalilov, Mahalaqua Nazli Khatib, Soewarta Kosen, G Anil Kumar, Huong Lan Nguyen, Savita Lasrado, Stephen Lim, Xuefeng Liu, Stany Lobo, Alaa Makki, Walter Mendoza, Kebadnew Mihretie, Ted R Miller, Mokhtar Mohammadi, Abdollah Mohammadian-Hafshejani, Ali H Mokdad, Seyed Sina Naghibi Irvani, Jean Jacques Noubiap, Bogdan Oancea, Andrew T Olagunju, Bolajoko Olusanya, Jacob Olusanya, Hans Orru, Mayowa Owolabi, Dr Jagadish Rao Padubidri, Keyvan Pakshir, Fatemeh Pashazadeh Kan, Maja Pasovic, Shrikant Pawar, Hai Quang Pham, Amir Radfar, Fakher Rahim, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Amir Masoud Rahmani, Chythra R Rao, Sowmya J Rao, Vahid Rashedi, David L Rawaf, Salman Rawaf, Andre Renzaho, Violet Rodrigues, Dr Umar Saeed, Abdallah M Samy, Milena Santric Milicevic, Brijesh Sathian, Maheswar Satpathy, Monika Sawhney, Allen Seylani, Masood Ali Shaikh, Mohd Shannawaz, Wondimeneh Shiferaw, Soraya Siabani, Jasvinder Singh, Jitendra Kumar Singh, Deepika Singhal, Valentin Skryabin, Anna Skryabina, Houman Sotoudeh, Animut Tagele Tamiru, Giang Thu Vu, Marcos Roberto Tovani-Palone, Bach Tran Xuan, Saif Ullah, Vasiliy Vlassov, Bay Vo, Ali Yadollahpour, Birhanu Wubale Yirdaw, Naohiro Yonemoto, Chuanhua Yu, Ismaeel Yunusa, Zhi-Jiang Zhang, Christopher J L Murray, Adrian Davis, Theo Vos, and Shelly Chadha contributed to providing data or critical feedback on data sources. Lydia Haile, Paul Briant, Aislyn Orji, Jaimie Steinmetz, Tarik Ahmed Rashid, Liaqat Ali, Hubert Amu, Palash Chandra Banik, Sonali Chaudhary, Shilpa Gaidhane, Farhad Ghamari, Ahmad Ghashghaee, Howard J Hoffman, Mehdi Hosseinzadeh, Mowafa Househ, Nawzad Kameran Al-Salihi, Rovshan Khalilov, Mahalaqua Nazli Khatib, Alaa Makki, Mokhtar Mohammadi, Ali H Mokdad, Mohammad Ali Moni, Amir Masoud Rahmani, Abdallah M Samy, Maheswar Satpathy, Deepika Singhal, Bay Vo, Mikhail Zastrozhin, Anastasiia Zastrozhina, Christopher J L Murray, and Theo Vos contributed to developing methods or computational machinery. Lydia Haile, Paul Briant, Aislyn Orji, Jaimie Steinmetz, Mohammad Abdollahi, Eman Abu-Gharbieh, Haroon Ahmed, Tarik Ahmed Rashid, Yonas Akalu, Hanadi Al Hamad, Fares Alahdab, Fahad Alanezi, Turki Alanzi, Liaqat Ali, Vahid Alipour, Rajaa Al-Raddadi, Hubert Amu, Jalal Arabloo, Morteza Arab-Zozani, Judie Arulappan, Zaheer-Ud-Din Babar, Atif Baig, Palash Chandra Banik, Till Bärnighausen, Amadou Barrow, Rose Bender, Akshaya Bhagavathula, Nikha Bhardwaj, Pankaj Bhardwaj, Sadia Bibi, Ali Bijani, Katrin Burkart, Christopher Cederroth, Jaykaran Charan, Sonali Chaudhary, Sonali Choudhari, Dinh Toi Chu, Rosa Couto, Amare Dagnew, Baye Dagnew, Saad Dahlawi, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Desta Debalkie Atnafu, Assefa Desalew, Deepak Dhamnetiya, Mandira Lamichhane Dhimal, Meghnath Dhimal, Kerrie Doyle, Michael Ekholuenetale, Irina Filip, Florian Fischer, Richard Franklin, Abhay Gaidhane, Shilpa Gaidhane, Ahmad Ghashghaee, Ghozali Ghozali, Ionela-Roxana Glăvan, Mahaveer Golechha, Bárbara Goulart, Veer Bala Gupta, Vivek Gupta, Samer Hamidi, Billy Hammond, Khezar Hayat, Golnaz Heidari, Howard J Hoffman, Kathleen Hopf, Mehdi Hosseinzadeh, Mowafa Househ, Rabia Hussain, Bing-Fang Hwang, Segun Emmanuel Ibitoye, Olayinka Ilesanmi, Sheikh Mohammed Shariful Islam, Masao Iwagami, Louis Jacob, Sathish Kumar Jayapal, Ravi Prakash Jha, Jost B Jonas, Rohollah Kalhor, Nawzad Kameran Al-Salihi, Himal Kandel, Ayele Semachew Kasa, Gbenga Kayode, Rovshan Khalilov, Ejaz Khan, Mahalaqua Nazli Khatib, Ai Koyanagi, G Anil Kumar, Huong Lan Nguyen, Savita Lasrado, Xuefeng Liu, Stany Lobo, Alessandra Lugo, Alaa Makki, Walter Mendoza, Amanual Mersha, Ted R Miller, Sanjeev Misra, Teroj Mohamed, Mokhtar Mohammadi, Abdollah Mohammadian-Hafshejani, Arif Mohammed, Ali H Mokdad, Mohammad Ali Moni, Seyed Sina Naghibi Irvani, Sandhya Neupane Kandel, Molly Nixon, Jean Jacques Noubiap, Bogdan Oancea, Victor Oguoma, Andrew T Olagunju, Bolajoko Olusanya, Jacob Olusanya, Hans Orru, Mayowa Owolabi, Dr Jagadish Rao Padubidri, Shahina Pardhan, Maja Pasovic, Shrikant Pawar, Akram Pourshams, Hai Quang Pham, Mohammad Rabiee, Navid Rabiee, Amir Radfar, Fakher Rahim, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Mosiur Rahman, Amir Masoud Rahmani, Juwel Rana, Chythra R Rao, Sowmya J Rao, Vahid Rashedi, David L Rawaf, Salman Rawaf, Andre Renzaho, Aziz Rezapour, Rezaul Karim Ripon, Violet Rodrigues, Neeti Rustagi, Dr Umar Saeed, Abdallah M Samy, Milena Santric Milicevic, Brijesh Sathian, Maheswar Satpathy, Monika Sawhney, Allen Seylani, Masood Ali Shaikh, Mohd Shannawaz, Wondimeneh Shiferaw, Soraya Siabani, Anjali Singal, Jasvinder Singh, Jitendra Kumar Singh, Deepika Singhal, Valentin Skryabin, Anna Skryabina, Houman Sotoudeh, Animut Tagele Tamiru, Md Tareque, Rekha Thapar, Giang Thu Vu, Marcos Roberto Tovani-Palone, Bach Tran Xuan, Saif Ullah, Francesco S Violante, Bay Vo, Avina Vongpradith, Jingkai Wei, Biruk Wogayehu, Ali Yadollahpour, Yigizie Yeshaw, Vahit Yiğit, Naohiro Yonemoto, Chuanhua Yu, Ismaeel Yunusa, Mohammad Zamani, Mikhail Zastrozhin, Anastasiia Zastrozhina, Jeff Zhao, Christopher J L Murray, Adrian Davis, Theo Vos, and Shelly Chadha contributed to providing critical feedback on methods or results. Lydia Haile, Kaloyan Kamenov, Paul Briant, Aislyn Orji, Jaimie Steinmetz, Eman Abu-Gharbieh, Haroon Ahmed, Yonas Akalu, Fares Alahdab, Liaqat Ali, Jalal Arabloo, Morteza Arab-Zozani, Atif Baig, Till Bärnighausen, Amadou Barrow, Rose Bender, Akshaya Bhagavathula, Christopher Cederroth, Dinh Toi Chu, Rosa Couto, Baye Dagnew, Deepak Dhamnetiya, Mandira Lamichhane Dhimal, Meghnath Dhimal, Bruce Duncan, Irina Filip, Florian Fischer, Silvano Gallus, Farhad Ghamari, Mahaveer Golechha, Bárbara Goulart, Veer Bala Gupta, Vivek Gupta, Simon I Hay, Golnaz Heidari, Ivo Iavicoli, Segun Emmanuel Ibitoye, Olayinka Ilesanmi, Sheikh Mohammed Shariful Islam, Louis Jacob, Sathish Kumar Jayapal, Ravi Prakash Jha, Jost B Jonas, Himal Kandel, Ayele Semachew Kasa, Gbenga Kayode, Rovshan Khalilov, Ejaz Khan, Ai Koyanagi, Huong Lan Nguyen, Iván Landires, Savita Lasrado, Walter Mendoza, Ted R Miller, Teroj Mohamed, Abdollah Mohammadian-Hafshejani, Arif Mohammed, Ali H Mokdad, Mohammad Ali Moni, Seyed Sina Naghibi Irvani, Sandhya Neupane Kandel, Molly Nixon, Jean Jacques Noubiap, Virginia Nuñez-Samudio, Victor Oguoma, Andrew T Olagunju, Bolajoko Olusanya, Jacob Olusanya, Hans Orru, Mayowa Owolabi, Dr Jagadish Rao Padubidri, Shahina Pardhan, Shrikant Pawar, Marina Pinheiro, Hai Quang Pham, Amir Radfar, Fakher Rahim, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Chythra R Rao, Sowmya J Rao, David L Rawaf, Salman Rawaf, Andre Renzaho, Rezaul Karim Ripon, Violet Rodrigues, Amirhossein Sahebkar, Abdallah M Samy, Milena Santric Milicevic, Maheswar Satpathy, Winfried Schlee, Maria Schmidt, Allen Seylani, Mohd Shannawaz, Anjali Singal, Jasvinder Singh, Valentin Skryabin, Anna Skryabina, Animut Tagele Tamiru, Giang Thu Vu, Marcos Roberto Tovani-Palone, Bach Tran Xuan, Sahel Valadan Tahbaz, Vasiliy Vlassov, Hossein Yahyazadeh, Yigizie Yeshaw, Vahit Yiğit, Naohiro Yonemoto, Mikhail Zastrozhin, Anastasiia Zastrozhina, Zhi-Jiang Zhang, Christopher J L Murray, Adrian Davis, and Shelly Chadha contributed to drafting the work or revising it critically for important intellectual content. Lydia Haile, Jaimie Steinmetz, Liaqat Ali, Sonali Chaudhary, Shilpa Gaidhane, Rovshan Khalilov, Mahalaqua Nazli Khatib, Ali H Mokdad, Shrikant Pawar, Abdallah M Samy, Maheswar Satpathy, Deepika Singhal, Emma Spurlock, Avina Vongpradith, and Vahit Yiğit contributed to extracting, cleaning, or cataloging data, and designing or coding figures and tables. Jaimie Steinmetz, Ashkan Afshin, Charlie Ashbaugh, Lalit Dandona, Simon I Hay, Ali H Mokdad, Molly Nixon, Christopher J L Murray, and Theo Vos managed the overall research enterprise.
GBD 2019 Hearing Loss Collaborators
Lydia M Haile, Kaloyan Kamenov, Paul Svitil Briant, Aislyn U Orji, Jaimie D Steinmetz, Amir Abdoli, Mohammad Abdollahi, Eman Abu-Gharbieh, Ashkan Afshin, Haroon Ahmed, Tarik Ahmed Rashid, Yonas Akalu, Fares Alahdab, Fahad Mashhour Alanezi, Turki M Alanzi, Hanadi Al Hamad, Liaqat Ali, Vahid Alipour, Rajaa M Al-Raddadi, Hubert Amu, Jalal Arabloo, Morteza Arab-Zozani, Judie Arulappan, Charlie Ashbaugh, Desta Debalkie Atnafu, Zaheer-Ud-Din Babar, Atif Amin Baig, Palash Chandra Banik, Till Winfried Bärnighausen, Amadou Barrow, Rose G Bender, Akshaya Srikanth Bhagavathula, Nikha Bhardwaj, Pankaj Bhardwaj, Sadia Bibi, Ali Bijani, Katrin Burkart, Christopher R Cederroth, Jaykaran Charan, Sonali Gajanan Choudhari, Dinh-Toi Chu, Rosa A S Couto, Amare Belachew Dagnew, Baye Dagnew, Saad M A Dahlawi, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Assefa Desalew, Deepak Dhamnetiya, Mandira Lamichhane Dhimal, Meghnath Dhimal, Kerrie E Doyle, Bruce B Duncan, Michael Ekholuenetale, Irina Filip, Florian Fischer, Richard Charles Franklin, Abhay Motiramji Gaidhane, Shilpa Gaidhane, Silvano Gallus, Farhad Ghamari, Ahmad Ghashghaee, Ghozali Ghozali, Syed Amir Gilani, Ionela-Roxana Glăvan, Mahaveer Golechha, Bárbara Niegia Garcia Goulart, Veer Bala Gupta, Vivek Kumar Gupta, Samer Hamidi, Billy Randall Hammond, Simon I Hay, Khezar Hayat, Golnaz Heidari, Howard J Hoffman, Kathleen Pillsbury Hopf, Mehdi Hosseinzadeh, Mowafa Househ, Rabia Hussain, Bing-Fang Hwang, Ivo Iavicoli, Segun Emmanuel Ibitoye, Olayinka Stephen Ilesanmi, Seyed Sina Naghibi Irvani, Sheikh Mohammed Shariful Islam, Masao Iwagami, Louis Jacob, Sathish Kumar Jayapal, Ravi Prakash Jha, Jost B Jonas, Rohollah Kalhor, Nawzad Kameran Al-Salihi, Himal Kandel, Ayele Semachew Kasa, Gbenga A Kayode, Rovshan Khalilov, Ejaz Ahmad Khan, Mahalaqua Nazli Khatib, Soewarta Kosen, Ai Koyanagi, G Anil Kumar, Iván Landires, Savita Lasrado, Stephen S Lim, Xuefeng Liu, Stany W Lobo, Alessandra Lugo, Alaa Makki, Walter Mendoza, Amanual Getnet Mersha, Kebadnew Mulatu Mihretie, Ted R Miller, Sanjeev Misra, Teroj Abdulrahman Mohamed, Mokhtar Mohammadi, Abdollah Mohammadian-Hafshejani, Arif Mohammed, Ali H Mokdad, Mohammad Ali Moni, Sandhya Neupane Kandel, Huong Lan Thi Nguyen, Molly R Nixon, Jean Jacques Noubiap, Virginia Nuñez-Samudio, Bogdan Oancea, Victor Maduabuchi Oguoma, Andrew T Olagunju, Bolajoko Olubukunola Olusanya, Jacob Olusegun Olusanya, Hans Orru, Mayowa O Owolabi, Jagadish Rao Padubidri, Keyvan Pakshir, Shahina Pardhan, Fatemeh Pashazadeh Kan, Maja Pasovic, Shrikant Pawar, Hai Quang Pham, Marina Pinheiro, Akram Pourshams, Navid Rabiee, Mohammad Rabiee, Amir Radfar, Fakher Rahim, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Mosiur Rahman, Amir Masoud Rahmani, Juwel Rana, Chythra R Rao, Sowmya J Rao, Vahid Rashedi, David Laith Rawaf, Salman Rawaf, Andre M N Renzaho, Aziz Rezapour, Rezaul Karim Ripon, Voilet Rodrigues, Neeti Rustagi, Umar Saeed, Amirhossein Sahebkar, Abdallah M Samy, Milena M Santric-Milicevic, Brijesh Sathian, Maheswar Satpathy, Monika Sawhney, Winfried Schlee, Maria Inês Schmidt, Allen Seylani, Masood Ali Shaikh, Mohammed Shannawaz, Wondimeneh Shibabaw Shiferaw, Soraya Siabani, Anjali Singal, Jasvinder A Singh, Jitendra Kumar Singh, Deepika Singhal, Valentin Yurievich Skryabin, Anna Aleksandrovna Skryabina, Houman Sotoudeh, Emma Elizabeth Spurlock, Biruk Wogayehu Taddele, Animut Tagele Tamiru, Md Ismail Tareque, Rekha Thapar, Marcos Roberto Tovani-Palone, Bach Xuan Tran, Saif Ullah, Sahel Valadan Tahbaz, Francesco S Violante, Vasily Vlassov, Bay Vo, Avina Vongpradith, Giang Thu Vu, Jingkai Wei, Ali Yadollahpour, Seyed Hossein Yahyazadeh Jabbari, Yigizie Yeshaw, Vahit Yiğit, Birhanu Wubale Yirdaw, Naohiro Yonemoto, Chuanhua Yu, Ismaeel Yunusa, Mohammad Zamani, Mikhail Sergeevich Zastrozhin, Anasthasia Zastrozhina, Zhi-Jiang Zhang, Jeff T Zhao, Christopher J L Murray, Adrian C Davis, Theo Vos, and Shelly Chadha.
Affiliations
Institute for Health Metrics and Evaluation (L M Haile BA, P S Briant BS, A U Orji BA, J D Steinmetz PhD, A Afshin MD, C Ashbaugh MA, R G Bender BS, K Burkart PhD, X Dai PhD, Prof L Dandona MD, Prof R Dandona PhD, Prof S I Hay FMedSci, Prof S S Lim PhD, Prof A H Mokdad PhD, M R Nixon PhD, M Pasovic MA, E E Spurlock BA, A Vongpradith BA, J T Zhao BA, Prof C J L Murray PhD, Prof T Vos PhD), Department of Health Metrics Sciences, School of Medicine (A Afshin MD, K Burkart PhD, Prof R Dandona PhD, Prof S I Hay FMedSci, Prof S S Lim PhD, Prof A H Mokdad PhD, Prof C J L Murray PhD, Prof T Vos PhD), University of Washington, Seattle, WA, USA; Department of Noncommunicable Diseases (K Kamenov PhD, S Chadha PhD), World Health Organization (WHO), Geneva, Switzerland; Department of Parasitology and Mycology (A Abdoli PhD), Jahrom University of Medical Sciences, Jahrom, Iran; The Institute of Pharmaceutical Sciences (TIPS) (Prof M Abdollahi PhD), School of Pharmacy (Prof M Abdollahi PhD), Digestive Diseases Research Institute (Prof A Pourshams MD), Metabolomics and Genomics Research Center (F Rahim PhD), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD), Tehran University of Medical Sciences, Tehran, Iran; Clinical Sciences Department (E Abu-Gharbieh PhD), Mass Communication Department (A Makki PhD), University of Sharjah, Sharjah, United Arab Emirates; Department of Biosciences (H Ahmed PhD), COMSATS Institute of Information Technology, Islamabad, Pakistan; Department of Computer Science and Engineering (T Ahmed Rashid PhD), University of Kurdistan Hewler, Erbil, Iraq; Department of Medical Physiology (Y Akalu MSc), Department of Human Physiology (B Dagnew MSc), School of Medicine (A G Mersha MD), Department of Midwifery (A T Tamiru MSc, B W Yirdaw MSc), Department of Epidemiology and Biostatistics (Y Yeshaw MPH), University of Gondar, Gondar, Ethiopia; Mayo Evidence-based Practice Center, Mayo Clinic Foundation for Medical Education and Research, Rochester, MN, USA (F Alahdab MSc); Health Information Management and Technology Department (T M Alanzi PhD), Environmental Health Department (S M A Dahlawi PhD), Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (F M Alanezi PhD); Geriatric and Long Term Care Department (H Al Hamad MD, B Sathian PhD), Rumailah Hospital (H Al Hamad MD), Hamad Medical Corporation, Doha, Qatar; Department of Biological Sciences, National University of Medical Sciences (NUMS), Rawalpindi, Pakistan (L Ali PhD); Health Management and Economics Research Center (V Alipour PhD, J Arabloo PhD, A Ghashghaee BSc, M Hosseinzadeh PhD, A Rezapour PhD), Student Research Committee (A Ghashghaee BSc), Tehran Institute of Psychiatry (V Rashedi PhD), Iran University of Medical Sciences, Tehran, Iran (F Pashazadeh Kan BSN); Department of Community Medicine (R M Al-Raddadi PhD), King Abdulaziz University, Jeddah, Saudi Arabia; Department of Population and Behavioural Sciences (H Amu PhD), University of Health and Allied Sciences, Ho, Ghana; Social Determinants of Health Research Center (M Arab-Zozani PhD), Birjand University of Medical Sciences, Birjand, Iran; Department of Maternal and Child Health, Sultan Qaboos University, Muscat, Oman (J Arulappan DSc); Department of Health System and Health Economics (D D Atnafu MPH), Department of Nursing (A B Dagnew MSc), Department of Adult Health Nursing (A Kasa MSc), Department of Epidemiology and Biostatistics (K M Mihretie MPH), Bahir Dar University, Bahir Dar, Ethiopia; Department of Pharmacy, University of Huddersfield, Huddersfield, UK (Prof Z Babar PhD); Unit of Biochemistry (A A Baig PhD), Universiti Sultan Zainal Abidin (Sultan Zainal Abidin University), Kuala Terengganu, Malaysia; Department of Non-communicable Diseases (P C Banik MPhil), Bangladesh University of Health Sciences, Dhaka, Bangladesh; Heidelberg Institute of Global Health (Prof T W Bärnighausen MD), Department of Ophthalmology (Prof J B Jonas MD), Heidelberg University, Heidelberg, Germany; Harvard T H Chan School of Public Health (Prof T W Bärnighausen MD, I Yunusa PhD), Harvard University, Boston, MA, USA; Department of Public and Environmental Health (A Barrow MPH), University of The Gambia, Brikama, The Gambia; Epidemiology and Disease Control Unit (A Barrow MPH), Ministry of Health, Kotu, The Gambia; Department of Social and Clinical Pharmacy (A S Bhagavathula PharmD), Charles University, Hradec Kralova, Czech Republic; Institute of Public Health (A S Bhagavathula PharmD), United Arab Emirates University, Al Ain, United Arab Emirates; Department of Anatomy (Prof N Bhardwaj MD), Government Medical College Pali, Pali, India; Department of Community Medicine and Family Medicine (P Bhardwaj MD, N Rustagi MD), School of Public Health (P Bhardwaj MD), Department of Pharmacology (J Charan MD), Department of Surgical Oncology (Prof S Misra MCh), All India Institute of Medical Sciences, Jodhpur, India; Institute of Soil and Environmental Sciences (S Bibi PhD, S Ullah PhD), University of Agriculture, Faisalabad, Faisalabad, Pakistan; Social Determinants of Health Research Center (A Bijani PhD), Student Research Committee (M Zamani MD), Babol University of Medical Sciences, Babol, Iran; Department of Physiology and Pharmacology (C R Cederroth PhD), Karolinska Institute, Stockholm, Sweden; National Institute of Health Research Nottingham Biomedical Research Centre (C R Cederroth PhD), University of Nottingham, Nottingham, UK; Department of Community Medicine (Prof S G Choudhari MD, Prof A M Gaidhane MD), Department of Medicine (S Gaidhane PhD), Global Evidence Synthesis Initiative (Prof M Khatib PhD), Department of Ophthalmology (Prof D Singhal MD), Datta Meghe Institute of Medical Sciences, Wardha, India; Center for Biomedicine and Community Health (D Chu PhD), VNU-International School, Hanoi, Vietnam; Department of Chemical Sciences (R A S Couto MD), Department of Chemistry (M Pinheiro PhD), University of Porto, Porto, Portugal; Public Health Foundation of India, Gurugram, India (Prof L Dandona MD, Prof R Dandona PhD, G Kumar PhD); Indian Council of Medical Research, New Delhi, India (Prof L Dandona MD); School of Nursing and Midwifery (A Desalew MSc), Haramaya University, Harar, Ethiopia; Department of Community Medicine (D Dhamnetiya MD, R P Jha MSc), Dr. Baba Sahib Ambedkar Medical College and Hospital, Delhi, India; Research and Social Development Department (M L Dhimal PhD), Nepal Pollution Control and Environment Centre, Lalitpur, Nepal; Health Research Section (M Dhimal PhD), Nepal Health Research Council, Kathmandu, Nepal; School of Medicine (Prof K E Doyle PhD), Western Sydney University, Sydney, NSW, Australia; School of Health and Biomedical Sciences (Prof K E Doyle PhD), Royal Melbourne Institute of Technology University, Melbourne, VIC, Australia; Postgraduate Program in Epidemiology (Prof B B Duncan PhD, Prof B N G Goulart DSc, Prof M I Schmidt PhD), Federal University of Rio Grande do Sul, Porto Alegre, Brazil; Department of Epidemiology and Medical Statistics (M Ekholuenetale MSc), Faculty of Public Health (M Ekholuenetale MSc), Department of Health Promotion and Education (S E Ibitoye MPH), Department of Community Medicine (O S Ilesanmi PhD), Department of Medicine (Prof M O Owolabi DrM), University of Ibadan, Ibadan, Nigeria; Psychiatry Department (I Filip MD), Kaiser Permanente, Fontana, CA, USA; School of Health Sciences (I Filip MD), A.T. Still University, Mesa, AZ, USA; Institute of Gerontological Health Services and Nursing Research (F Fischer PhD), Ravensburg-Weingarten University of Applied Sciences, Weingarten, Germany; School of Public Health, Medical, and Veterinary Sciences (R C Franklin PhD), James Cook University, Douglas, QLD, Australia; Department of Environmental Health Sciences (S Gallus DSc, A Lugo PhD), Mario Negri Institute for Pharmacological Research, Milan, Italy; Occupational Health Department (F Ghamari PhD), Arak University of Medical Sciences, Arak, Iran; Department of Public Health (G Ghozali PhD), University of Muhammadiyah Kalimantan Timur, Samarinda, Indonesia; Faculty of Allied Health Sciences (Prof S Gilani PhD), The University of Lahore, Lahore, Pakistan; Afro-Asian Institute, Lahore, Pakistan (Prof S Gilani PhD); Department of Statistics and Econometrics (I Glăvan PhD), Bucharest University of Economic Studies, Bucharest, Romania; Health Systems and Policy Research (M Golechha PhD), Indian Institute of Public Health Gandhinagar, Gandhinagar, India; Department of Clinical Medicine (Prof V K Gupta PhD), Macquarie University, Sydney, NSW, Australia; School of Medicine (V B Gupta PhD), Deakin University, Geelong, VIC, Australia; School of Health and Environmental Studies (Prof S Hamidi DrPH), Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates; Brain and Behavioral Sciences Program (Prof B R Hammond PhD), University of Georgia, Athens, GA, USA; Institute of Pharmaceutical Sciences (K Hayat MS), University of Veterinary and Animal Sciences, Lahore, Pakistan; Department of Pharmacy Administration and Clinical Pharmacy (K Hayat MS), Xian Jiaotong University, Xian, China; Santa Clara, CA, USA (G Heidari MD); National Institute on Deafness and Other Communication Disorders (H J Hoffman MA), Division of Scientific Programs (H J Hoffman MA), National Institute of Health, Bethesda, MD, USA; Virginia Beach, VA, USA (K P Hopf MPH); College of Science and Engineering (Prof M Househ PhD), Hamad Bin Khalifa University, Doha, Qatar; School of Pharmaceutical Sciences (R Hussain PhD), University of Science Malaysia, Penang, Malaysia; Department of Occupational Safety and Health (Prof B-F Hwang PhD), China Medical University, Taichung, Taiwan; Department of Public Health (Prof I Iavicoli PhD), University of Naples Federico II, Naples, Italy; Department of Community Medicine (O S Ilesanmi PhD), Department of Medicine (Prof M O Owolabi DrM), University College Hospital, Ibadan, Ibadan, Nigeria; Research Institute for Endocrine Sciences (S N Irvani MD), Shahid Beheshti University of Medical Sciences, Tehran, Iran; Institute for Physical Activity and Nutrition (S Islam PhD), Deakin University, Burwood, VIC, Australia; Sydney Medical School (S Islam PhD), Ophthalmology Department (H Kandel PhD), University of Sydney, Sydney, NSW, Australia; Department of Health Services Research (M Iwagami PhD), University of Tsukuba, Tsukuba, Japan; Department of Non-Communicable Disease Epidemiology (M Iwagami PhD), London School of Hygiene & Tropical Medicine, London, UK; Research and Development Unit (L Jacob MD), Biomedical Research Networking Center for Mental Health Network (CiberSAM), Barcelona, Spain; Faculty of Medicine (L Jacob MD), University of Versailles Saint-Quentin-en-Yvelines, Montigny-le-Bretonneux, France; Centre of Studies and Research (S Jayapal PhD), Ministry of Health, Muscat, Oman; Department of Community Medicine (R P Jha MSc), Banaras Hindu University, Varanasi, India; Beijing Institute of Ophthalmology (Prof J B Jonas MD), Beijing Tongren Hospital, Beijing, China; Institute for Prevention of Non-communicable Diseases (R Kalhor PhD), Health Services Management Department (R Kalhor PhD), Qazvin University of Medical Sciences, Qazvin, Iran; Department of Computer Science and Engineering (N Kameran Al-Salihi PhD), University of Kurdistan Hewler, Hewler, Iraq; Ophthalmology Department (H Kandel PhD), Sydney Local Health District, Sydney, NSW, Australia; International Research Center of Excellence (G A Kayode PhD), Institute of Human Virology Nigeria, Abuja, Nigeria; Julius Centre for Health Sciences and Primary Care (G A Kayode PhD), Utrecht University, Utrecht, Netherlands; Department of Biophysics and Biochemistry (Prof R Khalilov PhD), Baku State University, Baku, Azerbaijan; Russian Institute for Advanced Study (Prof R Khalilov PhD), Moscow State Pedagogical University, Moscow, Russia; Department of Epidemiology and Biostatistics (E A Khan MPH), Health Services Academy, Islamabad, Pakistan; Jakarta, Indonesia (S Kosen MD); Biomedical Research Networking Center for Mental Health Network (CiberSAM) (A Koyanagi MD), San Juan de Dios Sanitary Park, Sant Boi de Llobregat, Spain; Catalan Institution for Research and Advanced Studies (ICREA), Barcelona, Spain (A Koyanagi MD); Unit of Genetics and Public Health (Prof I Landires MD), Unit of Microbiology and Public Health (V Nuñez-Samudio PhD), Institute of Medical Sciences, Las Tablas, Panama; Department of Public Health (V Nuñez-Samudio PhD), Ministry of Health, Herrera, Panama (Prof I Landires MD); Department of Otorhinolaryngology (S Lasrado MS), Father Muller Medical College, Mangalore, India; Department of Systems, Populations, and Leadership (X Liu PhD), University of Michigan, Ann Arbor, MI, USA; Department of Professional and Medical Education (S W Lobo PhD), Meharry Medical College, Nashville, TN, USA; Department of Biomedical Sciences (S W Lobo PhD), Mercer University, Macon, GA, USA; Peru Country Office (W Mendoza MD), United Nations Population Fund (UNFPA), Lima, Peru; School of Medicine and Public Health (A G Mersha MD), University of Newcastle, Newcastle, NSW, Australia; Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); School of Public Health (T R Miller PhD), Curtin University, Perth, WA, Australia; College of Dentistry (T A Mohamed MSc), University of Duhok, Duhok, Iraq; Department of Information Technology (M Mohammadi PhD), Lebanese French University, Erbil, Iraq; Department of Epidemiology and Biostatistics (A Mohammadian-Hafshejani PhD), Shahrekord University of Medical Sciences, Shahrekord, Iran; Department of Biology (A Mohammed PhD), University of Jeddah, Jeddah, Saudi Arabia; WHO Centre on eHealth (M Moni PhD), University of New South Wales, Sydney, NSW, Australia; Bupa Clemton Park (S Neupane Kandel BSN), Bupa, Sydney, NSW, Australia; Institute for Global Health Innovations (H L T Nguyen MPH, H Q Pham MD), Duy Tan University, Hanoi, Vietnam; Centre for Heart Rhythm Disorders (J Noubiap MD), University of Adelaide, Adelaide, SA, Australia; Administrative and Economic Sciences Department (Prof B Oancea PhD), University of Bucharest, Bucharest, Romania; Health Research Institute (V M Oguoma PhD), University of Canberra, Canberra, NSW, Australia; Department of Psychiatry and Behavioural Neurosciences (A T Olagunju MD), McMaster University, Hamilton, ON, Canada; Department of Psychiatry (A T Olagunju MD), University of Lagos, Lagos, Nigeria; Centre for Healthy Start Initiative, Lagos, Nigeria (J O Olusanya MBA, B O Olusanya PhD); Institute of Family Medicine and Public Health (H Orru PhD), University of Tartu, Tartu, Estonia; Section of Sustainable Health (H Orru PhD), Umeå University, Umeå, Sweden; Kasturba Medical College, Mangalore (J Padubidri MD), Manipal Academy of Higher Education, Manipal, India; Department of Parasitology and Mycology (Prof K Pakshir PhD), Shiraz University of Medical Sciences, Shiraz, Iran; Vision and Eye Research Institute (Prof S Pardhan PhD), Anglia Ruskin University, Cambridge, UK; Department of Genetics (S Pawar PhD), Yale University, New Haven, CT, USA; Department of Chemistry (N Rabiee MSc), Sharif University of Technology, Tehran, Iran; Biomedical Engineering Department (Prof M Rabiee PhD), Amirkabir University of Technology, Tehran, Iran; College of Medicine (A Radfar MD), University of Central Florida, Orlando, FL, USA; Thalassemia and Hemoglobinopathy Research Center (F Rahim PhD), Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran; Department of Community Medicine (M Rahman PhD), Maharishi Markandeshwar Medical College & Hospital, Solan, India; Department of Population Science and Human Resource Development (M Rahman DrPH, Prof M I Tareque PhD), University of Rajshahi, Rajshahi, Bangladesh; Future Technology Research Center (A Rahmani PhD), National Yunlin University of Science and Technology, Yunlin, Taiwan; Institute of Research and Development (A Rahmani PhD), Duy Tan University, Da Nang, Vietnam; Department of Public Health (J Rana MPH), North South University, Dhaka, Bangladesh; Department of Biostatistics and Epidemiology (J Rana MPH), University of Massachusetts Amherst, Amherst, MA, USA; Department of Oral Pathology (S Rao MDS), Srinivas Institute of Dental Sciences, Mangalore, India; Department of Community Medicine (C R Rao MD), Kasturba Medical College, Manipal, India; Department of Primary Care and Public Health (Prof S Rawaf MD), WHO Collaborating Centre for Public Health Education and Training (D L Rawaf MD), Department of Surgery and Cancer (Prof A C Davis PhD), Imperial College London, London, UK; Academic Public Health England (Prof S Rawaf MD), Public Health England, London, UK; University College London Hospitals, London, UK (D L Rawaf MD); School of Social Sciences and Psychology (Prof A M N Renzaho PhD), Translational Health Research Institute (Prof A M N Renzaho PhD), Western Sydney University, Penrith, NSW, Australia; Department of Public Health (R K Ripon MSPH), Bangladesh Institute for Tropical Medicine, Dhaka, Bangladesh; Community Nursing Unit (V Rodrigues MSc), Ireland Hospital, Abbeyleix, Ireland; Department of Research and Development (U Saeed PhD), Islamabad Diagnostic Center (IDC) Pakistan, Islamabad, Pakistan; Halal Research Center (A Sahebkar PhD), Food and Drug Administration of the Islamic Republic of Iran, Tehran, Iran; Neurogenic Inflammation Research Center (A Sahebkar PhD), Mashhad University of Medical Sciences, Mashhad, Iran; Department of Entomology (A M Samy PhD), Ain Shams University, Cairo, Egypt; Faculty of Medicine (Prof M M Santric-Milicevic PhD), School of Public Health and Health Management (Prof M M Santric-Milicevic PhD), University of Belgrade, Belgrade, Serbia; Faculty of Health & Social Sciences (B Sathian PhD), Bournemouth University, Bournemouth, UK; UGC Centre of Advanced Study in Psychology (M Satpathy PhD), Utkal University, Bhubaneswar, India; Udyam-Global Association for Sustainable Development, Bhubaneswar, India (M Satpathy PhD); Department of Public Health Sciences (M Sawhney PhD), University of North Carolina at Charlotte, Charlotte, NC, USA; Department of Psychiatry and Psychotherapy (W Schlee PhD), University of Regensburg, Regensburg, Germany; National Heart, Lung, and Blood Institute (A Seylani BS), National Institute of Health, Rockville, MD, USA; Karachi, Pakistan (M A Shaikh MD); Department of Community Medicine (M Shannawaz PhD), BLDE University, Vijayapur, India; Department of Nursing (W S Shiferaw MSc), Debre Berhan University, Debre Berhan, Ethiopia; Department of Health Education and Health Promotion (S Siabani PhD), Kermanshah University of Medical Sciences, Kermanshah, Iran; School of Health (S Siabani PhD), University of Technology Sydney, Sydney, NSW, Australia; Department of Anatomy (A Singal PhD), All India Institute of Medical Sciences, Bathinda, India; School of Medicine (Prof J A Singh MD), Department of Radiology (H Sotoudeh MD), University of Alabama at Birmingham, Birmingham, AL, USA; Medicine Service (Prof J A Singh MD), US Department of Veterans Affairs (VA), Birmingham, AL, USA; Department of Community Medicine & Public Health (J Singh PhD), Tribhuvan University, Janakpur, Nepal; Department of Ophthalmology (Prof D Singhal MD), Gmers Medical College and Civil Hospital, Ahmedabad, India; Department No.16 (V Y Skryabin MD), Laboratory of Genetics and Genomics (Prof M S Zastrozhin PhD), Moscow Research and Practical Centre on Addictions, Moscow, Russia; Therapeutic Department (A A Skryabina MD), Balashiha Central Hospital, Balashikha, Russia; Department of Pharmacy (B W Taddele MPH), Arbaminch College of Health Sciences, Arba Minch, Ethiopia; Department of Community Medicine (R Thapar MD), Manipal Academy of Higher Education, Mangalore, India; Department of Pathology and Legal Medicine (M R Tovani-Palone PhD), University of São Paulo, Ribeirão Preto, Brazil; Modestum LTD, London, UK (M R Tovani-Palone PhD); Department of Health Economics (B X Tran PhD), Hanoi Medical University, Hanoi, Vietnam; Clinical Cancer Research Center (S Valadan Tahbaz PhD, S Yahyazadeh Jabbari MD), Milad General Hospital, Tehran, Iran; Department of Microbiology (S Valadan Tahbaz PhD), Islamic Azad University, Tehran, Iran; Department of Medical and Surgical Sciences (Prof F S Violante MD), University of Bologna, Bologna, Italy; Occupational Health Unit (Prof F S Violante MD), Sant'Orsola Malpighi Hospital, Bologna, Italy; Department of Health Care Administration and Economics (Prof V Vlassov MD), National Research University Higher School of Economics, Moscow, Russia; Faculty of Information Technology (B Vo PhD), Ho Chi Minh City University of Technology (HUTECH), Ho Chi Minh City, Vietnam; Center of Excellence in Behavioral Medicine (G T Vu BA), Nguyen Tat Thanh University, Ho Chi Minh City, Vietnam; Department of Epidemiology and Biostatistics (J Wei PhD), George Washington University, Washington, DC, USA; Psychology Department (A Yadollahpour PhD), University of Sheffield, Sheffield, UK; Department of Health Management (V Yiğit PhD), Süleyman Demirel Üniversitesi (Süleyman Demirel University), Isparta, Turkey; Department of Neuropsychopharmacology (N Yonemoto MPH), National Center of Neurology and Psychiatry, Kodaira, Japan; Department of Public Health (N Yonemoto MPH), Juntendo University, Tokyo, Japan; Department of Epidemiology and Biostatistics (Prof C Yu PhD), School of Medicine (Z Zhang PhD), Wuhan University, Wuhan, China; Department of Clinical Pharmacy and Outcomes Sciences (I Yunusa PhD), University of South Carolina, Columbia, SC, USA; Addictology Department (Prof M S Zastrozhin PhD), Pediatrics Department (A Zastrozhina PhD), Russian Medical Academy of Continuous Professional Education, Moscow, Russia; Ear Institute (Prof A C Davis PhD), University College London, London, UK.
Declaration of interests
LMH reports personal fees from WHO, outside the submitted work. PSB reports personal fees from WHO, outside the submitted work. CRC reports support from the UK National Institute for Health Research (NIHR) Biomedical Research Centre. B-FH was partially supported by China Medical University (CMU109-MF-63), Taichung, Taiwan. SMSI reports grants from National Heart Foundation of Australia and National Health and Medical Research Council (NHMRC); personal fees from WHO; and partial funding by the National Heart Foundation of Australia and NHMRC, outside the submitted work. WM is program analyst in population and development at the UN Population Fund country office in Peru, which does not necessarily endorse this study. JAS reports consultancy fees from Crealta/Horizon, Medisys, Fidia, Two labs, Adept Field Solutions, Clinical Care options, Clearview Healthcare Partners, Putnam Associates, Focus Forward, Navigant Consulting, Spherix, MedIQ, UBM, Trio Health, Medscape, WebMD, Practice Point communications, the National Institutes of Health, and the American College of Rheumatology; payment for lectures including service on Simply Speaking speaker's bureau; stock ownership in TPT Global Tech, Vaxart pharmaceuticals, and Charlotte's Web Holdings. JAS previously owned stock options in Amarin, Viking, and Moderna pharmaceuticals; held placement on the steering committee of OMERACT, an international organisation that develops measures for clinical trials and receives arm's length funding from 12 pharmaceutical companies; serves on the US Food and Drug Administration Arthritis Advisory Committee; is a member of the Veterans Affairs Rheumatology Field Advisory Committee; and is the editor and the Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis. ACD reports sponsorship for meeting from GN Foundation; personal fees from GN UK and EarGym; and grants from Siemens/Sivantos UK, during the conduct of the study. ACD has a patent, HearCheck Screener (University of Manchester), with royalties paid through the University of Manchester, and is a member of the WHO Technical Group for World Hearing Repor. All other authors declare no competing interests.
Contributor Information
GBD 2019 Hearing Loss Collaborators:
Lydia M Haile, Kaloyan Kamenov, Paul Svitil Briant, Aislyn U Orji, Jaimie D Steinmetz, Amir Abdoli, Mohammad Abdollahi, Eman Abu-Gharbieh, Ashkan Afshin, Haroon Ahmed, Tarik Ahmed Rashid, Yonas Akalu, Fares Alahdab, Fahad Mashhour Alanezi, Turki M Alanzi, Hanadi Al Hamad, Liaqat Ali, Vahid Alipour, Rajaa M Al-Raddadi, Hubert Amu, Jalal Arabloo, Morteza Arab-Zozani, Judie Arulappan, Charlie Ashbaugh, Desta Debalkie Atnafu, Zaheer-Ud-Din Babar, Atif Amin Baig, Palash Chandra Banik, Till Winfried Bärnighausen, Amadou Barrow, Rose G Bender, Akshaya Srikanth Bhagavathula, Nikha Bhardwaj, Pankaj Bhardwaj, Sadia Bibi, Ali Bijani, Katrin Burkart, Christopher R Cederroth, Jaykaran Charan, Sonali Gajanan Choudhari, Dinh-Toi Chu, Rosa A S Couto, Amare Belachew Dagnew, Baye Dagnew, Saad M A Dahlawi, Xiaochen Dai, Lalit Dandona, Rakhi Dandona, Assefa Desalew, Deepak Dhamnetiya, Mandira Lamichhane Dhimal, Meghnath Dhimal, Kerrie E Doyle, Bruce B Duncan, Michael Ekholuenetale, Irina Filip, Florian Fischer, Richard Charles Franklin, Abhay Motiramji Gaidhane, Shilpa Gaidhane, Silvano Gallus, Farhad Ghamari, Ahmad Ghashghaee, Ghozali Ghozali, Syed Amir Gilani, Ionela-Roxana Glavan, Mahaveer Golechha, Bárbara Niegia Garcia Goulart, Veer Bala Gupta, Vivek Kumar Gupta, Samer Hamidi, Billy Randall Hammond, Simon I Hay, Khezar Hayat, Golnaz Heidari, Howard J Hoffman, Kathleen Pillsbury Hopf, Mehdi Hosseinzadeh, Mowafa Househ, Rabia Hussain, Bing-Fang Hwang, Ivo Iavicoli, Segun Emmanuel Ibitoye, Olayinka Stephen Ilesanmi, Seyed Sina Naghibi Irvani, Sheikh Mohammed Shariful Islam, Masao Iwagami, Louis Jacob, Sathish Kumar Jayapal, Ravi Prakash Jha, Jost B Jonas, Rohollah Kalhor, Nawzad Kameran Al-Salihi, Himal Kandel, Ayele Semachew Kasa, Gbenga A Kayode, Rovshan Khalilov, Ejaz Ahmad Khan, Mahalaqua Nazli Khatib, Soewarta Kosen, Ai Koyanagi, G Anil Kumar, Iván Landires, Savita Lasrado, Stephen S Lim, Xuefeng Liu, Stany W Lobo, Alessandra Lugo, Alaa Makki, Walter Mendoza, Amanual Getnet Mersha, Kebadnew Mulatu Mihretie, Ted R Miller, Sanjeev Misra, Teroj Abdulrahman Mohamed, Mokhtar Mohammadi, Abdollah Mohammadian-Hafshejani, Arif Mohammed, Ali H Mokdad, Mohammad Ali Moni, Sandhya Neupane Kandel, Huong Lan Thi Nguyen, Molly R Nixon, Jean Jacques Noubiap, Virginia Nuñez-Samudio, Bogdan Oancea, Victor Maduabuchi Oguoma, Andrew T Olagunju, Bolajoko Olubukunola Olusanya, Jacob Olusegun Olusanya, Hans Orru, Mayowa O Owolabi, Jagadish Rao Padubidri, Keyvan Pakshir, Shahina Pardhan, Fatemeh Pashazadeh Kan, Maja Pasovic, Shrikant Pawar, Hai Quang Pham, Marina Pinheiro, Akram Pourshams, Navid Rabiee, Mohammad Rabiee, Amir Radfar, Fakher Rahim, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Mosiur Rahman, Amir Masoud Rahmani, Juwel Rana, Chythra R Rao, Sowmya J Rao, Vahid Rashedi, David Laith Rawaf, Salman Rawaf, Andre M N Renzaho, Aziz Rezapour, Rezaul Karim Ripon, Voilet Rodrigues, Neeti Rustagi, Umar Saeed, Amirhossein Sahebkar, Abdallah M Samy, Milena M Santric-Milicevic, Brijesh Sathian, Maheswar Satpathy, Monika Sawhney, Winfried Schlee, Maria Inês Schmidt, Allen Seylani, Masood Ali Shaikh, Mohammed Shannawaz, Wondimeneh Shibabaw Shiferaw, Soraya Siabani, Anjali Singal, Jasvinder A Singh, Jitendra Kumar Singh, Deepika Singhal, Valentin Yurievich Skryabin, Anna Aleksandrovna Skryabina, Houman Sotoudeh, Emma Elizabeth Spurlock, Biruk Wogayehu Taddele, Animut Tagele Tamiru, Md Ismail Tareque, Rekha Thapar, Marcos Roberto Tovani-Palone, Bach Xuan Tran, Saif Ullah, Sahel Valadan Tahbaz, Francesco S Violante, Vasily Vlassov, Bay Vo, Avina Vongpradith, Giang Thu Vu, Jingkai Wei, Ali Yadollahpour, Seyed Hossein Yahyazadeh Jabbari, Yigizie Yeshaw, Vahit Yigit, Birhanu Wubale Yirdaw, Naohiro Yonemoto, Chuanhua Yu, Ismaeel Yunusa, Mohammad Zamani, Mikhail Sergeevich Zastrozhin, Anasthasia Zastrozhina, Zhi-Jiang Zhang, Jeff T Zhao, Christopher J L Murray, Adrian C Davis, Theo Vos, and Shelly Chadha
Supplementary Material
References
- 1.Tellevik JM. Language and problem solving ability: a comparison between deaf and hearing adolescents. Scand J Psychol. 1981;22:97–100. doi: 10.1111/j.1467-9450.1981.tb00383.x. [DOI] [PubMed] [Google Scholar]
- 2.Livingston G, Huntley J, Sommerlad A. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin FR. Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011;66:1131–1136. doi: 10.1093/gerona/glr115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kramer SE, Kapteyn TS, Kuik DJ, Deeg DJH. The association of hearing impairment and chronic diseases with psychosocial health status in older age. J Aging Health. 2002;14:122–137. doi: 10.1177/089826430201400107. [DOI] [PubMed] [Google Scholar]
- 5.Li C-M, Zhang X, Hoffman HJ, Cotch MF, Themann CL, Wilson MR. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005–2010. JAMA Otolaryngol Head Neck Surg. 2014;140:293–302. doi: 10.1001/jamaoto.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monzani D, Galeazzi GM, Genovese E, Marrara A, Martini A. Psychological profile and social behaviour of working adults with mild or moderate hearing loss. Acta Otorhinolaryngol Ital. 2008;28:61–66. [PMC free article] [PubMed] [Google Scholar]
- 7.Olusanya BO, Newton VE. Global burden of childhood hearing impairment and disease control priorities for developing countries. Lancet. 2007;369:1314–1317. doi: 10.1016/S0140-6736(07)60602-3. [DOI] [PubMed] [Google Scholar]
- 8.Jung D, Bhattacharyya N. Association of hearing loss with decreased employment and income among adults in the United States. Ann Otol Rhinol Laryngol. 2012;121:771–775. doi: 10.1177/000348941212101201. [DOI] [PubMed] [Google Scholar]
- 9.The Lancet Hearing loss: time for sound action. Lancet. 2017;390 doi: 10.1016/S0140-6736(17)33097-0. [DOI] [PubMed] [Google Scholar]
- 10.Wilson BS, Tucci DL, O'Donoghue GM, Merson MH, Frankish H. A Lancet Commission to address the global burden of hearing loss. Lancet. 2019;393:2106–2108. doi: 10.1016/S0140-6736(19)30484-2. [DOI] [PubMed] [Google Scholar]
- 11.WHO . World Health Organization; Geneva: 2021. World report on hearing. [Google Scholar]
- 12.The mounting burden of hearing loss worldwide: gearing up global collaboration ENT Audioliogy News. Nov 1, 2017. https://www.entandaudiologynews.com/features/audiology-features/post/the-mounting-burden-of-hearing-loss-worldwide-gearing-up-global-collaboration
- 13.Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013;23:146–152. doi: 10.1093/eurpub/ckr176. [DOI] [PubMed] [Google Scholar]
- 14.Vos T, Lim SS, Abbafati C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flaxman AD, Vos DT, Murray CJL. University of Washington Press; Seattle, WA: 2015. An integrative metaregression framework for descriptive epidemiology. [Google Scholar]
- 16.Stevens GA, Alkema L, Black RE. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 17.Olusanya BO, Davis AC, Hoffman HJ. Hearing loss grades and the international classification of functioning, disability and health. Bull World Health Organ. 2019;97:725–728. doi: 10.2471/BLT.19.230367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moller A. Epidemiology of tinnitus in adults. In: Møller AR, Langguth B, DeRidder D, Kleinjung T, editors. Textbook of Tinnitus. Springer-Verlag; New York, NY: 2011. pp. 29–37. [Google Scholar]
- 19.Pascolini D, Smith A. Hearing impairment in 2008: a compilation of available epidemiological studies. Int J Audiol. 2009;48:473–485. doi: 10.1080/14992020902803120. [DOI] [PubMed] [Google Scholar]
- 20.NHANES survey methods and analytic guidelines. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx
- 21.GBD 2015 Healthcare Access and Quality Collaborators Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017;390:231–266. doi: 10.1016/S0140-6736(17)30818-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vollset SE, Goren E, Yuan C-W. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet. 2020;396:1285–1306. doi: 10.1016/S0140-6736(20)30677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tharpe AM. Unilateral and mild bilateral hearing loss in children: past and current perspectives. Trends Amplif. 2008;12:7–15. doi: 10.1177/1084713807304668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technol Assess. 2007;11:1–294. doi: 10.3310/hta11420. [DOI] [PubMed] [Google Scholar]
- 25.Kyle FE, Harris M. Predictors of reading development in deaf children: a 3-year longitudinal study. J Exp Child Psychol. 2010;107:229–243. doi: 10.1016/j.jecp.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 26.WHO . World Health Organization; Geneva: 2016. Childhood hearing loss: strategies for prevention and care.https://apps.who.int/iris/handle/10665/204632 [Google Scholar]
- 27.Baltussen R, Smith A. Cost-effectiveness of selected interventions for hearing impairment in Africa and Asia: a mathematical modelling approach. Int J Audiol. 2009;48:144–158. doi: 10.1080/14992020802538081. [DOI] [PubMed] [Google Scholar]
- 28.Orji A, Kamenov K, Dirac M, Davis A, Chadha S, Vos T. Global and regional needs, unmet needs and access to hearing aids. Int J Audiol. 2020;59:166–172. doi: 10.1080/14992027.2020.1721577. [DOI] [PubMed] [Google Scholar]
- 29.Bichey BG, Miyamoto RT. Outcomes in bilateral cochlear implantation. Otolaryngol Head Neck Surg. 2008;138:655–661. doi: 10.1016/j.otohns.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 30.Drennan WR, Banerjee S, Garrison L. PSS26—estimating cost-effective device prices for pediatric cochlear implantation in India. Value Health. 2015;18:A183. [Google Scholar]
- 31.Emmett SD, Tucci DL, Smith M. GDP matters: cost effectiveness of cochlear implantation and deaf education in Sub-Saharan Africa. Otol Neurotol. 2015;36:1357–1365. doi: 10.1097/MAO.0000000000000823. [DOI] [PubMed] [Google Scholar]
- 32.Murray JJ, Hall WC, Snoddon K. Education and health of children with hearing loss: the necessity of signed languages. Bull World Health Organ. 2019;97:711–716. doi: 10.2471/BLT.19.229427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reefhuis J, Honein MA, Whitney CG. Risk of bacterial meningitis in children with cochlear implants. N Engl J Med. 2003;349:435–445. doi: 10.1056/NEJMoa031101. [DOI] [PubMed] [Google Scholar]
- 34.Cunningham LL, Tucci DL. Hearing loss in adults. N Engl J Med. 2017;377:2465–2473. doi: 10.1056/NEJMra1616601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ray K. Hearing loss and diabetes mellitus. Nat Rev Endocrinol. 2010;6:243. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data presented in this manuscript are made publicly available at https://vizhub.healthdata.org/gbd-compare.