Abstract
Pelvic organ prolapse (POP) is a very common condition which can greatly impact a woman’s quality of life. Treatment options are individualized and typically involve a combination of physiotherapy, pessary insertion and surgical treatments. It is well known that nulliparous prolapse in India constitutes 1.5–2% of genital prolapse, while the incidence is even higher (5–8%) for young women who have delivered one or two children, thus making it one of the highest rates in the world. This has necessitated the development of numerous conservative surgical treatment options for POP, which allows women to retain their sexual and reproductive function and therefore allows for subsequent pregnancies. With the controversy surrounding the use of mesh, a variety of surgical treatment options should be considered. Such alternative treatments include the use of surgical sling procedures, which have been used widely in Indian practice for the treatment of POP for over 60 years. This review outlines some of the well-established conservative treatment options for POP. It also highlights the unique contribution of Indian Obstetricians in the development of these conservative surgical treatment options, from prominent Indian Gynecologists including Dr VN Shirodkar, Dr BN Purandare, VN Purandare, RP Soonawala, Brigadier SD Khanna and Dr RM Nadkarni.
Keywords: Pelvic organ prolapse, Conservative management of pelvic organ prolapse, Conservative surgical procedures for pelvic organ prolapse
Introduction
Pelvic organ prolapse (POP) or urogenital organ prolapse is a highly prevalent condition which can negatively affect a woman’s quality of life. Although not a disease, pelvic organ prolapse can cause significant discomfort and pain and can greatly impact activities of daily living, sexual activity and exercise, as well as having a negative effect on a woman’s body image [1].
The treatment options for POP are varied and should be tailored to the individual patient’s needs, though the general principal is that treatment should be given only to those that are symptomatic. Conservative management includes physiotherapy and pessary insertion. Well-established surgical options available include anterior and posterior colporrhaphy, sacrospinous fixation and abdominal sacrocolpopexy, and many of these procedures can be performed with or without the addition of synthetic mesh. There has been significant controversy in the use of mesh in recent years [2]. Although its use has been associated with good success rates [3], severe complications have been reported resulting in significant long-term disability [2, 4].
With the controversy surrounding the use of these mesh, other potential surgical options could be considered. Surgical sling procedures have been employed in India for the treatment of POP for over 60 years. Nulliparous prolapse in India constitutes 1.5–2% of genital prolapse. The incidence is even higher (5–8%) for young women who have delivered one or two children, thus making it one of the highest rates in the world which in turn has resulted in the development of numerous conservative surgical treatment options for POP [5]. Prominent Indian Gynecologists Dr VN Shirodkar [6], Dr BN Purandare [7], Brigadier SD Khanna [8], VN Purandare, RP Soonawala and Dr RM Nadkarni were some of the earliest surgeons to perform and describe these procedures. This article reviews the Indian contribution to the conservative treatment options available for the management of POP, in particular the various conservative surgical options. We also present the details on the surgical sling procedures, which are widely used in India. The conservative treatment options are of particular importance to young women who wish to have fertility sparing surgery.
Incidence
There is some difficulty in accurately determining the incidence of POP, as much of it is unreported. Figures from the UK show that POP accounts for 20% of women on the waiting list for major gynecological surgery [9, 10]. For women who have had a hysterectomy, the risk of prolapse increases with the time post-hysterectomy; the risk is 1% at 3 years post-hysterectomy, and 5% at 17 years after a hysterectomy [10, 11]. There is an increased risk of prolapse with age [10]. Figures from the USA show that nearly 25% of women suffer from pelvic floor disorders [12]. A US study by Nygaard et al. [12] showed that women aged 20–39 years had an incidence 9.7% of at least one pelvic floor disorder and that women aged 80 years or older had a rate of 49.7% (P < 0.01). In the USA, the lifetime risk of surgery for POP in the general female population is 11.1% [13]. A study by Wu et al. estimated that with the increasing aging population, it is expected that by the year 2050, 245,970 women will have surgery for POP [14]. The estimated direct costs of prolapse surgery in the USA alone are greater than $1 billion per year and are expected to rise in line with the predicted increased requirement for surgical procedures [14, 15].
POP is classified by both the anatomical compartment involved and the level of the prolapse. The degree of POP can be quantified using any number of classification systems. These include Jeffcoate’s classification, Shaw’s, Baden walker and Beecham, Malpaz’s, DeLancey’s levels of support, Baden Walker Halfway System and Pelvic Organ Prolapse Quantification (POPQ) [16].
Patients with POP typically present with symptoms such as a bulge or pressure symptoms [17], or something ‘coming out’ of the vagina, which may become worse with prolonged standing. The severity of symptoms does not always correlate with the stage of the prolapse [17–20]. Many women can be asymptomatic, and these women do not require treatment. Other symptoms described include urinary symptoms [19, 21], bowel symptoms [19, 20] and effects on sexual function [19]. Studies have found increased incidence of POP with parous women, particularly those with vaginal deliveries [17, 18], increased maternal age [17, 18] and increased body-mass index [11, 17] as some of the most consistent risk factors in the development of POP. Other factors which have been associated with an increased risk for the development of POP include hysterectomy, chronic straining/chronic constipation, connective tissue disorders [11, 17, 18] and obstetric factors including prolonged second stage [17], birthweight > 4500 g [17, 18] and forceps delivery [17].
Management
Treatment can be either surgical or non-surgical. Non-surgical intervention includes preventative strategies, physiotherapy and the use of pessaries. Lifestyle advice and physiotherapy, particularly directed pelvic floor muscle training (PFMT), are often used in cases of mild to moderate prolapse [22]. Pelvic floor exercises can also be used in conjunction with other conservative treatments, including pessary insertion, to improve symptomatic relief [23]. The use of vaginal pessaries is a suitable option for most women with POP and can be used for women with or without a hysterectomy. Continuous use of pessaries is also appropriate and effective in women who are not suitable for surgical intervention and has been used successfully for women with advanced prolapse [24]. Pessary insertion is also an option for symptomatic relief for patients awaiting surgery.
Surgical Treatments
The mainstay of treatment for symptomatic prolapse is surgical. The aims of surgical correction of POP are relief of symptoms, restoration of normal vaginal anatomy, preservation of coitus and urinary and anal continence. The surgical options can be either vaginal or abdominal, laparoscopic or open. Options for surgical treatment include anterior or posterior colporrhaphy with or without vaginal hysterectomy plus or minus sacrospinous fixation. Other recognized surgical procedures include the placement of surgical mesh, either abdominal sacrocolpopexy (laparoscopic or open) or vaginal mesh insertion. There is, however, controversy surrounding the use of various surgical meshes to treat prolapse, particularly in vaginal procedures, as when complications occur, they can have ‘Serious, life changing consequences’ [25]. Mesh, as an option for conservative vaginal surgery, is now avoided due to these potential complications, most notably erosion into the bladder, rectum or vagina.
Conservative Surgical Treatment Options
The choice of surgery is dependent on a number of factors. The desire to preserve reproductive and/or menstrual function and the desire to preserve the uterus are all factors in deciding on particular treatment options. Other factors include concomitant intrapelvic disease, e.g., urinary incontinence and the presence of vaginal vault prolapse in hysterectomized women. The patients’ suitability for surgery and other medical comorbidities also factor into the decision to proceed with different surgical options.
Preservation of Reproductive Function
For those who desire to preserve reproductive function, there are a number of surgical options available to them including: 1. Shirodkar’s Sling operation; 2. Shirodkar’s vaginal prolapse operation; 3. Purandare’s Cervicopexy; 4. Modification of Purandare’s Cervicopexy; 5. Khanna’s Sling operation; 6. The Composite Sling operation; 7. Soonawala’s sling operation; and 8. Nadkarni Operation. All of the above types of sling operations are performed abdominally either by open or laparoscopic techniques and may be associated with paravaginal repair of vaginal prolapse where necessary. The advantages of an endoscopic approach include a quicker recovery time and a shorter hospital stay for the patient, as well as better exposure and magnification of tissue. Anterior or posterior colporrhaphy can also be performed as part of the same procedure if clinically indicated. Although performed in India for over 60 years, there are less data to our knowledge on the long-term success and recurrence rates associated with these procedures. The data available are primarily in the form of case series, and data would suggest that these are acceptable treatment options for patients, with low complication rates and low recurrence rates [26]. However, more robust data are required in the form of randomized control trials in order to make more accurate recommendations and to determine the suitability of these procedures as alternative treatment options for POP.
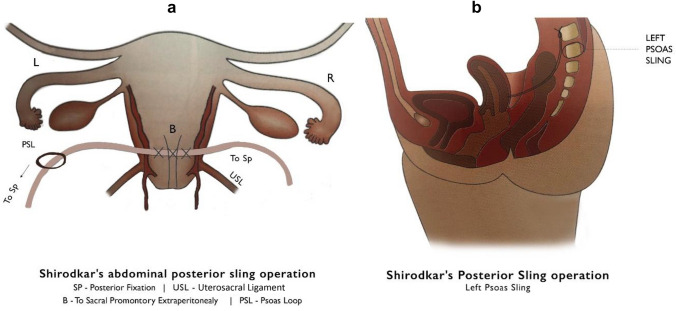
Shirodkar’s Sling operation (Fig. 1a, b) from VN Shirodkar (Image 1) [5, 6, 27] was one of the first described sling operations. His many surgical contributions include operations for prolapse repair, tuboplasty, the creation of a neovagina and the internationally acclaimed Shirodkar Cerclage [28]. The principles and techniques of Shirodkar’s surgeries highlight his appreciation of engineering. Dr. Shirodkar devised this operation for the management of prolapse in women of childbearing age [29]. Shirodkar’s sling operation could be described as technically near-perfect procedure. This procedure is performed abdominally, the aim of which is to strengthen or ‘recreate’ the uterosacral ligaments. The tape is fixed to the posterior aspect of cervix at the level of internal os and is then taken extra-peritoneally, toward sacral promontory and transfixed at this point. On the left side a tape loop is formed on psoas muscle, through which the tape is then passed. This avoids any resulting pressure or obstruction of the sigmoid colon by the tape placement. The advantages of this procedure include that this is the most anatomically correct operation and provides strong static support, with a decreased tendency for enterocoele formation [5]. The disadvantage is that this is technically difficult procedure to perform [5]. There is a risk of injury to the presacral veins and hematoma formation, as well as damage to external iliac vessels, ureters, sigmoid colon, nerve trunks in the retroperitoneal area and the left genitofemoral nerve and later a risk of bowel obstruction. A further disadvantage is that the cervix is displaced posteriorly and hence can impede dilatation of the cervix in a subsequent vaginal delivery.
Fig. 1.
Shirodkar's Abdominal Posterior Sling Operation
Image 1.
Dr V.N. Shirodkar
-
2.
In 1946 Dr Shirodkar devised an innovative approach of using the uterosacral ligaments for the repair of prolapse without amputation of cervix with good success rates [30] called Shirodkar’s vaginal prolapse operation (‘Modified Fothergill's or Manchester operation’) (Fig. 2). A circular incision is made on the cervix and the bladder dissected and pushed up, exposing the cervix. The posterior pouch is opened and both uterosacral ligaments are clamped, cut and ligated. They are then advanced anteriorly, crossing over and then fixed to the cervix at the level of internal os. The posterior pouch is then closed, and the vagina sutured circumferentially with interrupted sutures. In this procedure, the cervix is not amputated, as is performed in the Manchester procedure, as Shirodkar believed that cervical preservation is vital for further childbearing and thus avoids the risk of cervical incompetence secondary to amputation. A potential disadvantage is that caesarian delivery can be difficult due to uterosacral advancement.
-
3.
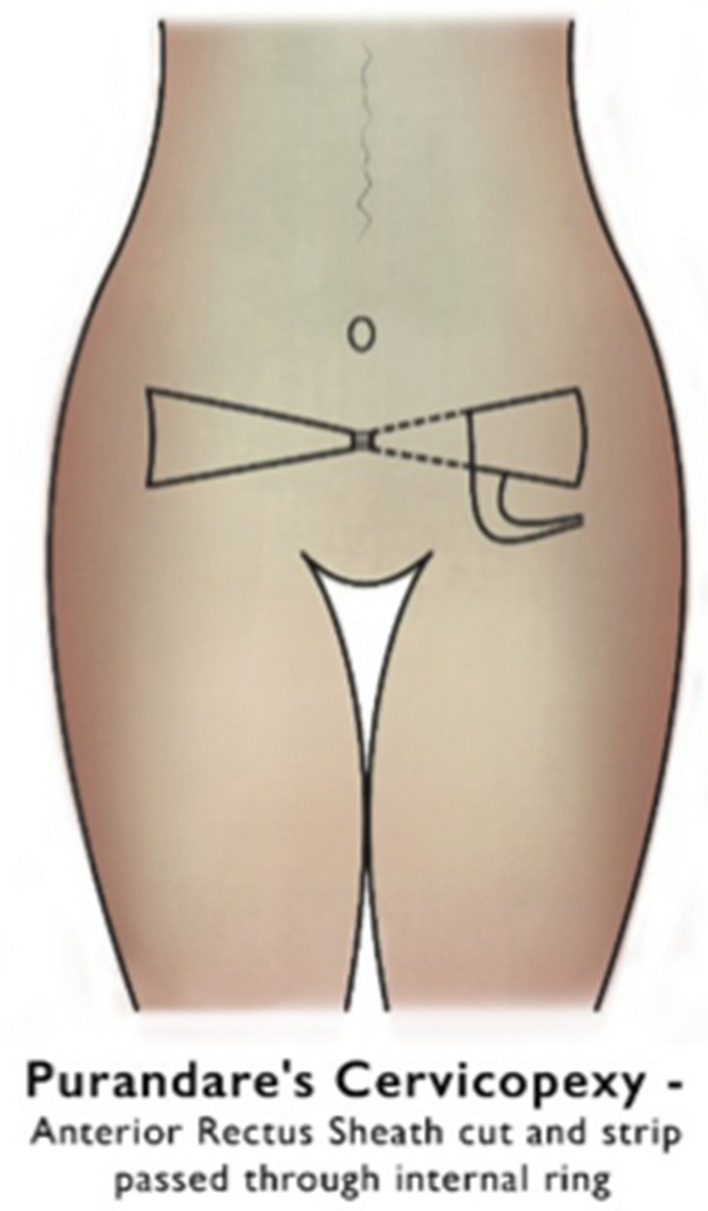
Purandare’s Cervicopexy (Fig. 3) was first described by Dr B.N. Purandare in 1965 (Image 2) [5, 7]. Dr B.N. Purandare was a premier vaginal surgeon with excellent skills, and he devised the abdominal cervicopexy operation for prolapse which revolutionized the conservative surgeries for prolapse [31]. It is a closed loop, anterior sling operation. In this procedure, slings are formed from the rectus sheath and fixed on the anterior surface of the uterus near the isthmus. This is a dynamic operation, as when the patient coughs the cervix is pulled up as the rectus sheath contracts. The fat is cleared over rectus sheath and the sheath dissected from rectus muscle. A strip of rectus sheath is then created on either side with a wider 2 cm base up to the ring, which is lateral to the rectus muscle. The tip of the strips created is transfixed with a long linen suture. Bladder peritoneum is incised and dissected downward. A long artery forceps is then used to pass the strips extra-peritoneally along the round ligament through internal ring and come out at the lateral aspect of rectus muscle, where the base of the strip is located. The tip of the forceps can then grasp the linen suture, and it is pulled in through the ring in front of the cervix. Both side sheath strips are then cross across and are transfixed onto the cervix at the level of the internal os. Vesicular peritoneum is then closed. Bilateral round ligament plication is done in order to antevert the uterus. The risks of this procedure include injury to the inferior epigastric vessels. In this procedure, the uterus becomes retroverted resulting in a tendency for enterocele formation [5]. Subsequent delivery by cesarean section can result in difficulty getting adequate exposure of the lower uterine segment, and the sling can be damaged [5].
Fig. 2.
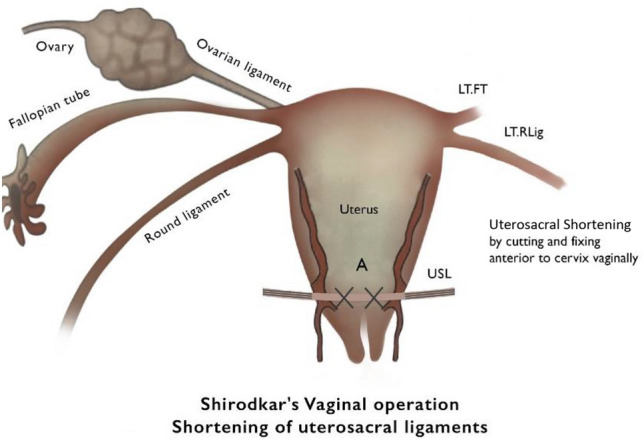
Shirodkar's Vaginal Operation
Fig. 3.
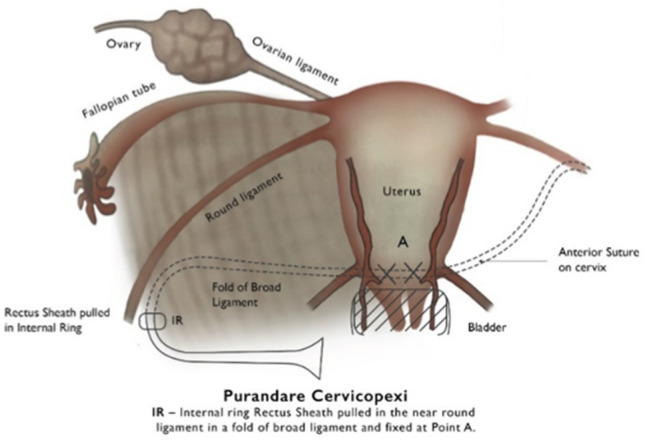
Purandare's Cervicopexy
Image 2.
Dr B.N. Purandare
-
4.
The Modified Purandare’s Cervicopexy (Fig. 4) by V.N. Purandare (Image 3) uses Mersilene tape [5, 32]. Dr. V. N. Purandare was a WHO Consultant for Mother and Child Health Research from 1970 to 1983. He was also a popular orator and presented lectures in several foreign universities including Japan, Sweden, UK, and USA. He was often invited to demonstrate his gynecological surgeries including his own vagino-abdominal hysterectomy [33]. The abdomen is opened by a suprapubic transverse incision. The peritoneum is opened, and the uterus is elevated using a uterus holding forceps. The utero-vesical (UV) fold is incised, and bladder reflected down. The Mersilene tape (30 cm long, 5 mm broad) is stitched at the uterine isthmus anteriorly. A Bonney’s round ligament forceps is used to pass the tape laterally through the rectus abdominus through the posterior sheath and then through the broad ligament to enter at the level of the UV fold. The tape is drawn out through the broad ligament and sutured to the aponeurosis of the external oblique muscle. The ends of the tape brought out should be pulled to keep the uterus in the anatomical position. The round ligaments are plicated, and the tapes are crossed in front of the recti and sutured to each other.
Fig. 4.
Purandare's Cervicopexy
Image 3

Dr V.N. Purandare
-
5.
Khanna’s sling operation (Fig. 5), devised by Brigadier SD Khanna (Image 4) in Mumbai, is an open, anatomically neutral sling operation. In 1972, Brigadier SD Khanna presented a video of his technique for the conservative treatment of nulliparous prolapse during a Maternal Mortality Conference in Mumbai [5]. The primary aim of Khanna’s sling is to bolster the cardinal ligaments [5]. The ends of the tape are attached to anterior superior iliac spines. The disadvantages include that the tape is superficial and can be easily felt by the patient [5]. There is also a risk of periostitis and a risk of the tape getting detached.
Fig. 5.
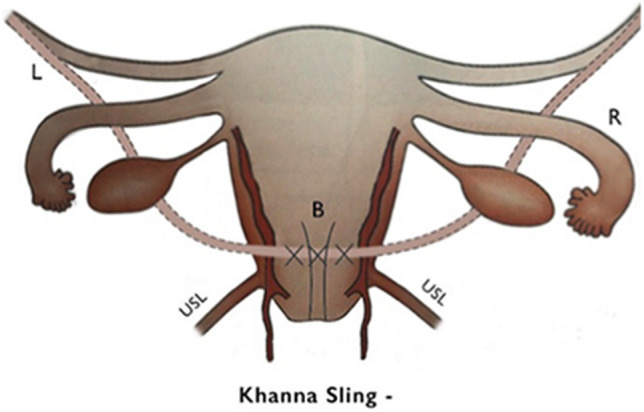
Khanna Sling
Image 4.
Brig. S.D. Khanna
-
6.
All the abdominal operations can now be performed laparoscopically. The Laparoscopic Composite Sling is a combination of the anterior sling on left side and posterior sling on right side, essentially combining both the Shirodkar and Purandare techniques [8]. The advantage is that it avoids compression of sigmoid on the left side. Disadvantages include that significant training is required to perform this complex laparoscopic procedure.
-
7.
Soonawala’s Sling Operation, devised by Dr R.P. Soonawala (Image 5), is a unilateral posterior sling surgery to reinforce the uterosacral ligaments [8]. Dr R.P. Soonawala is recognized for his many innovations including the modified Gynecological Operative Techniques, designing over 12 Gynecological Instruments and two Intrauterine Contraceptive Devices [34]. It is essentially a right-sided Shirodkar’s sling and with left side plication of the round ligaments to prevent deviation of uterus. The advantages of this procedure include that there is no risk of bowel obstruction or injury, though the position of the uterus may be distorted.
Image 5.

Dr R. P. Soonawala
-
8.
The Nadkarni Operation [35] was devised by Dr R M Nadkarni for supravaginal elongation of the cervix and is also termed the Nadkarni’s Sleeve Excision. Dr Nadkarni’s hypothesis was converse to Fothergill's operation, where the vaginal portion of the cervix which aides in fertility is removed. He hypothesized that it is in fact the supravaginal portion of cervix which is elongated and thus results in subsequent prolapse. In this prolapse operation, a semi-circular vaginal incision is placed in the cervix and both cardinal ligaments are then clamped and held as support. The bladder peritoneum is opened to expose the anterior pouch. At the level of the isthmus, an “I”-shaped incision is made between the body of the uterus and the lower one-third of cervix, i.e. the vaginal portion. A cylindrical wedge of the central core of the cervix is then removed, and body of the uterus is anastomosed to the vaginal portion of cervix with interrupted sutures over a Hegar dilator, which is passed through the cervix into body of the uterus for both support and easy delineation of cervical canal. The ‘I’-shaped fascial incision is then closed. The round ligament is shortened and plicated, but only anteversion of the uterus is achieved and it remains as a weak support of the uterus. The vagina is closed with interrupted sutures. A Foley catheter is inserted inside to cervix, with the balloon in the uterine cavity, for 5 days postoperatively to support the anastomosis. While there is the advantage of retaining the vaginal portion of cervix, the round ligaments are weakened through this procedure. A further disadvantage is that the anastomoses is a potential area of rupture in a subsequent pregnancy.
Preservation of Menstrual Function
For those desiring to preserve menstrual function or preserve the uterus but not reproductive function, the Manchester operation—1888 (Fothergill’s operation)—can be performed. This involves dilatation and curettage, followed by shortening of the cardinal ligaments, partial amputation of cervix and insertion of Sturmdorf sutures. This is usually accompanied by an anterior colporrhaphy ± posterior colporrhaphy. It is not recommended in women desiring reproductive function as it can result in cervical stenosis, infertility, an incompetent cervix and a high risk of recurrence of the prolapse after a subsequent pregnancy.
Options for Women Who DO Not Wish to Preserve Sexual Function
For postmenopausal women who have no desire to preserve sexual function, particularly for women with additional medical comorbidities and those that are medically unfit for surgery, the Le Forts procedure may be an acceptable conservative approach to treat prolapse in this cohort of patients. Le Forts procedure, sometimes called colpocleisis, involves suturing the front and back walls of the vagina together. Anterior to posterior fusion of vagina is done in the midline leaving gutters on either side to allow drainage of vaginal secretions. This automatically prevents uterus from descending in the midline. In the appropriate patient cohort surgical intervention of this type has been shown to have a positive impact on bowel, bladder, and prolapse symptoms, with a high rate of satisfaction and low levels of regret [36, 37].
Conclusion
POP is an extremely common condition and can have a significant impact on the daily activities of the women affected. Clinicians have multiple treatment options available to them to offer patients including advice on lifestyle modification, physiotherapy and focused PFMT, pessary insertion and surgical treatment. The distinctive surgical sling procedures, developed by prominent Indian gynecologists, highlight the importance of considering all treatment options and tailoring the treatment to each individual patient, particularly those wishing to preserve their reproductive function.
Dr Gillian A. Ryan MB BCh BAO MRCPI MRCOG MD
is a graduate of medicine from University College Dublin. She is currently the Maternal and Fetal Medicine RCOG Subspecialty Fellow in the National Maternity Hospital, Dublin. She has a special interest in education and training and is involved in the Royal College of Physicians Ireland.
Compliance with Ethical Standards
Conflict of interest
The authors report no conflict of interest.
Footnotes
Dr Gillian A Ryan MB BCh BAO MRCPI MRCOG MD is a graduate from University College Dublin, Ireland. She has completed an MD through UCD. She is currently the Maternal and Fetal Medicine RCOG Subspecialty Fellow in the National Maternity Hospital Dublin. Dr Nikhil Purandare is a Consultant Obstetrician and Gynaecologist and Fertility sub specialist at University College Hospital Galway. He is Hon. Senior Lecturer in the department of Obstetrics and Gynaecology at the National University of Ireland. He is clinical director at Fertility and Fetal Health, Galway. Dr Simran Ganeriwal MB BCh BAO (Hons) Graduate of the Royal College of Surgeons Ireland 2020. She is due to begin residency in the USA in July 2021. Professor Chittaranjan N Purandare MD FICOG FRCOG: Emeritus Dean Indian College of Obstetrics and Gynecology, India; Past President FIGO.
Figures provided by Nutan Ajgaonkar.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lowder JL, Ghetti C, Nikolajski C, Oliphant SS, Zyczynski HM. Body image perceptions in women with pelvic organ prolapse: a qualitative study. Am J Obstet Gynecol. 2011;204(5):441.e1. doi: 10.1016/j.ajog.2010.12.024. [DOI] [PubMed] [Google Scholar]
- 2.FDA U.S. Food and Drug Administration. 2011 UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA safety communication. http://wayback.archive-it.org/7993/20170722150848/; https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. [DOI] [PubMed]
- 3.Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CM. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;4:CD004014. doi: 10.1002/14651858.CD004014.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Barski D, Otto T, Gerullis H. Systematic review and classification of complications after anterior, posterior, apical, and total vaginal mesh implantation for prolapse repair. Surg Technol Int. 2014;24:217–224. [PubMed] [Google Scholar]
- 5.Virkud A. Conservative operations in genital prolapse. J Obst Gynaecol India. 2016;66(3):144–148. doi: 10.1007/s13224-016-0909-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shirodkar VN. C R Soc Franc Gynec. 1952;22:99. [PubMed] [Google Scholar]
- 7.Purandare VN. New surgical technique for surgical correction of genital prolapse in young women. J Obstet Gynaecol India. 1965:53–62.
- 8.Daftary SN, Desai SV. Selected topics in obstetrics and gynaecology-2: for postgraudates and practitioners: chapter 12, p 208–210.
- 9.Prolapse CL. In: Dewhurst’s textbook of obstetrics and gynaecology for postgraduates. Whitfield CR, editor. Oxford: Blackwell Science; 1995. pp. 642–652. [Google Scholar]
- 10.Ranee T, Stuart S. Management of genital prolapse. BMJ. 2002;324:1258. doi: 10.1136/bmj.324.7348.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104:579–585. doi: 10.1111/j.1471-0528.1997.tb11536.x. [DOI] [PubMed] [Google Scholar]
- 12.Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–1316. doi: 10.1001/jama.300.11.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 14.Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011;205(3):230.e1–230.e5. doi: 10.1016/j.ajog.2011.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001;98:646–651. doi: 10.1016/s0029-7844(01)01472-7. [DOI] [PubMed] [Google Scholar]
- 16.Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17. doi: 10.1016/S0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 17.Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369(9566):1027. doi: 10.1016/S0140-6736(07)60462-0. [DOI] [PubMed] [Google Scholar]
- 18.Samuelsson EC, Arne Victor FT, Tibblin G, Svardsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180:299–305. doi: 10.1016/S0002-9378(99)70203-6. [DOI] [PubMed] [Google Scholar]
- 19.Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–1337. doi: 10.1067/mob.2001.119078. [DOI] [PubMed] [Google Scholar]
- 20.Mouritsen L, Larsen JP. Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(2):122. doi: 10.1007/s00192-002-1024-1. [DOI] [PubMed] [Google Scholar]
- 21.Marinkovic SP, Stanton SL. Incontinence and voiding difficulties associated with prolapse. J Urol. 2004;171(3):1021. doi: 10.1097/01.ju.0000111782.37383.e2. [DOI] [PubMed] [Google Scholar]
- 22.Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;12:CD003882. doi: 10.1002/14651858.CD003882.pub4. [DOI] [PubMed] [Google Scholar]
- 23.Cheung RY, Lee JH, Lee LL, Chung TK, Chan SS. Vaginal pessary in women with symptomatic pelvic organ prolapse: a randomized controlled trial. Obstet Gynecol. 2016;128(1):73–80. doi: 10.1097/AOG.0000000000001489. [DOI] [PubMed] [Google Scholar]
- 24.Dueñas JL, Miceli A. Effectiveness of a continuous-use ring-shaped vaginal pessary without support for advanced pelvic organ prolapse in postmenopausal women. Int Urogynecol J. 2018;29(11):1629–1636. doi: 10.1007/s00192-018-3586-6. [DOI] [PubMed] [Google Scholar]
- 25.NICE Guideline Transvaginal mesh repair of anterior or posterior vaginal wall prolapse. Interventional procedures guidance. December 2017.
- 26.Khanam RA, Rubaiyat A, Azam MS. Sling for correcting uterine prolapse: twelve years’ experience. Mymensingh Med J. 2014;23(1):13–17. [PubMed] [Google Scholar]
- 27.Shirodkar VN. Second World Congress of International Federation of Gynaecology and Obstetrics, Montreal. 1958.
- 28.Purandare CN, Patel M, Balsarkar G. Indian contribution to obstetrics & gynecology. J Obstet Gynaecol India. 2011;61(6):624–625. doi: 10.1007/s13224-012-0126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dastur B, Gurubaxani G, Palnitkar SS. Shirodkar Sling operation in the treatment of genital prolapse. BJOG Int J Obst Gynaecol. 1967;74:125–128. doi: 10.1111/j.1471-0528.1967.tb03947.x. [DOI] [PubMed] [Google Scholar]
- 30.Shaikh R, Sardesai S. Shirodkar’s extended manchester repair: a conservative vaginal surgery for genital prolapse in young women and reinforcement of weak uterosacral ligaments with merselene tape: retrospective and prospective study. Int J Recent Trends Sci Technol. 2014;10(2):263–266. [Google Scholar]
- 31.Purandare CN, Patel M, Balsarkar G. Indian contribution to obstetrics & gynecology. J Obstet Gynaecol India. 2012;62(1):3–4. doi: 10.1007/s13224-012-0159-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rameshkumar R, Kamat L, Tungal S, Moni S. Modified purandare’s cervicopexy-a conservative surgery for genital prolapse: a retrospective study. Int J Reprod Contracept Obstet Gynecol. 2017;6(5):1777–1781. doi: 10.18203/2320-1770.ijrcog20171529. [DOI] [Google Scholar]
- 33.Purandare CN, Patel M, Balsarkar G. Indian contribution to obstetrics & gynecology. J Obstet Gynaecol India. 2013;63(4):216–217. doi: 10.1007/s13224-013-0464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Purandare CN, Patel M, Balsarkar G. Indian contribution to obstetrics & gynecology. J Obstet Gynaecol India. 2013;63(6):361–362. doi: 10.1007/s13224-013-0493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valecha S, Dhingra D. Nadkarni’s Sleeve excision anastomosis for pelvic organ prolapse due to cervical elongation. Int J Curr Res. 2015;7(01):11985–11988. [Google Scholar]
- 36.Crisp CC, Book NM, Smith AL, Cunkelman JA, Mishan V, et al. Body image, regret, and satisfaction following colpocleisis. Am J Obstet Gynecol. 2013;209(5):473.e1–473.e7. doi: 10.1016/j.ajog.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 37.Zebede S, Smith AL, Plowright LN, Hegde A, Aguilar VC, Davila GW. Obliterative LeFort colpocleisis in a large group of elderly women. Obstet Gynecol. 2013;121(2 Pt 1):279–284. doi: 10.1097/AOG.0b013e31827d8fdb. [DOI] [PubMed] [Google Scholar]