Abstract
Background
Atopic diseases, such as atopic dermatitis (AD) and food allergy (FA), have increased in prevalence in industrialized countries during the past few decades and pose a significant health burden. They appear to have a common underlying mechanism and a natural disease progression. AD is generally the first atopic disease to manifest followed by other atopic diseases, such as FA, allergic rhinitis, or allergic asthma suggesting that they are likely different manifestations of the same disease.
Body
Evidence suggests that allergic sensitization occurs through an impaired skin barrier, while consumption of these foods at an early age may actually result in tolerance. This has been termed the Dual-Allergen-Exposure hypothesis. Loss of barrier integrity has been hypothesized to enable penetration of allergens, pollutants, and microbes and initiation of an inflammatory immune cascade of events leading to sensitization. The immune dysfunction is thought to further exacerbate the impaired skin barrier to form a vicious cycle. There is much interest in preventing or protecting the skin barrier from developing a proinflammatory atopic state, which may potentially lead to the development of AD and subsequently, FA.
Conclusion
Research on preventing or treating skin barrier dysfunction is ongoing. A number of studies have evaluated the efficacy of emollients in preventing AD and FA with mixed results. Studies have differed in the study design, population characteristics, emollients type, and frequency, duration, and area of application. Emollient type has varied widely from oils, creams, petrolatum-based lotions, and trilipid creams. Current research is directed towards the use of trilipid emollients that are similar to the skin’s natural lipid composition with a 3:1:1 ratio of ceramides, cholesterol and free fatty acids and a pH that is similar to that of skin to determine their effectiveness for skin barrier repair and prevention of AD and FA.
Keywords: Atopic dermatitis, Ceramides, Eczema, Emollients, Filaggrin, Food allergy, Prevention, Skin barrier, Stratum corneum, Trilipids
Introduction
Allergic diseases, such as atopic dermatitis (AD) and food allergy (FA), have increased in prevalence in industrialized countries during the past few decades and pose a significant health burden. AD is a multifactorial, heterogeneous inflammatory skin disease that affects approximately 13% of children, one third of whom have moderate to severe disease [1]. AD is associated with pruritis, xerosis, lichenification, and eczematous lesions typically on the face (cheeks), neck, arms, and legs. In the US, AD is associated with an adjusted total incremental annual cost between $3,302 and $4,463, depending on the severity of the disease [2]; in Italy, the cost in adults was determined to be €4284 per patient per year [3].
In the US, it is currently estimated that FA affects approximately 1 in 10 adults and 1 in 12 children [4]. Among food-allergic children, a survey found that 42.3% reported ≥ 1 severe FA and 39.9% reported multiple FA [5]. Most allergic reactions are mild; however moderate and severe reactions occur frequently. National time trends show an upsurge of pediatric food-induced anaphylaxis-related hospitalizations and emergency departments visits in the US [6]. Data from a nationwide observational study conducted between 2004 through 2014 in children and adolescents reported 7310 food-induced anaphylaxis related emergency room visits [6]. While any food can cause an allergy, cow’s milk, hen’s egg, peanuts, soy, wheat, tree nuts, fish, and shellfish account for 90% of all FA [7]. Peanut allergy is the most common FA in the U.S. affecting approximately 2% of children [8]. This potentially serious condition usually develops during early childhood and continues into adulthood; approximately 80% of children with peanut allergy will remain peanut allergic throughout their lifetime [9]. FA significantly impacts the quality of life of those affected and their families. In the UK, total costs of peanut allergy were between £33 and 44 million in 2015 [10]; in the US, the overall economic cost of FA was estimated at $25 billion annually or $4184 per affected child per year [11]. Despite efforts of strict adherence to diets void of the offending FA, accidental exposures to food antigens are common due to the numerous possibilities for contamination. The increasing prevalence of atopic diseases and the economic and societal burden they pose presents an unmet and urgent need to develop strategies to reduce the incidence of IgE-mediated food allergies.
Allergic diseases, such as AD and FA, with a Th2-type proinflammatory immune response and increased production of IgE antibodies on exposure to small amounts of otherwise harmless food and environmental allergens are called atopic diseases. Other atopic diseases include allergic rhinitis and allergic asthma. Comorbid atopic diseases in the same individual occur frequently. Studies have found a strong association between AD, particularly AD that is early-onset and severe, and other forms of allergic disease, including FA and asthma [12]. A study found that infants with AD were six times more likely to have egg allergy and 11 times more likely to have peanut allergy by 12 months than infants without eczema [13]. A population-based study found that infants who developed AD within the first year of life were at greater risk for developing FA as confirmed by oral food challenge, within 12 months (one in five infants with AD had FA as compared to one in 25 without AD). Approximately 50% of infants who developed AD within the first 3 months of life requiring use of topical steroids developed FA [14].
Atopic diseases appear to have a natural progression with AD being the first to manifest, generally in infancy or childhood, followed by other atopic diseases, such as FA, allergic rhinitis, or allergic asthma [15]. This natural progression of atopic diseases is termed the “Allergic March” or “Atopic March.” The presence of IgE antibodies, proinflammatory Th2-type cytokines and the natural progression observed with atopic diseases have led some researchers to suggest that they are all different manifestations of the same disease. Researchers have also hypothesized that by preventing or treating AD in early infancy or childhood, it may be possible to prevent its progression to FA. This notion has further been strengthened by evidence of the skin as a route of sensitization for both AD and FA. The skin is thought to be the site of allergic sensitization with AD being the first manifestation of the atopic cascade, followed by a natural progression to FA and other atopic respiratory diseases.
Here we review the mechanism underlying immune dysregulation in atopic disease, current evidence that suggest that dysregulation of the epidermal barrier initiates a cascade of immune events leading to atopic sensitization and increased risk of AD and FA, and risk factors for development of atopic disease. We also review our current knowledge of early intervention to repair or treat skin barrier dysfunction as a strategy for prevention of AD and its progression to FA.
Immune mechanisms underlying atopic disease
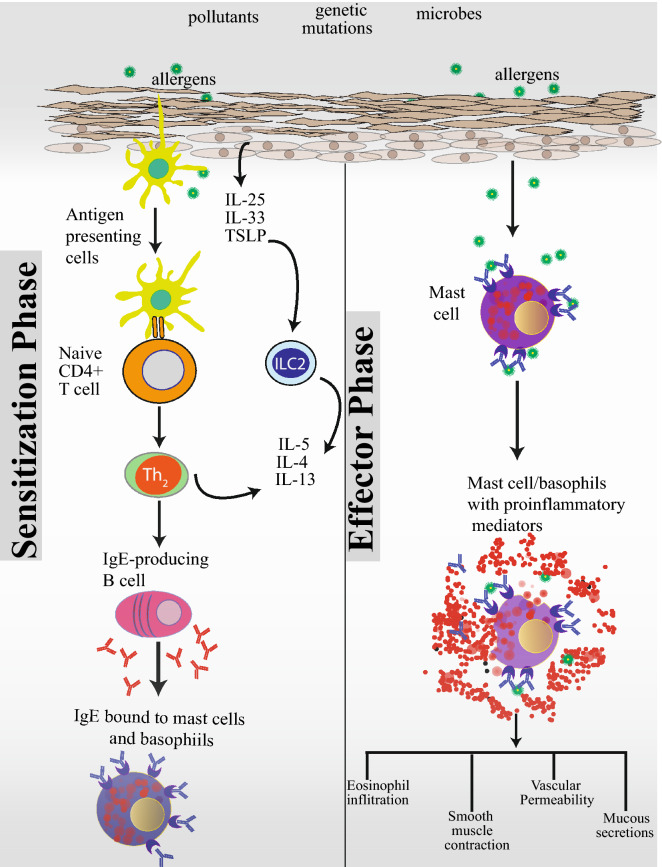
IgE-mediated reactions include two phases—a sensitization phase and an effector phase (Fig. 1). An impaired skin barrier promotes release of proinflammatory epithelial-derived cytokines, IL-25, IL-33, and thymic stromal lymphopoietin (TSLP), which initiate and propagate Type 2 inflammatory responses in AD, food-hypersensitivity reactions, and asthma [16]. These cytokines, initiate a cascade of reactions starting with the activation of dendritic cells and innate lymphoid cells type 2 (ILC2). Dendritic cells, which are present at barrier surfaces capture and present processed allergens through MHC class II molecules to naïve T cells in the draining lymph nodes. Naive T cells in the presence of IL‐4 differentiate into proinflammatory Th2 cells. Th2 cells are the major cell type that skews immune reaction towards allergy by producing cytokines IL-4, IL-5, IL-9, and IL-13. In the presence of IL-4 and IL-13, which are produced by both Th2 and ILC2 cells, B-cells undergo isotype class switching to IgE producing cells and differentiate into plasma cells. IgE antibodies then bind to high-affinity FcεRI receptors on the surface of mast cells and basophils and prime the cells to react on future encounters with the allergen, leading to sensitization.
Fig. 1.
A dysfunctional skin barrier caused by exposure to pollutants, pathogenic microbes, and genetic mutations predisposes towards atopic sensitization, the first manifestation of which is atopic dermatitis. An impaired skin barrier releases proinflammatory epidermal cytokines, IL-25, IL-33, and TSLP. In this proinflammatory environment, resident antigen presenting cells further skew naïve T cells towards a Th2 proinflammatory state. ILC2 cells also play a key role in allergic sensitization. ILC2 cells are found near barrier surfaces and are activated by IL-33. Th2 and ILC2 cells produce a number of cytokines, key among them being IL-4, IL-5 and IL-13. In the presence of IL-4 and IL-13, B-cells undergo isotype class switching to IgE producing cells. IgE antibodies then bind to high-affinity FcεRI receptors on the surface of mast cells and basophils and prime these cells for future encounters with the allergen leading to a state of atopic sensitization. In sensitized individuals, subsequent encounters with an allergen leads to cross linking of IgE bound to FcεRI receptors and degranulation and release of proinflammatory mediators by basophils and mast cells leading to eosinophilic infiltration, smooth muscle contraction, vascular permeability, and mucous secretion
When primed mast cells and basophils in sensitized individuals encounter an allergen, FcεRI-bound IgE antibodies crosslink and activate degranulation. Degranulation of mast cells and basophils lead to the release of histamine and other inflammatory chemical mediators (cytokines, interleukins, leukotrienes, and prostaglandins) into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion, tissue eosinophilic infiltration, and smooth muscle contraction leading to the symptoms of allergic reaction. Symptoms can be mild, moderate, severe, or even life-threatening. Further details of the mechanisms underlying atopic disease can be found in a number of excellent reviews [17].
Epidermal barrier and immune dysfunction: the inside-out, outside-in, and ouside-inside-outside hypothesis
Evidence suggests that allergic sensitization occurs through an impaired skin barrier (either through genetic defects, mechanical injury, or exposure to chemicals or toxins). Loss of barrier integrity has been hypothesized to enable penetration of allergens, pollutants, and microbes and initiation of an inflammatory immune cascade of events leading to sensitization [18]. Studies using murine models have found that repeated skin exposure to egg allergen induced eczematous skin lesions and asthma-like airway hyperresponsiveness following subsequent exposure to egg allergens aerosol [19]. In mice, exposure to peanut allergens via the application of peanut oil through a disrupted skin barrier (via tape stripping) increased total serum IgE [20]. In a study of around 1,900 infants, skin barrier dysfunction, as determined by transepidermal water loss (TEWL), predicted FA at 2 years of age, supporting the concept of transcutaneous allergen sensitization, even in infants who do not have AD [21]. The increased risk of peanut sensitization and FA has been associated with environmental exposure to peanut allergens. The amount of peanut consumed within the home is associated with the level of peanut allergen in household dust and bedding. [22] Increased exposure to peanut in households is associated with increased peanut sensitization and allergy in children with an impaired skin barrier [23] and AD [24], but not in children without these risk factors, suggesting that sensitization to environmental allergens occurs via an impaired skin barrier. The effect of environmental peanut allergen exposure on children with skin barrier dysfunction provides evidence that sensitization to environmental allergens occurs through the skin. Data from the Avon Longitudinal Study of Parents and Children, a geographically defined cohort study of 13,971 preschool children, suggested that sensitization to peanut protein may occur in children through the application of peanut oil to inflamed skin [25].
Gene mutations that increase skin barrier integrity have also been implicated in AD and FA. Twin studies of AD indicate a heritability of approximately 75% [26] with the remaining 25% attributed to environmental factors. The strongest known genetic risk factor for AD is a loss of function mutation of the gene encoding filaggrin (FLG) [27]. FLG aggregates keratin filaments and is crucial for maintaining skin barrier function. A loss of function mutation of FLG leads to epidermal barrier dysfunction making the skin more permeable to environmental allergens and pollutants, while increasing TEWL. Individuals with double allele mutations in FLG tend to develop early-onset and more severe AD [28]. A study in infants found that by 3 months of age, FLG mutations were associated with AD, dry skin, and increased TEWL. TEWL was elevated even in unaffected FLG mutation carriers suggesting that skin barrier impairment precedes clinical AD [29].
Evidence suggests that both epidermal barrier dysfunction, as well as immune deviation towards a Th2 proinflammatory profile, play important roles in allergic disease. However, whether epidermal barrier dysfunction is secondary to immune deviation (the inside-out hypothesis) or whether immune deviation is secondary to a dysfunctional epidermal barrier (the outside-in hypothesis) has been debated. The discovery of FLG mutation and its role in epidermal integrity and AD provided strong evidence of the outside-in hypothesis. Dupilumab, an anti-IL4R-monoclonal antibody (which blocks the action of IL-4 and IL-13) is approved for the treatment of AD. Similarly, omalizumab, an anti-IgE antibody is approved for the treatment of allergic asthma. These antibodies which ameliorate symptoms of AD and allergic asthma by targeting type-2 immune responses lend support for the inside-out hypothesis. The most recent hypothesis being put forth is the “outside-inside-outside” view, which suggests that the skin barrier deficiency leads to immune imbalance, which further exacerbates the impaired skin barrier to form a vicious cycle [30].
Environmental factors that influence epidermal barrier integrity and increase risk of AD and FA
With urbanization, barrier surfaces are increasingly exposed to air pollutants, which have been shown to affect skin barrier integrity and increase risk of atopic diseases. Increased hygiene has led to decreases in exposure to microbial diversity. In recent years, numerous studies have shown the importance of the gut and skin microbiome in maintaining immune health and barrier integrity. Factors associated with a healthy microbiome include vaginal delivery, breast feeding, and presence of older siblings. Dysbiosis of the microbiome is associated with Caesarean section, increased use of soaps and detergents, processed foods including formula milk, and exposure to antibiotics and antacids [31].
A study of AD patients found that the severity of AD symptoms was positively correlated with outdoor temperatures, relative humidity, precipitation, particulate matter (PM) with an aerodynamic diameter < 10 μm (PM10), NO2, ozone, and total pollen count [32]. Short-term exposure to PM was found to exacerbate AD in young children living in an industrial urban area. The study also found that PM2.5 had a stronger effect than PM10 on exacerbation of AD symptoms [33]. The study of 14,614 children from the Seoul Atopy Friendly School Project Survey in Seoul, Korea, in 2010 found increased risk of eczema was associated with NO2 and PM10 [34].
Studies indicate that low pH values in skin extracellular spaces play an important role in the regulation of enzyme activity, especially in keratinization and barrier regeneration [35]. Soaps and detergents have been implicated in increasing skin pH, enhancing the activity of proteases, decreasing the activity of enzymes associated with lipid synthesis, and disrupting epidermal integrity and cohesion [36]. In mice models of AD, antibiotic use was associated with increased TEWL compared to those treated with probiotics [37]. A large retrospective cohort study found that the use of acid-suppressive medications and antibiotics during the first 6 months of infancy was associated with subsequent development of allergic disease [38]. Clostridium difficile colonization during infancy has been associated with a higher risk of developing allergic diseases during early childhood [39]. In AD, colonization by Staphylococcus aureus in skin is commonly observed and has been correlated with increased expression of proinflammatory cytokines, IL-4, IL-13, IL-22, and TSLP [40].
Prevention of food allergy
Palforzia, a peanut allergen formulation, is currently the only FDA approved oral immunotherapy treatment for FA. For other food allergens, there are no approved treatments and standard of care remains avoidance of allergenic foods and acute management of allergic reactions with antihistamines or epinephrine. Allergen avoidance is difficult to accomplish as many allergenic foods are common ingredients in many foods. A study found that around 58% of individuals with peanut allergy accidentally consume peanuts within a 5-year period [41].
Oral tolerance: early introduction of allergic foods
Early guidelines for prevention of FA recommended delaying the introduction of allergenic foods to infants to 1–3 years of age [42]. However, even with the implementation of these new guidelines, rates of FA continued to increase. In 2015, results of the LEAP study were published [43]. The LEAP study was a large study of 640 infants between 4 through 11 months of age, randomized to various treatment arms. All of the infants had severe eczema, egg allergy or both. The study found that peanut avoidance was linked to a higher rate of peanut allergy compared to peanut consumption and that regular exposure resulted in a 11.8% decrease in the cumulative incidence of FA. The study provided evidence that early oral introduction of peanuts could prevent allergy in infants at high risk of allergy. The EAT study [44], randomized 1300 exclusively breastfed 3‐month‐old infants from the general population and compared the effect of early introduction of 6 common childhood food allergens (milk, egg, peanut, sesame, fish, and wheat) with exclusive breastfeeding until approximately 6 months of age. Overall, the study found that FA was lower in the group introduced to allergenic foods early but the difference was not statistically significant. As these newer findings did not support avoidance for prevention, guidelines were revised and in 2010 recommended introduction of allergenic foods, such as peanut, tree nuts, and egg at 4 to 6 months of age, after a period of exclusive breastfeeding [45]. Additionally, further analysis of the EAT study in 2019 also supported these guidelines as statistical differences were observed in specific groups of infants at high risk of developing FA: those sensitized to egg or to any food at enrollment and those with eczema of increasing severity at enrollment as compared to exclusively breastfed infants [46]. These studies led to the concept of oral ingestion of allergenic foods as a route to tolerance. This, in conjunction with current understanding of skin barrier defects as a route of atopic sensitization has led to the Dual-Allergen-Exposure hypothesis, which states that exposure to food allergens through the skin can lead to allergy, while consumption of these foods at an early age may actually result in tolerance. However, induction of tolerance through early introduction of food allergens presents a number of challenges [47, 48]. The protective effects of early food protein allergen exposure appear to be allergen-specific suggesting that early introduction of one food protein allergen does not prevent the development of FA to other allergens and that multiple food introductions in early life are necessary to prevent all FA. Another limitation of early allergenic food introduction as an approach to prevent multiple food allergies is the narrow window of time allowed for tolerance induction. Further, adherence presents logistic challenges in the inclusion of multiple allergenic foods in young infants is difficult.
Emollients for AD prevention and progression to FA
Current evidence suggests that skin barrier defects increase risk of AD, FA, and other atopic diseases. A study by Kelleher et al. found that impairment of skin barrier function, as determined by TEWL, at birth and at 2 months precedes clinical AD [49]. In another study, Kelleher found that neonatal skin barrier dysfunction predicts FA at 2 years of age [21]. In 2014, two randomized controlled trials evaluated the use of emollients in newborn infants at high risk of AD. The study by Simpson, et al. found that daily full body emollient use significantly reduced the cumulative incidence of atopic AD corresponding to a relative risk reduction of 50% [50]. These results were supported by a study by Horimukai, et al., where emollient use lowered AD by 32% [51]. Regular emollient use in newborn infants was also found to decrease diaper dermatitis. The study also measured face TEWL and body stratum corneum hydration (SCH) and found that while TEWL decreased, SCH increased providing further evidence that moisturizing skincare may prevent newborns' diaper dermatitis by improving skin barrier function. The PEBBLES pilot study in 2018 was the first to evaluate the role of emollients in preventing food sensitization in addition to AD. Emollient use demonstrated a non-significant trends towards decreased food sensitization at 6 and 12 months of age in addition to a non-significant trend towards a reduction in AD at 12 months. Per protocol analyses (only including infants who received ≥ 5 days/week of study treatment) revealed a significant reduction in food sensitization at 12 months in the treatment group [52]. McClanahan et al. conducted a 2-year randomized controlled trial of newborns at high risk of AD who received full body application of emollients started with 21 days of birth. In addition to AD, measures of skin barrier integrity and skin microbiome were assessed. The study found a decreasing trend in AD in the intervention group compared to controls at 2 years, but other measures of skin barrier function (TEWL, pH, stratum corneum integrity) or microbiome did not differ between the 2 groups [53]. These early studies showed promise and were followed by a larger randomized controlled study in 2019 by Dissanayake et al. (n = 549) [54]. The study evaluated skin emollients as well as synbiotics (Bifidobacterium bifidum OLB6378 plus fructo-oligosaccharides) and consisted of 4 groups: Synbiotics plus skincare, synbiotics only, skincare only, and a control group. The study evaluated food sensitization and AD at 1 year and found that neither synbiotics nor emollients decreased AD or sensitization to food or aeroallergens. Two additional large randomized controlled studies in 2020, the BEEP [55] (n = 1394) and the PreventADALL [56] (n = 2397) study similarly did not find differences between the control group and the emollient intervention group in decreasing incidence of AD. In addition, the BEEP study found no differences in rate of FA or food sensitization (milk, egg, or peanut), allergic rhinitis, wheeze, or aeroallergens at 2 years. The lack of positive results from the Dissanayake, et al., the BEEP, and the PreventADALL studies were surprising and disappointing in light of the promising results of earlier studies.
In the PreventADALL study, the role of skin emollients as well as food intervention was evaluated to see if they would have a synergistic effect in reducing AD. The study had 4 arms—a skin emollient group, a food intervention group, a skin emollient plus food intervention group, and a control group. The study found no benefits of food intervention or emollient in reducing AD. A major difference between studies are the emollients used, and it is now hypothesized that these differences may be due to the type of emollient used. The emollients used in the above studies have varied widely (Table 1) and have included both nonlipid or lipid emollients, which are likely to vary in effectiveness in preventing skin barrier dysfunction or repairing skin barrier integrity. Emollients vary with respect to pH and ability to hydrate the skin. Studies now suggest that trilipid creams may be the most effective as they are very similar to the skin’s natural lipid composition with a 3:1:1 ratio of ceramides, cholesterol, and free fatty acids and a pH that is similar to that of skin [57]. In a recent study, in infants under 10 weeks of age with dry skin or AD treated with a daily trilipid cream for 12 weeks, increases in immune parameters (total IgG4/total IgE) indicative of a decrease in atopic sensitization were observed [58]. In the same cohort, reduced TEWL was also observed [59]. The emollients used in the BEEP and PreventADALL studies were petrolatum based, which are now thought to be less effective than trilipid emollients in reducing TEWL. The only study that has used a trilipid emollient is the pilot study by Lowe, et al. (n = 77), which showed a trend towards reduced risks of AD and food sensitization in infants at 6 and 12 months [52]. Other factors that differed between these studies and which may account for the discrepancy between study results include risk of atopic sensitization, duration, frequency, and site of emollient application. The study by Dissanayake et al. [54] and PreventADALL [56] included infants from the general population, while earlier pilot studies selected a population at high risk for AD. Duration of intervention and evaluation of incidence of AD varied from 6 months [50], 8 months [51], 12 months [53–56], or 24 months [53, 55]. Frequency of application ranged from 4 times a week [56], daily, [55] to twice daily [52] with whole body application [53] or primarily on the face (cheeks and perioral area) [54]. Taken together, it is highly possible that variations in clinical study designs play a key role (or are a key factor) in the outcome of clinical trials and discrepancy of observed results.
Table 1.
Randomized trials of emollients for prevention of AD
| Study | Year | Study design | Treatment/intervention | Population | Primary endpoints | Results |
|---|---|---|---|---|---|---|
| Simpson et al. [50] | 2014 | RCT (n = 124). Treated (n = 64), untreated controls (n = 60) |
Various emollients: sunflower seed oil or double-base gel or liquid paraffin or Cetaphil cream or Aquaphor healing ointment Application: Full body once a day starting within 3 weeks of birth for 6 months |
Newborns at high risk for AD* | Cumulative incidence of AD at 6 months | AD: Statistically significant decreased risk of AD (relative risk reduction of 50%) P = 0.017 |
| Horimukai, et al. [51] | 2014 | RCT (n = 118);. Intervention group (n = 59), control group (n = 59) | Emulsion-type moisturizer (2e [Douhet] emulsion; Shiseido, Tokyo, Japan). Daily full body application from first week of life for 32 weeks | Newborns at high risk for AD* | Cumulative incidence of AD and eczema at 32 weeks | AD: At week 32, AD decreased by 32% (P = 0.012) in neonates who received emulsion-based moisturizer |
| Yonezawa et al. [60] | 2018 | RCT (n = 227). Intervention group (n = 113), control group (n = 114) | Pigeon Baby Milk Lotion [Pigeon] or Atopita Milky Lotion© [Tampei Pharmaceutical, Tokyo, Japan]. One or more applications per day for 12 weeks | Newborns | Incidence of diaper dermatitis, skin barrier function (TEWL, stratum corneum hydration, skin pH, and sebum secretion), and skin problems (redness, erythema, dryness and breakdown) at 1 and 3 months | Compared with the control, the intervention group had significantly lower face TEWL (14.69 ± 7.38 vs 17.08 ± 8.26 g/m [2] per h, P = 0.033), and higher face and body stratum corneum hydration (60.38 ± 13.66 vs 53.52 ± 14.55,. P = .001) and higher body SCH (58.89 ± 12.96 vs 53.02 ± 10.08 P < 0.001). Compared with the control, newborns in the intervention group had significantly lower rates of diaper dermatitis between birth and 1 month old (6.3%vs 15.9% P = 0.022) and tended to have lower rates of body skin problems between 1 and 3 months (42.1% vs 55.2% P = 0.064) |
| Lowe, et al. (PEBBLES Study) [52] | 2018 | RCT (n = 77). Intervention group (n = 39), control group (n = 38) |
Ceramide-dominant Emollient (EpiCeram®) applied twice daily to whole body for 6 months |
Newborns at high risk of AD (family history of atopic disease) | Incidence of AD, food sensitization at 6 and 12 months | Intention-to-treat analysis showed a non-significant trend towards reduced risks of AD and food sensitization at 6 and 12 months, respectively, in the intervention group. Intention to treat analysis showed non-significant trend towards reduced risks of food sensitization at 6 (12.8 vs 22.9 P = .36) and 12 months (8.8% vs 19.4 P = 0.31). Per protocol analyses (only including infants who received ≥ 5 days/week of study treatment) revealed a significant reduction in food sensitization at 12 months in treatment group |
| McClanahan, et al. [53] | 2019 | RCT (n = 100). Intervention group (n = 54), control group (n = 46) | Cetaphil® Restoraderm® (Galderma, Baie d’Urfé, Montreal, Canada). Daily full body application started with 21 days of birth through 2 years | Newborns at high risk of AD | Cumulative incidence of AD, filaggrin mutation analysis, skin microbiome analysis, TEWL, skin pH, stratum corneum integrity | Across all clinical end points, a numerical trend was observed in favour of the intervention, although not statistically significant. A decreasing trend in AD, although not statistically significant was observed at 1 and 2 years. There were no significant differences between groups in skin barrier or microbiome assessments |
| Dissanayake, et al. [54] | 2019 | RCT (n = 549). Synbiotics plus skincare (group 1; n = 137), synbiotics only (group 2; n = 137), skincare only (group 3; n = 138), no intervention (group 4; n = 137) |
Group 1 received a combination of synbiotics and skincare, group 2 received synbiotics only, group 3 received skincare only, and group 4 received no intervention. Skincare product: Locobase® REPAIR Cream (Daiichi Sankyo, Japan). Synbiotics: combination of 0.5 g (7 × 109 CFU/g)of Bifidobacterium bifidumOLB6378 (Meiji Holdings Co. Ltd., Japan) combined with 0.5 g of fructo-oligosaccharides (Meiji Food Materia Co., Ltd., Japan) twice a day Emollients applied 2–3 times a day on cheeks and the peri-oral area. The parents/guardians were allowed to apply the emollient on other parts of the body at their discretion and were not advised for or against it |
Newborns | AD, Sensitization to food and/or inhalant allergen at 12 months | Neither the emollient nor the synbiotic showed any effect on reducing the development of AD or sensitization to food or aeroallergens at 1 year of age |
| Chalmers, et al. (BEEP study) [55] | 2020 | RTC (n = 1,394). Intervention group (n = 693), control group (n = 701) | Doublebase Gel® (Dermal Laboratories Ltd.) or Diprobase Cream® (Merck Sharp & Dohme Ltd.). Daily application for 12 months | Newborns at high risk of AD | Incidence of AD at 12 and 24 months | There were no differences in AD, food allergy or food sensitization (milk, egg, peanut), at age 2 between the control group and the intervention group. Similarly, there was no difference in other allergens (grass pollen, cat dander, or dust mite) or incidence of wheeze or allergic rhinitis at age 2 |
| Skjerven, et al. (Prevent ADALL Study) [56] | 2020 | RCT (n = 2,397). Controls (n = 596), skin emollient group (n = 575), food intervention group (n = 642) skin and food intervention group (n = 583) |
Ceridal (GlaxoSmithKline Consumer Healthcare) Early complementary feeding consisted of peanut, cow’s milk, wheat, and egg. Application at least 4 times a week |
Newborns | Incidence of AD at 12 months | No statistically significant difference in AD between the control and interventional group. Neither skin emollients nor early complementary feeding reduced development of AD at 12 months |
*Newborns (0–3 months of age) at risk for AD are defined as having a parent or full sibling who has (or had) physician diagnosed AD, asthma, or allergic rhinitis
Summary
Evidence for the role of barrier defects and skin barrier dysfunction in atopic diseases is accumulating. There is much interest in preventing or protecting the skin barrier from developing a proinflammatory atopic state, which may potentially lead to the development of AD and subsequently, FA. Over the past few decades, we have gained a better understanding of the molecular mechanisms underlying FA and some of the common mechanism underlying all atopic diseases. Immunotherapy for peanut allergy is currently the only FDA-approved treatment available for peanut allergy. Avoidance of allergenic foods is the current standard of care for those diagnosed with FA with acute management of allergic reactions with antihistamines or epinephrine. A number of treatments, such as vaccines and biologics are in clinical trials for FA. There is much interest in finding ways to prevent AD and other atopic diseases. Current studies on emollients have shown mixed results and further research is warranted.
Abbreviations
- AD
Atopic dermatitis
- BEEP
Barrier Enhancement for Eczema Prevention
- CDC
Center for Disease Control and Prevention
- CI
Confidence interval
- EAT
Enquiring About Tolerance
- FA
Food allergy
- FLG
Filaggrin gene
- IgE
Immunoglobulin E
- IL
Interleukin
- ILC2
Innate lymphoid cells type 2
- LEAP
Learning early about peanut allergy
- MCH
Major histocompatibility complex
- NO2
Nitrogen dioxide
- PM
Particulate Matter
- PEBBLES
Prevention of Atopic Dermatitis by a Barrier Lipid Equilibrium Strategy
- PreventADALL
Preventing Atopic Dermatitis and Allergies in Children
- SPT
Skin prick test
- SCH
Stratum corneum hydration
- RCT
Randomized controlled trial
- TEWL
Transepidermal water loss
- Th
T helper cells
- TSLP
Thymic stromal lymphopoietin
- UK
United Kingdom
- US
United States
Authors’ contributions
All authors contributed to the writing and editing of the manuscript. All authors read and approved the final manuscript.
Funding
Sean N. Parker Center for Allergy and Asthma Research at Stanford University.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Dr. Nadeau reports grants from National Institute of Allergy and Infectious Diseases (NIAID), National Heart, Lung, and Blood Institute (NHLBI), and National Institute of Environmental Health Sciences (NIEHS); Food Allergy Research & Education (FARE), Director of World Allergy Organization (WAO) Center of Excellence at Stanford; Advisor at Cour Pharma; Co-founder of Before Brands, Alladapt, Latitude, and IgGenix; National Scientific Committee member at Immune Tolerance Network (ITN) and National Institutes of Health (NIH) clinical research centers; DSMB member for NHLBI, US patents for basophil testing, multifood immunotherapy and prevention, monoclonal antibody from plasmoblasts, and device for diagnostics. All other authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Silverberg JI. Public health burden and epidemiology of atopic dermatitis. Dermatol Clin. 2017;35:283–289. doi: 10.1016/j.det.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Drucker AM, Qureshi AA, Amand C, et al. Health care resource utilization and costs among adults with atopic dermatitis in the United States: a claims-based analysis. J Allergy Clin Immunol Pract. 2018;6:1342–1348. doi: 10.1016/j.jaip.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 3.Sciattella P, Pellacani G, Pigatto PD, et al. The burden of atopic dermatitis in adults in Italy. G Ital Dermatol Venereol. 2020;155:19–23. doi: 10.23736/S0392-0488.19.06430-7. [DOI] [PubMed] [Google Scholar]
- 4.Warren CM, Jiang J, Gupta RS. Epidemiology and burden of food allergy. Curr Allergy Asthma Rep. 2020;20:6. doi: 10.1007/s11882-020-0898-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta RS, Warren CM, Smith BM, et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics. 2018;144:S28. doi: 10.1542/peds.2018-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Motosue MS, Bellolio MF, Van Houten HK, Shah ND, Campbell RL. National trends in emergency department visits and hospitalizations for food-induced anaphylaxis in US children. Pediatr Allergy Immunol. 2018;29:538–544. doi: 10.1111/pai.12908. [DOI] [PubMed] [Google Scholar]
- 7.Bergmann MM, Caubet JC, Boguniewicz M, Eigenmann PA. Evaluation of food allergy in patients with atopic dermatitis. J Allergy Clin Immunol Pract. 2013;1:22–28. doi: 10.1016/j.jaip.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Venter C, Sicherer SH, Greenhawt M. Management of peanut allergy. J Allergy Clin Immunol Pract. 2019;7:345–355. doi: 10.1016/j.jaip.2018.10.043. [DOI] [PubMed] [Google Scholar]
- 9.Skolnick HS, Conover-Walker MK, Koerner CB, Sampson HA, Burks W, Wood RA. The natural history of peanut allergy. J Allergy Clin Immunol. 2001;107:367–374. doi: 10.1067/mai.2001.112129. [DOI] [PubMed] [Google Scholar]
- 10.Scott LA, Berni TR, Berni ER, De Vries J, Currie CJ. Evaluation of the healthcare resource use and the related financial costs of managing peanut allergy in the United Kingdom. Expert Rev Clin Immunol. 2019;15:889–896. doi: 10.1080/1744666X.2019.1641406. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167:1026–1031. doi: 10.1001/jamapediatrics.2013.2376. [DOI] [PubMed] [Google Scholar]
- 12.Hill DA, Spergel JM. The atopic march: critical evidence and clinical relevance. Ann Allergy Asthma Immunol. 2018;120:131–137. doi: 10.1016/j.anai.2017.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin PE, Eckert JK, Koplin JJ, et al. Which infants with eczema are at risk of food allergy? Results from a population-based cohort. Clin Exp Allergy. 2015;45:255–264. doi: 10.1111/cea.12406. [DOI] [PubMed] [Google Scholar]
- 14.Lowe AJ, Leung DYM, Tang MLK, Su JC, Allen KJ. The skin as a target for prevention of the atopic march. Ann Allergy Asthma Immunol. 2018;120:145–151. doi: 10.1016/j.anai.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Tsakok T, Woolf R, Smith CH, Weidinger S, Flohr C. Atopic dermatitis: the skin barrier and beyond. Br J Dermatol. 2019;180:464–474. doi: 10.1111/bjd.16934. [DOI] [PubMed] [Google Scholar]
- 16.Hammad H, Lambrecht BN. Barrier epithelial cells and the control of type 2 immunity. Immunity. 2015;43:29–40. doi: 10.1016/j.immuni.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Sicherer SH, Sampson HA. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141:41–58. doi: 10.1016/j.jaci.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Dharmage SC, Lowe AJ, Matheson MC, Burgess JA, Allen KJ, Abramson MJ. Atopic dermatitis and the atopic march revisited. Allergy. 2014;69:17–27. doi: 10.1111/all.12268. [DOI] [PubMed] [Google Scholar]
- 19.Spergel JM, Mizoguchi E, Brewer JP, Martin TR, Bhan AK, Geha RS. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 1998;101:1614–1622. doi: 10.1172/JCI1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benor S, Shani N, Etkin S, Bondar E, Kivity S, Langier S. Epicutaneous exposure to peanut oil induces systemic and pulmonary allergic reaction in mice. Int Arch Allergy Immunol. 2019;179:187–191. doi: 10.1159/000497382. [DOI] [PubMed] [Google Scholar]
- 21.Kelleher MM, Dunn-Galvin A, Gray C, et al. Skin barrier impairment at birth predicts food allergy at 2 years of age. J Allergy Clin Immunol. 2016;137:1111–1116. doi: 10.1016/j.jaci.2015.12.1312. [DOI] [PubMed] [Google Scholar]
- 22.Brough HA, Santos AF, Makinson K, et al. Peanut protein in household dust is related to household peanut consumption and is biologically active. J Allergy Clin Immunol. 2013;132:630–638. doi: 10.1016/j.jaci.2013.02.034. [DOI] [PubMed] [Google Scholar]
- 23.Brough HA, Simpson A, Makinson K, et al. Peanut allergy: effect of environmental peanut exposure in children with filaggrin loss-of-function mutations. J Allergy Clin Immunol. 2014;134:867–875. doi: 10.1016/j.jaci.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brough HA, Liu AH, Sicherer S, et al. Atopic dermatitis increases the effect of exposure to peanut antigen in dust on peanut sensitization and likely peanut allergy. J Allergy Clin Immunol. 2015;135:164–170. doi: 10.1016/j.jaci.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lack G, Fox D, Northstone K, Golding J, Avon Longitudinal Study of P, Children Study T. Factors associated with the development of peanut allergy in childhood. N Engl J Med. 2003;348:977–85. [DOI] [PubMed]
- 26.Loset M, Brown SJ, Saunes M, Hveem K. Genetics of atopic dermatitis: from DNA sequence to clinical relevance. Dermatology. 2019;235:355–364. doi: 10.1159/000500402. [DOI] [PubMed] [Google Scholar]
- 27.Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. 2018;4:1. doi: 10.1038/s41572-018-0001-z. [DOI] [PubMed] [Google Scholar]
- 28.Irvine AD, McLean WH, Leung DY. Filaggrin mutations associated with skin and allergic diseases. N Engl J Med. 2011;365:1315–1327. doi: 10.1056/NEJMra1011040. [DOI] [PubMed] [Google Scholar]
- 29.Flohr C, England K, Radulovic S, et al. Filaggrin loss-of-function mutations are associated with early-onset eczema, eczema severity and transepidermal water loss at 3 months of age. Br J Dermatol. 2010;163:1333–1336. doi: 10.1111/j.1365-2133.2010.10068.x. [DOI] [PubMed] [Google Scholar]
- 30.Mu Z, Zhang J. The role of genetics, the environment, and epigenetics in atopic dermatitis. Adv Exp Med Biol. 2020;1253:107–140. doi: 10.1007/978-981-15-3449-2_4. [DOI] [PubMed] [Google Scholar]
- 31.Mohajeri MH, Brummer RJM, Rastall RA, et al. The role of the microbiome for human health: from basic science to clinical applications. Eur J Nutr. 2018;57:1–14. doi: 10.1007/s00394-018-1703-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patella V, Florio G, Palmieri M, et al. Atopic Dermatitis Severity during Exposure to Air Pollutants and Weather Changes with an artificial neural network (ANN) analysis. Pediatr Allergy Immunol. 2020. [DOI] [PubMed]
- 33.Oh I, Lee J, Ahn K, et al. Association between particulate matter concentration and symptoms of atopic dermatitis in children living in an industrial urban area of South Korea. Environ Res. 2018;160:462–468. doi: 10.1016/j.envres.2017.10.030. [DOI] [PubMed] [Google Scholar]
- 34.Min KD, Yi SJ, Kim HC, et al. Association between exposure to traffic-related air pollution and pediatric allergic diseases based on modeled air pollution concentrations and traffic measures in Seoul, Korea: a comparative analysis. Environ Health. 2020;19:6. doi: 10.1186/s12940-020-0563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmid-Wendtner MH, Korting HC. The pH of the skin surface and its impact on the barrier function. Skin Pharmacol Physiol. 2006;19:296–302. doi: 10.1159/000094670. [DOI] [PubMed] [Google Scholar]
- 36.Cork MJ, Danby SG, Vasilopoulos Y, et al. Epidermal barrier dysfunction in atopic dermatitis. J Invest Dermatol. 2009;129:1892–1908. doi: 10.1038/jid.2009.133. [DOI] [PubMed] [Google Scholar]
- 37.Kim HJ, Lee SH, Hong SJ. Antibiotics-induced dysbiosis of intestinal microbiota aggravates atopic dermatitis in mice by altered short-chain fatty acids. Allergy Asthma Immunol Res. 2020;12:137–148. doi: 10.4168/aair.2020.12.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mitre E, Susi A, Kropp LE, Schwartz DJ, Gorman GH, Nylund CM. Association between use of acid-suppressive medications and antibiotics during infancy and allergic diseases in early childhood. JAMA Pediatr. 2018;172:e180315. doi: 10.1001/jamapediatrics.2018.0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee SH, Gong YN, Ryoo E. Clostridium difficile colonization and/or infection during infancy and the risk of childhood allergic diseases. Korean J Pediatr. 2017;60:145–150. doi: 10.3345/kjp.2017.60.5.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahn K, Kim BE, Kim J, Leung DY. Recent advances in atopic dermatitis. Curr Opin Immunol. 2020;66:14–21. doi: 10.1016/j.coi.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vander Leek TK, Liu AH, Stefanski K, Blacker B, Bock SA. The natural history of peanut allergy in young children and its association with serum peanut-specific IgE. J Pediatr. 2000;137:749–755. doi: 10.1067/mpd.2000.109376. [DOI] [PubMed] [Google Scholar]
- 42.Zeiger RS. Food allergen avoidance in the prevention of food allergy in infants and children. Pediatrics. 2003;111:1662–1671. [PubMed] [Google Scholar]
- 43.Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803–813. doi: 10.1056/NEJMoa1414850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perkin MR, Logan K, Tseng A, et al. Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med. 2016;374:1733–1743. doi: 10.1056/NEJMoa1514210. [DOI] [PubMed] [Google Scholar]
- 45.NIAID-Sponsored Expert Panel, Boyce JA, Assa’ad A, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126:S1–58. [DOI] [PMC free article] [PubMed]
- 46.Perkin MR, Logan K, Bahnson HT, et al. Efficacy of the Enquiring About Tolerance (EAT) study among infants at high risk of developing food allergy. J Allergy Clin Immunol. 2019;144:1606–1614. doi: 10.1016/j.jaci.2019.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Voorheis P, Bell S, Cornelsen L, et al. Challenges experienced with early introduction and sustained consumption of allergenic foods in the Enquiring About Tolerance (EAT) study: a qualitative analysis. J Allergy Clin Immunol. 2019;144:1615–1623. doi: 10.1016/j.jaci.2019.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fisher HR, Du Toit G, Bahnson HT, Lack G. The challenges of preventing food allergy: lessons learned from LEAP and EAT. Ann Allergy Asthma Immunol. 2018;121:313–319. doi: 10.1016/j.anai.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 49.Kelleher M, Dunn-Galvin A, Hourihane JO, et al. Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predates and predicts atopic dermatitis at 1 year. J Allergy Clin Immunol. 2015;135:930–935. doi: 10.1016/j.jaci.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 50.Simpson EL, Chalmers JR, Hanifin JM, et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014;134:818–823. doi: 10.1016/j.jaci.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Horimukai K, Morita K, Narita M, et al. Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol. 2014;134:824–830. doi: 10.1016/j.jaci.2014.07.060. [DOI] [PubMed] [Google Scholar]
- 52.Lowe AJ, Su JC, Allen KJ, et al. A randomized trial of a barrier lipid replacement strategy for the prevention of atopic dermatitis and allergic sensitization: the PEBBLES pilot study. Br J Dermatol. 2018;178:e19–e21. doi: 10.1111/bjd.15747. [DOI] [PubMed] [Google Scholar]
- 53.McClanahan D, Wong A, Kezic S, et al. A randomized controlled trial of an emollient with ceramide and filaggrin-associated amino acids for the primary prevention of atopic dermatitis in high-risk infants. J Eur Acad Dermatol Venereol. 2019;33:2087–2094. doi: 10.1111/jdv.15786. [DOI] [PubMed] [Google Scholar]
- 54.Dissanayake E, Tani Y, Nagai K, et al. Skin Care and Synbiotics for Prevention of Atopic Dermatitis or Food Allergy in Newborn Infants: A 2 x 2 Factorial, Randomized, Non-Treatment Controlled Trial. Int Arch Allergy Immunol. 2019;180:202–211. doi: 10.1159/000501636. [DOI] [PubMed] [Google Scholar]
- 55.Chalmers JR, Haines RH, Bradshaw LE, et al. Daily emollient during infancy for prevention of eczema: the BEEP randomised controlled trial. Lancet. 2020;395:962–972. doi: 10.1016/S0140-6736(19)32984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Skjerven HO, Rehbinder EM, Vettukattil R, et al. Skin emollient and early complementary feeding to prevent infant atopic dermatitis (PreventADALL): a factorial, multicentre, cluster-randomised trial. Lancet. 2020;395:951–961. doi: 10.1016/S0140-6736(19)32983-6. [DOI] [PubMed] [Google Scholar]
- 57.Man MM, Feingold KR, Thornfeldt CR, Elias PM. Optimization of physiological lipid mixtures for barrier repair. J Invest Dermatol. 1996;106:1096–1101. doi: 10.1111/1523-1747.ep12340135. [DOI] [PubMed] [Google Scholar]
- 58.Man G, Cheung C, Crumrine D, et al. An optimized inexpensive emollient mixture improves barrier repair in murine skin. Dermatol Sin. 2015;33:96–102. doi: 10.1016/j.dsi.2015.03.010. [DOI] [Google Scholar]
- 59.Mao-Qiang M, Brown BE, Wu-Pong S, Feingold KR, Elias PM. Exogenous nonphysiologic vs physiologic lipids. Divergent mechanisms for correction of permeability barrier dysfunction. Arch Dermatol. 1995;131:809–16. [DOI] [PubMed]
- 60.Yonezawa K, Haruna M, Matsuzaki M, Shiraishi M, Kojima R. Effects of moisturizing skincare on skin barrier function and the prevention of skin problems in 3-month-old infants: a randomized controlled trial. J Dermatol. 2018;45:24–30. doi: 10.1111/1346-8138.14080. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.