Abstract
Background
Asians and Hispanics currently have the highest incidence rates of hepatocellular carcinoma (HCC) in the United States. The numbers of these minority populations are rapidly increasing, reshaping the demographic in the United States and particularly California, where approximately one-third of US Asians and Hispanics reside. With the changing demographic and rising incidence of HCC that has tripled during the past three decades, it is important to forecast the future burden of HCC by age, sex, and race/ethnicity to plan prevention and control strategies for HCC.
Methods
We used four Surveillance, Epidemiology, and End Results Program registries to obtain incidence data for California during 2000 to 2013, and 14 registries to represent non-California states. We applied age-period-cohort models to estimate future HCC incidence rates, and estimated HCC burden by multiplying incidence forecasts by corresponding US Census population projections.
Results
Our forecasts for California suggest that in 2030 Hispanics and blacks will have the highest HCC incidence rates and Asians the lowest. While incidence among whites, blacks, and Hispanics in California increased successively for each birth year cohort from 1915 through 1955, incidence among Asians in California decreased for each successive birth year cohort from 1915 through 1975. In contrast, consistent declines were not seen among Asians in the rest of the United States. In California, the estimated burden of HCC is 6482 new cases in 2030, where 80.0% of these patients are older than 65 years (vs 44.5% in 2014). The relative increase of burden in 2030 vs 2014 for this 65 years and older age group is especially high among Hispanics (318.3%), whereas it is the lowest among Asians (53.2%) in California.
Conclusions
Prevention efforts in California should target persons currently ages 50 to 64 years who will make up the older age group (>65 years) in 2030, especially among Hispanics with the most rapid increase of HCC burden through 2030.
Liver cancer is the second leading cause of cancer deaths worldwide (1). The incidence of hepatocellular carcinoma (HCC), the predominant form (>80%) of liver cancer, has tripled in the United States during the past three decades (2–4). As of 2013, the incidence of HCC is 22.2 per 100 000 person-years in males and 5.7 per 100 000 person-years in females among individuals aged 35 to 84 years (5). The major risk factors for HCC include chronic infections with hepatitis B virus (HBV) and hepatitis C virus (HCV) (3,6–9). The incidence rate of HCC varies by sex, with males experiencing two to four times higher incidence than females (7), and it also varies by age, with the peak incidence observed in individuals ages 75 years and older (10). Other important risk factors for HCC include excessive alcohol consumption, aflatoxin, obesity, diabetes, and nonalcoholic fatty liver disease (7). HCC incidence also varies substantially by geography; the rate is high in Southeast Asia and sub-Saharan Africa and low in South and Central America and Europe (11,12).
In the United States, Asian and Hispanic populations have the highest incidence of HCC, with rates two- to threefold higher compared with whites (13,14). Approximately one-third of Asians and over one-fourth of Hispanics in the United States live in California, which has the nation’s largest population (with close to 40 million individuals and 12% of the US population) (14,15). Recent study showed that California is among the top 10 states with the highest overall mortality for both liver cancer and chronic liver disease (16). The numbers of these two minority groups are rapidly increasing, shaping a different demography in the United States (14,15). With the changing demographic and trends of HCC incidence, there is a need to plan better prevention strategies for HCC.
Although the rising trend of HCC in the United States has been well established (5,16–18), few studies have examined the dynamically changing trends of California or projected the expected numbers of new HCC cases in the United States or California. A recent study by Petrick et al. (5) projected liver cancer incidence rates by race/ethnicity for the entire United States using age-period-cohort (APC) forecasting models and data from the Surveillance, Epidemiology, and End Results Program (SEER) for the years 2000 to 2012. Although their forecasting of incidence rates was performed by race/ethnicity, birth cohort effects were not examined by race/ethnicity, and the study focused on the entire US data. In addition, the future burden of HCC was not investigated.
Public health planning requires estimates of the expected absolute numbers of new cases, the so-called burden of disease. Importantly, cancer burden depends on both incidence forecasts as well as population projections. In this study, therefore, we estimated HCC incidence and burden through 2030 by race/ethnicity and sex in California vs the rest of the United States to identify spatial and demographic heterogeneity and to quantify the future burden of HCC both nationally and in California using US Census population projections data.
Methods
Incidence Data
HCC incidence data during 2000 to 2013 in California were obtained from four SEER registries (Greater Bay Area Cancer Registry that includes San Francisco-Oakland and San Jose-Monterey, Los Angeles Cancer Registry, and Greater California Cancer Registry); the HCC cases in these three registries in California constitute 49.9% of the cases in SEER. HCC incidence in US states other than California were estimated from 14 other SEER registries (https://seer.cancer.gov/). We used single-year HCC incident case and population data for ages 35 to 84 years. We defined primary liver cancer using International Classification of Diseases for Oncology, 3rd Edition, using topography C22.0 code and histology codes 8170 to 8175, and excluded C22.1 (intrahepatic bile duct tumors). A total of 31 702 HCC cases were identified in the four California SEER registries and 31 784 cases in the 14 other non-California SEER registries (total N = 63 486).
Population Data
To project HCC burden from 2014 to 2030 taking into account the changing demographic profile of the United States, we multiplied HCC incidence rates from the APC forecasting models (see next subsection) by corresponding official population projections produced by the US Census Bureau (December 2014 release). These projections are based on estimates and assumptions about future demographic trends including future births, deaths, net international migration, and domestic migration. The estimates of the US population are stratified by sex, age, and race/ethnicity (non-Hispanic white, black, Asian/Pacific Islander, and Hispanic).
Statistical Analysis
APC Forecasting Model
We used an APC forecasting model to estimate the effects of age, period, and cohort on current and future HCC incidence rates (19). Period effects represent variations in vital rates over time that affect all age groups simultaneously; age effects summarize age-associated natural history; and birth cohort effects describe changes in incidence by calendar year of birth. More detailed information about our APC model is included in the Supplementary Materials (available online) with examples. The 95% confidence intervals of these estimates were calculated based on the standard delta method for a generalized linear regression model. In summaries of model results, we computed age-standardized incidence rates per 100 000 person-years using the 2000 US Standard Population.
Forecasting
We forecasted HCC incidence for 2014 to 2030 based on the observed age incidence curve and observed and extrapolated cohort and period effects as described in the Supplementary Materials (available online). Our base model, presented in the text, is the same as the age-cohort forecasting model used in the previous study by Petrick et al. (5). We estimated the absolute number of new HCC cases, that is, the burden, by multiplying the estimated age-specific incidence rates by corresponding population (person-year) projections. The underlying assumption of our APC forecasting model is that the effects of age, period, and cohort observed in the past data (2000–2013) will continue to hold in the future periods (2014–2030). We conducted sensitivity analysis under varying scenarios that are described in the Supplementary Methods (available online) and Supplementary Figures 2 and 3 (available online). Forecasts were constructed using custom MATLAB version 9.4 (R2018a) software.
Results
HCC Incidence Rate in 2000–2013 and Projection for 2014–2030
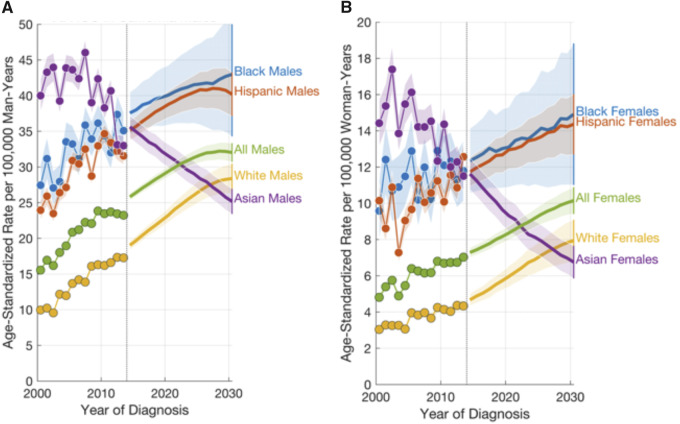
HCC incidence projections for California are shown in Figure 1, Aand B. Although Asians had the highest incidence in 2000 (40.0 per 100 000 for males and 14.3 for females), their rate started to decline by 2010 and is forecast to be the lowest in 2030 (25.1 per 100 000 for males and 6.9 for females). In contrast, blacks and Hispanics are expected to have the highest rates in 2030 (42.8 and 40.3 per 100 000 males and 14.9 and 14.4 per 100 000 females, respectively). Notably, there is a cross-over between the incidence rates of Asians and Hispanics around 2013 to 2014. Forecasts for the rest of the United States are qualitatively similar (Supplementary Figures 2 and 3, available online). The estimated annual percent change (EAPC) of HCC incidence during 2014 to 2030 in California is expected to be 1.6% (95% confidence interval [CI] = 1.4% to 1.7%) for the overall population, with the highest EAPC observed in the age group of 65 years and older (EAPC = 4.4%, 95% CI = 4.0% to 4.8%) and the lowest in the age group of 35 to 49 years (EAPC = −6.1%, 95% CI = −6.9 to −5.3) (see Table 1). Sensitivity analysis under varying scenarios is shown in Supplementary Figures 2 and 3 (available online), which suggest that the declines in forecast for Asian men and women are commonly observed across different models. The incidence of Hispanic females may increase at a faster rate in alternative models, whereas the rates of white males and females may plateau rather than increase.
Figure 1.
Age-standardized hepatocellular carcinoma incidence rates in California (CA) by period (2000–2013 for the observed period and 2014–2030 for the future period). A) Males. B) Females. The 95% confidence intervals are shown in the shaded areas.
Table 1.
Hepatocellular carcinoma burden forecasted by race/ethnicity and age in California*
| Race/ethnicity | Age, y | 2014 |
2020 |
2030 |
Change in burden 2030 vs 2014, % | EAPC in rate (95% CI) |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rates | Burden | Rates | Burden | Rates | Burden | 2000–2013 | 2014–2030 | |||
| All races | All | 15.9 | 3456 | 18.2 | 4695 | 20.2 | 6482 | 87.6 | 3.4 (2.7 to 4.0) | 1.6 (1.4 to 1.7) |
| 35–49 | 2.1 | 170 | 1.6 | 135 | 0.9 | 82 | −51.6 | −3.2 (−4.5 to −1.9) | −6.1 (−6.9 to −5.3) | |
| 50–64 | 23.1 | 1748 | 20.9 | 1763 | 14.1 | 1215 | −30.5 | 5.4 (4.4 to 6.5) | −3.0 (−3.3 to −2.8) | |
| 65+ | 35.6 | 1539 | 49.6 | 2797 | 69.0 | 5185 | 237.0 | 3.0 (2.5 to 3.5) | 4.4 (4.0 to 4.8) | |
| White | All | 11.4 | 1373 | 14.2 | 1919 | 17.5 | 2702 | 96.8 | 4.8 (4.0 to 5.6) | 2.8 (2.5 to 3.0) |
| 35–49 | 1.4 | 66 | 0.9 | 47 | 0.4 | 28 | −58.3 | −4.3 (−5.8 to −2.8) | −9.8 (−11.6 to −7.9) | |
| 50–64 | 18.1 | 903 | 16.4 | 826 | 11.7 | 449 | −50.2 | 7.9 (6.3 to 9.5) | −2.6 (−2.8 to −2.4) | |
| 65+ | 23.8 | 906 | 39.2 | 1555 | 61.5 | 2592 | 186.2 | 3.8 (3.1 to 4.5) | 6.2 (5.6 to 6.8) | |
| Black | All | 22.3 | 292 | 24.5 | 363 | 25.5 | 415 | 41.9 | 2.9 (1.8 to 4.1) | 0.7 (0.6 to 0.9) |
| 35–49 | 3.5 | 16 | 4.0 | 18 | 5.1 | 26 | 60.4 | −7.1 (−9.5 to −4.5) | 2.2 (1.5 to 2.9) | |
| 50–64 | 35.0 | 165 | 24.0 | 128 | 24.5 | 107 | −35.2 | 6.6 (4.7 to 8.5) | −2.9 (−4.1 to −1.9) | |
| 65+ | 45.1 | 111 | 68.4 | 218 | 70.2 | 282 | 153.5 | 0.9 (−0.7 to 2.6) | 2.9 (1.9 to 3.8) | |
| Asian | All | 21.5 | 633 | 18.7 | 687 | 14.8 | 723 | 14.1 | −1.4 (−2.4 to −0.5) | −2.3 (−2.3 to −2.3) |
| 35–49 | 4.4 | 52 | 3.4 | 44 | 3.3 | 43 | −18.3 | −3.9 (−5.8 to −2.2) | −2.0 (−2.8 to −1.2) | |
| 50–64 | 23.2 | 248 | 19.5 | 234 | 12.3 | 170 | −31.4 | −1.7 (−3.0 to −0.3) | −3.9 (−4.2 to −3.7) | |
| 65+ | 55.6 | 333 | 50.0 | 409 | 42.4 | 510 | 53.2 | −0.9 (−2.0 to 0.3) | −1.6 (−1.6 to −1.5) | |
| Hispanic | All | 22.2 | 1091 | 24.9 | 1587 | 26.6 | 2445 | 124.0 | 3.2 (2.4 to 3.9) | 1.2 (1.0 to 1.4) |
| 35–49 | 2.4 | 73 | 1.7 | 58 | 0.8 | 29 | −60.4 | −3.5 (−5.6 to −1.4) | −7.9 (−8.9 to −6.8) | |
| 50–64 | 29.0 | 560 | 27.1 | 683 | 14.9 | 502 | −10.6 | 5.1 (3.9 to 6.2) | −4.1 (−4.7 to −3.5) | |
| 65+ | 55.1 | 458 | 71.3 | 847 | 97.1 | 1914 | 318.3 | 2.9 (1.9 to 3.9) | 3.9 (3.6 to 4.1) | |
Burden is the number of cases per year within the age group. Rates are rates per 100 000 person-years. EAPC = estimated annual percent change; CI = confidence interval.
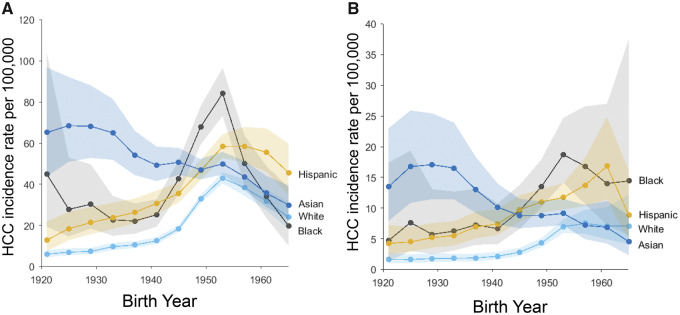
HCC Incidence by Birth Cohort
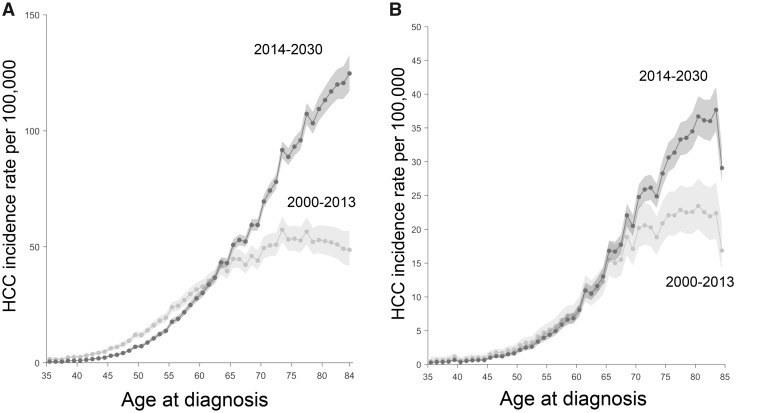
Estimated HCC incidence by birth cohort is shown in Figure 2, A and B for California (see Supplementary Figure 5, A and B, available online for non-California). While the HCC incidence rates of whites, blacks, and Hispanics in California increased from birth year 1920 through 1955, incidence for Asians in California decreased steadily for cohorts 1920 through 1965. Notably, this decreasing birth cohort trend among Asians in California is not seen among Asians in the rest of the United States (Supplementary Figure 5, available online). Comparisons of the cross-sectional age curves for California in the present (2000–2013) vs future (2014–2030) periods show that HCC incidence at ages 65 years and older is expected to be much higher in the future (Figure 3A). For example, HCC incidence rate at age 75 years increased by 70.4% from 52.5 per persons in 2000 to 2013 to 89.5 per persons in 2014 to 2030 among males. This pattern reflects the increases in incidence specifically among Hispanic and white males (Supplementary Figure 6, available online), whereas this pattern is not as clear among females (Supplementary Figure 7, available online). Corresponding cross-sectional age incidence curves in the rest of the United States are very similar for men and women in all races combined (Supplementary Figure 5, C and D, available online).
Figure 2.
Hepatocellular carcinoma (HCC) incidence rates in California (CA) by birth cohort and race/ethnicity. A) Males. B) Females. The 95% confidence intervals are shown in the shaded areas.
Figure 3.
Hepatocellular carcinoma (HCC) incidence rates by age at diagnosis (ie, cross-sectional age curve) in California (CA) for the past (2000–2013) vs the future (2014–2030). A) Males. B) Females. The 95% confidence intervals are shown in the shaded areas.
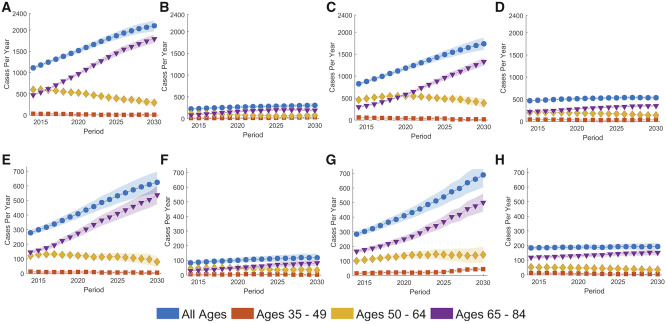
HCC Burden Projections
Burden forecasts reflect both changes in incidence as well as changes in population size. Our analysis shows that the population growth rate in California among Asians is expected to be considerably higher than among Asians in the rest of the United States for all ages 65 years and younger (Supplementary Figure 8, available online). Similarly, the Hispanic population younger than age 60 years is expected to increase more quickly in California than the rest of the United States.
In combination with APC forecasts of HCC, we project that the estimated HCC burden in California will rise by 87.6% to 6482 new cases in 2030 (Table 1), where 80.0% of these new cases are older than 65 years (vs 44.5% in 2014). In contrast, HCC cases ages 50 to 64 years are expected to constitute 18.7% of the total in 2030, down from 50.6% in 2014. It is notable that the percent increase of burden in 2030 vs 2014 for this 65 years and older age group is especially high among Hispanics (318.3%), whereas it is the lowest among Asians (53.2%) in California (Table 1; Figure 4).
Figure 4.
Forecasts of burden (absolute number of new hepatocellular carcinoma cases) by race/ethnicity and age in California (CA). A) White males. B) Black males. C) Hispanic males. D) Asian males. E) White females. F) Black females. G) Hispanic females. H) Asian females.
To examine whether HCC affects California disproportionately compared with the rest of the United States, we examined the proportion of HCC cases in California vs the proportion of individuals who live in California by race/ethnicity (Supplementary Figure 9, available online). As of 2014, 32.3% of the nation’s Asians live in California, whereas a larger proportion, 36.6%, of the total Asian HCC cases in the United States are registered in California. Similarly, for Hispanics, a disproportionately higher number of the nation’s Hispanic HCC cases (28.6%) are registered in California compared with the proportion of the nation’s Hispanics who live in California (27.4%). The results of projecting these trends to 2030 are shown in Supplementary Figure 9 (right) (available online), which show similar patterns to 2014, although the gaps between the two quantities (ie, HCC cases population vs the general population) become narrower in both ethnic groups.
Discussion
Historically Asians have had the highest rates of HCC in the United States. Our forecast shows that Asians are expected to have the lowest HCC incidence rates in California in 2030, whereas Hispanics and blacks are expected to have the highest rates, surpassing the incidence rates of Asians around 2013 to 2014. The estimated burden of HCC in California is around 6482 new cases in 2030, with 80% of the new cases older than 65 years. The relative increase of burden in 2030 vs 2014 in the older group is especially high among Hispanics, whereas it is lowest among Asians. It is notable that our analysis shows that California has distinct incidence patterns in both birth cohort effects and period effects compared with non-California. This distinction is especially clear among Asians, showing steeply decreasing incidence rates by birth year from 1915 through 1975, as well as by calendar year from 2000 to 2013. On the other hand, such patterns are not observed among Asians in US SEER states other than California. Reasons for this decrease in California are unclear but may be related to the increased awareness of HBV risk, enhanced outreach, and aggressive HBV screening and treatment campaigns in Asians populations in California (20). Despite the decreasing trend of HCC in Asians, HBV screening in high-risk Asian populations (ie, foreign-born Asians from HBV-endemic countries) across this country should continue. Linking those who are chronic carriers to proper treatment and HCC surveillance is key to sustaining the downward trend over time and achieving the goal of minimizing HCC burden in the high-risk Asian population.
To our knowledge, this study provides the first in-depth analysis of the HCC incidence projection and burdens in California by sex, race, and ethnicity. By separating the California data from the rest of the United States, we were able to identify several distinct characteristics in HCC incidence trends in California vs non-California. Although several prior studies used the entire 18 SEER registries data to characterize US incidence patterns of HCC (5,16–18), we found that the disproportionately higher proportion of SEER in California (with HCC cases in California accounting for 50% of the HCC cases in SEER) vs the general US population makes it challenging to conclude whether the observed incidence patterns using SEER are generalizable to the United States overall or specific to California. For example, Petrick et al. (5) reported the decreasing US trend of incidence of HCC among Asians during 2000 to 2012 using SEER 18. However, our analysis showed that this decreasing pattern among Asians was attributed to the results in California, where non-California did not show such trends.
Our analysis also showed increasing HCC incidence rates by birth cohort through 1955 among whites, Hispanics, and blacks in California, which is consistent with prior findings reported by Petrick et al. (5). Petrick et al. suggest, and we agree, that this birth cohort effect is mainly attributed to HCV infection in baby boomers born between 1945 and 1965 who acquired HCV infection through intravenous drug use and blood transfusions between the 1960s and 1980s. A key concept is that an APC birth cohort effect is a net effect of all known and unknown risk factors combined; the birth cohort effect for HCC presumably includes a contribution from each major risk factor that varies by cohort, including HCV. But it is reasonable to suppose that because HCV is such a strong risk factor, in cohorts such as white male baby boomers who experienced very high cumulative HCV infection rates, much of the overall cohort effect is likely driven by HCV. Indeed, baby boomers constitute about 66% of HCV-infected patients in the United States (6), with a peak prevalence of 4.3% in persons ages 40 to 49 years from 1999 to 2002 (21). The birth cohort effect was especially prominent among Hispanics and blacks in our analysis, which led to the highest HCC incidence projected in 2030 among these two populations. This is related to the fact that current Hispanic and black baby boomers who have high prevalence of HCV will enter an age group that is more likely to develop HCC in 2030. In addition to the birth cohort effect due to HCV infection, the increasing trends of HCC incidence among blacks and Hispanics can also be explained by the increasing prevalence of obesity and diabetes for which Hispanics and blacks have higher prevalence compared with whites or Asians (14,22). As expected, we did not see increasing birth cohort effects in Asians, among whom the incidence rate of HCC decreases successively by birth year from 1915 through 1975. This may be related to the fact that many of the Asians in these birth cohorts are less exposed to (or less affected by) HCV compared with whites; among Asians the main risk factor for HCC is HBV rather than HCV.
Despite several strengths, our study has limitations. First, SEER data do not include the complete information on viral hepatitis, nativity, socioeconomic status, or neighborhood enclaves. For example, the SEER data on nativity have become increasingly incomplete; thus, prior methods used to impute nativity for patients with unknown birthplace are less valid for recent cases (23). Among several studies that incorporated nativity information, Chang et al. (14) showed that although foreign-born Hispanic males had statistically significantly lower liver cancer incidence rates than US-born Hispanic males, foreign-born Asian males and females had up to fivefold higher rates than the US-born, which is consistent with the results of a recent study conducted by Pham et al. (24). Similarly, recent studies by Setiawan et al. (25) and Pinheiro et al. (26) also showed that incidence and mortality rates of liver cancer were radically different between US-born Hispanics and foreign-born Hispanics in California/Texas. This shows that the consideration of subgroups within broader ethnic groups, including birthplace, is important in investigating the trends in HCC incidence.
Second, the underlying assumption of our APC forecasting model is that the effects of age, period, and cohort observed in the past data (2000–2013) can be extrapolated to the future period (2014–2030). Although we believe our base model captures the observed patterns well and our sensitivity analyses cover a broad range of future scenarios, this is still a strong assumption and hence a limitation of our study. Also, some of the projected trends in our study appear linear (eg, Asians and whites in Figure 1), which may be increasingly less likely if strong period effects occur in the future. We obtained data for 2014 through 2015 from SEER and assessed the empirical forecast errors (see Supplementary Table 1, available online); in all groups, the predicted values of these years were in good agreement with the actual observed values. Third, our forecasting results for burden are also based on the population projections provided by the US Census. However, these population projections are dependent on the migration patterns of Asians and Hispanics that are subject to change (27), which can affect the accuracy of the forecasts for both incidence rates and burden estimates. Fourth, we focused on HCC incidence in our analysis, but mortality was not examined. Historically, HCC mortality rates tend to mirror HCC incidence rates, showing relatively stable incidence to mortality ratios (11,12).
In summary, our analysis shows that future prevention and control efforts for HCC in California in the next 15 years should target persons currently ages 50 to 64 years who will comprise the older age group (>65 years) circa 2030; this group will account for 80% of the new cases in 2030. Especially, the focus should be on an older (>65 years) Hispanic subgroup (ie, currently 50 to 64 years) with the steepest expected increase in HCC burden (318%) in 2030 vs 2014. Among Hispanics, the prevention effort should target HCV screening, education, treatment, and access to care. Additional effort on obesity and metabolic syndrome control and reduction is also needed because Hispanic women have a high prevalence of abdominal obesity, which can lead to metabolic syndrome and nonalcoholic fatty liver diseases, emerging and important risk factors for non-viral HCC. In addition, HBV screening and antiviral treatment among Asians needs to continue to ensure sustained reduction of HCC incidence in this high-risk group. Such intensified public health prevention efforts will help contribute to reducing the heavy burden of HCC and reversing the rising trends in HCC incidence in California and more broadly in the United States.
Funding
This work is supported by the Stanford Cancer Institute (grant no. 1164310–125-GHTD). Dr Hsing is a recipient of funding from the Stanford Cancer Institute.
Notes
Affiliations of authors: Stanford Cancer Institute (SSH, YL, BY, MN, SS, AWH), Department of Medicine (SSH, MN, AWH), and Department of Neurosurgery (SSH), Stanford University School of Medicine, Stanford, CA; Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, MD (SPK, PSR); Cancer Prevention Institute of California, Fremont, CA (YL); Department of Surgery (SS) and Stanford Prevention Research Center (AWH), Stanford University School of Medicine, Stanford, CA.
The authors have no conflicts of interest to disclose. The funder had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Supplementary Material
References
- 1.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. http://globocan.iarc.fr. Accessed June 2, 2014.
- 2. Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin. 2014;641:9–29. [DOI] [PubMed] [Google Scholar]
- 3. El-Serag HB, Davila JA, Petersen NJ, et al. The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med. 2003;13910:817–823. [DOI] [PubMed] [Google Scholar]
- 4. El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999;34010:745–750. [DOI] [PubMed] [Google Scholar]
- 5. Petrick JL, Kelly SP, Altekruse SF, et al. Future of hepatocellular carcinoma incidence in the United States forecast through 2030. J Clin Oncol. 2016;3415:1787–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davis GL, Roberts WL. The healthcare burden imposed by liver disease in aging Baby Boomers. Curr Gastroenterol Rep. 2010;121:1–6. [DOI] [PubMed] [Google Scholar]
- 7. Mittal S, El-Serag HB. Epidemiology of HCC: consider the population. J Clin Gastroenterol. 2013;47 Suppl0:S2–S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;612:69–90. [DOI] [PubMed] [Google Scholar]
- 9. El-Serag HB, Mason AC. Risk factors for the rising rates of primary liver cancer in the United States. Arch Intern Med. 2000;16021:3227–3230. [DOI] [PubMed] [Google Scholar]
- 10. Montalto G, Cervello M, Giannitrapani L, et al. Epidemiology, risk factors, and natural history of hepatocellular carcinoma. Ann N Y Acad Sci. 2002;9631:13–20. [DOI] [PubMed] [Google Scholar]
- 11. Nordenstedt H, White DL, El-Serag HB. The changing pattern of epidemiology in hepatocellular carcinoma. Dig Liver Dis. 2010;42Suppl 3:S206–S214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dhanasekaran R, Limaye A, Cabrera R. Hepatocellular carcinoma: current trends in worldwide epidemiology, risk factors, diagnosis, and therapeutics. Hepat Med. 2012;4:19–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Altekruse S, Kosary C, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2007, National Cancer Institute. Bethesda, MD. Based on November 2009 SEER data submission, posted to the SEER web site, 2010. https://seer.cancer.gov/.
- 14. Chang ET, Yang J, Alfaro-Velcamp T, et al. Disparities in liver cancer incidence by nativity, acculturation, and socioeconomic status in California Hispanics and Asians. Cancer Epidemiol Prev Biomarkers. 2010; 1912:3106–3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gomez SL, Glaser SL. Quality of birthplace information obtained from death certificates for Hispanics, Asians, and Pacific Islanders. Ethn Dis. 2004;142:292–295. [PubMed] [Google Scholar]
- 16. Altekruse SF, Henley SJ, Cucinelli JE, et al. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol. 2014;1094:542–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;7411:2913–2921. [DOI] [PubMed] [Google Scholar]
- 18. Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;279:1485–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosenberg PS, Check DP, Anderson WF. A web tool for age–period–cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Prev Biomarkers. 2014;2311:2296–2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross‐sectional study of Asians in California. Hepatology. 2007;464:1034–1040. [DOI] [PubMed] [Google Scholar]
- 21. Moyer VA. Screening for hepatitis C virus infection in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;1595:349–357. [DOI] [PubMed] [Google Scholar]
- 22. Flores YN, Yee HF Jr, Leng M, et al. Risk factors for chronic liver disease in Blacks, Mexican Americans, and Whites in the United States: results from NHANES IV, 1999–2004. Am J Gastroenterol. 2008;1039:2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pinheiro PS, Bungum TJ, Jin H. Limitations in the imputation strategy to handle missing nativity data in the Surveillance, Epidemiology, and End Results program. Cancer. 2014;12020:3261–3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pham C, Fong T-L, Zhang J, Liu L. Striking racial/ethnic disparities in liver cancer incidence rates and temporal trends in California, 1988–2012. J Natl Cancer Inst. 2018;11011:1259–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Setiawan VW, Wei PC, Hernandez BY, et al. Disparity in liver cancer incidence and chronic liver disease mortality by nativity in Hispanics: the Multiethnic Cohort. Cancer. 2016;1229:1444–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pinheiro PS, Callahan KE, Gomez SL, et al. High cancer mortality for US-born Latinos: evidence from California and Texas. BMC Cancer. 2017;171:478.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colby SL, Ortman JM. 2015. Projections of the size and composition of the US population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25-1143. US Census Bureau.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.