Abstract
The coronavirus disease 2019 (COVID-19) pandemic has imposed both physical and psychological burdens on healthcare workers (HCWs). What is more, few studies have focused on the gender differences in mental health problems (MHPs) among HCWs during such an outbreak. Thus, the current study investigated the prevalence and gender differences of various MHPs among HCWs in China during the COVID-19 outbreak. This nationwide survey was conducted online from January 29 to February 3, 2020. General information was collected by questions about socio-demographics, work-related factors, and living situations. Depressive, anxiety, stress, and insomnia symptoms were assessed by the Patient Health Questionnaire-9, the Generalized Anxiety Disorder-7, the Impact of Event Scale-Revised, and the Insomnia Severity Index, respectively. Among the 2198 contacted HCWs, 1563 (71.1%) responded with valid data, of whom 1293 (82.7%) were females. The prevalences of depressive, anxiety, stress, and insomnia symptoms in participants were 50.7%, 44.7%, 52.5%, and 36.1%, respectively. Female HCWs had significantly higher scores in all four scales (p < 0.001) and higher prevalences in all MHPs involved (range, odds ratio [OR] 1.55–1.97). After adjusting for potential confounders, female HCWs still had higher risks for all MHPs involved than males (range, adjusted OR 1.36–1.96). HCWs present high prevalences of depressive, anxiety, stress, and insomnia symptoms during the COVID-19 outbreak. Furthermore, female HCWs are more vulnerable to all MHPs involved. These findings highlight the need for timely, special care and support for HCWs during the outbreak, especially for females.
Keywords: Gender difference, Mental health problem, Healthcare worker, Coronavirus disease 2019
1. Introduction
In late January 2020, the coronavirus disease 2019 (COVID-19), which was initially reported in Wuhan, Hubei, spread rapidly throughout China and the world. The World Health Organization declared the COVID-19 outbreak as a pandemic on March 11, 2020 (World Health Organization, 2020). As of June 26, 2020, there were a total of 9,711,885 confirmed cases and 491,744 deaths around the world due to the COVID-19 pandemic (Johns Hopkins University, 2020). The huge and rapidly growing number of cases and deaths have raised great concern in the public throughout the world, especially among healthcare workers (HCWs) (Kang et al., 2020; Xiang et al., 2020).
In 2003, the severe acute respiratory syndrome (SARS) epidemic not only brought physical suffering in HCWs in affected countries or regions due to its high pathogenicity and high rates of nosocomial infection, but also led to mental distress that should not be ignored. Previous studies reported that about 10–75% of HCWs, especially the frontline workers fighting against SARS in mainland China (Wu et al., 2009), Hong Kong (Tam et al., 2004), Taiwan (Chong et al., 2004; Lu et al., 2006; Su et al., 2007), Singapore (Chan and Huak, 2004; Phua et al., 2005; Sim et al., 2004), and Canada (Maunder et al., 2006; Nickell et al., 2004), suffered from mental health problems (MHPs) during the epidemic. Compared with SARS, the number of confirmed cases of COVID-19 is more than 1100 times until now and still rising. In addition, the similar high risk of infection for HCWs, as well as the consequent heavy workload and severe shortage of protective equipment, have put more pressure on HCWs during the COVID-19 pandemic, which may give rise to various MHPs in this group. Thus, it is necessary to determine the mental health status among HCWs to carry out effective measures to relieve their stress and solve the subsequent MHPs.
What is more, previous studies have found apparent gender differences in the prevalence of certain kinds of MHPs in the general population. Females have almost twice the risk of depression, anxiety, and posttraumatic stress disorder (PTSD) (Kessler et al., 1994, 1995; Salk et al., 2017), as well as a 41% higher risk of insomnia than males (Zhang and Wing, 2006). One recent epidemiological study of mental disorders in China also found higher prevalences of depressive (males 3.0% vs. females 4.2%) and anxiety disorders (including PTSD in that survey) (males 4.8% vs. females 5.2%) among females in a nationally representative sample (Huang et al., 2019), although these gender disparities were not as large as those previously reported in other countries (Kessler et al., 1994, 1995). These gender differences exist at not only the diagnostic level but also the symptomatic or subclinical level (Haag et al., 2019). Regarding HCWs who have been reported with higher prevalences of MHPs than the general population (Kim et al., 2018; Wang et al., 2011), being female has also been found as a risk factor for the development of these problems (Guille et al., 2017; Kim et al., 2018; MacGregor et al., 2017). Nonetheless, to our knowledge, no studies have focused on the gender differences in MHPs among HCWs during the outbreak of infectious diseases such as SARS and Middle East respiratory syndrome (MERS). Only few studies reported female predominance in psychological morbidity during the SARS epidemic (Chong et al., 2004; Tam et al., 2004), and a recent study in Italy found that female HCWs perceived lower levels of well-being during the COVID-19 pandemic (De Sio et al., 2020). Given the differences in biological, psychological, and sociological characteristics that may contribute to different vulnerability to MHPs in men and women (Altemus et al., 2014; Hale et al., 2009; Ramikie and Ressler, 2018), it is necessary to understand the potential gender differences in these problems among HCWs during the COVID-19 pandemic in order to develop targeted strategies to better deal with these problems.
In view of this, the current study investigated the mental health conditions among HCWs in China during the COVID-19 outbreak, to determine: (1) the prevalence of various MHPs, including depressive, anxiety, stress, and insomnia symptoms; (2) the gender differences in these MHPs, in order to carry out targeted strategies and interventions to better prevent and control these problems in HCWs.
2. Methods
2.1. Participants and procedures
This study was part of a nationwide survey to investigate the MHPs, their related risk factors, and the demand for mental health services in HCWs throughout China during the COVID-19 outbreak. This anonymous investigation was carried out on the well-known Chinese online survey platform “Questionnaire Star” from January 29 to February 3, 2020, close to the epidemic peak in China. All participants were recruited online. Specifically, a link to this survey was distributed by investigators to different group chats of HCWs from one department each in 38 hospitals and five academic groups across the country through the WeChat program. Those who received the message of the link were voluntary to participate in this study with informed consent and could withdraw from the survey at any time. This online survey could be completed only once on the same device. The current study was approved by the research ethics committee of Nanfang Hospital, Southern Medical University.
2.2. Measures
2.2.1. Socio-demographics, work-related factors, and living situations
General information was collected by a list of questions about socio-demographics, work-related factors, and living situations in the past week. In particular, socio-demographic characteristics included gender, age (18–25, 26–30, 31–40, 41–50, or ≥51 years), ethnicity (Han or minority), marital status (unmarried, married, or divorced/widowed), and education level (secondary or below, tertiary, master's, or doctoral). Work-related factors contained staff type (doctor, nurse, or others), title (none, junior, intermediate, sub-senior, or senior), workplace (tertiary hospital, secondary hospital, or others), and direct contact with COVID-19 patients (yes or no). Living situations, such as place of residence, living in a city or countryside, and living status (alone, with family, or with others) during the past week, were also collected.
2.2.2. Depressive symptoms (Patient Health Questionnaire-9 ≥5)
Depressive symptoms were evaluated by the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001), a nine-item questionnaire inquiring the frequency of depressive symptoms during the past two weeks. Each item is rated by a four-point Likert scale (0 = not at all, 3 = nearly every day), yielding a total score ranging from 0 to 27. A total score of ≥5 was considered as experiencing depressive symptoms (Yu et al., 2012). This tool has demonstrated adequate psychometric properties in the Chinese population (Wang et al., 2014).
2.2.3. Anxiety symptoms (Generalized Anxiety Disorder-7 ≥5)
Anxiety symptoms were assessed by the Generalized Anxiety Disorder-7 (GAD-7), a short questionnaire evaluating the severity of anxiety over the past two weeks (Spitzer et al., 2006), which contains seven items rated by four-point scales (0–3) with a total score ranging from 0 to 21. Total scores ≥5 were regarded as suffering from anxiety symptoms (Qu and Sheng, 2015). The GAD-7 has been reported with satisfactory reliability and validity in Chinese (Qu and Sheng, 2015).
2.2.4. Stress symptoms (Impact of Event Scale-Revised ≥20)
Stress symptoms were measured by the Impact of Event Scale-Revised (IES-R), a commonly used scale to assess the severity of psychological stress after a stressful event during the past week (Wu and Chan, 2003). Five-point Likert scales (0 = not at all, 4 = extremely) are used to rate the 22 items with a total score of 0–88. A total score of ≥20 was regarded as experiencing stress symptoms according to previous studies during the SARS outbreak (Styra et al., 2008; Wu et al., 2009). Good psychometric properties of IES-R have been reported in China (Wu and Chan, 2003). In the current study, we particularly stated in this questionnaire that the stressful event here referred to the outbreak of COVID-19.
2.2.5. Insomnia symptoms (Insomnia Severity Index ≥8)
Insomnia symptoms were determined by the Insomnia Severity Index (ISI), a self-report instrument assessing the severity of insomnia during the past two weeks (Bastien et al., 2001). Each of the seven items is rated on a five-point scale (0–4), yielding a total score of 0–28. Total scores ≥8 were defined as having insomnia symptoms (Wong et al., 2017). The Chinese version of ISI has shown satisfactory psychometric properties (Wong et al., 2017). In addition, in the PHQ-9, GAD-7, and ISI, we particularly reminded the participants to focus on their feelings after the lockdown of Wuhan city.
2.3. Statistical analysis
Descriptive statistics were used to describe sample characteristics and distributions of MHPs. Continuous variables (scale scores) were reported as median (interquartile range [IQR]) due to the non-normal distributions, while discrete variables were stated as percentages. In univariate analyses, the Mann-Whitney U test or Pearson χ2 test was employed when appropriate to examine the associations of socio-demographics, work-related factors, and living situations with depressive, anxiety, stress, and insomnia symptoms. Those factors significantly associated with a certain kind of MHP would be further controlled in logistic regression models. In multivariate analyses, binary logistic regression was performed to determine the strengths of the relationships between gender and various MHPs, after adjusting for age using the enter method, as well as other socio-demographics, work-related factors, and living situations that significantly related to a certain MHP by using forward likelihood method. P-values <0.05 were defined as statistically significant. Statistical analyses were conducted using IBM SPSS 26.0.
3. Results
Among the 2198 contacted HCWs, 1563 (71.1%) responded with valid data. They came from all 31 provinces, autonomous regions, and municipalities around mainland China, among whom 1293 (82.7%) were females. The sample characteristics of participants are presented in Table 1 . The median (IQR) scores of PHQ-9, GAD-7, IES-R, and ISI among participants were 5.0 (2.0–8.0), 4.0 (0.0–7.0), 20.0 (8.0–33.0), and 5.0 (2.0–10.0), respectively. The prevalences of depressive, anxiety, stress, and insomnia symptoms in participants were 50.7%, 44.7%, 52.5%, and 36.1%, respectively (Table 3 ).
Table 1.
Comparisons of sample characteristics in participants with and without symptoms of depression and anxiety.
| Total sample n = 1563 | Without depressive symptoms n = 771 | With depressive symptoms n = 792 | p-valuea | Without anxiety symptoms n = 864 | With anxiety symptoms n = 699 | p-valuea | |
|---|---|---|---|---|---|---|---|
| Socio-demographics | |||||||
| Gender (female) | 1293 (82.7) | 603 (78.2) | 690 (87.1) | <0.001 | 679 (78.6) | 614 (87.8) | <0.001 |
| Age (years) | 0.231 | 0.291 | |||||
| 18–25 | 281 (18.0) | 139 (18.0) | 142 (17.9) | 152 (17.6) | 129 (18.5) | ||
| 26–30 | 445 (28.5) | 213 (27.6) | 232 (29.3) | 256 (29.6) | 189 (27.0) | ||
| 31–40 | 495 (31.7) | 235 (30.5) | 260 (32.8) | 263 (30.4) | 232 (33.2) | ||
| 41–50 | 241 (15.4) | 124 (16.1) | 117 (14.8) | 129 (14.9) | 112 (16.0) | ||
| ≥51 | 101 (6.5) | 60 (7.8) | 41 (5.2) | 64 (7.4) | 37 (5.3) | ||
| Ethnicity (Han) | 1485 (95.0) | 733 (95.1) | 752 (94.9) | 0.912 | 819 (94.8) | 666 (95.3) | 0.660 |
| Marital status | 0.858 | 0.512 | |||||
| Unmarried | 527 (33.7) | 257 (33.3) | 270 (34.1) | 293 (33.9) | 234 (33.5) | ||
| Married | 999 (63.9) | 497 (64.5) | 502 (63.4) | 554 (64.1) | 445 (63.7) | ||
| Divorced/widowed | 37 (2.4) | 17 (2.2) | 20 (2.5) | 17 (2.0) | 20 (2.9) | ||
| Education level | 0.211 | 0.639 | |||||
| Secondary or below | 33 (2.1) | 12 (1.6) | 21 (2.7) | 15 (1.7) | 18 (2.6) | ||
| Tertiary | 1197 (76.6) | 589 (76.4) | 608 (76.8) | 661 (76.5) | 536 (76.7) | ||
| Master's | 202 (12.9) | 97 (12.6) | 105 (13.3) | 112 (13.0) | 90 (12.9) | ||
| Doctoral | 131 (8.4) | 73 (9.5) | 58 (7.3) | 76 (8.8) | 55 (7.9) | ||
| Work-related factors | |||||||
| Staff type | 0.011 | 0.001 | |||||
| Doctor | 454 (29.0) | 241 (31.3) | 213 (26.9) | 271 (31.4) | 183 (26.2) | ||
| Nurse | 984 (63.0) | 458 (59.4) | 526 (66.4) | 511 (59.1) | 473 (67.7) | ||
| Othersb | 125 (8.0) | 72 (9.3) | 53 (6.7) | 82 (9.5) | 43 (6.2) | ||
| Title | 0.015 | <0.001 | |||||
| None | 192 (12.3) | 94 (12.2) | 98 (12.4) | 112 (13.0) | 80 (11.4) | ||
| Junior | 708 (45.3) | 336 (43.6) | 372 (47.0) | 393 (45.5) | 315 (45.1) | ||
| Intermediate | 447 (28.6) | 213 (27.6) | 234 (29.5) | 223 (25.8) | 224 (32.0) | ||
| Sub-senior | 160 (10.2) | 90 (11.7) | 70 (8.8) | 92 (10.6) | 68 (9.7) | ||
| Senior | 56 (3.6) | 38 (4.9) | 18 (2.3) | 44 (5.1) | 12 (1.7) | ||
| Workplace | 0.121 | 0.321 | |||||
| Tertiary hospital | 1338 (85.6) | 671 (87.0) | 667 (84.2) | 750 (86.8) | 588 (84.1) | ||
| Secondary hospital | 190 (12.2) | 88 (11.4) | 102 (12.9) | 96 (11.1) | 94 (13.4) | ||
| Others | 35 (2.2) | 12 (1.6) | 23 (2.9) | 18 (2.1) | 17 (2.4) | ||
| Direct contact with COVID-19 patients | 689 (44.1) | 284 (36.8) | 405 (51.1) | <0.001 | 322 (37.3) | 367 (52.5) | <0.001 |
| Living situations | |||||||
| Living in Hubei province | 1118 (71.5) | 514 (66.7) | 604 (76.3) | <0.001 | 584 (67.6) | 534 (76.4) | <0.001 |
| Living in a city | 1511 (96.7) | 743 (96.4) | 768 (97.0) | 0.507 | 833 (96.4) | 678 (97.0) | 0.522 |
| Living status | <0.001 | 0.014 | |||||
| Alone | 382 (24.4) | 183 (23.7) | 199 (25.1) | 218 (25.2) | 164 (23.5) | ||
| With family | 893 (57.1) | 478 (62.0) | 415 (52.4) | 509 (58.9) | 384 (54.9) | ||
| With others | 288 (18.4) | 110 (14.3) | 178 (22.5) | 137 (15.9) | 151 (21.6) | ||
P-values in bold indicate statistical significance. The sample characteristics significantly associated with a certain mental health problem would be further controlled in multivariate logistic regression models. Depressive symptoms: Patient Health Questionnaire-9 ≥ 5; anxiety symptoms: Generalized Anxiety Disorder-7 ≥ 5; COVID-19: coronavirus disease 2019. aχ2 test. bOthers refer to pharmacists, technicians, administrators, and logistics staff.
Table 3.
Associations between gender and the prevalence of mental health problems.
| Total sample n = 1563 | Prevalence of mental health problems |
Crude OR (95% CI)a | Adjusted OR (95% CI)b | ||
|---|---|---|---|---|---|
| Male n = 270 | Female n = 1293 | ||||
| Depressive symptoms, n (%) | 792 (50.7) | 102 (37.8) | 690 (53.4) | 1.88 (1.44–2.47)*** | 1.80 (1.36–2.39)*** |
| Anxiety symptoms, n (%) | 699 (44.7) | 85 (31.5) | 614 (47.5) | 1.97 (1.49–2.60)*** | 1.96 (1.46–2.63)*** |
| Stress symptoms, n (%) | 821 (52.5) | 107 (39.6) | 714 (55.2) | 1.88 (1.44–2.45)*** | 1.88 (1.42–2.50)*** |
| Insomnia symptoms, n (%) | 564 (36.1) | 76 (28.1) | 488 (37.7) | 1.55 (1.16–2.06)** | 1.36 (1.00–1.84)* |
Depressive symptoms: Patient Health Questionnaire-9 ≥ 5; anxiety symptoms: Generalized Anxiety Disorder-7 ≥ 5; stress symptoms: Impact of Event Scale-Revised ≥ 20; insomnia symptoms: Insomnia Severity Index ≥ 8. OR, odds ratio; CI, confidence interval. aχ2 test. bMultivariate binary logistic regression controlled for age (enter method) as well as other socio-demographics, work-related factors, and living situations significantly associated with a certain kind of mental health problem (forward likelihood ratio method). *p < 0.05, **p < 0.01, ***p < 0.001.
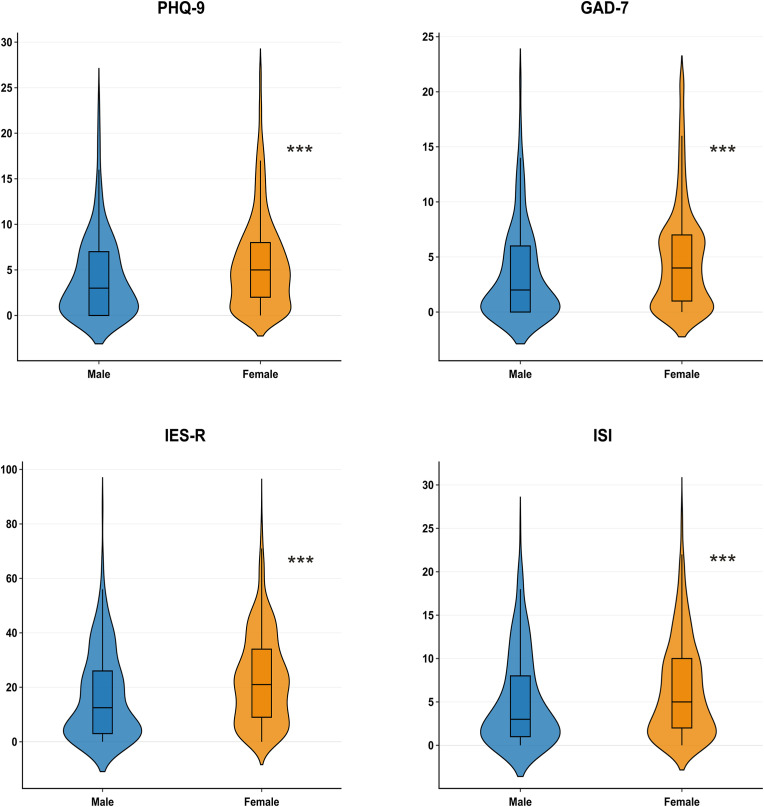
The gender differences in scale scores are depicted in Fig. 1 . Female HCWs had significantly higher scores in all these scales when compared with males (median [IQR] scores in males vs. females: PHQ-9, 3.0 [0.0–7.0] vs. 5.0 [2.0–8.0]; GAD-7, 2.0 [0.0–6.0] vs. 4.0 [1.0–7.0]; IES-R, 12.5 [3.0–26.0] vs. 21.0 [9.0–34.0]; ISI, 3.0 [1.0–8.0] vs. 5.0 [2.0–10.0]; all p < 0.001). Furthermore, compared with males, female HCWs reported a higher prevalence in each of these MHPs (range, odds ratio [OR] 1.55–1.97) (Table 3).
Fig. 1.
Gender differences in the total scores of PHQ-9, GAD-7, IES-R, and ISI. Female HCWs (orange) presented significantly higher scores in all four scales when compared with males (blue) (p < 0.001). Violin plots display the distribution of scale scores. The boxplots within the violins represent the median (the horizontal line in the box), first and third quartiles (box edges), and the minimum and maximum values within 1.5 interquartile range from the first and third quartiles (whiskers). PHQ-9: Patient Health Questionnaire-9; GAD-7: Generalized Anxiety Disorder-7; IES-R: Impact of Event Scale-Revised; ISI: Insomnia Severity Index. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The relationships between the characteristics of participants and various MHPs are presented in Table 1, Table 2. In socio-demographic factors, in addition to gender that was related to all MHPs involved, different age groups and educational levels were significantly associated with insomnia symptoms (p < 0.05). With respect to work-related characteristics, staff types, titles, and direct contact with COVID-19 patients or not were correlated with all MHPs mentioned (p < 0.05), except for titles with stress symptoms (p = 0.071). Regarding living situations during the past week, living in Hubei province or not and different living status were consistently related to all MHPs studied (p < 0.05). Those characteristics significantly related to a certain MHP were further controlled in multivariate analyses for the gender differences in these problems.
Table 2.
Comparisons of sample characteristics in participants with and without symptoms of stress and insomnia.
| Without stress symptoms n = 742 | With stress symptoms n = 821 | p-valuea | Without insomnia symptoms n = 999 | With insomnia symptoms n = 564 | p-valuea | |
|---|---|---|---|---|---|---|
| Socio-demographics | ||||||
| Gender (female) | 579 (78.0) | 714 (87.0) | <0.001 | 805 (80.6) | 488 (86.5) | 0.003 |
| Age (years) | 0.291 | 0.026 | ||||
| 18–25 | 136 (18.3) | 145 (17.7) | 160 (16.0) | 121 (21.5) | ||
| 26–30 | 213 (28.7) | 232 (28.3) | 291 (29.1) | 154 (27.3) | ||
| 31–40 | 243 (32.7) | 252 (30.7) | 318 (31.8) | 177 (31.4) | ||
| 41–50 | 99 (13.3) | 142 (17.3) | 155 (15.5) | 86 (15.2) | ||
| ≥51 | 51 (6.9) | 50 (6.1) | 75 (7.5) | 26 (4.6) | ||
| Ethnicity (Han) | 701 (94.5) | 784 (95.5) | 0.356 | 946 (94.7) | 539 (95.6) | 0.447 |
| Marital status | 0.289 | 0.053 | ||||
| Unmarried | 261 (35.2) | 266 (32.4) | 326 (32.6) | 201 (35.6) | ||
| Married | 467 (62.9) | 532 (64.8) | 655 (65.6) | 344 (61.0) | ||
| Divorced/widowed | 14 (1.9) | 23 (2.8) | 18 (1.8) | 19 (3.4) | ||
| Education level | 0.164 | 0.002 | ||||
| Secondary or below | 15 (2.0) | 18 (2.2) | 15 (1.5) | 18 (3.2) | ||
| Tertiary | 563 (75.9) | 634 (77.2) | 747 (74.8) | 450 (79.8) | ||
| Master's | 90 (12.1) | 112 (13.6) | 139 (13.9) | 63 (11.2) | ||
| Doctoral | 74 (10.0) | 57 (6.9) | 98 (9.8) | 33 (5.9) | ||
| Work-related factors | ||||||
| Staff type | 0.002 | <0.001 | ||||
| Doctor | 227 (30.6) | 227 (27.6) | 330 (33.0) | 124 (22.0) | ||
| Nurse | 440 (59.3) | 544 (66.3) | 589 (59.0) | 395 (70.0) | ||
| Othersb | 75 (10.1) | 50 (6.1) | 80 (8.0) | 45 (8.0) | ||
| Title | 0.071 | 0.006 | ||||
| None | 99 (13.3) | 93 (11.3) | 113 (11.3) | 79 (14.0) | ||
| Junior | 329 (44.3) | 379 (46.2) | 445 (44.5) | 263 (46.6) | ||
| Intermediate | 199 (26.8) | 248 (30.2) | 281 (28.1) | 166 (29.4) | ||
| Sub-senior | 80 (10.8) | 80 (9.7) | 114 (11.4) | 46 (8.2) | ||
| Senior | 35 (4.7) | 21 (2.6) | 46 (4.6) | 10 (1.8) | ||
| Workplace | 0.734 | 0.358 | ||||
| Tertiary hospital | 633 (85.3) | 705 (85.9) | 863 (86.4) | 475 (84.2) | ||
| Secondary hospital | 94 (12.7) | 96 (11.7) | 117 (11.7) | 73 (12.9) | ||
| Others | 15 (2.0) | 20 (2.4) | 19 (1.9) | 16 (2.8) | ||
| Direct contact with COVID-19 patients | 271 (36.5) | 418 (50.9) | <0.001 | 387 (38.7) | 302 (53.5) | <0.001 |
| Living situations | ||||||
| Living in Hubei province | 490 (66.0) | 628 (76.5) | <0.001 | 686 (68.7) | 432 (76.6) | <0.001 |
| Living in a city | 719 (96.9) | 792 (96.5) | 0.634 | 972 (97.3) | 539 (95.6) | 0.067 |
| Living status | 0.014 | <0.001 | ||||
| Alone | 176 (23.7) | 206 (25.1) | 229 (22.9) | 153 (27.1) | ||
| With family | 449 (60.5) | 444 (54.1) | 609 (61.0) | 284 (50.4) | ||
| With others | 117 (15.8) | 171 (20.8) | 161 (16.1) | 127 (22.5) | ||
P-values in bold indicate statistical significance. The sample characteristics significantly associated with a certain mental health problem would be further controlled in multivariate logistic regression models. Stress symptoms: Impact of Event Scale-Revised ≥ 20; insomnia symptoms: Insomnia Severity Index ≥ 8; COVID-19: coronavirus disease 2019. aχ2 test. bOthers refer to pharmacists, technicians, administrators, and logistics staff.
The gender differences in depressive, anxiety, stress, and insomnia symptoms are delineated in Table 3. Multivariate analyses adjusting for socio-demographics, work-related factors, and living situations revealed that female HCWs still had higher risks for all MHPs involved than males (range, adjusted OR 1.36–1.96).
4. Discussion
In this study, we found relatively high prevalences of depressive, anxiety, stress, and insomnia symptoms among HCWs in China during the COVID-19 outbreak, which are higher than the results of most studies on HCWs during the SARS epidemic (Chan and Huak, 2004; Lu et al., 2006; May et al., 2004; Nickell et al., 2004; Sim et al., 2004; Su et al., 2007; Wu et al., 2009) and those on the general population during the COVID-19 outbreak in China (Shi et al., 2020; Wang et al., 2020), while lower than or close to the findings of a few studies on HCWs during the SARS epidemic in China (Chong et al., 2004; Tam et al., 2004) and one study during the COVID-19 pandemic in Italy (De Sio et al., 2020). These differences may not only arise from different timing and tools for assessment together with the population investigated, but also reflect a relatively severe impact of the COVID-19 pandemic on the mental health of HCWs. What is more, significant gender differences were found in all prevalences of these symptoms. Specifically, female HCWs had higher vulnerability than males in all MHPs involved in the current investigation, which is consistent with previous research on the general population (Huang et al., 2019; Kessler et al., 1994, 1995; Salk et al., 2017) and on HCWs during the SARS (Chong et al., 2004; Tam et al., 2004) and COVID-19 outbreak (De Sio et al., 2020).
The high prevalence of MHPs in HCWs could be attributable to the following reasons. Firstly, similar to SARS, the high infectivity and virulence of SARS-coronavirus-2 (SARS-CoV-2) and the consequent high risk of infection among HCWs led to fear and anxiety in them, especially in those at the frontline (Maunder et al., 2003). Sometimes they had to take care of their infected colleagues, which may increase their fear and worry (Maunder et al., 2003). Moreover, the uncertainty about the clinical features, the lack of effective therapy, and the relatively high rate of severe cases and mortality of this novel disease also elicited frustration, powerlessness, self-doubt, and guilt among HCWs (Chong et al., 2004). Secondly, the large and rapidly growing number of cases has brought an increasing workload and subsequent heavy physical and mental burdens, especially among the frontline staff (Maunder et al., 2004). Being equipped with the cumbersome protective gear during working hours, the frontline workers could not even eat, drink, or go to the toilet due to the strict infection control procedures (Chen et al., 2006). What is more, the vast number of cases also resulted in a serious lack of protective equipment throughout China, which added to their hopelessness and anxiety (Chong et al., 2004). Finally, HCWs were not only worried about their own health, but also afraid of transmitting the infection to their family and friends. Thus, they always chose to avoid close contact with others, which might in turn aggravate their stress due to the lack of social communication and interaction (May et al., 2004). Furthermore, the perceived stigmatization and consequent social isolation contributed to their stress (Maunder et al., 2006). Taken together, the above factors may result in a list of emotional disturbances in HCWs, accompanied by insomnia, which may be the first and most prominent symptom attributed to such an outbreak (Maunder et al., 2003; Su et al., 2007).
The current study also found significant gender differences in the development of MHPs among HCWs during the COVID-19 pandemic, which is in line with previous findings in the SARS epidemic (Chong et al., 2004; Tam et al., 2004). Several mechanisms have been raised to explain female susceptibility (Hale et al., 2009; Ramikie and Ressler, 2018). Biologically, gender differences in the vulnerability to mental distress are partially based on the effects of sex chromosome genes and fluctuations of sex hormones, hypothalamic–pituitary–adrenal axis activity, and related monoamine neurotransmitters (Altemus et al., 2014; Li and Graham, 2017). These fluctuations may result in intermittently increased susceptibility to psychological distress together with consequent negative emotions, non-adaptive behaviors, and poor sleep quality in females attributable to poor responses in the central nervous system (Altemus et al., 2014; Li and Graham, 2017; Ramikie and Ressler, 2018). Psychologically, females present more rumination and tend to rely on emotion-focused coping styles under stress, such as self-blame, avoidance, suppression, and sense of incompetence, which are related to increased depressive, anxiety, and stress symptoms (Altemus et al., 2014; Kornfield et al., 2018). In addition, when encountering stressful events, females’ attentional bias to threat and behavioral inhibition temperament give rise to quick and rigid stimulus-response associations, which leads to more anxiety and stress symptoms, as well as insomnia as an early and common reaction to stress in females than in males (Catuzzi and Beck, 2014; Su et al., 2007). Sociologically, the gender differences in trauma type, symptoms reporting, economic resources, social support, and social roles may contribute to higher vulnerability to MHPs in women (Altemus et al., 2014; Wamser-Nanney and Cherry, 2018). All of these factors may cause or exacerbate the MHPs in female HCWs.
4.1. Clinical implications
A list of individual and systemic measures could be taken to deal with various MHPs in HCWs during the pandemic. First of all, cognitive guidance could be provided to HCWs that these MHPs are common responses to an extraordinary stressor (Maunder et al., 2004), and they should also accept the imperfection and failure of medicine because it is not omnipotent (Wong et al., 2005). Secondly, positive coping strategies, such as venting negative emotions, problem-solving, and support seeking, are encouraged to alleviate emotional distress (Styra et al., 2008; Wong et al., 2005). Active communication with peers and family rather than avoidance helps to mitigate the adverse effects of stigmatization and social isolation (May et al., 2004). Thirdly, mental health professionals should play a significant role in the early identification and intervention of the potential MHPs in at-risk individuals (Maunder et al., 2003). Finally, managers should take a series of measures to reduce the sense of insecurity, uncertainty, and work stress among HCWs (Brooks et al., 2018). Adequate training on the up-to-date knowledge of COVID-19 and infection control measures should be provided to HCWs to reduce their perceived risk and increase their confidence and self-efficacy (Brooks et al., 2018). A safe working environment for HCWs and an adequate supply of protective equipment should also be provided (Maunder et al., 2008). Moreover, HCWs could benefit from reasonable manpower allocation and scheduled working hours that ensure their enough rest (McAlonan et al., 2007). Besides, take good care of their families to relieve them of their worries (Brooks et al., 2018). All of these strategies may individually and systematically bolster the resilience of HCWs in order to relieve their mental distress and corresponding sleep disturbances during the outbreak (Brooks et al., 2018).
What is more, due to the gender differences in MHPs, different strategies and interventions should be performed according to different characteristics of male and female HCWs. Particularly, the large proportion of females in HCWs (Chen et al., 2020) and their high susceptibility to various MHPs warrant special attention to female workers. Biologically, proper rest and attention should be given to female HCWs during menstruation. Psychological education and cognitive restructuring could be conducted according to different stages of the menstrual cycle (Li and Graham, 2017). Psychologically, female HCWs should be guided to adopt positive coping styles and adaptive emotional regulation strategies (Li and Graham, 2017; Phua et al., 2005). Furthermore, different utilization of neural resources under stress between men and women allows gender-specific psychological interventions (Seo et al., 2017). Particularly, male HCWs may benefit more from cognitive behavioral therapy, while female HCWs may benefit more from mindfulness meditation (Seo et al., 2017). Sociologically, the income of female HCWs should be guaranteed and matched with males to deal with the unequal distribution of social capital resources (Wamser-Nanney and Cherry, 2018). Moreover, stronger social supports should be provided to females who are more vulnerable to the lack of supports (Wamser-Nanney and Cherry, 2018). In addition, given the work-family conflicts and caretaking roles of female HCWs, it is necessary to give special care to their elderly parents and young children so that they can work at ease (Guille et al., 2017). O verall, various emotional and sleep problems dominated by females could be alleviated pertinently by the above strategies and measures. However, this does not mean that the MHPs of male HCWs are not worthy of attention. The aforementioned strategies for both genders and a few suggestions for males can be well used to alleviate the MHPs in male staff.
4.2. Strengths and limitations
Our study has several strengths. To our knowledge, this is the first study focused on the gender differences in various MHPs of HCWs during the outbreak of infectious diseases such as SARS, MERS, and COVID-19. The relatively large sample size with a high response rate and participants from all over China made our study more representative. However, there are also some limitations. First, the cross-sectional design prevents us from determining the changes in mental health status of HCWs over time, which requires prospective studies with follow-up. Second, convenient sampling was employed to recruit participants, which may limit sample representativeness and the generalizability of findings to some degree (Shi et al., 2017). Third, although the response rate was 71.1% in this study, 28.9% of HCWs did not respond, which may lead to some bias. Fourth, there was a significant gender imbalance (females 82.7%) in the sample of this study. However, this proportion of females is only a little higher than that of Chinese HCWs (females 71.8%) (National Health Commission of the People's Republic of China, 2019). Additionally, previous research suggested that women are more willing to participate in online surveys (Smith, 2008). Fifth, only HCWs were included in this study, thus their MHPs and potential gender differences could not be compared directly with non-HCWs during this pandemic, which needs further investigation. Sixth, all data were collected by self-report questionnaires, which may increase the possibility of recall and social desirability biases (Liu et al., 2019). Nonetheless, self-administered questionnaires enable us to quickly obtain the data on mental health status in a large number of HCWs from all over the country through the Internet. Seventh, previous mental health disorders and health problems in general of the participants were not considered in this study. They may also have an effect on their mental health status during this pandemic to some extent. Eighth, the workload, such as working hours per day, working days during this period, which may also contribute to the MHPs of HCWs, was not taken into account in this survey. At last, other potential risk factors, such as living in Hubei province or having direct contact with COVID-19 patients, also need special attention. However, this study only focused on gender differences and thus did not elaborate on other possible related factors, which warrants further research.
4.3. Conclusions
In summary, this study indicates high prevalences of depressive, anxiety, stress, and insomnia symptoms among HCWs during the COVID-19 outbreak, and demonstrates significant gender differences that female HCWs are more vulnerable to all MHPs involved. These findings highlight the need for timely, special care and support for HCWs during the outbreak, especially for females.
CRediT authorship contribution statement
Shuai Liu: Formal analysis, Investigation, Resources, Writing - Original Draft, Visualization, Funding acquisition. Lulu Yang: Formal analysis, Investigation, Resources, Writing - Review & Editing, Visualization. Chenxi Zhang: Validation, Investigation, Resources, Writing - Review & Editing. Yan Xu: Investigation, Resources, Writing - Review & Editing. Lidan Cai: Investigation, Resources, Writing - Review & Editing. Simeng Ma: Investigation, Resources, Data Curation. Ying Wang: Investigation, Resources, Data Curation. Zhongxiang Cai: Investigation, Resources, Data Curation. Hui Du: Investigation, Resources. Ruiting Li: Investigation, Resources, Data Curation. Lijun Kang: Investigation, Resources, Data Curation. Huirong Zheng: Investigation, Resources. Zhongchun Liu: Conceptualization, Methodology, Investigation, Resources, Supervision, Project administration, Funding acquisition. Bin Zhang: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Supervision, Project administration, Funding acquisition.
Funding
This work was supported by the National Natural Science Foundation of China, China [S.L., grant number 81901348]; the Chinese Sleep Research Society Hansoh Project, China [S.L., grant number 2019HSC03]; the National Natural Science Foundation of China, China [B.Z., grant number 82071488]; the Science and Technology Planning Project of Guangdong Province, China [grant number 2017B020227010]; the President Foundation of Nanfang Hospital, Southern Medical University, China [B.Z., grant number 2019Z014]; and the National Key R & D Program of China, China [Z.L., grant number 2018YFC1314600]. The funders had no role in study design, data collection or analysis, manuscript preparation, or the decision to submit for publication.
Data statement
Data are available from corresponding authors upon reasonable request.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgements
We would like to thank all healthcare workers who participated in this study. We also thank Dhirendra Paudel for the careful revision and proofreading of the manuscript.
References
- Altemus M., Sarvaiya N., Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Dunn R., Amlot R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018;60(3):248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- Catuzzi J.E., Beck K.D. Anxiety vulnerability in women: a two-hit hypothesis. Exp. Neurol. 2014;259:75–80. doi: 10.1016/j.expneurol.2014.01.023. [DOI] [PubMed] [Google Scholar]
- Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. (Lond.) 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43(2):215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W., Bai Y., Chen C. 2020. How to better protect and care for the frontline medical staff in the fight against the epidemic.http://www.xinhuanet.com/2020-03/08/c_1125682438.htm (accessed 8 March 2020) [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C., Huang O.L., Wen J.K., Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- De Sio S., Buomprisco G., La Torre G., Lapteva E., Perri R., Greco E., Mucci N., Cedrone F. The impact of COVID-19 on doctors' well-being: results of a web survey during the lockdown in Italy. Eur. Rev. Med. Pharmacol. Sci. 2020;24(14):7869–7879. doi: 10.26355/eurrev_202007_22292. [DOI] [PubMed] [Google Scholar]
- Guille C., Frank E., Zhao Z., Kalmbach D.A., Nietert P.J., Mata D.A., Sen S. Work-family conflict and the sex difference in depression among training physicians. JAMA Intern Med. 2017;177(12):1766–1772. doi: 10.1001/jamainternmed.2017.5138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haag K., Fraser A., Hiller R., Seedat S., Zimmerman A., Halligan S.L. The emergence of sex differences in PTSD symptoms across development: evidence from the ALSPAC cohort. Psychol. Med. 2019;1–6 doi: 10.1017/s0033291719001971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L., Do D.P., Basurto-Davila R., Heron M., Finch B.K., Dubowitz T., Lurie N., Bird C.E. Does mental health history explain gender disparities in insomnia symptoms among young adults? Sleep Med. 2009;10(10):1118–1123. doi: 10.1016/j.sleep.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wang Y., Wang H., Liu Z., Yu X., Yan J., Yu Y., Kou C., Xu X., Lu J., Wang Z., He S., Xu Y., He Y., Li T., Guo W., Tian H., Xu G., Xu X., Ma Y., Wang L., Wang L., Yan Y., Wang B., Xiao S., Zhou L., Li L., Tan L., Zhang T., Ma C., Li Q., Ding H., Geng H., Jia F., Shi J., Wang S., Zhang N., Du X., Du X., Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet psychiatry. 2019;6(3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University . 2020. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)https://coronavirus.jhu.edu/map.html [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet psychiatry. 2020;7(3):e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., McGonagle K.A., Zhao S., Nelson C.B., Hughes M., Eshleman S., Wittchen H.U., Kendler K.S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the national comorbidity survey. Arch. Gen. Psychiatr. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Sonnega A., Bromet E., Hughes M., Nelson C.B. Posttraumatic stress disorder in the national comorbidity survey. Arch. Gen. Psychiatr. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kim M.S., Kim T., Lee D., Yook J.H., Hong Y.C., Lee S.Y., Yoon J.H., Kang M.Y. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Ann Occup Environ Med. 2018;30:31. doi: 10.1186/s40557-018-0244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield S.L., Hantsoo L., Epperson C.N. What does sex have to do with it? The role of sex as a biological variable in the development of posttraumatic stress disorder. Curr. Psychiatr. Rep. 2018;20(6):39. doi: 10.1007/s11920-018-0907-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S.H., Graham B.M. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet psychiatry. 2017;4(1):73–82. doi: 10.1016/s2215-0366(16)30358-3. [DOI] [PubMed] [Google Scholar]
- Liu S., Wing Y.K., Hao Y., Li W., Zhang J., Zhang B. The associations of long-time mobile phone use with sleep disturbances and mental distress in technical college students: a prospective cohort study. Sleep. 2019;42(2):zsy213. doi: 10.1093/sleep/zsy213. [DOI] [PubMed] [Google Scholar]
- Lu Y.C., Shu B.C., Chang Y.Y., Lung F.W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother. Psychosom. 2006;75(6):370–375. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- MacGregor A.J., Clouser M.C., Mayo J.A., Galarneau M.R. Gender differences in posttraumatic stress disorder among U.S. Navy healthcare personnel. J Womens Health (Larchmt) 2017;26(4):338–344. doi: 10.1089/jwh.2014.5130. [DOI] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ (Can. Med. Assoc. J.) 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M., Goldbloom D.S., Gupta M., Hunter J.J., McGillis Hall L., Nagle L.M., Pain C., Peczeniuk S.S., Raymond G., Read N., Rourke S.B., Steinberg R.J., Stewart T.E., VanDeVelde-Coke S., Veldhorst G.G., Wasylenki D.A. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K., Petryshen P., Steinberg R., Wasylenki D., Koh D., Fones C.S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- Maunder R.G., Leszcz M., Savage D., Adam M.A., Peladeau N., Romano D., Rose M., Schulman B. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can. J. Public Health. 2008;99(6):486–488. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May R.M., McLean A.R., Pattison J., Weiss R.A., Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., Chua S.E., Wong J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatr. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- National Health Commission of the People's Republic of China . first ed. Peking Union Medical College Press; Beijing: 2019. China Health Statistics Yearbook 2019. [Google Scholar]
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E.G. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ (Can. Med. Assoc. J.) 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phua D.H., Tang H.K., Tham K.Y. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad. Emerg. Med. 2005;12(4):322–328. doi: 10.1197/j.aem.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Qu S., Sheng L. Diagnostic test of screening generalized anxiety disorders in general hospital psychological department with GAD-7. Chin. Ment. Health J. 2015;29(12):939–944. doi: 10.3969/j.issn.1000-6729.2015.12.010. [DOI] [Google Scholar]
- Ramikie T.S., Ressler K.J. Mechanisms of sex differences in fear and posttraumatic stress disorder. Biol. Psychiatr. 2018;83(10):876–885. doi: 10.1016/j.biopsych.2017.11.016. [DOI] [PubMed] [Google Scholar]
- Salk R.H., Hyde J.S., Abramson L.Y. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017;143(8):783–822. doi: 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo D., Ahluwalia A., Potenza M.N., Sinha R. Gender differences in neural correlates of stress-induced anxiety. J. Neurosci. Res. 2017;95(1–2):115–125. doi: 10.1002/jnr.23926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Lu Z.A., Que J.Y., Huang X.L., Liu L., Ran M.S., Gong Y.M., Yuan K., Yan W., Sun Y.K., Shi J., Bao Y.P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Wang L., Jia X., Li Z., Mu H., Liu X., Peng B., Li A., Fan L. Prevalence and correlates of symptoms of post-traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross-sectional study. BMJ Open. 2017;7(7) doi: 10.1136/bmjopen-2017-016810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim K., Chong P.N., Chan Y.H., Soon W.S.W. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J. Clin. Psychiatr. 2004;65(8):1120–1127. doi: 10.4088/jcp.v65n0815. [DOI] [PubMed] [Google Scholar]
- Smith W.G. ERIC Document Reproduction Service; 2008. Does Gender Influence Online Survey Participation? A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; p. ED 501717. [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Styra R., Hawryluck L., Robinson S., Kasapinovic S., Fones C., Gold W.L. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J. Psychosom. Res. 2008;64(2):177–183. doi: 10.1016/j.jpsychores.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su T.P., Lien T.C., Yang C.Y., Su Y.L., Wang J.H., Tsai S.L., Yin J.C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007;41(1–2):119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34(7):1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- Wamser-Nanney R., Cherry K.E. Children's trauma-related symptoms following complex trauma exposure: evidence of gender differences. Child Abuse Negl. 2018;77:188–197. doi: 10.1016/j.chiabu.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Chen C., Hsu S., Lee S., Wang C., Yeh W. Active job, healthy job? Occupational stress and depression among hospital physicians in Taiwan. Ind. Health. 2011;49(2):173–184. doi: 10.2486/indhealth.ms1209. [DOI] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatr. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Wong M.L., Lau K.N.T., Espie C.A., Luik A.I., Kyle S.D., Lau E.Y.Y. Psychometric properties of the sleep condition indicator and insomnia severity Index in the evaluation of insomnia disorder. Sleep Med. 2017;33:76–81. doi: 10.1016/j.sleep.2016.05.019. [DOI] [PubMed] [Google Scholar]
- Wong T.W., Yau J.K., Chan C.L., Kwong R.S., Ho S.M., Lau C.C., Lau F.L., Lit C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005;12(1):13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 11 March 2020) [Google Scholar]
- Wu K.K., Chan K.S. The development of the Chinese version of impact of event scale – revised (CIES-R) Soc. Psychiatr. Psychiatr. Epidemiol. 2003;38(2):94–98. doi: 10.1007/s00127-003-0611-x. [DOI] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X., Tam W.W.S., Wong P.T.K., Lam T.H., Stewart S.M. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr. Psychiatr. 2012;53(1):95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Zhang B., Wing Y.K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]