Abstract
Objective
To provide evidence on the effects of expansions to private and public insurance programs on adolescent specialty substance use disorder (SUD) treatment use.
Data Source/Study Setting
The Treatment Episodes Data Set (TEDS), 1996 to 2017.
Study Design
A quasi‐experimental difference‐in‐differences design using observational data.
Data Collection
The TEDS provides administrative data on admissions to specialty SUD treatment.
Principal Findings
Expansions of laws that compel private insurers to cover SUD treatment services at parity with general health care increase adolescent admissions by 26% (P < .05). These increases are driven by nonintensive outpatient admissions, the most common treatment episodes, which rise by 30% (P < .05) postparity law. In contrast, increases in income eligibility for public insurance targeting those 6‐18 years old are not statistically associated with SUD treatment.
Conclusions
Private insurance expansions allow more adolescents to receive SUD treatment, while public insurance income eligibility expansions do not appear to influence adolescent SUD treatment.
Keywords: adolescents, health care, parity laws, public insurance, substance use disorders
What is Already Known on this Topic
Most adolescents who would benefit from SUD treatment do not receive such care
Costs and lack of insurance coverage are commonly stated barriers to SUD treatment receipt
State insurance policies increase adult treatment use, but effects on adolescents are unknown
What This Study Adds
Coverage for SUD services has increased over time through public insurance eligibility expansions and state mandates that compel private insurers to improve SUD coverage
State private market mandates increase adolescent SUD treatment admissions
Adolescent SUD treatment admissions do not change following state expansions of public insurance income eligibility
1. INTRODUCTION
Adolescence is a key developmental period in establishing health and human capital trajectories. 1 During adolescence, the prefrontal cortex region of the brain is developing and many substance use disorders (SUDs) emerge. Therefore, treatment received at this time period can have benefits throughout the life course. 2 , 3 , 4 As of 2018, 4.3% of United States adolescents meet diagnostic criteria for an SUD. 5 While effective SUD treatments are available, 6 , 7 , 8 only 10% of adolescents who could benefit from treatment receive care for this health condition in any given year. 9 Identifying factors that influence SUD treatment‐seeking during adolescence is therefore important for understanding health trajectories. Key barriers to treatment‐seeking are inability to pay and lack of insurance coverage. 9 Thus, expanding insurance coverage to reduce financial cost faced by patients and their families may encourage adolescent SUD treatment take‐up and improve health over the life course. To date, the literature has not explored this question, which suggests that the full benefits of insurance policies, private and public, may not be recognized.
Beginning in the 1990s, states adopted mandates that required private insurers to cover SUD treatment to various degrees. “Parity” laws compel private insurers to provide the same level of coverage for SUD treatment as they do for general health care services. In particular, beneficiary cost‐sharing, service limitations, and other utilization management techniques (eg, prior authorization) must be equal for SUD and general health care. The federal government imposed national parity in 2014 upon implementation of the Affordable Care Act (ACA). A solid foundation of research exists showing that these parity laws, and other private insurance mandates that require coverage of SUD treatment, increase SUD treatment use among adults. 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26
Public insurance also plays an important role in the financing of SUD treatment in the US. Medicaid and the Children's Health Insurance Program (CHIP) cover SUD treatment services for many lower income adolescents. After targeted federal and state expansions to pregnant women and infants in the 1980s, states began to increase income eligibility thresholds for older children (ie, 6‐18) in the 1990s. In 1997, CHIP was introduced to offer states a complementary policy lever to Medicaid. States can use CHIP funds to expand Medicaid eligibility or can add supplemental CHIP programs with income eligibility thresholds above those for Medicaid, sometimes exceeding 300% of the federal poverty level (FPL). 27 Over our study period, states expanded Medicaid programs, developed CHIP programs, and set income eligibility thresholds for both, with more than half of all children having been covered by one of these programs by 2016. 28 Research on the effects of public insurance expansions on SUD treatment has focused on adults and shows that income eligibility expansions increase treatment use within this population. 12 , 37
We exploit variation in the above‐noted state‐level parity laws and public coverage expansions targeting older children on specialty SUD treatment use among adolescents aged 12‐17. Both parity laws and increases in public insurance eligibility thresholds reduce the cost of SUD treatment for covered individuals. For parity laws, in addition to financial cost reductions, nonquantitative utilization management techniques (eg, annual service limitations) are also reduced, likely improving access. We hypothesize that postexpansion total admissions will increase, and admissions for patients with private and public coverage will also increase.
However, there are features of insurance that may offset the hypothesized increase in admissions. First, increases in private premiums following a parity law adoption may lead some beneficiaries to drop private coverage because the more generous coverage is now unaffordable, and they may not qualify for public coverage if their income is too high. 38 , 39 , 40 Second, some patients will drop the more costly private insurance and be eligible to take up the less costly public insurance, that is, “crowd‐out.” 41 Crowd‐out itself could increase treatment use as public insurance, on average, offers SUD treatment service coverage that is broader in terms of specific services included in the plan than private insurance. 42 However, limited access to providers for the publicly insured 43 , 44 may mute any crowd‐out–induced increases in treatment use. In addition, there is heterogeneity across insurance plans in coverage for SUD treatment, with some private plans offering broader coverage of these services than the public option.
In our empirical analysis, we consider the impact of insurance policies on total admissions, and separately on admissions that are or are not referred through the criminal justice system. We suspect that admissions not referred from the criminal justice system are potentially motivated by factors included in standard models of patient demand for health care. 30 In contrast, admissions referred to treatment through the criminal justice system may be guided by other factors (eg, judicial discretion in sentencing).
2. METHODS
2.1. Data
We use TEDS, an all‐payer administrative database compiled annually by the Substance Abuse and Mental Health Services Administration (SAMHSA). TEDS contains the near universe of specialty SUD treatment facilities that receive financial support from the state or federal government, are certified by the state to provide SUD treatment, or are tracked for a state‐specific reason. A specialty SUD treatment facility is a hospital, residential facility, outpatient treatment facility, or other facility with an SUD treatment program. Specialty care accounts for 37% of all SUD treatment spending in the US 45 and reflects 65% of SUD treatment received by adolescents. 46 Annually, TEDS includes information on two million specialty SUD treatment admissions. At the time of writing, data are available from 1992 to 2017.
TEDS is a standard dataset used within health services research to study SUD treatment. 26 , 30 , 47 , 48 Additionally, the federal government uses TEDS to estimate the national costs of SUD treatment. 49 While not a nationally representative sample, patients treated in TEDS‐tracked facilities are representative of the SUD treatment‐receiving population. 50
We exclude admissions for patients older than 17 years; age categories in TEDS do not allow us to include 18‐year‐olds. We also exclude detoxification‐only admissions as they are not viewed as treatment per se. 51 Although TEDS initiated in 1992, we begin our study period in 1996, a pivotal point in public insurance programs: Medicaid was delinked from cash welfare and became a stand‐alone program. Prior to 1996, we cannot disentangle public insurance effects from effects of other public assistance programs, which prevents clean identification of treatment effects.
2.2. Outcomes
We consider several SUD treatment outcomes. In particular, we consider total admissions and admissions by patient's insurance coverage: private, any public (Medicaid, Medicare, and other public), and no insurance. We also study the effect of policy changes on treatment setting: residential or hospital (“residential”), intensive outpatient (ie, treatment lasting two or more hours per day for three or more days per week), and nonintensive outpatient (ie, ambulatory treatment services including individual, family, and/or group services, and may include pharmacological therapies). Not all treatment modalities we study result in a patient being “admitted” to treatment (eg, outpatient care), but we use the term “admissions” for brevity.
While states are mandated by federal law to provide admissions data to TEDS, submission of patient insurance coverage information is voluntary. There is a nontrivial amount of missing insurance information. We retain state/year pairs with no more than 25% of the insurance information missing. 30 Table S1 reports the states in our analysis sample and the full TEDS sample. We have 42 states in our analysis sample.
2.3. Insurance policy data
2.3.1. Parity laws
We use data from Maclean et al 11 to construct our parity law variable. We match law effective dates to the TEDS as of January 1 of each year. During our study, 12 states passed their own parity laws, ten of which appear in our analysis sample. The years 2014‐2017 offer additional variation in parity laws. The ACA leveraged the already‐existing Mental Health Parity and Addiction Equity Act (MHPAEA), effective in 2010, which had mandated “parity if offered.” In particular, private insurers were not mandated to offer SUD care, but, if offered, services were required to be covered at parity with general health care. The ACA defines SUD treatment as one of the ten essential benefits that must be covered by private plans, and this Act requires that such plans are MHPAEA compliant, which implies that states impacted by these changes have parity from 2014 onward. In our sample, 32 states transition to parity in 2014. 52
The state parity laws that we study (ie, states that adopted their own parity laws) are “full parity” laws; that is, they require that private insurance plans (i) cover SUD treatment services, and (ii) cover SUD treatment and general health care services equally in terms of cost‐sharing, service limitations, and so forth. In particular, we do not study “mandated benefits” (which require only that private plans cover specific services) or parity if offered (defined above). We note that the state parity laws do not impact self‐insured plans due to the Employee Retirement Income Security Act (ERISA). 53 Small firms are less likely to self‐insure, and we control for the share of small firms in a state in regressions to account for ERISA. MHPAEA, in combination with the ACA, induces all states into parity as of January 1, 2014. All firms, self‐insured and not self‐insured, are impacted by this federal policy change.
The effects of a parity law potentially vary across states based on the regulation in place prior to passage of the law. Table S2 reports the effective date for each parity law and indicates whether states transitioned to full parity from no regulation of SUD treatment, or from a weaker law (eg, mandated benefits without parity). Given differences in the states that transitioned to parity from no regulation vs. from a weak law, the extent to which we expect heterogeneity in the laws’ effects is ex ante unclear. One might expect that the “parity dose” is larger when transitioning from no parity to parity than a transition from a minimum mandated benefit law. However, states with a preexisting SUD coverage law may have a better developed SUD treatment system that can absorb demand from the newly covered, and/or may have less stigma toward SUDs and associated treatment. Similarly, there could be differences across such states in terms of driving distance to treatment.
2.3.2. Medicaid and CHIP income eligibility thresholds targeting those six to 18 years
There is no central repository of states’ Medicaid and CHIP income eligibility thresholds. We use several sources (ie, American Academy of Pediatrics, Kaiser Foundation, 27 and our reading of original state documents) to assemble older children's income thresholds in each state each year, recording the Medicaid threshold for states without a separate CHIP program and the CHIP threshold otherwise, which is always higher than Medicaid (full details available on request). We take the perspective of the parent or guardian contemplating enrolling their child in public insurance: Only the income eligibility level is salient, not the name of the program. Table S3 reports the exact Medicaid or CHIP threshold (relative to the FPL) for children 6‐18 in each state in each year of our study period. We use the state income threshold in January.
For expanded eligibility for Medicaid and CHIP to influence SUD treatment, these insurance programs must cover such treatment. Through the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit, Medicaid must cover all services, including SUD treatment in the settings we study, for adolescents when medically necessary. 54 , 55 CHIP programs that are extensions of Medicaid are also bound by the EPSDT benefit and must cover SUD treatment, when medically necessary, for adolescents. Thus, these plans cover all settings that we examine over our study period. While stand‐alone CHIP programs are not under the mandate, our inspection of state‐specific coverage as described in think tank reports and journal articles indicates that nearly all CHIP programs cover the services we study (Table S4). 42 , 56 , 57 , 58
We note that Medicaid and CHIP programs have undergone changes in their operation and organization over our study period; thus, public coverage is not a uniform benefit structure and is instead better conceptualized as a policy that is continuously in motion. This changing structure is a feature of all Medicaid and CHIP studies of which we are aware. Particularly important changes, for our study, include the increased use of managed care organizations (MCO) over time, networks that often include somewhat limited access to all providers and behavioral health care providers in particular, and the use of behavioral health “carve‐outs.”
We do not study a public expansion of specialty SUD treatment coverage per se; however, all Medicaid and nearly all CHIP programs cover these services over our study period. Thus, raising the income eligibility threshold increases the number of adolescents eligible for coverage that includes SUD treatment.
2.4. Approach
We estimate a difference‐in‐differences (DD) model that leverages state‐level variation in two insurance policies: (i) parity laws and (ii) income eligibility for Medicaid and CHIP. Our DD regression model is outlined in Equation (1):
| (1) |
is an SUD treatment outcome among adolescents 12‐17 years in state s in year t. is an indicator for a parity law in state s in time t. is the income eligibility threshold (in terms of FPL) for older children's public health insurance in each state‐year. For example, a state with a threshold of 150% FPL is coded as 1.5. is a vector of state‐level characteristics (variables are listed in Table 1). 12 , 67 and are vectors of state and year fixed effects. is the error term. We use ordinary least squares and report 95% confidence intervals that account for within‐state correlations. 68 Outcomes are scaled per 100 000 adolescents 12‐17 years in the population; we calculate age‐shares from the American Community Survey 69 and obtain state population from the US Census. 70 Data are unweighted.
Table 1.
Summary statistics: Treatment Episode Data Set (1996‐2017)
| Variable | All admissions | Noncriminal justice system admissions | Criminal justice system admissions |
|---|---|---|---|
| Admissions overall (rate per 100 000 state adolescents averaged over the state‐years) | |||
| Total (all admissions regardless of insurance status or treatment setting) | 478.1 | 247.2 | 230.9 |
| Admissions by insurance status (rate per 100 000 state adolescents averaged over the state‐years) | |||
| Private insurance | 113.8 | 68.5 | 45.3 |
| Public insurance | 212.6 | 109.9 | 102.7 |
| No insurance | 151.7 | 68.8 | 82.9 |
| Admissions by treatment setting (rate per 100 000 state adolescents averaged over the state‐years) | |||
| Residential treatment | 77.0 | 42.1 | 34.9 |
| Intensive outpatient treatment | 69.3 | 32.3 | 37.1 |
| Nonintensive outpatient treatment | 331.8 | 172.8 | 158.9 |
| State‐level insurance variables (averaged over the state‐years) | |||
| Full parity law (share) | 0.28 | — | — |
| Public insurance income eligibility threshold targeting those 6‐18 years (/100) | 2.09 | — | — |
| State‐level characteristics (averaged over the state‐years) | |||
| Health Insurance Flexibility and Accountability Medicaid waiver (share) | 0.08 | — | — |
| Affordable Care Act Medicaid expansion (share) | 0.10 | — | — |
| Institutions of Mental Disease Medicaid waiver (share) | 0.01 | ||
| Medicaid Health Home (share) | 0.05 | ||
| Block grants in $1000s for the treatment and prevention of substance use disorder (rate per 100 000 state residents) | 608 | ||
| Medical marijuana legalized (share) | 0.20 | — | — |
| Recreational marijuana legalized (share) | 0.02 | — | — |
| Prescription drug monitoring program (share) | 0.59 | — | — |
| Small business (share) | 0.37 | — | — |
| Poverty (share) | 0.13 | — | — |
| Unemployment (share) | 0.06 | — | — |
| Governor Democrat (share) | 0.43 | — | — |
| Age in years (average) | 36.7 | — | — |
| Male (share) | 0.49 | — | — |
| Female (share) | 0.51 | — | — |
| Hispanic ethnicity (share) | 0.09 | — | — |
| White (share) | 0.18 | — | — |
| African American (share) | 0.31 | — | — |
| Other race (share) | 0.27 | — | — |
| Less than high school (share) | 0.24 | — | — |
| High school (share) | 0.81 | — | — |
| Some college (share) | 0.11 | — | — |
| College graduate (share) | 0.08 | — | — |
| Fatal adult alcohol poisonings and drug overdoses (rate per 100 000 state adults) | 4377 | — | — |
| Observations | 779 | 779 | 779 |
The unit of observation is a state‐year. Data are unweighted.
We also examine possible treatment effect heterogeneity by estimating our regressions separately for states based on their preparity legal landscape. Maintaining states without a state parity law as the comparison group in both regressions, we define treatment in one sample as states adopting parity who had no legal protections for SUD treatment prelaw and in another sample as those that had some existing legal protection for these services but less than full parity.
We take several measures to examine the robustness of our findings. First, we exclude all time‐varying state‐level controls from the regression model. Second, we exclude the years in which the major ACA provisions were in effect (ie, 2014‐2017). Third, we apply population weights where the weight is the state population 12‐17 years. Fourth, we estimate a Poisson model, converting coefficient estimates to average marginal effects. Fifth, we exclude the state of Maryland as this state adopted parity before the study period. Sixth, we exclude states that do not appear to cover SUD treatment services in their CHIP plans in some years (ie, Colorado, Georgia, Pennsylvania, and Wyoming). Seventh, we control for MCO penetration within Medicaid proxied by the share of enrollees covered by a Comprehensive Risk‐based MCO (CRMCO). 71 Finally, we add TEDS years 1992‐1995 to the analysis sample and estimate parity law effects; we cannot control for public insurance as the variable is available only beginning in 1996.
Our model relies on the assumption of parallel trends in outcomes; thus, we estimate event studies to explore the extent to which our data satisfy this assumption. For the parity law variable, we estimate an event study in the spirit of Autor 72 : We construct leads and lags around the event (law adoption). For the (continuous) public insurance variable, testing parallel trends is more complicated as there is no specific event; rather, states increase (and in some cases, decrease) income eligibility thresholds. We include the policy measured the years before (t‐1) and after (t + 1) the current period (ie, a distributed lag model). 73 , 74 If we observe that the coefficient estimates on the policy leads are small in magnitude and statistically indistinguishable from zero, this pattern of results would provide suggestive evidence that our data satisfy parallel trends.
We conduct one additional test of our design. We regress each of the insurance policy variables on all other covariates included in the regression model; that is, we examine the conditional independence assumption. 75 This exercise tests whether insurance policies are conditionally balanced across treatment and comparison groups.
3. RESULTS
3.1. Summary statistics
Table 1 reports summary statistics for the full sample and samples defined by referral status: noncriminal justice referred and criminal justice referred. The average number of total admissions per 100 000 adolescents is 478. There are 114, 213, and 152 admissions per 100 000 for patients with private coverage, public coverage, and no coverage, respectively. In terms of treatment setting, an average of 77, 69, and 332 adolescents per 100 000 are admitted to residential, intensive outpatient, and nonintensive outpatient treatment per state‐year. Total admissions are roughly split between admissions not referred and referred through the criminal justice system.
During our study period, 28% of state‐year pairs have a full parity law in place and the average income threshold for public insurance eligibility is 2.09 (209% of FPL). Figure 1 displays the geographic variation in the states that passed a parity law by 2013, prior to federally mandated parity. The majority of state laws were adopted in the 2000s and span all four regions of the country. Figure 2 identifies states with public insurance eligibility thresholds above 200% FPL in four years of our study: 1996, 2002, 2009, and 2017. The average state approximately doubled its threshold over this period.
Figure 1.
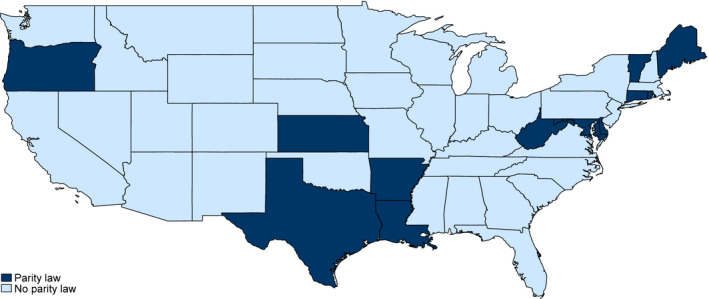
States that adopted a full parity law by 2013, before the 2014 federal parity mandate. Notes: See text for details. Alaska and Hawaii are suppressed for ease of viewing the figure, but these states did not adopt a parity law prior to the federal parity mandate. Note all states, due to the Affordable Care Act and Mental Health Parity and Addiction Equity Act, are considered full parity states over the period 2014 to 2017. We acknowledge that Rhode Island and Vermont do not appear in our analysis sample. See Table S3 [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2.
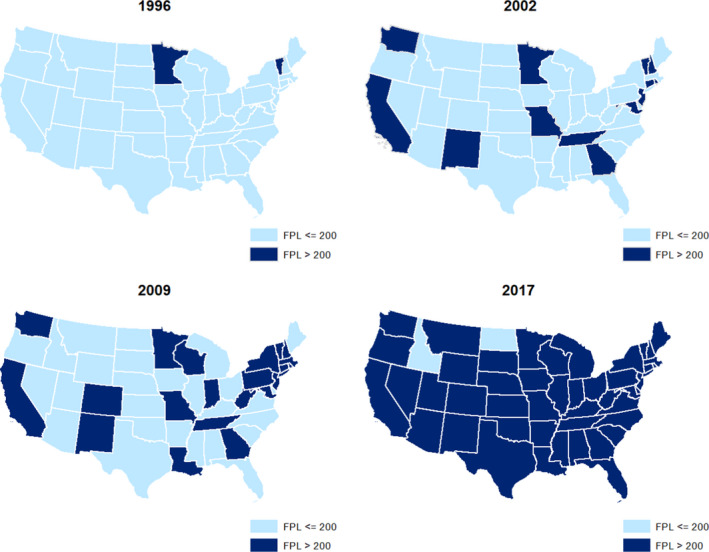
States with public insurance income eligibility thresholds for adolescents at or above 200% of the federal poverty level over the study period. Notes See text for details. Alaska and Hawaii are suppressed for ease of viewing the figure. Alaska had an income threshold below 200% of the federal poverty level in all years 1996 to 1999 and 2004 and 2017, and above that level in all other years. Hawaii had an income threshold below 200% of the federal poverty level in all years 1996 to 2000. We acknowledge that not all states appear in our sample sample. See Table S3 [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Difference‐in‐differences results
Table 2 reports results from our DD models. The first panel lists results based on the full sample of admissions, while the second two list results based on the sample not referred through the criminal justice system and referred through this system, respectively. While we will focus primarily on overall results, we note that the estimated impacts of both parity and public insurance expansions are smaller for criminal justice admissions.
Table 2.
Effect of insurance expansions on total, coverage‐specific, and treatment setting‐specific admissions rate per 100 000 adolescents: Treatment Episode Data Set (1996‐2017)
| Outcome: | Overall | Coverage type | Treatment setting | ||||
|---|---|---|---|---|---|---|---|
| Total | Private | Public | No insurance | Residential | Intensive outpatient | Nonintensive outpatient | |
| Panel A: All admissions | |||||||
| Sample mean | 478.1 | 113.8 | 212.6 | 151.7 | 77.0 | 69.3 | 331.8 |
| Full parity law | 124 (18, 231)** | 57 (2, 112)** | 91 (‒68, 250) | ‒23 (‒174, 127) | ‒1 (‒46, 45) | 26 (‒17, 68) | 99 (4, 195)** |
| Public insurance income eligibility threshold (/100) | 60 (‒56, 176) | 10 (‒32, 52) | 55 (‒20, 130) | ‒5 (‒75, 66) | 4 (‒17, 24) | 40 (7, 74)** | 16 (‒81, 113) |
| Panel B: Noncriminal justice system admissions | |||||||
| Sample mean | 247.2 | 68.5 | 109.9 | 68.8 | 42.1 | 32.3 | 172.8 |
| Full parity law | 99 (30, 168)*** | 40 (5, 75)** | 55 (‒22, 133) | 4 (‒72, 80) | 6 (‒15, 27) | 17 (1, 33)** | 76 (18, 133)** |
| Public insurance income eligibility threshold (/100) | 57 (‒22, 135) | 15 (‒18, 48) | 45 (‒2, 92)* | ‒3 (‒36, 29) | 6 (‒7, 18) | 18 (3, 34)** | 33 (‒34, 99) |
| Panel C: Criminal justice system admissions | |||||||
| Sample mean | 230.9 | 45.3 | 102.7 | 82.9 | 34.9 | 37.1 | 158.9 |
| Full parity law | 25 (‒41, 92) | 17 (‒5, 39) | 36 (‒53, 125) | ‒27 (‒111, 56) | ‒6 (‒34, 21) | 8 (‒23, 40) | 23 (‒33, 80) |
| Public insurance income eligibility threshold (/100) | 3 (‒54, 60) | ‒5 (‒24, 13) | 10 (‒30, 50) | ‒1 (‒44, 41) | ‒2 (‒11, 8) | 22 (0, 44)** | ‒17 (‒63, 29) |
The unit of observation is a state‐year. The number of observations included in each regression model is 779. Data are unweighted. All models are estimated with least squares and control for state characteristics, state fixed effects, and year fixed effects. 95% confidence intervals that account for within‐state clustering are reported in parentheses.
, **, and *statistically different from zero at the 1%, 5%, and 10% level.
Following passage of a parity law, total admissions increase by 124 per 100 000, with private admissions accounting for nearly one‐half of the increase. This implies a 25% and 50% increase relative to their sample means (all relative effect sizes are calculated in this manner henceforth) and is in line with our hypothesis of increased admissions postparity law. The estimated effects of mandates on public insurance admissions are of similar size but less precisely estimated. There is little evidence of any change among the uninsured.
The response to increases in income eligibility thresholds for public coverage appears to be more limited. While all public admissions estimates are positive as expected, only that among noncriminal justice admissions is statistically significant at the 10% confidence level. The estimates for private and no coverage are not statistically different from zero, and those for the noncriminal justice admissions are particularly close to zero.
The final three columns of Table 2 explore the effects of public and private expansions on admissions by treatment setting. Increases in admissions following parity law adoption appear to be driven by intensive and nonintensive outpatient treatment, particularly in the noncriminal justice subsample. In this subsample, admissions to intensive outpatient increase by 17 admissions per 100 000 (over 50%) and to nonintensive outpatient by 76 admissions per 100 000 (over 40%). Increases in the income eligibility threshold for public insurance are associated with statistically significant increases in intensive outpatient treatment in all three samples of more than 50%, with the criminal justice estimates suggestive of some possible substitution in outpatient care intensity from nonintensive to intensive.
3.3. Heterogeneity
The estimates for admissions effects that separately define treatment groups based on their preparity legal landscape are displayed in Table 3. The heterogeneity analysis indicates overall effects of a full parity law are more likely to be statistically distinguishable from zero using states with a prelaw policy as the treatment group as shown in Panel A. However, the size of the estimated effects on total admissions is just as large or larger in states that transitioned from no parity (but with wider confidence intervals) as shown in Panel B. This same pattern emerges for private coverage admissions in particular—a more precise (but smaller) estimated increase when transitioning from weak parity. For both treatment definitions, we continue to see an increase in publicly insured admissions when public insurance income thresholds increase, and these effects are relatively large (35%‐50%).
Table 3.
Effect of insurance expansions on total, coverage‐specific, and treatment setting‐specific admissions rate per 100 000 adolescents, with restricted treatment groups: Treatment Episode Data Set (1996‐2017)
| Outcome: | Overall | Insurance coverage type | Treatment setting | ||||
|---|---|---|---|---|---|---|---|
| Total | Private | Public | No insurance | Residential | Intensive outpatient | Nonintensive outpatient | |
| Panel A: weak parity law to strong parity law | |||||||
| All admissions | |||||||
| Sample mean | 471.3 | 107.7 | 211.2 | 152.4 | 76.3 | 67.9 | 327.1 |
| Full parity law | 119 (‒4, 242)* | 35 (‒6, 76) | 140 (‒65, 345) | ‒56 (‒228, 115) | ‒10 (‒55, 35) | 32 (‒23, 86) | 97 (‒17, 212)* |
| Public insurance income eligibility threshold (/100) | 89 (‒29, 208) | 14 (‒29, 56) | 74 (‒4, 152)* | 2 (‒66, 70) | 5 (‒18, 29) | 51 (14, 87)*** | 33 (‒66, 133) |
| Noncriminal justice admissions | |||||||
| Full parity law | 69 (‒12, 150)* | 23 (‒6, 52) | 72 (‒32, 176) | ‒27 (‒92, 39) | ‒2 (‒24, 19) | 12 (‒7, 32) | 59 (‒8, 126)* |
| Public insurance income eligibility threshold (/100) | 75 (‒5, 155)* | 18 (‒16, 51) | 54 (4, 104)** | 3 (‒23, 30) | 6 (‒8, 19) | 24 (9, 40)*** | 45 (‒24, 114) |
| Criminal justice admissions | |||||||
| Full parity law | 50 (‒1, 102)* | 12 (‒3,27) | 68 (‒37, 174) | ‒30 (‒137, 77) | ‒8 (‒36, 20) | 19 (‒18, 56) | 38 (‒19, 96) |
| Public insurance income eligibility threshold (/100) | 14 (‒46, 75) | ‒4 (‒24, 16) | 20 (‒21, 61) | ‒2 (‒45, 42) | ‒0 (‒11, 11) | 26 (2, 50)** | ‒12 (‒60, 37) |
| Panel B: no parity law to strong parity law | |||||||
| All admissions | |||||||
| Sample mean | 461.9 | 118.5 | 202.2 | 141.2 | 74.7 | 74.6 | 312.5 |
| Full parity law | 148 (‒74, 371) | 88 (‒52, 229) | ‒37 (‒163, 88) | 97 (‒103, 298) | 16 (‒58, 90) | 12 (‒30, 54) | 120 (‒40, 280) |
| Public insurance income eligibility threshold (/100) | 91 (‒31, 213) | 24 (‒17, 66) | 41 (‒36, 118) | 25 (‒45, 96) | ‒1 (‒21, 20) | 34 (0, 69)** | 57 (‒36, 150) |
| Noncriminal justice admissions | |||||||
| Full parity law | 177 (51, 302)*** | 64 (‒16, 144) | 11 (‒63, 84) | 101 (‒61, 264) | 22 (‒16, 61) | 32 (15, 48)*** | 123 (16, 229)** |
| Public insurance income eligibility threshold (/100) | 75 (‒9, 159)* | 25 (‒10, 60) | 42 (‒8, 93)* | 8 (‒26, 42) | 5 (‒8, 17) | 17 (1, 34)** | 53 (‒16, 122) |
| Criminal justice admissions | |||||||
| Full parity law | ‒28 (‒163, 106) | 24 (‒38, 86) | ‒48 (‒130, 34) | ‒4 (‒50, 41) | ‒6 (‒44, 31) | ‒19 (‒50, 11) | ‒3 (‒99, 93) |
| Public insurance income eligibility threshold (/100) | 16 (‒46, 77) | ‒0 (‒18, 17) | ‒1 (‒42, 39) | 17 (‒24, 59) | ‒5 (‒14, 4) | 17 (‒4, 38) | 4 (‒39, 47) |
The unit of observation is a state‐year. Data are unweighted. All models are estimated with least squares and control for state characteristics, state fixed effects, and year fixed effects. Panel A excludes states that transitioned to strong parity from no parity law from the analysis sample, and the number of observations included in each regression model using this sample is 719. Panel B excludes states that transitioned from partial to full parity laws from the analysis sample, and the number of observations included in each regression model using this sample is 659. See Table S1 for more details on preparity law environments. Both samples use the same comparison group of those who did not adopt parity until federally mandated in 2014. 95% confidence intervals that account for within‐state clustering are reported in parentheses.
, **, and *statistically different from zero at the 1%, 5%, and 10% level.
Table 3 also reports the same separate analyses for treatment settings. The estimated parity effect again suggests increases in nonintensive outpatient treatment and possibly intensive outpatient treatment, regardless of treatment definition. The public insurance expansions indicate their largest percent increases (and the only statistically significant ones) for intensive outpatient treatment, which increased by 50%‐80% depending on the subsample and treatment definition.
3.4. Sensitivity analysis
The results are broadly stable across the sensitivity checks that we apply. Table S5A‐B shows results without time‐varying state‐level controls. Table S6A‐B excludes the ACA Medicaid expansion years (2014‐2017). Table S7A‐B applies population weights based on state population ages 12‐17 years. The estimated effects of parity in this weighted model remain similar to the main estimates, while the estimated effects of increased public insurance eligibility thresholds on admissions by coverage type are all close to zero. Table S8A‐B displays average marginal effects from a Poisson model, which indicate similar results to the main coefficient estimates but provide stronger evidence that public insurance expansions allow substitution from nonintensive outpatient care to intensive outpatient care. Table S9A‐B shows that results without Maryland are similar to overall results but have a bit less precision. Estimates excluding states that (early in the sample period) had limited SUD coverage in their CHIP programs are shown in Table S10A‐B. Table S11A‐B reports specifications that include MCO penetration as a control variable, which is available only in 2003‐2017; the loss of the earlier years of the sample reduces power and the size of most estimates, but the effects of public insurance expansions on intensive outpatient admissions are larger and more precisely estimated than before. Table S12A‐B adds 1992‐1995 to the analysis sample (focused on parity). The results are qualitatively similar, but some estimated effect sizes are smaller and less statistically significant.
Our event study models reported in Table S13A‐C and 14A‐14C suggest broad support for the parallel trends assumption. While we note that a few policy lead variables in the parity law event studies for treatment modalities do rise to the level of statistical significance in the year before policy adoption, these estimates likely capture anticipation or ramp‐up effects rather than clear differential trends (vs. comparison states) in the most immediate preperiod, which if anything would bias our treatment effects toward zero. Similarly, the public insurance lead/lag models in Table S15A‐B shows statistical significance for only one of the lead coefficients in each table (for criminal justice admissions), supporting the lack of a systematic pretrend. Table S16 confirms that our covariates appear balanced. ACA Medicaid expansion (targeting adults) does predict public insurance generosity, but this finding likely reflects a state's overall public insurance strategy.
4. DISCUSSION
We provide evidence on the effect of US state‐level private and public insurance expansions on adolescent specialty SUD treatment use. While the insurance‐elasticity of health care is a well‐studied object within health services research, the importance of expansions for adolescent use of specialty SUD treatment has not been previously examined, suggesting that the full value of these policies has not been established. We leverage variation in coverage generated by state laws that require private insurers to cover SUD treatment “at parity” with general health care, as well as increases in children's public insurance eligibility afforded by increased Medicaid and CHIP income eligibility thresholds, over the period 1996‐2017.
Our question is timely as the US is currently in the midst of an unprecedented SUD epidemic, largely associated with opioid use. 76 Adolescents are not immune: 21% of adolescents report having used prescription opioids, and 17.9% of that group report misuse. 77 Governments are attempting to encourage SUD treatment uptake through various policy actions. 78 , 79 , 80 We test whether changes in service coverage in private markets and adolescent income eligibility thresholds impact adolescent use of SUD treatment. Understanding how insurance programs affect service use is particularly important at this time: There have been recent Congressional attempts to roll back SUD treatment provisions of the ACA, which compel insurers to cover SUD treatment, and CHIP has faced funding uncertainty throughout its history. 81 , 82 Our findings can help policy makers who are investigating these issues, in particular during the time of a widespread SUD epidemic.
We find that adoption of a state parity law increases the number of adolescents in treatment by 26% (P < .05). This increase is driven by adolescents not referred through the criminal justice system with private coverage and receiving outpatient care. We observe limited evidence that admissions increase as income thresholds for public insurance rise, though there may be some movement across treatment modalities. While our findings for parity laws are in line with our hypotheses, we note that our findings for public insurance sometimes depart from theoretical predictions. Thus, some other factor that we do not control for may play a role in our (primarily) null findings for public insurance. For example, our inability to control for utilization management in Medicaid, which has been increasing over our study period, may mute effects.
Our finding that parity effects are driven by outpatient admissions warrants further discussion. While we lack the data to explore this finding, we can offer two hypotheses. First, adolescents who gain access to SUD treatment through parity law adoption may have SUDs that are optimally treated in outpatient settings, or perhaps these adolescents or their parents/guardians have preferences for outpatient (vs. residential) treatment. For example, perhaps these adolescents had less severe SUDs that did not require inpatient treatment. Second, some residential facilities may not accept adolescents. For example, federal regulations prohibit adolescents from receiving care in facilities that offer a certified opioid treatment program. Thus, newly covered adolescents may be unable to access these settings.
Our study has limitations. First, we cannot rule out the possibility that our primarily null findings for public insurance could be attributable to lack of coverage for some modalities of SUD treatment by some CHIP programs. Second, our measure of public insurance in the TEDS includes Medicare and other public insurance, in addition to Medicaid and CHIP. Thus, we do not isolate Medicaid and CHIP in our analysis of admissions by insurance coverage, leading to measurement error. Third, we are not able to control for utilization management or privately run (but government financed) managed care in Medicaid over our study period; both of these factors have been increasingly common in Medicaid. Fourth, TEDS has limitations. For example, TEDS does not include for‐profit treatment programs in many states and reporting to TEDS may vary with economic, political, and social factors within states and over time. Finally, the dose of parity treatment may vary across the states that adopted their own state law prior to 2014 and the 32 states that were moved into parity with the ACA. The former set of laws do not impact those covered by self‐insured plans, whilte the federal mandate does.
Our study contributes new evidence to the SUD treatment and insurance literatures, offering information relevant to current decisions faced by federal and state policy makers. We show that expanding the generosity of private coverage, in terms of SUD services covered by the plans, increases adolescent SUD treatment uptake. Increasing the income eligibility threshold for two major public insurance programs (Medicaid and CHIP) among those six to 18 years, and therefore the number of adolescents eligible for these programs, does not lead to a corresponding increase in overall adolescent SUD treatment admissions but may shift treatment to intensive outpatient settings. These findings are important for understanding how insurance policies impact adolescent SUD treatment utilization.
Supporting information
Authormatrix
Appendix S1
ACKNOWLEDGEMENT
Joint Acknowledgement/Disclosure Statement: Hamersma: Syracuse University, Maclean: Temple University.
The only financial support for the paper was salary support for each others, there were no grants or contracts that supported this paper.
Hamersma S, Maclean JC. Insurance expansions and adolescent use of substance use disorder treatment. Health Serv Res.2021;56:256–267. 10.1111/1475-6773.13604
REFERENCES
- 1. Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312(5782):1900‐1902. [DOI] [PubMed] [Google Scholar]
- 2. Winters KC, Botzet AM, Fahnhorst T. Advances in adolescent substance abuse treatment. Current Psychiatry Reports. 2011;13(5):416‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson KG, Ramo DE, Cummins KM, Brown SA. Alcohol and drug involvement after adolescent treatment and functioning during emerging adulthood. Drug Alcohol Dependence. 2010;107(2):171‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark DB, Thatcher DL, Tapert SF. Alcohol, psychological dysregulation, and adolescent brain development. Alcohol Clin Exp Res. 2008;32(3):375‐385. [DOI] [PubMed] [Google Scholar]
- 5. Center for Behavioral Health Statistics and Quality . 2018 National Survey on Drug Use and Health: Methodological Summary and Definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2019. [Google Scholar]
- 6. Rajkumar AS, French MT. Drug abuse, crime costs, and the economic benefits of treatment. J Quant Criminol. 1997;13(3):291‐323. [Google Scholar]
- 7. Lu M, McGuire TG. The productivity of outpatient treatment for substance abuse. J Hum Resour. 2002;37(2):309‐335. [Google Scholar]
- 8. Murphy SM, Polsky D. Economic evaluations of opioid use disorder interventions. Pharmacoeconomics. 2016;34(9):863‐887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Center for Behavioral Health Statistics and Quality . Results from the 2018 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2019. [Google Scholar]
- 10. Dave D, Mukerjee S. Mental Health parity legislation, cost‐sharing and substance‐abuse treatment admissions. Health Econ. 2011;20(2):161‐183. [DOI] [PubMed] [Google Scholar]
- 11. Maclean JC, Popovici I, Stern ER. Health insurance expansions and providers' behavior: evidence from substance‐use‐ disorder treatment providers. J Law Econ. 2018;61(2):279‐310. [Google Scholar]
- 12. Wen H, Hockenberry JM, Cummings JR. The effect of medicaid expansion on crime reduction: evidence from hifa‐waiver expansions. J Public Econ. 2017;154(Supplement C):67‐94. [Google Scholar]
- 13. Wen H, Cummings JR, Hockenberry JM, Gaydos LM, Druss BG. State parity laws and access to treatment for substance use disorder in the united states: implications for federal parity legislation. JAMA Psychiatry. 2013;70(12):1355‐1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thalmayer AG, Harwood JM, Friedman S, et al. The mental health parity and addiction equity act evaluation study: impact on nonquantitative treatment limits for specialty behavioral health care. Health Serv Res. 2018;53(6):4584‐4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Friedman SA, Thalmayer AG, Azocar F, et al. The mental health parity and addiction equity act evaluation study: impact on mental health financial requirements among commercial “carve‐in” plans. Health Services Res. 2018;53(1):366‐388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Friedman SA, Azocar F, Xu H, Ettner SL. The mental health parity and addiction equity act (Mhpaea) evaluation study: did parity differentially affect substance use disorder and mental health benefits offered by behavioral healthcare carve‐out and carve‐in plans? Drug Alcohol Dependence. 2018;190:151‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thalmayer AG, Friedman SA, Azocar F, Harwood JM, Ettner SL. The Mental Health Parity and Addiction Equity Act (Mhpaea) evaluation study: Impact on quantitative treatment limits. Psychiat Serv. 2017;68(5):435‐442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hodgkin D, Horgan CM, Stewart MT, et al. Federal parity and access to behavioral health care in private health plans. Psychiat Serv. 2018;69(4):396‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horgan CM, Hodgkin D, Stewart MT, et al. Health plans’ early response to federal parity legislation for mental health and addiction services. Psychiat Serv. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McGinty EE, Busch SH, Stuart EA, et al. Federal parity law associated with increased probability of using out‐of‐network substance use disorder treatment services. Health Aff. 2015;34(8):1331‐1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Busch SH, Epstein AJ, Harhay MO, et al. The effects of federal parity on substance use disorder treatment. Am J Managed Care. 2014;20(1):76‐82. [PMC free article] [PubMed] [Google Scholar]
- 22. Ettner SL, Harwood J, Thalmayer A, et al. The mental health parity and addiction equity act evaluation study: impact on specialty behavioral health utilization and expenditures among “carve‐out” enrollees. J Health Econ. 2016;50:131‐143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Golberstein E, Busch SH, Zaha R, Greenfield SF, Beardslee WR, Meara E. Effect of the affordable care act's young adult insurance expansions on hospital‐based mental health care. Am J Psychiat. 2015;172(2):182‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Saloner B, Cook BL. An aca provision increased treatment for young adults with possible mental illnesses relative to comparison group. Health Aff. 2014;33(8):1425‐1434. [DOI] [PubMed] [Google Scholar]
- 25. Akosa Antwi Y, Moriya AS, Simon KI. Access to health insurance and the use of inpatient medical care: evidence from the affordable care act young adult mandate. Journal of Health Economics. 2015;39:171‐187. [DOI] [PubMed] [Google Scholar]
- 26. Saloner B, Akosa Antwi Y, Maclean JC, Cook BL. Access to health insurance and utilization of substance use disorder treatment: evidence from the affordable care act dependent coverage provision. Health Econ. 2018;27(1):50‐75. [DOI] [PubMed] [Google Scholar]
- 27. Kaiser Family Foundation . Health Insurance Coverage of Children 0–18. Oakland: Kaiser Family Foundation; 2019. [Google Scholar]
- 28. Centers for Medicare and Medicaid Services . Unduplicated Number of Children Ever Enrolled in Chip and Medicaid. Baltimore, MD: Centers for Medicare and Medicaid Services; 2017. [Google Scholar]
- 29. Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of medicaid expansion on medicaid‐covered utilization of buprenorphine for opioid use disorder treatment. Med Care. 2017;55(4):336‐341. [DOI] [PubMed] [Google Scholar]
- 30. Maclean JC, Saloner B. The effect of public insurance expansions on substance use disorder treatment: evidence from the affordable care act. J Policy Anal Manag. 2019;38(2):366‐393. [PMC free article] [PubMed] [Google Scholar]
- 31. Saloner B, Maclean JC. Specialty substance use disorder treatment admissions steadily increased in the four years after medicaid expansion. Health Aff. 2020;39(3):453‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Grooms J, Ortega A. examining medicaid expansion and the treatment of substance use disorders. AEA Papers Proc. 2019;109:187‐192. [Google Scholar]
- 33. Meinhofer A, Witman AE. The role of health insurance on treatment for opioid use disorders: evidence from the affordable care act medicaid expansion. J Health Econ. 2018;60:177‐197. [DOI] [PubMed] [Google Scholar]
- 34. Wen H, Druss BG, Cummings JR. Effect of medicaid expansions on health insurance coverage and access to care among low‐income adults with behavioral health conditions. Health Serv Res. 2015;50(6):1787‐1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Meara E, Golberstein E, Zaha R, Greenfield SF, Beardslee WR, Busch SH. Use of hospital‐based services among young adults with behavioral health diagnoses before and after health insurance expansions. JAMA Psychiatry. 2014;71(4):404‐411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maclean JC, Saloner B. Substance use treatment provider behavior and healthcare reform: evidence from Massachusetts. Health Econ. 2018;27(1):76‐101. [DOI] [PubMed] [Google Scholar]
- 37. Baicker K, Allen HL, Wright BJ, Finkelstein AN. The effect of medicaid on medication use among poor adults: evidence from Oregon. Health Aff. 2017;36(12):2110‐2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. French M, Maclean JC, Popovici I. Health Insurance and Traffic Fatalities: The Effects of Substance Use Disorder Parity Laws. Cambridge, MA: National Bureau of Economic Research, National Bureau of Economic Research Working Paper Series; 2017. [Google Scholar]
- 39. Bailey J, Blascak N. The effect of state health insurance benefit mandates on premiums and employee contributions. Appl Econ Lett. 2016;1–5. [Google Scholar]
- 40. Bailey J. The effect of health insurance benefit mandates on premiums. Eastern Econ J. 2014;40(1):119‐127. [Google Scholar]
- 41. Cutler DM, Gruber J. Does public insurance crowd out private insurance? Q J Econ. 1996;111(2):391‐430. [PubMed] [Google Scholar]
- 42. Garfield RL, Beardslee WR, Greenfield SF, Meara E. Behavioral health services in separate chip programs on the eve of parity. Adm Policy Mental Health Mental Health Serv Res. 2012;39(3):147‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Decker SL. In 2011 nearly one‐third of physicians said they would not accept new medicaid patients, but rising fees may help. Health Aff. 2012;31(8):1673‐1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wen H, Wilk AS, Druss BG, Cummings JR. Medicaid acceptance by psychiatrists before and after medicaid expansion. JAMA Psychiatry. 2019;76(9):981‐983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Substance Abuse and Mental Health Services Administration . National Expenditures for Mental Health Services and Substance Abuse Treatment, 1986–2009. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 46. Center for Behavioral Health Statistics and Quality . 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 47. Anderson DM. Does information matter? the effect of the meth project on meth use among youths. J Health Econ. 2010;29(5):732‐742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Grecu AM, Dave DM, Saffer H. Mandatory access prescription drug monitoring programs and prescription drug abuse. J Policy Anal Manag. 2019;38(1):181‐209. [PubMed] [Google Scholar]
- 49. Office of National Drug Control Policy . What America’s Users Spend on Illegal Drugs, 2000–2006. Washington, DC: Executive Office of the President; 2012. [Google Scholar]
- 50. Gfroerer J, Bose J, Trunzo D, Strashny A, Batts K, Pemberton M. Estimating Substance Abuse Treatment: A Comparison of Data from a Household Survey, a Facility Survey, and an Administrative Data Set. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 51. Center for Substance Abuse Treatment . Tip 45: Detoxification and Substance Abuse Treatment. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. [PubMed] [Google Scholar]
- 52. French MT, Homer J, Gumus G, Hickling L. Key provisions of the patient protection and affordable care act (aca): a systematic review and presentation of early research findings. Health Serv Res. 2016;51(5):1735‐1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Morrisey MA. State insurance mandates in the USA. In: Culyer AJ, ed. Encyclopedia of health economics. San Diego, CA: Elsevier; 2014:348‐351. [Google Scholar]
- 54. Medicaid.gov . Early and Periodic Screening, Diagnostic, and Treatment. Centers for Medicare and Medicaid Services;N/D. [Google Scholar]
- 55. Medicaid and CHIP Payment and Access Commission. Epsdt in Medicaid. N/D. [Google Scholar]
- 56. Pernice C, Wysen K, Riley T, Kaye N. Charting Schip: Report of the Second National Survey of the State Children’s Health Insurance Program. Portland, ME: National Academy for State Health Policy; 2001. [Google Scholar]
- 57. Pernice C, Riley T, Pelletier H, Kaye N. Charting Chip: Report of the First National Survey of the Children's Health Insurance Program. Portland, ME: National Academy for State Health Policy; 1999. [Google Scholar]
- 58. Kaye N, Pernice C, Cullen A. Charting Schip III: An Analysis of the Third Comprehensive Survey of State Children’s Health Insurance Programs. Portland, ME: National Academy for State Health Policy; 2006. [Google Scholar]
- 59. Kaiser Family Foundation . Status of State Action on the Medicaid Expansion Decision. Washington, DC: Kaiser Family Foundation; 2020. [Google Scholar]
- 60. Kaiser Commission on Medicaid and the Uninsured . Medicaid Waiver Tracker: Approved and Pending Section 1115 Waivers by State. Washington, DC: Kaiser Family Foundation; 2020. [Google Scholar]
- 61. McClellan CB, Maclean JC, Saloner B, McGinty EE, Pesko MF. Integrated care models and behavioral health care utilization: Quasi‐experimental evidence from Medicaid health homes. Health Econ. 2020;29(9):1086‐1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. ProCon.org . Legal Recreational Marijuana States and Dc. ProCon.org. 2020. [Google Scholar]
- 63. Ali MM, Dowd WN, Classen T, Mutter R, Novak SP. Prescription drug monitoring programs, nonmedical use of prescription drugs, and heroin use: evidence from the national survey of drug use and health. Addictive Behav. 2017;69:65‐77. [DOI] [PubMed] [Google Scholar]
- 64. University of Kentucky Center for Poverty Research . State Level Data of Economic, Political, and Transfer Program Information for 1980–2018. Lexington, KY: University of Kentucky Center for Poverty Research; 2020. [Google Scholar]
- 65. Flood S, King M, Ruggles S, Warren JR. Integrated Public Use Microdata Series, Current Population Survey. 4th edition. Minneapolis, MN: Integrated Public Use Microdata Series; 2020. [Google Scholar]
- 66. Centers for Disease Control and Prevention . Compressed Mortality File Underlying Cause‐of‐Death. Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 67. Small Business Administration . Firm Size Data. Small Business Administration. Small Business Administration; 2020. [Google Scholar]
- 68. Bertrand M, Duflo E, Mullainathan S. How much should we trust differences‐in‐differences estimates? Q J Econ. 2004;119(1):249‐275. [Google Scholar]
- 69. Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated Public Use Microdata Series: Version 7.0. Minneapolis, MN: University of Minnesota; 2020. [Google Scholar]
- 70. University of Kentucky Center for Poverty Research . Ukcpr National Welfare Data, 1980–2017. Lexington, KY: Gatto College of Business and Economics, University of Kentucky; 2019. [Google Scholar]
- 71. Kaiser Family Foundation . Medicaid Managed Care Market Tracker. Washington, DC: Kaiser Family Foundation; 2020. [Google Scholar]
- 72. Autor DH. Outsourcing at will: the contribution of unjust dismissal doctrine to the growth of employment outsourcing. J Labor Econ. 2003;21(1):1‐42. [Google Scholar]
- 73. Bondurant SR, Lindo JM, Swensen ID. Substance abuse treatment centers and local crime. J Urban Econ. 2018;104:124‐133. [Google Scholar]
- 74. Swensen ID. Substance‐abuse treatment and mortality. J Public Econ. 2015;122:13‐30. [Google Scholar]
- 75. Pei Z, Pischke J‐S, Schwandt H. Poorly measured confounders are more useful on the left than on the right. J Bus Econ Stat. 2018;37(2):1‐12. [Google Scholar]
- 76. Pardo B, Caulkins JP, Kilmer B, Pacula RL, Reuter P, Stein BD. The Synthetic Opioid Surge in the United States. Santa Monica, CA: RAND Corporation; 2019. [Google Scholar]
- 77. Hudgins JD, Porter JJ, Monuteaux MC, Bourgeois FT. Prescription opioid use and misuse among adolescents and young adults in the united states: a national survey study. PLoS Medicine. 2019;16(11):e1002922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. 115th Congress of the United States of America . Support for Patients and Communities Act. 2018. [Google Scholar]
- 79. 114th Congress of the United States of America . Comprehensive Addiction and Recovery Act of 2016. 2016. [Google Scholar]
- 80. Centers for Medicare & Medicaid Services . New Service Delivery Opportunities for Individuals with a Substance Use Disorder. Baltimore, MD: Centers for Medicare & Medicaid Services; 2015. [Google Scholar]
- 81. Congressional Budget Office . American Health Care Act. Washington, DC: Congressional Budget Office; 2017. [Google Scholar]
- 82. Kaiser Family Foundation . Summary of the 2018 Chip Funding Extension. Oakland: Kaiser Family Foundation; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Authormatrix
Appendix S1


