Abstract
Aims:
In response to the rapid spread of COVID-19, this paper provides health professionals with better accessibility to available evidence, summarising findings from a systematic overview of systematic reviews of the neurological symptoms seen in patients with COVID-19. Implications of so-called ‘Long Covid’ on neurological services and primary care and similarities with other neurological disorders are discussed.
Methods:
Firstly, a systematic overview of current reviews of neurological symptoms of COVID-19 was conducted. Secondly, the implications of these findings are discussed in relation to the potential effect on neurological services and the similarities in the experience of patients with COVID-19 and those with other neurological disorders. A total of 45 systematic reviews were identified within seven databases, published between 11 April 2020 and 15 October 2020, following a search in June 2020, updated on 20 October 2020.
Results:
The results indicated that COVID-19 exhibits two types of neurological symptoms; life-threatening symptoms such as Guillain–Barre Syndrome (GBS) and encephalitis, and less devastating symptoms such as fatigue and myalgia. Many of these so-called lesser symptoms appear to be emerging as longer-term for some sufferers and have been recently labelled Long Covid. When compared, these less devastating symptoms are very similar to other neurological conditions such as chronic fatigue syndrome (CFS) and functional neurological disorder (FND).
Conclusion:
Implications for neurological healthcare services in the United Kingdom (UK) may include longer waiting times and a need for more resources (including more qualified health professionals). There is also a possible change-effect on health professionals’ perceptions of other neurological conditions such as CFS and FND. Future research is recommended to explore changes in health professionals’ perceptions of neurological symptoms because of COVID-19.
Keywords: chronic fatigue syndrome, COVID-19, functional neurological disorder, Long Covid, neurological services
Introduction
As of 29 October 2020, over 44 million people worldwide have been affected by the novel coronavirus disease COVID-19.1 COVID-19 has been found to cause neurological manifestations in up to 50% of patients.2 Several systematic reviews have been conducted into the neurological symptoms of COVID-19. However, some reviews focussed purely on specific types of symptoms such as olfactory symptoms, whilst others focussed on studies only in specific countries; for example, a quarter of the studies within the reviews were undertaken in China. It was therefore deemed necessary firstly to conduct a systematic overview of previously conducted systematic reviews to summarise the neurological symptoms of COVID-19 seen so far.
Secondly, it is becoming clear that COVID-19 affects many patients neurologically and, in some cases, symptoms are persisting. A recent British Medical Journal (BMJ) webinar discussed the emergence of so-called ‘Long Covid’.3,4 This paper further discusses the concerns about the short- and long-term effects of COVID-19 on medical and holistic neurological practice, and where future resources will be required.
Thirdly, as COVID-19 is a new disease, the potential similarities with other neurological conditions have not yet been explored in the literature. The authors of this paper identified that many of the neurological symptoms of COVID-19 appear similar to the symptoms of functional neurological disorder (FND). In addition, the BMJ webinar and recent articles discussed the similarities between so-called ‘Long Covid’ and chronic fatigue syndrome (CFS), as it has become increasingly noticeable that symptoms are similar.4,5 Whilst FND is generally regarded as a psychological disorder, the authors of this paper argue that the emerging discussions about supporting patients with Long Covid should relate to other neurological disorders such as FND and CFS,6,7 questioning how these conditions are judged and how treatments are resourced for them as well as for Long Covid.
Neurological services in the United Kingdom (UK) offer diagnosis and treatment to patients with disorders of the nervous system.8 This research is therefore aimed at health professionals and commissioners in the field of neurology and in primary care in the UK. It aims to inform future service provision for those who develop long-term neurological symptoms due to COVID-19, as well as exploring the effect of COVID-19 on health professionals’ perceptions towards those with symptoms of FND.
Methods
A systematic overview of current systematic reviews was conducted to explore the potential impact of the longer-term neurological symptoms of COVID-19. The review protocol was not registered previously to avoid delay in researching and publishing findings related to COVID-19, particularly as the subject is of immediate concern. The implications of the findings of this overview were discussed, including potential effects on neurological and primary care services and on perceptions towards patients with other neurological disorders such as CFS and FND.
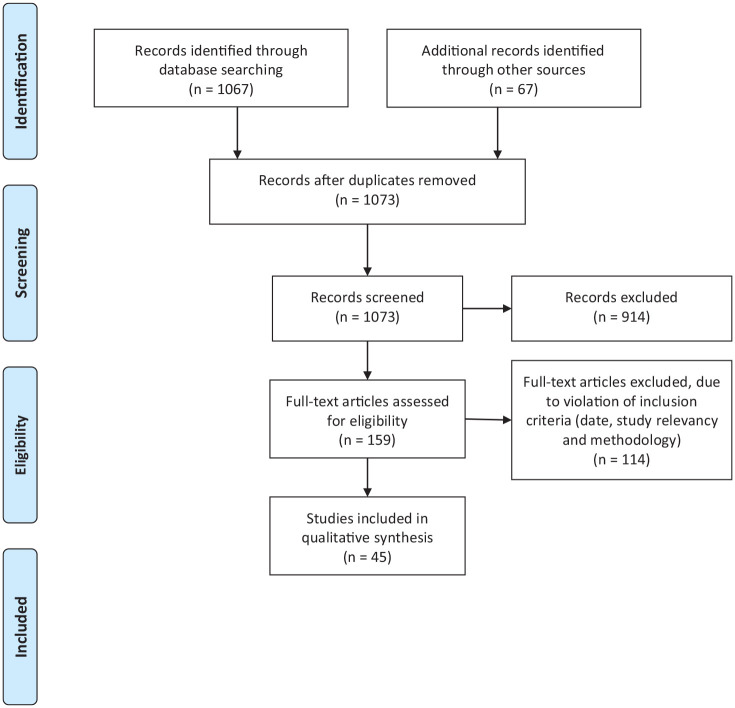
To conduct the systematic overview of systematic reviews, the recommendations outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement were followed (Figure 1).9 Following these recommendations reduces the risk of bias or selective reporting and demonstrates transparency in the process conducted. In June 2020, updated on the 20 October 2020, the following databases were searched, with date limitations between December 2019 and November 2020: ‘PubMed Central’, ‘Cochrane Database of Systematic Reviews,’ ‘Ovid’ ‘ScienceDirect’ ‘Biomed Central’ ‘BMJ’ and SAGE Journals. The following keywords within the title or abstract were used to conduct each search: ‘coronavirus’, ‘COVID-19’, ‘SARS-COV-2’, ‘neurological’, ‘nervous’ and ‘review’. For example, PubMed Central was searched using the following search terms: (((COVID-19 OR SARS-COV-2 OR coronavirus[Title]) OR (COVID-19 OR SARS-COV-2 OR coronavirus[Abstract])) AND ((neuro* OR nervous[Title]) OR (neuro* OR nervous[Abstract])) AND ((review[Title] OR (review[Abstract]))). Limitations: Date: 1 December 2019–1 September 2020. Only systematic reviews published in academic journals in English were retrieved. Reference lists of retrieved systematic reviews were also searched to ensure literature saturation.
Figure 1.
PRISMA flow diagram.
PRISMA, preferred reporting items for systematic reviews and meta-analyses.
The inclusion criteria consisted of systematic reviews only relating to neurological symptoms seen in patients with COVID-19 since 1 December 2019. Both authors participated through each step of the review independently (screening, eligibility and inclusion). Reviews were screened for relevancy against the inclusion criteria within title and abstract. Full-text reports for all potentially relevant reviews were obtained, including those where there was any uncertainty. The authors screened the full-text reports for relevancy and resolved any disagreement through discussions. Neither of the authors were blind to the journal titles, the authors’ of the reviews or institutions.
The Critical Appraisal Skills Programme (CASP) checklist for systematic reviews (2018) was used to establish the quality of each review included within this systematic overview.10 CASP does not suggest a scoring system, asking only whether each of the 10 criteria is achieved. However, for clarity the authors of this review included a ‘partly achieved’ option. All included reviews were deemed high quality, as they fulfilled at least 7 of the 10 criteria. The quality evaluation is set out in Table 1 (Supplemental Material 1). From our evaluation, 37 reviews fully achieved 9 of the 10 criteria, 7 reviews fully achieved 8 of the 10 criteria, whilst 1 review fully achieved 7 of the 10 criteria. None of the reviews met criterion eight: their findings could not be applied to a larger population as they explored predominantly specific symptoms of COVID-19 and/or its effects within a specific population.
Table 1.
Quality assessment using CASP criteria.10
| Lead author/CASP question | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Fully achieved |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdelaziz11 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Abdullahi12 | y | y | y | y | y | y | y | n | y | y | 9 |
| Abu-Rumeileh13 | y | y | y | y | y | y | y | n | y | y | 9 |
| Agyeman14 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Almqvist15 | y | y | y | y | y | y | y | n | y | y | 9 |
| Asadi-Pooya16 | y | y | partly | y | y | y | y | n | y | y | 8 |
| Bhatia17 | y | y | y | y | y | y | y | n | y | y | 9 |
| Carrillo-Larco18 | y | y | y | y | y | y | y | n | y | y | 9 |
| Ceravolo19 | y | y | y | y | y | y | y | n | y | y | 9 |
| Collantes20 | y | y | y | y | y | y | y | n | y | y | 9 |
| Correia21 | y | y | y | y | y | y | y | n | y | y | 9 |
| Di Carlo22 | y | y | y | y | y | y | y | n | y | y | 9 |
| Dinakaran23 | y | y | y | y | y | y | y | n | y | y | 9 |
| Fatima24 | y | y | y | y | y | y | y | n | y | y | 9 |
| Ghannam25 | y | y | y | y | y | y | y | n | y | y | 9 |
| Gittermann26 | y | y | y | y | y | y | y | n | y | y | 9 |
| Katal27 | y | y | y | y | y | y | y | n | y | y | 9 |
| Katyal28 | y | y | y | y | y | y | y | n | y | y | 9 |
| Leonardi29 | y | y | y | y | y | y | y | n | y | y | 9 |
| Liguoro30 | y | y | y | y | y | y | y | n | y | y | 9 |
| Montalvan31 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Narula32 | y | y | y | y | y | y | y | n | y | y | 9 |
| Nepal33 | y | y | y | y | y | y | y | n | y | y | 9 |
| Orru34 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Paliwali35 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Panda36 | y | y | y | y | y | y | y | n | y | y | 9 |
| Pinzon37 | y | y | y | y | y | y | y | n | y | y | 9 |
| Pousa38 | y | y | y | y | y | y | y | n | y | y | 9 |
| Raschetti39 | y | y | y | y | y | y | y | n | y | y | 9 |
| Rogers40 | y | y | y | y | y | y | y | n | y | y | 9 |
| Scoppettuolo41 | y | y | y | y | y | y | y | n | y | y | 9 |
| Sharifan42 | y | y | y | y | y | y | y | n | y | y | 9 |
| Taherifard43 | y | y | y | y | y | y | y | n | y | y | 9 |
| Tan44 | y | y | y | y | y | y | y | n | y | y | 9 |
| Trevisanuto45 | y | y | y | y | y | y | y | n | y | y | 9 |
| Tsai46 | y | y | y | y | y | y | y | n | y | y | 9 |
| Tsivgoulis47 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Uncini48 | y | y | y | y | y | y | y | n | y | y | 9 |
| Valiuddin49 | y | y | y | y | y | y | y | n | y | y | 9 |
| Vonck50 | y | y | y | y | y | y | y | n | y | y | 9 |
| Wang51 | y | y | y | y | y | y | y | n | y | y | 9 |
| Werner52 | y | y | y | y | y | y | y | n | y | y | 9 |
| Whittaker53 | y | y | y | partly | y | y | y | n | y | y | 8 |
| Wilson54 | y | y | partly | partly | y | y | y | n | y | y | 7 |
| Zahra55 | y | y | y | y | y | y | y | n | y | y | 9 |
Q1 Did the review address a clearly focused question? Q2 Did the authors look for the right type of papers? Q3 Do you think all the important, relevant studies were included? Q4 Did the review’s authors do enough to assess quality of the included studies? Q5 If the results of the review have been combined, was it reasonable to do so? Q6 What are the overall results of the review? (are they clear?). Q7 How precise are the results? Q8 Can the results be applied to the local population? Q9 Were all important outcomes considered? Q10 Are the benefits worth the harms and costs?
CASP, critical appraisal skills programme; n, no; y, yes.
All reviews were read in full by both authors. Microsoft Excel was used to compile a list of all the included reviews and the neurological symptoms mentioned in each. This list was completed and checked by both authors.
Next, neurological symptoms of COVID-19, CFS and FND were placed into a table to compare the symptoms, which led to a consideration of the implications for neurological healthcare services and primary care in the UK, and to the possible change-effect on perceptions towards CFS and FND.
Results
A systematic overview of systematic reviews of neurological symptoms of COVID-19
PRISMA guidelines were followed for the search strategy of the systematic overview as seen in Figure 1. The database search identified 1067 papers, with a further 67 papers identified within the reference lists of the included reviews; 61 duplicates were removed. From a total of 1073 papers, 914 were excluded after title and abstract review for relevance. The remaining 159 papers were reviewed in full. Of these, 114 were excluded as they did not meet the inclusion criteria (date, study design or methodology). Finally, 45 systematic reviews met the inclusion criteria and were included in this overview.11–55
The 45 systematic reviews were published between 11 April 2020 and 15 October 2020. The characteristics of the reviews can be seen in Table 2; the number of relevant studies reviewed within each review, the number of participants in each relevant study and the aims of each study. As mentioned, the CASP checklist was utilised to check for risk of bias in each review.
Table 2.
Characteristics of the reviews and number of studies in each country.
| First author | No. of studies referenced within each review* | No. of participants within each review* | Aim of review |
|---|---|---|---|
| Abdelaziz11 | 4 (25) | 217 (334) | This review of the literature analyses how HCoVs, in general, and SARS-CoV-2, in particular, affect the nervous system, highlights the various underlying mechanisms, addresses the associated neurological and psychiatric manifestations, and identifies the neurological risk factors involved. |
| Abdullahi12 | 60 | 10,314 (11,069) | To summarize the evidence on the neurological and musculoskeletal symptoms of the disease. This may help with early diagnosis, prevention of disease spread, and treatment planning. |
| Abu-Rumeileh13 | 52 | 58 (73) | To provide a comprehensive and updated overview of all case reports and series of COVID-19-related GBS to identify predominant clinical, laboratory, and neurophysiological patterns and to discuss the possible underlying pathophysiology. |
| Agyeman14 | 24 | 8438 | To estimate the prevalence of OGDs among patients infected with COVID-19. |
| Almqvist15 | 41 (378) | 11,509 (14,418) | To systematically summarise neurological and neuroimaging manifestations of all known HCoVs in order to provide possibilities to predict short- and long-term neurological complications of COVID-19. |
| Asadi- Pooy16 | 6 | 765 (not stated) | To discuss the evidence on the occurrence of CNS involvement and neurological manifestations in patients with COVID-19. |
| Bhatia17 | 30 | 115 | To report the characteristics of stroke in patients with COVID-19. |
| Carrillo- Larco18 | 8 | 12 | To summarise the main features of patients with GBS and COVID-19. |
| Ceravolo19 | 18 (36) | 346 (not stated) | To gather and present the current evidence informing rehabilitation of patients with COVID-19 and/or describing the consequences due to the disease and its treatment. |
| Collantes20 | 47 (49) | 6094 (6335) | To determine the neurological manifestations and complications, including laboratory findings, and outcomes among patients with COVID-19 101 infection. |
| Correia21 | 4 (7) | 329 (409) | To describe the main neurological manifestations related to coronavirus infection in humans. |
| Di Carlo22 | 19 | 6958 (12,157) | To analyse the overall rate of neurologic symptoms among COVID-19 patients. Secondary objective was to compare the results between patients with severe and non-severe infection. |
| Dinakaran23 | 31 (12) | 2552 (399) | To report the available evidence of neuropsychiatric morbidity during the current COVID-19 crisis. The authors also discuss the postulated neuronal mechanisms of the corona virus infection sequelae. |
| Fatima24 | 6 | 39 | To determine the aetiology, underlying risk factors and outcomes among patients with COVID-19 presenting with stroke. |
| Ghannam25 | 43 (42) | 314 (82) | To clarify the neurological complications of SARS-CoV-2 infection including the potential mechanisms and therapeutic options. |
| Gittermann26 | 24 | 30 | To analyse the available evidence on the symptoms of GBS associated with COVID-19 in the adult population. |
| Katal27 | 21 (28) | 681 (not stated) | To systematically review the available imaging findings of patients diagnosed with neurological symptoms associated with coronavirus infections. |
| Katyal28 | 11 | 16 | To analyse the current literature on neuromuscular complications associated with SARS-COV-2 and highlighted possible mechanisms of neuromuscular invasion. |
| Leonardi29 | 9 (29) | 510 (not stated) | To examine neurological manifestations associated with COVID-19 |
| Liguoro30 | 11 (65) | 34 (7480) | To systematically review main clinical characteristics and outcomes of SARS-CoV-2 infections in paediatric age. |
| Montalvan31 | 20 (67) | 749 | To review the neurological aspects of SARS-cov2 and other coronavirus, including transmission pathways, mechanisms of invasion into the nervous system, and mechanisms of neurological disease. |
| Narula32 | 11 | 13 | To review current literature on seizures linked with SARS-COV 2 infection |
| Nepal33 | 37 | 3152 | To inform and improve decision-making among the physicians treating COVID-19 by presenting a systematic analysis of the neurological manifestations experienced within these patients. |
| Orrù34 | 87 | 6890 | To review neurological complications of SARS-COV-2 |
| Paliwali35 | 80 | >15,858 | To focus on the neuromuscular manifestations of SARS-CoV-2 infection. |
| Panda36 | 26 | 3707 | To determine neurological manifestations of COVID-19. |
| Pinzon37 | 33 | 7113 (7559) | To conduct a systematic review and meta-analysis on the neurologic characteristics in patients with COVID-19. |
| Pousa38 | 28 | 199 | To summarize the most common extrapulmonary manifestations in paediatric patients with COVID-19, as well as to discuss clinical, epidemiological and pathophysiological aspects of these clinical presentations in children. |
| Raschetti39 | 74 | 176 | To clarify the transmission route, clinical features and outcomes of SARS-CoV-2 in neonates. |
| Rogers40 | 12 (72) | 1048 (3559) | To assess the psychiatric and neuropsychiatric presentations of SARS, MERS, and COVID-19. |
| Scoppettuolo41 | 40 (42) | 1640 (903) | To provide a clinical approach of SARS-CoV-2 neurological complications based on the direct or indirect (systemic/immune-mediated) role of the SARS-CoV-2 in their genesis. |
| Sharifan42 | 177 (208) | 17,595 (not stated) | To summarise available information regarding the potential effects of different types of CoV on the nervous system and describes the range of clinical neurological complications that have been reported thus far in COVID-19. |
| Taherifard43 | 21 (22) | 489 (57) | To systematically review the neurological complications in patients with SARS-CoV-2 infection and the methods used to diagnose both neurological complications and coronavirus infection. |
| Tan44 | 37 (39) | 4720 (135) | To characterise the clinical characteristics, neuroimaging findings and outcomes of AIS in COVID-19 patients. |
| Trevisanuto45 | 26 | 44 | To summarise currently reported neonatal cases of SARS-CoV-2 infection. |
| Tsai46 | 36 (142) | 3116 (not stated) | To review and integrate the neurologic manifestations of the COVID-19 pandemic, to aid medical practitioners who are combating the newly derived infectious disease. |
| Tsivgoulis47 | 13 (not stated) | 1641 (not stated) | To present the neurological manifestations associated with SARS-CoV-2 infection and COVID-19. We also evaluated the impact of the COVID-19 pandemic on the health care of neurological patients. |
| Uncini48 | 33 | 21 (42) | To clarify the clinical and electrophysiological phenotype, to discuss, on the basis of the available data, whether the disease mechanism could be parainfective or post-infective and to speculate on the possible pathogenesis. |
| Valiuddin49 | 26 | >61 | To update the clinical manifestations of COVID-19 concentrating on the neurological associations that have been described, including broad ranges in both central and peripheral nervous systems. |
| Vonck50 | 21 (20) | 3575 (3423) | To perform a review to describe neurological manifestations in patients with COVID-19 and possible neuro-invasive mechanisms of Sars-CoV-2. |
| Wang51 | 41 | 4345 (not stated) | To systematically collect and investigate the clinical manifestations and evidence of neurological involvement in COVID-19. |
| Werner52 | 14 (not stated) | 3351 (not stated) | To conduct a review of the reported data for studies concerning COVID-19 pathophysiology, neurological manifestations and neuroscience provider recommendations and guidelines. |
| Whittaker53 | 32 (31) | 2582 (2504) | To review the virus’ effects systemically, including that of the nervous system. |
| Wilson54 | 10 | 330 (not stated) | To evaluate and summarize the current status of the COVID-19 literature at it applies to neurology and neurosurgery. Neurological symptomatology, neurological risk factors for poor prognosis, pathophysiology for neuro-invasion, and actions taken by neurological or neurosurgical services to manage the current COVID-19 crisis are reviewed. |
| Zahra55 | 23 | 12,314 | To investigate the diagnostic value of symptoms of anosmia and dysgeusia for COVID-19. |
Many reviews referenced the same papers, in some cases reviews stated a different number of studies than were referenced within the review, some reviews did not state number of participants, or total number of participants, (number in brackets is total no. of studies/participants where the review included studies not relevant to this review, for example, reviews of symptoms of other coronaviruses, or number stated differed from no. found), when reviews differed in their report of participants numbers within the same study a consensus was assumed.
AIS, acute ischemic stroke; CNS, central nervous system; COVID-19, novel coronavirus disease 2019; GBS, Guillain–Barre syndrome; HCoV, human coronavirus; MERS, Middle East respiratory syndrome; OGD, olfactory and gustatory dysfunction; SARS, severe acute respiratory syndrome.
As can be seen in Table 2, some of the reviews explored issues outside the scope of this review. Within scope of this review, 611 studies relating to neurological symptoms of COVID-19 were reviewed within the 45 reviews. Most of the reviews included the same studies. For instance, Mao et al. was included in 30 reviews.56 Whilst numbers of participants were not always stated, more than 67,529 participants were included across the 611 studies reviewed.
Table 3 shows how many studies were carried out in each country. A quarter of the studies took place in China (107 studies with at least 27,445 participants). France, Italy, South Korea, Spain, Sweden, UK and the United States (US) also researched more than 2000 participants in each country. This gives an overview of the countries in which neurological symptoms of COVID-19 are under investigation, although it was not determined whether all participants were within the country stated. There may also be publication bias as this review excluded reviews that were not in English.
Table 3.
Number of studies and participants in each country.
| Country | Number of studies in total | Number of participants in total (where stated) | Number of studies where number of participants were not stated (within reviews) |
|---|---|---|---|
| Austria | 1 | 1 | |
| Bangladesh | 1 | 7 | |
| Belgium | 4 | 134 | |
| Brazil | 6 | 256 | 2 |
| Canada | 3 | 135 | 1 |
| China | 148 | 27,445 | 12 |
| Europe | 2 | 1837 | |
| France | 29 | 2569 | 4 |
| France/Spain | 1 | 1 | |
| France/Switzerland | 1 | 6 | |
| Germany | 11 | 188 | 1 |
| Hong Kong | 1 | 50 | |
| India | 6 | 99 | |
| Indonesia | 1 | 1 | |
| Iran | 20 | 100 | 5 |
| Israel | 2 | 170 | |
| Italy | 61 | 3708 | 7 |
| Japan | 3 | 3 | |
| Kuwait | 1 | 2 | |
| Latin America | 1 | 6 | |
| Mexico | 2 | 2 | |
| Morocco | 1 | 1 | |
| Netherlands | 4 | 447 | 1 |
| Norway | 1 | 2 | |
| Poland/USA | 1 | u/k | 1 |
| Peru | 1 | 1 | |
| Romania | 1 | 126 | |
| Russia | 1 | 1 | |
| Saudi Arabia | 2 | 2 | |
| Singapore | 1 | 870 | |
| South Korea | 5 | 3276 | |
| Spain | 24 | 5393 | 6 |
| Sudan | 1 | 1 | |
| Sweden | 2 | 2441 | |
| Switzerland | 7 | 17 | 1 |
| Thailand | 1 | u/k | 1 |
| Turkey | 11 | 176 | |
| United Arab Emirates | 2 | 1 | 1 |
| United Kingdom | 19 | 4916 | 2 |
| USA | 65 | 11,004 | 11 |
| Country not stated | 156 | 2134 | 69 |
| Total: 37 different countries (+ 3 dyads) | 611 novel studies | more than 67,529 participants | 125 studies where participants could not be counted |
Throughout the 611 studies, 18 neurological symptoms were described. These are summarised in Table 4. As can be seen, neurological manifestations of COVID-19 include catastrophic symptoms such as cerebrovascular disease (CVD), encephalitis and Guillain–Barre Syndrome (GBS), which are understandably hugely concerning and have therefore generated intense discussion and research. COVID-19 has also been found to cause symptoms such as fatigue, dizziness, ataxia, dysphagia and headache, which, although more benign, can be disabling if they become chronic.
Table 4.
Neurological symptoms of COVID-19.
| Review authors (first author) who discussed the named symptoms | Symptom | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acute CVDa | Altered Mental Statusb | Changes to smell and taste | Dizziness | Dysphagia | Encephalitisc | Fatigue | Guillain-Barre syndromed | Headache | Mental Health Issuese | Muscle Issuesf | Myelitis | Neuralgia/Polyneuropathy | Ondines Curseg | Polyneuritis Cranialis | Seizureh | Sensory Disturbancesi | Sleep issuesj | |
| Abdelaziz11 | x | x | x | x | x | x | x | x | ||||||||||
| Abdullahi12 | x | x | x | x | x | x | x | x | x | |||||||||
| Abu-Rumeileh13 | x | x | x | x | x | x | x | |||||||||||
| Agyeman14* | x* | |||||||||||||||||
| Almqvist15 | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Asadi-Pooya16 | x | x | x | x | x | x | ||||||||||||
| Bahtia17* | x* | |||||||||||||||||
| Carrillo18* | x* | |||||||||||||||||
| Ceravolo19 | x | x | x | x | x | x | x | |||||||||||
| Collantes20 | x | x | x | x | x | x | ||||||||||||
| Correia21 | x | x | x | x | x | x | x | x | x | |||||||||
| Di Carlo22 | x | x | x | x | x | |||||||||||||
| Dinakaran23 | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Fatima24* | x* | |||||||||||||||||
| Ghannam25 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Gittermann26* | x | x* | x | x | ||||||||||||||
| Katal27 | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Katyal28 | x | x | x | x | x | |||||||||||||
| Leonardi29 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Liguoro30 | x | |||||||||||||||||
| Montalvan31 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Narula32* | x | x | x | x | x | x* | ||||||||||||
| Nepal33 | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Orru34 | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Paliwali35 | x | x | x | x | x | x | x | |||||||||||
| Panda36 | x | x | x | x | x | x | x | |||||||||||
| Pinzon37 | x | x | x | x | x | x | x | x | x | |||||||||
| Pousa38 | x | x | x | x | x | |||||||||||||
| Raschetti39 | x | |||||||||||||||||
| Rogers40 | x | x | x | x | x | x | x | x | ||||||||||
| Scoppettuolo41 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Sharifan42 | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Taherifard43 | x | x | x | x | x | x | x | x | x | |||||||||
| Tan44* | x* | |||||||||||||||||
| Trevisanuto45 | x | |||||||||||||||||
| Tsai46 | x | x | x | x | x | x | x | x | x | |||||||||
| Tsivgoulis47 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Uncini48 | x | x | x | x | x | x | ||||||||||||
| Valiuddun49 | x | x | x | x | x | x | x | |||||||||||
| Vonck50 | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Wang51 | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Werner52 | x | x | x | x | x | x | x | x | x | |||||||||
| Whittaker53 | x | x | x | x | x | x | x | x | x | x | ||||||||
| Wilson54 | x | x | x | x | x | x | x | |||||||||||
| Zahara55* | x* | |||||||||||||||||
These studies specifically looked only at these symptoms.
Including strokes and blood clots thought to cause stroke.
Including confusion.
Including meningitis, encephalopathy.
Including Miller Fisher Syndrome.
Including suicidal ideation, psychosis, anxiety, depression.
Including ataxia, dystonia (specifically sustained upward gaze, dystonic bilateral leg extension, tongue deviation), hypertonia, hypotonia, myalgia, myasthenia gravis, muscle injury, muscle weakness, spasms.
Fatal respiratory failure in sleep.
Including epilepsy.
Including amblyopia.
Including insomnia.
A comparison between the neurological symptoms of COVID-19 and the most common symptoms of FND and CFS
The most common symptoms experienced by people with FND and those with CFS are compared with the neurological symptoms of COVID-19 in Table 5. The symptoms of FND and of CFS were collated from key National Health Service (NHS) sources and DSM-5.57–60 Neurological symptoms of COVID-19 include catastrophic symptoms requiring emergency care such as stroke, brain haemorrhage, encephalitis and GBS. However, 12 other neurological symptoms were shown to be similar in COVID-19 and FND and/or CFS (highlighted in Table 5). In fact, every non-catastrophic symptom of COVID-19, including the much-researched symptom of hyposmia, is also described as a symptom of FND and/or CFS. Furthermore, most of the symptoms of FND and CFS have been experienced by some people with COVID-19 neurological symptoms, particularly those with Long Covid.
Table 5.
Comparison between neurological symptoms in COVID-19, FND and CFS.
| Neurological symptoms in: | ||
|---|---|---|
| COVID-19 | FND | CFS |
| Acute CVDa | No | No |
| Encephalitisc | No | No |
| Guillain-Barre syndromed | No | No |
| Myelitis | No | No |
| Ondines Curseg | No | No |
| Polyneuritis cranialis | No | No |
| No | Bladder or bowel issues | No |
| No | No | Flu-like symptoms |
| Altered mental statusb | No | Problems thinking, remembering or concentrating |
| Dizziness | Dizziness | Dizziness |
| Dysphagia | Dysphagia | No |
| Facial pain | Facial pain & spasms | No |
| Fatigue | Fatigue | Fatigue |
| Headache | Headaches or migraines | Headaches |
| Hyposmia and/or hypogeusia | Olfactory symptoms | No |
| Mental Health Issuese | Personality changes (e.g. irritability, depression) | No |
| Muscle Issuesf | Movement disorders, limb weakness, speech symptoms (e.g. whispering, slurring or stuttering) | Muscle or joint pain |
| Neuralgia/polyneuropathy | Altered sensation (e.g. numbness, pain) | No |
| Seizureh | Altered awareness episodes (e.g. dissociative or non-epileptic seizures, faints) | No |
| Sensory disturbancesi | Visual symptoms (e.g. loss of vision, double vision, seeing flashing lights) and hearing loss | No |
| Sleep issuesj | Sleep problems | Sleep problems |
Including strokes and blood clots thought to cause strokes.
Including confusion.
Including meningitis.
Including Miller Fisher Syndrome.
Including suicidal ideation, psychosis, anxiety, depression.
Including myalgia, muscle injury, ataxia, spasms, dystonia.
Fatal respiratory failure in sleep.
Including epilepsy.
Including amblyopia.
Including insomnia.
CFS, chronic fatigue syndrome; FND, functional neurological disorder.
Discussion
From these results, this paper argues three main points: (1) COVID-19 appears to be becoming chronic for some patients, presenting similar neurological symptoms to FND and to CFS; (2) the long-term neurological effects of COVID-19 may impact neurological and wider health care services; (3) the neurological symptoms seen in COVID-19 may (and should) affect health professionals’ perceptions of FND and CFS.
Long Covid, FND and CFS present similar neurological symptoms
Long Covid, FND and CFS present similar neurological symptoms; every non-catastrophic symptom of COVID-19 (except for hypogeusia) is described as a symptom of FND and/or CFS. In addition, every symptom of FND (except bladder and bowel issues), and of CFS, (except flu symptoms and heart palpitations) have been experienced by some people with COVID-19. Notably, the main symptoms of Long Covid are increasingly similar to symptoms of CFS (fatigue, inability to concentrate, myalgia, headache).3
The impact of these findings on neurological healthcare services and primary care
Echoing concerns raised recently by the British Medical Association,7 the findings of this review highlight the impact that short- and long-term neurological symptoms of COVID-19 may have on current health services. Symptoms seen in Long Covid such as facial pain, muscle issues, neuralgia, fatigue and insomnia, may become long term and disabling, requiring sustained support from healthcare services such as pain-, fatigue- and sleep-clinics, neurological services and primary care. This is supported by other research that suggests rehabilitation required by patients following COVID-19 infection may be ‘very much along the same lines as existing services but with double the demand’.61 Consultant-led neurological services such as chronic fatigue clinics and headache clinics are already overstretched, with a shortage of neurology consultants and long waiting lists.62 Neurological symptoms of Long Covid may increase demand for these clinics and may indicate a need for more qualified health professionals and specialists in neurology. The effects of COVID-19 on these services is hard to predict, as the neuropathy, myopathy and sensory deficits of SARS resolved within 3 months of recovery.46 However, as COVID-19 appears to be becoming Long Covid for up to 10% of patients,3 support is likely to be required, potentially for a significant number of people, if their symptoms do not resolve spontaneously.
Additionally, COVID-19 is causing a wider impact on patient populations. For example, COVID-19 has affected delivery of health care services, through reduction in use of emergency services during the peak of the pandemic in the UK as patients were worried about contracting the virus from hospitals.63 There is evidence that some patients with long-term conditions have improved their self-care techniques, such as better use of medication and alternative therapies such as physiotherapy, cognitive behavioural therapy, and exercise. On the other hand, most outpatient appointments and elective surgeries were postponed, leading in some cases to deaths as an indirect result of COVID-19.64 There are now questions about whether there will be a rebound in demand, potentially overwhelming NHS services, or whether the reduction in demand can be sustained. Combined with the previously mentioned potential increase in demand for neurological services, there are likely to be wide reaching financial implications. This research is therefore useful for aiding future patient management while helping to develop policies for response to COVID-19 and its critical outcomes.
The effect of COVID-19 on perceptions of FND and CFS
Key sources differ in their description of FND symptoms, indicating that there is no comprehensive list of all FND symptoms.57–60 It is likely that this contributes to health professionals’ uncertainty in diagnosing FND.65 In addition, patients with both FND and CFS have experienced many years of scepticism from health professionals with negative consequences,5 including lack of support and poor access to services often contributing to poor mental health.66 In addition, lower value is given to health professionals’ role in managing poorly defined symptoms.67 FND and CFS, alongside other ambiguous uncertain conditions (e.g. fibromyalgia), are considered amongst the lowest conditions on the hierarchy of importance of conditions.68
Conversely, COVID-19 can be diagnosed quickly and easily with a test (leaving aside the possibilities of false results). The authors of this research are concerned that, within neurological services, priority may be given to patients who have had COVID-19, who may actually experience some level of prestige because they have survived a disease feared by all, and any neurological symptoms they experience might be automatically accepted, extensively researched and supported, to the detriment of other neurological conditions. There is already evidence of this skewing of services, as large sums of money and research at pace are contributing to a greater understanding of long-term symptoms of COVID-19,69 and the NHS has declared its intention to provide a COVID-19 rehabilitation service.6 Also, there is indication that the presence of Long Covid is unquestionably ‘believed’ by health professionals, as doctors and other professionals have written about their experiences with it and are recommending each other’s papers.3,5
However, some patients with emerging Long Covid have similar experiences to those with less accepted conditions, particularly those who were unable to get a test early in the pandemic.70 Patients feel doctors dismiss their symptoms, they feel desperate and disagree with diagnoses of anxiety. As Garner (2020) explained: ‘Doctors need to stop diagnosing this as anxiety. We have messed up before, let’s not do it again with long-term covid-19 illness.’5
It is important to highlight the similarities between symptoms of Long Covid and other conditions, providing education for health professionals, informing future practice and illustrating the need for more funding for neurological services to meet increased demand. Whilst research and services for COVID-19 are gaining funding, there is a lack of funding and research into understanding, treatment and support for those who suffer from FND and CFS.71 FND and CFS are likely to have lower prestige than COVID-19; however, the realisation that COVID-19 causes neurological symptoms similar to FND and CFS may lead to a potential shift in perceptions towards these conditions. They may be taken more seriously, and more funding may be made available for appropriate neurological services unrelated to the cause of the symptoms.
Limitations
Scientific reports centred on neurological effects of COVID-19 are still scarce, and risk of publication bias is high. For example, within the reviews included in this research, a quarter of the studies were undertaken in China (148) and a further quarter in Europe (179). Only three studies were conducted in the African continent and nine were conducted in the South American continent. Despite the status of COVID-19 as a pandemic, research into the neurological effects of COVID-19 so far has not been conducted worldwide.
This systematic review is grounding its results on previous reviews’ findings; thus, it is difficult to assess how reliable some of these results can be, for example many of the reviews (156) did not state the source country of their findings. Quality assessment has, however, been undertaken as described earlier and the reviews were deemed high quality. Retrospective and prospective studies of larger cohorts are necessary to correctly assess nervous system involvement, which has not been possible yet for COVID-19 as it is a very new disease and it is unclear how much it mimics other coronavirus diseases.
Conclusion and implications for future research
There is an array of evidence to show that COVID-19 causes neurological symptoms and, although it is difficult to ascertain how long term the symptoms may become, there is increasing evidence of the presence of Long Covid, symptoms persisting beyond 3 months. Although this paper is primarily UK-focussed, these concerns are likely to be similar in other countries. This research collates the evidence so far and provides insight into the neurological effects of COVID-19 in relation to FND symptoms. Concerns about the potential impact of these findings on the delivery of neurological and wider healthcare services are considered alongside the potential effect COVID-19 may have on perceptions of neurological symptoms, particularly those relating to FND and CFS. Further research is recommended to explore whether the neurological symptoms of COVID-19 will improve acceptance and understanding of FND, or whether this will worsen the experience for those who suffer from FND. Further thought for future planning of health care resources also needs to be taken into consideration in light of this pandemic.
Supplemental Material
Supplemental material, sj-pdf-1-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-2-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-3-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-4-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-5-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Footnotes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Tamar Wildwing  https://orcid.org/0000-0002-3685-701X
https://orcid.org/0000-0002-3685-701X
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Tamar Wildwing, Faculty of Health and Wellbeing, Canterbury Christ Church University Ringgold Standard Institution, North Holmes Road, Canterbury, UK.
Nicole Holt, Faculty of Health and Wellbeing, Canterbury Christ Church University Ringgold Standard Institution, Canterbury, Kent, UK.
References
- 1. John Hopkins University & Medicine and Coronavirus Resource Centre. COVID-19 data in motion, https://coronavirus.jhu.edu/ (2020).
- 2. Stevens R. How does coronavirus affect the brain? https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/how-does-coronavirus-affect-the-brain (2020).
- 3. Greenhalgh T, Knight M, A’Court C, et al. Management of post-acute covid-19 in primary care. BMJ 2020; 370: m3026. [DOI] [PubMed] [Google Scholar]
- 4. Nabavi N. Long covid: how to define it and how to manage it. BMJ 2020; 370: m3489. [DOI] [PubMed] [Google Scholar]
- 5. Garner P. Covid-19 at 14 weeks—phantom speed cameras, unknown limits, and harsh penalties, https://blogs.bmj.com/bmj/2020/06/23/paul-garner-covid-19-at-14-weeks-phantom-speed-cameras-unknown-limits-and-harsh-penalties/2020 (2020).
- 6. Mahase E. Covid-19: what do we know about “long covid”? BMJ 2020; 370: m2815. [DOI] [PubMed] [Google Scholar]
- 7. Rimmer A. Covid-19: impact of long-term symptoms will be profound, warns BMA. BMJ 2020; 370: m3218. [DOI] [PubMed] [Google Scholar]
- 8. Guys and St Thomas National Health Service (NHS) Foundation Trust. Neurological services, https://www.guysandstthomas.nhs.uk/our-services/neurology/overview (2020).
- 9. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 10. Critical Appraisal Skills Programme. CASP checklist for systematic reviews, https://casp-uk.net/wp-content/uploads/2018/01/CASP-Systematic-Review-Checklist_2018.pdf
- 11. Abdelaziz O, Waffa Z. Neuropathogenic human coronaviruses: a review. Rev Med Virol 2020; 30: e2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abdullahi A, Candan S, Abba M, et al. Neurological and musculoskeletal features of COVID-19: a systematic review and meta-analysis. Front Neurol 2020; 11: 687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abu-Rumeileh S, Abdelhak A, Foschi M, et al. Guillain-Barré syndrome spectrum associated with COVID-19: an up-to-date systematic review of 73 cases. Neurol. Epub ahead of print 25 August 2020. DOI: 10.1007/s00415-020-10124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Agyeman AA, Chin KL, Landersdorfer CB, et al. Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin Proc 2020; 95: 1621–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Almqvist J, Granberg T, Tzortzakakis A, et al. Neurological manifestations of coronavirus infections - a systematic review. Ann Clin Transl Neurol. Epub ahead of print 27 August 2020. DOI: 10.1002/acn3.51166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci 2020; 413: 116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bhatia R, Pedapati R, Komakula S, et al. Stroke in coronavirus disease 2019: a systematic review. J Stroke 2020; 22: 324–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carrillo-Larco RM, Altez-Fernandez C, Ravaglia S, et al. COVID-19 and Guillain-Barre syndrome: a systematic review of case reports. Wellcome Open Res 2020; 5: 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ceravolo MG, Arienti C, De Sire A, et al.; International Multi-professional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and Covid-19: the cochrane rehabilitation 2020 rapid living systematic review. Eur J Phys Rehabil Med. Epub ahead of print 24 July 2020. DOI: 10.23736/S1973-9087.20.06501-6. [DOI] [Google Scholar]
- 20. Collantes MEV, Espiritu AI, Sy MCC, et al. Neurological manifestations in COVID-19 infection: a systematic review and meta-analysis. Can J Neurol Sci. Epub ahead of print 15 July 2020. DOI: 10.1017/cjn.2020.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Correia A, Feitosa P, de Sousa Moreira J, et al. Neurological manifestations of COVID-19 and other coronaviruses: a systematic review. Neurol Psychiat Br 2020; 37: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Di Carlo DT, Montemurro N, Petrella G, et al. Exploring the clinical association between neurological symptoms and COVID-19 pandemic outbreak: a systematic review of current literature. J Neurol. Epub ahead of print 1 August 2020. DOI: 10.1007/s00415-020-09978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dinakaran D, Manjunatha N, Naveen Kumar C, et al. Neuropsychiatric aspects of COVID-19 pandemic: a selective review. Asian J Psychiatr 2020; 53: 102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fatima N, Saqqur M, Qamar F, et al. Impact of COVID-19 on neurological manifestations: an overview of stroke presentation in pandemic. Neurol Sci 2020; 41: 2675–2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ghannam M, Alshaer Q, Al-Chalabi M, et al. Neurological involvement of coronavirus disease 2019: a systematic review. J Neurol. Epub ahead of print 19 June 2020. DOI: 10.1007/s00415-020-09990-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trujillo Gittermann LM, Valenzuela Feris SN, von Oetinger Giacomanc A. Relation between COVID-19 and Guillain-Barré syndrome in adults: a systematic review. Neurolgia. Epub ahead of print 24 July 2020. DOI: 10.1016/j.nrl.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Katal S, Balakrishnan S, Gholamrezanezhad A. Neuroimaging and neurologic findings in COVID-19 and other coronavirus infections: a systematic review in 116 patients. Neuroradiol. Epub ahead of print 27 June 2020. DOI: 10.1016/j.neurad.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Katyal N, Narula N, Acharya S, et al. Neuromuscular complications with SARS-COV-2 infection: a review. Front Neurol 2020; 11: 1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Leonardi M, Padovani A, McArthur JC. Neurological manifestations associated with COVID-19: a review and a call for action. J Neurol 2020; 267: 1573–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liguoro I, Pilotto C, Bonanni M, et al. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr 2020; 79: 1029–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Montalvan V, Lee J, Bueso T, et al. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg 2020; 194: 105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Narula N, Joseph R, Katyal N, et al. Seizure and COVID-19: association and review of potential mechanism. Neurol Psychiatry Brain Res 2020; 38: 49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nepal G, Rehrig JH, Shrestha GS, et al. Neurological manifestations of COVID-19: a systematic review. Crit Care 2020; 24: 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Orrù G, Conversano C, Malloggi E, et al. Neurological complications of COVID-19 and possible neuroinvasion pathways: a systematic review. Int J Environ Res Public Health 2020; 17: 6688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Paliwali V, Garg R, Gupta A, et al. Neuromuscular presentations in patients with COVID-19. Neurol Sci 2020; 41: 3039–3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Panda PK, Sharawat IK, Panda P, et al. Neurological complications of SARS-CoV-2 infection in children: a systematic review and meta-analysis. J Trop Pediatr. Epub ahead of print 10 September 2020. DOI: 10.1093/tropej/fmaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pinzon R, Wijaya V, Buana R. Neurologic characteristics in coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Front Neurol 2020; 11: 565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pousa P, Mendonça T, Oliveira E, et al. Extrapulmonary manifestations of COVID-19 in children: a comprehensive review and pathophysiological considerations. J Pediatr (Rio J). Epub ahead of print 22 September 2020. DOI: 10.1016/j.jped.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Raschetti R, Vivanti A, Vauloup-Fellous C, et al. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat Commun 2020; 11: 5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020; 7: 611–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Scoppettuolo P, Borrelli S, Naeije G. Neurological involvement in SARS-CoV-2 infection: a clinical systematic review. Brain Behav Immun Health 2020; 6: 100094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sharifian-Dorchea M, Huota P, Osherova M, et al. Neurological complications of coronavirus infection; a comparative review and lessons learned during the COVID-19 pandemic. J Neurol Sci 2020; 417: 117085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Taherifard E, Taherifard E. Neurological complications of COVID-19: a systematic review. Neurol Res. Epub ahead of print 23 July 2020. DOI: 10.1080/01616412.2020.1796405. [DOI] [PubMed] [Google Scholar]
- 44. Tan Y-K, Goh C, Leow AST, et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis 2020; 50: 587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Trevisanuto D, Cavallin F, Cavicchiolo ME, et al. Coronavirus infection in neonates: a systematic review. Arch Dis Child Fetal Neonatal Ed. Epub ahead of print 17 September 2020. DOI: 10.1136/archdischild-2020-319837. [DOI] [PubMed] [Google Scholar]
- 46. Tsai S, Lu M, San S, et al. The neurologic manifestations of coronavirus disease 2019 pandemic: a systemic review. Front Neurol 2020; 19: 498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tsivgoulis G, Palaiodimou L, Katsanos A, et al. Neurological manifestations and implications of COVID-1 9 pandemic. Ther Adv Neurol Diso 2020; 13: 1756286420932036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Uncini A, Vallat J, Jacobs B. Guillain-Barré syndrome in SARS-CoV-2 infection: an instant systematic review of the first six months of pandemic. J Neurol Neurosurg Psychiatry. Epub ahead of print 27 August 2020. DOI: 10.1136/jnnp-2020-324491. [DOI] [PubMed] [Google Scholar]
- 49. Valiuddun H, Kalajdzic A, Rosati J, et al. Update on neurological manifestations of SARS-CoV-2. West J Emerg Med. Epub ahead of print 6 October 2020. DOI: 10.5811/westjem.2020.8.48839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vonck K, Garrez I, De Herdt V, et al. Neurological manifestations and neuro-invasive mechanisms of the severe acute respiratory syndrome coronavirus type 2. Eur J Neurol 2020; 27: 1578–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang L, Shen Y, Li M, et al. Clinical manifestations and evidence of neurological involvement in 2019 novel coronavirus SARS-CoV-2: a systematic review and meta-analysis. J Neurol. Epub ahead of print 11 June 2020. DOI: 10.1007/s00415-020-09974-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Werner C, Scullen T, Mathkour M, et al. Neurological impact of coronavirus disease (COVID-19): practical considerations for the neuroscience community. World Neurosurg 2020; 139: 344–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Whittaker A, Anson M, Harky A. Neurological manifestations of COVID-19: a systematic review and current update. Acta Neurol Scand 2020; 142: 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wilson MP, Jack AS. Coronavirus disease (COVID-19) in neurology and neurosurgery: a scoping review of the early literature. Clin Neurol Neurosurg 2020; 193: 105866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zahra SA, Iddawela S, Pillai K, et al. Can symptoms of anosmia and dysgeusia be diagnostic for COVID-19? Brain Behav. Epub ahead of print 16 September 2020. DOI: 10.1002/brb3.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020; 77: 683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Patient Info. Functional Neurological Disorder (FND), https://patient.info/brain-nerves/functional-neurological-disorder (acessed 13 September 2020).
- 58. National Health Service (NHS). Medically unexplained symptoms, https://www.nhs.uk/conditions/medically-unexplained-symptoms/ (accessed 13 September 2020).
- 59. Neurosymptoms.org. Functional Neurological Disorder (FND): a patient’s guide, https://www.neurosymptoms.org/ (accessed 13 September 2020).
- 60. Black D, Grant J. DSM-5® guidebook: the essential companion to the diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association Publishing, 2014, pp.201–215. [Google Scholar]
- 61. Thornton J. Covid-19: the challenge of patient rehabilitation after intensive care. BMJ 2020; 369: m1787. [DOI] [PubMed] [Google Scholar]
- 62. National Health Service (NHS) England. Transforming elective care services neurology: learning from the elective care development collaborative, https://www.england.nhs.uk/wp-content/uploads/2019/07/neurology-elective-care-handbook.pdf (accessed 1 June 2020).
- 63. The Kings Fund. Restarting health and care services will take months, www.kingsfund.org.uk/press/press-releases/restarting-health-and-care-services-will-take-many-months (accessed 1 June 2020).
- 64. Vaughan L. Where are the patients? The factors affecting the use of emergency care during COVID-19; Nuffield Trust. www.nuffieldtrust.org.uk/news-item/where-are-the-patients-the-factors-affecting-the-use-of-emergency-care-during-covid-19 (accessed 5 July 2020).
- 65. Canna M, Seligman R. Dealing with the unknown. Functional neurological disorder (FND) and the conversion of cultural meaning. Soc Sci Med 2020; 246: 112725. [DOI] [PubMed] [Google Scholar]
- 66. Robson CM, Lian OS. “Are you saying she’s mentally ill then?” Explaining medically unexplained seizures in clinical encounters. In: Forum Qualitative Sozial for schung/Forum: Qualitative Social Research 2015; 17: 1. (accessed 1 September 2020). [Google Scholar]
- 67. Marshall M. Redefining quality: valuing the role of the GP in managing uncertainty. Br J Gen Pract 2016; 66: e146–e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Album D, Westin S. Do diseases have a prestige hierarchy? A survey among physicians and medical students. Soc Sci Med 2008; 66: 182–188. [DOI] [PubMed] [Google Scholar]
- 69. National Institute of Health Research (NIHR). Major study into long term health effects of Covid-19 launch in the UK, https://www.nihr.ac.uk/news/major-study-into-long-term-health-effects-of-covid-19-launched-in-the-uk/25200 (accessed 1 September 2020).
- 70. Alwen NA. What exactly is mild covid-19? BMJ opinion, https://blogs.bmj.com/bmj/2020/07/28/nisreen-a-alwan-what-exactly-is-mild-covid-19/ (2020) (accessed 1 September 2020).
- 71. Nitkunan A, Lawrence J, Reilly MM. Neurology workforce survey conducted by the association of British neurologists. 2020; pp. 1–19. https://cdn.ymaws.com/www.theabn.org/resource/collection/219B4A48-4D25-4726-97AA-0EB6090769BE/2020_ABN_Neurology_Workforce_Survey_2018-19_28_Jan_2020.pdf (accessed 1 September 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-2-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-3-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-4-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease
Supplemental material, sj-pdf-5-taj-10.1177_2040622320976979 for The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services by Tamar Wildwing and Nicole Holt in Therapeutic Advances in Chronic Disease