Abstract
Background
Pain continues to be an important public health concern, especially given the opioid crisis in industrialized countries. It is important to understand the association between emotions such as fear and anxiety and the experience of pain as both a physiological and affective experience. Fear or anxiety about pain is in fact a well-known predictor of and close associate of pain. Nociception and pain history differ depending on age, yet little empirical evidence exists on how fear of pain varies over the life span. The purpose of this study was to provide a cross-sectional examination of the relations between age and fear of pain across the adult life span.
Methods
Using cross-sectional data from 4,122 participants who completed the Fear of Pain Questionnaire-9, structural equation modeling and regression techniques were used to examine the association between fear of pain and age.
Results
A positive linear association was discovered between age and fear of severe or minor pain, and a negative association was discovered between age and fear of medical or dental pain. Quadratic and cubic relations were also significant for fear of severe pain, fear of medical and dental pain, and overall fear of pain, but not for fear of minor pain.
Conclusions
Unique trajectories for different components of pain-related fear exist across the adult life span and may be affected by increased exposure to medical and dental experiences over time and by the awareness of a greater likelihood of experiencing pain later in the life span.
Keywords: Fear of Pain, Development, Age, Health Psychology, Pain
Introduction
As both a sensory and an emotional experience, the topic of pain is transdisciplinary, with many professional specialty groups collaborating to understand its etiology, treatment, and implications throughout the life course [1]. Variability of pain across age groups could be due, in part, to changing pain thresholds related to development and aging [2], different perceptions and reporting of pain across the life span [3, 4], increasing experience with pain as one ages [5] or, in research, the method of pain induction (e.g., pressure, suprathreshold, spatial vs temporal summation) [2]. Further exploration is necessary to ascertain the effects of age on pain in an attempt to facilitate helping individuals with pain in every stage of life. Studying the emotional aspects of the pain experience [1] presents at least one way to elucidate the experience of pain throughout life. The literature examining pain-related fear in relation to age differences and pain is sparse. Thus, continuing to examine the role of negative affect, including fear of pain across the adult life span, is important.
Fear and anxiety related to pain have been operationalized as constructs distinct from, yet interacting with and affected by, pain [6]. Fear and anxiety about pain can be described as the verbal, physiological, and overt behavior responses to potential or anticipated painful experiences [7, 8]. The fear avoidance model [9] has long been presented as a conceptual way to understand the role of fear in relation to pain. When pain occurs and is perceived as threatening (i.e., fear or anxiety inducing), that fear and anxiety can result in a “vicious cycle” [9] in which they lead to avoidance of adaptive behaviors and a hypervigilance toward pain-related sensations, which then maintain the pain-related fear and anxiety [9]. At present, the fear avoidance model does not, however, include a developmental component. That is, a dearth of research exists to explicate how fear and anxiety about pain change with age. Further understanding in this area may help to better understand the complex relations among age, fear of pain, and pain more broadly. Thus, this study was designed to explore and characterize the developmental association between age and pain-related fear and anxiety [1].
Methods
Participants and Procedure
Six existing archival data sets collected between the years of 1984 and 2017 including individual fear of pain data (n=3,294), along with a new supplement of participants (n=828) from Amazon’s Mechanical Turk (MTurk; www.mturk.com), were used to provide a robust sample (N=4,122). The archival data sets included the Fear of Pain Questionnaire-9 (FPQ-9) validation sample of undergraduate psychology students from two institutions (Oklahoma State University and West Virginia University) and chronic pain patients [6], adult participants from a population-based health study in Appalachia [10], a sample of dental patients in an oral diagnosis clinic [11], and two national samples from a previous study about oral health values that also used MTurk [12]. Each of these studies included data from different time periods and were cross-sectional in nature. The new data were collected via MTurk as part of a larger study of psychosocial correlates of oral health and disease. The psychometrics, including reliability, internal and external validity, and general acceptance of MTurk data, have been addressed elsewhere [13, 14]. MTurk has been shown to be a reputable alternative to and, depending on the research question, better than other traditional data collection methods (e.g., college samples) [13, 14]. TurkPrime [15], a software that helps automate MTurk, was also used in this study. This study was reviewed and approved by the institutional review board (No. 170870501) at West Virginia University and included written informed consent, as required.
Measures
Each of the archival data sets included age and gender as variables. Other demographic variables (i.e., race or ethnicity, income, education) were available and used for descriptive purposes. The new MTurk data set also included demographics of age, gender, race or ethnicity, income, and education.
Fear of Pain Questionnaire-9
The FPQ-9 [6] is a short form of the Fear of Pain Questionnaire-III (FPQ-III) [16] (its parent version) and includes three subscales: Fear of Severe Pain, Fear of Minor Pain, and Fear of Medical/Dental Pain. A number of studies in a variety of cultural and contextual contexts have examined both the FPQ-III and the FPQ-9 [17–20]. Data from the FPQ-9 have suggested good reliability (coefficient α = 0.72–0.94) and have produced evidence for adequate overall construct validity [6].
Validity Items
Given the importance of age for this study, four questions intended to ensure valid responses to age were included in the MTurk survey. Participants also reported age in three formats (i.e., in years twice and birth year once). If any discrepancy was found, that participant was excluded.
Data Analyses
A multi-tiered analytic approach was used to examine the association between age and pain-related fear. Analyses included structural equation models (SEMs) and ordinary least-squares regression models. Basic assumptions in SEMs are the same as in multiple linear regressions—namely, normality of data, independence of data, relatively equal variances, no evidence of extreme multicollinearity, and linearity of data [21]. Assumptions for the data were checked using basic descriptive analyses, frequency counts, and histograms.
Descriptive Statistics
Descriptive statistics were included to describe gender, age, race or ethnicity (where available), income (where available), education (where available), and the type of sample (e.g., undergraduate students, chronic pain patients, MTurk). Only participants from the MTurk study (originally n=1,033) who responded appropriately to validity items were included in the final analyses (n=828).
Structural Equation Models
To examine the relation between fear of pain and age, a confirmatory factor analysis (CFA) of the FPQ-9 subscales (i.e., Fear of Severe Pain, Fear of Minor Pain, and Fear of Medical/Dental Pain) was first conducted. The FPQ-9 subscales were then regressed on age and gender. A second SEM was conducted with total FPQ-9 scores modeled as a higher-order latent variable regressed on age and gender. SEM analyses were conducted using Mplus version 8.0 [22]. After the model was assessed linearly, age was squared and analyzed as a quadratic term and then cubed and analyzed as a cubic term to assess the possible curvilinearity of the relationship between fear of pain and age. Due to issues of variances for age after squaring and cubing it, the quadratic or cubic models could not be estimated. Instead, four separate ordinary least-squares regressions (one for each FPQ-9 subscale and one for the total score) were conducted with quadratic and cubic terms in SPSS version 25.0 (IBM, Armonk, New York) as observed rather than latent variables.
Results
Descriptive Statistics
Table 1 lists the descriptive statistics for each of the data sets, including archival data, new MTurk data, and the combined data. Overall, the total sample (N=4,122) had a mean age of 37.6 (SD = 14.0; range, 18–98) and included 2,427 women (58.9%) and 1,682 men (40.8%). The overall means were 24.0 (SD = 7.4; range, 9–45) for the total FPQ-9 score, 10.2 (SD = 3.4; range, 3–15) for the Fear of Severe Pain subscale, 6.2 (SD = 2.5; range, 3–15) for the Fear of Minor Pain subscale, and 7.7 (SD = 3.0; range, 3–15) for the Fear of Medical/Dental Pain subscale. For information on assumptions and missing data, as well as a table detailing the number of participants at each age, see the Supplementary Data.
Table 1.
Descriptive information for various archival data sets included in study
| Data Set | n | Gender, n (%) | Age Range, M (SD) | Race or Ethnicity, n (%) | ||
|---|---|---|---|---|---|---|
| Center for Oral Health Research in Appalachia (COHRA) [10] | 1,195 | Women | 762 (63.8%) | 18–81, 34.4 (9.5) | White | 1,061 (88.8%) |
| Men | 433 (36.2%) | African American | 100 (8.4%) | |||
| Asian American | 3 (0.3%) | |||||
| Hispanic or Latino | 9 (0.8%) | |||||
| Native American | 2 (0.2%) | |||||
| Other or multiracial | 7 (0.6%) | |||||
| Oral Health Values 1 [12] | 301 | Women | 175 (58.1%) | 21–70, 39.7 (11.9) | White | 226 (75.1%) |
| Men | 125 (41.1%)* | African American | 36 (12.0%) | |||
| Asian American | 24 (8.0%) | |||||
| Hispanic or Latino | N/A | |||||
| Native American | N/A | |||||
| Other or multiracial | 15 (5.0%) | |||||
| Oral Health Values 2 [12] | 307 | Women | 163 (53.1%) | 18–98, 36.0 (12.1) | White | 256 (83.4%) |
| Men | 142 (46.3%)† | African American | 24 (7.8%) | |||
| Asian American | 16 (5.2%) | |||||
| Hispanic or Latino | N/A | |||||
| Native American | 2 (0.7%) | |||||
| Other or multiracial | 9 (3.0%) | |||||
| FPQ-9 Development [6] | 826 | Women | 486 (58.8%) | 18–85, 31.9 (15.8) | White | 268 (93.1%)‡ |
| Men | 333 (40.3%)§ | African American | 11 (3.8%) | |||
| Asian American | 3 (1.0%) | |||||
| Hispanic or Latino | N/A | |||||
| Native American | 2 (0.7%) | |||||
| Other | 1 (0.3%) | |||||
| Oral Diagnosis [11] | 665 | Women | 353 (53.1%) | 18–90, 37.4 (15.0) | White | 614 (92.3%) |
| Men | 309 (46.5%)¶ | African American | 30 (4.5%) | |||
| Asian American | 6 (0.9%) | |||||
| Hispanic or Latino | 4 (0.6%) | |||||
| Native American | 4 (0.6%) | |||||
| Other | 7 (1.1%) | |||||
| New Valid MTurk | 828 | Women | 488 (58.9%) | 18–82, 48.0 (12.7) | White | 671 (81.0%) |
| Men | 340 (41.1%) | African American | 75 (9.1%) | |||
| Asian American | 46 (5.6%) | |||||
| Hispanic or Latino | 38 (4.6%) | |||||
| Native American | 16 (1.9%) | |||||
| Other | 8 (1.0%) | |||||
| Total | 4,122 | Women | 2,427 (58.9%) | 18–98, 37.6 (14.0) | White | 3,096 (75.1%) |
| Men | 1,682 (40.8%)‖ | African American | 276 (6.7%) | |||
| Asian American | 98 (2.4%) | |||||
| Hispanic or Latino | 51 (1.3%) | |||||
| Native American | 28 (0.7%) | |||||
| Other | 47 (1.1%) | |||||
N/A = not applicable; FPQ-9 = Fear of Pain Questionnaire-9; MTurk = Mechanical Turk.
One missing.
Two missing.
Of the 687 FPQ-9 Development participants, only 285 had race or ethnicity data; thus, percentage is a function of only those with data.
Seven unknown.
Three missing; FPQ-9 Development data set includes 455 undergraduates and 371 pain patients.
Thirteen missing on gender variable.
Structural Equation Models
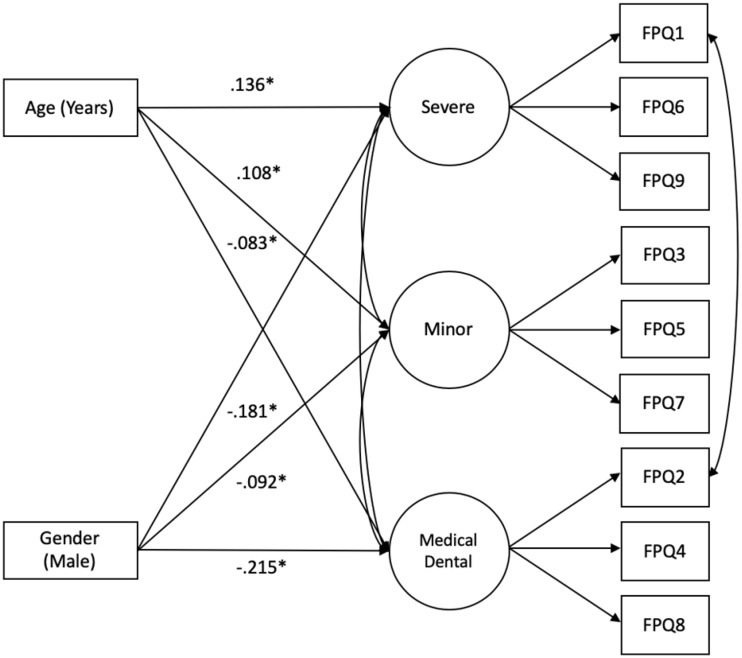
The results of the CFA (three subscales as latent variables with the indicators for each) were indicative of a well-fitting factor structure. After initially testing the full SEM with requested modification indices, items 1 and 2 of the FPQ-9 were allowed to correlate to improve overall model fit (Root Mean Square Error of Approximation [RMSEA] = 0.07; Comparative Fit Index [CFI] = 0.95; Tucker-Lewis Index [TLI] = 0.92; Standardized Root Mean Square Residual [SRMR] = 0.03). The FPQ-9 can be used with the individual subscales or as a total score, so it is expected that some of the items may correlate with each other, as did items 1 and 2. For all of the following results that include regression coefficients, each beta coefficient is standardized, as the units for age (years) are different than that of fear of pain, thus allowing for comparison. Each coefficient is interpreted as the expected increase in standardized units of pain-related fear given a 1 standard unit increase in the predicting variable (age). For example, Fear of Severe Pain subscale scores were significantly associated with age (β=0.136, P < 0.001), such that 1 standard deviation increase in age was related to slightly more than one-tenth of a standard deviation increase in fear of pain. Fear of Severe Pain subscale scores were also associated with gender (β=–0.181, P < 0.001), such that men reported lower Fear of Severe Pain subscale scores and women reported higher Fear of Severe Pain subscale scores. Fear of Minor Pain subscale scores were also related to age (β =0.108, P < 0.001) and gender (β=–0.092, P < 0.001), with men reporting lower scores and women reporting higher scores. Fear of Medical/Dental Pain subscale scores were negatively associated with age (β=–0.083, P < 0.001), indicative of greater age being associated with lower levels of medical and dental pain–related fear. Gender was associated with Fear of Medical/Dental Pain subscale scores such that men reported lower scores and women reported higher scores (β=–0.215, P < 0.001). The full SEM is shown in Figure 1.
Figure 1.
Standardized results and standard errors of a structural equation model (SEM) to show the association between age, gender, and FPQ-9 subscale scores. After using modification indices, items 1 and 2 (FPQ1 and FPQ2) from the Fear of Pain Questionnaire-9 were allowed to correlate, resulting in improved model fit (Root Mean Square Error of Approximation = 0.07; Comparative Fit Index = 0.95; Tucker-Lewis Index = 0.92; Standardized Root Mean Square Residual = 0.03). FPQ-9 = Fear of Pain Questionnaire-9. *P < 0.001.
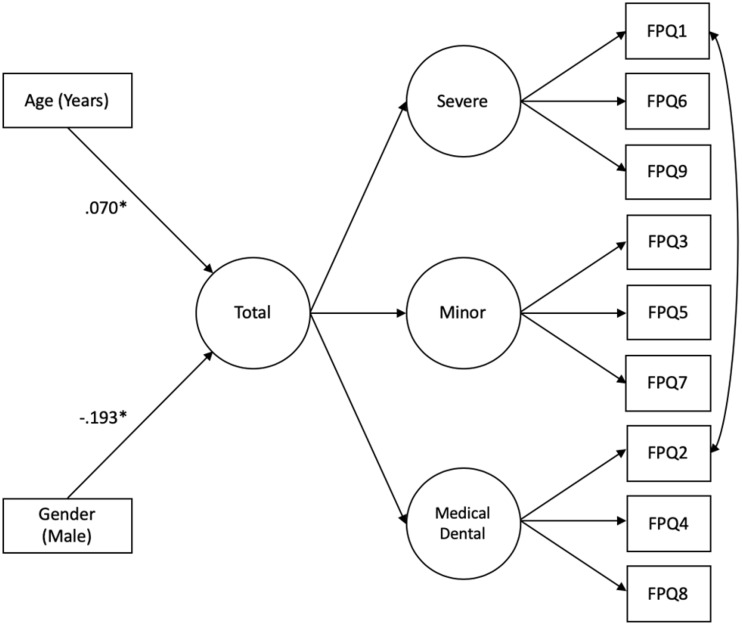
A similar model was tested using the higher-order factor structure of the FPQ-9, with the three subscales loading onto a single total score latent variable. Results of a CFA testing only the measurement portion were also indicative of a well-fitting model (RMSEA = 0.07; CFI = 0.93; TLI = 0.90; SRMR = 0.04). The total score latent variable was then regressed onto age and gender in the full model. Total fear of pain scores were significantly associated with age (β=0.070, P < 0.001), indicating that with greater age, there was a greater fear of pain. Gender was also associated with total fear of pain scores such that men have less fear of pain and women have a greater fear of pain (β=–0.193, P < 0.001). The full higher-order SEM is shown in Figure 2. Standardized results for all SEM models also are displayed in Table 2.
Figure 2.
Standardized results of a structural equation model (SEM) to show the association between age, gender, and total FPQ-9 score. After using modification indices, items 1 and 2 (FPQ1 and FPQ2) from the Fear of Pain Questionnaire-9 were allowed to correlate, resulting in improved model fit (Root Mean Square Error of Approximation = 0.07; Comparative Fit Index = 0.93; Tucker-Lewis Index = 0.90; Standardized Root Mean Square Residual = 0.04). FPQ-9 = Fear of Pain Questionnaire-9. *P < 0.001.
Table 2.
Mplus standardized coefficients from structural equation modeling regressions of age and gender predicting FPQ-9 scores
| Scale | β | Standard Error | Estimates/Standard Errors | P Value |
|---|---|---|---|---|
| Fear of Severe Pain subscale | ||||
| Gender, male | –0.181 | 0.017 | –10.920 | <0.001 |
| Age, y | 0.136 | 0.017 | 8.157 | <0.001 |
| Fear of Minor Pain subscale | ||||
| Gender, male | –0.092 | 0.018 | –5.137 | <0.001 |
| Age, y | 0.108 | 0.018 | 6.114 | <0.001 |
| Fear of Medical/Dental Pain subscale | ||||
| Gender, male | –0.215 | 0.017 | –12.351 | <0.001 |
| Age, y | –0.083 | 0.018 | –4.713 | <0.001 |
| Total | ||||
| Gender, male | –0.193 | 0.018 | –10.798 | <0.001 |
| Age, y | 0.070 | 0.019 | 3.711 | <0.001 |
FPQ-9 = Fear of Pain Questionnaire-9.
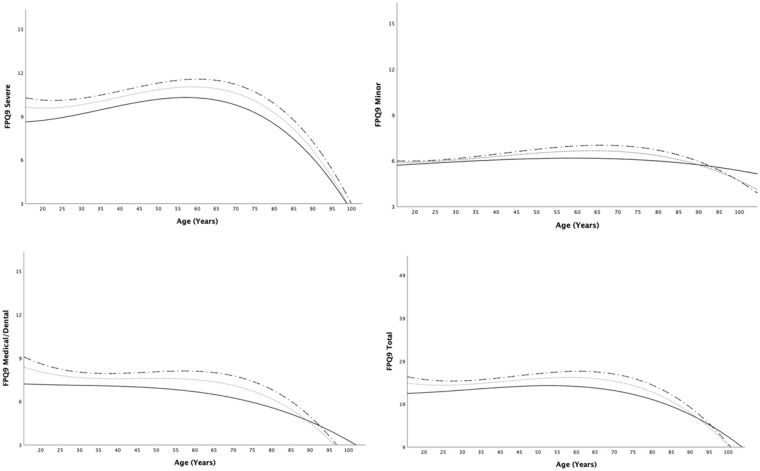
Ordinary least-squares regressions were conducted to examine the curvilinear relationships between age and Fear of Severe Pain subscale scores, Fear of Minor Pain subscale scores, Fear of Medical/Dental Pain subscale scores, and the total FPQ-9 score. The results are provided in Table 3. All models used gender as a covariate, and missing data were handled for these analyses using listwise deletion. Age was associated in both the quadratic (β=2.076, P < 0.001) and cubic (β=–1.278, P < 0.001) models for the Fear of Severe Pain subscale. Gender was also related such that men reported less fear of severe pain and women reported more fear of severe pain (β=–0.168, P < 0.001). For the Fear of Minor Pain subscale, the quadratic and cubic terms were nonsignificant, although the linear model of age was similar to that seen in the SEM model (β=0.094, P < 0.001). Men still indicated lower levels and women indicated higher levels (β=–0.076, P < 0.001). Fear of medical or dental pain was associated with both the quadratic (β=1.798, P = 0.001) and cubic (β=–0.974, P = 0.001) terms. Interestingly, when only the quadratic term was added, it was not significant, but once the cubic term was added, it became significant, indicating a better fit. Gender was also a significant contributor (β=–0.181, P < 0.001), with men having lower levels of fear of medical or dental pain and women having greater such levels. The total FPQ-9 model resulted in a similar pattern in which total scores were associated with both quadratic (β=1.904, P = 0.001) and cubic (β=–1.120, P < 0.001) terms. Gender was again significant (β=–0.176, P < 0.001) such that men were more likely to have lower total fear of pain scores and women were more likely to have higher total scores. Figures 3 and 4 include scatterplots with the best-fitting and mean lines to show the relationship of age with the FPQ-9 subscales and total scores, including panels stratified by gender. Additional figures for the subscales, as well as a table including frequency counts for each age group, are included in the Supplementary Data.
Table 3.
Ordinary least-squares regression models of age and gender predicting FPQ-9 scores with quadratic and cubic terms
| Scale | β | Standard Error | t | P Value |
|---|---|---|---|---|
| Fear of Severe Pain subscale | ||||
| Gender, male | –0.168 | 0.105 | –11.029 | <0.001 |
| Age, y | –0.722 | 0.067 | –2.625 | 0.009 |
| Age, quadratic | 2.076 | 0.002 | 3.761 | <0.001 |
| Age, cubic | –1.278 | 0.000 | –4.363 | <0.001 |
| Fear of Minor Pain subscale | ||||
| Gender, male | –0.076 | 0.079 | –4.867 | <0.001 |
| Age, y | –0.206 | 0.050 | –0.736 | 0.462* |
| Age, quadratic | 0.739 | 0.001 | 1.312 | 0.190 |
| Age, cubic | –0.457 | 0.000 | –1.527 | 0.127 |
| Fear of Medical/Dental Pain subscale | ||||
| Gender, male | –0.181 | 0.094 | –11.797 | <0.001 |
| Age, y | –0.929 | 0.060 | –3.353 | 0.001 |
| Age, quadratic | 1.798 | 0.001 | 3.233 | 0.001 |
| Age, cubic | –0.974 | 0.000 | –3.298 | 0.001 |
| Total | ||||
| Gender, male | –0.176 | 0.233 | –11.366 | <0.001 |
| Age, y | –0.765 | 0.147 | –2.749 | 0.006 |
| Age, quadratic | 1.904 | 0.003 | 3.411 | 0.001 |
| Age, cubic | –1.120 | 0.000 | –3.783 | <0.001 |
FPQ-9 = Fear of Pain Questionnaire-9.
*Because: quadratic and cubic terms are nonsignificant when taken out of the model and only age and gender are included, age is significantly associated in a linear fashion (β=0.094, P<0.001).
Figure 3.
Scatterplots for each of the three FPQ-9 subscales and the total FPQ-9 score to show cubic function results. In each scatterplot, the dashed black line indicates women, the solid black line indicates men, and the dashed gray line indicates the overall best-fitting line. FPQ-9 = Fear of Pain Questionnaire-9.
Figure 4.
Top panel: Mean total FPQ-9 scores for each age. Bottom panel: Mean scores by gender (white square and dashed line = women; black triangle and solid line = men). FPQ-9 = Fear of Pain Questionnaire-9.
The original intent of this study was to focus on age and its relation to fear of pain. Although other racial and ethnic group percentages were very low, approximately 7% of the sample identified as Black or African American. Therefore, an additional ordinary least-squares regression analysis was conducted in which race or ethnicity was dichotomized, selecting and contrasting those who identified as Black or African American with those who identified as White (which was the largest ethnic or racial group and the only other one with sufficient numbers to allow a comparison). The Black or African American or White identification was then included as a variable in an ordinary least-squares regression with age and gender, as outlined previously. Those who identified as Black or African American were more likely to endorse elevated levels of pain-related fear when accounting for age and gender (β=0.10, P < 0.001). That is, on average, those who identified as African American endorsed higher levels of fear of pain than those who identified as White. This finding held true across the total score model and all subscale models.
Discussion
Given the known associations between age and pain, pain perception, and pain experiences, this study was designed to examine the relations between age and pain-related fear. Data were collected from individuals across the adult life span (combined with other archival data sets), potential changes in fear of pain were portrayed, and age was used to predict fear of pain. Using a multi-tiered approach to analyze the data to look at general trends as well as specific potential subgroups, age was associated with fear of pain in a number of ways, each with implications for additional research, exploration, and consideration.
First, a general theme from the results of the SEM indicated the interesting association between age and the different types of fear of pain, all while taking into account the variance from the other types; that is, when examined linearly, although older age was associated with higher Fear of Severe and Minor Pain subscale scores, increased age was associated with lower Fear of Medical/Dental Pain subscale scores. This is interesting considering an exposure framework [23]. On average, 87.9% of patients over the age of 65 have been reported to have had one or more visits to a health care generalist within the last year compared with 65.1% of individuals 18 to 64 years old and 83.8% of individuals 2 to 17 years old [24]. Even with well visits made in the pediatric years, older adults visit generalists more often than other cohorts. It could be that as time goes on, older adults experience more medical and dental appointments than younger individuals and therefore perhaps more readily accept pain as a normal part of the aging process and can predict pain that might be experienced. It could be that older adults experience some type of habituation, but it could also be an experience of acceptance. Interestingly, adults 65 years and older have the lowest percentage of individuals with a visit to a mental health provider (4.8%) or a dentist (62.7%) compared with individuals 18 to 64 years old (8.8% and 64.0%, respectively) and 2 to 17 years old (8.7% and 84.7%, respectively) [24]. Although older adults have higher rates of medical visits, they visit dentists less often than do other age cohorts [20]. Thus, additional research is needed in this area to further explore potential exposure-related mechanisms between visits to general and oral health care providers, age, and Fear of Medical/Dental Pain subscale scores.
Greater Fear of Severe Pain subscale scores in older adults could be related to the etiology or consequences of the painful experiences. For example, severe bodily pain may be indicative of an acute pathological process, which may spawn fearfulness. Or perhaps the fear associated with breaking a bone (e.g., hip) could trigger anxiety or fears about loss of mobility. The meaning of pain therefore has profound implications [25], particularly for the older adult. Given prior literature [26, 27], perhaps fear of falling operates as a mediating variable or partially explains the relationship between age and fear of severe or minor pain. That said, prior work has also shown how some individuals with low fear of pain continue to have low fear of pain even after experiencing painful events [28]. Based on these findings, it is unclear whether having a history of painful experiences (e.g., falling) will increase or decrease one’s reported fear of pain. Furthermore, some younger adults face experiences (e.g., cancer treatment) that may influence their exposure to painful experiences and that may have implications for their idiographic or self-reported fear of pain. More could be done to explore these relations and help to elucidate how painful life experiences affect pain-related anxiety or fear. Additionally, older individuals face common challenges such as chronic disease, less social support, potential isolation, and more. Depression and stress have also been demonstrated to be similarly associated with pain, as well as fear and anxiety [29–33]. Some of the increases in fear of pain could be partially due to some of these biopsychosocial factors as well [34], although additional work is needed in this area.
The nonlinear regression models indicated a cubic relationship between age and Fear of Severe Pain subscale scores, Fear of Medical/Dental Pain subscale scores, and overall FPQ-9 scores. Although significant, the relationship was not dramatic but showed a slight increase in fear during the twenties and then a steady decrease after approximately age 65. Decision-making abilities and executive functioning continue to mature well into the twenties [35], which could be associated with how one’s affective response toward painful experiences develops over time. That is, perhaps as executive functioning and decision-making abilities facilitate wiser decisions, fear of pain becomes a type of protective factor aiding individuals to avoid more readily harmful situations.
The post hoc results demonstrating greater fear of pain among Black or African American adults when compared with White adults are consistent with those in the disparities literature documenting greater pain expression in Black or African American individuals relative to other racial or ethnic groups [36]. This finding is important when considering the minority stress framework, in which racial or ethnic minorities encounter numerous challenges across the life span at microsystemic and macrosystemic levels, which can have implications for health, emotion, and how an individual interacts with the world [37]. The results in this study support differences in at least one domain related to pain and aging—namely, in self-reported fear of pain. Additional research and applied work are needed to understand the biopsychosocial factors and systems or policies that may predispose, precipitate, or perpetuate [34] disparities related to pain-related fear and anxiety in racial or ethnic minority groups [36].
This study also highlights the importance of clinicians assessing and accounting for emotional factors in pain practice, particularly with the implications of fear possibly associated with older populations. Prior work has demonstrated the role of pain-related fear in exacerbating experienced pain, and the present study suggests that this association may be particularly true for older adults, although more prospective and experimental work needs to be done in this area. Furthermore, the results herein may suggest that there is not much of an emotional overlay (e.g., anticipation) for older adults in terms of medical and dental procedures, which does not imply that providers should avoid conversations about pain control in such settings with older adults. Finally, additional work is needed in order for researchers and providers to understand the role of fear of consequences related to painful experiences (e.g., fear of falling) and how such emotions may fall in line with or compete with the fear of the pain itself (e.g., understanding whether the fear of losing mobility and not being able to walk as a result of falling outcompetes or works in tandem with the fear of the pain itself).
Several limitations should be noted when considering the results and implications of this study. First, 205 participants from the new data collection were not included due to missing data or invalid responses on a series of validity items. As the missing data analyses indicated, there were significant differences in age, gender, and fear of pain levels between the valid responders and the invalid responses. Although there is no way to know for certain that the newly collected MTurk data were valid, the validity items and other requirements protected against the potential response bias.
The number of older adults in the sample, particularly those over age 70, was smaller than in younger ages, and likely is the reason for the increased variability in FPQ-9 scores observed in those age groups. In addition, many of these individuals were from the data sets collected on MTurk, although some of the older adults were not recruited through MTurk. Some researchers have cautioned against the use of MTurk or crowdsourcing to collect data on older adults, stating that these may not be the best representation of the aging population in the United States [38]. Indeed, this is a limitation; thus, interpretations of data should be guarded, and this study should serve as a starting point in understanding the relations between age and pain-related fear. Recent literature has also suggested that although the number of older adults is indeed consistently lower in MTurk data collection, the older people are not fundamentally different, and others recommend quota sampling to ensure an adequate number of older adults [39], which is what was done in this study. Additionally, future studies could build on this work by prospectively tracking fear of pain along with pain ratings in various groups to replicate this in a longitudinal manner. Other methodological approaches such as case-control designs could examine the relationship between fear of pain and age in patients who experience acutely or chronically painful conditions.
Given the prior literature examining the influence or relations of negative affect—including depression, anxiety, or stress—on or with pain and aging, one such limitation was the inability to include these factors as covariates in these models. Only a few of the demographic variables were included across all archival data sets, and thus it was not possible to include measures of depression or stress scores. Future work should include these variables as confounders to account for the high comorbidity between negative emotional experiences such as depression or anxiety and their relationship to fear of pain. The idea of teasing apart the independent contributions or relations of these negative affective experiences remains a challenge in the field of pain research [40].
The overall sample was diverse in terms of the time period in which it was collected and the types of individuals from which it was collected. Although this is advantageous for statistical purposes (i.e., greater variability), one could argue that age is associated with pain-related fear in different ways in different time periods or for different individuals (e.g., chronic pain patients vs undergraduate students). It could be that the experience of pain and the treatment of pain were different decades ago, making it difficult to include in one analysis (i.e., undergraduates from 20 years ago may respond to fear of pain items differently than those today). Although these are potential limitations, overall the variability was a strength and helped in generalizing overall averages for a diverse sample over multiple periods of time. Additional studies should be conducted, however, to further explore how fear of pain is affected by age in subpopulations such as chronic pain patients or in different time periods.
Conclusion
Fear of pain varies with age across the adult lifespan. Additionally, diverse types of pain-related fears are manifested differently depending on age. Fear of severe and minor pain is positively associated with age. Fear of medical or dental pain, however, is negatively associated with age. More work is needed to replicate and prospectively test the effects of age on fear of, and anxiety about, pain.
Supplementary Material
Acknowledgments
A special thanks is in order for the individuals who participated in any of the studies that were the focus of this article. We also wish to acknowledge the individuals who contributed to or facilitated the use of multiple data sets, including Cameron L. Randall, PhD; Cierra B. Edwards, MS; and the Center for Oral Health Research in Appalachia, including its field staff members as well as the past and present executive committee (Mary L. Marazita, PhD; Daniel W. McNeil, PhD, Betsy Foxman, PhD; Richard J. Crout, DMD, PhD; Kathy Neiswanger, PhD; John R. Shaffer, PhD, and Robert J. Weyant, DMD, DPhil, MPH). We also wish to thank Richard T. Gross, PhD and Nicholas A. Turiano, PhD for their technical assistance.
Supplementary Data
Supplementary Data may be found online at http://painmedicine.oxfordjournals.org.
Conflicts of interest: The authors have no conflicts of interest to report.
Funding sources: Financial and material support included the authors being funded in part by grants from the National Institute of General Medical Sciences (NIGMS T32-GM081741) and the National Institute of Dental and Craniofacial Research (NIDCR F31-DE027859, R01-DE014889, and R21-DE026540).
This article was based on a master’s thesis of the primary author (Casey D. Wright), supervised by the second author. The results were presented as part of a symposium at the Association for Behavioral and Cognitive Therapies in November 2019 in Atlanta, GA.
References
- 1. Merskey H, Bogduk N, eds.. Part III: Pain terms, a current list with definitions and notes on usage. In: Classification of Chronic Pain. 2nd ed. Seattle: IASP Press; 1994:209–14. [Google Scholar]
- 2. Lautenbacher S, Kunz M, Strate P, Nielsen J, Arendt-Nielsen L.. Age effects on pain thresholds, temporal summation and spatial summation of heat and pressure pain. Pain 2005;115(3):410–8. [DOI] [PubMed] [Google Scholar]
- 3. Shega JW, Tiedt AD, Grant K, Dale W.. Pain measurement in the National Social Life, Health, and Aging Project: Presence, intensity, and location. J Gerontol B Psychol Sci Soc Sci 2014;69(suppl 2):S191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zarit SH, Griffiths PC, Berg S.. Pain perceptions of the oldest old: A longitudinal study. Gerontologist 2004;44(4):459–68. [DOI] [PubMed] [Google Scholar]
- 5. Cole LJ, Farrell MJ, Gibson SJ, Egan GF.. Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging 2010;31(3):494–503. [DOI] [PubMed] [Google Scholar]
- 6. McNeil DW, Kennedy SG, Randall CL, et al. Fear of Pain Questionnaire‐9: Brief assessment of pain‐related fear and anxiety. Eur J Pain 2018;22(1):39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lang PJ. Fear reduction and fear behavior: Problems in treating a construct. In: Shlien JM, ed. Research in psychotherapy. Washington, DC: American Psychological Association; 1968:90–102. [Google Scholar]
- 8. McNeil DW, Vowles KE.. Assessment of fear and anxiety associated with pain: Conceptualization, methods, and measures. In: Asmundson G, Vlaeyen J, Crombez G, eds. Understanding and Treating Fear of Pain. New York: Oxford; 2004:189–211. [Google Scholar]
- 9. Vlaeyen J, Linton S.. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000;85(3):317–32. [DOI] [PubMed] [Google Scholar]
- 10. Polk DE, Weyant RJ, Crout RJ, et al. Study protocol of the Center for Oral Health Research in Appalachia (COHRA) etiology study. BMC Oral Health 2008;8(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Randall CL, Shulman GP, Crout RJ, McNeil DW.. Gagging and its associations with dental care-related fear, fear of pain and beliefs about treatment. J Am Dent 2014;145(5):452–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Edwards CB, Randall CL, Addicks SH, et al. Initial development of an Oral Health Values Scale. J Dent Res 2017;96:3709. [Google Scholar]
- 13. Berinsky AJ, Huber GA, Lenz GS.. Evaluating online labor markets for experimental research: Amazon.com’s Mechanical Turk. Polit Anal 2012;20(3):351–68. [Google Scholar]
- 14. Buhrmester M, Kwang T, Gosling SD.. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect Psychol Sci 2011;6(1):3–5. [DOI] [PubMed] [Google Scholar]
- 15. Litman L, Robinson J, Abberbock T.. TurkPrime.com: A versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav Res Methods 2017;49(2):433–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McNeil DW, Rainwater AJ III. Development of the Fear of Pain Questionnaire-III. J Behav Med 1998;21(4):169–90. [DOI] [PubMed] [Google Scholar]
- 17. Albaret MC, Sastre MTM, Cottencin A, Mullet E.. The Fear of Pain questionnaire: Factor structure in samples of young, middle-aged and elderly European people. Eur J Pain 2004;8(3):273–81. [DOI] [PubMed] [Google Scholar]
- 18. Osman A, Breitenstein JL, Barrios FX, Gutierrez PM, Kopper BA.. The Fear of Pain Questionnaire-III: Further reliability and validity with nonclinical samples. J Beh Med 2002;25(2):155–73. [DOI] [PubMed] [Google Scholar]
- 19. Roelofs J, Peters ML, Deutz J, Spijker C, Vlayen JWS.. The Fear of Pain Questionnaire (FPQ): Further psychometric examination in a non-clinical sample. Pain 2005;116(3):339–46. [DOI] [PubMed] [Google Scholar]
- 20. van Wijk AJ, Hoogstraten J.. Dutch translation of the Fear of Pain Questionnaire: Factor structure, reliability and validity. Eur J Pain 2006;10(6):479–86. [DOI] [PubMed] [Google Scholar]
- 21. Keith TZ. Multiple Regression and Beyond: An Introduction to Multiple Regression and Structural Equation Modeling. 2nd ed. New York: Routledge; 2014. [Google Scholar]
- 22. Muthén LK, Muthén BO.. Mplus User’s Guide. 7th ed. Los Angeles: Muthén & Muthén; 1998. –2015. [Google Scholar]
- 23. Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B.. Maximizing exposure therapy: An inhibitory learning approach. Behav Res Ther 2014;58:10–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics. Health, United States, 2016: With chartbook on long-term trends in health. 2016. Available at: https://www.cdc.gov/nchs/data/hus/hus16.pdf#076 (accessed May 2017). [PubMed]
- 25. Beecher HK. Relationship of significance of wound to pain experienced. JAMA 1956;161(17):1609–13. [DOI] [PubMed] [Google Scholar]
- 26. Martin RR, Hadjistavropoulos T, McCreary DR.. Fear of pain and fear of falling among younger and older adults with musculoskeletal pain conditions. Pain Res Manag 2005;10(4):211–9. [DOI] [PubMed] [Google Scholar]
- 27. Williams J, Hadjistavropoulos T, Asmundson G.. The effects of age and fear of pain on attentional and memory biases relating to pain and falls. Anxiety Stress Coping 2005;18(1):53–69. [Google Scholar]
- 28. McCracken LM, Gross RT, Sorg PJ, Edmands TA.. Prediction of pain in patients with chronic low back pain: Effects of inaccurate prediction and pain-related anxiety. Behav Res Ther 1993;31(7):647–52. [DOI] [PubMed] [Google Scholar]
- 29. Turk DC, Okifuji A, Scharff L.. Chronic pain and depression: Role of perceived impact and perceived control in different age cohorts. Pain 1995;61(1):93–101. [DOI] [PubMed] [Google Scholar]
- 30. McIlvane JM, Schiaffino KM, Paget SA.. Age differences in the pain-depression link for women with osteoarthritis. Functional impairment and personal control as mediators. Womens Health Issues 2007;17(1):44–51. [DOI] [PubMed] [Google Scholar]
- 31. Chaney JM, Uretsky DL, Mullins LL, et al. Differential effects of age and illness duration on pain-depression and disability-depression relationships in rheumatoid arthritis. Int J Rehab Health 1996;2(2):101–12. [Google Scholar]
- 32. Williamson GM, Schulz R.. Activity restriction mediates the association between pain and depressed affect: A study of younger and older adult cancer patients. Psychol Aging 1995;10(3):369–78. [DOI] [PubMed] [Google Scholar]
- 33. Wright GE, Parker JC, Smarr KL, Johnson JC, Hewett JE, Walker SE.. Age, depressive symptoms, and rheumatoid arthritis. Arthritis Rheum 1998;41(2):298–305. [DOI] [PubMed] [Google Scholar]
- 34. Wright CD, Tiani AL, Billingsley AL, Steinman SA, Larkin KT, McNeil DW.. A framework for understanding the role of psychological processes in disease development, maintenance, and treatment: The 3P-Disease Model. Front Psychol 2019;10:2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Johnson SB, Blum RW, Giedd JN.. Adolescent maturity and the brain: The promise and pitfalls of neuroscience research in adolescent health policy. J Adolesc Health 2009;45(3):216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Edwards CL, Fillingim RB, Keefe F.. Race, ethnicity and pain. Pain 2001;94(2):133–7. [DOI] [PubMed] [Google Scholar]
- 37. Forrester SN, Gallo JJ, Whitfield KE, Thorpe RJ Jr. A framework of minority stress: From physiological manifestations to cognitive outcomes. Gerontologist 2019;59(6):1017–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Patrick JH, Nehrkorn AM, Carney AK. How to use Amazon Mechanical Turk for research in aging. 2016. Available at: https://www.apadivisions.org/division-20/publications/newsletters/adult-development/2016/04/crowd-sourcing (accessed June 2020).
- 39. Litman L, Robinson J.. Conducting Online Research on Amazon Mechanical Turk and Beyond. Thousand Oaks, CA: Sage; 2021. [Google Scholar]
- 40. Felicione NJ, Blank MD, Wright CD, McNeil DW. Pain, fear, anxiety, and stress: Relation to beta-endorphins. In: Kerr P, Sirbu C, eds. Opioids from Inside Out: Scientific Foundations and Clinical Innovations of Endogenous Opioid Research. New York: Springer; In press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.