Abstract
Introduction
With obesity reaching pandemic proportions, its detrimental influence on many health-related conditions has recently become a focus of research. Musculoskeletal (MSK) pain is one of several disorders associated with obesity.
Materials and methods
This study was designed to identify MSK pain in individuals with severe obesity, recruited from a specialized obesity clinic, and to evaluate the correlation between the MSK symptoms and some individual criteria.
Results
In 466 patients (342 females and 124 males), with a mean BMI of 42,77 ± 5.64 kg/m², 90,3% reported MSK pain. Severe pain was reported by 57,8% of female vs 26,6% of male patients. Female patients showed higher mean pain level when compared with males. Body sites with a higher prevalence of pain were: knee (63.5%), lumbar region (46.8%), hip (29%) and ankle (23%), with a predominance of severe pain. BMI have shown a positive correlation to numeric rating scale score in female participants in three body regions: shoulder (P = 0.010), knee (P = 0.042) and ankle (P = 0.024). Body sites with higher pain prevalence were especially in areas of increased mechanical load.
Conclusions
Understanding the relationship between obesity and pain may provide insights into preventive measures and therapeutic strategies for MSK pain. Persistent MSK pain is a significant problem in obese patients that can have a negative relationship with quality of life and function. This fact highlights the importance that patients with obesity may have access to interdisciplinary care, for the prevention and rehabilitation of MSK disorders. To further understand this association, more robust studies are needed.
Keywords: obesity, musculoskeletal, pain, morbid obesity
Introduction
Obesity is yet a neglected public health concern. It is a chronic disease, with multifactorial genesis, requiring concerted efforts, posing as an important risk factor for the development and deterioration of another diseases [1]. Worldwide obesity has nearly tripled since 1975. In 2016, more than 1.9 billion adults were overweight. Of these, over 650 million were obese [2].
In 2015, the National Institute of Health Doutor Ricardo Jorge conducted a study that described the prevalence of overweight and obesity in the Portuguese population, verifying that 38.9% of the adults (25-74 years) living in Portugal was overweight and 28.7% suffered from obesity. The prevalence of overweight was higher in men (45.4%), while the prevalence of obesity was higher in women (32.1%) [3].
MSK pain is one of several disorders associated with obesity [4]. Mechanisms linking obesity and pain are complex and include behavioral, mechanical, biological and genetic factors. Pain affecting weight-bearing joints such as the knee, ankle and foot, as well as back pain, are among the most frequent complaints, often reported together as multisite pain [5,6]. Excessive weight increases mechanical stress to the joints and tissues of the body [7] and induces physical limitations and bodily pain. Self-reported bodily pain symptoms increase with progressively higher body mass index (BMI) values [8].
Reported risk factors for MSK pain include older age, female gender, high occupational workload and low physical activity [9-12]. Obesity is also closely related to MSK pain and physical dysfunction [13,14]. Specifically, increasing severity of pain is observed at higher BMI classifications [15,16].
The authors collected and detailed all the data of a sample of individuals with morbid obesity followed in an obesity and metabolic diseases unit. Additionally, the MSK pain was investigated in this group of patients, to evaluate the relationship between BMI and MSK pain.
Materials and methods
The authors conducted a cross-sectional study (data collected between 2017 and 2018). The patients were recruited from a specialized Obesity Clinic, named “Surgical Treatment Unit for Obesity and Metabolic Diseases” (englobing different medical and surgical specialties such as General Surgery; Internal Medicine; Endocrinology; Anesthesiology; Nutrition; Clinical Psychology; Physical Medicine and Rehabilitation; Gastroenterology; Plastic Surgery). All the participants were informed about the study, and verbal informed consent was obtained.
All the patients involved in the obesity and metabolic diseases program were enrolled in this study. The inclusion criteria for entering the obesity program were the following: age superior to 18 years; BMI ≥ 35Kg/m² with comorbidities or ≥ 40Kg/m² without comorbidities; more than two years of obesity-resistant to conservative medical treatment and educational/behavioral intervention.
Participants completed a Clinical Questionnaire to characterize their pain complaints regarding multiple musculoskeletal locations, characterizing the anatomic location and pain intensity in the last three months.
The population in the study was characterized namely regarding personal feature (gender, age and body mass index) and their pain complaints.
The patients completed a questionnaire referring the numeric rating scale [17] regarding pain in the following seven anatomical regions: hand & wrist, shoulder, lumbar region, hip, knee, ankle and foot. The authors considered the overall score pain to be equivalent to the highest reported pain per region by the patient, experienced in the last three months. The numeric rating scale, ranging from 0 to 10, was used to assess pain intensity in the seven anatomical regions. All the assessments reported were pre-surgery.
Statistical analysis was done using the Statistical Package for Social Sciences (SPSS), version 25.0 (IBM Corp., Armonk, NY). Statistical significance was determined at the level of P < 0.05. In order to assess the normal distribution of the continuous variables, Shapiro-Wilk Test was conducted. Spearman’s correlation coefficient (rho) was used to assess the correlation between the body mass index score and the level of pain per region. Cohen’s standard was used to analyze the correlation coefficients regarding the strength of the relationship [18].
Results
A total of 466 (342 female (73.4 %)) patients were analyzed. The mean age was 46.28 ± 10.59 years (female: 46.01 ± 10.59; male: 47.02 ± 10.61). The mean participants BMI was 42.77 ± 5.64 kg/m² (females: 42.52 ± 10.51; males: 43.44 ± 5.94), as shown in Table 1.
Table 1. Characteristics of participants.
| Variable | Group (N = 466) |
| Female Gender, N (%) | 342 (73.4) |
| Age in years, mean (SD) | 46.28 (10.59) |
| BMI in kg/m², mean (SD) | 42.77 (5.64) |
| Female (SD) | 42.52 (10.51) |
| Male (SD) | 43.44 (5.94) |
Level of pain by gender
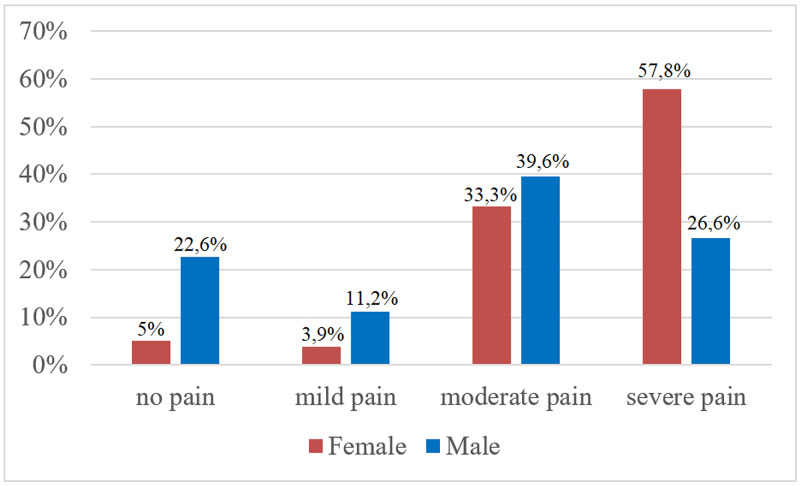
The overall prevalence of pain was 90,3%, female 95% vs male 77,4% (P < 0,001). Severe pain was reported by 57,8% of female vs 26,6% of male participants (Figure 1).
Figure 1. Prevalence and intensity of pain by gender.
Female participants showed a higher mean pain level when compared with male participants (female 6.57 ± 2.38 vs male 4.34 ± 2.89) (P < 0,001).
Prevalence of pain by body region
The prevalence of pain by body region were: hand & wrist 10.5% (N = 49), shoulder 15.7% (N = 73), lumbar region 46.8% (N = 218), hip 29% (N = 135), knee 63.5% (N = 295), ankle 23% (N = 107) and foot 12.4% (N = 58).
Correlation between pain by body region and BMI
BMI showed a moderate positive correlation to the numeric rating scale score in female participants in three body regions: shoulder (rho = 0.440, P = 0.010), knee (rho = 0.410, P = 0.042) and ankle (rho = 0.422, P = 0.024). No statistically significant associations were found in other body regions in both female and male patients, as presented in Table 2.
Table 2. Correlation coefficients between pain by body region and BMI.
| Body mass index (BMI) | ||||
| Female | Male | |||
| Spearman correlation | P | Spearman correlation | P | |
| Hand & wrist | 0.016 | 0.769 | 0.068 | 0.455 |
| Shoulder | 0.440 | 0.010 | 0.005 | 0.959 |
| Lumbar region | 0.004 | 0.942 | 0.040 | 0.660 |
| Hip | 0.052 | 0.336 | 0.089 | 0.328 |
| Knee | 0.410 | 0.042 | 0.013 | 0.888 |
| Ankle | 0.422 | 0.024 | 0.057 | 0.533 |
| Foot | 0.023 | 0.677 | 0.123 | 0.174 |
Discussion
Results from the current study showed a high MSK pain prevalence among the subjects (90,3%), more in females. An even higher prevalence was found in another study, in which 100% of the obese individuals evaluated during preoperative bariatric surgery reported MSK pain in at least one region of the body [19,20].
Body sites with a higher prevalence of pain were seen especially in areas of increased mechanical load: knee (63.5%), lumbar region (46.8%), hip (29%) and ankle (23%), with a predominance of severe pain. Larsson’s results showed that obese women had more MSK pain in the lower back, knee and foot [21]. A meta-analysis published in 2010 showed that obesity was strongly associated with an increased need for health care, for the treatment of acute and chronic lower back pain [22].
Female participants have reported more pain and a higher prevalence of moderate and intense pain when compared to male participants, as described by other studies reporting that female sex and obesity were factors significantly associated with the persistence or development of MSK pain [23,24], and with higher intensity [25].
Increased BMI ratio was significantly associated with MSK pain among women in shoulder, knee and ankle. It has been demonstrated that overweight is associated with adverse effects on the knees and feet, such as pain, stiffness and functional changes [26,27]. To provide preventive measures and therapeutic interventions for MSK pain, it is crucial to understand the relationship between obesity and pain. The proinflammatory effect of obesity in the pathogenesis of MSK diseases, independent of its biomechanical effect, has also been gaining interest [28]. A systematic review has shown a dose-response relationship between BMI and incident shoulder pain: overweight was associated with an increase of inflammatory factors, which could therefore be related to the development of shoulder disorders [29].
One of the limitations of this study is that the sample selection can contribute to an overestimation of the individuals’ probability of presenting MSK pain, since it is a population with a very high BMI. It is important to acknowledge that severe obesity increases the risk of developing MSK disorders [30].
The study remains ongoing - follow-up after bariatric surgery - to infer whether the expected weight loss is followed by a proportional decrease in pain complaints.
Conclusions
In conclusion, the authors found a high prevalence of MSK pain and intense pain among the patients, especially in the knee and lumbar regions. Persistent MSK pain is a significant problem in obese patients that can have a negative impact on the quality of life and function. This fact highlights the importance that obese subjects may adopt a preventive healthcare and may have access to an interdisciplinary care, to ensure a more effective intervention and rehabilitation, preventing MSK disorders. More robust studies are needed to detail and further investigate these associations.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Direção-Geral da Saúde. A obesidade como doença crónica. https://www.dgs.pt/doencas-cronicas/a-obesidade.aspx 2020
- 2.World Heath Organization. Obesity and Overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight 2020
- 3.Prevalence of overweight and obesity in Portugal: results from the first Portuguese Health Examination Survey (INSEF 2015) Gaio V, Antunes L, Barreto M, et al. Obes Res Clin Pract. 2017;12:40–50. doi: 10.1016/j.orcp.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 4.The association between musculoskeletal disorders and obesity. Kortt M, Baldry J. Aust Health Rev. 2002;25:207–214. doi: 10.1071/ah020207. [DOI] [PubMed] [Google Scholar]
- 5.Predictors of back pain in middle-aged women: data from the Australian longitudinal study of women's health. Brady SRE, Hussain SM, Brown WJ, et al. Arthritis Care Res. 2017;69:709–716. doi: 10.1002/acr.22982. [DOI] [PubMed] [Google Scholar]
- 6.Role of overweight and obesity in low back disorders among men: a longitudinal study with a life course approach. Frilander H, Solovieva S, Mutanen P, et al. BMJ Open. 2015;5:0. doi: 10.1136/bmjopen-2015-007805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Resistance exercise for knee osteoarthritis. Vincent KR, Vincent HK. PM R. 2012;4:0. doi: 10.1016/j.pmrj.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Relationship between body weight gain and significant knee, hip, and back pain in older Americans. Andersen RE, Crespo CJ, Bartlett SJ, Bathon JM, Fontaine KR. Obes Res. 2003;11:1159–1162. doi: 10.1038/oby.2003.159. [DOI] [PubMed] [Google Scholar]
- 9.Prevalence of widespread pain and its influence on quality of life: population study in Korea. Cho NH, Kim I, Lim SH, Kim HA. J Korean Med Sci. 2012;27:16–21. doi: 10.3346/jkms.2012.27.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Generalised musculoskeletal pain syndromes. Mourao AF, Blyth FM, Branco JC. Best Pract Res Clin Rheumatol. 2010;24:829–840. doi: 10.1016/j.berh.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Theories of work-related musculoskeletal disorders: implications for ergonomic interventions. Karsh BT. Theor Issues Ergonomics Sci. 2006;7:71–88. [Google Scholar]
- 12.Physical workload, leisure-time physical activity, obesity and smoking as predictors of multisite musculoskeletal pain: a 2-year prospective study of kitchen workers. Haukka E, Ojajarvi A, Takala EP, Viikari-Juntura E, Leino-Arjas P. Occup Environ Med. 2012;69:485–492. doi: 10.1136/oemed-2011-100453. [DOI] [PubMed] [Google Scholar]
- 13.Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment. Peltonen M, Lindroos AK, Torgerson JS. Pain. 2003;104:549–557. doi: 10.1016/S0304-3959(03)00091-5. [DOI] [PubMed] [Google Scholar]
- 14.Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain-a gender perspective. Bingefors K, Isacson D. Eur J Pain. 2004;8:435–450. doi: 10.1016/j.ejpain.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Comorbidity of obesity and pain in a general population: results from the Southern Pain Prevalence Study. Hitt HC, McMillen RC, Thornton-Neaves T, Koch K, Cosby AG. J Pain. 2007;8:430–436. doi: 10.1016/j.jpain.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Obesity and pain are associated in the United States. Stone AA, Broderick JE. Obesity. 2012;20:1491–1495. doi: 10.1038/oby.2011.397. [DOI] [PubMed] [Google Scholar]
- 17.Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Boonstra AM, Stewart RE, Koke AJ, et al. Front Psychol. 2016;7:1466–1485. doi: 10.3389/fpsyg.2016.01466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The role of anatomy computer-assisted learning on spatial abilities of medical students. Guimarães B, Machado JF, Tsisar S, et al. Anat Sci Educ. 2019;12:138–153. doi: 10.1002/ase.1795. [DOI] [PubMed] [Google Scholar]
- 19.Musculoskeletal findings in obese subjects before and after weight loss following bariatric surgery. Hooper MM, Stellato TA, Hallowell PT, Seitz BA, Moskowitz RW. Int J Obes. 2007;31:114–120. doi: 10.1038/sj.ijo.0803349. [DOI] [PubMed] [Google Scholar]
- 20.Prevalence of musculoskeletal symptoms in obese patients candidates for bariatric surgery and its impact on health related quality of life. Calenzani G, Santos FF, Wittmer VL, Freitas GK, Paro F. Arch Endocrinol Metab. 2017;61:319–325. doi: 10.1590/2359-3997000000237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Influence of weight loss on pain, perceived disability and observed functional limitations in obese women. Larsson UE. Int J Obes. 2004;28:269–277. doi: 10.1038/sj.ijo.0802534. [DOI] [PubMed] [Google Scholar]
- 22.The association between obesity and low back pain: a meta-analysis. Shiri R, Karppinen J, Leino-arjas P, Solovieva S, Viikari-juntura E. Am J Epidemiol. 2010;171:135–154. doi: 10.1093/aje/kwp356. [DOI] [PubMed] [Google Scholar]
- 23.Relationships between body mass index, fat mass, muscle mass, and musculoskeletal pain in community residents. Yoo JJ, Cho NH, Lim SH, Kim HA. Arthritis Rheumatol. 2014;66:3511–3520. doi: 10.1002/art.38861. [DOI] [PubMed] [Google Scholar]
- 24.Gender-specific associations between fat mass, metabolic syndrome and musculoskeletal pain in community residents: a three-year longitudinal study. Park IY, Cho NH, Lim SH, Kim HA. PLoS One. 2018;13:0. doi: 10.1371/journal.pone.0200138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sex differences and correlates of pain in patients with comorbid obesity and binge eating disorder. Masheb RM, White MA, Grilo CM. Eur Eat Disord Rev. 2016;24:247–250. doi: 10.1002/erv.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Association of weight gain with incident knee pain, stiffness, and functional difficulties: a longitudinal study. Tanamas SK, Wluka AE, Davies-Tuck M, et al. Arthritis Care Res. 2013;65:34–43. doi: 10.1002/acr.21745. [DOI] [PubMed] [Google Scholar]
- 27.The association between body fat and musculoskeletal pain: a systematic review and meta-analysis. Walsh TP, Arnold JB, Evans AM, Yaxley A, Damarell RA, Shanahan EM. BMC Musculoskelet Disord. 2018;19:233. doi: 10.1186/s12891-018-2137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tackling obesity in knee osteoarthritis. Wluka AE, Lombard CB, Cicuttini FM. Nat Rev Rheumatol. 2013;9:225–235. doi: 10.1038/nrrheum.2012.224. [DOI] [PubMed] [Google Scholar]
- 29.Risk factors of atherosclerosis and shoulder pain - Is there an association? A systematic review. Viikari-Juntura E, Shiri R, Solovieva S, Karppinen J, Leino-Arjas P. Eur J Pain. 2008;12:412–426. doi: 10.1016/j.ejpain.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 30.The link between musculoskeletal pain, lifestyle behaviors, exercise self-efficacy, and quality of life in overweight and obese individuals. Faghri PD, Chin WS, Huedo-Medina TB. Int J Phys Med Rehabil. 2015;3:255. doi: 10.4172/2329-9096.1000255. [DOI] [PMC free article] [PubMed] [Google Scholar]