Abstract
Background
Stress is a major risk factor for the impairment of psychological well-being. The present study aimed to evaluate the empirical evidence of the Transactional Stress Model proposed by Lazarus and Folkman in patients with psychosomatic health conditions.
Methods
A structural equation model was applied in two separate subsamples of inpatients from the Department of Psychosomatic Medicine (total n = 2,216) for consecutive model building (sample 1, n = 1,129) and confirmatory analyses (sample 2, n = 1,087) using self-reported health status information about perceived stress, personal resources, coping mechanisms, stress response, and psychological well-being.
Results
The initial model was created to reflect the theoretical assumptions by Lazarus and Folkman about their transactional stress concept. This model was modified until a sufficient model fit was reached (sample 1: CFI = 0.904, TLI = 0.898, RMSEA = 0.072 [0.071–0.074], SRMR = 0.061). The modified model was confirmed in a second sample (sample 2: CFI = 0.932, TLI = 0.928, RMSEA = 0.066 [0.065–0.068], SRMR = 0.052). Perceived external stressors and personal resources explained 91% of the variance of the stress response, which was closely related to symptoms of depression (63% variance explained). The attenuating effect of resources on stress response was higher (standardized β = -0.73, p < 0.001) than the impact of perceived stressors on stress response (standardized β = 0.34, p < 0.001).
Conclusion
The empirical data largely confirmed the theoretical assumption of the Transactional Stress Model, which was first presented by Lazarus and Folkman, in patients with a wide range of psychosomatic conditions. However, data analyses were solely based on self-reported health status. Thus, proposed inner psychological mechanisms such as the appraisal process could not be included in this empirical validation. The operationalization and understanding of coping processes should be further improved.
Keywords: stress, depression, Lazarus, transactional model, structural equation model
Introduction
The impact of psychological stress on health has been widely confirmed (Glaser and Kiecolt-Glaser, 2005; de Vente et al., 2006; Bengtsson et al., 2009; Lupien et al., 2009; Hemmerle et al., 2012; Gradus, 2017; Sgoifo et al., 2017). Stress is a major risk factor for the development of mental disorders such as major depression (Kessler, 1997; Uehara et al., 1999; Mino et al., 2006; Hankin et al., 2015), representing one of the most burdensome diseases worldwide (Lim et al., 2012). Yet, the pathway that connects stress exposure to a manifest disease is not well understood. It remains largely unknown why, in the face of adversity, some people turn ill whereas others remain healthy. Given the high number of stress-associated diseases (Forsen, 1991; Grassi et al., 2002), a better understanding of underlying stress processes is urgently needed. In disease prevention, knowledge about different response patterns to stress are highly important for the early identification of people in need of medical care (Caffo et al., 2008). In addition, individualized interventions could be designed based on an improved understanding of the underlying mechanisms in stress response. Therefore, in this study, we seek to empirically confirm or reject stress pathways as suggested by a common stress model.
In the resilience literature, a huge number of protective factors were identified that enable an individual to overcome adversity without negative consequences (Caffo et al., 2008; Davydov et al., 2010; Windle, 2011; Fletcher and Sarkar, 2013). These protective factors include sense of coherence, self-efficacy, and optimism (Eriksson and Lindstrom, 2006; Hart et al., 2006; Surtees et al., 2006; Kroninger-Jungaberle and Grevenstein, 2013; Braun-Lewensohn and Sagy, 2014; Campo et al., 2017; Kim et al., 2017). Over the past years, the focus of resilience research moved away from the identification of protective factors toward the understanding of underlying resilience processes (Luthar et al., 2000). Hence, a closer look at the pathways between stressors, resources, coping, stress response, and mental health is required to better understand how resilience impacts coping with stressors.
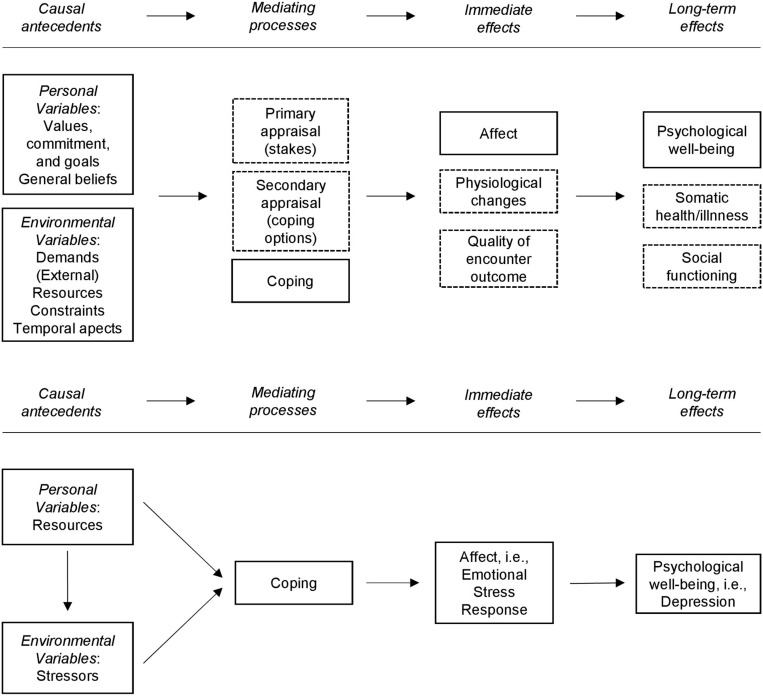
One of the most popular models describing stress pathways has been proposed by Lazarus and Folkman as early as in 1987 with the first reports dating back to 1966 (Lazarus, 1966; Lazarus and Folkman, 1984, 1987). Their Transactional Model provides the theoretical framework for the present study and is depicted in Figure 1 (upper model). The model emphasizes the person–environment transaction and suggests that a stress response is highly influenced by individual appraisal processes. Once confronted with stressors, the individual evaluates the relevance of the stressors (primary appraisal) and its own resources to overcome stress (secondary appraisal). Primary and secondary appraisals are believed to have an impact on the coping strategies chosen by the individual. Coping affects the immediate stress response as well as long-term health, psychological well-being, and social functioning. For simplicity, the authors depicted a linear section of the whole complex dynamic model and indicated the recursive nature of the model and the parallelism of the short- and long-term effects as footnotes to the figure (Lazarus and Folkman, 1987).
FIGURE 1.
Transactional model by Lazarus and Folkman (1987). Dashed frames indicate parts of the models that were not tested in the present study. Bottom: parts of the model that were tested in the present study.
Later, Lazarus and his co-authors formulated a cognitive–motivational–emotional theory that refined the analysis of specific different appraisal processes leading to different emotions (Smith and Lazarus, 1990). The transactional stress concept was embedded in the larger context of emotion theory (Smith and Lazarus, 1990; Lazarus, 1993), claiming to integrate stress and emotion research. In this study, we focus on the core piece of the transactional stress theory: the person–environment transaction. Consequently, we did not analyze specific appraisal processes and emotions, but rather the pathways from personal and environmental variables via coping to stress response and mental health.
Since the authors themselves evaluated the Transactional Model and confirmed the impact of personality factors, appraisals, and coping on psychological symptoms (Folkman et al., 1986), the entire Transactional Stress Model by Lazarus and Folkman (1987) has been tested in several studies. Despite of the number of previous studies, there are several drawbacks that suggest further empirical investigation of the structure of the Transactional Stress Model. For example, a majority of the studies only assessed parts of the theoretical model (Terry, 1991, 1994; Varni and Katz, 1997; Shewchuk et al., 1999; Zureck et al., 2015; Paek et al., 2016). Also, the studies that aimed to test the whole Transactional Model differed considerably in terms of the constructs included in the model, the operationalization of those constructs and the study populations, which reduces the comparability of the results (see Supplementary Table 1 for an overview). In addition, several studies used hierarchical linear regression analyses (Quine and Pahl, 1991; Honey et al., 2003; Bouchard et al., 2004; Hulbert-Williams et al., 2013) which rendered the inclusion of complex interactions (such as mediation) within the Transactional Model impossible. The studies that applied structural equation modeling often did not use the original conceptualization of the Transactional Model. For example, Kocalevent et al. (2007) simplified the complex model by specifying only three latent factors (“Resources,” “Stress Perception,” and “Health”). In addition, the authors varied the operationalization and naming of the three latent factors throughout the studies [Heinen et al. (2017): “Personal resources,” “Perceived Stress,” “Emotional Distress”; Kocalevent et al. (2013): “Resources,” “Chronic stress,” “Fatigue”; Kocalevent et al. (2014): “Resources,” “Stress,” “Mental health”]. Furthermore, some studies were based on small sample sizes, which may have led to unreliable models and invalid conclusions (Goh et al., 2010; Gonzalez-Ramirez et al., 2011; Kocalevent et al., 2014). Another drawback was that most of the previous studies analyzed very specific samples such as primiparous women or teachers (Supplementary Table 1).
Therefore, the aim of our study was to test a structural model based on the transactional stress concept by Lazarus and Folkman in a sufficiently large sample of patients with a wide range of health conditions that received inpatient treatment in a psychosomatic clinic. A sample of psychosomatic inpatients seemed to be well suited for the analysis of a stress model as many of the psychosomatic disorders can be associated with elevated stress levels or stressful life events (Cohen, 2000; Nakao, 2010). In contrast to previous studies that tested the Transactional Model using the PSQ (Kocalevent et al., 2007, 2014; Heinen et al., 2017), we focused on the person–environment interaction by modeling personal resources and perceived external stressors as the antecedents, coping as the mediating process, stress response as the immediate effect, and depression as the long-term effect (see Figure 1).
Materials and Methods
Sample and Procedure
Data were collected electronically via personal digital assistants (PDAs) as part of the clinical routine assessment at the inpatient clinic of the Department of Psychosomatic Medicine at Charité – Universitätsmedizin Berlin, Germany, between December 2007 and March 2014. The psychosomatic inpatient population encompassed a wide range of health conditions including somatoform disorders, eating disorders, and chronic pain disorders as well as physical conditions associated with mental disorders, such as depression and anxiety. The initial dataset included 2,359 cases. Only those cases with complete datasets (i.e., where patients had answered all instruments) were included in the cross-sectional analyses. Cases with incomplete data on any questionnaire were excluded (n = 145) leading to a total of n = 2,216 cases included in the study. Sensitivity analyses were carried out to evaluate whether the excluded cases differed from the included cases in their clinical or demographic characteristics. As the data were assessed electronically and as patients were forced to answer each item before the assessment was continued, there were no missing items within each assessed questionnaire. The sample was randomly split into two subsamples to allow model building in the first dataset (sample 1, n = 1,129) and confirmatory analyses in the second dataset (sample 2, n = 1,087).
Instruments
In the following paragraphs, we present the items used as indicator variables for the unobserved latent variables as well as additional data assessed in this study.
Resources
The latent factor Resources was built based on items of two different instruments that capture sense of coherence, self-efficacy and optimism, considering that these constructs have been identified as important protective factors of health (Eriksson and Lindstrom, 2006; Kroninger-Jungaberle and Grevenstein, 2013; Kim et al., 2017).
Sense of Coherence
Antonovsky (1979) defined the construct Sense of Coherence (SOC) in his salutogenetic model. It consists of three interrelated facets: comprehensibility, manageability, and meaningfulness. Based on Antonovsky’s 29-item Sense of Coherence scale (SOC-29) (Antonovsky, 1983), the Leipzig Short Scale (SOC-L9) was developed, which was used in this study. It consists of nine items and captures one global SOC factor. The SOC-L9 has demonstrated good psychometric properties; the internal consistency (Cronbach’s alpha) found in the development study was 0.87 (Schumacher et al., 2000).
Self-Efficacy and Optimism
Self-efficacy is a construct that captures the belief in one’s ability to deal with environmental demands (Bandura, 1997; Benight and Bandura, 2004). Optimism can be defined as a positive expectation toward one’s future (Scheier and Carver, 1992; Carver and Scheier, 2014). The subscales self-efficacy (five items) and optimism (two items) of the Self-efficacy, optimism, pessimism short scale (SWOP-K9) were administered in this study. The self-efficacy subscale and the optimism subscale showed appropriate psychometric properties in the development study. Internal consistencies (Cronbach’s alpha) were 0.86 and 0.78 for self-efficacy and optimism, respectively (Scholler et al., 1999).
Perceived Stressors
The latent factor Perceived Stressors was created using the five items included in the demands subscale of the Perceived Stress Questionnaire (PSQ) (Levenstein et al., 1993; Fliege et al., 2001, 2005). The PSQ was specifically designed for clinical research in psychosomatic patients, as the psychosomatic influences on structural changes of the body are difficult to assess given their subtlety (Levenstein et al., 1993). The original version with 30 items (Levenstein et al., 1993) has been shortened to 20 items. Along with this adaption, the original seven-factor structure was revised resulting in a four-factor solution with the subscales demands, tension, worries, and joy (Fliege et al., 2005). The 20-item version has been validated in several studies and has demonstrated sufficient psychometric properties (Fliege et al., 2001, 2005; Kocalevent et al., 2007). The items of the demands subscale assess the individual subjective perception of environmental stressors. The items are worded such that they are applicable to respondents in different situations, but still reflect relevant stressors in everyday life (e.g., “I feel under pressure from deadlines.”). The demands subscale showed an internal consistency (Cronbach’s alpha) of 0.79 (Fliege et al., 2005).
Coping
The latent factor Coping was included in the stress model to assess the mediating process between Resources, Perceived Stressors, and Stress Response as proposed by Lazarus and Folkman (1987). Although Appraisal is part of the transactional stress model, it was not directly measured in this study. However, Lazarus and Folkman suggested that Coping is closely related to the concept of cognitive appraisal. They defined Coping as “the cognitive and behavioral efforts made to master, tolerate, or reduce external and internal demands and conflicts among them” (Folkman and Lazarus, 1980, p. 223). The Brief Coping Questionnaire (Brief COPE, Carver, 1997) was used to operationalize coping in this study. It includes a total of 28 items. Four latent factors Evasive coping, Support seeking, Focus on positive, and Active coping were identified for the German version of the Brief COPE by Knoll et al. (2005). Evasive coping, Support seeking, Focus on positive, and Active coping demonstrated acceptable internal consistencies (Cronbach’s alpha) of 0.70, 0.76, 0.76, and 0.81, respectively (Knoll et al., 2005).
Stress Response
The latent factor Stress Response was created by the three dimensions tension, worries, and joy of the Perceived Stress Questionnaire (PSQ, Fliege et al., 2005). The Stress Response factor reflects emotional responses (e.g., “You feel tense.”), originally described by Lazarus and Folkman (1987) as an immediate stress reaction. Each subscale of the PSQ consists of five items. Fliege et al. (2005) suggested that the PSQ assesses two distinct stress dimensions, which is in line with previous findings of a two-factorial structure of stress (Lobel and Dunkel-Schetter, 1990). While the demands subscale captures the perception of environmental stressors, the tension, worries, and joy subscales—which are used to operationalize Stress Response in our study—measure stress reaction. The worries subscale, the tension subscale, and the joy subscale showed internal consistencies (Cronbach’s alpha) of 0.83, 0.80, and 0.83, respectively (Fliege et al., 2005).
Psychological Well-Being
Psychological well-being was proposed as the outcome in the original Transactional Model by Lazarus and Folkman (1987). To operationalize psychological well-being in this study, we used depressive symptoms as these reflect one major sub-construct of psychological well-being. The latent factor Depression was modeled with the items of the Patient Health Questionnaire nine-item depression scale (PHQ-9) (Kroenke et al., 2001). The PHQ-9 covers all aspects of depressive symptoms, as proposed in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV). The PHQ-9 has demonstrated good psychometric properties. The internal consistency (Cronbach’s alpha) was 0.89 in primary care patients (Kroenke et al., 2001).
Sociodemographic and Clinical Data
In addition, sociodemographic data (age, gender, education etc.) were assessed. As part of the clinical routine assessment, psychosomatic patients answered the ICD-Symptom Rating (ISR) including 29 items, covering five syndrome scales (Depression, Anxiety, Obsessive-compulsive, Somatoform, Eating disorder) and a supplementary scale (Tritt et al., 2008).
Statistical Analyses
Descriptive analyses were performed using IBM SPSS Statistics 24. T-Tests and Mann–Whitney U tests (non-parametric data) were used to compare characteristics between subsamples and in- and excluded cases. Structural equation modeling was carried out using the lavaan package (Rosseel, 2012) in R 4.0.3 (R Development Core Team, 2008). As the indicator variables were measured on 4- to 7-point-Likert scales, the weighted least squares means and variance adjusted estimator (WLSMV) was used, as suggested for ordinal data (DiStefano and Morgan, 2014). To allow model identification, the path from the first indicator variable to the latent variable was fixed to 1. Criteria for acceptable model fit were Comparative Fit Index (CFI) and Tucker–Lewis Index (TLI) > 0.9, root mean square error of approximation (RMSEA) < 0.08, and standardized root mean square residual (SRMR) < 0.08 (Browne and Cudeck, 1993; Kline, 2010; Little, 2013).
Model Building Analyses (Sample 1, n = 1,129)
The initial model was created to closely reflect the transactional stress concept of Lazarus and Folkman (1987). Thus, it included the impact of Resources on Perceived Stressors (primary appraisal), the influence of Resources and Perceived Stressors on Coping (secondary appraisal), the impact of Coping on Stress Response, and the effect of Stress Response on Psychological well-being (i.e., Depression) as shown in Figure 1 (bottom model). As suggested by the literature, Coping mediates the pathways from Perceived Stressors to Stress Response and from Resources to Stress Response, which in turn predicts Psychological well-being. Resources were hypothesized to attenuate Perceived Stressors, to enable appropriate Coping strategies and thereby to weaken the Stress Response.
To account for the multidimensional structure of the latent factors Resources, Coping, and Stress Response, second-order factor models were used. Whereas the first-order factors were measured by the items of each dimension (e.g., the first-order factor Sense of Coherence was measured by the items SOC01 to SOC09), the second-order factors were measured by the first-order factors (e.g., the second-order factor Resources was measured by the first-order factors Sense of Coherence, Self-efficacy, and Optimism).
First, we evaluated the fit of the individual measurement models by estimating first-order and second-order confirmatory factor analysis models. In a second step, the whole stress model was evaluated. To avoid overfitting the model to the specific population used in this study, modification indices were used cautiously. In fact, in this study, modification indices were only used in one case to guide the decision on removing a single item from the model.
Confirmatory Analyses (Sample 2, n = 1,087)
The final structural model obtained in sample 1 was estimated in sample 2 for confirmatory analyses.
Results
Sociodemographic Characteristics
Sociodemographic data of the two subsamples are presented in Table 1. We did not find any significant differences between the subsamples. On average, 80% of the two subsamples exceeded the cut-off score for mild symptom stress, 65% exceeded the cut-off for moderate symptom stress, and 24% exceeded the cut-off for severe symptom stress according to the ICD-10 Symptom Rating (ISR) Total score. Sensitivity analysis comparing in- and excluded cases showed that excluded cases were somewhat older (79 vs. 67 years) and that fewer people within the excluded patients were working full- or part-time (see Supplementary Table 2). It has to be noted, however, that only about 6% of the initial sample were excluded, which probably does not limit the generalizability much.
TABLE 1.
Characteristics of the two psychosomatic inpatient samples.
| Sample 1 (n = 1,129) | Sample 2 (n = 1,087) | Group difference p-value | |
| Sociodemographic characteristics | |||
| Age in years | |||
| M (SD) | 44.4 (14.8) | 44.8 (15.4) | 0.456 |
| Range | 17–86 | 17–87 | |
| Gender (% female) | 66.6 | 66.7 | 0.964 |
| Nationality (% German) | 92.6 | 91.0 | 0.179 |
| Employment status (% working) | 44.9 | 40.8 | 0.171 |
| Highest education (%) | |||
| University entrance diploma | 34.9 | 36.3 | 0.688 |
| Secondary school certificate | 44.6 | 42.4 | |
| Primary school certificate | 15.1 | 16.9 | |
| Without certificate | 3.3 | 2.4 | |
| Still in school | 0.8 | 1.3 | |
| Special needs school degree | 1.4 | 0.6 | |
| Partnership status (%) | |||
| Single | 33.4 | 34.4 | 0.496 |
| Married/with partner | 46.8 | 42.9 | |
| Divorced/separated | 17.6 | 17.9 | |
| Widowed | 2.2 | 4.8 | |
| Clinical characteristics | |||
| ISR [M (SD)/% above cut-off*] | |||
| Depression | 1.86 (1.02)/80.2 | 1.90 (1.06)/79.3 | 0.365 |
| Anxiety | 1.50 (1.14)/65.4 | 1.48 (1.13)/65.9 | 0.678 |
| Obsessive-compulsive | 1.06 (1.05)/49.8 | 1.07 (1.07)/50.9 | 0.824 |
| Somatoform | 1.28 (1.14)/57.0 | 1.25 (1.11)/56.4 | 0.531 |
| Eating disorder | 0.69 (1.01)/37.9 | 0.76 (1.09)/40.7 | 0.117 |
| ISR total score | 1.21 (0.66)/80.6 | 1.22 (0.67)/79.9 | 0.723 |
ISR, ICD-10-Symptom Ranking. ∗Cut-off scores for mild symptom stress are 1 for depressive, anxiety, and obsessive-compulsive syndrome scales; 0.75 for somatoform syndrome scale; 0.67 for eating disorder syndrome scale; and 0.6 for the ISR Total score.
Model Building in Sample 1 (n = 1,129)
The analyses of the measurement models resulted in acceptable model fit for all latent variables apart from Coping (Table 2). To further explore reasons for the insufficient model fit of the latent Coping factor, we estimated the measurement models of each of the four coping style factors and found—in contrast to Knoll et al. (2005)—unsatisfactory model fits for all latent coping style factors (Evasive Coping: CFI = 0.764, TLI = 0.606, RMSEA = 0.246 [0.230–0.263], SRMR = 0.125; Support Seeking: CFI = 0.778, TLI = 0.631, RMSEA = 0.389 [0.373–0.405], SRMR = 0.226; Focus on Positive: CFI = 0.795, TLI = 0.659, RMSEA = 0.242 [0.226–0.259], SRMR = 0.126) except for Active Coping (CFI = 0.979, TLI = 0.937, RMSEA = 0.146 [0.112–0.182], SRMR = 0.038). These results prompted us (1) to investigate the model fit of other (i.e., non-German) factor solutions, and (2) to develop new, sample-specific factor solutions. We evaluated the original factor structure for the Brief COPE by Carver (1997), which included 14 factors (Active Coping, Planning, Positive Reframing, Acceptance, Humor, Religion, Using Emotional Support, Using Instrumental Support, Self-Distraction, Denial, Venting, Substance Use, Behavioral Disengagement, Self-Blame), a 4-factor solution in a French sample which included 4 factors (Seeking Social Support, Problem Solving, Avoidance, Positive Thinking; Baumstarck et al., 2017), a 7-factor structure by Amoyal et al. (2011) (Active Coping, Avoidant Coping, Humor, Religion, Emotional Support, Venting, Acceptance), and a 2-factor solution that was found in Australian project managers (Aitken and Crawford, 2007; Problem-Focused Coping, Emotion-Focused Coping). In addition, 1-factor, 2-factor, 5-factor, and 9-factor structures were obtained in sample 1 using exploratory factor analysis. Unfortunately, none of the factor solutions was appropriate for inclusion in the structural stress model. The factor models either did not converge at all (literature-informed 14-factor and 2-factor solutions, and exploratory 2-factor solution), or demonstrated negative variances indicating problems with the measurement model (literature-informed 4-factor and 5-factor solutions, and exploratory 5-factor and 9-factor solutions). Thus, despite the unsatisfactory model fit of the factor model from Knoll et al. (2005), we used this factor structure to operationalize Coping.
TABLE 2.
Comparison of model fits and factor loadings for measurement models.
| Measurement model | Resources (second order) | Perceived stressors | Coping (second order) | Stress response (second order) | Psychological well-being (depression) |
| CFI | 0.947 | 0.987 | 0.707 | 0.953 | 0.979 |
| TLI | 0.937 | 0.974 | 0.669 | 0.944 | 0.971 |
| RMSEA | 0.103 [0.098–0.108] | 0.127 [0.106–0.150] | 0.135 [0.131–0.138] | 0.097 [0.092–0.103] | 0.074 [0.064–0.084] |
| SRMR | 0.047 | 0.036 | 0.130 | 0.048 | 0.044 |
| Standardized factor loadings (SE) of items | 0.54 (0.04)– 0.89 (0.02) | 0.71 (0.02)– 0.87 (0.02) | 0.37 (0.07)– 0.84 (0.03) | 0.68 (0.04)– 0.86 (0.03) | 0.57 (0.03)– 0.85 (0.03) |
| Standardized factor loadings (SE) of second-order factors | 0.89 (0.03)– 0.93 (0.03) | 0.24 (0.03)– 0.92 (0.13) | 0.88 (0.04)– 0.91 (0.04) |
CFI, Comparative Fit Index; TLI, Tucker–Lewis Index; RMSEA, root mean square error of approximation, 90% CI in square brackets; SRMR, standardized root mean square residual.
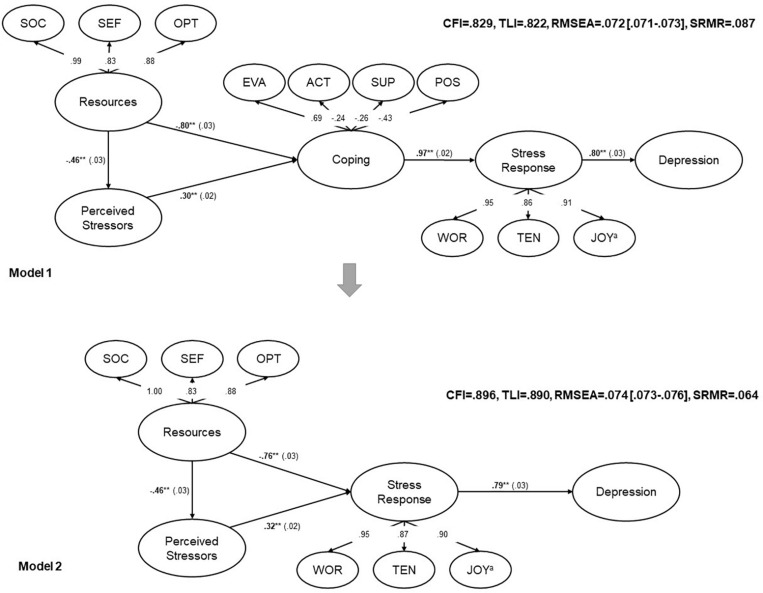
The estimation of the structural model resulted in insufficient model fit (Figure 2, upper model). In addition, negative residual variances occurred for a small number of coping items indicating that the model was not appropriate for the data (Ullman and Bentler, 2003). The attempt to include modifications as suggested by modification indices (residual covariances between coping items that were loading on the same factors) did not significantly improve the model fit and did not resolve the negative residual variances. Motivated by the good fit of the Active Coping factor, we estimated a structural model in which the second-order coping factor (including four coping style factors) was replaced by Active Coping. Unfortunately, the model did not converge. Therefore, we decided to exclude the latent Coping factor from model 1. The resulting structural model (model 2) is shown at the bottom of Figure 2. The major difference to model 1 is that Resources and Perceived Stressors predict Stress Response directly without being mediated by Coping. The resulting fit indices, however, did approach the cut-off of the fit indices but did not meet them. Modification indices showed that the item PSQ04 “You have too many things to do” was suggested to cross-load on several other factors. Therefore, we removed this item from the model (Table 3). The modified model 2 without the PSQ04 item yielded a largely acceptable model fit (CFI = 0.904, TLI = 0.898, RMSEA = 0.072 [0.071–0.074], SRMR = 0.061; Figure 3).
FIGURE 2.
Comparison of the two structural models. Circles: unobserved latent variables, numbers next to the arrows: standardized path coefficients, **p < 0.001, SE in parentheses. aInverted items on this factor. SOC, Sense of coherence; SEF, Self-efficacy; OPT, Optimism; EVA, Evasive coping; ACT, Active coping; SUP, Support seeking; POS, Focus on positive; WOR, Worries; TEN, Tension; CFI, Comparative Fit Index; TLI, Tucker–Lewis Index; RMSEA, root mean square error of approximation, 90% CI in square brackets; SRMR, standardized root mean square residual.
TABLE 3.
Modification indices (cut-off > 300).
| Variable 1 | Operator | Variable 2 | Modification index | Standardized expected parameter change |
| Resources | ∼∼ | Tension | 555.63 | 1.67 |
| Stressors | ∼∼ | Tension | 440.63 | 0.52 |
| Joy | =∼ | PSQ04 | 434.99 | −0.42 |
| Resources | ∼∼ | Joy | 415.01 | −1.66 |
| Stress reaction | =∼ | PSQ04 | 395.80 | −0.38 |
| Depression | =∼ | PSQ04 | 390.54 | −0.39 |
| Resources | =∼ | PSQ04 | 390.27 | 0.31 |
| Sense of coherence | =∼ | PSQ04 | 389.97 | 0.31 |
| optimism | =∼ | PSQ04 | 387.82 | 0.34 |
| Stressors | ∼∼ | Joy | 378.35 | −0.58 |
| Worries | =∼ | PSQ04 | 377.74 | −0.38 |
| Tension | =∼ | PSQ02 | 372.94 | 0.45 |
| Self−efficacy | =∼ | PSQ04 | 368.93 | 0.32 |
| Worries | =∼ | PSQ02 | 357.09 | 0.43 |
| Stress reaction | =∼ | PSQ02 | 348.22 | 0.42 |
| Sense of coherence | =∼ | PSQ02 | 335.86 | −0.33 |
| Resources | =∼ | PSQ02 | 335.85 | −0.33 |
| Tension | =∼ | PSQ16 | 330.06 | 0.42 |
| Sense of coherence | =∼ | PHQ06 | 323.30 | −0.57 |
| Resources | =∼ | PHQ06 | 323.23 | −0.57 |
| Optimism | =∼ | PSQ02 | 300.05 | −0.33 |
PSQ, Perceived Stress Questionnaire; PHQ, Patient Health Questionnaire; ∼∼ residual covariance; =∼ is measured by.
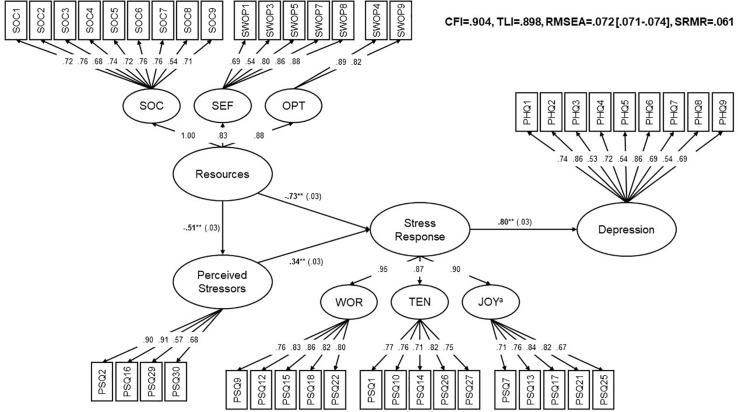
FIGURE 3.
Final Modified Stress Model (model 2 without item PSQ04). Rectangles: observed indicator variables. Circles: unobserved latent variables. For simplification, errors and thresholds were excluded from the figure. Numbers next to the arrows: standardized path coefficients, **p < 0.001, SE in parentheses, aInverted Items on this factor. SOC, Sense of coherence; SEF, Self-efficacy; OPT, Optimism; WOR, Worries; TEN, Tension; CFI, Comparative Fit Index; TLI, Tucker–Lewis Index; RMSEA, root mean square error of approximation, 90% CI in square brackets; SRMR, standardized root mean square residual.
Stress Response was predicted by Perceived Stressors and Resources demonstrating an explained variance of 91%. The impact of Resources on Stress Response was greater than the impact of Perceived Stressors on Stress Response. Resources also influenced Perceived Stressors. The impact of Stress Response on Depression was high which was expressed by an explained variance of 63% (Figure 3).
Confirmatory Analysis in Sample 2 (n = 1,087)
The proposed model was confirmed in the second sample of psychosomatic inpatients, yielding adequate model fit (CFI = 0.932, TLI = 0.928, RMSEA = 0.066 [0.065–0.068], SRMR = 0.052). The standardized path coefficients were very similar to the ones in the exploratory sample (Table 4). To investigate, whether we artificially overfitted the model by deleting the PSQ04 item, we estimated the initial model without this modification in sample 2. This resulted in a slightly lower, but still adequate fit (Table 4).
TABLE 4.
Comparison of model fits, standardized path coefficients, and explained variance of the final model.
| Structural models |
Sample 1 |
Sample 2 (confirmatory) |
||
| Model 2 | Model 2 without item PSQ04 | Model 2 | Model 2 without item PSQ04 | |
| CFI | 0.896 | 0.904 | 0.925 | 0.932 |
| TLI | 0.890 | 0.898 | 0.921 | 0.928 |
| RMSEA [CI] | 0.074 [0.073–0.076] | 0.072 [0.071–0.074] | 0.069 [0.067–0.070] | 0.066 [0.065–0.068] |
| SRMR | 0.064 | 0.061 | 0.056 | 0.052 |
| Standardized path coefficients | ||||
| • Resources→ Perceived Stressors | −0.46** (0.03) | −0.51** (0.03) | −0.48** (0.03) | −0.54** (0.03) |
| • Resources→ Stress Response | −0.76** (0.03) | −0.73** (0.03) | −0.77** (0.03) | −0.75** (0.03) |
| • Perceived Stressors→ Stress Response | 0.32** (0.03) | 0.34** (0.03) | 0.29** (0.02) | 0.32** (0.03) |
| • Stress Response → Depression | 0.79** (0.03) | 0.80** (0.03) | 0.86** (0.03) | 0.86** (0.03) |
| R2 Perceived Stressors | 0.21 | 0.26 | 0.23 | 0.29 |
| R2 Stress Response | 0.90 | 0.91 | 0.90 | 0.91 |
| R2 Depression | 0.63 | 0.63 | 0.73 | 0.73 |
**p < 0.001, SE in parantheses, R2: explained variance.
Discussion
This study largely confirmed the theoretical Transactional Model in a slightly modified version by excluding Coping in two randomly split psychosomatic subsamples. We were able to show empirically—as hypothesized by Lazarus and Folkman (1987)—that both resources and perceived stressors had an impact on the resulting stress response, which in turn strongly predicted depression. Further, resources had a stronger impact on the following stress response than perceived stressors. Resources did not only attenuate the stress response, but also influenced perceived stressors. These findings confirm the assumption of Lazarus and Folkman (1987) that stress is a highly individual concept resulting from a person–environment transaction. Furthermore, the results underline the importance of strengthening resources in psychotherapy and disease prevention and indicate a high relevance of resilience processes that allow an adaptive stress response in the face of adversity.
Coping had to be excluded from the model, as the measurement models for different literature-based and exploratory factor solutions did not fit the data and led to estimation problems in the complex structural stress model. The items of the Brief COPE did not consistently load on the four different factors proposed by Knoll (2002) and Knoll et al. (2005), which resulted in poor model fit. This is in line with previous research that reported different factor structures across different populations which indicates that the population-independent assessment of distinct coping styles remains difficult (Aitken and Crawford, 2007; Amoyal et al., 2011; Baumstarck et al., 2017). As coping is highly contextual and as coping strategies are most often not per se adequate or inadequate, they might be actually different between individuals and populations and thus assessment might be challenging. We think that further emphasis should be put on developing better self-report coping instruments or revise existing measures such that they are able to assess coping styles, independent from specific populations. This might be achieved by using modern measurement theory (i.e., item-response theory, IRT) to determine latent uni- or multidimensional coping style factors.
This same approach (i.e., using or even developing measurement models that enable the instrument- and population-independent assessment of latent factors) could potentially improve future analyses of the Transactional Stress Model (and other similar models). Those kinds of analyses would, however, require very large sample sizes to ensure reliable assessment across different populations. Once these measures have been developed, it would probably be far easier to create complex structural models by simply combining different IRT measures such as Stressors, Stress Response, or psychological well-being. Luckily, over the past years, there have been increasing efforts to develop IRT-based measures that are easily applicable in clinical and non-clinical samples, for example by the Patient-Reported Outcomes Measurement Information System (PROMIS) initiative (Cella et al., 2010), and those could be used as a blueprint for the development of specific instruments measuring latent stress, resilience, and coping constructs (Devine et al., 2016; Obbarius et al., 2018).
We empirically confirmed the core piece of the transactional theory, which describes that stress response is induced by a transaction between the person and the environment. This applies even though the pathways for coping and appraisal processes could not be directly analyzed given that Coping had to be excluded from the model and given that no direct measures of appraisals were included. Furthermore, it could be shown that depression is highly influenced by the individual response to stress. By modeling the different facets of the stress process, we addressed Lazarus’ claim that as stress is a complex, multivariate process, it has to be measured by a series of instruments that capture the different facets of the stress process (Lazarus, 1990).
Strengths and Limitations
The strengths of the present study design were that the large sample size allowed to perform consecutive model building and confirmatory analyses in two separate subsamples, and the inclusion of well-established questionnaire items as indicator variables for the latent factors. The Transactional Model from Lazarus and Folkman (1987) attributes significant importance on person–environment interaction and appraisal processes. Therefore, it seems logical that the indicator variables used were based on self-report measures where appraisal processes can be considered as inherent. For example, the Perceived Stress Questionnaire was designed to assess the individually perceived stress with a focus on cognitive appraisal (Levenstein et al., 1993). Another strength was the relevant sample of psychosomatic patients with a broad range of chronic conditions.
The present study has a cross-sectional design. Therefore, hypothesized causal relations must be treated with caution. Longitudinal data are needed to further confirm the Transactional Model. Furthermore, repeated-measurement designs will give more insight into intra-individual variations of the stress process in different encounters. In this way, research could focus more on the process character of stress, as was already suggested by Lazarus as early as 1978 (Lazarus, 1978).
Only patients with complete datasets for all questionnaires were included in the study. Post hoc analyses revealed statistically significant differences in gender and employment status between the dropouts and completers. This could be a possible bias of the study. However, compared with the whole sample size (n = 2,216), the number of non-completers (n = 145) was low.
A cut-off > 0.9 for the model fit indices CFI and TLI is regarded as sufficient fit by some authors (Little, 2013), although other authors propose more strict criteria (e.g., Hu and Bentler (1998) proposed CFI and TLI > 0.95). Yet, there is much debate about the usefulness of cut-off criteria (Heene et al., 2011). Cut-off recommendations should be considered tentative as model results are affected by numerous factors, e.g., sample size, number of indicators, and degree of model misspecification (Marsh et al., 2004). Alternative ways to assess sufficient model fit, for example, in the case of unidimensionality testing for IRT models, have been proposed to overcome the over-rejection of models due to strict cut-off criteria (Reise et al., 2013). Given the use of a robust WLSMV estimator, the consistent results for the model in both subsamples and the absence of indicators for model misspecification, we think that the presented structural model can be regarded as sufficiently proven.
In the past, there was much debate about the potential confounding of stress perception and psychopathology, given that they both rely on self-report measures (Dohrenwend et al., 1984). Yet, the subjectivity of stress measures is an explicit goal given that stress is a product of appraisal in line with Lazarus response to this critique. Research evidence showed that the manipulation of the item wording with the aim to be more objective did not affect the relationship between the stress items and health or well-being to a great extent (Lazarus et al., 1985).
Nevertheless, it would be interesting to include some objective criteria in future studies to evaluate the concordance of objective criteria and the subjective construal of reality.
Conclusion
The Transactional Model could be confirmed in empirical data of psychosomatic patients, although it was slightly modified by excluding Coping from the model. The main paths hypothesized by Lazarus and Folkman were embedded in the model: Stress response is strongly predicted by individual resources and perceived stressors. The individual stress response in turn highly predicts depression.
Data Availability Statement
The dataset generated and analyzed for this study can be obtained from the corresponding author upon reasonable request. Requests to access these datasets should be directed to NO, nina.obbarius@charite.de.
Ethics Statement
The study was reviewed and approved by the Charité’s Ethics Committee. The study was carried out in compliance with the Declaration of Helsinki. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
NO and MR planned the study. NO was in charge of the data analyses and drafted the initial version of the article. FF, GL, AO, and MR supported statistical analyses and interpretation. NO and AO drafted the first version of the revised manuscript. All authors discussed each section of the article, and commented on the article, and agreed to be accountable for the content of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. We acknowledge support from the German Research Foundation (DFG) and the Open Access Publication Fund of Charité – Universitätsmedizin Berlin.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.584333/full#supplementary-material
References
- Aitken A., Crawford L. (2007). Coping with stress: dispositional coping strategies of project managers. Int. J. Project Manag. 25 666–673. 10.1016/j.ijproman.2007.02.003 [DOI] [Google Scholar]
- Amoyal N. R., Mason S. T., Gould N. F., Corry N., Mahfouz S., Barkey A., et al. (2011). Measuring coping behavior in patients with major burn injuries: a psychometric evaluation of the BCOPE. J. Burn. Care Res. 32 392–398. 10.1097/BCR.0b013e318217f97a [DOI] [PubMed] [Google Scholar]
- Antonovsky A. (1979). Health, Stress, and Coping. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Antonovsky A. (1983). The sense of coherence: development of a research instrument. WS Schwartz Research Center for Behavioral Medicine, Tel Aviv University. Newsl. Res. Rep. 1 1–11. 10.21926/obm.transplant.1903082 [DOI] [Google Scholar]
- Bandura A. (1997). Self-efficacy: The Exercise of Control. New York, NY: Macmillan. [Google Scholar]
- Baumstarck K., Alessandrini M., Hamidou Z., Auquier P., Leroy T., Boyer L. (2017). Assessment of coping: a new french four-factor structure of the brief COPE inventory. Health Qual. Life Outcomes 15:8. 10.1186/s12955-016-0581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtsson C., Theorell T., Klareskog L., Alfredsson L. (2009). Psychosocial stress at work and the risk of developing rheumatoid arthritis: results from the Swedish EIRA study. Psychother. Psychosom. 78 193–194. 10.1159/000209351 [DOI] [PubMed] [Google Scholar]
- Benight C. C., Bandura A. (2004). Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav. Res. Ther. 42 1129–1148. 10.1016/j.brat.2003.08.008 [DOI] [PubMed] [Google Scholar]
- Bouchard G., Guillemette A., Landry-Léger N. (2004). Situational and dispositional coping: an examination of their relation to personality, cognitive appraisals, and psychological distress. Eur. J. Pers. 18 221–238. 10.1002/per.512 [DOI] [Google Scholar]
- Braun-Lewensohn O., Sagy S. (2014). Community resilience and sense of coherence as protective factors in explaining stress reactions: comparing cities and rural communities during missiles attacks. Commun. Ment. Health J. 50 229–234. 10.1007/s10597-013-9623-5 [DOI] [PubMed] [Google Scholar]
- Browne M. W., Cudeck R. (1993). Alternative ways of assessing model fit. Sage Focus Editions 154 136–136. [Google Scholar]
- Caffo E., Belaise C., Forresi B. (2008). Promoting resilience and psychological well-being in vulnerable life stages. Psychother. Psychosom. 77 331–336. 10.1159/000151386 [DOI] [PubMed] [Google Scholar]
- Campo R. A., Wu L. M., Austin J., Valdimarsdottir H., Rini C. (2017). Personal resilience resources predict post-stem cell transplant cancer survivors’ psychological outcomes through reductions in depressive symptoms and meaning-making. J. Psychosoc. Oncol 35 666–687. 10.1080/07347332.2017.1342306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C. S. (1997). You want to measure coping but your protocol’s too long: consider the brief COPE. Int. J. Behav. Med. 4 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver C. S., Scheier M. F. (2014). Dispositional optimism. Trends Cogn. Sci. 18 293–299. 10.1016/j.tics.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D., Riley W., Stone A., Rothrock N., Reeve B., Yount S., et al. (2010). The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 63 1179–1194. 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. I. (2000). Stress and mental health: a biobehavioral perspective. Issues Ment. Health Nurs. 21 185–202. 10.1080/016128400248185 [DOI] [PubMed] [Google Scholar]
- Davydov D. M., Stewart R., Ritchie K., Chaudieu I. (2010). Resilience and mental health. Clin. Psychol. Rev. 30 479–495. [DOI] [PubMed] [Google Scholar]
- de Vente W., Kamphuis J. H., Emmelkamp P. M. (2006). Alexithymia, risk factor or consequence of work-related stress? Psychother. Psychosom. 75 304–311. 10.1159/000093953 [DOI] [PubMed] [Google Scholar]
- Devine J., Fliege H., Kocalevent R., Mierke A., Klapp B. F., Rose M. (2016). Evaluation of Computerized Adaptive Tests (CATs) for longitudinal monitoring of depression, anxiety, and stress reactions. J. Affect. Disord. 190 846–853. 10.1016/j.jad.2014.10.063 [DOI] [PubMed] [Google Scholar]
- DiStefano C., Morgan G. B. (2014). A comparison of diagonal weighted least squares robust estimation techniques for ordinal data. Struct. Equat. Model. 21 425–438. 10.1080/10705511.2014.915373 [DOI] [Google Scholar]
- Dohrenwend B. S., Dohrenwend B. P., Dodson M., Shrout P. E. (1984). Symptoms, hassles, social supports, and life events: problem of confounded measures. J. Abnorm. Psychol. 93 222–230. 10.1037/0021-843x.93.2.222 [DOI] [PubMed] [Google Scholar]
- Eriksson M., Lindstrom B. (2006). Antonovsky’s sense of coherence scale and the relation with health: a systematic review. J. Epidemiol. Community Health 60 376–381. 10.1136/jech.2005.041616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher D., Sarkar M. (2013). Psychological resilience. Eur. Psychol. 18 12–23. 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- Fliege H., Rose M., Arck P., Levenstein S., Klapp B. (2001). Validierung des “perceived stress questionnaire”(PSQ) an einer deutschen stichprobe. Diagnostica 47 142–152. 10.1026//0012-1924.47.3.142 [DOI] [Google Scholar]
- Fliege H., Rose M., Arck P., Walter O. B., Kocalevent R. D., Weber C., et al. (2005). The Perceived Stress Questionnaire (PSQ) reconsidered: validation and reference values from different clinical and healthy adult samples. Psychosom. Med. 67 78–88. 10.1097/01.psy.0000151491.80178.78 [DOI] [PubMed] [Google Scholar]
- Folkman S., Lazarus R. S. (1980). An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 21 219–239. 10.2307/2136617 [DOI] [PubMed] [Google Scholar]
- Folkman S., Lazarus R. S., Gruen R. J., DeLongis A. (1986). Appraisal, coping, health status, and psychological symptoms. J. Pers. Soc. Psychol. 50 571–579. 10.1037/0022-3514.50.3.571 [DOI] [PubMed] [Google Scholar]
- Forsen A. (1991). Psychosocial stress as a risk for breast cancer. Psychother. Psychosom. 55 176–185. 10.1159/000288427 [DOI] [PubMed] [Google Scholar]
- Glaser R., Kiecolt-Glaser J. K. (2005). Stress-induced immune dysfunction: implications for health. Nat. Rev. Immunol. 5 243–251. 10.1038/nri1571 [DOI] [PubMed] [Google Scholar]
- Goh Y. W., Sawang S., Oei T. P. (2010). The revised transactional model (RTM) of occupational stress and coping: an improved process approach. Aust. N. Z. J. Org. Psychol. 3 13–20. 10.1375/ajop.3.1.13 [DOI] [Google Scholar]
- Gonzalez-Ramirez M. T., Garcia-Campayo J., Landero-Hernandez R. (2011). The role of stress transactional theory on the development of fibromyalgia: a structural equation model. Actas Esp. Psiquiatr. 39 81–87. [PubMed] [Google Scholar]
- Gradus J. L. (2017). Prevalence and prognosis of stress disorders: a review of the epidemiologic literature. Clin. Epidemiol. 9 251–260. 10.2147/CLEP.S106250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi L., Satriano J., Serra A., Biancosino B., Zotos S., Sighinolfi L., et al. (2002). Emotional stress, psychosocial variables and coping associated with hepatitis C virus and human immunodeficiency virus infections in intravenous drug users. Psychother. Psychosom. 71 342–349. 10.1159/000065993 [DOI] [PubMed] [Google Scholar]
- Hankin B. L., Young J. F., Abela J. R., Smolen A., Jenness J. L., Gulley L. D., et al. (2015). Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. J. Abnorm. Psychol. 124 803–816. 10.1037/abn0000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart K. E., Wilson T. L., Hittner J. B. (2006). A psychosocial resilience model to account for medical well-being in relation to sense of coherence. J. Health Psychol. 11 857–862. 10.1177/1359105306069082 [DOI] [PubMed] [Google Scholar]
- Heene M., Hilbert S., Draxler C., Ziegler M., Buhner M. (2011). Masking misfit in confirmatory factor analysis by increasing unique variances: a cautionary note on the usefulness of cutoff values of fit indices. Psychol. Methods 16 319–336. 10.1037/a0024917 [DOI] [PubMed] [Google Scholar]
- Heinen I., Bullinger M., Kocalevent R. D. (2017). Perceived stress in first year medical students – associations with personal resources and emotional distress. BMC Med. Educ. 17:4. 10.1186/s12909-016-0841-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmerle A. M., Herman J. P., Seroogy K. B. (2012). Stress, depression and Parkinson’s disease. Exp. Neurol. 233 79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honey K., Morgan M., Bennett P. (2003). A stress-coping transactional model of low mood following childbirth. J. Reprod. Infant Psychol. 21 129–143. 10.1080/0264683031000124082 [DOI] [Google Scholar]
- Hu L.-T., Bentler P. M. (1998). Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods 3:424. 10.1037/1082-989x.3.4.424 [DOI] [Google Scholar]
- Hulbert-Williams N. J., Morrison V., Wilkinson C., Neal R. D. (2013). Investigating the cognitive precursors of emotional response to cancer stress: re-testing Lazarus’s transactional model. Br. J. Health Psychol. 18 97–121. 10.1111/j.2044-8287.2012.02082.x [DOI] [PubMed] [Google Scholar]
- Kessler R. C. (1997). The effects of stressful life events on depression. Annu. Rev. Psychol. 48 191–214. 10.1146/annurev.psych.48.1.191 [DOI] [PubMed] [Google Scholar]
- Kim E. S., Hagan K. A., Grodstein F., DeMeo D. L., De Vivo I., Kubzansky L. D. (2017). Optimism and cause-specific mortality: a prospective cohort study. Am. J. Epidemiol. 185 21–29. 10.1093/aje/kww182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. (2010). Principles and Practice of Structural Equation Modeling, 3rd Edn. New York, NY: Guilford Press. [Google Scholar]
- Knoll N. (2002). Coping as a Personality Process: How Elderly Patients Deal with Cataract Surgery. Berlin: Freie Universität Berlin. [Google Scholar]
- Knoll N., Rieckmann N., Schwarzer R. (2005). Coping as a mediator between personality and stress outcomes: a longitudinal study with cataract surgery patients. Eur. J. Pers. 19 229–247. 10.1002/per.546 [DOI] [Google Scholar]
- Kocalevent R. D., Klapp B. F., Albani C., Brähler E. (2013). Zusammenhänge von Ressourcen, chronisch aktiviertem Distress und Erschöpfung in der deutschen Allgemeinbevölkerung. Psychother. Psych. Med. Psychol. 63 115–121. 10.1055/s-0032-1327705 [DOI] [PubMed] [Google Scholar]
- Kocalevent R. D., Levenstein S., Fliege H., Schmid G., Hinz A., Brahler E., et al. (2007). Contribution to the construct validity of the perceived stress questionnaire from a population-based survey. J. Psychosom. Res. 63 71–81. 10.1016/j.jpsychores.2007.02.010 [DOI] [PubMed] [Google Scholar]
- Kocalevent R. D., Mierke A., Danzer G., Klapp B. F. (2014). Adjustment disorders as a stress-related disorder: a longitudinal study of the associations among stress, resources, and mental health. PLoS One 9:e97303. 10.1371/journal.pone.0097303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroninger-Jungaberle H., Grevenstein D. (2013). Development of salutogenetic factors in mental health – Antonovsky’s sense of coherence and Bandura’s self-efficacy related to Derogatis’ symptom check list (SCL-90-R). Health Qual. Life Outcomes 11:80. 10.1186/1477-7525-11-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R., Folkman S. (1984). Stress, Appraisal and Coping. New York, NY: Springer Publishing Company. [Google Scholar]
- Lazarus R. S. (1966). Psychological Stress and the Coping Process. New York, NY: McGraw-Hill. [Google Scholar]
- Lazarus R. S. (1978). A strategy for research on psychological and social factors in hypertension. J. Hum. Stress 4 35–40. 10.1080/0097840X.1978.9934994 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S. (1990). Theory-based stress measurement. Psychol. Inquiry 1 3–13. 10.1207/s15327965pli0101_1 [DOI] [Google Scholar]
- Lazarus R. S. (1993). From psychological stress to the emotions: a history of changing outlooks. Annu. Rev. Psychol. 44 1–22. 10.1146/annurev.ps.44.020193.000245 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., DeLongis A., Folkman S., Gruen R. (1985). Stress and adaptational outcomes. The problem of confounded measures. Am. Psychol. 40 770–785. 10.1037/0003-066x.40.7.770 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1987). Transactional theory and research on emotions and coping. Eur. J. Pers. 1 141–169. 10.1002/per.2410010304 [DOI] [Google Scholar]
- Levenstein S., Prantera C., Varvo V., Scribano M. L., Berto E., Luzi C., et al. (1993). Development of the perceived stress questionnaire: a new tool for psychosomatic research. J. Psychosom. Res. 37 19–32. 10.1016/0022-3999(93)90120-5 [DOI] [PubMed] [Google Scholar]
- Lim S. S., Vos T., Flaxman A. D., Danaei G., Shibuya K., Adair-Rohani H., et al. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 2224–2260. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little T. D. (2013). Longitudinal Structural Equation Modeling. New York, NY: Guilford Press. [Google Scholar]
- Lobel M., Dunkel-Schetter C. (1990). Conceptualizing stress to study effects on health: environmental, perceptual, and emotional components. Anxiety Res. 3 213–230. 10.1080/08917779008248754 [DOI] [Google Scholar]
- Lupien S. J., McEwen B. S., Gunnar M. R., Heim C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 10 434–445. 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- Luthar S. S., Cicchetti D., Becker B. (2000). The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 71 543–562. 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh H. W., Hau K.-T., Wen Z. (2004). In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct. Equat. Model. 11 320–341. [Google Scholar]
- Mino Y., Babazono A., Tsuda T., Yasuda N. (2006). Can stress management at the workplace prevent depression? A randomized controlled trial. Psychother. Psychosom. 75 177–182. 10.1159/000091775 [DOI] [PubMed] [Google Scholar]
- Nakao M. (2010). Work-related stress and psychosomatic medicine. BioPsychoSocial Med. 4:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obbarius N., Fischer F., Obbarius A., Nolte S., Liegl G., Rose M. (2018). A 67-item stress resilience item bank showing high content validity was developed in a psychosomatic sample. J. Clin. Epidemiol. 100 1–12. [DOI] [PubMed] [Google Scholar]
- Paek M.-S., Ip E., Levine B., Avis N., Ip E. H., Avis N. E. (2016). Longitudinal reciprocal relationships between quality of life and coping strategies among women with breast cancer. Ann. Behav. Med. 50 775–783. 10.1007/s12160-016-9803-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quine L., Pahl J. (1991). Stress and coping in mothers caring for a child with severe learning difficulties: a test of Lazarus’ transactional model of coping. J. Commun. Appl. Soc. Psychol. 1 57–70. [Google Scholar]
- R Development Core Team (2008). R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing. [Google Scholar]
- Reise S. P., Scheines R., Widaman K. F., Haviland M. G. (2013). Multidimensionality and structural coefficient bias in structural equation modeling: a bifactor perspective. Educ. Psychol. Meas. 73 5–26. [Google Scholar]
- Rosseel Y. (2012). lavaan: an R package for structural equation modeling. J. Stat. Softw. 48 1–36. [Google Scholar]
- Scheier M. F., Carver C. S. (1992). Effects of optimism on psychological and physical well-being: theoretical overview and empirical update. Cogn. Ther. Res. 16 201–228. [Google Scholar]
- Scholler G., Fliege H., Klapp B. F. (1999). [Questionnaire of self-efficacy, optimism and pessimism: reconstruction, selection of items and validation of an instrument by means of examinations of clinical samples]. Psychother. Psychosom. Med. Psychol. 49 275–283. [PubMed] [Google Scholar]
- Schumacher J., Gunzelmann T., Brähler E. (2000). Deutsche Normierung der sense of coherence scale von Antonovsky. Diagnostica 46 208–213. [DOI] [PubMed] [Google Scholar]
- Sgoifo A., Montano N., Esler M., Vaccarino V. (2017). Stress, behavior and the heart. Neurosci. Biobehav. Rev. 74 257–259. 10.1016/j.neubiorev.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shewchuk R. M., Elliott T. R., MacNair-Semands R. R., Harkins S. (1999). Trait influences on stress appraisal and coping: an evaluation of alternative frameworks. J. Appl. Soc. Psychol. 29 685–704. 10.1111/j.1559-1816.1999.tb02019.x [DOI] [Google Scholar]
- Smith C. A., Lazarus R. S. (1990). “Emotion and adaptation,” in Handbook of Personality: Theory and Research, ed. Pervin L. A. (New York, NY: Guilford Press; ), 609–637. [Google Scholar]
- Surtees P. G., Wainwright N. W., Khaw K. T. (2006). Resilience, misfortune, and mortality: evidence that sense of coherence is a marker of social stress adaptive capacity. J. Psychosom. Res. 61 221–227. 10.1016/j.jpsychores.2006.02.014 [DOI] [PubMed] [Google Scholar]
- Terry D. J. (1991). Coping resources and situational appraisals as predictors of coping behavior. Pers. Indiv. Differ. 12 1031–1047. 10.1016/0191-8869(91)90033-8 [DOI] [Google Scholar]
- Terry D. J. (1994). Determinants of coping: the role of stable and situational factors. J. Pers. Soc. Psychol. 66 895–910. 10.1037/0022-3514.66.5.895 [DOI] [PubMed] [Google Scholar]
- Tritt K., von Heymann F., Zaudig M., Zacharias I., Söllner W., Loew T. (2008). Entwicklung des Fragebogens» ICD-10-Symptom-Rating «(ISR). Zeitschrift für Psychosomatische Medizin Psychotherapie 54 409–418. [DOI] [PubMed] [Google Scholar]
- Uehara T., Sakado K., Sakado M., Sato T., Someya T. (1999). Relationship between stress coping and personality in patients with major depressive disorder. Psychother. Psychosom. 68 26–30. 10.1159/000012307 [DOI] [PubMed] [Google Scholar]
- Ullman J. B., Bentler P. M. (2003). “Structural equation modeling,” in Handbook of Psychology, eds Schinka J. A., Velicer W. F. (Hoboken, NJ: John Wiley & Sons Inc; ), 607–634. [Google Scholar]
- Varni J. W., Katz E. R. (1997). Stress, social support and negative Affectivity in children with newly diagnosed cancer: a prospective transactional analysis. Psycho Oncol. 6 267–278. [DOI] [PubMed] [Google Scholar]
- Windle G. (2011). What is resilience? A review and concept analysis. Rev. Clin. Gerontol. 21 152–169. [Google Scholar]
- Zureck E., Altstötter-Gleich C., Gerstenberg F. X. R., Schmitt M. (2015). Perfectionism in the transactional stress model. Pers. Indiv. Differ. 83 18–23. 10.1016/j.paid.2015.03.029 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated and analyzed for this study can be obtained from the corresponding author upon reasonable request. Requests to access these datasets should be directed to NO, nina.obbarius@charite.de.