Abstract
Anti-Mullerian hormone (AMH) and testosterone (T) both play distinct roles in the early stages of folliculogenesis. However, the relationship between serum T and AMH levels is poorly understood. This study aimed to investigate the association between serum T and AMH levels in infertile women. A total of 1935 infertile women aged 20–46 years were included in the cross-sectional study and divided into four quartile groups (Q1 to Q4) based on serum T levels. Compared to the subjects in the highest T quartile (Q4), those in the lowest T quartile (Q1) showed significantly lower AMH levels. After adjustment for age, body weight, body mass index and FSH, increasing T quartile categories were associated with higher AMH levels. Binary logistic regression analyses revealed that the odds for the risk of diminished ovarian reserve (DOR) were 11.44-fold higher in Q1 than in Q4 and the odds for the risk of excess ovarian reserve (EOR) were 10.41-fold higher in Q4 than in Q1. Our data show that serum T levels are positively associated with serum AMH levels and suggest that androgen insufficiency may be a potential risk factor for DOR; androgen excess may lead to EOR in infertile women.
Subject terms: Infertility, Predictive markers
Introduction
Anti-Mullerian hormone (AMH), a glycoprotein belonging to the transforming growth factor β superfamily, is generated by granulosa cells (GCs) of growing follicles from the primary to the small antral follicles in the ovary1. The expression of AMH increases prior to follicle-stimulating hormone (FSH)-dependent selection (follicles up to 8 mm) and rapidly decreases after FSH-dependent selection (follicles > 8 mm)2. Serum AMH levels reflect the pool of growing follicles and thus are currently well known as a reliable biomarker for functional ovarian reserve3. Serum AMH levels gradually decline with age from the age of 25 years onward4,5. Serum AMH levels aid in the prediction of ovarian responses to controlled ovarian hyperstimulation6,7 and may be used in the individualization of starting doses of gonadotropin8,9. However, little is known about possible factors that affect serum AMH concentrations.
Androgens have been described to be involved in follicle recruitment and promotion of follicle growth10,11. The major circulating androgens in women include dehydroepiandrosterone sulfate (DHEA-S), dehydroepiandrosterone (DHEA), androstenedione, testosterone (T) and dihydrotestosterone (DHT). T and DHT, which are generated equally from the ovary and adrenals, are the only bioactive androgens that directly bind to the androgen receptor (AR)12. Similar to AMH, the action of T primarily occurs during the early stages of folliculogenesis because AR is the most abundant in the GCs of small follicles13. Peak serum T levels are achieved in early adulthood and show a decline with age as AMH14. Furthermore, studies have revealed that T supplementation may have a positive effect on antral follicle count (AFC) in poor ovarian responders (PORs)15,16 and T suppression by oral contraceptives might decrease the number of antral follicles and even serum AMH levels in polycystic ovary syndrome (PCOS) patients17,18.
Based on the abovementioned findings, we hypothesized that serum levels of T had a positive association with serum AMH levels. However, few large-scale studies have examined the relationship between serum T and AMH levels. Therefore, we conducted a large cross-sectional study in infertile women to clarify the association between serum T and AMH concentrations.
Results
The characteristics of the 1935 infertile women included in the study are shown in Table 1. The average age was 35.1 ± 4.7 years (range 21–46 years); the average body mass index (BMI) was 22.4 ± 3.8 kg/m2 (range 14.7–40.8 kg/m2). The mean serum T level was 0.33 ± 0.35 ng/mL (range 0.05–4.81 ng/mL) and the mean serum AMH level was 3.6 ± 2.8 ng/mL (range 0.03–22.08 ng/mL). Infertility causes included tubal factor (12.1%), male factor (11.6%), diminished ovarian reserve (13.0%), PCOS (9.6%), endometriosis (13.8%), uterine factor (8.0%), multiple factors (21.7%) and unexplained infertility (10.1%). In the group of women < 35 years (n = 887), the mean serum T level was 0.35 ± 0.31 ng/mL and the mean serum AMH level was 4.7 ± 3.1 ng/mL. In women ≥ 35 years (n = 1048), the average serum T level was 0.31 ± 0.38 ng/mL, and the average serum AMH level was 2.6 ± 2.0 ng/mL.
Table 1.
The characteristics of the study population.
| Variables | All population (n = 1935) | Age < 35 years (n = 887) | Age ≥ 35 years (n = 1048) |
|---|---|---|---|
| Age (years) | 35.1 ± 4.7 | 30.9 ± 2.7 | 38.6 ± 2.8 |
| Body height (cm) | 160.5 ± 5.8 | 160.8 ± 5.8 | 160.3 ± 5.7 |
| Body weight (kg) | 57.7 ± 10.5 | 56.8 ± 10.6 | 58.5 ± 10.3 |
| BMI (kg/m2) | 22.4 ± 3.8 | 22.0 ± 3.9 | 22.7 ± 3.8 |
| TSH (μIU/mL) | 1.7 ± 1.4 | 1.7 ± 1.8 | 1.7 ± 1.1 |
| Prolactin (ng/mL) | 15.6 ± 15.3 | 15.4 ± 12.0 | 15.7 ± 17.7 |
| 25-OH-vitamin D (ng/mL) | 21.8 ± 6.8 | 21.1 ± 6.2 | 22.2 ± 7.2 |
| FSH (mIU/mL) | 5.2 ± 3.3 | 4.8 ± 2.5 | 5.6 ± 3.8 |
| Testosterone (ng/mL) | 0.33 ± 0.35 | 0.35 ± 0.31 | 0.31 ± 0.38 |
| DHEA-S (μg/dL) | 239.5 ± 114.2 | 262.0 ± 107.7 | 220.1 ± 116.1 |
| AMH (ng/mL) | 3.6 ± 2.8 | 4.7 ± 3.1 | 2.6 ± 2.0 |
| Causes of infertility | |||
| Tubal factor | 12.1%(235/1,935) | 15.1%(134/887) | 9.6%(101/1,048) |
| Male factor | 11.6%(225/1,935) | 11.2%(99/887) | 12.0%(126/1,048) |
| DOR* | 13.0%(252/1,935) | 4.5%(40/887) | 20.2%(212/1,048) |
| PCOS* | 9.6%(186/1,935) | 12.1%(107/887) | 7.5%(79/1,048) |
| Endometriosis | 13.8%(267/1,935) | 15.3%(136/887) | 12.5%(131/1,048) |
| Uterine factor | 8.0%(155/1,935) | 9.9%(88/887) | 6.4%(67/1,048) |
| Multiple factors | 21.7%(420/1,935) | 16.5%(146/887) | 26.1%(274/1,048) |
| Unexplained infertility | 10.1%(195/1,935) | 15.4%(137/887) | 5.5%(58/1,048) |
Data are presented as the mean ± standard deviation.
BMI body mass index, TSH thyroid-stimulating hormone, FSH follicle stimulation hormone, DHEA-S dehydroepiandrosterone sulfate, AMH anti-Müllerian hormone.
*DOR, diminished ovarian reserve, was defined as AMH < 1.2 ng/mL based on POSEIDON criteria.
*PCOS, polycystic ovarian syndrome, was determined by Rotterdam criteria.
The subjects were then categorized into four quartile groups (Q1 to Q4) based on serum T concentrations (Table 2). AMH, DHEA-S, body weight and BMI were positively associated with the T quartile category, whereas age linearly decreased as the T quartile category rose from Q1 to Q4 (all p for tend < 0.001). Body height, TSH, prolactin, 25-OH-vitamin D and FSH were not significantly different among the T quartile categories. Furthermore, compared to the AMH levels in the subjects in the highest T quartile (Q4), those in the lower T quartile (Q1, Q2 and Q3) demonstrated significantly lower AMH levels (p < 0.05).
Table 2.
Clinical characteristics according to serum testosterone quartile categories.
| Variables | Quartile of serum testosterone | ||||
|---|---|---|---|---|---|
| Q1 (n = 481) | Q2 (n = 491) | Q3 (n = 478) | Q4 (n = 435) | p for tend | |
| Testosterone (ng/mL) | ≤ 0.21 | 0.22 ~ 0.27 | 0.28 ~ 0.35 | ≥ 0.36 | |
| Age (years) | 36.9 ± 4.5* | 35.4 ± 4.6* | 34.6 ± 4.5* | 33.3 ± 4.5 | < 0.001 |
| Body height (cm) | 160.5 ± 5.7 | 160.4 ± 5.6 | 160.4 ± 5.7 | 160.7 ± 6.0 | 0.723 |
| Body weight (kg) | 56.9 ± 9.2* | 56.4 ± 9.5* | 57.2 ± 10.2* | 60.9 ± 12.5 | < 0.001 |
| BMI (kg/m2) | 22.1 ± 3.3* | 21.9 ± 3.4* | 22.2 ± 3.9* | 23.6 ± 4.6 | < 0.001 |
| TSH (μIU/mL) | 1.7 ± 1.0 | 1.7 ± 1.9 | 1.6 ± 1.0 | 1.7 ± 1.6 | 0.743 |
| Prolactin (ng/mL) | 14.4 ± 11.1 | 16.5 ± 21.8 | 15.3 ± 10.2 | 16.0 ± 15.2 | 0.248 |
| Vitamin D (ng/mL) | 21.5 ± 7.5 | 21.5 ± 6.8 | 21.7 ± 6.2 | 22.4 ± 6.5 | 0.141 |
| FSH (mIU/mL) | 5.4 ± 3.6 | 5.1 ± 3.1 | 5.1 ± 3.1 | 5.2 ± 3.3 | 0.344 |
| DHEA-S (μg/dL) | 170.3 ± 70.1* | 221.4 ± 76.0* | 260.3 ± 96.9* | 319.1 ± 151.0 | < 0.001 |
| AMH (ng/mL) | 2.1 ± 1.5* | 3.3 ± 2.1* | 3.9 ± 2.7* | 5.6 ± 3.7 | < 0.001 |
Data are presented as the mean ± standard deviation.
p values for trends were generated by linear regression analysis.
*Statistically significantly different from the highest quartile category (Q4) using Bonferroni’s method in an analysis of variance (ANOVA) test.
BMI body mass index, TSH thyroid-stimulating hormone, Vitamin D 25-OH-vitamin D, FSH follicle stimulation hormone, DHEA-S dehydroepiandrosterone sulfate, AMH anti-Müllerian hormone.
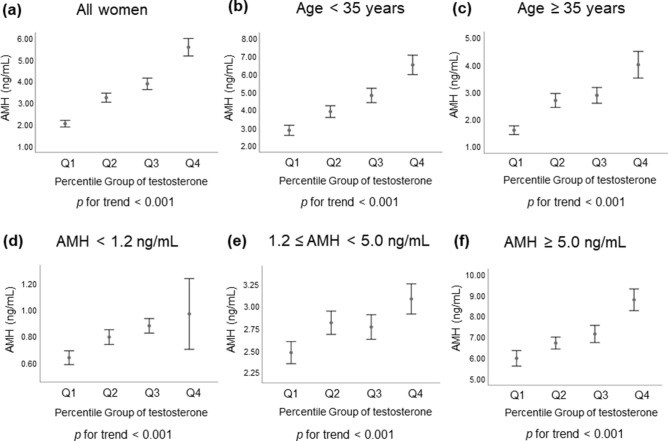
Generalized linear models were used to assess the independent association of serum T quartile categories with AMH levels after adjusting for potential confounding factors, including age, body weight, BMI and FSH. Regardless of all women or different age groups (< 35 or ≥ 35 years) or different AMH groups (< 1.2, 1.2–5.0, or ≥ 5.0 ng/mL), AMH levels significantly increased in a dose-dependent fashion across increasing T quartile categories in the multivariate adjustment model as shown in Fig. 1.
Figure 1.
Serum AMH levels according to serum testosterone quartile categories in different groups. (a) all women, (b) age < 35 years, (c) age ≥ 35 years, (d) AMH < 1.2 ng/mL, (e) 1.2 ≤ AMH < 5.0 ng/mL and (f) AMH ≥ 5.0 ng/mL. The p values for the trends were generated using generalized linear models after adjustment for multivariate confounders. Multivariable confounders included age, weight, body mass index, and FSH. Error bar represented 95% confidence interval of AMH. AMH anti-Mullerian hormone, Q quartile.
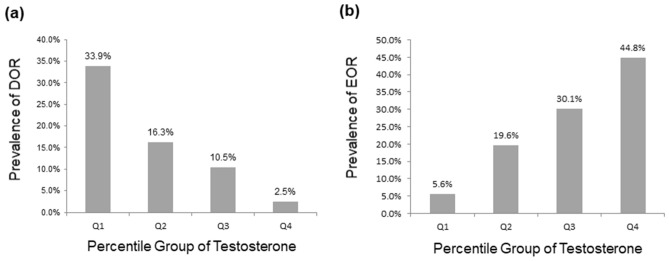
The overall proportions of subjects who met the criteria for diminished ovarian reserve (DOR, AMH < 1.2 ng/mL) and excess ovarian reserve (EOR, AMH ≥ 5.0 ng/mL) were 16.3% (242/1485) and 24.2% (359/1485), respectively. The prevalence of DOR among subjects in Q1, Q2, Q3 and Q4 was 33.9% (128/378), 16.3% (65/398), 10.5% (41/392) and 2.5% (8/317), respectively (Fig. 2a). Multiple logistic regression analyses revealed that the ORs for the risk of DOR dose-dependently increased across decreasing T quartile categories, and the odds for the risk of DOR were 11.44-fold higher in subjects in Q1 than in those in Q4 after adjustment for potential confounders (Table 3). The prevalence of EOR among subjects in Q1, Q2, Q3 and Q4 was 5.6% (21/378), 19.6% (78/398), 30.1% (118/392) and 44.8% (142/317), respectively (Fig. 2b). Multiple logistic regression analyses revealed that the ORs for the risk of EOR dose-dependently increased across increasing T quartile categories, and the odds for the risk of EOR were 10.41-fold higher in subjects in Q4 than in those in Q1 after adjustment for potential confounders (Table 3).
Figure 2.
Prevalence of (a) diminished ovarian reserve (DOR) and (b) excess ovarian reserve (EOR) according to serum T quartile categories. DOR was defined as serum AMH levels < 1.2 ng/mL; serum AMH levels ≥ 5.0 ng/mL were defined as EOR. Q quartile.
Table 3.
Risk for diminished ovarian reserve (DOR) or excess ovarian reserve (EOR) according to serum testosterone quartile categories.
| Variables | Risk for DOR (AMH < 1.2 ng/mL) | Risk for EOR (AMH ≥ 5.0 ng/mL) | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value | |
| T quartile categories | ||||
| Q1 (0.05 ~ 0.21 ng/mL) | 11.44 (4.75–27.53) | < 0.001 | 1.00 (Ref.) | |
| Q2 (0.22 ~ 0.27 ng/mL) | 5.45 (2.23–13.33) | < 0.001 | 3.74 (2.09–6.71) | < 0.001 |
| Q3 (0.28 ~ 0.35 ng/mL) | 3.12 (1.23–7.88) | 0.016 | 6.54 (3.70–11.54) | < 0.001 |
| Q4 (0.36 ~ 4.81 ng/mL) | 1.00 (Ref.) | 10.41 (5.84–18.55) | < 0.001 | |
ORs (95% CI) for DOR or EOR according to serum testosterone quartile categories after adjustment for multivariate confounders in infertile women (n = 1,935). Binary logistic regression analysis was performed. Multivariate confounders included age, weight, body mass index, and FSH.
T testosterone, AMH anti-Müllerian hormone, OR odds ratio, CI confidence interval, Q quartile, Ref. reference.
The age-dependent distribution of serum T levels in all patients (n = 1885) is shown in Table 4. The median serum T level in all patients was 0.27 ng/mL; the median serum T levels in the 20–25, 26–30, 31–35, 36–40 and 41–46 age groups were 0.36, 0.32, 0.28, 0.26 and 0.23 ng/mL, respectively.
Table 4.
Serum testosterone level distribution (ng/mL) based on age.
| Age (years) | Mean | Percentile | n | ||||
|---|---|---|---|---|---|---|---|
| 5th | 10th | Median | 90th | 95th | |||
| 20 ~ 25 | 0.38 | 0.20 | 0.21 | 0.36 | 0.63 | 0.76 | 35 |
| 26 ~ 30 | 0.40 | 0.17 | 0.21 | 0.32 | 0.56 | 0.89 | 288 |
| 31 ~ 35 | 0.34 | 0.16 | 0.18 | 0.28 | 0.47 | 0.54 | 688 |
| 36 ~ 40 | 0.32 | 0.15 | 0.17 | 0.26 | 0.42 | 0.51 | 627 |
| 41 ~ 46 | 0.27 | 0.13 | 0.15 | 0.23 | 0.37 | 0.45 | 247 |
| All | 0.33 | 0.15 | 0.17 | 0.27 | 0.46 | 0.55 | 1,885 |
Discussion
To the best of our knowledge, the present study is the largest clinical study to investigate the association between serum T and AMH levels in infertile women. In this large retrospective cross-sectional study of 1935 infertile women, higher serum T concentrations were associated with higher serum AMH levels after adjustment for potential confounders. Consistently, infertile women in the lowest T quartile had a 11.44-fold higher odds for the risk of DOR than those in the highest T quartile. The odds for the risk of EOR were 10.41-fold higher in infertile women in the highest T quartile than in those in in the lowest T quartile.
Androgens play important roles in the regulation of ovarian function. AR, expressed in oocytes, GCs and theca cells, is pivotal for normal follicular development10,11. AR is most highly expressed in the GCs of preantral and early antral follicles, and its expression decreases as the follicles grow13. Via the AR, androgens increase the FSH receptor and synergize with FSH to enhance follicle growth19–21. Moreover, androgens support follicle health by decreasing follicle atresia and GC apoptosis, and stimulating the proliferation and differentiation of GC20,22,23. Although AR is not expressed in primordial follicles, androgens promote primordial follicle initiation24,25 via indirect mechanisms, such as upregulation of insulin-like growth factor 1 expression25. The above information supports our results that lower T levels were associated with a higher risk of DOR. Studies have shown that women with DOR or POI demonstrated significantly lower serum T levels than controls26,27. On the other hand, androgen excess may lead to impaired ovarian function and dysregulated follicle development, displaying irregular cycles, oligo-ovulation and polycystic ovaries28,29. These findings agree with our results that infertile women with higher T levels had a higher risk of EOR. Thus, an optimal balance in androgenic actions is necessary for maintaining normal ovarian function. Serum T concentrations decline with age14. Thus, our study demonstrated an age-specific normal reference range for serum T levels to aid in identifying women who suffer from androgen insufficiency or excess (Table 4).
As mentioned above, androgens enhance FSH activity through increased FSH receptor expression20,21. FSH stimulates AMH expression30,31, which could inhibit the sensitivity of preantral follicles to FSH to avoid premature selection by FSH in the gonadotrophin-independent stage32,33. Therefore, Dewailly et al. proposed that androgens may promote AMH generation via enhancement of FSH-stimulated AMH expression34. Elevated AMH could attenuate FSH-induced aromatase activity, leading to an increase in androgen levels33. Moreover, via AMH receptor type 2 on the hypothalamus and pituitary, elevated AMH may boost GnRH-dependent LH pulsatility and secretion which stimulates androgen production in theca cells35,36. Taken together, it seems that androgens and AMH mutually stimulate each other. These results support our results that serum T concentrations positively correlated with serum AMH levels. Some studies also showed a positive correlation between serum androgens and AMH37–39. However, some studies revealed contradictory results, which indicated that androgens or FSH may have an inhibitory effect on AMH expression40–42. Thus, the accurate relationship between androgens and AMH remains unclear. Further studies with ideal experimental models are needed to clarify the relationship.
Serum T levels have been suggested to be positively associated with ovarian response43,44 and even pregnancy outcomes44,45 in women undergoing IVF cycles. Although some conflicting studies have shown that serum T levels do not predict IVF outcomes43,46, available data have indicated that T supplementation may improve ovarian response and IVF outcomes in PORs47,48. In a randomized controlled trial of 110 PORs undergoing IVF cycles, Kim et al. reported that pretreatment with transdermal T gel significantly increased AFC and reduced the day of stimulation and total dosage of gonadotropins. In addition, the numbers of oocytes retrieved, mature oocytes, fertilized oocytes, and good-quality embryos were significantly higher in the T pretreatment group than in the control group16. A meta-analysis of 7 randomized controlled trials conducted by Noventa and colleagues revealed that PORs receiving T therapy demonstrated higher numbers of total oocytes, MII oocytes and total embryos, as well as a higher clinical pregnancy rate and live birth rate than controls47. On the other hand, the addition of insulin sensitizing agents to suppress insulin resistance and excess androgen may ameliorate the results of ovulation induction in PCOS patients49,50. In the present study, we provided an age-specific normal reference range for serum T levels to help determine whether infertile women require agents for androgen enhancement or suppression (Table 4). Further large-scale, well-defined randomized controlled trials are still mandatory to confirm the effectiveness of androgen supplementation and androgen suppression by agents.
Several potential limitations should be taken into consideration when interpreting the data. First, the retrospective design of this study presented the major limitation. Second, since this is a cross-sectional study, a causal relationship could not be determined between serum T and AMH levels. Third, our study population only consisted of infertile women. We cannot be sure that our results would be applicable to the general population. Fourth, direct testosterone immunoassays have limitations for clinical use, particularly for low concentrations found in women and children51. This would be a relevant source of bias. Although high correlation (r ≥ 0.95) of serum T levels was observed between the ARCHITECT 2nd Generation Testosterone assay and the LCMS, the bias could not be totally excluded. Fifth, serum concentrations of free T, androstenedione, and sex hormone-binding globulin (SHBG) were not measured in our routine infertility evaluation. Thus, accurate androgen status would be uncertain in this study.
In conclusion, our data reveal an obvious positive association between serum T and AMH levels in infertile women. Additionally, the risk of DOR was significantly increased in a dose-dependent manner across decreasing T quartile categories; the risk of EOR dose-dependently increased across increasing T quartile categories. Long-term longitudinal studies are required to confirm our results.
Methods
Study design and participants
This was a retrospective cross-sectional study. Infertile women were first identified based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), code 628, from the clinical database in Kaohsiung Veterans General Hospital. To avoid any potential misclassifications, among the infertile women identified by the ICD-9-CM code, only subjects who received a complete infertility survey in the reproductive center of Kaohsiung Veterans General Hospital were selected. A total of 2476 infertile women were identified from May 2013 through March 2020. Then, we performed the chart review of these 2476 infertile women and selected the women who truly met the definition of infertility among them. Infertility was defined by the failure to achieve a successful pregnancy after 12 months or more of regular, unprotected sexual intercourse52. Moreover, we excluded the following subjects based on chart review: (1) subjected who experienced repeated surveys; (2) subjects who had extreme age (< 20 or > 46 years) (3) subjected who was diagnosed as primary ovarian insufficiency; (4) subjects who ever underwent ovarian surgery; (5) subjected who had a history of exposure to cytotoxic agents or pelvic irradiation for malignancy; (6) subjected who had androgen-secreting tumors; (7) subjected who was diagnosed as congenital adrenal hyperplasia (8) subjects who had androgen supplementation or hormonal therapy during the previous 3 months. A total of 1935 infertile women were finally included in the study. The study protocol was approved by the institutional review board in Kaohsiung Veterans General Hospital, with the identifier KSVGH20-CT11-03, and conformed to the “Declaration of Helsinki for Medical Research involving Human Subjects.” Need of informed consent was waived by the institutional review board in Kaohsiung Veterans General Hospital due to the retrospective design.
Biochemical measurements
For the infertility survey, we checked blood examinations including AMH, T, DHEA-S, FSH, luteinizing hormone (LH), estradiol, thyroid-stimulating hormone (TSH), prolactin and 25-OH-vitamin D levels. Serum AMH levels were measured by chemiluminescent immunoassay using the Access Immunoassay Systems, the Beckman Coulter enzyme-linked immunoassay (Beckman Coulter, Marseille, France). The analytical range of the lower limit of detection was 0.02 ng/mL. The intra-assay coefficient of variation (CV) was 3.0%, and the interassay CV was 7.0%. DOR was defined as serum AMH levels < 1.2 ng/mL based on the POSEIDON criteria53; serum AMH levels ≥ 5.0 ng/mL, modified from the revised Rotterdam criteria54, were considered EOR in this study.
Serum T was measured by chemiluminescent microparticle immunoassay using the ARCHITECT 2nd Generation Testosterone assay (Abbott GmbH, Max-Planck-Ring 2, Wiesbaden, Germany). The range was 0.04 ng/mL to 18.62 ng/mL. The assay had a limit of quantitation of ≤ 0.04 ng/mL and had a within-laboratory imprecision of ≤ 10% CV. Potential interference in the ARCHITECT 2nd Generation Testosterone assay from hemoglobin, bilirubin, triglycerides, protein and biotin was evaluated to be ≤ 10%. This assay had a correlation coefficient (r) of ≥ 0.95 for samples with testosterone concentrations ranging from 0.04 ng/mL to 10.09 ng/mL when compared to Liquid Chromatography-Tandem Mass Spectrometry (LCMS).
Serum DHEA-S, FSH, LH, estradiol, TSH, prolactin and 25-OH-vitamin D concentrations were measured by a chemiluminescent microparticle immunoassay on the ARCHITECT iSystem (Abbott, Longford, Ireland or Abbott, Wiesbaden, Germany). The total CV of these analyses were consistently < 3–10%. The specificity of these assays was determined by studying the cross-reactivity of structurally similar compounds. The cross-reactivity was calculated as a percent cross-reactivity. DHEA-S assay was shown to be 0% for testosterone, 0.003% for androstenedione, 0.025% for 19-hydroxyandrostenedione, 0.006% for DHEA glucuronide and 0.001% for estradiol. FSH assay was shown to be 0.002% for LH, 0.043% for TSH and 0.001% for hCG. LH assay was shown to be 0.01% for FSH, 0% for TSH and 0.01% for hCG. Estradiol assay was shown to be 0.1% for 17β-estradiol 3-sulfate and 0.7% for estrone. Prolactin assay was shown to be 0% for FSH, hCG, TSH and 0.001% for LH. TSH assay had an analytical specificity of < 10% cross reactivity with FSH, LH and hCG. 25-OH Vitamin D assay was shown to be 0.8% for vitamin D3 (Cholecalciferol), 0.4% for vitamin D2 (Ergocalciferol), 0.1% for 1,25-(OH)2-vitamin D3 and 0% for 1,25-(OH)2-vitamin D2. Blood samples were collected on the 2nd or 3rd day of the menstrual cycle. The reference intervals in the follicular phase were as follows: T, 0.14–0.53 ng/mL; DHEA-S, 35.0–430.0 µg/dL; FSH, 4–13 mIU/mL; LH, 1–18 mIU/mL; estradiol, 39–189 pg/mL; TSH, 0.35–4.94 μIU/mL; prolactin, 1.39–24.20 ng/mL; and 25-OH-vitamin D, 30 ~ 100 ng/mL.
Statistical analysis
The normality of the distribution was tested using the Kolmogorov–Smirnov test. Continuous variables were presented as the mean ± standard deviation. The subjects were categorized into four quartile groups (Q1 to Q4) based on serum T concentrations. Quantitative variables were evaluated using the analysis of variance (ANOVA) and linear regression analysis among T quartile categories. Bonferroni’s method was used for post hoc pairwise comparison in the ANOVA test. Generalized linear model was performed to examine the correlation between serum AMH levels and T quartile categories after adjusting for potential confounders including age, weight, BMI and FSH. Odds ratios (ORs) and 95% confidence intervals (CIs) for DOR and EOR among T quartile categories were assessed using binary logistic regression after adjustment for potential confounders (age, weight, BMI and FSH). All analyses were conducted using statistical software, Statistical Package for Social Sciences (SPSS) version 20.0 (Chicago, IL, USA). All statistical tests used a two-tailed α of 0.05, and statistical significance was defined as p < 0.05.
Ethics declarations
The study conformed to the ‘‘Declaration of Helsinki for Medical Research involving Human Subjects’’. Additionally, approval was obtained from the institutional review board at Kaohsiung Veterans General Hospital, with the identifier KSVGH20-CT11-03. The study was performed in accordance with approved guidelines. Need of informed consent was waived by the institutional review board in Kaohsiung Veterans General Hospital.
Acknowledgements
We acknowledge professor Huey-Shyan Lin for statistical counseling. We thank the Economy Company Ltd. for English editing service.
Author contributions
L.T and C.J contributed conception and design of the study; C.J organized the database; L.T performed the statistical analysis; L.T and K.H interpreted the data; L.T wrote the first draft of the manuscript; C.J and K.H substantively revised it. All authors reviewed the manuscript and approved the submitted version.
Funding
This work was generously supported by Grants from the Ministry of Science and Technology, Executive Yuan (MOST 109-2314-B-075B-014 -MY2).
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dewailly D, et al. The physiology and clinical utility of anti-Mullerian hormone in women. Hum. Reprod. Update. 2014;20:370–385. doi: 10.1093/humupd/dmt062. [DOI] [PubMed] [Google Scholar]
- 2.Jeppesen JV, et al. Which follicles make the most anti-Mullerian hormone in humans? Evidence for an abrupt decline in AMH production at the time of follicle selection. Mol. Hum. Reprod. 2013;19:519–527. doi: 10.1093/molehr/gat024. [DOI] [PubMed] [Google Scholar]
- 3.Moolhuijsen LME, Visser JA. Anti-mullerian hormone and ovarian reserve: Update on assessing ovarian function. J. Clin. Endocrinol. Metab. 2020 doi: 10.1210/clinem/dgaa513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelsey TW, Wright P, Nelson SM, Anderson RA, Wallace WH. A validated model of serum anti-müllerian hormone from conception to menopause. PLoS ONE. 2011;6:e22024. doi: 10.1371/journal.pone.0022024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lie Fong S, et al. Serum anti-müllerian hormone levels in healthy females: A nomogram ranging from infancy to adulthood. J. Clin. Endocrinol. Metab. 2012;97:4650–4655. doi: 10.1210/jc.2012-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Broer SL, et al. Prediction of an excessive response in in vitro fertilization from patient characteristics and ovarian reserve tests and comparison in subgroups: An individual patient data meta-analysis. Fertil. Steril. 2013;100:420–429.e427. doi: 10.1016/j.fertnstert.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 7.Broer SL, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: An individual patient data approach. Hum. Reprod. Update. 2013;19:26–36. doi: 10.1093/humupd/dms041. [DOI] [PubMed] [Google Scholar]
- 8.Lensen SF, et al. Individualised gonadotropin dose selection using markers of ovarian reserve for women undergoing in vitro fertilisation plus intracytoplasmic sperm injection (IVF/ICSI) Cochrane Database Syst. Rev. 2018;2:2693. doi: 10.1002/14651858.CD012693.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friis Petersen J, et al. A randomized controlled trial of AMH-based individualized FSH dosing in a GnRH antagonist protocol for IVF. Hum. Reprod. Open. 2019;2019:3. doi: 10.1093/hropen/hoz003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walters KA, Handelsman DJ. Role of androgens in the ovary. Mol. Cell. Endocrinol. 2018;465:36–47. doi: 10.1016/j.mce.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 11.Astapova O, Minor BMN, Hammes SR. Physiological and pathological androgen actions in the ovary. Endocrinology. 2019;160:1166–1174. doi: 10.1210/en.2019-00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davison SL, Davis SR. Androgens in women. J. Steroid Biochem. Mol. Biol. 2003;85:363–366. doi: 10.1016/s0960-0760(03)00204-8. [DOI] [PubMed] [Google Scholar]
- 13.Hillier SG, Tetsuka M, Fraser HM. Location and developmental regulation of androgen receptor in primate ovary. Hum. Reprod. 1997;12:107–111. doi: 10.1093/humrep/12.1.107. [DOI] [PubMed] [Google Scholar]
- 14.Davison SL, Bell R, Donath S, Montalto JG, Davis SR. Androgen levels in adult females: Changes with age, menopause, and oophorectomy. J. Clin. Endocrinol. Metab. 2005;90:3847–3853. doi: 10.1210/jc.2005-0212. [DOI] [PubMed] [Google Scholar]
- 15.Kim CH, et al. Ovarian features after 2 weeks, 3 weeks and 4 weeks transdermal testosterone gel treatment and their associated effect on IVF outcomes in poor responders. Dev. Reprod. 2014;18:145–152. doi: 10.12717/dr.2014.18.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim CH, Howles CM, Lee HA. The effect of transdermal testosterone gel pretreatment on controlled ovarian stimulation and IVF outcome in low responders. Fertil. Steril. 2011;95:679–683. doi: 10.1016/j.fertnstert.2010.07.1077. [DOI] [PubMed] [Google Scholar]
- 17.Park CH, Chun S. Influence of combined oral contraceptives on polycystic ovarian morphology-related parameters in Korean women with polycystic ovary syndrome. Obstet. Gynecol. Sci. 2020;63:80–86. doi: 10.5468/ogs.2020.63.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plouvier P, et al. Is the suppressive effect of cyproterone acetate on serum anti-Müllerian-hormone levels in women with polycystic ovary syndrome stronger than under oral contraceptive pill? Gynecol. Endocrinol. 2016;32:612–616. doi: 10.3109/09513590.2016.1145647. [DOI] [PubMed] [Google Scholar]
- 19.Vendola KA, Zhou J, Adesanya OO, Weil SJ, Bondy CA. Androgens stimulate early stages of follicular growth in the primate ovary. J. Clin. Invest. 1998;101:2622–2629. doi: 10.1172/jci2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sen A, et al. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc. Natl. Acad. Sci. U.S.A. 2014;111:3008–3013. doi: 10.1073/pnas.1318978111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laird M, et al. Androgen stimulates growth of mouse preantral follicles in vitro: interaction with follicle-stimulating hormone and with growth factors of the TGFβ superfamily. Endocrinology. 2017;158:920–935. doi: 10.1210/en.2016-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hickey TE, et al. Androgens augment the mitogenic effects of oocyte-secreted factors and growth differentiation factor 9 on porcine granulosa cells. Biol. Reprod. 2005;73:825–832. doi: 10.1095/biolreprod.104.039362. [DOI] [PubMed] [Google Scholar]
- 23.Wu YG, Bennett J, Talla D, Stocco C. Testosterone, not 5α-dihydrotestosterone, stimulates LRH-1 leading to FSH-independent expression of Cyp19 and P450scc in granulosa cells. Mol. Endocrinol. 2011;25:656–668. doi: 10.1210/me.2010-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang JL, et al. Testosterone induces redistribution of forkhead box-3a and down-regulation of growth and differentiation factor 9 messenger ribonucleic acid expression at early stage of mouse folliculogenesis. Endocrinology. 2010;151:774–782. doi: 10.1210/en.2009-0751. [DOI] [PubMed] [Google Scholar]
- 25.Vendola K, et al. Androgens promote oocyte insulin-like growth factor I expression and initiation of follicle development in the primate ovary. Biol. Reprod. 1999;61:353–357. doi: 10.1095/biolreprod61.2.353. [DOI] [PubMed] [Google Scholar]
- 26.Gleicher N, et al. Hypoandrogenism in association with diminished functional ovarian reserve. Hum. Reprod. 2013;28:1084–1091. doi: 10.1093/humrep/det033. [DOI] [PubMed] [Google Scholar]
- 27.Fuentes A, et al. Androgens profile in blood serum and follicular fluid of women with poor ovarian response during controlled ovarian stimulation reveals differences amongst POSEIDON stratification groups: A pilot study. Front. Endocrinol. 2019;10:458. doi: 10.3389/fendo.2019.00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mannerås L, et al. A new rat model exhibiting both ovarian and metabolic characteristics of polycystic ovary syndrome. Endocrinology. 2007;148:3781–3791. doi: 10.1210/en.2007-0168. [DOI] [PubMed] [Google Scholar]
- 29.Caldwell AS, et al. Characterization of reproductive, metabolic, and endocrine features of polycystic ovary syndrome in female hyperandrogenic mouse models. Endocrinology. 2014;155:3146–3159. doi: 10.1210/en.2014-1196. [DOI] [PubMed] [Google Scholar]
- 30.Taieb J, et al. FSH and its second messenger cAMP stimulate the transcription of human anti-Müllerian hormone in cultured granulosa cells. Mol. Endocrinol. 2011;25:645–655. doi: 10.1210/me.2010-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pierre A, et al. Loss of LH-induced down-regulation of anti-Müllerian hormone receptor expression may contribute to anovulation in women with polycystic ovary syndrome. Hum. Reprod. 2013;28:762–769. doi: 10.1093/humrep/des460. [DOI] [PubMed] [Google Scholar]
- 32.Durlinger AL, et al. Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinology. 2001;142:4891–4899. doi: 10.1210/endo.142.11.8486. [DOI] [PubMed] [Google Scholar]
- 33.Pellatt L, et al. Anti-Müllerian hormone reduces follicle sensitivity to follicle-stimulating hormone in human granulosa cells. Fertil. Steril. 2011;96:1246–1251.e1241. doi: 10.1016/j.fertnstert.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 34.Dewailly D, et al. Interactions between androgens, FSH, anti-Mullerian hormone and estradiol during folliculogenesis in the human normal and polycystic ovary. Hum. Reprod. Update. 2016;22:709–724. doi: 10.1093/humupd/dmw027. [DOI] [PubMed] [Google Scholar]
- 35.Cimino I, et al. Novel role for anti-Mullerian hormone in the regulation of GnRH neuron excitability and hormone secretion. Nat. Commun. 2016;7:10055. doi: 10.1038/ncomms10055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Silva MSB, Giacobini P. New insights into anti-Mullerian hormone role in the hypothalamic-pituitary-gonadal axis and neuroendocrine development. Cell Mol. Life Sci. 2020 doi: 10.1007/s00018-020-03576-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pigny P, et al. Elevated serum level of anti-mullerian hormone in patients with polycystic ovary syndrome: Relationship to the ovarian follicle excess and to the follicular arrest. J. Clin. Endocrinol. Metab. 2003;88:5957–5962. doi: 10.1210/jc.2003-030727. [DOI] [PubMed] [Google Scholar]
- 38.Dewailly D, et al. Reconciling the definitions of polycystic ovary syndrome: The ovarian follicle number and serum anti-Müllerian hormone concentrations aggregate with the markers of hyperandrogenism. J. Clin. Endocrinol. Metab. 2010;95:4399–4405. doi: 10.1210/jc.2010-0334. [DOI] [PubMed] [Google Scholar]
- 39.Lv PP, et al. Role of anti-Mullerian hormone and testosterone in follicular growth: A cross-sectional study. BMC Endocr. Disord. 2020;20:101. doi: 10.1186/s12902-020-00569-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crisosto N, et al. Testosterone-induced downregulation of anti-Müllerian hormone expression in granulosa cells from small bovine follicles. Endocrine. 2009;36:339–345. doi: 10.1007/s12020-009-9227-6. [DOI] [PubMed] [Google Scholar]
- 41.Caanen MR, et al. Antimüllerian hormone levels decrease in female-to-male transsexuals using testosterone as cross-sex therapy. Fertil. Steril. 2015;103:1340–1345. doi: 10.1016/j.fertnstert.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 42.Li Y, Wei LN, Liang XY. Follicle-stimulating hormone suppressed excessive production of antimullerian hormone caused by abnormally enhanced promoter activity in polycystic ovary syndrome granulosa cells. Fertil. Steril. 2011;95:2354–2358. doi: 10.1016/j.fertnstert.2011.03.047. [DOI] [PubMed] [Google Scholar]
- 43.Sun B, Wang F, Sun J, Yu W, Sun Y. Basal serum testosterone levels correlate with ovarian response but do not predict pregnancy outcome in non-PCOS women undergoing IVF. J. Assist. Reprod. Genet. 2014;31:829–835. doi: 10.1007/s10815-014-0246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qin Y, et al. Association of basal serum testosterone levels with ovarian response and in vitro fertilization outcome. Reprod. Biol. Endocrinol. 2011;9:9. doi: 10.1186/1477-7827-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu Q, et al. Low testosterone levels in women with diminished ovarian reserve impair embryo implantation rate: A retrospective case-control study. J. Assist. Reprod. Genet. 2014;31:485–491. doi: 10.1007/s10815-014-0186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Walters KA, et al. Steroid profiles by liquid chromatography-mass spectrometry of matched serum and single dominant ovarian follicular fluid from women undergoing IVF. Reprod. Biomed. Online. 2019;38:30–37. doi: 10.1016/j.rbmo.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 47.Noventa M, et al. Testosterone therapy for women with poor ovarian response undergoing IVF: A meta-analysis of randomized controlled trials. J. Assist. Reprod. Genet. 2019;36:673–683. doi: 10.1007/s10815-018-1383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang Y, et al. Adjuvant treatment strategies in ovarian stimulation for poor responders undergoing IVF: A systematic review and network meta-analysis. Hum. Reprod. Update. 2020;26:247–263. doi: 10.1093/humupd/dmz046. [DOI] [PubMed] [Google Scholar]
- 49.Sharpe A, Morley LC, Tang T, Norman RJ, Balen AH. Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database Syst. Rev. 2019;12:13505. doi: 10.1002/14651858.Cd013505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pundir J, et al. Inositol treatment of anovulation in women with polycystic ovary syndrome: A meta-analysis of randomised trials. BJOG. 2018;125:299–308. doi: 10.1111/1471-0528.14754. [DOI] [PubMed] [Google Scholar]
- 51.Auchus RJ. Steroid assays and endocrinology: Best practices for basic scientists. Endocrinology. 2014;155:2049–2051. doi: 10.1210/en.2014-7534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Practice Committee of the American Society for Reproductive Medicine. Electronic address, a. a. o. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil. Steril.113, 533–535, doi:10.1016/j.fertnstert.2019.11.025 (2020). [DOI] [PubMed]
- 53.Poseidon G, et al. A new more detailed stratification of low responders to ovarian stimulation: From a poor ovarian response to a low prognosis concept. Fertil. Steril. 2016;105:1452–1453. doi: 10.1016/j.fertnstert.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 54.Lauritsen MP, et al. The prevalence of polycystic ovary syndrome in a normal population according to the Rotterdam criteria versus revised criteria including anti-Mullerian hormone. Hum. Reprod. 2014;29:791–801. doi: 10.1093/humrep/det469. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.