Abstract
Background
Ethnomedicine, a study of traditional medicine, is significant in drug discovery and development. African traditional medicine has been in existence for several thousands of years, and several drugs have been discovered and developed from it.
Main text
The deadly coronavirus disease 2019 (COVID-19) caused by a novel coronavirus known as SARS-CoV-2 has widely spread globally with high mortality and morbidity. Its prevention, treatment and management still pose a serious challenge. A drug for the cure of this disease is yet to be developed. The clinical management at present is based on symptomatic treatment as presented by individuals infected and this is by combination of more than two drugs such as antioxidants, anti-inflammatory, anti-pyretic, and anti-microbials. Literature search was performed through electronic searches of PubMed, Google Scholar, and several research reports including WHO technical documents and monographs.
Conclusion
Drug discovery from herbs is essential and should be exploited for the discovery of drugs for the management of COVID-19. This review is aimed at identifying ethnomedicinal herbs available in Africa that could be used for the discovery and development of a drug for the prevention, treatment, and management of the novel coronavirus disease 2019.
Keywords: Coronavirus, SARS-CoV-2, COVID-19, Traditional medicine, Ethnomedicinal herbs
Background
Ethnomedicine is a study of traditional medicine involving bioactive compounds of plants and animals origin from diverse cultural groups. It comprises ethnobiology, ethnobotany, and ethnopharmacology. The significance of ethnomedicinal study is for drug discovery. Scientific ethnomedicinal studies have been used and adopted as a source of lead compound identification in drug discovery and development processes [1, 2].
Traditional medicine is the “sum total of the knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement, or treatment of physical and mental illness” [3]. African traditional medicine is highly dependent on cultural, religious, and spiritual belief. It is as old as the world and still in existence even after the introduction of science-based medicine by the Europeans [4].
The causative agent of the deadly coronavirus disease 2019 (COVID-19) is a novel coronavirus known as SARS-CoV-2. COVID-19 outbreak was declared as a pandemic by the World Health Organization on 11 March 2020 due to the fast, wide spread and severity of the disease in 114 countries globally. The treatment and management of the disease has posed a serious challenge. Various studies on how to mitigate the scourge of this pandemic is in progress. Studies on the use of ethnomedicinal herbs in the prevention, treatment, and management of COVID-19 are obtainable in literatures [5–7].
The clinical management of COVID-19 generally involves treatment of the symptoms associated with the disease usually involving the combination of more than two drugs such as antioxidants for the reduction of oxidative stress which may cause injury to the lung cells [8], anti-inflammatory agents for the reduction of inflammation due to rapid viral replication and cell infiltration [9], anti-pyretic agent for reduction of fever [10], anti-microbials for the reduction and treatment of opportunistic infections due to reduced immunity [11], anti-viral for inhibition of viral entry and reduction in viral replication [12], nutritional vitamins, and minerals like ascorbic acid and zinc to reinforce the immune system [13, 14].
Literature search was performed to identify and extract relevant information through electronic searches of PubMed, Google Scholar, and several research reports including WHO technical documents and monographs.
This review attempts to identify ethnomedicinal herbs (with their vernacular names for ease of identification) available in Africa that could be used to develop drugs for the prevention, treatment and management of the novel coronavirus disease 2019. Some of these plants are not indigenous to Africa but have been cultivated for their beneficial values. It is necessary to source for these herbs locally to reduce cost of research and development and for reproducibility and sustainability.
Main text
Abrus precatorius Linn. Gaertn
Family: Fabaceae
Common names: Rosary pea, Jequirity, Crab’s eyes
Local names: Mongaluchi (Swahili, Kenya); Mutiti (Lozi, Zambia) Ndela (Chagga, Tanzania); Mantumbi (Badyara, Senegal); Amabope (Ndebele, South Africa); nsimani (Tsonga, South Africa); Iwere-jeje, Ojuologbo (Yoruba, Nigeria); Anya nnunu (Igbo, Nigeria), Da marzaya (Hausa, Nigeria) [15–17].
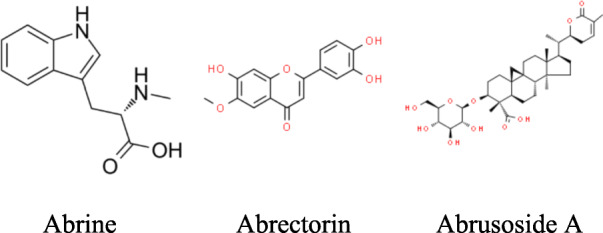
Bioactive compounds: Abrine, Abrectorin, Abrusoside A, Abricin, Abraline, Choline, Glycyrrhizin, Luteolin, Trigonelline [18, 19].
Abrus precatorius is an herbaceous, perennial, flowering climbing plant. It is indigenous to Africa, Asia, and Australia but now naturalized in many countries. The plant is widely distributed throughout Africa. The leaves are used in traditional medicine for the treatment of cough, cold, fever, conjunctivitis, pains, constipation, yellow fever, tuberculosis, and other pulmonary problems; the seeds are used as contraceptives and for the treatment of eye inflammation and joint pains; the stem bark and roots are used for the treatment of diabetes, venereal diseases, bacterial, and fungi diseases and as sedatives [15, 20].
Some of the pharmacological activities of Abrus precatorius that have been reported are anti-convulsant, anti-asthmatic, anti-inflammatory, analgesic, anti-arthritic, anti-rheumatic, anti-diabetic, anti-oxidant, anti-depressant, anti-microbial, and anti-viral activity [19, 21, 22].
The leaf and root of Abrus precatorius would be a potential source of anti-coronavirus drug since it contains glycyrrhizin as documented by [19, 23]. Several studies reported the activity of glycyrrhizin against coronaviruses [24–26].
Achyranthes aspera Linn.
Family: Amaranthaceae
Common names: Devil’s horsewhip, Prickly chaff flower
Local names: Isinama (Zulu South Africa); Moxato (Botswana); Bhomane (Lesotho); Udombo (Zimbabwe); Turura (Swahili, Kenya); Vatofosy (Madagascar); Epa aboro (Yoruba, Nigeria); Odụdu ngwele (Igbo, Nigeria) [27, 28].
Bioactive compounds: Ecdysterone, Eugenol, Betaine, Triacontanol [29].
Achyranthes aspera is an erect perennial herbal weed. The origin of the plant is not known but it is believed to be indigenous to either South Asia or/and Africa. It is widely naturalized in the tropics and sub-tropics. All the plant parts (leaves, seeds, roots, and shoots) are used in African traditional medicines for the treatment of malaria, ulcer, fever, arthritis, diarrhea, dysentery, hemorrhoids, itching, and headache [28]. It is also used as an antioxidant, anti-inflammatory agent, expectorant, diuretic, and inhalation for respiratory problems such as pneumonia and asthma [30, 31].
Achyranthes aspera possesses weak anti-viral activity [32]; however; it has good antioxidant and anti-inflammatory properties. It is rich in ascorbic acid which confers the antioxidant property that boosts immunity against infections like SARS-coronavirus [33, 34]. The anti-inflammatory properties could be beneficial in alleviating inflammation due to SARS-coronavirus [28, 35]. Achyranthes aspera will be effective in the management of COVID-19.
Allium sativum L.
Family: Liliaceae
Common names: Garlic
Local names: Thuum (Arabic, Egypt); Ivimbampunzi (Xhosa, South Africa); Kitunguu-saumu (Swahili, Tanzania); Tafarnuwa Hausa, Nigeria); Ayo-ishi (Igbo, Nigeria); Ayuu (Yoruba, Nigeria) [36–38].
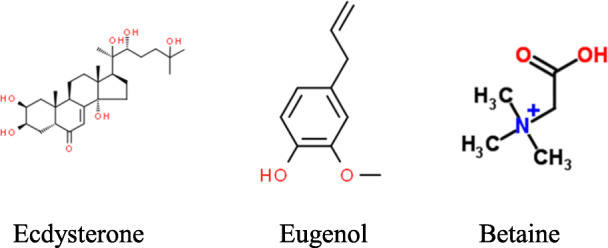
Bioactive constituents: Ajoene, Allicin, Diallyl disulfide, Vinyldithiins [39, 40].
Allium sativum is a monocotyledonous erect flowering plant native to central Asia. The plant is now widely cultivated and distributed all over the world. The part of the plant mainly utilized in traditional medicine in Africa and in other countries is the bulb. It has been used as a remedy in the past during epidemics such as amoebic dysentery, cholera, diphtheria, tuberculosis, and influenza in Egypt [41]. It is used in African traditional medicine in the treatment of skin diseases, intestinal disorders, respiratory diseases, bacterial infections, worm infestation, and tumors [42].
Pharmacological activities of garlic as highlighted in scientific literatures include anti-diabetic, anti-inflammatory, antioxidant, hepatoprotective, cardiovascular, anti-bacterial, anti-fungal, anti-viral, and anti-cancer activity [40, 42, 43].
Keyaerts et al. reported Allium sativum of possessing marked antiviral activity against coronaviruses [44]. Thuy et al. suggested Allium sativum to be a valuable source of anti-SARS-CoV-2 [45].
Annona muricata Linn.
Family: Annonaceae
Common names: Soursop, Graviola, Prickly custard apple
Local names: Soursap (Krio, Sierra Leone); Soursapi (Mende, Sierra Leone); Omusitafeli (Basoga Uganda); Ekitafeli (Baganda Uganda); Araticum (Benin); Sabasaba, Ebom beti (Cameroon); Apre (Ghana); Corossol (Madagascar); Ebo, Apekan (Yoruba, Nigeria); Fasadarur or Tuwon biri (Hausa, Nigeria); Sawansop (Ibo, Nigeria) [46–50].
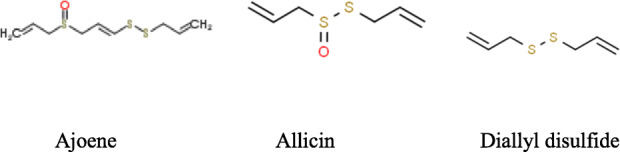
Bioactive compounds: Annonaceous acetogenins-Annocatalin, Annomuricin A, Annocatacin, Muricatocin [51].
Annona muricata is a perennial small woody evergreen tree considered to be native to North and South America. The plant is widely found in East and West Africa as cultivar. The leaf, back, root, and fruit have been in use for decades in African traditional medicine. The leaves are used as anti-inflammatory agent [52], and also used to treat diabetes, headaches, rheumatism, and insomnia [53]. The ground seeds are used to treat coughs, pain, and skin diseases [51].
Annona muricata has been reported to possess anti-microbial and anti-viral activity [54]. The seed is reported to possess anti-SARS coronavirus activity. Oyebamiji et al. discovered that Annona muricata seed has a promising ability to inhibit SARS coronavirus [55]. Trivedi et al. also highlighted that the seeds of Annona muricara can be used to inhibit COVID-19 pathway [56].
Artemisia afra Jacq. ex Willd.
Family: Asteraceae
Common names: Wild wormwood, African wormwood
Local names; Wilde-als (Afrikaans, South Africa); Umhlonyane (Xhosa, South Africa and Zimbabwe); Mhlonyane (Zulu, South Africa); Lengana (Zimbabwe); Nyumba (Luo, Kenya); Ariti (Amharic, Ethiopia) [57].
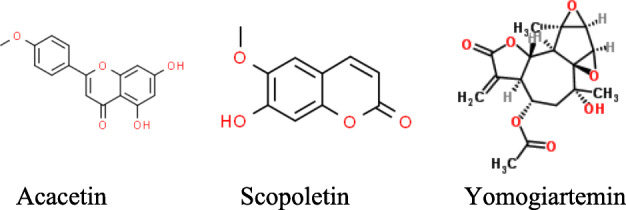
Bioactive compounds: Acacetin, Scopoletin, Yomogiartemin, Dihydroxybishopsolicepolide [58, 59].
Artemisia afra is a perennial woody shrub, a specie of Artemisia which is indigenous to Africa. It originates and widely distributed in South Africa, spreading to some countries in North and East Africa. The roots, stems, and leaves are used in African traditional medicine to treat coughs, respiratory diseases, fevers, asthma, malaria, colds, chills, gout, diabetes, influenza, and convulsions [59, 60]. Studies on the activity of the plant on viruses such as HIV and influenza have been reported in scientific publications [61, 62].
The traditional use of Artemisia afra to treat coughs, respiratory diseases like asthma, whooping cough, and bronchitis prompted researchers to carry out scientific studies on the plant to ascertain the claim of traditional practitioners. Some studies highlighted and established the activity of the plant as claimed by traditional practitioners [63, 64]. Since Artemisia afra has been established to possess activity for the treatment of respiratory diseases, it could be beneficial as a supplement in the management of SARS-coronavirus. Although there is no record in the literature which indicates that A. afra possesses activity against coronaviruses but it could be used to support the management of COVID 19.
A specie of Artemisia known Artemisia annua found in Asia has some documented scientific evidences of activity against coronaviruses [65, 66]. This plant is now widely cultivated is some countries in Africa especially East Africa (Kenya, Uganda, Tanzania, Ethiopia, Mozambique, Madagascar) [67].
Azadirachta indica A. Juss.
Family: Meliaceae
Common name: Neem
Local names: Aforo-oyinbo (Yoruba, Nigeria); Aku shorop, Ogwu iba, Ogwu akom (Igbo, Nigeria); Dogonyaro (Hausa, Nigeria); Nimtso (Krobo, Ghana); Kingtsho (Ga, Ghana); Dua gyare (Ashanti, Ghana); Liliti (Ewe, Ghana); Kinitsi (Togo); Mwarubaini, Mkilifi (Swahili, Kenya and Tanzania) [17, 68–70].
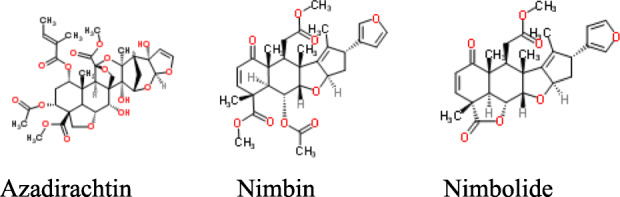
Bioactive compounds: Azadirachtin, Nimbin, Nimbolide, Nimbidin, Nimbidol [71, 72].
Azadirachta indica is an evergreen drought-resistant woody plant native to India and now widely seen growing in West and East Africa. Every part of the plant (stem, leaves, bark, roots, seeds, and flowers) has been used in traditional medicine in Nigeria and other countries like India to cure different conditions such as malaria, headache, stomach ulcers, jaundice, anemia, dental problems, bacterial, fungi, and viral infections [68, 73].
Anti-viral activity of Azadirachta indica has widely been reported on some viruses (apart from coronaviruses) such as coxsackieviruses, dengue virus, and hepatitis C virus [72, 74]. Recently, scientists have reported anti-viral activity of Azadirachta indica against coronaviruses as a result of the urgency required for the development of a specific anti-viral drug for the prevention, treatment, and management of COVID-19. Pooladanda et al. [75]; Borkotoky and Banerjee [76]; Ather and Costigliola [77] reported possible beneficial effect of Azadirachta indica in the treatment of SARS-CoV-2 infections.
Cryptolepis sanguinolenta (Lindl.) Schltr
Family: Asclepiadaceae
Common names: Ghana quinine, Yellow dye root
Local names: Nibima (Twi, Ghana); Kadze (Ewe, Ghana); Kɔli mekari (Bantu, Kenya); Paran pupa (Yoruba, Nigeria); Akpaoku (Igbo, Nigeria); Gangamau (Hausa, Nigeria); Ouidoukoi (Bambara, Mali) [78–80]..
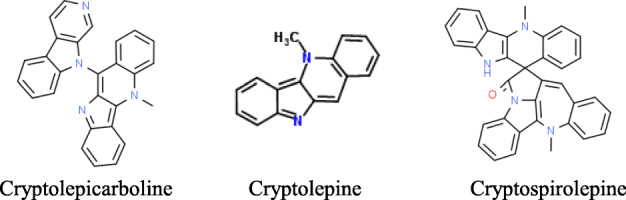
Bioactive compounds: Cryptolepicarboline, Cryptolepine, Cryptospirolepine, Cyptomisrine, Cryptoquindoline [81].
Cryptolepis sanguinolenta is a thin-stemmed, climbing, twining perennial flowering shrub. It is indigenous to Central, Eastern, and Western African regions. The root is used in African traditional medicine for the treatment of malaria, jaundice, hepatitis, hypertension, stomach and intestinal disorders, urinary and upper respiratory tract infections, rheumatism, amoebic dysentery, diarrhea, and venereal diseases [78, 82, 83]. The pharmacological activities of the plants are anti-plasmodial, anti-cancer, anti-fungal, anti-bacterial, anti-viral, hypotensive, anti-pyretic, anti-inflammatory, and anti-hyperglycemic activities [81, 84].
Cryptolepis sanguinolenta anti-viral activity on herpes implex virus 1 and 2 was reported by Buhner 2013 [85]. Gyebi et al. highlighted the plant as a potential inhibitor of coronavirus [86].
Curcuma longa Linn.
Family: Zingiberaceae
Common names: Turmeric
Local names: Mandano or Manjano (Swahili, Kenya); kurkum (Arabic, Somalia, Egypt); Ata ile pupa (Yoruba, Nigeria); Gangamau (Hausa, Nigeria); Nwandumo, Ohu boboch (Igbo, Nigeria) [87, 88].
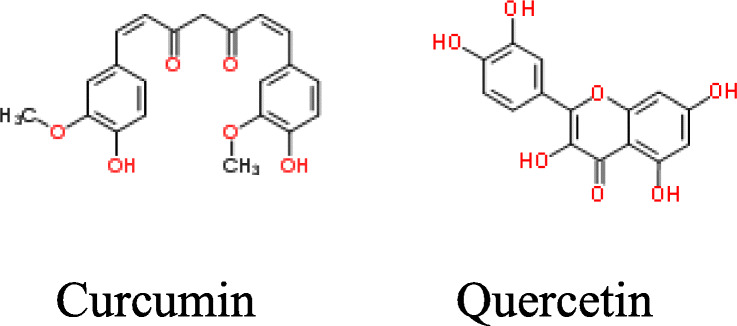
Bioactive constituents: Curcumin, Quercetin, Curcuminoids [89, 90].
Curcuma longa is a rhizomatous, perennial, small flowering herbaceous plant indigenous to South Asia. The plant is widely cultivated in many parts of East and West Africa and other continents for its culinary spicy and medicinal value. The rhizome is the most commonly used part in Africa for the traditional treatment of some ailments such as headache, skin diseases, jaundice, smallpox, microbial infections, diarrhea, diabetes, arthritis, anorexia, cough, sinusitis, conjunctivitis, and diabetic wounds [17, 91].
The pharmacological activities of Curcuma longa has been extensively studied and found to possess anti-inflammatory, anti-ulcer, antioxidant, anti-diabetic, anti-coagulant, anti-fertility, anti-neoplastic, anti-microbial, anti-viral, wound healing, cardiovascular protective, hepatoprotective, and immunostimulant activity [92, 93].
The plant has also been studied as a potential source of SARS coronavirus treatment, prevention, and management. Wen et al. [94] and Zahedipour et al. [95] reported Curcuma longa as a plant with potent anti-viral activity against SARS coronaviruses, so it could be effective in the treatment of SARS-CoV-2. Lin and Ying [96] exploited the antioxidant and anti-inflammatory activity of curcumin for the treatment of pneumonia in patients as a result of COVID-19 infection.
Euphorbia hirta Linn.
Family: Euphorbiaceae
Common names: Hairy spurge, Garden spurge, Milkweed, Asthma-plant.
Local names: Rooi euphorbia (South Africa); Makore selu (Badyara, Senegal); ku tim (Diola-flup, Senegal); Fuŋkele (Limba, Sierra Leone); kakaweadwe (Akan-Asante, Ghana); Ahinkogye (Twi, Ghana); Akubaa (Nzema, Ghana); Noonon Kurciyaa (Hausa, Nigeria); Obụ Anị, Oba Ala, Udani, ogwu ngwo (Igbo, Nigeria); Akun Esan, Buje, Ege-Ile, Emi-Ile (Yoruba, Nigeria) [97, 98].
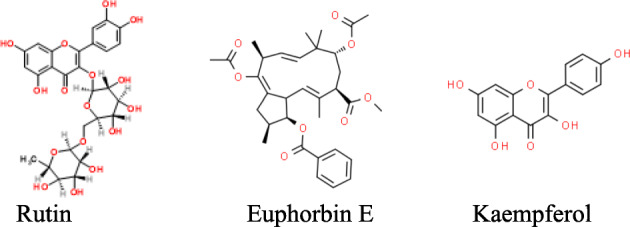
Bioactive compounds: Rutin, Euphorbin E, Kaempferol, Afzelin, Quercitrin, Myricitrin, Choline, Camphol [99].
Euphorbia hirta is a small annual hairy weed that is native to tropical America, and now widely spread to the tropics and subtropics. All the plant parts are widely used in African traditional herbal medicine for the treatment of wounds, boil, diarrhea, dysentery, respiratory and bronchial disorders, and malaria [17, 98].
Euphorbia hirta has been reported to possess anti-malarial, anti-helmintic, anti-asthmatic, anti-spasmodic, anti-fertility, sedative, wound healing, anti-bacterial, and anti-fungal properties [99, 100]. The plant was reported to possess anti-viral activity against HIV-1 and HIV-2 [101].
Euphorbia hirta has no anti-SARS-coronavirus activity but has good activity on respiratory problems which is a major symptom of coronavirus. Shahrajabian et al. listed it as one of the most important herb used for the treatment of respiratory diseases [102]. So, it can be used to support the treatment and management of COVID-19 patients. Onyeji highlighted in his study that Euphorbia Hirta can alleviate some of the respiratory symptoms associated with COVID-19 [103].
Garcinia kola Heckel
Family: Clusiaceae
Common names: Bitter kola
Local names: Tweapia (Anyi, Ghana); Akuilu (Igbo, Nigeria); Orogbo (Yoruba, Nigeria); Namijin goro (Hausa, Nigeria) [104, 105].
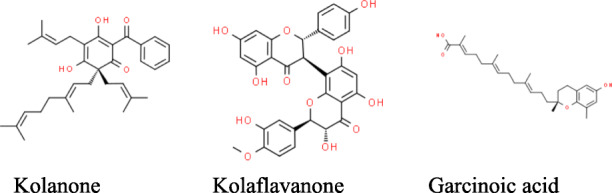
Bioactive constituents: Kolanone, Kolaflavanone, Garcinoic acid, Kolaviron, and Garciniflavanone [105, 106].
Garcinia kola is an evergreen, perennial, medium-sized flowering tree that is indigenous to Central and Western Africa especially Benin, Cameroon, Congo, Ivory Coast, Ghana, Liberia, Nigeria, and Senegal where they are mostly found and used. Every part of the plant (leaves, fruits, seeds, stems, barks, twigs, and roots) is used by African traditional medical practitioner in the treatment of various diseases such as bronchitis, throat infection, skin infection, headache, stomach ache, gastritis, cold, cough, malaria, tuberculosis, typhoid fever, malignant tumors, gonorrhea, fresh wounds, liver disorders, and jaundice [107, 108].
The pharmacological activities of the plant include anti-inflammatory, anti-oxidant, anti-asthma, anti-arthritis, anti-ulcer, anti-hypertensive, anti-microbial, anti-viral, anti-diabetic, and anti-hepatotoxic activities [106, 109].
Oladele et al. [110] observed that Garcinia kola has anti-SARS-CoV-2 inhibitory potential while Ikpa et al. [111] listed it as a plant with promising result against coronaviruses.
Glycyrrhiza glabra L.
Family: Fabaceae
Common names: Licorice
Local names: Susu (Swahili, Kenya); Dhalashada (Somali, Somalia); Irkessus (Arabic, Egypt); Ewe omisinmisin (Yoruba, Nigeria) [112, 113].
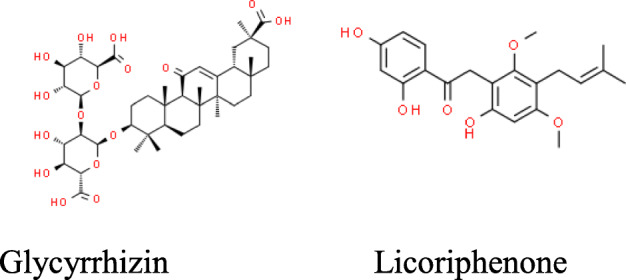
Bioactive constituents: Glycyrrhizin, Licoriphenone, Glycyrrhizic acid, Prenyllicoflavone A, etc. [114].
Glycyrrhiza glabra is an herbaceous perennial herb native to south-western Asia and southern Europe but widely cultivated for commercial purposes in North Africa (Egypt) and South Africa. The roots and rhizomes are used in ancient Egypt to treat upper respiratory disease like common cold, cough, bronchitis, and sore throats. It is used to treat heartburns and skin diseases [115].
Glycyrrhiza glabra possesses some pharmacological activities which includes anti-ulcer, anti-inflammatory, antioxidant, anti-hyperglycemic, anti-allergic, anti-cancer, anti-malarial, memory-enhancing, anti-microbial, and anti-viral activity [116, 117].
The anti-coronavirus activity of Glycyrrhiza glabra has been extensively studied and reported to be as a result of the presence of glycyrrhizic acid and glycyrrhizin [114, 118]. Several reports displaying anti-SARS-CoV activity of Glycyrrhiza glabra are highlighted in literatures. Hoever et al. confirmed in their research that licorice possesses anti-SARS-CoV [25].
In a recent study on COVID-19, Glycyrrhiza glabra was reported to successful inhibit SARS-CoV replication and was recommended for the management COVID-19 [25, 66, 119, 120].
Moringa oleifera Lam.
Family: Moringaceae
Common names: Horseradish tree, Drumstick
Local names: La-Banyu (Bwaba, Burkina Faso); Atiuwuse (Ewe, Ghana); Anamambo (Malagasy, Madagascar); Neverday (Wolof, Senega); Zagalanda (Tonga, Zambia); Mlonge (Swahili, Kenya, and Tanzania); Al-ruwag (Arabic, Sudan); Ewe ile, Ewe igbale (Yoruba , Nigeria); Odudu oyibo, Okwe oyibo (Igbo, Nigeria); Zongallagandi, Bagaruwar masar (Hausa , Nigeria) [121–123].
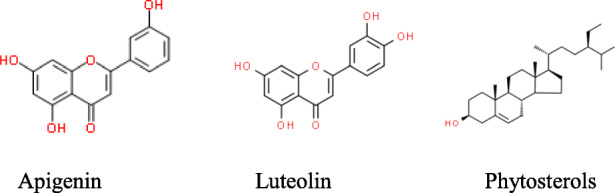
Bioactive constituents: Apigenin, Luteolin, Phytosterols, Quercetin, Terpenoids, Caffeic acid [124–126].
Moringa oleifera is a fast-growing drought-resistant, deciduous, perennial softwood tree which is native to India but now widely cultivated and naturalized in Africa and many other tropical and subtropical countries for variety of uses such as food and traditional herbal medicine. All the parts of the plant are used traditionally in many African countries for bone setting and enhancement of lactation. They are also used in the treatment of impotence, heartburn, asthma, flu, cough, pneumonia, common cold, bronchitis, syphilis, malnutrition, diabetes, hypertension, gastric ulcers, malaria, and fever [127, 128].
The pharmacological activities of Moringa oleifera are numerous and includes, analgesic, anti-inflammatory, local anesthetic, anti-allergic, anti-microbial, antioxidant, anti-cancer, cardiovascular, gastroprotective, hepatoprotective, neuroprotective, anti-ulcer, diuretic, anti-helmintic, hypoglycemic, blood lipid-reducing, immunomodulatory, and anti-diarrheal activity [124, 125, 129].
Moringa oleifera possesses some anti-viral activities but not on coronaviruses [130, 131]. However, they could be used to complement and supplement the management of SARS-CoV diseases because of its richness in minerals (zinc, potassium, calcium, magnesium), and vitamins (vitamin C) [132, 133]. Adejuwon et al. reported an herbal mixture formulation containing Moringa oleifera to possess SARS-CoV-2 inhibitory activity [134].
Nigella sativa L.
Family: Ranunculaceae
Common names: black seed, black cumin, fennel flower
Local names: Habbah Sawda’ or ‘Habbatul Barakah’ (Arabic, Egypt); Tikur azmud (Amharic, Ethopia); Habatu Sauda (Hausa, Nigeria); Asofeyeje (Yoruba, Nigeria ) [135, 136].
Bioactive compounds: Thymoquinone, Cymene, Carvacrol, Thymohydroquinone, Dihydrothymoquinone, thymol [137].
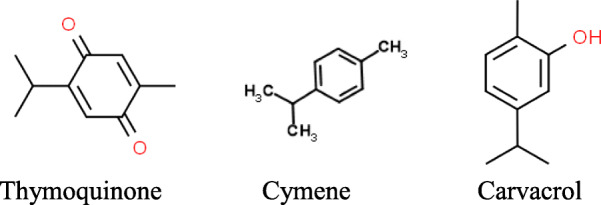
Nigella sativa is an annual flowering plant native to North Africa and some other regions like Eastern Mediterranean, the Indian subcontinent, and Southwest Asia. The seed of the plant has been in use for centuries in Africa and across many continents. It is widely used traditionally to treat asthma, cough, bronchitis, rheumatoid arthritis, diabetes, and hypertension, and to boost the body’s immune system to fight illness [138]. It possesses pharmacological properties such as anti-inflammatory, anti-cancer, analgesic, antioxidant, anti-microbial, anti-parasitic, and anti-viral properties [139, 140].
Ulasli et al. reported a decrease in the replication of Coronavirus with ethanol extract of Nigella sativa seed [141]. There are more recent studies which showed that Nigella sativa possesses potential anti-coronavirus activity [142–144].
Psidium guajava Linn.
Family: Myrtaceae
Common names: Guava
Local names: Koejawal (Afrikaans, South Africa), gouyav (Seychelles Creole, Seychelles),
Guava (Hausa, Nigeria); Gurfa (Yoruba, Nigeria); Gwaibwa (Igbo, Nigeria); Mupeera (Luganda, Uganda); Biabo (Mandinka, Mali); Mpera (Swahili, Tanzania, and Kenya); Zeitun, (Tigrigna, Eritrea) [145, 146].
Bioactive compounds: Ascorbic acid, Caryophyllene, Gallic acid [147].
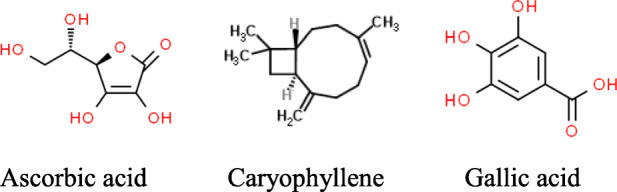
Psidium guajava is a perennial, shallow-rooted evergreen small tree; it is believed to be native to tropical America but now naturalized and widely cultivated and distributed in almost all African countries and other tropical and subtropical countries. The leaf and bark of the plant have been used for several decades in African traditional medicine. It is used for the treatment of malaria in South Africa, Nigeria, and Tanzania; treatment of hypertension and diabetes in Togo and Nigeria; tuberculosis in Nigeria; HIV in Tanzania; and bacterial infection in South Africa and Guinea [148–150].
Some of the pharmacological activities of Psidium guajava that are reported include anti-bacterial, anti-fungal, anti-hypertensive, anti-cancer, anti-inflammatory, antioxidant, immune-system stimulatory, anti-diabetic, and anti-plasmodial activities [151].
Psidium guajava was reported by Fukumoto et al. in a Taiwanese patent in 2010 to possess Anti-SARS coronavirus activity [152]. Some studies have been carried out showing that Psidium guajava has some potential bioactive compounds that can breakdown coronavirus proteins [126, 153, 154].
Zingiber officinale Roscoe
Family: Zingiberaceae
Common names: Ginger
Local names: Gnamakou (Dioula, Burkina Faso); Akakaduro (Akan, Ghana); Didière (Wolof, Senegal); Tangawizi (Swahili, Tanzania); Citta (Fulfulde, Nigeria); Citaraho (Hausa, Nigeria); Jinja (Igbo, Nigeria); Atale (Yoruba, Nigeria) [155–157].
Bioactive constituents: Zingiberene, Zingerone, Gingerol, Gingerdiol, Shogaol, Paradols, Curcumene, etc. [158, 159].
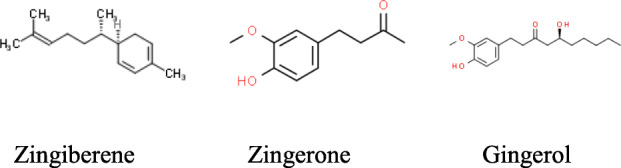
Zingiber officinale is a rhizomatous, perennial, herbaceous flowering plant which originates from Southeast Asia and now extensively cultivated in most tropical and subtropical countries including African countries like Burkina Faso, Cameroon, Ghana, Madagascar, Nigeria, Senegal, and Tanzania. All parts of the plant, especially the rhizome are used in African traditional medicine for the treatment of various conditions like indigestion, gastric ulcerations, constipation, nausea, vomiting, arthritis, rheumatism, pains, fever, cough and cold, sore throats, lung diseases, cramps, hypertension, infectious diseases, asthma, and diabetes [160, 161].
Zingiber officinale possesses high pharmacological activities such as antioxidant, anti-microbial, anti-inflammatory, anti-arthritic, anti-platelet, anti-rhinoviral, cardiovascular protection, glucose lowering, and anti-cancer activities [158, 162, 163].
Several studies on Zingiber officinale as a potential inhibitor of infections from coronaviruses have been reported in literature [126, 164, 165]. It was recommended as a component of a formulation for the treatment of SARS-CoV-2 [166, 167].
Conclusion
Drug discovery from herbs is of great importance which should be exploited for the discovery of drugs for the management of COVID-19. In this review, fifteen (15) ethnomedicinal herbs used in African traditional medicine from different countries in Africa which may be valuable in the prevention, treatment and management of coronavirus disease 2019 were identified (Table 1 and Fig. 1). Due to the complex nature of SARS-CoV-2 and clinical presentation of COVID-19 disease, combining two or more extracts with various pharmacological activity from these herbs in a standard dosage form such as capsule, tablets, syrups, and injections is necessary in the management of the disease. This combination would improve adherence but care must be taken to ensure that all ingredients in the formulation are compatible otherwise it may lead to therapeutic failure or toxicity.
Table 1.
Summary of the identified ethnomedicinal herbs
| S/N | Herb | Constituent | Pharmacological activity | Reference |
|---|---|---|---|---|
| 1. | Abrus precatorius Linn. | Abrine, Abrectorin, Abrusoside A, Abraline | Anti-convulsant, anti-asthmatic, anti-inflammatory, anti-viral | [15, 19–22] |
| 2. | Achyranthes aspera Linn. | Ecdysterone, Eugenol, Betaine, Triacontanol | Anti-inflammatory, antioxidant | [29, 33, 34] |
| 3. | Allium sativum Linn. | Ajoene, Allicin, Diallyl disulfide, Vinyldithiins | Anti-inflammatory, antioxidant, anti-viral, anti-cancer | [39, 40, 42, 43] |
| 4. | Annona muricata Linn. | Annocatalin, Annomuricin A, Annocatacin, Muricatocin | Anti-inflammatory, anti-microbial, anti-viral | [51, 52, 54] |
| 5. | Artemisia afra Jacq. | Acacetin, Scopoletin, Yomogiartemin | Anti-asthmatic, anti-malarial | [58–60] |
| 6. | Azadirachta indica A. Juss. | Azadirachtin, Nimbin, Nimbolide, Nimbidin | Anti-malarial, anti-bacterial, anti-fungal, anti-viral | [68, 71–73] |
| 7. | Cryptolepis sanguinolenta Lindl. | Cryptolepicarboline, Cryptolepine, Cryptospirolepine | Anti-inflammatory, anti-cancer anti-viral, anti-hyperglycemic | [81, 84, 85] |
| 8. | Curcuma longa Linn. | Curcumin, Quercetin, Curcuminoids | Anti-inflammatory, antioxidant, anti-diabetic, anti-coagulant, anti-microbial, anti-viral | [89, 90, 92, 93] |
| 9. | Euphorbia hirta Linn. | Rutin, Euphorbin E, Kaempferol, Afzelin | Anti-malarial, anthelmintic, anti-asthmatic, anti-spasmodic, anti-bacterial, anti-fungal, anti-viral | [99–101] |
| 10. | Garcinia kola Heckel | Kolanone, Kolaflavanone, Garcinoic acid, Kolaviron | Anti-oxidant, anti-asthma, anti-arthritis, anti-hypertensive, anti-microbial, anti-viral | [105, 106, 109] |
| 11. | Glycyrrhiza glabra Linn. | Glycyrrhizin, Licoriphenone, Glycyrrhizic acid | Anti-inflammatory, antioxidant, anti-allergic, anti-cancer, anti-microbial, anti-viral | [114, 116, 117] |
| 12. | Moringa oleifera Lam. | Apigenin, Luteolin, Phytosterols, Quercetin | Anti-inflammatory, antioxidant, anti-allergic, anti-microbial, anti-cancer, anti-ulcer, anti-viral | [124–126, 129, 130] |
| 13. | Nigella sativa Linn. | Thymoquinone, Cymene, Carvacrol, Thymohydroquinone | Anti-inflammatory, antioxidant, anti-cancer, analgesic, anti-viral anti-microbial, anti-parasitic | [137, 139, 140] |
| 14. | Psidium guajava Linn. | Ascorbic acid, Caryophyllene, Gallic acid | Anti-inflammatory, antioxidant, anti-microbial, anti-cancer, immune-system stimulatory | [147, 151] |
| 15. | Zingiber officinale Roscoe | Zingiberene, Zingerone, Gingerol, Gingerdiol | Anti-inflammatory, antioxidant, anti-microbial, anti-rhinoviral, anti-cancer | [158, 159, 162, 163] |
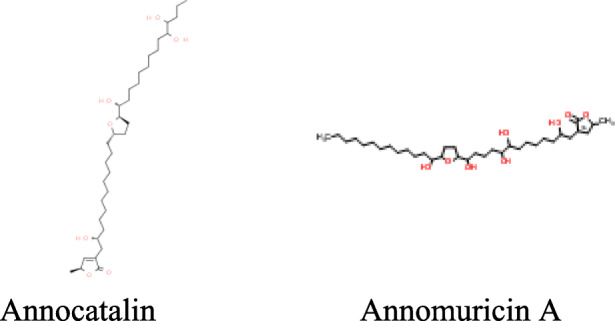
Fig. 1.
Photos of ethnomedicinal herbs with potential activity for the management of coronavirus disease 2019
In conclusion, this review will serve as a source of information for future research in the selection of herbs which could be used in the management of COVID-19. However, experimental analyses and clinical studies would be required for validation.
Acknowledgements
Not applicable.
Authors’ contributions
OAA: conception, design, literature search, drafting of the manuscript, revision of the manuscript, final approval of the manuscript. OAB: conception, design, literature search, drafting of the manuscript, revision of the manuscript, final approval of the manuscript. LG: literature search, revision of the manuscript, final approval of the manuscript. MN: conception, design, revision of the manuscript, final approval of the manuscript. AA: literature search, drafting of the manuscript, final approval of the manuscript. JS: design, revision of the manuscript, final approval of the manuscript. AO: literature search, drafting of the manuscript, final approval of the manuscript. OM: literature search, drafting of the manuscript, final approval of the manuscript. GF: literature search, drafting of the manuscript, final approval of the manuscript.
Funding
This review article did not receive funding from any agency.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Olutayo Ademola Adeleye, Email: olutayoadeleye@yahoo.com.
Mbang Nyong Femi-Oyewo, Email: mnfemioyewo@gmail.com.
Oluyemisi Adebowale Bamiro, Email: Bamroy67@yahoo.co.uk.
Lateef Gbenga Bakre, Email: lateefbakr@yahoo.com.
Akinyinka Alabi, Email: doctorakinyinkaonline@yahoo.com.
Joseph Senu Ashidi, Email: ashidisenu@yahoo.com.
Olalekan Adeyinka Balogun-Agbaje, Email: lamlexyy2@gmail.com.
Oluwakemi Mary Hassan, Email: khemihassan@gmail.com.
Gbemisola Fakoya, Email: gbemifakoya@gmail.com.
References
- 1.Johnson M, Sargent CF. Medical anthropology: Contemporary theory and method. Connecticut: Praeger; 1996. Ethnopharmacology: the conjunction of medical ethnography and the biology of therapeutic action; pp. 132–133. [Google Scholar]
- 2.Patwrdhan BK, Vaidya BD, Chorghade M. Ayurveda and natural products drug discovery. Curr Sci. 2004;86(6):789–799. [Google Scholar]
- 3.WHO . Traditional medicine: definitions. World Health Organization Fact sheet N°134. 2008. [Google Scholar]
- 4.Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8:115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benarba B, Pandiella A. Medicinal plants as sources of active molecules against COVID-19. Front Pharmacol. 2020;11:1189. doi: 10.3389/fphar.2020.01189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boukhatem MN, Setzer WN. Aromatic herbs, medicinal plant-derived essential oils, and phytochemical extracts as potential therapies for Coronaviruses: Future perspectives. Plants (Basel) 2020;9(6):800. doi: 10.3390/plants9060800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maxmen A. More than 80 clinical trials launch to test coronavirus treatments. Nature. 2020;578(7795):347–348. doi: 10.1038/d41586-020-00444-3. [DOI] [PubMed] [Google Scholar]
- 8.Ntyonga-Pono MP. COVID-19 infection and oxidative stress: an under-explored approach for prevention and treatment? Pan Afr Med. 2020;35(Suppl 2):12. doi: 10.11604/pamj.2020.35.2.22877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Runfeng L, Yunlong H, Jicheng H, Weiqi P, Quihai M, Yongxia S, et al. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol Res. 2020;156:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ang L, Song E, Lee HW, Lee MS. Herbal medicine for the treatment of coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis of randomized controlled trials. J Clin Med. 2020;9(5):1583. doi: 10.3390/jcm9051583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rossato L, Negrão FJ, Simionatto S. Could the COVID-19 pandemic aggravate antimicrobial resistance. Am J Infect Control. 2020;48(9):1129–1130. doi: 10.1016/j.ajic.2020.06.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panyod S, Ho CT, Sheen LY. Dietary therapy and herbal medicine for COVID-19 prevention: A review and perspective. J Tradit Complement. 2020;10(4):420–427. doi: 10.1016/j.jtcme.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aman F, Masood S. How nutrition can help to fight against COVID-19 pandemic. Pak J Med Sci. 2020;36(COVID19-S4):S121–S123. doi: 10.12669/pjms.36.COVID19-S4.2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar A, Kubota Y, Chernov M, Kasuya H. Potential role of zinc supplementation in prophylaxis and treatment of COVID-19. Med Hypotheses. 2020;144:109848. doi: 10.1016/j.mehy.2020.109848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erinoso SM, Aworinde DO. Ethnobotanical survey of some medicinal plants used in traditional health care in Abeokuta areas of Ogun State, Nigeria. Afr J Pharm Pharmaco. 2012;6(18):1352–1362. [Google Scholar]
- 16.Tandiwe N, Thulisile J. Abrus precatorius L. subsp. africanus Verdc. Leguminosae: Papilionoideae. Flowering Plants Afr. 2013;63:50–55. [Google Scholar]
- 17.Iwu MM. Handbook of African medicinal plants. 2. London: Taylor and Francis; 2014. [Google Scholar]
- 18.Garaniya N, Bapodra A. Ethno botanical and Phytophrmacological potential of Abrus precatorius L.: A review. Asian Pac J Trop Biomed. 2014;4(Suppl 1):S27–S34. doi: 10.12980/APJTB.4.2014C1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jain A, Gupta PP. In silico comparative molecular docking study and analysis of glycyrrhizin from Abrus precatorius (L.) against ntidiabetic activity. Eur J Med Plants. 2015;6(4):212–222. doi: 10.9734/EJMP/2015/13855. [DOI] [Google Scholar]
- 20.Umaru IJ, Aduwamai UH, Umaru FJ, John KI, Umaru M, Usman A, et al. Evaluation of some medicinal plants diversity and compendium information on the usage in Michika, Adamawa state. South Asian Res J Bio Appl Biosci. 2020;2(3):38–46. doi: 10.36346/sarjbab.2020.v02i03.003. [DOI] [Google Scholar]
- 21.Taur DJ, Patil RN, Patil RY. Antiasthmatic related properties of Abrus precatorius leaves on various models. J Tradit Complement Med. 2017;7(4):428–432. doi: 10.1016/j.jtcme.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mondal S, Ghosh S, Anusuri KC, Ganapaty S. Toxicological studies and assessment of pharmacological activities of Abrus precatorius L. (Fabaceae) ethanolic leaves extract in the management of pain, psychiatric and neurological conditions-An in-vivo study. J Appl Pharm Sci. 2017;7:207–216. doi: 10.7324/JAPS.2017.70229. [DOI] [Google Scholar]
- 23.Karwasara VS, Jain R, Tomar P, Dixit VK. Elicitation as yield enhancement strategy for glycyrrhizin production by cell cultures of Abrus precatorius Linn. In Vitro Cell Dev Biol Plant. 2010;46(4):354–362. doi: 10.1007/s11627-010-9278-7. [DOI] [Google Scholar]
- 24.Hoever G, Baltina L, Michaelis M, Kondratenko R, Tolstikov GA, Doer HW, et al. Antiviral activity of glycyrrhizic acid derivatives against SARS-coronavirus. J Med Chem. 2005;48(4):1256–1259. doi: 10.1021/jm0493008. [DOI] [PubMed] [Google Scholar]
- 25.Murck H. Symptomatic protective action of glycyrrhizin (Licorice) in COVID-19 infection? Front Immunol. 2020;11:1239. doi: 10.3389/fimmu.2020.01239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo P, Liu D, Li J. Pharmacological perspective: glycyrrhizin may be an efficacious therapeutic agent for COVID-19. Int J Antimicrob Agents. 2020;55(6):105995. doi: 10.1016/j.ijantimicag. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quattrocchi U. CRC world dictionary of plant names, common names, scientific names, eponyms, synonyms, and etymology. Florida: CRC Press; 1999. [Google Scholar]
- 28.Sharma V, Chaudhary U. An overview on indigenous knowledge of Achyranthes aspera. J Crit Rev. 2015;2(1):7–19. [Google Scholar]
- 29.Praveen KS. Achyranthes aspera: A potent immunostimulating plant for traditional medicine. Int J Pharm Sci Res. 2014;5(5):1601–1611. doi: 10.13040/IJPSR.0975-8232.5(5).1601-11. [DOI] [Google Scholar]
- 30.Ajibesin KK, Ekpo BA, Bala DN, Essien EE, Adesanya SA. Ethnobotanical survey of Akwa Ibom State of Nigeria. J Ethnopharmacol. 2008;115(3):387–408. doi: 10.1016/j.jep.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 31.Edwin S, Jarald SE, Deb L, Jain A, Kinger H, Dutt KR, et al. Wound healing and antioxidant activity of Achyranthes aspera. Pharm Bio. 2008;46(12):824–828. doi: 10.1080/13880200802366645. [DOI] [Google Scholar]
- 32.Mukherjee H, Ojha D, Bag P, Chandel HS, Bhattacharyya S, Chatterjee TK, Mukherjee PK, Chakraborti S, Chattopadhyay D. Anti-herpes virus activities of Achyranthes aspera: An Indian ethnomedicine, and its triterpene acid. Microbiol Res. 2013;168(4):238–244. doi: 10.1016/j.micres.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Beaulah A, Sadiq M, Santhi J. Antioxidant and antibacterial activity of Achyranthes aspera: An in vitro study. Der Pharma Chemica. 2011;3(5):662–670. [Google Scholar]
- 34.Carr AC, Maggini S. Vitamin C and immune function. Nutrients. 2017;9(11):1211. doi: 10.3390/nu9111211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vetrichelvan T, Jegadeesan M. Effect of alcohol extract of Achyranthes aspera Linn. on acute and subacute inflammation. Phytother Res. 2003;17(1):77–79. doi: 10.1002/ptr.1070. [DOI] [PubMed] [Google Scholar]
- 36.Sihotang VB. Ethnomedicinal study of the Sundanese people at the Bodogol area, Gede Pangrango Mountain National Park, West Java. Gard Bull Singapore. 2011;63:519–526. [Google Scholar]
- 37.Asowata-Ayodele AM, Afolayan AJ, Otunola GA. Ethnobotanical survey of culinary herbs and spices used in the traditional medicinal system of Nkonkobe Municipality, Eastern Cape, South Africa. South Afr J Bot. 2016;104:69–75. doi: 10.1016/j.sajb.2016.01.001. [DOI] [Google Scholar]
- 38.Tijani K, Alfa A, Sezor A. Studies on phytochemical, nutraceutical profiles and potential medicinal values of Allium sativum Linn (Lilliaceae) on bacterial meningitis. Int Neuropsych Dis J. 2019;13(2):1–15. doi: 10.9734/indj/2019/v13i230105. [DOI] [Google Scholar]
- 39.Zeng Y, Li Y, Yang J, Pu X, Du J, Yang X, et al. Therapeutic role of functional components in Alliums for preventive chronic disease in human being. Evid Based Complement Altern Med. 2017;2017:1–13. doi: 10.1155/2017/9402849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Batiha GE, Beshbishy AM, Wasef LG, Elewa YH, Al-Sagan AA, Abd El-Hack ME, et al. Chemical constituents and pharmacological activities of garlic (Allium sativum L.): A review. Nutrients. 2020;12(3):872. doi: 10.3390/nu12030872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petrovska BB, Cekovska S. Extracts from the history and medical properties of garlic. Pharmacogn Rev. 2010;4(7):106–110. doi: 10.4103/0973-7847.65321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sulaiman FA, Kazeem MO, Waheed AM, Temowo SO, Azeez IO, Faridat I, et al. Antimicrobial and toxic potential of aqueous extracts of Allium sativum, Hibiscus sabdariffa and Zingiber officinale in Wistar rats. J Taibah Univ Sci. 2014;8(4):315–322. doi: 10.1016/j.jtusci.2014.05.004. [DOI] [Google Scholar]
- 43.Kumar P, Yadav J, Jain M, Yadav P, Goel AK, Yadava PM. Bactericidal efficacy of Allium sativum (garlic) against multidrug resistant Vibrio cholerae o1 epidemic strains. Defence Sci J. 2016;66(5):479–484. doi: 10.14429/dsj.66.10701. [DOI] [Google Scholar]
- 44.Keyaerts E, Vijgen L, Pannecouque C, Damme EV, Peumans W, Egberink H, et al. Plant lectins are potent inhibitors of coronaviruses by interfering with two targets in the viral replication cycle. Antiviral Res. 2007;75(3):179–187. doi: 10.1016/j.antiviral.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thuy BT, My TT, Hai NT, Hieu LT, Hoa TT, Loan HT, et al. Investigation into SARS-CoV-2 resistance of compounds in garlic essential oil. ACS Omega. 2020;5(14):8312–8320. doi: 10.1021/acsomega.0c00772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Asase A, Hesse DN, Simmonds MS. Uses of multiple plants prescriptions for treatment of malaria by some communities in southern Ghana. J Ethnopharmacol. 2012;144(2):448–452. doi: 10.1016/j.jep.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 47.Roger T, Pierre-Marie M, Igor V, Patrick V. Phytochemical screening and antibacterial activity of medicinal plants used to treat typhoid fever in Bamboutos division, West Cameroon. J Appl Pharm Sci. 2015;5(6):34–49. doi: 10.7324/JAPS.2015.50606. [DOI] [Google Scholar]
- 48.Ssenyange CW, Namulindwa A, Oyik B, Ssebuliba J. Plants used to manage type II diabetes mellitus in selected districts of central Uganda. Afri Health Sci. 2015;15(2):496–502. doi: 10.4314/ahs.v15i2.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Coria-Téllez A, Montalvo-Gonzalez E, Yahia E, Obledo-Vázquez E. Annona muricata: a comprehensive review on its traditional medicinal uses, phytochemicals, pharmacological activities, mechanisms of action and toxicity. Arab J Chem. 2018;11(5):662–691. doi: 10.1016/j.arabjc.2016.01.004. [DOI] [Google Scholar]
- 50.Gavamukulya Y, Wamunyokoli F, El-Shemy HA. Annona muricata: Is the natural therapy to most disease conditions including cancer growing in our backyard? A systematic review of its research history and future prospects. Asian Pac J Trop Med. 2017;10(9):835–848. doi: 10.1016/j.apjtm.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 51.Moghadamtousi SZ, Fadaeinasab M, Nikzad S, Mohan G, Ali HM, Kadir HA. Annona muricata (Annonaceae): A review of its traditional uses, isolated acetogenins and biological activities. Int J Mol Sci. 2015;16(7):15625–15658. doi: 10.3390/ijms160715625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abdul Wahab SM, Jantan I, Haque MA, Arshad L. Exploring the leaves of Annona muricata L. as a source of potential anti-inflammatory and anticancer agents. Front Pharmacol. 2018;9:661. doi: 10.3389/fphar.2018.00661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adewole SO, Caxton-Martins EA. Morphological changes and hypoglycemic effects of Annona muricata Linn. (Annonaceae) leaf aqueous extract on pancreatic B-cells of streptozotocin-treated diabetic rats. Afr J Biomed Res. 2006;9:173–187. doi: 10.4314/ajbr.v9i3.48903. [DOI] [Google Scholar]
- 54.Wahab NZ, Ibrahim N, Kamarudin MK, Lananan F, Juahir H, Ghazali A, et al. Cytotoxicity and antiviral activity of Annona muricata aqueous leaves extract against dengue virus type 2. J Fundam Appl Sci. 2018;10(1S):580–589. doi: 10.4314/jfas.v10i1s.41. [DOI] [Google Scholar]
- 55.Oyebamiji AK, Oladipo EK, Olotu TM, Awoyelu HE, Adamolekun E, Semire B. In-vitro investigation on selected compounds in Annona muricata seed: A potential SARS-CoV nsp12 polymerase inhibitors down regulating 2019-nCoV. Int J Trad Nat Med. 2020;10(1):13–23. [Google Scholar]
- 56.Trivedi GN, Karlekar JT, Dhameliya HA, Panchal H. A review on the novel coronavirus disease based on in-silico analysis of various drugs and target proteins. J Pure Appl Microbiol. 2020;14(suppl 1):849–860. doi: 10.22207/JPAM.14.SPL1.22. [DOI] [Google Scholar]
- 57.Liu NQ, Van der Kooy F, Verpoorte R. Artemisia afra: A potential flagship for African medicinal plants? S Afr J Bot. 2009;75(2):185–195. doi: 10.1016/j.sajb.2008.11.001. [DOI] [Google Scholar]
- 58.More G, Lall N, Hussein A, Tshikalange TM (2012) Antimicrobial constituents of Artemisia afra Jacq. ex Willd. against periodontal pathogens. Evid Based Complement Altern Med. 10.1155/2012/252758 [DOI] [PMC free article] [PubMed]
- 59.Moyo P, Kunyane P, Selepe MA, Eloff JN, Niemand J, Louw AI, Maharaj VJ, Birkholtz LM. Bioassay-guided isolation and identification of gametocytocidal compounds from Artemisia afra (Asteraceae) Malar J. 2019;18(1):65. doi: 10.1186/s12936-019-2694-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thring SA, Weitz FM. Medicinal plant use in the Bredasdorp/Elim region of the Southern Overberg in the Western Cape Province of South Africa. J Ethnopharmacol. 2006;103(2):261–275. doi: 10.1016/j.jep.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 61.Lubbe A, Seibert I, Klimkait T, der Kooy F. Ethnopharmacology in overdrive: The remarkable anti-HIV activity of Artemisia annua. J Ethnopharmacol. 2012;1419(3):854–859. doi: 10.1016/j.jep.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 62.Salehi B, Kumar NVA, Şener B, Sharifi-Rad M, Kılıç M, Mahady GB, Vlaisavljevic S, Iriti M, Kobarfard F, Setzer W, Ayatollahi S, Ata A, Sharifi-Rad J. Medicinal plants used in the treatment of human immunodeficiency virus. Int J Mol Sci. 2018;19(5):1459. doi: 10.3390/ijms19051459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.WHO (2019) Technical document of the use of non-pharmaceutical forms of Artemisia; Malaria Policy Advisory Committee Meeting 2–4 October 2019. Geneva, World Health Organisation Technical report document
- 64.van de Venter M, Pruissen M, Koekemoer T, Sowemimo A, Govender S. In vitro anti-HIV and -TB activities of Annona muricata and Artemisia afra extracts. Planta Med. 2014;80:P1L29. doi: 10.1055/s-0034-1394687. [DOI] [Google Scholar]
- 65.Li SY, Chen C, Zhang HQ, Guo HY, Wang H, Wang L, Zhang X, Hua SN, Yu J, Xiao PG, Li RS, Tan X. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antiviral Res. 2005;67(1):18–23. doi: 10.1016/j.antiviral.2005.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Orhan IE, Senol Deniz FS. Natural products as potential leads against coronaviruses: could they be encouraging structural models against SARS-CoV-2? Nat Prod Bioprospect. 2020;10(4):171–186. doi: 10.1007/s13659-020-00250-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Willcox ML, Burton S, Oyweka R, Namyalo R, Challand S, Lindsey K. Evaluation and pharmacovigilance of projects promoting cultivation and local use of Artemisia annua for malaria. Malar J. 2011;10(1):84. doi: 10.1186/1475-2875-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ogbuewu IP, Odoemenam VU, Obikaonu HO, Opara MN, Emenalom OO, Uchegbu MC. The growing importance of neem (Azadirachta indica a. juss) in agriculture, industry, medicine and environment: A review. Res J Med Plants. 2011;5:230–245. doi: 10.3923/rjmp.2011.230.245. [DOI] [Google Scholar]
- 69.Kumar VS, Navaratnam V. Neem (Azadirachta indica): prehistory to contemporary medicinal uses to humankind. Asian Pac J Trop Biomed. 2013;3(7):505–514. doi: 10.1016/S2221-1691(13)60105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Amoateng P, Quansah E, Karikari TK, Asase A, Osei-Safo D, Kukuia KW et al (2018) Medicinal plants used in the treatment of mental and neurological disorders in Ghana. Evid Based Complement Altern Med. 10.1155/2018/8590381 [DOI] [PMC free article] [PubMed]
- 71.Xuan TD, Tsuzuki E, Hiroyuki T, Mitsuhiro M, Khanh TD, Chung I. Evaluation on phytotoxicity of neem (Azadirachta indica A. Juss) to crops and weeds. Crop Prot. 2004;23(4):335–345. doi: 10.1016/j.cropro.2003.09.004. [DOI] [Google Scholar]
- 72.Ashfaq UA, Jalil A, Ul Qamar MT. Antiviral phytochemicals identification from Azadirachta indica leaves against HCV NS3 protease: an in silico approach. Nat Prod Res. 2016;30(16):1866–1869. doi: 10.1080/14786419.2015.1075527. [DOI] [PubMed] [Google Scholar]
- 73.Iyare EE, Obaji NN. Effects of aqueous leaf extract of azadirachta indica on some haematological parameters and blood glucose level in female rats. Niger J Exp Clin Biosci. 2014;2(1):54. doi: 10.4103/2348-0149.135731. [DOI] [Google Scholar]
- 74.Dwivedi VD, Tripathi IP, Mishra SK. In silico evaluation of inhibitory potential of triterpenoids from Azadirachta indica against therapeutic target of dengue virus, NS2B-NS3 protease. J Vector Borne Dis. 2016;53(2):156–161. [PubMed] [Google Scholar]
- 75.Pooladanda V, Thatikonda S, Godugu C. The current understanding and potential therapeutic options to combat COVID-19. Life Sci. 2020;254:117765. doi: 10.1016/j.lfs.2020.117765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Borkotoky S, Banerjee M (2020) A computational prediction of SARS-CoV-2 structural protein inhibitors from Azadirachta indica (Neem). J Biomol Struct Dyn:1–17. 10.1080/07391102.2020.1774419 [DOI] [PMC free article] [PubMed]
- 77.Ather A, Costigliola V. Treatment and control of Covid-19 (Corona Virus Disease 2019) by non-invasive (h.i.p) non-drug therapy in combination anti-influenza an (Oseltamivir (rx) Tamiflue) drug-novel case report. Int J Life Sci. 2020;6(2):2480–2486. doi: 10.21276/SSR-IIJLS.2020.6.2.1. [DOI] [Google Scholar]
- 78.Tempesta MS. The clinical efficacy of Cryptolepis sanguinolenta in the treatment of malaria. Ghana Med J. 2010;44(1):1–2. [PMC free article] [PubMed] [Google Scholar]
- 79.Odoh UE, Akwuaka C. Pharmacognostic profile of root of Cryptolepis sanguinolenta (lindl.) Schlechter Pharmacogn J. 2012;4(28):40–44. doi: 10.5530/pj.2012.28.8. [DOI] [Google Scholar]
- 80.Martey ON, Shittah-Bay O, Owusu J, Okine LK. The antiplasmodial activity of an herbal antimalarial, am 207 in plasmodium berghei-infected balb/c mice: Absence of organ specific toxicity. J Med Sci. 2013;13(7):537–545. doi: 10.3923/jms.2013.537.545. [DOI] [Google Scholar]
- 81.Osafo N, Mensah KB, Yeboah OK (2017) Phytochemical and pharmacological review of Cryptolepis sanguinolenta (Lindl.) Schlechter. Adv Pharmacol Sci:3026370. 10.1155/2017/3026370 [DOI] [PMC free article] [PubMed]
- 82.Sofowora A. Medicinal plants and traditional medicine in Africa. Chichester: Wiley; 1982. pp. 221–223. [DOI] [PubMed] [Google Scholar]
- 83.Addy M. Cryptolepis: An african traditional medicine that provides hope for Malaria victims. Herbal Gram. 2003;60:54–59. [Google Scholar]
- 84.Amissah JN, Osei-Safo D, Asare CM, Missah-Assihene B, Danquah EY, Addae-Mensah I. Influence of age and staking on the growth and cryptolepine concentration in cultivated roots of Cryptolepis sanguinolenta (Lindl.) Schlt. J Med Plants Res. 2016;10(9):113–121. doi: 10.5897/JMPR2015.5793. [DOI] [Google Scholar]
- 85.Gyebi GA, Ogunro OB, Adegunloye AP, Ogunyemi OM, Afolabi SO (2020) Potential inhibitors of coronavirus 3-chymotrypsin-like protease (3CLpro): an insilico screening of alkaloids and terpenoids from African medicinal plants. J Biomol Struct Dyn.:1–13. 10.1080/07391102.2020.1764868 [DOI] [PMC free article] [PubMed]
- 86.Buhner SH. In: Natural remedies for emerging resistant and epidemic viral infections: Herbal antivirals. Ringer N, editor. Massachusetts: Storey; 2013. [Google Scholar]
- 87.WHO . Monographs on selected medicinal plants. 1999. [Google Scholar]
- 88.Nwaekpe JO, Anyaegbunam HN, Okoye BC, Asumugha GN. Promotion of turmeric for the food/pharmaceutical industry in Nigeria. Am J Exp Agric. 2015;8(6):335–341. [Google Scholar]
- 89.Sahne F, Mohammadi M, Najafpour GD, Moghadamnia AA. Enzyme-assisted ionic liquid extraction of bioactive compound from turmeric (Curcuma longa L.): Isolation, purification and analysis of curcumin. Indusrial Crops and Products. Ind Crops Prod. 2017;95:686–694. doi: 10.1016/j.indcrop.2016.11.037. [DOI] [Google Scholar]
- 90.Pal K, Chowdhury S, Dutta SK, Chakraborty S, Chakraborty M, Pandit GK, et al. Analysis of rhizome colour content, bioactive compound profiling and ex-situ conservation of turmeric genotypes (Curcuma longa L.) from sub-Himalayan terai region of India. Ind Crops Prod. 2020;150:112401. doi: 10.1016/j.indcrop.2020.112401. [DOI] [Google Scholar]
- 91.Omosa LK, Midiwo O, Kuete V. Medicinal spices and vegetables from Africa therapeutic potential against metabolic, inflammatory, infectious and systemic diseases, Curcuma longa. Amsterdam: Elservier; 2017. pp. 425–435. [Google Scholar]
- 92.Ayati Z, Ramezani M, Amiri MS, Moghadam AT, Rahimi H, Abdollahzade A, Sahebkar A, Emami SA. Ethnobotany, phytochemistry and traditional uses of curcuma spp. and pharmacological profile of two important species (C. longa and C. zedoaria): A review. Curr Pharm Des. 2019;25(8):871–935. doi: 10.2174/1381612825666190402163940. [DOI] [PubMed] [Google Scholar]
- 93.Saronee F, Bekinbo MT, Ojeka SO, Dapper DV. Comparative assessment of methanolic extracts of hog plum (spondias mombin linn.) leaves and turmeric (Curcuma longa L.) rhizomes on blood glucose and glycosylated haemoglobin in male wistar rats. J Appl Sci Environ Manage. 2019;23(9):1631–1636. [Google Scholar]
- 94.Wen CC, Kuo YH, Jan JT, Liang PH, Wang SY, Liu HG, Lee CK, Chang ST, Kuo CJ, Lee SS, Hou CC, Hsiao PW, Chien SC, Shyur LF, Yang NS. Specific plant terpenoids and lignoids possess potent antiviral activities against severe acute respiratory syndrome coronavirus. J Med Chem. 2007;50(17):4087–4095. doi: 10.1021/jm070295s. [DOI] [PubMed] [Google Scholar]
- 95.Zahedipour F, Hosseini SA, Sathyapalan T, Majeed M, Jamialahmadi T, Al-Rasadi K, et al. Potential effects of curcumin in the treatment of COVID -19 infection. Phytother Res. 2020;34(11):1–10. doi: 10.1002/ptr.6738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Liu Z, Ying Y. The inhibitory effect of curcumin on virus-induced cytokine storm and its potential use in the associated severe pneumonia. Front Cell Dev Biol. 2020;8:479. doi: 10.3389/fcell.2020.00479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ampong-Nyarko K, De Datta SK. A handbook for weed control in rice. Manila: IRRI; 1991. [Google Scholar]
- 98.Jeje TO, Ibraheem O, Brai BIC, Ibukun EO. Pharmacological potential of asthma weed (euphorbia hirta) extract toward eradication of plasmodium berghei in infected albino mice. Int J Toxicol Pharmacol Res. 2016;8(3):130–137. [Google Scholar]
- 99.Kumar S, Malhotra R, Kumar D. Euphorbia hirta: Its chemistry, traditional and medicinal uses, and pharmacological activities. Pharmacogn Rev. 2010;4(7):58–61. doi: 10.4103/0973-7847.65327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tuhin RH, Begum M, Rahman M, Karim R, Begum T, Ahmed SU, et al. Wound healing effect of Euphorbia hirta linn. (Euphorbiaceae) in alloxan induced diabetic rats. BMC Complement Altern Med. 2017;17:423. doi: 10.1186/s12906-017-1930-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gyuris A, Szlávik L, Minárovits J, Vasas A, Molnár J, Hohmann J. Antiviral activities of extracts of Euphorbia hirta L. against HIV-1, HIV-2 and SIVmac251. In Vivo. 2009;23(3):429–432. [PubMed] [Google Scholar]
- 102.Shahrajabian MH, Sun W, Shen H, Cheng Q. Chinese herbal medicine for SARS and SARS-CoV-2 treatment and prevention, encouraging using herbal medicine for COVID-19 outbreak. Acta Agr Scand B-S P. 2020;70(5):437–443. [Google Scholar]
- 103.Onyeji C. Management of coronavirus disease 2019 (covid-19) – is there a role for complementary and herbal medicinal products? Afr J Complement Altern Med. 2020;17(1):33–38. doi: 10.21010/ajtcam.v17i1.4. [DOI] [Google Scholar]
- 104.AduTutu M, Afful Y, Asante-Appiah K, Lieberman D, Hall JB, Elvin-Lewis M. Chewing stick usage in Southern Ghana. Econ Bot. 1979;33(3):320–328. doi: 10.1007/BF02858262. [DOI] [Google Scholar]
- 105.Ekene EN, Erhirhie EO. Garcinia kola: A review of its ethnomedicinal, chemical and pharmacological properties. Int J Cur Res Rev. 2014;6(11):1–7. [Google Scholar]
- 106.Kalu WO, Okafor PN, Ijeh II, Eleazu C. Effect of kolaviron, a biflavanoid complex from Garcinia kola on some biochemical parameters in experimentally induced benign prostatic hyperplasic rats. Biomed Pharmacother. 2016;83:1436–1443. doi: 10.1016/j.biopha.2016.08.064. [DOI] [PubMed] [Google Scholar]
- 107.Seanego CT, Ndip RN. Identification and antibacterial evaluation of bioactive compounds from Garcinia kola (Heckel) seeds. Molecules. 2012;17(6):6569–6584. doi: 10.3390/molecules17066569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Konziase B. Protective activity of biflavanones from Garcinia kola against Plasmodium infection. J Ethnopharmacol. 2015;172(22):214–218. doi: 10.1016/j.jep.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 109.Maňourová A, Leuner O, Tchoundjeu Z, Van Damme P, Verner V, Přibyl O, et al. Medicinal potential, utilization and domestication status of bitter kola (Garcinia kola Heckel) in West and Central Africa. Forests. 2019;10(2):124. doi: 10.3390/f10020124. [DOI] [Google Scholar]
- 110.Oladele JO, Ajayi EI, Oyeleke OM, Oladele OT, Olowookere BD, Adeniyi BM, Oyewole OI, Oladiji AT. A systematic review on COVID-19 pandemic with special emphasis on curative potentials of Nigeria based medicinal plants. Heliyon. 2020;6(9):e04897. doi: 10.1016/j.heliyon.2020.e04897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ikpa BC, Maduka OD, Christian EE, Ikezu JM. Potential plants for treatment and management of COVID-19 in Nigeria. Academic J Chem. 2020;5(6):69–80. doi: 10.32861/ajc.56.69.80. [DOI] [Google Scholar]
- 112.WHO . Monographs on medicinal plants commonly used in the Newly Independent States (NIS) 2010. [Google Scholar]
- 113.Lim TK. Edible medicinal and non-medicinal plants. 2015. Glycyrrhiza glabra; pp. 354–457. [Google Scholar]
- 114.Batiha GE, Beshbishy AM, El-Mleeh A, Abdel-Daim MM, Devkota HP. Traditional uses, bioactive chemical constituents, and pharmacological and toxicological activities of Glycyrrhiza glabra L. (Fabaceae) Biomolecules. 2020;10(3):352. doi: 10.3390/biom10030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Watt JM, Breyer-Brandwijk MG. Medicinal and poisonous plants of Southern and Eastern Africa. Edinburgh: Livingstone; 1962. p. 1457. [Google Scholar]
- 116.Karahan F, Avsar C, Ozyigit II, Berber I. Antimicrobial and antioxidant activities of medicinal plant Glycyrrhiza glabra var. glandulifera from different habitats. Biotech Biotech Equip. 2016;30(4):797–804. doi: 10.1080/13102818.2016.1179590. [DOI] [Google Scholar]
- 117.Kuang Y, Li B, Fan J, Qiao X, Ye M. Antitussive and expectorant activities of licorice and its major compounds. Biol Org Med Chem. 2018;26(1):278–284. doi: 10.1016/j.bmc.2017.11.046. [DOI] [PubMed] [Google Scholar]
- 118.Sun ZG, Zhao TT, Lu N, Yang YA, Zhu HL. Research progress of glycyrrhizic acid on antiviral activity. Mini Rev Med Chem. 2019;19(10):826–832. doi: 10.2174/1389557519666190119111125. [DOI] [PubMed] [Google Scholar]
- 119.Mirzaie A, Halaji M, Dehkordi FS, Ranjbar R, Noorbazargan H. A narrative literature review on traditional medicine options for treatment of corona virus disease 2019 (COVID-19) Complement Ther Clin Pract. 2020;40:101214. doi: 10.1016/j.ctcp.2020.101214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chen L, Hu C, Hood M, Zhang X, Zhang L, Kan J, du J. A novel combination of vitamin C, curcumin and glycyrrhizic acid potentially regulates immune and inflammatory response associated with coronavirus infections: a perspective from system biology analysis. Nutrients. 2020;12(4):1193. doi: 10.3390/nu12041193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fahey JW. Moringa oleifera: A review of the medical evidence for its nutritional therapeutic, and prophylactic properties. Part 1. Trees Life J. 2005;1(5):1–24. doi: 10.1201/9781420039078.ch12. [DOI] [Google Scholar]
- 122.Popoola JO, Obembe OO. Local knowledge, use pattern and geographical distribution of Moringa oleifera Lam. (Moringaceae) in Nigeria. J Ethnopharmacol. 2013;150(2):682–691. doi: 10.1016/j.jep.2013.09.043. [DOI] [PubMed] [Google Scholar]
- 123.Olsen ME, Palada MC, Foidl N, Bate RM. Botany and propagation In: Ebert AW, Joshi RC (eds) The miracle tree: Moringa oleifera. Indiana: Xlibris Corporation; 2019. [Google Scholar]
- 124.Vergara-Jimenez M, Almatrafi MM, Fernandez ML. Bioactive components in Moringa oleifera leaves protect against chronic disease. Antioxidants (Basel) 2017;6(4):91. doi: 10.3390/antiox6040091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Leone A, Spada A, Battezzati A, Schiraldi A, Aristil J, Bertoli S. Cultivation, Genetic, Ethnopharmacology, Phytochemistry and Pharmacology of Moringa oleifera Leaves: An overview. Int J Mol Sci. 2015;16(12):12791–12835. doi: 10.3390/ijms160612791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Laksmiani NL, Larasanty LP, Santika AJ, Prayoga PA, Dewi AK, Dewi NK. Active Compounds Activity from the Medicinal Plants Against SARS-CoV-2 using in Silico Assay. Biomed Pharmacol J. 2020;13(2):873–881. doi: 10.13005/bpj/1953. [DOI] [Google Scholar]
- 127.Khalafalla MM, Abdellatef E, Dafalla HM, Nassrallah AA, Aboul-Enein KM, Lightfoot DA, et al. Active principle from Moringa oleifera Lam leaves effective against two leukemias and a hepatocarcinoma. Afr J Biotechnol. 2010;9(49):8467–8471. doi: 10.5897/AJB10.996. [DOI] [Google Scholar]
- 128.Matic I, Guidi A, Kenzo M, Mattei M, Galgani A. Investigation of medicinal plants traditionally used as dietary supplements: A review on Moringa oleifera. J Public Health Afr. 2018;9(3):841. doi: 10.4081/jphia.2018.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bhattacharya A, Tiwari P, Sahu PK, Kumar S. A review of the phytochemical and pharmacological characteristics of Moringa oleifera. J Pharm Bioallied Sci. 2018;10(4):181–191. doi: 10.4103/JPBS.JPBS_126_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Naithani R, Mehta RG, Shukla D, Chandersekera SN, Moriarty RM. Antiviral activity of phytochemicals: A current perspective. In: Watson R, Zibadi S, Preedy V, editors. Dietary components and immune function. New Jersey: Humana Press; 2010. [Google Scholar]
- 131.Imran I, Altaf I, Ashraf M, Javeed A, Munir N. In vitro evaluation of antiviral activity of leaf extracts of Azadirachta indica, Moringa oleifera, and Morus alba against the foot and mouth disease virus on BHK-21 cell line. Sci Asia. 2016;42(6):392–396. doi: 10.2306/scienceasia1513-1874.2016.42.392. [DOI] [Google Scholar]
- 132.Olson ME, Sankaran RP, Fahey JW, Grusak MA, Odee D, Nouman W. Leaf protein and mineral concentrations across the “miracle tree” genus Moringa. PLoS ONE. 2016;11(7):e0159782. doi: 10.1371/journal.pone.0159782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rasha KA, Elsharbasy FS, Fadlelmula AA. Nutritional values of moringa oleifera, total protein, amino acid, vitamins, minerals, carbohydrates, total fat and crude fiber, under the semi-arid conditions of Sudan. J Microb Biochem Technol. 2018;10(2):56–58. doi: 10.4172/1948-5948.1000396. [DOI] [Google Scholar]
- 134.Shaji D (2020) Computational Identification of drug lead compounds for COVID-19 from Moringa Oleifera. ChemRxiv. Preprint. 10.26434/chemrxiv.12535913.v1
- 135.Padhye S, Banerjee S, Ahmad A, Mohammad R, Sarkar FH. From here to eternity - the secret of Pharaohs: Therapeutic potential of black cumin seeds and beyond. Cancer Ther. 2008;6(b):495–510. [PMC free article] [PubMed] [Google Scholar]
- 136.Yimer EM, Tuem KB, Karim A, Ur-Rehman N, Anwar F (2019) Nigella sativa L. (Black Cumin): A promising natural remedy for wide range of illnesses. Evid Based Complement Alternat Med. 10.1155/2019/1528635 [DOI] [PMC free article] [PubMed]
- 137.Sahak MK, Kabir N, Abbas G, Draman S, Hashim NH, Hasan Adli DS. The role of nigella sativa and its active constituents in learning and memory. Evid Based Complement Alternat Med. 2016;2016:1–6. doi: 10.1155/2016/6075679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ahmad A, Husain A, Mujeeb M, Khan SA, Najmi AK, Siddique NA. A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pac J Trop Biomed. 2013;3(5):337–352. doi: 10.1016/S2221-1691(13)60075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Islam MT, Khan MR, Mishra SK. Phytochemistry, pharmacology and therapeutic promises of Nigella sativa L. Orient Pharm Exp Med. 2018;19(2):115–129. doi: 10.1007/s13596-019-00363-3. [DOI] [Google Scholar]
- 140.Molla S, Azad MK, Al Hasib MA, Hossain MM, Ahammed MS, Rana S, et al. A review on antiviral effects of Nigella sativa L. Pharmacologyonline. 2019;2:47–53. [Google Scholar]
- 141.Ulasli M, Gurses SA, Bayraktar R, Yumrutas O, Oztuzcu S, Igci M, Igci YZ, Cakmak EA, Arslan A. The effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) extracts on the replication of coronavirus and the expression of TRP genes family. Mol Biol Rep. 2014;41(3):1703–1711. doi: 10.1007/s11033-014-3019-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Eldeeb E, Belal A. Two promising herbs that may help in delaying corona virus progression. Int J Trend Sci Res Dev. 2020;4(4):764–766. [Google Scholar]
- 143.Koshak AE, Koshak EA. Nigella sativa L as a potential phytotherapy for coronavirus disease 2019: A mini review of in silico studies. Curr Ther Res. 2020;93:100602. doi: 10.1016/j.curtheres.2020.100602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rahman MT. Potential benefits of combination of nigella sativa and zn supplements to treat COVID-19. J Herb Med. 2020;23:100382. doi: 10.1016/j.hermed.2020.100382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.El-Mahmood MA. The use of Psidium guajava Linn. in treating wound, skin and soft tissue infections. Sci Res Essay. 2009;4(6):605–611. [Google Scholar]
- 146.Barbalho SM, Farinazzi-Machado FM, Goulart RA, Brunnati AS, Ottoboni AM, Nicolau CC. Psidium Guajava (Guava): A Plant of Multipurpose Medicinal Applications. Med Aromat Plants. 2012;1(4):1–6. doi: 10.4172/2167-0412.1000104. [DOI] [Google Scholar]
- 147.El-Ahmady SH, Ashour ML, Wink M. Chemical composition and anti-inflammatory activity of the essential oils of Psidium guajava fruits and leaves. J Essent Oil Res. 2013;25(6):475–481. doi: 10.1080/10412905.2013.796498. [DOI] [Google Scholar]
- 148.Magassouba FB, Diallo A, Kouyaté M, Mara F, Mara O, Bangoura O, Camara A, Traoré S, Diallo AK, Zaoro M, Lamah K, Diallo S, Camara G, Traoré S, Kéita A, Camara MK, Barry R, Kéita S, Oularé K, Barry MS, Donzo M, Camara K, Toté K, Berghe DV, Totté J, Pieters L, Vlietinck AJ, Baldé AM. Ethnobotanical survey and antibacterial activity of some plants used in Guinean traditional medicine. J Ethnopharmacol. 2007;114(1):44–53. doi: 10.1016/j.jep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 149.Gutiérrez RM, Mitchell S, Solis RV. Psidium guajava: A review of its traditional uses, phytochemistry and pharmacology. J Ethnopharmacol. 2008;117(1):1–27. doi: 10.1016/j.jep.2008.01.025. [DOI] [PubMed] [Google Scholar]
- 150.Innocent E, Hassanali A, Kisinza WN, Mutalemwa PP, Magesa S, Kayombo E. Anti-mosquito plants as an alternative or incremental method for malaria vector control among rural communities of Bagamoyo District, Tanzania. J Ethnobiol Ethnomed. 2014;10(1):56. doi: 10.1186/1746-4269-10-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Irondi EA, Agboola SO, Oboh G, Boligon AA, Athayde ML, Shode FO. Guava leaves polyphenolics-rich extract inhibits vital enzymes implicated in gout and hypertension in vitro. J Intercult Ethnopharmacol. 2016;5(2):122–130. doi: 10.5455/jice.20160321115402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fukumoto S, Goto T, Hayashi S. Anti-SARS coronavirus agent, and product containing anti-SARS coronavirus agent. Taiwan Patent TW201018473A, 15 April 2010. 2010. [Google Scholar]
- 153.Tungadi R, Tuloli TS, Abdulkadir W, Thomas N, Hasan AM, Sapiun Z, et al. COVID-19: Clinical characteristics and molecular levels of candidate compounds of prospective herbal and modern drugs in Indonesia. Pharm Sci. 2020;26(Covid-19):S12–S23. doi: 10.34172/PS.2020.49. [DOI] [Google Scholar]
- 154.Erlina L, Paramita RI, Kusuma WA, Fadilah F, Tedjo A, Pratomo IP, et al. Virtual screening on Indonesian herbal compounds as COVID-19 supportive therapy: machine learning and pharmacophore modeling approaches. BMC Med Inform Decis. 2020;1(6):2–35. doi: 10.21203/rs.3.rs-29119/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sombie EN, Tibiri A, Ndo JY, Traore TK, Ouedraogo N, Hilou A, et al. Ethnobotanical study and antioxidant activity of anti-hepatitis plants extracts of the COMOE province. Burkina Faso Int J Biol Chem.Sci. 2018;12(3):1308–1319. doi: 10.4314/ijbcs.v12i3.19. [DOI] [Google Scholar]
- 156.Oforma CC, Udourioh GA, Ojinnaka CM. Characterization of essential oils and fatty acids composition of stored ginger (Zingiber officinale Roscoe) J Appl Sci Environ Manage. 2019;23(12):2231–2238. [Google Scholar]
- 157.Diatta K, Diatta W, Fall AD, Dieng SIM, Mbaye AI, Sarr A, Seye MB. Ethnopharmacological survey of medicinal plants used to treat human diseases in the Tivaouane Department, Senegal. Eur J Med Plants. 2019;30(3):1–13. doi: 10.9734/ejmp/2019/v30i330178. [DOI] [Google Scholar]
- 158.Taoheed AA, Tolulope AA, Saidu AB, Odewumi O, Sunday RM, Usman M. Phytochemical properties, proximate and mineral composition of Curcuma longa Linn. and Zingiber officinale Rosc.: A comparative study. J Sci Res Rep. 2017;13(4):1–7. doi: 10.9734/JSRR/2017/32623. [DOI] [Google Scholar]
- 159.Mao QQ, Xu XY, Cao SY, Gan RY, Corke H, Beta T, Li HB. Bioactive compounds and bioactivities of ginger (Zingiber officinale Roscoe) Foods. 2019;8(6):185–190. doi: 10.3390/foods8060185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Abdurahman HN, Ranitha M, Azhari HN. Extraction and characterization of essential oil from Ginger (Zingiber officinale roscoe) and Lemongrass (Cymbopogon citratus) by microwave-assisted Hydrodistillation. Int J Chem Environ Eng. 2013;4:221–226. [Google Scholar]
- 161.Otunola GA, Afolayan AJ. Antidiabetic effect of combined spices of Allium sativum, Zingiber officinale and Capsicum frutescens in alloxan-induced diabetic rats. Front Life Sci. 2015;4(4):314–323. doi: 10.1080/21553769.2015.1053628. [DOI] [Google Scholar]
- 162.Kumar NV, Murthy PS, Manjunatha JR, Bettadaiah BK. Synthesis and quorum sensing inhibitory activity of key phenolic compounds of ginger and their derivatives. Food Chem. 2014;159:451–457. doi: 10.1016/j.foodchem.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 163.Zhang M, Viennois E, Prasad M, Zhang Y, Wang L, Zhang Z, et al. Edible ginger-derived nanoparticles: a novel therapeutic approach for the prevention and treatment of inflammatory bowel disease and colitis-associated cancer. Biomaterials. 2016;101:321–340. doi: 10.1016/j.biomaterials.2016.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rathinavel T, Palanisamy M, Palanisamy S, Subramanian A, Thangaswamy S. Phytochemical 6-Gingerol – a promising drug of choice for COVID-19. Int J Adv Sci Eng. 2020;6(4):1482–1489. doi: 10.29294/IJASE.6.4.2020.1482-1489. [DOI] [Google Scholar]
- 165.Mbadiko CM, Inkoto CL, Gbolo BZ, Lengbiye EM, Kilembe JT, Matondo A, Mwanangombo DT, Ngoyi EM, Bongo GN, Falanga CM, Tshibangu DST, Tshilanda DD, Ngbolua KTN, Mpiana PT. A mini review on the phytochemistry, toxicology and antiviral activity of some medically interesting zingiberaceae species. J Complement Alt Med Res. 2020;9(4):44–56. doi: 10.9734/jocamr/2020/v9i430150. [DOI] [Google Scholar]
- 166.Prasad A, Muthamilarasan M, Prasad M. Synergistic antiviral effects against SARS-CoV-2 by plant-based molecules. Plant Cell Rep. 2020;39(9):1109–1114. doi: 10.1007/s00299-020-02560-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Cinatl J, Morgenstern B, Bauer G, Chandra P, Rabenau H, Doerr HW (2003) Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet 361(9374):2045–6. 10.1016/S0140-6736(03)13615-X [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.



