Abstract
The ability to identify and label one’s emotions is associated with effective emotion regulation, rendering emotional awareness important for mental health. We evaluated how emotional awareness was related to psychopathology and whether low emotional awareness was a transdiagnostic mechanism explaining the increase in psychopathology during the transition to adolescence and as a function of childhood trauma—specifically violence exposure. In Study 1, children and adolescents (N=120, aged 7–19 years) reported on emotional awareness and psychopathology. Emotional awareness was negatively associated with psychopathology (p-factor) and worsened across age in females but not males. In Study 2 (N=262, aged 8–16 years), we replicated these findings and demonstrated longitudinally that low emotional awareness mediated increases in p-factor as a function of age in females and violence exposure. These findings indicate that low emotional awareness may be a transdiagnostic mechanism linking adolescent development, sex, and trauma with the emergence of psychopathology.
Emotional awareness reflects one’s subjective understanding of their emotional state (Lane & Schwartz, 1987; Lumley et al., 2007). Emotional awareness is central to the experience of discrete emotions (Barrett, 2006) and is thought to be a prerequisite to many forms of effective emotion regulation (Barrett et al., 2001; Kalokerinos et al., 2019). Low emotional awareness is associated with many forms of psychopathology (Deborde et al., 2015; Frewen et al., 2008; Hendryx et al., 1991), suggesting that it may represent a transdiagnostic factor associated with increased vulnerability for psychopathology. We investigate this possibility in the current study. We additionally evaluate whether low emotional awareness is a mechanism that contributes to other well-established patterns of risk for transdiagnostic psychopathology. Specifically, we test whether low emotional awareness explains increases in transdiagnostic psychopathology symptoms during the transition to adolescence and as a function of exposure to trauma in childhood—specifically, interpersonal violence exposure. Greater insight into these transdiagnostic mechanisms may inform the development of more effective early interventions for broad mental health problems.
The construct of emotional awareness can be understood through the lens of the constructionist model of emotion, which posits that individuals use emotion concepts to “construct” specific emotional experiences from an instance of core affect, one’s momentary neurophysiological state that emerges within an environmental context (Barrett, 2006, 2017). Thus, emotional awareness requires perceiving one’s internal bodily state—a process called interoception—and conceptualizing it in terms of an emotion label that best unites the current context with past experience (Satpute & Lindquist, 2019). This construction of an emotional experience then guides regulatory responses to the individual’s current context (Kashdan et al., 2015). As such, factors that give rise to individual differences in interoception or emotion conceptualization across development may influence emotional awareness, emotion regulation, and ultimately psychopathology (Brewer et al., 2015; Murphy et al., 2017).
Although one might posit that emotional awareness should improve across adolescence as individuals master increasingly sophisticated emotional and non-emotional language (Nook, Sasse, Lambert, McLaughlin, & Somerville, 2017), adolescents actually exhibit greater difficulty differentiating their emotions compared to both younger and older ages (Nook, Sasse, Lambert, McLaughlin, & Somerville, 2018). These opposing forces impacting emotion conceptualization across age (i.e., increasing verbal abilities vs. decreasing ease at identifying emotional states) could generate either increased or decreased emotional awareness. In fact, studies on the development of emotional awareness have produced inconsistent results: Some studies show increased emotional awareness across ages 11–18 (Gatta et al., 2014; Säkkinen et al., 2007), but others find decreased emotional awareness with pubertal development (van der Cruijsen et al., 2019). If emotional awareness decreases during the transition to adolescence, it might be one factor explaining the well-established increase in risk for psychopathology that emerges transdiagnostically during this period (Kessler et al., 2005).
In addition to these developmental patterns, exposure to childhood adversity—particularly trauma exposure—is a potent risk factor for multiple forms of psychopathology (Green et al., 2010; McLaughlin et al., 2012), as well as for the transdiagnostic general psychopathology factor (i.e., p-factor) (Caspi et al., 2014; Weissman, Bitran, et al., 2019). Trauma exposure may contribute to lower emotional awareness through impacts on both interoception and emotion conceptualization. Exposure to extreme or uncontrollable stressors during childhood—like exposure to violence and other forms of trauma—has been associated with blunted autonomic nervous system and cortisol reactivity to stressors as well as disruptions in diurnal cortisol patterns, typically with low morning levels and a shallow decline across the day (Carpenter et al., 2011; Gordis et al., 2010; Gunnar & Vazquez, 2001; Harkness et al., 2011; Heleniak et al., 2016; MacMillan et al., 2009; McLaughlin, Sheridan, et al., 2014; Trickett et al., 2010). These changes to physiological stress response systems may weaken the coupling between subjective experiences of negative emotion and corresponding physiological reactivity, ultimately manifesting as low emotional awareness.
Indeed, childhood adversity, including violence exposure, is associated with problems identifying and differentiating between emotions (Pears & Fisher, 2005; Shenk et al., 2013), which may be attributable to less frequent use of emotional words and poorer scaffolding of emotional concepts and experiences by parents (Denham, Mitchell-Copeland, Strandberg, Auerbach, & Blair, 1997; Pollak, Cicchetti, Hornung, & Reed, 2000; Salmon, O’Kearney, Reese, & Fortune, 2016). Children exposed to violence become particularly attuned to the detection of anger at the expense of differentiating between other negative emotions (Pollak et al., 2000; Pollak & Sinha, 2002; Shenk et al., 2013). Thus, violence exposure may contribute to reduced sensitivity to changes in one’s own bodily state as well as a more limited emotional vocabulary and less differentiated emotion concepts. Consistent with this possibility, exposure to stressful life events in adolescence prospectively predicts declines in emotional awareness over time (McLaughlin et al., 2009; McLaughlin & Hatzenbuehler, 2009).
Existing evidence suggests that low emotional awareness (i.e. alexithymia) may be a factor that contributes to the association of multiple risk factors with transdiagnostic psychopathology. Indeed, low emotional awareness is associated with many forms of psychopathology, including substance abuse (Rybakowski et al., 1988; Taylor et al., 1990), conduct disorder (Deborde et al., 2015), depression (Honkalampi et al., 2002), anxiety (Hendryx et al., 1991), PTSD (Frewen et al., 2008), obsessive compulsive disorder (Grabe et al., 2006), and schizophrenia (van ‘t Wout et al., 2007). Two potential pathways could explain these associations. First, low emotional awareness may disrupt the ability to regulate emotions (Barrett et al., 2001; Kalokerinos et al., 2019). Second, because low emotional awareness is associated with more difficulty recognizing emotions in others (Grynberg et al., 2012), low emotional awareness could impair social functioning and in turn contribute to multiple forms of psychopathology (Collin et al., 2013). Both of these pathways could explain why low emotional awareness may be a transdiagnostic mechanism conveying risk for multiple forms of psychopathology emerging in middle childhood and adolescence.
In line with this perspective, recent conceptualizations of psychopathology have shifted away from categorical diagnoses and instead advocated for focusing on underlying dimensions that reflect broader psychopathology. Empirical evidence supports the existence of a transdiagnostic psychopathology factor, termed the general factor or p-factor, that reflects the co-occurrence of psychopathology symptoms in children, adolescents, and adults (Caspi et al., 2014; Castellanos-Ryan et al., 2016; Gomez et al., 2018; Laceulle et al., 2015; Lahey et al., 2012; Martel et al., 2017; Murray et al., 2016; Neumann et al., 2016; Patalay et al., 2015; Schaefer et al., 2018; Snyder et al., 2017). Adolescence is a period of risk for the onset of most forms of psychopathology (Kessler et al., 2005), and considerable evidence supports the notion that childhood violence exposure is associated with transdiagnostic risk for psychopathology (Caspi et al., 2014; Keyes et al., 2012; Weissman, Bitran, et al., 2019). However, the mechanisms that underlie this transdiagnostic risk have only recently been examined. In prior work, we demonstrated that elevations in emotional reactivity, engagement in maladaptive emotion regulation strategies (e.g., rumination), and altered patterns of neural response in the brain’s salience network to threat cues are mechanisms linking childhood violence exposure with the emergence of psychopathology over time (Weissman, Bitran, et al., 2019; Weissman, Jenness, et al., 2019). Here, we investigate whether low emotional awareness may be an additional mechanism linking both adolescent development and violence exposure with the p-factor.
We investigated factors that influence emotional awareness in childhood and adolescence and the association between self-reported emotional awareness and the p-factor in two studies. In Study 1 we modeled the structure of psychopathology in a community sample of children and adolescents and evaluated the age-related differences in p-factor and self-reported emotional awareness, and the association between emotional awareness the p-factor concurrently. In Study 2, we extended this work by examining the influence of both age and childhood violence exposure on emotional awareness and the p-factor both concurrently and prospectively over time. Finally, we investigated whether low emotional awareness was a mechanism underlying the association of age and violence exposure with increases in the p-factor over time. Given prior work suggesting that the developmental trajectory of emotional awareness varies in males and females (van der Cruijsen et al., 2019), we also investigated whether sex was related to emotional awareness or moderated associations of age and violence exposure with emotional awareness in both studies.
Study 1
Method
The following are all the measures, conditions, and data exclusions evaluated in this investigation.
Participants.
Data were drawn from a cross-sectional study of emotional development (Nook et al., 2017a, 2018a, 2019) conducted in a community sample spanning ages 4 to 25 years. Psychopathology measures were only validated for participants aged 7–19 years. Thus, our analytic sample was restricted to the 120 participants (62 female) in this age range. Participants’ races were Asian American (n=5, 4%), Black (n=12, 10%), Latinx (n=9, 8%), White (n=77, 64%), Multi-racial (n=15, 13%), and “Other” (n=2, 2%). All participants were native English speakers who were compensated for their time and recruited from communities surrounding Harvard University and the University of Washington. Participants provided informed written consent/assent, and minor participants received written permission for their participation from a parent or legal guardian. The Committee on the Use of Human Subjects at Harvard University and the University of Washington Institutional Review Board approved all research procedures.
Emotional awareness.
Low emotional awareness was measured using 12 items (e.g. “I have feelings I can’t quite identify”) from the Alexithymia Questionnaire for Children, excluding the 8 items of the externally oriented thinking subscale, which has low reliability in children and adolescents (Rieffe et al., 2006). Items are rated on a 5-point Likert scale from “Strongly Disagree” to “Strongly Agree.” This scale reliably measures low emotional awareness in children and adolescents (Heaven et al., 2010; Loas et al., 2017) and had good internal consistency in this sample (α =.89). Higher scores indicate lower emotional awareness. Emotional awareness measures were available for 104 of the 120 participants.
Symptoms of psychopathology.
Depression symptoms were assessed via child self-report with the Children’s Depression Inventory-2 (CDI), a recently revised version of the widely used self-report measure of depressive symptoms in children and adolescents (Kovacs, 1992, 2011). The CDI has demonstrated good reliability and validity among children and adolescents (Craighead et al., 1998), and it demonstrated excellent internal consistency in our sample (α = .90). Nine participants exceeded a recommended cutoff score of 15 for depression on the CDI. Anxiety symptoms were assessed via child self-report with the Screen for Child Anxiety Related Emotional Disorders (SCARED), which measures anxiety disorder symptoms across five domains: panic/somatic, generalized anxiety, separation anxiety, social phobia, and school phobia (Birmaher et al., 1997). The SCARED has sound psychometric properties (Birmaher et al., 1997, 1999) and excellent internal consistency in our sample (α = .93). Sixteen participants exceeded a recommended cutoff score of 25 for anxiety on the SCARED. Externalizing symptoms were assessed using both child and caregiver reports on the Youth Self-Report (YSR) and Child Behavior Checklist (CBCL) (Achenbach, 1991). The YSR/CBCL scales are among the most widely used measures of youth emotional and behavioral problems. Eleven participants exceeded a recommended a cutoff T-score of 65 for Externalizing Problems on the YSR/CBCL. The higher raw score between the CBCL and YSR was used from the Attention Problems, Rule Breaking Behaviors, and Aggressive Behavior subscales. Symptoms of PTSD were assessed using child- and parent-report versions of the UCLA PTSD Reaction Index (PTSD-RI) (The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index, 2004). The PTSD-RI assesses PTSD re-experiencing, avoidance/numbing, and hyper-arousal symptoms according to DSM-IV criteria. A total symptom severity score is generated by summing all items. The PTSD-RI has sound psychometric properties (Steinberg et al., 2013), and had excellent internal consistency in our sample (α = .92). The higher of the parent and child reported PTSD symptom severity score was used. Five participants exceeded a recommended cutoff score of 35 for PTSD. The use of the higher of parent or child report on the CBCL, YSR, and PTSD-RI is an implementation of the standard “or” rule used in combining parent and child reports of psychopathology. In this approach, if either a parent or child endorses a particular symptom, it is counted, and the reporter endorsing the higher level of symptoms or impairment is used. This is a standard approach in the literature on child psychopathology - for example it is how mental disorders are diagnosed in population-based studies of psychopathology in children and adolescents (e.g. Kessler et al., 2012; Merikangas et al., 2010).
Defining p-factor.
Following Caspi et al. (2014) and recent replications (Laceulle et al., 2015; Schaefer et al., 2018; Weissman, Bitran, et al., 2019), we performed confirmatory factor analysis (CFA) to test two standard models: a correlated-factors model specifying Internalizing and Externalizing latent factors and a bi-factor model specifying both a General Psychopathology latent factor (p-factor) and residual Internalizing and Externalizing factors. In order to ensure that our latent factors were not being driven by one or more indicators simply because of measurement differences across psychopathology instruments (i.e., different number of items, scoring, etc.), we binned scores on each indicator into deciles prior to CFA analyses. We used this method to transform skewed and zero-inflated data and place it on the same scale for CFA. We used deciles because this is the maximum number of bins allowed in MPlus. Supplemental analyses binning scores by quartiles instead of deciles did not meaningfully change the results (see Supplemental Materials). All CFA analyses were performed in MPlus version 8.1 (Muthén & Muthén, 2012). Given that our observed indicator variables were slightly skewed and kurtotic, we used the robust maximum likelihood estimator (MLR), which employs a sandwich estimator to arrive at standard errors robust to non-normality of observations. MLR performs well in modest sample sizes with skewed data, as in the present study (Li, 2016). We assessed the relative fit of each model using the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC) and the Sample Adjusted BIC.
Analysis.
Linear regression was used to evaluate associations of age, sex, and their interaction with low emotional awareness and of low emotional awareness with latent factor scores for psychopathology, controlling for age, sex, and their interaction. All data and code are available at https://github.com/dgweissman/EMAware_P.
Results
Model of general psychopathology.
In initial models, PTSD symptoms did not load significantly onto the general factor in the bifactor model or to the internalizing factor in the correlated-factors model. Therefore, PTSD symptoms were excluded from final models. Consistent with prior work, the bifactor and correlated-factors model provided similar fit to the data. Fit indices for the bi-factor model were: AIC = 2681.05, BIC = 2869.94, Sample adjusted BIC = 2708.20. Standardized factor loadings for the latent p-factor ranged from 0.47 to 0.93 (all p’s < .001). Fit indices for the correlated-factors model were: AIC = 2684.00, BIC = 2825.50, Sample adjusted BIC = 2676.76. Standardized factor loadings for the Internalizing (CDI, SCARED) latent factor were 0.99 and 0.67 respectively, both p’s <.001. Standardized factor loadings for the Externalizing (Aggressive Behaviors, Rule Breaking Behaviors, Attention Problem) latent factor ranged from 0.55 to 0.80, all p’s < .001. The internalizing and externalizing factors were correlated at .715, p < .001.
We extracted general factor scores from the bifactor model for further analyses because i) our primary interest was in psychopathology across the externalizing and internalizing spectrum, ii) both models fit the data similarly, and iii) we had some concerns about the reliability of the internalizing factor in the correlated factors model when estimated by only two indicators (Kline, 2015).
Age and Sex Differences in Emotional Awareness.
Emotional awareness was marginally correlated with age (r = .19, p = .056), and males and females did not differ significantly in emotional awareness (Cohen’s d = .10, t = 0.49, p = .625; Table 1). However, there was a significant age × sex interaction in relation to emotional awareness (B = 1.53, SE = 0.67, p = .024). Low emotional awareness was positively associated with age in females (r = .39, p = .004) but not males (r = −.05, p = .752, Figure 1). Thus, emotional awareness decreased from childhood to adolescence for females but not males.
Table 1:
Descriptive Statistics and Intercorrelations for Study 1
| Cohen’s d | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Female | 52 | 62 | .07 | .10 | .21 | .02 | .12 | −.25 | −.30 | −.31 | |
| Racial/ethnic minority | 36 | 43 | .06 | −.08 | .45* | .34 | .12 | −.08 | .03 | −.09 | |
| Correlations | |||||||||||
| N | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| 1. Age | 120 | 13.05 | 10.78 | - | |||||||
| 2. Emotional awareness | 104 | 25.00 | 3.44 | .19 | - | ||||||
| 3. Anxiety | 102 | 13.79 | 12.00 | .16 | .62* | - | |||||
| 4. Depression | 100 | 6.29 | 6.56 | .19 | .51* | .62* | - | ||||
| 5. PTSD | 110 | 11.43 | 13.76 | −.07 | .08 | .15 | .14 | - | |||
| 6. Aggression | 120 | 6.78 | 4.58 | −.15 | .32* | .23* | .48* | .13 | - | ||
| 7. Attention Problems | 120 | 6.27 | 3.31 | −.06 | .36* | .26* | .57* | .20* | .60* | - | |
| 8. Rule Breaking | 120 | 3.60 | 2.99 | .31* | .32* | .24* | .48* | .07 | .48* | .35* | - |
Note:
p < .05, N = number of participants with valid data on that measure, High scores on Emotional awareness indicate lower emotional awareness.
Figure 1: Scatterplots of relations between sex, age, low emotional awareness, and the p-factor.
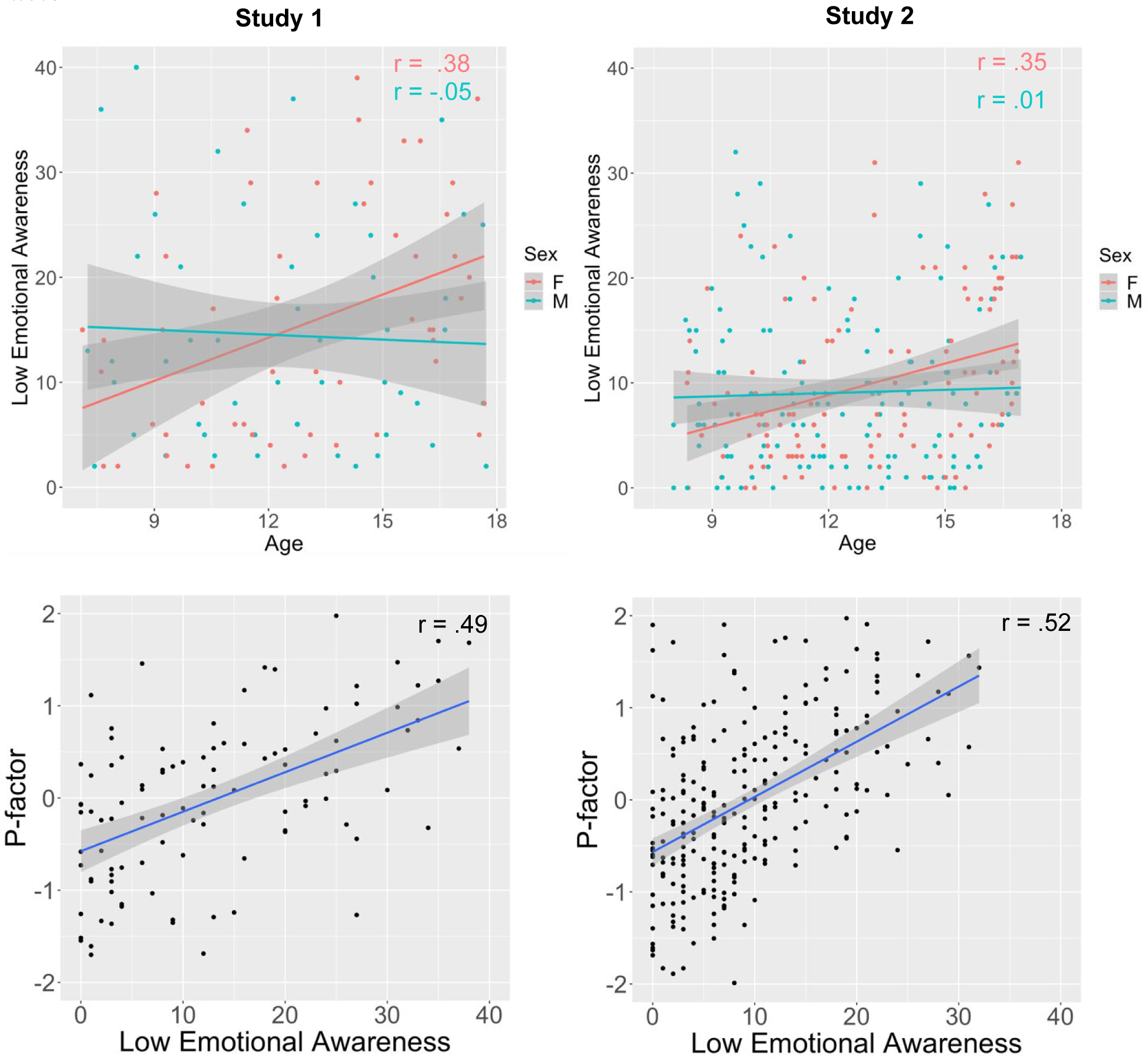
Low emotional awareness was measured with different instruments in studies 1 and 2. For ease of interpretation and visualization purposes, both scales were centered on their minimum value. Higher scores indicate lower emotional awareness. M = male, F = female, Age is in years.
Age, Sex, and Psychopathology.
The p-factor was marginally correlated with age (r = .17, p = .059). Males and females did not differ in the magnitude of the p-factor (Cohen’s d = −.23, t = −1.29, p = .200). The age × sex interaction in relation to the p-factor was marginal (B =.09, SE = .05, p = .068).
Emotional awareness and psychopathology.
Low emotional awareness was moderately and significantly correlated with the p-factor (r = .49, p < .001; Figure 1) in an unadjusted model. The association remained significant controlling for age, sex, and their interaction (B = .04, SE = .008, p < .001).
Discussion
Study 1 demonstrated that emotional awareness declines and psychopathology increases with age across middle childhood and adolescence among females, but not males, and that low emotional awareness was strongly associated with the p-factor. Although it may be intuitive to think that emotional awareness would improve across childhood and adolescence, we found the opposite. This finding replicates and extends prior work (e.g., van der Cruijsen et al., 2019) by showing that worsening emotional awareness across this age window explains symptoms of broad transdiagnostic psychopathology in females but not males. Additionally, the strong concurrent association between low emotional awareness and the p-factor suggests that it may be a transdiagnostic risk factor contributing to psychopathology. However, the cross-sectional nature of this study’s design leaves the direction of this relationship unclear: low emotional awareness could also be a shared consequence of many forms of psychopathology symptoms. Similarly, even though these results suggest that increasing difficulties in emotional awareness in females might explain their increased symptoms of psychopathology during adolescence, the lack of a longitudinal design limits the application of mediation approaches (Maxwell & Cole, 2007).
Consequently, Study 2 aimed to replicate the findings of Study 1 in a larger dataset and extend them in two important ways. First, Study 2 utilized two waves of longitudinal data to examine whether low emotional awareness was not only concurrently associated with psychopathology, but if it predicted change in psychopathology prospectively over time and whether it explained age-related differences in psychopathology among females. Second, Study 2 evaluated if childhood violence exposure was associated with low emotional awareness, and further if low emotional awareness was a mechanism linking violence exposure with psychopathology over time.
Study 2
Method
The following are all the measures, conditions, and data exclusions evaluated in this investigation.
Participants.
As reported on previously (Weissman, Bitran, et al., 2019), youth aged 8–16 years and a parent or guardian were recruited to participate in a study examining child violence exposure, emotion regulation, and psychopathology. A total of 262 youth aged 8–16 years were enrolled into the study. Exposure to violence and other inclusion and exclusion criteria were assessed during the first study visit, along with several behavioral and self-report measures. Youth and caregivers were recruited for participation at schools, after-school and prevention programs, adoption programs, food banks, shelters, parenting programs, medical clinics, and the general community in Seattle, WA between January 2015 and June 2017. Recruitment efforts were targeted at recruiting a sample with variation in exposure to violence. To do so, we recruited from neighborhoods with high levels of violent crime, from clinics that served a predominantly low-SES catchment area, and agencies that work with families who have been victims of violence (e.g., domestic violence shelters, programs for parents mandated to receive intervention by Child Protective Services). Inclusion criteria for the violence-exposed group included exposure to physical or sexual abuse or direct witnessing of domestic violence. Children in the control group were matched to children in the maltreated group on age, sex, and handedness; inclusion criteria required an absence of exposure to maltreatment or other forms of significant interpersonal violence.
Exclusion criteria included IQ < 80, presence of pervasive developmental disorder, active psychotic symptoms or mania, active substance abuse, and presence of safety concerns. IQ was measured with the Wechsler Abbreviated Intelligence Scale (WASI) (Wechsler, 2011) in the first study visit. Pervasive developmental disorders were assessed via parent report. Of the 262 children enrolled in the first study visit, three were excluded from all analysis due to low IQ (n=1), presence of pervasive developmental disorder (n=1), and presence of psychotic symptoms and drug abuse (n=1). The total sample size for the present analysis was 259 children and adolescents (118 female). Participants’ races were Asian American (n=28, 11%), Black (n=76, 29%), Latinx (n=29, 11%), White (n=101, 39%), and “Other” (n=25, 10%). A longitudinal follow-up assessment was conducted approximately two years after baseline assessments (M = 21.96 months, SD = 7.88 months) to assess symptoms of psychopathology. A total of 198 children and adolescents (76.4%) completed the follow-up visit. Of the 65 children that dropped out, 44 were maltreated (28% attrition), and 21 were not (20% attrition). Attrition did not differ significantly between maltreated or control groups (χ2 = 2.38, p = .123).
All procedures were approved by the Institutional Review Board at the University of Washington. Written informed consent was obtained from legal guardians; children provided written assent. Maltreatment not previously reported to the relevant authorities was reported to Child Protective Services using standard clinical procedures. Children with active safety concerns were not enrolled in the study.
Measures.
Violence exposure.
For the purposes of this study, violence exposure included physical and sexual abuse, and chronic exposure to domestic violence. We used a multi-informant, multi-method approach for assessing exposure to violence. Children completed two interviews with a trained member of our research team assessing child maltreatment experiences and exposure to interpersonal violence: the Childhood Experiences of Care and Abuse (CECA) Interview (Bifulco et al., 1994) and the Violence Exposure Scale for Children-Revised (VEX-R) (Raviv et al., 1999, 2001). The CECA assesses caregiving experiences, including physical and sexual abuse. We modified the interview to ask parallel questions about witnessing domestic violence (i.e., directly observing violence directed at a caregiver). Inter-rater reliability for maltreatment reports is excellent, and validation studies suggest high agreement between siblings on maltreatment reports (Bifulco et al., 1997). The VEX-R assesses the frequency of exposure to different forms of violence. Children are presented with a cartoon and caption depicting a child of the same sex witnessing a type of violence (e.g., “Chris sees a person slap another person really hard”) and experiencing that same type of violence (e.g., “A person slaps Chris really hard”). Children are then asked to report how frequently they have witnessed or experienced that type of violence (e.g., “How many times have you seen a person slap another person really hard?”; “How many times has a person slapped you really hard?”) on a Likert scale ranging from 0 (Never) to 3 (Lots of times). We added follow-up questions for each item that was endorsed to gather additional information (e.g., the perpetrator, age of onset). The VEX-R demonstrates good reliability and has been validated with children as young as second grade (Raviv et al., 1999, 2001).
Children also completed two self-report measures: the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 1997) and the UCLA PTSD Reaction Index (PTSD-RI) (The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index, 2004). The CTQ is a 28-item scale that assesses the frequency of maltreatment during childhood, including physical and sexual abuse. Validated thresholds for exposure to physical and sexual abuse (Walker et al., 1999) were applied here in evaluating abuse exposure based on the CTQ. The CTQ has excellent psychometric properties including internal consistency, test-retest reliability, and convergent and discriminant validity with interviews and clinician reports of maltreatment (Bernstein et al., 1994, 1997). The PTSD-RI includes a trauma screen that assesses exposure to numerous traumatic events, including physical abuse, sexual abuse, and domestic violence and additionally assesses PTSD symptoms. The PTSD-RI has good internal consistency and convergent validity (Steinberg et al., 2013).
Caregivers completed three self-report measures: the Conflict Tactics Scale-Parent Child Version (CTS) (Straus et al., 1998), the Juvenile Victimization Questionnaire (JVQ) lifetime caregiver report (Finkelhor et al., 2005), and the caregiver version of the PTSD-RI. The CTS includes 22 items assessing caregiver responses to child disobedience or misbehavior in the past year. Caregivers indicate how frequently they have used each strategy (e.g., shook him/her) on a Likert scale ranging from 0 (This has never happened) to 6 (more than 20 times in the past year) and can also indicate if they have used the strategy in the past but not in the last year. The CTS has adequate reliability and good discriminant and construct validity (Straus et al., 1998). The JVQ includes 34 items assessing exposure to crime, child maltreatment, peer and sibling victimization, sexual victimization, and witnessing and indirect victimization and has excellent psychometric properties, including test-retest reliability and construct validity (Finkelhor et al., 2005). Caregivers endorsed whether their child had experienced each event in his/her lifetime. Caregivers also completed the trauma screen included in the PTSD-RI, described above. A trained interviewer followed up with the caregiver if the endorsed any form of abuse or domestic violence to gather additional information about the experience.
Children were classified as experiencing physical or sexual abuse if abuse was endorsed by the child (on the CECA interview, PTSD-RI trauma screen, or above the validated CTQ threshold) or parent (on the CTS, JVQ, or PTSD-RI trauma screen). A total of 100 children (38.6%) experienced physical or sexual abuse. Inter-rater reliability was fair to good for child and caregiver reports (82.0% agreement; kappa=0.62). Exposure to domestic violence (on the VEX-R interview or PTSD-RI trauma screen) was determined based on child report only. A total of 99 children (38.2%) reported witnessing domestic violence. Exposure to violence was coded dichotomously, with a 1 indicating that participants had been exposed to physical abuse, sexual abuse, or domestic violence, and a 0 indicating no exposure to those types of violence.
Emotional awareness.
Emotional awareness was measured using the 8-item (e.g. “I have feelings that I can’t figure out”) Poor Emotional Awareness subscale of the Emotional Expressiveness Scale for Children (EESC), a well validated measure in children and adolescents (Penza-Clyve & Zeman, 2002). The scale had excellent reliability in this sample (α = .91). Items are rated on a 5-point Likert scale from “not at all true” to “extremely true.” Higher scores indicate lower emotional awareness.
Psychopathology.
Symptoms of psychopathology were measured using the same instruments as in Study 1, and the p-factor was defined using the same methods and criteria as in Study 1 (and as in Weissman et al., 2019). The CDI was used to measure depressive symptoms. 39 participants exceeded a recommended cutoff score of 15 for depression on the CDI. Anxiety symptoms were assessed with the SCARED. 73 participants exceeded a recommended cutoff score of 25 for anxiety on the SCARED. Attention problems, rule breaking behaviors, and aggressive behavior were assessed on the YSR and CBCL. 69 participants exceeded a recommended cutoff T-score of 65 for Externalizing Problems on the YSR/CBCL. Post-traumatic stress disorder symptoms were assessed with the PTSD-RI. 52 participants exceeded a recommended cutoff score of 35 for PTSD. We performed CFA to test a correlated-factors model and a bi-factor model. We binned scores on each indicator into deciles prior to CFA analyses. All CFA analyses were performed in MPlus version 8.1 using MLR. As assessed by relative fit indices and factor loadings, both models fit the data well at the baseline assessment, with a relatively better fit for the bi-factor model. Latent factor scores for the p-factor from this model at baseline and follow-up were extracted for further analysis.
Analysis.
First, linear regression was used to evaluate associations between age, sex, and their interaction with emotional awareness and between violence exposure and emotional awareness. We controlled for racial/ethnic minority status and income-to-needs ratio in these analyses, as these characteristics varied between violence-exposed and unexposed youth (see Supplemental Materials Table S1). Racial/ethnic minority status was a dichotomous variable indicating whether participants identified with a race or ethnicity other than white. Income-to-needs ratio was calculated by dividing the parent-reported family income by the poverty threshold for a family of that size as indicated by the U. S. Census Bureau (U.S. Census Bureau, 2019). Second, we investigated the association between age, sex, and their interaction with p-factor scores at baseline, and between violence exposure and p-factor scores at baseline, controlling for racial/ethnic minority status, and income-to-needs ratio.
Third, we evaluated the associations between emotional awareness and p-factor scores at baseline and at the follow-up, controlling for p-factor scores at baseline and the time elapsed from baseline to follow-up. Age, sex, their interaction, violence exposure, income-to-needs ratio, and racial/ethnic minority status were included as covariates in both analyses, due to their hypothesized association with emotional awareness and/or the p-factor. Controlling for the time elapsed between visits ensures that any differences in longitudinal change in the p-factor is not attributable to differences in the length of time since the previous measurement of the p-factor.
Fourth, a parallel mediation model with bootstrapped confidence intervals (10,000 iterations) was estimated using the lavaan package in R (Rosseel, 2012) to evaluate whether emotional awareness mediated the association between violence exposure and the p-factor at follow-up and between the age and the p-factor at follow-up. A moderated mediation model was additionally evaluated to determine whether low emotional awareness mediated age-related increases in p-factor among females only. Because results of regression analyses revealed that the p-factor at baseline was the only covariate associated with the p-factor at follow-up, no other covariates were included in the mediation model. All data and code are available for download at https://github.com/dgweissman/EMAware_P.
Results
Descriptive statistics and intercorrelations are summarized in Table S1 in Supplementary Materials.
Model of general psychopathology.
As described previously (Weissman, Bitran, et al., 2019), the correlated factor model and the bifactor model fit the data similarly, with a slightly better model fit for the bifactor model. In contrast to the models in Study 1, PTSD symptoms loaded significantly onto the p-factor in the bifactor model and onto the internalizing factor in the correlated factors model and were therefore included in the models. Factor scores for the p-factor were extracted for further analyses.
Age, sex, and emotional awareness.
Age and low emotional awareness were positively correlated at baseline (r = .18, p = .005). Low emotional awareness did not differ significantly between males and females (Cohen’s d = .11, t = 0.85, p = .398). There was a significant age × sex interaction in relation to emotional awareness (B = .963, SE = 0.364, p = .009), such that low emotional awareness was positively associated with age in females (r = .35, p < .001) but not males (r = .01, p = .878, Figure 1).
Childhood violence exposure and emotional awareness.
Violence-exposed youth had higher scores on low emotional awareness than children and adolescents with no history of violence exposure (Cohen’s d = .59, t = 4.92, p < .001). This association remained robust and significant even after controlling for income-to-needs ratio, and racial minority status (B = 4.51, SE = 1.17, p < .001).
Age, sex, childhood violence exposure and psychopathology.
There was a small but significant positive correlation between age and the p-factor at baseline (r = .14, p = .021). P-factor scores at baseline did not differ significantly between male and female adolescents (Cohen’s d = .02, t = 0.19, p = .851), and the age × sex interaction in relation to p-factor at baseline was not significant (B = .0491, SE = .0429, p = .254).
Emotional awareness and psychopathology.
Low emotional awareness was significantly correlated with the p-factor with a moderate effect size (r = .52, p < .001; Figure 1). This association remained robust and significant even after controlling for age, sex, their interaction, violence exposure, income-to-needs ratio, and racial minority status (B = .044, SE = .006, p < .001).
Low emotional awareness as a transdiagnostic mechanism.
Low emotional awareness was significantly associated with the p-factor at follow-up, controlling for the p-factor at baseline, violence exposure, time between visits, age, sex, their interaction, racial minority status, and income-to-needs ratio (B = .019, SE = .007, p = .011; Table 2). When comparing the mediation and moderated mediation models, including the interaction between sex and age significantly improved model fit (χ2 = 123.37, p < .001), so the moderated mediation model was used. In both models, the indirect effect of violence exposure on the p-factor at follow-up via low emotional awareness did not include 0 (Unstandardized Estimate = .07, SE = .04, 95% CI = .01–.15), providing evidence of mediation of the effect of violence exposure on the p-factor by emotional awareness in all participants (Figure 2). The conditional indirect effect of age on the p-factor at follow-up, with the path from age to emotional awareness conditional on sex, did not include 0, providing evidence of moderated mediation (Unstandardized Estimate = .02, SE = .01, 95% CI = .002–.04), such that lower emotional awareness only explained age-related increases in the p-factor in females (Figure 2).
Table 2:
Regression table of the relation between low emotional awareness and “p” at follow-up in Study 2
| P (follow-up) | ||||
|---|---|---|---|---|
| Predictors | B | SE | β | p |
| P (baseline) | .595* | .080 | .598 | <.001 |
| Low emotional awareness | .0186* | .0073 | .165 | .011 |
| Violence exposure | −.074 | .138 | −.042 | .592 |
| Age (Baseline) | .0773* | .0184 | .231 | <.001 |
| Female | .0200 | .0956 | .011 | .834 |
| Age × Female | −.0655 | .0370 | −.097 | .079 |
| Time between visits (years) | .0612 | .0745 | .046 | .413 |
| Racial/ethnic minority status | −.085 | .105 | −.050 | .402 |
| Income-to-needs ratio | −.0006 | .0220 | −.002 | .979 |
Observations 174
R2 / adjusted R2 0.536/0.11
p < .05
Figure 2: Parallel mediation/moderated mediation of violence exposure and age (among females) on the p-factor through low emotional awareness in Study 2.
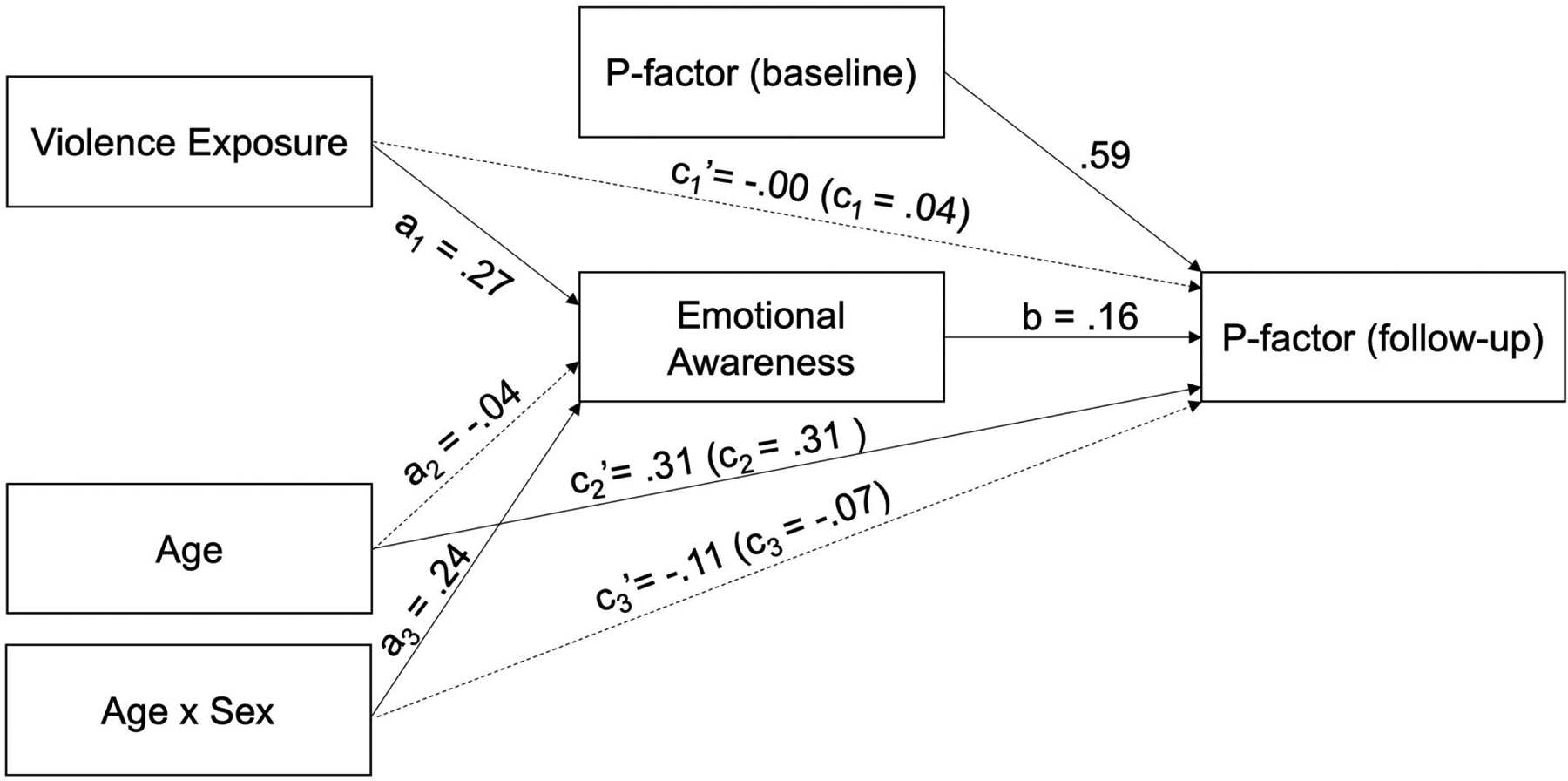
All coefficients are standardized. Solid lines indicate significant paths. Dotted lines indicate nonsignificant paths. Main effects sex (female = 1) on emotional awareness and p-factor at follow-up were not significant and are not displayed but were also included in the model.
Discussion
In a large longitudinal sample of children and adolescents, many of whom had been exposed to violence in the form of physical or sexual abuse or domestic violence, age was associated with low emotional awareness in females but not males, and low emotional awareness was positively associated with the p-factor at both baseline and follow-up. These results replicated the associations found in Study 1. When turning to other risk factors, we also found that exposure to violence was associated with lower emotional awareness. Finally, low emotional awareness predicted increases in the p-factor over time and mediated associations of both violence exposure and age with the p-factor, although the latter was true only for females. These results suggest that low emotional awareness may be a transdiagnostic mechanism linking childhood violence exposure with psychopathology and a mechanism of age-related increases in psychopathology among females.
General Discussion
We demonstrated in two studies of children and adolescents that emotional awareness declines from middle childhood through adolescence, is associated with transdiagnostic psychopathology concurrently, and predicts increased psychopathology over time. This suggests that low emotional awareness may be a factor that increases risk for the emergence of multiple forms of psychopathology across the internalizing and externalizing spectrum in adolescence. These longitudinal findings extend prior work associating low emotional awareness and specific forms of psychopathology (Hendryx et al., 1991; Honkalampi et al., 2002; Taylor et al., 1990; van der Cruijsen et al., 2019). Low emotional awareness also emerged as a factor explaining increases in transdiagnostic psychopathology as a function of adolescent development among females and exposure to violence. These findings suggesting that low emotional awareness may be a mechanism contributing to increased risk for emerging psychopathology during adolescence.
Low emotional awareness may contribute to psychopathology across the internalizing and externalizing spectrum in a number of ways. Difficulty assigning emotional labels to negative affect has been found to disrupt effective emotion regulation in prior studies (Barrett et al., 2001; Kalokerinos et al., 2019), and difficulties with emotion regulation are a well-established transdiagnostic risk factor for psychopathology (Aldao et al., 2010; Burns et al., 2010; McLaughlin, Aldao, et al., 2014a, 2014b; McLaughlin & Nolen-Hoeksema, 2011; Messman-Moore & Bhuptani, 2017). Thus, low emotional awareness may connect these two lines of work: Difficulties understanding what one is feeling may disrupt effective emotion regulation, leading to the emergence of multiple forms of psychopathology. However, low emotional awareness could also lead to psychopathology via a more social or interpersonal route. Low emotional awareness is associated with difficulties recognizing emotions in others (Collin et al., 2013; Grynberg et al., 2012; Nook et al., 2015). Difficulties identifying what other people are feeling may produce downstream issues in social support and interpersonal emotion regulation, which are associated with psychopathology (Hofmann, 2014; Marroquín, 2011; Williams et al., 2018). Finally, assigning a label to emotional pictures results in reduced self-reported distress, psychophysiological responses, and amygdala reactivity in children, adolescents, and adults (Burklund, David Creswell, Irwin, & Lieberman, 2014; Gee et al., 2015; Lieberman, Inagaki, Tabibnia, & Crockett, 2011; Lieberman et al., 2007; Tabibnia, Lieberman, & Craske, 2008). Given that heightened amygdala responses to affectively salient cues, particularly threatening stimuli, is associated with many forms of psychopathology in children and adolescents (Beesdo et al., 2009; Dotterer et al., 2017; Monk et al., 2008; Swartz et al., 2015), this could be another pathway through which lower emotional awareness contributes to psychopathology risk. Thus, children and adolescents with low emotional awareness may lack a foundation for effective intrapersonal and interpersonal emotion regulation, putting them increased risk for psychopathology. However, specifically identifying the mechanistic processes through which these symptoms emerge remains an important area of future study.
In both studies, age was significantly related to low emotional awareness, but only in females. This finding suggests that the transition into adolescence may generate difficulties for females in identifying their emotions. These difficulties with emotional awareness, in turn, may contribute to increased risk for psychopathology. This is consistent with prior work suggesting that emotional awareness worsened across childhood and adolescence, and that low emotional awareness explained variance in the emergence of depression across age only in females (van der Cruijsen et al., 2019). Building upon the ideas presented above, one potential explanation of these sex differences is that low emotional awareness may interfere with social support specifically in adolescent females. Indeed, longitudinal research in adolescents has found that emotional awareness is associated with number of friends in females but not males (Rowsell et al., 2014). Thus, entering adolescence without strong emotion identification and skills may lead females (but not males) to struggle to build friendships, leading to difficulties finding social support, lower self-esteem and mood, and potentially the emergence of psychopathology.
We also found that childhood violence exposure was associated with low emotional awareness, and low emotional awareness mediated the association between childhood violence exposure and increases in the p-factor over time. Children exposed to violence and other forms of adversity have difficulties with labeling and differentiating between emotions (Pears & Fisher, 2005; Shenk et al., 2013), potentially due to stress-related disruptions in detecting internal bodily states (Barrett & Simmons, 2015; McEwen, 1998), chronic dysregulation in physiological stress response systems that may create a de-coupling between subjective affect and physiological activation (Carpenter et al., 2011; Gordis et al., 2010; Gunnar & Vazquez, 2001; Harkness et al., 2011; Heleniak et al., 2016; MacMillan et al., 2009; McLaughlin, Sheridan, et al., 2014; Trickett et al., 2010), a lack of consistent scaffolding and use of emotion language by parents (Denham et al., 1997; Pollak et al., 2000), or specialization in the detection of anger at the expense of differentiating between other types of negative emotions (Shenk et al., 2013). These findings extend prior work demonstrating that more normative forms of stressful life events, such as peer victimization, are associated with reductions in emotional awareness over time during adolescence (McLaughlin & Hatzenbuehler, 2009; McLaughlin et al., 2009). Thus, it may be that not only exposure to violence but a wider range of stressful experiences contribute to lower facility at categorizing emotions, leading to low emotional awareness, and worsening psychopathology over time. Further research is needed to examine this empirically.
Both studies identified similar hierarchical structures of psychopathology. However, in Study 1, PTSD symptoms did not load significantly on to the p-factor or the internalizing factor in the correlated factors model. This may reflect the unique characteristics of PTSD relative to the other diagnoses included in the analyses, in that the existence of PTSD symptoms is contingent on the experiencing of a traumatic event. Because the Study 2 sample had far more participants who experienced trauma, PTSD symptoms may have been more likely to share an etiology with symptoms of other disorders in Study 2 than Study 1. This speculation is supported by the finding in Study 1 that PTSD symptom severity was significantly correlated with low emotional awareness among youth who experienced trauma. The bifactor model and the correlated factor model fit the data similarly in both Study 1 and Study 2. The precise structure of psychopathology in childhood and adolescence is a topic of rich, ongoing investigation in much larger datasets, which are better suited to answering that question (Castellanos-Ryan et al., 2016; Gomez et al., 2018; Laceulle et al., 2015; Martel et al., 2017; Murray et al., 2016; Neumann et al., 2016; Patalay et al., 2015; Schaefer et al., 2018; Snyder et al., 2017). However, both models converged in demonstrating that symptoms of psychopathology are highly comorbid in samples of children and adolescents and that low emotional awareness is transdiagnostically associated with higher psychopathology.
These findings point to the possibility that interventions aimed at improving emotional awareness could be effective at preventing the emergence of psychopathology, particularly in adolescent females and children who have experienced violence. Improving emotional awareness may also be useful as a treatment target for multiple forms of psychopathology. Better emotional awareness is thought to be an important mechanism through which existing effective interventions, such as the Unified Protocol, dialectical behavioral therapy, and mindfulness based therapies, operate (Ellard et al., 2010; Hölzel et al., 2011; Lynch et al., 2006). A better understanding of emotional awareness and its relation with violence exposure and psychopathology may contribute to improvements in existing evidence-based interventions.
This investigation had several strengths, including replication of findings across samples (one normative sample and one that included children with high levels of exposure to violence and psychopathology), integration of multiple measures of violence exposure from both youth and parents, and longitudinal measures of psychopathology. However, some limitations constrain interpretation and suggest directions for future research. First, while the use of multiple reporters for quantifying violence exposure in Study 2 and psychopathology symptoms in both studies allays some concerns about associations being attributable to shared method variance, work utilizing behavioral and ecological (e.g., experience sampling) measures of emotional awareness (e.g. Aaron, Snodgress, Blain, & Park, 2018) would provide necessary additional support to our findings. Second, in Study 2, although violence-exposed and unexposed youth were matched on both age and sex, youth exposed to violence had significantly lower income and a higher proportion of youth who are racial or ethnic minorites. These factors frequently co-occur, and all analyses controlled for income-to-needs ratio and racial minority status. However, potential confounds from this collinearity cannot be entirely ruled out. In addition, it is possible that structural inequalities based on race and socioeconomic status may not only increase risk for violence exposure but also alter one’s response to and resources to cope with it. Future work in samples recruited specifically to examine interactions among violence exposure, race/ethnicity and socioeconomic status could help identify and disentangle more complex potential associations of race, ethnicity, socioeconomic status and violence exposure with emotional awareness and psychopathology.
Finally, the bifactor model has been criticized because fit indices tend to be biased in its favor relative to other model types (e.g. Greene et al., 2019). Moreover, with sample sizes of 120 and 249, binning of the raw psychopathology data into deciles was necessary to achieve model convergence. However, while this may call into question investigations that attempt to characterize the “true” structure of psychopathology, our goal here is instead to operationalize transdiagnostic psychopathology for the purposes of relating it to emotional awareness. There is substantial evidence supporting the utility of the p-factor in quantifying the impact of important risk factors on psychopathology broadly, suggesting that elucidating the role of emotional awareness in contributing to the p-factor may significantly advance clinical science (Caspi & Moffitt, 2018; Snyder & Hankin, 2017). Further, to illustrate the robustness of the associations reported here, we have included analyses in which psychopathology symptom counts were binned into quartiles instead of deciles, and using CBCL/YSR internalizing and externalizing problems as psychiatric outcome variables instead of the p-factor in Supplementary Materials, and the results are overall consistent with those reported here.
Low emotional awareness is a transdiagnostic mechanism underlying psychopathology in middle childhood and adolescence, as demonstrated by replication in two independent samples. Moreover, low emotional awareness appears to be a mechanism linking childhood violence exposure with psychopathology over time as well as age-related increases in psychopathology in females. Improving emotional awareness may therefore be an important target for early interventions designed to prevent psychopathology, particularly among adolescent females and youth exposed to violence.
Supplementary Material
Acknowledgements
This research was funded by the National Institute of Mental Health (R01-MH103291 to McLaughlin; K01-MH116325 to Miller), an Early Career Research Fellowship from the Jacobs Foundation (McLaughlin), and a OneMind Institute Rising Star Award (McLaughlin), and a National Science Foundation Graduate Research Fellowship (DGE1144152 to Nook).
References
- Aaron RV, Snodgress MA, Blain SD, & Park S (2018). Affect labeling and other aspects of emotional experiences in relation to alexithymia following standardized emotion inductions. Psychiatry Research. 10.1016/j.psychres.2018.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM (1991). Manual for the child behavior checklist/4–18 and 1991 profile. In Burlington VT. [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. In Clinical Psychology Review. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Barrett LF (2006). Solving the Emotion Paradox: Categorization and the Experience of Emotion. Personality and Social Psychology Review, 10(1), 20–46. 10.1207/s15327957pspr1001_2 [DOI] [PubMed] [Google Scholar]
- Barrett LF (2017). The theory of constructed emotion: An active inference account of interoception and categorization. Social Cognitive and Affective Neuroscience. 10.1093/scan/nsw154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett LF, Gross J, Christensen TC, & Benvenuto M (2001). Knowing what you’re feeling and knowing what to do about it: Mapping the relation between emotion differentiation and emotion regulation. Cognition & Emotion, 15(6), 713–724. 10.1080/02699930143000239 [DOI] [Google Scholar]
- Barrett LF, & Simmons WK (2015). Interoceptive predictions in the brain. In Nature Reviews Neuroscience. 10.1038/nrn3950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K, Lau JYF, Guyer AE, McClure-Tone EB, Monk CS, Nelson EE, Fromm SJ, Goldwin MA, Wittchen HU, Leibenluft E, Ernst M, & Pine DS (2009). Common and distinct amygdala-function perturbations in depressed vs anxious adolescents. Archives of General Psychiatry, 66(3), 275–285. 10.1001/archgenpsychiatry.2008.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L (1997). Validity of the childhood trauma questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry, 36(3), 340–348. 10.1097/00004583-199703000-00012 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, & Ruggiero J (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 10.1176/ajp.151.8.1132 [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, & Harris TO (1994). Childhood Experience of Care and Abuse (CECA): A Retrospective Interview Measure. Journal of Child Psychology and Psychiatry, 35(8), 1419–1435. 10.1111/j.1469-7610.1994.tb01284.x [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, & Jarvis J (1997). Memories of childhood neglect and abuse: Corroboration in a series of sisters. Journal of Child Psychology and Psychiatry and Allied Disciplines. 10.1111/j.1469-7610.1997.tb01520.x [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1230–1236. 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SMK (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 545–553. 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Brewer R, Happé F, Cook R, & Bird G (2015). Commentary on “Autism, oxytocin and interoception”: Alexithymia, not Autism Spectrum Disorders, is the consequence of interoceptive failure. Neuroscience & Biobehavioral Reviews, 56, 348–353. 10.1016/j.neubiorev.2015.07.006 [DOI] [PubMed] [Google Scholar]
- Burklund LJ, David Creswell J, Irwin MR, & Lieberman MD (2014). The common and distinct neural bases of affect labeling and reappraisal in healthy adults. Frontiers in Psychology. 10.3389/fpsyg.2014.00221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns EE, Jackson JL, & Harding HG (2010). Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment and Trauma, 19(8), 801–819. 10.1080/10926771.2010.522947 [DOI] [Google Scholar]
- Carpenter LL, Shattuck TT, Tyrka AR, Geracioti TD, & Price LH (2011). Effect of childhood physical abuse on cortisol stress response. Psychopharmacology, 214(1), 367–375. 10.1007/s00213-010-2007-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, & Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, appi.ajp.2018.17121383. 10.1176/appi.ajp.2018.17121383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Briere FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, Biichel C, Flor H, Frouin V, Gallinat J, Garavan H, Martinot JL, Nees F, Paus T, Pausova Z, Rietschel M, Smolka MN, Robbins TW, Whelan R, … The IMAGEN Consortium. (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology. 10.1037/abn0000193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin L, Bindra J, Raju M, Gillberg C, & Minnis H (2013). Facial emotion recognition in child psychiatry: A systematic review. Research in Developmental Disabilities, 34(5), 1505–1520. 10.1016/j.ridd.2013.01.008 [DOI] [PubMed] [Google Scholar]
- Craighead WE, Smucker MR, Craighead LW, & Ilardi SS (1998). Factor analysis of the Children’s Depression Inventory in a community sample. Psychological Assessment, 10(2), 156–165. 10.1037/1040-3590.10.2.156 [DOI] [Google Scholar]
- Deborde A-S, Vanwalleghem Maury S, & Aitel S (2015). Emotion regulation in adolescents with conduct disorder and controls. Encephale. 10.1016/j.encep.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Denham SA, Mitchell-Copeland J, Strandberg K, Auerbach S, & Blair K (1997). Parental contributions to preschoolers’ emotional competence: Direct and indirect effects. Motivation and Emotion. 10.1023/A:1024426431247 [DOI] [Google Scholar]
- Dotterer HL, Hyde LW, Swartz JR, Hariri AR, & Williamson DE (2017). Amygdala reactivity predicts adolescent antisocial behavior but not callous-unemotional traits. Developmental Cognitive Neuroscience, 24, 84–92. 10.1016/j.dcn.2017.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, & Barlow DH (2010). Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders: Protocol Development and Initial Outcome Data. Cognitive and Behavioral Practice, 17(1), 88–101. 10.1016/j.cbpra.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, & Turner H (2005). The Juvenile Victimization Questionnaire: Reliability, validity, and national norms. In Child Abuse and Neglect. 10.1016/j.chiabu.2004.11.001 [DOI] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, Neufeld RWJ, & Lanius RA (2008). Meta-analysis of alexithymia in posttraumatic stress disorder. Journal of Traumatic Stress. 10.1002/jts.20320 [DOI] [PubMed] [Google Scholar]
- Gatta M, Facca I, Colombo E, Svanellini L, Montagnese S, & Schiff S (2014). Alexithymia, psychopathology and alcohol misuse in adolescence: A population based study on 3556 teenagers. Neuroscience and Medicine, 05(01), 60–71. 10.4236/nm.2014.51009 [DOI] [Google Scholar]
- Gee DG, Mcewen SC, Forsyth JK, Haut KM, Bearden CE, Addington J, Goodyear B, Cadenhead KS, Mirzakhanian H, Cornblatt BA, Olvet D, Mathalon DH, Mcglashan TH, Perkins DO, Belger A, Seidman LJ, Thermenos H, Tsuang MT, van Erp TGM, … Cannon TD (2015). Reliability of an fMRI paradigm for emotional processing in a multisite longitudinal study. Human Brain Mapping. 10.1002/hbm.22791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez R, Stavropoulos V, Vance A, & Griffiths MD (2018). Re-evaluation of the Latent Structure of Common Childhood Disorders: Is There a General Psychopathology Factor (P-Factor)? International Journal of Mental Health and Addiction, 1–21. 10.1007/s11469-018-0017-3 [DOI] [Google Scholar]
- Gordis EB, Feres N, Olezeski CL, Rabkin AN, & Trickett PK (2010). Skin Conductance Reactivity and Respiratory Sinus Arrhythmia Among Maltreated and Comparison Youth: Relations with Aggressive Behavior. Journal of Pediatric Psychology, 35(5), 547–558. 10.1093/jpepsy/jsp113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabe HJ, Ruhrmann S, Ettelt S, Müller A, Buhtz F, Hochrein A, Schulze-Rauschenbach S, Meyer K, Kraft S, Reck C, Pukrop R, Klosterkötter J, Falkai P, Maier W, Wagner M, John U, & Freyberger HJ (2006). Alexithymia in obsessive-compulsive disorder—Results from a family study. Psychotherapy and Psychosomatics. 10.1159/000093954 [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67(2), 113–123. 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene AL, Eaton NR, Li K, Forbes MK, Krueger RF, Markon KE, Waldman ID, Cicero DC, Conway CC, Docherty AR, Fried EI, Ivanova MY, Jonas KG, Latzman RD, Patrick CJ, Reininghaus U, Tackett JL, Wright AGC, & Kotov R (2019). Are fit indices used to test psychopathology structure biased? A simulation study. Journal of Abnormal Psychology, 128(7), 740–764. 10.1037/abn0000434 [DOI] [PubMed] [Google Scholar]
- Grynberg D, Chang B, Corneille O, Maurage P, Vermeulen N, Berthoz S, & Luminet O (2012). Alexithymia and the Processing of Emotional Facial Expressions (EFEs): Systematic Review, Unanswered Questions and Further Perspectives. PLoS ONE, 7(8). 10.1371/journal.pone.0042429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar MR, & Vazquez DM (2001). Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology, 13(3), 515–538. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Stewart JG, & Wynne-Edwards KE (2011). Cortisol reactivity to social stress in adolescents: Role of depression severity and child maltreatment. Psychoneuroendocrinology, 36(2), 173–181. 10.1016/j.psyneuen.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Heaven PCL, Ciarrochi J, & Hurrell K (2010). The distinctiveness and utility of a brief measure of alexithymia for adolescents. Personality and Individual Differences, 49(3), 222–227. 10.1016/j.paid.2010.03.039 [DOI] [Google Scholar]
- Heleniak C, McLaughlin KA, Ormel J, & Riese H (2016). Cardiovascular reactivity as a mechanism linking child trauma to adolescent psychopathology. Biological Psychology, 120, 108–119. 10.1016/j.biopsycho.2016.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryx MS, Haviland MG, & Shaw DG (1991). Dimensions of Alexithymia and Their Relationships to Anxiety and Depression. Journal of Personality Assessment 10.1207/s15327752jpa5602_4 [DOI] [PubMed] [Google Scholar]
- Hofmann SG (2014). Interpersonal Emotion Regulation Model of Mood and Anxiety Disorders. Cognitive Therapy and Research, 38(5), 483–492. 10.1007/s10608-014-9620-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, & Ott U (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. In Perspectives on Psychological Science. 10.1177/1745691611419671 [DOI] [PubMed] [Google Scholar]
- Honkalampi K, Hintikka J, Laukkanen E, & Viinamäki JLH (2002). Alexithymia and Depression: A Prospective Study of Patients With Major Depressive Disorder. Psychosomatics. 10.1176/appi.psy.42.3.229 [DOI] [PubMed] [Google Scholar]
- Kalokerinos EK, Erbas Y, Ceulemans E, & Kuppens P (2019). Differentiate to Regulate: Low Negative Emotion Differentiation Is Associated With Ineffective Use but Not Selection of Emotion-Regulation Strategies. Psychological Science, 30(6), 863–879. 10.1177/0956797619838763 [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Barrett LF, & McKnight PE (2015). Unpacking Emotion Differentiation: Transforming Unpleasant Experience by Perceiving Distinctions in Negativity. Current Directions in Psychological Science, 24(1), 10–16. 10.1177/0963721414550708 [DOI] [Google Scholar]
- Kessler RC, Avenevoli S, Costello J, Green JG, Gruber MJ, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, & Merikangas KR (2012). Severity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 69(4), 381–389. 10.1001/archgenpsychiatry.2011.1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry. 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and Practice of Structural Equation Modeling, Fourth Edition. Guilford Publications. [Google Scholar]
- Kovacs M (1992). Children’s Depression Inventory CDI Manual. New York: Multi-Health Systems. 10.1103/PhysRevLett.101.208303 [DOI] [Google Scholar]
- Kovacs M (2011). Children’s depression inventory (CDI2). Multi-Health Systems Inc. [Google Scholar]
- Laceulle OM, Vollebergh WAM, & Ormel J (2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science. 10.1177/2167702614560750 [DOI] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, & Rathouz PJ (2012). Is There a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 10.1037/a0028355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane RD, & Schwartz GE (1987). Levels of emotional awareness: A cognitive-developmental theory and its application to psychopathology. The American Journal of Psychiatry, 144(2), 133–143. 10.1176/ajp.144.2.133 [DOI] [PubMed] [Google Scholar]
- Li CH (2016). Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behavior Research Methods. 10.3758/s13428-015-0619-7 [DOI] [PubMed] [Google Scholar]
- Lieberman Matthew D., Inagaki TK, Tabibnia G, & Crockett MJ (2011). Subjective responses to emotional stimuli during labeling, reappraisal, and distraction. Emotion, 11(3), 468–480. 10.1037/a0023503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MD, Eisenberger NI, Crockett MJ, Tom SM, Pfeifer JH, & Way BM (2007). Putting feelings into words. Psychological Science 10.1111/j.1467-9280.2007.01916.x [DOI] [PubMed] [Google Scholar]
- Loas G, Braun S, Delhaye M, & Linkowski P (2017). The measurement of alexithymia in children and adolescents: Psychometric properties of the Alexithymia Questionnaire for Children and the twenty-item Toronto Alexithymia Scale in different non-clinical and clinical samples of children and adolescents. PLoS ONE, 12(5). 10.1371/journal.pone.0177982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, Neely LC, & Burger AJ (2007). The Assessment of Alexithymia in Medical Settings: Implications for Understanding and Treating Health Problems. Journal of Personality Assessment, 89(3), 230–246. 10.1080/00223890701629698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, Chapman AL, Rosenthal MZ, Kuo JR, & Linehan MM (2006). Mechanisms of change in dialectical behavior therapy: Theoretical and empirical observations. Journal of Clinical Psychology, 62(4), 459–480. 10.1002/jclp.20243 [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, Tanaka M, Gensey S, Spree S, Vella E, Walsh CA, De Bellis MD, Van der Meulen J, Boyle MH, & Schmidt LA (2009). Cortisol Response to Stress in Female Youths Exposed to Childhood Maltreatment: Results of the Youth Mood Project. Biological Psychiatry, 66(1). 10.1016/j.biopsych.2008.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín B (2011). Interpersonal emotion regulation as a mechanism of social support in depression. Clinical Psychology Review, 31(8), 1276–1290. 10.1016/j.cpr.2011.09.005 [DOI] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, Manfro GG, Miguel EC, Paus T, Bressan RA, Rohde LA, & Salum GA (2017). A general psychopathology factor (P Factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology. 10.1037/abn0000205 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12(1), 23–44. 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Aldao A, Wisco BE, & Hilt LM (2014a). Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. Journal of Abnormal Psychology. 10.1037/a0035358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Aldao A, Wisco BE, & Hilt LM (2014b). Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. Journal of Abnormal Psychology. 10.1037/a0035358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry. 10.1001/archgenpsychiatry.2011.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Hatzenbuehler ML (2009). Mechanisms Linking Stressful Life Events and Mental Health Problems in a Prospective, Community-Based Sample of Adolescents. Journal of Adolescent Health. 10.1016/j.jadohealth.2008.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, & Hilt LM (2009). Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting and Clinical Psychology, 77(5), 894–904. 10.1037/a0015760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Nolen-Hoeksema S (2011). Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 10.1016/j.brat.2010.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Alves S, & Mendes WB (2014). Child Maltreatment and Autonomic Nervous System Reactivity: Identifying Dysregulated Stress Reactivity Patterns by Using the Biopsychosocial Model of Challenge and Threat. Psychosomatic Medicine, 76(7), 538–546. 10.1097/PSY.0000000000000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, & Swendsen J (2010). Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. 10.1016/J.JAAC.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, & Bhuptani PH (2017). A Review of the Long-Term Impact of Child Maltreatment on Posttraumatic Stress Disorder and Its Comorbidities: An Emotion Dysregulation Perspective. Clinical Psychology: Science and Practice. 10.1111/cpsp.12193 [DOI] [Google Scholar]
- Monk CS, Telzer EH, Mogg K, Bradley BP, Mai X, Louro HMC, Chen G, McClure-Tone EB, Ernst M, & Pine DS (2008). Amygdala and Ventrolateral Prefrontal Cortex Activation to Masked Angry Faces in Children and Adolescents With Generalized Anxiety Disorder. Archives of General Psychiatry, 65(5), 568–576. 10.1001/archpsyc.65.5.568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J, Brewer R, Catmur C, & Bird G (2017). Interoception and psychopathology: A developmental neuroscience perspective. Developmental Cognitive Neuroscience, 23, 45–56. 10.1016/J.DCN.2016.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray AL, Eisner M, & Ribeaud D (2016). The Development of the General Factor of Psychopathology ‘p Factor’ Through Childhood and Adolescence. Journal of Abnormal Child Psychology. 10.1007/s10802-016-0132-1 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User’s Guide (7th ed.). Muthén & Muthén. [Google Scholar]
- Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, Bakermans-Kranenburg MJ, Moffitt TE, van IJzendoorn MH, & Tiemeier H (2016). Single Nucleotide Polymorphism Heritability of a General Psychopathology Factor in Children. Journal of the American Academy of Child and Adolescent Psychiatry, 55(12), 1038–1045. 10.1016/j.jaac.2016.09.498 [DOI] [PubMed] [Google Scholar]
- Nook EC, Lindquist KA, & Zaki J (2015). A new look at emotion perception: Concepts speed and shape facial emotion recognition. Emotion (Washington, D.C.), 15(5), 569–578. 10.1037/a0039166 [DOI] [PubMed] [Google Scholar]
- Nook EC, Sasse SF, Lambert HK, McLaughlin KA, & Somerville LH (2017a). Increasing verbal knowledge mediates development of multidimensional emotion representations. Nature Human Behaviour. 10.1038/s41562-017-0238-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nook EC, Sasse SF, Lambert HK, McLaughlin KA, & Somerville LH (2017b). Increasing verbal knowledge mediates development of multidimensional emotion representations. Nature Human Behaviour, 1(12), 881–889. 10.1038/s41562-017-0238-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nook EC, Sasse SF, Lambert HK, McLaughlin KA, & Somerville LH (2018a). The Nonlinear Development of Emotion Differentiation: Granular Emotional Experience Is Low in Adolescence. Psychological Science. 10.1177/0956797618773357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nook EC, Sasse SF, Lambert HK, McLaughlin KA, & Somerville LH (2018b). The nonlinear development of emotion differentiation: Granular emotional experience Is low in adolescence. Psychological Science, 29(8), 1346–1357. 10.1177/0956797618773357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nook EC, Stavish CM, Sasse SF, Lambert HK, Mair P, McLaughlin KA, & Somerville LH (2019). Charting the development of emotion comprehension and abstraction from childhood to adulthood using observer-rated and linguistic measures. Emotion (Washington, D.C.). 10.1037/emo0000609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patalay P, Fonagy P, Deighton J, Belsky J, Vostanis P, & Wolpert M (2015). A general psychopathology factor in early adolescence. British Journal of Psychiatry. 10.1192/bjp.bp.114.149591 [DOI] [PubMed] [Google Scholar]
- Pears K, & Fisher PA (2005). Emotion understanding and theory of mind among maltreated children in foster care: Evidence of deficits. Development and Psychopathology. 10.1017/S0954579405050030 [DOI] [PubMed] [Google Scholar]
- Penza-Clyve S, & Zeman J (2002). Initial Validation of the Emotion Expression Scale for Children (EESC). Journal of Clinical Child and Adolescent Psychology. 10.1207/S15374424JCCP3104_12 [DOI] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Hornung K, & Reed A (2000). Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology. 10.1037/0012-1649.36.5.679 [DOI] [PubMed] [Google Scholar]
- Pollak Seth D., & Sinha P (2002). Effects of early experience on children’s recognition of facial displays of emotion. Developmental Psychology. 10.1037/0012-1649.38.5.784 [DOI] [PubMed] [Google Scholar]
- Raviv A, Erel O, Fox NA, Leavitt LA, Raviv A, Dar I, Shahinfar A, & Greenbaum CW (2001). Individual measurement of exposure to everyday violence among elementary schoolchildren across various settings. Journal of Community Psychology. [DOI] [Google Scholar]
- Raviv A, Raviv A, Shimoni H, Fox NA, & Leavitt LA (1999). Children’s Self-Report of Exposure to Violence and Its Relation to Emotional Distress. Journal of Applied Developmental Psychology, 20(2), 337–353. 10.1016/S0193-3973(99)00020-9 [DOI] [Google Scholar]
- Rieffe C, Oosterveld P, & Terwogt MM (2006). An alexithymia questionnaire for children: Factorial and concurrent validation results. Personality and Individual Differences, 40(1), 123–133. 10.1016/j.paid.2005.05.013 [DOI] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Rowsell HC, Ciarrochi J, Heaven PCL, & Deane FP (2014). The role of emotion identification skill in the formation ofmale and female friendships: A longitudinal study. Journal of Adolescence, 37(2), 103–111. 10.1016/j.adolescence.2013.11.005 [DOI] [PubMed] [Google Scholar]
- Rybakowski J, Ziółkowski M, Zasadzka T, & Brzeziński R (1988). High prevalence of alexithymia in male patients with alcohol dependence. Drug and Alcohol Dependence. 10.1016/0376-8716(88)90058-0 [DOI] [PubMed] [Google Scholar]
- Säkkinen P, Kaltiala-Heino R, Ranta K, Haataja R, & Joukamaa M (2007). Psychometric Properties of the 20-Item Toronto Alexithymia Scale and Prevalence of Alexithymia in a Finnish Adolescent Population. Psychosomatics, 48(2), 154–161. 10.1176/appi.psy.48.2.154 [DOI] [PubMed] [Google Scholar]
- Salmon K, O’Kearney R, Reese E, & Fortune C-A (2016). The Role of Language Skill in Child Psychopathology: Implications for Intervention in the Early Years. Clinical Child and Family Psychology Review, 19(4), 352–367. 10.1007/s10567-016-0214-1 [DOI] [PubMed] [Google Scholar]
- Satpute AB, & Lindquist KA (2019). The Default Mode Network’s Role in Discrete Emotion. Trends in Cognitive Sciences, 0(0). 10.1016/j.tics.2019.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer JD, Moffitt TE, Arseneault L, Danese A, Fisher HL, Houts R, Sheridan MA, Wertz J, & Caspi A (2018). Adolescent Victimization and Early-Adult Psychopathology: Approaching Causal Inference Using a Longitudinal Twin Study to Rule Out Noncausal Explanations. Clinical Psychological Science, 6(3), 352–371. 10.1177/2167702617741381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenk CE, Putnam FW, & Noll JG (2013). Predicting the accuracy of facial affect recognition: The interaction of child maltreatment and intellectual functioning. Journal of Experimental Child Psychology. 10.1016/j.jecp.2012.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, & Hankin BL (2017). All Models Are Wrong, but the p Factor Model Is Useful: Reply to Widiger and Oltmanns (2017) and Bonifay, Lane, and Reise (2017). Clinical Psychological Science, 5(1), 187–189. 10.1177/2167702616659389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong Homotypic Continuity in Common Psychopathology-, Internalizing-, and Externalizing-Specific Factors Over Time in Adolescents. Clinical Psychological Science. 10.1177/2167702616651076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index, 6 Current Psychiatry Reports 96 (2004). 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, Gully KJ, & Pynoos RS (2013). Psychometric Properties of the UCLA PTSD Reaction Index: Part I. Journal of Traumatic Stress. 10.1002/jts.21780 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, & Runyan D (1998). Identification of child maltreatment with the parent-child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse and Neglect. 10.1016/S0145-2134(97)00174-9 [DOI] [PubMed] [Google Scholar]
- Swartz JR, Knodt AR, Radtke SR, & Hariri AR (2015). A Neural Biomarker of Psychological Vulnerability to Future Life Stress. Neuron, 85(3), 505–511. 10.1016/J.NEURON.2014.12.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabibnia G, Lieberman MD, & Craske MG (2008). The lasting effect of words on feelings: Words may facilitate exposure effects to threatening images. Emotion, 8(3), 307–317. 10.1037/1528-3542.8.3.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor GJ, Parker JDA, & Bagby RM (1990). A preliminary investigation of alexithymia in men with psychoactive substance dependence. American Journal of Psychiatry. 10.1176/ajp.147.9.1228 [DOI] [PubMed] [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, & Putnam FW (2010). Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology, 22(1), 165–175. 10.1017/S0954579409990332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau US. (2019). Poverty Thresholds. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html [Google Scholar]
- van der Cruijsen R, Murphy J, & Bird G (2019). Alexithymic traits can explain the association between puberty and symptoms of depression and anxiety in adolescent females. PLOS ONE, 14(1), e0210519. 10.1371/journal.pone.0210519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van ‘t Wout M, Aleman A, Bermond B, & Kahn RS (2007). No words for feelings: Alexithymia in schizophrenia patients and first-degree relatives. Comprehensive Psychiatry. 10.1016/j.comppsych.2006.07.003 [DOI] [PubMed] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, Koss MP, & Katon W (1999). Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry. 10.1001/archpsyc.56.7.609 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence—Second Edition (WASI-II). In Wechsler Abbreviated Scale of Intelligence—Second Edition (WASI-II). Pearson. https://doi.org/citeulike-article-id:6135820 [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 1–17. 10.1017/S0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman DG, Jenness JL, Colich NL, Miller AB, Sambrook KA, Sheridan MA, & McLaughlin KA (2019). Altered Neural Processing of Threat-Related Information in Children and Adolescents Exposed to Violence: A Transdiagnostic Mechanism Contributing to the Emergence of Psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 10.1016/j.jaac.2019.08.471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams WC, Morelli SA, Ong DC, & Zaki J (2018). Interpersonal emotion regulation: Implications for affiliation, perceived support, relationships, and well-being. Journal of Personality and Social Psychology, 115(2), 224–254. 10.1037/pspi0000132 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


