Abstract
Aims
COVID-19 is associated with diabetic ketoacidosis (DKA), hyperglycaemic hyperosmolar state (HHS) and euglycaemic DKA (EDKA); however, evidence regarding parameters affecting outcome and mortality rates is scarce.
Methods
A systematic literature review was conducted using EMBASE, PubMed/Medline, and Google Scholar from January 2020 to 7 January 2021 to identify all studies describing clinical profile, outcome and mortality rates regarding DKA, HHS, DKA/HHS and EDKA cases in COVID-19 patients. The appropriate Joanna Briggs Institute tools were used for quality assessment; quality of evidence was approached using GRADE. Univariate and multivariate analyses were used to assess correlations between clinical characteristics and outcome based on case reports. Combined mortality rates (CMR) were estimated from data reported in case report series, cross-sectional studies, and meta-analyses. The protocol was submitted to PROSPERO (ID: 229356/230737).
Results
From 312 identified publications, 44 were qualitatively and quantitatively analyzed. Critical COVID-19 necessitating ICU (P = 3 × 10–8), DKA/HHS presence (P = 0.021), and AKI (P = 0.037) were independently correlated with death. Increased COVID-19 severity (P = 0.003), elevated lactates (P < 0.001), augmented anion gap (P < 0.001), and AKI (P = 0.002) were associated with DKA/HHS. SGLT-2i were linked with EDKA (P = 0.004) and negatively associated with AKI (P = 0.023). CMR was 27.1% (95% CI 11.2–46.9%) with considerable heterogeneity (I2 = 67%).
Conclusion
Acute diabetes-related metabolic emergencies in COVID-19 patients lead to increased mortality; key determinants are critical COVID-19 illness, coexistence of DKA/HHS and AKI. Previous SGLT-2i treatment, though associated with EDKA, might preserve renal function in COVID-19 patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13340-021-00502-9.
Keywords: COVID-19, Diabetes complications, Diabetic ketoacidosis, Hyperosmolar hyperglycemic state, Euglycaemic diabetic ketoacidosis, Acute kidney injury
Introduction
Diabetes mellitus (DM), especially type 2 diabetes mellitus (T2D), has been identified as a risk factor for poor outcomes in patients with COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1, 2]. COVID-19 might either induce new onset diabetes or unmask previously undiagnosed diabetes [3]. Diabetes patients have an increased risk of infection and acute respiratory distress syndrome compared with the general population and the risk is similar [4] or even greater in those with type 1 diabetes mellitus (T1D) than in T2D [5–8]; direct cytopathic effects of SARS-CoV-2 on pancreatic b-cell populations [9] as well as the over-activity of immune system might further explain COVID-19-related severe and resistant to conventional therapy DKA episodes [10, 11]. However, whether SARS-CoV-2 directly infects b-cells in vivo has been debated [12].
COVID-19 is associated with hyperglycaemic emergencies with overrepresentation of T2D in patients presenting with DKA and long-lasting ketosis [13, 14]. DKA was the most common reason for hospitalization of T1D patients with COVID-19 [6, 15]. Emergency admissions due to acute metabolic crisis in patients with diabetes remain some of the most common and challenging conditions; along with DKA, Hyperglycaemic Hyperosmolar State (HHS) and Euglycaemic DKA (EDKA) are life-threatening different entities. DKA and HHS have distinctly different pathophysiology though sharing basic management protocols. EDKA resembles DKA but without hyperglycaemia [16]. Ketoacidosis is the hallmark of DKA and is attributed to absolute insulin deficiency; therefore, it is found mostly in T1D. DKA is less commonly seen in T2D with triggers such as severe infection [17] and sodium-glucose co-transporter-2 inhibitor (SGLT-2i) therapy [18]. On the other hand, HHS is developed under insulin sufficiency, at least enough to prevent ketosis [16]. As T2D patients tend to be younger, while T1D intertwines with T2D over time in a considerable proportion leading to double or hybrid diabetes [19], DKA is no more specific for T1D, nor HHS for T2D, as the mixed entity (HHS/DKA) is not uncommon.
Predominant features of DKA and EDKA are ketonemia and high anion gap metabolic acidosis. Both DKA and EDKA are defined as pH < 7.3 and/or bicarbonate < 15 mmol/L, and detection of ketones in blood (ketonemia > 3.0 mmol/L) or urine (2 + in urine); however, blood glucose > 11 mmol/L is indicative of DKA while < 11 mmol/L of EDKA. In contrast, HHS is characterized by very high glucose levels (> 33.3 mmol/L) along with very high serum osmolality (> 320 mOsm/kg).
Several case reports concerning acute emergencies related to glucose metabolism in COVID-19 patients have been published. Additionally, high mortality in COVID-19 and DKA has been reported [20]. A systematic review concluded that mortality rate from DKA among COVID-19 patients might approach 50% and insisted on differentiating isolated DKA from combined DKA/HHS as the latter, which represents nearly one-fifth of the DKA cases, tends to have higher mortality than DKA alone [21]. Diabetic COVID-19 patients should be assessed for disease severity and presence of complications of diabetes, while undiagnosed diabetes should be considered, especially in patients feeling unwell [22].
The present systematic review and meta-analysis aimed to examine diabetes-related acute metabolic emergencies in COVID-19 patients combining two consecutive steps; the first account for an effort to describe clinical profile in relation with outcome in DKA, HHS, DKA/HHS and EDKA episodes among COVID-19 patients based on individualized data retrieved from case reports and the second to assess mortality rates of diabetes-related acute metabolic emergencies from data available in the literature. In detail, we aimed to identify all case reports describing DKA, HHS, DKA/HHS, and EDKA, in patients with confirmed COVID-19 infection and provide further evidence by describing both primary (survival/discharge vs. death) and secondary (type of metabolic emergency) outcome in relation with origin, coexistence of DKA/HHS, age, body mass index (BMI), HbA1c, prior administration of antidiabetic treatment, comorbidities, days from onset of symptoms, disease status (DS), C-reactive protein (CRP), ferritin, d-dimers, glucose, osmolarity, arterial pH, bicarbonates, ketones, lactates, β-hydroxybutyric acid (β-ΗΒ), anion gap, as well as acute kidney injury (AKI). Furthermore, we aimed to identify all sources reporting mortality rate data regarding COVID-19-related acute metabolic emergencies and summarize their results.
Materials and methods
Literature search
A systematic literature review was conducted using EMBASE and PubMed/Medline from January 2020 until 9 January 2021 to identify all case reports describing DKA, HHS, DKA/HHS, and EDKA, in patients with confirmed COVID-19 infection through positive RT-PCR for SARS-CoV-2 RNA in nasopharyngeal swab or bronchoalveolar lavage, using the search strategy that included the terms (diabetes AND ketoacidosis AND covid) OR (diabetic AND ketoacidosis AND covid) OR (euglycemic AND diabetic AND ketoacidosis AND covid) OR (hyperglycaemic AND hyperosmolar AND state AND covid). Google Scholar database was used as an additional pool of published data; iterative search was performed until no additional publication could be traced. Unpublished dissertations and other unpublished work were scavenged. Personal communication was attempted where necessary. No software was used for study retrieval. The review methods were established prior to the conduct of the review. No significant deviations from the protocol were allowed. No funding was received.
As evidence for diabetic emergencies among COVID-19 cases had been scarce in literature, mainly scattered in the form of case reports while rarer organized in case series, it would be desirable to summarize all available data. As the present study represented two closely related though methodologically distinct processes, two separated study protocols were submitted to PROSPERO database. The first protocol, under the title “Acute Metabolic Emergencies in Diabetes and COVID-19: a systematic review and meta-analysis of case reports” (from now on referred as “case reports meta-analysis”) was dispatched on 5 January, 2021 and was corrected on 8 January 2021 (ID: 229356). The second protocol, under the title “Mortality of Diabetes-related Acute Metabolic Emergencies in COVID-19 patients: a systematic review and meta-analysis” (from now on referred as “mortality rates meta-analysis”) was dispatched on 10 January 2021 (ID: 230737). The above mentioned study protocols were also submitted to the relevant institutional ethical committee (Xanthi General Hospital Scientific Committee; Approval Number/Date: not applicable).
Study selection
Eligible studies were all that (1) refer to COVID-19 patients who had developed either DKA, or HHS, or combined DKA/HHS, or EDKA, (2) are case reports reporting data regarding both primary (survival/discharge vs. death) and secondary (type of metabolic emergency) outcome in relation with origin, coexistence of ketotic and hyperosmotic state, age, BMI, HbA1c, prior administration of antidiabetic treatment including insulin, metformin, sulfonylureas, dipeptidyl peptidase-4 inhibitors (DPP-4i), glucagon-like peptide-1 receptor agonists (GLP-1 RAs), SGLT-2i, and pioglitazone, comorbidities including T1D/T2D, arterial hypertension, hyperlipidemia, coronary artery disease, asthma and others, days from onset of symptoms, DS (as described in the Supplemental Material), CRP, ferritin, d-dimers, glucose, osmolarity, arterial pH, bicarbonates, ketones, lactates, β-ΗΒ, anion gap, as well as AKI retrievable at individual level (to be included in “case report meta-analysis”); (3) are either case report series or cross-sectional studies or meta-analyses of case reports that report mortality rates or enough data to compute it as well as a relevant measure of statistical significance (to be included in “mortality rates meta-analysis”); and (4) are not duplicates. “Google translate” tool was used to address article published in languages other than English.
No restrictions were considered regarding publication time as no outdated studies existed due to the novelty of the topic. Due to the inflated interest on publishing new works on the field, we proceeded to pre-run searches prior to the final analysis aiming to include any further studies identified. No software was used for recording decisions; all data were transformed to appropriate Word tables. Sources of financial support were traced where possible.
Outcome measures
The present study was conducted in accordance to the PRISMA statement for systematic reviews and meta-analyses [23]. Concerning the “case reports meta-analysis”, both primary (survival/discharge vs. death) and secondary (type of metabolic emergency) outcome was assessed in relation with origin, coexistence of ketotic and hyperosmotic state, age, BMI, HbA1c, prior administration of antidiabetic treatment including insulin, metformin, sulfonylureas, dipeptidyl peptidase-4 inhibitors (DPP-4i), glucagon-like peptide-1 receptor agonists (GLP-1 RAs), SGLT-2i, and pioglitazone, comorbidities including T1D/T2D, arterial hypertension, hyperlipidemia, coronary artery disease, asthma and others, days from onset of symptoms, DS (as described in the Supplemental Material), CRP, ferritin, d-dimers, glucose, osmolarity, arterial pH, bicarbonates, ketones, lactates, β-ΗΒ, anion gap, as well as AKI. Additionally, regarding “mortality rates meta-analysis”, mortality rates were assessed between different types of acute metabolic emergencies in diabetes (DKA, HHS, EDKA, and DKA/HHS) was performed. AMSTAR 2 checklist was used to assess the quality of the present study [24, 25].
Data extraction
A structured data collection form was used to extract all necessary data from each study. As far as “case report meta-analysis” is referred, all details concerning study title, first author, DKA/HHS presence, age, BMI, HbA1c, antidiabetic treatment, comorbidities, days from onset of symptoms, DS, CRP, ferritin, d-dimers, glucose, osmolarity, arterial pH, bicarbonates, ketones, lactates, β-ΗΒ, anion gap, AKI, and outcome were carefully assembled. Furthermore, as far as “mortality rates meta-analysis” is referred, data concerning title of the study, name of the first author, year of publication, study design, country where the study was conducted, total number of patients per type of acute metabolic emergency, total number of survivors, and total number of non-survivors were collected. No additional information was gained from personal communication.
Quality assessment of the studies
The Joanna Briggs Institute (JBI) critical appraisal checklist for case reports, which includes eight questions addressing the internal validity and risk of bias of case reports designs, particularly confounding and information bias, in addition to the importance of clear reporting, was used for quality assessment of case reports and case reports series [26–29]. All studies that failed to fulfill requirements of first six questions were considered as of “suboptimal quality”; controversially, an “optimal quality” remark was given.
Moreover, the JBI critical appraisal list for case control studies, which includes 12 questions addressing the internal validity and risk of bias of case control studies, was used for quality assessment of case series [27, 28]. All studies that were characterized as of “fair” or “poor” quality were considered as of “suboptimal quality”; controversially, an “optimal quality” remark was given.
Furthermore, quality of evidence was approached using GRADE (Grading of Recommendations, Assessment, Development and Evaluations), transparent framework for developing and presenting summaries of evidence [30–32]. GRADE level of evidence was rated down for risk of bias, imprecision, inconsistency, indirectness, and publication bias, whereas was rated up for large magnitude of effect.
Data synthesis
Classical regression without weighing each data point was used for data synthesis for the purposes of the “case reports meta-analysis”. The relevant odds ratios (OR) were used to construct a forest plot for visualization purposes using Revman 5.3 software [33].
As far as “mortality rates meta-analysis”, data synthesis was performed using MedCalc® Statistical Software version 19.6 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020). As effect estimates, mortality rates were extracted from each study and combined together using the random effects, generic inverse variance method of DerSimonian and Laird, which assigned the weight of each study in the pooled analysis inversely to its variance [34]. Random-effects model allows generalizing common effect size beyond the (narrowly defined) population included in the analysis [35]. However, as I2 has a substantial bias when the number of studies is small (positive when the true fraction of heterogeneity is small and negative when the true fraction of heterogeneity is large), the point estimate I2 should be interpreted cautiously when a meta-analysis has few studies; in fact, in small meta-analyses, confidence intervals should supplement or replace the biased point estimate I2 [36].
Statistical analysis
Regarding “mortality rates meta-analysis”, publication bias (small size effect) was assessed by funnel plot visualization for asymmetry and use of Egger’s and Begg’s tests. Heterogeneity was based on Q test and I2; Q test P value < 0.10 and/or I2 > 50% was indicative of significant heterogeneity and was further analyzed. Analysis of heterogeneity was performed through sensitivity analysis focusing on types of studies, types of acute metabolic emergencies, quality assessment, and GRADE level of evidence to seek whether qualitative or quantitative interaction exists. Univariate comparisons were performed with the use of Pearson’s χ2 test for discrete variables. All statistical tests were carried out using IBM SPSS Statistics software, version 26.0.0.0, for Windows (IBM Corp©).
Results
Case reports meta-analysis
Study characteristics
During the final pre-run search prior to the final analysis carried out on 7 January, 2021, 312 potentially relevant publications were identified through a thorough search of literature; 172 in EMBASE, 138 in PubMed/Medline, while two more publications of interest were identified through Google Scholar. No unpublished data of interest were detected. Personal contact contributed further information.
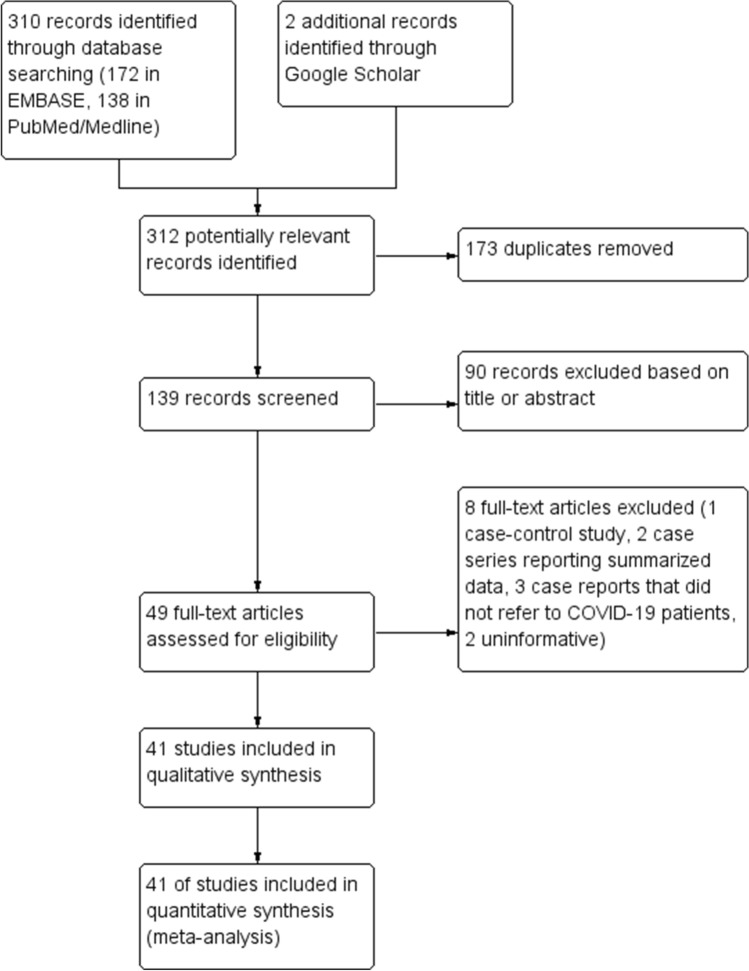
After the exclusion of 173 duplicates, all the remaining 139 publications were initially reviewed based only on title and abstract; 90 excluded as being ineligible. Thus, 49 full-text publications were further assessed for eligibility; from these, 8 failed to fulfill the eligibility criteria; three case reports did not refer to COVID-19 patients. All detailed data are provided in the supplementary Table 1, while relevant references have been included as supplementary ones at the “Supplementary Material” section. Forty-one publications referring to 71 separate case reports included in qualitative and quantitative synthesis (Fig. 1). All study characteristics are analytically presented in supplementary Table 2. The quality of the present study was evaluated as “high” using the AMSTAR 2 checklist.
Table 1.
“Case reports meta-analysis”: characteristics of COVID-19 patients in relation with outcome
| Parameters | N | Mean (± 95%CI)a, nb | Univariate analysis OR [95%CI] for death |
Univariate analysis P (Ρ after 1000 × bootstrapping) |
|---|---|---|---|---|
| Survivors | ||||
| Yes | 68 | 46 | NA | NA |
| No | 22 | |||
| Type of acute metabolic emergency | ||||
| DKA | 71 | 45 | NA | NA |
| EDKA | 6 | |||
| DKA/HHS | 19 | |||
| HHS | 1 | |||
| USA Origin | ||||
| USA | 71 | 36 | 1.71 [0.56–5.21] | 0.342 (0.335) |
| Other countries (except USA) | 35 | |||
| Combined DKA/HHS | ||||
| Yes | 71 | 19 | 4.72 [1.44–15.44] | 0.004 (0.006) |
| No | 52 | |||
| Male sex | ||||
| Yes | 67 | 45 | 0.97 [0.30–3.33] | 0.961 (0.955) |
| No | 22 | |||
| Age | ||||
| Mean (± 95 CI) | 67 | 47.8 [43.8–51.8] | 1.39 [0.97–2.00] per 10 increment | 0.073 (0.120) |
| BMI | ||||
| Mean (± 95 CI) | 32 | 28.6 [25.8–31.4] | 1.65 [0.92–2.97] per 5 increment | 0.096 (0.071) |
| HbA1c | ||||
| Mean (± 95 CI) | 50 | 11.7 [10.9–12.5] | 1.02 [0.82–1.26] | 0.891 (0.868) |
| New onset T1D/T2D | ||||
| Yes | 68 | 25 | 0.36 [0.10–1.25] | 0.108 (0.071) |
| No | 43 | |||
| Previous insulin treatment | ||||
| Yes | 17 | 9 | 5.99 [0.48–76.9]c | 0.165 (0.071) |
| No | 8 | |||
| Previous metformin treatment | ||||
| Yes | 18 | 10 | 0.14 [0.01–2.52]d | 0.184 (0.036) |
| No | 8 | |||
| Comorbidity number | ||||
| Mean (± 95 CI) | 55 | 1.8 [1.5–2.2] | 1.34 [0.86–2.09] per unit | 0.203 (0.171) |
| Day from onset of symptoms | ||||
| Mean (± 95 CI) | 64 | 6.6 [4.5–8.7] | 1.22 [0.83–1.80] per unit | 0.302 (0.203) |
| Disease status | ||||
| Mean (± 95 CI) | 64 | 3.0 [2.7–3.3] | 1.20 [0.90–1.60] per unit | 0.207 (0.083) |
| CRP | ||||
| Mean (± 95 CI) | 26 | 123 [76–150] | 1.60 [0.51–3.11] per 100 increment | 0.626 (0.653) |
| Ferritin | ||||
| Mean (± 95 CI) | 27 | 2075 [735–3410] | 1.54 [0.80–2.94] per 1000 increment | 0.179 (0.123) |
| D-dimers | ||||
| Mean (± 95 CI) | 29 | 3.9 [2.2–5.7] | 1.05 [0.89–1.23] per unit | 0.581 (0.595) |
| Glucose | ||||
| Mean (± 95 CI) | 71 | 626 [547–705] | 1.14 [0.97–1.33] per 100 increment | 0.115 (0.134) |
| Osmolarity | ||||
| Mean (± 95 CI) | 44 | 323 [315–331] | 1.25 [0.98–1.60] per 10 increment | 0.078 (0.076) |
| pH | ||||
| Mean (± 95 CI) | 63 | 7.13 [7.09–7.16] | 0.68 [0.44–1.04] per tenth increment | 0.074 (0.063) |
| Bicarbonates | ||||
| Mean (± 95 CI) | 47 | 9.7 [8.2–11.2] | 0.92 [0.80–1.05] per unit | 0.232 (0.301) |
| Ketones | ||||
| Mean (± 95 CI) | 15 | 5.4 [3.9–7.0] | 1.15 [0.67–1.97] per unit | 0.614 (0.325) |
| Lactates | ||||
| Mean (± 95 CI) | 22 | 4.1 [2.1–6.2] | 1.04 [0.85–1.27] per unit | 0.705 (0.602) |
| β-ΗΒ | ||||
| Mean (± 95 CI) | 16 | 5.9 [4.7–7.1] | 1.54 [0.60–3.94] per unit | 0.369 (0.052) |
| Anion gap | ||||
| Mean (± 95 CI) | 40 | 26.2 [23.5–28.9] | 1.05 [0.97–1.14] per unit | 0.249 (0.259) |
| Acute Kidney Injury | ||||
| Yes | 53 | 23 | 7.52 (1.95–28.9) | 0.003 (0.001) |
| No | 30 |
NA not applicable
aContinuous variables
bDiscrete variables
cReferring to patients with either T1D or T2D record
dReferring to patients with T2D record
Fig. 1.
“Case reports meta-analysis”: Study flow diagram
Table 2.
“Mortality rate meta-analysis”: Eligible studies along with study characteristics and quality / risk of bias assessment based on NOS
| Study | Design | Region | Type of emergency | N | Survivors | Non-survivors | Mortality rate | QA | GRADE level of evidence |
|---|---|---|---|---|---|---|---|---|---|
| Present study (“Case report meta-analysis”) | Meta-analysis | Greece | Overall | 68 | 46 | 22 | 0.324 | O |  |
| DKA | 44 | 32 | 12 | ||||||
| HHS | 1 | 1 | 0 | ||||||
| DKA/HHS | 18 | 8 | 10 | ||||||
| EDKA | 5 | 5 | 0 | ||||||
| Armeni [13] | Case series | UK | Overall | 26 | 24 | 2 | 0.077 | O |  |
| DKA | 11 | 10 | 1 | ||||||
| HHS | 2 | 2 | 0 | ||||||
| DKA/HHS | 13 | 12 | 1 | ||||||
| Alkundi [37] | Cross-sectional study | UK | Overall | 7 | 6 | 1 | 0.129 | S |  |
| DKA | 7 | 6 | 1 | ||||||
| Chamorro-Pareja [20] | Case series | USA | Overall | 50 | 25 | 25 | 0.500 | S |  |
| DKA | 50 | 25 | 25 |
QA quality assessment, L low, VL very low
Quality assessment of the studies
Quality remarks are provided in supplementary Table 2; all details concerning quality assessment items are depicted analytically in supplementary Table 3. The inter-rater agreement between the two authors carried out the quality assessment process was high, as kappa was 0.87 (95% CI 0.79–0.95). There was no difference between studies of “optimal” and “suboptimal” quality regarding outcome (P = 0.756).
Table 3.
“Mortality rate meta-analysis”: Sensitivity analysis
| Mortality rate | I2 | ||||
|---|---|---|---|---|---|
| Combined mean | 95% CI | Mean | 95% CI | P | |
| Overall result | |||||
| All studies included | 0.271 | 0.112–0.469 | 82.8 | 56.1–93.3 | 0.0006 |
| Sensitivity analysis according to study type | |||||
| Meta-analyses excluded | 0.241 | 0.027–0.574 | 88.6 | 68.4–95.9 | 0.0002 |
| Sensitivity analysis according to emergency type | |||||
| Only DKA patients included | 0.289 | 0.134–0.475 | 71.8 | 20.0–90.1 | 0.0138 |
| Only HHS patients included | 0.112 | 0.009–0.495 | 0.0 | 0.0–0.0 | 0.8523 |
| Only EDKA patients included | 0.000 | N/A | N/A | N/A | N/A |
| Only DKA/HHS patients included | 0.315 | 0.012–0.780 | 86.8 | 48.2–96.7 | 0.0058 |
| Sensitivity analysis according to quality assessment | |||||
| Studies of “suboptimal” quality excluded | 0.203 | 0.030–0.475 | 85.7 | 42.5–96.4 | 0.0082 |
| Sensitivity analysis according to GRADE level of evidence | |||||
| Studies of GRADE “very low” level of evidence excluded | 0.203 | 0.030–0.475 | 85.7 | 42.5–96.4 | 0.0082 |
| Sensitivity analysis at study level | |||||
| Present study (“case reports meta-analysis”) excluded | 0.241 | 0.027–0.574 | 88.6 | 68.4–95.9 | 0.0002 |
| Armeni, 2020 excluded | 0.360 | 0.207–0.529 | 67.2 | 0.0–90.5 | 0.0472 |
| Alkundi, 2020 excluded | 0.296 | 0.110–0.528 | 87.6 | 65.1–95.6 | 0.0003 |
| Chamorro-Pareja, 2020 excluded | 0.196 | 0.057–0.391 | 72.9 | 8.7–91.9 | 0.0251 |
N/A not applicable
Primary outcome
The types of acute metabolic emergencies observed were DKA (45/71, 63.4%), EDKA (6/71, 8.5%), combined DKA/HHS (19/71, 26.8%), and HHS (1/71, 1.4%). Overall mortality was 32.4% (22/68 patients; 3 missing).
Absence of combined DKA/HHS (P = 0.006), and absence of AKI (P = 0.001) are correlated with increased OR for survival. Among patients with T1D or T2D, administration of insulin was associated with an increased OR of succumbing (5.99; 95% CI 0.48–76.9). In contrast, T2D patients who received metformin had an OR of 0.14 (95% CI 0.01–2.52).
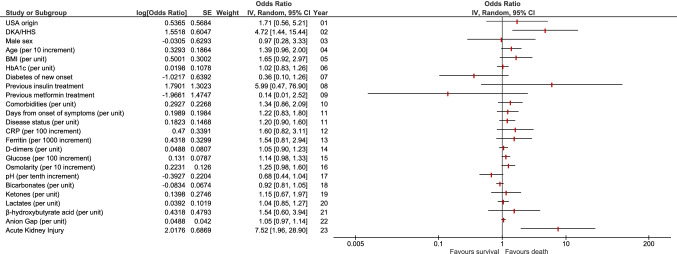
BMI (P = 0.071), new onset of diabetes, either T1D or T2D (P = 0.071), DS (P = 0.083), osmolarity (P = 0.076), pH value (P = 0.063), and β-ΗΒ (P = 0.052) were considered needing further evaluation and, thus, were included in multivariate regression analysis. Detailed univariate analysis concerning correlations of patients characteristics with outcome is analytically presented at Table 1 and Fig. 2.
Fig. 2.
“Case reports meta-analysis”: Forest plot depicting various patients’ characteristics odds ratios OR for death
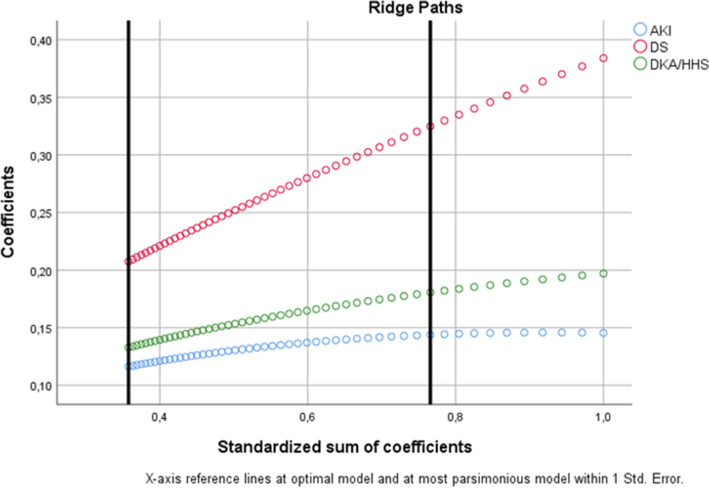
The most parsimonious multivariate model is highly significant (P = 10–4), suggesting that COVID-19 DS4 (P = 3 × 10–8), presence of DKA/HHS (P = 0.021), and development of AKI (P = 0.037) are all independently correlated with death (Fig. 3).
Fig. 3.
“Case reports meta-analysis”: Ridge paths as derived from optimal scaling regularization process for the most parsimonious multivariate model
Secondary outcome
Increased DS (P = 0.003), elevated lactates (P < 0.001), augmented anion gap (P < 0.001), and presence of AKI (P = 0.002) were associated with DKA/HHS.
SGLT-2i administration was linked with EDKA (Fisher’s exact P = 0.004); however, a negative association with AKI was noted (P = 0.023). Furthermore, metformin use was not associated with lactic acidosis (P = 0.042).
Mortality rates meta-analysis
Study characteristics
During the final pre-run search prior to the final analysis carried out on January 7, 2021, 312 potentially relevant publications were identified through a thorough search of literature; 172 in EMBASE, 138 in PubMed/Medline, while two more publications of interest were identified through Google Scholar. A single source of unpublished data of interest was detected, namely that of the present study concerning the results derived from “case reports meta-analysis”. No personal contact with any author that considered necessary contributed any additional information.
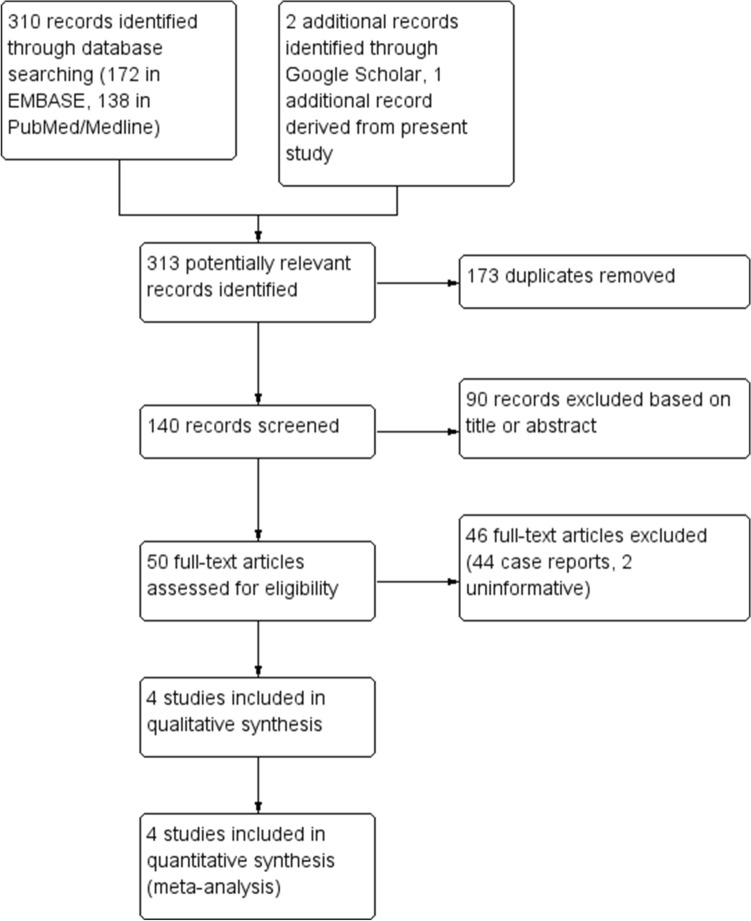
After the exclusion of 173 duplicates, all the remaining 140 publications were initially reviewed based only on title and abstract; 90 excluded as being ineligible. Thus, 50 full-text publications were further assessed for eligibility; from these, 46 failed to fulfill the eligibility criteria. The remaining 4 publications included in qualitative synthesis and quantitative synthesis/statistical analysis. These publications included 152 patients (Fig. 4).
Fig. 4.
“Mortality rate meta-analysis”: Study flow diagram
All characteristics regarding title of the study, name of the first author, country where the study was conducted, type of diabetes-related acute metabolic emergency, total number of survivors, total number of non-survivors, and mortality rate are analytically presented in Table 2.
Quality assessment and risk of bias
Quality remarks are provided in Table 2. All details concerning the JBI critical appraisal checklist for case reports quality assessment items are depicted analytically in Supplementary Table 4; similarly, the JBI critical appraisal list for case–control studies quality assessment items are shown in Supplementary Table 5. GRADE level of evidence is presented in Supplementary Table 6.
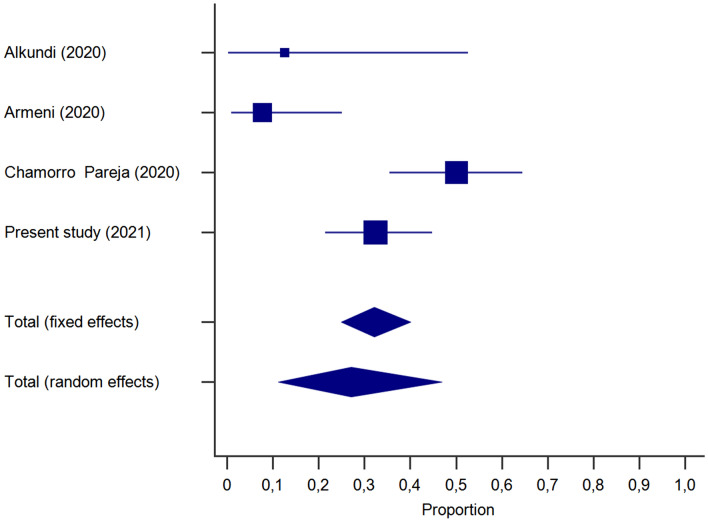
Primary outcome
Combined mortality rate was found to be 27.1% (95% CI 11.2–46.9%) (Fig. 5). Heterogeneity was considerable (I2 = 83%; 95% CI 56–93%), corrected to 67% according to Von Hippel adjustment for small meta-analyses; this value was based on an approximation for I2 = 80% yielding a real value 64%, and consequently, an bias leading to 16% overestimation (Supplementary Figure 1).
Fig. 5.
“Mortality rate meta-analysis”: Forest plot depicting combined mortality rate from diabetes-associated acute metabolic emergencies in COVID-19 patients
Publication bias (small size effect)
No significant publication bias (small size effect) was detected as funnel plot presented no apparent asymmetry (Supplementary Figure 2). Moreover, both Egger’s and Begg’s tests yielded an insignificant result (P = 0.44 and P = 0.50, respectively).
Analysis of heterogeneity
Sensitivity analysis was carried out according to: (i) study type (meta-analyses included vs. excluded), (ii) emergency type (DKA patients included vs. excluded, EDKA patients included vs. excluded, HHS patients included vs. excluded, DKA/HHS patients included vs. excluded), (iii) quality assessment (studies of “suboptimal” quality included vs. excluded), (iv) GRADE level of evidence (studies of “very low” level of evidence excluded vs. included); furthermore, sensitivity analysis was performed at single study level. There was no difference as deduced by the inspection of the relevant confidence intervals and thus, sensitivity analysis typically failed to explain the observed heterogeneity (Table 3).
Nevertheless, sensitivity analysis provided some hints that combined mortality rate may vary considerably according to the type of metabolic emergency. In detail, COVID-19 patients with DKA had a combined mortality rate of 28.9% (95% CI 13.4–47.5%); I2 was considerable, reaching (I2 = 72%; 95% CI 20–90%); when mixed DKA/HHS was present, the combined mortality observed reached 31.5% (95% CI 1.2–78.0%) accompanied by a high I2 value (I2 = 87%; 95% CI 48–97%). In contrast, COVID-19 patients with HHS (without ketoacidosis) had more compromised combined mortality rate (11.2%, 95% CI 0.9–49.5%); I2 was null. Lastly, only one study contributed EDKA patients, who all survived; thus, combined mortality rate for COVID-19 patients with EDKA is in fact a constant (0%) (Table 3).
Discussion
We describe three major determinants of unfavorable outcome during acute metabolic emergencies in diabetes (DKA, HHS, EDKA, and DKA/HHS) in COVID-19 patients: (i) COVID-19 critical illness necessitating mechanical ventilation (DS4), (ii) simultaneous presence of ketoacidosis and hyperosmosis, and (iii) AKI.
Moreover, we summarize all data available on mortality due to diabetes-associated acute metabolic emergencies in COVID-19 patients (7.7% [13], 12.9% [37], 50% [20], and 32.4% from “case report meta-analysis” of ours), concluding that these entities are characterized by a considerable mortality (CMR: 27.1%; 95% CI 11.2–46.9%).
Our findings regarding the independent correlation of critical illness and mortality during COVID-19-related acute metabolic emergencies in diabetes confront with the observation that survivors presented lower CRP levels when compared with non-survivors; additionally, the former required intubation and mechanical ventilation more frequently [20].
Furthermore, we exhibited an independent correlation of AKI with mortality during COVID-19-related DKA, EDKA, DKA/HHS, and HHS. AKI is quite common among patients without critical illness and usually has a mixed etiology intertwining sepsis, ischemia and nephrotoxicity [38]. AKI was observed in 92% (23/25) and 60% (15/25) of COVID-19-related DKA non-survivors and survivors, respectively; these data indicate that AKI is significantly correlated with death in patients with COVID-19-related DKA. Similarly, renal replacement therapy was required in 40% (10/25) and 4% (1/25) COVID-19-related DKA non-survivors and survivors, respectively, implying that renal replacement therapy is significantly correlated with death in these patients [20].
Additionally, we demonstrated an independent correlation of mixed DKA/HHS related to COVID-19 infection with non-surviving. Our results are in keeping with Pal et al., who describe a statistically significant difference in arterial blood pH between COVID-19-related DKA survivors when compared with non-survivors [21]. Despite that data linking increased osmolarity with increased fatality rate in COVID-19 patients are lacking, it is well known that death occurs in 5–16% of patients with HHS in general, a rate that is about tenfold higher than that reported for DKA [39–41]. Moreover, a hypertonic environment impairs the immune response, thus facilitating the development of infection [42].
We have noticed that all patients but one (a patient with gestational diabetes) who had developed EDKA received SGLT-2i treatment; however, a negative association with AKI was noted, thus implying a prophylactic effect on renal function. Treatment with SGLT-2i has been reported to trigger EDKA in T2D patients with or without COVID-19 infection, usually during other infections, sepsis or surgery [43–45]. These regimens might be prescribed even for T1D; interestingly, a single case report of a patient with T1D who received empagliflozin 25 mg q24h and developed EDKA during COVID-19 pneumonia has been recently published [46]. Glycaemic stability can mislead the clinician, since hyperglycosuria induced by SGLT-2i may blunt hyperglycaemia during infection and contribute to a lack of insulin, finally promoting ketogenesis [43]. Therefore, it is strongly advised that the use of SGLT-2i should be discontinued at once as soon as COVID-19 is diagnosed, while the exclusive administration of insulin is considered the safest choice [45, 46]. Nevertheless, our finding deserves further evaluation being in keeping with the fact that SGLT2-i administration slows the decline observed in the annual renal function in T2D patients with eGFR < 60 ml/min/1.73 m2, in non-COVID-19 patients [47].
We have not detected any correlation of antidiabetic drug category other than SGLT-2i with any special type of metabolic emergency or outcome; this observation conveys the limitations of the small sample size of the present study. GLP-1 RAs reduce circulating inflammatory biomarkers in diabetic and/or obese patients, while insulin reduces these biomarkers in critically ill patients. Moreover, the DPP-4 is the entry receptor of MERSCoV, raising concerns about the impact of DPP-4i during the course of coronavirus infection [48]. Indeed, SGLT2i has been associated with a 3.7% risk for death from COVID-19, which is comparable with that of GLP1-RA (3.8%; RR 1.03) but lower than that of DPP-4i (10.6%; RR 2.6), implying that use of DPP-4i before infection with SARS-CoV-2 might even have a harmful effect [49].
Interestingly, we demonstrated that insulin-treated patients presented an increased OR to succumb in contrast with those treated with metformin; furthermore, we observed that prior metformin use was not correlated with concomitant lactic acidosis. Though insulin administration had been associated with poor prognosis by another group of investigators [50], it restores ACE and ACE2 serum levels, thus hypothesizing that it exerts a protective effect at least in patients that are non-insulin-depleted [51]. Therefore, this finding of ours could reflect a confounder effect due to either the type of diabetes, or increased age. T1D patients, who are by definition insulin dependent, when compared with T2D patients, are more prone to adverse outcome during COVID-19 infection [5]; moreover, unfavorable outcome was observed more often in older patients presenting COVID-19-related DKA [20].
COVID-19 might either induce new onset diabetes or unmask previously undiagnosed T1D or T2D; elevated HbA1c values at admission confronts for the latter [3]. Both SARS and COVID-19 have been reported to trigger transient insulin resistance and hyperglycaemia. SARS results in elevated glucose during admission; however, glucose intolerance is resolved at hospital discharge [52]. SARS-CoV-2 can trigger severe diabetic ketoacidosis at presentation in individuals with new-onset diabetes despite that evidence etiologically linking SARS-CoV-2 with T1D are lacking [53]. This COVID-19-induced insulin resistance may partly explain poor responses to DKA management [52].
Emerging data indicate a bidirectional relationship between T2D and COVID-19 [54]. Impairment of innate and adaptive immunity tames the ability to fight infection in patients with diabetes and particularly in obese. The association between COVID-19 and hyperglycemia in elderly patients with T2D might reflect metabolic inflammation and exaggerated cytokine release. SARS-CoV2 infection can deteriorate glycemic control by enhancing insulin resistance and impaired insulin secretion, thus leading to DKA [11, 55]. The unique interactions between SARS-CoV-2 and the RAAS might provide yet another mechanism in the pathophysiology of DKA first by direct entry of SARS-CoV-2 into pancreatic islet cells worsening b-cell injury, and second by downregulation of ACE2 after viral entry that can lead to unopposed angiotensin II and subsequent insulin secretion impedance [56, 57]. Moreover, as the relationship between SARS-CoV-2 and the RAAS increases pulmonary vascular permeability and worsens damage to lung parenchyma, fluid replacement needs to be administered judiciously to avoid aggravating pulmonary injury [54, 58, 59].
Concerning mortality rates in COVID-19 patients who had developed DKA, EDKA, DKA/HHS, and HHS, they have been reported to range from values as low as 7.7% (2/26 patients) [13] and 12.9% (1/7 patients) [37], to 50% (25/50 patients) in the three published case series or cross-sectional studies till present [20]. Interestingly, our “case reports meta-analysis”, which was based on individualized data throughout the whole world, concluded to an overall mortality of 32.4% (22/68 patients; 3 missing), which is fairly close to the CMR resulted from the above mentioned data, as processed during our “mortality rate meta-analysis”.
Armeni et al. had a substantial contribution to the topic by analytically describing 35 patients with COVID-19, 26 of which had either DKA (n = 11), or HHS (n = 2), or mixed DKA/HHS (n = 13). This study, although being a case series, is multicenter and of well-established quality [13].
Of interest, Chamorro-Pareja et al. reported an unusually high mortality rate among 50 COVID-19 patients who presented DKA (50%) [20]. In fact, comparing relevant data from all included studies over a 2 × 4 contingency table (df = 3), a statistically significant result is obtained (χ2 P = 0.014); this variability is partly explained by the current “case report meta-analysis” of ours who reported that, apart from the presence of mixed DKA/HHS, two other parameters, namely the presence of acute kidney injury as well as the necessity for mechanical ventilation of COVID-19 patients (critical illness or disease status 4 illness) are key determinants of outcome.
Alkundi et al. report the intriguing—if not controversial—finding that COVID-19 patients presented with DKA, when compared with COVID-19 patients who had not developed DKA, were more likely to survive (P = 0.046). Their analysis was carried out with the use of Kaplan–Meier survival curves. However, the authors did not adjust their finding for potent confounders, using Cox-regression, most probably due to the small number of sample size. As a matter of fact, their result needs at least to be considered cautiously and has to be further evaluated in larger studies [37].
There are several limitations that characterize the present study to be further discussed and considered. Concerning “case report meta-analysis”, it relies exclusively in case reports, which lack the ability to generalize or establish cause-effect relationship, while conveying all danger of over-interpretation, publication bias, retrospective design, and distraction of reader when focusing on the unusual. However, the major merits of case reporting focus on detecting novelties, and generating hypotheses, which are considered absolutely necessary during the course of COVID-19 pandemic [60]. Another serious query could focus on the decision to proceed to the meta-analysis despite the considerable amount of heterogeneity. However, several reasons might support our approach: (1) there was little evidence of publication bias, (2) there was no considerable qualitative interaction, and (3) sensitivity analysis provided hints that heterogeneity might be correlated with the type of metabolic emergency: DKA and mixed DKA/HHS present a considerable CMR of about 30%, while HHS (and perhaps EDKA) is characterized by less aggravated clinical course, presenting a CMR of about 10% or even less.
Furthermore, as far as the “mortality rates meta-analysis” is referred, the crucial limitation might be dual: first, the combination of data derived from different kind of studies, namely two case report series, one case–control study, and the present “case report meta-analysis” and second, the very small number of studies included [61]; however, as the topic is totally novel, any study that respects adherence to protocol followed, investigates causes of heterogeneity, and assesses the impact of risk of bias on the evidence synthesis might be valuable. Furthermore, we are totally aware that including a self-report in a meta-analysis can import a severe bias. In fact, there are at least four reasons which alleviate this danger: first, our “case reports meta-analysis” exhibits the least deviation from the vertical line of the funnel plot, representing the mean; second, sensitivity analysis did not reveal any profound difference regarding combined mortality rate and I2; third, it is of “optimal” quality and has a GRADE “low” level of evidence, namely the best that a study of such a kind can achieve at first; fourth, it is the most representative as it is the only that includes patients presenting all four different kind of emergencies (DKA, HHS, EDKA, and combined DKA/HHS) as well as patients from 41 different sources.
As a conclusion, coexistence of COVID-19 and diabetes-related acute metabolic emergencies lead to increased mortality. COVID-19 critical illness necessitating intubation and mechanical ventilation, coexistence of hyperosmosis along with ketoacidosis and development of AKI are all positively correlated with mortality. Previous SGLT-2i treatment, though linked with EDKA, demonstrated a negative association with AKI thus implying a prophylactic effect on renal function; therefore, the impact of these regimens in COVID-19 patients remains to be further evaluated.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Six reviewers (VP, M-VK, D-GZ, S-AB, PA, and NT) performed study selection, data extraction, and quality assessment working simultaneously as three independent couples (one for screening and the other for checking decisions). These couples were blinded to each other's decisions. D.F. was responsible to dissolve any disagreement.
Declarations
Conflict of interest
Author VP, Author M-VK, Author D-GZ, Author S-AB, Author PA, Author NT, and Author DF declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and/or with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma WX, Ran XW. The management of blood glucose should be emphasized in the treatment of COVID-19. Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51(2):146–150. doi: 10.12182/20200360606. [DOI] [PubMed] [Google Scholar]
- 3.Kuchay MS, Reddy PK, Gagneja S, et al. Short term follow-up of patients presenting with acute onset diabetes and diabetic ketoacidosis during an episode of COVID-19. Diabetes Metab Syndr. 2020;14(6):2039–2041. doi: 10.1016/j.dsx.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gregory JM, Slaughter JC, Duffus SH, et al. COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic's impact in type 1 and type 2 diabetes. Diabetes Care. 2021;44(2):526–532. doi: 10.2337/dc20-2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGurnaghan SJ, Weir A, Bishop J, et al.; Public Health Scotland COVID-19 Health Protection Study Group; Scottish Diabetes Research Network Epidemiology Group. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diabetes Endocrinol. 2020. 8587(20)30405–8.
- 6.Al Hayek AA, Robert AA, Alotaibi ZK, et al. Clinical characteristics of hospitalized and home isolated COVID-19 patients with type 1 diabetes. Diabetes Metab Syndr. 2020;14(6):1841–1845. doi: 10.1016/j.dsx.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chowdhury S, Goswami S. COVID-19 and type 1 diabetes: dealing with the difficult duo. Int J Diabetes Dev Ctries. 2020;14:1–6. doi: 10.1007/s13410-020-00846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China JAMA Intern Med. 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang JK, Lin SS, Ji XJ, et al. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47(3):193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muniangi-Muhitu H, Akalestou E, Salem V, et al. Covid-19 and diabetes: a complex bidirectional relationship. Front Endocrinol (Lausanne) 2020;8(11):582936. doi: 10.3389/fendo.2020.582936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coate KC, Cha J, Shrestha S, Wang W, HPAP Consortium. Brissova M, et al. Powers AC SARS-CoV-2 cell entry factors ACE2 and TMPRSS2 are expressed in the microvasculature and ducts of human pancreas but are not enriched in β cells. Cell Metab. 2020;32(6):1028–1040. doi: 10.1016/j.cmet.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Armeni E, Aziz U, Qamar S, et al. Protracted ketonaemia in hyperglycaemic emergencies in COVID-19: a retrospective case series. Lancet Diabetes Endocrinol. 2020;8(8):660–663. doi: 10.1016/S2213-8587(20)30221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai PH, Lai WY, Lin YY, et al. Clinical manifestation and disease progression in COVID-19 infection. J Chin Med Assoc. 2021;84(1):3–8. doi: 10.1097/JCMA.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 15.Beliard K, Ebekozien O, Demeterco-Berggren C, et al. Increased DKA at presentation among newly diagnosed type 1 diabetes patients with or without COVID-19: Data from a multi-site surveillance registry. J Diabetes. 2021;13(3):270–272. doi: 10.1111/1753-0407.13141. [DOI] [PubMed] [Google Scholar]
- 16.Muneer M, Akbar I. acute metabolic emergencies in diabetes: DKA, HHS and EDKA. Adv Exp Med Biol. 2021;1307:85–114. doi: 10.1007/5584_2020_545. [DOI] [PubMed] [Google Scholar]
- 17.Umpierrez G, Korytkowski M. Diabetic emergencies—ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12(4):222–232. doi: 10.1038/nrendo.2016.15. [DOI] [PubMed] [Google Scholar]
- 18.Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care. 2015;38(9):1638–1642. doi: 10.2337/dc15-1380. [DOI] [PubMed] [Google Scholar]
- 19.Khawandanah J. Double or hybrid diabetes: a systematic review on disease prevalence, characteristics and risk factors. Nutr Diabetes. 2019;9(1):33. doi: 10.1038/s41387-019-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chamorro-Pareja N, Parthasarathy S, Annam J, et al. Letter to the editor: unexpected high mortality in COVID-19 and diabetic ketoacidosis. Metabolism. 2020;110:154301. doi: 10.1016/j.metabol.2020.154301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pal R, Banerjee M, Yadav U, et al. Clinical profile and outcomes in COVID-19 patients with diabetic ketoacidosis: a systematic review of literature. Diabetes Metab Syndr. 2020;14(6):1563–1569. doi: 10.1016/j.dsx.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleming N, Sacks LJ, Pham C, et al. An overview of COVID-19 in people with diabetes pathophysiology and considerations in the inpatient setting. Diabet Med. 2020;29:e14509. doi: 10.1111/dme.14509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;21(358):j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rainkie DC, Abedini ZS, Abdelkader NN. Reporting and methodological quality of systematic reviews and meta-analysis with protocols in Diabetes Mellitus Type II: a systematic review. PLoS ONE. 2020;15(12):e0243091. doi: 10.1371/journal.pone.0243091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–2133. doi: 10.11124/JBISRIR-D-19-00099. [DOI] [PubMed] [Google Scholar]
- 27.Ma LL, Wang YY, Yang ZH, et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7(1):7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute, 2017. https://reviewersmanual.joannabriggs.org/
- 29.Murad MH, Sultan S, Haffar S, et al. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23(2):60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, GRADE Working Group What is "quality of evidence" and why is it important to clinicians? BMJ. 2008;336(7651):995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guyatt GH, Oxman AD, Vist GE, GRADE Working Group et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 33.Review Manager Web (RevMan Web). The Cochrane Collaboration, 2019. revman.cochrane.org
- 34.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 36.Von Hippel PT. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med Res Methodol. 2015;14(15):35. doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alkundi A, Mahmoud I, Musa A. Clinical characteristics and outcomes of COVID-19 hospitalized patients with diabetes in the United Kingdom: a retrospective single centre study. Diabetes Res Clin Pract. 2020;165:108263. doi: 10.1016/j.diabres.2020.108263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Makris K, Spanou L. Acute kidney injury: definition, pathophysiology and clinical phenotypes. Clin Biochem Rev. 2016;37(2):85–98. [PMC free article] [PubMed] [Google Scholar]
- 39.Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Diabetes Care. 2014;37(11):3124–3131. doi: 10.2337/dc14-0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bhowmick SK, Levens KL, Rettig KR. Hyperosmolar hyperglycemic crisis: an acute life-threatening event in children and adolescents with type 2 diabetes mellitus. Endocr Pract. 2005;11(1):23–29. doi: 10.4158/EP.11.1.23. [DOI] [PubMed] [Google Scholar]
- 41.Fadini GP, de Kreutzenberg SV, Rigato M, et al. Characteristics and outcomes of the hyperglycemic hyperosmolar non-ketotic syndrome in a cohort of 51 consecutive cases at a single center. Diabetes Res Clin Pract. 2011;94(2):172–179. doi: 10.1016/j.diabres.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 42.Lang KS, Weigert C, Braedel S, et al. Inhibition of interferon-gamma expression by osmotic shrinkage of peripheral blood lymphocytes. Am J Physiol Cell Physiol. 2003;284(1):C200–C208. doi: 10.1152/ajpcell.00259.2002. [DOI] [PubMed] [Google Scholar]
- 43.Menghoum N, Oriot P, Hermans MP, et al. Cétose ou acidocétose diabétique euglycémique chez des patients diabétiques de type 2 traités par inhibiteurs du SGLT2: une série de cas cliniques en Belgique [Diabetic euglycemic ketosis or ketoacidosis in individuals with type 2 diabetes treated by SGLT2 inhibitors: a series of Belgian clinical cases] Rev Med Intern. 2020;41(4):226–231. doi: 10.1016/j.revmed.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 44.Ozer O, Yorulmaz G. Euglycemic diabetic ketoacidosis associated with empagliflozin use in the course of the SARS-Cov-2 pandemic. J Coll Physicians Surg Pak. 2020;30(10):110–111. doi: 10.29271/jcpsp.2020.supp2.110. [DOI] [PubMed] [Google Scholar]
- 45.Milder TY, Stocker SL, Day RO, et al. Potential safety issues with use of sodium-glucose cotransporter 2 inhibitors, particularly in people with type 2 diabetes and chronic kidney disease. Drug Saf. 2020;43(12):1211–1221. doi: 10.1007/s40264-020-01010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koufakis T, Metallidis S, Zebekakis P, et al. Sodium-glucose cotransporter 2 inhibitors in the era of COVID-19 pandemic: is the benefit to risk ratio still favorable? J Diabetes Sci Technol. 2020;14(4):745–747. doi: 10.1177/1932296820932155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hirai T, Kitada M, Monno I, et al. Sodium-glucose cotransporter 2 inhibitors in type 2 diabetes patients with renal function impairment slow the annual renal function decline, in a real clinical practice. J Diabetes Investig. 2021 doi: 10.1111/jdi.13502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Orioli L, Hermans MP, Thissen JP, et al. COVID-19 in diabetic patients: related risks and specifics of management. Ann Endocrinol (Paris) 2020;81(2–3):101–109. doi: 10.1016/j.ando.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Israelsen SB, Pottegård A, Sandholdt H, Madsbad S, Thomsen RW, Benfield T. Comparable COVID-19 outcomes with current use of GLP-1 receptor agonists, DPP-4 inhibitors or SGLT-2 inhibitors among patients with diabetes who tested positive for SARS-CoV-2. Diabetes Obes Metab. 2021 doi: 10.1111/dom.14329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen Y, Yang D, Cheng B, et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020;43(7):1399–1407. doi: 10.2337/dc20-0660. [DOI] [PubMed] [Google Scholar]
- 51.Roca-Ho H, Riera M, Palau V, et al. Characterization of ACE and ACE2 expression within different organs of the NOD mouse. Int J Mol Sci. 2017;18(3):563. doi: 10.3390/ijms18030563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goldman N, Fink D, Cai J, et al. High prevalence of COVID-19-associated diabetic ketoacidosis in UK secondary care. Diabetes Res Clin Pract. 2020;166:108291. doi: 10.1016/j.diabres.2020.108291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boddu SK, Aurangabadkar G, Kuchay MS. New onset diabetes, type 1 diabetes and COVID-19. Diabetes Metab Syndr. 2020;14(6):2211–2217. doi: 10.1016/j.dsx.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Apicella M, Campopiano MC, Mantuano M, et al. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8(9):782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sandooja R, Vura NVRK, Morocco M. Heightened ACE activity and unfavorable consequences in COVID-19 diabetic subjects. Int J Endocrinol. 2020;16(2020):7847526. doi: 10.1155/2020/7847526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chee YJ, Tan SK, Yeoh E. Dissecting the interaction between COVID-19 and diabetes mellitus. J Diabetes Investig. 2020;11(5):1104–1114. doi: 10.1111/jdi.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fignani D, Licata G, Brusco N, et al. SARS-CoV-2 receptor angiotensin i-converting enzyme type 2 (ACE2) is expressed in human pancreatic β-cells and in the human pancreas microvasculature. Front Endocrinol (Lausanne) 2020;13(11):596898. doi: 10.3389/fendo.2020.596898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bornstein SR, Rubino F, Khunti K, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(6):546–550. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Priyambada L, Wolfsdorf JI, Brink SJ, et al. ISPAD clinical practice consensus guideline: diabetic ketoacidosis in the time of COVID-19 and resource-limited settings-role of subcutaneous insulin. Pediatr Diabetes. 2020;21(8):1394–1402. doi: 10.1111/pedi.13118. [DOI] [PubMed] [Google Scholar]
- 60.Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes. 2014;23(7):264. doi: 10.1186/1756-0500-7-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Michael H, Thornton S, Xie M, et al. Exact inference on the random-effects model for meta-analyses with few studies. Biometrics. 2019;75(2):485–493. doi: 10.1111/biom.12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.