Key Points
Question
Is disturbed sleep associated with depression in children and youths?
Findings
In this meta-analysis of 16 studies including 27 073 patients, pooled estimates supported the role of disturbed sleep as a risk factor for depression in children and youths. Effect size estimates were small but statistically significant.
Meaning
This study suggests that disturbed sleep is a component of the multifaceted risk profile of depression and should be included in prevention programs as early as childhood.
Abstract
Importance
Disturbed sleep represents a potentially modifiable risk factor for depression in children and youths that can be targeted in prevention programs.
Objective
To evaluate the association between disturbed sleep and depression in children and youths using meta-analytic methods.
Data Sources
Embase, MEDLINE, PsycINFO, Scopus, Web of Science, and ProQuest Dissertations & Theses Global were searched for articles published from 1980 to August 2019.
Study Selection
Prospective cohort studies reporting estimates, adjusted for baseline depression, of the association between disturbed sleep and depression in 5- to 24-year-old participants from community and clinical-based samples with any comorbid diagnosis. Case series and reports, systematic reviews, meta-analyses, and treatment, theoretical, and position studies were excluded. A total of 8700 studies met the selection criteria. This study adhered to the guidelines of the Preferred Reporting Items for Systematic Reviews (PRISMA) and Meta-analyses and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) statements.
Data Extraction and Synthesis
Study screening and data extraction were conducted by 2 authors at all stages. To pool effect estimates, a fixed-effect model was used if I2 < 50%; otherwise, a random-effects model was used. The I2 statistic was used to assess heterogeneity. The risk of bias was assessed using the Research Triangle Institute Item Bank tool. Metaregression analyses were used to explore the heterogeneity associated with type of ascertainment, type of and assessment tool for disturbed sleep and depression, follow-up duration, disturbed sleep at follow-up, and age at baseline.
Main Outcome and Measures
Disturbed sleep included sleep disturbances or insomnia. Depression included depressive disorders or dimensional constructs of depression. Covariates included age, sex, and sociodemographic variables.
Results
A total of 22 studies (including 28 895 patients) were included in the study, of which 16 (including 27 073 patients) were included in the meta-analysis. The pooled β coefficient of the association between disturbed sleep and depression was 0.11 (95% CI, 0.06-0.15; P < .001; n = 14 067; I2 = 50.8%), and the pooled odds ratio of depression in those with vs without disturbed sleep was 1.50 (95% CI, 1.13-2.00; P = .005; n = 13 006; I2 = 87.7%). Metaregression and sensitivity analyses showed no evidence that pooled estimates differed across any covariate. Substantial publication bias was found.
Conclusions and Relevance
This meta-analysis found a small but statistically significant effect size indicating an association between sleep disruption and depressive symptoms in children and youths. The high prevalence of disturbed sleep implies a large cohort of vulnerable children and youths who could develop depression. Disrupted sleep should be included in multifaceted prevention programs starting in childhood.
This systematic review and meta-analysis evaluates the association between disturbed sleep and depression in children and youths.
Introduction
Worldwide, depression is the third leading cause of disability, and its prevalence is increasing.1 Depression can start in childhood, and onset usually peaks at 20 years of age.2 Factors associated with first-onset depression in young adulthood include female sex, familial history of mood disorders, childhood sexual abuse, anxiety disorder, poor physical health, and subthreshold depressive symptoms, including disturbed sleep.3 Treatment of depression during adolescence has shown limited effectiveness.4,5,6 As a result, early identification and prevention may be a critical complementary tool to attenuate the risk trajectory of depression.
Emerging concepts for depression prevention point to multifaceted approaches to increase the level and duration of the intervention effects.7 Targeting modifiable risk factors is an additional, promising strategy for depression prevention. Multiple risk factors underpin an individual’s vulnerability to depression,2 and understanding the makeup of the risk profile is crucial for planning prevention programs. A meta-analysis of randomized clinical trials (RCTs) on depression prevention programs in 5- to 18-year-old participants found minimal impact that decayed over time, stressing the importance of developing innovative approaches.8
Disturbed sleep in adult and elderly individuals has been increasingly recognized as a risk factor for depression.9,10,11,12,13,14 Consequently, sleep has been the target of several selective and indicated depression prevention programs, with promising results.15
In children and youths, disturbed sleep and depression often co-occur in both clinical16 and community-based17 samples, with prevalence rates varying widely across studies.18 Disturbed sleep can be assessed by subjective measures, including child-, teacher-, or parent-reported questionnaires and interviews. The prevalence of disturbed sleep is 19.5% among children and is equally distributed among boys and girls; among youths, the prevalence rate is 17.4% and higher among girls (19.9%).19 There is evidence for a prospective association between disturbed sleep and depression in children and youths, whereas there is little support for the reverse association.20,21 Studies investigating the bidirectionality between the 2 constructs have provided mixed results,22,23,24,25,26 suggesting that a more complex cause may underlie this association. In a systematic review summarizing studies on the prospective association between insomnia and depression from 2014 to 2017, Pigeon et al10 found that, among 4 studies of children and youths, 3 found a significant association between insomnia and depression.23,27,28 Two meta-analyses provided quantitative data on the prospective association between disturbed sleep and depression in children and youths.20,29 The meta-analysis by Baglioni et al29 included 3 studies representing 7404 participants between 6 and 16 years of age and provided a pooled odds ratio (OR) of 2.0 (95% CI, 1.5-2.7) from community-based samples. The meta-analysis by Lovato et al20 included 7 studies representing 283 individuals with clinical depression aged 12 to 20 years and reported pooled effect sizes ranging from 0.43 to 0.58. The extent to which these pooled estimates differed across common moderators is currently unknown.
Whether treating sleep disturbances reduces depression in children and youths is still debated. A recent meta-analysis reported a pooled effect size in the small range based on 4 RCTs of youths with subthreshold mental health problems.30 Similar RCTs of children and in clinical populations are lacking, to our knowledge.
The primary aim of this study was to provide an updated systematic review and meta-analysis of prospective cohort studies that examined the association of disturbed sleep with the development of later depression among 5- to 24-year-old individuals. For a wider scope compared with previous reviews, we opted for broad definitions of disturbed sleep and depression. Based on prior systematic reviews,20,29 we expected to find that the pooled effect sizes were significant and in the small range.
Methods
The Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline31 was followed and fulfilled. This study also adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline.
Search Strategy, Study Selection, and Data Extraction
The search strategy is detailed in eMethods 1 in the Supplement. Title and abstract screening was performed by 2 authors (M.W. and X.J.) until a κ score32 of 0.8 was achieved, with the remainder being selected by 1 reviewer (M.W. or X.J.). Full-text screening was performed independently by 2 authors (M.W. and X.J.). Disagreements were solved by discussion and, if needed, referred to a third, senior-author reviewer (C.M.).
Studies were included if they were prospective, observational studies reporting quantitative estimates of the association between disturbed sleep and depression in participants belonging to either community or clinical-based samples with any comorbid psychiatric, neurologic, or medical diagnosis. Case series, case reports, systematic reviews, meta-analyses, and retrospective, cross-sectional, treatment, theoretical, and position studies were excluded.
Studies were included if participants’ mean age at baseline was between 5 and 24 years. This age range was chosen to cover the whole age range at risk for depression in children and youths and to include the period of peak incidence for depression at 20 years of age.2,33 In our review, we identified the following 3 age categories: childhood, between 5 and 9 years of age; adolescence, between 10 and 19 years of age; and young adulthood, between 20 and 24 years of age.34 Studies were included if both disturbed sleep and depression were measured at a mean age between 5 and 24 years and if the duration between baseline and follow-up was at least 1 month.
Definitions of disturbed sleep and depression are in eMethods 2 in the Supplement. Studies were included if they reported estimates adjusted for depression at baseline and at least 1 common moderating factor, such as age, sex, and socioeconomic status. To avoid duplicate publications, studies that shared samples, sample sizes, 1 or more authors, setting, numbers of participants at baseline and follow-up, date and duration of the study, and exposure and outcome were excluded. Data extraction is described in eMethods 3 in the Supplement.
Risk-of-Bias Assessment
Risk of bias of included studies was appraised using the 13-item version of the Research Triangle Institute Item Bank tool,35,36 which is a development of the 29-item original questionnaire.37 The 13-item Research Triangle Institute Item Bank is a tool for observational studies assessing selection, confounding, performance, attrition, detection, and reporting biases, with high interrater reliability (75%). We dropped 2 items because they were not relevant to the body of literature of the included studies and added 1 question to further refine the attrition bias domain. eTable 1 in the Supplement reports the final included 12 questions. The risk-of-bias appraisal was performed by 2 authors (M.W. and X.J.) independently, with discrepancies being resolved by discussion and, if needed, by a third author (C.M.). Items were scored as high, low, unclear, or not applicable risk of bias. An overall risk-of-bias score was given to each study, based on the ratio between high and valid items (excluding not applicable items) and an arbitrary cutoff of 50%.35 The Covidence systematic review software was used for title and abstract and full-text screening, as well as extraction and quality assessment for included studies.
Data Synthesis and Data Analysis
Data were synthesized by meta-analysis if a minimum of 2 studies were available. Studies were included in the meta-analysis if they reported effect size estimates, measures of precision, and P values. The I2 index was applied to quantify the heterogeneity among different studies, describing the percentage of variability in effect size estimates that is due to heterogeneity.38 I2 ≥ 50% means substantial heterogeneity. A fixed-effect model was used if I2 < 50%. A Dersimonian and Laird random-effects model was used when I2 ≥ 50%, based on the assumption that observed variance is due to heterogeneity among studies in populations and methods, rather than sampling error. Pooled estimates of ORs and β coefficients were obtained by the inverse variance–weighted method to account for the precision of the effect size. Odds ratios were log-transformed prior to meta-analysis to achieve approximate normality.
Pooled estimates were calculated for combined insomnia and sleep disturbances. When multiple follow-ups were available from 1 study, the longest follow-up was used in the meta-analysis; if follow-ups were of equal duration, we arbitrarily opted to use the earliest follow-up.
We fit meta-regressions to explore the heterogeneity associated with type of ascertainment, definition of and assessment tool for disturbed sleep and depression, follow-up duration, disturbed sleep at follow-up, and age at baseline.13 When 3 groups were compared, dummy variables were generated for comparison. A permutation test was implemented to derive P values for each subgroup analysis. Because previous meta-analyses16,29 did not perform metaregressions, no a priori hypotheses were formulated regarding the outcome.
Sensitivity analysis was performed by excluding studies with a high risk-of-bias score and studies with less than 200 participants, arbitrarily chosen as a cutoff to denote small sample sizes. Potential publication bias was assessed by visual inspection of the symmetry of funnel plots, fail-safe numbers,39 and Egger tests.40
Studies not included in the meta-analysis were synthesized based on Synthesis Without Meta-analysis (SWiM) guidelines (eMethods 4 in the Supplement).41 The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to evaluate the quality of evidence of synthesis with and without meta-analysis separately.42 Meta-analysis, metaregression, and a test of heterogeneity were performed using STATA, version 14 (StataCorp). All P values were from 2-tailed tests and results were deemed statistically significant at P < .05.
Results
Search Results
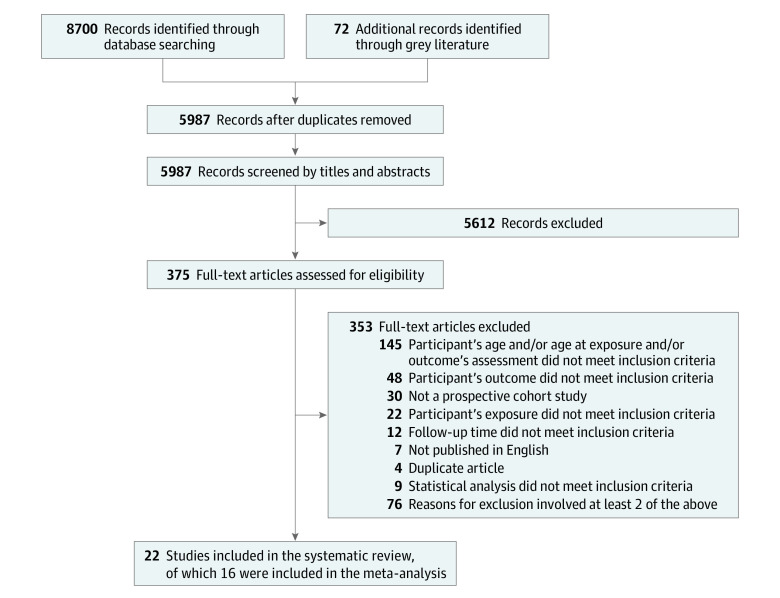
After screening 8700 articles, 375 articles were selected for full-text review, and 22 studies were included.22,25,27,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61 The PRISMA flowchart with studies included and excluded at each step, along with the rationale for the exclusion, is depicted in Figure 1.
Figure 1. PRISMA Flow Diagram of Included Studies.
Studies Characteristics
The Table22,25,27,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 shows the characteristics of the included studies. eTable 2 and eResults in the Supplement show a summary of the included studies.
Table. Characteristics of Included Studies.
| Source | Sample | Follow-up | Sample size, No. | Age at baseline, mean (SD), y | Male sex, % | Factors associated with outcomes | Outcome | Confounders | |
|---|---|---|---|---|---|---|---|---|---|
| No. | Duration, mo | ||||||||
| Dichotomous outcome | |||||||||
| Fan et al,48 2017 (China) | School-based cohort | 1 | 12 | 1237 | 15 (1.3) | 45.8 | Sleep disturbance; PSQI62; self-report; sleep duration; broadly defined sleep problems; categorical | DSRS-C63; self-report; depression; categorical | Sex, age, residence location, only child, father’s educational level, earthquake exposure, and disturbed sleep at follow-up |
| Haraden et al,60 2017 (US) | School-based cohort | 1 | 12 | 360 | 15.0 (2.3) [range, 11-19] | 43.5 | Sleep disturbances; MESC64; self-report; chronotype; continuous | KSADS-PL65; interview; depression; categorical | Pubertal status |
| Kouros et al,49 2016 (US) | School-based cohort; stratified on maternal depression | 1 | 72 | 240 | 11.9 (0.6) | 46 | Sleep disturbances; CDRS-R66; interview; broadly defined sleep problems; categorical | LIFE67; interview; depression; categorical and continuous | Maternal depression, baseline sad mood, irritability, anhedonia, and sex |
| Luo et al,51 2018 (China) | School-based cohort | 1 | 24 | 246 | 17.7 (0.6) | 49 | Sleep disturbances; ESS68; self-report; daytime sleepiness; categorical | BDI69; self-report; depression; categorical | Age, sex, and disturbed sleep at follow-up |
| Luo et al,52 2013 (China) | School-based cohort | 1 | 12 | 2787 | 15.0 (1.5) | 48.9 | Insomnia; ISI70; self-report; continuous | BDI69; self-report; depression; categorical | Age, sex, and disturbed sleep at follow-up |
| Roane et al,59 2008 (US) | School-based cohort | 1 | 72 | 3582 | 15.8 (1.5) | 47.6 | Insomnia; single-item questionnaire: “How often did you have trouble falling asleep or staying asleep in the past 12 months?”; self-report; categorical | Single-item questionnaire: “Have you been previously diagnosed with depression?”; self-report; depression; categorical | Sex and existing mental disorder |
| Roberts et al,53 2013 (US) | Community-based cohort | 1 | 12 | 3134 | Range, 11-17 | 51.1 | Insomnia; 5-item questionnaire: “In the past 4 weeks, have you had (1) trouble falling asleep, (2) waking up in the middle of the night and finding it hard to go back to sleep, (3) waking up frequently but able to go back to sleep, (4) waking up very early, and (5) having nonrestorative sleep?”; self-report; categorical | DISC-IV71; interview; depression; categorical | Age, sex, and family income |
| Shanahan et al,57 2014 (US) | Community-based cohort | NA | NA | 1420 | Range, 9-13 | 12 | Sleep disturbance; CAPA72; interview; broadly defined sleep; continuous | CAPA72; interview; depression; categorical | Sex, race, age, pubertal status, and disturbed sleep at follow-up |
| Buysse et al,44 2008 (Switzerland) | Community-based cohort; stratified on high risk for psychiatric syndromes | 1 | 24 | 591 | Male mean, 19; and female mean, 20 | 49.4 | Insomnia; SPIKE73; interview; categorical | SPIKE73; interview; depression; categorical | Disturbed sleep at follow-up |
| Johnson et al,46 2000 (US) | Community-based cohort; stratified on low birth weight and low SES | 1 | 60 | 686 | 6 | 48.3 | Sleep disturbance; single-item questionnaire: “Trouble sleeping during the past 6 mo”; self-report; broadly defined sleep problems | CBCL, TRF74; self-report; depression with anxiety; categorical | Mother’s history of depression, low birth weight, site (suburban vs urban), and sex |
| Continuous outcome | |||||||||
| Becker et al,43 2015 (US) | Clinical-based cohort, ADHD | 1 | 12 | 81 | 12.2 (1.0) [range, 10-14] | 75 | Sleep disturbance; CBCL sleep items74; self-report; broadly defined sleep problems; continuous | RADS-275; self-report; depression; continuous | Age, sex, race, comorbid ODD, CD, anxiety disorder, and ADHD |
| Doane et al,22 2015 (US) | School-based cohort | 3 | 5, 4, 9 | 82 | 18.1 (0.41) | 24 | Sleep disturbance; Actiwatch (Phillips Respironics Inc); objective; sleep onset latency, sleep duration; PSQI62; self-report; broadly defined sleep problems; continuous | CES-D76; self-report; depression; continuous | Sex, race/ethnicity, parental educational level, living at home, and disturbed sleep at follow-up |
| Gregory et al,45 2009 (UK) | Clinical-based, twin cohort | 1 | 24 | 250 | 8 | 43 | Sleep disturbance; CSHQ77; self-report; broadly defined sleep problems; continuous | CDI78; self-report; depression; continuous | Age, sex, and disturbed sleep at follow-up |
| Chang et al,47 2017 (China) | School-based cohort | 1 | 12 | 1893 | Male, 14.7 (0.5); and female, 14.7 (0.5) | 51.2 | Sleep disturbance; PSQI62; self-report; broadly defined sleep problems; continuous | CES-D76; self-report; depression; continuous | Sex, age, family structure, family economic stress, stressful life events, pubertal development, prior peer victimization, and prior sleep problems |
| El-Sheikh et al,61 2010 (US) | School-based cohort | 1 | 24 | 176 | 8.7 (0.4) | 44 | Sleep disturbance; CSHQ77; parent-report; SHS79; self-report; broadly defined sleep problems; daytime sleepiness; continuous; Actigraph (Ambulatory Monitoring Inc); sleep duration; objective; continuous | PIC80; parent-report; CDI78; self-report; depression with anxiety; continuous | Sex, SES, and ethnicity |
| Alvaro et al,27 2017 (Australia) | School-based cohort | 1 | 6 | 255 | 15.0 (1.3) | NA | Insomnia; ISI70; self-report; continuous | RCADS81; self-report; depression; continuous | Age, sex, and chronotype |
| Ksinan Jiskrova et al,50 2019 (Czech Republic) | General population, birth cohort | 2 | 48, 36 | 3485 | 7 | 51.2 | Sleep disturbances; 7-item questionnaire82; parent-report; sleep duration; chronotype; broadly defined sleep problems; continuous | SDQ83; parent-report; depression with anxiety; continuous | Sex, family structure, SES, maternal internalizing problems, and disturbed sleep at follow-up |
| Schneiderman et al,54 2018 (US) | Case-control sample, maltreatment vs no maltreatment | 1 | 54 | Case, 247; control, 138 | 13.7 (1.4) | 48.3 | Sleep disturbance; PSQI62; self-report; broadly defined sleep problems; sleep duration; continuous | CDI78; self-report; depression; continuous | Age, sex, and disturbed sleep at follow-up |
| Wong et al,55 2012 (US) | Community-based cohort | 2 | 12, 12 | 6504 | 16.0 (1.8) | NA | Sleep disturbance; single-item questionnaire: “Please tell me how often you have had each of the following conditions in the past 12 months? – trouble falling asleep or staying asleep”; self-report; broadly defined sleep problems; continuous | CES-D76; self-report; depression; continuous | Age, sex, race, school grade, parental poverty, chronic health problems (allergies, asthma, migraines, diabetes, or obesity), alcohol and drug use disorders, and disturbed sleep at follow-up |
| Urrila et al,56 2014 (Finland) | Clinical-based cohort, depression | 1 | 13 | 142 | 16.5 (1.6) [range, 13-19] | 17.5 | Insomnia; KSADS-PL65; interview; continuous | BDI69; self-report; depression; continuous | Age, sex, within-individual correlation, and disturbed sleep at follow-up |
| Mulraney et al,25 2016 (Australia) | Case-control sample, ADHD vs control | 3 | 6, 6, 12 | 270 | 10.1 (1.9) | 85.9 | Sleep disturbance; CSHQ77; self-report; broadly defined sleep problems; continuous | SDQ83; parent-report; depression; continuous | Age, sex, ADHD symptom severity, primary caregiver educational level, and disturbed sleep at follow-up |
| Reynolds et al,58 2016 (US) | Community-based cohort | 1 | 72 | 1089 | 9 | 51.7 | Sleep disturbance; CSHQ77; parent-report; broadly defined sleep problems; wake after sleep onset; continuous | YSR74; self-report; depression with anxiety; continuous | Total family income, marital status, and sex |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BDI, Beck Depression Inventory; CAPA, Child and Adolescent Psychiatric Assessment; CBCL, Child Behavior Checklist; CD, conduct disorder; CDI, Children’s Depression Inventory; CDRS-R, Children’s Depression Rating Scale–Revised; CES-D, Center for Epidemiological Studies Depression Scale; CSHQ, Children’s Sleep Habits Questionnaire; DISC-IV, Diagnostic Interview Schedule for Children Version IV; DSRS-C, Depression Self-Rating Scale for Children; ESS, Epworth Sleepiness Scale; ISI, Insomnia Severity Index; KSADS-PL, Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version; LIFE, Longitudinal Interval Follow-up Evaluation; MESC, Morningness–Eveningness Scale for Children; NA, not available; ODD, oppositional defiant disorder; PIC, Personality Inventory for Children; PSQI, Pittsburgh Sleep Quality Index; RADS-2, Reynolds Adolescent Depression Scale–second edition; RCADS, Revised Child Anxiety and Depression Scale; SDQ, Strengths and Difficulties Questionnaire; SES, socioeconomic status; SHS, Sleep Habits Survey; SPIKE, Structured Psychopathological Interview and Rating of the Social Consequences of Psychological Disturbances for Epidemiology; TRF, Teacher Report Form; YSR, Youth Self-Report.
Risk-of-Bias Assessment
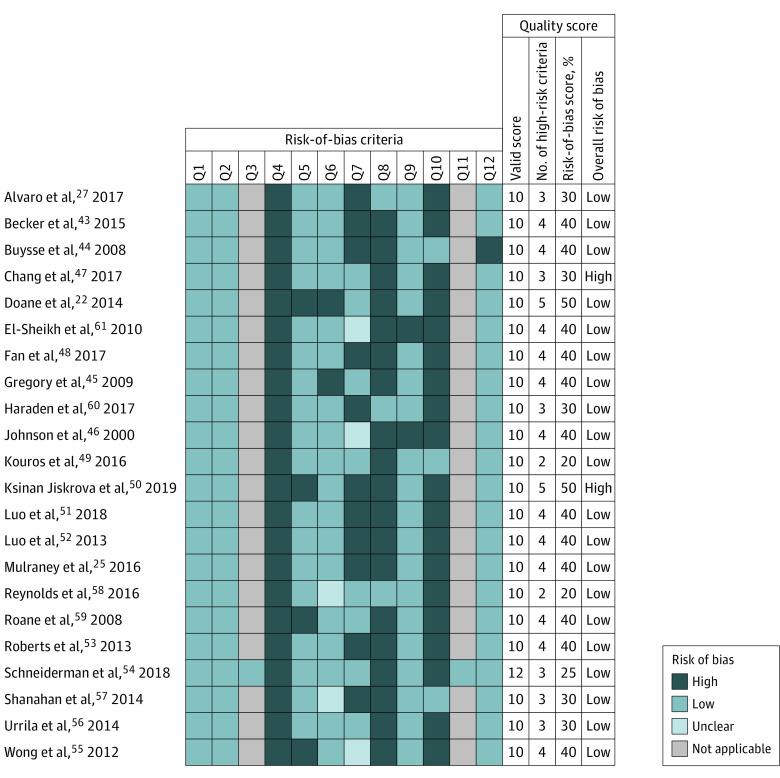
Figure 222,25,27,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61 reports the results of the risk-of-bias assessment by a heat map. The mean overall risk of bias was 36.1% (7.95 of 22), where lower scores indicated lower risk of bias. The mean number of high risk-of-bias responses was 3.64. Two studies22,50 were rated as having a high overall risk of bias (ie, overall risk-of-bias scoring ≥50%, which corresponded to 5 high risk-of-bias responses).35,37
Figure 2. Risk-of-Bias Assessment of the Included Studies Based on the Research Triangle Institute Item Bank, by Heat Map.
The overall risk-of-bias score was based on the ratio between the number of high and valid items (excluding not applicable items) times 100; scores of 50 or more identified high risk of bias.
Synthesis With Meta-analysis
Sixteen studies presented sufficient data to allow synthesis via meta-analysis.25,27,43,45,47,48,49,50,51,52,53,55,57,58,59,60 Subgroup meta-analysis based on sex was precluded owing to insufficient data.
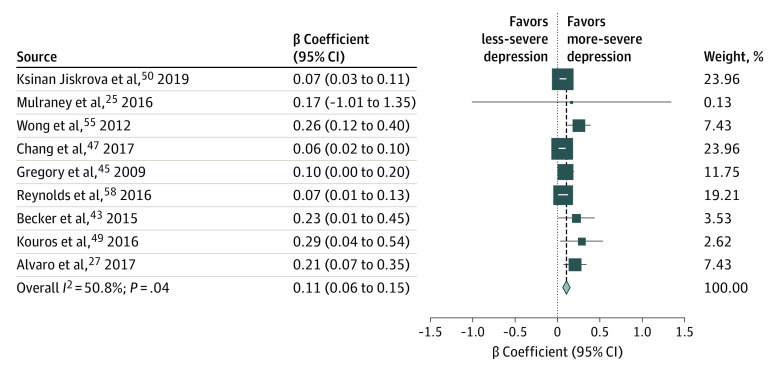
Pooled Estimates of β Coefficients
Complete data on β coefficients were available from 1 study on insomnia and depression27 and from 8 studies on sleep disturbances and depression25,43,45,47,49,50,55,58 (eTable 3 in the Supplement). The pooled β coefficient of the association between disturbed sleep and depression was 0.11 (95% CI, 0.06-0.15; P < .001; n = 14 067; I2 = 50.8%; P = .04) (Figure 3). Metaregressions showed no evidence that the pooled estimate differed significantly across any covariate (eTable 4 in the Supplement). In sensitivity analysis that excluded studies with a high risk-of-bias score and studies of less than 200 participants, the pooled estimate remained of comparable magnitude (0.08; 95% CI, 0.05-0.11; P < .001; I2 = 34.9%; P = .16) and heterogeneity (0.10; 95% CI, 0.06-0.14; P < .001; I2 = 51.3%; P = .045).
Figure 3. Forest Plot for Standardized β Coefficient.
Weights are from random-effects analysis.
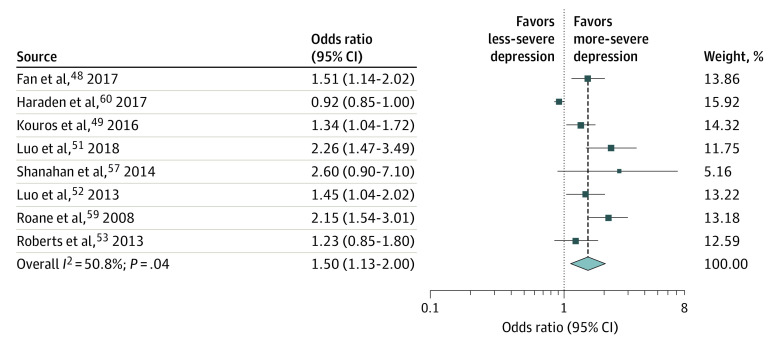
Pooled Estimates of ORs
Complete data on ORs were available from 3 studies on insomnia and depression52,53,59 and from 5 studies on sleep disturbances and depression48,49,51,57,60 (eTable 5 in the Supplement). In 3 studies,48,51,52 depression was based on cutoff scores applied to self-reported questionnaires (ie, 20 in the Beck Depression Inventory69 and 15 in the Depression Self-Rating Scale for Children63). Both cutoffs had been validated to identify depression with acceptable psychometric scores.84,85 The pooled OR estimate of depression in those with vs without disturbed sleep was 1.50 (95% CI, 1.13-2.00; P = .005; n = 13 006; I2 = 87.7%; P < .001) (Figure 4). Metaregressions showed no evidence that the pooled estimate differed significantly across any covariate (eTable 6 in the Supplement). All studies had low risk-of-bias scores and more than 200 participants; therefore, sensitivity analyses were not performed.
Figure 4. Forest Plot for Odds Ratio.
Publication Bias
Visual inspection of the funnel plots identified substantial asymmetry for both pooled estimates (eFigures 1 and 2 in the Supplement). The Egger test identified substantial publication biases. We performed a leave-one-out sensitivity analysis by iteratively removing 1 study at a time and recalculating the pooled OR and β. Point estimates were within the 95% CI of the complete analysis (eFigures 3 and 4 in the Supplement). For both pooled estimates, the fail-safe number was larger than the number of studies (ie, 170 for the β coefficient and 92 for the OR coefficient).
Quality of Evidence
According to GRADE,42 the overall body of evidence was rated as very low (eTable 8 in the Supplement), which means that the confidence in the effect size estimates is very limited.
Synthesis of Studies Without Meta-analysis
For 6 studies,22,44,46,54,56,61 inclusion in the meta-analysis was precluded owing to effect size estimates being incomplete (eTable 7 in the Supplement). For the dichotomous outcome, disturbed sleep was significantly associated with an increase of depression in 1 study44 and not significantly associated in another.46 For the continuous outcome, disturbed sleep was significantly associated with an increase of depression in 1 study56 and was significantly associated with an increase of depression for the female subgroup only in an another study.54 Finally, 3 studies reported that findings were nonsignificant, although the direction of the findings was not clear.22,54,61 According to GRADE,42 the overall body of evidence was rated very low, which means that confidence in the effect size estimates is very limited (eTable 9 in the Supplement). Based on studies that provided direction of associations, the overall pattern supported an association between disturbed sleep and increased depression.
Discussion
The present study provides summarized quantitative evidence of the prospective association between disturbed sleep and depression in children and youths after controlling for baseline depression. In line with our expectation, we found that the residual association after controlling for baseline depression was significant and of small magnitude. In fact, it is known that depression results from the joint action of a wide range of risk factors of small effect,86 and disturbed sleep is increasingly supported as one of these risk factors. Different mechanisms have been proposed to explain the association between disturbed sleep and depression, including an activation of inflammatory pathways, altered neuroplasticity and learning, and a disruption of circadian rhythm.87 Prevention of depression should target multicomponent risk profiles, possibly including sleep, and synthesis data are needed for the selection of the modifiable risk factors to target and the prioritization and timing of the prevention plan.7
Compared with previous meta-analyses on the association between disturbed sleep and depression in children and youths,20,29 our study is substantiated by a larger number of studies and broader inclusion criteria, which makes the results from this systematic review updated, more robust, and comprehensive. Furthermore, given that we included only studies controlling for baseline depression, pooled estimates depict the association between baseline disturbed sleep and residual depression at follow-up.
The pooled β coefficient of the association between disturbed sleep and depression was 0.11 (95% CI, 0.06-0.15) and was based on 9 studies representing 14 067 participants between 5 and 19 years of age.25,27,43,45,47,49,50,55,58 Metaregressions showed no evidence that the pooled estimate differed across any covariate, supporting the applicability of the pooled estimate to a broad spectrum of settings.
Metaregression shows that the pooled β coefficient did not differ by age at baseline, which is in line with previous literature,20,29 and showed that children with disturbed sleep are equally as vulnerable to later depression as youths. This finding is of particular relevance because it informs the timing of prevention strategies. Sleep problems are often underdiagnosed in childhood88 and are rarely treated,89 which may generate a large cohort of individuals vulnerable to depression.
The meta-analytic OR of the association between disturbed sleep and depression was 1.50 (95% CI, 1.13-2.00), in line with the pooled OR by Baglioni et al29 of 2.0 (95% CI, 1.5-2.7). The meta-analytic OR in our study was based on 8 studies representing 15 438 participants between 10 and 19 years of age.48,49,51,52,53,57,59,60 Despite heterogeneity, pooled studies were homogeneous along most characteristics (ie, age at baseline [10-19 years], type of ascertainment [community-based samples], depression without anxiety, sample size [>200], and risk-of-bias score [low]). Furthermore, metaregressions showed no evidence that the pooled estimate differed across any covariate, indicating that heterogeneity, although present, remains largely unexplained and may be clinically unimportant. Metaregression showed that the pooled OR did not differ according to the tool used for the assessment of disturbed sleep (single-item questionnaire vs multi-item questionnaire vs interview), supporting single-item questionnaires as valuable alternatives to more costly and time-consuming tools.
Strategies to prevent depression could start as early as childhood and possibly include treating disturbed sleep. Even though disturbed sleep can be effectively treated,90,91,92,93,94 only 2 RCTs targeting improvement of sleep to prevent depression have been completed, and they included participants older than 12 years,95,96 suggesting that more RCTs are needed, especially for children.
Limitations
The present meta-analysis has several limitations. First, broad definitions of disturbed sleep and depression may have been associated with the variance of estimates across studies and did not allow us to test whether subtypes of disturbed sleep and depression had different association patterns. Second, there was a possible publication bias in the results. However, the leave-one-out test indicated that results were not associated with any single study, and the fail-safe numbers indicated that findings were robust against publication bias. Third, we included only English-language literature. Fourth, we included studies that did and did not control for disturbed sleep at follow-up; therefore, we were not able to assess that the association under study was significant over and above within-time covariation with depression. However, metaregressions were not significant, suggesting that heterogeneity could not be associated with disturbed sleep at follow-up. Fifth, the pooled estimate of β coefficients in children was based on 3 studies, suggesting caution is warranted in the interpretation of this result. Sixth, our review was not limited to studies assessing both disturbed sleep and depression repeatedly at each time point and, therefore, could not clarify temporal precedence, directionality, or reciprocity of associations. Seventh, the pooled estimate of β coefficients included 3 clinical-based studies, which could have been associated with the effect size owing to a more restricted range of variability of measures compared with community-based studies. However, metaregressions showed no significant differences. Eighth, common to all meta-analyses, the pooled ORs were dependent on the scale of the disturbed sleep measures of each study. Ninth, we were not able to assess the associations separately by sex owing to insufficient data; therefore, we could not exclude the possibility that sex was a confounding variable.
Conclusions
This systematic review and meta-analysis found that disturbed sleep was prospectively associated with depression and provides quantitative estimates of the pooled effect sizes among children and youths. Although the pooled effect sizes are small, the high prevalence of children and youths with disturbed sleep implies the existence of a large cohort of vulnerable individuals who could develop depression. Disturbed sleep could be one of the many risk factors to address in depression prevention programs. Randomized clinical trials targeting disturbed sleep as early as childhood are needed to inform the planning and evaluation of depression prevention programs. These findings must be considered in the context of the limitations and the overall very low quality of evidence of the included studies.
eMethods 1. Search Strategy
eMethods 2. Study Selection
eMethods 3. Data Extraction
eMethods 4. Synthesis of Studies Without Meta-Analysis
eResults.
eTable 1. Included Questions for Risk of Bias Assessment From the Research Triangle Institute Item Bank (RTI-IB) Tool
eTable 2. Summary of Included Studies (n=22)
eTable 3. Included Studies with Beta Coefficients
eTable 4. Meta-Regression Analysis of Pooled Beta Coefficients for the Association Between Disturbed Sleep and Depression
eTable 5. Included Studies With Odds Ratio Values
eTable 6. Meta-Regression Analysis of Pooled ORs for the Association Between Disturbed Sleep and Depression
eTable 7. Synthesis of Studies Without Meta-Analysis by Applying a Simple Vote-Counting by Direction of Effects
eTable 8. Grading of Recommendations Assessment, Development and Evaluation (GRADE) for the Studies Included in the Synthesis With Meta-Analysis
eTable 9. Grading of Recommendations Assessment, Development and Evaluation (GRADE) for the Studies Included in the Synthesis Without Meta-Analysis
eFigure 1. Funnel Plot for Standardized Beta
eFigure 2. Funnel Plot for Odds Ratio
eFigure 3. Leave-One-Out Forest Plot for Standardized Beta
eFigure 4. Leave-One-Out Forest Plot for Odds Ratio
eReferences.
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37-44. doi: 10.1016/j.jaac.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klein DN, Glenn CR, Kosty DB, Seeley JR, Rohde P, Lewinsohn PM. Predictors of first lifetime onset of major depressive disorder in young adulthood. J Abnorm Psychol. 2013;122(1):1-6. doi: 10.1037/a0029567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. 2016;388(10047):881-890. doi: 10.1016/S0140-6736(16)30385-3 [DOI] [PubMed] [Google Scholar]
- 5.Eckshtain D, Kuppens S, Ugueto A, et al. Meta-analysis: 13-year follow-up of psychotherapy effects on youth depression. J Am Acad Child Adolesc Psychiatry. 2020;59(1):45-63. doi: 10.1016/j.jaac.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 6.Weisz JR, Kuppens S, Ng MY, et al. Are psychotherapies for young people growing stronger? tracking trends over time for youth anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems. Perspect Psychol Sci. 2019;14(2):216-237. doi: 10.1177/1745691618805436 [DOI] [PubMed] [Google Scholar]
- 7.Hoare E, Callaly E, Berk M. Can depression be prevented? if so, how? JAMA Psychiatry. 2020. doi: 10.1001/jamapsychiatry.2020.1273 [DOI] [PubMed] [Google Scholar]
- 8.Stockings EA, Degenhardt L, Dobbins T, et al. Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychol Med. 2016;46(1):11-26. doi: 10.1017/S0033291715001725 [DOI] [PubMed] [Google Scholar]
- 9.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147-1156. doi: 10.1176/appi.ajp.160.6.1147 [DOI] [PubMed] [Google Scholar]
- 10.Pigeon WR, Bishop TM, Krueger KM. Insomnia as a precipitating factor in new onset mental illness: a systematic review of recent findings. Curr Psychiatry Rep. 2017;19(8):44. doi: 10.1007/s11920-017-0802-x [DOI] [PubMed] [Google Scholar]
- 11.Bao YP, Han Y, Ma J, et al. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: meta-analysis and systematic review. Neurosci Biobehav Rev. 2017;75:257-273. doi: 10.1016/j.neubiorev.2017.01.032 [DOI] [PubMed] [Google Scholar]
- 12.Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96-105. doi: 10.1016/j.smrv.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 13.Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16(1):375. doi: 10.1186/s12888-016-1075-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakar A, Yao PC, Ningrum V, Liu CT, Lee SC. Beneficial biological activities of Cinnamomum osmophloeum and its potential use in the alleviation of oral mucositis: a systematic review. Biomedicines. 2020;8(1):E3. doi: 10.3390/biomedicines8010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ye YY, Zhang YF, Chen J, et al. Internet-based cognitive behavioral therapy for insomnia (ICBT-i) improves comorbid anxiety and depression—a meta-analysis of randomized controlled trials. PLoS One. 2015;10(11):e0142258. doi: 10.1371/journal.pone.0142258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lovato N, Short MA, Micic G, Hiller RM, Gradisar M. An investigation of the longitudinal relationship between sleep and depressed mood in developing teens. Nat Sci Sleep. 2017;9:3-10. doi: 10.2147/NSS.S111521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41(8):964-971. doi: 10.1097/00004583-200208000-00015 [DOI] [PubMed] [Google Scholar]
- 18.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16(2):129-136. doi: 10.1016/j.smrv.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 19.Barclay NL, Gehrman PR, Gregory AM, Eaves LJ, Silberg JL. The heritability of insomnia progression during childhood/adolescence: results from a longitudinal twin study. Sleep. 2015;38(1):109-118. doi: 10.5665/sleep.4334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18(6):521-529. doi: 10.1016/j.smrv.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 21.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059-1068. doi: 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolesc. 2015;44(2):389-404. doi: 10.1007/s10964-014-0150-7 [DOI] [PubMed] [Google Scholar]
- 23.Hayley AC, Skogen JC, Sivertsen B, et al. Symptoms of depression and difficulty initiating sleep from early adolescence to early adulthood: a longitudinal study. Sleep. 2015;38(10):1599-1606. doi: 10.5665/sleep.5056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol. 2014;50(4):1137-1147. doi: 10.1037/a0034501 [DOI] [PubMed] [Google Scholar]
- 25.Mulraney M, Giallo R, Lycett K, Mensah F, Sciberras E. The bidirectional relationship between sleep problems and internalizing and externalizing problems in children with ADHD: a prospective cohort study. Sleep Med. 2016;17:45-51. doi: 10.1016/j.sleep.2015.09.019 [DOI] [PubMed] [Google Scholar]
- 26.Quach JL, Nguyen CD, Williams KE, Sciberras E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 2018;172(2):e174363. doi: 10.1001/jamapediatrics.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alvaro PK, Roberts RM, Harris JK, Bruni O. The direction of the relationship between symptoms of insomnia and psychiatric disorders in adolescents. J Affect Disord. 2017;207:167-174. doi: 10.1016/j.jad.2016.08.032 [DOI] [PubMed] [Google Scholar]
- 28.Ritter PS, Höfler M, Wittchen HU, et al. Disturbed sleep as risk factor for the subsequent onset of bipolar disorder—data from a 10-year prospective-longitudinal study among adolescents and young adults. J Psychiatr Res. 2015;68:76-82. doi: 10.1016/j.jpsychires.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 29.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1-3):10-19. doi: 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 30.Gee B, Orchard F, Clarke E, Joy A, Clarke T, Reynolds S. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2019;43:118-128. doi: 10.1016/j.smrv.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 31.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 32.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 33.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in US Children. J Pediatr. 2019;206:256-267.e3. doi: 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bundy DAP, de Silva N, Horton S, et al. ; Disease Control Priorities-3 Child and Adolescent Health and Development Authors Group. Investment in child and adolescent health and development: key messages from Disease Control Priorities, 3rd Edition. Lancet. 2018;391(10121):687-699. doi: 10.1016/S0140-6736(17)32417-0 [DOI] [PubMed] [Google Scholar]
- 35.Viswanathan M, Patnode CD, Berkman ND, et al. Recommendations for assessing the risk of bias in systematic reviews of health-care interventions. J Clin Epidemiol. 2018;97:26-34. doi: 10.1016/j.jclinepi.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 36.Viswanathan M, Berkman ND, Dryden DM, Hartling L. Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank. AHRQ publication 13-EHC106-EF. Agency for Healthcare Research and Quality; 2013. [PubMed]
- 37.Viswanathan M, Berkman ND. Development of the RTI Item Bank on risk of bias and precision of observational studies. J Clin Epidemiol. 2012;65(2):163-178. doi: 10.1016/j.jclinepi.2011.05.008 [DOI] [PubMed] [Google Scholar]
- 38.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 39.Rosenthal R. The file drawer problem and tolerance for null results. Psychological Bull. 1979;86(3):638-641. doi: 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- 40.Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ. 1997;315(7121):1533-1537. doi: 10.1136/bmj.315.7121.1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guyatt GH, Oxman AD, Vist GE, et al. ; GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. doi: 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Becker SP, Langberg JM, Evans SW. Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2015;24(8):897-907. doi: 10.1007/s00787-014-0636-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473-480. doi: 10.1093/sleep/31.4.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gregory AM, Rijsdijk FV, Lau JY, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32(2):189-199. doi: 10.1093/sleep/32.2.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Res. 2000;94(2):93-102. doi: 10.1016/S0165-1781(00)00145-1 [DOI] [PubMed] [Google Scholar]
- 47.Chang LY, Chang HY, Wu WC, Lin LN, Wu CC, Yen LL. Body mass index and depressive symptoms in adolescents in Taiwan: testing mediation effects of peer victimization and sleep problems. Int J Obes (Lond). 2017;41(10):1510-1517. doi: 10.1038/ijo.2017.111 [DOI] [PubMed] [Google Scholar]
- 48.Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry. 2017;78(7):882-888. doi: 10.4088/JCP.15m10206 [DOI] [PubMed] [Google Scholar]
- 49.Kouros CD, Morris MC, Garber J. Within-person changes in individual symptoms of depression predict subsequent depressive episodes in adolescents: a prospective study. J Abnorm Child Psychol. 2016;44(3):483-494. doi: 10.1007/s10802-015-0046-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ksinan Jiskrova G, Vazsonyi AT, Klánová J, Dušek L. Sleep quantity and problems as mediators of the eveningness-adjustment link during childhood and adolescence. J Youth Adolesc. 2019;48(3):620-634. doi: 10.1007/s10964-018-0965-8 [DOI] [PubMed] [Google Scholar]
- 51.Luo C, Zhang J, Chen W, Lu W, Pan J. Course, risk factors, and mental health outcomes of excessive daytime sleepiness in rural Chinese adolescents: a one-year prospective study. J Affect Disord. 2018;231:15-20. doi: 10.1016/j.jad.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 52.Luo C, Zhang J, Pan J. One-year course and effects of insomnia in rural Chinese adolescents. Sleep. 2013;36(3):377-384. doi: 10.5665/sleep.2454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord. 2013;148(1):66-71. doi: 10.1016/j.jad.2012.11.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schneiderman JU, Ji J, Susman EJ, Negriff S. Longitudinal relationship between mental health symptoms and sleep disturbances and duration in maltreated and comparison adolescents. J Adolesc Health. 2018;63(1):74-80. doi: 10.1016/j.jadohealth.2018.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46(7):953-959. doi: 10.1016/j.jpsychires.2012.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Urrila AS, Karlsson L, Kiviruusu O, et al. ; Adolescent Depression Study group . Sleep complaints in adolescent depression: one year naturalistic follow-up study. BMC Psychiatry. 2014;14:283. doi: 10.1186/s12888-014-0283-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(5):550-558. doi: 10.1016/j.jaac.2013.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reynolds KC, Alfano CA. Childhood bedtime problems predict adolescent internalizing symptoms through emotional reactivity. J Pediatr Psychol. 2016;41(9):971-982. doi: 10.1093/jpepsy/jsw014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351-1356. [PMC free article] [PubMed] [Google Scholar]
- 60.Haraden DA, Mullin BC, Hankin BL. The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence. Depress Anxiety. 2017;34(10):967-976. doi: 10.1002/da.22682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.El-Sheikh M, Kelly RJ, Buckhalt JA, Benjamin Hinnant J. Children’s sleep and adjustment over time: the role of socioeconomic context. Child Dev. 2010;81(3):870-883. doi: 10.1111/j.1467-8624.2010.01439.x [DOI] [PubMed] [Google Scholar]
- 62.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 63.Birleson P, Hudson I, Buchanan DG, Wolff S. Clinical evaluation of a self-rating scale for depressive disorder in childhood (Depression Self-Rating Scale). J Child Psychol Psychiatry. 1987;28(1):43-60. doi: 10.1111/j.1469-7610.1987.tb00651.x [DOI] [PubMed] [Google Scholar]
- 64.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16(3):258-262. doi: 10.1093/sleep/16.3.258 [DOI] [PubMed] [Google Scholar]
- 65.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980-988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 66.Poznanski EO, Cook SC, Carroll BJ. A depression rating scale for children. Pediatrics. 1979;64(4):442-450. [PubMed] [Google Scholar]
- 67.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540-548. doi: 10.1001/archpsyc.1987.01800180050009 [DOI] [PubMed] [Google Scholar]
- 68.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545. doi: 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 69.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561-571. doi: 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- 70.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307. doi: 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 71.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28-38. doi: 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- 72.Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M. The Child and Adolescent Psychiatric Assessment (CAPA). Psychol Med. 1995;25(4):739-753. doi: 10.1017/S003329170003498X [DOI] [PubMed] [Google Scholar]
- 73.Binder J, Angst J. Social consequences of psychic disturbances in the population: a field study on young adults. Arch Psychiatr Nervenkr (1970). 1981;229(4):355-370. [DOI] [PubMed] [Google Scholar]
- 74.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 75.Osman A, Gutierrez PM, Bagge CL, Fang Q, Emmerich A. Reynolds Adolescent Depression Scale–second edition: a reliable and useful instrument. J Clin Psychol. 2010;66(12):1324-1345. doi: 10.1002/jclp.20727 [DOI] [PubMed] [Google Scholar]
- 76.Faulstich ME, Carey MP, Ruggiero L, Enyart P, Gresham F. Assessment of depression in childhood and adolescence: an evaluation of the Center for Epidemiological Studies Depression Scale for Children (CES-DC). Am J Psychiatry. 1986;143(8):1024-1027. doi: 10.1176/ajp.143.8.1024 [DOI] [PubMed] [Google Scholar]
- 77.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043-1051. doi: 10.1093/sleep/23.8.1d [DOI] [PubMed] [Google Scholar]
- 78.Kovacs M. The Children’s Depression Inventory: CDI Manual. Multi-Health Systems Inc; 2001. [Google Scholar]
- 79.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213-216. doi: 10.1093/sleep/26.2.213 [DOI] [PubMed] [Google Scholar]
- 80.Lachar D, Butkus M, Hryhorczuk L. Objective personality assessment of children: an exploratory study of the Personality Inventory for Children (PIC) in a child psychiatric setting. J Pers Assess. 1978;42(5):529-537. doi: 10.1207/s15327752jpa4205_15 [DOI] [PubMed] [Google Scholar]
- 81.Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther. 2000;38(8):835-855. doi: 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- 82.Humphreys JS, Gringras P, Blair PS, et al. Sleep patterns in children with autistic spectrum disorders: a prospective cohort study. Arch Dis Child. 2014;99(2):114-118. doi: 10.1136/archdischild-2013-304083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38(5):581-586. doi: 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- 84.Su L, Wang K, Zhu Y, et al. Norm of the Depression Self-rating Scale for Children in Chinese urban children. Article in Chinese. Zhongguo Xin Li Wei Sheng Za Zhi. 2003;17(8):547-549. doi: 10.3321/j.issn:1000-6729.2003.08.011 [DOI] [Google Scholar]
- 85.Wang XD, Wang XL, Ma H. Rating Scales for Mental Health. Mental Health Journal Press; 1999. [Google Scholar]
- 86.Köhler CA, Evangelou E, Stubbs B, et al. Mapping risk factors for depression across the lifespan: an umbrella review of evidence from meta-analyses and Mendelian randomization studies. J Psychiatr Res. 2018;103:189-207. doi: 10.1016/j.jpsychires.2018.05.020 [DOI] [PubMed] [Google Scholar]
- 87.Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020;45(1):74-89. doi: 10.1038/s41386-019-0411-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Meltzer LJ, Johnson C, Crosette J, Ramos M, Mindell JA. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics. 2010;125(6):e1410-e1418. doi: 10.1542/peds.2009-2725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Meltzer LJ, Plaufcan MR, Thomas JH, Mindell JA. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. J Clin Sleep Med. 2014;10(4):421-426. doi: 10.5664/jcsm.3620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zisapel N. Paediatric use of melatonin: letter to the Editor regarding the manuscript “Current role of melatonin in pediatric neurology: clinical recommendations” by Bruni et al. Eur J Paediatr Neurol. 2015 Mar;19(2):122-33. Eur J Paediatr Neurol. 2017;21(2):418-419. doi: 10.1016/j.ejpn.2016.07.013 [DOI] [PubMed] [Google Scholar]
- 91.Bruni O, Alonso-Alconada D, Besag F, et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol. 2015;19(2):122-133. doi: 10.1016/j.ejpn.2014.12.007 [DOI] [PubMed] [Google Scholar]
- 92.Ma ZR, Shi LJ, Deng MH. Efficacy of cognitive behavioral therapy in children and adolescents with insomnia: a systematic review and meta-analysis. Braz J Med Biol Res. 2018;51(6):e7070. doi: 10.1590/1414-431x20187070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kalak N, Gerber M, Kirov R, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health. 2012;51(6):615-622. doi: 10.1016/j.jadohealth.2012.02.020 [DOI] [PubMed] [Google Scholar]
- 94.van Maanen A, Meijer AM, Smits MG, van der Heijden KB, Oort FJ. Effects of melatonin and bright light treatment in childhood chronic sleep onset insomnia with late melatonin onset: a randomized controlled study. Sleep. 2017;40(2). doi: 10.1093/sleep/zsw038 [DOI] [PubMed] [Google Scholar]
- 95.de Bruin EJ, Bögels SM, Oort FJ, Meijer AM. Improvements of adolescent psychopathology after insomnia treatment: results from a randomized controlled trial over 1 year. J Child Psychol Psychiatry. 2018;59(5):509-522. doi: 10.1111/jcpp.12834 [DOI] [PubMed] [Google Scholar]
- 96.Blake M, Waloszek JM, Schwartz O, et al. The SENSE study: post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. J Consult Clin Psychol. 2016;84(12):1039-1051. doi: 10.1037/ccp0000142 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Search Strategy
eMethods 2. Study Selection
eMethods 3. Data Extraction
eMethods 4. Synthesis of Studies Without Meta-Analysis
eResults.
eTable 1. Included Questions for Risk of Bias Assessment From the Research Triangle Institute Item Bank (RTI-IB) Tool
eTable 2. Summary of Included Studies (n=22)
eTable 3. Included Studies with Beta Coefficients
eTable 4. Meta-Regression Analysis of Pooled Beta Coefficients for the Association Between Disturbed Sleep and Depression
eTable 5. Included Studies With Odds Ratio Values
eTable 6. Meta-Regression Analysis of Pooled ORs for the Association Between Disturbed Sleep and Depression
eTable 7. Synthesis of Studies Without Meta-Analysis by Applying a Simple Vote-Counting by Direction of Effects
eTable 8. Grading of Recommendations Assessment, Development and Evaluation (GRADE) for the Studies Included in the Synthesis With Meta-Analysis
eTable 9. Grading of Recommendations Assessment, Development and Evaluation (GRADE) for the Studies Included in the Synthesis Without Meta-Analysis
eFigure 1. Funnel Plot for Standardized Beta
eFigure 2. Funnel Plot for Odds Ratio
eFigure 3. Leave-One-Out Forest Plot for Standardized Beta
eFigure 4. Leave-One-Out Forest Plot for Odds Ratio
eReferences.