Summary
The lack of access to full‐service restaurants (FSRs) is generally thought to be a risk factor for childhood obesity, as it could discourage healthful eating‐out behaviours while increasing the exposure to unhealthful food venues as “compensatory” options. However, the association between FSR access and childhood obesity has not been comprehensively reviewed previously. A literature search was conducted on PubMed and Web of Science for articles published before 1 January 2019 that examined the association between FSR access and weight‐related behaviours and outcomes among children and adolescents. Eighteen studies conducted in three countries were identified, published from 2006 to 2018 with a median sample size of 2352 (ranging from 323 to 529 367). Findings were mixed among these 18 studies that reported on the association between access to FSRs and weight‐related outcomes. Our meta‐analyses showed that there were no significant associations of FSR access with the level of body mass index (BMI) and the BMI z‐score among children. Also, there was no apparent evidence on the association between FSR access and the risk of overweight/obesity. Our results need to be interpreted with caution, considering the menu quality of FSRs and heterogeneity of eligible studies in this meta‐analysis. Well‐designed epidemiologic studies are warranted to further elaborate on the potential association between FSR access and children's weight status.
Keywords: diet, food environment, obesity, restaurant, child
1. INTRODUCTION
Obesity is a leading cause of morbidity and premature mortality worldwide. 1 A recent study showed that the global age‐standardized prevalence of obesity had reached 5.8% for girls and 7.8% for boys in 2016. 2 The increasing prevalence of overweight and obesity in children can contribute to a greater risk for noncommunicable diseases throughout the life course, such as diabetes, cardiovascular diseases and cancers. 3 Healthy food environments have been well‐known as one of the key factors in the fight against obesity, for example, easy access to healthy food outlets in residential and school neighbourhoods, limited or no access to sugar beverage in schools and childcare centres and strong nutrition standards for foods served at public facilities. 4 They can affect individual's dietary behaviours and subsequently weight status. 5 Therefore, it is important to promote healthy food venues in the neighbourhood.
A full‐service restaurant (FSR) primarily provides table services and sit‐down eatery services to customers and is one of the most important and widely studied food environmental features in obesity research. 6 Over the past years, the availability of FSRs and foods consumed at FSRs have both substantially increased, paralleled by the amount of times children eating at FSRs, which may be associated with children's weight status through different pathways. 7 On one hand, children's meals at FSRs tend to have a higher level of calories, fat, carbohydrates and sugar than those prepared at home 8 , 9 ; excess calories intake, increased portion size and sugar consumptions at FSRs are important risk factors for developing childhood obesity. 10 On the other hand, FSRs may provide healthier food options than other types of food venues, such as fast‐food restaurants, which could make FSR access a potential protective factor for childhood obesity. The reported associations between FSR access in the neighbourhood and the risk for childhood obesity have been inconsistent across studies, and the overall association of FSR access with children's weight‐related outcomes remains not well characterized.
To fill this knowledge gap, we conducted a systematic review and meta‐analysis to quantify the association between FSR access and weight‐related behaviours and outcomes among children and adolescents. We hypothesized that less or lack of access to FSRs in the neighbourhood was associated with a lower level of intake of healthful food, a higher level of compensatory intake of unhealthful food and higher weight status among children and adolescents. Among the included studied, FSR access and the youth's weight‐related behaviours and outcomes were all measured in various forms, which were further compared and summarized in this review. This study would provide a timely, comprehensive overview of measures of FSR access and their association with childhood obesity.
2. METHODS
A systematic review and meta‐analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses.
2.1. Search strategy and literature filtering
A keyword search was performed in PubMed and Web of Science. The search strategy included all possible combinations of keywords related to full‐service restaurants, children, and weight‐related behaviours or outcomes (Appendix S1). Titles and abstracts of the articles identified through the keyword search were screened against the study selection criteria. Potentially relevant articles were retrieved for an evaluation of the full text. Two reviewers independently conducted the title and abstract screening and identified potentially relevant articles for the full‐text review. Discrepancies were screened by a third reviewer. The three reviewers jointly determined the list of articles for the full‐text review. Then, two reviewers independently reviewed the full texts of all studies in the list and determined the final pool of studies included in the review.
2.2. Study selection criteria
Studies that met all of the following criteria were included in the review: (1) study design: observational studies including cross‐sectional and longitudinal studies; (2) study subject: children and adolescents aged <18; (3) exposure variable: FSR access (e.g., number or density of FSRs, distance to the nearest FSR); (4) study outcome: weight‐related behaviours (e.g., eating behaviours) and/or outcomes (e.g., body mass index [BMI, kg/m2], overweight, obesity, waist circumference, waist‐to‐hip ratio and body fat); (5) article type: peer‐reviewed publications that are not letters, editorials, study/review protocols or review articles; (6) time of publication: from the inception of the electronic bibliographic database to 31 December 2018 and (7) language: English.
2.3. Data extraction and preparation
A standardized data extraction form was used to collect methodological and outcome variables from each selected study, including author(s), year of publication, study area, study scale, sample size, sample age, sample characteristics (follow‐up status for longitudinal studies), statistical model, measures of weight‐related behaviours/outcomes, measure(s) of FSR access, other environmental factors adjusted for in the model and key findings on the association between FSR access and weight‐related behaviours/outcomes. If one study reported the estimates by quartiles of the measure of FSR access for the same outcome, we extracted the estimate of the highest quantile compared with lowest quantile. Two reviewers independently extracted data from each study included in the review, and discrepancies were resolved by a third reviewer.
2.4. Meta‐analysis
A meta‐analysis was performed to estimate the pooled associations of FSR access with each weight‐related behaviour and outcome used in the included studies. Weight‐related outcomes included BMI, BMI z‐score, overweight and obesity. The BMI was calculated by dividing the weight (kg) by the squared height (m2). Overweight (BMI ≥85th percentile) and obesity (BMI ≥95th percentile) were defined based on the 2000 age‐ and sex‐specific Centers for Disease Control and Prevention (CDC) Growth Charts, 11 or the International Obesity Task Force (IOTF)‐recommended age‐ and sex‐specific cut‐offs. 12 Several studies were not included in meta‐analyses due to the following reasons: (1) neither standard error nor confidence interval (CI) was reported; (2) the effect size was unable to be transformed into a standardized coefficient (i.e., beta coefficient) due to the limited information reported; (3) a unit change of the exposure variable was inconsistent with others and (4) two or less studies reported the same outcome variables.
The level of study heterogeneity was assessed by the I 2 index and interpreted as modest (I 2 ≤ 25%), moderate (25% < I 2 ≤ 50%), substantial (50% < I 2 ≤ 75%), or considerable (I 2 > 75%). A fixed‐effect model was estimated when a modest to moderate heterogeneity was present, and a random‐effect model was estimated when a substantial to considerable heterogeneity was present. All statistical analyses were conducted by using the Stata 14.2 SE version (StataCorp, College Station, TX). All analyses used two‐sided tests and p < 0.05 was considered statistically significant.
2.5. Study quality assessment
We used the National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies to assess the quality of each included study, which helped to measure the strength of scientific evidence, but was not used to determine the inclusion of studies. This assessment tool rated each study based on 14 criteria. For each criterion, a score of one was assigned if ‘yes’ was the response, whereas a score of zero was assigned otherwise (i.e., an answer of ‘no’, ‘not applicable’, ‘not reported’, or ‘cannot determine’). A study‐specific global score ranging from 0 to 14 was calculated by summing up the scores across all criteria.
3. RESULTS
3.1. Study selection and characteristics
We identified 988 studies from two databases through the keyword search. After deleting 277 duplicates, the remaining 711 studies underwent title and abstract screening, and 662 articles were excluded. The full texts of the remaining 49 studies were reviewed against the study inclusion criteria, and another 31 studies were further excluded. The remaining 18 studies that examined the association between access to FSRs and children's weight‐related behaviours or outcomes were included in this systematic review (Figure 1). 6 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29
FIGURE 1.
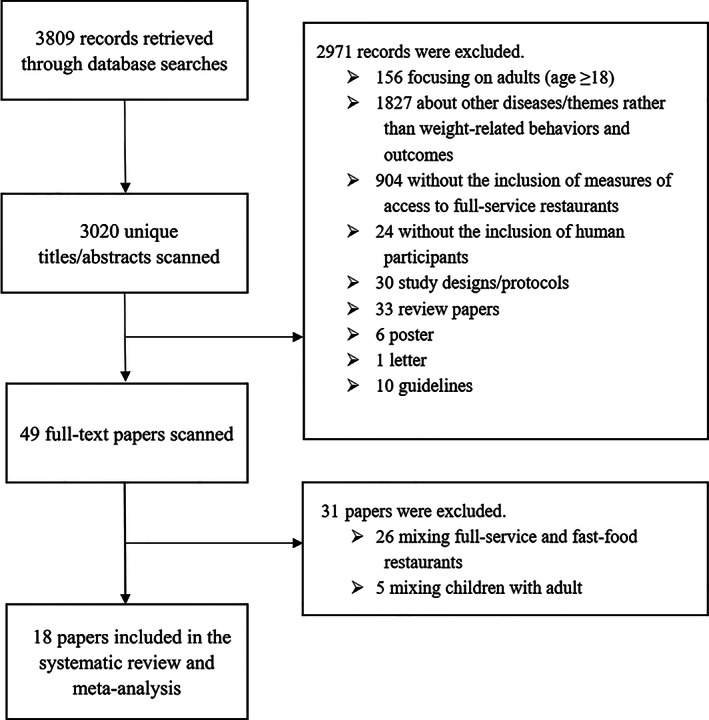
Study exclusion and inclusion flowchart
Eighteen included studies, consisting of 11 cross‐sectional studies and seven cohort studies, were published from 2006 to 2018 (Table 1). Sixteen of those were conducted in the United States and the other two in Canada and China separately. The number of participants ranged from 323 to 529 367 among the 11 cross‐sectional studies and from 348 to 21 639 among the seven cohort studies.
TABLE 1.
Basic characteristics of 18 studies included
| First author (year) | Study area, country a | Sample size | Sample age (years, range and/or mean ± SD) b | Sample characteristics (follow‐up status for longitudinal studies) | Statistical model |
|---|---|---|---|---|---|
| Cohort studies | |||||
| Chen (2016) 26 | Arkansas, USA [S] | 21 639 | In 2003–2004 | School children (followed up from academic year 2003/2004 to 2009/2010 with seven repeated measures) | Growth curve model and cox regression |
| Lee (2012) 29 | USA [N] | 7710 | 6.2 ± 0.4 in 1999 | School children (follow up from 1999 to 2004 with four repeated measures and an attrition rate of 43.0%) | Multilevel linear regression |
| Leung (2011) 6 | California, USA [CT4] | 353 | 6–7 in 2005 | Girls (followed up from 2005 to 2008 with three repeated measures and an attrition rate of 20.5%) | Generalized linear and logistic regression |
| Powell (2009) 21 | USA [N] | 5215 | 12–17 (15.5 ± 1.7) in 1997 | Adolescents living at home (followed up from 1997 to 2000 with four repeated measures) | Multilevel linear regression |
| Shier (2016) 24 | USA [N] | 933 | 12–13 in 2013 | Children in military families | Multiple linear regression |
| Sturm (2005) 15 | USA [N] | 13 282 | 6.2 ± 0.4 in 1999 | Elementary school children (followed up from 1999 to 2002 with three repeated measures and an attrition rate of 42.4%) | Multilevel linear regression |
| Zhang (2016) 23 | China [S9] | 348 | 6–17 (10.9 ± 2.8) in 2009 | Followed up from 2009 to 2011 with two repeated measures | Generalized estimating equation |
| Cross‐sectional studies | |||||
| Auld (2009) 20 | USA [N] | 73 041 | 14.7 in 1997–2003 | School children in Grades 8 and 10 | Quantile regression |
| Davis (2009) 27 | California, USA [S] | 529 367 | In 2002–2005 | Middle and high school students | Linear and logistic regression |
| Fiechtner (2013) 28 | Massachusetts, USA [S] | 438 | 2–6.9 in 2006–2009 | Overweight and obese preschool‐age children | Multivariate linear regression |
| Fiechtner (2015) 22 | Massachusetts, USA [S] | 49 770 | 4–18 in 2011–2012 | Paediatric patients | Multivariate linear regression |
| Galvez (2009) 18 | New York, USA [C] | 323 | 6–8 in 2004 | NA | Multivariate logistic regression |
| Gorski Findling (2018) 19 | USA [N] | 3748 | 2–18 in 2012–2013 | NA | Logistic regression |
| Li (2015) 17 | Alabama, USA [S] | 613 | 4–13 in 2013 | Elementary school children | Multilevel regression |
| Mellor (2011) 16 | Virginia, USA [S] | 2023 | 11.4 ± 1.7 in 2006 | Grades 3, 6, and 7 students | Linear and logistic regression |
| Powell (2007) 13 | USA [N] | 73 079 | 14.7 ± 1.2 in 1997–2003 | School children at Grades 8–10 (seven annual repeated measures from 1997 to 2003) | Multilevel linear regression |
| Seliske (2009) 14 | Canada [N] | 7281 | 11–16 in 2005–2006 | Grades 6–10 school children | Multilevel logistic regression |
| Wall (2012) 25 | Minneapolis/St. Paul, USA [C] | 2682 | 14.5 ± 2.0 in 2009–2010 | Public middle and high school students | Multivariate linear regression |
Abbreviation: NA, not available.
Study area: [N], national; [S], state (e.g., in the United States) or equivalent unit (e.g., province in China and Canada); [Sn], n states or equivalent units; [CT], county or equivalent unit; [CTn], n counties or equivalent units; [C], city; [Cn], n cities.
Sample age: age in baseline year for cohort studies or mean age in survey year for cross‐sectional studies.
3.2. Measures of FSR access
The measures of FSR access mainly included the absolute or per capital number of FSRs within administrative units or catchment areas (i.e., buffer zones), as well as the distance from children's homes/schools to the nearest FSRs (Table 2). The FSR access was measured in five studies as the straight‐line or road‐network distance to the nearest FSRs; in six studies as the number of FSRs within the buffer with a certain radius around homes/schools and in eight studies as the density of FSRs per 10 000 persons within the buffer around homes/schools, or within postal zones where homes/schools were located. One study measured FSR access using a composite score of probability that a child patronized FSRs. The weight‐related behaviours were used in only one study, where the frequency of consumption of fruits, vegetables, soda, sweet snacks, salty snacks, ready‐made dinner and ready‐made dinner were recorded by a modified version of the Beverage and Snack Questionnaire. The weight‐related outcomes were measured in 10 studies, self‐reported in six studies and extracted from electronic health record in two studies.
TABLE 2.
Measures of the access to grocery stores and body‐weight status in 18 included studies
| First author (year) | Measures of access to full‐service restaurants (FSR) | Other environmental factors adjusted for in the model | Measures of weight‐related outcomes or behaviours | Results of weight‐related outcomes or behaviours |
|---|---|---|---|---|
| Cohort studies | ||||
| Chen (2016) 26 | Number of FSRs along the most direct street route from home to school within 50‐m buffer on either side of the street | The same measure for fast food restaurants | • Measured BMI z‐score (based on the 2000 U.S. CDC growth charts) | Better access to FSRs on the route from a student's home to school was associated with lower hazard for the onset of obesity over the study period. |
| • Obesity: BMI ≥ 95th percentile | ||||
| Lee (2012) 29 | • Density of FSRs per 1.6 km2 in home census tract | Density of convenience stores, grocery stores and fast‐food chain restaurants | Measured BMI percentile (based on the 2000 U.S. CDC growth charts) | Less affluent and minority areas also have significantly greater access to food establishments that are not obviously linked to obesity risk, including large‐scale grocery stores and FSRs. |
| • Density of FSRs per 1000 persons in home census tract | ||||
| Leung (2011) 6 | Density of FSRs per 1000 persons in 0.4/1.6‐km home road‐network buffer (in tertiles and quintiles) | NA | • Measured BMI z‐score (based on the 2000 U.S. CDC growth charts) | There were no significant associations between the availability of restaurants within a 0.4‐km network buffer and girls' overweight or BMI z‐scores. |
| • Overweight (BMI ≥85th percentile on the 2000 U.S. CDC growth charts) | ||||
| Powell (2009) 21 | Density of FSRs per 10 000 persons in home county | The same measure for fast‐food restaurants, supermarkets, convenience stores and physical activity facilities | • Self‐reported BMI | No association was found between density of FSRs and BMI. |
| • Overweight: age‐sex specific BMI percentile ≥95th (based on the 2000 U.S. CDC growth charts) | ||||
| Shier (2016) 24 | Number of FSRs in 3.2‐km home straight‐line buffer | Residential region | • Measured BMI z‐score and BMI percentile (based on the 2000 U.S. CDC growth charts) | • Neither the actual nor the perceived availability of particular food outlets in the neighbourhood is associated with children's diet or BMI. |
| • Obese or overweight: if the BMI percentile ≥85th | • Availability of FSRs was unrelated to children's dietary behaviours or how often children eat restaurant meals. | |||
| • Children's dietary behaviours were collected via a modified version of the Beverage and Snack Questionnaire | ||||
| Sturm (2005) 15 | Density of FSRs per 1000 persons in home/school postal zone | NA | Measured BMI | The per capita number of restaurants sometimes became significant, but this result disappeared when we included prices or switched to a different method for adjusting for the clustering. |
| Zhang (2016) 23 | Straight‐line distance from home to the nearest FSRs (in quartiles) | Distance from home to the nearest grocery store, free market and food stall | Measured BMI | The Chinese restaurants seemed to have protective effects, with boys and girls in the second quartile of the proximity to the nearest Chinese restaurant having lower BMI compared to those in the first quartile. |
| Cross‐sectional studies | ||||
| Auld (2009) 20 | Density of FSRs per 10 000 persons in school postal zone | NA | Self‐reported BMI (based on the 2000 CDC growth charts) | • Restaurant availability is not associated with weight. |
| • Restaurant density has very little effect on any conditional quantile of distribution of BMI. | ||||
| • Restaurant access is not statistically or economically associated with BMI. | ||||
| Davis (2009) 27 | • Density of FSRs within 0.8 km from school | The same measure for fast‐food restaurant and other types of establishments such as gas stations, motels and grocery stores | • Measured BMI | There was a smaller relationship between FSRs and a youth's weight status. |
| • Number of FSRs within 0.8‐km road‐network buffer around school | • Overweight (BMI ≥85th percentile) and obesity (BMI ≥95th percentile on the U.S. CDC growth charts) | |||
| Fiechtner (2013) 28 | Road‐network distance from home to the nearest FSRs | Road‐network distance from home address to nearest convenience stores/bakeries/coffee shops/candy stores/supermarkets. | • BMI obtained from the electronic health record | The association between proximity to FSRs and child BMI was not observed. |
| • Overweight (BMI 25 to 30 kg/m2) | ||||
| • Obese (BMI ≥30 kg/m2) | ||||
| Fiechtner (2015) 22 | Road‐network distance from home to the nearest FSRs | Road‐network distance from home address to nearest convenience stores/bakeries/coffee shops/candy stores/supermarkets | BMI z‐score obtained from the electronic health record | Living in closest proximity to FSRs was associated with a higher BMI z‐score versus those living farthest away (β = 0.07, 95% CI: 0.01, 0.14). |
| Galvez (2009) 18 | Number of FSRs in home census tract | NA | • Measured BMI according to a standardized protocol | Statistically significant associations between BMI percentile and number of restaurants on a child's census block were not observed likely due to the small sample size. |
| • Age‐ and sex‐specific BMI percentiles based on the 2000 CDC growth charts | ||||
| Gorski Findling (2018) 19 | Number of FSRs within 1.6‐km straight‐line buffer around home | Rural versus urban household location, vehicle access and closest SNAP retailer | • Self‐reported BMI | There were no other statistically significant relationships between any store types and overweight/obesity when access was set at 0.4 km or 3.2 km. |
| • Overweight/obesity: BMI ≥ 85th percentile (based on the 2000 CDC growth chart) | ||||
| Li (2015) 17 | Composite score of probabilities that a child patronizes FSRs equation: where Sj is the attraction (FSR size) of FSRj, Dij is the street distance from home of child i to FSRj, β is a parameter that reflects the effect of distance on shopping and n is the number of FSRs | NA | • BMI and self‐report BMI (based on the CDC growth charts) | Children with higher probabilities of patronizing FSRs tend to be overweight or obese. The indices of FSRs are negatively associated with children's percentile of BMI. |
| • Overweight: BMI 85th–94th | ||||
| • Obese: BMI > 95th (based on the 2012 CDC growth charts) | ||||
| Mellor (2011) 16 | • Density of FSRs within 0.8‐km road‐network buffer around home | NA | • Measured BMI | • The proximity of FSRs to residences did not have a significant positive association with either BMI or overweight. |
| • Number of FSRs within 0.16‐/0.4‐/0.8‐/1.6‐km road‐network buffer around home | • Obesity: BMI ≥95th percentile (based on the 2000 U.S. CDC growth charts) | • The presence of a FSR within one tenth of 1.6 m from the home has a significant negative association with BMI and obesity. | ||
| Powell (2007) 13 | Density of FSRs per 10 000 persons in school postal zone | Density of chain supermarkets, non‐chain supermarkets, convenience stores, grocery stores and fast‐food restaurants | • Self‐reported BMI | BMI is higher when there are fewer full‐service restaurants. |
| • Obesity: BMI ≥95th percentile (based on the 2000 U.S. CDC growth charts) | ||||
| Seliske (2009) 14 | Density of FSRs per 10 000 persons in 5‐km school straight‐line buffer (in categories of none, low, medium and high exposures) | Density of grocery stores, fast‐food restaurants, sub/sandwich retailers, doughnut/coffee shops and convenience stores | • Self‐reported BMI | Compared with attending schools in neighbourhoods with no FSRs, participants attending schools in neighbourhoods with medium and high numbers of FSRs were less likely to be overweight. |
| • Overweight and obesity: on the basis of IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults) | ||||
| Wall (2012) 25 | • Density of FSRs in 1.6‐km home straight‐line buffer. | NA | Measured BMI z‐score (based on the 2000 U.S. CDC growth charts) | Nearby access to restaurants was associated with higher BMI z‐score in girls suggesting girls may be more influenced by exposure to potentially unhealthy neighbourhood food sources. |
| • Straight‐line distance from home to the nearest FSRs. | ||||
Abbreviations: BMI, body mass index; CDC, Center for Disease Control and Prevention; D&B, Dun and Bradstreet; ECLS‐K, The Early Childhood Longitudinal Study–Kindergarten; FSRs, full‐service restaurants; GIS, geographic information systems; IOTF, International Obesity Task Force; NAICS, North American Industry Classification System; NEMS‐S, Nutrition Environment Measures Survey for Stores; NA, not available; SNAP, Supplemental Nutrition Assistance Program; WHO, World Health Organization.
3.3. Associations between FSR access and obesity‐related behaviours and outcomes
Findings were mixed among 18 studies that reported on the association between FSR access and weight‐related outcomes. Of 18 included studies, one study reported that FSR access, measured by number of FSRs in 3.2‐km home straight‐line buffer, was not associated with children's dietary behaviours or how often children eat restaurant meals. 26 Eight studies found that FSR access was associated with weight‐related outcomes: four studies reported the association of greater access to FSRs with a higher BMI, 27 a higher BMI z‐score 22 , 25 and a higher risk of obesity 17 ; however, five studies reported an opposite association. 13 , 14 , 17 , 23 , 26 Also, eight studies reported that there was no significant association between FSR access and weight‐related outcomes. 6 , 15 , 18 , 19 , 20 , 24 , 28 , 29 Furthermore, two studies reported an interactive effect of sex, where the association between the straight‐line distance from home to the nearest FSR and BMI was found to be stronger in girls than boys. 23 , 25
3.4. Meta‐analysis of weight‐related status
The estimated effects of FSR access on weight‐related behaviours and outcomes were summarized (Table 3). The results of our meta‐analysis showed that there was no significant association between FSR access and children's BMI and BMI z‐score, with pooled estimates of 0.030 (95% CI: −0.014, 0.074; I 2 = 39.7%, τ2 = 0.0010) (Figure 2) and −0.023 (95% CI: −0.085, 0.039; I 2 = 72.7%, τ2 = 0.0031) (Figure 3), respectively. There was no significant evidence of the association between FSR access and the risk for overweight/obesity (OR = 0.997, 95% CI: 0.992, 1.002; I 2 = 60.1%, τ2 = 0.0001) (Figure 4). The associations remained not significant in subgroup analyses by measure of FSR access or by study design. For example, the density of FSRs (number per 10 000 persons) was not associated with the children's BMI (β = 0.025, 95% CI: −0.009, 0.059); the association between the distance from home to the nearest FSRs and children's BMI was also found not to be significant (β = 0.193, 95% CI: −1.291, 1.676).
TABLE 3.
Associations between access to full‐service restaurants and weight‐related behaviours and outcomes in 18 included studies
| ID | Study design | Country | N | Exposure | Outcome | Estimated effect β (SE) or OR [95% CI] | Pooled effect size [95% CI] | I 2 index (%) |
|---|---|---|---|---|---|---|---|---|
| BMI | ||||||||
| Auld (2009) 20 | CS | USA | 73 041 | Density of FSRs per 10 000 persons in school postal zone | Self‐reported BMI | 0.0011 (0.4) | β = 0.025 [−0.09, 0.059] | 36.2 |
| Powell (2007) 13 | CS | USA | 72 854 | Density of FSRs per 10 000 persons in home county | Self‐reported BMI | 0.0039 (0.0029) | ||
| Powell (2009) 21 | CO | USA | 585 | Density of FSRs per 10 000 persons in home county | Self‐reported BMI | 0.0323 (0.0276) | ||
| Davis (2009) 27 | CS | USA | 529 367 | Density of FSRs within 0.8 km from school | Measured BMI | 0.08 [0.01, 0.14] | ||
| Mellor (2011) 16 | CS | USA | 2023 | Density of FSRs within 1.6‐km road‐network buffer around home | Measured BMI | −0.06 [−0.74, 0.62] | ||
| Fiechtner (2013) 28 | CS | USA | 438 | Road‐network distance from home to the nearest FSRs | Measured BMI | 0.21 [−1.35, 1.76] | β = 0.193 [−1.291, 1.676] | 61.9 |
| Zhang (2016) 23 | CO | China | 348 | Straight‐line distance from home to the nearest FSRs (in quartiles) | Measured BMI | 1.97 [−0.05, 4.0] for boys | ||
| −1.70 [−4.29, 0.9] for girls | ||||||||
| Mellor (2011) 16 | CS | USA | 2023 | Number of FSFRs within 1.6‐km road‐network buffer around home | Measured BMI | 0.02 [−0.02, 0.06] | NA | NA |
| BMI percentile | ||||||||
| Lee (2012) 29 | CO | USA | 7730 | Density of FSRs per 1.6 km2 in home census tract | Measured BMI percentile (change) | −0.19 (0.56) | NA | NA |
| Li (2015) 17 | CS | USA | 646 | Composite score of probabilities that a child patronizes FSRs | Measured BMI percentile | −3.45 (SE is NA) | NA | NA |
| BMI z‐score | ||||||||
| Leung (2011) 6 | CO | USA | 353 | Density of FSRs per 1000 persons in 0.4/1.6‐km home road‐network buffer (in tertiles and quintiles) | Measured BMI z‐score | −0.06 [−0.2, 0.07)] | β = −0.091 [−0.195, 0.014] | 55.6 |
| Wall (2012) 25 | CS | USA | 2682 | Density of FSRs in 1.6‐km home straight‐line buffer | Measured BMI z‐score | −0.2 (0.066) for boys | ||
| −0.026 (0.051) for girls | ||||||||
| Wall (2012) 25 | CS | USA | 2682 | Straight‐line distance from home to the nearest FSRs | Measured BMI z‐score | 0.066 (0.065) for boys | β = 0.005 [−0.121, 0.132] | 81.0 |
| −0.122 (0.051) for girls | ||||||||
| Fiechtner (2015) 22 | CS | USA | 49 770 | Road‐network distance from home to the nearest FSRs | Measured BMI z‐score | 0.07 [0.01, 0.14] | ||
| Shier (2016) 24 | CO | USA | 933 | Number of FSRs in 3.2‐km home straight‐line buffer | Measured BMI z‐score | −0.001 (0.002) | NA | NA |
| Overweight/obesity | ||||||||
| Auld (2009) 20 | CS | USA | 73 041 | Density of FSRs per 10 000 persons in school postal zone. | Overweight | 0.0002 (1.15) | OR = 1.011 [0.984, 1.040] | 33.9 |
| Davis (2009) 27 | CS | USA | 529 367 | Density of FSRs within 0.8 km from school | Overweight/obesity | 1.04 [1.01, 1.08] | ||
| Leung (2011) 6 | CO | USA | 353 | Density of FSRs per 1,000 persons in 0.4/1.6‐km home road‐network buffer (in tertiles and quintiles) | Overweight/obesity | 0.75 [0.16, 3.43] | ||
| Mellor (2011) 16 | CS | USA | 2023 | Density of FSRs within 1.6‐km road‐network buffer around home | Obesity | 0.93 [0.67, 1.28] | ||
| Powell (2007) 13 | CS | USA | 72 854 | Density of FSRs per 10 000 persons in home county | Overweight | −0.0002 (0.0002) | ||
| Chen (2016) 26 | CO | USA | 21 639 | Number of FSRs along the most direct street route from home to school within 50‐m buffer on either side of the street | Measured obesity | 0.98 [0.97, 0.99] | OR = 0.977 [0.989, 1.004] | 76.6 |
| Galvez (2009) 18 | CS | USA | 323 | Number of FSRs in home census tract | Obesity | 1.26 [0.74, 2.14] | ||
| Gorski Findling (2018) 19 | CS | USA | 3742 | Number of FSRs within 1.6‐km straight‐line buffer around home | Overweight/obesity | 1.00 [0.99, 1.00] | ||
| Mellor (2011) 16 | CS | USA | 2023 | Number of FSFRs within 1.6‐km road‐network buffer around home | Obesity | 1.02 [0.99, 1.04] | ||
| Shier (2016) 24 | CO | USA | 933 | Number of FSRs in 3.2‐km home straight‐line buffer | Overweight/obesity | −0.001 (0.001) | ||
| Weight‐related dietary behaviours | ||||||||
| Shier (2016) 24 | CO | USA | 933 | Number of FSRs in 3.2‐km home straight‐line buffer | Dietary behaviours (times per week) | 0.001 (0.011) for fruits | NA | NA |
| 0.016 (0.012) for vegetable | ||||||||
| 0.005 (0.009) for soda | ||||||||
| 0.023 (0.017) for sweet snacks | ||||||||
| −0.014 (0.008) for salty snacks | ||||||||
| −0.003 (0.004) for ready‐made dinner | ||||||||
Abbreviations: BMI, body mass index; FSRs, full‐service restaurants; NA, not applicable in meta‐analysis.
FIGURE 2.
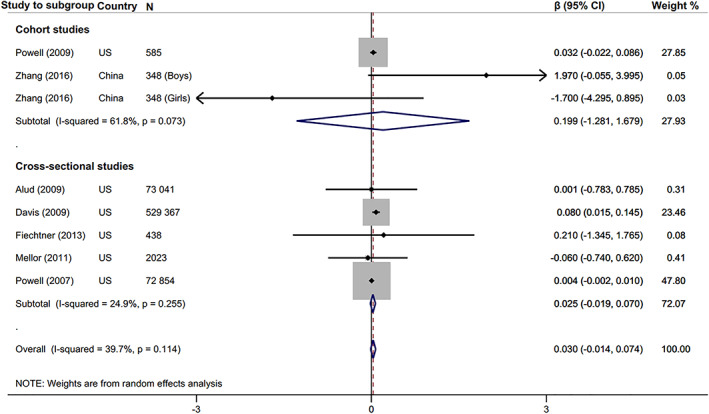
Forest plot of the associations between access to full‐service restaurants and body mass index
FIGURE 3.
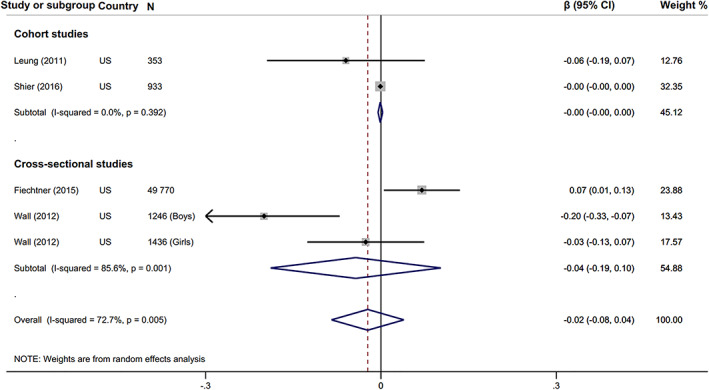
Forest plot of the associations between access to full‐service restaurants and body mass index z‐score
FIGURE 4.
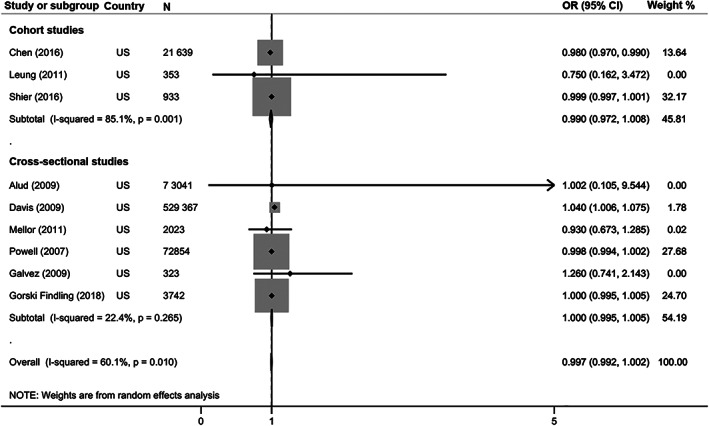
Forest plot of the associations between access to full‐service restaurants and risk for overweight/obesity
3.5. Study quality assessment
According to the criterion‐specific and global ratings from the study quality assessment, the included studies scored 9 out of 14 on average, with a range from 7 to 12 (Table 4).
TABLE 4.
Quality assessment of 18 included studies (see 14 questions in Appendix S2)
|
Criterion study |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen (2016) 26 | ● | ● | ● | ● | ○ | ● | ● | ○ | ● | ○ | ● | ○ | ● | ● | 10 |
| Lee (2012) 29 | ● | ● | ● | ● | ○ | ● | ● | ● | ● | ○ | ● | ○ | ● | ● | 11 |
| Leung (2011) 6 | ● | ● | ● | ● | ○ | ● | ● | ● | ● | ○ | ● | ○ | ● | ● | 11 |
| Powell (2009) 21 | ● | ● | ● | ○ | ○ | ○ | ○ | ○ | ● | ○ | ● | ○ | ● | ● | 7 |
| Shier (2016) 24 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Sturm (2005) 15 | ● | ● | ● | ● | ○ | ● | ● | ○ | ● | ○ | ● | ○ | ● | ● | 10 |
| Zhang (2016) 23 | ● | ● | ● | ● | ○ | ● | ● | ● | ● | ○ | ● | ○ | ● | ● | 11 |
| Auld (2009) 20 | ● | ● | ● | ● | ○ | ○ | ○ | ○ | ● | ○ | ● | ○ | ● | ● | 8 |
| Davis (2009) 27 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Fiechtner (2013) 28 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Fiechtner (2015) 22 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Galvez (2009) 18 | ● | ● | ● | ● | ● | ● | ● | ● | ● | ○ | ● | ○ | ● | ● | 12 |
| Gorski Findling (2018) 19 | ● | ● | ● | ● | ○ | ○ | ○ | ○ | ● | ○ | ● | ○ | ● | ● | 8 |
| Li (2015) 17 | ● | ● | ● | ● | ○ | ○ | ○ | ○ | ● | ○ | ● | ○ | ● | ● | 8 |
| Mellor (2011) 16 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Powell (2007) 13 | ● | ● | ● | ○ | ○ | ○ | ○ | ○ | ● | ○ | ● | ○ | ● | ● | 7 |
| Seliske (2009) 14 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
| Wall (2012) 25 | ● | ● | ● | ● | ○ | ○ | ○ | ● | ● | ○ | ● | ○ | ● | ● | 9 |
Note: ● denotes the answer ‘Yes’, and ○ denotes the answer ‘No’.
4. DISCUSSION
We found that the associations between FSR access and children's weight status reported in previous studies were mixed. Eight out of 18 included studies found no significant associations of FSR access with BMI, BMI z‐score and overweight/obesity. However, some studies found that greater access to FSRs was associated with a higher BMI, BMI z‐score and risk for overweight/obesity, while some reporting an opposite association. In the meta‐analyses, we did not find any significant associations between FSR access and children's weight‐related outcomes (BMI, BMI z‐score or overweight/obesity).
Among included studies, the cohort study with the largest sample size reported that greater access to FSRs was significantly associated with a decreased risk for overweight or obesity. However, the cross‐sectional study with the largest sample size reported an opposite association. Our meta‐analysis showed that there was a weak, not significant association of greater access to FSRs with the decreased risk for overweight or obesity. The study conducted in Canada reported that middle school students with greater access to FSRs had a lower risk for overweight. 14 The potential mechanism behind this relationship may be that greater access to FSRs could provide an opportunity to select healthier food in the Canadian context. Most included studies could not find any significant associations between FSR access and children's weight‐related outcomes, which might be because FSRs provide not only healthy foods but also unhealthy foods, so their effects on weight status might have been offset. Also, the limited number of included studies may weaken the statistical power of our meta‐analysis, thereby leading to lack of the observed significant associations.
The association between access to FSRs and children's weight status is complex. The frequency of eating at FSRs might be an important factor mediating this association. 30 However, none of the included studies investigated a potential mediation effect through the frequency of eating at FSRs. The menu in these restaurants may also influence children's dietary intake, where, if FSRs provide more options of healthful foods, they could help children decrease their overall calorie intake and thus maintain or improve their weight status. 7 , 31 The household income and lifestyles of parents could be other mediators between FSR access and children's weight status, which could also explain inconsistent associations across the included studies. The different socio‐economic factors in the context of individual studies may also affect the pooled estimates in our meta‐analysis; the association between FSR access and children's weights status may alter with or without adjusting for socio‐economic factors. For example, a significant negative association between the density of FSRs and obesity prevalence was initially found across the United States, but disappeared after adjusting for additional socio‐economic factors. 32 The density or number of FSRs are principally larger in high‐income areas than in low‐income areas. 33 Although wealthier and more educated individuals have more access to FSRs, they have better food environments and dietary behaviours in general, thus are less susceptible to obesity. Underlying the mediation effects might be important heterogeneities in socio‐economic factors. Therefore, our findings in this study need to be interpreted with caution.
Although this study is a comprehensive synthesis of evidence of the associations between FSR access and children's weight‐related outcomes, there are also some limitations in the study. First, the types of food served in FSRs may vary across subcategories of FSRs, especially in large study areas. 34 This issue also exists in the studies on other types of food environmental features. 35 , 36 , 37 , 38 , 39 Hence, more studies using detailed subcategories of FSRs or even FSR menus would further advance this field. 40 , 41 Second, the measures of FSR access varied across those studies, which hindered comparability across studies. 42 We tried to mitigate this issue by conducting subgroup analyses for each measure of FSR access, which, however, included a limited number of eligible studies in each analysis and thereby weakened the robustness of the findings. Therefore, reporting quality of interdisciplinary studies should be improved by following relevant reporting guidelines. 43 Third, subgroup analyses by income status and country, which might function as potential effect modifiers of the associations of interest, were not performed because of the limited number of studies. Doing so in the future would help to better understand the patterns of visiting FSRs, so future study designs could be improved with consideration of more unidentified confounders. Fourth, other components of the built environmental exposure may affect the association among food environments, diets and weight status. 44 , 45 For example, active transport could coincide with eating out, so energy balance should be evaluated by better interdisciplinary approaches in the future. Fifth, this study did not examine whether the association of FSR access with childhood obesity was confounded or modified by the relative access to the fast‐food restaurants. Lastly, most of the included studies are cross‐sectional studies, which may subject to reverse causation. Longitudinal studies with food environment also measured in the same frequency at least are warranted to consolidate the current association. 46
5. CONCLUSIONS
In this study, our meta‐analyses showed that there was no evidence of the significant associations between FSR access and weight‐related outcomes. Although evidence is limited, it is still important to advocate FSRs to provide higher quality food, which could make individuals with better access to FSRs less likely to be susceptible to diet‐related diseases. The improvement of children's eating environments remains an important potential strategy to curb the global obesity epidemic. Given the low feasibility of the randomized clinical trials directly testing the primary prevention of obesity by FSR access, providing more well‐designed prospective cohort studies and more evidence for policies focusing on children's environments are needed to further elaborate on the association between FSR access and children's weight status.
CONFLICT OF INTEREST
No conflict of interest was declared.
Supporting information
Data S1. Supporting information
ACKNOWLEDGEMENTS
We thank the International Institute of Spatial Lifecourse Epidemiology (ISLE) and the National Natural Science Foundation of China (91746205) for research support. [Correction added on 8 February 2021, after first online publication: Acknowledgements have been revised.]
Jia P, Yang H, Cao X, et al. Association between access to full‐service restaurants and childhood obesity. Obesity Reviews. 2021;22(S1):e13076. 10.1111/obr.13076
Peng Jia and Hongxi Yang contributed equally to this study.
[Correction added on 8 February 2021, after first online publication: Peng Jia's correspondence details have been updated. Also, affiliations 1 and 2 were interchanged.]
[Correction added on 8 February 2021, after first online publication: Funding Information have been revised.]
Contributor Information
Peng Jia, Email: jiapengff@hotmail.com.
Yaogang Wang, Email: wyg@tmu.edu.cn.
REFERENCES
- 1. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980‐2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Collaboration NCDRF . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population‐based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627‐2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jia P, Ma S, Qi X, Wang Y. Spatial and temporal changes in prevalence of obesity among Chinese children and adolescents, 1985‐2005. Prev Chronic Dis. 2019;16:E160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Swinburn B, Kraak V, Rutter H, et al. Strengthening of accountability systems to create healthy food environments and reduce global obesity. Lancet. 2015;385(9986):2534‐2545. [DOI] [PubMed] [Google Scholar]
- 5. Jia P, Cheng X, Xue H, Wang Y. Applications of geographic information systems (GIS) data and methods in obesity‐related research. Obes Rev. 2017;18(4):400‐411. [DOI] [PubMed] [Google Scholar]
- 6. Leung CW, Laraia BA, Kelly M, et al. The influence of neighborhood food stores on change in young girls' body mass index. Am J Prev Med. 2011;41(1):43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Powell LM, Nguyen BT. Fast‐food and full‐service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatr. 2013;167(1):14‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eissa MA, Hearne K, Saavedra N. Comparison of Children's menu items at full‐ and quick‐service restaurants. South Med J. 2018;111(4):192‐197. [DOI] [PubMed] [Google Scholar]
- 9. Wolfson JA, Moran AJ, Jarlenski MP, Bleich SN. Trends in sodium content of menu items in large chain restaurants in the U.S. Am J Prev Med. 2018;54:28‐36. [DOI] [PubMed] [Google Scholar]
- 10. Sliwa S, Anzman‐Frasca S, Lynskey V, Washburn K, Economos C. Assessing the availability of healthier children's meals at leading quick‐service and full‐service restaurants. J Nutr Educ Behav. 2016;48:242‐249. e1 [DOI] [PubMed] [Google Scholar]
- 11. Kuczmarski RJ, Ogden CL, Grummer‐Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;314:1‐27. [PubMed] [Google Scholar]
- 12. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ (Clin Res Ed). 2000;320:1240‐1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Powell LM, Auld MC, Chaloupka FJ, O'Malley PM, Johnston LD. Access to fast food and food prices: relationship with fruit and vegetable consumption and overweight among adolescents. Adv Health Econ Health Serv Res. 2007;17:23‐48. [PubMed] [Google Scholar]
- 14. Seliske LM, Pickett W, Boyce WF, Janssen I. Association between the food retail environment surrounding schools and overweight in Canadian youth. Public Health Nutr. 2009;12(9):1384‐1391. [DOI] [PubMed] [Google Scholar]
- 15. Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059‐1068. [DOI] [PubMed] [Google Scholar]
- 16. Mellor JM, Dolan CB, Rapoport RB. Child body mass index, obesity, and proximity to fast food restaurants. Int J Pediatr Obes. 2011;6(1):60‐68. [DOI] [PubMed] [Google Scholar]
- 17. Li Y, Robinson LE, Carter WM, Gupta R. Childhood obesity and community food environments in Alabama's Black Belt region. Child Care Health Dev. 2015;41:668‐676. [DOI] [PubMed] [Google Scholar]
- 18. Galvez MP, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food‐store availability in an inner‐city community. Acad Pediatr. 2009;9(5):339‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gorski Findling MT, Wolfson JA, Rimm EB, Bleich SN. Differences in the neighborhood retail food environment and obesity among US children and adolescents by SNAP participation. Obesity (Silver Spring, md). 2018;26:1063‐1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Auld MC, Powell LM. Economics of food energy density and adolescent body weight. Economica. 2009;76(304):719‐740. [Google Scholar]
- 21. Powell LM. Fast food costs and adolescent body mass index: evidence from panel data. J Health Econ. 2009;28(5):963‐970. [DOI] [PubMed] [Google Scholar]
- 22. Fiechtner L, Sharifi M, Sequist T, et al. Food environments and childhood weight status: effects of neighborhood median income. Child Obes (Print). 2015;11(3):260‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang J, Xue H, Cheng X, et al. Influence of proximities to food establishments on body mass index among children in China. Asia Pac J Clin Nutr. 2016;25(1):134‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shier V, Nicosia N, Datar A. Neighborhood and home food environment and children's diet and obesity: evidence from military personnel's installation assignment. Soc Sci Med. 2016;158:122‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wall MM, Larson NI, Forsyth A, et al. Patterns of obesogenic neighborhood features and adolescent weight: a comparison of statistical approaches. Am J Prev Med. 2012;42(5):e65‐e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen D, Thomsen MR, Nayga RM Jr, Bennett JL. Persistent disparities in obesity risk among public schoolchildren from childhood through adolescence. Prev Med. 2016;89:207‐210. [DOI] [PubMed] [Google Scholar]
- 27. Davis B, Carpenter C. Proximity of fast‐food restaurants to schools and adolescent obesity. Am J Public Health. 2009;99(3):505‐510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fiechtner L, Block J, Duncan DT, et al. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool‐age children. Prev Med. 2013;56(3‐4):218‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee H. The role of local food availability in explaining obesity risk among young school‐aged children. Soc Sci Med. 2012;74:1193‐1203. [DOI] [PubMed] [Google Scholar]
- 30. Ayala GX, Rogers M, Arredondo EM, et al. Away‐from‐home food intake and risk for obesity: examining the influence of context. Obesity (Silver Spring, Md). 2008;16:1002‐1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Robinson E, Jones A, Whitelock V, Mead BR, Haynes A. (Over)eating out at major UK restaurant chains: observational study of energy content of main meals. BMJ (Clin Res Ed). 2018;363:k4982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mazidi M, Speakman JR. Higher densities of fast‐food and full‐service restaurants are not associated with obesity prevalence. Am J Clin Nutr. 2017;106(2):603‐613. [DOI] [PubMed] [Google Scholar]
- 33. Guarnizo‐Herreno CC, Courtemanche C, Wehby GL. Effects of contextual economic factors on childhood obesity. Matern Child Health J. 2019;23(10):1317‐1326. [DOI] [PubMed] [Google Scholar]
- 34. Zhang X, Zhang M, Zhao ZP, et al. Obesogenic environmental factors of adult obesity in China: a nationally representative cross‐sectional study. Environ Res Lett: ERL [Web Site]. 2020;15:044009. [Google Scholar]
- 35. Yang S, Zhang X, Feng P, et al. Access to fruit and vegetable markets and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xin J, Zhao L, Wu T, et al. Association between access to convenience stores and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jia P, Luo M, Li Y, Zheng JS, Xiao Q, Luo J. Fast‐food restaurant, unhealthy eating, and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li Y, Luo M, Wu X, Xiao Q, Luo J, Jia P. Grocery store access and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhou Q, Zhao L, Zhang L, et al. Neighborhood supermarket access and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jia P, Xue H, Cheng X, Wang Y. Effects of school neighborhood food environments on childhood obesity at multiple scales: a longitudinal kindergarten cohort study in the USA. BMC Med. 2019;17(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang Y, Jia P, Cheng X, Xue H. Improvement in food environments may help prevent childhood obesity: evidence from a 9‐year cohort study. Pediatr Obes. 2019;14:e12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jia P, Xue H, Yin L, Stein A, Wang M, Wang Y. Spatial technologies in obesity research: current applications and future promise. Trends Endocrinol Metabol: TEM. 2019;30(3):211‐223. [DOI] [PubMed] [Google Scholar]
- 43. Jia P, Yu C, Remais JV, et al. Spatial lifecourse epidemiology reporting standards (ISLE‐ReSt) statement. Health Place. 2020;61:102243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Xu F, Jin L, Qin Z, et al. Access to public transport and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Jia P, Zou Y, Wu Z, et al. Street connectivity, physical activity, and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12943.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jia P, Lakerveld J, Wu J, et al. Top 10 research priorities in spatial lifecourse epidemiology. Environ Health Perspect. 2019;127(7):74501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information


