In The Lancet, Stephanie Salyer and colleagues' comprehensive and elegant cross-sectional analysis of COVID-19 case counts, response measures, and mortality rates highlights the diversity of the COVID-19 burden and response across Africa.1 Between Feb 14 and Dec 31, 2020, 2 763 421 COVID-19 cases and 65 602 deaths were reported in African countries, accounting for 3·4% of the 82 312 150 cases and 3·6% of the 1 798 994 deaths reported globally. Their Article shows the variable effects of COVID-19 across Africa, which more severely affected the Northern and Southern regions during both waves of the pandemic. Strikingly, 43% of the reported COVID-19 cases and 46% of the deaths occurred in the Southern region, in contrast to 3% of the reported cases and 2% of the deaths in the Central region. At the end of 2020, there was clear asymmetry in the pandemic's toll: nine countries (South Africa, Morocco, Tunisia, Egypt, Ethiopia, Libya, Algeria, Kenya, and Nigeria) accounted for 82·6% (2 283 613) of the cases reported and five countries (South Africa, Egypt, Morocco, Tunisia, and Algeria) accounted for 77% of the deaths reported. Although the statistics reported by Salyer and colleagues are sobering, they are limited by incomplete data for surveillance, testing, and reporting of COVID-19 cases, as well as potentially inconsistent case definitions.1 Thus, it is possible that the toll of COVID-19 on African countries could be higher than reported here, especially within some demographic strata.
The pandemic response, notably lockdown measures, also varied across African countries according to whether cases were high or low. The data used by Salyer and colleagues to show these associations came from various sources—both official government reports and unofficial data sources that were verified by an official source before they were included in this analysis. Although the authors were meticulous in ensuring the accuracy of case and mortality estimates, incomplete official case reporting leads us to question whether case and mortality estimates fully reflect the pandemic's toll in all African countries. Consideration needs to be given as to why Africa is home to 17% of the world's population but only 3·4% of the global COVID-19 cases.2 Among many possible answers are differences in population structure, comorbidities, pre-existing cross-reactive SARS-CoV-2 immunity, household composition, lifestyle factors such as mobility and population mixing, and varying effectiveness of different response strategies.3, 4, 5 These points emphasise the authors' call for robust, clear, and timely data reporting as a critical step towards combating the pandemic.
Adequate COVID-19 testing is a crucial part of the pandemic response, providing essential data for case numbers. However, Salyer and colleagues found that as of Dec 31, 2020, 17 of the 55 member states in Africa reported tests per case ratios less than the recommended ten to 30 tests per case ratio; 36% (four of 11 countries for which data were available) had adequate testing capacity (tests per case ratios >10) at the peak of the second wave. At the start of the first wave, testing strategies varied widely in terms of target population and pretest probability of having a positive result. As a result, the tests per case measure probably belies heterogeneity in testing algorithms, populations, and local access within countries, and might not always reflect adequate testing capacity. The data challenges faced by Salyer and colleagues underline the severe need for stronger official data collection at every level. Furthermore, they report on the heterogeneous nature of COVID-19 case definitions used by African countries, leading the authors to assume that case definitions met WHO criteria; the need for this assumption further indicates the requirement to devote resources to case finding and reporting in most African countries. We need to improve data collection and communication and strengthen pathology and laboratory systems across Africa,6 because an absence of information about cases limits our understanding of heterogeneity in disease burden and hinders our response.
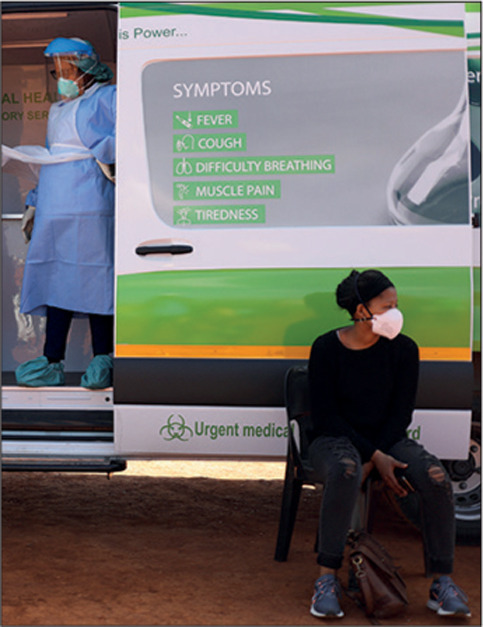
© 2021 Siphiwe Sibeko/Reuters
The authors highlight the political dynamics that often influence public health and social measures, as well as their effectiveness. During the first wave, nearly all countries implemented stringent measures,3 whereas only 72% of countries did so during the second wave.1 Decisions to relax or not implement stringent measures were sometimes made despite increasing case counts, ostensibly to limit the socioeconomic effects of potential lockdowns. There is ample opportunity for individual countries and regional and international health organisations to learn from the visualisations in the Article by Salyer and colleagues showing the correlation between public health measures and COVID-19 case counts and adapt their responses to mitigate the ongoing second wave. Unfortunately, as the authors report, the second COVID-19 wave has hit many African countries harder than the first. More transmissible SARS-CoV-2 variants are likely to be a driver of this surge,7 but fewer and less stringent public health and social measures and so-called lockdown fatigue also contribute.8 One solution, COVID-19 vaccination, began in Africa on March 1, 2021.9 However, vaccination roll-out has already varied substantially across African countries, with the Southern region leading the distribution of the vaccines.10 Vaccination challenges include insufficient vaccine doses for Africa. A strong step forward would be integrating COVID-19 vaccination efforts with ongoing vaccination programmes and promoting equitable access to vaccines worldwide, far beyond the existing COVAX initiative, which will not be sufficient for African countries in need of vaccines. There is a long delay between the western and southern countries in roll-out and the aim to vaccinate 20% of the population in COVAX participating countries is far less than the 60% target of the African Union to reach population immunity.11 Ultimately, unequal COVID-19 vaccine access reflects global structural inequalities in resources and health care, which must be remedied through multilateral investment in health system strengthening and efforts to redress global inequality.12
An important conclusion from the Article by Salyer and colleagues is the need for country-specific solutions. No one-size-fits-all approach will succeed within a continent as diverse as Africa. Countries with a high number of COVID-19 deaths desperately need vaccination to prevent further illness and deaths from severe COVID-19. Some countries might not request the vaccines because of their COVID-19 epidemiology, whereas other countries have a greater need but will be limited by the 20% allowance. By contrast, countries with low case fatality ratios could instead invest in community engagement, health system strengthening, surveillance, and case reporting to adequately handle high case counts during this wave and beyond. Mental health issues have become an increasing concern during the pandemic, with a high prevalence of anxiety and depression,13, 14 while extant infectious diseases such as measles and cholera have gained a stronger foothold, evidenced by increasing case counts and inadequate vaccination.15, 16 During the pandemic, prevention and treatment services for tuberculosis, HIV, and malaria have been disrupted and concerted investments and efforts are needed to strengthen endemic disease programmes.17 Focusing on such efforts could help countries better adjust local measures to balance COVID-19 transmission control with other health needs and economic opportunity and stability.
As African countries continue to face the COVID-19 pandemic, innovative and homegrown solutions, including local production of vaccine and rapid diagnostic tests, stronger involvement of community workers in disease surveillance, and telemedicine, have never been more important. Local solutions should ensure COVID-19 is not only a challenge that is met, but also an opportunity to strengthen health systems before the next pandemic.
This online publication has been corrected. The corrected version first appeared at thelancet.com on June 17, 2021
Acknowledgments
We declare no competing interests.
References
- 1.Salyer SJ, Maeda J, Sembuche S, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. 2021 doi: 10.1016/S0140-6736(21)00632-2. published online March 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . World Health Organization; Geneva: 2020. Coronavirus disease (COVID-19). Global epidemiological situation.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20201005-weekly-epi-update-8.pdf [Google Scholar]
- 3.Massinga Loembé M, Tshangela A, Salyer SJ, Varma JK, Ouma AEO, Nkengasong JN. COVID-19 in Africa: the spread and response. Nat Med. 2020;26:999–1003. doi: 10.1038/s41591-020-0961-x. [DOI] [PubMed] [Google Scholar]
- 4.Mbow M, Lell B, Jochems SP, et al. COVID-19 in Africa: dampening the storm? Science. 2020;369:624–626. doi: 10.1126/science.abd3902. [DOI] [PubMed] [Google Scholar]
- 5.WHO . World Health Organization; Geneva: 2020. Coronavirus disease (COVID-19). Situation reports and dashboard.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situationreports [Google Scholar]
- 6.Sayed S, Cherniak W, Lawler M, et al. Improving pathology and laboratory medicine in low-income and middle-income countries: roadmap to solutions. Lancet. 2018;391:1939–1952. doi: 10.1016/S0140-6736(18)30459-8. [DOI] [PubMed] [Google Scholar]
- 7.Tessema SK, Inzaule SC, Christoffels A, et al. Accelerating genomics-based surveillance for COVID-19 response in Africa. Lancet Microbe. 2020;1:e227–e228. doi: 10.1016/S2666-5247(20)30117-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilesanmi OS, Bello AE, Afolabi AA. COVID-19 pandemic response fatigue in Africa: causes, consequences, and counter-measures. Pan Afr Med J. 2020;37(suppl 1):37. doi: 10.11604/pamj.supp.2020.37.1.26742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO . World Health Organization; Geneva: 2021. First COVID-19 COVAX vaccine doses administered in Africa.https://www.who.int/news/item/01-03-2021-first-covid-19-covax-vaccine-doses-administered-in-africa [Google Scholar]
- 10.Boum Ii Y, Ouattara A, Torreele E, Okonta C. How to ensure a needs-driven and community-centred vaccination strategy for COVID-19 in Africa. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-005306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Lancet Access to COVID-19 vaccines: looking beyond COVAX. Lancet. 2021;397:941. doi: 10.1016/S0140-6736(21)00617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivers LC, Walton DA. COVID-19: Global health equity in pandemic response. Am J Trop Med Hyg. 2020;102:1149–1150. doi: 10.4269/ajtmh.20-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mviena JLM, Fanne M, Gondo R, et al. How mental health care is changing in Cameroon because of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:e62–e63. doi: 10.1016/S2215-0366(20)30390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guha-Sapir D, Moitinho de Almeida M, Keita M, Greenough G, Bendavid E. COVID-19 policies: remember measles. Science. 2020;369:261. doi: 10.1126/science.abc8637. [DOI] [PubMed] [Google Scholar]
- 16.Hassan OB, Nellums LB. Cholera during COVID-19: the forgotten threat for forcibly displaced populations. EClinicalMedicine. 2021;32 doi: 10.1016/j.eclinm.2021.100753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sands P. HIV, tuberculosis, and malaria: how can the impact of COVID-19 be minimised? Lancet Glob Health. 2020;8:e1102–e1103. doi: 10.1016/S2214-109X(20)30317-X. [DOI] [PMC free article] [PubMed] [Google Scholar]


