This cohort study assesses patterns of telehealth use across surgical specialties before and during the COVID-19 pandemic.
Key Points
Question
What were telehealth use patterns across surgical specialties before and during the COVID-19 pandemic?
Findings
In this statewide cohort study that included 4405 surgeons, telehealth use grew substantially during the early pandemic period and declined during the later period; this use varied by surgical specialty. Compared with 2019 visit volume, telehealth salvaged only a small portion of 2020 surgical visits.
Meaning
Telehealth is being used in surgical fields at rates higher than before the pandemic, and its use varies across surgical specialties.
Abstract
Importance
While telehealth use in surgery has shown to be feasible, telehealth became a major modality of health care delivery during the COVID-19 pandemic.
Objective
To assess patterns of telehealth use across surgical specialties before and during the COVID-19 pandemic.
Design, Setting, and Participants
Insurance claims from a Michigan statewide commercial payer for new patient visits with a surgeon from 1 of 9 surgical specialties during one of the following periods: prior to the COVID-19 pandemic (period 1: January 5 to March 7, 2020), early pandemic (period 2: March 8 to June 6, 2020), and late pandemic (period 3: June 7 to September 5, 2020).
Exposures
Telehealth implementation owing to the COVID-19 pandemic in March 2020.
Main Outcomes and Measures
(1) Conversion rate defined as the rate of weekly new patient telehealth visits divided by mean weekly number of total new patient visits in 2019. This outcome adjusts for a substantial decrease in outpatient care during the pandemic. (2) Weekly number of new patient telehealth visits divided by weekly number of total new patient visits.
Results
Among 4405 surgeons in the cohort, 2588 (58.8%) performed telehealth in any patient care context. Specifically for new patient visits, 1182 surgeons (26.8%) used telehealth. A total of 109 610 surgical new outpatient visits were identified during the pandemic. The median (interquartile range) age of telehealth patients was 46.8 (34.1-58.4) years compared with 52.6 (38.3-62.3) years for patients who received care in-person. Prior to March 2020, less than 1% (8 of 173 939) of new patient visits were conducted through telehealth. Telehealth use peaked in April 2020 (week 14) and facilitated 34.6% (479 of 1383) of all new patient visits during that week. The telehealth conversion rate peaked in April 2020 (week 15) and was equal to 8.2% of the 2019 mean weekly new patient visit volume. During period 2, a mean (SD) of 16.6% (12.0%) of all new patient surgical visits were conducted via telehealth (conversion rate of 5.1% of 2019 mean weekly new patient visit volumes). During period 3, 3.0% (2168 of 71 819) of all new patient surgical visits were conducted via telehealth (conversion rate of 2.5% of 2019 new patient visit volumes). Mean (SD) telehealth conversion rates varied by specialty with urology being the highest (14.3% [7.7%]).
Conclusions and Relevance
Results from this study showed that telehealth use grew across all surgical specialties in Michigan in response to the COVID-19 pandemic. While rates of telehealth use have declined as in-person care has resumed, telehealth use remains substantially higher across all surgical specialties than it was prior to the pandemic.
Introduction
The COVID-19 pandemic created an urgent need to overhaul health care delivery. The US health care system suddenly faced 2 new mandates: minimize patient and clinician exposure to COVID-19 and maintain patient access to health care. Telehealth, in the form of video and audio-only visits, had the potential to address these challenges. In the pandemic’s early months, national telehealth use in Medicare beneficiaries grew from 13 000 visits per week to nearly 1.7 million.1 Within surgical fields, telehealth had been previously used for preoperative and postoperative follow-up visits2,3,4,5 although at low levels prior to the COVID-19 pandemic.6,7 While telehealth use in surgery has shown to be feasible, the profession found itself in a novel situation during the COVID-19 pandemic, wherein telehealth became a major modality of health care delivery.
While it is clear that telehealth uptake has increased during the COVID-19 pandemic, several unknowns remain. First is the extent to which surgical specialties used telehealth vs in-person care during the COVID-19 pandemic. While some specialties (eg, psychiatry) do not require the physical examination and in-office testing, this is not the case for surgical specialties. Additionally, the amount of care provided through telehealth is expected to vary from the early months of the pandemic (March to June 2020) through to the later part of the pandemic (June to September 2020) because during the later period, many health care systems and practices allowed in-person visits because of the availability of masks and social distancing practices. Second, it is not known whether surgical specialties were able to convert in-person appointments to telehealth. National data indicate that 60% to 70% of patients deferred care during the pandemic.7,8 In this study, conversion rate refers to the extent to which surgical specialties were able to salvage visits compared with patient volumes in 2019. Finally, the variation in these patterns of telehealth use across surgical subspecialties is not known. The capacity for telehealth conversion in each surgical specialty may differ because of differences in the balance of outpatient vs inpatient care, the range of diagnoses able to be determined without tactile portions of the physical examination, the sensitivity of the visit’s content, and whether cases were elective vs urgent or emergent.
Few studies of telehealth exist because of the relatively new nature of patients accessing telehealth from home.9 Prior studies of surgical telehealth have limited their scope primarily to patient acceptability and the feasibility of the clinic to use telehealth.4 Other contemporary studies have also been limited to single institutions or specific diagnoses and operations.10,11,12 The objective of this study is to assess the patterns of telehealth use across surgical specialties before and during the COVID-19 pandemic with the hypothesis that there will be significant variation by surgical specialty.
Methods
Data and Study Population
We used claims from a large commercial insurance payer in Michigan for this analysis. The plan covers 3.5 million individuals per year, approximately 700 000 of whom saw a surgeon in 2019. For our primary analysis, we identified new adult outpatient visits with a surgeon (Current Procedural Terminology [CPT] codes 92002, 92004, 99201-99205) during a 9-month period (January 5 to September 5, 2020). We focused our primary analysis on new patient visits, which are more reliably billed for and thus more reliably included in claims data. Postoperative visits for established patients may be part of a global or bundled payment for surgery and thus are more likely to be missing from claims data. While our primary analysis was limited to new patient visits, we performed a sensitivity analysis using all surgical evaluation and management claims. We included all 9 available surgical specialties: colorectal surgery, general surgery, neurosurgery, obstetrics and gynecology, ophthalmology/ear, nose, and throat (ENT), orthopedics, plastic surgery, thoracic surgery, and urology. The study was deemed exempt from review by the University of Michigan institutional review board given that all data were deidentified.
Identifying Telehealth Visits
We categorized new patient visits by in-person office visits or telehealth visits (audio-only or video visits), using appropriate telehealth modifier codes. Because of relaxed billing rules during the pandemic, we could not reliably differentiate audio-only visits from video visits and therefore did not report audio-only visits separately. However, we did perform a sensitivity analysis that included audio-only billing codes (CPT codes 99441-99443). We counted only 1 visit per day per patient; for patients with multiple visits in 1 day, we categorized them as having a telehealth visit that day if one of the visits was by telehealth. These excluded claims accounted for 0.5% of total claims.
During our 9-month study period, we defined 3 pandemic time periods based on trends observed in the raw data: period 1 (pre–COVID-19 pandemic), period 2 (early pandemic), and period 3 (late pandemic). Period 1 represents January 5 to March 7, 2020. Because clinics began to accelerate in-person care several weeks into the pandemic, we examined 2 periods during the COVID-19 pandemic. Period 2 represents the early pandemic and spans March 8 to June 6, 2020, when national and state telehealth regulations were relaxed to accommodate social distancing measures and Michigan stay-at-home orders were executed.13 Period 3 represents the late pandemic when emergency orders, such as the ban on elective procedures, lifted and spans June 7 to September 5, 2020. Our control group comprised new patient visits in the prior year (2019) for the same calendar weeks of each period. All of the examined visits are associated with a surgeon.
Defining Telehealth Conversion
Our primary outcomes describe telehealth conversion due to telehealth implementation in 2020. Telehealth conversion is the rate of new patient telehealth visits per week divided by the mean weekly total new patient visit volume in the prior year (2019). Mean weekly total new patient visit volume in the prior year is calculated over the corresponding dates in each period the prior year: January 6 to September 7, 2019. We then examined telehealth conversion after telehealth implementation by surgical specialty to determine which specialties were more or less likely to convert in-person appointments to telehealth. We examined the mean telehealth conversion rates in each study period.
Statistical Analysis
We performed a descriptive analysis of the surgical telehealth uptake in 2020 compared with in-person visits. In addition to demographics, we examined whether patients were from rural areas as determined by zip code with a Rural-Urban Commuting Area code of 2 or 314 and whether patients were from higher-income areas as determined by zip code median income higher than the median income for all patients.15 Univariate χ2 and Wilcoxon rank sum test analyses were used as appropriate to assess differences in patient characteristics between those who used telehealth vs those who received care in person. We plotted the trends in overall telehealth surgical use over time.
Sensitivity Analysis
We performed a sensitivity analysis to assess the robustness of our primary findings. Some surgical specialties may have reserved telehealth use for established patients, while some may have coded audio-only visits outside of the new and established visit codes. Thus, we performed a sensitivity analysis for period 2 to examine whether adding established patient visits or audio-only visits to the cohort changed which specialties were more or less likely to adopt telehealth. In our first sensitivity analysis, we added established patient visits (CPT codes 92012, 92014, 99211-99215). In a second sensitivity analysis, we added audio-only visits (CPT codes 99441-99443) to the new and established patient visits.
We used SAS statistical software version 9.6 (SAS Institute) to prepare our cohorts and perform all statistical analyses. All statistical tests were 2-sided and performed at the 5% significance level.
Results
Overall Surgical Telehealth Conversion
Telehealth was used by 2588 of 4405 active surgeons (58.8%) in any patient care context. Active surgeons were those with at least 1 new patient visit in 2020. Specifically for new patient visits, 1182 active surgeons (26.8%) used telehealth (Figure 1). We identified 109 610 surgical new outpatient visits from March 8, 2020, through September 5, 2020. Of these visits, there were 6634 telehealth visits (6.1%) and 102 976 in-person visits (94.0%). This is compared with the 8 telehealth visits (<0.1% of 173 939 total visits) during the same time in 2019.
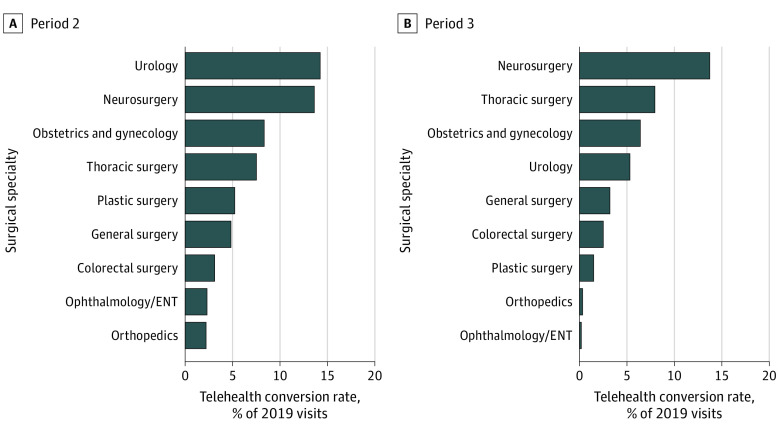
Figure 1. Surgeon Telehealth Use in New Patient Visits by Surgical Specialty in 2020.
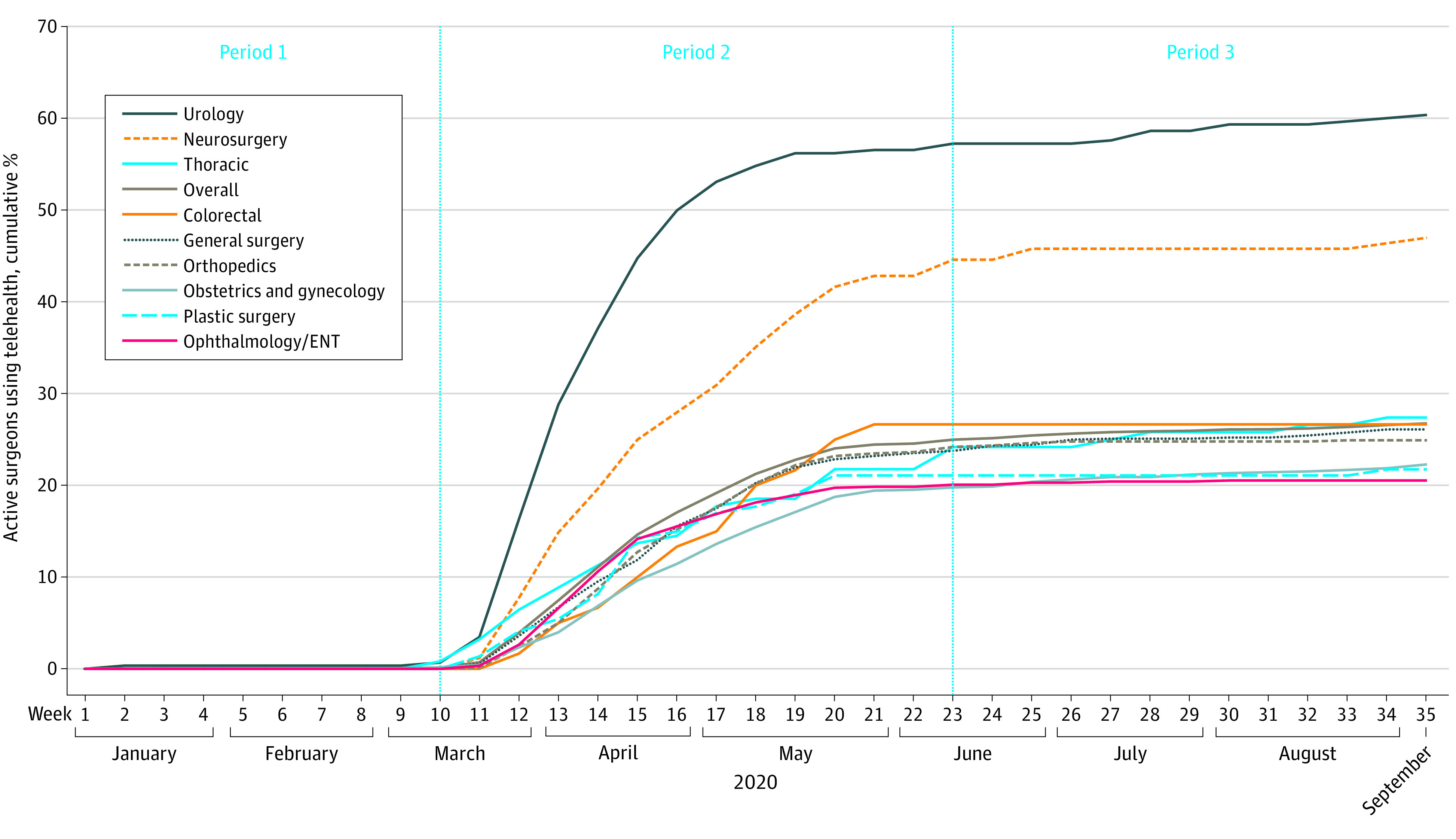
The number of active surgeons during 2020 for each specialty are as follows: urology (n = 288), neurosurgery (n = 168), thoracic (n = 124), colorectal (n = 60), general surgery (n = 892), orthopedics (n = 698), obstetrics and gynecology (n = 1152), plastic surgery (n = 147), ophthalmology/ear, nose, and throat (ENT) (n = 876). The overall number of surgeons was 4405.
Weekly telehealth use peaked in April 2020 (week 14), accounting for 34.6% (479 of 1383) new patient visits for that week. The Table shows patient characteristics for patients who used telehealth vs in-person visits following telehealth implementation (periods 2 and 3). The median (interquartile range) age of telehealth patients was 46.8 (34.1-58.4) years compared with 52.6 (38.3-62.3) years for patients who received care in-person (P < .001). There were more women than men among all surgical patients. Rural patients were less likely to use telehealth visits than nonrural patients (867 of 18 531 [4.7%] vs 5655 of 82 910 [6.8%]; χ2 = 115.5; P < .001). Patients who lived in below–median income zip codes were less likely to use telehealth compared with those who lived in above–median income zip codes (3065 of 50 304 [6.1%] vs 3457 of 51 137 [6.8%]; χ2 = 18.8; P < .001).
Table. Characteristics of New Patients Who Had a Surgical Telehealth vs In-Person Visit After Telehealth Implementationa.
| Characteristic | Patients, No. (%) | P value | |
|---|---|---|---|
| Telehealth visit (n = 6522) | In-person visit (n = 94 919) | ||
| Female | 3885 (59.6) | 54 558 (57.5) | .001 |
| Male | 2637 (40.4) | 40 361 (42.5) | |
| Age, y | |||
| Median (IQR) | 46.8 (34.1-58.4) | 52.6 (38.3-62.3) | <.001 |
| ≥60 | 1390 (21.3) | 29 902 (31.5) | <.001 |
| <60 | 5132 (78.7) | 65 017 (68.5) | |
| Zip code | |||
| Rural | 867 (13.3) | 17 664 (18.6) | <.001 |
| Nonrural | 5655 (86.7) | 77 255 (81.4) | |
| Median income zip code | |||
| Aboveb | 3457 (53.0) | 47 680 (50.2) | <.001 |
| Below | 3065 (47.0) | 47 239 (49.8) | |
Abbreviation: IQR, interquartile range.
The period after telehealth implementation is defined as March 8 to September 5, 2020 (periods 2 and 3).
The median income for all zip codes included in our sample was $56 458.
Weekly telehealth conversion rates from January 5 to September 5, 2020, are shown in Figure 2. The mean (SD) weekly rate of telehealth use over period 2 (early pandemic) was 16.6% (12.0%), corresponding with a telehealth conversion rate of 5.1% of prior year (2019) visits. The mean (SD) weekly rate of telehealth use over period 3 (late pandemic) was 3.0% (0.7%) in 2020, corresponding with a telehealth conversion rate of 2.5% of prior year visits. The telehealth conversion rate peaked in April 2020 (week 15 of the study period) at 8.2% of prior year visits. At the end of the study period, the weekly telehealth conversion rate was 2.1%.
Figure 2. Telehealth, In-Person, and Total Surgical New Patient Visits in 2020.
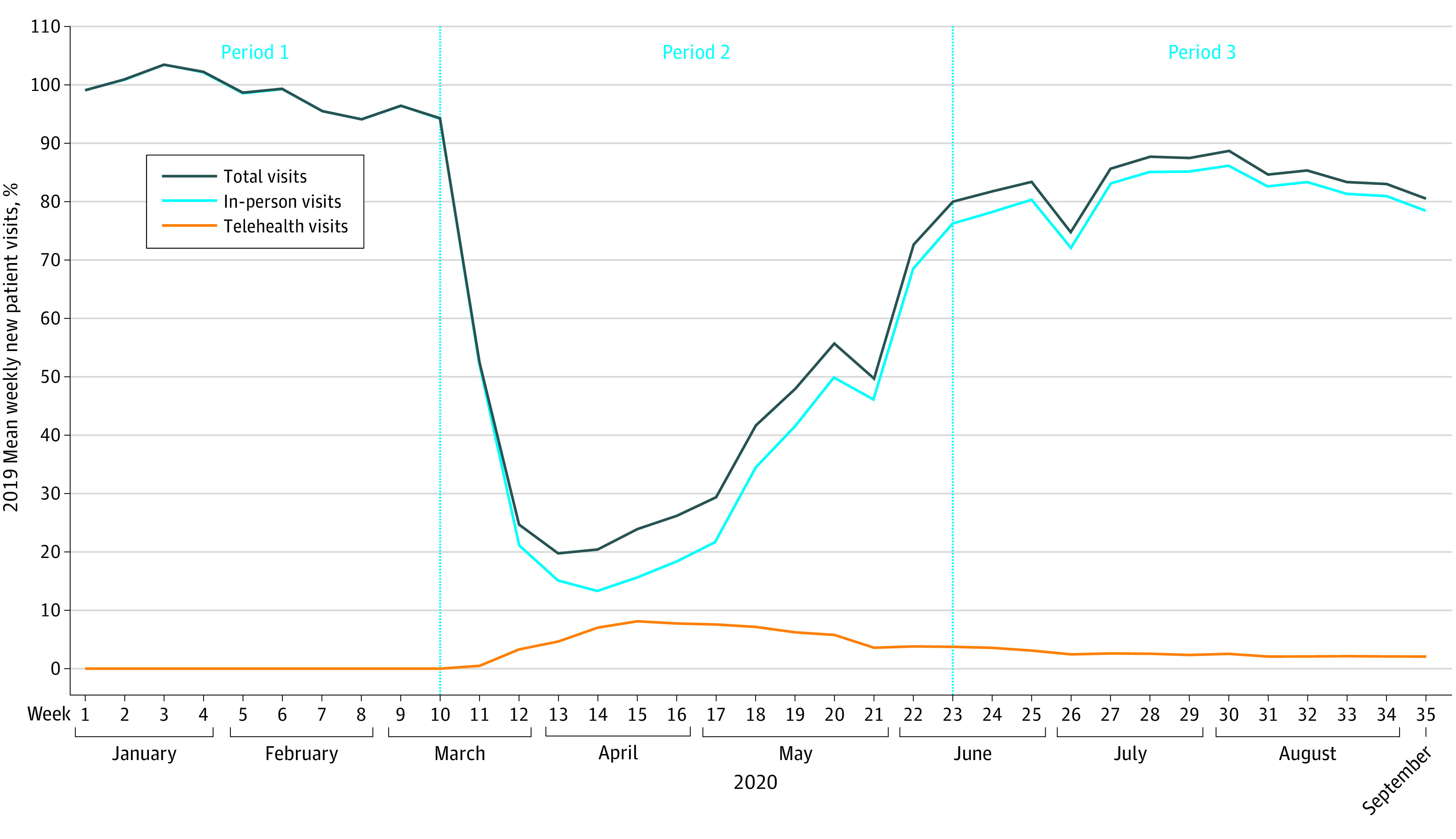
Usage rates by week are calculated by total number of visits in 2020 divided by the mean weekly new patient visits in 2019 over the same period. Week 10 corresponds with the start of the COVID-19 pandemic in 2020 in the US. In 2019, there was a mean in period 1 of 6869, period 2 of 6769, and period 3 of 6610 total new patient surgical visits per week. In 2020, there was a mean of 6791 new patient surgical visits per week in preimplementation period 1. After telehealth implementation, period 2 (early pandemic) had 2907 and period 3 (late pandemic) had 5525 mean total new patient surgical visits per week.
In-person visits continued to contribute to the majority of new patient visits. During preimplementation period 1, the volume of in-person visits in 2020 was 98.9% (61 111 of 61 818) of total volume in 2019. During period 3, the in-person visit volume was 37.9% (33 343 of 88 003) of total volume in the prior year.
Total visit volume following telehealth implementation was at first low and then rose as the pandemic continued. The period 2 2020 total visit volume was 42.9% (37 791 of 88 003) of total volume in the prior year. Total volume increased throughout periods 2 and 3 to a peak of 88.7% (5864 of 6610) of prior year volume and was 80.6% (5325 of 6610) of prior year volume at the end of the study period. Weekly telehealth conversion rates, as well as in-person visit use, are included in eTable 1 in the Supplement.
Variation in Telehealth Conversion by Surgical Specialty
The telehealth conversion rate for most surgical subspecialties was less than 10%. The specialties with the highest rates of telehealth conversion were neurosurgery and urology (Figure 3). The mean (SD) telehealth conversion rate for urology in period 2 was 14.3% (7.7%) of new patient visits in the prior year. The mean (SD) telehealth conversion rate for neurosurgery in period 3 was 13.8% (3.7%) of new patient visits in the prior year. Urology had the greatest weekly telehealth conversion rate of period 2 at 24.8%, while neurosurgery had the greatest peak weekly telehealth conversion rate of period 3 at 20.7%. Telehealth conversion rates decreased over time, for urology more quickly than neurology. The specialty with the lowest telehealth conversion during period 2 was orthopedics, with a mean (SD) telehealth conversion of 2.3% (1.6%). The specialty with the lowest telehealth conversion during period 3 was ophthalmology/ENT, with a mean (SD) telehealth conversion of 0.3% (0.2%). The mean (SD) telehealth conversion rates for the specialties during period 2 were 3.2% (2.1%) for colorectal surgery, 4.9% (2.4%) for general surgery, 13.7% (7.7%) for neurosurgery, 8.4% (4.6%) for obstetrics and gynecology, 2.4% (1.6%) for ophthalmology/ENT, 5.3% (4.3%) for plastic surgery, and 7.6% (3.6%) for thoracic surgery.
Figure 3. Mean Telehealth Conversion Rates After Telehealth Implementation in 2020 by Surgical Specialty.
ENT indicates ear, nose, and throat.
Our primary findings did not change substantially with our sensitivity analysis. When we added established patient visits, the specialty with the greatest mean (SD) telehealth conversion was still urology (21.6% [11.0%]). The lowest telehealth conversion was among ophthalmology/ENT (mean [SD], 2.5% [1.5%]). When including audio-only visits, the specialty with the greatest mean (SD) telehealth conversion remained urology (26.3% [13.7%]) and the lowest, ophthalmology/ENT (3.2% [1.8%]). The mean telehealth conversion by specialty for each of these cohorts is shown in eTable 2 in the Supplement.
Discussion
During the COVID-19 pandemic, there was a substantial increase in telehealth use across all surgical specialties, with a slow decline after June 2020. When comparing 2019 and 2020 total patient volumes, we found that 2020 telehealth salvaged only a small portion of total care delivered in 2019. Finally, we found substantial variation between surgical specialties in telehealth conversion.
The growth in surgical telehealth during the COVID-19 pandemic mirrors the growth (and eventual decline of telehealth) for other specialties, albeit at slightly lower levels. Mehrotra et al16 found that early on in the pandemic, telehealth facilitated approximately 30.4% of all outpatient visits. Data from the Epic Health Research Network showed telehealth use peaked in ambulatory visits at 69% in mid-April.8 However, as the pandemic continued, telehealth use declined, starting June 2020.8,16 This was likely for 3 reasons. First, clinics began to reopen for in-person care, and so the total number of patients receiving care increased while the number of telehealth visits did not, proportionally. Second, a large number of patients who initially deferred care at the beginning of the pandemic returned for in-person care. Third, patients and surgeons alike may have viewed the use of telehealth as a temporary means to meet the needs of the pandemic. So, when in-person visits were once again available, telehealth use did not continue.
Our finding that surgical telehealth conversion rates were low is consistent with other studies that have identified barriers to adoption of telehealth in surgery. Prior to the pandemic, surgical fields have been less likely to use telehealth than other specialties.6 The Kane and Gillis cross-sectional study,6 surgical specialties’ use of telehealth was 11.4%, the lowest compared with other specialties, which ranged from 12.7% in primary care to 39.5% in radiology. We found in our study that even during the pandemic when telehealth became a safer option for care and insurance policies changed to ensure reimbursement, still only about 25% of surgeons were using telehealth for new patient visits. When examining telehealth use in any context, approximately 59% of all surgeons used telehealth. Thus, surgical telehealth adoption remains particularly difficult compared with other specialties. There are a variety of likely barriers to the adoption of surgical telehealth, despite the potential benefits for patients4 and health care systems.10,11 Policy-level barriers include concerns that the reimbursement of telehealth may disappear once the threat of the pandemic has passed. This was found to be a concern for 76% of surgeons in a survey performed summer 2020.17 Thus, investing time and resources to update clinical workflows and to learn how to engage patients meaningfully through telehealth may be too high of a burden. Additionally, in a field where physical examination is used to diagnose and to determine treatment plans, many surgeons have not been trained in how to assess patients via telehealth. Thus, many may consider it unsafe or inefficient (should patients need a second visit for in-person evaluation) to provide care via telehealth.
We also found that there was significant variation between surgical specialties in telehealth conversion. The surgical specialties with the highest rates of telehealth conversion were urology and neurosurgery. This may be because many urologists were already using telehealth and could more easily convert their new patient visits to telehealth. A 2018 study showed that urologists were more likely than general surgeons, obstetricians and gynecologists, ophthalmologists, otolaryngologists, and orthopedic surgeons to have used telehealth at some point in patient care.6 Separately, it is possible that neurosurgery is a field better poised to transition to telehealth care given the established telehealth networks for teleneurology throughout the United States.14 These 2 specialties may also be able to rely more heavily than other surgical specialties on imaging for diagnosis, making it easier to perform telehealth consultations for new patients.
Patient barriers to telehealth use also remained during the pandemic, which may have prevented higher rates of telehealth use. To complete a telehealth visit, there were a number of necessities: private space, stable telephone or internet connection, device on which to contact clinicians, and an understanding of how to engage with telephone or virtual platforms.18,19,20 Lack of any of these resources would have led to a decreased visit conversion rate.
Limitations
Our study has several limitations. First, we used an insurance claims data set. Therefore, we were unable to access the clinical details of each patient case. It is possible that patients who underwent in-person visits did so because they required an in-person evaluation. Thus, it would have been inappropriate for these patients to receive care via telehealth. Second, because we were unable to reliably assess rates of postoperative telehealth within the global period, we focused our primary analysis on new patient visits (which are reliably available in insurance claims). While our findings should be taken within the context of new patient visits, the sensitivity analyses using established visit codes showed no substantial change in our results. Third, race and ethnicity data were not available through this data set. It is well established in previous research that systemic racism affects access to health care and health outcomes. Moving forward, research in telehealth use should look at racial and ethnic disparities in access to telehealth as well as clinical and health care utilization outcomes associated with telehealth use.
Telehealth, although not a new technology, is being newly used and on a massive scale. As we continue to monitor telehealth’s effects on clinical outcomes for patients, our study shows that surgical visits cannot be considered in aggregate given the heterogeneity in telehealth conversion by surgical specialty. Future studies must focus next on whether telehealth truly replaces in-person visits or increases health care utilization and whether it maintains surgical outcomes by specialty given that the quality of surgical care via telehealth in this new era remains unknown.21 The effect on patients, payers, and clinicians from a cost standpoint is also an important future area of research.
Conclusions
In this study of insurance claims from a Michigan statewide commercial payer for new patient visits with a surgeon, telehealth was used by surgeons during the COVID-19 pandemic at much higher rates than in the past, with significant variation across specialties. This study shows that telehealth conversion in surgery is not a one-size-fits-all solution. Determining the ideal rate of conversion to telehealth depends on the clinical needs of patients. Therefore, future research must focus on clinical outcomes for patients. These trends in telehealth utilization should continue to be followed after the public health emergency.
eTable 1. Surgical Weekly New Patient Telehealth and In-Person Visit Numbers and Rates
eTable 2. Sensitivity Analysis of Telehealth Conversion Rates with Expanded Cohorts in Period II
References
- 1.Varma S. Early impact of CMS expansion of Medicare telehealth during COVID-19. Health Affairs Blog. Published July 15, 2020. Accessed March 8, 2021. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/
- 2.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823-827. doi: 10.1001/jamasurg.2013.2672 [DOI] [PubMed] [Google Scholar]
- 3.Kummerow Broman K, Roumie CL, Stewart MK, et al. Implementation of a telephone postoperative clinic in an integrated health system. J Am Coll Surg. 2016;223(4):644-651. doi: 10.1016/j.jamcollsurg.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 4.Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018;4:11. doi: 10.21037/mhealth.2018.04.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viers BR, Lightner DJ, Rivera ME, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68(4):729-735. doi: 10.1016/j.eururo.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 6.Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood). 2018;37(12):1923-1930. doi: 10.1377/hlthaff.2018.05077 [DOI] [PubMed] [Google Scholar]
- 7.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: practices are adapting to the new normal. The Commonwealth Fund. Updated June 25, 2020. Accessed November 15, 2020. https://www.commonwealthfund.org/publications/2020/jun/impact-covid-19-pandemic-outpatient-visits-practices-adapting-new-normal
- 8.Fox BT, Sizemore JO. Telehealth: fad or the future. Epic Health Research Network. Published August 18, 2020. Accessed March 8, 2021. https://www.ehrn.org/articles/telehealth-fad-or-the-future/ [Google Scholar]
- 9.Ellimoottil C, Boxer RJ. Bringing surgical care to the home through video visits. JAMA Surg. 2018;153(2):177-178. doi: 10.1001/jamasurg.2017.4926 [DOI] [PubMed] [Google Scholar]
- 10.Wamsley CE, Kramer A, Kenkel JM, Amirlak B. Trends and challenges of telehealth in an academic institution: the unforeseen benefits of the COVID-19 global pandemic. Aesthet Surg J. 2021;41(1):109-118. doi: 10.1093/asj/sjaa212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chao GF, Ehlers AP, Ellimoottil C, Varban OA, Dimick JB, Telem DA. Convergent mixed methods exploration of telehealth in bariatric surgery: maximizing provider resources and access. Obes Surg. Published online October 27, 2020. doi: 10.1007/s11695-020-05059-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lightsey HM, Crawford AM, Xiong GX, Schoenfeld AJ, Simpson AK. Surgical plans generated from telemedicine visits are rarely changed after in-person evaluation in spine patients. Spine J. 2021;21(3):359-365. doi: 10.1016/j.spinee.2020.11.009 [DOI] [PubMed] [Google Scholar]
- 13.The Office of Governor Gretchen Whitmer. Executive order 2020-04: declaration of state of emergency. Accessed May 1, 2020. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-521576--,00.html
- 14.USDA Economic Research Service. Rural-urban commuting area codes. Updated August 17, 2020. Accessed March 8, 2021. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx
- 15.United States Census Bureau . 2018 Table S1901 at census tract level: income in the past 12 months (in 2018 inflation-adjusted dollars). Published 2018. Accessed July 1, 2020. https://data.census.gov/cedsci/table?q=2018%20Table%20S1901%20at%20census%20tract%20level&tid=ACSST1Y2018.S1901&hidePreview=false
- 16.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider EC. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. The Commonwealth Fund. Updated October 15, 2020. Accessed November 15, 2020. https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels
- 17.The COVID-19 Healthcare Coalition Telehealth Impact Study Work Group . Telehealth impact: physician survey analysis. COVID-19 Healthcare Coalition. Updated October 22, 2020. Accessed November 15, 2020. https://c19hcc.org/telehealth/physician-survey-analysis/
- 18.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4-12. doi: 10.1177/1357633X16674087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147-1148. doi: 10.1093/jamia/ocaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mishori R, Antono B. Telehealth, rural America, and the digital divide. J Ambul Care Manage. 2020;43(4):319-322. doi: 10.1097/JAC.0000000000000348 [DOI] [PubMed] [Google Scholar]
- 21.Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180-1181. doi: 10.1016/S0140-6736(20)30818-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Surgical Weekly New Patient Telehealth and In-Person Visit Numbers and Rates
eTable 2. Sensitivity Analysis of Telehealth Conversion Rates with Expanded Cohorts in Period II