Abstract
Background
Nursing home (NH) populations have borne the brunt of morbidity and mortality of COVID-19. We surveyed Michigan NHs to evaluate preparedness, staffing, testing, and adaptations to these challenges.
Methods
Interpandemic survey responses were collected May 1-12, 2020. We used Pearson's Chi-squared test, Fisher's exact test, and logistic regression to evaluate relationships.
Results
Of 452 Michigan NHs contacted via e-mail, 145 (32.1%) opened the survey and of these, 143 (98.6%) responded. Sixty-eight percent of respondents indicated their response plan addressed most issues. NHs reported receiving rapidly changing guidance from many sources. Two-thirds reported shortages of personal protective equipment and other supplies. Half (50%) lacked sufficient testing resources with only 36% able to test residents and staff with suspected COVID-19. A majority (55%) experienced staffing shortages. Sixty-three percent experienced resignations, with front-line clinical staff more likely to resign, particularly in facilities caring for COVID-19 patients (P < .001). Facilities adapted quickly, creating COVID-19 units (78%) to care for patients on site. To reduce isolation, NHs facilitated communication via phone calls (98%), videoconferencing (96%), and window visits (81%). A majority continued to provide requisite therapies (90%).
Conclusions
NHs experienced shortages of resources, testing supplies, and staffing challenges. COVID-19 in the facility was a key predictor of staff resignations. Facilities relied on rapidly changing, often conflicting advice from multiple sources, suggesting high-yield areas of improvement.
Keywords: Preparedness, Staffing, Infection prevention and control, Pandemic
Nursing homes (NHs) have borne a disproportionate burden of the Coronavirus Disease 2019 (COVID-19) pandemic, accounting for over 472,487 confirmed and suspected cases, and 40% of all COVID-19 deaths in the United States.1 Long-term care facility residents currently account for approximately 7% of cases and 30% of deaths due to COVID-19 in the state of Michigan.2 NH residents have been uniquely vulnerable to COVID-19 due to heightened risk of transmission in high-density congregate living settings with limited infection prevention resources, high staff turnover, and have greater risk of poor outcomes among infected residents due to high rates of medical comorbidities and low functional status.3, 4, 5, 6
Michigan's first case of COVID-19 was reported on March 10, 2020. A survey of pandemic response plans completed by 130 Michigan NHs March 11-16, 2020 showed that NHs had already begun planning for the pandemic and identified challenges if their facilities were to face an outbreak.7 Higher rates of established lines of communication with public health officials were found when compared to a prior 2007 survey of NH preparedness plans for pandemic H1N1 influenza. However, the March 2020 survey found 42% of respondents were concerned about supply shortages and 32% were concerned about maintaining adequate staffing during the pandemic. Facilities received guidance from a variety of sources including the Centers for Medicare and Medicaid Services (CMS), Centers for Disease Control and Prevention (CDC), state public health officials, and facility parent corporations. Guidance from professional societies did not appear to reach a majority of NHs.
In the setting of 47,237 cases and 4,341 deaths statewide as of May 1,8 we disseminated an online survey to state registered NHs to characterize their experience during the first pandemic wave. The goal of this interpandemic study was to evaluate whether pandemic planning prior to COVID-19 proved adequate in the first 2 months of the Michigan outbreak. We were particularly interested in the rapid adaptations that NHs made in response to challenges with a focus on those that could be mitigated in the event of a fall resurgence.
Methods
Survey distribution strategy
A cross-sectional interpandemic survey was developed and distributed by e-mail to NH contacts registered in the state of Michigan. These NH contacts were identified with state partners responsible for licensing and were the same contacts used for our previous survey assessing COVID-19 pandemic preparedness.7 The COVID-19 interpandemic response survey was sent to NH administrators on May 1, 2020. NH administrators were encouraged to include others at the facility in order to accurately answer the survey questions (eg, Director of Nursing, Infection Preventionist). A reminder e-mail was sent to nonresponders on May 8 and a final e-mail request was distributed on May 12, the last day that responses were accepted.
Survey instrument development
A 43-question survey was prepared online using Qualtrics survey software.9, 10, 11, 12, 13 Survey domains included facility characteristics, guidance referenced during pandemic response, staffing and supply challenges, education, and adaptations made in the midst of the situation. Forty questions were administered in multiple choice format, with follow-up questions soliciting further detail and options available to add comments.
Analysis
Statistical analyses were conducted using Stata/IC 15.1 (StataCorp). To evaluate the significance of potential associations, we used Pearson's Chi-squared test and Fisher's Exact test where the distribution of responses yielded a cell size of less than 10. We used logistic regression to evaluate relationships between outcomes of interest and ordinal predictors. We hypothesized that facility ownership (for-profit vs not), facility bed capacity, current presence of COVID-19 positive patients, and an existing designated unit for COVID-19 patients would be associated with outcomes including supply shortages, provision of staff education, use of telemedicine, and staffing challenges.
Results
Response rates
The interpandemic survey was e-mailed to 452 NH contacts. Of the 145 (32.1%) contacts who opened the survey via the link provided, 143 (98.6%) responded.
Facility characteristics
The majority (66.9%) of surveyed facilities operate on a for-profit basis (Supplementary Table S1). Almost 3 quarters (73.9%) reported that daily occupancy had been lower than usual during the pandemic. In the first 2 months of the pandemic in Michigan (March 10 to completion of survey May 1-12, 2020), only 9.9% of surveyed NHs maintained occupancy of 90% or more, compared to 23% of respondents reporting >90% occupancy in the quarter before the pandemic. Over a third (36.2%) operated at 81%-90% occupancy, and 23.4% at 71%-80% occupancy. The remainder (30.5%) operated below 70% occupancy.
Overall pandemic response planning
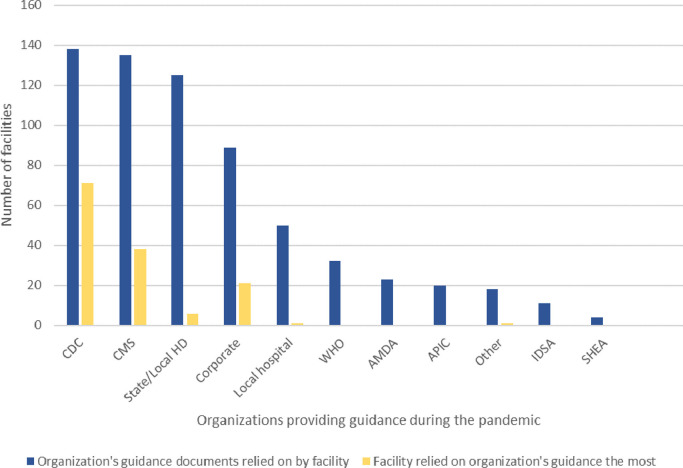
All but 3 facilities had a pandemic response plan for COVID-19 (Table 1 ). The majority of respondents (67.6%) felt that their facility response plan addressed most elements of the pandemic well, addressing >90% of issues that arose. All but one facility (138/139, 99.3%) referred to guidance from the CDC when addressing the pandemic (Fig 1 ). Also frequently referenced were guidance documents from CMS (97.1%), state or local health departments (89.9%), and corporate leadership (64.0%). When asked which organization's guidance was relied on the most, 51.5% answered CDC; 27.5% answered CMS; 15.2% corporate; and 4.4% state or local health department. While local hospital or healthcare organization guidance was referenced by 36.0% of respondents, only 1 facility reported relying on each of these sources the most, suggesting that federal guidance held precedence over local guidance.
Table 1.
Pandemic response planning: management of personal protective equipment supplies and training
| Question | N (%) |
| How well has your facility's Pandemic Response Plan for COVID-19 addressed actual issues? | |
| Very well; plan addressed >90% of issues | 94/139 (67.6%) |
| Fair; plan addresses most but not all issues | 40/139 (28.8%) |
| Not very well; plan addressed <50% of issues | 2/139 (1.4%) |
| Not applicable; we did not have a Pandemic Response Plan for COVID-19 | 3/139 (2.2%) |
| Has your facility experienced a shortage of any supplies? | |
| Yes | 91/139 (65.5%) |
| No | 48/139 (34.5%) |
| Which supplies ran low or out? | |
| Gowns | 76/91 (83.5%) |
| Alcohol-based sanitizer | 54/91 (59.3%) |
| N95 respirators | 47/91 (51.7%) |
| Masks (surgical) | 38/91 (41.8%) |
| Eye shields/goggles | 18/91 (19.8%) |
| Gloves | 15/91 (16.5%) |
| Other | 10/91 (11.0%) |
| Who helped your facility obtain supplies when they ran short/out? (check all that apply) | |
| Corporate | 52/91 (57.1%) |
| County/local health department | 47/91 (51.7%) |
| Community | 44/91 (48.4%) |
| State government | 28/91 (30.8%) |
| Local hospitals | 11/91 (12.1%) |
| Federal government | 11/91 (12.1%) |
| Other | 30/91 (33.0%) |
| As the COVID-19 pandemic was evolving, were facility staff given additional education on PPE use? | |
| Yes | 139/139 (100.0%) |
| No | 0 |
| Don't know | 0 |
| What source was used for PPE education? | |
| CDC | 120/139 (86.3%) |
| Corporate | 84/139 (60.4%) |
| State and/or local health department | 73/139 (52.5%) |
| Social media | 6/139 (4.3%) |
| Other | 12/139 (8.6%) |
| How was this education presented? (check all that apply) | |
| In-person, one-on-one training | 109/138 (80.0%) |
| Written policy/procedure, “read and sign” | 92/138 (66.7%) |
| In-person, group training | 86/138 (62.3%) |
| On-demand computer training (eg, modules) | 47/138 (34.1%) |
| Live virtual training (eg, Skype, Zoom) | 24/138 (17.4%) |
| Other | 3/138 (2.2%) |
| Does your facility do any of the following re: PPE education? (check all that apply) | |
| Perform random audits of PPE use with direct feedback to staff | 123/137 (89.8%) |
| Repeat education periodically (eg, monthly, staff meetings, etc.) | 117/137 (85.4%) |
| Use a trained staff “observer” to ensure PPE is used correctly | 112/137 (81.8%) |
| Other | 2/137 (1.5%) |
| No ongoing education or audits at this time | 6/137 (4.4%) |
Fig 1.
Organizations providing guidance relied on during the pandemic. Facilities referred to guidance from a variety of organizations during the pandemic. Federal organizations, such as CDC and CMS, were frequently reported to be relied upon the most.
Personal protective equipment
Many respondents (65.5%) experienced a shortage of supplies (Table 1). Gowns (83.5% of facilities), alcohol-based sanitizer (59.3%), and N95 respirators (51.7%) were often in short supply. Corporate leadership (57.1%), health departments (51.7%), and the local community (48.4%) helped facilities obtain needed supplies. All surveyed facilities provided additional education on PPE use as the COVID-19 pandemic was evolving. Modes of education delivery and the various methods used are detailed in Table 1.
Staffing challenges
Many facilities were affected by staff absences due to confirmed or possible COVID-19 infection (Table 2 ). Half (51.1%) reported that 1-10 direct care staff members required time off for this reason, and 2 facilities (1.5%) had more than 50 staff members who required time off. Facilities also experienced staff absences due to elevated risk for severe COVID-19 infection (due to a compromised immune system, advanced age, or pregnancy, for example). More than half (65.0%) had 1-10 direct care staff members who required time off due to elevated risk. A majority of facilities (63.0%) also experienced staff resignations in the midst of the pandemic. Resigning staff most often provided direct patient care, with the greatest proportions of facilities reporting losses among nursing assistants (83.9%) and nurses (64.4%) (Supplementary Fig S1). Absences and illness contributed to staffing shortages at 55.1% of facilities. These shortages were mostly filled by existing staff, whether volunteering to work extra hours (79.0%), nonclinical staff filling new roles (60.5%), or working mandatory extra hours (47.4%) (Table 2). Agency or contracted staff were also utilized in 35.5% of facilities with shortages.
Table 2.
Effects of COVID-19 on staff absences, resignations, and shortages
| Question | N (%) |
| How many of your direct care staff required time off work due to their confirmed or possible COVID-19 infection | |
| None | 22/137 (16.1%) |
| 1-10 | 70/137 (51.1%) |
| > 10 | 45/137 (32.9%) |
| How many of your direct care staff required time off work due to elevated risk of COVID-19 infection? | |
| None | 35/137 (25.6%) |
| 1-10 | 89/137 (65.0%) |
| > 10 | 13/137 (9.5%) |
| Has your facility experienced staff shortages due to absences and illness during the COVID-19 pandemic? | |
| Yes | 76/138 (55.1%) |
| No | 62/138 (44.9%) |
| Who helped with staff shortages? (check all that apply) | |
| Remaining staff volunteered to work extended hours | 60/76 (79.0%) |
| Non-clinical staff filled different roles | 46/76 (60.5%) |
| Remaining staff mandated to work extended hours | 36/76 (47.4%) |
| Agency/contracted staff | 27/76 (35.5%) |
| We didn't get additional help | 2/76 (2.6%) |
| Volunteers from the community | 1/76 (1.3%) |
| Other | 7/76 (9.2%) |
| Has your facility experienced loss of staff (resignations) in the midst of COVID-19? | |
| Yes | 87/138 (63.0%) |
| No | 51/138 (37.0%) |
| Don't know | 0 |
Staff education
Among respondents, 3 quarters (75.2%) provided nursing staff with instruction on appropriate sample collection methods for COVID-19 testing, including swabbing technique and proper PPE worn for the procedure (Supplementary Table S2). Where training was provided, the most common mode of presentation was in-person, including one-on-one sessions (71.7%) and group training (25.3%). Written attestations (24.2%) were used by some facilities. To reinforce PPE education, 89.8% performed random audits with direct feedback to staff; 85.4% repeated education periodically; and 81.8% used a trained staff “observer” to audit and ensure proper use. All facilities provided COVID-19 updates and guidance to employees, with 44.1% providing daily updates. These updates were provided through multiple modes, with written (eg, signage posted in the facility) and verbal (eg, during staff meetings and in one-on-one interactions) modes being most common, used in 87.4% and 82.2% of facilities, respectively. Using open-ended comments, 12 facilities reported use of text/instant message for updates, including via workplace applications.
Testing
During the survey period, most facilities were able to perform some symptom-based testing (Supplementary Fig S2). More than a third (36.0%) were able to test residents and any staff (including nonclinical) with symptoms. However, 42.7% were able to test only residents with symptoms. Nearly half (49.6%) of respondents were able to conduct surveillance testing of asymptomatic residents or staff. A quarter (25.2%) had the resources to perform surveillance testing of all residents and staff, and 24.4% could only conduct surveillance testing of residents.
Communication and therapy adaptations
To adapt to restrictions of visitors and nonessential healthcare personnel, facilities used a variety of alternate modes of communication for visitors and care providers (Table 3 ). To enable communication, 97.8% facilitated phone calls, 96.3% used videoconferencing, and 80.9% allowed window visits. Most (71.1%) facilities used telemedicine visits, which were new to 60.7% of facilities. Facilities have also adapted modes of providing therapy to patients. At the peak of the pandemic, most (90.4%) provided individual physical and occupational therapy in the patient room (Supplementary Table S3). Individual speech therapy was also provided in the patient room at 91.1% of facilities.
Table 3.
Adaptations to restrictions and evaluation of communication with external stakeholders
| Question | N (%) |
| How does your facility address communication between residents and their family/loved ones? | |
| Phone calls | 133/136 (97.8%) |
| Videoconferencing | 131/136 (96.3%) |
| Window visits | 110/136 (80.9%) |
| Other (eg, social media, mail/letters) | 21/136 (15.4%) |
| Does your facility use telemedicine visits? | |
| Yes, and telemedicine was new to our facility with COVID-19 | 82/135 (60.7%) |
| Yes, and telemedicine has been used at our facility in the past | 14/135 (10.4%) |
| No, we do not use telemedicine | 38/135 (28.2%) |
| Don't know | 1/135 (0.7%) |
| Are telemedicine visits by video or telephone? | |
| Video | 41/96 (42.7%) |
| Telephone | 3/96 (3.1%) |
| By both video and telephone | 52/96 (54.2%) |
| How well have your nearby hospitals communicated with your facility on COVID-19? | |
| Communication is very good | 71/136 (52.2%) |
| Communication is fair | 47/136 (34.6%) |
| Communication is poor | 18/136 (13.2%) |
| How well have state and local public health officials communicated with your facility on COVID-19? | |
| Communication is very good | 99/136 (72.8%) |
| Communication is fair | 34/136 (25.0%) |
| Communication is poor | 3/136 (2.2%) |
| How would you describe transfer of a resident with confirmed or possible COVID-19 infection from your facility to the local referral hospital(s)? | |
| Straightforward, uncomplicated, no issues for >90% of transfers | 105/131 (80.2%) |
| Somewhat more difficult to send these residents to the hospital | 19/131 (14.5%) |
| Not at all straightforward, issues with >50% of resident transfers | 7/131 (5.3%) |
| Do you currently have any COVID-19 residents in your facility? | |
| Yes | 47/136 (34.6%) |
| No | 89/136 (65.4%) |
| Does your facility accept NEW residents (not readmits) with confirmed COVID-19 infections? | |
| Yes | 46/136 (33.8%) |
| No | 90/136 (66.2%) |
| Please indicate what has prevented admission to your facility. (check all that apply) | |
| Staffing issues | 23/136 (16.9%) |
| Bed not available | 21/136 (15.4%) |
| Corporate policy not to accept patient | 22/136 (16.2%) |
| Not enough PPE | 20/136 (14.7%) |
| State guidance not to accept patient | 10/136 (7.4%) |
| Other | 38/136 (27.9%) |
| What testing is required before accepting a new resident with unknown COVID status? | |
| One negative COVID test | 47/135 (34.8%) |
| Two negative COVID tests >24 hours apart | 31/135 (23.0%) |
| No testing for COVID required but only accepting asymptomatic patients | 22/135 (16.3%) |
| None, accepting all possible/confirmed COVID patients | 13/135 (9.6%) |
| Other | 22/135 (16.3%) |
| Has your facility created a dedicated COVID unit or wing? | |
| Yes | 105/134 (78.4%) |
| No | 29/134 (21.6%) |
Hospital engagement and admission processes
The perceived quality of engagement with local hospitals varied: 52.2% of facilities rated communication with nearby hospitals as very good; 34.6% rated communication as fair; and 13.2% said communication was poor (Table 3). However, 80.2% reported that transfer of residents with suspected or confirmed COVID-19 to local hospitals was straightforward. Among 7 facilities (5.3%) reporting issues with more than 50% of transfers, 2 respondents indicated in comments that these issues were with emergency medical service (EMS) transport, not the transferring facility.
At the time of the survey, over one third (34.6%) of respondents had patients with COVID-19 in the facility (Table 3). Most (78.4%) facilities had created a dedicated COVID unit or wing, but only 33.8% accepted new (not readmitted) patients with confirmed COVID-19 diagnosis. Conditions preventing new COVID-19 positive admissions included staffing issues (16.9%); lack of available beds (15.4%); corporate policies (16.2%); insufficient PPE (14.7%); and state guidance (7.4%). Among 38 facilities that noted other barriers, 12 (31.6%) indicated their facility was unable to create an isolation unit due to limited beds or lack of single rooms/bathrooms; 5 (13.2%) described a policy not to knowingly introduce SARS-CoV-2 to their facility (having no cases to date); and 3 (7.9%) said that corporate leaders directed any referred COVID-19 positive patients to a sister facility. Additionally, most facilities had procedures in place to reduce the risk of admitting new patients with unknown COVID-19 infection status, although these processes varied significantly: 34.8% required 1 negative COVID-19 test before admission; 23.0% required 2 negative COVID-19 tests more than 24 hours apart; and 16.3% only accepted asymptomatic patients.
Factors influencing patient care during the COVID-19 pandemic
We were particularly interested in predictors that influenced various elements of pandemic planning such as staff education, use of telemedicine, staffing and supply shortages. First, we examined responses reflecting staff education on protocol for COVID-19 testing. While all facilities reported providing PPE education to staff during the pandemic, facilities were more likely to provide staff with education on testing procedures as facility size increased (Supplementary Table S4). Among facilities with less than 50 licensed beds, only half (50.0%) provided their staff with this education, while 87.5% of the largest (>150 beds) facilities provided the education (P = .005). New use of telemedicine was significantly associated with presence of a designated COVID-19 unit in the facility (P = .016). Although new telemedicine use was also more common in facilities with current COVID-19 positive patients, this association was not significant (Supplementary Table S5).
Staffing shortages were significantly associated with presence of current COVID-19 positive patients. Among facilities with a current COVID-19 patient, 78.7% experienced a staffing shortage, compared to 41.6% of facilities without a current COVID-19 patient experiencing a shortage (P < .001, Table 4 ). Individual components of staffing challenges – including requiring time off due to confirmed or possible infection, requiring time off due to elevated risk of severe infection, and resignations – were all significantly associated with current COVID-19 positive patients in the facility (P < .001 for all). Additionally, staff resignations nearly uniformly co-occurred with COVID-19-related staff absences – of 84 facilities that experienced resignations, 80 (95.2%) also lost staffing due to absences. Resignations were experienced at a much higher rate in facilities with COVID-19 positive patients; among facilities with infected patients, 87.0% lost staff compared to 49.4% of facilities without a current case of COVID-19 (P < .001). PPE supply shortages, particularly gown shortages were significantly associated with both overall staff shortages (P = .017) and staff resignations (P = .013) (Supplementary Table S6).
Table 4.
Predictors of staffing shortages and specific types of staff losses
| Predictors of overall staffing shortages | |||
| Staff shortages (any) | |||
| Facility characteristics | Any staff shortages | No staff shortages | P-value |
| Ownership | |||
| For-Profit | 50 (56.2) | 39 (43.8) | .86* |
| Non-Profit/Government | 24 (54.6) | 20 (45.5) | |
| Bed size | |||
| < 50 beds | 10 (41.7) | 14 (58.3) | .072† |
| 51-100 beds | 24 (49.0) | 25 (51.0) | |
| 101-150 beds | 33 (67.4) | 16 (32.7) | |
| > 150 beds | 9 (56.3) | 7 (43.8) | |
| COVID + patients currently | |||
| Yes | 37 (78.7) | 10 (21.3) | <.001* |
| No | 37 (41.6) | 52 (58.4) | |
| COVID unit/wing in facility | |||
| Yes | 55 (52.4) | 50 (47.6) | .35* |
| No | 18 (62.1) | 11 (37.9) | |
| Associations between Presence of COVID-19 Positive Patients and Specific Types of Staff Losses | |||
| COVID+ patients currently at facility | No COVID+ patients currently at facility | P-value | |
| Staff shortage (any) | |||
| No | 10 (21.3) | 52 (58.4) | <.001* |
| Yes | 37 (78.7) | 37 (41.6) | |
| Staff required time off due to confirmed/possible infection | |||
| None | 2 (4.4) | 19 (21.6) | <.001† |
| 1-10 staff members | 18 (39.1) | 52 (59.1) | |
| >10 staff members | 26 (56.5) | 17 (19.3) | |
| Staff required time off due to elevated risk of infection | |||
| None | 5 (10.9) | 29 (32.6) | <.001† |
| 1-10 staff members | 30 (65.2) | 58 (65.2) | |
| >10 staff members | 11 (23.9) | 2 (2.3) | |
| Staffing loss due to resignation | |||
| No | 6 (12.8) | 45 (50.6) | <.001† |
| Yes | 41 (87.2) | 44 (49.4) | |
| Composite staff reduction types | |||
| None | 0 (0.0) | 5 (5.6) | <.001† |
| Staff requiring time off only | 6 (12.8) | 40 (44.9) | |
| Staff resignations‡ | 40 (87.0) | 44 (49.4) |
Significance determined using Pearson's chi2 test.
Significance determined using logistic regression.
Staff resignations are accompanied by staff requiring time off 80/84 instances (95%) for which all data points available.
Discussion
Nursing homes were disproportionately impacted by COVID-19 due to several factors including a vulnerable host, highly contagious virus and a congregate care setting with suboptimal resources devoted to infection prevention. Our previous work just before COVID-19 cases appeared in Michigan NHs showed that a majority of responding facilities had a pandemic preparedness plan, had a designated staff person to lead preparedness efforts, had instituted visitation policies and restrictions but fully anticipated staff and supply shortages.7 In this paper, we discuss the experience of these NHs during the pandemic, their vulnerabilities and opportunities for improvement.
First, NHs received information from a variety of sources which often conflicted with each other.14 Although 99.3% of NHs referred to CDC guidelines, only 51.4% of them reported that this was their primary source. Guidance, particularly during the first 3 months of the pandemic, came from a variety of agencies and changed rapidly and significantly as researchers learned more about transmission dynamics of SARS-CoV-2 as well as the host and the population that was most vulnerable. While NHs relied on CDC, CMS, state and corporate guidance, communications with their local health system were suboptimal – highlighting a possible opportunity for collaboration with NHs and acute care hospitals.15 , 16
Second, two-thirds of facilities faced supply shortages. The most common items in shortage were gowns, alcohol-based hand sanitizer, and N95 respirators. Supply chain issues that affected many settings likely contributed to the lack of gowns, N95 respirators, and other shortages. In anticipation of a hospital surge, NHs were not prioritized in supply distribution.17 In addition to corporate and health department assistance with supply shortages, nearly half (48.4%) of facilities received help from the community in obtaining supplies. Planning efforts and resource allocation have to take into account the population and setting most impacted. Such efforts should be nimble to readjust based on emerging guidance on the transmission and contagiousness of the implicating virus. State and national leadership, taking ethical principles into consideration by maximizing benefits, should drive these discussions about resource allocations.18 , 19
Third, NHs along with all healthcare and community settings faced significant testing challenges. Testing of symptomatic residents and staff and surveillance for asymptomatic infection are key to preventing COVID-19 outbreaks in these facilities.20 The ability of NHs to test symptomatic residents and staff was low. Only 36.0% of facilities at the time of this survey were able to test those with symptoms, and even less were able to perform asymptomatic (surveillance) testing for all residents and staff. Collaborations with local hospitals, their laboratories and local public health officials were crucial in conducting point prevalence surveillance to identify asymptomatic cases and rapidly implementing strategies to curtail outbreaks.15 , 16 , 21 The state of Michigan has now mandated weekly testing of all residents and staff in NHs but public health resources remain limited to support this mandate and guide next steps including identifying laboratories to run tests, receive and log results and institute preventive measures.
Despite NHs experiencing low occupancy rates in the midst of the pandemic, these facilities confronted significant staff shortages and resignations. Nearly 75% of facilities had direct patient care staff who took time off due to confirmed or suspected COVID-19 infection with many remaining staff working extended hours. Several facilities compensated their staff with benefits such as hazard pay and paid accommodations to reduce transmission to their families. Having patients with COVID-19 and supply shortages correlated with staff resignations and can be overcome with adequate stockpiling, support from state public health, local hospitals as well as parent corporations.22 Facilities were prompt in providing education and training to their staff with 80.0% of respondents providing in-person one-on-one training to their frontline staff on PPE use, and 71.7% providing one-on-one training on obtaining nasopharyngeal swabs. A majority of the respondents also provided rapid communications to their staff reflecting their commitment to transparency.
It should be mentioned that selection bias from responding nursing homes may affect findings. As the survey was anonymous, we did not examine characteristics that may have allowed respondents time and/or resources to open and complete the survey. For example, a facility leader may be more apt to participate in the survey if they were fully staffed with low turnover, or they had a higher quality rating. The COVID-19 pandemic has taken an incredible toll on the nation's NHs with mortality being significantly high in these facilities.23 NHs constitute an integral part of the US healthcare system. Adequate resources and dissemination of updated recommendations are critical to provide safe, high-quality care.24 Future planning should focus on strengthening all aspects of infection prevention but particularly having a dedicated full-time infection preventionist (who is provided with adequate resources, training and decision-making authority),25 ensuring that NHs are incorporated in overall disaster preparedness alongside hospitals and other entities,26 having adequate training and resources (including conducting table-top exercises, fit-testing of N-95 respirators and continuous training for evidence-based infection prevention practices such as hand hygiene and PPE use), and developing strategies to improve staffing ratios and retain staff by enhancing their compensation and reducing leadership turnovers.27 To enhance co-ordination efforts regionally, hospitals should incorporate NHs when performing their own tabletop emergency preparedness exercises. Key lessons learned from this survey have led to policy recommendations provided to the state of Michigan.28 Furthermore, the Agency for Health Research and Quality (AHRQ) has funded a large initiative with the Institute for Healthcare Improvement (IHI) using the Project ECHO (Extension for Community Healthcare Outcomes) framework to standardize knowledge for nursing homes across the country.29 NIH has set forth a framework to support research and help reduce inequities for underserved populations that have been disproportionately affected by the disease.30 Future research should evaluate the efficacy and acceptance of these programs in order to manage future outbreaks and pandemics, particularly in vulnerable populations.
Footnotes
Conflicts of interest: The authors declare no potential conflicts of interest.
Funding: This work is supported by the Agency for Healthcare Research & Quality (RO1 HS25451).
Sponsor's role: Study sponsors had no involvement in survey design, data acquisition, data analyses, or manuscript preparation.
Data sharing: Data collected will be made available on request following manuscript publication. Data will be provided for research purposes only, after investigator approval of proposal for data use.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.ajic.2021.03.016.
Appendix. SUPPLEMENTARY MATERIALS
REFERENCES
- 1.COVID 19 Nursing Homes Data. Centers for Medicare and Medicaid Services (online). Available at: https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg Updated November 8, 2020. Accessed November 20, 2020.
- 2.Coronavirus Long Term Care Data. State of Michigan (online). Available at: https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173-526911–,00.html Updated October 11, 2020. Accessed October 13, 2020.
- 3.Wu C, Chen X, Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arentz M, Yim E, Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W, Zheng N, Hu Y. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith PW, Shostrom V, Smith A, Kaufmann M, Mody L. Preparedness for pandemic influenza in nursing homes: a 2-state survey. JAMA. 2008;300:392–394. doi: 10.1001/jama.300.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones KM, Mantey J, Mills JP. COVID-19 preparedness in Michigan Nursing Homes. J Am Geriatr Soc. 2020;68:937–939. doi: 10.1111/jgs.16490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cumulative Confirmed Cases and Deaths among Confirmed Cases. State of Michigan (online). Available at: https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173—,00.html Updated December 19, 2020. Accessed December 20, 2020.
- 9.Doernberg S, Tran TTT, Tong S. Good studies evaluate the disease while great studies evaluate the patient: development and application of a desirability of outcome ranking endpoint for Staphylococcus aureus bloodstream infection. Clin Infect Dis. 2019;68:1691–1698. doi: 10.1093/cid/ciy766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doernberg S, Abbo L, Burdette S. Essential resources and strategies for antibiotic stewardship programs in the acute care setting. Clin Infect Dis. 2018;67:1168–1174. doi: 10.1093/cid/ciy255. [DOI] [PubMed] [Google Scholar]
- 11.Budak J, Sears D, Wood B. HIV training pathways in residency: a national survey of curricula and outcomes. Clin Infect Dis. 2021;72:1623–1626. doi: 10.1093/cid/ciaa301. [DOI] [PubMed] [Google Scholar]
- 12.Melber D, Teherani A, Schwartz B. A comprehensive survey of preclinical microbiology curricula among US medical schools. Clin Infect Dis. 2016;63:164–168. doi: 10.1093/cid/ciw262. [DOI] [PubMed] [Google Scholar]
- 13.Carey N, Alkahamees N, Cox A, Sund-Levander M, Tingstrom P, Mold F. Exploring views and experiences of how infections are detected and managed in practice by nurses, care workers and manager's in nursing homes in England and Sweden: a survey protocol. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-038390. e038390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic. JAMDA. 2021;22:199–203. doi: 10.1016/j.jamda.2020.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mody L, Washer L, Flanders S. Can infection prevention programs in hospitals and nursing facilities be integrated? From silos to partners. JAMA. 2018;319:1089–1090. doi: 10.1001/jama.2018.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montoya A, Jenq G, Mills JP. Partnering with local hospitals and public health to manage COVID-19 outbreaks in nursing homes. J Am Geriatr Soc. 2021;69:30–36. doi: 10.1111/jgs.16869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGarry B, Grabowski D, Barnett M. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic. Health Affairs. 2020;39:1812–1821. doi: 10.1377/hlthaff.2020.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frank L, Concannon TW, Patel K. RAND Corporation; Santa Monica, CA: 2020. Health Care Resource Allocation Decision making During a Pandemic.https://www.rand.org/pubs/research_reports/RRA326-1.html (online). Available at: Accessed December 19, 2020. [Google Scholar]
- 19.Emanuel EJ, Persad G, Upshur R. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 20.Arons MM, Hatfield KM, Reddy SC. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stall NM, Farquharson C, Fan-Lun C. A hospital partnership with a nursing home experiencing a COVID-19 outbreak: description of a multiphase emergency response in Toronto, Canada. J Am Geriatr Soc. 2020;68:1376–1381. doi: 10.1111/jgs.16625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu H, Intrator O, Bowblis JR. Shortages of staff in nursing homes during the COVID-19 pandemic: what are the driving factors? JAMDA. 2020;21:1371–1377. doi: 10.1016/j.jamda.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMichael TMC, Currie DW, Clark S. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes (REVISED). Centers for Medicare & Medicaid Services (online). Available at: https://www.cms.gov/files/document/qso-20-14-nh-revised.pdf Updated September 28, 2020. Accessed October 13, 2020.
- 25.Preparing for COVID-19: Long-term care Facilities, Nursing Homes. Centers for Disease Control and Prevention (online). Available at: https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/prevent-spread-in-long-term-care-facilities.html Updated November 20, 2020. Accessed December 20, 2020.
- 26.Siu HYH, Kristof L, Elston D, Hafid A, Mather F. A cross-sectional survey assessing the preparedness of the long-term care sector to respond to the COVID-19 pandemic in Ontario. Canada. BMC Geriatrics. 2020;20:241. doi: 10.1186/s12877-020-01828-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mills JP, Kaye KS, Mody L. COVID-19 in older adults: clinical, psychosocial, and public health considerations. JCI Insight. 2020;5 doi: 10.1172/jci.insight.139292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keeping Nursing Home Residents Safe and Advancing Health in Light of COVID-19: Analysis and Recommendations for the State of Michigan. Center for Health and Research Transformation, Ann Arbor, MI. Available at: https://www.michigan.gov/documents/coronavirus/KeepingNursingHomeResidentsSafe_SummaryReport_9-8-2020_1_702212_7.pdf Accessed November 20, 2020.
- 29.AHRQ Establishes National Nursing Home COVID Action Network. Agency for Healthcare Research and Quality, Rockville, MD. Available at: https://www.ahrq.gov/news/newsroom/press-releases/covid-action-network.html Accessed November 20, 2020.
- 30.Tromberg BJ, Schwetz TA, Peres-Stable EJ. Rapid scaling up of Covid-19 diagnostic testing in the United States – the NIH RADx initiative. N Engl J Med. 2020;383:1071–1077. doi: 10.1056/NEJMsr2022263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.