Abstract
Cancers are serious life-threatening diseases which annually are responsible for millions of deaths across the world. Despite many developments in therapeutic approaches for affected individuals, the rate of morbidity and mortality is high. The survival rate and life quality of cancer patients is still low. In addition, the poor prognosis of patients and side effects of the present treatments underscores that finding novel and effective complementary and alternative therapies is a critical issue. Melatonin is a powerful anticancer agent and its efficiency has been widely documented up to now. Melatonin applies its anticancer abilities through affecting various mechanisms including angiogenesis, apoptosis, autophagy, endoplasmic reticulum stress and oxidative stress. Regarding the implication of mentioned cellular processes in cancer pathogenesis, we aimed to further evaluate the anticancer effects of melatonin via these mechanisms.
Keywords: Melatonin, Cancer, Angiogenesis, Apoptosis, Autophagy, Endoplasmic reticulum stress, Oxidative stress, Inflammation
Introduction
As the second cause of mortality worldwide, new cases of cancer have recently been reported to increase by 2025 (approximately 19.3 million annually) [1]. Cancer growth control, complete eradication and preventing its incidence are main purposes for cancer-associated investigations. Chemotherapy, radiotherapy and surgery are the major conventional anticancer treatments. The restricted efficiency of these treatments as well as their dangerous side effects have forced researchers to find novel effective anticancer therapies based on herbal extracts and natural compounds as single or combined therapies [2–4].
Melatonin, a multifunctional pleiotropic neurohormone secreted by the pineal gland and other organs including bone marrow, retina, and skin. It is an immune regulatory agent and powerful antioxidant with a capability of preventing cell death in oxidative stress situations. [5, 6]. Moreover, melatonin interrupts cell death mechanisms, inflammation, and redox activity probably resulting in cancer cells sensitization to chemotherapy and radiation [7].
Furthermore, in addition to diverse therapeutic potentials for several diseases [8, 9], melatonin has been shown to possess anticancer abilities against skin cancer [10], glioma [11], lung cancer [12], gastrointestinal cancers [13], gynecological cancers [14, 15], and hematological cancers [16, 17]. Although mechanistic impacts of melatonin on various cancers have been widely demonstrated, in the present review we discuss anticancer effects of melatonin with focusing on molecular pathways including angiogenesis, apoptosis, autophagy, endoplasmic reticulum stress, and oxidative stress.
Melatonin, a neurohormone with a broad spectrum functions
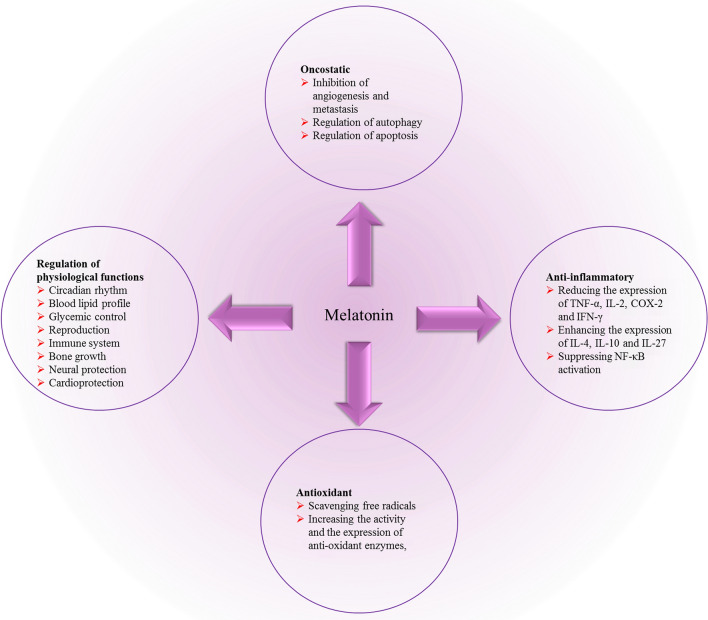
Monitoring of circadian rhythm is one of the several properties of melatonin, which also possesses oncostatic, vasoregulation, antioxidant, anti-inflammatory, and immunomodulatory abilities [18, 19]. It has been demonstrated that the normally enhanced melatonin levels at night help in the organization of homeostatic metabolic rhythms of targeted organs and systems [20]. Of note, disruption of circadian rhythm has been shown as one of the contributing factors in cancer progression and development [21].
Melatonin, as an antioxidant agent, scavenges free radicals. Melatonin has protective effects on neurodegenerative disorders, epilepsy, and cancer through inhibiting oxidative stress in vitro and in vivo [22, 23]. Melatonin increases the activity and expression of enzymes, including catalase, superoxide dismutase and glutathione peroxidase, implicated in antioxidant abilities [24, 25]. Melatonin also has anti-inflammatory impacts and attenuates pathogenic inflammation through modulating different pathways, including reducing the secretion of tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-2) and interferon-gamma (IFN-γ), and enhancing the amounts of IL-4, IL-10 and IL-27. Melatonin alleviates pro-inflammatory cytokines secretion via suppressing nuclear factor kappa B (NF-κB) [26–28]. In addition, in neurodegenerative disorders, melatonin blocks cyclooxygenase-2 (COX-2) expression, a pro-inflammatory mediator [29]. Melatonin inhibits apoptosis through regulating Bax/Bcl2 and decreasing caspase-3 activity and expression, proposing that melatonin modulates apoptotic functions in the protection against malignancy and neurodegenerative disorders [30–32].
Melatonin regulates multiple physiological and neural functions (Fig. 1). Among of them, effects on blood lipid profile, glycemic control, gestation, reproduction, and fetal development, neural protection, immune system, and cardiovascular system have been widely documented [33, 34]. Melatonin prevents the growth and promotion of spontaneous and chemically mediated breast tumors [35, 36]. Moreover, at physiological concentrations, melatonin suppresses cell invasiveness and proliferation in breast cancer cells [37].
Fig. 1.
Melatonin with a broad spectrum functions
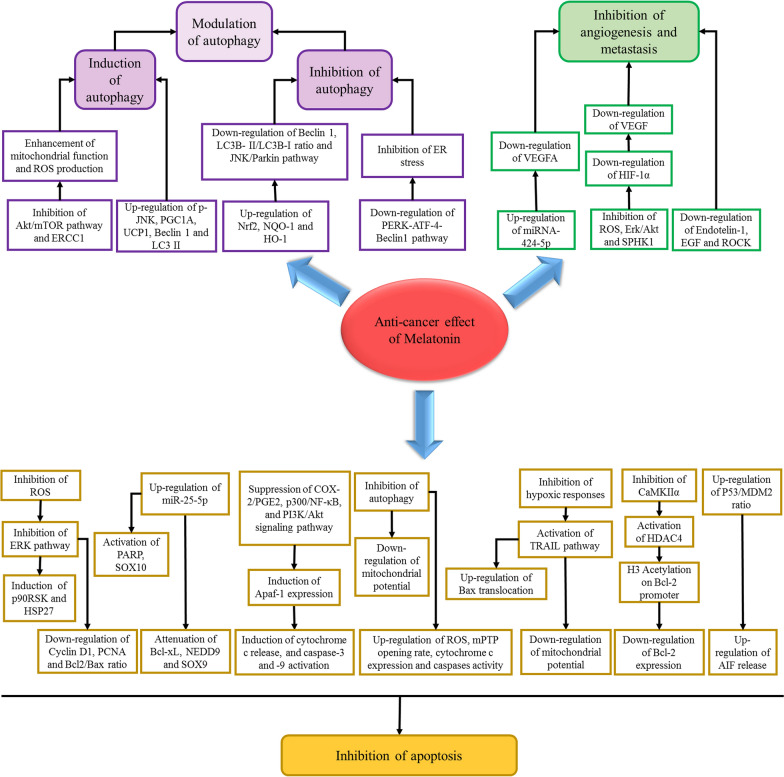
Melatonin and cancer: effect on different molecular mechanisms and cellular pathways
In this section we describe the effect of melatonin on oxidative stress and endoplasmic reticulum stress, and various signaling pathways including angiogenesis, apoptosis, autophagy affected by melatonin in different cancer cells (Fig. 2).
Fig. 2.
Effects of melatonin on various molecular mechanisms and cellular pathways
Melatonin and angiogenesis
Angiogenesis is a crucial event implicated in the progression of tumor as well as its metastasis [38]. Hypoxia in the central areas of solid tumor is a leading cause of angiogenesis via activation of angiogenic mediators [38, 39]. Vascular endothelial growth factor (VEGF), the specific mitogen of endothelial cells and the most active pro-angiogenic agent, is a powerful angiogenesis enhancer which increases vascular permeability. Numerous data suggest that, in tumor development, anti-VEGF therapy has important roles in the suppression of tumor cell growth, leading to a considerable amelioration in progression-free survival [40]. Hypoxia-inducible factor-1 (HIF-1) is another key factor in angiogenesis, which modulates hypoxia-activated genes transcription and consists of HIF-1α and HIF-1β heterodimer. The α subunit of HIF-1 is stabilized under hypoxia and degraded under normoxic situations, however, HIF-1β is expressed constitutively [41].
Melatonin has been shown to have regulatory role in angiogenesis process [42]. In other words, melatonin possesses various impacts on neovascularization under diverse pathological and physiological situations. In skin lesions, gastric ulcers, and some physiologic events, melatonin promotes angiogenesis, while in a hypoxic environment, in age-related ocular diseases, and in tumors melatonin suppresses neovascularization in tissues [43].
Melatonin exerts its antitumor potentials via inhibiting HIF-1-induced angiogenesis [44]. Furthermore, melatonin inhibits the accumulation of HIF-1α through suppressing the formation of ROS and the sphingosine kinase 1 (SPHK1) pathway in prostate cancer cells under hypoxic conditions [45]. Melatonin plays an important role in the paracrine interaction between proximal endothelial cells and malignant epithelial cells by a downmodulatory effect on the expression of VEGF in breast tumor cells, which reduces VEGF levels around endothelial cells [46].
Of note, anti-angiogenic potential of melatonin is a key factor resulting in the inhibition of proliferation of cancer cells, as demonstrated in various investigations. For instance, melatonin attenuates proliferation of prostate cancer cells triggered by epidermal growth factor [47]. Melatonin also hampers vasculogenic mimicry of oral cancer cells via inhibition of ROS-activated Akt and ERKs signaling pathway implicating the HIF-α pathway [48]. Melatonin up-regulates TGF-β1 expression in tumor tissues during the inhibition of gastric cancer tumor growth process [49]. Furthermore, apoptotic and anti-proliferative effects of melatonin on breast cancer cells are mediated by the simultaneous activation of the Apaf-1/caspase-dependent apoptotic pathway and the inhibition of PI3K/Akt, p300/NF-κB, and COX-2/PGE2 signaling pathways [32].
Endothelin-1 is a peptide acting as a survival factor in colon cancer, promoting angiogenesis and mediating cell proliferation. Melatonin suppresses endothelin-1 mRNA expression. Also, melatonin blocks the activity of endothelin-1 promoter modulated by NF-κβ and FoxO1 [50]. Melatonin represses ROCK-1, VEGF and HIF-1α genes expressions in oral cancer [51]. Melatonin alters the expression of inflammatory and angiogenic proteins in both co-culture and monoculture of cancer cells and cancer-associated fibroblasts [52]. Melatonin suppresses tumor angiogenesis and the growth of gastric cancer cells in tumor-bearing nude mice. Moreover, melatonin decreases the expression of VEGF and HIF-1α at translational and transcriptional levels within gastric cancer cells during tumorigenesis [53]. Reduced serum levels of VEGF have been reported in cancer subjects treated with melatonin [54]. Vimalraj et al. [55] showed that melatonin upregulates miR-424-5p expression in osteosarcoma cells suppressing VEGFA. Furthermore, it inhibits tumor angiogenesis, regulating surrounding endothelial cells migration and proliferation, and angiogenic growth factors and the morphology of blood vessels E (Table 1).
Table 1.
Melatonin fights against different cancers trough angiogenesis modulation
| Type of malignancy | Melatonin dose/concentration | Angiogenesis-related targets | Key findings | Model | Cell line | Refs. |
|---|---|---|---|---|---|---|
| Breast cancer | 1 mM | VEGF, ANG-1, ANG-2 | Downregulated angiopoietins with a decrease in VEGF | In vitro | MCF-7 | [125] |
| Dalton's lymphoma | 1 and 5 mM | VEGF, FGF, TIMP3 | Decreased the Dalton’s lymphoma ascites–mediated angiogenesis | In vivo, in vitro | A549 and SiHa | [126] |
|
serous papillary ovarian cancer |
200 µg/100 g b.w | VEGF, HIF-1α | Significantly decreased angiogenesis-associated markers, ovarian cancer size and microvessel density | In vivo | - | [127] |
| canine mammary tumor cells | 1 mM | VEGF |
Decreased cell viability, enhanced caspase-3 cleaved and proteins implicated in the apoptotic pathway and diminished pro-angiogenic VEGFA |
In vitro | CF-41, CMT-U229 | [128] |
| Neuroblastoma | 1 mM or 1 nM | VEGF | Inhibited proliferation and migration of cancer cells | In vitro | SH-SY5Y | [129] |
| Gastric cancer |
3 mM 100, 150 mg/kg |
VEGF, HIF-1α, RZR/RORγ, SENP1 |
Suppressed gastric cancer growth and blockaded tumor angiogenesis Decreased the expression of melatonin nuclear receptor RZR/RORγ |
In vitro, in vivo | SGC-7901 | [130] |
| Breast cancer | 1 mM | - |
Regulated inflammation Decreased cancer cell viability and cancer associated fibroblasts |
In vitro | MDA-MB-231 | [52] |
| Breast cancer | 1 mM | HIF-1α, VEGF, EGFR, angiogenin, | Reduced protein and gene expression of angiogenesis markers and also decreased cancer cell viability | In vitro | MCF-7, MDA-MB-231 | [131] |
| Breast cancer | 10 mg/kg | VEGF | The combination of melatonin and P. acnes cured forty percent of treated mice, suppressed metastasisand decreased angiogenesis and mediated apoptosis | In vivo | EMT6/P | [132] |
| Prostate cancer | 1 mM | HIF-1α, VEGF | Upregulationn of miRNA374b and miRNA3195 mediated melatonin-induced anti-angiogenic properties | In vitro | PC-3 | [133] |
| Oral cancer | 1 mM | HIF-1α, VEGF | Decreased cancer cell viability, inhibited metastasis and angiogenesis | In vitro | SCC9, SCC25 | [51] |
| Hepatocellular carcinoma | 1 mM | VEGF, HIF-1α, STAT3 | Melatonin exerted its anti-angiogenic effects through interfering with the transcriptional activation of mentioned markers | In vitro | HepG2 | [134] |
| Breast cancer | 1 mM | VEGF | Inhibited stimulatory impacts on the proliferation of human umbilical vein endothelial cells (HUVECs) as well as VEGF protein levels | In vitro | MCF-7 | [46] |
| Renal cancer |
20 mg/kg 10 µM |
HIF-1α | Inhibited tumor growth, blocked tumor angiogenesis and diminished HIF-1α protein expression within the tumor mass during tumorigenesis | In vivo, in vivo | RENCA | [135] |
| Breast cancer |
1 mM 40 mg/kg |
VEGFR2, micro-vessel density (MVD) | Inhibited tumor growth and proliferation | In vivo, in vitro | MDA-MB-231 | [136] |
| Colon cancer | 1 mM | VEGF, HIF-1α | Suppressed invasion and migration | In vitro | HCT116 | [44] |
| Breast cancer |
40 mg 0.001 mM, 0.01 mM, 0.1 mM and 1 mM |
VEGF, IGF-IR, HIF-1α | Increased miR-152-3p expression leading to suppress breast cancer | In vitro | MDA-MB-468 | [137] |
| Breast cancer | - | IGF-1R, VEGF |
Inhibited survival, migration and invasion of breast cancer cells Increased the gene level of miR-148a-3p |
In vivo, in vitro | MDA-MB-231 | [138] |
| Advanced cancer patients (CRC, HCC, RCC, NSCLC) | 20 mg | VEGF | Controlled tumor growth by anti-angiogenic roles | Human | - | [54] |
Melatonin and oxidative stress
In normal cellular condition, there is a balance between the production of oxidants, so called reactive oxygen species (ROS), and their neutralizing compounds, named antioxidants. The state of excess ROS, in which the oxidant content of the cells dominates the neutralizing capacity of antioxidants, is defined as oxidative stress [56, 57]. Sustained oxidative stress increases the risk of cancer development either through inducing mutagenesis or by promoting the expression of proto-oncogenes such as cyclin D1. It also plays a signaling role in the activation of several genes involved in the cancer progression including the mitogen-activated protein kinase (MAPK), extracellular signal-regulated kinase (ERK) and JUN N-terminal kinase (JNK) [58, 59].
Melatonin role as a natural ally against oxidative stress has been revealed in many in vitro and in vivo studies. Detoxification of oxidants by melatonin is triggered by several direct or indirect mechanisms. In direct scenario, melatonin neutralizes the oxidants by its nonreceptor‐mediated free radical scavenging capacity. As indirect scenario, melatonin reduces the oxidative content through several mechanisms such as activating anti-oxidative enzymes and suppressing pro‐oxidative enzymes. It also stabilizes the mitochondrial inner membrane, thereby maintaining mitochondrial integrity leading to a reduced electron leakage and ROS generation [60, 61].
The inducing role of oxidative stress in cancer progression and preventive role of melatonin in the production and function of oxidants indicated a possible oncostatic property for melatonin [62]. Subsequently, it was revealed that melatonin reduces the oxidative damage to cellular components under conditions where toxic oxygen derivatives are acknowledged to be released [63, 64]. Moreover, in vitro studies demonstrated that melatonin treatment reduces the amount of oxidative contents in a variety of cancer cells, which was further supported by in vivo studies (Table 2).
Table 2.
Melatonin acts as an antioxidant in cancer models
| Cancer | Melatonin dose/concentration | Key findings | Model | Cell line/animal | Refs. |
|---|---|---|---|---|---|
| Breast cancer |
1 μM 5, 10, 50 mg/kg |
Limited paclitaxel-mediated mitochondrial dysfunction and protected against paclitaxel-mediated neuropathic pain | In vitro, in vivo |
MCF-7 Male and female Sprague Dawley rats |
[198] |
| Neuroblastoma | 10 μM | Reduced oxaliplatin-induced neurotoxicity | In vitro | SH-SY5Y | [199] |
| Breast cancer | 0.3 mM | Supported doxorubicin effects by apoptosis and TRPV1activation, and through mediating cancer cell death | In vitro | MCF-7 | [200] |
| Cervical cancer | 1 mM | Enhanced cisplatin-mediated cytotoxicity and apoptosis | In vitro | HeLa | [163] |
| Lung cancer | 1 nm, 1 μm, 1 mm | Exerted immunomodulatory effects | In vitro | SK‐LU‐1 | [201] |
| Pancreatic cancer | 26.8 mg | capecitabine and melatonin provided an amelioration in antioxidant status and synergistic antitumoral effects | In vivo | Male Syrian hamsters | [202] |
| Leukemia | 1 mM | Protected healthy cells from chemotherapy-mediated ROS production and induced tumor cell death | In vitro | HL-60 | [180] |
| Hepatocellular carcinoma | 1, 100 μM | The responses of angiogenic chemokine genes to melatonin were determined by the characteristics of cancer cells | In vitro | HCC24/KMUH, | [203] |
| Pancreatic cancer | 53.76 mg | Exerted more potent beneficial effects than celecoxib on the decrease in tumor nodules, oxidative stress and death | In vivo | Male Syrian hamsters | [204] |
| Breast cancer | 2.5 mg/kg | Antioxidant effects | In vivo | Female Sprague Dawley rats | [205] |
| Pancreatic cancer | 26.88, 53.76 mg | Decreased oxidative damage and cancer nodules mediated by BOP in the pancreas | In vivo | Male Syrian hamsters | [206] |
| Cervical cancer | 10–1000 μM | This study showed melatonin effects on radiotherapy is dose-dependent | In vitro | HeLa | [207] |
| Hepatocellular carcinoma | 20 mg/kg | Fostered the survival and therapeutic potential of MSCs in HCC, by inhibition of oxidative stress and inflammation as well as apoptosis induction | In vivo | Adult female rats | [120] |
| Cervical cancer | 10 μM | Enhanced TNF-α-mediated cervical cancer cells mitochondrial apoptosis | In vitro | HeLa | [14] |
| Bladder cancer |
1 mM 100 mg/kg |
Inhibited the growth, migration, and invasion of cancer cells | In vivo, in vitro |
HT1197, HT1376, T24, RT4 Male C57B/L6 mice |
[208] |
| Lung cancer | 0.25–2.5 mM | Enhanced palladium-nanoparticle-induced cytotoxicity and apoptosis | In vitro | A549, H1299 | [209] |
| Lymphoma, cervical cancer, hepatoblastoma, gastric cancer, breast, colon and lung adenocarcinoma, | 0–2 mM | Sensitizees shikonin-mediated cancer cell death induced by oxidative stress | In vitro | U937, HeLa, Hep-G2, AGS, MCF-7, SW480, A549 | [210] |
Melatonin and endoplasmic reticulum stress
Endoplasmic reticulum (ER) is an entry site for secretory proteins and most integral membrane proteins for proper folding and covalent modifications to assemble into a functional complex. In addition to the processing of proteins, ER is involved in various cellular functions including lipid synthesis, fatty acid turnover, detoxification, Ca2+ homeostasis. The ER network extends into all cell compartments to sense intrinsic and extrinsic perturbations and integrate the stress signals for maintenance of cellular homeostasis to preserve proper cellular and organismal function [65, 66]. However, the ER function can be impacted and disturbed by a multitude of exogenous and endogenous factors, leading to the accumulation of mis/unfolded proteins in the ER. This causes the imbalance between the client proteins load in the lumen of ER and the folding capacity of this organelle leading to the failure of the ER to cope with unusual high protein folding load, which is termed 'ER stress' [67]. To restore protein homeostasis, an adaptive signal transduction pathway called the unfolded protein response (UPR) is activated to induce compensatory responses to stressors for recovering normal ER function [68]. Signaling proteins sensing UPR include inositol-requiring protein-1α (IRE1α), activating transcription factor 6α (ATF6α) and protein kinase RNA (PKR)-like ER kinase (PERK). In nonstressed cells, UPR stress sensors are maintained in an inactive state through direct binding to the ER chaperone proteins, Bip (78-kDa glucose regulated protein, GRP78). Upon ER stress, aggregation of misfolded proteins leads to the dissociation of UPR sensors from Bip, which causes activation of UPR signals [69]. Although activation of UPR signaling pathways is a cellular strategy to increase survival, this pathway will instead activate cell death signaling pathways when the intensity or duration of cellular stress increases. Therefore, certain anti-cancer patterns may activate ER stress/UPR pathway to induce apoptosis in cancer cells [70].
Melatonin induces mitochondria-mediated apoptosis in colorectal cancer cells through reducing the expression of PrPC and PINK1 resulting in the enhancement of superoxide production and induction of ER stress [71]. Melatonin also ameliorates ER-stress mediated insulin resistance. ER stress induces autophagy in pancreatic β cells, which this pathway plays an important role in insulin production and secretion. In the glucose analog 2-DG-treated rat insulinoma INS-1E cells, melatonin reduces insulin production via ER stress-induced autophagy [72]. Combination of melatonin with ER stress inducer tunicamycin increases the sensitivity of cancer cells to apoptosis through inhibiting the expression of COX-2 and increasing the Bax/Bcl-2 ratio and CHOP levels [73]. Selective inhibition of ATF-6 by melatonin results in the suppression of COX-2 production and enhancement of cancer cells to ER-stress induced apoptosis [74].
Melatonin increases apoptosis through enhancing caspase-3, -8 and -9 activities, Bax/Bcl-2 ratio, PARP cleavage and cytochrome c, p53 and Fas-L proteins concentrations in hepatocellular carcinoma, which this effect is mediated by the elevation of ER stress characterized by up-regulation of ATF6, CHOP and Bip [75]. Furthermore, melatonin increases the sensitivity of hepatocellular carcinoma cells to sorafenib through targeting the PERK-ATF4-Beclin1 pathway [76]. The same results have been reported in gastric cancer; melatonin inhibits cell proliferation through inducing activation of the IRE/JNK/Beclin1 signaling [77].
Melatonin in combination with the ER stressor thapsigargin increases the expression level of nuclear mammalian RNA-binding protein (HuD) resulting in the reduction of intracellular biosynthesis of insulin. Suppression of AKT/PI3K pathway and induction of nuclear mTOR (Ser2481, Ser2448) expressions by melatonin sensitizes rat insulinoma INS-1E cells to insulin through increasing the expression of insulin receptor substrate [78]. In contrast with these reports, melatonin has been reported to inhibit tunicamycin-induced ER stress in human hepatocellular carcinoma cells and increase the response of these cells to cytotoxic effects of doxorubicin; this is accompanied by inhibition of the PI3K/AKT pathway, elevation of CHOP and reduction of Survivin [79]. These evidences suggest that melatonin could improve the toxic effect of anti-cancer agents on cancer cells through regulating ER stress in cells (Table 3).
Table 3.
Melatonin suppressive effects on various cancers via regulation of ER stress
| Cancer | Melatonin dose/concentration | Effect on ER stress | Key findings | Model | Cell line/animal | Refs. |
|---|---|---|---|---|---|---|
| Gastric cancer |
1, 2, 3 mM 50 mg/kg |
Activate | Melatonin-mediated inhibition of cancer cell proliferation is induced by the IRE/JNK/Beclin1 signaling activation | In vitro, in vivo |
AGS, SGC-7901 cells Male BALB/c nude mice |
[77] |
| Lung, liver and cervical cancer | 2 mM | Activate | Induced apoptosis by ROS generation and JNK activation | In vitro | HepG2, A549, HeLa | [211] |
| Hepatocellular carcinoma | 10–5 M | - | enhanced HCC sensitivity to sorafenib through suppressing autophagy | In vitro | HepG2, 7721, Huh7, LO2 | [76] |
| Colorectal cancer | 0–1 mM | Activate | Induced mitochondria-induced cellular apoptosis | In vitro |
SNUC5/ WT |
[71] |
| Hepatoma | 10–7-10–3 mM | - | Melatonin was shown as a novel selective ATF-6 inhibitor that can sensitize human hepatoma cells to ER stress inducing apoptosis | In vitro | HepG2 | [74] |
| Insulinoma | 100 μM | Activate | Melatonin-induced insulin synthesis involved autophagy and EDC3 protein in rat insulinoma cells and subsequently resulted in a resuction in intracellular production of insulin | In vitro | INS-1E | [72] |
| Hepatocellular carcinoma | 1 mg/kg/d | Activate | Activated ER stress and apoptosis | In vivo | Male Wistar rats | [75] |
| Insulinoma | 10, 50 μM | - |
Decreased nuclear and cellular expressions of p85α Decreased cellular expression of HuD and led to a reduction in cellular insulin level and rise in insulin secretion |
In vitro | INS-1E | [78] |
| Hepatocellular carcinoma | 10–3 M | Inhibit | Attenuated ER stress-mediated resistance to doxorubicin by downregulating the PI3K/AKT pathway, enhancing CHOP levels and reducing Survivin levels | In vitro | HepG2, SMMC-7721 | [79] |
| Hepatoma | 10–9, 10–7, 10–5, 10–3 μM | Activate | Sensitized cancer cells to ER stress-mediated apoptosis by downregulating COX-2 expression, enhancing the levels of CHOP and reducing the Bcl-2/Bax ratio | In vitro | HepG2, HL-7702 | [73] |
Melatonin and autophagy
Autophagy is a complicated process maintaining intracellular homeostasis by eliminating degraded proteins and organelles during cellular stress. Autophagy is principally considered as a pro-survival process, but, excessive or inappropriate autophagy contributes to the cell death, a process known as autophagic cell death or type II programmed cell death [80].
Autophagy is a complicated process, which consists of five sequential steps, including: (a) initiation complex formation and double-membrane phagophore (nucleation) maturation; (b) membrane elongation and autophagosome formation sequestering cargo; (c) fusion with lysosome; (d) inner membrane disruption leading to degradation of cargo by hydrolases; and (e) macromolecular component utilization [81]. These steps of the autophagy pathway are regulated by more than 35 autophagy related genes (ATGs) and proteins most of which function in complexes. The initiation phase is regulated by Unc-51-like kinase1 (mammalian homologues of Atg1, ULK1)–Atg13–Atg101–FIP200 (mammalian homologues of Atg17) protein complex. Unc-51-like kinase1 phosphorylates and activates Beclin-1 (mammalian homologue of Atg6). Beclin-1 is a part of multiprotein-complex, class III PI3-kinase Vps34–p150 (mammalian homolog of Vps15)–Atg14-like protein (Atg14L)–Beclin-1, promoting nucleation [81–83]. The elongation phase is regulated by two ubiquitin-like conjugation systems, Atg12 and LC3 (mammalian homologue of Atg8). In the first conjugation system, Atg12 is activated by Atg7 (E1-like enzyme), transferred to Atg10 (E2-like enzyme) and conjugated to Atg5. The Atg12–Atg5 conjugates further couples with Atg16 (Atg16L in mammals) to form the E3-like complex. In the LC3 conjugation system, LC3 is cleaved by a cysteine protease, Atg4, forming LC3-I. Thereafter, LC3-I is activated by Atg7 (E1-like enzyme), transferred to Atg3 (E1-like enzyme) and conjugated to phosphatidylethanolamine (PE) to form LC3-II; this process is facilitated by the E3-like complex. This lipidated form of LC3, LC3-II, is recruited to the autophagosome membrane. Finally, the Atg9 dependent pathway promotes autophagosome membrane expansion [81–83].
Cargo sequestration can be selective or non-selective; the selectivity is based on autophagy receptors such as P62/SQSTM1, NBR1, NDP52, NIX/BNIP3L, BNIP3 and FUNDC1 [82]. Fusion of autophagosome with lysosome is the next step. The inner vesicle is degraded by lysosomal hydrolases, including cathepsin B, D (a homolog of proteinase A), and L. The degradation products are released to the cytosol and used in different anabolic pathways [84]. ER stress-induced activation of UPR pathways promotes induction of autophagy [85]. Activated PERK/ATF4 pathway up-regulates the expression of ATG genes including ATG5, ATG7, and ATG10 [86]. The conversion of LC3-I conversion to LC3-II is also induced by PERK pathway [87]. Activation of IRE1α pathway induces the expression of Beclin1 and the phosphorylation of Bcl-2 by JNK, which subsequently results in the Bcl-2–Beclin 1 dissociation [88–90]. The release of Ca2+ from ER to cytosol triggers autophagy pathway through activating several mechanisms including (I) inhibition of mTOR by Ca2+/calmodulin dependent kinase kinase-β-mediated activation of AMP-activated protein kinase (AMPK) [91], and (II) dissociation of Bcl-2–Beclin 1 by inducing death-associated protein kinase (DAPK) 3-mediated Beclin 1 phosphorylation [92].
Melatonin has a modulatory effect on autophagy in various cell types and different conditions. Melatonin indirectly modulates autophagy through affecting oxidative stress, ER stress and inflammation [69]. Melatonin enhances the effectiveness of cisplatin and radiotherapy in head and neck squamous cell carcinoma, which this effect is mediated by the excessive activation of mitochondria leading to the over-production of ROS and subsequent induction of autophagy and apoptosis [93]. Melatonin also increases cytotoxic effects of rapamycin in cancer cells. Combination of rapamycin and melatonin suppresses AKT/mTOR pathway activation, which this effect leads to the enhancement of mitochondrial function and ROS production resulting in the induction of apoptosis and mitophagy [94]. Melatonin induces autophagy in clear cell renal cell carcinoma through activating transcriptional coactivator peroxisome proliferator-activated receptor gamma coactivator 1A (PGC1A) and uncoupling protein 1 (UCP1); this is associated with the elimination of lipid deposits without generating ATP, which subsequently leads to the tumor size reduction [95].
Melatonin reduces the viability liver cancer cells through transient induction autophagy by up-regulating JNK phosphorylation. However, ATG5 silencing sensitizes cancer cells to melatonin-induced apoptosis. This suggests that modulation of autophagy by melatonin has dual effect on cell death [96]. Similarly, disruption of autophagy sensitizes glioblastoma cells and tongue squamous cell carcinoma to melatonin-induced apoptosis [97]. Melatonin-induced autophagy is suggested to be mediated by activation of melatonin membrane receptor in tongue squamous cell carcinoma and suppression of melatonin membrane receptor-dependent autophagy may be strategy for treatment of tongue squamous cell carcinoma [98].
Several studies indicate that melatonin may induce apoptosis in cancer cells through inhibiting autophagy pathway. Melatonin down-regulates Beclin-1 and p62 expressions and LC3B-II/LC3B-I ratio in colitis-associated colon carcinogenesis in mice; this effect is associated with the increased level of Nrf2 and its downstream antioxidant enzymes including NAD(P)H:quinone oxidoreductase (NQO-1) and heme oxygenase-1 (HO-1). These suggest that the ameliorative effect of melatonin on inflammation and oxidative stress results in the reduction of autophagy [99]. Induction of ER stress is associated with the activation of autophagy in sorafenib-treated hepatocellular carcinoma cells, which this contributes to the resistance of cancer cells to apoptosis. Combination of melatonin with sorafenib inhibits ER stress-related autophagy through suppressing the PERK-ATF4-Beclin1 pathway leading to the sensitivity of hepatocellular carcinoma cells to sorafenib [76]. Co-stimulation of cancer cells with cisplatin and melatonin induce apoptosis in HeLa cells, which this effect is accompanied by inactivating mitophagy via blockade of JNK/Parkin pathway [100]. In contrast with this report, melatonin has been found to reversed the effects of cisplatin in HepG2 cells through suppression of mTOR and DNA excision repair cross complementary 1 (ERCC1) proteins expressions and up-regulation of Beclin-1 and LC3II expressions [101]. Taken together, different effects of melatonin on autophagy may be related to type of cancer cells, the stage of cancer and dose of melatonin (Table 4).
Table 4.
The effect of melatonin on autophagy machinery in recently reported findings
| Cancer | Melatonin dose/concentration | Autophagy-related targets | Effect on autophagy | Key findings | Model | Cell line | Refs. |
|---|---|---|---|---|---|---|---|
| Lung, liver and cervical cancer | 2 mM | LC3 | Activate | Induced apoptosis by ROS generation and JNK activation | In vitro | HepG2, A549, HeLa | [124] |
| Glioblastoma | 1 mM | Beclin 1, LC3-II | Activate | Autophagy disruption stimulated the melatonin-mediated apoptosis in cancer cells | In vitro | A172, U87-MG | [97] |
| Uterine leiomyoma |
25 mg/kg 0.1, 0.5, 1, 1.5, 2 mM |
Beclin1 and LC3 | Activate | Reduced tumor growth and proliferation | In vivo, in vitro | ELT3 cells, orthotopic uterine leiomyoma mouse model | [192] |
| Hepatocellular carcinoma | 10−5_ 10–3 M | PERK-ATF4-Beclin1 pathway | Inhibit | enhanced HCC sensitivity to sorafenib through suppressing autophagy | Human | - | [76] |
| Colorectal cancer | 10 μM | LC3-II | Activate | Induced interplay of apoptosis, autophagy, and senescence | In vitro | HCT116 | [171] |
| Clear cell renal cell carcinoma |
200 mg/kg 0.5, 1, 2 μM |
PGC1A, UCP1, LC3‐II | Activate | Melatonin/PGC1A/UCP1 promoted tumor slimming and repressed tumor progression through initiating autophagy and lipid browning | In vivo, in vitro |
HK2, 786‐O, A498, Caki‐1, and ACHN cells Mice |
[95] |
| Neuroblastoma |
0.1‐ 10 nM 40‐80 mg/kg |
LC3II | Activate | Promoted cancer cell differentiation through activation of hyaluronan synthase 3-mediated mitophagy | In vivo, in vitro |
N2a N2a‐allografted nude mice |
[193] |
| Head and neck squamous cell carcinoma | 0.1, 0.5, 1, 1.5 mM | ATG12-ATG5 | Activate | Induced intracellular ROS | In vitro | Cal-27, SCC-9 | [93] |
| Hepatocellular carcinoma | 1 mM | mTOR, Beclin-1 | Activate | Decreased cisplatin-mediated cell death by a counter-balance between the roles of apoptotic- and autophagy-related proteins | In vitro | HepG2 | [101] |
| Hepatocellular carcinoma | 2 mM | Beclin-1, p62, LC3II, LAMP-2 | Activate | Ceramide metabolism regulated apoptotic and autophagy cell death mediated by melatonin | In vitro | HepG2 | [96] |
| Neuroblastoma | 1 μM | Beclin‐1, LC3‐II | Activate | Enhanced autophagic activity by the SIRT1 signaling | In vitro | SH‐SY5Y | [194] |
| Gastric cancer | 10−4 M | LC3 | Activate | Hyperbaric oxygen sensitized cancer cells to melatonin-mediated apoptosis | In vitro | SGC7901 | [151] |
| Colon cancer | 1 mg/kg | Beclin-1, LC3B-II/LC3B-I ratio, p62 | Inhibit | Decreased autophagy by improving oxidative stress and inflammation | In vivo | Male Swiss Albino mice | [99] |
| Glioblastoma | 1 mM | LC3, Beclin-1 | Activate | Inhibited tumor bulk proliferation, and enhanced chemotherapy effects | In vitro | Glioblastoma-initiating cells | [195] |
| Oral cancer | 0.5–2 mM | LC3-II | Activate | Decreased drug resistance, and induced autophagy and apoptosis | In vitro | SAS, SCC9, SASV16, SASV32, SCC9V16, SCC9V32 | [139] |
| Gastric cancer |
50 mg/kg 1, 2, 3 mM |
p62, Beclin-1, LC3A/B-II | Activate | Melatonin-mediated inhibition of cancer cell proliferation is induced by the IRE/JNK/Beclin1 signaling activation | In vivo, in vitro |
AGS, SGC-7901 Male BALB/c nude mice |
[77] |
| Hepatocellular carcinoma |
10, 20 mg/kg 100 μM |
Beclin-1, LC3-I/LC3-II | Activate | Induced protective autophagy preventing hepatoma cells from undergoing apoptosis | In vitro, in vivo | H22 | [196] |
| Insulinoma | 100 μM | LC3II | Activate | Melatonin-induced insulin synthesis involved autophagy and EDC3 protein in rat insulinoma cells and subsequently resulted in a resuction in intracellular production of insulin | In vitro | INS-1E | [72] |
| Chriocarcinoma | 1 mM | LC3B | Inhibit | Modulated autophagy and the Nrf2 pathway in normal vs. tumor trophoblast cells, being cytoprotective in normal cells whilst enhancing apoptosis in tumoral trophoblast cells | In vitro | BeWo | [197] |
| Cervical cancer | 1 mM | JNK/Parkin | Inhibit | Sensitized cancer cells to cisplatin-mediated apoptosis by suppression of JNK/Parkin/mitophagy pathways | In vitro | HeLa | [100] |
| Head and neck squamous cell carcinoma |
0.1, 0.5 or 1 mM 300 mg/kg |
LC3-II, Nix | Activate | Enhanced ROS production, increased apoptosis and mitophagy, and could be used as an adjuvant agent with rapamycin | In vitro, in vivo |
Cal-27, SCC-9 Harlan Sprague–Dawley mice |
[94] |
| Tongue squamous cell carcinoma |
0, 0.5, 1, 2 mM 100 mg/kg |
LC3, ATG7 | Activate | Suppression of MT2-TFE3-dependent autophagy enhanced melatonin-mediated apoptosis | In vitro, in vivo |
Cal27, SCC9 Male athymic nude mice |
[98] |
Melatonin and apoptosis
The balance between cell proliferation and death in tissues is maintained by apoptosis, a classical form of programmed cell death. Apoptosis is associated with the disassembly of apoptotic cells into membrane-enclosed vesicles, which are removed by macrophages without inducing inflammatory responses. Apoptosis is mediated by two principle signaling pathways, including extrinsic and intrinsic pathways [102]. The extrinsic apoptotic signaling pathways, defined as death receptor pathways, are initiated by the interaction of transmembrane death receptors (Fas, TNFR1, DR4 and DR5) with extracellular ligands (FasL, TNFα, TRAIL, and TNFSF10) resulting in the activation of adaptor proteins such as Fas-associated death domain (FADD). Activated FADD recruits initiator caspases (caspase 8 and caspase 10) to form the death-inducing signal complex (DISC). Formation of DISC leads to the proteolytic activation of caspase 8, which is the main initiator caspase of the extrinsic apoptotic signaling pathway. Caspase 8 activates executioner caspases (caspase 3, caspase 6, and caspase 7) and cleaves Bid, a BH3-only domain member of the B cell lymphoma-2 (Bcl-2) family. Truncated Bid (tBid) translocates to mitochondria and activates other proapoptotic Bcl-2 family members including Bak or Bax [102, 103].
The intrinsic apoptosis pathway, defined as mitochondrial-mediated apoptotic pathway, is activated by exogenous and endogenous stimuli such as DNA damage, oxidative stress, chemotherapy and radiotherapy. This apoptosis pathway is mediated by insertion of pro-apoptotic Bcl-2 family members (Bax/Bak) into mitochondrial membrane leading to the mitochondrial outer membrane permeabilization and release of pro-apoptotic factors such as cytochrome c, Smac/DIABLO, the nuclease EndoG, the oxidoreductase AIF, and the protease HtrA2/Omi [104]. Therefore, activation of pro-apoptotic Bcl-2 family members (Bax/Bak) is essential for cancer therapy. In contrast, elevation of anti-apoptotic Bcl-2 family proteins inhibits apoptosis in cancer cells through heterodimerization with Bax/Bak preventing the release of pro-apoptotic factors from mitochondria; this could result in the resistance of cancer cells to immune-surveillance [105, 106]. Once in the cytosol, cytochrome c combines with Apaf–1 and procaspase-9 to drive the assembly of the apoptosome; this molecular platform activates caspase 9, which this is followed by the activation of caspase-3 cascade of apoptosis [107]. Smac/DIABLO and HtrA2/Omi induce apoptosis through degrading inhibitor of apoptosis protein (IAP) family, neutralizing the inhibitory effect of IAPs on caspases [108]. The nuclease EndoG and the oxidoreductase AIF translocate to the nucleus, where they trigger internucleosomal DNA fragmentation independently of caspases [109].
As mentioned earlier, UPR signaling may promote the apoptotic pathways. Upon ER stress, apoptosis signal-regulating kinase 1 (ASK1) is recruited by IRE1α-TNF receptor-associated factor 2 (TRAF2) complex, causing activation of ASK1 and the downstream JNK pathway. Activation of JNK results in the phosphorylation of Bcl-2 and Bax; phosphorylation of Bcl-2 family suppresses antiapoptotic activity of Bcl-2, while induces mitochondrial translocation of Bax and activation of apoptosis pathway. Activated JNK also activates C/EBP homologous protein (CHOP), a stress-induced transcription factor inducing the expression of pro-apoptotic Bcl-2 family members. Furthermore, IRE1α-TRAF2 complex triggers the activation of caspase-12, which this caspase translocates from the ER to the cytosol, where it activates caspase-9, independent from the apoptosome pathway [110]. Furthermore, Activated PERK phosphorylates eIF2α, promoting the expression of activating transcriptional factor 4 (ATF4); ATF4 translocates to the nucleus where it induces CHOP expression [111].
Melatonin is reported to restrict tumor growth and cancer cell proliferation through inducing apoptosis in cancer cells (Table 5). As a powerful antioxidant melatonin inhibits ROS-induced activation of extracellular-regulated protein kinases (ERKs) and Akt pathways which are involved in the cancer cell survivor; inactivation of ROS-dependent Akt signaling contributes to the down-regulation of cyclin D1, PCNA, and Bcl-2 and up-regulation of Bax in cancer cells [48]. Inhibition of MDM2 expression is a mechanism by which melatonin induces apoptosis through upregulating the activity of caspase-3 and -9; MDM2 is an E3 ubiquitin ligase, which negatively regulates the p53 tumor suppressor [112, 113]. Under hypoxic conditions, tumor cells become resistant to TRAIL-induced cell apoptosis; this contributes to the up-regulation of anti-apoptotic protein expression and reduction of pro-apoptotic protein expression. Treatment with melatonin blocks hypoxic responses leading to the induction of apoptosis in TRAIL resistance tumor cells by the regulation of mitochondrial transmembrane potential and induction of Bax translocation [114]. Melatonin inhibits cancer cell growth by increasing cell cycle arrest in the G2/M phase, which this effect is coincident with the induction of apoptosis through up-regulating the expression of p53, p21, caspase-3/8/9, PARP, cytochrome c, Bax, JNK 1,-2 and -3 and p38 MAPKs in cancer cells [115]. Melatonin triggers two distinct apoptotic processes including TGFβ1 and caspase-independent early apoptosis and TGFβ1 and caspases-dependent late apoptosis. Early apoptosis is associated with the elevation level of p53/MDM2 ratio and up-regulation of AIF release; this process is independent to caspase activity or cleavage of PARP. Late apoptosis is associated with elevation of caspases-9 and -7 activity and cleaved-PARP level as well as reduction of Bcl-2/Bax ratio [116]. Melatonin also induces apoptosis through simultaneous suppression of COX-2/PGE2, p300/NF-κB, and PI3K/Akt signaling pathway. Inhibition of these pathways leads to the induction of Apaf-1 expression triggering cytochrome c release, and caspase-3 and -9 activation and cleavage [32].
Table 5.
Anticancer effects of melatonin by apoptosis induction in experimental investigations
| Cancer | Melatonin dose/concentration | Apoptosis-related targets | Key findings | Model | Cell line | Refs. |
|---|---|---|---|---|---|---|
| Oral cancer | 0.5–2 mM | caspase-3, caspase-9, PARP | Decreased drug resistance, and induced autophagy and apoptosis | In vitro |
SCC9V32, SCC9V16, SASV32, SASV16, SAS, SCC9 |
[139] |
|
Lung cancer Hepatocellular carcinoma Cervical cancer |
2 mM | caspase-3, PARP, Bax, Bcl-2 | Decreased cell viability and increased LDH release | In vitro |
Hela A549 HepG2 |
[124] |
| Glioblastoma | 1 mM | Bax, Bcl-2 | Induced apoptosis and autophagy | In vitro |
A172 U87-MG |
[97] |
| Colorectal cancer | 0.5, 1 mM | caspase-3, PARP, NEDD9, SOX9, Bcl-xL, SOX10 | Enhanced apoptosis through miR-25-5p induced NEDD9 suppression in cancer cells | In vitro | CCD-18Co, HT29, SW480, HCT116 | [121] |
| Breast cancer |
3.5–20 mM 2 mg/kg |
caspase-3 | Repressed drug resistance through apoptosis induction and angiogenesis inhibition | In vitro, in vivo | EMT6/CPR, EMT6/VCR/R | [140] |
| Lung cancer | 2, 4, 6 mM | HDAC9 | HDAC9 knockdown increased the anticancer potentials of melatonin | In vitro, in vivo | A549, H838, H1299, and Calu-1 | [118] |
|
Ehrlich carcinoma |
20 mg/kg | Bcl‐2, caspase-3, caspase-9, | Inhibited the proliferation and growth of tumor via inducing apoptosis and through suppressing tumor vascularization | In vivo | EAC | [141] |
| Head and neck squamous cell carcinoma | 0.1, 0.5, 1, and 1.5 mM | Bax, Bcl-2 | Potentiated the cytotoxic impacts of radiotherapy and CDDP, and induced intracellular ROS leading to mitochondria-induced autophagy and apoptosis | In vitro | SCC-9, Cal-27 | [93] |
| Hepatocellular carcinoma | 20 mg/kg | Caspase-3, Bax, Bcl-2, survivin | Fostered the survival and therapeutic potential of MSCs in HCC, by inhibition of oxidative stress and inflammation as well as apoptosis induction | In vivo | - | [120] |
| Cervical cancer | 10 μM | CaMKII/Parkin/mitophagy, caspase-3, caspase-9 | Enhanced TNF-α-mediated cervical cancer cells mitochondrial apoptosis | In vitro | HeLa | [119] |
| Gastric cancer | 3 mmol/L | Caspase 9, Caspase 3, AKT, MDM2 | Promoted apoptosis through downregulation of MDM2and AKT | In vitro | AGS, MGC803 | [112] |
| Melanoma |
1 M 25 mg/kg |
cytochrome c, caspase-3, caspase-9, Bcl-2 | Synergized the antitumor effects of vemurafenib through suppressing cell proliferation and cancer-stem cell traits by targeting NF-κB/iNOS/hTERT signaling | In vitro, in vitro | G361, A431, A375, SK-Mel-28 | [142] |
| Breast cancer | 1 mM | caspase-3 | Increased apoptosiss and decreased proliferation in cancer cells | In vitro | MDA-MB-231, MCF-7 | [143] |
| Pancreatic cancer | 10–10, 10–12 M | Bax, Bcl-2, caspase-3, caspase-9 | Improved the anti-tumor effects of gemcitabine through apoptosis regulation | In vitro | PANC-1 | [144] |
| Breast cancer | 25 µM | Bax, Bcl-2 | Decreased the cell proliferation and increased apoptosis and differentiation in cancer cells | In vitro | MCF-7, HEK293 | [145] |
| Leukemia | 1 mM | Bcl-2, Bcl-xL | Synergistic effect on chemotherapeutic agent | In vitro | HL-60 | [146] |
| Breast cancer |
0.1–5 mm 1 mg/kg |
- | Melatonin caused apoptosis induction, angiogenesis inhibition, and activation of T helper 1 | In vitro, in vivo | EMT6/P | [147] |
| Colorectal cancer | 1 mM | BAX, caspase3, PARP1 | Induced mitochondria-induced cellular apoptosis | In vitro | SNUC5/WT | [71] |
| Breast cancer | 1 nM and 100 nM | c-IAP1, XIAP, survivin, MCL-1, BCL-2, | Enhanced cytotoxic effects of arsenic trioxide and apoptosis induction | In vitro | MCF-7 | [148] |
| Pancreatic cancer |
0.1, 1, or 2 mM 40 mg/kg |
cytochrome c XIAP, Mcl-1, Survivin, Bcl-2, PARP |
Reinforced the anticancer effect of sorafenib via downregulation of PDGFR-β/STAT3 signaling | In vitro, in vivo | MIAPaCa-2, PANC-1 | [149] |
| Glioblastoma | 1 mM, 3 mM | - | Delayed cell cycle progression and potentiated the decrease of cell survival due to treatment with temozolomide | In vitro | U87MG | [150] |
| Oral cancer |
1 mM 40 mg/kg |
cyclin D1, PCNA, Bcl-2, Bax |
Suppressed the invasion and migration of cancer cells through repressing ROS-activated Akt signaling Hampered vasculogenic mimicry and retarded tumorigenesis of cancer cells |
In vitro, in vivo | SCC25, SCC9, Tca8113, Cal27, and FaDu | [48] |
| Gastric cancer | 10−4 mol/L | Bcl-2, Bax, p53, caspase3, | Hyperbaric oxygen sensitized cancer cells to melatonin-mediated apoptosis | In vitro | SGC7901 | [151] |
| Thyroid cancer |
1, 2, 4, 8, 15 mM 25 mg/kg |
caspase 3/7, PARP, cytochrome c |
Reduced cell viability, inhibited cell migration and induced apoptosis Synergized with irradiation to induce cytotoxicity to thyroid cancer cells |
In vitro, in vivo | 8505c, ARO | [152] |
| Gastric cancer | 1, 2, 3, 4 or 5 mM | Bax, Bcl-xL, caspase-9, caspase-3 | Induced cell cycle arrest and induced apoptosis | In vitro | SGC-7901 | [153] |
| Neural cancer | 0.5, 1 mM | Bax, Bcl-2, caspase-9, cytochrome c | Mitochondrial cytochrome P450 1B1 is responsible for melatonin-induced apoptosis | In vitro | U118, SH-SY5Y, U87, U251, A172 | [154] |
| Gastric cancer | 1, 5 µM | - | Inhibited the proliferation of cancer cells by regulating the miR-16-5p-Smad3 pathway | In vitro | BSG823, SGC-7901 | [155] |
| Head and neck squamous cell carcinoma | 0.1, 0.5, or 1 mM | Bax, Bcl-2 | Enhanced ROS production, increased apoptosis and mitophagy, and could be used as an adjuvant agent with rapamycin | In vitro | Cal-27, SCC-9 | [94] |
| Ovarian cancer, colorectal cancer | 0.1, 1.0, and 10 μM | - | Induced apoptosis and showed antioxidant effects | In vitro | DLD1, A2780 | [156] |
| Cervical cancer | 1 mM | JNK/Parkin/mitophagy, caspase-9 | Sensitized cancer cells to cisplatin-mediated apoptosis by suppression of JNK/Parkin/mitophagy pathways | In vitro | HeLa | [100] |
|
Melanoma Breast cancer |
Melatonin: 10−5 − 10−3 M Melatonin analogues (UCM 1037): 10−6 − 10−4 M and 16 mg/Kg |
Bcl-2, Bax, caspase-3 |
Inactivated mitophagy by suppression of JNK/Parkin, leading to the inhibition of anti-apoptotic mitophagy Sensitized cervical cancer cells to cisplatin-mediated apoptosis |
In vitro, in vivo | DX3, WM-115, MCF-7, MDA-MB231 | [157] |
| Bladder cancer |
10 mg/kg 1.0 mM |
caspase-3, Bcl-2, BAX | Synergized the inhibitory effects of curcumin against the growth of bladder cancer through increasing the anti-proliferation, anti-migration, and pro-apoptotic properties | In vivo, in vitro | T24, UMUC3, 5637 | [158] |
| Colorectal cancer | 1 mM | caspase-3 | Increased the sensitivity of cancer cells to 5-FU | In vitro | HT-29 | [159] |
| Lung cancer |
25 mg/kg 1 mM |
caspse-9, Bcl-2, PARP, cytochrome C | Increased antitumor activities of berberine through activating caspase/Cyto C and suppressing AP-2β/hTERT, NF-κB/COX-2 and Akt/ERK pathways | In vitro, in vivo | H1299, A549 | [160] |
| Gastric cancer | 1, 2 mM | caspase-3, Bcl-2, BAX | Suppressed cell viability, clone formation, cell migration and invasion and induced apoptosis | In vitro | AGS | [161] |
| Ovarian cancer | 200 μg/100 g b.w | p53, BAX, caspase-3, Bcl-2, survivin | Promoted apoptosis | In vivo | - | [162] |
| Cervical cancer | 1 mM | Caspase-3 | Enhanced cisplatin-mediated cytotoxicity and apoptosis | In vitro | HeLa | [163] |
| Rhabdomyosarcoma | 0.01, 0.1, 1, 2 mM | Bax, Bcl-2, caspase-3 | Enhanced the sensitivity of cancer cells to apoptosis | In vitro | U57810, U23674 | [164] |
| Hepatocellular carcinoma | 2 mM | PARP, Bax | Ceramide metabolism regulated apoptotic and autophagy cell death mediated by melatonin | In vitro | HepG2 | [96] |
| Neuroblastoma | 0.25, 0.5, 1, 2 mM | - | Exerted cytotoxic potentials against cancer cells | In vitro | SH-SY5Y | [165] |
| Colorectal cancer | 0.1–2.0 mM | HDAC4, Bcl-2, CaMKIIα | Melatonin-induced apoptosis depends on the nuclear import of HDAC4 and subsequent H3 deacetylation by CaMKIIα inactivation | In vitro | LoVo | [117] |
| RCC, CRC, Head and neck cancer, Prostate cancer, breast cancer | 1 mM | PUMA, Mcl-1, Bcl-xL, Bim, COX-2 | Enhanced antitumor effects by COX-2 downregulation and Bim up-regulation | In vitro |
MDA-MB-231, Caki, HN4, HCT116, PC3 |
[123] |
| Cholangiocarcinoma |
1 nM, 1 μM 0.5, 1, 2 mM |
Caspase-3/7, cytochrome c | Functioned as a pro-oxidant through activating ROS-dependent DNA damage and hence leading to the apoptosis of cancer cells | In vitro | KKU-M055, KKU-M214 | [166] |
| Lung cancer | 1–5 mM | caspases-3/7 | Increased cisplatin-induced cytotoxicity and apoptosis in lung cancer cells | In vitro | SK-LU-1 | [167] |
| Gastric cancer | 25, 50, 100 mg/kg | Bcl-2, Bax, p21, p53 | Inhibited tumor growth by apoptosis induction | In vivo | MFC | [168] |
| Lung cancer | 1, 5, 10 mM | caspase-3/7 | Showed anticancer impacts by changing biomolecular structure of lipids, nucleic acids and proteins | In vitro | SK-LU-1 | [169] |
| Lung cancer |
10−13 M (subphysiological), 10−10 M (physiological) 10−7, 10−4, 10− 3 M (Cytotoxic) |
CCAR2 | Cell cycle and apoptosis regulator 2 (CCAR2) is critical for maintaining cell survival in the presence of melatonin | In vitro | A549, A427 | [170] |
| Lung cancer | 500 μM | Bcl-2, Bcl-xL, TRAIL | Induced apoptosis in TRAIL-resistant hypoxic tumor cells trough diminishing the anti-apoptotic signals induced by hypoxia | In vitro | A549 | [114] |
| Breast cancer | 1 nM | p53, MDM2/MDMX/p300 | Enhanced p53 acetylation by regulating the MDM2/MDMX/p300 pathway | In vitro | MCF-7 | [113] |
| Colorectal cancer | 10 μM | Bax, Bcl-xL, | Activated cell death programs early and induced G1-phase arrest at the advanced phase | In vitro | HCT116 | [171] |
| Renal cancer | 0.1, 0.5,1 mM | Bim | Induced apoptosis by the upregulation of Bim expression | In vitro | Caki | [172] |
| Leukemia | 1 mM | Bax, cytochrome c | Induced apoptosis by a caspase-dependent but ROS-independent manner | In vitro | Molt-3 | [173] |
| Gastric cancer | 10–4 mol/l | Caspase-3 | Inhibited tumor cell proliferation and reduced the metastatic potential of cancer cells | In vitro | SGC7901 | [174] |
| Colorectal cancer | 1 mM | caspase-3/9, PARP | Potentiated the anti-proliferative and pro-apoptotic impacts of Ursolic acid in cancer cells | In vitro | SW480, LoVo | [175] |
| Pancreatic cancer |
1.5 mmol/L 20 mg/kg |
Bax, Bcl-2 | Melatonin may be a pro-apoptotic and pro-necrotic molecule for cancer cells by its regulation of Bcl-2/Bax balance | In vitro, in vivo | SW-1990 | [176] |
| Breast cancer | 10–3 M | COX-2/PGE2, p300/NF-κB, PI3K/Akt, Apaf-1/caspase-3/9 | Inhibited cell proliferation and induced apoptosis | In vitro | MDA-MB-361 | [32] |
| Hepatocellular carcinoma | 10–9, 10–7, 10–5, 10–3 μM | CHOP, Bcl-2, Bax, COX-2 | Sensitized cancer cells to ER stress-mediated apoptosis by downregulating COX-2 expression, enhancing the levels of CHOP and reducing the Bcl-2/Bax ratio | In vitro | HepG2 | [73] |
| Ovarian cancer | 0, 0.5, 1, 2 mM | ERK/p90RSK/HSP27 | Enhanced cisplatin-mediated apoptosis through the inactivation of ERK/p90RSK/HSP27 pathway | In vitro | SK-OV-3 | [122] |
| Gastric cancer | 2 mM | NF-κB, MAPK | Conflicting growth signals in cells may suppress melatonin efficacy in the treatment of gastric cancer | In vitro | SGC7901 | [177] |
| Hepatocellular carcinoma | 10–3, 10–5, 10–7, 10–9 mmol/L | COX-2, Bcl-2, Bax | Melatonin was shown as a novel selective ATF-6 inhibitor that can sensitize human hepatoma cells to ER stress inducing apoptosis | In vitro | HepG2 | [74] |
| Glioma | 1 μM | - | Inhibited miR-155 expression and hence repressed glioma cell proliferation, invasion and migration | In vitro | U87, U373, U251 | [178] |
| Breast cancer | 1 mM | caspase-3, hTRA, XIAP, TNFRII, P53, P21, Livin, IGF-1R, IGF-1, IGFPB-6, IGFBP-5, IGFBP-3, DR6, CYTO-C | Showed pro-apoptotic, anti-angiogenic and oncostatic properties | In vitro | MDA-MB-231, MCF-7 | [179] |
| Leukemia | 1 mM | ROS, caspase-3/8/9 | Enhanced apoptotic effects of hydrogen peroxide | In vitro | HL-60 | [180] |
| Renal cancer | 1 nM | CHOP, PUMA | PUMA up-regulation contributed to the sensitizing impact of melatonin plus kahweol on apoptosis | In vitro | Caki | [181] |
| Pancreatic cancer | 10−8 –10−12 M | Bcl-2, Bax, caspase-9 | Induced pro-apoptotic pathways by interaction with the Mel-1 A/B receptors | In vitro | PANC-1 | [182] |
| Ewing sarcoma | 50 μM-1 mM | caspase-3/8/9, Bid | Showed cytoprotective effects on noncancer cells and induced apoptosis | In vitro | SK-N-MC | [183] |
| Glioma | 1 mM | Survivin, Bcl-2 | Increased cell sensitivity to TRAIL-mediated cell apoptosis | In vitro | A172, U87 | [184] |
| Leukemia |
1 mM 250 mg/kg |
Bax, Bcl-2, p53 | Enhanced radiation-mediated apoptosis in cancer cells, while decreasin radiation-meditated apoptosis in normal cells | In vitro, in vivo | Jurkat | [185] |
| Breast cancer | 1 nM | Caspase-7/9, p53, MDM2, PARP, Bcl-2, Bax | Induced apoptosis in cancer cells | In vitro | MCF-7 | [116] |
| Hepatocellular carcinoma | 1000–10,000 μM | caspase-3/8/9, PARP, cytochrome c, Bax, p53, p21 | Induced cell cycle arrest and apoptosis | In vitro | HepG2 | [115] |
| Pheochromocytoma | 100 μM | GSH | Apoptotic and antioxidant effects | In vitro | PC12 | [186] |
| Neuroblastoma | 100 μM | Caspase-3 | Induced apoptosis | In vitro | SK-N-MC | [187] |
|
Leukemia Cervical cancer |
50 μM | Caspase-3 | Protectted normal and cancer cells against genotoxic treatment and apoptosis induced by idarubicin | In vitro |
K562, HeLa |
[188] |
| Colorectal cancer | 1 mM | Caspase-3 | Potentiated flavone-mediated apoptosis in cancer cells | In vitro | HT-29 | [189] |
| Breast cancer | 1 nM | Bax, p53, p21, WAF1, bcl-XL, bcl-2 | Decreased cancer cell proliferation through regulating cell-cycle length by the control of the p53-p21 pathway | In vitro | MCF-7 | [190] |
| Esophageal cancer |
0–5 mM 25 mg/kg |
PARP, caspase-3/7/8 | Increased cytotoxicity of 5-Fu | In vivo, in vitro | KYSE30, KYSE150, KYSE410, KYSE520 | [191] |
Melatonin induces dephosphorylation and nuclear import of histone deacetylase 4 (HDAC4) in cancer cells; melatonin exerts this effect through inactivation of Ca2+/calmodulin-dependent protein kinase II alpha (CaMKIIα), leading to the H3 acetylation on Bcl-2 promoter and subsequent reduction of Bcl-2 expression [117]. Furthermore, inhibition of HDAC9 expression is a mechanism of melatonin to promote apoptosis in non-small cell lung cancer; the increased level of HDAC9 in patients with non-small cell lung cancer is correlated with worse overall survival and poor prognosis [118]. Melatonin promotes TNF-α-mediated apoptosis via inhibiting mitophagy in tumor cells. Since activation of mitophagy suppresses mitochondrial apoptosis, inhibition of mitophagy by melatonin results in the repression of mitochondrial potential, elevation of ROS generation, augmentation of mPTP opening rate and up-regulation of cytochrome c expression and caspases activity. Melatonin inhibits autophagy in tumor cells through inhibiting CaMKII activity leading to the suppression of Parkin expression [119]. In diethylnitrosamine (DEN)-induced hepatocellular carcinoma (HCC), melatonin increases therapeutic potential of mesenchymal stem cells (MSCs) through reduction of oxidative stress and inflammation, and induction of apoptosis [120].
Melatonin has been reported to increase therapeutic potential of anti-cancer agents, which this effect may result from its stimulatory effect on apoptosis. Co-treatment of melatonin and pterostilbene in colorectal cancer cells synergically enhances ROS production and apoptosis. Combination of these two agents upregulates the mRNA level of miR-25-5p, which this results in the activation of PARP and sex-determining region Y-Box10 (SOX10), and attenuation of Bcl-xL, neural precursor cell expressed developmentally downregulated protein 9 (NEDD9), and SOX9 expressions [121]. Melatonin synergically enhances anticancer potential of cisplatin through inducing apoptosis; melatonin increases the effect of cisplatin to the inhibition of ERK phosphorylation and induction of 90-kDa ribosomal S6 kinase (p90RSK) and heat shock protein 27 (HSP27) dephosphorylation [122]. Treatment with melatonin enhances ER stress–mediated apoptosis in tunicamycin-treated cancer cells; this effect is associated with the down-regulation of COX-2 and Bcl-2 expressions and up-regulation of Bim, CHOP and Bax expressions [73]. Melatonin inhibits tunicamycin-induced COX-2 activation in tumor cells through inhibiting NF-ĸB and p38 MAPK activation and p65 nuclear translocation [123]. Combination of melatonin with phenylarsine oxide also induces endoplasmic reticulum stress-induced cell death, accompanied by JNK activation, PARP cleavage, ROS generation and caspase-3 activation [124].
Conclusions
This review summarizes the anti-carcinogenic potentials of melatonin by evaluating various signaling pathways. Melatonin inhibits proliferation of cancer cells through triggering cell cycle arrest and causes cell death by induction of apoptosis. Melatonin suppresses metastasis angiogenesis, and proliferation of cancer cells through affecting various signaling pathways in tumor cells. Melatonin also regulates autophagy pathway in cancer cell by affecting oxidative stress condition in tumor cells. These findings suggest that melatonin may increase the sensitivity of cancer cells to anti-cancer agents and may be a potential treatment for cancers either alone or in combination with other anti-cancer drugs. However, further clinical studies are needed to clarify the effect of this molecule in different cancers and obtain affective dose of melatonin for patients with cancer.
Acknowledgements
Not applicable.
Abbreviations
- JNK
C-Jun N-terminal kinase
- ROS
Reactive oxygen species
- VEGF
Vascular endothelial growth factor
- TNF-α
Tumor necrosis factor-α
- IL-2
Interleukin-2
- Nrf2
Nuclear factor erythroid 2-related factor 2
- Apaf-1
Apoptotic protease activating factor-1
- COX-2
Cyclooxygenase-2
- Sirt1
Sirtuin
- HIF
Hypoxia-inducible factor
- TRAIL
TNF-related apoptosis-inducing ligand
- PARP-1
Poly [ADP-ribose] polymerase 1
- ATG
Autophagy related genes
- IRE1
Inositol-requiring enzyme 1
- ATF6
Activating transcription factor 6
- ERK
Extracellular signal-regulated kinase
- MEK
Mitogen-activated protein kinase kinase
- MAPK
Mitogen-activated protein kinase
- CHOP
CCAAT-enhancer-binding proteins homologous protein
- PUMA
P53-upregulated modulator of apoptosis
- Bcl-2
B cell lymphoma-2
- Bim
Bcl-2-interacting mediator of cell death
- PI3K
Phosphatidylinositol-3-kinase
- Akt
Protein kinase B
- UPR
Unfolded protein response
- ATF6α
Activating transcription factor 6α
- ER
Endoplasmic reticulum
- PERK
Protein kinase RNA-like ER kinase
- ERK
Extracellular signal-regulated kinase
- SPHK1
Sphingosine kinase 1
- IFN-γ
Interferon-gamma
- PGC1A
Peroxisome proliferator-activated receptor gamma coactivator 1A
- NQO-1
NAD(P)H:quinone oxidoreductase
- HO-1
Heme oxygenase-1
- FADD
Fas-associated death domain
- tBid
Truncated Bid
- ASK1
Apoptosis signal-regulating kinase 1
- TRAF2
IRE1α-TNF receptor-associated factor 2
- ERKs
Extracellular-regulated protein kinases
- CaMKIIα
Ca2+/calmodulin-dependent protein kinase II alpha
- DEN
Diethylnitrosamine
- HCC
Hepatocellular carcinoma
- MSCs
Mesenchymal stem cells
- NEDD9
Neural precursor cell expressed developmentally downregulated protein 9
- p90RSK
90-KDa ribosomal S6 kinase
- HSP27
Heat shock protein 27
Authors' contributions
Conception and design: AH and SM. Performing the literature search: MHP, AM and FM. Drafting the manuscript: all authors. Approving the final version: all authors. AH is responsible for the integrity of the work as a whole. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for-profit sectors.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Saeed Mehrzadi and Mohammad Hossein Pourhanifeh contributed equally to this work
References
- 1.Block KI, Gyllenhaal C, Lowe L, Amedei A, Amin A, Amin A, Aquilano K, Arbiser J, Arreola A, Arzumanyan A, et al. Designing a broad-spectrum integrative approach for cancer prevention and treatment. Seminars Cancer Biol. 2015;35 Suppl(Suppl):S276–S304. doi: 10.1016/j.semcancer.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alobaedi OH, Talib WH, Basheti IA. Antitumor effect of thymoquinone combined with resveratrol on mice transplanted with breast cancer. Asian Pac J Trop Med. 2017;10(4):400–408. doi: 10.1016/j.apjtm.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 3.Talib WH. Consumption of garlic and lemon aqueous extracts combination reduces tumor burden by angiogenesis inhibition, apoptosis induction, and immune system modulation. Nutrition (Burbank, Los Angeles County, Calif) 2017;43–44:89–97. doi: 10.1016/j.nut.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Falah RR, Talib WH, Shbailat SJ. Combination of metformin and curcumin targets breast cancer in mice by angiogenesis inhibition, immune system modulation and induction of p53 independent apoptosis. Therapeutic Adv Med Oncol. 2017;9(4):235–252. doi: 10.1177/1758834016687482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slominski A, Fischer TW, Zmijewski MA, Wortsman J, Semak I, Zbytek B, Slominski RM, Tobin DJ. On the role of melatonin in skin physiology and pathology. Endocrine. 2005;27(2):137–148. doi: 10.1385/ENDO:27:2:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pourhanifeh MH, Mehrzadi S, Hosseinzadeh A. Melatonin and regulation of miRNAs: novel targeted therapy for cancerous and noncancerous disease. Epigenomics. 2020;13:65–81. doi: 10.2217/epi-2020-0241. [DOI] [PubMed] [Google Scholar]
- 7.Pourhanifeh MH, Hosseinzadeh A, Juybari KB, Mehrzadi S. Melatonin and urological cancers: a new therapeutic approach. Cancer Cell Int. 2020;20(1):444. doi: 10.1186/s12935-020-01531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bahrampour Juybari K, Pourhanifeh MH, Hosseinzadeh A, Hemati K, Mehrzadi S. Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Res. 2020;287:198108. doi: 10.1016/j.virusres.2020.198108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehrzadi S, Karimi MY, Fatemi A, Reiter RJ, Hosseinzadeh A. SARS-CoV-2 and other coronaviruses negatively influence mitochondrial quality control: beneficial effects of melatonin. Pharmacol Ther. 2021;224:107825–107825. doi: 10.1016/j.pharmthera.2021.107825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pourhanifeh MH, Mahdavinia M, Reiter RJ, Asemi Z. Potential use of melatonin in skin cancer treatment: a review of current biological evidence. J Cell Physiol. 2019;234(8):12142–12148. doi: 10.1002/jcp.28129. [DOI] [PubMed] [Google Scholar]
- 11.Anderson G. The effects of melatonin on signaling pathways and molecules involved in glioma: melatonin and glioblastoma: pathophysiology and treatment. Fundam Clin Pharmacol. 2020;34(2):189–191. doi: 10.1111/fcp.12538. [DOI] [PubMed] [Google Scholar]
- 12.Pourhanifeh MH, Sharifi M, Reiter RJ, Davoodabadi A, Asemi Z. Melatonin and non-small cell lung cancer: new insights into signaling pathways. Cancer Cell Int. 2019;19:131. doi: 10.1186/s12935-019-0853-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pourhanifeh MH, Mehrzadi S, Kamali M, Hosseinzadeh A. Melatonin and gastrointestinal cancers: Current evidence based on underlying signaling pathways. Eur J Pharmacol. 2020 doi: 10.1016/j.ejphar.2020.173471. [DOI] [PubMed] [Google Scholar]
- 14.Zhao Q, Wang W, Cui J. Melatonin enhances TNF-α-mediated cervical cancer HeLa cells death via suppressing CaMKII/Parkin/mitophagy axis. Cancer Cell Int. 2019;19:58. doi: 10.1186/s12935-019-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Bu S, Wang Q, Sun J, Li X, Gu T, Lai D. Melatonin suppresses chronic restraint stress-mediated metastasis of epithelial ovarian cancer via NE/AKT/β-catenin/SLUG axis. Cell Death Dis. 2020;11(8):644. doi: 10.1038/s41419-020-02906-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan G, Lei H, He M, Gong R, Wang Y, He X, Li G, Pang P, Li X, Yu S, et al. Melatonin triggers autophagic cell death by regulating RORC in Hodgkin lymphoma. Biomed Pharmacother. 2020;123:109811. doi: 10.1016/j.biopha.2020.109811. [DOI] [PubMed] [Google Scholar]
- 17.Tian T, Li J, Li Y, Lu YX, Tang YL, Wang H, Zheng F, Shi D, Long Q, Chen M, et al. Melatonin enhances sorafenib-induced cytotoxicity in FLT3-ITD acute myeloid leukemia cells by redox modification. Theranostics. 2019;9(13):3768–3779. doi: 10.7150/thno.34327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reiter RJ, Tan DX, Fuentes-Broto L. Melatonin: a multitasking molecule. Prog Brain Res. 2010;181:127–151. doi: 10.1016/S0079-6123(08)81008-4. [DOI] [PubMed] [Google Scholar]
- 19.Bonnefont-Rousselot D, Collin F. Melatonin: action as antioxidant and potential applications in human disease and aging. Toxicology. 2010;278(1):55–67. doi: 10.1016/j.tox.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Slominski RM, Reiter RJ, Schlabritz-Loutsevitch N, Ostrom RS, Slominski AT. Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol Cell Endocrinol. 2012;351(2):152–166. doi: 10.1016/j.mce.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens RG, Brainard GC, Blask DE, Lockley SW, Motta ME. Breast cancer and circadian disruption from electric lighting in the modern world. CA Cancer J Clin. 2014;64(3):207–218. doi: 10.3322/caac.21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He R, Cui M, Lin H, Zhao L, Wang J, Chen S, Shao Z. Melatonin resists oxidative stress-induced apoptosis in nucleus pulposus cells. Life Sci. 2018;199:122–130. doi: 10.1016/j.lfs.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 23.Reiter RJ, Tan DX, Erren TC, Fuentes-Broto L, Paredes SD. Light-mediated perturbations of circadian timing and cancer risk: a mechanistic analysis. Integr Cancer Ther. 2009;8(4):354–360. doi: 10.1177/1534735409352026. [DOI] [PubMed] [Google Scholar]
- 24.Pourhanifeh MH, Hosseinzadeh A, Dehdashtian E, Hemati K, Mehrzadi S. Melatonin: new insights on its therapeutic properties in diabetic complications. Diabetol Metab Syndr. 2020;12:1–20. doi: 10.1186/s13098-020-00537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dehdashtian E, Pourhanifeh MH, Hemati K, Mehrzadi S, Hosseinzadeh A. Therapeutic application of nutraceuticals in diabetic nephropathy: current evidence and future implications. Diabetes Metab Res Rev. 2020;36:e3336. doi: 10.1002/dmrr.3336. [DOI] [PubMed] [Google Scholar]
- 26.Rosales-Corral S, Tan DX, Reiter RJ, Valdivia-Velázquez M, Martínez-Barboza G, Acosta-Martínez JP, Ortiz GG. Orally administered melatonin reduces oxidative stress and proinflammatory cytokines induced by amyloid-beta peptide in rat brain: a comparative, in vivo study versus vitamin C and E. J Pineal Res. 2003;35(2):80–84. doi: 10.1034/j.1600-079X.2003.00057.x. [DOI] [PubMed] [Google Scholar]
- 27.Hosseinzadeh A, Javad-Moosavi SA, Reiter RJ, Hemati K, Ghaznavi H, Mehrzadi S. Idiopathic pulmonary fibrosis (IPF) signaling pathways and protective roles of melatonin. Life Sci. 2018;201:17–29. doi: 10.1016/j.lfs.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 28.Daryani A, Montazeri M, Pagheh AS, Sharif M, Sarvi S, Hosseinzadeh A, Reiter RJ, Hadighi R, Joghataei MT, Ghaznavi H. The potential use of melatonin to treat protozoan parasitic infections: a review. Biomed Pharmacother. 2018;97:948–957. doi: 10.1016/j.biopha.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 29.Yokota O, Terada S, Ishizu H, Ishihara T, Ujike H, Nakashima H, Nakashima Y, Kugo A, Checler F, Kuroda S. Cyclooxygenase-2 in the hippocampus is up-regulated in Alzheimer's disease but not in variant Alzheimer's disease with cotton wool plaques in humans. Neurosci Lett. 2003;343(3):175–179. doi: 10.1016/S0304-3940(03)00339-2. [DOI] [PubMed] [Google Scholar]
- 30.Juybari KB, Hosseinzadeh A, Ghaznavi H, Kamali M, Sedaghat A, Mehrzadi S, Naseripour M. Melatonin as a modulator of degenerative and regenerative signaling pathways in injured Retinal Ganglion Cells. Curr Pharm Des. 2019;25(28):3057–3073. doi: 10.2174/1381612825666190829151314. [DOI] [PubMed] [Google Scholar]
- 31.Menéndez-Menéndez J, Hermida-Prado F, Granda-Díaz R, González A, García-Pedrero JM, Del-Río-Ibisate N, González-González A, Cos S, Alonso-González C, Martínez-Campa C. Deciphering the molecular basis of melatonin protective effects on breast cells treated with doxorubicin: TWIST1 a transcription factor involved in EMT and metastasis, a novel target of melatonin. Cancers. 2019;11(7):1011. doi: 10.3390/cancers11071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J, Xiao X, Zhang Y, Shi D, Chen W, Fu L, Liu L, Xie F, Kang T, Huang W, et al. Simultaneous modulation of COX-2, p300, Akt, and Apaf-1 signaling by melatonin to inhibit proliferation and induce apoptosis in breast cancer cells. J Pineal Res. 2012;53(1):77–90. doi: 10.1111/j.1600-079X.2012.00973.x. [DOI] [PubMed] [Google Scholar]
- 33.Cipolla-Neto J, Amaral FGD. Melatonin as a hormone: new physiological and clinical insights. Endocr Rev. 2018;39(6):990–1028. doi: 10.1210/er.2018-00084. [DOI] [PubMed] [Google Scholar]
- 34.Pourhanifeh MH, Dehdashtian E, Hosseinzadeh A, Sezavar SH, Mehrzadi S. Clinical application of melatonin in the treatment of cardiovascular diseases: current evidence and new insights into the cardioprotective and cardiotherapeutic properties. Cardiovasc Drugs Ther. 2020;14:1–25. doi: 10.1007/s10557-020-07052-3. [DOI] [PubMed] [Google Scholar]
- 35.Sánchez-Barceló EJ, Cos S, Fernández R, Mediavilla MD. Melatonin and mammary cancer: a short review. Endocr Relat Cancer. 2003;10(2):153–159. doi: 10.1677/erc.0.0100153. [DOI] [PubMed] [Google Scholar]
- 36.Cos S, Sánchez-Barceló EJ. Melatonin and mammary pathological growth. Front Neuroendocrinol. 2000;21(2):133–170. doi: 10.1006/frne.1999.0194. [DOI] [PubMed] [Google Scholar]
- 37.Cos S, Fernández R, Güézmes A, Sánchez-Barceló EJ. Influence of melatonin on invasive and metastatic properties of MCF-7 human breast cancer cells. Can Res. 1998;58(19):4383–4390. [PubMed] [Google Scholar]
- 38.Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nat Rev Cancer. 2003;3(6):401–410. doi: 10.1038/nrc1093. [DOI] [PubMed] [Google Scholar]
- 39.Vaupel P. The role of hypoxia-induced factors in tumor progression. Oncologist. 2004;9(Suppl 5):10–17. doi: 10.1634/theoncologist.9-90005-10. [DOI] [PubMed] [Google Scholar]
- 40.Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 41.Jeong JW, Bae MK, Ahn MY, Kim SH, Sohn TK, Bae MH, Yoo MA, Song EJ, Lee KJ, Kim KW. Regulation and destabilization of HIF-1alpha by ARD1-mediated acetylation. Cell. 2002;111(5):709–720. doi: 10.1016/S0092-8674(02)01085-1. [DOI] [PubMed] [Google Scholar]
- 42.Mirza-Aghazadeh-Attari M, Reiter RJ, Rikhtegar R, Jalili J, Hajalioghli P, Mihanfar A, Majidinia M, Yousefi B. Melatonin: an atypical hormone with major functions in the regulation of angiogenesis. IUBMB Life. 2020;72(8):1560–1584. doi: 10.1002/iub.2287. [DOI] [PubMed] [Google Scholar]
- 43.Ma Q, Reiter RJ, Chen Y. Role of melatonin in controlling angiogenesis under physiological and pathological conditions. Angiogenesis. 2020;23(2):91–104. doi: 10.1007/s10456-019-09689-7. [DOI] [PubMed] [Google Scholar]
- 44.Park SY, Jang WJ, Yi EY, Jang JY, Jung Y, Jeong JW, Kim YJ. Melatonin suppresses tumor angiogenesis by inhibiting HIF-1alpha stabilization under hypoxia. J Pineal Res. 2010;48(2):178–184. doi: 10.1111/j.1600-079X.2009.00742.x. [DOI] [PubMed] [Google Scholar]
- 45.Cho SY, Lee HJ, Jeong SJ, Lee HJ, Kim HS, Chen CY, Lee EO, Kim SH. Sphingosine kinase 1 pathway is involved in melatonin-induced HIF-1α inactivation in hypoxic PC-3 prostate cancer cells. J Pineal Res. 2011;51(1):87–93. doi: 10.1111/j.1600-079X.2011.00865.x. [DOI] [PubMed] [Google Scholar]
- 46.Alvarez-García V, González A, Alonso-González C, Martínez-Campa C, Cos S. Regulation of vascular endothelial growth factor by melatonin in human breast cancer cells. J Pineal Res. 2013;54(4):373–380. doi: 10.1111/jpi.12007. [DOI] [PubMed] [Google Scholar]
- 47.Siu SW, Lau KW, Tam PC, Shiu SY. Melatonin and prostate cancer cell proliferation: interplay with castration, epidermal growth factor, and androgen sensitivity. Prostate. 2002;52(2):106–122. doi: 10.1002/pros.10098. [DOI] [PubMed] [Google Scholar]
- 48.Liu R, Wang HL, Deng MJ, Wen XJ, Mo YY, Chen FM, Zou CL, Duan WF, Li L, Nie X. Melatonin inhibits reactive oxygen species-driven proliferation, epithelial-mesenchymal transition, and vasculogenic mimicry in oral cancer. Oxid Med Cell Longev. 2018;2018:3510970. doi: 10.1155/2018/3510970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu H, Zhu Y, Zhu H, Cai R, Wang KF, Song J, Wang RX, Zhou RX. Role of transforming growth factor β1 in the inhibition of gastric cancer cell proliferation by melatonin in vitro and in vivo. Oncol Rep. 2019;42(2):753–762. doi: 10.3892/or.2019.7190. [DOI] [PubMed] [Google Scholar]
- 50.León J, Casado J, Jiménez Ruiz SM, Zurita MS, González-Puga C, Rejón JD, Gila A, Muñoz de Rueda P, Pavón EJ, Reiter RJ, et al. Melatonin reduces endothelin-1 expression and secretion in colon cancer cells through the inactivation of FoxO-1 and NF-κβ. J Pineal Res. 2014;56(4):415–426. doi: 10.1111/jpi.12131. [DOI] [PubMed] [Google Scholar]
- 51.Goncalves Ndo N, Rodrigues RV, Jardim-Perassi BV, Moschetta MG, Lopes JR, Colombo J, Zuccari DA. Molecular markers of angiogenesis and metastasis in lines of oral carcinoma after treatment with melatonin. Anticancer Agents Med Chem. 2014;14(9):1302–1311. doi: 10.2174/1871520614666140812110246. [DOI] [PubMed] [Google Scholar]
- 52.Maschio-Signorini LB, Gelaleti GB, Moschetta MG, Borin TF, Jardim-Perassi BV, Lopes JR, Lacerda JZ, Roela RA, Bordin NA, Corrêa LA, et al. Melatonin regulates angiogenic and inflammatory proteins in MDA-MB-231 cell line and in co-culture with cancer-associated fibroblasts. Anticancer Agents Med Chem. 2016;16(11):1474–1484. doi: 10.2174/1871520616666160422105920. [DOI] [PubMed] [Google Scholar]
- 53.Wang RX, Liu H, Xu L, Zhang H, Zhou RX. Melatonin downregulates nuclear receptor RZR/RORγ expression causing growth-inhibitory and anti-angiogenesis activity in human gastric cancer cells in vitro and in vivo. Oncol Lett. 2016;12(2):897–903. doi: 10.3892/ol.2016.4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lissoni P, Rovelli F, Malugani F, Bucovec R, Conti A, Maestroni GJ. Anti-angiogenic activity of melatonin in advanced cancer patients. Neuro Endocrinol Lett. 2001;22(1):45–47. [PubMed] [Google Scholar]
- 55.Vimalraj S, Saravanan S, Raghunandhakumar S, Anuradha D. Melatonin regulates tumor angiogenesis via miR-424-5p/VEGFA signaling pathway in osteosarcoma. Life Sci. 2020;256:118011. doi: 10.1016/j.lfs.2020.118011. [DOI] [PubMed] [Google Scholar]
- 56.Duracková Z. Some current insights into oxidative stress. Physiol Res. 2010;59(4):459–469. doi: 10.33549/physiolres.931844. [DOI] [PubMed] [Google Scholar]
- 57.Bagherifard A, Kadijani AA, Yahyazadeh H, Rezazadeh J, Azizi M, Akbari A, Mirzaei A. The value of serum total oxidant to the antioxidant ratio as a biomarker of knee osteoarthritis. Clin Nutr ESPEN. 2020;38:118–123. doi: 10.1016/j.clnesp.2020.05.019. [DOI] [PubMed] [Google Scholar]
- 58.Saha SK, Lee SB, Won J, Choi HY, Kim K, Yang G-M, Dayem AA, Cho S-G. Correlation between oxidative stress, nutrition, and cancer initiation. Int J Mol Sci. 2017;18(7):1544. doi: 10.3390/ijms18071544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49(11):1603–1616. doi: 10.1016/j.freeradbiomed.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang HM, Zhang Y. Melatonin: a well-documented antioxidant with conditional pro-oxidant actions. J Pineal Res. 2014;57(2):131–146. doi: 10.1111/jpi.12162. [DOI] [PubMed] [Google Scholar]
- 61.Galano A, Tan DX, Reiter RJ. Melatonin as a natural ally against oxidative stress: a physicochemical examination. J Pineal Res. 2011;51(1):1–16. doi: 10.1111/j.1600-079X.2011.00916.x. [DOI] [PubMed] [Google Scholar]
- 62.Li Y, Li S, Zhou Y, Meng X, Zhang J-J, Xu D-P, Li H-B. Melatonin for the prevention and treatment of cancer. Oncotarget. 2017;8(24):39896–39921. doi: 10.18632/oncotarget.16379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sun TC, Liu XC, Yang SH, Song LL, Zhou SJ, Deng SL, Tian L, Cheng LY. Melatonin inhibits oxidative stress and apoptosis in cryopreserved ovarian tissues via Nrf2/HO-1 signaling pathway. Front Mol Biosci. 2020;7:163. doi: 10.3389/fmolb.2020.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.He L, He T, Farrar S, Ji L, Liu T, Ma X. Antioxidants maintain cellular redox homeostasis by elimination of reactive oxygen species. Cell Physiol Biochem. 2017;44(2):532–553. doi: 10.1159/000485089. [DOI] [PubMed] [Google Scholar]
- 65.Yoo YS, Han HG, Jeon YJ. Unfolded protein response of the endoplasmic reticulum in tumor progression and immunogenicity. Oxid Med Cell Longev. 2017;2017:2969271. doi: 10.1155/2017/2969271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu H, Carvalho P, Voeltz GK. Here, there, and everywhere: the importance of ER membrane contact sites. Science. 2018;361(6401):eaan5835. doi: 10.1126/science.aan5835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schönthal AH. Endoplasmic reticulum stress: its role in disease and novel prospects for therapy. Scientifica. 2012;2012:857516. doi: 10.6064/2012/857516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hotamisligil GS. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell. 2010;140(6):900–917. doi: 10.1016/j.cell.2010.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mehrzadi S, Hemati K, Reiter RJ, Hosseinzadeh A. Mitochondrial dysfunction in age-related macular degeneration: melatonin as a potential treatment. Expert Opin Ther Targets. 2020;24(4):359–378. doi: 10.1080/14728222.2020.1737015. [DOI] [PubMed] [Google Scholar]
- 70.Lin Y, Jiang M, Chen W, Zhao T, Wei Y. Cancer and ER stress: Mutual crosstalk between autophagy, oxidative stress and inflammatory response. Biomed Pharmacother. 2019;118:109249. doi: 10.1016/j.biopha.2019.109249. [DOI] [PubMed] [Google Scholar]
- 71.Yun CW, Kim S, Lee JH, Lee SH. Melatonin promotes apoptosis of colorectal cancer cells via superoxide-mediated ER stress by inhibiting cellular prion protein expression. Anticancer Res. 2018;38(7):3951–3960. doi: 10.21873/anticanres.12681. [DOI] [PubMed] [Google Scholar]
- 72.Kim HS, Han TY, Yoo YM. Melatonin-mediated intracellular insulin during 2-deoxy-d-glucose treatment is reduced through autophagy and EDC3 protein in insulinoma INS-1E cells. Oxid Med Cell Longev. 2016;2016:2594703. doi: 10.1155/2016/2594703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zha L, Fan L, Sun G, Wang H, Ma T, Zhong F, Wei W. Melatonin sensitizes human hepatoma cells to endoplasmic reticulum stress-induced apoptosis. J Pineal Res. 2012;52(3):322–331. doi: 10.1111/j.1600-079X.2011.00946.x. [DOI] [PubMed] [Google Scholar]
- 74.Bu LJ, Yu HQ, Fan LL, Li XQ, Wang F, Liu JT, Zhong F, Zhang CJ, Wei W, Wang H, et al. Melatonin, a novel selective ATF-6 inhibitor, induces human hepatoma cell apoptosis through COX-2 downregulation. World J Gastroenterol. 2017;23(6):986–998. doi: 10.3748/wjg.v23.i6.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moreira AJ, Ordoñez R, Cerski CT, Picada JN, García-Palomo A, Marroni NP, Mauriz JL, González-Gallego J. Melatonin activates endoplasmic reticulum stress and apoptosis in rats with diethylnitrosamine-induced hepatocarcinogenesis. PLoS ONE. 2015;10(12):e0144517. doi: 10.1371/journal.pone.0144517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhou B, Lu Q, Liu J, Fan L, Wang Y, Wei W, Wang H, Sun G. Melatonin increases the sensitivity of hepatocellular carcinoma to sorafenib through the PERK-ATF4-beclin1 pathway. Int J Biol Sci. 2019;15(9):1905–1920. doi: 10.7150/ijbs.32550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zheng Y, Tu J, Wang X, Yu Y, Li J, Jin Y, Wu J. The therapeutic effect of melatonin on GC by inducing cell apoptosis and autophagy induced by endoplasmic reticulum stress. Onco Targets Ther. 2019;12:10187–10198. doi: 10.2147/OTT.S226140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yoo YM. Melatonin-mediated insulin synthesis during endoplasmic reticulum stress involves HuD expression in rat insulinoma INS-1E cells. J Pineal Res. 2013;55(2):207–220. doi: 10.1111/jpi.12064. [DOI] [PubMed] [Google Scholar]
- 79.Fan L, Sun G, Ma T, Zhong F, Lei Y, Li X, Wei W. Melatonin reverses tunicamycin-induced endoplasmic reticulum stress in human hepatocellular carcinoma cells and improves cytotoxic response to doxorubicin by increasing CHOP and decreasing survivin. J Pineal Res. 2013;55(2):184–194. doi: 10.1111/jpi.12061. [DOI] [PubMed] [Google Scholar]
- 80.Zhu B, Ma AQ, Yang L, Dang XM. Atorvastatin attenuates bleomycin-induced pulmonary fibrosis via suppressing iNOS expression and the CTGF (CCN2)/ERK signaling pathway. Int J Mol Sci. 2013;14(12):24476–24491. doi: 10.3390/ijms141224476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bento CF, Renna M, Ghislat G, Puri C, Ashkenazi A, Vicinanza M, Menzies FM, Rubinsztein DC. Mammalian autophagy: how does it work? Annu Rev Biochem. 2016;85:685–713. doi: 10.1146/annurev-biochem-060815-014556. [DOI] [PubMed] [Google Scholar]
- 82.Glick D, Barth S, Macleod KF. Autophagy: cellular and molecular mechanisms. J Pathol. 2010;221(1):3–12. doi: 10.1002/path.2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Noda NN, Inagaki F. Mechanisms of autophagy. Annu Rev Biophys. 2015;44:101–122. doi: 10.1146/annurev-biophys-060414-034248. [DOI] [PubMed] [Google Scholar]
- 84.Stolz A, Ernst A, Dikic I. Cargo recognition and trafficking in selective autophagy. Nat Cell Biol. 2014;16(6):495–501. doi: 10.1038/ncb2979. [DOI] [PubMed] [Google Scholar]
- 85.Song S, Tan J, Miao Y, Li M, Zhang Q. Crosstalk of autophagy and apoptosis: Involvement of the dual role of autophagy under ER stress. J Cell Physiol. 2017;232:2977–2984. doi: 10.1002/jcp.25785. [DOI] [PubMed] [Google Scholar]
- 86.B'Chir W, Maurin AC, Carraro V, Averous J, Jousse C, Muranishi Y, Parry L, Stepien G, Fafournoux P, Bruhat A. The eIF2alpha/ATF4 pathway is essential for stress-induced autophagy gene expression. Nucleic Acids Res. 2013;41(16):7683–7699. doi: 10.1093/nar/gkt563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kouroku Y, Fujita E, Tanida I, Ueno T, Isoai A, Kumagai H, Ogawa S, Kaufman RJ, Kominami E, Momoi T. ER stress (PERK/eIF2alpha phosphorylation) mediates the polyglutamine-induced LC3 conversion, an essential step for autophagy formation. Cell Death Differ. 2007;14(2):230–239. doi: 10.1038/sj.cdd.4401984. [DOI] [PubMed] [Google Scholar]
- 88.Margariti A, Li H, Chen T, Martin D, Vizcay-Barrena G, Alam S, Karamariti E, Xiao Q, Zampetaki A, Zhang Z, et al. XBP1 mRNA splicing triggers an autophagic response in endothelial cells through BECLIN-1 transcriptional activation. J Biol Chem. 2013;288(2):859–872. doi: 10.1074/jbc.M112.412783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pattingre S, Tassa A, Qu X, Garuti R, Liang XH, Mizushima N, Packer M, Schneider MD, Levine B. Bcl-2 antiapoptotic proteins inhibit Beclin 1-dependent autophagy. Cell. 2005;122(6):927–939. doi: 10.1016/j.cell.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 90.Yamamoto K, Ichijo H, Korsmeyer SJ. BCL-2 is phosphorylated and inactivated by an ASK1/Jun N-terminal protein kinase pathway normally activated at G(2)/M. Mol Cell Biol. 1999;19(12):8469–8478. doi: 10.1128/MCB.19.12.8469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hoyer-Hansen M, Bastholm L, Szyniarowski P, Campanella M, Szabadkai G, Farkas T, Bianchi K, Fehrenbacher N, Elling F, Rizzuto R, et al. Control of macroautophagy by calcium, calmodulin-dependent kinase kinase-beta, and Bcl-2. Mol Cell. 2007;25(2):193–205. doi: 10.1016/j.molcel.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 92.Zalckvar E, Berissi H, Eisenstein M, Kimchi A. Phosphorylation of Beclin 1 by DAP-kinase promotes autophagy by weakening its interactions with Bcl-2 and Bcl-XL. Autophagy. 2009;5(5):720–722. doi: 10.4161/auto.5.5.8625. [DOI] [PubMed] [Google Scholar]
- 93.Fernandez-Gil BI, Guerra-Librero A, Shen YQ, Florido J, Martínez-Ruiz L, García-López S, Adan C, Rodríguez-Santana C, Acuña-Castroviejo D, Quiñones-Hinojosa A, et al. Melatonin enhances cisplatin and radiation cytotoxicity in head and neck squamous cell carcinoma by stimulating mitochondrial ROS generation, apoptosis, and autophagy. Oxid Med Cell Longev. 2019;2019:7187128. doi: 10.1155/2019/7187128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shen YQ, Guerra-Librero A, Fernandez-Gil BI, Florido J, García-López S, Martinez-Ruiz L, Mendivil-Perez M, Soto-Mercado V, Acuña-Castroviejo D, Ortega-Arellano H, et al. Combination of melatonin and rapamycin for head and neck cancer therapy: Suppression of AKT/mTOR pathway activation, and activation of mitophagy and apoptosis via mitochondrial function regulation. J Pineal Res. 2018;64(3):e12461. doi: 10.1111/jpi.12461. [DOI] [PubMed] [Google Scholar]
- 95.Xiao W, Xiong Z, Xiong W, Yuan C, Xiao H, Ruan H, Song Z, Wang C, Bao L, Cao Q, et al. Melatonin/PGC1A/UCP1 promotes tumor slimming and represses tumor progression by initiating autophagy and lipid browning. J Pineal Res. 2019;67(4):e12607. doi: 10.1111/jpi.12607. [DOI] [PubMed] [Google Scholar]
- 96.Ordonez R, Fernandez A, Prieto-Dominguez N, Martinez L, Garcia-Ruiz C, Fernandez-Checa JC, Mauriz JL, Gonzalez-Gallego J. Ceramide metabolism regulates autophagy and apoptotic cell death induced by melatonin in liver cancer cells. J Pineal Res. 2015;59(2):178–189. doi: 10.1111/jpi.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhou N, Wei ZX, Qi ZX. Inhibition of autophagy triggers melatonin-induced apoptosis in glioblastoma cells. BMC Neurosci. 2019;20(1):63. doi: 10.1186/s12868-019-0545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fan T, Pi H, Li M, Ren Z, He Z, Zhu F, Tian L, Tu M, Xie J, Liu M, et al. Inhibiting MT2-TFE3-dependent autophagy enhances melatonin-induced apoptosis in tongue squamous cell carcinoma. J Pineal Res. 2018;64(2):e12457. doi: 10.1111/jpi.12457. [DOI] [PubMed] [Google Scholar]
- 99.Trivedi PP, Jena GB, Tikoo KB, Kumar V. Melatonin modulated autophagy and Nrf2 signaling pathways in mice with colitis-associated colon carcinogenesis. Mol Carcinog. 2016;55(3):255–267. doi: 10.1002/mc.22274. [DOI] [PubMed] [Google Scholar]
- 100.Chen L, Liu L, Li Y, Gao J. Melatonin increases human cervical cancer HeLa cells apoptosis induced by cisplatin via inhibition of JNK/Parkin/mitophagy axis. In Vitro Cell Dev Biol Anim. 2018;54(1):1–10. doi: 10.1007/s11626-017-0200-z. [DOI] [PubMed] [Google Scholar]
- 101.Bennukul K, Numkliang S, Leardkamolkarn V. Melatonin attenuates cisplatin-induced HepG2 cell death via the regulation of mTOR and ERCC1 expressions. World J Hepatol. 2014;6(4):230–242. doi: 10.4254/wjh.v6.i4.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fattman CL. Apoptosis in pulmonary fibrosis: too much or not enough? Antioxid Redox Signal. 2008;10(2):379–386. doi: 10.1089/ars.2007.1907. [DOI] [PubMed] [Google Scholar]
- 103.Huang K, Zhang J, O'Neill KL, Gurumurthy CB, Quadros RM, Tu Y, Luo X. Cleavage by Caspase 8 and mitochondrial membrane association activate the BH3-only protein bid during TRAIL-induced apoptosis. J Biol Chem. 2016;291(22):11843–11851. doi: 10.1074/jbc.M115.711051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hollville E, Romero SE, Deshmukh M. Apoptotic cell death regulation in neurons. FEBS J. 2019;286(17):3276–3298. doi: 10.1111/febs.14970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hattori T, Ookawa N, Fujita R, Fukuchi K. Heterodimerization of Bcl-2 and Bcl-X(L) with Bax and Bad in colorectal cancer. Acta oncologica (Stockholm, Sweden) 2000;39(4):495–500. doi: 10.1080/028418600750013410. [DOI] [PubMed] [Google Scholar]
- 106.Thomas S, Quinn BA, Das SK, Dash R, Emdad L, Dasgupta S, Wang X-Y, Dent P, Reed JC, Pellecchia M. Targeting the Bcl-2 family for cancer therapy. Expert Opin Ther Targets. 2013;17(1):61–75. doi: 10.1517/14728222.2013.733001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Thannickal VJ, Horowitz JC. Evolving concepts of apoptosis in idiopathic pulmonary fibrosis. Proc Am Thorac Soc. 2006;3(4):350–356. doi: 10.1513/pats.200601-001TK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Suzuki Y, Takahashi-Niki K, Akagi T, Hashikawa T, Takahashi R. Mitochondrial protease Omi/HtrA2 enhances caspase activation through multiple pathways. Cell Death Differ. 2004;11(2):208–216. doi: 10.1038/sj.cdd.4401343. [DOI] [PubMed] [Google Scholar]
- 109.Sevrioukova IF. Apoptosis-inducing factor: structure, function, and redox regulation. Antioxid Redox Signal. 2011;14(12):2545–2579. doi: 10.1089/ars.2010.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kim C, Kim B. Anti-cancer natural products and their bioactive compounds inducing ER stress-mediated apoptosis: a review. Nutrients. 2018;10(8):1021. doi: 10.3390/nu10081021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liao Y, Fung TS, Huang M, Fang SG, Zhong Y, Liu DX. Upregulation of CHOP/GADD153 during coronavirus infectious bronchitis virus infection modulates apoptosis by restricting activation of the extracellular signal-regulated kinase pathway. J Virol. 2013;87(14):8124–8134. doi: 10.1128/JVI.00626-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Song J, Ma SJ, Luo JH, Liu H, Li L, Zhang ZG, Chen LS, Zhou RX. Downregulation of AKT and MDM2, melatonin induces apoptosis in AGS and MGC803 Cells. Anatomical Rec. 2019;302(9):1544–1551. doi: 10.1002/ar.24101. [DOI] [PubMed] [Google Scholar]
- 113.Proietti S, Cucina A, Dobrowolny G, D'Anselmi F, Dinicola S, Masiello MG, Pasqualato A, Palombo A, Morini V, Reiter RJ, et al. Melatonin down-regulates MDM2 gene expression and enhances p53 acetylation in MCF-7 cells. J Pineal Res. 2014;57(1):120–129. doi: 10.1111/jpi.12150. [DOI] [PubMed] [Google Scholar]
- 114.Lee YJ, Lee JH, Moon JH, Park SY. Overcoming hypoxic-resistance of tumor cells to TRAIL-induced apoptosis through melatonin. Int J Mol Sci. 2014;15(7):11941–11956. doi: 10.3390/ijms150711941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Martín-Renedo J, Mauriz JL, Jorquera F, Ruiz-Andrés O, González P, González-Gallego J. Melatonin induces cell cycle arrest and apoptosis in hepatocarcinoma HepG2 cell line. J Pineal Res. 2008;45(4):532–540. doi: 10.1111/j.1600-079X.2008.00641.x. [DOI] [PubMed] [Google Scholar]
- 116.Cucina A, Proietti S, D’Anselmi F, Coluccia P, Dinicola S, Frati L, Bizzarri M. Evidence for a biphasic apoptotic pathway induced by melatonin in MCF-7 breast cancer cells. J Pineal Res. 2009;46(2):172–180. doi: 10.1111/j.1600-079X.2008.00645.x. [DOI] [PubMed] [Google Scholar]
- 117.Wei JY, Li WM, Zhou LL, Lu QN, He W. Melatonin induces apoptosis of colorectal cancer cells through HDAC4 nuclear import mediated by CaMKII inactivation. J Pineal Res. 2015;58(4):429–438. doi: 10.1111/jpi.12226. [DOI] [PubMed] [Google Scholar]
- 118.Ma Z, Liu D, Di S, Zhang Z, Li W, Zhang J, Xu L, Guo K, Zhu Y, Li X, et al. Histone deacetylase 9 downregulation decreases tumor growth and promotes apoptosis in non-small cell lung cancer after melatonin treatment. J Pineal Res. 2019;67(2):e12587. doi: 10.1111/jpi.12587. [DOI] [PubMed] [Google Scholar]
- 119.Zhao Q, Wang W, Cui J. Melatonin enhances TNF-alpha-mediated cervical cancer HeLa cells death via suppressing CaMKII/Parkin/mitophagy axis. Cancer Cell Int. 2019;19:58. doi: 10.1186/s12935-019-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 120.El-Magd MA, Mohamed Y, El-Shetry ES, Elsayed SA, Abo Gazia M, Abdel-Aleem GA, Shafik NM, Abdo WS, El-Desouki NI, Basyony MA. Melatonin maximizes the therapeutic potential of non-preconditioned MSCs in a DEN-induced rat model of HCC. Biomed Pharmacother. 2019;114:108732. doi: 10.1016/j.biopha.2019.108732. [DOI] [PubMed] [Google Scholar]
- 121.Jung JH, Shin EA, Kim JH, Sim DY, Lee H, Park JE, Lee HJ, Kim SH. NEDD9 inhibition by miR-25–5p activation is critically involved in co-treatment of melatonin- and pterostilbene-induced apoptosis in colorectal cancer cells. Cancers. 2019;11(11):1684. doi: 10.3390/cancers11111684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kim JH, Jeong SJ, Kim B, Yun SM, Choi DY, Kim SH. Melatonin synergistically enhances cisplatin-induced apoptosis via the dephosphorylation of ERK/p90 ribosomal S6 kinase/heat shock protein 27 in SK-OV-3 cells. J Pineal Res. 2012;52(2):244–252. doi: 10.1111/j.1600-079X.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- 123.Woo SM, Min KJ, Kwon TK. Melatonin-mediated Bim up-regulation and cyclooxygenase-2 (COX-2) down-regulation enhances tunicamycin-induced apoptosis in MDA-MB-231 cells. J Pineal Res. 2015;58(3):310–320. doi: 10.1111/jpi.12217. [DOI] [PubMed] [Google Scholar]
- 124.Zakki SA, Muhammad JS, Li JL, Sun L, Li ML, Feng QW, Li YL, Cui ZG, Inadera H. Melatonin triggers the anticancer potential of phenylarsine oxide via induction of apoptosis through ROS generation and JNK activation. Metallomics Integr Biometal Sci. 2020;12:396–407. doi: 10.1039/C9MT00238C. [DOI] [PubMed] [Google Scholar]
- 125.Gonzalez-Gonzalez A, Gonzalez A, Alonso-Gonzalez C, Menendez-Menendez J, Martinez-Campa C, Cos S. Complementary actions of melatonin on angiogenic factors, the angiopoietin/Tie2 axis and VEGF, in cocultures of human endothelial and breast cancer cells. Oncol Rep. 2018;39(1):433–441. doi: 10.3892/or.2017.6070. [DOI] [PubMed] [Google Scholar]
- 126.Kumari R, Rawat K, Kumari A, Shrivastava A. Amelioration of Dalton's lymphoma-induced angiogenesis by melatonin. Tumour Biol. 2017;39(6):1010428317705758. doi: 10.1177/1010428317705758. [DOI] [PubMed] [Google Scholar]
- 127.Zonta YR, Martinez M, Camargo IC, Domeniconi RF, Lupi Junior LA, Pinheiro PF, Reiter RJ, Martinez FE, Chuffa LG. Melatonin reduces angiogenesis in serous papillary ovarian carcinoma of ethanol-preferring rats. Int J Mol Sci. 2017;18(4):763. doi: 10.3390/ijms18040763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gelaleti GB, Borin TF, Maschio-Signorini LB, Moschetta MG, Hellmen E, Viloria-Petit AM, Zuccari D. Melatonin and IL-25 modulate apoptosis and angiogenesis mediators in metastatic (CF-41) and non-metastatic (CMT-U229) canine mammary tumour cells. Vet Comp Oncol. 2017;15(4):1572–1584. doi: 10.1111/vco.12303. [DOI] [PubMed] [Google Scholar]
- 129.González A, González-González A, Alonso-González C, Menéndez-Menéndez J, Martínez-Campa C, Cos S. Melatonin inhibits angiogenesis in SH-SY5Y human neuroblastoma cells by downregulation of VEGF. Oncol Rep. 2017;37(4):2433–2440. doi: 10.3892/or.2017.5446. [DOI] [PubMed] [Google Scholar]
- 130.Wang RX, Liu H, Xu L, Zhang H, Zhou RX. Melatonin downregulates nuclear receptor RZR/RORgamma expression causing growth-inhibitory and anti-angiogenesis activity in human gastric cancer cells in vitro and in vivo. Oncol Lett. 2016;12(2):897–903. doi: 10.3892/ol.2016.4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Jardim-Perassi BV, Lourenco MR, Doho GM, Grigolo IH, Gelaleti GB, Ferreira LC, Borin TF, Moschetta MG, Pires de Campos Zuccari DA. Melatonin regulates angiogenic factors under hypoxia in breast cancer cell lines. Anticancer Agents Med Chem. 2016;16(3):347–358. doi: 10.2174/1871520615666150511094201. [DOI] [PubMed] [Google Scholar]
- 132.Talib WH, Saleh S. Propionibacterium acnes augments antitumor, anti-angiogenesis and immunomodulatory effects of melatonin on breast cancer implanted in mice. PLoS ONE. 2015;10(4):e0124384. doi: 10.1371/journal.pone.0124384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sohn EJ, Won G, Lee J, Lee S, Kim SH. Upregulation of miRNA3195 and miRNA374b mediates the anti-angiogenic properties of melatonin in hypoxic PC-3 prostate cancer cells. J Cancer. 2015;6(1):19–28. doi: 10.7150/jca.9591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Carbajo-Pescador S, Ordonez R, Benet M, Jover R, Garcia-Palomo A, Mauriz JL, Gonzalez-Gallego J. Inhibition of VEGF expression through blockade of Hif1alpha and STAT3 signalling mediates the anti-angiogenic effect of melatonin in HepG2 liver cancer cells. Br J Cancer. 2013;109(1):83–91. doi: 10.1038/bjc.2013.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kim KJ, Choi JS, Kang I, Kim KW, Jeong CH, Jeong JW. Melatonin suppresses tumor progression by reducing angiogenesis stimulated by HIF-1 in a mouse tumor model. J Pineal Res. 2013;54(3):264–270. doi: 10.1111/j.1600-079X.2012.01030.x. [DOI] [PubMed] [Google Scholar]
- 136.Jardim-Perassi BV, Arbab AS, Ferreira LC, Borin TF, Varma NR, Iskander AS, Shankar A, Ali MM, de Campos Zuccari DA. Effect of melatonin on tumor growth and angiogenesis in xenograft model of breast cancer. PLoS ONE. 2014;9(1):e85311. doi: 10.1371/journal.pone.0085311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Marques JHM, Mota AL, Oliveira JG, Lacerda JZ, Stefani JP, Ferreira LC, Castro TB, Aristizabal-Pachon AF, Zuccari D. Melatonin restrains angiogenic factors in triple-negative breast cancer by targeting miR-152-3p: In vivo and in vitro studies. Life Sci. 2018;208:131–138. doi: 10.1016/j.lfs.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 138.Lacerda JZ, Ferreira LC, Lopes BC, Aristizabal-Pachon AF, Bajgelman MC, Borin TF, Zuccari D. Therapeutic potential of melatonin in the regulation of MiR-148a-3p and angiogenic factors in breast cancer. MicroRNA (Shariqah, United Arab Emirates) 2019;8(3):237–247. doi: 10.2174/2211536608666190219095426. [DOI] [PubMed] [Google Scholar]
- 139.Hsieh MJ, Lin CW, Su SC, Reiter RJ, Chen AW, Chen MK, Yang SF. Effects of miR-34b/miR-892a upregulation and inhibition of ABCB1/ABCB4 on melatonin-induced apoptosis in VCR-resistant oral cancer cells. Mol Ther Nucleic Acids. 2020;19:877–889. doi: 10.1016/j.omtn.2019.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Talib WH. A ketogenic diet combined with melatonin overcomes cisplatin and vincristine drug resistance in breast carcinoma syngraft. Nutrition (Burbank, Los Angeles County, Calif) 2019;72:110659. doi: 10.1016/j.nut.2019.110659. [DOI] [PubMed] [Google Scholar]
- 141.Amin AH, El-Missiry MA, Othman AI, Ali DA, Gouida MS, Ismail AH. Ameliorative effects of melatonin against solid Ehrlich carcinoma progression in female mice. J Pineal Res. 2019;67(2):e12585. doi: 10.1111/jpi.12585. [DOI] [PubMed] [Google Scholar]
- 142.Hao J, Fan W, Li Y, Tang R, Tian C, Yang Q, Zhu T, Diao C, Hu S, Chen M, et al. Melatonin synergizes BRAF-targeting agent vemurafenib in melanoma treatment by inhibiting iNOS/hTERT signaling and cancer-stem cell traits. J Exp Clin Cancer Res. 2019;38(1):48. doi: 10.1186/s13046-019-1036-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sonehara NM, Lacerda JZ, Jardim-Perassi BV, de Paula R, Moschetta-Pinheiro MG, Souza YST, de Andrade JCJ, De Campos Zuccari DAP. Melatonin regulates tumor aggressiveness under acidosis condition in breast cancer cell lines. Oncol Lett. 2019;17(2):1635–1645. doi: 10.3892/ol.2018.9758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Leja-Szpak A, Nawrot-Porabka K, Goralska M, Jastrzebska M, Link-Lenczowski P, Bonior J, Pierzchalski P, Jaworek J. Melatonin and its metabolite N1-acetyl-N2-formyl-5-methoxykynuramine (afmk) enhance chemosensitivity to gemcitabine in pancreatic carcinoma cells (PANC-1) Pharmacol Rep. 2018;70(6):1079–1088. doi: 10.1016/j.pharep.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 145.Kocak N, Donmez H, Yildirim IH. Effects of melatonin on apoptosis and cell differentiation in MCF-7 derived cancer stem cells. Cell Mol Biol. 2018;64(12):56–61. doi: 10.14715/cmb/2018.64.12.12. [DOI] [PubMed] [Google Scholar]
- 146.Krestinina O, Fadeev R, Lomovsky A, Baburina Y, Kobyakova M, Akatov V. Melatonin can strengthen the effect of retinoic acid in HL-60 cells. Int J Mol Sci. 2018;19(10):2873. doi: 10.3390/ijms19102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Odeh LH, Talib WH, Basheti IA. Synergistic effect of thymoquinone and melatonin against breast cancer implanted in mice. J Cancer Res Ther. 2018;14(Supplement):S324–s330. doi: 10.4103/0973-1482.235349. [DOI] [PubMed] [Google Scholar]
- 148.Safaroghli-Azar A, Pourbagheri-Sigaroodi A, Bashash D, Nooshinfar E, Anjam-Najmedini A, Sadeghi S, Rezaie-Tavirani M, Akbari ME. Stimulatory effect of indolic hormone on As2O3 cytotoxicity in breast cancer cells: NF-kappaB-dependent mechanism of action of melatonin. Int J Mol Cell Med. 2018;7(3):158–168. doi: 10.22088/IJMCM.BUMS.7.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Fang Z, Jung KH, Yan HH, Kim SJ, Rumman M, Park JH, Han B, Lee JE, Kang YW, Lim JH, et al. Melatonin synergizes with sorafenib to suppress pancreatic cancer via melatonin receptor and PDGFR-beta/STAT3 Pathway. Cell Physiol Biochem. 2018;47(5):1751–1768. doi: 10.1159/000491058. [DOI] [PubMed] [Google Scholar]
- 150.Franco DG, Moretti IF, Marie SKN. Mitochondria transcription factor A: a putative target for the effect of melatonin on u87mg malignant glioma cell line. Molecules. 2018;23(5):1129. doi: 10.3390/molecules23051129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wei X, Qi Y, Jia N, Zhou Q, Zhang S, Wang Y. Hyperbaric oxygen treatment sensitizes gastric cancer cells to melatonin-induced apoptosis through multiple pathways. J Cell Biochem. 2018;119(8):6723–6731. doi: 10.1002/jcb.26864. [DOI] [PubMed] [Google Scholar]
- 152.Zou ZW, Liu T, Li Y, Chen P, Peng X, Ma C, Zhang WJ, Li PD. Melatonin suppresses thyroid cancer growth and overcomes radioresistance via inhibition of p65 phosphorylation and induction of ROS. Redox Biol. 2018;16:226–236. doi: 10.1016/j.redox.2018.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Song J, Ma SJ, Luo JH, Zhang H, Wang RX, Liu H, Li L, Zhang ZG, Zhou RX. Melatonin induces the apoptosis and inhibits the proliferation of human gastric cancer cells via blockade of the AKT/MDM2 pathway. Oncol Rep. 2018;39(4):1975–1983. doi: 10.3892/or.2018.6282. [DOI] [PubMed] [Google Scholar]
- 154.Yu Z, Tian X, Peng Y, Sun Z, Wang C, Tang N, Li B, Jian Y, Wang W, Huo X, et al. Mitochondrial cytochrome P450 (CYP) 1B1 is responsible for melatonin-induced apoptosis in neural cancer cells. J Pineal Res. 2018;65(1):e12478. doi: 10.1111/jpi.12478. [DOI] [PubMed] [Google Scholar]
- 155.Zhu C, Huang Q, Zhu H. Melatonin inhibits the proliferation of gastric cancer cells through regulating the miR-16-5p-Smad3 pathway. DNA Cell Biol. 2018;37(3):244–252. doi: 10.1089/dna.2017.4040. [DOI] [PubMed] [Google Scholar]
- 156.Chovancova B, Hudecova S, Lencesova L, Babula P, Rezuchova I, Penesova A, Grman M, Moravcik R, Zeman M, Krizanova O. Melatonin-induced changes in cytosolic calcium might be responsible for apoptosis induction in tumour cells. Cell Physiol Biochem. 2017;44(2):763–777. doi: 10.1159/000485290. [DOI] [PubMed] [Google Scholar]
- 157.Gatti G, Lucini V, Dugnani S, Calastretti A, Spadoni G, Bedini A, Rivara S, Mor M, Canti G, Scaglione F, et al. Antiproliferative and pro-apoptotic activity of melatonin analogues on melanoma and breast cancer cells. Oncotarget. 2017;8(40):68338–68353. doi: 10.18632/oncotarget.20124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Shrestha S, Zhu J, Wang Q, Du X, Liu F, Jiang J, Song J, Xing J, Sun D, Hou Q, et al. Melatonin potentiates the antitumor effect of curcumin by inhibiting IKKbeta/NF-kappaB/COX-2 signaling pathway. Int J Oncol. 2017;51(4):1249–1260. doi: 10.3892/ijo.2017.4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Pariente R, Bejarano I, Rodriguez AB, Pariente JA, Espino J. Melatonin increases the effect of 5-fluorouracil-based chemotherapy in human colorectal adenocarcinoma cells in vitro. Mol Cell Biochem. 2018;440(1–2):43–51. doi: 10.1007/s11010-017-3154-2. [DOI] [PubMed] [Google Scholar]
- 160.Lu JJ, Fu L, Tang Z, Zhang C, Qin L, Wang J, Yu Z, Shi D, Xiao X, Xie F, et al. Melatonin inhibits AP-2beta/hTERT, NF-kappaB/COX-2 and Akt/ERK and activates caspase/Cyto C signaling to enhance the antitumor activity of berberine in lung cancer cells. Oncotarget. 2016;7(3):2985–3001. doi: 10.18632/oncotarget.6407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Li W, Fan M, Chen Y, Zhao Q, Song C, Yan Y, Jin Y, Huang Z, Lin C, Wu J. Melatonin induces cell apoptosis in AGS Cells through the activation of JNK and P38 MAPK and the suppression of nuclear Factor-Kappa B: a novel therapeutic implication for gastric cancer. Cell Physiol Biochem. 2015;37(6):2323–2338. doi: 10.1159/000438587. [DOI] [PubMed] [Google Scholar]
- 162.Chuffa LG, Alves MS, Martinez M, Camargo IC, Pinheiro PF, Domeniconi RF, Junior LA, Martinez FE. Apoptosis is triggered by melatonin in an in vivo model of ovarian carcinoma. Endocr Relat Cancer. 2016;23(2):65–76. doi: 10.1530/ERC-15-0463. [DOI] [PubMed] [Google Scholar]
- 163.Pariente R, Pariente JA, Rodríguez AB, Espino J. Melatonin sensitizes human cervical cancer HeLa cells to cisplatin-induced cytotoxicity and apoptosis: effects on oxidative stress and DNA fragmentation. J Pineal Res. 2016;60(1):55–64. doi: 10.1111/jpi.12288. [DOI] [PubMed] [Google Scholar]
- 164.Codenotti S, Battistelli M, Burattini S, Salucci S, Falcieri E, Rezzani R, Faggi F, Colombi M, Monti E, Fanzani A. Melatonin decreases cell proliferation, impairs myogenic differentiation and triggers apoptotic cell death in rhabdomyosarcoma cell lines. Oncol Rep. 2015;34(1):279–287. doi: 10.3892/or.2015.3987. [DOI] [PubMed] [Google Scholar]
- 165.Tosun M, Soysal Y, Mas NG, Karabekir HS. Comparison of the effects of 13-cis retinoic acid and melatonin on the viabilities of SH-SY5Y neuroblastoma cell line. J Korean Neurosurg Soc. 2015;57(3):147–151. doi: 10.3340/jkns.2015.57.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Laothong U, Hiraku Y, Oikawa S, Intuyod K, Murata M, Pinlaor S. Melatonin induces apoptosis in cholangiocarcinoma cell lines by activating the reactive oxygen species-mediated mitochondrial pathway. Oncol Rep. 2015;33(3):1443–1449. doi: 10.3892/or.2015.3738. [DOI] [PubMed] [Google Scholar]
- 167.Plaimee P, Weerapreeyakul N, Barusrux S, Johns NP. Melatonin potentiates cisplatin-induced apoptosis and cell cycle arrest in human lung adenocarcinoma cells. Cell Prolif. 2015;48(1):67–77. doi: 10.1111/cpr.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xu L, Jin QD, Gong X, Liu H, Zhou RX. Anti-gastric cancer effect of melatonin and Bcl-2, Bax, p21 and p53 expression changes. Sheng li xue bao : [Acta physiologica Sinica] 2014;66(6):723–729. [PubMed] [Google Scholar]
- 169.Plaimee P, Weerapreeyakul N, Thumanu K, Tanthanuch W, Barusrux S. Melatonin induces apoptosis through biomolecular changes, in SK-LU-1 human lung adenocarcinoma cells. Cell Prolif. 2014;47(6):564–577. doi: 10.1111/cpr.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kim W, Jeong JW, Kim JE. CCAR2 deficiency augments genotoxic stress-induced apoptosis in the presence of melatonin in non-small cell lung cancer cells. Tumour Biol. 2014;35(11):10919–10929. doi: 10.1007/s13277-014-2370-6. [DOI] [PubMed] [Google Scholar]
- 171.Hong Y, Won J, Lee Y, Lee S, Park K, Chang KT, Hong Y. Melatonin treatment induces interplay of apoptosis, autophagy, and senescence in human colorectal cancer cells. J Pineal Res. 2014;56(3):264–274. doi: 10.1111/jpi.12119. [DOI] [PubMed] [Google Scholar]
- 172.Park EJ, Woo SM, Min KJ, Kwon TK. Transcriptional and post-translational regulation of Bim controls apoptosis in melatonin-treated human renal cancer Caki cells. J Pineal Res. 2014;56(1):97–106. doi: 10.1111/jpi.12102. [DOI] [PubMed] [Google Scholar]
- 173.Perdomo J, Cabrera J, Estevez F, Loro J, Reiter RJ, Quintana J. Melatonin induces apoptosis through a caspase-dependent but reactive oxygen species-independent mechanism in human leukemia Molt-3 cells. J Pineal Res. 2013;55(2):195–206. doi: 10.1111/jpi.12062. [DOI] [PubMed] [Google Scholar]
- 174.Zhang S, Qi Y, Zhang H, He W, Zhou Q, Gui S, Wang Y. Melatonin inhibits cell growth and migration, but promotes apoptosis in gastric cancer cell line, SGC7901. Biotechn Histochem. 2013;88(6):281–289. doi: 10.3109/10520295.2013.769633. [DOI] [PubMed] [Google Scholar]
- 175.Wang J, Guo W, Chen W, Yu W, Tian Y, Fu L, Shi D, Tong B, Xiao X, Huang W, et al. Melatonin potentiates the antiproliferative and pro-apoptotic effects of ursolic acid in colon cancer cells by modulating multiple signaling pathways. J Pineal Res. 2013;54(4):406–416. doi: 10.1111/jpi.12035. [DOI] [PubMed] [Google Scholar]
- 176.Xu C, Wu A, Zhu H, Fang H, Xu L, Ye J, Shen J. Melatonin is involved in the apoptosis and necrosis of pancreatic cancer cell line SW-1990 via modulating of Bcl-2/Bax balance. Biomed Pharmacother. 2013;67(2):133–139. doi: 10.1016/j.biopha.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 177.Li W, Wang Z, Chen Y, Wang K, Lu T, Ying F, Fan M, Li Z, Wu J. Melatonin treatment induces apoptosis through regulating the nuclear factor-kappaB and mitogen-activated protein kinase signaling pathways in human gastric cancer SGC7901 cells. Oncol Lett. 2017;13(4):2737–2744. doi: 10.3892/ol.2017.5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gu J, Lu Z, Ji C, Chen Y, Liu Y, Lei Z, Wang L, Zhang HT, Li X. Melatonin inhibits proliferation and invasion via repression of miRNA-155 in glioma cells. Biomed Pharmacother. 2017;93:969–975. doi: 10.1016/j.biopha.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 179.Gelaleti GB, Borin TF, Maschio-Signorini LB, Moschetta MG, Jardim-Perassi BV, Calvinho GB, Facchini MC, Viloria-Petit AM, de Campos Zuccari DAP. Efficacy of melatonin, IL-25 and siIL-17B in tumorigenesis-associated properties of breast cancer cell lines. Life Sci. 2017;183:98–109. doi: 10.1016/j.lfs.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 180.Bejarano I, Espino J, Marchena AM, Barriga C, Paredes SD, Rodríguez AB, Pariente JA. Melatonin enhances hydrogen peroxide-induced apoptosis in human promyelocytic leukaemia HL-60 cells. Mol Cell Biochem. 2011;353(1–2):167–176. doi: 10.1007/s11010-011-0783-8. [DOI] [PubMed] [Google Scholar]
- 181.Um HJ, Park JW, Kwon TK. Melatonin sensitizes Caki renal cancer cells to kahweol-induced apoptosis through CHOP-mediated up-regulation of PUMA. J Pineal Res. 2011;50(4):359–366. doi: 10.1111/j.1600-079X.2010.00851.x. [DOI] [PubMed] [Google Scholar]
- 182.Leja-Szpak A, Jaworek J, Pierzchalski P, Reiter RJ. Melatonin induces pro-apoptotic signaling pathway in human pancreatic carcinoma cells (PANC-1) J Pineal Res. 2010;49(3):248–255. doi: 10.1111/j.1600-079X.2010.00789.x. [DOI] [PubMed] [Google Scholar]
- 183.Casado-Zapico S, Rodriguez-Blanco J, García-Santos G, Martín V, Sánchez-Sánchez AM, Antolín I, Rodriguez C. Synergistic antitumor effect of melatonin with several chemotherapeutic drugs on human Ewing sarcoma cancer cells: potentiation of the extrinsic apoptotic pathway. J Pineal Res. 2010;48(1):72–80. doi: 10.1111/j.1600-079X.2009.00727.x. [DOI] [PubMed] [Google Scholar]
- 184.Martín V, García-Santos G, Rodriguez-Blanco J, Casado-Zapico S, Sanchez-Sanchez A, Antolín I, Medina M, Rodriguez C. Melatonin sensitizes human malignant glioma cells against TRAIL-induced cell death. Cancer Lett. 2010;287(2):216–223. doi: 10.1016/j.canlet.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 185.Jang SS, Kim WD, Park WY. Melatonin exerts differential actions on X-ray radiation-induced apoptosis in normal mice splenocytes and Jurkat leukemia cells. J Pineal Res. 2009;47(2):147–155. doi: 10.1111/j.1600-079X.2009.00694.x. [DOI] [PubMed] [Google Scholar]
- 186.Raza H, John A, Brown EM, Benedict S, Kambal A. Alterations in mitochondrial respiratory functions, redox metabolism and apoptosis by oxidant 4-hydroxynonenal and antioxidants curcumin and melatonin in PC12 cells. Toxicol Appl Pharmacol. 2008;226(2):161–168. doi: 10.1016/j.taap.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 187.García-Santos G, Antolín I, Herrera F, Martín V, Rodriguez-Blanco J, Carrera MdP, Rodriguez C. Melatonin induces apoptosis in human neuroblastoma cancer cells. J Pineal Res. 2006;41(2):130–135. doi: 10.1111/j.1600-079X.2006.00342.x. [DOI] [PubMed] [Google Scholar]
- 188.Majsterek I, Gloc E, Blasiak J, Reiter RJ. A comparison of the action of amifostine and melatonin on DNA-damaging effects and apoptosis induced by idarubicin in normal and cancer cells. J Pineal Res. 2005;38(4):254–263. doi: 10.1111/j.1600-079X.2005.00197.x. [DOI] [PubMed] [Google Scholar]
- 189.Wenzel U, Nickel A, Daniel H. Melatonin potentiates flavone-induced apoptosis in human colon cancer cells by increasing the level of glycolytic end products. Int J Cancer. 2005;116(2):236–242. doi: 10.1002/ijc.20837. [DOI] [PubMed] [Google Scholar]
- 190.Cos S, Mediavilla MD, Fernández R, González-Lamuño D, Sánchez-Barceló EJ. Does melatonin induce apoptosis in MCF-7 human breast cancer cells in vitro? J Pineal Res. 2002;32(2):90–96. doi: 10.1034/j.1600-079x.2002.1821.x. [DOI] [PubMed] [Google Scholar]
- 191.Lu Y-X, Chen D-L, Wang D-S, Chen L-Z, Mo H-Y, Sheng H, Bai L, Wu Q-N, Yu H-E, Xie D. Melatonin enhances sensitivity to fluorouracil in oesophageal squamous cell carcinoma through inhibition of Erk and Akt pathway. Cell Death Dis. 2016;7(10):e2432–e2432. doi: 10.1038/cddis.2016.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Lin PH, Tung YT, Chen HY, Chiang YF, Hong HC, Huang KC, Hsu SP, Huang TC, Hsia SM. Melatonin activates cell death programs for the suppression of uterine leiomyoma cell proliferation. J Pineal Res. 2020;68(1):e12620. doi: 10.1111/jpi.12620. [DOI] [PubMed] [Google Scholar]
- 193.Lee WJ, Chen LC, Lin JH, Cheng TC, Kuo CC, Wu CH, Chang HW, Tu SH, Ho YS. Melatonin promotes neuroblastoma cell differentiation by activating hyaluronan synthase 3-induced mitophagy. Cancer Med. 2019;8(10):4821–4835. doi: 10.1002/cam4.2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Nopparat C, Sinjanakhom P, Govitrapong P. Melatonin reverses H(2) O(2) -induced senescence in SH-SY5Y cells by enhancing autophagy via sirtuin 1 deacetylation of the RelA/p65 subunit of NF-κB. Journal of pineal research 2017;63(1). [DOI] [PubMed]
- 195.Martín V, Sanchez-Sanchez AM, Puente-Moncada N, Gomez-Lobo M, Alvarez-Vega MA, Antolín I, Rodriguez C. Involvement of autophagy in melatonin-induced cytotoxicity in glioma-initiating cells. J Pineal Res. 2014;57(3):308–316. doi: 10.1111/jpi.12170. [DOI] [PubMed] [Google Scholar]
- 196.Liu C, Jia Z, Zhang X, Hou J, Wang L, Hao S, Ruan X, Yu Z, Zheng Y. Involvement of melatonin in autophagy-mediated mouse hepatoma H22 cell survival. Int Immunopharmacol. 2012;12(2):394–401. doi: 10.1016/j.intimp.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 197.Sagrillo-Fagundes L, Bienvenue-Pariseault J, Vaillancourt C. Melatonin: The smart molecule that differentially modulates autophagy in tumor and normal placental cells. PLoS ONE. 2019;14(1):e0202458. doi: 10.1371/journal.pone.0202458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Galley HF, McCormick B, Wilson KL, Lowes DA, Colvin L, Torsney C. Melatonin limits paclitaxel-induced mitochondrial dysfunction in vitro and protects against paclitaxel-induced neuropathic pain in the rat. J Pineal Res. 2017;63(4):e12444. doi: 10.1111/jpi.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Waseem M, Sahu U, Salman M, Choudhury A, Kar S, Tabassum H, Parvez S. Melatonin pre-treatment mitigates SHSY-5Y cells against oxaliplatin induced mitochondrial stress and apoptotic cell death. PLoS ONE. 2017;12(7):e0180953. doi: 10.1371/journal.pone.0180953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Koşar PA, Nazıroğlu M, Övey İS, Çiğ B. Synergic effects of doxorubicin and melatonin on apoptosis and mitochondrial oxidative stress in MCF-7 breast cancer cells: involvement of TRPV1 channels. J Membr Biol. 2016;249(1–2):129–140. doi: 10.1007/s00232-015-9855-0. [DOI] [PubMed] [Google Scholar]
- 201.Plaimee P, Khamphio M, Weerapreeyakul N, Barusrux S, Johns NP. Immunomodulatory effect of melatonin in SK-LU-1 human lung adenocarcinoma cells co-cultured with peripheral blood mononuclear cells. Cell Prolif. 2014;47(5):406–415. doi: 10.1111/cpr.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ruiz-Rabelo J, Vázquez R, Arjona A, Perea D, Montilla P, Túnez I, Muntané J, Padillo J. Improvement of capecitabine antitumoral activity by melatonin in pancreatic cancer. Pancreas. 2011;40(3):410–414. doi: 10.1097/MPA.0b013e318201ca4f. [DOI] [PubMed] [Google Scholar]
- 203.Lin ZY, Chuang WL. Pharmacologic concentrations of melatonin have diverse influence on differential expressions of angiogenic chemokine genes in different hepatocellular carcinoma cell lines. Biomed Pharmacother. 2010;64(10):659–662. doi: 10.1016/j.biopha.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 204.Padillo FJ, Ruiz-Rabelo JF, Cruz A, Perea MD, Tasset I, Montilla P, Túnez I, Muntané J. Melatonin and celecoxib improve the outcomes in hamsters with experimental pancreatic cancer. J Pineal Res. 2010;49(3):264–270. doi: 10.1111/j.1600-079X.2010.00791.x. [DOI] [PubMed] [Google Scholar]
- 205.Moselhy SS, Al mslmani MA. Chemopreventive effect of lycopene alone or with melatonin against the genesis of oxidative stress and mammary tumors induced by 7,12 dimethyl(a)benzanthracene in sprague dawely female rats. Mol Cell Biochem. 2008;319(1–2):175–180. doi: 10.1007/s11010-008-9890-6. [DOI] [PubMed] [Google Scholar]
- 206.Ruiz-Rabelo JF, Vázquez R, Perea MD, Cruz A, González R, Romero A, Muñoz-Villanueva MC, Túnez I, Montilla P, Muntané J, et al. Beneficial properties of melatonin in an experimental model of pancreatic cancer. J Pineal Res. 2007;43(3):270–275. doi: 10.1111/j.1600-079X.2007.00472.x. [DOI] [PubMed] [Google Scholar]
- 207.Zhu H, Chen Y, Bai LC, Cao XR, Xu R. Different effects of melatonin on X-rays-irradiated cancer cells in a dose-dependent manner. Dose-Response. 2019;17(3):1559325819877271. doi: 10.1177/1559325819877271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Chen YT, Yang CC, Shao PL, Huang CR, Yip HK. Melatonin-mediated downregulation of ZNF746 suppresses bladder tumorigenesis mainly through inhibiting the AKT-MMP-9 signaling pathway. J Pineal Res. 2019;66(1):e12536. doi: 10.1111/jpi.12536. [DOI] [PubMed] [Google Scholar]
- 209.Gurunathan S, Jeyaraj M, Kang MH, Kim JH. Melatonin Enhances Palladium-Nanoparticle-Induced Cytotoxicity and Apoptosis in Human Lung Epithelial Adenocarcinoma Cells A549 and H1229. Antioxidants (Basel, Switzerland) 2020;9(4):357. doi: 10.3390/antiox9040357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Li M, Wu C, Muhammad JS, Yan D, Tsuneyama K, Hatta H, Cui ZG, Inadera H. Melatonin sensitises shikonin-induced cancer cell death mediated by oxidative stress via inhibition of the SIRT3/SOD2-AKT pathway. Redox Biol. 2020;36:101632. doi: 10.1016/j.redox.2020.101632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Zakki SA, Muhammad JS, Li JL, Sun L, Li ML, Feng QW, Li YL, Cui ZG, Inadera H. Melatonin triggers the anticancer potential of phenylarsine oxide via induction of apoptosis through ROS generation and JNK activation. Metallomics Integr Biometal Sci. 2020;12(3):396–407. doi: 10.1039/C9MT00238C. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.