Abstract
Identity concealment affects all sexual minority individuals, with potentially complex mental health implications. Concealing a sexual minority identity can simultaneously generate the stress of hiding, protect against the stress of discrimination, and keep one apart from sexual minority communities and their norms and supports. Not surprisingly, existing studies of the association between sexual orientation concealment and mental health problems show contradictory associations—from positive to negative to null. This meta-analysis attempts to resolve these contradictions. Across 193 studies (n = 92,236) we find a small positive association between sexual orientation concealment and internalizing mental health problems (i.e., depression, anxiety, distress, problematic eating; ESr = 0.126; 95% CI [0.102, 0.151]) and a small negative association between concealment and substance use problems (ESr = ‒0.061; 95% CI [‒0.096, ‒0.026]). The association between concealment and internalizing mental health problems was larger for those studies that assessed concealment as lack of open behavior, those conducted recently, and those with younger samples; it was smaller in exclusively bisexual samples. Year of data collection, study location, and sample gender, education, and racial/ethnic composition did not explain between-study heterogeneity. Results extend existing theories of stigma and sexual minority mental health, suggesting potentially distinct stress processes for internalizing problems versus substance use problems, life course fluctuations in the experience of concealment, distinct experiences of concealment for bisexual individuals, and measurement recommendations for future studies. Small overall effects, heavy reliance on cross-sectional designs, relatively few effects for substance use problems, and the necessarily coarse classification of effect moderators in this meta-analysis suggest future needed methodological advances to further understand the mental health of this still-increasingly visible population.
Keywords: bisexual, depression and anxiety, sexual orientation, stigma concealment, substance use problems
From its start, the field of stigma studies has distinguished between visible and concealable stigmas in terms of the unique psychosocial challenges they pose to the stigmatized. Goffman (1963) highlights this distinction when referring to visible stigmas, such as being a racial or ethnic minority or having an obvious physical disability, as “discredited,” and concealable stigmas, such as being a sexual minority or having had an abortion, as “discreditable.” The visibly stigmatized must contend with the interpersonal costs, including stereotypes and discrimination, of being publicly known as a stigmatized individual; they are thereby, without choice, discredited as a matter of existence in a stigmatizing world. In contrast, those with a concealable stigma uniquely face the intrapsychic costs of choosing whether, when, how, and to whom to disclose their stigma (Chaudoir & Fisher, 2010); they are only discreditable when known by others to possess a stigma. Experimental and observational studies show that concealing a stigma is associated with negative cognitive (e.g., preoccupation), affective (e.g., shame), behavioral (e.g., social avoidance), and self-evaluative (e.g., lack of access to group-based protective resources) consequences (e.g., Frable, Platt, & Hoey, 1998; Major & Gramzow, 1999; Smart & Wegner, 1999), whereas stigma disclosure can potentially alleviate these burdens if met with a supportive reaction (Chaudoir & Fisher, 2010; Pachankis & Bränström, 2018).
The psychosocial challenges of possessing a concealable stigma have been proposed to be an important stressor that begins early in development and partially explains the substantial disparities in mental health problems affecting sexual minorities (e.g., those who identify as lesbian, gay, bisexual; Meyer, 2003). Sexual minorities most commonly become aware of their minority sexual orientation in adolescence and first disclose their sexual orientation several years later, in early adulthood according to the best-available population-based estimates (Calzo, Antonucci, Mays, & Cochran, 2011), and perhaps earlier among more recent cohorts (Russell & Fish, 2019). However, even after their initial disclosure, sexual minority individuals often continue to conceal their sexual orientation by choice or necessity from various individuals and in various situations (Beals, Peplau, & Gable, 2009; Pachankis, Westmaas, & Dougherty, 2011) and even initial disclosure can range from a simple statement to a lifelong conversation (Mohr & Fassinger, 2000). Thus, sexual orientation disclosure is not necessarily only a single event but rather can represent an ongoing response to contextual demands and personal decision making (Chaudoir & Fisher, 2010). Through the cognitive, affective, behavioral, and self-evaluative demands facing individuals with a concealable stigma, the stress of sexual orientation concealment is hypothesized to partially drive sexual minorities’ increased experience of stress-sensitive mental health problems, including internalizing mental health problems (e.g., depression, anxiety, psychological distress, problematic eating) and substance use problems (Pachankis, 2007).
Despite this plausible hypothesis—that sexual orientation concealment should be associated with stress-sensitive mental health problems—quantitative studies of this association have produced contradictory results. Indeed, some studies show positive associations between sexual orientation concealment and mental health problems (e.g., Ayala & Coleman, 2000; Lehavot & Simoni, 2011), others show negative associations (e.g., Dyar & London, 2018; Huebner & Davis, 2005), and still others show no significant association (e.g., Kamen, Jabson, Mustian, & Boehmer, 2017; Lewis, Milletich, Mason, & Derlega, 2014). Explanations for these inconsistencies have only recently emerged (e.g., Jackson & Mohr, 2016; Meidlinger & Hope, 2014; Schrimshaw, Siegel, Downing, & Parsons, 2013) and potentially include: (a) the relative lack of population-based sampling in studies of sexual orientation concealment, yielding systematic underrepresentation of those who highly conceal; (b) inconsistencies in the operationalization of concealment; (c) use of different mental health outcomes, including internalizing mental health problems and substance use problems, without consideration of their conceptually meaningful distinctions; and (d) typically unexamined contextual and personal background factors that might affect the association between sexual orientation concealment and mental health problems.
The Challenge of Studying Sexual Minorities Who Conceal
Any study of sexual orientation concealment faces the known methodological challenges of ascertaining representative sexual minority samples (Meyer & Wilson, 2009) combined with the added challenge of ascertaining individuals across the range of concealment experiences, especially those who are highly concealed. Only two published studies of sexual orientation concealment and mental health problems have used probability-based sampling, in which all residents of the geographic area of study have equal likelihood of being selected into the sample. The results of these studies—that concealment is associated with fewer mental health problems, at least among some sexual minorities (Pachankis, Cochran, & Mays, 2015; van der Star, Pachankis, & Bränström, 2019)—perhaps contradict the assumption drawn across the more common nonrepresentative sampling approaches—that concealment predicts greater mental health problems (e.g., Jackson & Mohr, 2016). Yet studies relying on nonprobability samples overrepresent the experience of sexual minorities who are relatively out and who are otherwise unrepresentative of the general sexual minority population (e.g., consistently younger; Hottes, Bogaert, Rhodes, Brennan, & Gesink, 2016; Kuyper, Fernee, & Keuzenkamp, 2016).
Highlighting the importance of probability-based sampling for sexual orientation concealment-related research questions in particular, the two published studies utilizing such sampling find that a sizable proportion (around 10%) of sexual minorities, in both California (Pachankis et al., 2015) and Sweden (van der Star et al., 2019), report completely concealing their sexual orientation from all others. One of these studies found that sexual minority men who have never told another person of their sexual minority status experienced significantly lower odds of major depression than out sexual minority men (Pachankis et al., 2015), whereas the other found that sexual orientation concealment protects against depression for sexual minorities with high social support (van der Star et al., 2019). Population-based studies would likely find that sexual minority individuals living in less-supportive environments are even more likely to conceal their sexual orientation from all others, with potentially distinct pathways to and buffers against mental health problems compared with those living in California and Sweden (Pachankis & Bränström, 2018).
Yet, even probability-based sampling cannot overcome the fact that some sexual minorities will not feel comfortable identifying themselves as such to researchers. For example, 30% of sexual minority male respondents in a nonprobability-based study indicate that they would not provide their sexual orientation on a national health survey (Ferlatte, Hottes, Trussler, & Marchand, 2017), with significant impact on estimates of mental health outcomes (Hottes et al., 2016). This challenge is amplified by the fact that most studies of sexual orientation concealment identify their samples through their endorsement of a sexual minority identity (e.g., as lesbian, gay, or bisexual; e.g., Puckett, Maroney, Levitt, & Horne, 2016), rather than a recent and/or persistent pattern of same-sex behavior or same-sex attraction, thereby excluding sexual minority individuals who might be uncomfortable identifying as such despite otherwise possessing a sexual minority orientation. Even more challenging is that, theoretically, some sexual minorities might not feel comfortable identifying as such even to themselves (Stein, 1999). Thus, studies of sexual orientation concealment will always be biased by the very phenomenon under investigation. Although this problem poses particular challenge to generating accurate estimates of the size of the sexual minority population and prevalence estimates of mental health problems therein, it poses less threat to the validity of studies examining associations between mental health problems and its determinants, as long as there is sufficient variation in both (Meyer & Wilson, 2009).
The Inconsistent Operationalization of Sexual Orientation Concealment
The inconsistent operationalization of sexual orientation concealment across studies has also been raised as a potential explanation for the inconsistent associations between sexual orientation concealment and mental health (Meidlinger & Hope, 2014), but has received scant empirical attention. Indeed, measures of concealment range from self-reports of a lack of sexual orientation disclosure—a relatively objective behavior (e.g., spoken disclosure of one’s sexual orientation to others)—to self-reports of general, more poorly defined states such as a lack of general “openness” (e.g., “Are you open about your sexual orientation with [a] family, with [b] friends, with [c] acquaintances, with [d] colleagues?” Persson, Pfaus, & Ryder, 2015), or a lack of public knowledge (e.g., “how many people know [that you are a sexual minority]?” Sandfort, Bos, & Reddy, 2018). As reviewed below, these approaches capture potentially distinct phenomena with distinct implications for mental health.
Terminology
Here we review not only the variability in how self-report scales operationalize concealment (from the absence of active behavioral disclosure to more general states), but also the variability in terms used to describe it. Across studies, the construct is variably referred to as a lack of disclosure (e.g., Rosario, Schrimshaw, & Hunter, 2009), lack of open behavior (e.g., Kosciw, Palmer, & Kull, 2015), which is also sometimes called a lack of outness (e.g., Paul, Smith, Mohr, & Ross, 2014); and lack of general openness (e.g., Meidlinger & Hope, 2014). Throughout this review, we treat a lack of disclosure as the lack of an “active indication of one’s sexual orientation through speech or action” (Meidlinger & Hope, 2014; p. 490). Lack of open behavioral refers to whether and to what extent one discusses or otherwise behaviorally manages their sexual orientation in interactions with others (Mohr & Fassinger, 2000). Lack of general openness, in contrast, represents one’s perception that they conceal their sexual orientation; however, lack of general openness does not necessarily capture whether or not disclosure has occurred. Lack of public knowledge represents an additional related construct referring to one’s perception that others’ do not know about one’s sexual orientation, regardless of whether or not disclosure has occurred (Sandfort et al., 2018).
We use concealment as an umbrella term for the related constructs we explore throughout this article (e.g., Pachankis, 2007). Concealment refers to a behavioral construct (e.g., the observable reality of not disclosing or not discussing one’s sexual orientation) informed by cognitive factors (i.e., the perception that one is not open with others about their sexual orientation and that others are not aware of one’s sexual orientation). In addition to including reports of behavioral manifestations, our operationalization of concealment also includes these latter cognitive factors given that the self-perception of not being open with others and the perception of others’ not knowing one’s sexual orientation are likely strong indicators of one’s actual concealment behavior.
When referring to the specific behavioral or cognitive aspects of concealment, we use the respective terms “lack of disclosure,” “lack of open behavior,” “lack of general openness,” and “lack of public knowledge” intentionally. Of course, we are also intentional about direction, such that we always refer to concealment in terms of a lack of disclosure, lack of openness, lack of general openness, and lack of public knowledge. We do this for ease of interpretation despite the fact that many studies frame concealment in terms of its opposite (e.g., disclosure).
In the following sections, we review various approaches to measuring concealment organized into four categories: lack of disclosure, lack of open behavior, lack of general openness, and lack of public knowledge.
Lack of Active Disclosure (Category 1)
Several studies assess sexual orientation concealment as a behavior, namely the number or proportion of people in a given social category (e.g., friends, family, medical providers) to whom a sexual minority individual has not explicitly disclosed their sexual orientation (e.g., Ragins, Singh, & Cornwell, 2007; Shilo & Savaya, 2012). Because it focuses on objective behavior—namely, explicit disclosure acts to distinct people—this approach likely more reliably assesses concealment than those that rely on self-report of less behaviorally defined states, such as a lack of general openness. This assessment approach effectively distinguishes, for example, between an individual who has not shared their sexual orientation with many people in many domains from an individual who has actively disclosed their sexual orientation to many family, friends, and coworkers. Across these studies, the number or proportion of people to whom one has not disclosed their sexual orientation is typically (e.g., Shilo & Savaya, 2012), although not always (Bosker, 2002; Oetjen & Rothblum, 2000; Ragins et al., 2007), related to more symptoms of depression, anxiety, and general psychological distress.
Lack of Open Behavior (Category 2)
Recognizing that disclosure is not necessarily a static event with static interpersonal and mental health implications, other studies have attempted to capture both whether others know or do not know about one’s sexual orientation and how frequently or infrequently one’s sexual orientation is presently discussed in various relationships (e.g., Mohr & Fassinger, 2000). Because this approach captures lack of active discussion, or other behavioral indicators of concealing one’s sexual orientation (e.g., the monitoring of appearance or mannerisms; Jackson & Mohr, 2016), it can be considered relatively behavioral in nature, although importantly, it does not capture lack of active disclosure (i.e., direct explicit statement of one’s sexual orientation) unlike those measures in Category 1. The most common measure that employs this approach—the Outness Inventory (Mohr & Fassinger, 2000)—asks respondents to describe their relationships with 11 categories of people (e.g., mother, father, work peers) by selecting one of seven descriptions that combine whether those people know of their sexual orientation (from “definitely does not know” to “definitely knows”) with how often they openly talk about it with those people (from “never” to “openly”). This assessment approach can distinguish, for example, between an individual who does not discuss their sexual orientation, takes steps to hide or downplay their orientation, and of whose sexual orientation few others are aware from an individual who openly discusses their sexual orientation at least on occasion and does not particularly hide or downplay verbal or behavioral indicators of their sexual orientation. Studies that use the Outness Inventory and similar scales (e.g., Clemens, 2004) sometimes find positive associations between sexual orientation concealment and mental health problems (e.g., Birichi, 2015; Chiang, 2009; Foster, Brewster, Velez, Eklund, & Keum, 2017) and sometimes find negative or no such association (e.g., Beaber, 2008; Livingston, Christianson, & Cochran, 2016; Nance, 2008; Paul et al., 2014).
Lack of General Openness (Category 3)
A less behavioral, more abstract way of assessing sexual orientation concealment is to measure concealment as a general state by asking sexual minorities to indicate how generally open or not open they are (e.g., McGarrity & Huebner, 2014; Pilkington & D’Augelli, 1995). This approach does not assess specific behavior, unlike those that assess lack of active disclosure (Category 1) or lack of open behavior (Category 2). This approach can simply distinguish individuals who do not believe or perceive that they are open about their sexual orientation from those who do. Because this approach relies on sexual minorities’ overall perceptions of their concealment, it is likely influenced by general psychological tendencies, reporting style, and personality factors (Larson, Chastain, Hoyt, & Ayzenberg, 2015). To the degree that these factors similarly influence both the relevant predictors (e.g., concealment) and outcomes (e.g., reports of depression, anxiety, or psychological distress), this approach might yield inflated estimates due to same-source confounding (Watson & Pennebaker, 1989). In fact, many studies using this approach find positive associations between lack of general openness and mental health problems (e.g., Meidlinger & Hope, 2014; Velez, Moradi, & Brewster, 2013), although whether these associations are valid or instead due to same-source confounding remains unknown.
Lack of Public Knowledge (Category 4)
Some concealment measures altogether avoid capturing any active behavioral indicators of concealment (e.g., lack of active disclosure, lack of open behaviors, lack of general openness) and instead only assess whether others do not know about one’s sexual orientation (e.g., Sandfort et al., 2018). Assessing concealment as whether others do not know about one’s sexual orientation weakens construct validity because whether or not others know about one’s sexual orientation is influenced by numerous, often unexamined factors potentially unrelated to a person’s behavioral attempts to conceal. In fact, for some sexual minorities, “being out” (i.e., being known as a sexual minority) represents a nonvolitional, externally imposed circumstance. For example, if a sexual minority is discovered engaging in same-sex sexual behavior, news of their behavior and of their assumed sexual minority identity could become public knowledge. Although this person would be “not concealed” according to a scale that simply assesses others’ knowledge of their sexual orientation, they might have never disclosed their sexual orientation and, instead, might have preferred to keep it concealed (D’Augelli, Hershberger, & Pilkington, 1998; Friedman, Marshal, Stall, Cheong, & Wright, 2008). As another example, gender nonconforming expression represents a visible sign through which others may (often correctly) assume one’s sexual orientation even without disclosure (e.g., Rieger, Linsenmeier, Gygax, Garcia, & Bailey, 2010). At the same time, for most individuals, lack of public knowledge is likely a strong indicator of whether that person has, in fact, successfully concealed their sexual orientation. Still, studies assessing sexual orientation concealment in this way tend to produce small (e.g., Kuyper & Bos, 2016) or nonsignificant (e.g., Sandfort et al., 2018) associations with mental health problems.
Use of Dichotomous Versus Continuous Measures of Concealment
Studies that use dichotomous measures of concealment should show smaller associations with mental health problems than those that use continuous measures. Dichotomous measures of concealment likely preclude capturing at least some variance in the phenomenon under study, thereby excluding important information, missing any nonlinearity in associations with mental health problems, and reducing statistical power to detect associations with mental health problems (Altman & Royston, 2006).
Distinctions Between Internalizing Mental Health Problems and Substance Use Problems in the Study of Sexual Minority Mental Health Determinants
Whether the association between concealment and mental health problems differs depending on the specific mental health problem under investigation has not been systematically examined despite its importance for theoretical accounts of sexual minority stigma, stress, and mental health.
Most studies of the association between sexual orientation concealment and mental health examine depression, anxiety, and general psychological distress as outcomes (Jackson & Mohr, 2016; Meidlinger & Hope, 2014). A few other studies examine problematic eating and substance use problems (Currin et al., 2018; Lehavot & Simoni, 2011; Mason, Lewis, & Heron, 2017; Watson, Velez, Brownfield, & Flores, 2016). All of these mental health problems are united in being particularly sensitive to social stressors such as concealment (Hammen, 2005; Mineka & Zinbarg, 2006) and in being elevated among sexual minorities compared with heterosexuals (Cochran & Mays, 2009; Feldman & Meyer, 2007; Meyer, 2003). However, substance use problems differ from depression, anxiety, psychological distress, and problematic eating in being an externalizing mental health problem (Forbush et al., 2010; Krueger, Markon, Patrick, Benning, & Kramer, 2007; Mitchell, Wolf, Reardon, & Miller, 2014). Whereas internalizing mental health problems share high comorbidity and underlying mechanisms grounded in cognitive-affective neuroscience models of stress, emotions, and coping (Clark & Watson, 1991; Krueger, Watson, & Barlow, 2005; Shin & Liberzon, 2010), externalizing problems are united in sharing underlying tendencies toward disinhibition (Krueger, Markon, Patrick, & Iacono, 2005). Externalizing problems also differ from internalizing problems in their outward display of behavior, rather than inward direction of distress (Krueger et al., 2005).
Substance use problems are also often influenced by social network characteristics (Rosenquist, Murabito, Fowler, & Christakis, 2010). In fact, a few studies have suggested that the sexual orientation disparity in substance use problems might be at least partially explained by sexual orientation differences in sexual network characteristics (Hatzenbuehler, McLaughlin, & Xuan, 2015), including greater perceptions of normative substance use by sexual minorities compared with heterosexuals (Cochran, Grella, & Mays, 2012; Hatzenbuehler, Corbin, & Fromme, 2008). Yet, most studies simply explain sexual minorities’ greater tendency to use substances in terms of their disproportionate exposure to minority stressors such as concealment and associated discrimination (Feinstein, Dyar, & London, 2017), viewing it through the same theoretical lens as internalizing problems. This approach might obscure distinct determinants of internalizing versus externalizing mental health problems among sexual minorities, which emerging research suggests might exist (Rodriguez-Seijas, Eaton, & Pachankis, 2019).
Sexual orientation concealment is expected to show positive and similarly sized associations with all internalizing problems—whether depression, anxiety, psychological distress, and eating problems—given their high degree of comorbidity and symptom overlap with the cognitive (e.g., rejection hyper-vigilance), affective (e.g., guilt), and behavioral (e.g., avoidance) stressors of concealment (Pachankis, 2007). In fact, similar associations across diverse internalizing mental health problems have been found for other minority stressors, such as internalized homophobia (Newcomb & Mustanski, 2010).
Yet, we hypothesize that concealment might show negative associations with substance use problems given that concealment might keep sexual minorities from the more normative substance use in sexual minority, compared with heterosexual, communities (Cochran et al., 2012; Hatzenbuehler et al., 2008; Hatzenbuehler et al., 2015), likely in part owing to the history of more normative socializing in venues in which substance use is common among sexual minorities (Hughes, Wilsnack, & Kantor, 2016; Trocki, Drabble, & Midanik, 2005). Finding opposite associations for concealment with internalizing mental health problems versus substance use problems would expand minority stress theory’s focus on the solely stress-related consequences of concealment (Meyer, 2003) to other social influences on sexual minority health, including those stemming from exposure to sexual minority community norms and network influences (e.g., Burton, Clark, & Pachankis, 2020; Pachankis et al., 2020).
Similar to the scaling considerations for sexual orientation concealment described above, when measured dichotomously, mental health outcomes are expected to show smaller associations with concealment than when mental health outcomes are measured continuously (Altman & Royston, 2006).
Potential Contextual and Personal Moderators of the Association Between Sexual Orientation Concealment and Mental Health
It is unclear to what extent often-unexamined contextual and personal factors might explain the inconsistent association between concealment and mental health problems across studies (Legate, Ryan, & Weinstein, 2012). Indeed, rather than uniformly placing sexual minorities at risk of stress-sensitive mental health problems, concealment might exert a less stressful effect for some sexual minorities or might even protect some sexual minorities against other minority stressors like homophobic/biphobic discrimination (McGarrity & Huebner, 2014; Pachankis & Bränström, 2018; Pachankis et al., 2015). The ability of concealment to potentiate or protect against stress likely varies as a function of contextual or personal factors. As reviewed below, relevant factors potentially include age, the time period in which sexual minorities live, the geographic location in which sexual minorities live, gender, educational background, race and ethnicity, and bisexuality.
Age
A life course approach to sexual minority mental health and its determinants requires consideration of both age and period effects. In terms of age, although concealment has some adaptive benefits across the life span, those benefits might be more outweighed by concealment’s risks earlier in development. Concealment might pose a greater mental health burden to younger sexual minorities because younger individuals might possess fewer psychological resources for coping with stress than older individuals (Casey, Jones, & Hare, 2008). Further, younger sexual minorities might exist in more constrained environments than older sexual minorities, such as under conditions of parental control or limited options for social or geographic mobility or affirmative mental health care (Durso & Meyer, 2013; Hatzenbuehler & Pachankis, 2016), and therefore have fewer material resources for coping with concealment. Further, to the extent that concealment drives chronic and anxious expectations of rejection and negative emotions such as shame (Pachankis, 2007), evidence suggests that these experiences have their greatest mental health impact during the developmentally sensitive periods of adolescence and young adulthood (Andersen & Teicher, 2008; Charmandari, Kino, Souvatzoglou, & Chrousos, 2003; Leussis & Andersen, 2008; Murphy, Slavich, Rohleder, & Miller, 2013; Romeo et al., 2006). Although outness certainly has risks across the lifespan (Pachankis & Bränström, 2018), including among younger sexual minorities (D’Augelli, 2002), weight of the evidence suggests a stronger association between concealment and mental health problems for younger, compared with older, sexual minorities.
Time Period
Life course models of sexual minority mental health highlight the impact of the rapidly changing societal context surrounding this population (e.g., Cohler & Hammack, 2007). Indeed, the experience of being a sexual minority has changed so rapidly that distinct sexual minority experiences can be found not just across successive generations, but even decade-to-decade or possibly year-to-year (e.g., Hammack, Frost, Meyer, & Pletta, 2018; Russell & Fish, 2019). For instance, over the span of 10 years in the United States, same-sex behavior was decriminalized (2003), federal hate crimes laws were expanded to recognize sexual orientation (2009), sexual minorities were allowed to serve openly in the military (2010), and the definition of marriage as between a man and woman was declared unconstitutional (2013). Concealment might represent an experience whose meaning and mental health implications have changed concomitantly fast over recent history. Given the relatively rapid increase in public support for sexual minorities in many countries in recent periods, concealment might be less adaptive as a protection against discrimination and victimization for sexual minorities today than in years past. In fact, recent evidence shows that the mental health of sexual minorities has improved over time as a function of their decreased exposure to discrimination and victimization (Hatzenbuehler, Bränström, & Pachankis, 2018). At the same time, perhaps today’s more supportive climates raise the threshold required for concealment, such that those who are most burdened by poor mental health are most likely to conceal. In fact, societal improvements affecting the stigmatized can exacerbate inequalities within them, such that those who are otherwise disadvantaged do not benefit as much from those societal improvements as those who are not so relatively disadvantaged (Phelan, Link, & Tehranifar, 2010). Those who conceal for reasons other than societal constraints against openness might also be those who experience poorer mental health as a result of other causes. Conversely, concealment would be expected to be associated with better mental health in past periods given the greater threat facing open sexual minorities. For these reasons, concealment is likely associated with poorer mental health in studies in which data were more recently collected.
Study Location
Theoretical accounts of stigma concealment suggest that sexual minorities living in more structurally homophobic geographic contexts face higher consequences to disclosure than those living in structurally supportive contexts (Pachankis, 2007). In fact, recent data collected across 28 structurally diverse countries finds that sexual orientation concealment is only associated with positive life satisfaction in structurally homophobic contexts, but not in structurally supportive contexts (Pachankis & Bränström, 2018). This effect was mediated by exposure to discrimination and victimization. In structurally homophobic contexts (i.e., those containing discriminatory laws, policies, and community attitudes affecting sexual minorities; Hatzenbuehler, 2016), concealment protected against discrimination and victimization, whereas in structurally supportive contexts (i.e., those with laws, policies and attitudes that offer protection for sexual minorities), the likelihood of discrimination and victimization were equally low for highly concealed and nonconcealed sexual minorities. Mental health problems were not assessed in this study, and to our knowledge, no such cross-country examination of sexual orientation concealment and mental health problems exists. Because most studies of sexual orientation concealment and mental health problems are conducted in North America, insufficient evidence exists from which to hypothesize whether other global regions would demonstrate similar associations between concealment and mental health problems. Also unknown is whether a sufficient number of non–North American studies exists to test such a hypothesis.
Gender
The mental health cost of disclosure is likely greater for sexual minority men than for sexual minority women. Several studies, for instance, find that sexual minority men experience more homophobic victimization than do sexual minority women (Balsam, Rothblum, & Beauchaine, 2005; D’Augelli, Pilkington, & Hershberger, 2002; Herek, 2000). Further, in one of the only population-based studies of sexual orientation concealment and mental health, sexual minority men who had disclosed their sexual orientation reported higher odds of major depressive disorder than sexual minority men who concealed their sexual orientation from all others; sexual minority women experienced comparable odds of depression regardless of their concealment status (Pachankis et al., 2015). Of course, within sexual minority populations, the experience of gender often cannot be separated from the experience of sexual identity, such that sexual minority men often identify as gay men and sexual minority women often identify as lesbian women. Examinations of gender within sexual minority populations are therefore often conflated with these distinct sexual identities.
Educational Attainment
Recent evidence suggests that the health benefits of being out might be limited to sexual minorities with higher educational attainment. In fact, among sexual minority men with higher educational attainment, a positive association between being out and physical health has been found, whereas a negative association exists between being out and physical health for sexual minority men with lower educational attainment (McGarrity & Huebner, 2014). Whereas this evidence is limited to physical health among sexual minority men, it coheres with population-based evidence that sexual minorities, across the gender spectrum, with lower educational attainment are burdened by poorer mental health than those with higher educational attainment (Barnes, Hatzenbuehler, Hamilton, & Keyes, 2014). Further supporting the potential disproportionate mental health benefits of being out for sexual minorities with higher educational attainment, sexual minorities from lower socioeconomic positions are less likely to receive support from sexual minority communities (Barrett & Pollack, 2005) and are more likely to report stress from those communities (Pachankis et al., 2019), thereby diminishing this potential benefit of being out.
Race and Ethnicity
For racial and ethnic minorities, being out as a sexual minority might not confer the same mental health benefit that it does for nonracial/ethnic-minority individuals. First, racial and ethnic identities are often more central than sexual minority identities; therefore, coming out as a sexual minority might be of secondary importance compared with possessing a more central racial or ethnic identity (Akerlund & Cheung, 2000; Ross, 2005). Second, racial and ethnic minorities might face racial and ethnic stigma from within gay communities at the same time that they might lose support from their racial and ethnic minority communities when they are out (Akerlund & Cheung, 2000; Dubé & Savin-Williams, 1999; Ross, 2005). In fact, concealment has shown associations with mental health problems only for White sexual minority men, but not for Latino sexual minority men (Villicana, Delucio, & Biernat, 2016). Research has shown that, compared with White sexual minorities, Latinx sexual minorities might be more likely to engage in tacit disclosure, whereby they do not actively hide their sexual orientation at the same time that they have not disclosed it (e.g., bringing a same-gender partner to a family event despite never having verbally disclosed their sexual orientation). Tacit disclosure might be just as indicative of an authentic self-presentation for some racial and ethnic minorities as verbal disclosure (Villicana et al., 2016). Overall, research suggests that sexual orientation concealment might have weaker implications for mental health among racial and ethnic minority individuals than it does for nonracial/ethnic minorities.
Bisexual Identity
Although bisexual individuals consistently report poorer mental health than gay men and lesbian women (Bostwick, Boyd, Hughes, & McCabe, 2010; Conron, Mimiaga, & Landers, 2010) and are more likely to conceal their sexual orientation than gay men and lesbian women (Balsam & Mohr, 2007; Lewis, Derlega, Brown, Rose, & Henson, 2009; Rosario, Schrimshaw, & Hunter, 2008; Stokes, Vanable, & McKirnan, 1997), existing evidence suggests that concealment has a relatively weaker influence on the mental health of bisexuals than gay men and lesbian women. Although their higher likelihood of concealment might explain why bisexuals experience less homophobic victimization and discrimination than gay men and lesbian women (Chesir-Teran & Hughes, 2009; Herek, 2009; Kuyper & Fokkema, 2011), bisexuals’ sexual identities have been found to be less central to their overall identities than gay men and lesbian women’s sexual identities (Dyar, Feinstein, & London, 2015). Therefore, concealment of a bisexual identity might have a relatively small impact on mental health than concealment of a gay or lesbian identity. Further, to the extent that bisexual individuals’ identities are less reflected in institutions and normative discourse both within general society and within gay and lesbian communities (Steinman, 2000), any protective effects of disclosure, such as increased social support or access to other identity-specific protections (Chaudoir & Fisher, 2010), are likely to be smaller, and thus the costs of concealment are likely not as high as they are for gay and lesbian individuals (Beals et al., 2009).
Aims and Hypotheses
The present meta-analysis aggregates the results of all previous studies that have examined the association between sexual orientation concealment and mental health problems to determine the overall association between these variables. Previous studies typically show null, small, or contradictory associations between sexual orientation concealment and mental health problems. As reviewed above, lack of representative sampling, inconsistent measurement of concealment, lack of conceptual distinction between internalizing and externalizing mental health problems, and unexamined contextual or personal factors in this literature might explain inconsistent effects across studies. Therefore, in addition to calculating the average effect size across studies, we also attempt to examine heterogeneity across studies as a function of approach to operationalizing concealment; mean participant age; time period of data collection; the gender composition of the sample; educational attainment of the sample; racial and ethnic composition of the sample; whether the sample was composed exclusively of bisexual individuals; and whether the study used dichotomous or continuous concealment and mental health scales. Further, to begin to extend the conceptual distinction between internalizing and externalizing mental health problems to theorizing about sexual minority mental health and its determinants, we also examine the association between sexual orientation and mental health problems distinctly for internalizing mental health problems and substance use problems.
In terms of a priori directional hypotheses, we expected that studies utilizing behavioral operationalizations of concealment (e.g., lack of active disclosure, lack of open behavior) will show larger associations between concealment and mental health problems than studies using nonbehavioral operationalizations (e.g., lack of general openness, lack of public knowledge) given potentially extraneous influences captured by nonbehavioral measures. We expected to find the smallest association between concealment operationalized as lack of public knowledge and mental health problems given the threats to construct validity posed by the many potential factors influencing whether others know of one’s sexual orientation.
In terms of contextual and personal moderators of the association between sexual orientation concealment and mental health problems, based on the evidence reviewed above, we hypothesized, a priori, that studies containing younger samples, conducted more recently, composed of mostly men, with a greater proportion of individuals with lower educational attainment, with a greater proportion of White individuals, and whose sample composition is exclusively bisexual would evidence larger associations between concealment and mental health problems. As a post hoc exploration, we examined whether studies utilizing dichotomous measures of concealment and/or mental health would yield smaller effect sizes than those utilizing continuous measures of those constructs. As a second post hoc exploration, we examined whether studies of internalizing problems would show positive associations with concealment, whereas studies of substance use problems would show negative associations with concealment.
Results of this meta-analysis, the first to examine the association between sexual orientation concealment and mental health problems, have the potential to resolve increasingly obvious inconsistencies across studies into these constructs. This study can bring us closer to answering how and under what circumstances sexual orientation concealment—a pervasive aspect of the sexual minority experience—comes to shape the mental health of this increasingly visible population. By testing the above hypotheses, this analysis can support existing, and perhaps advance novel, theories regarding sexual minority mental health.
Method
Inclusion and Exclusion Criteria
Studies included in the final analyses: (a) contained a measure of the statistical association between sexual orientation concealment (i.e., lack of disclosure, lack of open behavior, lack of general openness, lack of public knowledge) and depression, anxiety, general psychological distress, problematic eating, and/or substance use problems or the author provided such an association upon request; (b) included sexual minority participants and reported a separate analyses for these participants; and (c) used unique data in their analyses (i.e., data that were not analyzed in any other report included in the meta-analysis). Otherwise, studies were only excluded if they did not include an appropriate concealment measure or mental health measure or if information necessary for calculating an association between concealment and mental health was not available within the study or provided by the studies’ authors.
Search Strategy
A search strategy was implemented across three electronic databases (i.e., PsycINFO, Medline, and Web of Science) to identify studies related to sexual orientation concealment and mental health problems among sexual minorities. Publication date was not restricted; thus, the search included the earliest relevant studies up until the date the final search was carried out (i.e., May 22, 2019). Using their respective controlled terms, customized search strategies were developed for each database consisting of key terms related to sexual orientation concealment, mental health problems, and sexual minorities (see the Appendix for full PsycINFO search strategy). Databases were searched for both published peer-reviewed studies and dissertations.
A reference librarian, experienced in meta-analytic searches, reviewed our Boolean and proximity indicators, subject headings and controlled terms, search term spelling and syntax, and limits and filters; advised our text word search process (e.g., identifying missing terms, missing word forms); suggested databases to retrieve non–English language studies; and tested our searches.
The reference lists of all records suitable for inclusion were manually checked, and the authors of all records deemed eligible for inclusion were emailed to request potentially relevant unpublished data in their possession. Specifically, we contacted 148 authors of studies initially marked for inclusion to request any unpublished data that may be relevant for inclusion in the meta-analysis. We received replies from 35.1% of authors, leading to the inclusion of an additional 15 studies. We also posted requests for relevant data on the listservs of professional organizations of scholars conducting sexual minority mental health research, resulting in the inclusion of three additional studies. For those studies containing assessments of sexual orientation concealment and mental health problems that were missing other key information (e.g., an effect size), we requested missing information from the authors. Specifically, we contacted 102 authors whose study (or studies) was (were) missing this information; 22% of authors replied with the requested data. In three of these cases, the provided data led us to deem the study as not suitable for inclusion.
Data Extraction
Two reviewers independently screened the abstracts of all records retrieved in the search. Following the abstract review, both reviewers read the full texts of records deemed potentially eligible for inclusion. We generated multiple measures of interrater reliability at various stages of the review process. Cohen’s statistic estimates chance agreement between two coders and removes it from the estimation of reliability (Viera & Garrett, 2005). A Cohen’s κ score was calculated to determine the level of agreement between the two coders at the abstract review and full-text review stages. The following indices were used to interpret the results: values ≤0 indicate no agreement and 0.01–0.20 as none to slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement (McHugh, 2012). Interrater reliability was subtantial at the abstract review (κ = .86) and full-text review stage (κ = .73). Discrepancies between reviewers’ inclusion determinations were solved through further discussion among all study authors.
Data extracted from each record included authors’ name, sample size, type of publication (i.e., journal article, dissertation, or unpublished), year of publication, location, sample characteristics (i.e., age, gender composition, racial and ethnic composition, educational attainment [% some college education or above], and sexual orientation composition [i.e., exclusively bisexual]), sexual orientation concealment measures used, and mental health outcome measures used. Table 1 summarizes all extracted data.
Table 1.
Summary of Hypothesized Moderators in Terms of Their Extracted Information, Coding, and Average Distribution Across Studies
| Moderator | Value | Coding description and criteria | Descriptive statistics |
|---|---|---|---|
| Concealment operationalization | |||
| Lack of active disclosure | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a concealment measure that captured the number or proportion of people in a given social category (e.g., friends, family) to whom a sexual minority individual has not explicitly disclosed their sexual orientation. |
k = 193 No k = 171 (88.6%) Yes k = 22 (11.4%) |
| Lack of open behavior | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a concealment measure that captured both the extent to which people in a given social category (e.g., coworkers, heterosexual friends) do not know about an individual’s sexual orientation and how infrequently one’s sexual orientation is presently discussed in those relationships. |
k = 193 No k = 106 (54.9%) Yes k = 87 (45.1%) |
| Lack of general openness | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a concealment measure that captured an individual’s lack of general openness about their sexual orientation with people in a given social category (e.g., parents, people in general). |
k = 193 No k = 135 (69.9%) Yes k = 58 (30.1%) |
| Lack of public knowledge | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a concealment measure that captured a lack of public knowledge on behalf of people in a given social category (e.g., peers, spouse’s family) regarding an individual’s sexual orientation. |
k = 193 No k = 160 (82.9%) Yes k = 33 (17.1%) |
| Study characteristics | |||
| Time period | Continuous | Continuous variable representing estimated year of data collection (or year of publication minus 8 years for studies lacking this information). |
k = 193 M = 2007 SD = 8 Range = 1983–2019 |
| Study location | 0 = Outside North America 1 = Within North America 2 = Combination of Outside and Within North America |
Categorical variable representing whether the sample was drawn from outside North America, within North America, or a combination of the two. |
k = 193 Outside North America k = 34 (17.6%) Within North America k = 148 (76.7%) Combination k = 9 (4.7%) Missing k = 2 (1.0%) |
| Use of dichotomous measure of concealment | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a dichotomous measure of concealment. |
k = 193 No k = 186 Yes k = 7 |
| Use of dichotomous measure of mental health problems | 0 = No 1 = Yes |
Categorical variable representing whether or not the study used a dichotomous measure of concealment. |
k = 193 No k = 189 Yes k = 4 |
| Sample characteristics | |||
| Age | Continuous | Continuous variable representing the mean age of the sample. |
k = 170 M = 31.60 SD = 10.08 Range = 16.00–66.90 |
| Gender | Continuous | Continuous variable representing the proportion of the sample that identified as cisgender males. |
k = 192 M = 52.44 SD = 35.18 Range = 0–100 |
| Educational attainment | Continuous | Continuous variable representing the proportion that had completed at least some college. |
k = 139 M = 76.57 SD = 23.22 Range = 0–100 |
| Race/ethnicity | 0 = No 1 = Yes |
Categorical variable representing whether or not the majority of participants identified as racial/ethnic minority. |
k = 193 No k = 140 (72.5%) Yes k = 25 (13.0%) Missing k = 28 (14.5%) |
| Exclusive bisexual composition | 0 = No 1 = Yes |
Categorical variable representing whether the sample consisted exclusively of bisexual participants. |
k = 193 No k = 169 (87.6%) Yes = 10 (5.2%) Missing k = 14 (7.3%) |
| Dependent variable characteristics | |||
| Depression symptoms | 0 = No 1 = Yes |
Categorical variable representing whether or not the study included a measure of depression symptoms. |
k = 193 No k = 72 (37.3%) Yes k = 121 (62.7%) |
| Anxiety symptoms | 0 = No 1 = Yes |
Categorical variable representing whether or not the study included a measure of anxiety symptoms (including generalized anxiety, social anxiety, and fear of negative evaluation). |
k = 193 No k = 126 (65.3%) Yes k = 67 (34.7%) |
| General psychological distress | 0 = No 1 = Yes |
Categorical variable representing whether or not the study included a measure of general psychological distress (including rumination and combined measures of anxiety and depression). |
k = 193 No k = 128 (66.3%) Yes k = 65 (33.7%) |
| Problematic eating | 0 = No 1 = Yes |
Categorical variable representing whether or not the study included a measure of problematic eating. |
k = 193 No k = 186 (96.4%) Yes k = 7 (3.6%) |
| Substance use problems | 0 = No 1 = Yes |
Categorical variable representing whether or not the study included a measure of substance use (i.e., drug and alcohol use) problems. |
k = 193 No k = 174 (90.2%) Yes k = 19 (9.8%) |
Most of the included records reported Pearson product–moment correlations. Being an appropriate measure of effect size, the correlation coefficient was therefore chosen as the effect size statistic (ESr). In cases where records did not report a correlation coefficient, a request was sent to the study authors. When the authors did not reply or were unable to retrieve the relevant correlation coefficient, the reported statistics (e.g., from an ANOVA) were converted to ESr, when available.
Measures of Sexual Orientation Concealment
A variety of sexual orientation concealment measures were used in the included studies, which we categorized using the four categories described above: Lack of active disclosure (Category 1), lack of open behavior (Category 2), lack of general openness (Category 3), and lack of public knowledge (Category 4). Studies in Category 1 used a concealment measure that captured the number or proportion of people in a given social category (e.g., friends, family) to whom a sexual minority individual had not explicitly disclosed their sexual orientation. Studies in Category 2 used a concealment measure that captured both the extent to which people in a given social category (e.g., coworkers, heterosexual friends) do not know about an individual’s sexual orientation and how infrequently one’s sexual orientation is presently discussed in those relationships. Studies in Category 3 used a concealment measure that captured an individual’s lack of general openness about their sexual orientation with people in a given social category (e.g., parents, people in general). Studies in Category 4 used a concealment measure that captured a lack of public knowledge among people in a given social category (e.g., peers, spouse’s family) regarding an individual’s sexual orientation.
Concealment measures that captured multiple categories could not be assigned a category but instead only contributed to analyses of pooled effect sizes (e.g., Nash, 1990; Schrimshaw et al., 2013; Shilo & Savaya, 2011). For studies that used multiple measures of sexual orientation concealment (k = 17), separate effect sizes were extracted for each of the four categories. The majority (54.4%) of effects derived from commonly used concealment measures (e.g., the Outness Inventory) with high reliability and established psychometric properties. The remaining effects derive from one-item (31.5%) or multiitem (14.1%) instruments without established reliability.
In our search, we also identified a small number of studies whose concealment measures did not match any of our four a priori concealment categories, but which we nonetheless decided to retain since they did capture sexual orientation concealment. These studies (n = 3) all captured concealment from one other person or a small group of people in a very circumscribed social domain (i.e., mental health providers, Owens, Riggle, & Rostosky, 2007; health care provider, Sun, Tobin, Spikes, & Latkin, 2019; and adult children, Tornello & Patterson, 2018). Although these very specific domains of concealment were not expected to have broad implications for mental health, we nonetheless included these three studies in a sensitivity analysis of our primary analysis to determine the robustness of our results when these specific manifestations of concealment are included.
To establish the reliability of our concealment categorization, one coder classified each measure used in each study. The second coder then reviewed this classification and indicated whether he agreed. Raters agreed on almost every (97.5%) classification of effects into the four concealment categories.
Measures of Mental Health Problems
The studies in the final sample utilized various measures of mental health problems, listed in Table 2. The types of measures were classified into five main categories: depression, anxiety, general psychological distress, problematic eating, and substance use problems, which were further classified as internalizing mental health problems (depression, anxiety, general psychological distress, problematic eating) and substance use problems, based on empirically derived psychiatric classification schemes (Forbush et al., 2010; Krueger & Markon, 2006). For studies that reported more than one outcome or more than one measure of mental health problems, we extracted all relevant data separately. We also included fear of negative evaluation and rumination as outcomes given that fear of negative evaluation is a pathognomonic feature of social anxiety disorder and that rumination is associated with depression and anxiety disorders.
Table 2.
Descriptive Information of Included Studies of Sexual Orientation Concealment and Mental Health Problems
| Study | Type of publication | Sample size | Actual or estimated year of data collection | Study location | Age (M) | Age (SD)d | Proportion cisgender male | Proportion completed some college | Proportion racial/ethnic minority | Exclusive bisexual composition | Concealment operationalization | Mental health outcomes | Effect size (ESr)a |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antebi-Gruszka and Schrimshaw (2018) | Journal article | 203 | 2007–2010 | USA | 36.9 | 11.2 | 100.0 | 69.5 | 73.4 | No | Lack of Active Identity Disclosure; Lack of Public Knowledge | Mental Health Inventory | 0.05 |
| Aranda (2010) | Dissertation | 349b | 2000–2005 | USA | 38.4 | 11.9 | 0.0 | 59.8 | 46.2 | No | Lack of Public Knowledge | Diagnostic Interview Schedule | −0.07 |
| Ayala and Coleman (2000) | Journal article | 117 | 1997–1998 | Canada | – | – | 0.0 | 82.9 | 9.0 | No | Lack of General Openness | Generalized Contentment Scale | 0.30 |
| Baams, Dubas, Russell, Buikema, and van Aken (2018); Kaufman, Baams, and Dubas (2017) | Journal article; Unpublished effect size | 209b | 2014 | The Netherlands | 17.6 | 1.9 | 28.8 | 66.4 | – | No | Lack of Public Knowledge | Depressive Mood List; Screen for Child Anxiety-Related Emotional Disorders | 0.15 |
| Baams, Grossman, and Russell (2015) | Journal article | 876 | 2007* | USA | 18.3 | 1.8 | 46.2 | 34.1 | 56.0 | No | Lack of Public Knowledge | Beck Depression Inventory for Youth | 0.17 |
| Balsam and Mohr (2007) | Journal article | 613 | 1999* | USA | 36.3 | 11.5 | 36.4 | 75.7 | 9.6 | No | Lack of Open Behavior | Brief Symptom Inventory | 0.15 |
| Beaber (2008) | Dissertation | 208 | 2000* | Global | 30.3 | 8.7 | 0.0 | 91.9 | 24.9 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.11 |
| Beard, Eames, and Withers (2017) | Journal article | 139 | 2012–2013 | UK | 38.3 | 11.6 | 95.0 | – | 5.8 | No | Lack of Open Behavior | BBC Well-being Scale | 0.30 |
| Becraft (1992) | Master’s thesis | 42 | 1984* | USA | 30.7 | 5.6 | 0.0 | 95.2 | 24.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | 0.12 |
| Bejakovich and Flett (2018) | Journal article | 402 | 2010* | New Zealand | 28.7 | 10.2 | 27.9 | – | 18.9 | No | Lack of Open Behavior | Affectometer 2 | 0.36 |
| Birichi (2015) | Dissertation | 226 | 2007* | USA | 29.1 | 9.5 | 100.0 | 88.6 | 28.8 | No | Lack of Open Behavior | Positive and Negative Affect Scale |
0.17 |
| Bittner (2016, Full study) | Dissertation | 263 | 2008* | USA | 29.5 | 11.6 | 33.3 | 40.2 | 9.5 | No | Lack of Active Identity Disclosure | Symptom Checklist-90-Revised | 0.25 |
| Blashill (2016) | Unpublished | 231 | 2016 | USA | 24.7 | 5.4 | 100 | – | 38.8 | No | Lack of Open Behavior | Dysmorphic Concerns Questionnaire | 0.30 |
| Blashill (2018) | Unpublished | 961 | 2018 | USA | 23.7 | 3.7 | 49.8 | – | 66.9 | No | Lack of Open Behavior | Dysmorphic Concerns Questionnaire; Eating Disorder Examination Questionnaire | 0.33 |
| Bosker (2002) | Dissertation | 102 | 2001 | USA | 43.9 | 16–73 | 57.8 | 66.7 | 15.7 | No | Lack of Active Identity Disclosure; Lack of Public Knowledge | Beck Anxiety Inventory; Beck Depression Inventory-II | 0.05 |
| Bränström (2019) | Unpublished effect size | 2,539 | 2016 | Sweden | 34.6 | 13.0 | 87.4 | 42.8 | – | No | Lack of General Openness | Alcohol Use Disorders Identification Test; Brief Symptom Inventory | 0.04 |
| Brewster, Moradi, DeBlaere, and Velez (2013); Brewster (2011) | Dissertation; Journal article | 411 | 2003* | USA | 34.3 | 14.0 | 37.0 | 91.0 | 21.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-21 | 0.08 |
| Byrd (2015, sexual minority sample) | Dissertation | 93 | 2013–2014 | USA | 16.3 | 1.1 | 30.1 | 0.0 | 33.3 | No | Lack of Active Identity Disclosure | Center for Epidemiologic Studies Depression Scale; Screen for Child Anxiety-Related Emotional Disorders | −0.02 |
| Carden (2009) | Dissertation | 183 | 2009 | USA | – | – | 49.2 | – | 15.2 | No | Lack of Open Behavior | Mood and Anxiety Symptom Questionnaire—Short Form | 0.16 |
| Carroll (1995) | Dissertation | 205 | 1994 | USA | 41.0 | 10.7 | 0.0 | 94.1 | 42.5 | No | Lack of General Openness | Symptom Checklist-90-Revised | −0.14 |
| Chan (2017) | Dissertation | 140 | 2016 | Hong Kong | 26.7 | 5.3 | 36.4 | – | 100.0 | No | Lack of General Openness | Brief Symptom Inventory | 0.15 |
| Chan, Operario, and Mak (2020) | Journal article | 931 | 2011* | Hong Kong | 25.3 | 6.6 | 50.3 | 89.4 | 96.5 | No | Lack of Open Behavior | Generalized Anxiety Disorder-7; Patient Health Questionnaire-9 | 0.17 |
| Chaudoir and Quinn (2016) | Journal article; Unpublished effect size | 9 | 2008 | USA | 18.6 | 0.8 | 44.4 | 100.0 | 33.3 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale | 0.51 |
| Chiang (2009) | Dissertation | 136 | 2009 | USA | 36.2 | 18–79 | 97.3 | 92.0 | 42.0 | No | Lack of Open Behavior | Hospital Anxiety and Depression Scale | 0.27 |
| Clark (2012) | Dissertation | 271 | 2004* | USA | 32.3 | 9.5 | 0.0 | 96.3 | 17.6 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.17 |
| Clemens (2004) | Dissertation | 113 | 1999–2001 | USA | 40.0 | 9.5 | 0.0 | 62.7 | 100.0 | No | Lack of Active Identity Disclosure; Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale | −0.05 |
| Cohen (2016, Study 1)c; Cohen, Blasey, Barr Taylor, Weiss, and Newman (2016) | Dissertation; Journal article | 156 | 2014–2015 | USA | 18.8 | 1.1 | 36.0 | 100.0 | 26.5 | No | Lack of General Openness | Beck Depression Inventory-II; Generalized Anxiety Disorder Questionnaire-IV; Social Phobia Diagnostic Questionnaire | 0.22 |
| Cohen (2016, Study 2)c | Dissertation | 101 | 2008* | USA | 21.4 | 36 | 100.0 | 100.0 | 38.7 | No | Lack of General Openness | Beck Depression Inventory-II; Brief Fear of Negative Evaluation Scale; Generalized Anxiety Disorder Questionnaire-IV; Social Phobia Diagnostic Questionnaire | −0.01 |
| Cole, Kemeny, Taylor, Visscher, and Fahey (1996) | Journal article | 80 | 1984–1993 | USA | – | 23–50 | 100.0 | 86.0 | 4.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale; Profile of Mood States; Taylor Manifest Anxiety Scale | −0.04 |
| Corrington, Nittrouer, Trump-Steele, and Hebl (2019) | Journal article | 219 | 2010* | Amazon Mechanical Turk | 32.1 | 8.7 | 100.0 | – | 22.0 | No | Lack of Open Behavior | Brief Symptom Inventory | 0.31 |
| Currin et al. (2018) | Journal article | 209 | 2010* | USA | 34.6 | 12.7 | 100.0 | 82.8 | 19.7 | No | Lack of Open Behavior; Lack of Public Knowledge | Alcohol Use Disorders Identification Test; Center for Epidemiologic Studies Depression Scale Revised; Drug Abuse Screening Test-10 | 0.05 |
| D’Augelli (2002); D’Augelli (2003) | Journal article | 500 | 1987–1989; 1995–1997 | Canada, USA | 19.1 | 1.5 | 62.0 | – | – | No | Lack of General Openness | Brief Symptom Inventory | 0.09 |
| Deitch (2002) | Dissertation | 362 | 1994* | USA | 36.6 | 9.0 | 47.0 | – | 11.0 | No | Lack of General Openness; Lack of Public Knowledge | Brief Symptom Inventory | 0.01 |
| De Lucia, Smith, Ross, Mohr, and King (2018) | Unpublished | 718 | 2018 | USA | 38.3 | 13.9 | 100.0 | – | 21.2 | Yes | Lack of Open Behavior | State-Trait Anxiety Inventory | 0.14 |
| Detwiler (2015) | Dissertation | 189 | 2007* | USA | 60.4 | 7.8 | – | 97.3 | 10.0 | No | Lack of Open Behavior | Kessler Psychological Distress Scale | 0.02 |
| Diaz et al. (2018) | Unpublished | 421 | 2010–2013 | USA | 30.6 | 9.5 | 100.0 | 78.1 | – | No | Lack of Public Knowledge | Patient Health Questionnaire-9 | −0.06 |
| DiPlacido (1998) | Book chapter | 17 | 1990* | USA | 32.0 | – | 0.0 | – | 12.0 | No | No category | Center for Epidemiologic Studies Depression Scale; Negative affect | 0.55 |
| Doane (2017, Wave 1 pilot)c | Dissertation | 337 | 2016 | Amazon Mechanical Turk | 32.1 | 10.2 | 44.8 | 92.4 | 21.4 | No | Lack of General Openness; Lack of Open Behavior | Five-item index of mental health | 0.27 |
| Doane (2017, Study 1)c | Dissertation | 2,115 | 2016 | USA | 36.5 | 14.7 | 64.0 | 94.9 | 16.7 | No | Lack of General Openness | Depression Anxiety and Stress Scale-21; Positive and Negative Affect Scale | 0.26 |
| Dunn, Gonzalez, Costa, Nardi, and Iantaffi (2014) | Journal article | 388 | 2012 | Brazil | 25.3 | 7.9 | 100.0 | 75.9 | 44.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | −0.18 |
| Dyar (2016); Dyar and London (2018) | Dissertation; Journal article; Unpublished effect size | 180 | 2008* | USA | 28.7 | 3.8 | 0.0 | 99.5 | 7.9 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale; Generalized Anxiety Disorder-7 | −0.40 |
| Dyar, Feinstein, and London (2014); Dyar, Feinstein, Eaton, and London (2016, Study 2); Dyar, Feinstein, Eaton, and London (2018) | Journal article | 300 | 2006* | Australia, Canada, UK, USA | 26.8 | 8.5 | 0.0 | 89.4 | 23.6 | No | Lack of Open Behavior | Brief Fear of Negative Evaluation Scale; Generalized Anxiety Disorder-7 | 0.16 |
| Dyar, Feinstein, Schick, and Davila (2017) | Journal article; Unpublished effect size | 390 | 2009* | USA | 27.2 | 9.9 | 26.7 | 87.4 | 17.9 | No | Lack of Open Behavior | Generalized Anxiety Disorder-7; Patient Health Questionnaire-8 | −0.03 |
| Earle (1999) | Dissertation | 82 | 1991* | USA | 28.8 | 18–66 | 0.0 | 92.6 | 9.8 | No | Lack of General Openness | Multiscore Depression Inventory-Short Form | 0.18 |
| Elizur and Ziv (2001) | Journal article | 114 | 1993* | Israel | – | 16–55 | 100.0 | 57.0 | – | No | Lack of Public Knowledge | Mental Health Inventory | 0.22 |
| Escher et al. (2019) | Journal article | 102 | 2011* | USA | 62.4 | 5.9 | 55.9 | 77.5 | 15.6 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | −0.38 |
| Evans (2016); Evans et al. (2018) | Dissertation; Journal article | 236 | 2014–2015 | USA | 30.1 | – | 71.8 | 91.3 | 15.0 | No | Lack of Open Behavior | Generalized Anxiety Disorder-7; Patient Health Questionnaire-8 | 0.15 |
| Fairlie, Feinstein, Lee, and Kaysen (2018) | Journal article | 670 | 2010* | USA | 21.2 | 2.1 | 0.0 | 64.8 | 32.7 | No | Lack of Open Behavior | Young Adult Alcohol Consequences Questionnaire | 0.06 |
| Feinstein (2019) | Unpublished | 633b | 2018 | USA | 26.1 | 8.2 | 27.0 | 84.1 | 16.9 | No | Lack of Open Behavior; Lack of Public Knowledge | Generalized Anxiety Disorder-7; Patient Health Questionnaire-8 | 0.08 |
| Feinstein et al. (2019) | Journal article | 169 | 2007–2014 | USA | 20.7 | 1.3 | 41.4 | 48.5 | 84.0 | No | Lack of Open Behavior | Brief Symptom Inventory | −0.02 |
| Feinstein, Dyar, and London (2017) | Journal article | 288 | 2009* | USA | 26.9 | 8.6 | 0.0 | 89.8 | 22.3 | No | Lack of Open Behavior | Drug Abuse Screening Test-10; The Brief Michigan Alcoholism Screening Test | −0.08 |
| Feldman (2012) | Dissertation | 192 | 2004* | USA | 31.6 | 10.1 | 51.0 | – | 26.2 | No | Lack of Open Behavior | Brief Symptom Inventory | 0.18 |
| Flojo (2005) | Dissertation | 236 | 1997* | USA | 36.4 | 10.0 | 53.0 | 83.5 | 18.5 | No | Lack of Open Behavior | Brief Symptom Inventory | 0.25 |
| Foster, Brewster, Velez, Eklund, and Keum (2017) | Journal article | 212 | 2009* | USA | 36.6 | 14.0 | 45.0 | 93.0 | 30.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-21 | 0.22 |
| Fredriksen-Goldsen, Shiu, Bryan, Goldsen, and Kim (2017) | Journal article | 2,463 | 2010 | USA | 66.7 | 8.9 | 63.2 | – | 13.2 | No | Lack of Public Knowledge | SF-8 Health Survey | −0.06 |
| Friedman et al. (2019) | Journal article; Unpublished effect size | 4,430 | 2014–2017 | USA | – | – | 100.0 | 72.0 | 100.0 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale-10 | −0.24 |
| Frost and Meyer (2009) | Journal article | 396 | 2004–2005 | USA | 32.4 | 9.2 | 50.0 | 78.0 | 66.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | 0.07 |
| Giordano (2016) | Dissertation | 144 | 2008* | Amazon Mechanical Turk, USA | – | – | 41.7 | 88.9 | 50.0 | No | Lack of Open Behavior | Generalized Anxiety Disorder-7 | 0.20 |
| Goodman (2008) | Dissertation | 398 | 2000* | Global | 38.3 | 12.9 | 49.0 | – | 31.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-21 | 0.21 |
| Griffith and Hebl (2002) | Journal article | 379 | 1994* | USA | 39.0 | 10.0 | 58.0 | 69.0 | 18.0 | No | Lack of General Openness; Lack of Open Behavior | Single item assessing for job-related anxiety | 0.13 |
| Guschlbauer, Grant Smith, DeStefano, and Soltis (2019) | Journal article | 181 | 2011* | Global | 34.6 | 12.3 | 35.4 | – | 14.0 | No | Lack of Open Behavior | Kessler Psychological Distress Scale-10 | 0.17 |
| Habarth (2008) | Dissertation; Unpublished effect size | 178 | 2007–2008 | USA | 44.1 | 11.5 | 53.9 | 98.4 | 6.2 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale | 0.16 |
| Handelman (2016) | Dissertation | 214 | 2008* | USA | 21.0 | 15.0 | 47.7 | 96.8 | 34.5 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale; Social Avoidance and Distress Scale | 0.10 |
| Haug (2018) | Dissertation | 132 | 2017 | USA | – | – | 34.1 | 100.0 | 29.6 | No | No category | Hopkins Symptoms Checklist-21 | 0.17 |
| Herek, Cogan, Gillis, and Glunt (1998) | Journal article | 147 | 1990* | USA | 33.0 | 16–68 | 49.7 | – | 18.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | −0.09 |
| Hietpas-Wilson (2007, Wave 3) | Dissertation | 130 | 2001–2002 | USA | 22.2 | 1.9 | 46.5 | – | 32.3 | No | Lack of Public Knowledge | Seven-item index of depressive symptoms | 0.15 |
| Hoy-Ellis (2015); Hoy-Ellis (2016); Hoy-Ellis and Fredriksen-Goldsen (2016) | Dissertation; Journal article | 2,349 | 2010 | USA | 66.9 | 9.0 | 64.6 | 92.4 | 13.0 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale-10 | −0.05 |
| Huebner and Davis (2005) | Journal article | 71 | 1997* | USA | 38.1 | 10.6 | 100.0 | 45.0 | 27.0 | No | Lack of Public Knowledge | Positive and Negative Affect Scale | −0.27 |
| Jackson and Mohr (2016, Study 2) | Journal article | 301 | 2010 | Canada, USA | 23.2 | 5.6 | 42.5 | 99.3 | 23.1 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.22 |
| Jiang, Wang, Hu, and Wang (2019) | Journal article | 315 | 2011* | China | 26.8 | 4.8 | 53.3 | – | – | No | Lack of Open Behavior | Three-item index of job anxiety | 0.34 |
| Jones (2017) | Dissertation; Unpublished effect size | 309 | 2016 | USA | 30.6 | 12.9 | 36.2 | – | 19.8 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Drug Abuse Screening Test-10; Hopkins Symptoms Checklist-58; Ruminative Responses Scale | 0.04 |
| Jordan (1995); Jordan and Deluty (1998) | Dissertation; Journal article | 499 | 1987* | USA | 32.5 | 19–76 | 0.0 | 95.0 | 16.8 | No | Lack of Active Identity Disclosure | State-Trait Anxiety Inventory | 0.17 |
| Juster, Smith, Ouellet, Sindi, and Lupien (2013); Juster et al. (2016) | Journal article | 46 | 2010 | Canada | 23.9 | 0.8 | 56.5 | 97.5 | 29.8 | No | Lack of Active Identity Disclosure | Beck Depression Inventory-II; State-Trait Anxiety Inventory | 0.38 |
| Kamen, Jabson, Mustian, and Boehmer (2017) | Journal article | 201 | 2009* | USA | 53.0 | 8.5 | 0.0 | 75.6 | 11.9 | No | Lack of Open Behavior | Hospital Anxiety and Depression Scale | −0.11 |
| Kappler (2011) | Dissertation | 105 | 2010 | Canada, USA | 59.7 | 11.4 | 100.0 | – | 18.5 | No | Lack of Active Identity Disclosure | The Depression-Happiness Scale | 0.10 |
| Kauth, Barrera, and Latini (2019) | Journal article; Unpublished effect size | 119 | 2015 | USA | 48.4 | 14.5 | 64.7 | 92.1 | 19.8 | No | Lack of Open Behavior | Overall Anxiety Severity and Impairment Scale; Patient Health Questionnaire-9 | 0.08 |
| Kavanaugh, Taylor, Stuhlsatz, Neppl, and Lohman (2019) | Journal article | 941 | 2010 | USA | 21.4 | 18–24 | 46.0 | – | 100.0 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | 0.18 |
| Knight (2006) | Dissertation | 164 | 1998* | USA | 39.0 | 9.7 | 100.0 | 97.0 | 32.9 | No | Lack of Open Behavior | Positive and Negative Affect Scale | 0.23 |
| Konik (2005) | Dissertation | 229 | 1997* | USA | 44.3 | 19–74 | 43.4 | – | 8.4 | No | Lack of General Openness | Brief Symptom Inventory | 0.13 |
| Kosciw, Palmer, and Kull (2015) | Journal article | 7,816 | 2011 | USA | 16.0 | 13–20 | 35.2 | 0.0 | 32.1 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | 0.08 |
| Kuyper (2015) | Journal article; Unpublished effect size | 518 | 2012–2013 | The Netherlands | 42.8 | 11.7 | 40.2 | 55.1 | – | No | Lack of Public Knowledge | Mental Component Summary of the Short Form 36 Health Survey Questionnaire | 0.17 |
| Kuyper (n.d.) | Unpublished | 1,373 | 2012–2013 | The Netherlands | 49.6 | 9.4 | 39.3 | 16.2 | – | No | Lack of Public Knowledge | Mental Component Summary of the Short Form 36 Health Survey Questionnaire | 0.06 |
| Lambe (2013) | Dissertation | 203 | 2005* | USA | 32.2 | 8.3 | 0.0 | 94.6 | 18.2 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.24 |
| Legate (2014); Legate, Ryan, and Weinstein (2012) | Dissertation; Journal article | 145 | 2004* | USA | 29.9 | 18–65 | 38.5 | – | 19.9 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.26 |
| Legate, Weinstein, Ryan, DeHaan, and Ryan (2018) | Journal article; Unpublished effect size | 484 | 2016 | Amazon Mechanical Turk | 28.4 | 9.2 | 37.4 | – | 28.1 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale; State-Trait Anxiety Inventory | 0.19 |
| Lehavot (2011); Lehavot and Simoni (2011) | Dissertation; Journal article | 1,381 | 2003* | USA | 33.5 | 12.1 | 0.0 | 87.0 | 26.0 | No | Lack of General Openness | The Brief Michigan Alcoholism Screening Test; Center for EpidemiologicStudies Depression Scale-10; Drug Abuse Screening Test-10; Generalized Anxiety Disorder-7 |
0.11 |
| Lewis (n.d.a) | Unpublished | 1,051 | 2011* | USA | 28.8 | 4.3 | 0.0 | 94.6 | 22.6 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale | 0.09 |
| Lewis (n.d.b) | Unpublished | 656 | 2011* | USA | 22.7 | 3.5 | 0.0 | 81.4 | 23.0 | No | Lack of General Openness; Lack of Open Behavior; Lack of Public Knowledge | Mental Health Inventory-5 | 0.15 |
| Lewis, Milletich, Mason, and Derlega (2014) | Journal article | 220 | 2006* | USA | 54.0 | 11.3 | 0.0 | 93.6 | 5.0 | No | Lack of Open Behavior | Positive and Negative Affect Scale; Ruminative Responses Scale | 0.02 |
| Li (2018) | Dissertation | 357 | 2010* | USA | 30.9 | 9.5 | 41.7 | – | 39.1 | No | Lack of General Openness | Hospital Anxiety and Depression Scale | −0.32 |
| Li (2019) | Unpublished | 417 | 2011* | USA | 30.0 | 7.8 | 39.6 | – | 40.4 | No | Lack of General Openness | Hospital Anxiety and Depression Scale | −0.29 |
| Li and Samp (2019) | Journal article; Unpublished effect size | 251 | 2011* | USA | 31.2 | 9.7 | 41.8 | – | 37.6 | No | Lack of General Openness | Hospital Anxiety and Depression Scale | −0.26 |
| Liu et al. (2018) | Journal article | 134b | 2017 | China | 27.9 | 8.8 | 100.0 | 62.4 | 100.0 | No | Lack of General Openness | Symptom Checklist-90-Revised | 0.79 |
| Liubovich (2003) | Dissertation | 149 | 1995* | USA | 36.0 | 9.9 | 0.0 | 86.8 | 12.8 | No | Lack of Public Knowledge | Eating Disorders Inventory | −0.31 |
| Livingston, Christianson, and Cochran (2016) | Journal article; Unpublished effect size | 397b | 2008* | USA | 20.8 | 2.1 | 29.0 | – | 13.1 | No | Lack of Open Behavior | Depression Anxiety and Stress Scale-21 | 0.09 |
| Luu (2011) | Dissertation | 662 | 2003* | USA | 32.5 | 18–76 | 70.7 | 61.6 | 100.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-25 | 0.34 |
| Mahon, Kiernan, and Gallagher (2019) | Unpublished | 508 | 2018 | Ireland | 29.3 | 9.7 | 51.2 | 83.0 | 3.7 | No | Lack of General Openness; Lack of Open Behavior | Brief Fear of Negative Evaluation Scale; Liebowitz Social Anxiety Scale | 0.21 |
| Marsack and Stephenson (2017) | Journal article | 771 | 2014 | USA | 32.4 | 0.4 | 59.1 | 78.0 | 11.0 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale-11 | 0.05 |
| Martinez (2006) | Dissertation | 168 | 1998* | USA | 40.0 | 11.7 | 79.2 | 89.0 | 35.2 | No | Lack of Open Behavior | Mental Health Inventory | 0.23 |
| Mason (2016); Mason, Lewis, and Heron (2017) | Journal article | 428 | 2008* | USA | 21.9 | 2.9 | 0.0 | 84.0 | 22.7 | No | Lack of General Openness | Eating Disorder Diagnostic Scale; Eating Disorder Inventory; Positive and Negative Affect Scale; SCOFF | 0.10 |
| McConnell, Clifford, Korpak, Phillips, and Birkett (2017) | Journal article | 155 | 2013–2014 | USA | 23.1 | 1.6 | 38.3 | – | 88.4 | No | Lack of General Openness | Brief Symptom Inventory | −0.02 |
| Meidlinger and Hope (2014) | Journal article | 149 | 2006* | USA | 28.9 | 11.1 | 49.0 | – | 12.6 | No | Lack of General Openness; Lack of Open Behavior; Lack of Public Knowledge | Brief Fear of Negative Evaluation Scale; Positive and Negative Affect Scale | 0.33 |
| Michaels, Parent, and Torrey (2016) | Journal article | 167 | 2007* | USA | 46.9 | 12.2 | 100.0 | – | 19.2 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale-7 | 0.22 |
| Mohr, Jackson, and Sheets (2017, Study 2) | Journal article | 240 | 2006 | USA | 22.0 | 4.1 | 17.5 | 99.2 | 16.3 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.10 |
| Mohr and Kendra (2011, Study 1) | Journal article; Unpublished effect size | 654 | 2003* | Canada, USA | 22.9 | 5.6 | 46.2 | 99.7 | 25.4 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale; Positive and Negative Affect Scale | 0.17 |
| Morandini, Pinkus, and Dar-Nimrod (2018) | Journal article | 163 | 2010* | Australia | 24.5 | 7.1 | 0.0 | 56.5 | 15.5 | No | Lack of General Openness | Depression Anxiety and Stress Scale-21 | 0.12 |
| Mustanski, Newcomb, and Garofalo (2011) | Journal article | 425 | 2004–2005 | USA | 20.2 | 2.3 | 70.3 | 54.8 | 65.8 | No | No category | Brief Symptom Inventory-18 | 0.01 |
| Nance (2008) | Dissertation | 529 | 2007 | Canada, USA | – | – | 100.0 | 95.8 | 5.0 | No | Lack of Open Behavior | Depression Anxiety and Stress Scale-21 | −0.14 |
| Nash (1990) | Dissertation | 134 | 1986–1988 | USA | – | 38–47 | 100.0 | 96.0 | 4.5 | No | No category | State-Trait Anxiety Inventory | 0.20 |
| Nickels (2013, Quantitative sample) | Dissertation | 252 | 2010 | USA | 16.8 | 2.1 | 35.6 | – | 31.1 | No | Lack of General Openness | Single item assessing presence of depressive episode in past 12 months | −0.18 |
| Norcini Pala (2010) | Unpublished | 104 | 2009–2010 | Italy | 40.3 | 9.7 | 100.0 | 38.1 | – | No | No category | Patient Health Questionnaire-9; Positive and Negative Affect Scale | −0.12 |
| Norcini Pala (2012a) | Unpublished | 54 | 2012 | Italy | 36.6 | 7.9 | 100.0 | 38.9 | 0.0 | No | No category | Patient Health Questionnaire-9 | 0.30 |
| Norcini Pala (2012b, Female-identified participants)c | Unpublished | 65 | 2012 | Italy | 27.3 | 5.1 | 0.0 | 38.8 | – | No | Lack of Public Knowledge | Patient Health Questionnaire-9 | 0.36 |
| Norcini Pala (2012b, Male-identified participants)c | Unpublished | 54 | 2012 | Italy | 28.8 | 7.4 | 100.0 | 40.6 | – | No | No category | Patient Health Questionnaire-9 | 0.21 |
| Oetjen and Rothblum (2000) | Journal article | 167 | 1992* | USA | 33.0 | 20–60 | 0.0 | 75.0 | 8.0 | No | Lack of Active Identity Disclosure | Center for Epidemiologic Studies Depression Scale | 0.03 |
| Oldenburg et al. (2014) | Journal article; Unpublished effect size | 300 | 2010 | Vietnam | 22.4 | 5.0 | 100.0 | – | 100.0 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale-10 | −0.02 |
| Orban (2003) | Dissertation | 145 | 1995* | USA | 17.3 | 13–21 | 63.0 | 15.9 | 93.2 | No | Lack of General Openness | Mental Health Inventory | 0.15 |
| Owens, Riggle, and Rostosky (2007)e | Journal article | 226 | 1999* | USA | 37.6 | 11.5 | 32.0 | 67.0 | 16.0 | No | Concealment from mental health service providers; used in sensitivity analysis only | Center for Epidemiologic Studies Depression Scale; Depression Anxiety and Stress Scale | −0.11 |
| Pachankis (n.d.) | Unpublished | 254 | 2017–2019 | USA | 26.6 | 4.2 | 98.4 | 90.9 | 43.7 | No | Lack of General Openness | Alcohol Use Disorders Identification Test; Beck Anxiety Inventory; Brief Symptom Inventory; Hamilton Rating Scale for Depression; Mini International Neuropsychiatric Interview; Overall Anxiety Severity and Impairment Scale; Overall Depression Severity and Impairment Scale; Short Inventory of Problems-Alcohol and Drugs; Social Interaction Anxiety Scale | −0.01 |
| Pachankis, McConocha, et al. (2019) | Unpublished | 60 | 2018–2019 | USA | 25.6 | 3.3 | 0.0 | 100.0 | 30.0 | No | Lack of General Openness | Alcohol Use Disorders Identification Test; Brief Symptom Inventory; Center for Epidemiologic Studies Depression Scale; Overall Anxiety Severity and Impairment Scale; Overall Depression Severity and Impairment Scale Short Inventory of Problems-Alcohol; Short Inventory of Problems-Drugs; Social Interaction Anxiety Scale; State-Trait Anxiety Inventory | 0.16 |
| Pachankis, Williams, et al. (2019) | Unpublished | 108 | 2017–2018 | USA | 23.7 | 3.1 | 28.7 | 46.3 | 13.91 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Beck Anxiety Inventory; Brief Symptom Inventory-18; Center for Epidemiologic Studies Depression Scale; Short Inventory of Problems-Modified for Drug Use | 0.13 |
| Pachankis and Bernstein (2012) | Journal article | 136 | 2004 | USA | 20.7 | 2.1 | 100.0 | 100.0 | 28.6 | No | Lack of Open Behavior | Positive and Negative Affect Scale | 0.28 |
| Pachankis, Clark, et al. (2020) | Unpublished | 937 | 2016 | USA | 30.8 | 9.8 | 100.0 | 83.6 | 32.2 | No | Lack of General Openness | Alcohol Use Disorders Identification Test; Brief Symptom Inventory | −0.08 |
| Pachankis and Goldfried (2006, Gay-identified sample) | Journal article | 87 | 1998 | USA | 20.4 | 1.3 | 100.0 | 100.0 | 26.4 | No | Lack of General Openness | Social Interaction Anxiety Scale; Social Phobia Scale | 0.24 |
| Pachankis, Sullivan, Feinstein, and Newcomb (2018) | Journal article | 128 | 2009–2018 | USA | 20.7 | 2.1 | 100.0 | 100.0 | 28.1 | No | Lack of General Openness | Center for Epidemiologic Studies Depression Scale; Social Interaction Anxiety Scale | 0.24 |
| Parker, Lõhmus, Mangine, and Rüütel (2016); Rüütel, Valk, and Lõhmus (2017) | Journal article; Unpublished effect size | 265 | 2013 | Estonia | 32.3 | 9.7 | 100.0 | 43.0 | – | No | Lack of Public Knowledge | Emotional State Questionnaire | −0.03 |
| Paul, Smith, Mohr, and Ross (2014, CFA sample)c | Journal article | 215 | 2006 | USA | 38.4 | 13.7 | 46.4 | 95.3 | 18.2 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | −0.15 |
| Paul et al. (2014, EFA sample)c | Journal article | 207 | 2006 | USA | 38.4 | 13.7 | 46.4 | 95.3 | 18.2 | Yes | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.03 |
| Persson, Pfaus, and Ryder (2015) | Journal article | 200 | 2011–2014 | Canada | 24.4 | 6.4 | 0.0 | 93.0 | – | No | Lack of General Openness | Beck Anxiety Inventory; Beck Depression Inventory-II | 0.32 |
| Pimentel (2015) | Dissertation; Unpublished effect size | 406 | 2013 | USA | 38.3 | 14.7 | 99.3 | 84.0 | 35.9 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.08 |
| Prell and Traeen (2018, Bisexual-identified participants)c | Journal article | 122 | 2016 | Norway | – | 18–73 | 0.0 | 53.8 | – | Yes | Lack of Open Behavior | Common Mental Disorders Questionnaire | 0.31 |
| Prell and Traeen (2018, Lesbian-identified participants)c | Journal article | 273 | 2016 | Norway | – | 18–73 | 0.0 | 61.9 | – | No | Lack of Open Behavior | Common Mental Disorders Questionnaire | 0.24 |
| Puckett, Maroney, Levitt, and Horne (2016); Puckett, Surace, Levitt, and Horne (2016) | Journal article | 383 | 2008* | USA | 39.3 | 13.4 | 34.5 | – | 19.9 | No | Lack of General Openness | 5-item Symptom Checklist; Social Interaction Anxiety Scale-6 | 0.23 |
| Puckett, Wolff, Gunn, Woodward, and Pantalone (2018) | Journal article; Unpublished effect size | 217 | 2010* | USA | 36.4 | 14.0 | 45.6 | – | 22.1 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.19 |
| Ragins, Singh, and Cornwell (2007) | Journal article | 534 | 1999* | USA | 41.1 | 8.7 | 68.0 | 84.7 | 30.3 | No | Lack of Active Identity Disclosure | Work-Related Anxiety Scale; Work-Related Depression Scale | −0.03 |
| Ray (2016, Sample 1)c | Dissertation | 341 | 2008* | USA | – | 18–54 | 26.7 | 94.3 | 8.4 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Drug Use Disorders Identification Test | −0.05 |
| Ray (2016, Sample 2)c | Dissertation | 180 | 2008* | USA | – | 18–64 | 35.6 | 84.8 | 23.8 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Drug Use Disorders Identification Test | −0.10 |
| Rhoades et al. (2018) | Journal article; Unpublished effect size | 365 | 2015–2017 | USA | 17.7 | 3.1 | 39.5 | 13.2 | 39.4 | No | Lack of Public Knowledge | Studies Depression Scale-4 | −0.04 |
| Ribeiro Gonçalves (2019) | Unpublished | 110 | 2017–2018 | Portugal | 63.5 | 3.4 | 100.0 | 52.7 | – | No | Lack of Public Knowledge | Kessler Psychological Distress Scale | 0.44 |
| Riggle, Rostosky, Black, and Rosenkrantz (2017) | Journal article | 373 | 2009* | USA | 31.2 | 12.7 | 47.6 | 85.6 | 27.4 | No | Lack of Active Identity Disclosure; Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale-10 | 0.20 |
| Robinson, Sanches, and MacLeod (2016); Ross et al. (2014) | Journal article; Unpublished effect size | 367 | 2011–2012 | Canada | 31.6 | – | 27.7 | 82.0 | 35.8 | Yes | Lack of Open Behavior | Overall Anxiety Severity and Impairment Scale; Patient Health Questionnaire-9 | −0.04 |
| Roper (1997) | Dissertation | 141 | 1989* | USA | – | 20–63 | 0.0 | 95.0 | 15.0 | No | Lack of Public Knowledge | Brief Symptom Inventory | 0.01 |
| Rosario, Hunter, Maguen, Gwadz, and Smith (2001); Rosario, Schrimshaw, and Hunter (2006); Rosario, Schrimshaw, and Hunter (2009, Male-identified participants)c | Journal article | 80 | 1993–1995 | USA | 18.3 | 1.7 | 100.0 | 31.0 | 77.0 | No | Lack of Active Identity Disclosure | Brief Symptom Inventory; Diagnostic Interview Schedule for Children | 0.00 |
| Rosario et al. (2001); Rosario et al. (2009, Female identified participants)c | Journal article | 76 | 1993–1995 | USA | 18.3 | 1.7 | 0.0 | 31.0 | 79.0 | No | Lack of Active Identity Disclosure | Brief Symptom Inventory | 0.01 |
| Rosario-Hernández, Millán, Cruz, Neris, and Acevedo (2009) | Journal article | 110 | 2001* | USA (Puerto Rico) | – | – | 65.5 | – | – | No | Lack of General Openness | Multiple Affect Adjective Checklist | 0.09 |
| Rosser et al. (2008) | Unpublished | 1,579 | 2008 | USA | 33.2 | 10.5 | 100.0 | 88.8 | 22.3 | No | Lack of General Openness | CAGE Questionnaire; Center for Epidemiologic Studies Depression Scale-10 | 0.01 |
| Rosser et al. (2013) | Journal article; Unpublished effect size | 1,265 | 2011 | USA | – | – | 100.0 | 89.9 | 47.0 | No | Lack of General Openness | Positive and Negative Affect Scale | 0.00 |
| Rosser et al. (2019) | Unpublished | 193 | 2015–2016 | USA | 63.4 | 8.2 | 99.5 | 96.4 | 10.9 | No | Lack of General Openness | Mental Component Summary of the Short Form 36 Health Survey Questionnaire | 0.01 |
| Rostosky, Riggle, Horne, and Miller (2009) | Journal article | 574 | 2006 | USA | 38.9 | 12.8 | 44.0 | 72.0 | 10.9 | No | Lack of Active Identity Disclosure | Center for Epidemiologic Studies Depression Scale-10 | 0.15 |
| Rubino, Case, and Anderson (2018) | Journal article | 225 | 2010* | Australia | 23.2 | 7.4 | 0.0 | 43.4 | 26.5 | No | Lack of Active Identity Disclosure | Center for Epidemiologic Studies Depression Scale | 0.26 |
| Ryan (2017, Study 2); Ryan, Legate, Weinstein, and Rahman (2017) | Dissertation; Journal article | 156 | 2009* | UK | 26.0 | 9.1 | 41.7 | – | – | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale; General Health Questionnaire | 0.17 |
| Salway et al. (2018) | Journal article; Unpublished effect size | 7,872 | 2014–2015 | Canada | – | – | – | 43.7 | 16.8 | No | Lack of Public Knowledge | Single item assessing for discussion with healthcare provider about self-defined past-12-month problems with depression and/or substance abuse | −0.14 |
| Sandfort, Bos, Knox, and Reddy (2016) | Journal article | 199 | 2008 | South Africa | 26.7 | 5.8 | 100.0 | – | 100.0 | No | Lack of Public Knowledge | Depression Anxiety and Stress Scale | 0.12 |
| Sandil, Robinson, Brewster, Wong, and Geiger (2015) | Journal article | 142 | 2006* | USA | 32.5 | 7.5 | 67.0 | 98.0 | 99.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-21 | 0.10 |
| Sattler, Wagner, and Christiansen (2016) | Journal article | 1,188 | 2014 | Germany | 38.0 | 11.0 | 100.0 | 54.0 | – | No | Lack of General Openness | Brief Symptom Inventory; Diagnostic Interview of Mental Disorders | 0.13 |
| Sattler, Zeyen, and Christiansen (2017) | Journal article; Unpublished effect size | 787 | 2015 | Germany | 36.9 | 13.3 | 64.04 | – | – | No | Lack of General Openness | Brief Symptom Inventory-18 | 0.04 |
| Schope (2004) | Journal article | 443b | 1996* | USA | 40.0 | 11.6 | 100.0 | 77.0 | 9.0 | No | Lack of General Openness | Fear of Negative Evaluation Scale | 0.11 |
| Schrimshaw, Siegel, Downing, and Parsons (2013) | Journal article | 203 | 2007–2010 | USA | 36.9 | 11.2 | 100.0 | 69.0 | 73.0 | No | No category | Mental Health Inventory | 0.03 |
| Scott (2016, Partner 1)c | Dissertation | 103 | 2008* | USA | 33.7 | 9.0 | 0.0 | – | 26.7 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Center for Epidemiologic Studies Depression Scale | −0.07 |
| Scott (2016, Partner 2)c | Dissertation | 103 | 2008* | USA | 33.7 | 9.0 | 0.0 | – | 26.7 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Center for Epidemiologic Studies Depression Scale | 0.03 |
| Sedlovskaya (2011, Study 5); Sedlovskaya et al. (2013, Study 5) | Dissertation; Journal article | 34 | 2011 | USA | – | – | 100.0 | 92.1 | 34.2 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.37 |
| Shilo, Antebi, and Mor (2015) | Journal article | 890 | 2015 | Israel | 32.1 | 5.5 | 51.9 | 30.1 | – | No | Lack of Active Identity Disclosure | Mental Health Inventory | 0.14 |
| Shilo and Mor (2015) | Journal article | 445 | 2010 | Israel | 22.5 | 4.7 | 100.0 | – | – | No | Lack of Active Identity Disclosure | Mental Health Inventory | 0.12 |
| Shilo and Savaya (2011); Shilo and Savaya (2012) | Journal article | 461 | 2006 | Israel | 18.2 | 1.8 | 50.3 | – | – | No | Lack of Open Behavior | Mental Health Inventory | 0.16 |
| Shilo, Yossef, and Savaya (2016) | Journal article | 113 | 2012 | Israel | 28.4 | 8.3 | 100.0 | 64.5 | – | No | Lack of Active Identity Disclosure | Mental Health Inventory | 0.19 |
| Smith (1996) | Dissertation | 305 | 1996 | USA | 21.7 | 18–25 | 100.0 | – | 24.0 | No | No category | Hopkins Symptoms Checklist-21 | 0.12 |
| Smith et al. (2017) | Journal article | 33 | 2009* | USA | 21.9 | 2.2 | 100.0 | – | 45.4 | No | Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale; State-Trait Anxiety Inventory for Cognitive and Somatic Anxiety | 0.37 |
| Smith and Ingram (2004) | Journal article | 97 | 1996* | USA | 34.7 | 10.0 | 59.0 | 94.0 | 17.0 | No | Lack of General Openness | Brief Symptom Inventory; Center for Epidemiologic Studies Depression Scale | 0.24 |
| Sun, Tobin, Spikes, and Latkin (2019)e | Journal article | 226 | 2006–2009 | USA | 37.9 | 10.6 | 100.0 | 42.5 | 100.0 | No | Concealment from main healthcare provider; used in sensitivity analysis only | Alcohol Use Disorders Identification Test | 0.18 |
| Swearingen (2006) | Dissertation | 385 | 2005 | USA | 29.7 | 11.5 | 34.1 | – | 21.0 | No | Lack of Open Behavior | The Eating Attitudes Test | 0.15 |
| Szymanski and Sung (2010) | Journal article | 144 | 2002* | USA | 30.7 | 8.6 | 39.0 | 87.0 | 100.0 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-21 | 0.17 |
| Tabaac, Perrin, and Trujillo (2015) | Journal article; Unpublished effect size | 150 | 2007* | USA | 31.9 | 12.0 | 0.0 | 94.0 | 70.7 | No | Lack of Open Behavior | Hopkins Symptoms Checklist-25 | 0.15 |
| Tabb (2016) | Dissertation | 95 | 2014–2015 | USA | – | – | 52.6 | 64.2 | 100.0 | No | Lack of Open Behavior | Alcohol Use Disorders Identification Test; Generalized Anxiety Disorder-7; Patient Health Questionnaire-8 | 0.13 |
| Talley and Bettencourt (2011) | Journal article | 83 | 2003* | USA | 19.1 | 1.6 | 65.1 | 100.0 | 9.6 | No | Lack of Active Identity Disclosure | Center for Epidemiologic Studies Depression Scale | 0.17 |
| Thies (2015) | Dissertation | 181 | 2007* | USA | 31.8 | 11.3 | 53.6 | – | 32.0 | No | Lack of Public Knowledge | Center for Epidemiologic Studies Depression Scale; Generalized Anxiety Disorder-7 | 0.04 |
| Timmins, Rimes, and Rahman (2018) | Journal article | 38 | 2009* | Global | 29.2 | 19–50 | 34.2 | – | 5.3 | No | Lack of General Openness; Lack of Open Behavior | Generalized Anxiety Disorder-7; Patient Health Questionnaire Anxiety and Depression Scale | 0.43 |
| Timmins, Rimes, and Rahman (2020) | Journal article | 4,248 | 2011* | Global | 29.9 | 16–82 | 57.1 | – | 10.8 | No | Lack of General Openness; Lack of Open Behavior | Generalized Anxiety Disorder-7; Patient Health Questionnaire-9; Ruminative Responses Scale | −0.14 |
| Tomori et al. (2016) | Journal article | 363 | 2008* | India | – | – | 100.0 | – | 100.0 | No | Lack of Active Identity Disclosure | Patient Health Questionnaire-9 | −0.25 |
| Tornello and Patterson (2018)e | Journal article | 79 | 2008–2009 | USA | 61.0 | 8.8 | 100.0 | 96.2 | 1.3 | No | Concealment from children and grandchildren; used in sensitivity analysis only | Mental Component Summary of the Short Form 12 Health Survey Questionnaire | −0.02 |
| Ullrich, Lutgendorf, and Stapleton (2003); Ullrich, Lutgendorf, Stapleton, and Horowitz (2004) | Journal article | 73 | 1995* | USA | 37.0 | 23–56 | 100.0 | 64.0 | 11.0 | No | Lack of General Openness | Beck Depression Inventory | 0.36 |
| van der Star, Pachankis, and Bränström (2019) | Journal article | 80 | 2016 | Sweden | 33.5 | 13.2 | 41.3 | 47.5 | – | No | Lack of General Openness | Patient Health Questionnaire-9 | −0.09 |
| Velez and Moradi (2016) | Journal article | 514 | 2008* | USA | 31.5 | 13.0 | 47.0 | 95.0 | 23.0 | No | Lack of Open Behavior | Hopkins Symptom Checklist-21 | 0.23 |
| Velez, Moradi, and Brewster (2013) | Journal article | 326 | 2012 | North America | 38.4 | 12.1 | 43.0 | 97.0 | 20.0 | No | Lack of Open Behavior | Hopkins Symptom Checklist-21 | 0.31 |
| Velez, Watson, Cox, and Flores (2017) | Journal article | 813 | 2009* | USA | 23.7 | 6.7 | 22.0 | 79.0 | 39.0 | No | Lack of Open Behavior | Hopkins Symptom Checklist-21 | 0.12 |
| Vincke and van Heeringen (2002) | Journal article | 197 | 1994* | Belgium | 19.9 | 2.5 | 61.4 | – | – | No | Lack of Open Behavior | General Health Questionnaire | 0.01 |
| Walch, Ngamake, Bovornusvakool, and Walker (2016) | Journal article; Unpublished effect size | 443 | 2010 | USA | 31.4 | 9.8 | 35.3 | 79.1 | 21.1 | No | Lack of Open Behavior | Depression Anxiety and Stress Scale | −0.01 |
| Waldo (1997); Waldo (1999) | Dissertation; Journal article | 287 | 1989* | USA | 38.2 | 9.0 | 58.5 | – | 8.4 | No | No category | Brief Symptom Inventory | 0.10 |
| Watson, Velez, Brownfield, and Flores (2016) | Journal article | 353 | 2008* | USA | 27.1 | 7.9 | 0.0 | 94.3 | 23.2 | No | Lack of Open Behavior | The Eating Attitudes Test-26 | 0.18 |
| White, Sandfort, Morgan, Carpenter, and Pierre (2016) | Journal article | 106 | 2008* | Jamaica | – | 18–56 | 100.0 | 45.2 | – | No | Lack of General Openness | Zung Depression Inventory | −0.11 |
| Wilkerson, Noor, Galos, and Rosser (2016) | Journal article | 1,475 | 2011 | USA | – | – | 100.0 | 88.9 | 26.9 | No | Lack of Genera Openness; Lack of Open Behavior | Center for Epidemiologic Studies Depression Scale | 0.13 |
| Williams, Mann, and Fredrick (2017) | Journal article | 218 | 2009* | USA | 27.5 | 12.1 | 42.4 | – | 15.1 | No | Lack of Open Behavior | Kessler Psychological Distress Scale | 0.15 |
| Willoughby (2008) | Dissertation | 81 | 2000* | USA | 19.7 | 1.8 | 69.0 | – | 46.0 | No | Lack of Open Behavior | Personal Experience Screening Questionnaire | 0.07 |
| Wolff, Himes, Soares, and Kwon (2016) | Journal article | 401 | 2008* | USA | 27.7 | 9.4 | 51.0 | 100.0 | 14.0 | No | Lack of Open Behavior | Counseling Center Assessment of Psychological Symptoms | 0.19 |
| Woodford et al. (2018) | Journal article; Unpublished effect size | 562 | 2013 | USA | 22.7 | 5.5 | 44.0 | 97.1 | 24.7 | No | Lack of General Openness | Patient Health Questionnaire-9 | −0.07 |
| Xu, Zheng, Xu, and Zheng (2017) | Journal article; Unpublished effect size | 435 | 2014–2015 | China | – | – | 100.0 | 70.3 | 100.0 | No | Lack of Active Identity Disclosure | Kessler Psychological Distress Scale-6 | 0.03 |
| Zuckerman (1998) | Dissertation | 43 | 1990* | USA | 38.3 | 8.3 | 100.0 | 90.0 | 43.0 | No | Lack of Active Identity Disclosure | Beck Depression Inventory; Profile of Mood States; State-Trait Anxiety Inventory | 0.12 |
Notes. CFA = confirmatory factor analysis; EFA = exploratory factor analysis.
Positive effect sizes indicate a positive association between concealment and mental health problems; negative effect sizes indicate a negative association between concealment and mental health problems.
Certain effects derived from these studies used a somewhat reduced n, typically due to missing data contained within the studies.
These studies each contain two distinct subsamples, for which effects are presented separately. In some cases, demographics were only available for the overall sample and therefore could not be disaggregated by study subsample.
The range of participants’ ages, if available, is provided when the standard deviation for age is unavailable.
Studies included in sensitivity analysis only.
The year of data collection was unknown and was therefore estimated as the mean publication lag across studies included here (i.e., 8 years).
The majority (98.4%) of effects derived from commonly used mental health measures (e.g., the Center for Epidemiological Studies Depression Scale) with high reliability and established psychometric properties. The remainder of effects (1.6%) derived from instruments without established reliability.
Hypothesized Effect Moderators
Table 1 summarizes all hypothesized moderators in terms of their extracted information, coding, and average distribution across studies. In addition to the four distinct categories of concealment described above, hypothesized moderators of the association between sexual orientation concealment and mental health problems included: time period (i.e., estimated year of data collection [for studies lacking this information, we used year of publication minus the average publication lag across studies (i.e., 8 years)]), study location (i.e., studies conducted in North America vs. studies conducted outside of North America), whether the study used dichotomous measures for concealment and mental health problems, age (i.e., mean age of study participants), gender (i.e., proportion of the sample composed of male participants), educational attainment (i.e., proportion of the sample that had completed at least some college), race/ethnicity (i.e., studies containing a majority of racial/ethnic minority participants), and studies with an exclusive bisexual sample.
Analytic Strategies
Correlation coefficients were used as the measure of effect size. All effects were coded such that a positive effect indicates an association between concealment and mental health problems whereas a negative effect indicates an association between concealment and favorable mental health. Before the primary analyses, we transformed the correlations derived from the studies with Fisher’s r-to-z transformation to be able to compare studies on a scale with approximately normal distribution and stabilized variance. After the analyses, results were transformed back to r for interpretation. Random effect models were used to calculate pooled effect sizes; these are presented as correlations. Because many studies contributed multiple effect sizes, we both (a) calculated the standardized average mean of mental health problems for each study and (b) used robust variance estimation models to make use of all effect sizes available in each study adjusting for dependency between effect sizes coming from the same study (Hedges, Tipton, & Johnson, 2010; Tanner-Smith & Tipton, 2014). We interpret effect sizes as small (r = .1), medium (r = .3), and large (r = .5), according to Cohen’s conventions (Cohen, 1988; Cohen, 1992). Heterogeneity between studies was examined with the Q, I2, and τ2 statistics, to assess both the size and significance of heterogeneity between studies.
We conducted post hoc moderation analyses using metaregression, examining the potential effect of various study and sample characteristics as explanatory factors of between-study heterogeneity. The variables examined as potential moderators of the association between sexual orientation concealment and mental health problems were: type of mental health problem (i.e., depression, anxiety, general distress, problematic eating, substance use problems); type of measure used to assess sexual orientation concealment (i.e., Category 1 to 4); study characteristics (i.e., time period, study location, use of dichotomous measure of concealment, use of dichotomous measure of mental health problems); and sample characteristics (i.e., age, gender, educational attainment, race/ethnicity, exclusive bisexual sample composition).
We analyzed study heterogeneity across a number of steps. First, we assessed whether the relationship between sexual orientation concealment and mental health problems differed based on the type of mental health problem. For these analyses we entered dummy-coded variables for each type of mental health problem (i.e., depression, anxiety, general distress, problematic eating, and substance use) into separate bivariate metaregression analyses. For these analyses, we included all studies that contributed effect sizes for any mental health problem. For studies in which effect sizes could be extracted separately for more than one mental health problem, multiple separate effect sizes were used in the analysis.
Second, we examined whether the relationship between sexual orientation concealment and mental health problems differed based on the type of sexual orientation concealment classification derived from our four-category scheme. In these analyses, studies measuring concealment using more than one type of concealment measure were allowed to contribute multiple effect sizes. Similar to the analyses of different mental health outcomes, dummy-coded variables for each type of concealment measure were entered separately into bivariate metaregression analyses. Third, we examined study and sample characteristics as potential moderators using bivariate metaregression analyses. Finally, we entered all variables that significantly contributed to heterogeneity in the bivariate analyses into a multivariate metaregression analysis; nonsignificant moderators were removed using backward deletion
We conducted several tests to ascertain potential study selection bias and to examine indications that statistically nonsignificant, or unexpected, results are systematically excluded from the literature (i.e., “file-drawer bias”). First, we analyzed the potential moderating effect of publication type (i.e., whether data were published in a peer-reviewed journal vs. unpublished) using metaregression. Second, we used the trim-and-fill procedure to search for indications of publication bias and to examine whether effect sizes change in analyses that adjust for this bias (Duval & Tweedie, 2000; Egger, Davey Smith, Schneider, & Minder, 1997). Third, we conducted sensitivity analyses comparing the average effect size using all studies with the average effect size using only sufficiently powered studies (Carter, Schönbrodt, Gervais, & Hilgard, 2019; Stanley, Doucouliagos, & Ioannidis, 2017).
Finally, we conducted sensitivity analyses that included the three studies that utilized highly specific manifestations of concealment. These sensitivity analyses were performed on both the overall association between sexual orientation concealment and mental health outcomes as well as on associations between sexual orientation concealment and each of the internalizing (i.e., depression, anxiety, general psychological distress, and problematic eating) and externalizing (i.e., substance use) mental health problems.
Statistical analyses were performed using Stata 15 and the macros metan, metareg, and robumeta (StataCorp, 2017).
Results
Figure 1 illustrates the selection process. The initial electronic searches yielded 5,988 records, and 49 additional records were located through manually searching reference lists of included reports and contacting authors of these reports. There were 4,184 unique records once duplicates were removed. Overall, 3,546 records were excluded at the abstract review stage. The remaining 638 records were reviewed in full, and 428 records were excluded at this stage (see Figure 1 for reasons for exclusion). Two hundred ten records detailing 193 unique studies were deemed eligible for inclusion (see Table 1). The 193 studies included a total of 92,236 study participants. The majority of these studies (k = 119; 61.7%) were published in peer-reviewed journals, 51 (26.6%) were unpublished doctoral dissertations, and 21 studies (10.9%) were unpublished; one study was published in a book chapter and one study was an unpublished master’s thesis. We extracted 423 effects of the association between sexual orientation concealment and mental health problems from these 193 unique samples.
Figure 1.
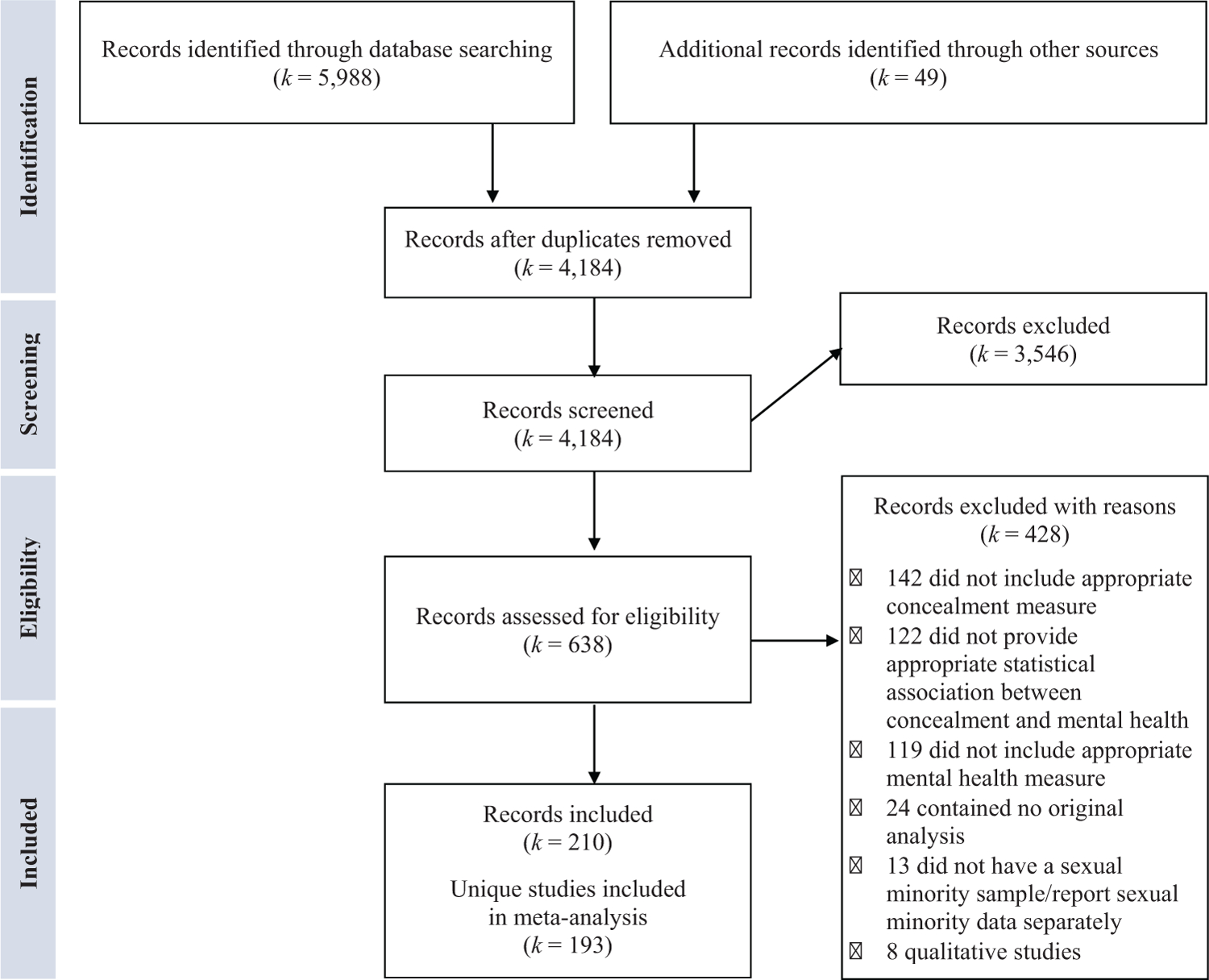
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of article selection.
Overall Effect Size
Table 3 presents the results from the main analysis examining the association between standardized sexual orientation concealment and mental health problems. The analyses showed a small positive association between sexual orientation concealment and mental health problems (k = 193; effect size [ESr] = 0.116 [p < .001]; 95% CI [0.093, 0.141]). Considerable heterogeneity existed between studies: 94.9% of variation between studies was attributable to heterogeneity rather than chance (I2 = 94.9%; τ2 = 0.0325).
Table 3.
Total Mean Association Between Sexual Orientation Concealment and Mental Health Problems (k = 193; n = 92,236)
| Measure | M ESra,b based on study averages | 95% confidence interval | p ESrb | M ESra,b using robust variance estimation | 95% confidence interval | df | Total number of ES | p ESrb | Heterogeneity χ2 | p χ2 | τ2 | I2 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any mental health problem (k = 193) | 0.106 | [0.079, 0.134] | <.001 | 0.116 | [0.093, 0.141] | 192 | 430 | <.001 | 3763.84 | <.001 | 0.0325 | 94.9% |
| Internalizing mental health problems | 0.123 | [0.103, 0.144] | <.001 | 0.126 | [0.102, 0.151] | 187 | 396 | <.001 | 3165.36 | <.001 | 0.0242 | 91.8% |
| Depression (k = 121) | 0.101 | [0.067, 0.133] | <.001 | 0.113 | [0.076, 0.148] | 120 | 179 | <.001 | 1902.44 | <.001 | 0.0296 | 93.7% |
| Anxiety (k = 67) | 0.126 | [0.092, 0.160] | <.001 | 0.134 | [0.088, 0.180] | 66 | 120 | <.001 | 443.86 | <.001 | 0.0153 | 85.1% |
| General psychological distress (k = 65) | 0.155 | [0.122, 0.189] | <.001 | 0.163 | [0.122, 0.204] | 64 | 84 | <.001 | 504.89 | <.001 | 0.0154 | 87.3% |
| Problematic eating (k = 7) | 0.176 | [0.083, 0.266] | <.001 | 0.168 | [0.043, 0.288] | 6 | 13 | 0.017 | 37.18 | <.001 | 0.0134 | 83.9% |
| Substance use problems | ||||||||||||
| Substance use problems (k = 20) | −0.056 | [−0.093, −0.020] | 0.002 | −0.061 | [−0.096, −0.026] | 19 | 34 | 0.002 | 61.24 | <.001 | 0.0033 | 70.6% |
Notes. ES = effect size.
Positive effect sizes indicate a positive association between concealment and mental health problems; negative effect sizes indicate a negative association between concealment and mental health problems.
Effect size based on average correlations across studies.
Factors Contributing to Between-Study Heterogeneity: For Whom and Under What Conditions Is Sexual Orientation Concealment Associated With Mental Health Problems?
In our first analysis of study heterogeneity, we explored potential differences attributable to the type of outcome measure used to assess mental health problems (i.e., depression, anxiety, general psychological distress, problematic eating, and substance use problems). These analyses utilized all available effect sizes from all studies. The analyses showed that mental health problems measured as general psychological distress (b = 0.061 [p = .018]; 95% CI [0.011, 0.111]) and substance use problems (b = ‒0.166 [p = .001]; 95% CI [‒0.247, ‒0.085]) significantly contributed to between-study heterogeneity. Because the type of mental health problem contributed to between-study heterogeneity, we calculated pooled average effects sizes for each mental health problem separately using robust variance estimation (see Table 3). Studies using a measure of general psychological distress to assess mental health problems demonstrated the strongest association between sexual orientation concealment and mental health problems (k = 65; ESr = 0.163 [p < .001]; 95% CI [0.122, 0.204]). Studies using a measure of substance use problems—the only externalizing mental health problem examined here—showed an association between sexual orientation concealment and mental health in the opposite direction, indicating a negative association between concealment and substance use problems (k = 20; ESr = ‒0.061 [p = .002]; 95% CI [‒0.096, ‒0.026]). That is, whereas sexual orientation concealment showed a small positive association with internalizing mental health problems, it showed a small negative association with substance use problems.
Because the results above showed that the association between sexual orientation concealment and mental health problems operated in opposite directions for internalizing mental health problems and substance use problems, subsequent analyses of heterogeneity were stratified and analyzed separately for these two broad types of mental health problems. Power calculations (Valentine, Pigott, & Rothstein, 2010) were used to assess the appropriateness of subsequent tests of moderation. Given the high number of studies contributing effect sizes for internalizing mental health problems (k = 188; average sample size: n = 482), analyses of study heterogeneity could be conducted with sufficient power for all hypothesized moderators. Yet, given the relatively smaller number of studies contributing effect sizes for substance use problems (k = 20; average sample size: n = 886), analyses of heterogeneity for these studies must be interpreted with caution because the nonsignificant results for these analyses could be due to insufficient power, rather than true lack of association.
As the next step in examining the contribution of study and sample characteristics to between-study heterogeneity, we conducted metaregressions in which type of measure of sexual orientation concealment (i.e., lack of active disclosure, lack of open behavior, lack of general openness, and lack of public knowledge), time period (i.e., year of data collection), study location, use of dichotomous measure of concealment, use of dichotomous measure of mental health problem, mean age of participants, proportion of the sample that is male, proportion of the sample that completed at least some college, whether the sample was composed of mostly racial/ethnic minority participants, and whether the sample was exclusively bisexual were used to predict between-study heterogeneity in separate bivariate metaanalyses (see Table 4).
Table 4.
Results From Bivariate Metaregression Analyses of Sexual Orientation Concealment and Mental Health Problems as a Function of Study and Sample Characteristics
| Measure | Bivariate analyses |
|||||||
|---|---|---|---|---|---|---|---|---|
| Internalizing mental health problems |
Substance use problems |
|||||||
| B | SE | 95% CI | p | B | SE | 95% CI | p | |
| Study characteristics | ||||||||
| Type of sexual orientation concealment measure | ||||||||
| 1. Lack of active disclosure | −0.075 | 0.030 | [−0.133, −0.016] | 0.012 | — | — | — | — |
| 2. Lack of open behavior | 0.080 | 0.018 | [0.044, 0.116] | <.001 | 0.016 | 0.028 | [−0.040, 0.074] | .551 |
| 3. Lack of general openness | −0.004 | 0.020 | [−0.043, 0.035] | 0.853 | 0.002 | 0.028 | [−0.061, 0.056] | .934 |
| 4. Lack of public knowledge | −0.089 | 0.025 | [−0.138, −0.040] | <.001 | −0.037 | 0.042 | [−0.123, 0.048] | .383 |
| Time period (year of data collection) | 0.005 | 0.001 | [0.002, 0.008] | <.001 | −0.004 | 0.005 | [−0.009, 0.009] | .932 |
| Study location (North America vs. other regions) | −0.002 | 0.021 | [−0.043, 0.039] | 0.928 | −0.046 | 0.589 | [−0.166, 0.074] | .440 |
| Studies using dichotomous measure of concealment | −0.218 | 0.055 | [−0.326, −0.110] | <.001 | — | — | — | — |
| Studies using dichotomous measure of mental health | −0.142 | 0.052 | [−0.244, −0.039] | 0.007 | −0.065 | 0.030 | [−0.126, −0.005] | .036 |
| Sample characteristics | ||||||||
| Mean age of participants | −0.003 | 0.001 | [−0.0045, −0.0006] | 0.011 | −0.0006 | 0.004 | [−0.008, 0.007] | .879 |
| Proportion male vs. female | 0.0001 | 0.0003 | [−0.0004, 0.0006] | 0.732 | 0.0002 | 0.0003 | [−0.0004, 0.0009] | .480 |
| Proportion completed some college or above | 0.0007 | 0.0005 | [−0.0003, 0.002] | 0.171 | −0.0004 | 0.0008 | [−0.0021, 0.0013] | .651 |
| Proportion racial/ethnic minority | 0.020 | 0.029 | [−0.036, 0.077] | 0.478 | −0.132 | 0.118 | [−0.109, 0.374] | .271 |
| Samples of exclusive bisexual composition | −0.099 | 0.044 | [−0.186, −0.011] | 0.027 | — | — | — | — |
In bivariate analyses among studies examining the association between concealment and internalizing mental health problems, those that measured sexual orientation concealment as lack of open behavior and had data that were collected more recently showed stronger associations between concealment and internalizing mental health problems. In contrast, studies that measured sexual orientation concealment as lack of active disclosure or public knowledge, used a dichotomous measure of concealment, contained participants with an older mean age, and utilized exclusively bisexual samples showed significantly smaller associations between concealment and internalizing mental health problems. We graphically depicted the bivariate associations involving continuous variables. Figure 2 graphically depicts the bivariate association between time period and study effect for the association between sexual orientation concealment and internalizing mental health problems, whereas Figure 3 displays the bivariate association between mean age of study participants and study effect for the association between sexual orientation concealment and internalizing mental health problems. Only one of the proposed moderators was found to significantly explain between-study heterogeneity in the association between concealment and substance use problems, namely whether studies employed a dichotomous measure of substance use problems. Specifically, studies using a dichotomous measure of substance use problems showed significantly smaller associations between concealment and substance use problems than studies using continuous measures of substance use problems. The small number of significant moderators of between-study heterogeneity for substance use problems could, as noted above, be attributable to low power rather than lack of true effect.
Figure 2.
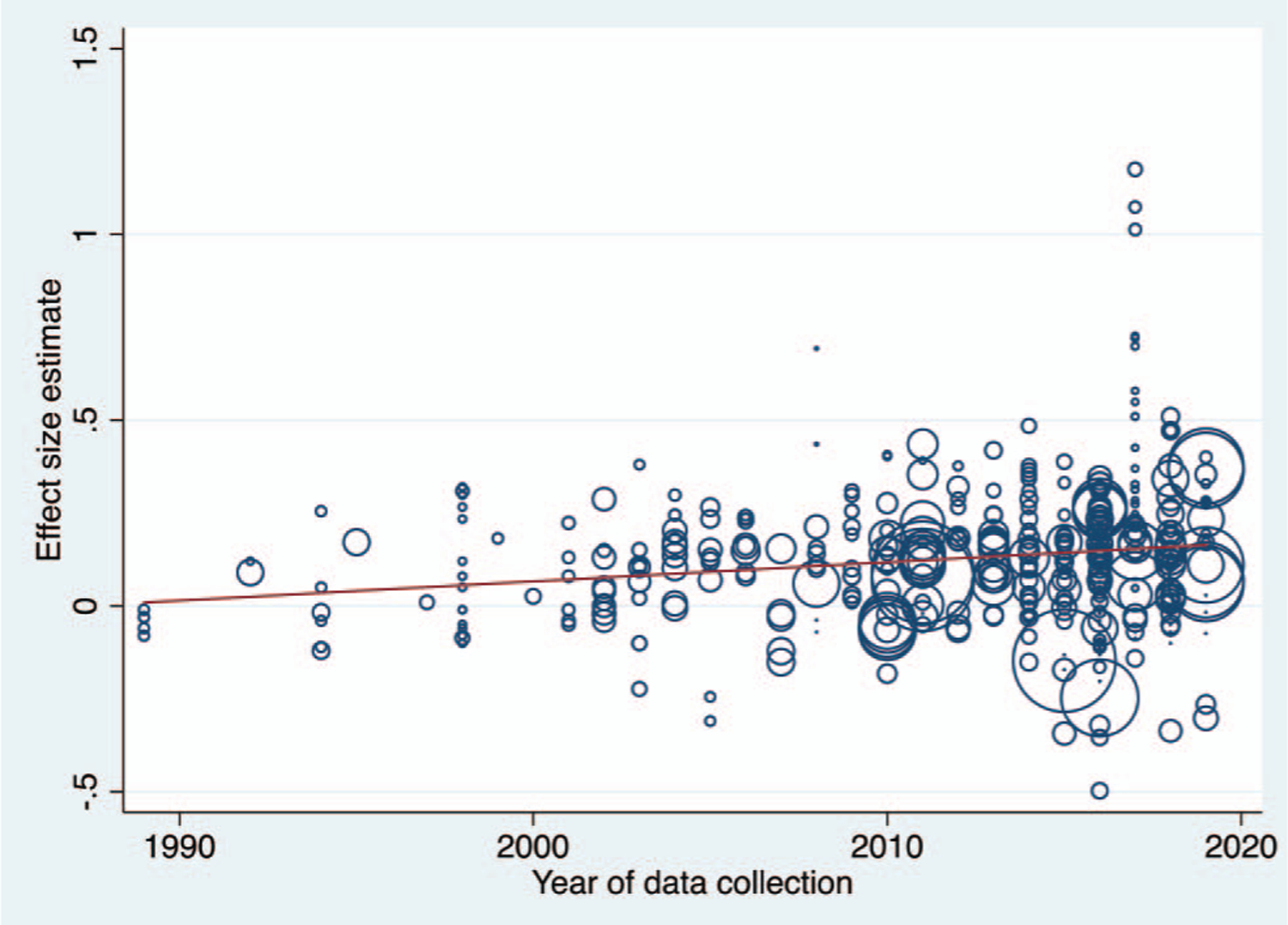
Year of data collection as moderator of the association between sexual orientation concealment and internalizing mental health problems.
Figure 3.
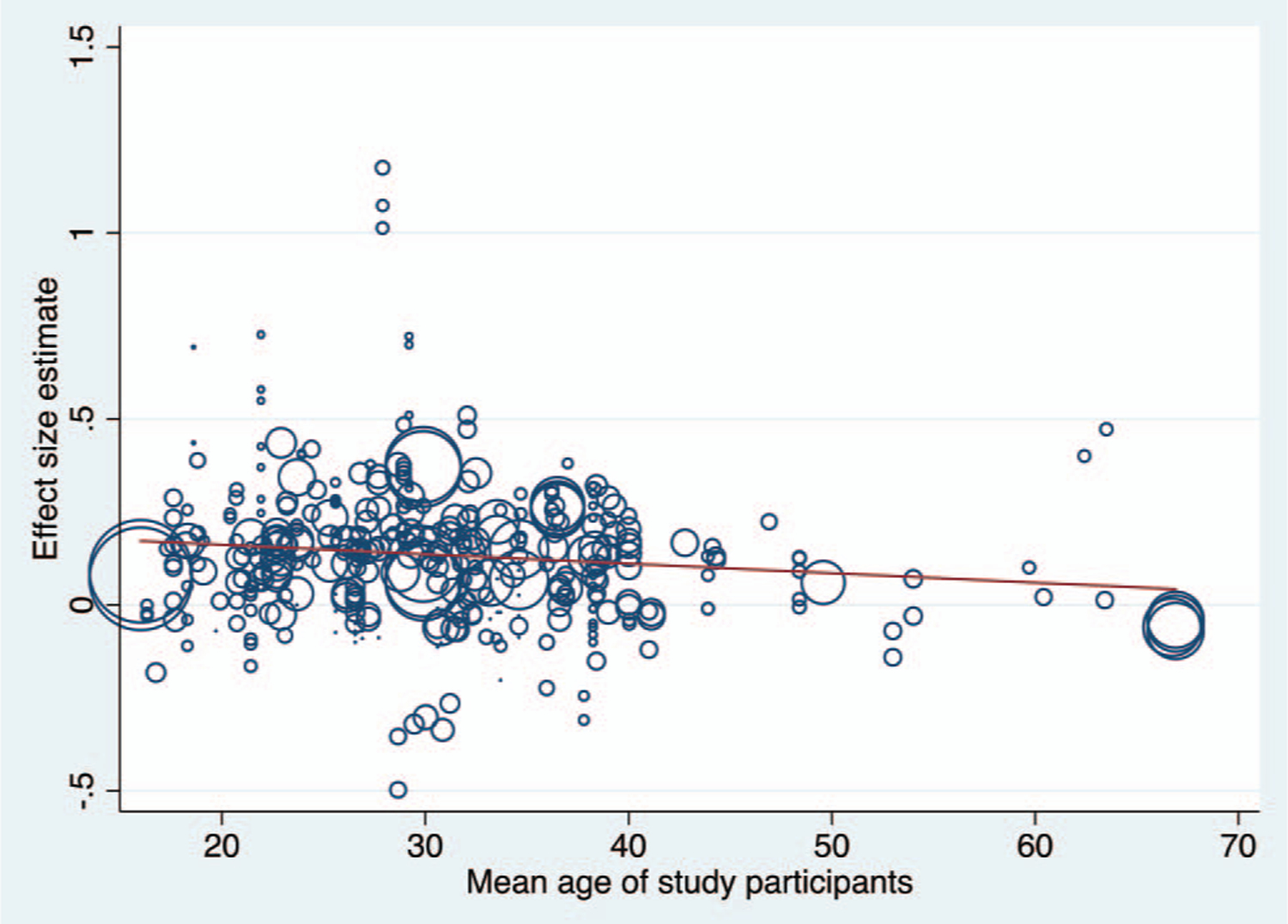
Mean age of study participants as moderator of the association between sexual orientation concealment and internalizing mental health problems.
All variables that significantly contributed to between-study heterogeneity in the association between concealment and internalizing mental health problems in the above bivariate analyses were then entered into a multivariate metaregression analysis, and nonsignificant moderators were removed using backward deletion. The results of the final multivariate metaregression analyses are presented in Table 5. The model included studies measuring sexual orientation concealment as lack of open behavior, mean age of participants, studies using exclusively bisexual samples, and studies using a dichotomous measure of concealment as moderators. The model showed that 16.2% of between-study heterogeneity could be explained by these variables, although a fair amount of unexplained between-study variance remained.
Table 5.
Results From Multivariate Metaregression Analyses of Sexual Orientation Concealment and Internalizing Mental Health Problems
| Internalizing mental health problems |
||||
|---|---|---|---|---|
| Measure | B | SE | 95% CI | p |
| Type of measure of sexual orientation concealment | ||||
| Lack of open behavior | 0.062 | 0.020 | [0.022, 0.102] | .003 |
| Study characteristics | ||||
| Mean age of participants | −0.003 | 0.001 | [−0.005, −0.001] | .007 |
| Samples of exclusive bisexual composition | −0.169 | 0.044 | [−0.256, −0.083] | <.001 |
| Studies using dichotomous measure of concealment | −0.186 | 0.078 | [−0.341, −0.032] | .018 |
| Studies using dichotomous measure of mental health | −0.153 | 0.053 | [−0.258, −0.048] | .005 |
Publication Bias
We conducted several tests to ascertain potential publication bias. First, we analyzed the potential moderating effect of publication type (i.e., whether data were published in a peer-reviewed journal vs. unpublished) using metaregression. The effect reported in published studies was not significantly different from the effect reported in unpublished studies (internalizing mental health problems: b = 0.032 [p = .094]; 95% CI [‒0.005, 0.069]; substance use problems: b = ‒0.050 [p = .079]; 95% CI [‒0.106, 0.006]. Second, we used the trim-and-fill procedure to inspect potential change in the effect size in analyses that adjusted for publication bias. Using the trim-and-fill procedure, we did not estimate any “missing” studies; that is, the distribution of study effect sizes was sufficiently symmetric for studies of both internalizing mental health problems and substance use problems. As a third strategy to analyze potential publication bias, we conducted sensitivity analyses comparing the average effect size using all studies with the average effect size using only sufficiently powered studies. We identified a total of 34 sufficiently powered studies using internalizing mental health problems as an outcome. A sensitivity analysis of the average effect size using only sufficiently powered studies (i.e., studies with Ns > 645) produced a slightly lower average effect size (k = 34; ESr = .080 [p = .005]; 95% CI [0.027, 0.134]) than the effect size found across all studies (k = 188; ESr = .123 [p < .001]; 95% CI [0.103, 0.144]). For studies reporting results for substance use problems, there was only one sufficiently powered study in our records, precluding additional sensitivity analyses. Based on these three means of testing potential publication bias, we conclude that it is unlikely that publication bias substantially affected these meta-analytic results. Potentially, there might be a slight overestimation of our average effect size for studies of the association between concealment and internalizing mental health problems, although the fact that our review finds several null or unexpected associations provides evidence that there is not systematic bias on selecting only significant effects into the literature.
Sensitivity Analysis
In a sensitivity analysis that included the three identified studies using concealment measures that did not match any of the four categories, but which nonetheless captured sexual orientation concealment, albeit from very limited domains (i.e., mental health providers, health care provider, and adult children), we found an identical pattern of results with the only difference from the primary analyses being slightly smaller effect sizes for the associations between sexual orientation concealment and mental health in the sensitivity analysis (see Table 1 in the online supplemental materials).
Discussion
Across 193 unique studies containing a total of 92,236 participants, this conceptual and meta-analytic review finds a small positive association between sexual orientation concealment and mental health problems. Studies that measured mental health in terms of general psychological distress and substance use problems explained a significant proportion of between-study heterogeneity. Studies that examined associations between sexual orientation concealment and internalizing mental health problems (i.e., depression, anxiety, psychological distress, eating problems) showed a small positive association, whereas those that examined associations between sexual orientation concealment and substance use problems showed a small negative association. Further, studies that assessed sexual orientation concealment as lack of open behavior (vs. lack of active disclosure, lack of general openness, and lack of public knowledge) showed larger associations between concealment and internalizing mental health problems. Among studies of internalizing mental health outcomes, those conducted more recently, with younger participants, with exclusively bisexual samples, and with continuous measures of concealment and/or mental health problems showed larger associations than those conducted in the more distant past, with older participants, with heterogeneous minority sexual identities, and with dichotomous measures of concealment and mental health problems. In the multivariate model, the significant moderating effect of time period disappeared but the other significant bivariate moderating effects remained. Study location, sample gender composition, educational attainment, and sample racial and ethnic composition did not explain between-study heterogeneity. Our examination of potential publication bias indicated that the pooled effects of this meta-analysis are likely not influenced by publication bias. Results have implications for conceptual distinctions among mental health problems, measurement selection, life course considerations, and the distinct determinants of bisexual mental health in the study of sexual minority mental health.
Implications for Internalizing Versus Externalizing Mental Health Problems
Results have implications for the conceptual distinction between internalizing and externalizing mental health problems in studies of sexual orientation concealment, and perhaps for the study of sexual minority mental health more broadly. Whereas minority stress theory (Meyer, 2003) represents the most plausible explanation for the association between sexual orientation concealment and internalizing mental health problems, social norms within sexual minority communities have also been found to serve as an additional source of the sexual orientation disparity in substance use (e.g., Cochran et al., 2012; Hatzenbuehler et al., 2008; Hatzenbuehler et al., 2015), although less thoroughly considered than minority stress. On the one hand, our results are consistent with minority stress theory (Meyer, 2003) and the psychosocial model of stigma concealment (Pachankis, 2007), which propose that sexual orientation concealment drives internalizing mental health problems because of its associations with cognitive, affective, and behavioral stress responses to anticipated rejection upon disclosure. On the other hand, our results also expand those theories to further consider the perhaps paradoxical negative association of concealment with substance use problems—the one externalizing mental health problem examined here. Specifically, perhaps sexual minorities who conceal are less embedded within sexual minority communities than those who are open, which would lead to less exposure to the more permissive norms about substance use in sexual minority communities (compared with heterosexual communities) and therefore less substance use among sexual minorities who conceal (Cochran et al., 2012). This finding is further supported by sociological accounts of substance use within sexual minority communities, which find that stigma has historically constrained sexual minority socializing to venues in which substance use is common (Hughes et al., 2016; Trocki et al., 2005).
Taken together, results are consistent with minority stress theory’s proposed positive association between concealment and mental health problems when those problems are operationalized as internalizing problems. Although the minority stress of concealment might also contribute to sexual minorities’ substance use, other protective factors seem to outweigh those stressors to predict a negative association between concealment and this externalizing outcome. Based on the present findings, future studies of sexual minority mental health might seriously consider examining distinct determinants of, or distinct patterns of associations between, social determinants of mental health and internalizing versus externalizing mental health problems separately. At the same time, the average size of the association between concealment and both internalizing mental health problems and substance use problems is small, making tentative any practical implications of these findings.
Implications for Measurement
Results also have implications for measurement. Studies that measured sexual orientation as lack of open behavior showed significantly larger associations between concealment and internalizing mental health problems than studies that measured sexual orientation concealment as lack of active disclosure, lack of general openness, and participants’ perceptions that others were not aware of their sexual orientation. Studies of concealment as lack of open behavior are those that focus on behaviorally managing the visibility of one’s sexual minority status in interactions with others (e.g., through avoiding certain topics of conservation, such as dating). This construct is most frequently measured with the Outness Inventory (Mohr & Fassinger, 2000), which assesses both whether important others do not know of one’s sexual orientation and how infrequently it is discussed with them, thereby distinguishing it from studies of lack of active disclosure, lack of general openness, or lack of public knowledge. Our finding of a comparatively larger association between this measure of concealment (vs. the other concealment operationalizations) and internalizing mental problems therefore suggests that sexual orientation concealment, when conceptualized as this deeper, more ongoing level of engagement with one’s identity (rather than an all-or-nothing disclosure on the one hand or general openness on the other), has significantly stronger implications for mental health. Perhaps some sexual minorities who are “out” nonetheless still grapple with their sexual identity. This grappling, perhaps, is captured by the “how infrequently it is discussed” component of the Outness Inventory, which applies even to those who are already out. Measures in our open behavior category catch this nuance and its implications for mental health, but measures in the other categories may not distinguish as well between those who are out without ambivalence and those who may be out but still find their sexual orientation to be difficult to discuss or to otherwise more deeply engage on an ongoing basis. Of course, given that our analysis cannot establish directionality, perhaps the inverse is also true—that internalizing mental health problems leads one to avoid that type of deeper, ongoing public engagement of their sexual orientation more than it leads them to avoid more discrete disclosures or more general open behavior.
The larger association with internalizing mental health problems found for studies measuring concealment as lack of open behavior might also be a function of the types of studies represented in this review. Because most studies concerning sexual orientation concealment and mental health problems are conducted using nonprobability samples of relatively open participants in relatively accepting societies, perhaps many participants have already actively disclosed their sexual orientation to many or most others in their lives (Category 1: lack of active disclosure) and consider themselves to be generally open (Category 3: lack of general openness). Therefore, measuring concealment in these ways might not yield sufficient variation from which to meaningfully predict mental health. Still, even those sexual minorities who have disclosed their sexual orientation and are generally open might nonetheless suppress open behavior, mannerisms, and appearance on a day-to-day basis, especially depending on their daily social context. Therefore, we recommend that future studies conducted with relatively open sexual minority samples in relatively accepting societal contexts at least assess sexual orientation concealment as lack of open behavior (Category 2: lack of open behavior), whether or not they also assess concealment using one of the other approaches reviewed here. Of course, future studies in contexts in which acceptance, and therefore openness, are not the norm might find that assessing concealment as lack of active disclosure and lack of general openness also yields sufficient variation for meaningful prediction.
Practically, our results show that researchers might wish to conceptualize and measure sexual orientation concealment in terms of lack of open behavior rather than lack of active disclosure, lack of general openness, or lack of public knowledge, when examining associations with mental health. Of course, construct selection depends on study purpose and studies seeking to understand mental health implications of discrete disclosures or general open behavior ought to select measures of those respective constructs and be prepared to understand the theoretical meaning of weak associations that might result. The present meta-analysis did not investigate associations between concealment and outcomes other than mental health (e.g., physical health, social behavior) or social determinants of concealment (e.g., childhood influences, current social context). Researchers of those constructs should therefore consider the present findings in light of the theoretical associations among those constructs.
Life Course Implications
Results also have implications for the life course study of sexual minority mental health. Compared with more distantly conducted studies, more recently conducted studies demonstrated a significantly larger association between sexual orientation concealment and internalizing mental health problems. This finding can potentially be interpreted in terms of the substantial cohort effects affecting this population (e.g., Cohler & Hammack, 2007; Hammack et al., 2018; Russell & Fish, 2019). For instance, the association between concealment and internalizing mental health problems might be more marked for more recent cohorts because of the relatively fewer benefits of remaining closeted today than in years past, at least in the relatively accepting contexts in which most of the included studies were conducted. The disclosure process model (Chaudoir & Fisher, 2010) suggests that the decision to conceal a stigmatized identity is a function of the perceived benefits of concealment weighed against the costs of disclosure. In the primarily North American research field that we review in the present study, the costs of disclosure for today’s sexual minorities are, for many, notably fewer than the costs of concealment because of the rapid societal change that has afforded sexual minorities numerous advantages of disclosure that did not exist in previous decades (e.g., Flores, 2019).
Life course considerations of sexual minority mental health are also expanded by the age effects found here. Specifically, we find that studies of younger participants demonstrated a larger association between concealment and mental health problems than studies of older participants, inviting the possibility that younger sexual minorities possess fewer psychological (e.g., emotion regulation) and contextual (e.g., geographic mobility, affirmative mental health care) resources for coping with the stressors of concealment than older sexual minorities (Casey et al., 2008; Durso & Meyer, 2013; Hatzenbuehler & Pachankis, 2016). Further, social stressors such as concealment—especially if motivated by fears of targeted rejection—might have a relatively larger impact during adolescence and young adulthood than in later adulthood (Andersen & Teicher, 2008; Charmandari et al., 2003; Leussis & Andersen, 2008; Murphy et al., 2013; Romeo et al., 2006). Notably, although several studies in this review were comprised of young adults (e.g., D’Augelli et al., 2002; Rosario, Schrimshaw, & Hunter, 2006; Shilo & Savaya, 2012), very few were comprised solely of adolescents (e.g., Kosciw et al., 2015). Together, these results suggest the essential role of life course considerations in studies of sexual orientation concealment and mental health problems and call for future studies across age cohorts, as further emphasized below.
Distinct Implications of Concealing Bisexuality
Results also have implications for understanding the significant mental health disparity between bisexual versus gay and lesbian individuals (Bostwick et al., 2010). We find that the association between concealment and internalizing mental health problems is smaller for bisexual compared with gay and lesbian individuals. As noted earlier, bisexual individuals endorse less centrality of their minority sexual identities to their overall sense of self than do gay and lesbian individuals (e.g., Dyar, Feinstein, & London, 2014). Any stressors associated with such an identity are therefore likely to be less impactful for bisexual individuals’ mental health, as their bisexual identities might not be as deeply tied to their overall sources of personal and collective esteem as are gay and lesbian identities (Ashmore, Deaux, & McLaughlin-Volpe, 2004). Further, the smaller association between concealment and mental health problems found for studies of exclusive bisexual composition might be attributble to stigma. Specifically, because bisexual individuals’ identities are less reflected in institutions and normative discourse both within general society and within gay and lesbian communities (Steinman, 2000), any protective effects of disclosure, such as increased social support or access to other identity-specific protections (Chaudoir & Fisher, 2010), are likely to be smaller. Of course, bisexuality comprises a remarkably diverse set of experiences, calling for future research to examine subgroup differences within bisexual populations in the association between concealment and mental health problems and the mechanisms that unite them or not in this population.
Methodological Limitations of Existing Research and Future Directions
The fact that study location, sample gender composition, educational attainment, and sample racial and ethnic composition did not explain between-study heterogeneity highlights some of the distinct methodological features and limitations of the studies included here. These common study limitations in turn suggest several methodological improvements for future research.
First, understanding the mental health consequences of concealment requires methodological designs capable of establishing causal inference. With notable exceptions (e.g., Pachankis, Sullivan, Feinstein, & Newcomb, 2018; Rosario et al., 2009), few longitudinal studies have been conducted on the association between sexual orientation concealment and mental health and no experimental study has been conducted that has manipulated the concealment demands placed upon sexual minorities to examine downstream mental health. Related research has found that sexual minorities exposed to a discriminatory video clip are less likely to disclose their sexual orientation in a subsequent written reflection task than those exposed to an affirming video clip (Seager, 2016). Conversely, other experimental research shows that sexual minority men who write about minority stress experiences are more likely to disclose their sexual orientation three months later (Pachankis & Goldfried, 2010). Whereas these studies suggest that discrimination can cause sexual orientation concealment and writing about minority stress can encourage disclosure, they do not examine whether sexual orientation concealment causes mental health problems. Experimental research with other populations with concealable stigmas (e.g., those with eating disorders) suggests that stigma concealment can drive cognitive, affective, and behavioral manifestations of internalizing problems (e.g., Smart & Wegner, 1999). Still, future research is needed to rule out reverse causality, as depression and anxiety might also diminish sexual orientation disclosure (Mohr & Fassinger, 2003), perhaps through personality traits that explain tendencies toward both concealment and internalizing problems (e.g., Larson et al., 2015).
Second, nearly all studies included in this meta-analysis utilized nonprobability sampling and many recruited participants by posting messages in online forums geared to sexual minority communities. Although nonprobability sampling can generate samples of sexual minorities that are uncharacteristic of the total sexual minority population, this concern is particularly problematic when the sample unrepresentativeness directly relates to the variables under study (Meyer & Wilson, 2009), as is the case with studies of concealment. Specifically, nonprobability sampling overrepresents the experience of sexual minorities who are open about their sexual orientation, compared with those who are not open (Hottes et al., 2016; Kuyper et al., 2016). Nonprobability samples also tend to overrepresent the experience of those who are young, preventing stronger tests of the life course effects suggested here. The very few published population-based studies of sexual orientation concealment and mental health find that a substantial number of sexual minorities in the general population report not being out to others and that mental health varies as a function of concealment (Pachankis et al., 2015; van der Star et al., 2018). Future research ought to take advantage of increasing opportunities to use probability-based designs, which are particularly suited to studying phenomena like concealment that are directly related to sampling. Population-based cohort studies, in particular, would allow a strong test of both developmental and cohort influences on concealment and mental health problems, thereby offering a stronger test of the causal direction of these variables than currently exists.
Third, the lack of significant moderating effects for certain demographic factors might be explained by the necessarily crude approach used to classify moderator variables across 193 studies. For instance, this meta-analysis examined race and ethnicity as the proportion of the study sample that was composed of racial and ethnic minority participants. The crude manner by which we examined the moderating influence of ethnicity and race (i.e., in terms of the proportion of the sample that identified as any racial or ethnic minority) prevented us from examining distinct experiences among different racial and ethnic minority subgroups. Indeed, concealment is unlikely to be experienced identically across all races and ethnicities (e.g., Villicana et al., 2016). Therefore, future investigations into the concealment-related experiences of diverse sexual minority populations might consider first qualitatively exploring whether and how diverse populations experience sexual orientation concealment (e.g., Bowleg, Burkholder, Teti, & Craig, 2008) so as to capture relevant mechanisms or moderators of the association between concealment and mental health problems across subgroups.
Fourth, study location was coded as whether or not a study was conducted in North America. Several factors limited our ability to conduct a finer-grained examination of the geographic influences on the association between concealment and mental health. First, preventing analysis of state/provincial effects, approximately two thirds of included studies were collected in general U.S. samples across multiple states and regions, many completely online. Preventing analysis of country effects, only 22.3% of studies contained data collected outside of North America. Given wide variation of sexual minority-related structural stigma within states/provinces and countries, ideally geographic effects would utilize structural stigma measured at the city, municipality, or county level. Yet, only 4.2% of studies contained this information and nearly all of these reported data from large U.S. cities (e.g., New York, Los Angeles, Miami) that contain high degrees of sexual minority acceptance, precluding sufficient variation in geography-bound structural stigma necessary to detect its influence on the association between concealment and mental health. Nonetheless, the finding regarding the lack of difference in effects between studies conducted within versus outside North America tentatively suggests the geographic generalizability of the effect found here. Future research could link indicators of community-level structural stigma, such as those in the General Social Survey or Project Implicit, to nationwide surveys that contain measures of sexual orientation concealment and mental health (e.g., Lattanner et al., 2020).
Fifth, measurement approaches commonly utilized across studies of sexual orientation concealment and mental health problems constrain results and suggest future directions. For instance, most studies utilized self-reports of concealment and mental health. In addition to introducing same-source confounding, such measurements potentially weaken associations because of weak psychometric properties. Although most included studies utilized established measures of mental health outcomes with high reliability, distinct outcomes (e.g., depression and anxiety) were often examined using subscales of the same scale, potentially introducing artificial overlap not explained by true comorbidity across conditions. To increase validity of findings in this area, future research ought to employ interviewer-based assessments with strong construct validity. Our findings also suggest that the use of continuous measures of concealment and mental health outcomes are likely to yield stronger effects, given preserved power when using continuous rather than dichotomous measures (Altman & Royston, 2006). Future studies might also consider expanding outcomes to include physical health outcomes. In fact, compelling evidence suggests that stigma-related stress can have distinct, even opposite, implications for physical and mental health (Jackson, Knight, & Rafferty, 2010), which our analysis could not capture.
Finally, this meta-analysis finds a small average effect size between concealment and mental health problems, suggesting that future research, including meta-analytic studies, seek to identify the relative mental health impact of concealment alongside the other factors suggested by existing theories of stigma and sexual minority mental health. As noted earlier, minority stress theory (Meyer, 2003), the psychological mediation framework (e.g., Hatzenbuehler, 2009), and the disclosure process model (Chaudoir & Fisher, 2010) specify numerous other factors that likely contribute to this population’s mental health, which studies are increasingly examining simultaneously (e.g., Timmins, Rimes, & Rahman, 2020). To the extent that meta-analytic evidence could be brought to bear on the relative influence of these factors—from discrimination and victimization to anticipated rejection, rumination, social support, and community norms—psychological science will be best positioned to intervene effectively.
Conclusions
In conclusion, this meta-analysis reveals a small positive association between sexual orientation concealment and internalizing mental health problems and a small negative association between sexual orientation concealment and substance use problems. The association between sexual orientation concealment and internalizing mental health problems was somewhat larger in those studies that assessed concealment as lack of open behavior, those conducted recently, and those with younger samples; it was smaller in exclusively bisexual samples. This review highlights several directions in future measurement of sexual orientation concealment and the need for stronger tests of causality, representative sampling, more nuanced assessment of potential effect moderators, geographic diversity, more valid measurement approaches, and meta-analytic examinations of concealment alongside the numerous other determinants of this population’s mental health. Although these recommendations apply to all sexual minority mental health research, they are particularly relevant to the study of sexual orientation concealment given the distinct methodological challenges posed by this phenomenon. These advances will allow researchers to come closer to answering how and under what circumstances sexual orientation concealment—a pervasive aspect of the sexual minority experience—comes to shape the health of this population.
Supplementary Material
Public Significance Statement.
Across 193 studies, sexual orientation concealment demonstrates small positive associations with internalizing mental health problems (i.e., depression, anxiety, distress, problematic eating) and a small negative association with substance use problems, suggesting potentially distinct pathways to these outcomes among sexual minorities. The association between sexual orientation concealment and mental health likely depends on the time period in which the study was conducted, the specific measurement of concealment used, and the age and sexual identity of sexual minority participants.
Acknowledgments
Skyler D. Jackson’s contributions were supported by a training grant from the National Institute of Mental Health (T32 MH020031). The content is the sole responsibility of the authors and does not represent the official views of the National Institute of Mental Health or the National Institutes of Health. The authors acknowledge the helpful input of Kate Nyhan who provided research librarian support including reviewing our Boolean and proximity indicators, subject headings and MeSH terms, the text word search process, search spelling and syntax, and limits and filters; suggesting databases to retrieve non–English language studies; and testing our searches. We also thank Dominic Schnabel for his contributions to database searching and record review. Finally, we thank the many researchers who responded to our requests by sharing the information necessary to conduct this meta-analysis.
Appendix. Full PsycINFO Search Strategy
Field Labels
exp/= exploded controlled term
/= non exploded controlled term
.ti,ab,id. = title, abstract and author keywords
cq,ca,in = Correspondence address, corporate/institutional author, institution
adjx = within x words, regardless of order
* = truncation of word for alternate endings
bisexuality/
exp homosexuality/
same sex intercourse/
same sex couples/
same sex marriage/
(queer* or LGB* or LGBTQ or LGBQ or LGBTQI or GLB or LGB or LGBT or GLBT or homosexual* or lesbian* or gay* or bisexual* or bisexual* or sexual minorit* or sexual orientation* or bicurious or lesbigay* or men who have sex with men or MSM or MSMW or men loving men or same sex or same sex couple* or same sex relation* or women loving women or “women who have sex with women” or WSW or same gender loving or same-gender loving or same-gender-loving or asexual* or demisexual* or pansexual* or polysexual* or polyamor*).ti,ab,id.
or/1–6
exp mental disorders/
exp mental health/
exp chronic mental illness/
exp anxiety disorders/
exp affective disorders/
exp eating disorders/
exp substance use disorder/
exp drug seeking/
exp drug addiction/
exp drug usage/
exp amphetamine/
exp hallucinogenic drugs/
exp alcohol drinking patterns/
exp alcoholism/
cocaine/
tobacco smoking/
binge eating/
anxiety/
social anxiety/
“depression (emotion)”/
stress/
chronic stress/
psychological stress/
social stress/
(mental health or mental disorder* or mental illness* or behavioral health or behavioral health or anxiety or feeding disorder* or eating disorder* or appetite disorder* or anorexi* or binge-eating or bulimi* or rumination disorder or food addict* or compulsive eating or night eating or pica or allotriophagy or geophagia or mood disorder* or affective disorder or depressive or depression or melancholia* or dysthymic or stress* or psychological distress* or distress* or psychological wellbeing or wellbeing or psychological well-being or well-being or addict* or etoh or alcohol* or alcohol us* or alcohol abuse or alcohol dependen* or drug* or drug us* or drug abuse or drug dependen* or substance* or substance us* or substance abuse or substance dependence or cocaine or amphetamine* or methamphetamine* or smoking or cigarette or tobacco or marijuana or cannabis or hallucinogen* or ecstasy or crystal meth or heroin or MDMA or GHB or ketamine or LSD).ti,ab,id.
or/8–32
(conceal* OR closet* OR disclos* OR nondisclos* OR undisclos* OR outness OR coming-out OR coming out OR open* OR cover*).ti,ab,id.
7 and 33 and 34
Footnotes
Supplemental materials: http://dx.doi.org/10.1037/bul0000271.supp
Study data and analysis code for all analyses contained in this article are located at https://osf.io/4e2bs/.
Contributor Information
John E. Pachankis, Department of Social and Behavioral Sciences, Yale School of Public Health
Skyler D. Jackson, Department of Social and Behavioral Sciences, Yale School of Public Health.
Benjamin K. Fetzner, Department of Social and Behavioral Sciences, Yale School of Public Health.
Conor P. Mahon, School of Psychology, Dublin City University
Richard Bränström, Department of Social and Behavioral Sciences, Yale School of Public Health, and Department of Clinical Neuroscience, Karolinska Institutet..
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Akerlund M, & Cheung M (2000). Teaching beyond the deficit model. Journal of Social Work Education, 36, 279–292. 10.1080/10437797.2000.10779008 [DOI] [Google Scholar]
- Altman DG, & Royston P (2006). The cost of dichotomising continuous variables. British Medical Journal, 332, 1080. 10.1136/bmj.332.7549.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen SL, & Teicher MH (2008). Stress, sensitive periods and maturational events in adolescent depression. Trends in Neurosciences, 31, 183–191. 10.1016/j.tins.2008.01.004 [DOI] [PubMed] [Google Scholar]
- *Antebi-Gruszka N, & Schrimshaw EW (2018). Negative attitudes toward same-sex behavior inventory: An internalized homonegativity measure for research with bisexual, gay, and other non–gay-identified men who have sex with men. Psychology of Sexual Orientation and Gender Diversity, 5, 156–168. 10.1037/sgd0000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Aranda F (2010). Coming out in color: The effects of level of outness on depression (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3417538)
- Ashmore RD, Deaux K, & McLaughlin-Volpe T (2004). An organizing framework for collective identity: Articulation and significance of multidimensionality. Psychological Bulletin, 130, 80–114. 10.1037/0033-2909.130.1.80 [DOI] [PubMed] [Google Scholar]
- *Ayala J, & Coleman H (2000). Predictors of depression among lesbian women. Journal of Lesbian Studies, 4, 71–86. 10.1300/J155v04n03_0424802684 [DOI] [Google Scholar]
- *Baams L, Dubas JS, Russell ST, Buikema RL, & van Aken MAG (2018). Minority stress, perceived burdensomeness, and depressive symptoms among sexual minority youth. Journal of Adolescence, 66, 9–18. 10.1016/j.adolescence.2018.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Baams L, Grossman AH, & Russell ST (2015). Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Developmental Psychology, 51, 688–696. 10.1037/a0038994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Balsam KF, & Mohr JJ (2007). Adaptation to sexual orientation stigma: A comparison of bisexual and lesbian/gay adults. Journal of Counseling Psychology, 54, 306–319. 10.1037/0022-0167.54.3.306 [DOI] [Google Scholar]
- Balsam KF, Rothblum ED, & Beauchaine TP (2005). Victimization over the life span: A comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical Psychology, 73, 477–487. 10.1037/0022-006X.73.3.477 [DOI] [PubMed] [Google Scholar]
- Barnes DM, Hatzenbuehler ML, Hamilton AD, & Keyes KM (2014). Sexual orientation disparities in mental health: The moderating role of educational attainment. Social Psychiatry and Psychiatric Epidemiology, 49, 1447–1454. 10.1007/s00127-014-0849-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett DC, & Pollack LM (2005). Whose gay community? Social class, sexual self-expression, and gay community involvement. The Sociological Quarterly, 46, 437–456. 10.1111/j.1533-8525.2005.00021.x [DOI] [Google Scholar]
- *Beaber T (2008). Well-being among bisexual females: The roles of internalized biphobia, stigma consciousness, social support, and self-disclosure (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3310083)
- Beals KP, Peplau LA, & Gable SL (2009). Stigma management and well-being: The role of perceived social support, emotional processing, and suppression. Personality and Social Psychology Bulletin, 35, 867–879. 10.1177/0146167209334783 [DOI] [PubMed] [Google Scholar]
- *Beard K, Eames C, & Withers P (2017). The role of self-compassion in the well-being of self-identifying gay men. Journal of Gay & Lesbian Mental Health, 21, 77–96. 10.1080/19359705.2016.1233163 [DOI] [Google Scholar]
- *Becraft RS (1992). Lesbian identity and self-disclosure: Effects on depression (Master’s thesis). California State University, Long Beach. [Google Scholar]
- *Bejakovich T, & Flett R (2018). “Are you sure?”: Relations between sexual identity, certainty, disclosure, and psychological well-being. Journal of Gay & Lesbian Mental Health, 22, 139–161. 10.1080/19359705.2018.1427647 [DOI] [Google Scholar]
- *Birichi DK (2015). Minority stress and well-being in adult gay men: The mediating role of authenticity (Doctoral dissertation). Retrieved from Open Access Dissertations database. (No. 1503)
- *Bittner KE (2016). Trans*forming understanding of sexual orientation and gender variant minorities: Testing the minority stress model with a diverse sample (Doctoral dissertation). Retrieved from Iowa State University Capstones, Theses and Dissertations Digital Repository. (No. 15879)
- *Blashill AJ (2016). Dysmorphia in sexual minorities. Unpublished raw data, Department of Psychology, San Diego State University, San Diego, CA. [Google Scholar]
- *Blashill AJ (2018). Dysmorphia in sexual minorities. Unpublished raw data, Department of Psychology, San Diego State University, San Diego, CA. [Google Scholar]
- *Bosker MJ (2002).Assessing level of outness among gay, lesbian, and bisexual individuals and its relation to depression, anxiety, and self-esteem (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3083228)
- Bostwick WB, Boyd CJ, Hughes TL, & McCabe SE (2010). Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. American Journal of Public Health, 100, 468–475. 10.2105/AJPH.2008.152942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Burkholder G, Teti M, & Craig ML (2008). The complexities of outness: Psychosocial predictors of coming out to others among Black lesbian and bisexual women. Journal of LGBT Health Research, 4, 153–166. 10.1080/15574090903167422 [DOI] [PubMed] [Google Scholar]
- Bränström R (2019). Community-based stress in sexual minorities. Unpublished raw data, Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden. [Google Scholar]
- *Brewster ME (2011).The roles of cognitive flexibility, bicultural self-efficacy, and minority stress in the mental health of bisexual individuals (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3586294) [DOI] [PubMed]
- *Brewster ME, Moradi B, DeBlaere C, & Velez BL (2013). Navigating the borderlands: The roles of minority stressors, bicultural self-efficacy, and cognitive flexibility in the mental health of bisexual individuals. Journal of Counseling Psychology, 60, 543–556. 10.1037/a0033224 [DOI] [PubMed] [Google Scholar]
- Burton CL, Clark KA, & Pachankis JE (2020). Risk from within: Intraminority gay community stress and sexual risk-taking among sexual minority men. Annals of Behavioral Medicine. Advance online publication. 10.1093/abm/kaaa014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Byrd JL (2015). The role of cyberbullying victimization in sexual minority adolescents’ reported levels of depression and anxiety (Doctoral dissertation). Retrieved from Scholarship & Creative Works @ Digital UNC.
- Calzo JP, Antonucci TC, Mays VM, & Cochran SD (2011). Retrospective recall of sexual orientation identity development among gay, lesbian, and bisexual adults. Developmental Psychology, 47, 1658–1673. 10.1037/a0025508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Carden. (2009). Relationship of thought suppression and emotion suppression to lesbians’ and gay men’s levels of outness: Investigating the effects of chronic suppression. (Doctoral dissertation). Retrieved from http://etd.auburn.edu/handle/10415/1802
- *Carroll RE (1995). The relationship of internalized heterosexism and outness about a lesbian sexual orientation to psychological adjustment (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9605347)
- Carter EC, Schönbrodt FD, Gervais WM, & Hilgard J (2019). Correcting for bias in psychology: A comparison of meta-analytic methods. Advances in Methods and Practices in Psychological Science, 2, 115–144. 10.1177/2515245919847196 [DOI] [Google Scholar]
- Casey BJ, Jones RM, & Hare TA (2008). The adolescent brain. Annals of the New York Academy of Sciences, 1124, 111–126. 10.1196/annals.1440.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chan AKN (2017). The role of interpersonal competence in relation to psychological symptoms among lesbian and gay adults in Hong Kong (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10620098)
- *Chan RCH, Operario D, & Mak WWS (2020). Bisexual individuals are at greater risk of poor mental health than lesbians and gay men: The mediating role of sexual identity stress at multiple levels. Journal of Affective Disorders, 260, 292–301. 10.1016/j.jad.2019.09.020 [DOI] [PubMed] [Google Scholar]
- Charmandari E, Kino T, Souvatzoglou E, & Chrousos GP (2003). Pediatric stress: Hormonal mediators and human development. Hormone Research, 59, 161–179. 10.1159/000069325 [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, & Fisher JD (2010). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity. Psychological Bulletin, 136, 236–256. 10.1037/a0018193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chaudoir SR, & Quinn DM (2016). Evidence that anticipated stigma predicts poorer depressive symptom trajectories among emerging adults living with concealable stigmatized identities. Self and Identity, 15, 139–151. 10.1080/15298868.2015.1091378 [DOI] [Google Scholar]
- Chesir-Teran D, & Hughes D (2009). Heterosexism in high school and victimization among lesbian, gay, bisexual, and questioning students. Journal of Youth and Adolescence, 38, 963–975. 10.1007/s10964-008-9364-x [DOI] [PubMed] [Google Scholar]
- *Chiang SYX (2009). The impact of coming-out and internalized homo-negativity on Asian and Caucasian gay men’s psychological wellbeing and distress (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3615553)
- *Clark EA (2012). Monogamously-partnered bisexual women’s experiences of prejudice and support (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3559678)
- Clark LA, & Watson D (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316–336. 10.1037/0021-843X.100.3.316 [DOI] [PubMed] [Google Scholar]
- *Clemens SC (2004). Extent of outness, depressive distress, and mental health concerns among African American lesbians (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3133422)
- Cochran SD, Grella CE, & Mays VM (2012). Do substance use norms and perceived drug availability mediate sexual orientation differences in patterns of substance use? Results from the California Quality of Life Survey II. Journal of Studies on Alcohol and Drugs, 73, 675–685. 10.15288/jsad.2012.73.675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, & Mays VM (2009). Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology, 118, 647–658. 10.1037/a0016501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112, 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- *Cohen JM (2016). Anxiety and related disorders and concealment in sexual minority young adults (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10247473) [DOI] [PMC free article] [PubMed]
- *Cohen JM, Blasey C, Barr Taylor C, Weiss BJ, & Newman MG (2016). Anxiety and related disorders and concealment in sexual minority young adults. Behavior Therapy, 47, 91–101. 10.1016/j.beth.2015.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohler BJ, & Hammack PL (2007). The psychological world of the gay teenager: Social change, narrative, and normality. Journal of Youth and Adolescence, 36, 47–59. 10.1007/s10964-006-9110-1 [DOI] [Google Scholar]
- *Cole SW, Kemeny ME, Taylor SE, Visscher BR, & Fahey JL (1996). Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosomatic Medicine, 58, 219–231. 10.1097/00006842-199605000-00005 [DOI] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. 10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Corrington A, Nittrouer CL, Trump-Steele RCE, & Hebl M (2019). Letting him B: A study on the intersection of gender and sexual orientation in the workplace. Journal of Vocational Behavior, 113, 129–142. 10.1016/j.jvb.2018.10.005 [DOI] [Google Scholar]
- *Currin JM, Hubach RD, Crethar HC, Hammer TR, Lee HS, & Larson M (2018). Barriers to accessing mental healthcare for gay and bisexual men living in Oklahoma. Sexuality Research & Social Policy, 15, 483–496. 10.1007/s13178-018-0321-5 [DOI] [Google Scholar]
- *D’Augelli AR (2002). Mental health problems among lesbian, gay, and bisexual youths ages 14 to 21. Clinical Child Psychology and Psychiatry, 7, 433–456. 10.1177/1359104502007003039 [DOI] [Google Scholar]
- *D’Augelli AR (2003). Lesbian and bisexual female youths aged 14 to 21: Developmental challenges and victimization experiences. Journal of Lesbian Studies, 7, 9–29. 10.1300/J155v07n04_02 [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Hershberger SL, & Pilkington NW (1998). Lesbian, gay, and bisexual youth and their families: Disclosure of sexual orientation and its consequences. American Journal of Orthopsychiatry, 68, 361–371. 10.1037/h0080345 [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Pilkington NW, & Hershberger SL (2002). Incidence and mental health impact of sexual orientation victimization of lesbian, gay, and bisexual youths in high school. School Psychology Quarterly, 17, 148–167. 10.1521/scpq.17.2.148.20854 [DOI] [Google Scholar]
- *Deitch EA (2002). Concealable stigma and well-being: The role of social identity as a buffer against sexual orientation discrimination in the workplace (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3046640)
- *De Lucia R, Smith NG, Ross LE, Mohr JJ, & King B (2018, August). The relationship of bisexual men’s discrimination, concealment, and depression. American Psychological Association Annual Convention. Poster session presented at the 2018 convention of the American Psychological Association, San Francisco, CA. [Google Scholar]
- *Detwiler BP (2015). Minority stress in the sexual minority older adult population: Exploring the relationships among discrimination, mental health, and quality of life (Doctoral dissertation). Retrieved from Lehigh Preserve, Theses and Dissertations Database. (No. 2571)
- *Diaz JE, Schrimshaw EW, Nandi V, Koblin B, van Tieu H, & Frye V (2018). Syndemic factors associated with HIV risk among Latino MSM: The moderating role of outness. Manuscript in preparation.
- DiPlacido J (1998). Minority stress among lesbians, gay men, and bisexuals: A consequence of heterosexism, homophobia, and stigmatization. In Herek GM (Ed.), Psychological perspectives on lesbian and gay issues: Vol. 4. Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals (pp. 138–159). Thousand Oaks, CA: Sage. 10.4135/9781452243818.n7 [DOI] [Google Scholar]
- *Doane MJ (2017). The role of stigma visibility on stigma-related stress, coping, and health: An exploration among gay men and lesbians (Doctoral dissertation). Retrieved from University of Nevada, Reno Theses and Dissertations Database. http://hdl.handle.net/11714/2017
- Dubé EM, & Savin-Williams RC (1999). Sexual identity development among ethnic sexual-minority male youths. Developmental Psychology, 35, 1389–1398. 10.1037/0012-1649.35.6.1389 [DOI] [PubMed] [Google Scholar]
- *Dunn TL, Gonzalez CA, Costa AB, Nardi HC, & Iantaffi A (2014). Does the minority stress model generalize to a non-U.S. sample? An examination of minority stress and resilience on depressive symptomatology among sexual minority men in two urban areas of Brazil. Psychology of Sexual Orientation and Gender Diversity, 1, 117–131. 10.1037/sgd0000032 [DOI] [Google Scholar]
- Durso LE, & Meyer IH (2013). Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sexuality Research & Social Policy, 10, 35–42. 10.1007/s13178-012-0105-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56, 455–463. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- *Dyar C (2016). Examining the effects of binegativity on components of sexual identity and internalizing symptomatology among bisexual women using a longitudinal study design (Doctoral dissertation). Retrieved from Stony Brook Institutional Repository http://hdl.handle.net/11401/76792
- *Dyar C, Feinstein BA, Eaton NR, & London B (2016). Development and initial validation of the sexual minority women rejection sensitivity scale. Psychology of Women Quarterly, 40, 120–137. 10.1177/0361684315608843 [DOI] [Google Scholar]
- *Dyar C, Feinstein BA, Eaton NR, & London B (2018). The mediating roles of rejection sensitivity and proximal stress in the association between discrimination and internalizing symptoms among sexual minority women. Archives of Sexual Behavior, 47, 205–218. 10.1007/s10508-016-0869-1 [DOI] [PubMed] [Google Scholar]
- *Dyar C, Feinstein BA, & London B (2014). Dimensions of sexual identity and minority stress among bisexual women: The role of partner gender. Psychology of Sexual Orientation and Gender Diversity, 1, 441–451. 10.1037/sgd0000063 [DOI] [Google Scholar]
- Dyar C, Feinstein BA, & London B (2015). Mediators of differences between lesbians and bisexual women in sexual identity and minority stress. Psychology of Sexual Orientation and Gender Diversity, 2, 43–51. 10.1037/sgd0000090 [DOI] [Google Scholar]
- *Dyar C, Feinstein BA, Schick V, & Davila J (2017). Minority stress, sexual identity uncertainty, and partner gender decision making among nonmonosexual individuals. Psychology of Sexual Orientation and Gender Diversity, 4, 87–104. 10.1037/sgd0000213 [DOI] [Google Scholar]
- *Dyar C, & London B (2018). Bipositive events: Associations with proximal stressors, bisexual identity, and mental health among bisexual cisgender women. Psychology of Sexual Orientation and Gender Diversity, 5, 204–219. 10.1037/sgd0000281 [DOI] [Google Scholar]
- *Earle HA (1999). The relationship of internalized homophobia, level of outness, perceived social support, and self-esteem to depression in lesbians (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9934880)
- Egger M, Davey Smith G, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Elizur Y, & Ziv M (2001). Family support and acceptance, gay male identity formation, and psychological adjustment: A path model. Family Process, 40, 125–144. 10.1111/j.1545-5300.2001.4020100125.x [DOI] [PubMed] [Google Scholar]
- *Escher C, Gomez R, Paulraj S, Ma F, Spies-Upton S, Cummings C, … Goldblum P (2019). Relations of religion with depression and loneliness in older sexual and gender minority adults. Clinical Gerontologist, 42, 150–161. 10.1080/07317115.2018.1514341 [DOI] [PubMed] [Google Scholar]
- *Evans WR (2016). Military service members’ sexual identity disclosure, satisfaction, victimization, unit acceptance, and mental health (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10194804)
- *Evans WR, Bliss SJ, Rincon CM, Johnston SL, Bhakta JP, Webb-Murphy JA, … Balsam KF (2018). Military service members’ satisfaction with outness: Implications for mental health. Armed Forces and Society. Advance online publication. 10.1177/0095327X17751111 [DOI] [Google Scholar]
- *Fairlie AM, Feinstein BA, Lee CM, & Kaysen D (2018). Subgroups of young sexual minority women based on drinking locations and companions and links with alcohol consequences, drinking motives, and LGBTQ-related constructs. Journal of Studies on Alcohol and Drugs, 79, 741–750. 10.15288/jsad.2018.79.741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Feinstein BA (2019). Anxiety and depression in sexual minorities. Unpublished raw data, Institute for Sexual and Gender Minority Health and Wellbeing, Northwestern University, Chicago, IL. [Google Scholar]
- *Feinstein BA, Dyar C, Li DH, Whitton SW, Newcomb ME, & Mustanski B (2019). The longitudinal associations between outness and health outcomes among gay/lesbian versus bisexual emerging adults. Archives of Sexual Behavior, 48, 1111–1126. 10.1007/s10508-018-1221-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Feinstein BA, Dyar C, & London B (2017). Are outness and community involvement risk or protective factors for alcohol and drug abuse among sexual minority women? Archives of Sexual Behavior, 46, 1411–1423. 10.1007/s10508-016-0790-7 [DOI] [PubMed] [Google Scholar]
- Feldman MB, & Meyer IH (2007). Eating disorders in diverse lesbian, gay, and bisexual populations. International Journal of Eating Disorders, 40, 218–226. 10.1002/eat.20360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Feldman SE (2012). The impact of outness and lesbian, gay, and bisexual identity formation on mental health (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3522040)
- Ferlatte O, Hottes TS, Trussler T, & Marchand R (2017). Disclosure of sexual orientation by gay and bisexual men in government-administered probability surveys. LGBT Health, 4, 68–71. 10.1089/lgbt.2016.0037 [DOI] [PubMed] [Google Scholar]
- *Flojo JR (2005). Disclosure, identity, and discrimination: Lesbian, gay, and bisexual minority stressors in the workplace (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3190518)
- Flores AR (2019). Social acceptance of LGBT people in 174 countries: 1981–2017. Los Angeles: Williams Institute, UCLA School of Law. Retrieved from https://williamsinstitute.law.ucla.edu/publications/global-acceptance-index-lgbt/ [Google Scholar]
- Forbush KT, South SC, Krueger RF, Iacono WG, Clark LA, Keel PK, … Watson D (2010). Locating eating pathology within an empirical diagnostic taxonomy: Evidence from a community-based sample. Journal of Abnormal Psychology, 119, 282–292. 10.1037/a0019189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Foster AB, Brewster ME, Velez BL, Eklund A, & Keum BT (2017). Footprints in the sand: Personal, psychological, and relational profiles of religious, spiritual, and atheist LGB individuals. Journal of Homosexuality, 64, 466–487. 10.1080/00918369.2016.1191237 [DOI] [PubMed] [Google Scholar]
- Frable DES, Platt L, & Hoey S (1998). Concealable stigmas and positive self-perceptions: Feeling better around similar others. Journal of Personality and Social Psychology, 74, 909–922. 10.1037/0022-3514.74.4.909 [DOI] [PubMed] [Google Scholar]
- *Fredriksen-Goldsen KI, Shiu C, Bryan AEB, Goldsen J, & Kim HJ (2017). Health equity and aging of bisexual older adults: Pathways of risk and resilience. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences, 72, 468–478. 10.1093/geronb/gbw120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Friedman MR, Bukowski L, Eaton LA, Matthews DD, Dyer TV, Siconolfi D, & Stall R (2019). Psychosocial health disparities among Black bisexual men in the U. S.: Effects of sexuality nondisclosure and gay community support. Archives of Sexual Behavior, 48, 213–224. 10.1007/s10508-018-1162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Stall R, Cheong J, & Wright ER (2008). Gay-related development, early abuse and adult health outcomes among gay males. AIDS and Behavior, 12, 891–902. 10.1007/s10461-007-9319-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Frost DM, & Meyer IH (2009). Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology, 56, 97–109. 10.1037/a0012844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Giordano NG (2016). Concealing stigmatized sexual orientation, accepting versus non-accepting attitudes, and ego depletion (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10163631)
- Goffman E (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- *Goodman MB (2008). Roles of spirituality in lesbian, gay, and bisexual persons’ experiences of minority stress, psychological distress, and well-being (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3334461)
- *Griffith KH, & Hebl MR (2002). The disclosure dilemma for gay men and lesbians: “coming out” at work. Journal of Applied Psychology, 87, 1191–1199. 10.1037/0021-9010.87.6.1191 [DOI] [PubMed] [Google Scholar]
- *Guschlbauer A, Grant Smith N, DeStefano J, & Soltis DE (2019). Minority stress and emotional intimacy among individuals in lesbian and gay couples: Implications for relationship satisfaction and health. Journal of Social and Personal Relationships, 36, 855–878. 10.1177/0265407517746787 [DOI] [Google Scholar]
- *Habarth JM (2008). Thinking ‘straight’: Heteronormativity and associated outcomes across sexual orientation (Doctoral dissertation). Retrieved from University of Michigan Dissertations and Theses Database. http://hdl.handle.net/2027.42/60664
- Hammack PL, Frost DM, Meyer IH, & Pletta DR (2018). Gay men’s health and identity: Social change and the life course. Archives of Sexual Behavior, 47, 59–74. 10.1007/s10508-017-0990-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. 10.1146/annurev.clinpsy.1.102803.143938 [DOI] [PubMed] [Google Scholar]
- *Handelman MS (2016). The role of minority stress in social anxiety and depression among lesbian and gay adults (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10119484)
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135, 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2016). Structural stigma: Research evidence and implications for psychological science. American Psychologist, 71, 742–751. 10.1037/amp0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Bränström R, & Pachankis JE (2018). Societallevel explanations for reductions in sexual orientation mental health disparities: Results from a ten-year, population-based study in Sweden. Stigma and Health, 3, 16–26. 10.1037/sah0000066 [DOI] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, & Fromme K (2008). Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: Results from a prospective study. Developmental Psychology, 44, 81–90. 10.1037/0012-1649.44.1.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, & Xuan Z (2015). Social networks and sexual orientation disparities in tobacco and alcohol use. Journal of Studies on Alcohol and Drugs, 76, 117–126. 10.15288/jsad.2015.76.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Pachankis JE (2016). Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: Research evidence and clinical implications. Pediatric Clinics of North America, 63, 985–997. 10.1016/j.pcl.2016.07.003 [DOI] [PubMed] [Google Scholar]
- *Haug RM (2018). Perceived belongingness, self-esteem, and outness level of psychosocial distress among lesbian, gay, and bisexual individuals (Doctoral dissertation). Retrieved from Scholarship & Creative Works @ Digital UNC. (No. 490)
- Hedges LV, Tipton E, & Johnson MC (2010). Robust variance estimation in meta- regression with dependent effect size estimates. Research Synthesis Methods, 1, 39–65. 10.1002/jrsm.5 [DOI] [PubMed] [Google Scholar]
- Herek GM (2000). Sexual prejudice and gender: Do heterosexuals’ attitudes toward lesbians and gay men differ? Journal of Social Issues, 56, 251–266. 10.1111/0022-4537.00164 [DOI] [Google Scholar]
- Herek GM (2009). Sexual stigma and sexual prejudice in the United States: A conceptual framework. In Hope DA (Ed.), Contemporary perspectives on lesbian, gay, and bisexual identities (pp. 65–111). New York, NY: Springer. 10.1007/978-0-387-09556-1_4 [DOI] [Google Scholar]
- *Herek GM, Cogan JC, Gillis JR, & Glunt EK (1998). Correlates of internalized homophobia in a community sample of lesbians and gay men. Journal of the Gay and Lesbian Medical Association, 2, 17–25. [Google Scholar]
- *Hietpas-Wilson T (2007). Sexual minority adolescents’ sexual identity: Prevalence, disclosure, self-labeling, fluidity, and psychological well-being (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3312066)
- Hottes TS, Bogaert L, Rhodes AE, Brennan DJ, & Gesink D (2016). Lifetime prevalence of suicide attempts among sexual minority adults by study sampling strategies: A systematic review and meta-analysis. American Journal of Public Health, 106, e1–e12. 10.2105/AJPH.2016.303088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hoy-Ellis CP (2015). The mental health of lesbian, gay, bisexual, and transgender older adults: Do sexual orientation and gender identity play differential roles (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3724004)
- *Hoy-Ellis CP (2016). Concealing concealment: The mediating role of internalized heterosexism in psychological distress among lesbian, gay, and bisexual older adults. Journal of Homosexuality, 63, 487–506. 10.1080/00918369.2015.1088317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hoy-Ellis CP, & Fredriksen-Goldsen KI (2016). Lesbian, gay, & bisexual older adults: Linking internal minority stressors, chronic health conditions, and depression. Aging & Mental Health, 20, 1119–1130. 10.1080/13607863.2016.1168362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Huebner DM, & Davis MC (2005). Gay and bisexual men who disclose their sexual orientations in the workplace have higher workday levels of salivary cortisol and negative affect. Annals of Behavioral Medicine, 30, 260–267. 10.1207/s15324796abm3003_10 [DOI] [PubMed] [Google Scholar]
- Hughes TL, Wilsnack SC, & Kantor LW (2016). The influence of gender and sexual orientation on alcohol use and alcohol-related problems: Toward a global perspective. Alcohol Research: Current Reviews, 38, 121–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, & Rafferty JA (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100, 933–939. 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jackson SD, & Mohr JJ (2016). Conceptualizing the closet: Differentiating stigma concealment and nondisclosure processes. Psychology of Sexual Orientation and Gender Diversity, 3, 80–92. 10.1037/sgd0000147 [DOI] [Google Scholar]
- *Jiang Z, Wang Y, Hu X, & Wang Z (2019). Open workplace climate and LGB employees’ psychological experiences: The roles of self-concealment and self-acceptance. Journal of Employment Counseling, 56, 2–19. 10.1002/joec.12099 [DOI] [Google Scholar]
- *Jones PC (2017). Evaluating the relationship between minority stress and working memory: The influence of psychological distress and identity valence (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10279711)
- *Jordan KM (1995). Coming out and relationship quality for lesbian women (Doctoral dissertation). University of Maryland, MD. [Google Scholar]
- *Jordan KM, & Deluty RH (1998). Coming out for lesbian women: Its relation to anxiety, positive affectivity, self-esteem, and social support. Journal of Homosexuality, 35, 41–63. 10.1300/J082v35n02_03 [DOI] [PubMed] [Google Scholar]
- *Juster RP, Ouellet É, Lefebvre-Louis JP, Sindi S, Johnson PJ, Smith NG, & Lupien SJ (2016). Retrospective coping strategies during sexual identity formation and current biopsychosocial stress. Anxiety, Stress, and Coping, 29, 119–138. 10.1080/10615806.2015.1004324 [DOI] [PubMed] [Google Scholar]
- *Juster RP, Smith NG, Ouellet É, Sindi S, & Lupien SJ (2013). Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosomatic Medicine, 75, 103–116. 10.1097/PSY.0b013e3182826881 [DOI] [PubMed] [Google Scholar]
- *Kamen C, Jabson JM, Mustian KM, & Boehmer U (2017). Minority stress, psychosocial resources, and psychological distress among sexual minority breast cancer survivors. Health Psychology, 36, 529–537. 10.1037/hea0000465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kappler S (2011). Internalized homophobia, sexual identity formation, and the psychological well-being of Roman Catholic gay priests (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3503496)
- *Kaufman TML, Baams L, & Dubas JS (2017). Microaggressions and depressive symptoms in sexual minority youth: The roles of rumination and social support. Psychology of Sexual Orientation and Gender Diversity, 4, 184–192. 10.1037/sgd0000219 [DOI] [Google Scholar]
- Kauth MR, Barrera TL, & Latini DM (2019). Lesbian, gay, and transgender veterans’ experiences in the Veterans Health Administration: Positive signs and room for improvement. Psychological Services, 16, 346–351. 10.1037/ser0000232 [DOI] [PubMed] [Google Scholar]
- *Kavanaugh SA, Taylor AB, Stuhlsatz GL, Neppl TK, & Lohman BJ (2019). Family and community support among sexual minorities of color: The role of sexual minority identity prominence and outness on psychological well-being. Journal of GLBT Family Studies. Advance online publication. 10.1080/1550428X.2019.1593279 [DOI] [Google Scholar]
- *Knight AM (2006). Psychosocial variables related to subjective wellbeing in gay and bisexual men (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3229792)
- *Konik JA (2005). Harassment as a system for policing traditional gender norms in the workplace: The structure and process of sexual harassment and heterosexist harassment (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3163849)
- *Kosciw JG, Palmer NA, & Kull RM (2015). Reflecting resiliency: Openness about sexual orientation and/or gender identity and its relationship to well-being and educational outcomes for LGBT students. American Journal of Community Psychology, 55, 167–178. 10.1007/s10464-014-9642-6 [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. 10.1146/annurev.clinpsy.2.022305.095213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, & Kramer MD (2007). Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology, 116, 645–666. 10.1037/0021-843X.116.4.645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, & Iacono WG (2005). Externalizing psychopathology in adulthood: A dimensional-spectrum conceptualization and its implications for DSM–V. Journal of Abnormal Psychology, 114, 537–550. 10.1037/0021-843X.114.4.537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Watson D, & Barlow DH (2005). Introduction to the special section: Toward a dimensionally based taxonomy of psychopathology. Journal of Abnormal Psychology, 114, 491–493. 10.1037/0021-843X.114.4.491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kuyper L (2015). Differences in workplace experiences between lesbian, gay, bisexual, and heterosexual employees in a representative population study. Psychology of Sexual Orientation and Gender Diversity, 2, 1–11. 10.1037/sgd0000083 [DOI] [Google Scholar]
- *Kuyper L (n.d.). Lesbian, gay and bisexual Dutch employees. Unpublished raw data, Universiteit Utrecht, the Netherlands. [Google Scholar]
- Kuyper L, & Bos H (2016). Mostly heterosexual and lesbian/gay young adults: Differences in mental health and substance use and the role of minority stress. Journal of Sex Research, 53, 731–741. 10.1080/00224499.2015.1071310 [DOI] [PubMed] [Google Scholar]
- Kuyper L, Fernee H, & Keuzenkamp S (2016). A comparative analysis of a community and general sample of lesbian, gay, and bisexual individuals. Archives of Sexual Behavior, 45, 683–693. 10.1007/s10508-014-0457-1 [DOI] [PubMed] [Google Scholar]
- Kuyper L, & Fokkema T (2011). Minority stress and mental health among Dutch LGBs: Examination of differences between sex and sexual orientation. Journal of Counseling Psychology, 58, 222–233. 10.1037/a0022688 [DOI] [PubMed] [Google Scholar]
- *Lambe JN (2013). Well-being and relationship satisfaction among bisexual women in same-and other-gender couple relationships: The impact of minority stress (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3566602)
- Larson DG, Chastain RL, Hoyt WT, & Ayzenberg R (2015). Self-concealment: Integrative review and working model. Journal of Social and Clinical Psychology, 34, 705–774. 10.1521/jscp.2015.34.8.705 [DOI] [Google Scholar]
- Lattanner M, Bo N, Tu W, Ford J, Dodge B, Pachankis J, & Hatzenbuehler ML (2020). Stigmatizing environments increase the likelihood of identity concealment among gay men: A multi-level analysis. Unpublished manuscript, Columbia University School of Public Health. [Google Scholar]
- *Legate N (2014). Autonomy support and daily experiences with sexual identity disclosure and concealment (Doctoral dissertation). Retrieved from University of Rochester Theses and Dissertations Database. http://hdl.handle.net/1802/29204
- *Legate N, Ryan RM, & Weinstein N (2012). Is coming out always a “good thing”? Exploring the relations of autonomy support, outness, and wellness for lesbian, gay, and bisexual individuals. Social Psychological and Personality Science, 3, 145–152. 10.1177/1948550611411929 [DOI] [Google Scholar]
- *Legate N, Weinstein N, Ryan WS, DeHaan CR, & Ryan RM (2018). Parental autonomy support predicts lower internalized homophobia and better psychological health indirectly through lower shame in lesbian, gay and bisexual adults. Stigma and Health, 4, 367–376. 10.1037/sah0000150 [DOI] [Google Scholar]
- *Lehavot K (2011). Minority stress, coping, and health among sexual minority women (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3485514)
- *Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. 10.1037/a0022839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leussis MP, & Andersen SL (2008). Is adolescence a sensitive period for depression? Behavioral and neuroanatomical findings from a social stress model. Synapse, 62, 22–30. 10.1002/syn.20462 [DOI] [PubMed] [Google Scholar]
- *Lewis RJ (n.d. a). Minority stress and concealment in sexual minority females. Unpublished raw data, Department of Psychology, Old Dominion University, Norfolk, VA. [Google Scholar]
- *Lewis RJ (n.d. b). Sexual minority women health study. Unpublished raw data, Department of Psychology, Old Dominion University, Norfolk, VA. [Google Scholar]
- Lewis RJ, Derlega VJ, Brown D, Rose S, & Henson JM (2009). Sexual minority stress, depressive symptoms, and sexual orientation conflict: Focus on the experiences of bisexuals. Journal of Social and Clinical Psychology, 28, 971–992. 10.1521/jscp.2009.28.8.971 [DOI] [Google Scholar]
- *Lewis RJ, Milletich RJ, Mason TB, & Derlega VJ (2014). Pathways connecting sexual minority stressors and psychological distress among lesbian women. Journal of Gay & Lesbian Social Services, 26, 147–167. 10.1080/10538720.2014.891452 [DOI] [Google Scholar]
- *Li Y (2018). Developing, applying, and extending the theory of coming out message production (Doctoral dissertation). Retrieved from personal contact with author.
- *Li Y (2019). LGB individuals coming out to their heterosexual romantic partners: Predictors and outcomes of disclosure message features. Manuscript in preparation.
- *Li Y, & Samp JA (2019). Predictors and outcomes of initial coming out messages: Testing the theory of coming out message production. Journal of Applied Communication Research, 47, 69–89. 10.1080/00909882.2019.1566631 [DOI] [Google Scholar]
- *Liu X, Jiang D, Chen X, Tan A, Hou Y, He M, … Mao Z (2018). Mental health status and associated contributing mental health status and associated contributing. International Journal of Environmental Research and Public Health, 15, 1065. 10.3390/ijerph15061065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Liubovich I (2003). Sociocultural factors influencing vulnerability to eating disorders in lesbians and heterosexual women (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3092072)
- *Livingston NA, Christianson N, & Cochran BN (2016). Minority stress, psychological distress, and alcohol misuse among sexual minority young adults: A resiliency-based conditional process analysis. Addictive Behaviors, 63, 125–131. 10.1016/j.addbeh.2016.07.011 [DOI] [PubMed] [Google Scholar]
- *Luu TD (2011). Variables impacting depressive symptoms in lesbian, gay, bisexual, and transgender Asian and Pacific Islander Americans (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3502037)
- *Mahon C, Kiernan G, & Gallagher P (2019). Social anxiety in sexual minorities. Unpublished raw data, School of Psychology, Dublin City University, Ireland. [Google Scholar]
- Major B, & Gramzow RH (1999). Abortion as stigma: Cognitive and emotional implications of concealment. Journal of Personality and Social Psychology, 77, 735–745. 10.1037/0022-3514.77.4.735 [DOI] [PubMed] [Google Scholar]
- *Marsack J, & Stephenson R (2017). Sexuality-based stigma and depression among sexual minority individuals in rural United States. Journal of Gay & Lesbian Mental Health, 21, 51–63. 10.1080/19359705.2016.1233164 [DOI] [Google Scholar]
- *Martinez RP (2006). The moderating effects of adult attachment and self-schemas to the relation between the degree of self-disclosing sexual orientation and psychological adjustment among lesbian, gay, and bisexual adults (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3255531)
- *Mason TB (2016). Binge eating and overweight and obesity among young adult lesbians. LGBT Health, 3, 472–476. 10.1089/lgbt.2015.0119 [DOI] [PubMed] [Google Scholar]
- *Mason TB, Lewis RJ, & Heron KE (2017). Indirect pathways connecting sexual orientation and weight discrimination to disordered eating among young adult lesbians. Psychology of Sexual Orientation and Gender Diversity, 4, 193–204. 10.1037/sgd0000220 [DOI] [Google Scholar]
- *McConnell EA, Clifford A, Korpak AK, Phillips G II., & Birkett M (2017). Identity, victimization, and support: Facebook experiences and mental health among LGBTQ youth. Computers in Human Behavior, 76, 237–244. 10.1016/j.chb.2017.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrity LA, & Huebner DM (2014). Is being out about sexual orientation uniformly healthy? The moderating role of socioeconomic status in a prospective study of gay and bisexual men. Annals of Behavioral Medicine, 47, 28–38. 10.1007/s12160-013-9575-6 [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22, 276–282. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Meidlinger PC, & Hope DA (2014). Differentiating disclosure and concealment in measurement of outness for sexual minorities: The Nebraska outness scale. Psychology of Sexual Orientation and Gender Diversity, 1, 489–497. 10.1037/sgd0000080 [DOI] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, & Wilson PA (2009). Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology, 56, 23–31. 10.1037/a0014587 [DOI] [Google Scholar]
- *Michaels MS, Parent MC, & Torrey CL (2016). A minority stress model for suicidal ideation in gay men. Suicide & Life-Threatening Behavior, 46, 23–34. 10.1111/sltb.12169 [DOI] [PubMed] [Google Scholar]
- Mineka S, & Zinbarg R (2006). A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. American Psychologist, 61, 10–26. 10.1037/0003-066X.61.1.10 [DOI] [PubMed] [Google Scholar]
- Mitchell KS, Wolf EJ, Reardon AF, & Miller MW (2014). Association of eating disorder symptoms with internalizing and externalizing dimensions of psychopathology among men and women. International Journal of Eating Disorders, 47, 860–869. 10.1002/eat.22300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, & Fassinger RE (2000). Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development, 33, 66–90. 10.1080/07481756.2000.12068999 [DOI] [Google Scholar]
- Mohr JJ, & Fassinger RE (2003). Self-acceptance and self-disclosure of sexual orientation in lesbian, gay, and bisexual adults: An attachment perspective. Journal of Counseling Psychology, 50, 482–495. 10.1037/0022-0167.50.4.482 [DOI] [Google Scholar]
- *Mohr JJ, Jackson SD, & Sheets RL (2017). Sexual orientation self-presentation among bisexual-identified women and men: Patterns and predictors. Archives of Sexual Behavior, 46, 1465–1479. 10.1007/s10508-016-0808-1 [DOI] [PubMed] [Google Scholar]
- *Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58, 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- *Morandini JS, Pinkus RT, & Dar-Nimrod I (2018). Does partner gender influence relationship quality among non-monosexual women? Sexual and Relationship Therapy, 33(1–2), 146–165. 10.1080/14681994.2017.1419568 [DOI] [Google Scholar]
- Murphy MLM, Slavich GM, Rohleder N, & Miller GE (2013). Targeted rejection triggers differential pro- and anti-inflammatory gene expression in adolescents as a function of social status. Clinical Psychological Science, 1, 30–40. 10.1177/2167702612455743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mustanski B, Newcomb M, & Garofalo R (2011). Mental health of lesbian, gay, and bisexual youth: A developmental resiliency perspective. Journal of Gay & Lesbian Social Services, 23, 204–225. 10.1080/10538720.2011.561474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Nance JC (2008). Measuring levels of stress, anxiety, and depression from sexual orientation identity, internalized homophobia, level of outness, and marital satisfaction within the population of men in heterosexual marriages who choose to engage in sexual activities with other men (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3305960)
- *Nash JP (1990). Stress, ego identity, and the disclosure of a homosexual orientation among midlife transition male religious professionals in the Roman Catholic Church (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9113976)
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30, 1019–1029. 10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- *Nickels SJ (2013). The role of the social environment in non-suicidal self-injury among LGBTQ youth: A mixed methods study (Doctoral dissertation). Retrieved from University of Denver Electronic Theses and Dissertations Database. (No. 992)
- *Norcini Pala A (2010). Negative affect and depression in sexual minority men. Unpublished raw data, School of Social Work, Columbia University, New York, NY. [Google Scholar]
- *Norcini Pala A (2012a). Depression in sexual minority men. Unpublished raw data, School of Social Work, Columbia University, New York, NY. [Google Scholar]
- *Norcini Pala A (2012b). Depression in sexual minorities. Unpublished raw data, School of Social Work, Columbia University, New York, NY. [Google Scholar]
- *Oetjen H, & Rothblum ED (2000). When lesbians aren’t gay: Factors affecting depression among lesbians. Journal of Homosexuality, 39, 49–73. 10.1300/J082v39n01_04 [DOI] [PubMed] [Google Scholar]
- *Oldenburg CE, Biello KB, Colby D, Closson EF, Mai T, Nguyen T, … Mimiaga MJ (2014). Stigma related to sex work among men who engage in transactional sex with men in Ho Chi Minh City, Vietnam. International Journal of Public Health, 59, 833–840. 10.1007/s00038-014-0562-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Orban LA (2003). Protective factors and psychological well-being in lesbian, gay and bisexual youth: An ecological framework (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3098120)
- *Owens GP, Riggle ED, & Rostosky SS (2007). Mental health services access for sexual minority individuals. Sexuality Research & Social Policy, 4, 92–99. 10.1525/srsp.2007.4.3.92 [DOI] [Google Scholar]
- Pachankis JE (2007). The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychological Bulletin, 133, 328–345. 10.1037/0033-2909.133.2.328 [DOI] [PubMed] [Google Scholar]
- *Pachankis JE (n.d.). A unified intervention for young gay and bisexual men’s minority stress, mental health, and HIV risk. Unpublished raw data, Yale School of Public Health, New Haven, CT. [Google Scholar]
- *Pachankis JE, & Bernstein LB (2012). An etiological model of anxiety in young gay men: From early stress to public self-consciousness. Psychology of Men & Masculinity, 13, 107–122. 10.1037/a0024594 [DOI] [Google Scholar]
- Pachankis JE, & Bränström R (2018). Hidden from happiness: Structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. Journal of Consulting and Clinical Psychology, 86, 403–415. 10.1037/ccp0000299 [DOI] [PubMed] [Google Scholar]
- *Pachankis JE, Clark K, Burton C, White Hughto JM, Bränström R, & Keene DE (2020). Sex, status, competition, and exclusion: Intra-minority stress from within the gay community and sexual minority men’s mental health. Journal of Personality and Social Psychology. Advance online publication. 10.1037/pspp0000282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Cochran SD, & Mays VM (2015). The mental health of sexual minority adults in and out of the closet: A population-based study. Journal of Consulting and Clinical Psychology, 83, 890–901. 10.1037/ccp0000047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pachankis JE, & Goldfried MR (2006). Social anxiety in young gay men. Journal of Anxiety Disorders, 20, 996–1015. 10.1016/j.janxdis.2006.01.001 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, & Goldfried MR (2010). Expressive writing for gay-related stress: Psychosocial benefits and mechanisms underlying improvement. Journal of Consulting and Clinical Psychology, 78, 98–110. 10.1037/a0017580 [DOI] [PubMed] [Google Scholar]
- *Pachankis JE, McConocha EM, Clark KA, Wang K, Behari K, Fetzner BK, … Lehavot K (2019). A transdiagnostic minority stress intervention for sexual minority women’s depression, anxiety, and unhealthy alcohol use: A randomized controlled trial. Unpublished manuscript, Yale University, New Haven, CT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pachankis JE, Sullivan TJ, Feinstein BA, & Newcomb ME (2018). Young adult gay and bisexual men’s stigma experiences and mental health: An 8-year longitudinal study. Developmental Psychology, 54, 1381–1393. 10.1037/dev0000518 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Westmaas JL, & Dougherty LR (2011). The influence of sexual orientation and masculinity on young men’s tobacco smoking. Journal of Consulting and Clinical Psychology, 79, 142–152. 10.1037/a0022917 [DOI] [PubMed] [Google Scholar]
- *Pachankis JE, Williams SL, Behari K, Job S, McConocha EM, & Chaudoir SR (2019). Brief online interventions for LGBTQ young adult mental and behavioral health: A randomized controlled trial in a high-stigma, low-resource context. Unpublished manuscript, Yale University, New Haven, CT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Parker RD, Lõhmus L, Mangine C, & Rüütel K (2016). Homonegativity and associated factors among men who have sex with men in Estonia. Journal of Community Health, 41, 717–723. 10.1007/s10900-015-0145-7 [DOI] [PubMed] [Google Scholar]
- *Paul R, Smith NG, Mohr JJ, & Ross LE (2014). Measuring dimensions of bisexual identity: Initial development of the bisexual identity inventory. Psychology of Sexual Orientation and Gender Diversity, 1, 452–460. 10.1037/sgd0000069 [DOI] [Google Scholar]
- *Persson TJ, Pfaus JG, & Ryder AG (2015). Explaining mental health disparities for non-monosexual women: Abuse history and risky sex, or the burdens of non-disclosure? Social Science & Medicine, 128, 366–373. 10.1016/j.socscimed.2014.08.038 [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51, S28–S40. [DOI] [PubMed] [Google Scholar]
- Pilkington NW, & D’Augelli AR (1995). Victimization of lesbian, gay, and bisexual youth in community settings. Journal of Community Psychology, 23, 34–56. [DOI] [Google Scholar]
- *Pimentel ML (2015). Male same-sex intimate partner violence: Syndemic theory minority stress theory & the community of protective measures (Doctoral dissertation). Retrieved from Nursing Electronic Theses and Dissertations (UMKC).
- *Prell E, & Traeen B (2018). Minority stress and mental health among bisexual and lesbian women in Norway. Journal of Bisexuality, 18, 278–298. 10.1080/15299716.2018.1518180 [DOI] [Google Scholar]
- *Puckett JA, Maroney MR, Levitt HM, & Horne SG (2016). Relations between gender expression, minority stress, and mental health in cisgender sexual minority women and men. Psychology of Sexual Orientation and Gender Diversity, 3, 489–498. 10.1037/sgd0000201 [DOI] [Google Scholar]
- *Puckett JA, Surace FI, Levitt HM, & Horne SG (2016). Sexual orientation identity in relation to minority stress and mental health in sexual minority women. LGBT Health, 3, 350–356. 10.1089/lgbt.2015.0088 [DOI] [PubMed] [Google Scholar]
- *Puckett JA, Wolff JR, Gunn HA, Woodward EN, & Pantalone DW (2018). An investigation of religion and spirituality of sexual minorities in the United States: Exploring perceptions, intrinsic religiosity, and outness to religious communities. International Journal for the Psychology of Religion, 28, 145–161. 10.1080/10508619.2018.1464858 [DOI] [Google Scholar]
- *Ragins BR, Singh R, & Cornwell JM (2007). Making the invisible visible: Fear and disclosure of sexual orientation at work. Journal of Applied Psychology, 92, 1103–1118. 10.1037/0021-9010.92.4.1103 [DOI] [PubMed] [Google Scholar]
- *Ray JM (2016). Minority stress and substance use in lesbian, gay, bisexual, queer, and questioning adults: An exploration of outness and family attachment (Doctoral dissertation). Retrieved from Bowling Green State University Electronic Theses and Dissertations Center. Retrieved from http://rave.ohiolink.edu/etdc/view?acc_num=bgsu1477949207825152
- *Rhoades H, Rusow JA, Bond D, Lanteigne A, Fulginiti A, & Goldbach JT (2018). Homelessness, mental health and suicidality among LGBTQ youth accessing crisis services. Child Psychiatry and Human Development, 49, 643–651. 10.1007/s10578-018-0780-1 [DOI] [PubMed] [Google Scholar]
- *Ribeiro Gonçalves JA (2019). Psychological distress in sexual minorities. Unpublished raw data, Instituto Universitário, Lisbon, Portugal. [Google Scholar]
- Rieger G, Linsenmeier JA, Gygax L, Garcia S, & Bailey JM (2010). Dissecting “gaydar”: Accuracy and the role of masculinity-femininity. Archives of Sexual Behavior, 39, 124–140. 10.1007/s10508-008-9405-2 [DOI] [PubMed] [Google Scholar]
- *Riggle EDB, Rostosky SS, Black WW, & Rosenkrantz DE (2017). Outness, concealment, and authenticity: Associations with LGB individuals’ psychological distress and well-being. Psychology of Sexual Orientation and Gender Diversity, 4, 54–62. 10.1037/sgd0000202 [DOI] [Google Scholar]
- *Robinson M, Sanches M, & MacLeod MA (2016). Prevalence and mental health correlates of illegal cannabis use among bisexual women. Journal of Bisexuality, 16, 181–202. 10.1080/15299716.2016.1147402 [DOI] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, & Pachankis JE (2019). Prevalence of psychiatric disorders at the intersection of race and sexual orientation: Results from the National Epidemiologic Survey of Alcohol and Related Conditions-III. Journal of Consulting and Clinical Psychology, 87, 321–331. 10.1037/ccp0000377 [DOI] [PubMed] [Google Scholar]
- Romeo RD, Bellani R, Karatsoreos IN, Chhua N, Vernov M, Conrad CD, & McEwen BS (2006). Stress history and pubertal development interact to shape hypothalamic-pituitary-adrenal axis plasticity. Endocrinology, 147, 1664–1674. 10.1210/en.2005-1432 [DOI] [PubMed] [Google Scholar]
- *Roper K (1997). Lesbian couple dynamics and individual’s psychological adjustment (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9734318)
- *Rosario M, Hunter J, Maguen S, Gwadz M, & Smith R (2001). The coming-out process and its adaptational and health-related associations among gay, lesbian, and bisexual youths: Stipulation and exploration of a model. American Journal of Community Psychology, 29, 133–160. 10.1023/A:1005205630978 [DOI] [PubMed] [Google Scholar]
- *Rosario M, Schrimshaw EW, & Hunter J (2006). A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education and Prevention, 18, 444–460. 10.1521/aeap.2006.18.5.444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, & Hunter J (2008). Predicting different patterns of sexual identity development over time among lesbian, gay, and bisexual youths: A cluster analytic approach. American Journal of Community Psychology, 42, 266–282. 10.1007/s10464008-9207-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rosario M, Schrimshaw EW, & Hunter J (2009). Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: Critical role of disclosure reactions. Psychology of Addictive Behaviors, 23, 175–184. 10.1037/a0014284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rosario-Hernández E, Millán LVR, Cruz CFL, Neris M, & Acevedo G (2009). Saliendo del closet en el trabajo: La relación entre el manejo de la identidad sexual, heterosexismo organizacional percibido, actitudes de trabajo y bienestar psicológico [Coming out of the closet at work: The relationship between the management of sexual identity, perceived organizational heterosexism, work attitudes, and psychological well-being]. Revista Puertorriqueña de Psicología, 20, 103–143. [Google Scholar]
- Rosenquist JN, Murabito J, Fowler JH, & Christakis NA (2010). The spread of alcohol consumption behavior in a large social network. Annals of Internal Medicine, 152, 426–433. 10.7326/0003-4819-152-7-201004060-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ross LE, Bauer GR, MacLeod MA, Robinson M, MacKay J, & Dobinson C (2014). Mental health and substance use among bisexual youth and non-youth in Ontario, Canada. PLoS ONE, 9, e101604. 10.1371/journal.pone.0101604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross MB (2005). Beyond the closet as raceless paradigm. In Johnson EP & Henderson MG (Eds.), Black queer studies: A critical anthology (pp. 161–189). Durham, NC: Duke University Press. [Google Scholar]
- *Rosser BRS, Kohli N, Polter EJ, Lesher L, Capistrant BD, Konety BR, … Kilian G (2019). The sexual functioning of gay and bisexual men following prostate cancer treatment: Results from the Restore Study. Archives of Sexual Behavior. Advance online publication. 10.1007/s10508-018-1360-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rosser BRS, Oakes M, Jones-Webb R, Brady SS, Carpenter D, Horvath K, … Nygaard K (2008). Alcohol use and depression in sexual minority men. Unpublished raw data, School of Public Health, University of Minnesota, Minneapolis, MN. [Google Scholar]
- *Rosser BR, Smolenski DJ, Erickson D, Iantaffi A, Brady SS, Grey JA, … Wilkerson JM (2013). The effects of gay sexually explicit media on the HIV risk behavior of men who have sex with men. AIDS and Behavior, 17, 1488–1498. 10.1007/s10461-013-0454-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rostosky SS, Riggle EDB, Horne SG, & Miller AD (2009). Marriage amendments and psychological distress in lesbian, gay, and bisexual (LGB) adults. Journal of Counseling Psychology, 56, 56–66. 10.1037/a0013609 [DOI] [Google Scholar]
- *Rubino C, Case R, & Anderson A (2018). Internalized homophobia and depression in lesbian women: The protective role of pride. Journal of Gay & Lesbian Social Services, 30, 244–260. 10.1080/10538720.2018.1470419 [DOI] [Google Scholar]
- Russell ST, & Fish JN (2019). Sexual minority youth, social change, and health: A developmental collision. Research in Human Development, 16, 5–20. 10.1080/15427609.2018.1537772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rüütel K, Valk A, & Lõhmus L (2017). Suicidality and associated factors among men who have sex with men in Estonia. Journal of Homosexuality, 64, 770–785. 10.1080/00918369.2016.1236578 [DOI] [PubMed] [Google Scholar]
- *Ryan WS (2017). The impact of autonomy support on identity disclosure and well-being among sexual minority individuals
- *Ryan WS, Legate N, Weinstein N, & Rahman Q (2017). Autonomy support fosters lesbian, gay, and bisexual identity disclosure and wellness, especially for those with internalized homophobia. Journal of Social Issues, 73, 289–306. 10.1111/josi.12217 [DOI] [Google Scholar]
- *Salway T, Gesink D, Ibrahim S, Ferlatte O, Rhodes AE, Brennan DJ, … Trussler T (2018). Evidence of multiple mediating pathways in associations between constructs of stigma and self-reported suicide attempts in a cross-sectional study of gay and bisexual men. Archives of Sexual Behavior, 47, 1145–1161. 10.1007/s10508-017-1019-0 [DOI] [PubMed] [Google Scholar]
- *Sandfort T, Bos H, Knox J, & Reddy V (2016). Gender nonconformity, discrimination, and mental health among Black South African men who have sex with men: A further exploration of unexpected findings. Archives of Sexual Behavior, 45, 661–670. 10.1007/s10508-015-0565-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandfort TGM, Bos H, & Reddy V (2018). Gender expression and mental health in Black South African men who have sex with men: Further explorations of unexpected findings. Archives of Sexual Behavior, 47, 2481–2490. 10.1007/s10508-018-1168-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sandil R, Robinson M, Brewster ME, Wong S, & Geiger E (2015). Negotiating multiple marginalizations: Experiences of South Asian LGBQ individuals. Cultural Diversity and Ethnic Minority Psychology, 21, 76–88. 10.1037/a0037070 [DOI] [PubMed] [Google Scholar]
- *Sattler FA, Wagner U, & Christiansen H (2016). Effects of minority stress, group-level coping, and social support on mental health of German gay men. PLoS ONE, 11, e0150562. 10.1371/journal.pone.0150562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sattler FA, Zeyen J, & Christiansen H (2017). Does sexual identity stress mediate the association between sexual identity and mental health? Psychology of Sexual Orientation and Gender Diversity, 4, 296–303. 10.1037/sgd0000232 [DOI] [Google Scholar]
- *Schope RD (2004). Practitioners need to ask: Culturally competent practice requires knowing where the gay male client is in the coming out process. Smith College Studies in Social Work, 74, 257–270. 10.1080/00377310409517715 [DOI] [Google Scholar]
- *Schrimshaw EW, Siegel K, Downing MJ Jr., & Parsons JT (2013). Disclosure and concealment of sexual orientation and the mental health of non-gay-identified, behaviorally bisexual men. Journal of Consulting and Clinical Psychology, 81, 141–153. 10.1037/a0031272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Scott SB (2016). Lesbian couple dynamics and heterosexist stressors: Building a foundation for culturally competent relationship interventions (Doctoral dissertation). University of Denver, Denver, CO. https://digitalcommons.du.edu/etd/1183 [Google Scholar]
- Seager I (2016). Regulating discrimination: The effects of emotion regulation on experiences of pride and shame, and subsequent self-disclosure among lesbian, gay, and bisexual adults (Unpublished master’s thesis). The Ohio State University, Columbus, OH. Retrieved from http://rave.ohiolink.edu/etdc/view?acc_numosu1462805898 [Google Scholar]
- *Sedlovskaya A (2011). Concealable stigma and the distinction between public and private selves: Implications for psychological well-being (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3467837)
- *Sedlovskaya A, Purdie-Vaughns V,Eibach RP, LaFrance M, Romero-Canyas R, & Camp NP (2013). Internalizing the closet: Concealment heightens the cognitive distinction between public and private selves. Journal of Personality and Social Psychology, 104, 695–715. 10.1037/a0031179 [DOI] [PubMed] [Google Scholar]
- *Shilo G, Antebi N, & Mor Z (2015). Individual and community resilience factors among lesbian, gay, bisexual, queer and questioning youth and adults in Israel. American Journal of Community Psychology, 55, 215–227. 10.1007/s10464-014-9693-8 [DOI] [PubMed] [Google Scholar]
- *Shilo G, & Mor Z (2015). Seeking sex online: Social and sexual risk factors among adolescent and young gay and bisexual men. Sexual Health, 12, 217–223. 10.1071/SH14229 [DOI] [PubMed] [Google Scholar]
- *Shilo G, & Savaya R (2011). Effects of family and friend support on LGB youths’ mental health and sexual orientation milestones. Family Relations, 60, 318–330. 10.1111/j.1741-3729.2011.00648.x [DOI] [Google Scholar]
- *Shilo G, & Savaya R (2012). Mental health of lesbian, gay, and bisexual youth and young adults: Differential effects of age, gender, religiosity, and sexual orientation. Journal of Research on Adolescence, 22, 310–325. 10.1111/j.1532-7795.2011.00772.x [DOI] [Google Scholar]
- *Shilo G, Yossef I, & Savaya R (2016). Religious coping strategies and mental health among religious Jewish gay and bisexual men. Archives of Sexual Behavior, 45, 1551–1561. 10.1007/s10508-0150567-4 [DOI] [PubMed] [Google Scholar]
- Shin LM, & Liberzon I (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35, 169–191. 10.1038/npp.2009.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart L, & Wegner DM (1999). Covering up what can’t be seen: Concealable stigma and mental control. Journal of Personality and Social Psychology, 77, 474–486. 10.1037/0022-3514.77.3.474 [DOI] [PubMed] [Google Scholar]
- *Smith NG, Hart TA, Kidwai A, Vernon JRG, Blais M, & Adam B (2017). Results of a pilot study to ameliorate psychological and behavioral outcomes of minority stress among young gay and bisexual men. Behavior Therapy, 48, 664–677. 10.1016/j.beth.2017.03.005 [DOI] [PubMed] [Google Scholar]
- *Smith NG, & Ingram KM (2004). Workplace heterosexism and adjustment among lesbian, gay, and bisexual individuals: The role of unsupportive social interactions. Journal of Counseling Psychology, 51, 57–67. 10.1037/0022-0167.51.1.57 [DOI] [Google Scholar]
- *Smith RB (1996). The impact of gay identity development on AIDS-risk behavior among younger gay men (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9719829)
- Stanley TD, Doucouliagos H, & Ioannidis JPA (2017). Finding the power to reduce publication bias. Statistics in Medicine, 36, 1580–1598. 10.1002/sim.7228 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata statistical software: Release 15. College Station, TX: Author. [Google Scholar]
- Stein E (1999). The mismeasure of desire: The science, theory, and ethics of sexual orientation. New York, NY: Oxford University Press. [Google Scholar]
- Steinman E (2000). Interpreting the invisibility of male bisexuality. Journal of Bisexuality, 1(2–3), 15–45. 10.1300/J159v01n02_02 [DOI] [Google Scholar]
- Stokes JP, Vanable P, & McKirnan DJ (1997). Comparing gay and bisexual men on sexual behavior, condom use, and psychosocial variables related to HIV/AIDS. Archives of Sexual Behavior, 26, 383–397. 10.1023/A:1024539301997 [DOI] [PubMed] [Google Scholar]
- *Sun CJ, Tobin K, Spikes P, & Latkin C (2019). Correlates of same-sex behavior disclosure to health care providers among Black MSM in the United States: Implications for HIV prevention. AIDS Care, 31, 1011–1018. 10.1080/09540121.2018.1548753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Swearingen CE (2006). The role of internalized homophobia, sexual orientation concealment and social support in eating disorders and body image disturbances among lesbian, gay and bisexual individuals (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3238472)
- *Szymanski DM, & Sung MR (2010). Minority stress and psychological distress among Asian American sexual minority persons. The Counseling Psychologist, 38, 848–872. 10.1177/0011000010366167 [DOI] [Google Scholar]
- *Tabaac AR, Perrin PB, & Trujillo MA (2015). Multiple mediational model of outness, social support, mental health, and wellness behavior in ethnically diverse lesbian, bisexual, and queer women. LGBT Health, 2, 243–249. 10.1089/lgbt.2014.0110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tabb K (2016). Black sexual minorities coping with multiple minority stress (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (ProQuest No. 10189996)
- *Talley AE, & Bettencourt BA (2011). The moderator roles of coping style and identity disclosure in the relationship between perceived sexual stigma and psychological distress. Journal of Applied Social Psychology, 41, 2883–2903. 10.1111/j.1559-1816.2011.00863.x [DOI] [Google Scholar]
- Tanner-Smith EE, & Tipton E (2014). Robust variance estimation with dependent effect sizes: Practical considerations including a software tutorial in Stata and SPSS. Research Synthesis Methods, 5, 13–30. 10.1002/jrsm.1091 [DOI] [PubMed] [Google Scholar]
- *Thies KE (2015). Internalized homonegativity and relationship quality in same-sex romantic couples: A test of mental health mechanisms and gender as a moderator (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3663337)
- *Timmins L, Rimes KA, & Rahman Q (2018). Minority stressors, rumination, and psychological distress in monozygotic twins discordant for sexual minority status. Psychological Medicine, 48, 1705–1712. 10.1017/S003329171700321X [DOI] [PubMed] [Google Scholar]
- *Timmins L, Rimes KA, & Rahman Q (2020). Minority stressors, rumination, and psychological distress in lesbian, gay, and bisexual individuals. Archives of Sexual Behavior, 49, 661–680. 10.1007/s10508-019-01502-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tomori C, McFall AM, Srikrishnan AK, Mehta SH, Solomon SS, Anand S, … Celentano DD (2016). Diverse rates of depression among men who have sex with men (MSM) across India: Insights from a multi-site mixed method study. AIDS and Behavior, 20, 304–316. 10.1007/s10461-015-1201-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tornello SL, & Patterson CJ (2018). Adult children of gay fathers: Parent–child relationship quality and mental health. Journal of Homosexuality, 65, 1152–1166. 10.1080/00918369.2017.1406218 [DOI] [PubMed] [Google Scholar]
- Trocki KF, Drabble L, & Midanik L (2005). Use of heavier drinking contexts among heterosexuals, homosexuals and bisexuals: Results from a National Household Probability Survey. Journal of Studies on Alcohol, 66, 105–110. 10.15288/jsa.2005.66.105 [DOI] [PubMed] [Google Scholar]
- *Ullrich PM, Lutgendorf SK, & Stapleton JT (2003). Concealment of homosexual identity, social support and CD4 cell count among HIV-seropositive gay men. Journal of Psychosomatic Research, 54, 205–212. 10.1016/S0022-3999(02)00481-6 [DOI] [PubMed] [Google Scholar]
- *Ullrich PM, Lutgendorf SK, Stapleton JT, & Horowitz M (2004). Self regard and concealment of homosexuality as predictors of CD4+ cell count over time among HIV seropositive gay men. Psychology & Health, 19, 183–196. 10.1080/08870440310001652704 [DOI] [Google Scholar]
- Valentine JC, Pigott TD, & Rothstein HR (2010). How many studies do you need? A primer on statistical power for meta-analysis. Journal of Educational and Behavioral Statistics, 35, 215–247. 10.3102/1076998609346961 [DOI] [Google Scholar]
- *van der Star A, Pachankis J, & Bränström R (2019). Sexual orientation openness and depression symptoms: A population-based study. Psychology of Sexual Orientation and Gender Diversity, 6, 369–381. 10.1037/sgd0000335 [DOI] [Google Scholar]
- *Velez BL, & Moradi B (2016). A moderated mediation test of minority stress: The role of collective action. The Counseling Psychologist, 44, 1132–1157. 10.1177/0011000016665467 [DOI] [Google Scholar]
- *Velez BL, Moradi B, & Brewster ME (2013). Testing the tenets of minority stress theory in workplace contexts. Journal of Counseling Psychology, 60, 532–542. 10.1037/a0033346 [DOI] [PubMed] [Google Scholar]
- *Velez BL, Watson LB, Cox R Jr., & Flores MJ (2017). Minority stress and racial or ethnic minority status: A test of the greater risk perspective. Psychology of Sexual Orientation and Gender Diversity, 4, 257–271. 10.1037/sgd0000226 [DOI] [Google Scholar]
- Viera AJ, & Garrett JM (2005). Understanding interobserver agreement: The kappa statistic. Family Medicine, 37, 360–363. [PubMed] [Google Scholar]
- Villicana AJ, Delucio K, & Biernat M (2016). “Coming out” among gay Latino and gay White men: Implications of verbal disclosure for well-being. Self and Identity, 15, 468–487. 10.1080/15298868.2016.1156568 [DOI] [Google Scholar]
- *Vincke J, & van Heeringen K (2002). Confidant support and the mental wellbeing of lesbian and gay young adults: A longitudinal analysis. Journal of Community & Applied Social Psychology, 12, 181–193. 10.1002/casp.671 [DOI] [Google Scholar]
- *Walch SE, Ngamake ST, Bovornusvakool W, & Walker SV (2016). Discrimination, internalized homophobia, and concealment in sexual minority physical and mental health. Psychology of Sexual Orientation and Gender Diversity, 3, 37–48. 10.1037/sgd0000146 [DOI] [Google Scholar]
- *Waldo CR (1997). Working in a majority context: A structural model of the antecedents and outcomes of heterosexism in the workplace (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 10119484)
- *Waldo CR (1999). Working in a majority context: A structural model of heterosexism as minority stress in the workplace. Journal of Counseling Psychology, 46, 218–232. 10.1037/0022-0167.46.2.218 [DOI] [Google Scholar]
- Watson D, & Pennebaker JW (1989). Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychological Review, 96, 234–254. 10.1037/0033-295X.96.2.234 [DOI] [PubMed] [Google Scholar]
- *Watson LB, Velez BL, Brownfield J, & Flores MJ (2016). Minority stress and bisexual women’s disordered eating: The role of maladaptive coping. The Counseling Psychologist, 44, 1158–1186. 10.1177/0011000016669233 [DOI] [Google Scholar]
- *White Y, Sandfort T, Morgan K, Carpenter K, & Pierre R (2016). Family relationships and sexual orientation disclosure to family by gay and bisexual men in Jamaica. International Journal of Sexual Health, 28, 306–317. 10.1080/19317611.2016.1227015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wilkerson JM, Noor SW, Galos DL, & Rosser BRS (2016). Correlates of a single-item indicator versus a multi-item scale of outness about same-sex attraction. Archives of Sexual Behavior, 45, 1269–1277. 10.1007/s10508-015-0605-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Williams SL, Mann AK, & Fredrick EG (2017). Proximal minority stress, psychosocial resources, and health in sexual minorities. Journal of Social Issues, 73, 529–544. 10.1111/josi.12230 [DOI] [Google Scholar]
- *Willoughby BLB (2008). Victimization, family rejection, and outcomes of lesbian, gay, and bisexual young people: The role of negative LGB Identity (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3322797)
- *Wolff JR, Himes HL, Soares SD, & Kwon EM (2016). Sexual minority students in non-affirming religious higher education: Mental health, outness, and identity. Psychology of Sexual Orientation and Gender Diversity, 3, 201–212. 10.1037/sgd0000162 [DOI] [Google Scholar]
- *Woodford MR, Weber G, Nicolazzo Z, Hunt R, Kulick A, Coleman T, … Renn KA (2018). Depression and attempted suicide among LGBTQ college students: Fostering resilience to the effects of heterosexism and cisgenderism on campus. Journal of College Student Development, 59, 421–438. 10.1353/csd.2018.0040 [DOI] [Google Scholar]
- *Xu W, Zheng L, Xu Y, & Zheng Y (2017). Internalized homophobia, mental health, sexual behaviors, and outness of gay/bisexual men from Southwest China. International Journal for Equity in Health, 16, 36. 10.1186/s12939-017-0530-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Zuckerman MJ (1998). Sexual orientation disclosure and its relationship to psychological distress, immune, and physical health status variables in HIV-infection men (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 9915370)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


