PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/odi.13805.
Dear Editor,
In September 2020, a 78‐year‐old patient was referred to the Oral Medicine Unit of the University of Bologna, because of longstanding, painful, and widespread oral ulcerative lesions and erosive plaques (Figure 1a).
FIGURE 1.
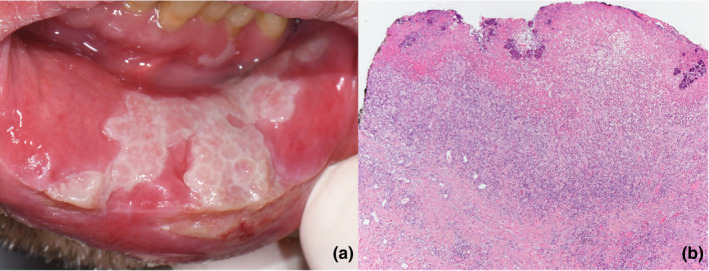
(a) Painful ulcerated plaque of the mucosal side of the inferior lip. Similar lesions affected both margins of the tongue, both lips, and soft palate. (b) At low power, the oral mucosa was ulcerated with granulation tissue and fibrino‐leukocytic material including bacterial colonies. Dense inflammatory infiltrate was present in the submucosa
In March 2020, the patient had been hospitalized because of SARS‐COV‐2‐related severe pneumonia and acute respiratory distress. Diagnosis of SARS‐COV‐2 infection was confirmed by positive RT‐PCR on nasopharyngeal swab. Patient's medical history also included a previous diagnosis of follicular Lymphoma, in remission.
Oral lesions appeared few days after the onset of respiratory symptoms and worsened during hospitalization. However, since priority was given to therapy for SARS‐COV‐2‐related pneumonia, oral care was delayed.
Pneumonia was treated with hydroxychloroquine, steroids, ciprofloxacin, and tocilizumab.
In April 2020, the patient was discharged from hospital but, despite apparent COVID‐19 remission, he still required home oxygen therapy and no improvements of oral ulcers were experienced.
In September, a biopsy for histopathological examination was performed. Oral mucosa was ulcerated, with granulation tissue and fibrino‐leukocytic material including bacterial colonies. Neither dysplasia nor fungal invasion was observed (Figure 1b). Direct Immunofluorescence showed a non‐specific deposit of fibrinogen. Immunohistochemical search for HSV 1, HSV 2, and CMV‐related proteins was negative. Sub‐mucosal vessels were normal without features of vasculitis or thrombosis.
Laboratory screening tests for systemic HSV, CMV, EBV viral infections or for oral manifestations of gastrointestinal disorders were inconclusive. A marked lymphopenia (5%, 0.77 109/L), excessive neutrophil count (88%, 11.3 109/L), and high ferritin values (1,485 ng/ml) were recorded.
Therapeutic attempts to relief patient's painful condition with topical betamethasone, Chlorhexidine gel, and topical lidocaine were unable to achieve improvements in pain reduction.
Finally, in October acute respiratory conditions worsened, patient refused a new hospitalization and in November 2020 died of respiratory failure.
The suspicion that oral lesions could be related to SARS‐COV‐2 infection was raised.
SARS‐COV‐2 virus invades human cells via the ACE2 receptor which is abundant in mucosa cells of the oral cavity (Xu et al., 2020). It has been speculated that oral tissues might thus provide not only a possible route of entry for the SARS‐COV‐2 but also an extrapulmonary target.
It is still unclear whether oral lesions in COVID‐19 patients reflect a direct viral cytopathic damage or represent a consequence of systemic deterioration (Amorim Dos Santos et al., 2020; Mo et al., 2020; Ye et al., 2020).
Unlike previous cases, in our patient, ulcerative lesions were associated with persistent immunological impairment and did not heal after SARS‐COV‐2 eradication. Noteworthy, lymphopenia and neutrophilia have been described by many authors as a predictor of severity and poor prognosis in COVID‐19 older patients (Mo et al., 2020; Wang et al., 2020; Ye et al., 2020).
It may be speculated that non‐healing oral ulcerations may represent a sign of a persisting immunological storm‐related damage after SARS‐COV‐2 eradication.
The present case, in agreement with emerging research, highlights the relevance of oral examination in proved or suspected COVID‐19 patients in order to relate oral health conditions with general prognosis.
CONFLICT OF INTEREST
All authors have no conflict of interest to declare.
AUTHOR CONTRIBUTIONS
Andrea Gabusi: Conceptualization; Data curation; Investigation; Writing‐original draft; Writing‐review & editing. Davide Bartolomeo Gissi: Conceptualization; Investigation; Supervision; Writing‐review & editing. Roberto Rossi: Investigation; Writing‐review & editing. Maria P Foschini: Methodology; Supervision; Validation; Writing‐review & editing. Lucio Montebugnoli: Conceptualization; Methodology; Supervision; Validation; Writing‐review & editing.
Gabusi A, Gissi DB, Rossi R, Foschini MP, Montebugnoli L. Persistent lesions in oral cavity after SARS‐CoV‐2 infection. Oral Dis. 2021;00:1–2. 10.1111/odi.13805
REFERENCES
- Amorim dos Santos, J. , Normando, A. G. C. , Carvalho da Silva, R. L. , De Paula, R. M. , Cembranel, A. C. , Santos‐Silva, A. R. , & Guerra, E. N. S. (2020). Oral mucosal lesions in a COVID‐19 patient: New signs or secondary manifestations? International Journal of Infectious Diseases, 97, 326–328. 10.1016/j.ijid.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo, P. , Xing, Y. , Xiao, Y. U. , Deng, L. , Zhao, Q. , Wang, H. , Xiong, Y. , Cheng, Z. , Gao, S. , Liang, K. E. , Luo, M. , Chen, T. , Song, S. , Ma, Z. , Chen, X. , Zheng, R. , Cao, Q. , Wang, F. , & Zhang, Y. (2020). Clinical characteristics of refractory COVID‐19 pneumonia in Wuhan, China. Clinical Infectious Diseases. Epub ahead of print. ciaa270. 10.1093/cid/ciaa270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, F. , Nie, J. , Wang, H. , Zhao, Q. , Xiong, Y. , Deng, L. , Song, S. , Ma, Z. , Mo, P. , & Zhang, Y. (2020). Characteristics of peripheral lymphocyte subset alteration in COVID‐19 pneumonia. Journal of Infectious Diseases, 221, 1762–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, H. , Zhong, L. , Deng, J. , Peng, J. , Dan, H. , Zeng, X. , Li, T. , & Chen, Q. (2020). High expression of ACE2 receptor of 2019‐nCoV on the epithelial cells of oral mucosa. International Journal of Oral Science, 12, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye, G. , Pan, Z. , Pan, Y. , Deng, Q. , Chen, L. , Li, J. , Li, Y. , & Wang, X. (2020). Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. Journal of Infection, 80, e14–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]


