Abstract
In light of the current coronavirus disease 2019 (COVID-19) pandemic and potential future infectious disease outbreaks, a comprehensive understanding of the negative effects of epidemics and pandemics on healthcare workers' mental health could inform appropriate support interventions. Thus, we aimed to synthesize and quantify the psychological and psychosomatic symptoms among frontline medical staff. We searched four databases up to March 19, 2020 and additional literature, with daily search alerts set up until October 26, 2020. Studies reporting psychological and/or psychosomatic symptoms of healthcare workers caring for patients with severe acute respiratory syndrome, H1N1, Ebola, Middle East respiratory syndrome, or COVID-19 were eligible for inclusion. Two reviewers independently conducted the search, study selection, quality appraisal, data extraction, and synthesis and involved a third reviewer in case of disagreement. We used random effects modeling to estimate the overall prevalence rates of psychological/psychosomatic symptoms and the I2 statistic. We included 86 studies, reporting data from 75,991 participants. Frontline staff showed a wide range of symptoms, including concern about transmitting the virus to the family (60.39%, 95% CI 42.53–76.96), perceived stress (56.77%, 95% CI 34.21–77.95), concerns about own health (45.97%, 95% CI 31.08–61.23), sleeping difficulties (39.88%, 95% CI 27.70–52.72), burnout (31.81%, 95% CI 13.32–53.89), symptoms of depression (25.72%, 95% CI 18.34–33.86), symptoms of anxiety (25.36%, 95% CI 17.90–33.64), symptoms of posttraumatic stress disorder (24.51%, 95% CI 18.16–31.46), mental health issues (23.11%, 95% CI 15.98–31.10), and symptoms of somatization (14.68%, 95% CI 10.67–19.18). We found consistent evidence for the pervasive and profound impact of large-scale outbreaks on the mental health of frontline healthcare workers. As the COVID-19 crisis continues to unfold, guaranteeing easy access to support structures for the entire healthcare workforce is vitally important.
Keywords: Severe acute respiratory syndrome, Coronavirus disease 2019, Epidemic, Pandemic, Healthcare providers
Introduction
In the last 20 years, climate change, environmental destruction, frequent zoonotic spillover, overpopulation, and poverty have contributed to an increasing occurrence of emerging and re-emerging infectious diseases [1, 2, 3]. Notable outbreaks have included the 2003 severe acute respiratory syndrome (SARS) epidemic [4], the 2009 H1N1 pandemic [5], the Middle East respiratory syndrome (MERS) epidemic first reported in 2012 [6], the 2014–2016 West Africa Ebola epidemic [7], and the current coronavirus disease 2019 (COVID-19) pandemic [8].
For public health, ensuring high standards of care during and after these emergencies is a top priority linked to numerous logistic, organizational, and clinical challenges. Healthcare workers play a key role at all levels of caregiving, but these large-scale outbreaks have shown that the enormous psychological burden of working under such stressful circumstances can severely affect their well-being and, consequently, work performance [9, 10, 11, 12, 13]. Although the strategic and ethical value of preserving and enhancing healthcare workers' well-being and resilience has been recognized [14, 15, 16], pursuing this goal during a global pandemic is challenging. Healthcare workers at the frontlines of COVID-19 care experience high levels of stress [17], face difficult ethical decisions, such as how to allocate limited ventilators [18, 19, 20], and are prone to developing psychological and psychosomatic symptoms [21, 22]. The psychological trauma has even led some healthcare providers to suicide [23, 24].
The COVID-19 pandemic cannot be compared to disasters like hurricanes or wildfires since it is not “confined in time and space” [25]. Indeed, more than 8 months after the World Health Organization declared COVID-19 a pandemic on March 11, 2020 [8], countries across Europe, Russia, and the United States are seeing a dramatic resurgence in infections [26, 27, 28]. Since healthcare institutions will have to deal with COVID-19 and its psychological consequences for many months to come, a thorough understanding of the negative effects of epidemics and pandemics on healthcare workers' mental health is needed to mitigate the traumatic impact and to develop appropriate support interventions.
In recent months, a few rapid reviews [29, 30, 31, 32] have already investigated some of these aspects, but a systematic review and meta-analysis of the literature addressing the role of previous epidemics and pandemics has not been conducted.
In this study, we aimed to comprehensively synthesize and quantify the psychological and psychosomatic symptoms of healthcare providers on the frontline of past epidemics/pandemics (i.e., Ebola, H1N1, SARS, MERS) and the current pandemic (i.e., COVID-19).
Methods
The protocol of this study is registered in the International Prospective Register of Systematic Reviews (PROSPERO), registration number CRD42020175135.
Search and Selection Process
We systematically searched the electronic databases PubMed, Web of Science Core Collection, MEDLINE, and PsycINFO up to March 19, 2020, without restriction to publication date or language. The search strategy read as follows: (swine flu OR A/H1N1 OR 2009 H1N1 OR H1N1 OR [H1N1]pdm09 virus OR viral hemorrhagic fever OR Ebola OR Ebola virus disease OR Ebola hemorrhagic fever OR EVD OR coronavirus infection OR coronavirus disease OR COVID-19 OR 2019 novel coronavirus OR 2019-nCoV OR severe acute respiratory syndrome coronavirus 2 OR SARS-CoV-2 OR SARS-CoV OR SARS coronavirus OR severe acute respiratory syndrome OR SARS OR MERS-CoV OR Middle East respiratory syndrome OR MERS) AND (healthcare worker OR healthcare provider OR health professional OR health personnel OR nurse OR physician OR clinician) AND (emotion OR professional burnout OR mental health OR psychological impact OR psychosocial effect OR experience OR psychological response OR psychological symptom OR feeling OR psychosomatic symptom OR emotional distress) (see online suppl. File 1; for all online suppl. material, see www.karger.com/doi/10.1159/000513733).
To identify additional literature, we searched reference lists of reviews, general discussion papers, commentaries, and editorials and screened grey literature by using specific databases (i.e., Open Grey database, Grey Literature Project; see online suppl. File 2). Moreover, to identify newly published, potentially eligible articles, we set up automatic, daily e-mail search alerts for the database PubMed from March 20, 2020 to October 26, 2020.
Studies were considered eligible for inclusion if (1) original findings were reported, (2) participants were healthcare workers exposed to/taking care of patients infected with or suspected to have SARS, H1N1, Ebola, MERS, or COVID-19 and/or working in high-risk settings, such as emergency departments, infectious disease departments, fever clinics, radiology units, or intensive care units, (3) the psychological impact of these epidemics/pandemics on healthcare workers was reported quantitatively, and (4) they were published in English, Italian, or German (languages spoken by the authors). No restrictions on setting (inpatient or outpatient care), healthcare profession, age, sex, or other sociodemographic characteristics were applied. Editorials, general discussion papers, commentaries, letters, book chapters, single case studies, case series, qualitative studies, and all types of reviews were excluded.
Two reviewers (I.M.B. and F.M.) independently screened the titles and abstracts of the retrieved records using Rayyan, a systematic review web application [33]. The two reviewers retrieved and independently evaluated the full texts of all potentially eligible studies. In case of disagreement, they discussed the appropriateness of inclusion/exclusion and involved a third reviewer (M.R.) to further assess it.
We recorded the search and selection process following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement by Moher et al. [34].
Quality Appraisal
Two appraisers (I.M.B. and M.R.) independently assessed the methodological quality of the included studies applying the standardized 8-item Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross-Sectional Studies [35] or the 11-item Joanna Briggs Institute Critical Appraisal Checklist for Cohort Studies [36] for cross-sectional and longitudinal studies, respectively. Any potential disagreement was resolved by discussion and/or by involving a third appraiser (F.M.).
Main Outcomes
The main outcomes were the prevalence rates, the mean scores (standard deviations), and/or the median scores of psychological and psychosomatic symptoms (e.g., emotional distress, anxiety, depression) of healthcare workers on the frontline of epidemics/pandemics (i.e., SARS, H1N1, Ebola, MERS, COVID-19) at baseline, and, if available, at follow-up.
If available, potential differences in psychological and psychosomatic symptoms between frontline and non-frontline healthcare workers/general public and/or odds ratios and the respective 95% CI were described.
Data Extraction and Synthesis
Two reviewers (I.M.B. and M.R.) independently collected the study characteristics (e.g., authors, year, country, setting and population, sample size) as well as the outcome measures (i.e., psychological and psychosomatic symptoms) and the results of the selected studies. Microsoft Excel was used for data extraction, storage, and synthesis. Discrepancies between the reviewers were discussed and, if necessary, a third reviewer (F.M.) was involved.
We applied the following general rules for data extraction and synthesis:
(1) If primary studies assessed two or more groups of participants with different levels of exposure to the respective virus: (a) We only reported the data that were separately available for these groups. Data on mixed populations were not taken into account. (b) We extracted only the outcome measures (psychological and psychosomatic symptoms) for which data on frontline healthcare workers were available. Outcomes measures that were only administered to subsamples with low/no risk of exposure were not taken into account.
(2) We only reported data on psychological and psychosomatic symptoms separately for different professions (e.g., nurses, doctors) if numbers for the entire group of frontline healthcare workers were not provided.
(3) If primary studies reported the distribution of severity of symptoms (e.g., mild, moderate, severe) among frontline healthcare workers, we extracted only the data on moderate and severe symptoms.
(4) We only reported odds ratios or prevalence ratios if the strength of the association between exposure to the respective virus and psychological/psychosomatic outcome was described. Odds ratios or prevalence ratios measuring the association between other potential risk factors (e.g., sex, age) and psychological/psychosomatic outcomes were not extracted.
(5) If data on subscores of questionnaires were presented in the primary studies, we reported only the differences in the specific subscores between frontline and non-frontline groups, without mentioning means (standard deviations) and/or median scores.
Meta-Analyses
To account for potential heterogeneity across studies, we applied random effects modeling for all meta-analyses using Stata 16 [37, 38]. To calculate the overall prevalence of psychological and psychosomatic symptoms among frontline healthcare workers (95% CI), we pooled the individual prevalence rates of at least three primary studies at baseline using the “metaprop” command in Stata [38]. To do this, we grouped the variables of interest, extracted from the primary studies, which corresponded in terms of content and wording (see online suppl. File 3).
We investigated statistical heterogeneity by visually assessing forest plots and calculating I2 statistics (0–40%: not important; 30–60%: moderate heterogeneity; 50–90%: substantial heterogeneity; 75–100%: considerable heterogeneity) [39].
Formal Narrative Synthesis
Additionally, we performed a formal narrative synthesis of the findings extracted from the primary studies, following, where applicable, the Synthesis without Meta-Analysis guidelines [40] to enhance transparency. We provide (1) a structured tabulation of study characteristics and statistically significant and nonsignificant results of the primary studies grouped by the type of epidemic/pandemic (i.e., SARS, H1N1, Ebola, MERS, COVID-19), (2) a structured tabulation of statistically significant differences in psychological and psychosomatic symptoms between frontline and non-frontline healthcare workers/general public, and (3) a synthesis of long-term mental outcomes in frontline healthcare workers as reported by the included longitudinal studies, presented as narrative text.
Results
Selection and Inclusion of Studies
We retrieved 1,640 records from the electronic databases (after removal of duplicates) and 355 from the additional searches. After screening of title and/or abstract, we assessed 417 full texts for eligibility, of which 331 were excluded for a variety of reasons (e.g., mismatch with inclusion criteria, mixed population, wrong focus), and 86 [41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126] were included that met all inclusion criteria (see online suppl. Files 4 and 5).
Quality Appraisal
All 79 cross-sectional studies [41, 42, 44, 45, 46, 47, 48, 49, 50, 52, 53, 54, 56, 57, 58, 59, 60, 61, 62, 63, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 124, 125, 126] met four or more quality criteria, with 38 studies meeting all eight [41, 44, 48, 50, 54, 57, 59, 60, 63, 65, 66, 67, 74, 78, 79, 80, 83, 87, 88, 89, 91, 93, 96, 99, 100, 101, 102, 104, 105, 107, 108, 109, 113, 119, 120, 121, 124, 126]. Most of the studies clearly defined criteria for inclusion in the sample, described study subjects and setting in detail, measured the exposure in a valid, reliable way, and used objective standard criteria for measurement of condition and appropriate statistical analysis. However, several studies had shortcomings regarding the identification of confounding factors [45, 47, 62, 112, 116, 122], strategies to deal with confounders [42, 45, 47, 53, 62, 63, 90, 92, 111, 112, 116, 117, 122], and the measurement of outcomes in a valid and reliable way [42, 45, 46, 62, 73, 90, 106].
The seven studies [43, 51, 55, 64, 75, 76, 123] with a longitudinal design showed satisfactory quality, meeting seven or more criteria. However, no study met all eleven criteria. In most of the studies, the two groups were similar and recruited from the same population, exposures were measured similarly, exposures and outcomes were assessed in a valid and reliable way, and appropriate statistical analysis was used. However, all articles lacked clarity regarding whether or not participants were free of psychological and psychosomatic symptoms at the start of the study or at the moment of exposure. Some studies also showed shortcomings in dealing with incomplete follow-up [51, 64] and confounding factors [43, 64]. Appraisers' judgments of each study are presented in detail in online supplementary Files 6 and 7, respectively.
Characteristics of Primary Studies
The 86 included primary studies, published between 2004 and 2020 and all written in English, reported sample sizes ranging from 18 [58] to 10,178 [87], reaching a total number of 75,991 participants (referring to sample sizes at baseline). Online supplementary Files 8–12 give a detailed overview of the study characteristics, the outcome measures, and the main findings of the primary studies (statistically significant findings highlighted in bold).
Seventeen articles focused on the 2003 SARS epidemic [41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57], 61 on the current COVID-19 pandemic [66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126], four on the MERS epidemic of 2015 and 2016 [62, 63, 64, 65], and two each on the 2014–2016 West Africa Ebola epidemic [60, 61] and on the 2009 H1N1 pandemic [58, 59].
The included SARS studies were performed in Taiwan (n = 5) [43, 46, 47, 49, 55], Hong Kong (n = 5) [42, 44, 51, 53, 56], Singapore (n = 2) [41, 52], China (n = 2) [48, 57], and Canada (n = 3) [45, 50, 54], countries that represented SARS hotspots. The primary studies on H1N1 were published in New Zealand [58] and Japan [59], the studies on Ebola in Germany [60] and Libera [61], and the articles on MERS covered the outbreaks in South Korea [63, 64, 65] and Saudi Arabia [62]. The majority of the studies on COVID-19 were published in China (n = 32) [67, 73, 74, 75, 76, 84, 85, 86, 88, 91, 92, 93, 95, 96, 97, 99, 101, 102, 107, 110, 113, 114, 116, 117, 118, 119, 121, 122, 123, 124, 125, 126] and Italy (n = 6) [71, 72, 78, 79, 83, 103]. Other studies were conducted in the United States [68, 89, 106], Iran [100, 105, 112], Turkey [80, 104, 111], Germany [90, 120], Pakistan [66, 87], Poland [115], India [108], Egypt [81], Brazil [77], France [70], Spain [94], Saudi Arabia [98], and Singapore [109]. Two studies recruited participants from different countries [69, 82]. Several articles (e.g., Honey and Wang [58], Elshami et al. [82], An et al. [67]) resulted from international collaboration.
Most of the 86 studies applying a cross-sectional study design assessed the psychological impact at a single point in time. Namely, 29 studies performed data collection in earlier phases of the outbreak in the respective country [64, 65, 66, 77, 79, 80, 81, 84, 85, 86, 87, 88, 89, 91, 96, 98, 100, 103, 105, 106, 108, 109, 111, 112, 113, 114, 115, 120, 126], nine during the outbreak [69, 73, 82, 95, 97, 101, 110, 118, 125], 32 in later phases [41, 42, 44, 45, 46, 50, 53, 54, 56, 59, 60, 61, 67, 68, 70, 71, 72, 74, 78, 83, 90, 92, 93, 94, 102, 104, 107, 117, 119, 121, 122, 124], and eight after the end of the outbreak [47, 48, 49, 52, 57, 58, 63, 99]. Another seven studies focusing on SARS [43, 51, 55], MERS [64], and COVID-19 [75, 76, 123] also included follow-up data.
More than two-thirds of the studies (n = 60) [41, 42, 43, 44, 45, 47, 48, 50, 51, 53, 54, 55, 57, 59, 60, 62, 63, 64, 65, 66, 67, 68, 71, 72, 74, 75, 78, 79, 80, 83, 87, 88, 89, 90, 91, 92, 93, 99, 100, 101, 102, 103, 104, 105, 107, 108, 109, 111, 112, 113, 114, 115, 116, 117, 119, 120, 121, 122, 124, 126] compared psychological and psychosomatic symptoms between frontline staff and other groups of participants (e.g., non-frontline healthcare providers, general public).
Prevalence of Psychological and Psychosomatic Symptoms
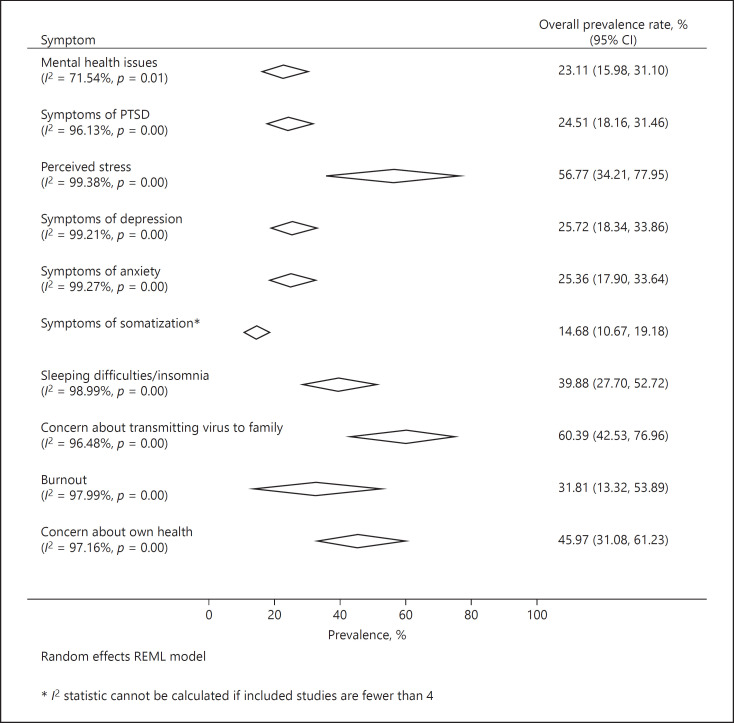
Meta-Analyses. We computed the overall prevalence rates for ten symptoms experienced by healthcare providers working at the frontline of epidemics/pandemics, namely concern about transmitting the virus to the family (60.39%, 95% CI 42.53–76.96), perceived stress (56.77%, 95% CI 34.21–77.95), concerns about own health (45.97%, 95% CI 31.08–61.23), sleeping difficulties/insomnia (39.88%, 95% CI 27.70–52.72), burnout (31.81%, 95% CI 13.32–53.89), symptoms of depression (25.72%, 95% CI 18.34–33.86), symptoms of anxiety (25.36%, 95% CI 17.90–33.64), symptoms of posttraumatic stress disorder (PTSD) (24.51%, 95% CI 18.16–31.46), mental health issues (23.11%, 95% CI 15.98–31.10), and symptoms of somatization (14.68%, 95% CI 10.67–19.18) (Fig. 1). I2 estimates ranged from 71.54 to 99.38%, indicating substantial to considerable heterogeneity across studies [39]. A table subdividing the studies included in the meta-analysis by epidemic/pandemic as well as all individual forest plots can be found in online supplementary Files 13 and 14, respectively.
Fig. 1.
Overall prevalence rates of the psychological and psychosomatic symptoms among frontline healthcare staff. PTSD, posttraumatic stress disorder.
Additional Psychological Symptoms (Unpooled Prevalence Rates). Due to insufficient data from the primary studies and/or too heterogeneous variables of interest, we were not able to pool all the extracted prevalence rates. Namely, prevalence rates of suicidal ideation (12.0% [74]; 13.0% [124]), fatigue (70.3% [51]; 71.0% [44]), fear of social contact (41.7% [51]; 46.0% [44]), and worry related to uncertainty about the future course of the outbreak among frontline healthcare workers (45% [117]; 92.3% [46]) were each reported twice. Lastly, for other psychological conditions and symptoms, such as allostatic load (15.8% [99]), low quality of life (44.44% [108]), poor subjective well-being (71.42% [78]), sadness (49.6% [70]), obsessive-compulsive symptoms (7.3% [88]), and feeling of isolation (4.3% [65]), prevalence rates were only recorded once.
Comparison between Frontline and Non-Frontline Healthcare Workers/the General Public
As mentioned above, 61 primary studies compared different groups and/or subgroups, i.e., healthcare staff working in high-risk settings (i.e., contact with/caring for patients diagnosed with the disease, contact with/caring for patients under investigation) and staff working in low-risk settings or in nonclinical areas (i.e., not providing direct care/working in other clinical departments, working in nonclinical areas). Few studies used additional subgroups, such as nonmedical workers or the general public [92, 99, 112, 124]. A structured synthesis of statistically significant group differences in psychological and psychosomatic symptoms is provided in online supplementary File 15.
A variety of psychological (e.g., depression, anxiety, PTSD) and psychosomatic symptoms (e.g., insomnia, bodily pain) were compared between groups. Whereas all studies on SARS, H1N1, Ebola, and MERS demonstrated worse mental health and lower psychological well-being among frontline healthcare providers versus non-frontline groups, the findings of the recent COVID-19 studies are less consistent. Indeed, three studies [92, 109, 117] found higher scores of trauma as well as higher prevalence of burnout and anxiety among non-frontline groups versus frontline groups. However, as it can be seen in online supplementary Files 8–12, not all group comparisons revealed significant differences between frontline and non-frontline staff.
Trends in the Psychological Distress of Frontline Healthcare Workers over Time
As noted above, seven studies also conducted follow-ups. While five studies [43, 55, 64, 75, 76] revealed a general trend towards improvement of frontline healthcare workers' emotional well-being at follow-up, two studies [51, 123] showed a worsening of psychological symptoms in this population.
Notably, Lee et al. [64], examining hospital workers involved in MERS-related tasks, observed lower but still elevated subjective distress levels at the second time point. Similarly, Chen et al. [43], assessing healthcare workers belonging to a SARS task force, found a significant improvement in their general health status (p < 0.05). Likewise, Su et al. [55], investigating nurses working in SARS units (i.e., general SARS unit, SARS intensive care unit) found an improvement of depressive and PTSD symptoms over time (p < 0.001) as well as anxiety, but noted that the sleep quality of those working in the regular SARS units was still impaired at the end of the study (p < 0.05). Chen et al. [43] and Cai et al. [75], assessing healthcare providers at the COVID-19 frontline, found a significant decrease in mental health issues (p < 0.05) and a significantly lower risk for depression, anxiety, and PTSD symptoms (p < 0.01) at follow-up.
In contrast, McAlonan et al. [51] reported an increase in the stress levels of the SARS frontline group 1 year later (p < 0.05), and Zhao et al. [123] documented a worsening of sleep quality among COVID-19 frontline workers at 1-month follow-up (p < 0.001).
Discussion
This appears to be the first systematic review and meta-analysis to comprehensively synthesize and quantify the wide range of psychological and psychosomatic symptoms among healthcare workers delivering care in different global infectious disease outbreaks. The focus on past epidemics as well as the current global pandemic allowed us to draw a broad picture of the psychological trauma experienced by frontline medical workers in different countries.
Our results suggest that a substantial number of frontline healthcare workers suffer greatly from a variety of psychological and psychosomatic problems ranging from sleep disturbance, somatization symptoms, anxiety, and perceived stress to depression, PTSD, and burnout. These symptoms are commonly triggered by stressful, traumatic events and can have far-reaching consequences for healthcare providers' physical and psychological well-being, relationships to others, and performance at work [127, 128, 129].
Further, in the studies that assessed psychological reactions to uncertainty or perceived risk of infection (i.e., worry about own health, concern about spreading the virus to the family, fear of social contact, worry related to uncertainty regarding the future course of the outbreak), a great proportion of healthcare workers expressed concerns and worries. This corroborates the idea from previous research [130] that a core element underlying the onset of global psychological distress could be the perceived lack of control of one's own professional and personal life. However, considering the large number of frontline healthcare workers who were infected with SARS [131], H1N1 [132], MERS [133], Ebola [134], and COVID-19 [135], the fears of infection were well-founded.
Given the risk of infection and the numerous other stressors faced by frontline workers, it is surprising that three of the included studies on COVID-19 [92, 109, 117] reported higher levels of traumatization, symptoms of PTSD, burnout, and anxiety for non-frontline than for frontline groups. Possible explanations for this unexpected finding may be the greater availability of psychological support for frontline staff, more up-to-date information on the outbreak, policies and infection control measures, and use of personal protective equipment in this group [92, 109, 117]. However, caution is due here because the comparison group in one of the three studies [92], which included also the general public, was poorly defined. It is possible that the participants in the comparison group differed from the specialized and highly educated medical staff with regard to educational and socioeconomic background. The fact that lower educational level and socioeconomic status are associated with worse physical and mental health [136, 137] might be another explanation for why these participants fared worse psychologically than those on the frontlines. Moreover, it is important to bear in mind that the general public may have faced a greater risk of becoming unemployed during the pandemic than the hospital staff [99], thus possibly adding to the psychological distress.
Unfortunately, it seems inevitable that emerging and re-emerging infectious diseases will be a recurring threat to healthcare systems in the future [1]. To maintain high standards of care, it is essential to prepare healthcare staff for future similar events, as also suggested by one of the included publications [109]. Tan et al. [109] reported a much lower prevalence of PTSD among healthcare workers during the COVID-19 pandemic than Chan and Huak [41] and Phua et al. [52], who examined healthcare worker in the same city (Singapore) during the SARS outbreak in 2003. According to Tan et al. [109], this observed difference could be explained in part by better mental preparedness among healthcare staff and the adoption of rigid infection control measures after SARS. However, considering the heterogeneity among these studies, this finding must be interpreted with caution. For instance, while the two SARS studies [41, 52] collected data in later phases of the SARS outbreak in Singapore, Tan et al. [109] recorded the data in earlier phases of the COVID-19 outbreak in Singapore.
Lastly, we sought to explore whether the psychological distress following an epidemic/pandemic tends to improve or worsen over time. Although five of the seven follow-up studies seemed to suggest an overall improvement, only one [75] mentioned that psychological support interventions were available to the staff. The other studies did not report whether and what kind of psychological support was offered. Thus, no firm conclusion can be drawn from the findings of this small subsample, and future studies should examine this aspect further. In any case, previous research has found that high levels of stress, feeling of lack of control, anxiety, depression, insomnia − all symptoms with a high overall prevalence rate in our sample − can represent, if not properly acknowledged and managed, precursors to allostatic overload as well as burnout syndrome [18, 138, 139, 140, 141].
Recommendations for Healthcare Organizations during the COVID-19 Pandemic
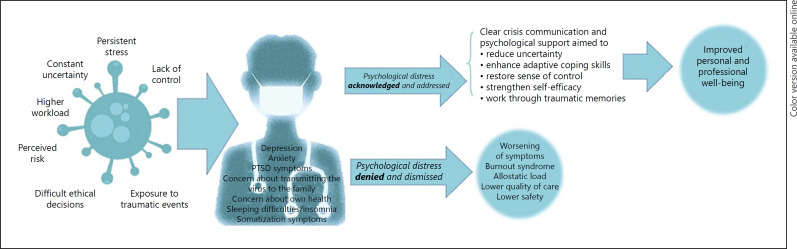
To prevent an increase in psychological and psychosomatic symptoms and burnout among the healthcare workforce on the frontlines of COVID-19, we urge healthcare organizations to acknowledge and address healthcare providers' psychological distress (Fig. 2). Clear, transparent crisis communication by leadership and supervisors offering accurate, updated information [63, 80, 117, 142, 143] and provision of psychological support, which gives healthcare workers the chance to work through traumatic memories, may help to reduce uncertainty, restore a sense of control, and strengthen self-efficacy. This may ultimately lead to improved personal and professional well-being and positive functioning, and thus also to better quality of care and patient safety [129, 144, 145].
Fig. 2.
Acknowledging and addressing healthcare workers' psychological distress during the current pandemic. PTSD, posttraumatic stress disorder.
Psychological support should be made available not only to healthcare workers directly caring for patients with COVID-19, but also to those who are exposed to the virus in other ways (e.g., laboratory, environmental services, laundry service) as well as to medical staff working in other departments. We recommend that healthcare institutions implement or expand already existing peer support programs to ensure easy and timely access to psychological first aid and emotional support and, if necessary, referral to mental health professionals.
As emphasized by Theorell [18] and Greenberg et al. [146], healthcare organizations should also actively monitor healthcare workers in the aftermath of the initial crisis to identify those struggling with the long-term effects of the traumatic experience and in need of psychological help. This is especially important given that after disasters, communities and individuals usually go through different phases in moods [142, 147]. With many countries facing again drastic surges in COVID-19 infections, hospitalizations, and deaths and with the future course of the pandemic being uncertain, the current “disillusionment phase” can be described as particularly lengthy and discouraging for healthcare workers. Enhancing healthcare providers' psychological resilience by acknowledging the experienced distress and by fostering adaptive coping skills [18, 129, 148] can not only help them to face acute critical situations in the care for COVID-19 patients, such as difficult ethical decisions, adverse events, and breaking bad news to patients [149], but also to better deal with the persistent stress in the coming months, which, in turn, may lower the risk of high allostatic load and burnout [18, 140, 141].
Aside from actions directly at the provider level, like mental health prevention and support, protecting healthcare workers' psychological and physical well-being also includes actions taken at the organizational and structural level [150]. As pointed out by Theorell [18], healthcare managers should ensure flexible work schedules, which would allow healthcare providers to rest between tiring shifts and to maintain a healthy sleep hygiene, arrange for support systems for healthcare workers' families, and involve healthcare workers in decision processes to enhance their sense of self-efficacy and belonging.
Finally, to reduce human and financial losses [1] in potential future infectious disease outbreaks, healthcare institutions should plan ahead by creating infection control teams [42] and developing strategies to optimize the supply of personal protective equipment [151].
Limitations
This study should be interpreted in light of certain limitations. First, the observational design of the primary studies did not allow drawing causal conclusions between exposure and outcomes. Second, the majority of the included studies recruited participants on a voluntary basis, had a cross-sectional study design, and used self-report questionnaires. Therefore, it is possible that certain biases (e.g., self-selection bias, social desirability bias) might have influenced the results and in turn also the findings of our study. Moreover, in those studies that retrospectively assessed frontline healthcare workers' well-being, recall bias may have been introduced. Third, the included studies were heterogeneous in many regards, such as settings, populations, applied questionnaires, and cutoff scores, as shown by the high I2 statistics and the wide CI around overall estimates of prevalence. The primary studies also differed in the timing of baseline data collection. While some studies administered the surveys in the beginning of the respective outbreak, others collected data in later phases. For instance, as noted by Cai et al. [73], articles assessing healthcare workers' mental health in the beginning of an outbreak may underestimate its negative emotional impact as psychological stress often increases over time. Similarly, exhaustion and depression may take longer to develop. On the contrary, it might also be possible that some healthcare providers feel more affected and anxious in the beginning of an epidemic/pandemic, when knowledge of the newly emerged disease is scarce and clinical work processes adapted to the new situation have not yet been optimized. Fourth, in several studies, the comparison groups including the general public and/or staff working in nonclinical areas were poorly defined with regard to socioeconomic and educational background as well as medical history. This might have confounded our findings to a certain degree. Fifth, considering the unprecedented surge in publications focusing on COVID-19 [152], we may have missed important papers published after we stopped screening the automatic daily search alerts on PubMed on October 26, 2020. Finally, data extraction and formal narrative synthesis can be prone to subjective assessment and interpretation. Aiming to overcome this limitation, we followed, where applicable, the Synthesis without Meta-Analysis guidelines [40] and established a set of strict rules for extracting and synthesizing the data, which was then applied by two independent reviewers.
Directions for Future Research
Further research should be undertaken to prospectively assess frontline providers' mental health during different phases of the ongoing pandemic, such as, e.g., the current second waves of COVID-19 infections sweeping Europe as well as the long-term effects of this crisis.
The trajectory of healthcare workers' emotional well-being still needs to be defined. More data are needed to determine whether healthcare workers experience an improvement of symptoms at follow-up or further impairment, as suggested by the phases of disaster model [147]. Future longitudinal studies need to take into account whether participants received psychological support during or after the pandemic. Other potentially contributing factors, such as healthcare workers' history of mental disorders or the overall length of the outbreak, should also be considered.
Moreover, further investigation is needed of the differences and similarities between frontline and non-frontline groups, taking into account potential confounders such as educational, employment, and health status. Lastly, international collaboration should be strongly promoted in future work as a critical part of a global pandemic response in order to share expertise, good practice, and clinical guidelines as well as disseminate knowledge [153].
Conclusions
Our systematic review and meta-analysis provides a comprehensive picture of the psychological burden on frontline health workers of epidemics and the current pandemic spanning two decades (i.e., SARS, H1N1, Ebola, MERS, and COVID-19). Including data from 75,991 participants, we found consistent evidence for the pervasive and profound impact of these infectious disease outbreaks on healthcare workers' mental health. As the current COVID-19 crisis continues to unfold, it will be vitally important to guarantee easy access for the entire healthcare workforce to psychological support structures so they can cope better with acute critical situations as well as prolonged periods of stress.
Conflict of Interest Statement
None of the authors have any conflicts of interest to declare.
Funding Sources
There are no funding sources to declare.
Author Contributions
All authors jointly designed the study. I.M. Busch, F. Moretti, and M. Rimondini were involved in the search and selection process, the quality assessment, the data extraction, and the formal narrative synthesis. M. Mazzi conducted the meta-analysis. I.M. Busch and M. Rimondini drafted the initial manuscript, which was then revised by F. Moretti, A.W. Wu, and M. Mazzi. All authors approved the final manuscript.
References
- 1.Ross AG, Crowe SM, Tyndall MW. Planning for the Next Global Pandemic. Int J Infect Dis. 2015 Sep;38:89–94. doi: 10.1016/j.ijid.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alirol E, Getaz L, Stoll B, Chappuis F, Loutan L. Urbanisation and infectious diseases in a globalised world. Lancet Infect Dis. 2011 Feb;11((2)):131–41. doi: 10.1016/S1473-3099(10)70223-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plowright RK, Parrish CR, McCallum H, Hudson PJ, Ko AI, Graham AL, et al. Pathways to zoonotic spillover. Nat Rev Microbiol. 2017 Aug;15((8)):502–10. doi: 10.1038/nrmicro.2017.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention [Internet] CDC SARS Response Timeline [cited 2020 Nov 27] Available from: https://www.cdc.gov/about/history/sars/timeline.htm.
- 5.Centers for Disease Control and Prevention [Internet] H1N1 Pandemic (H1N1pdm09 virus) [cited 2020 Sep 7] 2009. Available from: https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html.
- 6.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012 Nov;367((19)):1814–20. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention [Internet] 2014-2016 Ebola Outbreak in West Africa [cited 2020 Nov 27] Available from: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html.
- 8.World Health Organization [Internet] WHO Director-General's opening remarks at the media briefing on COVID-1 9 - 11 March 2020. [cited 2020 Nov 27]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- 9.Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004 Sep;55((9)):1055–7. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 10.Gershon R, Dernehl LA, Nwankwo E, Zhi Q, Qureshi K. Experiences and Psychosocial Impact of West Africa Ebola Deployment on US Health Care Volunteers. PLoS Curr. 2016 Sep;:8. doi: 10.1371/currents.outbreaks.c7afaae124e35d2da39ee7e07291b6b5. ecurrents.outbreaks.c7afaae124e35d2da39ee7e07291b6b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang HS, Son YD, Chae SM, Corte C. Working experiences of nurses during the Middle East respiratory syndrome outbreak. Int J Nurs Pract. 2018 Oct;24((5)):e12664. doi: 10.1111/ijn.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ulrich CM. Ebola is causing moral distress among African healthcare workers. BMJ. 2014 Nov;349(nov07 2):g6672. doi: 10.1136/bmj.g6672. [DOI] [PubMed] [Google Scholar]
- 13.Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010 Nov;10((1)):322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Busch IM, Moretti F, Travaini G, Wu AW, Rimondini M. Humanization of Care: Key Elements Identified by Patients, Caregivers, and Healthcare Providers. A Systematic Review. Patient. 2019 Oct;12((5)):461–74. doi: 10.1007/s40271-019-00370-1. [DOI] [PubMed] [Google Scholar]
- 15.Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Dealing With Adverse Events: A Meta-analysis on Second Victims' Coping Strategies. J Patient Saf. 2020 Jun;16((2)):e51–60. doi: 10.1097/PTS.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 16.McCann CM, Beddoe E, McCormick K, Huggard P, Kedge S, Adamson C, et al. Resilience in the health professions: a review of recent literature. IJW. 2013 Mar;3((1)):60–81. [Google Scholar]
- 17.Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, et al. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother Psychosom. 2020;89((4)):252–4. doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theorell T. COVID-19 and Working Conditions in Health Care. Psychother Psychosom. 2020;89((4)):193–4. doi: 10.1159/000507765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joos A. Psychosomatic Medicine and Covid-19 Pandemic. Psychother Psychosom. 2020;89((4)):263–4. doi: 10.1159/000507640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Truog RD, Mitchell C, Daley GQ. The Toughest Triage - Allocating Ventilators in a Pandemic. N Engl J Med. 2020 May;382((21)):1973–5. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 21.Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89((4)):242–50. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020 Oct;292:113312. doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Federazione Nazionale Ordini Professioni Infermieristiche[Internet] Al fronte di COVID-19 non si muore solo per il virus [cited 2020 Nov 27] Available from: https://www.fnopi.it/2020/03/24/san-gerardo-infermiera-suicida/
- 24.The New York Times Top E.R. Doctor Who Treated Virus Patients Dies by Suicide [cited 2020 Nov 27] Available from: https://www.nytimes.com/2020/04/27/nyregion/new-york-city-doctor-suicide-coronavirus.html.
- 25.Yong E. The Atlantic [Internet]. Our pandemic summer [cited 2020 Nov 27] Available from: https://www.theatlantic.com/health/archive/2020/04/pandemic-summer-coronavirus-reopening-back-normal/609940/
- 26.The Washington Post [Internet] Coronavirus updates: United States tops 100,000 new virus cases in a day for first time [cited 2020 Nov 27] Available from: https://www.washingtonpost.com/nation/2020/11/03/covid-coronavirus-updates-2/
- 27.Looi MK. Covid-19: Is a second wave hitting Europe? BMJ. 2020 Oct;371:m4113. doi: 10.1136/bmj.m4113. [DOI] [PubMed] [Google Scholar]
- 28.Johns Hopkins University & Medicine Coronavirus Resource Center New cases of COVID- 19 in world countries. Available from: https://coronavirus.jhu.edu/data/new-cases [cited November 27, 2020]
- 29.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020 May;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr Psychiatry Rep. 2020 Jul;22((8)):43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stuijfzand S, Deforges C, Sandoz V, Sajin CT, Jaques C, Elmers J, et al. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health. 2020 Aug;20((1)):1230. doi: 10.1186/s12889-020-09322-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav Immun Health. 2020 Oct;8:100144. doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec;5((1)):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tezlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009 Aug;151((4)):264–69, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 35.The Joanna Briggs Institute JBI Critical appraisal checklist for analytical cross-sectional studies. Available from: https://joannabriggs.org/sites/default/files/2020-08/Checklist_for_Analytical_Cross_Sectional_Studies.pdf [cited November 27, 2020]
- 36.The Joanna Briggs Institute [Internet] JBI Critical appraisal checklist for cohort studies [cited 2020 Nov 27] Available from: https://joannabriggs.org/sites/default/files/2020-08/Checklist_for_Cohort_Studies.pdf.
- 37.StataCorp . Stata Statistical Software: Release 16. College Station (TX): StataCorp LLC; 2019. [Google Scholar]
- 38.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014 Nov;72((1)):39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deeks JJ, Higgins JP, Altman DG. Chapter 9: analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration, 2011. Available at: http://www.handbook.cochrane.org. Accessed May 22, 2019.
- 40.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020 Jan;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond) 2004 May;54((3)):190–6. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan SS, Leung GM, Tiwari AF, Salili F, Leung SS, Wong DC, et al. The impact of work-related risk on nurses during the SARS outbreak in Hong Kong. Fam Community Health. 2005 Jul-Sep;28((3)):274–87. doi: 10.1097/00003727-200507000-00008. [DOI] [PubMed] [Google Scholar]
- 43.Chen NH, Wang PC, Hsieh MJ, Huang CC, Kao KC, Chen YH, et al. Impact of severe acute respiratory syndrome care on the general health status of healthcare workers in taiwan. Infect Control Hosp Epidemiol. 2007 Jan;28((1)):75–9. doi: 10.1086/508824. [DOI] [PubMed] [Google Scholar]
- 44.Chua SE, Cheung V, Cheung C, McAlonan GM, Wong JW, Cheung EP, et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004 Jun;49((6)):391–3. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 45.Grace SL, Hershenfield K, Robertson E, Stewart DE. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. 2005 Sep-Oct;46((5)):385–91. doi: 10.1176/appi.psy.46.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee SH, Juang YY, Su YJ, Lee HL, Lin YH, Chao CC. Facing SARS: psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen Hosp Psychiatry. 2005 Sep-Oct;27((5)):352–8. doi: 10.1016/j.genhosppsych.2005.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin CY, Peng YC, Wu YH, Chang J, Chan CH, Yang DY. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. 2007 Jan;24((1)):12–7. doi: 10.1136/emj.2006.035089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012 Jan;53((1)):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lu YC, Shu BC, Chang YY, Lung FW. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom. 2006;75((6)):370–5. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- 50.Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D, Balderson K, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004 Nov-Dec;66((6)):938–42. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 51.McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007 Apr;52((4)):241–7. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 52.Phua DH, Tang HK, Tham KY. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad Emerg Med. 2005 Apr;12((4)):322–8. doi: 10.1197/j.aem.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 53.Poon E, Liu KS, Cheong DL, Lee CK, Yam LY, Tang WN. Impact of severe respiratory syndrome on anxiety levels of front-line health care workers. Hong Kong Med J. 2004 Oct;10((5)):325–30. [PubMed] [Google Scholar]
- 54.Styra R, Hawryluck L, Robinson S, Kasapinovic S, Fones C, Gold WL. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J Psychosom Res. 2008 Feb;64((2)):177–83. doi: 10.1016/j.jpsychores.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007 Jan-Feb;41((1-2)):119–30. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wong TW, Yau JK, Chan CL, Kwong RS, Ho SM, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. 2005 Feb;12((1)):13–8. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 57.Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009 May;54((5)):302–11. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Honey M, Wang WY. New Zealand nurses perceptions of caring for patients with influenza A (H1N1) Nurs Crit Care. 2013 Mar-Apr;18((2)):63–9. doi: 10.1111/j.1478-5153.2012.00520.x. [DOI] [PubMed] [Google Scholar]
- 59.Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci. 2012 Jun;66((4)):353–60. 4. doi: 10.1111/j.1440-1819.2012.02336.x. [DOI] [PubMed] [Google Scholar]
- 60.Lehmann M, Bruenahl CA, Addo MM, Becker S, Schmiedel S, Lohse AW, et al. Acute Ebola virus disease patient treatment and health-related quality of life in health care professionals: A controlled study. J Psychosom Res. 2016 Apr;83:69–74. doi: 10.1016/j.jpsychores.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 61.Li L, Wan C, Ding R, Liu Y, Chen J, Wu Z, et al. Mental distress among Liberian medical staff working at the China Ebola Treatment Unit: a cross sectional study. Health Qual Life Outcomes. 2015 Sep;13((1)):156. doi: 10.1186/s12955-015-0341-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bukhari EE, Temsah MH, Aleyadhy AA, Alrabiaa AA, Alhboob AA, Jamal AA, et al. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak perceptions of risk and stress evaluation in nurses. J Infect Dev Ctries. 2016 Aug;10((8)):845–50. doi: 10.3855/jidc.6925. [DOI] [PubMed] [Google Scholar]
- 63.Jung H, Jung SY, Lee MH, Kim MS. Assessing the Presence of Post-Traumatic Stress and Turnover Intention Among Nurses Post-Middle East Respiratory Syndrome Outbreak: The Importance of Supervisor Support. Workplace Health Saf. 2020 Jul;68((7)):337–45. doi: 10.1177/2165079919897693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018 Nov;87:123–7. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring Nursing Intention, Stress, and Professionalism in Response to Infectious Disease Emergencies: The Experience of Local Public Hospital Nurses During the 2015 MERS Outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci) 2017 Sep;11((3)):230–6. doi: 10.1016/j.anr.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Amin F, Sharif S, Saeed R, Durrani N, Jilani D. COVID-19 pandemic- knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatry. 2020 Sep;20((1)):459. doi: 10.1186/s12888-020-02864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020 Nov;276:312–5. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Arnetz JE, Goetz CM, Sudan S, Arble E, Janisse J, Arnetz BB. Personal Protective Equipment and Mental Health Symptoms Among Nurses During the COVID-19 Pandemic. J Occup Environ Med. 2020 Nov;62((11)):892–7. doi: 10.1097/JOM.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 69.Azoulay E, De Waele J, Ferrer R, Staudinger T, Borkowska M, Povoa P, et al. ESICM Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020 Aug;10((1)):110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Azoulay E, Cariou A, Bruneel F, Demoule A, Kouatchet A, Reuter D, et al. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am J Respir Crit Care Med. 2020 Nov;202((10)):1388–98. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Babore A, Lombardi L, Viceconti ML, Pignataro S, Marino V, Crudele M, et al. Psychological effects of the COVID-2019 pandemic: perceived stress and coping strategies among healthcare professionals. Psychiatry Res. 2020 Nov;293:113366. doi: 10.1016/j.psychres.2020.113366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Buselli R, Corsi M, Baldanzi S, Chiumiento M, Del Lupo E, Dell'Oste V, et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19) Int J Environ Res Public Health. 2020 Aug;17((17)):6180. doi: 10.3390/ijerph17176180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID‑19) in Hubei, China. Med Sci Monit. 2020 Apr;26:e924171. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cai Q, Feng H, Huang J, Wang M, Wang Q, Lu X, et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J Affect Disord. 2020 Oct;275:210–5. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020 Dec;131:132–7. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen H, Sun L, Du Z, Zhao L, Wang L. A cross-sectional study of mental health status and self-psychological adjustment in nurses who supported Wuhan for fighting against the COVID-19. J Clin Nurs. 2020 Nov;29((21-22)):4161–70. doi: 10.1111/jocn.15444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Civantos AM, Bertelli A, Gonçalves A, Getzen E, Chang C, Long Q, et al. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: A national study. Am J Otolaryngol. 2020 Nov-Dec;41((6)):102694. doi: 10.1016/j.amjoto.2020.102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.De Sio S, Buomprisco G, La Torre G, Lapteva E, Perri R, Greco E, et al. The impact of COVID-19 on doctors' well-being: results of a web survey during the lockdown in Italy. Eur Rev Med Pharmacol Sci. 2020 Jul;24((14)):7869–79. doi: 10.26355/eurrev_202007_22292. [DOI] [PubMed] [Google Scholar]
- 79.Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. 2020 Dec;26((6)):1583–7. doi: 10.1111/jep.13444. [DOI] [PubMed] [Google Scholar]
- 80.Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020 Aug;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Elkholy H, Tawfik F, Ibrahim I, Salah El-Din W, Sabry M, Mohammed S, et al. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: a call for action. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020960192. doi: 10.1177/0020764020960192 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 82.Elshami W, Akudjedu TN, Abuzaid M, David LR, Tekin HO, Cavli B, et al. The radiology workforce's response to the COVID-19 pandemic in the Middle East, North Africa and India. Radiography (Lond) 2020 doi: 10.1016/j.radi.2020.09.016. doi: 10.1016/j.radi.2020.09.016 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front Psychol. 2020 Jul;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine. 2020 Jun;24:100424. doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huang L, Wang Y, Liu J, Ye P, Chen X, Xu H, et al. Short report: factors determining perceived stress among medical staff in radiology departments during the COVID-19 outbreak. Psychol Health Med. 2020 Oct;:1–6. doi: 10.1080/13548506.2020.1837390. [DOI] [PubMed] [Google Scholar]
- 86.Huang L, Wang Y, Liu J, Ye P, Chen X, Xu H, et al. Factors Influencing Anxiety of Health Care Workers in the Radiology Department with High Exposure Risk to COVID-19. Med Sci Monit. 2020 Jul;26:e926008. doi: 10.12659/MSM.926008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Imran N, Masood HM, Ayub M, Gondal KM. Psychological impact of COVID-19 pandemic on postgraduate trainees: a cross-sectional survey. Postgrad Med J. 2020 Aug;:postgradmedj-2020-138364. doi: 10.1136/postgradmedj-2020-138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Juan Y, Yuanyuan C, Qiuxiang Y, Cong L, Xiaofeng L, Yundong Z, et al. Psychological distress surveillance and related impact analysis of hospital staff during the COVID-19 epidemic in Chongqing, China. Compr Psychiatry. 2020 Nov;103:152198. doi: 10.1016/j.comppsych.2020.152198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kannampallil TG, Goss CW, Evanoff BA, Strickland JR, McAlister RP, Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One. 2020 Aug;15((8)):e0237301. doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kramer V, Papazova I, Thoma A, Kunz M, Falkai P, Schneider-Axmann T, et al. Subjective burden and perspectives of German healthcare workers during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. 2020 doi: 10.1007/s00406-020-01183-2. doi: 10.1007/s00406-020-01183-2 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020 Mar;3((3)):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020 Aug;88:916–9. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020 Jun;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Martínez-López JÁ, Lázaro-Pérez C, Gómez-Galán J, Fernández-Martínez MD. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J Clin Med. 2020 Sep;9((9)):3029. doi: 10.3390/jcm9093029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020 Jul;28((5)):1002–9. doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. J Clin Nurs. 2020 Nov;29((21-22)):4217–26. doi: 10.1111/jocn.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pan X, Xiao Y, Ren D, Xu ZM, Zhang Q, Yang LY, et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: A cross-sectional survey. Asia-Pac Psychiatry. 2020 Oct;:e12427. doi: 10.1111/appy.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pasay-An E. Exploring the vulnerability of frontline nurses to COVID-19 and its impact on perceived stress. J Taibah Univ Med Sci. 2020 Oct;15((5)):404–9. doi: 10.1016/j.jtumed.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Peng M, Wang L, Xue Q, Yin L, Zhu BH, Wang K, et al. Post-COVID-19 Epidemic: Allostatic Load among Medical and Nonmedical Workers in China. Psychother Psychosom. 2020 Nov;:1–10. doi: 10.1159/000511823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pouralizadeh M, Bostani Z, Maroufizadeh S, Ghanbari A, Khoshbakht M, Alavi SA, et al. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: A web-based cross-sectional study. Int J Afr Nurs Sci. 2020;13:100233. doi: 10.1016/j.ijans.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Qi J, Xu J, Li BZ, Huang JS, Yang Y, Zhang ZT, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020 Aug;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020 Jun;33((3)):e100259. doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open. 2020 May;3((5)):e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of Depression, Anxiety, Distress and Insomnia and Related Factors in Healthcare Workers During COVID-19 Pandemic in Turkey. J Community Health. 2020 Dec;45((6)):1168–77. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sarboozi Hoseinabadi T, Kakhki S, Teimori G, Nayyeri S. Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of Coronavirus Disease -COVID-19- in Iran. Invest Educ Enferm. 2020 Jul;38((2)) doi: 10.17533/udea.iee.v38n2e03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sharma M, Creutzfeldt CJ, Lewis A, Patel PV, Hartog C, Jannotta GE, et al. Healthcare professionals' perceptions of critical care resource availability and factors associated with mental well-being during COVID-19: results from a US survey. Clin Infect Dis. 2020 Sep;:ciaa1311. doi: 10.1093/cid/ciaa1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020 Aug;9((1)):113. doi: 10.1186/s40249-020-00724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Suryavanshi N, Kadam A, Dhumal G, Nimkar S, Mave V, Gupta A, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020 Nov;10((11)):e01837. doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL, et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann Intern Med. 2020 Aug;173((4)):317–20. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine (Baltimore) 2020 Jun;99((26)):e20769. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Uyaroğlu OA, Başaran NÇ, Ozisik L, Karahan S, Tanriover MD, Guven GS, et al. Evaluation of the effect of COVID-19 pandemic on anxiety severity of physicians working in the internal medicine department of a tertiary care hospital: a cross-sectional survey. Intern Med J. 2020 Nov;50((11)):1350–8. doi: 10.1111/imj.14981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry. 2020 Aug;20((1)):402. doi: 10.1186/s12888-020-02804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang Y, Ma S, Yang C, Cai Z, Hu S, Zhang B, et al. Acute psychological effects of Coronavirus Disease 2019 outbreak among healthcare workers in China: a cross-sectional study. Transl Psychiatry. 2020 Oct;10((1)):348. doi: 10.1038/s41398-020-01031-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med (Lond) 2020 Jul;70((5)):364–9. doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wańkowicz P, Szylińska A, Rotter I. Assessment of Mental Health Factors among Health Professionals Depending on Their Contact with COVID-19 Patients. Int J Environ Res Public Health. 2020 Aug;17((16)):5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wu K, Wei X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med Sci Monit Basic Res. 2020 May;26:e924085. doi: 10.12659/MSMBR.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, et al. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J Pain Symptom Manage. 2020 Jul;60((1)):e60–5. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020 Mar;26:e923549. doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yang X, Zhang Y, Li S, Chen X. Risk factors for anxiety of otolaryngology healthcare workers in Hubei province fighting coronavirus disease 2019 (COVID-19) Soc Psychiatry Psychiatr Epidemiol. 2020 Aug; doi: 10.1007/s00127-020-01928-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19 - a survey conducted at the University Hospital Augsburg. Ger Med Sci. 2020 Jun;18:Doc05. doi: 10.3205/000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhan Y, Liu Y, Liu H, Li M, Shen Y, Gui L, et al. Factors associated with insomnia among Chinese front-line nurses fighting against COVID-19 in Wuhan: A cross-sectional survey. J Nurs Manag. 2020 Oct;28((7)):1525–35. doi: 10.1111/jonm.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Y, Xie S, Wang P, Wang G, Zhang L, Cao X, et al. Factors Influencing Mental Health of Medical Workers During the COVID-19 Outbreak. Front Public Health. 2020 Sep;8:491. doi: 10.3389/fpubh.2020.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhao X, Zhang T, Li B, Yu X, Ma Z, Cao L, et al. Job-related factors associated with changes in sleep quality among healthcare workers screening for 2019 novel coronavirus infection: a longitudinal study. Sleep Med. 2020 Nov;75:21–6. doi: 10.1016/j.sleep.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhou Y, Wang W, Sun Y, Qian W, Liu Z, Wang R, et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: workload should be concerned. J Affect Disord. 2020 Dec;277:510–4. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front Psychiatry. 2020 Apr;11:386. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020 Jun;24:100443. doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010 Jan;24((1)):1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and Psychosomatic Symptoms of Second Victims of Adverse Events: a Systematic Review and Meta-Analysis. J Patient Saf. 2020 Jun;16((2)):e61–74. doi: 10.1097/PTS.0000000000000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brooks SK, Rubin GJ, Greenberg N. Traumatic stress within disaster-exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. Br Med Bull. 2019 Mar;129((1)):25–34. doi: 10.1093/bmb/ldy040. [DOI] [PubMed] [Google Scholar]
- 130.Marchand A, Demers A, Durand P. Do occupation and work conditions really matter? A longitudinal analysis of psychological distress experiences among Canadian workers. Sociol Health Illn. 200 Jul 5;27((5)):602–27. doi: 10.1111/j.1467-9566.2005.00458.x. [DOI] [PubMed] [Google Scholar]
- 131.Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018 Mar;60((3)):248–57. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 132.Lietz J, Westermann C, Nienhaus A, Schablon A. The Occupational Risk of Influenza A (H1N1) Infection among Healthcare Personnel during the 2009 Pandemic: A Systematic Review and Meta-Analysis of Observational Studies. PLoS One. 2016 Aug;11((8)):e0162061. doi: 10.1371/journal.pone.0162061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zumla A, Hui DS. Infection control and MERS-CoV in health-care workers. Lancet. 2014 May;383((9932)):1869–71. doi: 10.1016/S0140-6736(14)60852-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.World Health Organization [Internet] Unprecedented number of medical staff infected with Ebola [cited 2020 Nov 27] Available from: https://www.who.int/mediacentre/news/ebola/25-august-2014/en/
- 135.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. COronavirus Pandemic Epidemiology Consortium Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020 Sep;5((9)):e475–83. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Macintyre A, Ferris D, Gonçalves B, Quinn N. What has economics got to do with it? The impact of socioeconomic factors on mental health and the case for collective action. Palgrave Commun. 2018;4((1)):10. [Google Scholar]
- 137.Niemeyer H, Bieda A, Michalak J, Schneider S, Margraf J. Education and mental health: do psychosocial resources matter? SSM Popul Health. 2019 Mar;7:100392. doi: 10.1016/j.ssmph.2019.100392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Aydemir O, Icelli I. Burnout: Risk Factors. In: Bährer-Kohler S, editor. Burnout for Experts. Boston (MA): Springer; 2013. [Google Scholar]
- 139.Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007 Oct;13((5)):482–8. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 140.Fava GA, McEwen BS, Guidi J, Gostoli S, Offidani E, Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019 Oct;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 141.Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on health. A systematic review. Psychother Psychosom. 2021;90((1)):11–27. doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- 142.Wu AW, Connors C, Everly GS., Jr COVID-19: Peer Support and Crisis Communication Strategies to Promote Institutional Resilience. Ann Intern Med. 2020 Jun;172((12)):822–3. doi: 10.7326/M20-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Everly GS, Jr, Wu AW, Crumpsty-Fowler CJ, Dang D, Potash JB. Leadership principles to decrease psychological casualties in COVID-19 and other disasters of uncertainty. Disaster Med Public Health Prep. 2020 Oct;:1–10. doi: 10.1017/dmp.2020.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fava GA. The clinical role of psychological well-being. World Psychiatry. 2012 Jun;11((2)):102–3. doi: 10.1016/j.wpsyc.2012.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rangachari P, L Woods J. Preserving Organizational Resilience, Patient Safety, and Staff Retention during COVID-19 Requires a Holistic Consideration of the Psychological Safety of Healthcare Workers. Int J Environ Res Public Health. 2020 Jun;17((12)):4267. doi: 10.3390/ijerph17124267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020 Mar;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 147.Substance Abuse and Mental Health Services Administration Phases of disaster. Available from: https://www.samhsa.gov/dtac/recovering-disasters/phases-disaster [cited November 27, 2020]
- 148.Maunder RG, Leszcz M, Savage D, Adam MA, Peladeau N, Romano D, et al. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008 Nov-Dec;99((6)):486–8. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Busch IM, Saxena A, Wu AW. Putting the patient in patient safety investigations: barriers and strategies for involvement. J Patient Saf. 2020 doi: 10.1097/PTS.0000000000000699. doi: 10.1097/PTS.0000000000000699. [DOI] [PubMed] [Google Scholar]
- 150.Wu AW, Buckle P, Bellandi T, Haut ER, Koizumi S, Mair A, et al. Supporting the Emotional Well-being of Health Care Workers During the COVID-19 Pandemic. J Patient Saf Risk Manag. 2020 Jun;25((3)):86–90. [Google Scholar]
- 151.Centers for Disease Control and Prevention [Internet] Optimizing Supply of PPE and Other Equipment during Shortages [cited 2020 Nov 27] Avalaible from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html.
- 152.Kambhampati SB, Vaishya R, Vaish A. Unprecedented surge in publications related to COVID-19 in the first three months of pandemic: A bibliometric analytic report. J Clin Orthop Trauma. 2020 May;11(Suppl 3):S304–6. doi: 10.1016/j.jcot.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Fry CV, Cai X, Zhang Y, Wagner CS. Consolidation in a crisis: patterns of international collaboration in early COVID-19 research. PLoS One. 2020 Jul;15((7)):e0236307. doi: 10.1371/journal.pone.0236307. [DOI] [PMC free article] [PubMed] [Google Scholar]