Abstract
Emerging evidence suggests that emotion regulation (ER) impairment in those with ASD is associated with poor mental health. This study used the Emotion Dysregulation Inventory, a new norm-referenced ER measure with clinical cut-offs, developed and validated in ASD and non-ASD samples, to establish rates of ER impairment and understand its association with psychiatric service use in ASD. Parents of 6–17 year olds in three well-characterized samples (nationally representative US n = 1,000; community ASD n = 1,169; inpatient ASD n = 567) completed a battery of questionnaires about their child. The prevalence of ER impairment was significantly higher in the ASD groups compared to the nationally representative sample and highest in the psychiatric Inpatient ASD group. The community ASD and inpatient ASD samples were four and seven times more likely, respectively, to exceed clinical cutoffs for emotional reactivity than the general US sample. Similarly, history of psychiatric hospitalization, recent emergency services use (police contact, emergency room visits, or in-home crisis evaluations for emotional or behavioral concerns in the past 2 months), and psychotropic medication prescriptions were significantly higher in the ASD groups. ER impairment was significantly associated with all forms of psychiatric service use, after controlling for demographics (age, sex, race), co-occurring intellectual disability, and ADHD symptoms. This is the first large-scale study to document substantially higher rates of ER impairment in youth with ASD compared to the general population. The importance of ER impairment is underscored by its association with higher utilization of inpatient, emergency, and medication services in ASD, after accounting for demographics and ADHD-related symptoms.
Keywords: autism spectrum disorder, emotion regulation, outcomes, inpatient, psychotropic medication
Lay Summary:
This study compared problems with emotion regulation in large samples of youth with and without ASD. An ASD community sample had two to four times more youth with clinically elevated regulation impairments compared to youth without ASD. Emotion regulation impairment was also related to using psychiatric hospitalizations, emergency services, and medications in the ASD group. This study suggests that screening for emotion regulation difficulties in ASD is important and treatment may have a wide ranging impact.
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by social-communication difficulties and the presence of restricted and repetitive behaviors, interests, and sensory differences [American Psychiatric Association, 2013]. A diagnosis of ASD has been associated with significant health-care expenditures across the lifespan [Croen, Najjar, Ray, Lotspeich, & Bernal, 2006]. In an analysis of health-care records, youth with ASD were seven times more likely to have outpatient psychiatric visits, and mean health-care costs were 45% higher for youth with ASD compared to non-ASD youth with a psychiatric diagnosis. Psychotropic medication usage was thought to be a contributing factor given that the youth with ASD in this sample were almost nine times more likely to take psychotropic medications [Croen et al., 2006]. One-third to nearly two-thirds of youth with ASD are prescribed at least one psychotropic medication [Rosenberg et al., 2010; Spencer et al., 2013]. Although two atypical antipsychotics are FDA-approved for the treatment of irritability in ASD, many other medications are used off-label and polypharmacy is wide-spread [King, Rynkiewicz, Janas-Kozik, & Tyszkewicz-Nwafor, 2020]. Furthermore, children and adolescents with ASD are nine times more likely than their non-ASD counterparts to require emergency room visits for psychiatric reasons [Kalb, Stuart, Freedman, Zablotsky, & Vasa, 2012] and 12 times more likely to require psychiatric hospitalization [Croen et al., 2006]. Twelve percent of youth with ASD will require psychiatric hospitalization by the time they turn 21 [Mandell, 2008].
Some factors associated with inpatient and emergency service utilization in ASD have been identified. Individual characteristics include lower income, later age of ASD diagnoses, older age, lower adaptive functioning, and greater social-communication deficits [Mandell, 2008; Righi et al., 2018; Turcotte, Shea, & Mandell, 2018]. Co-occurring psychiatric conditions have also been shown to increase the risk of psychiatric hospitalization [Mandell, 2008; Righi et al., 2018] and emergency room visits [Kalb et al., 2012], but with no consistency in the type of co-occurring condition. For example, the top two conditions associated with psychiatric hospitalization included attention-deficit hyperactivity disorder (ADHD) and obsessive compulsive disorder in the study by Mandell [2008] and mood disorders, sleep disorders, and disruptive behavior disorders in the study by Righi et al. [2018], whereas Kalb et al. [2012] found a composite of externalizing disorders and psychotic disorders to be most predictive of emergency room visits. Overall, there remains a need to better understand factors associated with hospitalization and the use of emergency services, particularly those that may be modifiable.
Emotion Regulation
Emotion regulation (ER) impairment may be a transdiagnostic risk factor for the use of psychotropic medications, emergency services, and psychiatric hospitalization. ER is defined as an individual’s ability to modulate the experience and expression of emotions in a way that is socially acceptable and in line with personal goals [Gross & Thompson, 2006]. Mounting evidence suggests that ER is impaired in ASD. Individuals with ASD may have a propensity for impaired ER, given common difficulties with emotion identification in self and others, perspective taking, reading social situations, and response inhibition [Mazefsky et al., 2013]. In fact, core features of ASD such as social difficulties and repetitive behaviors have been linked to ER impairment [Berkovits, Eisenhower, & Blacher, 2017; Samson, Hardan, Lee, Phillips, & Gross, 2015]. Observational studies of children in response to structured tasks have found that children with ASD exhibited stronger and longer negative emotional reactions to triggering events, and used more unconstructive strategies like avoidance, yelling, and hitting a toy during a frustrating task as compared to typically developing children [Jahromi, Meek, & OberReynolds, 2012]. Adolescents and adults with ASD have been found to overly rely on traditionally maladaptive ER strategies, including avoidance and rumination, and to less frequently use adaptive strategies such as reappraisal [Cai, Richdale, Uljarevic, Dissanayake, & Samson, 2018; Samson, Wells, Phillips, Hardan, & Gross, 2015].
Prior research also suggests that youth with ASD are more likely than non-ASD youth to have psychiatric diagnoses [Joshi et al., 2010; Salazar et al., 2015]. This is important given that psychiatric comorbidities have been implicated as a factor related to hospitalization, emergency services, and medication prescription in ASD, and a growing body of research suggests that ER is associated with a higher likelihood of co-occurring psychiatric disorders and problems [Cai et al., 2018; Charlton, Smith, Mazefsky, & White, 2020]. The association between ER and psychiatric symptoms has also been supported when ER was measured using a new measure of emotion dysregulation validated in ASD, called the Emotion Dysregulation Inventory [EDI; Mazefsky, Yu, White, Siegel, & Pilkonis, 2018]. For example, concurrent validity of the EDI was supported by positive correlations with measures of internalizing and externalizing symptoms (Child Behavior Checklist and Aberrant Behavior Checklist) in both ASD and non-ASD samples [Mazefsky, Yu, & Pilkonis, 2020; Mazefsky et al., 2018,b]. Similar findings have been reported in other samples as well, such as a positive correlation between EDI scores and a measure of overall psychiatric burden in a sample of minimally verbal children and adolescents with ASD [Plesa Skwerer, Joseph, Eggleston, Meyer, & Tager-Flusberg, 2019].
Because of complexities in the differential diagnosis of psychiatric conditions in ASD [Mazefsky et al., 2012; Witwer & Lecavalier, 2010], as well as inconsistencies in prior research on which particular co-occurring disorder is related to psychiatric service use outcomes, it would be helpful to understand whether ER impairment (the possible underlying mechanism) is also associated with a greater likelihood of high intensity psychiatric services and medication use. This question would be most appropriately addressed with a measure like the EDI, which offers clinical cut-offs that may provide an option for screening. Importantly, unlike other ER questionnaires used in earlier ASD research [Chetcuti, Uljarević, & Hudry, 2019], the EDI is norm-referenced, validated in ASD, and designed for use across all verbal and intellectual abilities [Mazefsky, Day, et al., 2018; Mazefsky, Yu, et al., 2018]. Because it is also validated in the general population, there is a new opportunity to compare ER across samples of youth with ASD and general population youth.
Therefore, the purpose of the current study is to: (a) compare rates of psychiatric hospitalization, emergency services, and psychiatric medication utilization across a community-based sample of youth with ASD, youth with ASD admitted for psychiatric hospitalization, and a US Census-matched youth sample; (b) compare rates of ER impairment across these three samples; (c) investigate whether ER impairment predicts hospitalization, emergency service use, and psychiatric medication utilization in ASD, above and beyond demographics (e.g., age, sex, race), presence of ID, and ADHD symptoms. ADHD symptoms were included in the model given their prominence and clinical impact in ASD [Reiersen & Todd, 2008], and because prior ADHD research suggests that nonemotional self-regulation impairment can also lead to poor mental health and poor overall outcomes in adulthood [Molina et al., 2009]. The goal was to more conservatively estimate the role of ER by accounting for other potentially important aspects of self-regulation difficulties such as attentional/inhibitory control that are commonly impaired in ASD. It was hypothesized that ER impairment and use of psychotropic medications, emergency services, and psychiatric hospitalization would be significantly more prevalent among ASD groups, and highest in the inpatient ASD sample. Further, it was hypothesized that ER impairment would be significantly associated with the use of inpatient, emergency, and medication psychiatric services in the ASD groups after controlling for demographics, ability level, and ADHD symptoms.
Methods
Participants
The samples were collected for development of the Emotion Dysregulation Inventory (R01 HD079512–05 PI: Mazefsky). The samples were intended to be representative of the population from which they were sampled rather than matched to each other on demographics.
Inpatient psychiatric ASD sample (Autism Inpatient Collection).
The Autism Inpatient Collection (AIC) is a six-site study of patients admitted to specialized inpatient psychiatric units for youth with ASD. The full methods of the AIC have been published [Siegel et al., 2015]. The AIC includes participants between the ages of 4–20 years old, although for the purposes of this study only participants 6–17 years old were included to match the age range of the other two samples (excluded n = 58). Inclusion in the AIC required confirmation of ASD diagnosis by the Autism Diagnostic Observation Schedule-2 [ADOS-2; Lord et al., 2012]. When assessing the role of ADHD symptoms on the relationship between these outcomes and ER impairment, participants from Year 3 of AIC (when the Child Behavior Checklist was added) and onward were included in analyses (n = 335). AIC exclusion criteria included the lack of availability of a caregiver proficient in English or prisoner status for the individual with ASD.
Community ASD sample (Interactive Autism Network).
Participants were recruited through the Interactive Autism Network (IAN), an online registry developed to support Internet-based research studies, in order to provide a sample representative of parents of youth with professional ASD diagnoses that was recruited outside of a clinical setting. Participants in IAN’s registry were invited to complete this study if they had a Social Communication Questionnaire-Lifetime Version [SCQ; Rutter, Bailey, & Lord, 2003] score ≥ 12 and were between the ages of 6–17 years old. The SCQ is a 40-item caregiverreport questionnaire of Yes/No questions that measures ASD symptoms over a person’s lifetime. While prior research has debated which cutoff to use for the SCQ, some research has advocated using the lower cutoff of ≥12 with younger populations and those with higher verbal ability [Corsello et al., 2007; Norris & Lecavalier, 2010]. The SCQ has shown strong discriminative validity between those with and without ASD, including sensitivity >0.80, when using the ≥12 cutoff [Corsello et al., 2007]. Parent-reported professional diagnosis of ASD has been verified by medical records in previous research [Daniels et al., 2012]. Community professional diagnosis of ASD has also been validated [Lee et al., 2010; Marvin et al., 2014] and the distribution of participants in IAN on ASD measures replicates those seen in other, clinically defined research samples [Lee et al., 2010]. To be included in the IAN registry, caregivers were required to provide evidence of a community diagnosis of ASD. Invitations to participate in this study were sent to 11,648 registrants; 9,926 did not respond, 1,642 expressed an interest, and 1,323 participated. Of the 1,323 participants, 1,169 (88.36%) completed all of the measures in the current study and were thus included. Inclusion criteria included the ability to read in English.
US census-matched general youth population sample (YouGov).
Participants were recruited from YouGov, a web-based polling company, to obtain a general population sample of parents of youth representative of the US Census. YouGov collected data from 1,000 caregivers representative of the US population of adults with related children in the household, ages 6–17. YouGov staff interviewed 1,055 respondents, who were then reduced to a sample of 1,000 to produce the final dataset, as described in detail in the study by Mazefsky et al. [2020]. In brief, simple random sampling and weighted propensity scores based on a stratification of gender, age (4-categories), race (4-categories), education (4-categories), and US region were applied to create a final data set matched to the US Census American Community Survey [US Census Bureau, 2016] from the over two million registered US users.
Measures
Demographics and Service Utilization.
The demographic questionnaire collected information on the child and caregiver, including race, ethnicity, and sex. Caregivers were also asked about their child’s verbal ability and IQ. In addition, caregivers completed several questions about current and past use of psychiatric and emergency services, which were combined into the following dichotomous variables: whether the child had any previous psychiatric hospitalizations, current psychotropic medication use (use of any antipsychotic, anti-depressant, mood stabilizer, or anxiolytic), and whether the child accessed emergency services in the past 2 months (police contact, emergency room visits for emotional or behavioral concerns, or in-home crisis evaluations). Medication categories were selected that are most commonly utilized to manage some aspect of ER. Stimulant medications were not included given their primary indication for inattention and hyperactivity, which would be considered other (non-ER) aspects of self-regulation. However, we conducted a sensitivity analysis including stimulants which found that the pattern of results did not change (e.g., significant predictors were the same with and without stimulants in the model; results available upon request).
Child Behavior Checklist (CBCL).
The CBCL is a parent-reported questionnaire of psychiatric symptoms for youth age 6–18 years old [Achenbach & Rescorla, 2001]. Items are rated based on the past 6 months on a 3-point Likert scale as either 0 = Not True, 1 = Somewhat or Sometimes True, or 2 = Very True or Often True. The CBCL has been widely used and is considered well-validated, including in ASD samples [e.g., Stratis & Lecavalier, 2017]. For this study, we used the ADHD Problems scale t-score (M = 50; SD = 15) as a measure of ADHD symptoms.
Emotion Dysregulation Inventory (EDI).
The EDI is a valid, change sensitive, 30-item informant questionnaire for individuals of at least 6 years of age [Mazefsky et al., 2020; Mazefsky, Day, et al., 2018; Mazefsky, Yu, et al., 2018]. The EDI was developed using item response theory (IRT) analysis and none of the final items had evidence of differential item functioning (e.g., psychometric biases) by gender, age, intellectual ability, or verbal ability, making it suitable for use across heterogeneous populations. Parents rate how much of a problem each item has been in the past 7 days on a 5-point scale ranging from Not at all = 0 to Very Severe = 4. The EDI is comprised of a primary 24-item Reactivity scale and a 6-item Dysphoria scale. The Reactivity scale measures intense, rapidly escalating, and sustained emotional reactions, while the Dysphoria scale measures low positive affect, sadness, and unease. Raw scores can be converted into theta scores or t-scores based on a sample of 1,755 youth with ASD [Mazefsky, Yu, et al., 2018] or based on a sample of 1,000 youth matched to the US census [Mazefsky et al., 2020]; the latter can be considered general population norms [Mazefsky et al., 2020]. The autism t-score conversions were used in this study, which provide greater sensitivity to more severe manifestations of ER impairment [Mazefsky et al., 2020]. T-scores have a mean of 50 and SD of 10. Clinical cut-offs for the EDI are based on scoring +1 SD above the general population mean, or a t-score of 60 based on general population conversions. For Reactivity, a t-score of 60 based on the general population norms corresponds to a raw score of 26, which is a t-score of 46.4 based on the autism/clinical conversions. For Dysphoria, a t-score of 60 based on the general population norms corresponds to a raw score of 6, which is a t-score of 52.2 based on the autism/clinical conversions.
Procedure
For the inpatient ASD sample, data were collected during the hospital stay. Caregivers who consented within 10 days of admission were enrolled and completed a questionnaire battery while their child was hospitalized. The community ASD and US Census-matched samples completed the questionnaires online.
Analyses
Aim 1.
To compare rates of dichotomous inpatient psychiatric and emergency services, and psychotropic medication use (history of psychiatric hospitalizations, use of emergency services in the past 2 months, and psychotropic medications use) across the three groups, logistic regressions were run with sex and race as covariates.
Aim 2.
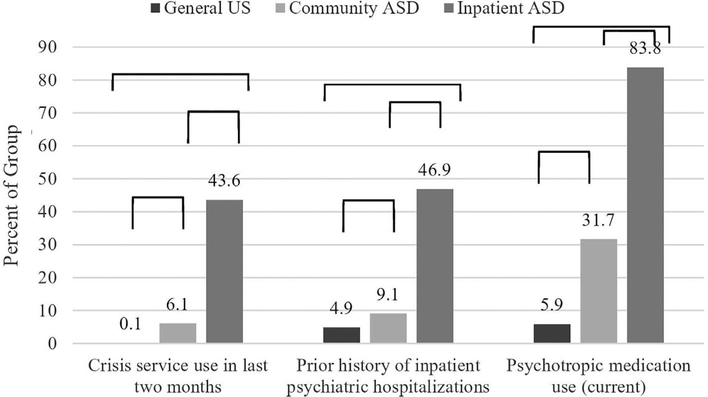
Table 1 includes demographic and descriptive data. The percentage of participants in each group with scores above the clinical cutoff on the EDI was visually depicted in a pie chart (see Fig. 1). A one-way ANOVA was used to compare EDI scores between the three groups after controlling for sex and race. Planned comparison post hoc tests were also examined for any significant ANOVA findings.
Table 1.
Demographic and Descriptive Data by Group
| General US (n = 1,000) |
Community ASD (n = 1,169) |
Inpatient ASD (n = 567) |
|
|---|---|---|---|
| Group | % (n) | % (n) | % (n) |
| Mean age (SD) | 12.05 (3.55) | 12.04 (3.19) | 12.77 (3.07) |
| Male | 50.6% (506) | 79.8% (933) | 78.7% (446) |
| Hispanic/Latino | 17.5% (175) | 9.3% (109) | 6.5% (37) |
| Race | |||
| White | 65.1% (651) | 91.5% (1070) | 85.4% (484) |
| Black | 14.5% (145) | 6.3% (74) | 10.2% (58) |
| Asian | 4.3% (43) | 2.0% (23) | 4.4% (25) |
| Native American | 3.8% (38) | 2.5% (29) | 2.3% (13) |
| Other | 2.2% (22) | 3.9% (46) | 1.8% (10) |
| Missing | 0.0% (0) | 0.4% (5) | 3.4% (19) |
| ID | 1.3% (13) | 54.0% (631) | 46.6% (264) |
| Minimally verbal | 3.4% (34) | 43.6% (510) | 47.4% (269) |
| History of previous psychiatric hospitalization | 4.9 (49) | 9.1 (106) | 46.9 (266) |
| Use of emergency services in past 2 months | 0.1 (1) | 6.1 (71) | 43.6 (247) |
| Current use of psychotropic medication; Yes/No | 5.9 (59) | 31.7 (371) | 83.8 (475)a |
| M (SD) | M (SD) | M (SD) | |
| EDI-Reactivity t-score | 38.00 (7.85) | 47.14 (8.46) | 58.75 (8.16) |
| EDI-Dysphoria t-score | 43.11 (7.80) | 48.27 (8.77) | 55.52 (8.41) |
| CBCL ADHD Problems t-score | 54.13 (6.38) | 62.65 (8.24) | 67.90 (7.66) |
Abbreviations: EDI, emotion dysregulation inventory; CBCL, child behavior checklist; ID, intellectual disability; SCQ, social communication questionnaire.
For the Inpatient ASD group, medication use was assessed at admission. EDI-Reactivity t-scores were converted from raw scores using the autism/clinical norms.
Figure 1.
Percentage of participants endorsing dichotomous outcome variables by group (all group differences P < 0.001).
Aim 3.
In order to investigate whether ER impairment is a predictor of psychiatric hospitalization, emergency services use, and medication use among those with ASD, we first performed receiver operating characteristics (ROC) analyses for each of the three service outcomes to explore the validity of ER impairment in predicting service use. Next, we completed logistic regressions in Community and Inpatient ASD groups separately where the presence or absence of services was used as dichotomous dependent variables. Covariates consisted of demographic factors (age, sex, race, and ID) entered at the first step, followed by parent- reported ADHD symptoms (CBCL ADHD Problems t-score) at step two, and ER impairment (EDI-Reactivity t-score) at the final step. Each regression was then re-run with the EDI-Dysphoria score at the final step.
Results
Aim 1: Prevalence of Inpatient, Emergency, and Medication Psychiatric Services
Reported history of psychiatric hospitalization (B = 5.89; P < 0.001), emergency service utilization in the prior 2 months (B = 17.59; P < 0.001), and psychotropic medication use (B = 10.08; P < 0.001) all significantly differed by group. When examining the percent of each sample that endorsed each service, the general US sample was lowest, followed by the Community and the Inpatient ASD groups, which had the highest level of each service surveyed (See Fig. 1).
Aim 2: Prevalence of ER Impairment
As shown in Figure 2, the Community ASD group had nearly four times more youth in the clinically elevated range for EDI Reactivity (EDI-R = 53.2% vs. 13.6%) and twice the number of youth in the clinical range for EDI Dysphoria than the general US sample (EDI-D = 32.1% vs. 15.1%). As expected, an even higher proportion of the ASD inpatient sample had clinically elevated scores on both measures (EDI-R = 92.9%; EDI-D = 71.3%). Accordingly, group average scores differed by about 1 SD on the EDI-R (General US Mean = 38.00, SD = 7.85; Community ASD Mean = 47.14, SD = 8.46; Inpatient ASD Mean = 58.75, SD = 8.16) and differed slightly less on the EDI-D (General US Mean = 43.11, SD = 7.80; Community ASD Mean = 48.27, SD = 8.77; Inpatient ASD Mean = 55.52, SD = 8.41). Of note, the Community ASD Mean was in the clinical range for Reactivity.
Figure 2.
EDI-reactivity and EDI-dysphoria scores by group (whether or not scores are above clinical cut-offs is based on being one standard deviation above the general population mean).
EDI-R scores significantly differed between the three groups (F(2,2731) = 1082.43; P < 0.001). Neither sex nor race were significant covariates. Planned contrasts revealed that both ASD groups had significantly higher EDI-R scores (t(2483.93) = 37.46; P < 0.001) than the General US group, and that the Inpatient ASD group scores were significantly higher than the Community ASD group (t(1734) = 27.13; P < 0.001). Similarly, EDI-D significantly differed between the groups (F(2,2731) = 379.23; P < 0.001), with neither sex nor race as significant covariates. Planned contrasts indicated that the ASD groups combined scored higher on EDI-D scores than the General US group (t(2382.84) = 22.64; P < 0.001), and that Inpatient ASD group scores were significantly higher than the Community ASD group (t(1734) = 16.37; P < 0.001).
Aim 3: Association between ER Impairment and Service Use in ASD
We conducted ROC analyses with the ASD samples using the EDI-R and EDI-D as predictors of psychiatric hospitalization, using emergency services, and psychotropic medication use. The area under the curve (AUC) analyses for using emergency services in the past 2 months were significant (EDI-R AUC = 0.80, 95%CI = 0.77–0.82; EDI-D AUC = 0.69, CI = 0.66–0.72), as were AUCs for a history of inpatient psychiatric hospitalizations (EDI-R AUC = 0.75, CI = 0.72–0.78; EDI-D AUC = 0.68, CI = 0.65–0.71) and psychotropic medication use (EDI-R AUC = 0.72, CI = 0.70–0.75; EDI-D AUC = 0.65, CI = 0.62–0.68).
Prior Psychiatric Hospitalizations
In the Community ASD group, the likelihood of having been psychiatrically hospitalized was significantly associated with older age, being White, having ID, and higher EDI-R scores (See Table 2). With the Inpatient ASD group, only older age and having ID were associated with prior hospitalization.
Table 2.
Regressions of Group Status on Outcomes Using EDI-Reactivity
| Community ASD (n = 1,152) |
Inpatient ASD (n = 323) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Prior psychiatric hospitalization | B | Wald | Stand. beta | 95% CI | B | Wald | Stand. beta | 95% CI |
| Age | 0.31 | 57.08*** | 1.36 | 1.26–1.47 | 0.18 | 19.58*** | 1.20 | 1.11–1.29 |
| Sex | −0.03 | 0.01 | 0.97 | 0.58–1.63 | 0.20 | 0.45 | 1.22 | 0.69–2.16 |
| Race | 0.85 | 6.17* | 2.34 | 1.20–4.58 | 0.07 | 0.03 | 1.07 | 0.48–2.36 |
| ID | 0.67 | 8.76** | 1.95 | 1.25–3.04 | 0.67 | 7.22** | 1.95 | 1.20–3.18 |
| CBCL ADHD Problems t-score | 0.02 | 1.63 | 1.02 | 0.99–1.05 | 0.03 | 2.19 | 1.03 | 0.99–1.06 |
| EDI-reactivity t-score | 0.09 | 35.94*** | 1.09 | 1.06–1.12 | 0.01 | 0.93 | 1.01 | 0.99–1.04 |
| Emergency services use | (n = 1,142) | (n = 279) | ||||||
| Age | 0.12 | 8.54** | 1.13 | 1.04–1.23 | 0.11 | 6.73** | 1.12 | 1.03–1.21 |
| Sex | 0.55 | 2.40 | 1.73 | 0.87–3.46 | 0.12 | 0.16 | 1.13 | 0.62–2.05 |
| Race | 1.25 | 12.42*** | 3.49 | 1.74–7.00 | 0.45 | 1.00 | 1.57 | 0.65–3.81 |
| ID | −0.17 | 0.37 | 0.85 | 0.50–1.44 | 0.56 | 4.68* | 1.74 | 1.05–2.89 |
| CBCL ADHD Problems t-score | 0.01 | 0.13 | 1.01 | 0.97–1.04 | 0.02 | 0.98 | 1.02 | 0.98–1.06 |
| EDI-Reactivity t-score | 0.11 | 44.69*** | 1.12 | 1.08–1.16 | 0.42 | 6.37** | 1.04 | 1.01–1.08 |
| Psychotropic medication use (Current) | (n = 1,154) | (n = 323) | ||||||
| Age | 0.13 | 35.88*** | 1.14 | 1.09–1.19 | 0.16 | 9.79** | 1.17 | 1.06–1.30 |
| Sex | 0.19 | 1.26 | 1.20 | 0.87–1.66 | 0.34 | 0.85 | 1.40 | 0.68–2.89 |
| Race | −0.10 | 0.16 | 0.91 | 0.57–1.46 | 0.39 | 0.56 | 1.48 | 0.53–4.11 |
| ID | −0.18 | 1.89 | 0.83 | 0.64–0.88 | 0.42 | 1.74 | 1.52 | 0.82–2.81 |
| CBCL ADHD Problems t-score | 0.04 | 18.40*** | 1.04 | 1.02–1.06 | −0.01 | 0.04 | 1.00 | 0.95–1.04 |
| EDI-Reactivity t-score | 0.03 | 10.63*** | 1.03 | 1.01–1.05 | 0.05 | 3.19** | 1.05 | 1.01–1.09 |
Abbreviations: EDI, emotion dysregulation inventory; CBCL, child behavior checklist; ID, intellectual disability.
P< 0.05
P< 0.01
P< 0.001.
When EDI-D was in the model instead of EDI-R, the same variables (with the addition of higher ADHD symptom scores) were associated with psychiatric hospitalizations in the community ASD sample (See Table 3). In the inpatient ASD sample, again only older age and having ID were associated with prior psychiatric hospitalization.
Table 3.
Regressions of Group Status on Outcomes Using EDI-Dysphoria
| Community ASD (n = 1,152) |
Inpatient ASD (n = 323) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Prior psychiatric hospitalization | B | Wald | Stand. beta | 95% CI | B | Wald | Stand. beta | 95% CI |
| Age | 0.26 | 42.96*** | 1.30 | 1.20–1.41 | 0.17 | 18.90*** | 1.19 | 1.10–1.29 |
| Sex | 0.04 | 0.03 | 1.04 | 0.62–1.75 | 0.19 | 0.41 | 1.21 | 0.68–2.14 |
| Race | 0.74 | 4.72* | 2.10 | 1.08–4.10 | 0.08 | 0.04 | 1.09 | 0.49–2.39 |
| ID | 0.46 | 4.49* | 1.59 | 1.04–2.45 | 0.65 | 6.91** | 1.92 | 1.18–3.11 |
| CBCL ADHD Problems t-score | 0.04 | 8.50** | 1.04 | 1.01–1.07 | 0.03 | 3.05 | 1.03 | 1.00–1.06 |
| EDI-Dysphoria t-score | 0.06 | 22.28*** | 1.06 | 1.03–1.08 | 0.01 | 0.09 | 1.00 | 0.98–1.03 |
| Emergency services use | (n = 1,142) | (n = 279) | ||||||
| Age | 0.07 | 2.87 | 1.07 | 0.99–1.17 | 0.10 | 5.25* | 1.10 | 1.01–1.19 |
| Sex | 0.60 | 2.98 | 1.83 | 0.92–3.63 | 0.14 | 0.21 | 1.15 | 0.64–2.08 |
| Race | 1.08 | 9.86** | 2.94 | 1.50–5.75 | 0.44 | 0.97 | 1.55 | 0.65–3.68 |
| ID | −0.39 | 2.12 | 0.68 | 0.41–1.14 | 0.51 | 4.12* | 1.67 | 1.02–2.74 |
| CBCL ADHD Problems t-score | 0.03 | 3.77 | 1.03 | 1.00–1.07 | 0.03 | 0.21 | 1.03 | 1.00–1.07 |
| EDI-Dysphoria t-score | 0.07 | 23.12*** | 1.07 | 1.04–1.10 | 0.01 | 0.21 | 1.01 | 0.98–1.04 |
| Psychotropic medication use (Current) | (n = 1,154) | (n = 323) | ||||||
| Age | 0.12 | 30.08*** | 1.13 | 1.08–1.18 | 0.14 | 7.81** | 1.15 | 1.04–1.27 |
| Sex | 0.19 | 1.29 | 1.21 | 0.87–1.66 | 0.33 | 0.78 | 1.38 | 0.67–2.85 |
| Race | −0.13 | 0.29 | 0.88 | 0.55–1.41 | 0.42 | 0.66 | 1.53 | 0.55–4.25 |
| ID | −0.22 | 2.69 | 0.81 | 0.62–1.04 | 0.41 | 1.69 | 1.51 | 0.81–2.79 |
| CBCL ADHD Problems t-score | 0.05 | 31.49*** | 1.05 | 1.03–1.07 | 0.01 | 0.03 | 1.01 | 0.96–1.05 |
| EDI-Dysphoria t-score | 0.01 | 1.09 | 1.01 | 0.99–1.02 | 0.04 | 4.16* | 1.04 | 1.01–1.08 |
Abbreviations: EDI, emotion dysregulation inventory; CBCL, child behavior checklist; ID, intellectual disability.
P< 0.05
P< 0.01
P< 0.001.
Emergency Services Use
When predicting factors associated with emergency services use in the past 2 months, older age, being White, and higher EDI-R scores were significantly associated with using emergency services in the community ASD sample. For the inpatient ASD sample, older age, having ID, and higher EDI-R scores were significantly associated with using emergency services in the last 2 months.
In the model with the EDI-D instead of EDI-R, being White and higher EDI-D scores were significantly associated with using emergency services in the past 2 months in the Community ASD group. In the Inpatient ASD group, the same factors (older age, having ID) were significantly associated with emergency service use; however, EDI-D was not a significant predictor.
Psychotropic Medication Use
Older age, higher ADHD symptom scores, and higher EDI-R scores were significantly associated with using psychotropic medication in the Community ASD group. In the Inpatient ASD group, only older age and higher EDI-R scores were associated with psychotropic medication use.
In the model with EDI-D instead of EDI-R, the same variables (older age, higher ADHD symptom scores) were significantly associated with medication use in the community ASD sample, except EDI-D was not a significant predictor. For the inpatient ASD sample, again, older age and higher EDI-D scores were associated with medication use.
Discussion
The purpose of the current study was to compare rates of ER impairment and use of psychiatric hospitalization, emergency services, and psychotropic medication use across three large samples, community and hospitalized youth with ASD and a general youth sample, as well as to assess whether ER impairment is associated with these outcomes in ASD. Results confirmed a significantly higher prevalence of ER impairment in the Community ASD group than a US Census-matched group, and a significantly higher prevalence of ER impairment in an Inpatient ASD sample than both the Community ASD and US Census-matched groups. This study is the first to compare the prevalence of ER impairment in large samples of youth with and without ASD and supports prior research suggesting that youth with ASD are more likely to have ER impairment. Strikingly, even a community-based sample of ASD youth had mean Reactivity scores in the clinical range, and was four times more likely to have clinically elevated levels of ER impairment as compared to general population youth. Youth with ASD who are in an inpatient psychiatric setting had the highest levels of ER impairment, which further supports the link between ER and the co-occurring behavioral problems and psychiatric conditions that are the chief complaint for inpatient psychiatric admissions [Righi et al., 2018; Siegel & Gabriels, 2014].
Furthermore, the three groups significantly differed in each psychiatric service area studied: psychotropic medication prescription, using behavioral emergency services in the past 2 months, and history of psychiatric hospitalizations. These findings are in accordance with prior research indicating higher psychiatric service utilization in youth with ASD than those without ASD [Kalb et al., 2012; Mandell, 2008; Righi et al., 2018; Turcotte et al., 2018]. Given the high cost of these services, it is important for research to continue to examine contributing factors for increased health-care services and interventions that can reduce reliance on such services. Similarly, both ASD groups were significantly more likely to utilize psychotropic medications, in line with previous research suggesting a high rate of psychotropic medication use in youth with ASD [King et al., 2020].
ER impairment was also significantly associated with prior psychiatric hospitalization, use of emergency services, and psychotropic medication prescription in both the Community and Inpatient ASD groups. These associations were significant even when accounting for demographic factors, ID diagnosis, and ADHD symptoms. This association between ER impairment and psychiatric service use adds to the burgeoning literature tying ER impairment to psychiatric symptoms, problem behaviors, and poor outcomes in youth with ASD [Cai et al., 2018; Samson, Hardan, et al., 2015]. It will be important for future research to consider how improving ER impairment could produce downstream effects in reducing psychiatric service use.
The results predicting psychiatric services in youth with ASD from the EDI-R vs. EDI-D were predominantly the same. Reactivity, as measured by the EDI, captures core aspects of ER impairment, including a propensity for strong negative emotion that escalates rapidly and is poorly downregulated. Dysphoria, on the other hand, is a more specific manifestation of ER impairment that captures poorly upregulated positive affect and general unease. While the need to focus on emotion dysregulation in ASD has become more broadly acknowledged, up-regulation of positive emotions has received much less attention [Cai, Richdale, Dissanayake, Trollor, & Uljarević, 2019].
There were two differences in findings between EDI-R and EDI-D in their association with use of services. First, EDI-D was not predictive of emergency services use in the past 2 months for the Inpatient ASD group, whereas it was for the Community ASD group. The most likely explanation for this is the high severity of Reactivity in the hospitalized youth. It seems plausible that within the 2 months before hospitalization, behavioral, and emotional reactivity symptoms may overshadow more internalizing manifestations of ER impairment, particularly given that the specialized units from which participants were recruited predominantly admit youth for primary complaints related to overt behaviors such as aggression or self-injurious behaviors [Siegel & Gabriels, 2014]. Second, EDI-D was not a significant predictor of psychotropic medication prescription in the Community ASD group, although it was in the Inpatient ASD group. Interestingly, a line-item analysis of the outcome measure used in the trials leading to FDA-approval of atypical antipsychotics for irritability in ASD, the Aberrant Behavior Checklist, found the largest effect sizes for items that align with reactivity as opposed to items in the measure tapping behaviors such as self-injury and aggression [Aman et al., 2010]. Therefore, it may not be surprising that Reactivity is associated with a higher likelihood of psychotropic medication prescription in a community sample. On the other hand, there have been no trials with Dysphoria as an outcome measure in ASD, and there is a dearth of psychopharmacologic clinical trials with related constructs of depression and anxiety as outcomes [King et al., 2020], which may partially explain the lack of association between Dysphoria and medication prescription in the Community group. It may also be that Dysphoria is easier than Reactivity to overlook until severe enough to warrant emergency or inpatient services. The fact that Dysphoria was related to medication prescription in the Inpatient group may relate to the explicit focus on medication management in inpatient settings by specialty providers who are accustomed to working with youth with high reactivity. A previously published analysis of medication prescriptions in a subset of this inpatient sample reported rates of prescription (>90% on at least one medication) and polypharmacy (over half) that are much higher than seen in outpatient settings, in addition to a relatively high rate of antidepressant prescriptions in particular (nearly half on an anti-depressant at some point during the admission) [Wink et al., 2018]. In this context of high medication use, complex presentations, and specialty care, it is perhaps not surprising that Dysphoria was more likely to be associated with prescriptions.
Demographic factors were also significantly associated with inpatient psychiatric, emergency services, and psychotropic medication prescription. Older age was the most consistent demographic predictor across models, which corresponds with increases in psychopathology during adolescence in neurotypical populations [Merikangas, He, & Burstein, 2010]. Older age has also been consistently implicated in prior studies of risk factors for hospitalization in ASD [Mandell, 2008; Righi et al., 2018; Turcotte et al., 2018]. Further, psychotropic medications prescription in ASD has been previously shown to be more common among older youth and adolescents than younger children [Spencer et al., 2013]. This finding is also consistent with the idea of adolescence being a highrisk period for youth with ASD [Picci & Scherf, 2015] and emphasizes the importance of supporting emotional and behavioral health during this age range.
Although understanding sex differences was not a specific aim of this study, it was interesting that sex was not a significant covariate in group comparisons of emotion dysregulation and it also was not a significant predictor of any of the service utilization outcomes. Sex-based findings have been inconsistent across research on co-occurring psychiatric conditions in ASD [Rosen, Mazefsky, Vasa, & Lerner, 2018]. Some studies find no sex differences, while others report that females have higher internalizing symptoms and males have higher externalizing symptoms [Lai, Lombardo, Auyeung, Chakrabarti, & Baron-Cohen, 2015]. Importantly, both manifestations may relate to poor ER and very little research has looked at sex as it relates to ER in particular. One prior study reported higher EDI Reactivity scores in female inpatients with ASD as compared to male inpatients, but the effect size was small [Wieckowski, Luallin, Pan, Righi, & Gabriels, 2020]. Our findings are consistent with prior research on hospitalization and emergency service utilization in ASD that also did not identify sex as a significant predictor [Kalb et al., 2012; Mandell, 2008; Righi et al., 2018; Turcotte et al., 2018]. It should be noted that none of these studies, including ours, were specifically designed to test for sex differences. This may be important as studies aimed at understanding sex differences have reported relatively large differences between sexes, for example, a study of toddlers with ASD found that females were almost two times more likely to present with high psychopathology as compared to males [Nordahl et al., 2020]. Future studies with larger samples of females may be warranted to more conclusively determine the role of sex in emotion dysregulation and use of psychiatric services.
The significance of other covariates was more variable across models. First, interestingly, identifying as White was a significant predictor for using emergency services and inpatient hospitalizations, but only in the Community ASD group. No racial differences were seen in the Inpatient ASD group. These findings contrast with previous ASD research that found that having a minority racial background was a significant predictor for psychotropic medication prescription as well as for psychiatric hospitalizations and using emergency services [e.g., Mandell, 2008]. Our findings may need to be interpreted with caution given the relatively low number of minorities in the IAN sample. Second, having an ID diagnosis was significantly associated with a history of prior psychiatric hospitalization in both Community and Inpatient ASD samples and of emergency services in the Inpatient ASD group. In models with Dysphoria, it only remained significant in relation to hospitalization. Given that individuals with co-occurring ASD and ID may struggle to access psychiatric care [Siegel & Gabriels, 2014], perhaps psychotropic medication and inpatient hospitalizations are used more frequently as first-line interventions. Lastly, higher ADHD symptoms were not a significant predictor in any of the inpatient models. It may be that ADHD symptoms alone are less predictive in the context of complex case presentations. ADHD was a significant predictor of medication prescription in the Community ASD group, which might be expected given that ADHD medications are the most commonly prescribed medication class in ASD and stimulants have received relatively more research [King et al., 2020]. Otherwise, ADHD symptoms were a significant predictor of hospitalization in the model with Dysphoria, but not in the model with Reactivity. This suggests that Reactivity may be more predictive of hospitalization than ADHD symptoms, among community samples.
Limitations
This study has several limitations. All samples used parent-reported data. Self-report of symptoms, particularly ER impairment, would be helpful to better understand individuals’ own perceptions of emotional experiences, though self-report in the more severely affected ASD population is a major challenge. Further, health records or other confirmation of service utilization was not available. This concern is offset somewhat by the use of dichotomous measures (e.g., a parent may not accurately recall the number of hospitalizations but is likely to accurately recall whether their child was ever hospitalized). Future research with verified medical record or insurance utilization information may help provide an even richer understanding of the relationship between the intensity and frequency of service utilization and ER impairment. While inclusion of an inpatient ASD sample provides access to a wider range of ER impairment, collection of data during an inpatient stay for acute crisis (as opposed to the online, self-selecting samples for Community ASD and General US) likely increases the chances of high levels of ER impairment. Due to the secondary nature of these data, no consistent measure of ASD symptomatology was available in all three subgroups. Given that prior research has suggested that increased ASD symptom severity may be associated with increased ER impairment [Berkovits et al., 2017; Samson, Hardan, et al., 2015], it is important that future research include measures of ASD symptom severity. For example, it is possible that the Inpatient ASD participants have higher average ASD symptom severity than the Community ASD group, contributing to ER impairment differences. Additionally, future research with comparison of psychiatric, non-ASD samples is needed to understand how the degree of ER impairment in autism compares to other clinical groups, as well as if there is any differential impact on its association with service utilization. It is important to note that this study was cross-sectional, so longitudinal research is needed to provide an understanding of causality. Finally, the parents who participated in the IAN-derived data are a self-selected research sample and thus like any other research study, do not represent all parents of youth with ASD.
Conclusions and Clinical Implications
In conclusion, this study contributes to the growing evidence suggesting that ER impairment is an important variable related to functional outcomes in ASD. ER impairment has been previously associated with a range of co-occurring psychiatric symptoms and problem behaviors in ASD [Cai et al., 2018] and is thought to contribute to functional impairments, social outcomes, academic success, and employment [Mazefsky et al., 2013]. Given that prior research results have been inconsistent as to which co-occurring psychiatric disorders contribute to outcomes like hospitalization, focusing on a transdiagnostic process like ER impairment may be more fruitful.
Importantly, both Reactivity and Dysphoria were significantly related to the use of psychiatric hospitalization and the emergency services, and Dysphoria has also been associated with increased likelihood of suicidal ideation in a prior ASD study [Conner et al., 2020]. Overall, this emphasizes the importance of screening for both manifestations of ER impairment, as well as a continued need for clinical trials addressing Dysphoria in ASD. The high frequency of emergency service use (43.6%) in the prior 2 months in the Inpatient ASD group also indicates that recent use of emergency services and prior inpatient hospitalizations may serve as key indicators for the need to increase supports for an individual and potentially reduce inpatient admissions.
Future research that focuses on longitudinal methodologies to determine the systemic and mechanistic influence of ER impairment on outcomes is needed. This study focused on school-aged youth, but it will also be important for future research to include studies on ER impairment in early childhood in order to fully understand trajectories as well as opportunities for prevention efforts. Similarly, understanding how ER impairment manifests in adults with ASD and its association with services is needed, particularly given relatively less well-developed service delivery options for adults, and findings that older age increased risk for service utilization. Overall, there is great potential for a focus on ER in ASD across the lifespan to contribute to improved outcomes and quality of life.
Acknowledgments
This study was supported with funding from NICHD (R01 HD079512; C.M.), the Ritvo-Slifka Award for Innovation in Autism Research (C.M.), and the Simons Foundation Autism Research Initiative and the Nancy Lurie Marks Family Foundation (M.S.). IAN is a partnership project of the Kennedy Krieger Institute and the Simons Foundation. IAN is also partially funded through a Patient-Centered Outcomes Research Institute (PCORI) Award for development of the National Patient-Centered Clinical Research Network, known as PCORnet. Subjects were recruited and data obtained in partnership with the Interactive Autism Network (IAN) Research Database at the Kennedy Krieger Institute, Baltimore, MD. IAN collaborating investigators and staff included: Paul H. Lipkin, MD, J. Kiely Law, MD, MPH, and Alison R. Marvin, PhD. Data were also collected in partnership with the Autism and Developmental Disorders Inpatient Research Collaborative (ADDIRC) through use of Autism Inpatient Collection (AIC) data and YouGov. The ADDIRC is made up of the co-investigators: Matthew Siegel, MD (PI) (Maine Medical Center Research Institute; Tufts University), Craig Erickson, MD (Cincinnati Children’s Hospital; University of Cincinnati), Robin L. Gabriels,PsyD (Children’s Hospital Colorado; University of Colorado), Desmond Kaplan, MD and Rajeesh Mahajan, MD (Sheppard Pratt Health System), Carla Mazefsky, PhD (UPMC Western Psychiatric Hospital; University of Pittsburgh), Eric M. Morrow, MD, PhD (Bradley Hospital; Brown University), Giulia Righi, PhD (Bradley Hospital; Brown University), Susan L Santangelo, ScD (Maine Medical Center Research Institute; Tufts University), and Logan Wink, MD (Cincinnati Children’s Hospital; University of Cincinnati). Collaborating investigators and staff: Jill Benevides, BS, Carol Beresford,MD, Carrie Best, MPH, Katie Bowen, LCSW, Catalina Cumpanasoiu, BS, Briar Dechant, BS, Tom Flis, BCBA, LCPC, Holly Gastgeb, PhD, Angela Geer, BS, Louis Hagopian, PhD, Benjamin Handen, PhD, BCBA-D, Adam Klever, BS, Martin Lubetsky, MD, Kristen MacKenzie, BS, Zenoa Meservy, MD, John McGonigle, PhD, Kelly McGuire, MD, Faith McNeil, BS, Joshua Montrenes, BS, Tamara Palka, MD, Ernest Pedapati, MD, Kahsi A. Pedersen, PhD, Christine Peura, BA, Joseph Pierri, MD, Christie Rogers, MS, CCCSLP, Brad Rossman, MA, Jennifer Ruberg, LISW, Elise Sannar, MD, Cathleen Small, PhD, Nicole Stuckey, MSN, RN, Barbara Tylenda, PhD, Brittany Troen, MA, RDMT, Mary Verdi, MA, Jessica Vezzoli, BS, and Deanna Williams, BA. The authors thank the study staff for the time and energy they dedicated to this work. Special thanks also to the AIC research participants and their families that made this research possible.
Abbreviations
- ER
Emotion Regulation
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Pittsburgh Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study. Emotion Dysregulation is Substantially Elevated in Autism Compared to the General Population: Impact on Psychiatric Services.
Data from one of the samples were presented as a poster at the 2017 University of Pittsburgh Department of Psychiatry Annual Research Day. A portion of this project was accepted for presentation at the 2020 International Society of Autism Research Annual Conference.
Contributor Information
Caitlin M. Conner, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA.
Josh Golt, University of Alabama, Tuscaloosa, Alabama, USA.
Rebecca Shaffer, Cincinnati Children’s Hospital, Cincinnati, Ohio, USA; Department of Pediatrics, University of Cincinnati School of Medicine, Cincinnati, Ohio, USA.
Giulia Righi, Brown University, Providence, Rhode Island, USA.
Matthew Siegel, Maine Medical Center, Maine, USA; Tufts University School of Medicine, Boston, Massachusetts, USA.
Carla A. Mazefsky, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA.
References
- Achenbach T, & Rescorla LA (2001). Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, and Families. [Google Scholar]
- Aman MG, Kasper W, Manos G, Mathew S, Marcus R, Owen R, & Mankoski R (2010). Line-item analysis of the aberrant behavior checklist: Results from two studies of aripiprazole in the treatment of irritability associated with autistic disorder. Journal of Child and Adolescent Psychopharmacology, 20(5), 415–422. 10.1089/cap.2009.0120 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition: DSM-5. Arlington, VA: American Psychiatric Association. [Google Scholar]
- Berkovits L, Eisenhower A, & Blacher J (2017). Emotion regulation in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 47(1), 68–79. 10.1007/s10803-016-2922-2 [DOI] [PubMed] [Google Scholar]
- Cai RY, Richdale A, Uljarevic M, Dissanayake C, & Samson AC (2018). Emotion regulation in autism spectrum disorder: Where we are and where we need to go. Autism Research, 11(7), 962–978. 10.1002/aur.1968 [DOI] [PubMed] [Google Scholar]
- Cai RY, Richdale AL, Dissanayake C, Trollor J, & Uljarević M (2019). Emotion regulation in autism: Reappraisal and suppression interactions. Autism, 23(3), 737–749. 10.1177/1362361318774558 [DOI] [PubMed] [Google Scholar]
- Charlton AS, Smith IC, Mazefsky CA, & White SW (2020). The role of emotion regulation on co-occurring psychopathology in emerging adults with ASD. Journal of Autism and Developmental Disorders, 50, 2585–2592. 10.1007/s10803-019-03983-5 [DOI] [PubMed] [Google Scholar]
- Chetcuti L, Uljarević M, & Hudry K (2019). Editorial Perspective: Furthering research on temperament in autism spectrum disorder. Journal of Child Psychology and Psychiatry, 60(2), 225–228. 10.1111/jcpp.12957. [DOI] [PubMed] [Google Scholar]
- Conner CM, Golt J, Righi G, Shaffer R, Siegel M, & Mazefsky CA (2020). A comparative study of suicidality and its association with emotion regulation impairment in large ASD and US census-matched samples. Journal of Autism and Developmental Disorders, 50, 3545–3560. 10.1007/s10803-020-04370-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsello C, Hus V, Pickles A, Risi S, Cook EH, Leventhal BL, & Lord C (2007). Between a ROC and a hard place: Decision making and making decisions about using the SCQ. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(9), 932–940. 10.1111/j.1469-7610.2007.01762.x [DOI] [PubMed] [Google Scholar]
- Croen LA, Najjar DV, Ray GT, Lotspeich L, & Bernal P (2006). A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics, 118(4), e1203–e1211. 10.1542/peds.2006-0127 [DOI] [PubMed] [Google Scholar]
- Daniels AM, Rosenberg RE, Anderson C, Law JK, Marvin AR, & Law PA (2012). Verification of parent-report of child autism spectrum disorder diagnosis to a web-based autism registry. Journal of Autism and Developmental Disorders, 42(2), 257–265. 10.1007/s10803-011-1236-7 [DOI] [PubMed] [Google Scholar]
- Gross JJ, & Thompson RA (2006). Emotion regulation: Conceptual foundations. In Gross JJ (Ed.), Handbook of emotion regulation (pp. 3–26). New York, NY: Guilford Press. [Google Scholar]
- Jahromi LB, Meek SE, & Ober-Reynolds S (2012). Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53(12), 1250–1258. 10.1111/j.1469-7610.2012.02560.x [DOI] [PubMed] [Google Scholar]
- Joshi G, Petty C, Wozniak J, Henin A, Fried R, Galdo M, … Biederman J (2010). The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders, 40(11), 1361–1370. 10.1007/s10803-010-0996-9 [DOI] [PubMed] [Google Scholar]
- Kalb LG, Stuart EA, Freedman B, Zablotsky B, & Vasa R (2012). Psychiatric-related emergency department visits among children with an autism spectrum disorder. Pediatric Emergency Care, 28(12), 1269–1276. 10.1097/PEC.0b013e3182767d96 [DOI] [PubMed] [Google Scholar]
- King BH, Rynkiewicz A, Janas-Kozik M, & Tyszkewicz-Nwafor M (2020). Medications to treat co-occurring psychiatric conditions in autism spectrum disorder. In White SW, Maddox BB, & Mazefsky CA (Eds.), The Oxford handbook of autism and co-occurring psychiatric conditions. New York, NY: Oxford University Press. [Google Scholar]
- Lai MC, Lombardo MV, Auyeung B, Chakrabarti B, & Baron-Cohen S (2015). Sex/gender differences and autism: Setting the scene for future research. Journal of the American Academy of Child and Adolescent Psychiatry, 54(1), 11–24. 10.1016/j.jaac.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Marvin AR, Watson T, Piggot J, Law JK, Law PA, … Nelson SF (2010). Accuracy of phenotyping of autistic children based on internet implemented parent report. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics, 153(6), 1119–1126. 10.1002/ajmg.b.31103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop SL (2012). Autism Diagnostic Observation Schedule-2. Los Angeles: Western Psychological Services. [Google Scholar]
- Mandell DS (2008). Psychiatric hospitalization among children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(6), 1059–1065. 10.1007/s10803-007-0481-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvin AR, Law PA, Law JK, Arthur RM, Mortenson EM, Abbacchi AM, & Constantino JN (2014). Non- verbal children with ASD (NV-ASD): Validating a registry and characterizing a population. Poster presented at 2014 International Meeting for Autism Research. [Google Scholar]
- Mazefsky CA, Day TN, Siegel M, White SW, Yu L, & Pilkonis PA (2018). Development of the Emotion Dysregulation Inventory: A PROMIS®ing Method for Creating Sensitive and Unbiased Questionnaires for Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48 (11), 3736–3746. 10.1007/s10803-016-2907-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, & White SW (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52(7), 679–688. 10.1016/j.jaac.2013.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Oswald DP, Day TN, Eack SM, Minshew NJ, & Lainhart JE (2012). ASD, a psychiatric disorder, or both? Psychiatric diagnoses in adolescents with high-functioning ASD. Journal of Clinical Child and Adolescent Psychology, 41(4), 516–523. 10.1080/15374416.2012.686102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Yu L, & Pilkonis PA (2020). Psychometric properties of the emotion dysregulation inventory in a nationally representative sample of youth. Journal of Clinical Child and Adolescent Psychology. 10.1080/15374416.2019.1703710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Yu L, White SW, Siegel M, & Pilkonis PA (2018). The emotion dysregulation inventory: Psychometric properties and Item Response Theory calibration in an autism spectrum disorder sample. Autism Research, 11(6), 928–941. 10.1002/aur.1947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K, He J, & Burstein M (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, … Houck PR (2009). The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry, 48(5), 484–500. 10.1097/CHI.0b013e31819c23d0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordahl CW, Iosif AM, Young GS, Hechtman A, Heath B, Lee JK, … Ozonoff S (2020). High psychopathology subgroup in young children with autism: Associations with biological sex and Amygdala volume. Journal of the American Academy of Child and Adolescent Psychiatry, 59(12), 1353–1363.e2. 10.1016/j.jaac.2019.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris M, & Lecavalier L (2010). Screening accuracy of level 2 autism spectrum disorder rating scales: A review of selected instruments. Autism, 14(4), 263–284. 10.1177/1362361309348071 [DOI] [PubMed] [Google Scholar]
- Picci G, & Scherf KS (2015). A Two-Hit Model of Autism: Adolescence as the Second Hit. Clinical Psychological Science, 3 (3), 349–371. 10.1177/2167702614540646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plesa Skwerer D, Joseph RM, Eggleston B, Meyer SR, & Tager-Flusberg H (2019). Prevalence and correlates of psychiatric symptoms in minimally verbal children and adolescents with ASD. Frontiers in Psychiatry, 10, 1–43. 10.3389/fpsyt.2019.00043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiersen AM, & Todd RD (2008). Co-occurrence of ADHD and autism spectrum disorders: Phenomenology and treatment. Expert Review of Neurotherapeutics, 8(4), 657–669. 10.1586/14737175.8.4.657 [DOI] [PubMed] [Google Scholar]
- Righi G, Benevides J, Mazefsky C, Siegel M, Sheinkopf SJ, Morrow EM, … Lubetsky M (2018). Predictors of inpatient psychiatric hospitalization for children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(11), 3647–3657. 10.1007/s10803-017-3154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen TE, Mazefsky CA, Vasa RA, & Lerner MD (2018). Co-occurring psychiatric conditions in autism spectrum disorder. International Review of Psychiatry, 30(1), 40–61. 10.1080/09540261.2018.1450229 [DOI] [PubMed] [Google Scholar]
- Rosenberg RE, Mandell DS, Farmer JE, Law JK, Marvin AR, & Law PA (2010). Psychotropic medication use among children with autism spectrum disorders enrolled in a national registry, 2007–2008. Journal of Autism and Developmental Disorders, 40(3), 342–351. 10.1007/s10803-009-0878-1 [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). The Social Communication Questionnaire. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Salazar F, Baird G, Chandler S, Tseng E, O’sullivan T, Howlin P, … Simonoff E (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2283–2294. 10.1007/s10803-015-2361-5 [DOI] [PubMed] [Google Scholar]
- Samson AC, Hardan AY, Lee IA, Phillips JM, & Gross JJ (2015). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders, 45(11), 3424–3432. 10.1007/s10803-015-2388-7 [DOI] [PubMed] [Google Scholar]
- Samson AC, Wells WM, Phillips JM, Hardan AY, & Gross JJ (2015). Emotion regulation in autism spectrum disorder: Evidence from parent interviews and children’s daily diaries. Journal of Child Psychology and Psychiatry, 56 (8), 903–913. 10.1111/jcpp.12370 [DOI] [PubMed] [Google Scholar]
- Siegel M, & Gabriels RL (2014). Psychiatric hospital treatment of children with autism and serious behavioral disturbance. Child and Adolescent Psychiatric Clinics of North America, 23(1), 125–142. 10.1016/j.chc.2013.07.004 [DOI] [PubMed] [Google Scholar]
- Siegel M, Smith KA, Mazefsky C, Gabriels RL, Erickson C, Kaplan D, … Santangelo SL (2015). The autism inpatient collection: Methods and preliminary sample description. Molecular Autism, 6(61), 1–10. 10.1186/s13229-015-0054-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer D, Marshall J, Post B, Kulakodlu M, Newschaffer C, Dennen T, … Jain A (2013). Psychotropic medication use and polypharmacy in children with autism spectrum disorders. Pediatrics, 132(5), 833–840. 10.1542/peds.2012-3774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratis EA, & Lecavalier L (2017). Predictors of parent–teacher agreement in youth with autism spectrum disorder and their typically developing siblings. Journal of Autism and Developmental Disorders, 47(8), 2575–2585. 10.1007/s10803-017-3173-6. [DOI] [PubMed] [Google Scholar]
- Turcotte P, Shea LL, & Mandell D (2018). School discipline, hospitalization, and police contact overlap among individuals with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(3), 883–891. 10.1007/s10803-017-3359-y [DOI] [PubMed] [Google Scholar]
- United States Census Bureau (2016). American Community Survey. Retrieved from https://www.census.gov/programssurveys/acs/news/data-releases.html?#
- Wieckowski AT, Luallin S, Pan Z, Righi G, & Gabriels RL (2020). Gender differences in emotion dysregulation in an autism inpatient psychiatric sample. Autism Research, 13, 1343–1348. 10.1002/aur.2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wink LK, Pedapati EV, Adams R, Erickson CA, Pedersen KA, Morrow EM, … Tager-Flusberg H (2018). Characterization of medication use in a multicenter sample of pediatric inpatients with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(11), 3711–3719. 10.1007/s10803-017-3153-x [DOI] [PubMed] [Google Scholar]
- Witwer AN, & Lecavalier L (2010). Validity of comorbid psychiatric disorders in youngsters with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 22(4), 367–380. 10.1007/s10882-010-9194-0 [DOI] [Google Scholar]