Abstract
Introduction: Health services research has demonstrated the association between patient satisfaction and treatment outcomes illustrating the importance of satisfaction in determining favorable treatment outcomes. Despite abundant evidence in the acute care setting, few researchers have explored these associations among patients receiving speech rehabilitation or therapeutic treatment particularly those receiving treatment through nontraditional delivery methods.
Objective: To examine the satisfaction with a community-based telepractice approach for treating aphasia among stroke survivors who reside in rural areas and assess potential correlations between satisfaction and patient outcomes.
Methods: In total, 22 adults with poststroke aphasia who resided in rural areas received comprehensive language-oriented treatment (LOT) for aphasia through community-based telepractice. Post-treatment satisfaction with the telepractice approach was assessed using the Client Satisfaction Questionnaire-8 (CSQ-8).
Results: After 12 sessions of LOT, Western Aphasia Battery-revised (WAB-R) aphasia quotients (AQs) improved on average 4.64 U. Mean scores on the CSQ-8 averaged 31.0/32.0, indicating a high level of satisfaction with the telepractice approach. In addition, each 1 U of improvement in patient satisfaction was associated with a 1.75 U increase in the WAB-R AQ.
Conclusions: Examination of post-treatment satisfaction indicated that satisfaction was highly predictive of effectiveness—a one-point increase in satisfaction was associated with a nearly two-point increase in WAB-R AQ. Results echo findings from acute care studies underscoring the importance of the patient experience in treatment efficacy.
Keywords: aphasia, speech–language pathology, telepractice, satisfaction
Background
In recent years, patient satisfaction has become increasingly important in health care. Not only is it an important outcome criterion, but it also provides a critical measure of health care quality.1 Satisfaction is a complex concept that relates to many factors, including lifestyle, past experiences, and future expectations, as well as individual values and those of society.2 Patient satisfaction may indicate the degree to which a patient feels they have received high-quality health care.3 It encompasses treatment itself as well as the treatment experience and delivery. Evidence suggests patient satisfaction and treatment outcomes are linked, thereby demonstrating overall patient satisfaction correlates with treatment outcomes.4,5
In the treatment of patients with chronic disease, Michie et al. found correlations between patient satisfaction, treatment compliance, and improvements in physical health.6 Similarly, Plewnia et al. noted a strong correlation in rehabilitation settings.7 Despite the evidence linking satisfaction to clinical outcomes, little is known about patient satisfaction among individuals receiving treatment for aphasia, a common communication disorder that occurs after stroke that results in significant communication difficulties. Persons with aphasia (PWA) experience problems with listening comprehension, verbal expression, reading, and writing, thereby limiting their communication interactions.8
PWA require substantial rehabilitation and there is an expansive literature related to aphasia rehabilitation and outcomes.9 However, few studies have examined PWA satisfaction with aphasia treatment. Tomkins et al. conducted a qualitative analysis of treatment satisfaction among 50 PWA receiving face-to-face treatment.10 They found seven factors that contributed to patient satisfaction, including (1) forming relationships; (2) manner and methods of service delivery; (3) information, communication, and knowledge; (4) structure and relevance of therapy; (5) organizational management; (6) individual support; and (7) positivity and improvement. In addition, PWA determined their level of satisfaction based on what information was provided, how much information was provided, how the information was provided, and their ability to engage in the communication exchange. Ultimately, the authors concluded that measures of satisfaction with aphasia treatment were influenced by both tangible factors and personal values.10
Although the use of rehabilitation to treat aphasia is a widely accepted practice, the use of telepractice approaches and other alternative delivery methods was unique in the United States until the onset of the novel coronavirus in 2019 (COVID-19). The American Speech-Language-Hearing Association (ASHA) defines “telepractice” as “the application of telecommunications technology to the delivery of speech–language pathology and audiology professional services at a distance by linking clinician to client or clinician to clinician for assessment, intervention, and/or consultation.”11 ASHA designated the term “telepractice” rather than telemedicine or telehealth to minimize the misperception that such services are only utilized in health care settings.11 Consequently, with the emergence of telepractice approaches to aphasia treatment, there is a need to understand the impact of this shift in practice patterns from primarily face-to-face to telepractice approaches. The rapid spread of COVID-19 demanded a dramatic and urgent shift to the use of remote forms of treatment delivery for aphasia.12–14 Similarly, there was a need to understand the impact of this shift in practice on patient satisfaction.
Tousignant et al. previously examined patient satisfaction after telepractice for poststroke aphasia using a sample of 20 patients receiving 3 weeks of telepractice treatment in Canada.15 They measured satisfaction with a French adaptation of the Telemedicine Satisfaction Questionnaire after the completion of a pragmatic approach to aphasia treatment. They showed that patients with poststroke aphasia receiving speech teletherapy were very satisfied with this service delivery method.
A second study by Pitt and colleagues completed in Australia also found high patient satisfaction after a group-based 2-week intensive constraint-induced language therapy delivered through web-based videoconferencing program.16 Finally, aphasia telepractice studies by Choi et al. in South Korea17 and by Fink et al.18 in the United States both included measures of satisfaction but did not focus on satisfaction as a primary determinant nor include a standardized measure of satisfaction. To date, studies in the United States have not specifically emphasized satisfaction with telepractice approaches for treating aphasia.
This study was designed to examine the relationship between patient satisfaction and treatment outcomes after comprehensive treatment (addressing verbal expression and auditory comprehension) for aphasia using a community-based sample of PWA receiving treatment through a telepractice approach. We were interested in understanding patient satisfaction with a community-based telepractice approach for treating aphasia among stroke survivors who reside in rural areas and assess potential correlations between satisfaction and patient outcomes. Community-based treatment allows clients to receive treatment close to their homes from providers that may not be available in their local communities.
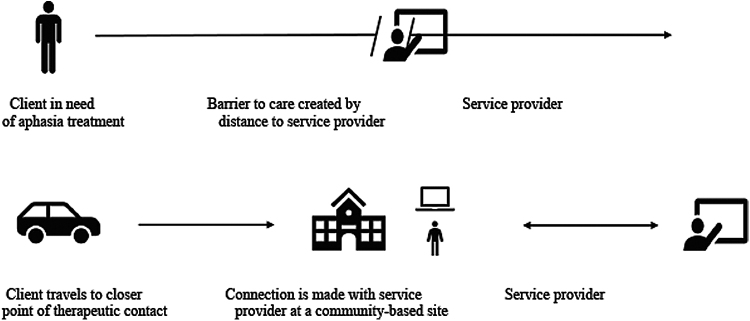
Increased accessibility of care increases the likelihood that the estimated 2.2–2.5 million PWA living in the United States will receive the needed treatment for the condition.19 Thus, access to care is improved without extraneous travel requirement or contact with individuals outside of one's own local area.20 For PWA living in rural areas specifically, such an approach can improve access to care by (1) reducing drive time to the point of therapeutic contact that is typically in more urban areas and (2) increasing the likelihood of service provision (Fig. 1).
FIG. 1.
Point of therapeutic contact improved through utilization of telepractice at a community-based site.
Finally, it is also possible that community-based telepractice approaches for PWA offer greater opportunities for community reintegration that are frequently absent among PWA.21–23 Therefore, the objective of the study was to examine the satisfaction with a community-based telepractice approach for treating aphasia among stroke survivors who reside in rural areas and assess potential correlations between satisfaction and patient outcomes.
Methods
Study participants
Twenty-two PWA were enrolled in the study. The study inclusion criteria included (1) communication skills necessary to complete telepractice sessions, (2) ability to answer 70% of yes/no questions on the Western Aphasia Battery-revised (WAB-R),24 and (3) at least 18 years of age. The WAB-R yes/no questions provided the key metric for inclusion in the study. Inclusion criteria based on the WAB-R AQ would have excluded individuals with significant expressive language and motor speech deficits who would have the comprehension skills to engage in the treatment approach.25 Individuals who scored >93.8 on the WAB-R AQ (cutoff score for aphasia) were included in the study if they (1) had a previously confirmed diagnosis of aphasia and (2) reported persisting word retrieval issues.26 Exclusion criteria included (1) participants who had dementia, a progressive neurological or cognitive disorder or a severe communication disorder that would prevent participation and (2) participants who were unable to drive or have a family member or caregiver who was willing to participate in the study to ensure transportation to the community-based site. Participants also had to agree to at least 6 weeks of treatment, two times per week.
Recruitment
All potential participants resided in rural counties in eastern North Carolina, defined as population density <80 people per square mile.27 Participants were recruited locally from local inpatient and outpatient clinics at a local hospital, Veterans Administration health care clinic, and community senior centers. Speech–language pathologists at the aforementioned clinics were notified at the onset of the study, and periodically, about the goals and objectives of the study. The participants treating (and referring) clinician provided them with information about the study, as outlined in the institutional review board (IRB) approval. Potential participants then contacted the study's principal investigator and scheduled a face-to-face meeting at the last author's (C.E.) laboratory to evaluate their ability to meet inclusion criteria and enroll in the study. Language evaluations for inclusion were completed by C.E. or graduate students supervised by C.E. Those who met inclusion criteria provided written consent and scheduled their first appointment at the designated community location.
Telepractice platform
The aphasia rehabilitation treatment was delivered by Lenovo T570 ThinkPad laptop computers with 15″ monitors through Webex™, a cloud-based videoconferencing program that allows real-time exchange of video and audio for individuals at a distant location through a secure internet connection. Webex offers both full screen and side-by-side sharing views, which allowed the research team and patient collaborative sharing of treatment materials and other documents required for the administration of the aphasia treatment. The treating clinician for the project provided the aphasia telepractice from a medical campus aphasia laboratory site, and the PWA received the treatment at a remote community-based site (local school or senior center). Student facilitators (undergraduate and graduate students enrolled in a Communication Sciences and Disorders program) were available at the remote treatment site to set up the equipment and assist the participants.
Aphasia treatment details
Participants were scheduled to complete 12 treatment sessions for a 6-week period. The provider, a certified speech–language pathologist, had ∼30 years' experience. Participants received their telepractice during individual sessions in a quiet room with the student facilitators present. Some caregivers were also present during the session but did not participate. The general aphasia treatment used through telepractice was the language-oriented treatment (LOT).28,29 The LOT was designed to address a range of language issues among PWA. The LOT approach is highly structured that is advantageous for measuring fidelity and replication. Treatment targets for comprehension included improving access to word meanings and changing the individual's communication environment to support auditory comprehension. Targets for expression included spoken output with written letters, repetition, and reading aloud. Whereas LOT facilitated the general approach to treatment, participants required individualized programs to address aphasia-related deficits.
Consequently, the team utilized a range of evidence-based treatments designed to improve overall communication including semantic feature analysis,30 verb network strengthening treatment,31 and combined aphasia and apraxia of speech treatment.32 Similarly, PWA frequently have coexisting motor speech production disorders (apraxia and dysarthria). For those individuals, we addressed those deficits using the Mayo Clinic approach for treatment of motor speech disorders that is a systematic treatment approach.33
Outcome measures
Aphasia impairment was measured pre- and post-treatment using the WAB-R AQ. Impairment change scores were calculated based on pre- and post-treatment WAB-R AQs.24 Treatment satisfaction was assessed using the eight-item Client Satisfaction Questionnaire (CSQ-8).34 All eight questions assign numeric scores ranging from 1 (low satisfaction) to 4 (high satisfaction) with a cumulative score of 32.
Statistical analysis
Descriptive statistics were calculated for all demographic characteristics and treatment outcomes using R version 3.6.4. The association between treatment effectiveness and satisfaction was assessed using Bayesian random effects models. Bayesian analytics allow prior information to be incorporated into covariate specific probability distributions. It also allows for the estimation of a large number of random variance components without the large data requirements needed for frequentists methods.
Results
Sample demographics
The mean age of the sample was 61 (standard deviation [SD] 14.2) years and a mean education of 14.0 (SD 2.3) years (Table 1). The sample was on average 42.5 months (SD 15.5) poststroke onset with participants ranging from 1 to 288 months postonset.
Table 1.
Patient Demographic and Outcomes Data for Telepractice Study
| Mean (SD) | Median | Range | |
|---|---|---|---|
| Pretreatment | |||
| Age (years) | 61.0 (14.2) | 64.5 | 33–96 |
| Education (years) | 14.0 (2.3) | 2.39 | 9–20 |
| Time poststroke onset (months) | 42.5 (15.5) | 15.5 | 1–288 |
| WAB-AQ initial | 73.9 (23.4) | 83.7 | 26.2–99.0 |
| Posttreatment | |||
| WAB AQ change | 4.64 (6.53) | 4.15 | −8.1 to 14.5 |
| CSQ-8 satisfaction score | 31.0 (1.4) | 32.0 | 28–32 |
AQ, aphasia quotient; CSQ-8, Client Satisfaction Questionnaire-8; SD, standard deviation; WAB, Western Aphasia Battery.
Aphasia impairment
Baseline WAB-R AQ was 74.9 (SD 23.4) (Table 2). WAB-R AQ scores increased on average 4.64 points. Change scores ranged from −8.1 to 14.5.
Table 2.
Bayesian Mixed Effects Estimation Results
| Estimate | Estimated error | 95% CI lower | 95% CI upper | |
|---|---|---|---|---|
| Intercept | −47.4 | 40.75 | −129.74 | 30.9 |
| CSQ-8 | 1.8 | 1.38 | −0.97 | 4.6 |
| TPO months | −0.02 | 0.04 | −0.11 | 0.05 |
| Age | −0.1 | 0.13 | −0.36 | 0.17 |
| African American | 1.42 | 3.84 | −5.84 | 9.37 |
| Broca's aphasia | 4.03 | 4.25 | −4.04 | 12.46 |
| Conduction aphasia | 8.48 | 5.3 | −2.72 | 18.85 |
| Estimate | Estimated error | Quant. 1 | Quant.3 | |
|---|---|---|---|---|
|
R2 |
0.41 |
0.08 |
0.19 |
0.56 |
| Reference category: anomia | ||||
| Dependent variable: ΔWAB-R AQ = WAB-R AQ final−WAB-R AQ initial | ||||
CI, confidence interval; TPO, time postonset; WAB-R, WAB-revised.
Satisfaction
Scores on the CSQ-8, for the 22 participants who completed the study, averaged 31.0 (SD 1.4) out of a maximum score of 32. Participant scores ranged from 28 to 32. Scores on the CSQ-8 indicated a high level of satisfaction with the telepractice treatment approach.
Patient satisfaction as a function of aphasia impairment
Each 1 U of improvement in patient satisfaction was associated with a 1.75 (standard error [SE] = 1.26) U increase in the WAB-R AQ. This increase was substantially larger than the change in WAB-R AQ observed from age (−0.14, SE = 0.13), race (0.77, SE = 3.67), or months postonset (−0.03, SE = 0.05). Type-specific fixed effects and individual-specific intercepts accounted for condition and individual-specific variations in effectiveness. Therefore, the effect of satisfaction is observed even after accounting for variation by type of aphasia.
Discussion
This study examined patient satisfaction in community-based telepractice treatment for aphasia and tested the relationship between patient satisfaction with community-based aphasia treatment and treatment outcomes. The findings of this study are significant on two levels. First, evidence suggests that ∼20% of stroke survivors experience aphasia.35 Telepractice provides an additional mechanism to treat this growing population particularly when traditional face-to-face treatments may not be feasible. Second, the recent COVID-19 pandemic forced many providers to abruptly transition to remote treatment and this study offers practitioners clear evidence about the efficacy, feasibility, and satisfaction of aphasia treatment telepractice and in particular to address the treatment needs of rural residents.
PWA CSQ-8 scores ranged from 28 to 32 indicating high satisfaction with the telepractice approach. These findings align with those of Tousignant and colleagues who also noted high levels of patient satisfaction in a 3-week telepractice intervention for chronic aphasia.15 More importantly, this study showed that patient satisfaction was closely tied to clinical improvement—change in WAB-R AQ. Patients improved between 0.2 and 12.4 U with an average of 4.64 U. Typically, a five-point improvement on WAR-AQ is considered a clinically relevant change.36 Improvement directly corresponded with satisfaction such that for each one-point increase in satisfaction, aphasia impairment improved by nearly two points.
The improved clinical outcomes in relationship with satisfaction are not entirely a surprise. Previous studies have shown that telepractice approaches can improve a range of skills after aphasia, including naming, fluency, and auditory comprehension while reducing overall level of aphasia impairment.17,37 Studies also indicate that a range of different telepractice approaches can be successful in improving aphasia outcomes such computer/tablet-based and in-home telepractice.38–42 More importantly, it is well established that telepractice approaches can have other positive outcomes beyond communication such as improved overall quality of life.43,44
Despite some participants' limited technological experience, the incorporation of technology did not hinder satisfaction with the approach. PWA expressed specific satisfaction with two treatment aspects. First, nearly all patients commented that seeing the therapist and stimuli simultaneously was advantageous compared with traditional face-to-face treatment requiring clients to look down at the stimuli, thus limiting their ability to view the therapist's feedback. Second, participants were highly satisfied with the sound and video quality of the computer connection. With regard to these aspects, PWA expressed higher satisfaction with telepractice than face-to-face speech–language pathology service treatments for aphasia. More importantly, the approach utilized in this study allowed individuals to receive treatment within their local areas.
Despite these interesting findings, there are some limitations. Many of the PWA were many years poststroke onset. Thus, it was unclear whether their satisfaction was primarily influenced by the novel telepractice approach or their ability to receive much needed services. In addition, the PWA in this study included a wide range of severity levels with large variation in functional ability. Given the presence of aphasia, responses to the outcome scales could have been subject to misunderstanding or misinterpretation. Similarly, the treatment was primarily provided by one therapist, thus creating the possibility of bias in the satisfaction reports. Finally, the scores achieved on the satisfaction scale were all high and within a few points, thus not allowing the investigators to determine any significant distinction between the participants. Despite these potential limitations, the data inarguably show high level of both communication ability and treatment satisfaction.
Conclusions
Using a community-based telepractice treatment for aphasia, this study tested the association between treatment outcomes and patient satisfaction—a hypothesis frequently proven in acute and primary care research. In addition to a significant improvement in fluency, patients were highly satisfied with treatment. Satisfaction level was highly predictive of treatment outcome, validating findings from other health care sectors. Results underscore the important role that patient experience plays in treatment efficacy. Future studies will be needed to a larger sample to further examine spread of the satisfaction measure scores. Future studies must also be designed to compare the satisfaction of telepractice for aphasia with in-person treatment for aphasia.
Abbreviations Used
- AQ
aphasia quotient
- ASHA
American Speech-Language-Hearing Association
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- CSQ-8
Client Satisfaction Questionnaire-8
- IRB
institutional review board
- LOT
language-oriented treatment
- PWA
persons with aphasia
- SD
standard deviation
- SE
standard error
- TPO
time postonset
- WAB
Western Aphasia Battery
- WAB-R
WAB-revised
Authors' Contributions
Each listed authors contributed to this study and has reviewed and agreed to the submission of the article to Telemedicine Reports.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was funded by the Agency for Healthcare Research and Quality, Grant No.: 1 R03 HS025043-01A1 awarded to C.E.
Cite this article as: Jacobs M, Briley PM, Fang X, Ellis C (2021) Telepractice treatment for aphasia: association between clinical outcomes and client satisfaction, Telemedicine Reports 2:1, 118–124, DOI: 10.1089/tmr.2020.0024.
References
- 1. Körner M. Patient-centered care through internal and external participation in medical rehabilitation. Health 2013;5:48–55 [Google Scholar]
- 2. Carr-Hill RA. The measurement of patient satisfaction. J Public Health 1992;14:236–249 [PubMed] [Google Scholar]
- 3. Locker D, Dunt D. Theoretical and methodological issues in sociological studies of consumer satisfaction with medical care. Soc Sci Med 1978;12:283–292 [PubMed] [Google Scholar]
- 4. Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual 2013;35:37–43 [DOI] [PubMed] [Google Scholar]
- 5. Carroll JG. Crossing the quality chasm: a new health system for the 21st century. Qual Manag Healthcare 2002;10:60–61 [Google Scholar]
- 6. Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: What is it and does it matter? Patient Educ Couns 2003;51:197–206 [DOI] [PubMed] [Google Scholar]
- 7. Plewnia A, Bengel J, Körner M. Patient-centeredness and its impact on patient satisfaction and treatment outcomes in medical rehabilitation. Patient Educ Couns 2016;99:2063–2070 [DOI] [PubMed] [Google Scholar]
- 8. American Speech-Language-Hearing Association, Adult Speech and Language. Aphasia. 2020. Available at www.asha.org/public/speech/disorders/Aphasia/ Accessed June10, 2020
- 9. Brady MC, Kelly H, Godwin J, et al. Speech and language therapy for aphasia following stroke. Cochrane Database of Syst Rev 2016:CD000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tomkins B, Siyambalapitiya S, Worrall L. What do people with aphasia think about their health care? Factors influencing satisfaction and dissatisfaction. Aphasiology 2013;27:972–991 [Google Scholar]
- 11. American Speech-Language-Hearing Association, Adult Speech and Language. Telepractice. 2020. Available at https://www.asha.org/Practice-Portal/Professional-Issues/Telepractice/ Accessed June10, 2020
- 12. Aggarwal K, Patel R, Ravi R. Uptake of telepractice among speech-language therapists following COVID-19 pandemic in India. Speech Lang Hear 2020;1–7: DOI: 10.1080/2050571X.2020.1812034 [DOI] [Google Scholar]
- 13. American Speech-Language-Hearing Association, Telepractice Resources During COVID-19. 2020. Available at https://www.asha.org/about/telepractice-resources-during-covid-19/ Accessed June10, 2020
- 14. Fong R, Tsai CF, Yiu OY. The implementation of telepractice in speech language pathology in Hong Kong during the COVID-19 pandemic. Telemed J E Health. 2020;27:30–38 [DOI] [PubMed] [Google Scholar]
- 15. Tousignant M, Macio, J, Martel-Sauvageu V, et al. Satisfaction with in-home speech telerehabilitation in chronic post-stroke aphasia: an exploratory analysis. J Int Soc Telemed E Health 2018;6:e11 [Google Scholar]
- 16. Pitt R, Theodoros D, Hill AJ, et al. The feasibility of delivering constraint-induced language therapy via the Internet. Digit Health 2017; DOI: 10.1177/2055207617718767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Choi YH, Park HK, Paik NJ. A telerehabilitation approach for chronic aphasia following stroke. Telemed E Health 2016;22:434–440 [DOI] [PubMed] [Google Scholar]
- 18. Fink R, Brecher A, Sobel P, et al. Computer-assisted treatment of word retrieval deficits in aphasia. Aphasiology 2005;19:943–954 [Google Scholar]
- 19. Simmons-Mackie N. Aphasia in North America. 2018. Available at https://www.aphasiaaccess.org/white-paper Accessed June10, 2020
- 20. Arcury TA, Gesler WM, Preisser JS, et al. The effects of geography and spatial behavior on health care utilization among residents of a rural region. Health Serv Res 2005;40:135–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee H, Lee Y, Choi H, et al. Community integration and quality of life in aphasia after stroke. Yonei Med J 2015;56:1694–1702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Manning M, McFarlane A, Hickey A, et al. Perspectives of people with aphasia post-stroke towards personal recovery and living successfully: a systematic review and thematic analysis. PLoS One 2019;14:e0214200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wray E, Clarke D. Longer-term needs of stroke survivors with communication difficulties living in the community: a systematic review and thematic analysis. BMJ Open 2017;7:e017944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kertesz A. The Western Aphasia Battery—Revised. Texas: Harcourt Assessments, 2007 [Google Scholar]
- 25. Ellis C, Peach RK, Rothermich K. Relative weight analysis of the Western Aphasia Battery. Aphasiology 2020; DOI: 10.1080/02687038.2020.1787947 [DOI] [Google Scholar]
- 26. Fromm D, Forbes M, Holland A, et al. Discourse characteristics in aphasia beyond the Western Aphasia Battery cutoff. Am J Speech Lang Pathol 2017;26:762–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. United States Census Bureau. Urban and Rural. 2020. Available at https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html Accessed June10, 2020
- 28. Bandur DL, Shewan CM. Language-oriented treatment: A psycholinguisticapproach to aphasia. In: Chapey R, ed. Language Intervention Strategies in Aphasia and Related Neurogenic Communication Disorders. Philadelphia: Lippincott, Williams & Wilkins, 2008; pp. 756–799 [Google Scholar]
- 29. Shewan CM, Bandur DL Treatment of Aphasia: A Language Oriented Approach. Austin, TX: Pro-Ed, 1986 [Google Scholar]
- 30. Efstratiadou EA, Papathanasiou I, Holland R, et al. A systematic review of semantic feature analysis therapy studies for aphasia. J Speech Lang Hear Res 2018;61:1261–1278 [DOI] [PubMed] [Google Scholar]
- 31. Edmonds LA, Babb M. Effect of verb network strengthening treatment in moderate-severe-aphasia. Am J Speech Lang Pathol 2011;20:131–145 [DOI] [PubMed] [Google Scholar]
- 32. Wambaugh JL, Wright S, Nessler C, et al. Combined aphasia and apraxia of speech treatment (CAAST): effects of a novel therapy. J Speech Lang Hear Res 2014;57:2191–2207 [DOI] [PubMed] [Google Scholar]
- 33. Duffy JR. Motor Speech Disorders: Substrates, Differential Diagnosis, and Management, 2nd ed. St. Louis, MO: Elsevier Mosby, 2005 [Google Scholar]
- 34. Attkisson CC, Greenfield TK. The UCSF client satisfaction scales i. The client satisfaction questionnaire-8. In: Maruish M, ed. The Use of Psychological Testing for Treatment Planning and Outcome Assessment. Mawah, NJ: Lawrence Erlbaum Associates, 2004 [Google Scholar]
- 35. Ellis C, Hardy RY, Lindrooth RC, et al. Rate of aphasia among stroke patients discharged from hospitals in the United States. Aphasiology 2017;32:1075–1086 [Google Scholar]
- 36. Katz RC, Wertz RT. The efficacy of computer-provided reading treatment for chronic aphasic adults. J Speech Lang Hear Res 1997;40:493–507 [DOI] [PubMed] [Google Scholar]
- 37. Dechene L, Tousignant M, Boissy P, et al. Simulated in-home teletreatment for anomia. International J Telerehabil 2011;3:3–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Agostini M, Garzon M, Benavides-Varela S, et al. Telerehabilitation in poststroke anomia. BioMed Res Int 2014;2014:706909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fridler N, Rosen K, Herzberg O, et al. Tele-rehabilitation vs face-to-face therapy for aphasic patients. eTelemedicine 2012;1–6 [Google Scholar]
- 40. Kurland J, Liu A, Stokes P. Effects of a tablet-based home practice program with telepractice on treatment outcomes in chronic aphasia. J Speech Lang Hear Res 2018;61:1140–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maresca G, Maggio MG, Latella D. et al. Toward improving post-stroke aphasia: a pilot study on the growing use of telerehabilitation for the continuity of care. J Stroke Cerebrovasc Dis 2019;28:104303. [DOI] [PubMed] [Google Scholar]
- 42. Woolf C, Caute A, Haigh Z, et al. A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: a quasi-randomised controlled feasibility study. Clin Rehabil 2015;30:359–373 [DOI] [PubMed] [Google Scholar]
- 43. Hill AJ, Miller LE. A survey of the clinical use of telehealth in speech-language pathology across Australia. J Clin Pract Speech Lang Pathol 2012;14:110–117 [Google Scholar]
- 44. Weidner K, Lowman J. Telepractice for adult speech-language pathology services: a systematic review. Perspect ASHA Spec Interest Groups 2020;5:326–338 [Google Scholar]