Abstract
Primary hyperparathyroidism has been associated with bone loss, especially at cortical skeletal sites. Results from studies evaluating the mineral density of cancellous bone have been more difficult to interpret. Most densitometry studies support the concept that the parathyroid hormone appears to be catabolic at cortical sites and may have anabolic effects at cancellous bone sites. Studies completed to date, however, have been limited by design, definitions of fracture and inadequate control groups. Primary hyperparathyroidism is now increasingly being detected during the asymptomatic phase. The need for parathyroidectomy has been questioned in such patients because there may be no disease progression in the absence of surgery. Medical management of primary hyperparathyroidism has to date been limited to estrogen replacement therapy in postmenopausal women. Identification of the calcium receptor has improved our understanding of calcium homeostasis, and significant reductions in calcium receptor levels have been detected in parathyroid adenomas. Thus, a new class of therapeutics may include the calcimimetic agents. Bisphosphonates are also currently being evaluated with regard to their impact on fracture prevention and their beneficial effects on bone mineral density.
Primary hyperparathyroidism was previously characterized by severe hypercalcemia, recurrent nephrolithiasis, osteoporosis and osteitis fibrosa cystica (cystic bone destruction).1 In the 1970s mild hypercalcemia became easily detectable with the introduction of the autoanalyser, and thus a 4-fold increase in the incidence of primary hyperparathyroidism was seen.2 Most people are asymptomatic at the time of diagnosis. Recently a decline in the incidence of primary hyperparathyroidism has been reported.3 With the limitation on screening that is now occurring in the United States and Canada, the incidence of primary hyperparathyroidism could decline further. Currently the prevalence rates are about 1 to 4 per 1000, with a female:male ratio ratio of 3:1.4 In Sweden about 3% of postmenopausal women are affected.5
This paper reviews the pathophysiology of primary hyperparathyroidism in the context of the current understanding of calcium homeostasis, the effect of primary hyperparathyroidism on bone mineral density, and advances in the clinical management of the disorder.
Pathophysiology
Parathyroid hormone (PTH) secretion is normally stimulated by a fall in the extracellular calcium concentration. PTH subsequently increases renal calcium reabsorption in the cortical thick ascending limb. It stimulates the hydroxylation of 25-hydroxy-vitamin D at the proximal convoluted tubule in the kidney and increases bone resorption through stimulation of osteoclast-activating factors such as interleukin-6 from osteoblasts.6 Through these actions PTH helps to restore any tendency to hypocalcemia (Fig. 1).
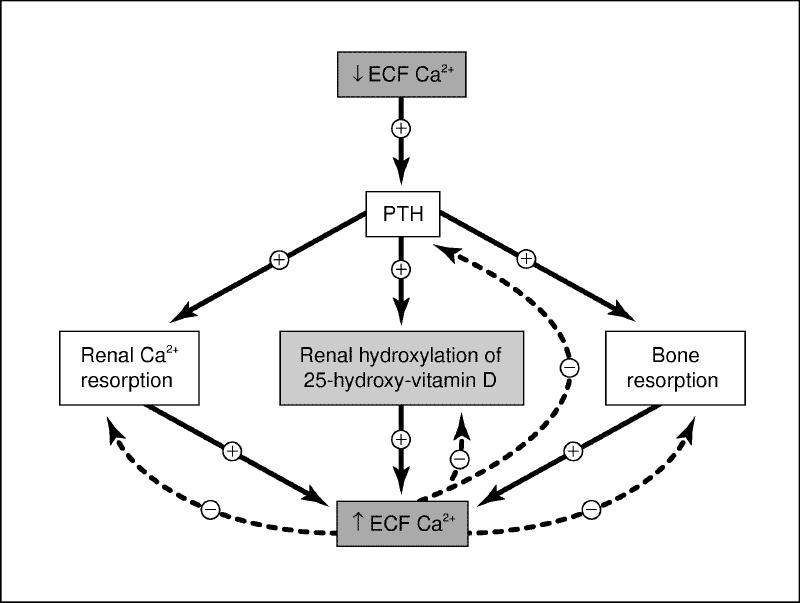
Fig. 1: Calcium homeostasis with regulation of serum calcium levels via feedback inhibition through the calcium receptor. ECF = extracellular, Ca = calcium, PTH = parathyroid hormone. Photo by: Christine Kenney
Current understanding of calcium homeostasis has been advanced by the discovery of the calcium receptor that allows calcium to act with PTH and 1,25-dihydroxy-vitamin D3 in maintaining calcium homeostasis.7 When extracellular calcium binds to the calcium receptor in the parathyroid cell, PTH secretion and parathyroid cell growth are inhibited (Fig. 2). At the kidney this interaction between calcium and the calcium receptor inhibits the 1-hydroxylation of 25-hydroxy-vitamin D. Calcium affects the thyroid C cells, stimulating calcitonin release, and in bone may potentially regulate bone resorption.8
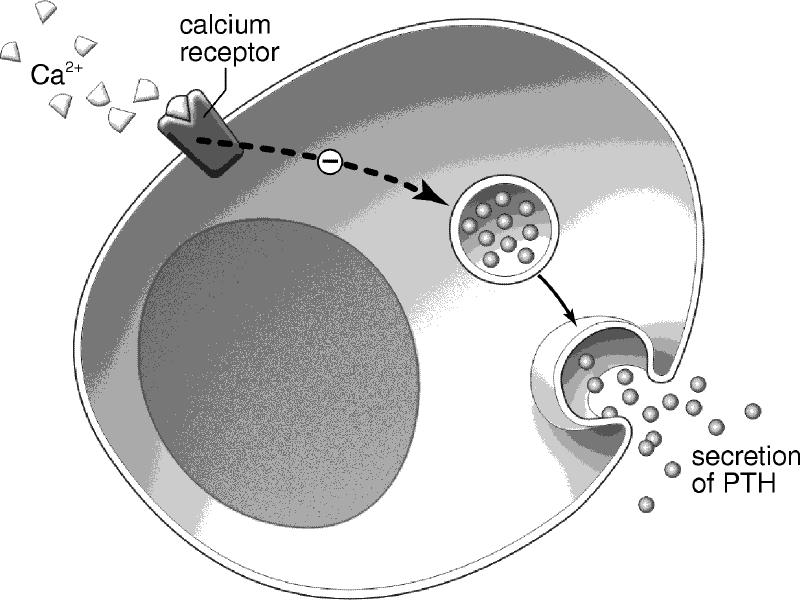
Fig. 2: Schematic illustration of calcium binding to the calcium receptor at the parathyroid cell and inhibiting PTH secretion. Photo by: Christine Kenney
The identification of 2 clinical conditions caused by mutations in the calcium receptor gene has confirmed the key role that the calcium receptor plays in calcium homeostasis.9,10 The first condition is familial hypocalciuric hypercalcemia. Heterozygous inactivating mutations of the calcium receptor result in mild hypercalcemia and hypocalciuria. A relative resistance leads to a higher set point required for inhibition of PTH secretion by calcium, as well as impaired urinary calcium excretion. The renal defect persists following total parathyroidectomy. Levels of PTH tend to be normal or only slightly elevated in this condition.9 The second condition is that of an autosomal dominant activating mutation of the calcium receptor.10 In this condition the calcium receptor is abnormally sensitive to calcium, leading to suppression of PTH secretion at hypocalcemic levels. This is a form of hypoparathyroidism. Relative hypercalciuria also occurs.
In primary hyperparathyroidism mutations of the calcium receptor gene have not been identified. However, significant reductions in calcium receptor mRNA levels have been detected in parathyroid adenomas.11 >The pathophysiological significance of this observation is unclear because the reductions could be secondary to the chronic hypercalcemia and not the primary cause.
Up to 10% of cases of primary hyperparathyroidism are hereditary. These hereditary forms are due usually to multiple endocrine neoplasia I (MEN I) or to MEN II. Familial primary hyperparathyroidism in the absence of other endocrine disease also occurs. It has been shown recently that as many as 25%-30% of people with sporadic primary hyperparathyroidism can have abnormalities in the gene responsible for MEN I.12,13,14
Effect on bone
Primary hyperparathyroidism is associated with a reduction in bone mineral density. Older cross-sectional studies used single photon absorptiometry to assess density at the forearm. More recent studies have used dual energy x-ray absorptiometry to quantify bone mineral density at 3 sites: the lumbar spine, the hip and the forearm. It appears that primary hyperparathyroidism is associated with bone loss largely at cortical sites.15,16,17
Data evaluating the density of cancellous bone are more difficult to interpret. Some studies have shown a modest decrease at cancellous bone sites.18,19,20,21 Other studies, however, indicate that bone density is relatively well preserved.17,22
The largest and longest study comes from Silverberg and colleagues,23 who demonstrated stable bone mineral density in the majority of people with primary hyperparathyroidism in the absence of surgical intervention. One hundred and twenty-one people with a mean age of 55 years were followed prospectively over 10 years. Bone mineral density was stable in the majority of the patients, although a subgroup of about 25% showed a decrease in bone mineral density. This subgroup consisted of women who had entered menopause without estrogen supplementation, those with advanced primary hyperparathyroidism and those whose parathyroidectomy had failed. These findings support the need to monitor patients with primary hyperparathyroidism who are not planning to undergo parathyroid surgery.
These studies have shown that there may be differing responses to elevated PTH levels, depending on the skeletal site. Thus, most densitometry studies support the concept that PTH appears to be catabolic at cortical sites and may in fact have anabolic effects at cancellous bone sites. In some patients, however, cancellous bone density of the lumbar spine can be substantially reduced.24
A number of retrospective and case-control studies have not shown an increase in fracture incidence among patients with primary hyperparathyroidism,25,26,27 >whereas others have.28,29,30 These studies are limited by their cross-sectional design, inadequate control groups, ascertainment biases and imprecise definitions of fracture. There clearly is a need for large prospective controlled studies to evaluate fracture incidence in primary hyperparathyroidism.
Clinical management
Surgical
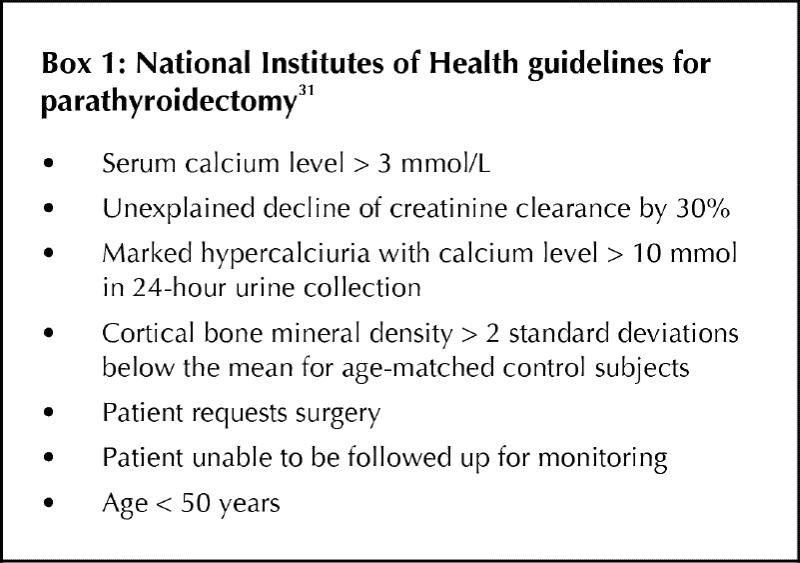
The need for parathyroidectomy in patients with asymptomatic disease has been questioned. In 1990 the National Institutes of Health held a consensus development conference on asymptomatic primary hyperparathyroidism.31 Guidelines for surgical intervention were developed, and it was agreed that people with mild disease who were asymptomatic could be followed safely with medical monitoring (Box 1). About half the patients with primary hyperparathyroidism will have 1 or more of these criteria for surgical intervention. Patient preference is also an important consideration in choosing the appropriate intervention. Localization tests include ultrasonography, computed tomography, magnetic resonance imaging and technetium-99m sestamibi scanning. Sestamibi scanning with computed tomography provides better resolution. Preoperative localization studies are indicated in those patients who have had prior neck surgery. They are not recommended routinely because the surgical success rate in experienced hands is better than in current imaging technology. After parathyroidectomy, increases in bone mineral density at the lumbar spine and femoral neck have been observed in a large prospective study.23
Box.
Medical
Hormone replacement therapy in the management of primary hyperparathyroidism has been evaluated in several studies.18,32,33 >Conjugated equine estrogen, 0.625 mg/d, and medroxyprogesterone acetate, 5 mg/d, over 2 years were effective in improving bone mineral density in the lumbar spine (by 5.2% ± 1.4%, p = 0.002) and in the femoral neck (by 3.4% ± 1.5%, p = 0.05). Total body bone mineral density (bone mineral density measured over the entire skeleton) also increased (by 1.3% ± 0.4%, p = 0.004).32 Increases at the proximal femur were also seen compared with baseline values.32 These findings have been supported by those of other investigators.18,33,34 Hormone replacement therapy appears to slow bone loss and increase bone mineral density in patients with primary hyperparathyroidism.
Bisphosphonates represent a potential alternative in the medical management of primary hyperparathyroidism. Clodronate has been evaluated in hyperparathyroidism,35,36,37,38 and reductions in serum calcium levels have been documented accompanied by a significant decline in bone loss with decreases in urinary calcium and urinary hydroxyproline excretion.36 No significant associated change in PTH levels has been noted.35 Treatment for more than 3 months with clodronate has, however, been associated with a partial recurrence of hypercalcemia because of a compensatory rise in serum PTH levels.37,38 The short-term effectiveness of risedronate has been evaluated in patients with primary hyperparathyroidism.31 The serum calcium concentration was again found to decrease after drug therapy, and an associated compensatory increase in PTH levels was documented. Bone loss was inhibited, as shown by reductions in the fasting urinary hydroxyproline:creatinine ratio and the serum alkaline phosphatase level.37 The bisphosphonate etidronate has been found to have little effect on serum calcium levels in primary hyperparathyroidism.39
Data regarding alendronate in primary hyperparathyroidism are limited to a few abstracts.40,41 Patients treated with this drug have gained bone at the lumbar spine, hip and radius. Bone loss was evident at all sites except the lumbar spine in the untreated patients.40 Alendronate is being evaluated further in primary hyperparathyroidism in studies that use a more rigorous experimental design.
Calcimimetic agents mimic the effect of calcium at the calcium receptor. One such agent is the phenylalkylamine compound R568, which has been shown in animal studies to be effective in decreasing cytoplasmic calcium levels, PTH secretion and serum calcium levels.42 R568 has been shown to reduce PTH secretion and ionized calcium levels in 20 postmenopausal women with asymptomatic primary hyperparathyroidism.43 Other calcimimetic agents are being evaluated in clinical trials and may become effective treatment options in the medical management of primary hyperparathyroidism.
Conclusion
People with primary hyperparathyroidism that is mild and asymptomatic can be followed without surgical intervention, because most patients with asymptomatic disease who do not undergo surgery do not demonstrate disease progression. Medical options are limited to estrogen therapy in postmenopausal women; the potential efficacy of bisphosphonates and calcimimetics remains to be demonstrated. Medical follow-up should include annual bone densitometry, with monitoring of both cancellous and cortical bone mass. If only one bone site is to be assessed it should be a site rich in cortical bone, preferably the distal one-third of the radius. Medical management has not been shown to affect adversely morbidity and mortality in people with asymptomatic hyperparathyroidism. When surgery has been deemed to be necessary, significant increases in bone mineral density at the lumbar spine and femoral neck have been documented after parathyroidectomy .
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Aliya Khan, 209-331 Sheddon Ave., Oakville ON L6J 1X8; fax 905 844-8966; avkhan@aol.com
References
- 1.Khan AA. Primary hyperparathyroidism: diagnosis and management — a review. Endocrine Practice 1997;3:22-6. [DOI] [PubMed]
- 2.Melton LJ III. Epidemiology of primary hyperparathyroidism. J Bone Miner Res 1991;6(Suppl 2):S25-30. [DOI] [PubMed]
- 3.Wermers RA, Khosla S, Atkinson EJ, Hodgson SF, O‚Fallon WM, Melton LJ III. The rise and fall of primary hyperparathyroidism: a population-based study in Rochester, Minnesota, 1965-1992. Ann Intern Med 1997;126: 433-40 [DOI] [PubMed]
- 4.Heath DA. Primary hyperparathyroidism. Clinical presentation and factors influencing clinical management. Endocrinol Metab Clin North Am 1989; 18:631-46. [PubMed]
- 5.Palmer M, Jakobsson S, Akerstrom G, Ljunghall S. Prevalence of hypercalcemia in a health survey: a 14-year follow-up study of serum calcium values. Eur J Clin Invest 1988;18:39-46. [DOI] [PubMed]
- 6.Grey A, Mitnick MA, Shapses S, Ellison A, Gundberg C, Insogna K. Circulating levels of interleukin-6 and tumor necrosis factor-alpha — a clinical research center study. J Clin Endocrinol Metab 1996;81:3450-4. [DOI] [PubMed]
- 7.Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, et al. Cloning and characterization of an extracellular Ca2+-sensing receptor from bovine parathyroid. Nature 1993;366:575-80. [DOI] [PubMed]
- 8.Brown E, Pollak M, Hebert SC. The extracellular calcium-sensing receptor: its role in health and disease. Annu Rev Med 1998:49:15-29. [DOI] [PubMed]
- 9.Attie MF, Gill JR Jr, Stock JL, Spiegel AM, Downs RW Jr, Levine MA, et al. Urinary calcium excretion in familial hypocalciuric hypercalcemia. Persistence of relative hypocalciuria after induction of hypoparathyroidism. J Clin Invest 1983;72:667-76. [DOI] [PMC free article] [PubMed]
- 10.Baron J, Winer KK, Yanovski JA, Cunningham AW, Laue L, Zimmerman D, et al. Mutations in the Ca2+-sensing receptor gene cause autosomal dominant and sporadic hypoparathyroidism. Hum Mol Genet 1996;5:601-6. [DOI] [PubMed]
- 11.Kifor O, Moore FD Jr, Wang P, Goldstein M, Vassilev P, Kifor I, et al. Reduced immunostaining for the extracellular Ca2+-sensing receptor in primary and uremic secondary hyperparathyroidism. J Clin Endocrinol Metab 1996; 81:1598-606. [DOI] [PubMed]
- 12.Chandrasekharappa SC, Guru SC, Manickam P, Olufemi SE, Collins FS, Emmert-Buck MR, et al. Positional cloning of the gene for multiple endocrine neoplasia-type I. Science 1997;276: 404-7. [DOI] [PubMed]
- 13.Mulligan LM, Kwok JB, Healey CS, Elsdon MJ, Eng C, Gardner E, et al. Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 1993;363:458-60. [DOI] [PubMed]
- 14.Ledger GA, Khosla S, Lindor NM, Thibodeau SN, Gharib N. Genetic testing in the diagnosis and management of multiple endocrine neoplasia type II. Ann Intern Med 1995;122:118-24. [DOI] [PubMed]
- 15.Seeman E, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL. Differential effects of endocrine dysfunction on the axial and the appendicular skeleton. J Clin Invest 1982;69:1302-9. [DOI] [PMC free article] [PubMed]
- 16.Larsson K, Lindh E, Lind L, Persson I, Ljunghall S. Increased fracture risk in hypercalcemia. Bone mineral content measured in hyperparathyroidism. Acta Orthop Scand 1989;60:268-70. [DOI] [PubMed]
- 17.Silverberg SJ, Shane E, de la Cruz L, Dempster DW, Feldman F, Seldin D, et al. Skeletal disease in primary hyperparathyroidism. J Bone Miner Res 1989;4:283-91. [DOI] [PubMed]
- 18.Guo CY, Thomas WEG, Al-Dehaimi AW, Assiri AM, Eastell R. Longitudinal changes in bone mineral density and bone turnover in post-menopausal women with primary hyperparathyroidism. J Clin Endocrinol Metab 1996;81:3487-91. [DOI] [PubMed]
- 19.Rico H, Revilla M. Arribas I, Villa LF, Alvarez de Buergo M. Total and regional bone mineral content in primary hyperparathyroidism: sex differences. Miner Electrolyte Metab 1994;20:112-6. [PubMed]
- 20.Pfeilschifter J, Siegrist E, Wuster C, Blind E, Ziegler R. Serum levels of intact parathyroid hormone and alkaline phosphatase correlate with cortical and trabecular bone loss in primary hyperparathyroidism. Acta Endocrinol (Copenh) 1992;127:319-23. [DOI] [PubMed]
- 21.Grey AB, Stapleton JP, Evans MC, Reid IR. Accelerated bone loss in post-menopausal women with primary hyperparathyroidism. Clin Endocrinol (Oxf) 1996;44:697-702. [DOI] [PubMed]
- 22.Grey AB, Cundy TF, Reid JR. Continuous combined oestrogen/progestin therapy is well tolerated and increases bone mineral density at the hip and spine in post-menopausal osteoporosis. Clin Endocrinol (Oxf) 1994;40:671-7. [DOI] [PubMed]
- 23.Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med 1999;341:1249-55. [DOI] [PubMed]
- 24.Silverberg SJ, Locker FG, Bilezikian JP. Vertebral osteopenia: a new indication of surgery in primary hyperparathyroidism. J Clin Endocrinol Metab 1996;81:4007-12. [DOI] [PubMed]
- 25.Melton LJ III, Atkinson EJ, O‚Fallon WM, Heath H III. Risk of age-related fractures in patients with primary hyperparathyroidism. Arch Intern Med 1992;152:2269-73. [PubMed]
- 26.Larsson K, Ljunghall S, Krusemo UB, Naessen T, Lindh E, Persson I. The risk of hip fractures in patients with primary hyperparathyroidism: a population-based cohort study with a follow-up of 19 years. J Intern Med 1993; 234:585-93. [DOI] [PubMed]
- 27.Wilson RJ, Rao S, Ellis B, Kleerekoper M, Parfitt AM. Mild asymptomatic primary hyperparathyroidism is not a risk factor for vertebral fractures. Ann Intern Med 1998;109:959-62. [DOI] [PubMed]
- 28.Kenny AM, MacGillivray DC, Pilbeam CC, Crombie HD, Raisz LG. Fracture incidence in postmenopausal women with primary hyperparathyroidism. Surgery 1995;118:109-14. [DOI] [PubMed]
- 29.Dauphine RT, Riggs BL, Scholz DA. Back pain and vertebral crush fractures: an unemphasized mode of presentation for primary hyperparathyroidism. Ann Intern Med 1975;83:365-7. [DOI] [PubMed]
- 30.Kochersberger G, Buckley NJ, Leight GS, Martinez S, Studenski S, Vogler J, et al. What is the clinical significance of bone loss in primary parathyroidism? Arch Intern Med 1987;47:1951-3. [PubMed]
- 31.National Institutes of Health. Consensus development conference statement. J Bone Miner Res 1991;6(Suppl 2):S9-13. [DOI] [PubMed]
- 32.Grey AB, Stapleton JP, Evans MC, Reid JR. The effect of hormone replacement therapy on bone mineral density in post-menopausal women with primary hyperparathyroidism. A randomized controlled trial. Ann Intern Med 1996;125:360-9. [DOI] [PubMed]
- 33.Selby P, Peacock M. Ethynyl estradiol and norethindrone in the treatment of primary hyperparathyroidism in post-menopausal women. N Engl J Med 1986;314:1481-5. [DOI] [PubMed]
- 34.Marcus R, Madvig P, Crim M, Pont A, Kosek J. Conjugated estrogen in the treatment of post-menopausal women with hyperparathyroidism. Ann Intern Med 1984;100:633-40. [DOI] [PubMed]
- 35.Shane E, Baquiran DC, Bilezikian JP. Effects of dichloromethylene diphosphonate on serum and urinary calcium in primary hyperparathyroidism. Ann Intern Med 1981;95:23-7. [DOI] [PubMed]
- 36.Hamdy NA, Gray RE, McCloskey E, Galloway J, Rattenbury JM, Brown CB, et al. Clodronate in the medical management of hyperparathyroidism. Bone 1987;8(Suppl 1):69-77. [PubMed]
- 37.Reasner CA, Stone MD, Hosking DJ, Ballah A, Mundy GR. Acute changes in calcium homeostasis during treatment of primary hyperparathyroidism with risedronate. J Clin Endocrinol Metab 1993;77:1067-71. [DOI] [PubMed]
- 38.Adami S, Mian M, Bertoldo F, Rossini M, Jayawerra P, O‚Riordan JL, et al. Regulation of calcium-parathyroid hormone feedback in primary hyperthyroidism: effects of bisphosphonate treatment. Clin Endocrinol (Oxf) 1990;33:391-7. [DOI] [PubMed]
- 39.Licata AA, O‚Hanlon O. Treatment of hyperparathyroidism with etidronate disodium. JAMA 1983;249:2063-4. [PubMed]
- 40.Parker CR, Blackwell PJ, Hosking DJ. Alendronate in the treatment of primary hyperparathyroidism-related osteoporosis [abstract]. American Society of Bone Mineral Research annual meeting; 1998 Dec 1-6; San Francisco.
- 41.Hassani S, Brickman AS, Hershman JM. Alendronate therapy of primary hyperparathyroidism [abstract]. Endocrine Society annual meeting; 1998 June 24-27; New Orleans.
- 42.Steffey ME, Fox J, VanWagenen BC, Delmar EG, Balandrin MF, Nemeth EF. Calcimimetics: structurally and mechanistically novel compounds that inhibit hormone secretion from parathyroid cells [abstract]. J Bone Miner Res 1993;8(Suppl 1):S175.
- 43.Silverberg SJ, Bone HG III, Marriott TB, Locker FG, Thys-Jacobs S, Dziem G, et al. Short-term inhibition of parathyroid hormone secretion by a calcium-receptor agonist in patients with primary hyperparathyroidism. N Engl J Med 1997;337:1506-10. [DOI] [PubMed]


