Abstract
Hypertension is an important public health issue due to its association with a number of serious diseases, including cardiovascular disease and stroke. The importance of evaluating hypertension taking into account different blood pressure (BP) profiles and BP variability (BPV) is increasingly being recognized, and is particularly relevant in Asian populations given the specific features of hypertension in the region (including greater salt sensitivity and a high rate of nocturnal hypertension). Ambulatory BP monitoring (ABPM) is the gold standard for diagnosing hypertension and assessing 24‐hour BP and provides data on several important parameters that cannot be obtained using any other form of BP measurement. In addition, ABPM parameters provide better information on cardio‐ and cerebrovascular risk than office BP. ABPM should be used in all patients with elevated BP, particularly those with unstable office or home BP, or who are suspected to have white‐coat or masked hypertension. ABPM is also an important part of hypertension diagnosis and monitoring in high‐risk patients. ABPM needs to be performed using a validated device and good practice techniques, and has a role both in hypertension diagnosis and in monitoring the response to antihypertensive therapy to ensure strict BP control throughout the 24‐hour period. Use of ABPM in clinical practice may be limited by cost and accessibility, and practical education of physicians and patients is essential. The ABPM evidence and practice points in this document are based on the Hypertension Cardiovascular Outcome Prevention and Evidence (HOPE) Asia Network expert panel consensus recommendations for ABPM in Asia.
Keywords: ambulatory blood pressure monitoring, blood pressure control, clinical practice, guidelines, hypertension
ABPM plays an important role in the diagnosis and management of hypertension, and is recognized as an essential part of good clinical practice in the field. The goal of the practice points provided is to help clinicians incorporate ABPM into their everyday practice to help improve patient outcomes.

1. INTRODUCTION
Hypertension is an important risk factor for serious diseases, including cardiovascular disease and stroke, making it an important public health issue. 1 , 2 Ethnic differences in the pathogenesis and cardiovascular complications of hypertension, 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 and the rapidly aging population demographic in the region mean that hypertension is a particularly relevant problem in Asia. 6 , 15 As a result, it is important to use the latest tools and techniques to diagnose and manage hypertension.
Out‐of‐office blood pressure (BP) monitoring is highlighted by several major international guidelines as playing a central role in hypertension diagnosis and management. 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 Out‐of‐office techniques include home blood pressure monitoring (HBPM) and ambulatory blood pressure monitoring (ABPM). ABPM is considered the state‐of‐the art technology for BP measurement, and its use is endorsed by major international guidelines for North America, 23 , 25 , 26 Europe, 17 , 19 , 24 Korea, 27 Japan, 22 China, 28 and Taiwan. 16
Asia‐specific evidence and guidance for the use of HBPM are now available. 29 , 30 , 31 In addition, comprehensive consensus–based expert panel recommendations on ABPM from the Hypertension, brain, cardiovascular and renal Outcome Prevention and Evidence in Asia (HOPE Asia) Network have recently been published. 32 This practice‐focused document provides key messages from the expert panel recommendations and presents a set of ABPM practice points (Figure 1) that can be easily implemented in clinical settings.
Figure 1.
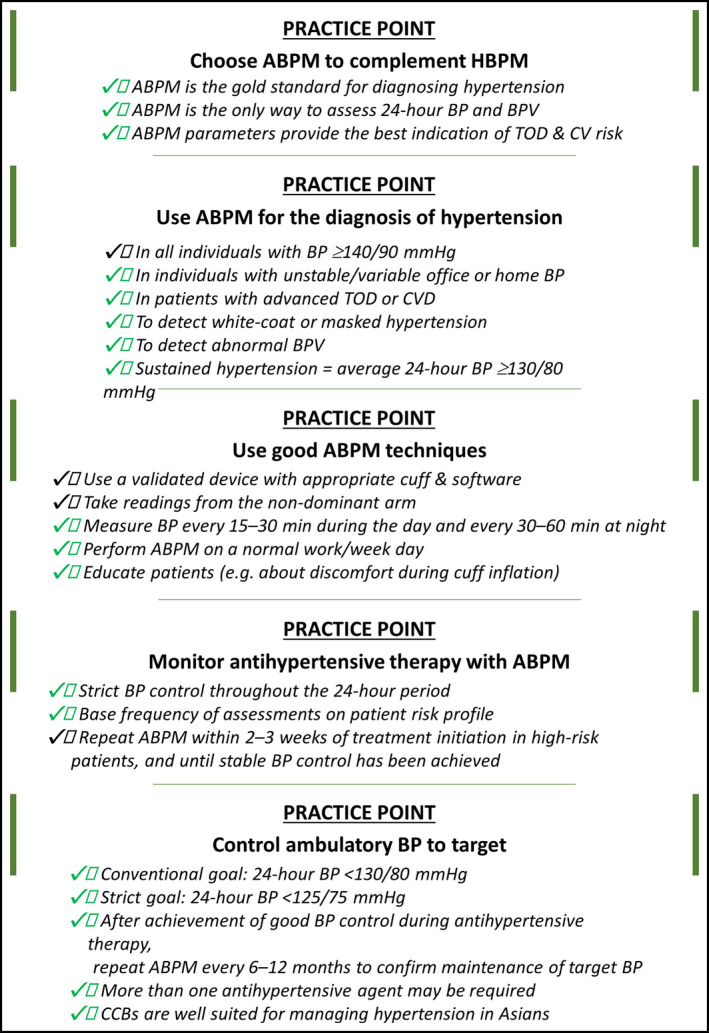
Ambulatory blood pressure monitoring (ABPM) practice points. BP, blood pressure; BPV, blood pressure variability; CCBs, calcium channel blockers; CV, cardiovascular; CVD, cardiovascular disease; TOD, target organ damage
2. ABPM PARAMETERS AND PHENOTYPES
BP reflects the hemodynamic state and is not a static phenomenon. As a result, there are both short‐term and long‐term variations in BP, referred to as blood pressure variability (BPV). Factors contributing to BPV include genetics, mechanical forces generated during ventilation, local vasomotor phenomena, sympathetic nervous system activity, electrolytes, neurohumoral factors, physical activity, arterial wall thickness, baroreflex mechanisms, time of day, seasonal influences, and possibly also environmental factors. 33 The importance of different BP profiles and BPV is increasingly being recognized. ABPM is one of the tools that facilitate determination of these profiles and variability, allowing patients to be classified into different BP phenotype groups. The clock‐based definition of daytime, nighttime, and the morning was from awakening to going to bed, from going to bed to awaking, and the 2 hours after awaking, respectively (Figure 2).
Figure 2.

Blood pressure measures determined using ambulatory blood pressure monitoring. BP, blood pressure (adapted from Kario et al 2003) 41
BP is usually higher during the day (or periods of wakefulness) and lower at night (or periods of sleep). The expected physiological fall in nighttime BP is > 10% (dipping), whereas a reduction of < 10% in BP at night is defined as non‐dipping; patients with a riser (or reverse dipping) pattern show an increase in BP during sleeping hours to levels (BP fall is < 0%) that may be higher than those during the day (ie, nocturnal hypertension). 34 Extreme dipping refers to patients who show a marked (>20%) nocturnal fall in systolic BP (SBP) and or diastolic BP (DBP), or have a night/day SBP or DBP ratio of < 0.8. 20 Given that the circadian rhythm of BP is predominantly determined not by awake‐sleep behavior rather than the day‐night cycle, 35 the nocturnal dipping status of shift workers should be determined by awake BP (during nighttime) and sleep BP (during daytime).
Nocturnal BP may be the most reproducible and reliable ABPM parameter for risk stratification. 36 Nocturnal hypertension (BP ≥ 120/70 mmHg) could indicate the presence of comorbidities such as obstructive sleep apnea (OSA), and the riser pattern of nighttime BP is associated with a particularly poor prognosis with respect to the occurrence of stroke and cardiac events. 37 , 38 , 39 Stroke risk also appears to be increased in elderly hypertensive patients with an extreme dipper pattern. 40 Another important BPV parameter is the morning BP surge (the difference between the lowest nighttime BP and morning BP measured 2 hours after awakening). Early morning BP surge is associated with an increased risk of cardiovascular and cerebrovascular adverse events, especially hemorrhagic stroke. 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52
Excessive BPV could result in large dynamic surges that have the potential to trigger adverse cardiovascular events (the resonance hypothesis), and the risk of these events is exaggerated in high‐risk patients with vascular disease. 53 Greater variability in SBP is a significant independent predictor of mortality. 54 , 55
ABPM data can be used to calculate a number of important measures of short‐term BPV, including the standard deviation (SD), coefficient of variation (CV), average real variability (ARV), variability independent of the mean (VIM) for daytime and nighttime BP, weighted SD of 24‐hour BP values, and peak and trough values for daytime and nighttime BP. 32 However, although short‐term BPV has been used successfully for risk stratification, use in clinical practice is currently limited by a lack of accepted thresholds defining normal and pathologic short‐term BPV. 19
3. ASIA‐SPECIFIC FEATURES OF THE 24‐HOUR BP PROFILE
There is a possibility that Asia‐specific features of hypertension include greater salt sensitivity and lower body mass index compared with Western populations. 9 , 10 Prevalence rates for masked (uncontrolled) hypertension, excessive morning BP surge and morning hypertension, and nocturnal hypertension are all higher in Asians than in Westerners. 46 , 56 , 57 , 58 , 59 , 60 There are also ethnic variations in the complications of hypertension. Although coronary heart disease (CHD) is the most common complication of hypertension in Western subjects, the rate of stroke is higher than that of CHD in many of the Asian countries. 8 , 12 In addition, the slope of the relationship between increasing BP and the rate of cardiovascular events, especially stroke, is steeper in Asians than in Westerners. 4 , 61 , 62 , 63
4. WHY IS IT IMPORTANT TO MONITOR AMBULATORY BP?
ABPM is the reference standard, because neither clinic nor home BP measurements alone had sufficient sensitivity or specificity to perform the diagnosis of hypertension compared with ABPM. 64 ABPM also provides data on several important parameters that cannot be obtained using any other form of BP measurement, including 24‐hour BP, BPV (particularly over the short term), nocturnal “dipping status,” and BP morning surge. In addition, ABPM readings reflect an individual's BP in their usual daily environment, allowing the effects of environmental and emotional factors on BP to be determined. 19 , 65 Importantly, ABPM measures correlate better with the occurrence of cardiovascular events in patients with hypertension than office BP 39 , 66 , 67 , 68 , 69 , 70 and therefore provides better information with which to manage cardiovascular risk. ABPM parameters have also been associated with target organ damage (TOD) in patients with hypertension (eg, left ventricular hypertrophy, diastolic dysfunction, microvascular disease, atherosclerosis, and cognitive dysfunction). 42 , 85
5. ABPM VERSUS HBPM
In clinical practice, use of ABPM together with HBPM is recommended because ABPM and HBPM provide complementary data. 19 , 20 , 24 The differential features of ABPM and HBPM are shown in Table 1. However, ABPM is preferable to HBPM depending on physicians or clinical situation. 86 There are a number of reasons for this. Firstly, there is more evidence for the association between antihypertensive treatment and improved cardiovascular outcomes when BP is assessed using ABPM rather than HBPM. Secondly, although HBPM devices may be readily available, many are not validated or reliable, especially if purchased online. 87 Thirdly, not all patients with hypertension are capable of complying with HBPM monitoring requirements, especially over the longer term.
Table 1.
Differential characteristics of out‐of‐office blood pressure measurement tools
| ABPM | HBPM | |
|---|---|---|
| Convenient | No | Yes |
| Validated | Yes | Yes (but not all devices) |
| Evidence for association with cardiovascular outcome | +++ | ++ |
| Evidence for monitoring drug efficacy | +++ | ++ |
| Reimbursement | Yes | No |
Abbreviations: ABPM, ambulatory blood pressure monitoring; HBPM, home blood pressure monitoring.
Nevertheless, data for the association between HBPM parameters and cardiovascular outcomes are accumulating, 88 and newer HBPM devices can monitor nighttime home BP, which may provide better prognostic information than nighttime BP measured using ABPM. 89 In Japan in particular, guidelines recommend the initial use of HBPM in patients with hypertension, 22 and a variety of validated HBPM devices have been used extensively in clinical practice because device sale is regulated by the government and limited to validated options. Ultimately, the choice of when and how to use ABPM and/or HBPM will depend on the specific health care environment in each country and the currently available evidence. 31
6. WHO NEEDS ABPM?
Guidelines recommend the use of out‐of‐office BP monitoring, including ABPM, to facilitate the diagnosis of hypertension, including detection and confirmation of white‐coat hypertension (WCH) and masked hypertension (MH). 16 , 17 , 18 , 36 , 90 Individuals who show unstable and/or variable BP on office or home measurements are ideal candidates for ABPM because these people are more likely to have WCH or MH. 19 ABPM should also be used in patients with advanced TOD, secondary hypertension, drug‐resistant hypertension, and to monitor antihypertensive drug therapy. 32 ABPM may also be useful for patients working in a stressful environment who are suspected of having hypertension, who have been shown to demonstrate higher BP in the worksite compared with morning home BP and office BP. 91 The clinical indications for ABPM are summarized in Table 2.
Table 2.
Clinical indications for using ambulatory blood pressure monitoring in addition to home blood pressure monitoring
| Indication |
|---|
| Increased BPV on HBPM or abnormal 24‐hour BP patterns |
| Presence of advanced target organ damage |
| Suspected masked hypertension |
| Suspected white‐coat hypertension |
| Secondary hypertension |
| Monitoring of antihypertensive therapy |
| Treatment‐resistant hypertension |
Abbreviations: BPV, blood pressure variability; HBPM, home blood pressure monitoring.
7. HOW AND WHEN SHOULD ABPM BE MEASURED?
Use of an ABPM device that has been validated against accepted international standards, with associated software providing the data of interest, is recommended. 19 At a minimum, this should include details of all BP readings showing daytime and nighttime windows with an indication of normal BP, average SBP, average DBP, and heart rate, the percentage change in SBP and DBP at night, and summary statistics for time‐weighted average SBP, DBP, and pulse rate for the 24‐hour period, daytime, and nighttime, with standard deviations and number of valid BP readings. 19
Use of the non‐dominant arm is recommended to obtain good ABPM readings, and an appropriate cuff should be provided. 19 During the day, measures should be taken every 15‐30 minutes, while measurements every 30‐60 min are adequate at night. 19 Overall, at least 70% of readings throughout the 24‐hour period should be valid, and there should be at least 20 valid daytime and at least 7 valid nighttime measurements. 65 In addition, performing ABPM on a normal workday (rather than the weekend or an unusually restful day) will provide data that best reflects a patient's typical BP profile. 65
8. ABPM DIAGNOSTIC THRESHOLDS
Diagnosis of hypertension using ABPM should be made based on the following thresholds (Figure 3): ≥130/80 mmHg for average 24‐hour BP (sustained hypertension); ≥135/85 mmHg for average daytime BP (daytime hypertension); ≥120/70 mmHg for average nighttime BP (nocturnal hypertension); and ≥135/85 mmHg for average morning BP (morning hypertension). 31 , 32 Diagnosis of WCH is made when office/clinic BP is ≥ 140/90 mmHg plus all of the following on ABPM: 24‐hour BP < 130/80 mmHg; daytime BP < 135/85 mmHg; nighttime BP < 120/70 mmHg; and morning BP < 135/85 mmHg. 31 , 32 Diagnosis of MH is made when office/clinic BP is < 140/90 mmHg plus 24‐hour BP ≥ 130/80 mmHg, daytime BP ≥ 135/85 mmHg (masked daytime hypertension), nighttime BP ≥ 120/70 mmHg (masked nocturnal hypertension), and/or morning BP ≥ 135/85 mmHg (masked morning hypertension). 31 , 32
Figure 3.

Hypertension classifications based on office and ambulatory blood pressure. Source: Kario K. et al, 32 J Clin Hypertens (Greenwich). 2019; 21:1250‐1283
9. ABPM MONITORING OF ANTIHYPERTENSIVE THERAPY
The importance of achieving adequate, consistent reductions in BP cannot be overemphasized. Strict BP control throughout the 24‐hour period is important for all patients, but is particularly critical in those of Asian ethnicity. 3 Given the greater effect of BP reductions in stroke and heart failure versus CHD, 92 and the higher rate of these events in Asians, 8 , 12 the beneficial effects of BP lowering may be more marked in Asian compared with Western populations. 4
The only way to reliably monitor the effects of antihypertensive treatment is to repeat ABPM. After good BP control has been achieved and documented, regular reassessment using ABPM will facilitate the maintenance of 24‐hour BP control. 32 Conventional goal BP thresholds using ABPM are < 130/80 mmHg for average 24‐hour BP, <135/85 mmHg for average daytime BP, <120/70 mmHg for average nighttime BP, and < 135/85 mmHg for average morning BP. Applying strict goal thresholds, target BP would be < 125/75 mmHg for average 24‐hour BP, <130/80 mmHg for average daytime BP, <110/65 mmHg for average nighttime BP, and < 130/80 mmHg for average morning BP. 32
Adjustment of antihypertensive therapy based on 24‐hour data from ABPM has been shown to provide the same level of BP control with less intensive therapy compared with treatment managed using office BP. 93 In addition, the proportion of patients achieving target BP in primary care was higher (by up to 26%) when antihypertensive therapy was managed using ABPM compared with office BP. 94 , 95 However, there is a lack of current guideline recommendations about how to use ABPM to monitor antihypertensive therapy. Therefore, the best approach might be to base the frequency of ABPM assessments on the risk profile of each patient. Repeating ABPM annually in conjunction with home and office BP readings may be adequate for low‐risk patients. In unstable high‐risk patients, for whom tight BP control throughout the 24‐hour period is particularly important, it might be better to repeat ABPM more frequent, for example, every few weeks. 96 In patients with treatment‐resistant hypertension, use of ABPM allows categorization of patients as having true resistance rather than white‐coat resistance, 97 , 98 which facilitates appropriate targeting of additional therapeutic interventions.
Calcium channel blocker (CCB) therapy appears to be particularly well suited to the characteristics of Asian patients with hypertension because the BP‐lowering activity of these agents is independent of salt sensitivity and salt intake. 99 Treatment with a long‐acting CCB has been shown to be effective for lowering office, home morning, and 24‐hour ambulatory BP, and reducing exaggerated BPV, independently of salt intake and salt sensitivity. 99 , 100 , 101 , 102
Combination antihypertensive therapy is often required to achieve good BP control. Clinical trial data obtained using ABPM indicate that combinations including an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker plus a CCB effectively reduce 24‐hour BP and other ABPM parameters (eg, nocturnal hypertension, morning BP surge) in Japanese patients with hypertension. 103 , 104 , 105 , 106 Novel approaches to lowering BP are being investigated in patients with treatment‐resistant hypertension, and ABPM has been included as an important assessment tool in trials evaluating renal denervation in this setting. 107 , 108 , 109
10. ABPM IN ASIA: CURRENT PRACTICE AND BARRIERS TO USE
ABPM devices are widely available in certain Asian countries. However, there are limited data on how this important out‐of‐office BP monitoring technique is used in routine clinical practice throughout the region. Cost (including reimbursement) and accessibility are potential issues that could limit the use of ABPM in some settings and/or countries, 110 , 111 , 112 although longer term savings are likely to offset the short‐term costs of ABPM use. 19 In Japan, ABPM is reimbursed by the National Health Insurance scheme, based on the superiority of ABPM over other forms of BP measurement for predicting the development of cardio‐ and cerebrovascular events, and the cost‐effectiveness of this approach. 113 Modeled data estimated that introduction of ABPM for hypertension monitoring in Japan would save 10 trillion yen over 10 years, reduce the number of strokes by more than 59,500, and save almost 19,000 lives. 114
In addition to the cost and having access to a validated device, there are a number of factors that contribute to decisions about whether and how often to use ABPM. These include patient engagement and acceptability, physician knowledge and attitude to training, education and training of both the physician and patient, and available resources (both in terms of staffing and funding). 32 The perceived complexity of ABPM by patients means that physicians need to allocate adequate time to provide appropriate and thorough education, including letting the patient know that there may be some discomfort during BP cuff inflation. 19
Region‐wide strategies are needed to improve access to APBM devices, provide physician training, and develop suitable education materials (supplemental material) to facilitate more widespread use of ABPM in Asia. 32
11. TELEMEDICINE AND NEW OPPORTUNITIES
New information and communication technology (ICT)–based devices that perform automatic, fixed‐interval BP measurement during sleep and store or transmit the data (telemedicine) are now available, and could facilitate a novel approach to manage patients with hypertension. 115 Health and information technology (HIT) solutions such as these are becoming recognized as important advances in health care, and the emerging role of HIT was highlighted in the latest version of the American College of Cardiology/American Heart Association hypertension guidelines. 23 Furthermore, a Web‐based ABPM recording platform is established in China. 116 With this platform, ABPM data are uploaded to the system and analyzed in a remote server. Analyzed data can be forwarded to the patients and physicians. The goal with these devices is to obtain information that allows anticipation of cardiovascular events and early intervention to prevent them. The ultimate aim would be to eliminate cardiovascular events in patients with hypertension altogether. This approach is referred to as “anticipation medicine” for zero cardiovascular events, 117 within which BPV is a key biomarker. 3 , 118
12. CONCLUSIONS
ABPM plays an important role in the diagnosis and management of hypertension, and is recognized as an essential part of good clinical practice in the field. It is currently the only out‐of‐office BP monitoring technique that can provide information on the 24‐hour BP profile, including BPV, nocturnal hypertension, and morning BP surge, all of which are important predictors of TOD and cardio‐ and cerebrovascular risk. ABPM is particularly relevant in Asia due to the specific characteristics of hypertension in the region, including greater BPV and a higher rate of nocturnal hypertension, both of which are best identified using ABPM. ABPM also has an important role in the effective initiation and management of antihypertensive therapy and allows determination of 24‐hour BP control. The goal of the practice points provided is to help clinicians incorporate ABPM into their everyday practice to help improve patient outcomes.
Disclosures
K Kario reports research grants from Omron Healthcare, Fukuda Denshi, A&D, and Pfizer Japan, and honoraria from Omron Healthcare. YC Chia has received speaker honorarium and sponsorship to attend conferences and seminars from Boehringer Ingelheim, Pfizer, Omron, Servier, and Xepa‐Soul, and investigator‐initiated research grants from Pfizer and Omron. S Siddique has received honoraria from Bayer, Novartis, Pfizer, ICI, and Servier; and travel, accommodation, and conference registration support from Hilton Pharma, Atco Pharmaceutical, Highnoon Laboratories, Horizon Pharma, and ICI. J Shin has received lecture honoraria from Pfizer Inc, Hanmi Pharm. Co. Ltd., Yuhan Co. Ltd., and Boryung Pharmaceutical Co. Ltd.; consulting fees from Hanmi Pharm. Co. Ltd. And Handok Kalos Medical Inc; and research grants from Sanofi Pharm. and Hanmi Pharm. Co. Ltd. CH Chen reports personal fees from Novartis, Sanofi, Daiichi Sankyo, Servier, Bayer, and Boehringer Ingelheim Pharmaceuticals, Inc HM Cheng received speakers’ honorarium and sponsorship to attend conferences and CME seminars from Eli Lilly and AstraZeneca; Pfizer Inc; Bayer AG; Boehringer Ingelheim Pharmaceuticals, Inc; Daiichi Sankyo, Novartis Pharmaceuticals, Inc; Servier; Co., Pharmaceuticals Corporation; Sanofi; TAKEDA Pharmaceuticals International; Menarini Co., Ltd.; and served as an advisor or consultant for ApoDx Technology, Inc JM Nailes has received honorarium and sponsorship to attend conferences and seminars from Pfizer and Omron, and received an investigator‐initiated research grant from Pfizer. JG Wang reports having received research grants from Chengdu Di‐Ao and Omron, and lecture and consulting fees from AstraZeneca, Novartis, Omron, Servier, and Takeda. All other authors report no potential conflicts of interest in relation to this article.
AUTHOR CONTRIBUTION
K. Kario had the primary responsibility of writing this paper. K. Kario and S. Hoshide wrote the essential part of the manuscript. JG. Wang, YC Chia, P. Buranakitjaroen, S. Siddique, J. Shin, Y. Turana, S. Park, K. Tsoi, CH Chen, HM Cheng, T. Fujiwara, Y. Li, VM Huynh, M. Nagai, J. Nailes, J. Sison, AA Soenarta, GP Sogunuru, A. Sukonthasarn, JC Tay, BW Teo, N. Verma, TD Wang, and Y. Zhang reviewed/edited the manuscript.
13.
Table 3.
Ambulatory blood pressure values corresponding to clinic measurements
| Clinic BP (mmHg) | Ambulatory BP (mmHg) | |||
|---|---|---|---|---|
| Daytime | Nighttime | 24‐Hour | Morning | |
| 120/80 | 120/80 | 100/65 | 115/75 | 120/80 |
| 130/80 | 130/80 | 110/65 | 125/75 | 130/80 |
| 140/90* | 135/85* | 120/70* | 130/80* | 135/85* |
| 160/100 | 145/90 | 140/85 | 145/90 | 145/90 |
Abbreviation: BP, blood pressure. Source: Kario K. et al, 32 J Clin Hypertens (Greenwich). 2019; 21:1250‐1283.
Pathologic threshold.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
Writing and editorial support was provided by Nicola Ryan, independent medical writer; this support was funded by Pfizer.
Kario K, Hoshide S, Chia Y‐C, et al; the Hypertension Cardiovascular Outcome Prevention, Evidence (HOPE) Asia Network . Guidance on ambulatory blood pressure monitoring: A statement from the HOPE Asia Network. J Clin Hypertens. 2021;23:411–421. 10.1111/jch.14128
Funding information
Pfizer.
REFERENCES
- 1. World Health Organization . Global Health Observatory (GHO) data. Raised blood pressure. Available from: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/ Last accessed: 16 Sep 2020.
- 2. World Health Organization . A global brief on hypertension. Silent killer, global public health crisis. (2013). Available from: https://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/. Last accessed 16 Sep 2020
- 3. Kario K. Evidence and perspectives on the 24‐hour management of hypertension: hemodynamic biomarker‐Initiated ‘anticipation medicine' for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262‐281. [DOI] [PubMed] [Google Scholar]
- 4. Kario K, Chen CH, Park S, et al. Consensus document on improving hypertension management in Asian patients, taking Into account Asian characteristics. Hypertension. 2018;71:375‐382. [DOI] [PubMed] [Google Scholar]
- 5. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702‐2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Park JB, Kario K, Wang JG. Systolic hypertension: an increasing clinical challenge in Asia. Hypertens Res. 2015;38:227‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arima H, Murakami Y, Lam TH, et al. Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia‐Pacific Region. Hypertension. 2012;59:1118‐1123. [DOI] [PubMed] [Google Scholar]
- 8. Ishikawa Y, Ishikawa J, Ishikawa S, et al. Prehypertension and the risk for cardiovascular disease in the Japanese general population: the Jichi Medical School Cohort Study. J Hypertens. 2010;28:1630‐1637. [DOI] [PubMed] [Google Scholar]
- 9. Ishikawa Y, Ishikawa J, Ishikawa S, et al. Prevalence and determinants of prehypertension in a Japanese general population: the Jichi Medical School Cohort Study. Hypertens Res. 2008;31:1323‐1330. [DOI] [PubMed] [Google Scholar]
- 10. Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res. 2003;26:521‐525. [DOI] [PubMed] [Google Scholar]
- 11. Lawes CM, Bennett DA, Parag V, et al. Blood pressure indices and cardiovascular disease in the Asia Pacific region: a pooled analysis. Hypertension. 2003;42:69‐75. [DOI] [PubMed] [Google Scholar]
- 12. Ueshima H. Explanation for the Japanese paradox: prevention of increase in coronary heart disease and reduction in stroke. J Atheroscler Thromb. 2007;14:278‐286. [DOI] [PubMed] [Google Scholar]
- 13. Kario K, Chia YC, Sukonthasarn A, et al. Diversity of and initiatives for hypertension management in Asia‐Why we need the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:331‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kario K. The HOPE Asia Network activity for "zero" cardiovascular events in Asia: Overview 2020. J Clin Hypertens (Greenwich). 2020;22:321‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chung N, Baek S, Chen MF, et al. Expert recommendations on the challenges of hypertension in Asia. Int J Clin Pract. 2008;62:1306‐1312. [DOI] [PubMed] [Google Scholar]
- 16. Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1‐47. [DOI] [PubMed] [Google Scholar]
- 17. National Institute for Health and Care Excellence . Hypertension in adults: diagnosis and management. NICE guideline [NG136] Published date: 28 August 2019. Available from: https://www.nice.org.uk/guidance/ng136. Last accessed: Sep 2020
- 18. Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506‐525. [DOI] [PubMed] [Google Scholar]
- 19. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731‐1768. [DOI] [PubMed] [Google Scholar]
- 20. Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359‐1366. [DOI] [PubMed] [Google Scholar]
- 21. Sharman JE, Howes FS, Head GA, et al. Home blood pressure monitoring: Australian expert consensus statement. J Hypertens. 2015;33:1721‐1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235‐1481. [DOI] [PubMed] [Google Scholar]
- 23. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199‐2269.29146533 [Google Scholar]
- 24. Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, Clement D, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope LM, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus RJ, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018: 28 Aug [Epub ahead of print]. doi:10.1093/eurheartj/ehy1339. [DOI] [PubMed] [Google Scholar]
- 25. Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada's 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016;32:569‐588. [DOI] [PubMed] [Google Scholar]
- 26. Siu AL. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778‐786. [DOI] [PubMed] [Google Scholar]
- 27. Lee HY, Shin J, Kim GH, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II‐diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension . Chinese guidelines for the management of hypertension [Chinese]. Chin J Cardiol. 2010;2011:39. [Google Scholar]
- 29. Park S, Buranakitjaroen P, Chen CH, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249‐258. [DOI] [PubMed] [Google Scholar]
- 30. Kario K, Park S, Buranakitjaroen P, et al. Guidance on home blood pressure monitoring: A statement of the HOPE Asia Network. J Clin Hypertens (Greenwich). 2018;20:456‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kario K, Park S, Chia YC, et al. 2020 Consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:351‐362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kario K, Shin J, Chen CH, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: The HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:1250‐1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sogunuru GP, Kario K, Shin J, et al. Morning surge in blood pressure and blood pressure variability in Asia: Evidence and statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:324‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kario K, Shimada K. Risers and extreme‐dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004;26:177‐189. [DOI] [PubMed] [Google Scholar]
- 35. Yamasaki F, Schwartz JE, Gerber LM, Warren K, Pickering TG. Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. Hypertension. 1998;32:417‐423. [DOI] [PubMed] [Google Scholar]
- 36. Hoshide S, Cheng HM, Huang Q, et al. Role of ambulatory blood pressure monitoring for the management of hypertension in Asian populations. J Clin Hypertens (Greenwich). 2017;19:1240‐1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kario K, Hoshide S, Mizuno H, et al. Nighttime blood pressure phenotype and cardiovascular prognosis. practitioner‐based nationwide JAMP Study. Circulation. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ohkubo T, Hozawa A, Yamaguchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24‐h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183‐2189. [DOI] [PubMed] [Google Scholar]
- 39. Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282:539‐546. [DOI] [PubMed] [Google Scholar]
- 40. Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852‐857. [DOI] [PubMed] [Google Scholar]
- 41. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401‐1406. [DOI] [PubMed] [Google Scholar]
- 42. Gosse P, Lasserre R, Minifie C, Lemetayer P, Clementy J. Blood pressure surge on rising. J Hypertens. 2004;22:1113‐1118. [DOI] [PubMed] [Google Scholar]
- 43. Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149‐154. [DOI] [PubMed] [Google Scholar]
- 44. Pierdomenico SD, Pierdomenico AM, Cuccurullo F. Morning blood pressure surge, dipping, and risk of ischemic stroke in elderly patients treated for hypertension. Am J Hypertens. 2014;27:564‐570. [DOI] [PubMed] [Google Scholar]
- 45. Bombelli M, Fodri D, Toso E, et al. Relationship among morning blood pressure surge, 24‐hour blood pressure variability, and cardiovascular outcomes in a white population. Hypertension. 2014;64:943‐950. [DOI] [PubMed] [Google Scholar]
- 46. Hoshide S, Kario K, de la Sierra A, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015;66:750‐756. [DOI] [PubMed] [Google Scholar]
- 47. Israel S, Israel A, Ben‐Dov IZ, Bursztyn M. The morning blood pressure surge and all‐cause mortality in patients referred for ambulatory blood pressure monitoring. Am J Hypertens. 2011;24:796‐801. [DOI] [PubMed] [Google Scholar]
- 48. Luo Y, Wang YL, Wu YB, et al. Association between the rate of the morning surge in blood pressure and cardiovascular events and stroke. Chin Med J (Engl). 2013;126:510‐514. [PubMed] [Google Scholar]
- 49. Cheng HM, Wu CL, Sung SH, et al. Prognostic Utility of Morning Blood Pressure Surge for 20‐Year All‐Cause and Cardiovascular Mortalities: Results of a Community‐Based Study. J Am Heart Assoc. 2017;6: e007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Li Y, Thijs L, Hansen TW, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040‐1048. [DOI] [PubMed] [Google Scholar]
- 51. Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens. 2015;28:30‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Xie JC, Yan H, Zhao YX, Liu XY. Prognostic value of morning blood pressure surge in clinical events: a meta‐analysis of longitudinal studies. J Stroke Cerebrovasc Dis. 2015;24:362‐369. [DOI] [PubMed] [Google Scholar]
- 53. Kario K. New Insight of Morning Blood Pressure Surge Into the Triggers of Cardiovascular Disease‐Synergistic Resonance of Blood Pressure Variability. Am J Hypertens. 2016;29:14‐16. [DOI] [PubMed] [Google Scholar]
- 54. Hsu PF, Cheng HM, Wu CH, et al. High short‐term blood pressure variability predicts long‐term cardiovascular mortality in untreated hypertensives but not in normotensives. Am J Hypertens. 2016;29:806‐813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kikuya M, Hozawa A, Ohokubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000;36:901‐906. [DOI] [PubMed] [Google Scholar]
- 56. Kario K. Essential Manual on Perfect 24‐hour Blood Pressure Management from Morning to Nocturnal Hypertension: Up‐to‐date for Anticipation Medicine. Wiley Publishing Japan. 2018:1‐309.
- 57. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic diurnal blood pressure variability between Japanese and American treatment‐resistant hypertensive populations. Circ J. 2017;81:1337‐1345. [DOI] [PubMed] [Google Scholar]
- 58. Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013;61:278‐283. [DOI] [PubMed] [Google Scholar]
- 59. Omboni S, Aristizabal D, De la Sierra A, et al. Hypertension types defined by clinic and ambulatory blood pressure in 14 143 patients referred to hypertension clinics worldwide. Data from the ARTEMIS study. J Hypertens. 2016;34:2187‐2198. [DOI] [PubMed] [Google Scholar]
- 60. Li Y, Staessen JA, Lu L, Li LH, Wang GL, Wang JG. Is isolated nocturnal hypertension a novel clinical entity? Findings from a Chinese population study. Hypertension. 2007;50:333‐339. [DOI] [PubMed] [Google Scholar]
- 61. Kario K. Global Impact of 2017 American Heart Association/American College of Cardiology Hypertension Guidelines: A perspective from Japan. Circulation. 2018;137:543‐545. [DOI] [PubMed] [Google Scholar]
- 62. Kario K, Wang JG. Could 130/80 mm Hg be adopted as the diagnostic threshold and management goal of hypertension in consideration of the characteristics of Asian Populations? Hypertension. 2018;71:979‐984. [DOI] [PubMed] [Google Scholar]
- 63. Wang JG, Liu L. Global Impact of 2017 American College of Cardiology/American Heart Association Hypertension Guidelines: A Perspective From China. Circulation. 2018;137:546‐548. [DOI] [PubMed] [Google Scholar]
- 64. Hodgkinson J, Mant J, Martin U, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011;342:d3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Grossman E. Ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Diabetes Care. 2013;36(Suppl 2):S307‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hara A, Tanaka K, Ohkubo T, et al. Ambulatory versus home versus clinic blood pressure: the association with subclinical cerebrovascular diseases: the Ohasama Study. Hypertension. 2012;59:22‐28. [DOI] [PubMed] [Google Scholar]
- 67. Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens. 2000;18:847‐854. [DOI] [PubMed] [Google Scholar]
- 68. Burr ML, Dolan E, O'Brien EW, O'Brien ET, McCormack P. The value of ambulatory blood pressure in older adults: the Dublin outcome study. Age Ageing. 2008;37:201‐206. [DOI] [PubMed] [Google Scholar]
- 69. Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp‐Pedersen C. Ambulatory blood pressure and mortality: a population‐based study. Hypertension. 2005;45:499‐504. [DOI] [PubMed] [Google Scholar]
- 70. Huang CM, Wang KL, Cheng HM, et al. Central versus ambulatory blood pressure in the prediction of all‐cause and cardiovascular mortalities. J Hypertens. 2011;29:454‐459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kaneda R, Kario K, Hoshide S, Umeda Y, Hoshide Y, Shimada K. Morning blood pressure hyper‐reactivity is an independent predictor for hypertensive cardiac hypertrophy in a community‐dwelling population. Am J Hypertens. 2005;18:1528‐1533. [DOI] [PubMed] [Google Scholar]
- 72. Pregowska‐Chwala B, Prejbisz A, Kabat M, et al. Morning blood pressure surge and markers of cardiovascular alterations in untreated middle‐aged hypertensive subjects. J Am Soc Hypertens. 2016;10(790–798):e792. [DOI] [PubMed] [Google Scholar]
- 73. Yano Y, Hoshide S, Inokuchi T, Kanemaru Y, Shimada K, Kario K. Association between morning blood pressure surge and cardiovascular remodeling in treated elderly hypertensive subjects. Am J Hypertens. 2009;22:1177‐1182. [DOI] [PubMed] [Google Scholar]
- 74. Alpaydin S, Turan Y, Caliskan M, et al. Morning blood pressure surge is associated with carotid intima‐media thickness in prehypertensive patients. Blood Press Monit. 2017;22:131‐136. [DOI] [PubMed] [Google Scholar]
- 75. Caliskan M, Caliskan Z, Gullu H, et al. Increased morning blood pressure surge and coronary microvascular dysfunction in patient with early stage hypertension. J Am Soc Hypertens. 2014;8:652‐659. [DOI] [PubMed] [Google Scholar]
- 76. Fan HQ, Li Y, Thijs L, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010;28:2036‐2045. [DOI] [PubMed] [Google Scholar]
- 77. Hoshide S, Kario K, Hoshide Y, et al. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community‐dwelling normotensives. Am J Hypertens. 2003;16:434‐438. [DOI] [PubMed] [Google Scholar]
- 78. Mousa T, Elsayed M, Motawea A, Salama M, Elhendy A. Association of blunted nighttime blood pressure dipping with coronary artery stenosis in men. Am J Hypertens. 2004;17:977‐980. [DOI] [PubMed] [Google Scholar]
- 79. Chen CH, Ting CT, Lin SJ, et al. Relation between diurnal variation of blood pressure and left ventricular mass in a Chinese population. Am J Cardiol. 1995;75:1239‐1243. [PubMed] [Google Scholar]
- 80. Hoshide S, Ishikawa J, Eguchi K, Ojima T, Shimada K, Kario K. Masked nocturnal hypertension and target organ damage in hypertensives with well‐controlled self‐measured home blood pressure. Hypertens Res. 2007;30:143‐149. [DOI] [PubMed] [Google Scholar]
- 81. Jerrard‐Dunne P, Mahmud A, Feely J. Circadian blood pressure variation: relationship between dipper status and measures of arterial stiffness. J Hypertens. 2007;25:1233‐1239. [DOI] [PubMed] [Google Scholar]
- 82. Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension. 1996;27:130‐135. [DOI] [PubMed] [Google Scholar]
- 83. Watanabe N, Imai Y, Nagai K, et al. Nocturnal blood pressure and silent cerebrovascular lesions in elderly Japanese. Stroke. 1996;27:1319‐1327. [DOI] [PubMed] [Google Scholar]
- 84. Cho N, Hoshide S, Nishizawa M, Fujiwara T, Kario K. Relationship between blood pressure variability and cognitive function in elderly patients with good blood pressure control. Am J Hypertens. 2018;31:293‐298. [DOI] [PubMed] [Google Scholar]
- 85. Sakakura K, Ishikawa J, Okuno M, Shimada K, Kario K. Exaggerated ambulatory blood pressure variability is associated with cognitive dysfunction in the very elderly and quality of life in the younger elderly. Am J Hypertens. 2007;20:720‐727. [DOI] [PubMed] [Google Scholar]
- 86. Hoshide S, Wang JG, Park S, et al. Treatment considerations of clinical physician on hypertension management in Asia. Curr Hypertens Rev. 2016;12:164‐168. [DOI] [PubMed] [Google Scholar]
- 87. Picone DS, Deshpande RA, Schultz MG, et al. Nonvalidated home blood pressure devices dominate the online marketplace in Australia: Major implications for cardiovascular risk management. Hypertension. 2020;75:1593‐1599. [DOI] [PubMed] [Google Scholar]
- 88. Hoshide S, Yano Y, Haimoto H, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge‐Home Blood Pressure Study. Hypertension. 2016;68:54‐61. [DOI] [PubMed] [Google Scholar]
- 89. Kario K, Shimbo D, Hoshide S, et al. Emergence of home blood pressure‐guided management of hypertension based on global evidence. Hypertension. 2019;74:229‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Franklin SS, O'Brien E, Thijs L, Asayama K, Staessen JA. Masked hypertension: a phenomenon of measurement. Hypertension. 2015;65:16‐20. [DOI] [PubMed] [Google Scholar]
- 91. Tomitani N, Hoshide S, Kario K. Self‐measured worksite blood pressure and its association with organ damage in working adults: Japan Morning Surge Home Blood Pressure (J‐HOP) worksite Study. J Clin Hypertens (Greenwich). 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta‐analysis. Lancet. 2016;387:957‐967. [DOI] [PubMed] [Google Scholar]
- 93. Staessen JA, Byttebier G, Buntinx F, Celis H, O'Brien ET, Fagard R. Antihypertensive treatment based on conventional or ambulatory blood pressure measurement. A randomized controlled trial. Ambulatory Blood Pressure Monitoring and Treatment of Hypertension Investigators. JAMA. 1997;278:1065‐1072. [PubMed] [Google Scholar]
- 94. Uallachain GN, Murphy G, Avalos G. The RAMBLER study: the role of ambulatory blood pressure measurement in routine clinical practice: a cross‐sectional study. Ir Med J. 2006;99:276‐279. [PubMed] [Google Scholar]
- 95. Banegas JR, de la Cruz JJ, Graciani A, et al. Impact of ambulatory blood pressure monitoring on reclassification of hypertension prevalence and control in older people in Spain. J Clin Hypertens (Greenwich). 2015;17:453‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. O'Brien E, White WB, Parati G, Dolan E. Ambulatory blood pressure monitoring in the 21st century. J Clin Hypertens (Greenwich). 2018;20:1108‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. de la Sierra A, Segura J, Banegas JR, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898‐902. [DOI] [PubMed] [Google Scholar]
- 98. Brambilla G, Bombelli M, Seravalle G, et al. Prevalence and clinical characteristics of patients with true resistant hypertension in central and Eastern Europe: data from the BP‐CARE study. J Hypertens. 2013;31:2018‐2024. [DOI] [PubMed] [Google Scholar]
- 99. Wang JG, Kario K, Lau T, et al. Use of dihydropyridine calcium channel blockers in the management of hypertension in Eastern Asians: a scientific statement from the Asian Pacific Heart Association. Hypertens Res. 2011;34:423‐430. [DOI] [PubMed] [Google Scholar]
- 100. Eguchi K, Kario K, Hoshide Y, et al. Comparison of valsartan and amlodipine on ambulatory and morning blood pressure in hypertensive patients. Am J Hypertens. 2004;17:112‐117. [DOI] [PubMed] [Google Scholar]
- 101. Kario K, Hoshide S. Age‐related difference in the sleep pressure‐lowering effect between an angiotensin II receptor blocker and a calcium channel blocker in Asian hypertensives: the ACS1 Study. Hypertension. 2015;65:729‐735. [DOI] [PubMed] [Google Scholar]
- 102. Rothwell PM, Howard SC, Dolan E, et al. Effects of beta blockers and calcium‐channel blockers on within‐individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469‐480. [DOI] [PubMed] [Google Scholar]
- 103. Kario K, Hoshide S, Uchiyama K, et al. Dose timing of an Angiotensin II Receptor Blocker/Calcium Channel Blocker combination in hypertensive patients with paroxysmal atrial fibrillation. J Clin Hypertens (Greenwich). 2016;18:1036‐1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Fujiwara T, Hoshide S, Yano Y, Kanegae H, Kario K. Comparison of morning vs bedtime administration of the combination of valsartan/amlodipine on nocturnal brachial and central blood pressure in patients with hypertension. J Clin Hypertens (Greenwich). 2017;19:1319‐1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kario K, Tomitani N, Kanegae H, et al. Comparative Effects of an Angiotensin II Receptor Blocker (ARB)/Diuretic vs. ARB/Calcium‐channel blocker combination on uncontrolled nocturnal hypertension evaluated by information and communication technology‐based nocturnal home blood pressure monitoring‐ the NOCTURNE study. Circ J. 2017;81:948‐957. [DOI] [PubMed] [Google Scholar]
- 106. Fujiwara T, Tomitani N, Kanegae H, Kario K. Comparative effects of valsartan plus either cilnidipine or hydrochlorothiazide on home morning blood pressure surge evaluated by information and communication technology‐based nocturnal home blood pressure monitoring. J Clin Hypertens (Greenwich). 2018;20:159‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Kandzari DE, Böhm M, Mahfoud F, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6‐month efficacy and safety results from the SPYRAL HTN‐ON MED proof‐of‐concept randomised trial. Lancet. 2018;391:2346‐2355. [DOI] [PubMed] [Google Scholar]
- 108. Kario K, Bohm M, Mahfoud F, et al. Twenty‐four‐hour ambulatory blood pressure reduction patterns after renal denervation in the SPYRAL HTN‐OFF MED Trial. Circulation. 2018;138:1602‐1604. [DOI] [PubMed] [Google Scholar]
- 109. Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter‐based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN‐OFF MED): a randomised, sham‐controlled, proof‐of‐concept trial. Lancet. 2017;390:2160‐2170. [DOI] [PubMed] [Google Scholar]
- 110. Imai Y, Obara T, Asamaya K, Ohkubo T. The reason why home blood pressure measurements are preferred over clinic or ambulatory blood pressure in Japan. Hypertens Res. 2013;36:661‐672. [DOI] [PubMed] [Google Scholar]
- 111. Mancia G, Bombelli M, Brambilla G, et al. Long‐term prognostic value of white coat hypertension: an insight from diagnostic use of both ambulatory and home blood pressure measurements. Hypertension. 2013;62:168‐174. [DOI] [PubMed] [Google Scholar]
- 112. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3‐15. [DOI] [PubMed] [Google Scholar]
- 113. Guidelines for the clinical use of 24 hour ambulatory blood pressure monitoring (ABPM) (JCS 2010): ‐ digest version. Circ J. 2010;2012(76):508‐519. [DOI] [PubMed]
- 114. Tamaki Y, Ohkubo T, Kobayashi M, et al. [Cost effectiveness of hypertension treatment based on the measurement of ambulatory blood pressure]. Yakugaku Zasshi. 2010;130:805‐820. [DOI] [PubMed] [Google Scholar]
- 115. Kario K. Nocturnal hypertension: new technology and evidence. Hypertension. 2018;71:997‐1009. [DOI] [PubMed] [Google Scholar]
- 116. Wang JG. Unique approaches to hypertension control in China. Ann Transl Med. 2018;6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Kario K. Hemodynamic biomarker‐Initiated anticipation medicine in the future management of hypertension. Am J Hypertens. 2017;30:226‐228. [DOI] [PubMed] [Google Scholar]
- 118. Kario K, Tomitani N, Kanegae H, et al. Development of a new ICT‐based multisensor blood pressure monitoring system for use in hemodynamic biomarker‐initiated anticipation medicine for cardiovascular disease: the National IMPACT Program project. Prog Cardiovasc Dis. 2017;60:435‐449. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


