Abstract
Over one‐third of the population in Indonesia has hypertension, almost two‐thirds of treated patients have uncontrolled blood pressure (BP), and the majority of patients with hypertension also have comorbidities. Home BP monitoring (HBPM) is a useful tool for diagnosing and managing hypertension. The use of HBPM is recommended by the latest consensus from the Indonesian Society of Hypertension (2019), and nearly, all doctors recommend HBPM for hypertensive patients. However, the use of HBPM in Indonesia is limited by the cost of devices and a perception that these devices are unreliable. In addition, knowledge about proper procedures is lacking. Withdrawal of mercury sphygmomanometers from the end of 2018 is expected to encourage the use of digital sphygmomanometers and the implementation of HBPM. The most common antihypertensive agent used in Indonesia varies by patient age, being angiotensin‐converting enzyme (ACE) inhibitors in those aged 40‐60 years and calcium channel blockers (CCBs) in older patients. Across all age groups, combination therapy with a CCB plus an angiotensin receptor blocker was common (41%‐42% of patients). The high prevalence of hypertension in Indonesia has an important economic impact, and approaches to increase awareness of the disease and adherence to therapy are needed, particularly given data showing the benefits of strict BP control.
Keywords: home blood pressure monitor, hypertension, Indonesia
1. CARDIOVASCULAR DISEASE INCIDENCE AND HYPERTENSION MANAGEMENT IN INDONESIA
Hypertension is the most significant risk factor contributing to disease burden in Southeast Asia, East Asia, and Oceania.1 The largest standardized screening campaign for blood pressure (BP) measurement, May Measurement Month (MMM) in 2017, showed that 34.5% of 69 307 individuals screened in Indonesia had hypertension.2 Of these, 20% were untreated, and 63% of those receiving antihypertensive medication had uncontrolled BP.2 Awareness and control rates were also low in another analysis, which showed that, of the 47.8% of patients who had hypertension, 70% had not received a formal diagnosis.3 Only 37% of patients with hypertension were aware that they had the disease, and only 25% had well‐controlled BP.3
A preliminary analysis in 2018 showed an increase in the prevalence of hypertension in Indonesia to 34.1% (from 26.5% in 2013), with the highest prevalence in the province of South Kalimantan (44.1%), and the lowest in Papua (22.2%).4 This increment was accompanied by an increase in other vascular risk factors such as diabetes, obesity, smoking, lack of physical activity, and prevalence of stroke.4 Only 28.0% of patients with hypertension in Indonesia do not have any comorbidities.3
2. CURRENT STATUS OF HBPM MONITORING IN THE MANAGEMENT OF HYPERTENSION IN INDONESIA
Use of home BP monitoring (HBPM), conditions such as white‐coat hypertension, masked morning hypertension, and controlled hypertension can be detected.5, 6 There are two main reasons why HBPM is not routinely conducted in Indonesia. The first is that digital BP monitors are expensive and are only affordable for a subset of individuals. Secondly, there is a perception that HBPM devices are unreliable. Nevertheless, a survey of general practitioners and specialists (n = 606) from Jakarta in February 2019 showed that most doctors (95.3%) recommended HBPM in hypertensive patients.7 The main reason for recommending HBPM was to evaluate the success of therapy (80.3%) and variations in BP (65%). Nearly half of the respondents (47.3%) recommended measurement of home BP every day, with 21.0% suggesting measurement three times/week and 60.7% recommending measurement two times/week; only 28.3% suggested using average measurements in the recording.7 Although most healthcare practitioners suggested HBPM, there was still a low level of knowledge about the technique. For example, 14.7% of respondents stated that target HBPM was <140 mm Hg, and detailed instructions were lacking (only 66.2% of respondents instructed patients to measure home BP after urinating, 53.0% before taking antihypertensive medication, and 34.8% provided no instructions relating to timing of measurement before or after meals).7 Challenges associated with HBPM included limited follow‐up/consultation time (50.3%) and poor patient compliance (63.0%).7
3. INDONESIA SUB‐ANALYSIS OF THE ASIABP@HOME STUDY
AsiaBP@Home study6, 8 data from Indonesia (n = 202) showed that 32% and 36% of patients had well‐controlled clinic and morning home BP, respectively, based on conventional thresholds. Changing to the new 2017 American College of Cardiology (ACC)/American Heart Association (AHA) threshold had a significant impact on the proportion of patients in both categories, decreasing to 13% and 26%, respectively. In addition, only 10% of patients remained well‐controlled for morning BP using the new threshold, which is a much lower rate than when conventional thresholds are used (Figure 1).
Figure 1.
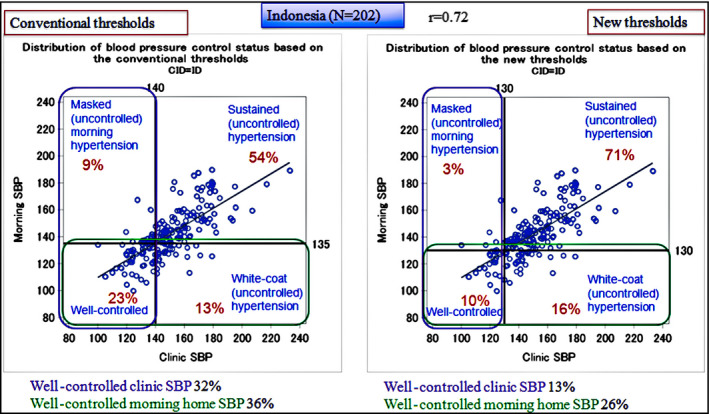
Distributions of blood pressure (BP) control status based on different clinic and morning home BP thresholds in the Indonesia sub‐analysis from the AsiaBP@Home study. Left panel represents the results based on cut‐off values of 140 mm Hg for clinic systolic BP (SBP) and 135 mm Hg for home SBP. Right panel represents the results based on cut‐off values of 130 mm Hg for both clinic SBP and home SBP
4. POSITIONING OF HBPM IN THE INDONESIAN HYPERTENSION GUIDELINES
Current use of HBPM in Indonesia is based on guidance from the HOPE Asia Network9, 10 and the 2019 Indonesian Society of Hypertension (InaSH).11 The new InaSH hypertension consensus was launched at the society's 2019 meeting, which highlighted the vital role of HBPM and provided guidelines for its use.11 There has been a focus on increasing the use of HBPM in Indonesia since 2018.12 At the end of 2018, the Indonesian Ministry of Health issued a regulation for the withdrawal of mercury sphygmomanometers. This is expected to encourage the use of digital sphygmomanometers and the implementation of HBPM.
5. TRADITIONAL ANTIHYPERTENSIVE THERAPY AND POPULAR ANTIHYPERTENSIVE DRUGS IN INDONESIA
Local data show that antihypertensive agents given as monotherapy in patients aged 40‐60 years were mostly angiotensin‐converting enzyme (ACE) inhibitors (46.1%) and calcium channel blockers (CCBs; 25.7%); only 18.1% of patients were using angiotensin receptor blockers (ARBs). For those aged >60 years, CCBs were most common (43.5%), followed by ARBs (25.7%) and ACE inhibitors (20.3%). Nearly half of all patients across all age groups who received combination therapy (41%‐42%) were using CCB + ARB. 7
6. SPECIFIC CONCERNS AND PERSPECTIVES FOR HYPERTENSION MANAGEMENT IN INDONESIA
Despite a number of campaigns over the last decade, awareness of hypertension in Indonesia remains low.3 Furthermore, polypharmacy is common due to hypertension‐related comorbidities, meaning that compliance with treatment is low.13 The high prevalence of hypertension has an important economic impact. According to national insurance data, the amount spent on hypertension services increases every year, from IDR 2.8 trillion in 2014 to IDR 4.2 billion in 2016.14 Intensive treatment of hypertension could significantly reduce the risk of developing cardio‐ and cerebrovascular disease, including target organ damage and mortality.15, 16, 17 The 2019 InaSH consensus recommends lower targets than previous guidelines: systolic BP ≤130 mm Hg but no <120 mm Hg, if tolerated by the patient.11
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
All Author contributed to the concept, review, and revision of the final version of the manuscript.
ACKNOWLEDGMENTS
English language editing assistance was provided by Nicola Ryan, independent medical writer, funded by the HOPE Asia Network.
Turana Y, Tengkawan J, Soenarta AA. Asian management of hypertension: Current status, home blood pressure, and specific concerns in Indonesia. J Clin Hypertens. 2020;22:483–485. 10.1111/jch.13681
REFERENCES
- 1. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Widyantoro B, Situmorang TD, Turana Y, et al. May measurement month 2017: an analysis of the blood pressure screening campaign results in Indonesia‐South‐East Asia and Australasia. Eur Heart J Suppl. 2019;21:D63‐D65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hussain MA, Mamun AA, Reid C, et al. Prevalence, awareness, treatment and control of hypertension in Indonesian adults aged >/=40 years: findings from the Indonesia family life survey (IFLS). PLoS One. 2016;11:e0160922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ministry of Health and National Institute of Health Research and Development . National report on basic health research, Riskesdas, 2018. Jakarta, Indonesia, 2018. [Google Scholar]
- 5. Chia YC, Buranakitjaroen P, Chen CH, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2017;19:1192‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kario K, Tomitani N, Buranakitjaroen P, et al. Rationale and design for the Asia BP@Home study on home blood pressure control status in 12 Asian countries and regions. J Clin Hypertens (Greenwich). 2018;20:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Turana Y, Suswanti I, Soenarta AA, et al. Diagnosis and treatment of hypertension: gaps between guideines and clinical practices in Indonesia (in press), 2019. [Google Scholar]
- 8. Kario K, Tomitani N, Buranakitjaroen P, et al. Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: results of the Asia BP@Home study. J Clin Hypertens (Greenwich). 2018;20:1686‐1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kario K, Park S, Buranakitjaroen P, et al. Guidance on home blood pressure monitoring: a statement of the HOPE Asia Network. J Clin Hypertens (Greenwich). 2018;20:456‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Park S, Buranakitjaroen P, Chen C‐H, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249‐258. [DOI] [PubMed] [Google Scholar]
- 11. Indonesian Society of Hypertension . Treatment of Hypertension Consensus. Jakarta, Indonesia: Indonesian Society of Hypertension; 2019. [Google Scholar]
- 12. Media Indonesia . Monitor blood pressure to prevent deadly complications (media release). Available from: http://mediaindonesia.com/read/detail/147166-cek-tekanan-darah-cegah-komplikasi-mematikan. Accessed 21 Mar 2019.
- 13. Sumantra IG. The level of medication compliance of hypertension in adults and elderly patients (abstract). J Hypertens. 2015;33:e43. [Google Scholar]
- 14. Kesehatan BPJS. Prevent cardiometabolic risks by PROLANIS optimalization, 2017. Available from: https://www.bpjs-kesehatan.go.id/bpjs/index.php/post/read/2017/536/Avoid-Cardiometabolic-by-Optimalized-PROLANIS. Accessed 6 Mar, 2019.
- 15. Williamson JD, Pajewski NM, Auchus AP, et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321:553‐561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yaffe K. Prevention of cognitive impairment with intensive systolic blood pressure control. JAMA. 2019;321:548‐549. [DOI] [PubMed] [Google Scholar]


