Abstract
At the time of the Great East Japan earthquake and tsunami (March 2011), the authors developed a web‐based information and communications technology (ICT)–based blood pressure (BP) monitoring system (the Disaster CArdiovascular Prevention [DCAP] Network) and introduced it in an area that was catastrophically damaged (Minamisanriku town) to help control the survivors' BP. Using this system, home BP (HBP) was monitored and the data were automatically transmitted to a central computer database and to the survivors' attending physicians. The study participants, 341 hypertensive patients, continued to use this system for 4 years after the disaster and all of the obtained HBP readings were analyzed. This DCAP HBP‐guided approach helped achieve a decrease in the participants' HBPs (initial average: 151.3±20.0/86.9±10.2 mm Hg to 120.2±12.1/70.8±10.2 mm Hg) over the 4 years. In addition, the amplitude of seasonal BP variation was suppressed and the duration from the summer lowest HBP values to the winter peak HBP values was gradually prolonged. This ICT‐based approach was useful to achieve strict HBP control and minimize the seasonal BP variation even in a catastrophically damaged area during a 4‐year period after the disaster, suggesting that this approach could be a routine way to monitor BP in the community.
Japan has experienced several major earthquakes over the past few decades. Most recently, on April 14, 2016, at 9:26 pm (local time), a strong earthquake (magnitude 6.5) occurred in the Kumamoto area of Kyushu, followed by a second, stronger earthquake (magnitude 7.3) on April 16, 2016, at 1:25 am. Immediately after the Kumamoto earthquake occurred, the Japanese Society of Hypertension (JSH) issued online messages (JSH Online, April 16, 2016) to physicians in the JSH network with guidelines for the management of disaster‐related cardiovascular disease.1
Hypertension is one of the important triggers of disaster‐related cardiovascular disease.2, 3 The control of blood pressure (BP) is important to prevent cardiovascular disease after a major disaster. The March 11, 2011, Great East Japan Earthquake that occurred in Tohoku, in the northeast region of Honshu, Japan's main island, had a magnitude of 9.0. A significant characteristic of this earthquake is that it triggered a huge tsunami. Immediately after that earthquake, we developed a web‐based home BP (HBP) monitoring system (the Disaster CArdiovascular Prevention [DCAP] Network), and we introduced the DCAP network into a catastrophically damaged town, Minamisanriku‐cho—where the tsunami destroyed approximately 60% of the residential area and completely destroyed all medical resources—for better control of the survivors' BP.4, 5
It has been documented that self‐measured HBP has a stronger association with cardiovascular disease risk compared with office BP, and several guidelines have thus recommended the use of HBP measurement for the management of hypertension.6, 7 Although there have been reports on an increase in HBP after a major earthquake, all of these reports were only short‐term, retrospective surveys.8, 9, 10, 11, 12 To the best of our knowledge, there are no reports of the long‐term follow‐up of HBP data after a disaster.
The DCAP network is still a work in progress, and even 5 years after the Great East Japan earthquake, patients continue to measure their HBP. The present report is the first regarding a real‐world long‐term follow‐up of HBP control status after the introduction of an information and communications technology (ICT)–based BP management system in a catastrophically damaged area after a major disaster.
Participants and Methods
We have described the DCAP network in earlier reports.4, 5 Briefly, this ICT‐based system was implemented after the 2011 Great East Japan Earthquake to reduce the risks of disaster‐associated cardiovascular events among the residents of disaster areas. We asked survivors to answer a survey on risk and preventive scores, taking advantage of our previous experience with the 1995 Hanshin‐Awaji earthquake, and we provided real‐time feedback to these survivors. With this system, in order to formulate an approach to the management of disaster‐related hypertension, we instructed the patients to perform HBP monitoring as described below, and the BP data obtained were automatically transmitted to a central computer database.
The participants were survivors visiting the Shizugawa clinic, a temporary structure built next to the main shelter of the town of Minamisanriku. Each participant was given an automated HBP monitoring device (UA767PBT‐C, A&D, Saitama, Japan). All of the participants were hypertensive with office BP >140/90 mm Hg, or were taking antihypertensive medication, when they were enrolled in the study. After a participant was enrolled in the study, we asked him or her to measure the seated HBP twice a day, once in the morning and once in the evening. We calculated the monthly average BP values. During the course of this study, lifestyle modification counseling and antihypertensive treatment were performed by one physician (M.N.) at the Shizugawa clinic, based on the 2014 JSH guidelines.6 An “increase in antihypertensive medication” was defined as the addition of a different antihypertensive drug or an increase in the dose of an antihypertensive drug that the participant was taking. A “decrease in antihypertensive medication” was defined as the discontinuation of an antihypertensive drug or a decrease in the dose of an antihypertensive drug. The monthly average outdoor temperatures in the area were obtained from the Shizugawa Meteorological Observatory. In our statistical considerations, our main perspective concerned overall changes in HBP readings after the disaster. These analyses used all of the available data.
The study protocol was approved by the ethics committee of the Jichi Medical University School of Medicine. We received informed consent from all patients for this research.
Results
The HBP readings of 351 participants were monitored via the DCAP network during the period of May 2011 to June 2015 (the recent Great East Japan Earthquake occurred on March 11, 2011). Thus, the HBP monitoring began approximately 7 weeks after the earthquake. The characteristics of the participants are shown in the Table. The Figure illustrates the values of systolic BP (SBP), diastolic BP, pulse rate, monthly temperature average, and percentage change in the increase or decrease in the dosage of antihypertensive drugs. This DCAP HBP‐guided approach helped achieve a decrease in the participants' HBPs (initial average: 151.3±20.0/86.9±10.2 mm Hg on May 2011 to 120.2±12.1/70.8±10.2 mm Hg on June 2015 during the 4 years) (Figure). All of the lowest BP values during each year occurred during the summer months. When we defined the “winter BP surge” as the difference between the lowest BP month in summer and the highest BP month in winter, we observed that during three successive years, these differences gradually decreased to 8.7, 8.1, and 6.9 mm Hg in SBP. In addition, the interval between the lowest BP month in summer and the highest BP in winter increased from 3 months to 5 months and then to 8 months in successive years.
Table 1.
Characteristics of the 351 Hypertensive Participants From the Earthquake‐Ravaged Town of Minamisanriku, Japan, in May 2011
| Age, y | 71.2±12.1 |
| Men/women, No. (%) | 151/200 (43/57) |
| Body mass index, kg/m2 | 24.7±3.8 |
| Death/hospitalization of one or more family members, % | 12.2 |
| Completely or partially (>half) destroyed housing, % | 59.7 |
| Diabetes, % | 18.6 |
| Medical history, % | |
| Angina | 3.4 |
| Myocardial infarction | 0.6 |
| Heart failure | 0.6 |
| Stroke | 3.1 |
Data are shown as mean±standard deviation or percentage.
Figure 1.
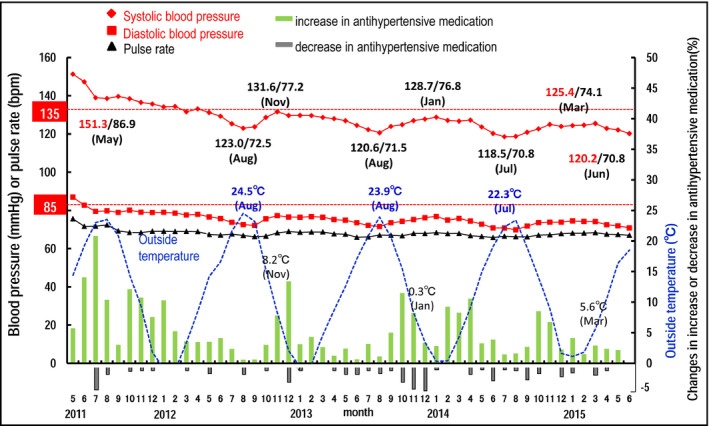
Changes in blood pressure, pulse rate, outside temperature, and increase or decrease in antihypertensive medication by the 351 participants after the March 2011 Great East Japan Earthquake and tsunami.
Discussion
In this study, we prospectively introduced an ICT‐based HBP monitoring system (the DCAP system) to facilitate the BP control of participants in the acute post‐disaster phase in an area catastrophically damaged by the Great East Japan Earthquake and Tsunami, where the medical resources had been markedly destroyed. We have successfully continued this DCAP system for more than 5 years as of April 30, 2016, and the participants in this system have achieved strict HBP control at around 120/70 mm Hg. There have been some reports about data collected from disaster survivors who measured their HBP readings themselves,8, 9, 10, 11, 12 but those reports were of short‐term retrospective surveys of patients who were already recording their own HBP readings before the disaster. The present study is the first prospective intervention to demonstrate that an ICT‐based approach is feasible just after a disaster, and that such an approach is useful for long‐term strict HBP control.
Strict BP Control
In this study, strict BP control to around 120 to 125 mm Hg in SBP has been successfully achieved. Recently, the Systolic Blood Pressure Intervention Trial (SPRINT)13 clearly demonstrated that strict office SBP at <120 mm Hg was superior to the usual office SBP at <140 mm Hg for reducing cardiovascular events. The Home BP Measurement With Olmesartan‐Naive Patients to Establish Standard Target Blood pressure (HONEST) study,14, 15 an observational study of the relationship between HBP readings and cardiovascular events, showed that home SBP readings associated with minimum risk were <125 mm Hg. From those previous results, the strict BP control in our findings might effectively prevent cardiovascular events.
Seasonal BP Variation
To our knowledge, there has been no study on the seasonal variation of BP after a disaster. Several unique findings of our study emerged when we explored the seasonal variation of BP. First, there was no significant seasonal BP variation in the first year after the disaster, but there was variation found beginning in the second year. This means that a short‐term pressor effect of a disaster might overwhelm the seasonal variation of BP by this long‐term HBP monitoring. However, the prevalence of increase in antihypertensive drug was high during the first year. Hence, the effect of antihypertensive drugs might also mask the seasonal variation of BP. Second, our data demonstrated that the amplitude of winter BP surge each year was gradually suppressed. Third, the peak of winter BP surge was gradually delayed year after year by the ICT‐based antihypertensive approach. When we look at the trend in drug titration, we see that early intervention, using aggressive antihypertensive treatment by the immediate judgment of drug titration, was initiated from autumn to winter based on the anticipation of the tendency of winter BP surge using the time‐trend of BP control, which was first made available by ICT‐based HBP monitoring systems. As the winter BP surge may partly account for the increase in cardiovascular events in the winter, especially in elderly hypertensive patients,16 our findings indicate that an individual ICT‐based HBP monitoring approach for the management of hypertension might enable the suppression of seasonal BP variation, contributing to the reduction of winter increase in cardiovascular events.
Study Limitations
We could not assess the direct pressor effect of the earthquake. The tsunami washed away all of the town's medical records, and thus no BP data from before the disaster were available (Figure S1). In addition, we did not perform a comparison with residents of areas that were not damaged by the earthquake/tsunami. Thus, strictly the impact of the disaster on the initial HBP values of the hypertensive patients in this study was not evaluated.
Conclusions
This is the first long‐term follow‐up study demonstrating that strict BP control with a minimized winter BP surge is feasible by using an ICT‐based HBP monitoring system from the acute to chronic phases after a disaster. The question of whether the ICT‐based individual approach could be a routine way to monitor BP in communities for the effective prevention of cardiovascular events should be addressed in future studies.
Disclosure
The authors declare no conflict of interest.
Supporting information
Figure S1. Tsunami is hitting. The building in the center of picture was only one hospital in Minamisanriku‐town where the first author was working.
Acknowledgments
This study was financially supported in part by a grant from Banyu Life Science Foundation International and a grant from the Japanese Circulation Society.
J Clin Hypertens (Greenwich). 2017;19:26–29. DOI: 10.1111/jch.12864. © 2016 Wiley Periodicals, Inc.
References
- 1. JCS, JSH and JCC Joint Working Group . Guidelines for disaster medicine for patients with cardiovascular diseases (JCS 2014/JSH 2014/JCC – digest version. Circ J. 2015;80:261–284. [DOI] [PubMed] [Google Scholar]
- 2. Kario K, McEwen BS, Pickering TG. Disasters and the heart: a review of the effects of earthquake‐induced stress on cardiovascular disease. Hypertens Res. 2003;26:355–367. [DOI] [PubMed] [Google Scholar]
- 3. Kario K. Disaster hypertension – its characteristics, mechanism, and management. Circ J. 2012;76:553–562. [DOI] [PubMed] [Google Scholar]
- 4. Kario K, Nishizawa M, Hoshide S, et al. Development of a disaster cardiovascular prevention network. Lancet. 2011;378:1125–1127. [DOI] [PubMed] [Google Scholar]
- 5. Nishizawa M, Hoshide S, Shimpo M, Kario K. Disaster hypertension: experience from the Great East Japan Earthquake of 2011. Curr Hypertens Rep. 2012;14:375–381. [DOI] [PubMed] [Google Scholar]
- 6. Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–387. [DOI] [PubMed] [Google Scholar]
- 7. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 8. Minami J, Kawano Y, Ishimitsu T, et al. Effect of the Hanshin‐Awaji earthquake on home blood pressure in patients with essential hypertension. Am J Hypertens. 1997;10:222–225. [DOI] [PubMed] [Google Scholar]
- 9. Gerin W, Chaplin W, Schwartz JE, et al. Sustained blood pressure increase after an acute stressor: the effects of the 11 September 2001 attack on the New York City World Trade Center. J Hypertens. 2005;23:279–284. [DOI] [PubMed] [Google Scholar]
- 10. Watanabe K, Tani Y, Tanaka K, et al. Acute changes in home blood pressure after the Great East Japan Earthquake among patients with chronic kidney disease in Fukushima City. Clin Exp Nephrol. 2013;17:718–724. [DOI] [PubMed] [Google Scholar]
- 11. Satoh M, Kikuya M, Ohkubo T, Imai Y. Acute and subacute effects of the Great East Japan Earthquake on home blood pressure values. Hypertension. 2011;58:e193–e194. [DOI] [PubMed] [Google Scholar]
- 12. Tanaka K, Nakayama M, Kanno M, et al. Home blood pressure control after the Great East Japan Earthquake in patients on chronic hemodialysis. Ther Aphere Dial. 2014;18:149–154. [DOI] [PubMed] [Google Scholar]
- 13. Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. New Engl J Med. 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large‐scale prospective, real‐world observational study. Hypertension. 2014;64:989–996. [DOI] [PubMed] [Google Scholar]
- 15. Kario K, Saito I, Kushiro T, et al. Morning home blood pressure a strong predictor of coronary artery disease: the HONEST Study. J Am Coll Cardiol. 2016;67:1519–1527. [DOI] [PubMed] [Google Scholar]
- 16. Kario K. Caution for winter morning surge in blood pressure: a possible link with cardiovascular risk in the elderly. Hypertension. 2006;47:139–140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Tsunami is hitting. The building in the center of picture was only one hospital in Minamisanriku‐town where the first author was working.


