Abstract
Background:
Identifying factors that contribute to the occurrence of injury is an important step in designing training programs to minimize the risk of injury. However, despite high injury rates, variables contributing to injury in field hockey players remain relatively unexplored.
Purpose:
To identify factors that may predict injury in professional and youth field hockey players.
Study Design:
Cohort study; Level of evidence, 2.
Method:
Professional and youth hockey players completed preseason neuromuscular performance testing and were monitored for injuries, training, and game exposure throughout the subsequent 12-month indoor and outdoor hockey season. Least absolute shrinkage and selection operator analysis was conducted to identify injury risk factors. Receiver operating characteristic curves were then calculated to determine the individual predictive accuracy of the identified variables.
Results:
A total of 83 players (mean ± SD age, 20.7 ± 4.9 years; 34.9% female) with complete performance, injury, and exposure data were included for data analysis. Almost half of players (44.6%) sustained a time-loss injury during the season, and 73% of these injuries occurred in the lower limb. Playing more games and having an older age, asymmetrical and poor dynamic postural control, and better explosive performance were identified as jointly influencing the risk of injury. When considered individually, number of games played throughout the season was the most accurate predictor of injury risk (area under the curve [AUC] = 0.74; P < .001), while asymmetrical and poor dynamic postural control (AUCs = 0.61-0.65; P = .01-.04) and better explosive athletic performance (AUCs = 0.65-0.67; P < .01) were identified as moderate individual predictors of sustaining a general or lower limb injury.
Conclusion:
A number of modifiable factors were individually and jointly associated with an increased injury risk in field hockey players, providing initial evidence for the design of targeted and sport-specific training programs to mitigate the risk of injury.
Keywords: field hockey, injury prediction, risk factors, exposure, neuromuscular performance
Field hockey is a globally prominent sport that is played in 125 countries and has been featured in 23 Olympic Games. Field hockey players are at a high risk of injury that is comparable with the risk observed in other popular team and Olympic sports.25,26,48 A recent study of the German national hockey leagues reported an incidence of 3.7 time-loss injuries per 1000 exposure hours (9.7 game-related injuries per 1000 exposure hours) over a 12-month outdoor and indoor hockey season.25 During periods of increased game congestion, such as in-season tournaments, the reported injury incidence intensifies to between 20.8 and 90.9 injuries per 1000 game hours.52
Although field hockey players uniquely experience a relatively high rate of hand and finger injuries,25 injuries occur most frequently in the lower limb.9,25,40,41 According to Dick et al9 and Hollander et al,25 the most frequently reported injury type in male and female players during a hockey season is thigh muscle strains, especially of the hamstrings. However, the review of Murtaugh41 included more than a dozen studies on injuries during tournaments and playing seasons in junior and elite hockey players and observed that ankle sprains occurred with the highest prevalence.
To address the substantial health, economic, and performance burdens related to injuries,5,10,22 considerable research has recently been devoted to the prevention of injury in team sports. While there is increasing evidence showing the beneficial effect of preventive measures, such as targeted neuromuscular training49 and well-developed physical capacities,17,35,36,42 the success of such interventions is likely enhanced by the reliable identification of factors that are associated with injury risk.
Findings of prospective studies and systematic reviews have indicated a relationship between the likelihood of lower extremity injuries, such as hamstring strains, anterior cruciate ligament ruptures, and ankle sprains, and multiple external or internal factors in team sport athletes.7,21,27,59 While factors such as an increased age and injury history are among the metrics consistently linked with injuries,16,20 modifiable risk factors are of great interest because they provide the potential for risk mitigation through targeted intervention strategies. Widely discussed modifiable injury risk factors for team sports include training and game load, dynamic postural control, muscle strength, flexibility, and proprioception.27,37,44,55,59 The use of neuromuscular screening is widespread, as evidenced by 94% of surveyed elite European football teams performing injury risk screening.32
Despite the popularity of load monitoring and neuromuscular screening, there is inconclusive and conflicting evidence for their potential to identify injury-related risk factors in team sports.27,55 In addition, methodologic limitations, such as study design, cohort overlap, and lack of assessment of potential cutoff values,3 complicate the generalizability of findings. Nonetheless, well-designed injury risk factor analysis that includes predictive analysis constitutes an essential step in disentangling the complex injury matrix and creating evidence-based and successful injury risk mitigation programs.37
Importantly, given that injury mechanisms and the contributing risk factors are likely sport specific,53 each sport should be individually assessed. Although comprehensive risk factor analysis has been performed for other team sports,7,13,21 no such analysis has been performed to identify injury risk factors in field hockey players, despite the global popularity of the sport and its prominence at the Olympic Games. Therefore, to better understand the complex and multifactorial etiology of field hockey injuries and to contribute to the development of evidence-based intervention programs, the aim of this study was to determine the relationship between injuries in hockey players and a spectrum of potential risk factors. We used a comprehensive suite of potential risk factors including external load metrics related to training and game involvement as well as modifiable and nonmodifiable intrinsic factors of athletes to encompass the broad influences on injury occurrence.
Methods
Study Design, Participants, and Injury Surveillance
The setting, recruitment procedure, and inclusion criteria of the current prospective cohort study were previously described by Hollander et al.25 Accordingly, the presidents from all 28 clubs in the regional hockey association of the Hamburg Hockey Federation (Hamburger Hockey-Verband) were contacted. After they agreed to participate, coaches from the first, second, third, regional, and youth division teams (female and male teams) were contacted via email and telephone. Ethical approval was obtained from the local ethics committee, and the medical research guidelines of the Helsinki Declaration were followed. Written consent was obtained from all participants or their parents/legal guardians.
The study consisted of a preseason baseline examination for risk factors and a 12-month prospective documentation of injuries related to practice and games during the 2015-2016 outdoor and indoor hockey season. An injury was defined as any musculoskeletal complaint (acute or chronic) that occurred during the documentation period26 leading to time loss from sport ≥1 day. Injuries were collected using a standardized form by the team physical therapist, physician, or coach.
Risk Factor Assessment
Player Characteristics
Players were measured for height, weight, and leg length at baseline. Leg length was assessed from the greater trochanter to the lower margin of the lateral malleolus. Other relevant information collected at baseline was age; sex; playing position; league; and playing indoor or outdoor season, or both.
External Load Measures
The practice and game exposures of each player were documented by coaches using a standardized report form (modified based on the study of Fuller et al15) on a daily basis and collected weekly by the study staff. Analyzed risk factors were training sessions per week, training minutes per week, and number of games.
Neuromuscular Testing Protocols
Ankle flexibility was measured using the weightbearing lunge test.4 The players stood in a lunge position, facing a wall. The big toe of the tested leg and the knee touched the wall. With the knee kept on the wall, the foot was then moved backward until a maximum distance was reached without lifting the heel. The maximum reach distance from the wall to the big toe was then measured.
A shortened version of the Star Excursion Balance Test (SEBT) was used to evaluate dynamic balance.19,23 Players were instructed to place the foot of the nontested leg in the middle of 6 measuring tapes on the floor. Their hands were placed on the iliac crests. The measuring tapes were aligned in the anterior, anteromedial, anterolateral, posterior, posteromedial, and posterolateral directions. The players were asked to reach the tested leg as far as possible in each direction. The maximum distance reached was measured. Errors were defined as hands losing contact with the iliac crests, lifting the forefoot or heel of the stance leg, or losing balance. If an error occurred, the trial in that direction was repeated. Players were given 3 trials in each direction to familiarize themselves with the test. Reach distances were normalized to leg length by dividing the absolute value by the participant’s leg length.
A sit-and-reach box (Baseline-12 Sit n’ Reach Trunk Flexibility Box; Baseline) was used to evaluate hamstring flexibility.2 Players sat upright with extended knees and with feet touching each other and placed against the sit-and-reach box. They reached their extended arms as far as possible in the direction of the feet without bending their knees. The maximum reach distance was recorded using the metric scale on top of the box.
Jump performance was analyzed using the squat jump, countermovement jump, and depth jump. To perform the squat jump, participants flexed their knees to 90° then jumped upward as high as possible. The countermovement jump required participants to stand in an upright position then bend and jump as high as possible. The depth jump was performed from a box of 40-cm height. Players were asked to leave the box with a step forward and then immediately jump vertically after the foot touched the ground to keep the contact time as short as possible. Each jump test was performed with shoes, hands on the hips, and 3 repetitions per jump condition. The highest squat and countermovement jump heights and the shortest depth jump time were used for data analysis. The jump height and depth jump time were measured using wearable inertial measurement units (Sensor DX3.1; Humotion) secured by a strap on the back of the players.
Maximum sprint time was assessed using the flying 30-m sprint test. Time between 0 and 5 m, 0 and 10 m, and 0 and 30 m was recorded using a magnetic sensor system with magnetic gates (SmarTracks Diagnostics; Humotion). The athletes were asked to choose a starting point several meters before the first magnetic gate, ensuring that the maximum speed was reached at 0 m. The maximum speed was to be maintained over the entire sprint distance. Each athlete was given 3 trials. The best trial with the fastest 30-m time was used for data analysis.
Agility was assessed using the Change-of-Direction and Acceleration Test, which was developed to evaluate speed while running with several changes of direction.40 The test starts with a straight sprint over 5 m and 4 diagonal direction changes (2 × 45° and 2 × 90°) with 3-m sprints in between (zig-zag pattern), and it finishes with a straight sprint over 10 m. The players were instructed to complete the test as quickly as possible.
All neuromuscular tests have been shown to be reliable and valid in previous studies.2,23,29,31,45
Statistical Analysis
All data were collected in a database (Excel for Mac 11, Version 14.7.1; Microsoft Corp), and all statistical analyses were conducted using the statistical software program R (Version 3.6.2; R Core Team). Although the prospective nature of the study limited the risk of bias, separate researchers were responsible for injury screening and data processing to reduce the risk. Descriptive statistics were calculated as means with SDs. Variable selection was conducted by applying a least absolute shrinkage and selection operator (LASSO) logistic regression analysis54 via the glmnet package14 to all injuries and lower limb injuries separately. The LASSO approach refers to an L1 penalization technique that applies a constraint on the sum of the regression coefficients’ absolute values. This way, coefficients are shrunk toward 0, and less important effects can even be set to exactly 0; hence, the corresponding predictors are excluded from the model.
To assess the predictive capacity of the individual risk factors, receiver operating characteristic (ROC) curves were then calculated to determine the area under the curve (AUC) and cutoff score for any variable that the LASSO model identified as being relevant for injury occurrence. The AUC of a ROC curve reflects how capable a variable is of distinguishing between athletes who sustained an injury and those who remained uninjured.1,46 An AUC value equal to 0.5 indicates that the variable cutoff value is no better than random chance at discriminating between injured and noninjured athletes, whereas a value equal to 1 represents a test with perfect discrimination accuracy. AUCs >0.70 are generally classified as “good” predictors of injury.33,38 The sensitivity of the curve ranks the ability of the variable cutoff value to correctly identify injured athletes, whereas the specificity identifies the ability of the cutoff value to correctly identify uninjured athletes.1 To determine the optimal cutoff point discriminating between injured and uninjured athletes, the maximum vertical distance between the ROC curve and the bisecting line was chosen to maximize sensitivity and specificity, per the Youden index method.43 P values <.05 were considered significant.
Results
Player Characteristics
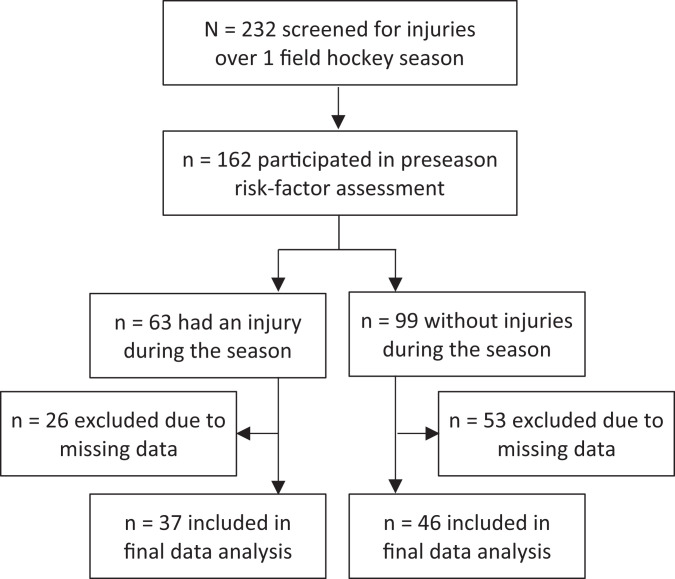
A total of 232 athletes from 14 teams agreed to participate in the study, and 162 completed at least 1 risk factor assessment at baseline (Figure 1). The 83 players with complete injury and risk factor data were included in the final analysis (mean ± SD age, 20.73 ± 4.94 years; 34.9% female) (Tables 1 and 2). About half of the players (n = 37; 44.6%) were injured at some point throughout the hockey season. Of these, 27 players (32.5%) sustained injuries in the lower limb (totalling 73% of all injuries).
Figure 1.
Flowchart of study participants from recruitment through injury screening.
Table 1.
Player Characteristics and Exposure Dataa
| All Injuries | Lower Limb Injuries | ||||
|---|---|---|---|---|---|
| All Players | Injured Players | Noninjured Players | Injured Players | Noninjured Players | |
| Sample size | 83 | 37 (44.6) | 46 (55.4) | 27 (32.5) | 56 (67.5) |
| Players by division | |||||
| First (Bundesliga) | 41 | 23 (56.1) | 18 (43.9) | 14 (34.1) | 27 (65.9) |
| Second (2. Bundesliga) | 7 | 2 (28.6) | 5 (71.4) | 2 (28.6) | 5 (71.4) |
| Third (Regionalliga) | 15 | 8 (53.3) | 7 (46.7) | 7 (46.6) | 8 (53.4) |
| Fourth (Verbandsliga) | 6 | 0 (0.0) | 6 (100) | 0 (0.0) | 6 (100) |
| Youth | 14 | 4 (28.6) | 10 (71.4) | 4 (28.6) | 10 (71.4) |
| Playing indoor and field season | 76 (91.6) | 35 (94.6) | 41 (89.1) | 26 (96.2) | 50 (89.3) |
| Player by positionb | |||||
| Defense | 28 (33.7) | 11 (39.4) | 17 (60.6) | 6 (21.4) | 22 (78.6) |
| Midfield | 18 (21.7) | 9 (50) | 9 (50) | 8 (44.4) | 10 (55.6) |
| Striker | 27 (32.5) | 14 (51.9) | 13 (48.1) | 12 (44.4) | 15 (55.6) |
| Goalkeeper | 10 (12.0) | 3 (30) | 7 (70) | 1 (10) | 9 (90) |
| Training per week | |||||
| Sessions | 3.93 ± 2.06 | 4.26 ± 1.98 | 3.67 ± 2.11 | 4.00 ± 1.56 | 3.9 ± 2.27 |
| Minutes | 495.09 ± 216.26 | 548.78 ± 260.70 | 451.90 ± 256.38 | 528.52 ± 233.43 | 478.97 ± 274.22 |
| Games playedb | 50.08 ± 21.63 | 60.16 ± 20.75 | 41.98 ± 18.91 | 57.37 ± 21.35 | 46.57 ± 21.06 |
| Sex | |||||
| Female | 29 (34.9) | 10 (34.5) | 19 (65.5) | 7 (34.5) | 22 (65.5) |
| Male | 54 (65.10) | 27 (50) | 27 (50) | 20 (37) | 34 (63) |
| Age, yb | 20.73 ± 4.94 | 21.68 ± 5.41 | 19.68 ± 4.44 | 21.30 ± 5.77 | 20.46 ± 4.51 |
| Height, cm | 176.61 ± 8.89 | 177.24 ± 8.25 | 176.11 ± 9.43 | 177.6 ± 7.76 | 176.14 ± 9.41 |
| Weight, kg | 71.47 ± 11.06 | 72.99 ± 8.95 | 70.25 ± 12.47 | 72.54 ± 9.95 | 70.96 ± 11.61 |
aData are presented as raw total (percentage of total player population) or group mean ± SD. bVariable identified by the least absolute shrinkage and selection operator model as being relevant for injury occurrence.
Table 2.
Neuromuscular Control and Performance Variablesa
| All Injuries | Lower Limb Injuries | ||||
|---|---|---|---|---|---|
| All Players (N = 83) | Injured Players (n = 37) | Noninjured Players (n = 46) | Injured Players (n = 27) | Noninjured Players (n = 56) | |
| Sit-and-reach test, cm | 8.31 ± 10.42 | 8.85 ± 12.97 | 7.88 ± 8.04 | 9.1 ± 14.6 | 7.93 ± 7.68 |
| Ankle flexibility, cmb | 12.37 ± 2.83 | 12.06 ± 2.72 | 12.61 ± 2.93 | 11.85 ± 2.78 | 12.62 ± 2.85 |
| Ankle flexibility asymmetry, cm | 1.64 ± 1.29 | 1.52 ± 1.25 | 1.73 ± 1.33 | 1.49 ± 1.32 | 1.78 ± 1.28 |
| Leg-length difference, cm | 0.55 ± 0.75 | 0.53 ± 0.72 | 0.56 ± 0.78 | 0.45 ± 0.59 | 0.59 ± 0.81 |
| SEBTb | |||||
| Anterior | 94.00 ± 8.44 | 93.96 ± 7.04 | 94.04 ± 9.49 | 93.29 ± 6.53 | 94.35 ± 9.26 |
| Anteromedial | 78.93 ± 9.64 | 77.46 ± 7.66 | 80.12 ± 10.91 | 77.49 ± 7.02 | 79.63 ± 10.66 |
| Anterolateral | 91.24 ± 7.90 | 90.84 ± 7.28 | 90.62 ± 7.27 | 90.04 ± 7.59 | 90.75 ± 7.36 |
| Posterior | 86.40 ± 7.38 | 85.27 ± 6.75 | 87.32 ± 7.81 | 84.84 ± 6.97 | 87.16 ± 7.52 |
| Posteromedialc | 81.51 ± 7.55 | 79.71 ± 6.34 | 82.96 ± 8.36 | 78.78 ± 6.32 | 82.83 ± 7.94 |
| Posterolateral | 87.75 ± 7.18 | 86.53 ± 6.38 | 88.74 ± 7.69 | 85.96 ± 6.41 | 88.62 ± 7.42 |
| SEBT asymmetry, cm | |||||
| Anterior | 4.2 ± 3.11 | 4.09 ± 2.74 | 4.39 ± 3.40 | 3.9 ± 2.65 | 4.35 ± 3.32 |
| Anteromedial | 4.93 ± 4.31 | 5.53 ± 4.07 | 4.45 ± 4.08 | 5.06 ± 3.92 | 4.87 ± 4.52 |
| Anterolateralc | 3.68 ± 3.70 | 3.87 ± 4.42 | 3.52 ± 3.03 | 4.44 ± 4.74 | 3.31 ± 3.06 |
| Posterior | 3.62 ± 3.03 | 4.03 ± 3.04 | 3.30 ± 3.02 | 4.06 ± 2.90 | 3.41 ± 3.1 |
| Posteromedial | 4.66 ± 4.09 | 4.58 ± 3.82 | 4.72 ± 4.33 | 4.39 ± 4.18 | 4.97 ± 4.07 |
| Posterolateralc | 3.88 ± 4.02 | 4.61 ± 4.57 | 3.29 ± 3.46 | 5.09 ± 5.19 | 3.30 ± 3.22 |
| Countermovement jump height, cmc | 39.70 ± 5.96 | 41.45 ± 5.90 | 38.61 ± 5.77 | 42.02 ± 6.02 | 38.81 ± 5.76 |
| Drop-jump ground-reaction time, msc | 204.64 ± 40.37 | 197.41 ± 36.96 | 210.46 ± 42.42 | 197.9 ± 38.38 | 207.89 ± 41.24 |
| Sprint time, s | |||||
| 0-5 m | 0.99 ± 0.08 | 0.98 ± 0.07 | 1.00 ± 0.08 | 0.99 ± 0.07 | 0.99 ± 0.09 |
| 0-10 m | 1.74 ± 0.15 | 1.71 ± 0.16 | 1.77 ± 0.13 | 1.73 ± 0.12 | 1.75 ± 0.16 |
| 0-30 mc | 4.40 ± 0.36 | 4.30 ± 0.46 | 4.48 ± 0.33 | 4.32 ± 0.34 | 4.44 ± 0.36 |
| Agility, s | 6.10 ± 0.47 | 6.08 ± 0.42 | 6.11 ± 0.51 | 6.05 ± 0.46 | 6.12 ± 0.48 |
aData are presented as mean ± SD. SEBT, Star Excursion Balance Test.
bMean of the left and right legs.
cVariable identified by the least absolute shrinkage and selection operator model as being relevant for injury occurrence.
Risk Factor Analysis
All Injuries
LASSO regression analysis revealed that more games played ( = 0.0286), older age ( = 0.0066), a lower SEBT posteromedial distance ( = –0.0272), a greater SEBT posterolateral asymmetry ( = 0.0047), a higher countermovement jump height ( = 0.0571), a lower drop-jump ground-reaction time ( = –0.0006), and a faster 30-m sprint time ( = –0.0004) were all relevant for injury occurrence. No other measured variables were identified as being associated with general injury risk.
Lower Limb Injuries
LASSO regression analysis identified that midfielders were more likely to sustain a lower limb injury than were defenders ( = 0.2665) and goalkeepers were less likely to sustain an injury than were defenders ( = –0.1214). More games played ( = 0.0103), lower SEBT posteromedial score ( = 0.0445), greater asymmetries on the SEBT in the anterolateral ( = 0.0077) and posterolateral ( = 0.0181) directions, and higher countermovement jump height ( = 0.0625) were associated with lower limb injuries during the subsequent hockey season. No other measured variables were detected as being relevant for lower limb injury occurrence.
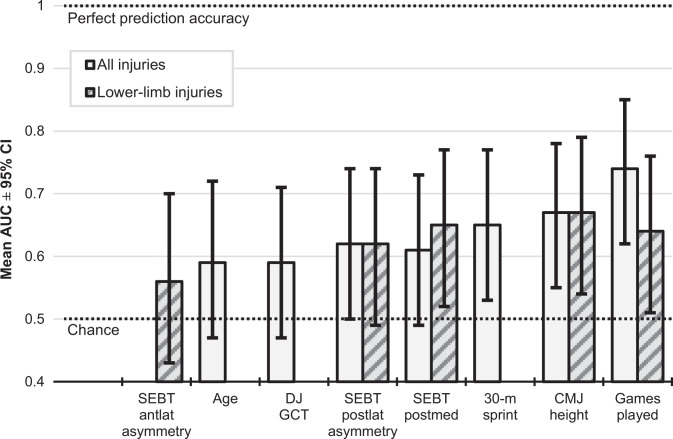
Discriminative Accuracy of Individual Injury Predictors
ROC curve analyses for the individual variables selected by the LASSO model are detailed in Table 3 (all injuries), Table 4 (lower limb injuries), and Figure 2.
Table 3.
Discriminative Accuracy of Each Variable/Category for Predicting All Injuries in Hockey Determined Using Receiver Operating Characteristic Curvesa
| Predictor Variable | Cutoff Value | AUCb (95% CI) | Sensitivity, % | Specificity, % | P Valuec |
|---|---|---|---|---|---|
| No. of games | 43.5 | 0.74 (0.63-0.85) | 83.8 | 56.5 | <.001 |
| Age, y | 18.5 | 0.59 (0.47-0.72) | 70.3 | 47.8 | .072 |
| SEBT posteromedial, cm | 86.1 | 0.61 (0.49-0.73) | 86.5 | 32.6 | .043 |
| SEBT asymmetry: posterolateral, cm | 2.9 | 0.62 (0.50-0.74) | 67.6 | 56.5 | .031 |
| Countermovement jump height, cm | 40.6 | 0.67 (0.55-0.79) | 67.6 | 67.4 | .003 |
| Drop-jump ground-reaction time, ms | 213.8 | 0.59 (0.47-0.72) | 78.4 | 45.6 | .063 |
| 30-m sprint time, s | 4.3 | 0.65 (0.53-0.77) | 54.1 | 76.1 | .008 |
aAUC, area under the curve; SEBT, Star Excursion Balance Test.
bAUC scores range from 0 (no accuracy) to 1 (perfect accuracy).
cBold P values indicate statistical significance (P < .05).
Table 4.
Discriminative Accuracy of Each Variable/Category for Predicting Lower Limb Injuries in Hockey Determined Using Receiver Operating Characteristic Curvesa
| Predictor Variable | Cutoff Value | AUC (95% CI)b | Sensitivity, % | Specificity, % | P Valuec |
|---|---|---|---|---|---|
| No. of games | 38.5 | 0.64 (0.51-0.76) | 88.9 | 37.5 | .022 |
| SEBT posteromedial, cm | 87.3 | 0.65 (0.53-0.77) | 96.3 | 28.6 | .014 |
| SEBT asymmetry, cm | |||||
| Anterolateral | 10.2 | 0.56 (0.43-0.70) | 18.5 | 98.2 | .178 |
| Posterolateral | 3.5 | 0.62 (0.49-0.76) | 55.6 | 66.1 | .037 |
| Countermovement jump height, cm | 42.2 | 0.67 (0.54-0.79) | 59.3 | 71.4 | .008 |
aAUC, area under the curve; SEBT, Star Excursion Balance Test.
bAUC scores range from 0 (no accuracy) to 1 (perfect accuracy).
cBold P values indicate statistical significance (P < .05).
Figure 2.
Area under the curve (AUC) results from the receiver operating characteristic curve analysis performed on variables selected via the least absolute shrinkage and selection operator models. Error bars represent 95% CI. antlat, anterolateral; CMJ, countermovement jump; DJ GCT, drop-jump ground contact time; postlat, posterolateral; postmed, posteromedial; SEBT, Star Excursion Balance Test.
Discussion
This is the first study to utilize a comprehensive suite of player characteristics, exposure, and neuromuscular performance measures to identify factors associated with the risk of injury in field hockey players across a full indoor and outdoor season. Key factors identified as being relevant predictors of general and lower limb injury occurrence included a greater exposure (number of games), asymmetrical and poor dynamic postural control in the posterior directions, and better explosive athletic performance. Furthermore, midfielders were more likely to sustain a lower limb injury than were defenders, while goalkeepers were less likely. Importantly, these risk factors combine to jointly affect the injury risk in an integrated manner, as demonstrated via LASSO regression analysis. Despite most selected variables being poorly to moderately predictive of injury when assessed in isolation via ROC curve analyses, discussion of each identified factor is warranted to inform targeted injury risk mitigation strategies.
Player Characteristics Associated With Injury Risk
Age is a particularly well-established injury risk factor, and it appears to influence most types of noncontact injury in team sports.16,56 However, age was among the poorest individual predictors of general injury identified by our model (AUC = 0.59) and was not associated with lower limb injuries. Furthermore, our age cutoff value of 18.5 years, which was not statistically significant, is low compared with that reported in research citing elevated hamstring injury risk in football in ages >23 years.60 Therefore, age may be relevant for field hockey injury prediction only when considered alongside other risk factors.
The observed difference in lower limb injury risk among field hockey positions may be due to the inherent differences in position requirements, as reported in other team sports.6,34 While protective equipment is expected to diminish injury risk in goalkeepers, it has also been suggested that the unique locomotive demands of each position could influence the risk of injury. Global positioning system analyses have revealed that hockey midfielders cover more total distance than do other position players,39 forwards typically play fewer game minutes than do midfielders,57 and defenders spend less time in high-velocity running zones and reach lower peak velocities than do other outfield players.28,39 Combined, this may explain why field hockey midfielders are at an increased risk of lower limb injury over defenders, given that related elements of running exposure are associated with hamstring injury risk, for example.47 These observations are in general agreement with our finding that certain elements of exposure were associated with injury risk in field hockey players.
Exposure Variables Associated With Injury Risk
Our model recognized game exposure as the strongest predictor of general injury, with the cutoff value of 43.5 games successfully identifying 83.8% of injured athletes. Players participating in >38.5 games were also at an increased risk of sustaining a lower limb injury. These findings support evidence that injury risk in other team sports (eg, rugby union) increases linearly with games played and that athletes playing >28 games per season are at an especially elevated risk of sustaining an injury.59 The identification of game exposure as an injury risk factor is perhaps not surprising, considering observations that injury rates are considerably higher in games than they are during training in team sports.12,24,30 However, it is not simply the volume of exposure that is important but also the context of the exposure including factors such as the type and rate of exposure.17,35,36 This partially explains why periods of game congestion amplify injury rates in field hockey.52 The interaction between the short- and longer-term workloads may be a particularly important mediator of the exposure-injury relationship, and rapid spikes in exposure combined with chronic training loads that are too low or too high have been reported to increase the risk of injury.8,11,17 However, no relationship between training exposure variables and injury risk in field hockey players was detected in our study.
Neuromuscular Performance Variables Associated With Injury Risk
Poor performance in multiple directions of the SEBT was associated with an increased injury risk during the hockey season, which supports the hypothesis that generally poor or asymmetrical dynamic postural control increases injury risk.44,50,51 However, while research has suggested that asymmetry in the anterior directions of the SEBT is the most relevant predictor of injury,44,50 our results indicated that anterolateral asymmetry was marginally more likely to predict a lower limb injury than chance (AUC = 0.56), and our cutoff value did not reach statistical significance. Instead, we observed that posterolateral asymmetries >3.5 cm (AUC = 0.62) and >2.9 cm (AUC = 0.62) better predicted injury risk for general and lower limb injuries, respectively, and that poor absolute posteromedial SEBT performance was predictive of general (AUC = 0.61) and lower limb (AUC = 0.65) injury occurrence. However, the predictive accuracy of our results is poor when compared with that of other studies reporting AUC values >0.82 with a sensitivity of 88% and a specificity of 67%.50 There is evidence that SEBT performance is sport specific,51 so our novel findings regarding the posterior directions of the SEBT may reflect the unique mechanics and postures associated with hockey locomotion and skill execution.58
We also observed that superior preseason performance on a series of explosive tasks increased the risk of injury during the field hockey season. This could be considered paradoxical in light of findings that well-developed physical capacities, including sprint speed, may be protective against injury.17,35 However, our finding that faster 30-m sprint time was a risk factor for general injury is supported by links between faster sprint capacity and an increased likelihood of groin injury in amateur footballers13 and general injury in elite junior Australian footballers.7 The countermovement jump performance was one of the strongest predictors of injury in our study. Although research on the countermovement jump as a predictor of injury risk in team sports is limited, there is some precedent for lower injury rates being linked with lower vertical jump performance.7,18 Ground contact times during depth jumps are also rarely reported in team sports injury risk factor research, meaning that our finding that better depth jump ground contact times may increase general injury risk is novel. This should, however, be interpreted with caution. Although the LASSO model identified it as being relevant for injury risk, the cutoff value identified was not statistically significant.
Limitations
Because of a complex and multifactorial nature, injury risk research typically has moderate to poor predictive accuracy,3,46 and our study was not immune to this issue. Despite the use of a broad range of potential risk factors, an advanced multivariate regression model to identify relevant predictors, and predictive statistical methods, our results confirmed the limited predictive accuracy of individual injury risk factor analysis, with a mean selected variable AUC of 0.63. A major strength, however, was the LASSO regression, which enabled a thorough and multivariate risk factor analysis for injury risk. Among the limitations specific to our study was using only 1 preseason time point for neuromuscular testing, which neglected to address the temporal dynamics of risk factors. The general categorization of injuries also did not take into account the role of injury mechanism and type—for example, contact versus noncontact injuries and hamstring versus ankle sprain, which are likely to have different risk factors. This general classification of injuries may partially explain a lack of strong association with well-validated injury risk factors such as age and previous injury, as these are unlikely to heavily mediate the incidence of contact injuries, for instance. Last, the crude measures of training exposure in this study did not take into account additional factors that may influence injury risk such as load intensity and changes in load over time. Combined, these factors may have limited the predictive capacity of our observations.
Practical Recommendations
Despite well-documented limitations, the widespread use and perceived success of injury risk screening and injury prevention programs at the elite level in team sports are encouraging.42 When skilled and informed practitioners are armed with well-designed risk factor screening, they can combine it with their intimate knowledge of the sports-specific context of these results, including previous and upcoming exposures. This allows them to make informed individual player availability and training design decisions that may mitigate the risk of injury and ultimately maximize team performance.
Based on the results of the current study, neuromuscular training programs for injury risk mitigation in field hockey should target asymmetries and poor performance in posterior directions of dynamic postural control. Furthermore, despite the observations in this study, concerns regarding the injury risk of explosive performance improvement should be balanced against the need to maximize performance. In team sports involving high-intensity intermittent activity such as field hockey, improvements in jump and sprint performance should be considered in harmony with similar improvements in protective capacities, such as eccentric strength and aerobic capacity,36,42 and implemented as part of carefully considered exposures to mitigate the risk of injury. As injury is linked with sprint speed and game exposure, training should also be designed with sufficient dosages of high-velocity running and chronic load, the combination of which is purported to minimize injury risk.35,36 Finally, this study demonstrated that LASSO analysis is a valuable tool in assessing injury risk in team sports, with the potential to identify overall injury risk based on the combination of individual factors assessed via athlete screening. Future studies should utilize multiple time points for neuromuscular testing and use more sensitive measures of game and training exposure to elucidate the factors contributing to the risk of injury in field hockey players.
Conclusion
The results of this study provide the first evidence of factors associated with injury occurrence during a 12-month indoor and outdoor hockey season. Multiple risk factors jointly affected the risk of injury in an integrated manner. Although individual risk factors aside from game exposure were not strongly predictive of injury risk, a number of moderate associations between individual risk factors and injury were detected, with implications for the design of injury risk mitigation strategies in field hockey players.
Acknowledgment
The authors thank the Hamburg Hockey Association and all teams for their participation in the study.
Footnotes
Final revision submitted November 23, 2020; accepted January 5, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the German Federal Institute for Sport Science. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hamburg Medical Association (protocol PV4893).
References
- 1. Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644–647. [DOI] [PubMed] [Google Scholar]
- 2. Ayala F, de Baranda PS, Croix MD, Santonja F. Absolute reliability of five clinical tests for assessing hamstring flexibility in professional futsal players. J Sci Med Sport. 2012;15(2):142–147. [DOI] [PubMed] [Google Scholar]
- 3. Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review. Br J Sports Med. 2016;50(13):776–780. [DOI] [PubMed] [Google Scholar]
- 4. Bennell K, Talbot R, Wajswelner H, Techovanich W, Kelly D, Hall AJ. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44(3):175–180. [DOI] [PubMed] [Google Scholar]
- 5. Carling C, Le Gall F, McCall A, Nédélec M, Dupont G. Squad management, injury and match performance in a professional soccer team over a championship-winning season. Eur J Sport Sci. 2015;15(7):573–582. [DOI] [PubMed] [Google Scholar]
- 6. Carling C, Orhant E, LeGall F. Match injuries in professional soccer: inter-seasonal variation and effects of competition type, match congestion and positional role. Int J Sports Med. 2010;31(4):271–276. [DOI] [PubMed] [Google Scholar]
- 7. Chalmers S, Magarey ME, Esterman A, Speechley M, Scase E, Heynen M. The relationship between pre-season fitness testing and injury in elite junior Australian football players. J Sci Med Sport. 2013;16(4):307–311. [DOI] [PubMed] [Google Scholar]
- 8. Colby MJ, Dawson B, Peeling P, et al. Multivariate modelling of subjective and objective monitoring data improve the detection of non-contact injury risk in elite Australian footballers. J Sci Med Sport. 2017;20(12):1068–1074. [DOI] [PubMed] [Google Scholar]
- 9. Dick R, Hootman JM, Agel J, et al. Descriptive epidemiology of collegiate women’s field hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2002-2003. J Athl Train. 2007;42:211–220. [PMC free article] [PubMed] [Google Scholar]
- 10. Drew MK, Raysmith BP, Charlton PC. Injuries impair the chance of successful performance by sportspeople: a systematic review. Br J Sports Med. 2017;51(16):1209–1214. [DOI] [PubMed] [Google Scholar]
- 11. Eckard TG, Padua DA, Hearn DW, Pexa BS, Frank BS. The relationship between training load and injury in athletes: a systematic review. Sports Med. 2018;48(8):1929–1961. [DOI] [PubMed] [Google Scholar]
- 12. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 13. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for groin injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38(10):2051–2057. [DOI] [PubMed] [Google Scholar]
- 14. Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1. [PMC free article] [PubMed] [Google Scholar]
- 15. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med. 2006;40:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gabbe BJ, Bennell KL, Finch CF. Why are older Australian football players at greater risk of hamstring injury? J Sci Med Sport. 2006;9(4):327–333. [DOI] [PubMed] [Google Scholar]
- 17. Gabbett TJ. The training—injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50(5):273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gómez-Piqueras P, González-Víllora S, de Baranda Andújar S, Del Pilar M, Contreras-Jordán OR. Functional assessment and injury risk in a professional soccer team. Sports. 2017;5(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321. [PMC free article] [PubMed] [Google Scholar]
- 20. Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hägglund M, Waldén M, Ekstrand J. Risk factors for lower extremity muscle injury in professional soccer: the UEFA Injury Study. Am J Sports Med. 2013;41(2):327–335. [DOI] [PubMed] [Google Scholar]
- 22. Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):738–742. [DOI] [PubMed] [Google Scholar]
- 23. Hertel J, Miller S, Denegar C. Intratester and intertester reliability during the Star Excursion Balance Test. J Sport Rehabil. 2000;9:104–116. [Google Scholar]
- 24. Hoffman DT, Dwyer DB, Tran J, Clifton P, Gastin PB. Australian Football League injury characteristics differ between matches and training: a longitudinal analysis of changes in the setting, site, and time span from 1997 to 2016. Orthop J Sports Med. 2019;7(4):2325967119837641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hollander K, Wellmann K, zu Eulenburg C, Braumann KM, Junge A, Zech A. Epidemiology of injuries in outdoor and indoor hockey players over one season: a prospective cohort study. Br J Sports Med. 2018;52(17):1091–1096. [DOI] [PubMed] [Google Scholar]
- 26. Junge A, Engebretsen L, Mountjoy ML, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med. 2009;37:2165–2172. [DOI] [PubMed] [Google Scholar]
- 27. Kobayashi T, Tanaka M, Shida M. Intrinsic risk factors of lateral ankle sprain: a systematic review and meta-analysis. Sports Health. 2016;8(2):190–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Liu H, Zhao G, Gómez AM, Molinuevo SJ, Giménez JV, Kang H. Time-motion analysis on Chinese male field hockey players. Int J Perform Anal Sport. 2013;13(2):340–352. [Google Scholar]
- 29. Lockie RG, Schultz AB, Callaghan SJ, Jeffriess MD, Berry SP. Reliability and validity of a new test of change-of-direction speed for field-based sports: the Change-of-Direction and Acceleration Test (CODAT). J Sports Sci Med. 2013;12(1):88. [PMC free article] [PubMed] [Google Scholar]
- 30. López-Valenciano A, Ruiz-Pérez I, Garcia-Gómez A, et al. Epidemiology of injuries in professional football: a systematic review and meta-analysis. Br J Sports Med. 2020;54(12):711–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. MacDonald K, Bahr R, Baltich J, Whittaker JL, Meeuwisse WH. Validation of an inertial measurement unit for the measurement of jump count and height. Phys Ther Sport. 2017;25:15–19. [DOI] [PubMed] [Google Scholar]
- 32. McCall A, Dupont G, Ekstrand J. Injury prevention strategies, coach compliance and player adherence of 33 of the UEFA Elite Club Injury Study teams: a survey of teams’ head medical officers. Br J Sports Med. 2016;50(12):725–730. [DOI] [PubMed] [Google Scholar]
- 33. McCall A, Dupont G, Ekstrand J. Internal workload and non-contact injury: a one-season study of five teams from the UEFA Elite Club Injury Study. Br J Sports Med. 2018;52(23):1517–1522. [DOI] [PubMed] [Google Scholar]
- 34. Mallo J, Dellal A. Injury risk in professional football players with special reference to the playing position and training periodization. J Sports Med Phys Fitness. 2012;52(6):631–638. [PubMed] [Google Scholar]
- 35. Malone S, Hughes B, Doran DA, Collins K, Gabbett TJ. Can the workload-injury relationship be moderated by improved strength, speed and repeated-sprint qualities? J Sci Med Sport. 2019;22(1):29–34. [DOI] [PubMed] [Google Scholar]
- 36. Malone S, Roe M, Doran DA, Gabbett TJ, Collins KD. Aerobic fitness and playing experience protect against spikes in workload: the role of the acute:chronic workload ratio on injury risk in elite Gaelic football. Int J Sports Physiol Perform. 2016;12(3):393–401. [DOI] [PubMed] [Google Scholar]
- 37. Meeuwisse WH, Tyreman H, Hagel B, Emery C. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215–219. [DOI] [PubMed] [Google Scholar]
- 38. Menaspà P, Sassi A, Impellizzeri FM. Aerobic fitness variables do not predict the professional career of young cyclists. Med Sci Sports Exerc. 2010;42(4):805–812. [DOI] [PubMed] [Google Scholar]
- 39. Morencos E, Romero-Moraleda B, Castagna C, Casamichana D. Positional comparisons in the impact of fatigue on movement patterns in hockey. Int J Sports Physiol Perform. 2018;13(9):1149–1157. [DOI] [PubMed] [Google Scholar]
- 40. Murtaugh K. Field hockey injuries. Curr Sports Med Rep. 2009;8:267–272. [DOI] [PubMed] [Google Scholar]
- 41. Murtaugh K. Injury patterns among female field hockey players. Med Sci Sports Exerc. 2001;33(2):201–207. [DOI] [PubMed] [Google Scholar]
- 42. Opar D, Williams M, Timmins R, Hickey J, Duhig S, Shield A. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med Sci Sports Exerc. 2015;47(4):857–865. [DOI] [PubMed] [Google Scholar]
- 43. Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006;163(7):670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. [DOI] [PubMed] [Google Scholar]
- 45. Powden CJ, Hoch JM, Hoch MC. Reliability and minimal detectable change of the weight-bearing lunge test: a systematic review. Man Ther. 2015;20(4):524–532. [DOI] [PubMed] [Google Scholar]
- 46. Ruddy JD, Cormack SJ, Whiteley R, Williams MD, Timmins RG, Opar DA. Modeling the risk of team sport injuries: a narrative review of different statistical approaches. Front Physiol. 2019;10:829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Small K, McNaughton LR, Greig M, Lohkamp M, Lovell R. Soccer fatigue, sprinting and hamstring injury risk. Int J Sports Med. 2009;30(08):573–578. [DOI] [PubMed] [Google Scholar]
- 48. Soligard T, Steffen K, Palmer D, et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: a prospective study of 11274 athletes from 207 countries. Br J Sports Med. 2017;51(17):1265–1271. [DOI] [PubMed] [Google Scholar]
- 49. Steib S, Rahlf AL, Pfeifer K, Zech A. Dose-response relationship of neuromuscular training for injury prevention in youth athletes: a meta-analysis. Front Physiol. 2017;14(8):920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Stiffler MR, Bell DR, Sanfilippo JL, Hetzel SJ, Pickett KA, Heiderscheit BC. Star Excursion Balance Test anterior asymmetry is associated with injury status in Division I collegiate athletes. J Orthop Sports Phys Ther. 2017;47(5):339–346. [DOI] [PubMed] [Google Scholar]
- 51. Stiffler MR, Sanfilippo JL, Brooks MA, Heiderscheit BC. Star Excursion Balance Test performance varies by sport in healthy Division I collegiate athletes. J Orthop Sports Phys Ther. 2015;45(10):772–780. [DOI] [PubMed] [Google Scholar]
- 52. Theilen TM, Mueller-Eising W, Bettink PW, Rolle U. Injury data of major international field hockey tournaments. Br J Sports Med. 2016;50(11):657–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Theisen D, Frisch A, Malisoux L, Urhausen A, Croisier JL, Seil R. Injury risk is different in team and individual youth sport. J Sci Med Sport. 2013;16(3):200–204. [DOI] [PubMed] [Google Scholar]
- 54. Tibshirani R. Regression shrinkage and selection via the LASSO. J R Stat Soc Series B. 1996;58(1):267–288. [Google Scholar]
- 55. Van Beijsterveldt AM, van de Port IG, Vereijken AJ, Backx FJ. Risk factors for hamstring injuries in male soccer players: a systematic review of prospective studies. Scand J Med Sci Sports. 2013;23(3):253–262. [DOI] [PubMed] [Google Scholar]
- 56. van Dyk N, Bahr R, Burnett AF, et al. A comprehensive strength testing protocol offers no clinical value in predicting risk of hamstring injury: a prospective cohort study of 413 professional football players. Br J Sports Med. 2017;51(23):1695–1702. [DOI] [PubMed] [Google Scholar]
- 57. Vescovi JD, Frayne DH. Motion characteristics of Division I college field hockey: Female Athletes in Motion (FAiM) study. Int J Sports Physiol Perform. 2015;10(4):476–481. [DOI] [PubMed] [Google Scholar]
- 58. Wdowski MM, Gittoes MJ. Kinematic adaptations in sprint acceleration performances without and with the constraint of holding a field hockey stick. Sports Biomech. 2013;12(2):143–153. [DOI] [PubMed] [Google Scholar]
- 59. Williams S, Trewartha G, Kemp SP, et al. How much rugby is too much? A seven-season prospective cohort study of match exposure and injury risk in professional rugby union players. Sports Med. 2017;47(11):2395–2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of hamstring injuries. Br J Sports Med. 2004;38(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]